Acute Pain - final version - Faculty of pain medicine - Australian and ...
Acute Pain - final version - Faculty of pain medicine - Australian and ...
Acute Pain - final version - Faculty of pain medicine - Australian and ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<br />
<br />
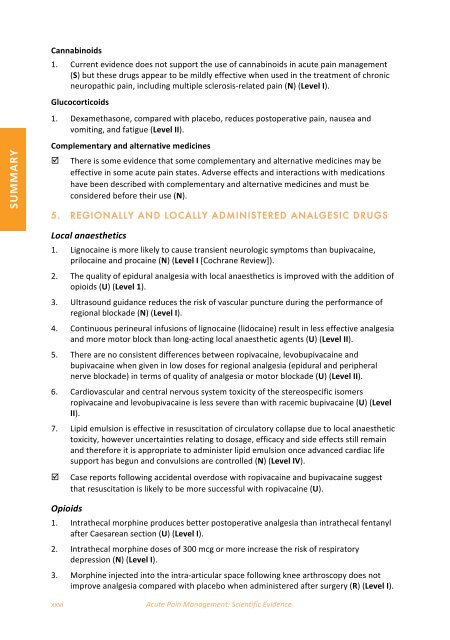
SUMMARY <br />
Cannabinoids <br />
1. Current evidence does not support the use <strong>of</strong> cannabinoids in acute <strong>pain</strong> management <br />
(S) but these drugs appear to be mildly effective when used in the treatment <strong>of</strong> chronic <br />
neuropathic <strong>pain</strong>, including multiple sclerosis‐related <strong>pain</strong> (N) (Level I). <br />
Glucocorticoids <br />
1. Dexamethasone, compared with placebo, reduces postoperative <strong>pain</strong>, nausea <strong>and</strong> <br />
vomiting, <strong>and</strong> fatigue (Level II). <br />
Complementary <strong>and</strong> alternative <strong>medicine</strong>s <br />
<br />
There is some evidence that some complementary <strong>and</strong> alternative <strong>medicine</strong>s may be <br />
effective in some acute <strong>pain</strong> states. Adverse effects <strong>and</strong> interactions with medications <br />
have been described with complementary <strong>and</strong> alternative <strong>medicine</strong>s <strong>and</strong> must be <br />
considered before their use (N). <br />
5. REGIONALLY AND LOCALLY ADMINISTERED ANALGESIC DRUGS<br />
Local anaesthetics <br />
1. Lignocaine is more likely to cause transient neurologic symptoms than bupivacaine, <br />
prilocaine <strong>and</strong> procaine (N) (Level I [Cochrane Review]). <br />
2. The quality <strong>of</strong> epidural analgesia with local anaesthetics is improved with the addition <strong>of</strong> <br />
opioids (U) (Level 1). <br />
3. Ultrasound guidance reduces the risk <strong>of</strong> vascular puncture during the performance <strong>of</strong> <br />
regional blockade (N) (Level I). <br />
4. Continuous perineural infusions <strong>of</strong> lignocaine (lidocaine) result in less effective analgesia <br />
<strong>and</strong> more motor block than long‐acting local anaesthetic agents (U) (Level II). <br />
5. There are no consistent differences between ropivacaine, levobupivacaine <strong>and</strong> <br />
bupivacaine when given in low doses for regional analgesia (epidural <strong>and</strong> peripheral <br />
nerve blockade) in terms <strong>of</strong> quality <strong>of</strong> analgesia or motor blockade (U) (Level II). <br />
6. Cardiovascular <strong>and</strong> central nervous system toxicity <strong>of</strong> the stereospecific isomers <br />
ropivacaine <strong>and</strong> levobupivacaine is less severe than with racemic bupivacaine (U) (Level <br />
II). <br />
7. Lipid emulsion is effective in resuscitation <strong>of</strong> circulatory collapse due to local anaesthetic <br />
toxicity, however uncertainties relating to dosage, efficacy <strong>and</strong> side effects still remain <br />
<strong>and</strong> therefore it is appropriate to administer lipid emulsion once advanced cardiac life <br />
support has begun <strong>and</strong> convulsions are controlled (N) (Level IV). <br />
<br />
Opioids <br />
Case reports following accidental overdose with ropivacaine <strong>and</strong> bupivacaine suggest <br />
that resuscitation is likely to be more successful with ropivacaine (U). <br />
1. Intrathecal morphine produces better postoperative analgesia than intrathecal fentanyl <br />
after Caesarean section (U) (Level I). <br />
2. Intrathecal morphine doses <strong>of</strong> 300 mcg or more increase the risk <strong>of</strong> respiratory <br />
depression (N) (Level I). <br />
3. Morphine injected into the intra‐articular space following knee arthroscopy does not <br />
improve analgesia compared with placebo when administered after surgery (R) (Level I). <br />
xxvi <br />
<strong>Acute</strong> <strong>Pain</strong> Management: Scientific Evidence