Acute Pain - final version - Faculty of pain medicine - Australian and ...
Acute Pain - final version - Faculty of pain medicine - Australian and ...
Acute Pain - final version - Faculty of pain medicine - Australian and ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<br />
<br />
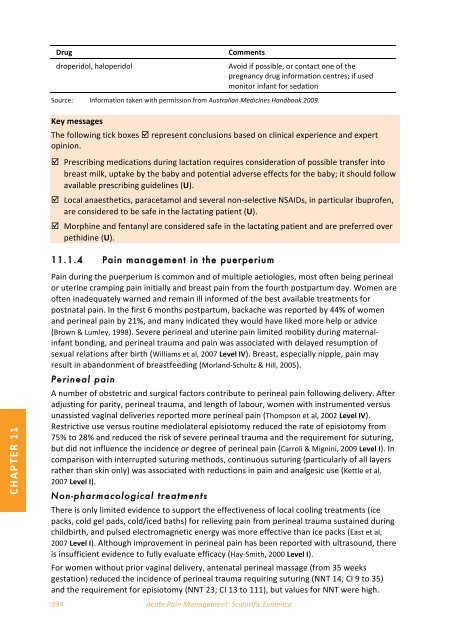
Drug <br />
droperidol, haloperidol <br />
Source: <br />
Key messages <br />
Comments <br />
Avoid if possible, or contact one <strong>of</strong> the <br />
pregnancy drug information centres; if used <br />
monitor infant for sedation <br />
Information taken with permission from <strong>Australian</strong> Medicines H<strong>and</strong>book 2009. <br />
The following tick boxes represent conclusions based on clinical experience <strong>and</strong> expert <br />
opinion. <br />
Prescribing medications during lactation requires consideration <strong>of</strong> possible transfer into <br />
breast milk, uptake by the baby <strong>and</strong> potential adverse effects for the baby; it should follow <br />
available prescribing guidelines (U). <br />
Local anaesthetics, paracetamol <strong>and</strong> several non‐selective NSAIDs, in particular ibupr<strong>of</strong>en, <br />
are considered to be safe in the lactating patient (U). <br />
Morphine <strong>and</strong> fentanyl are considered safe in the lactating patient <strong>and</strong> are preferred over <br />
pethidine (U). <br />
11.1.4 <strong>Pain</strong> management in the puerperium<br />
CHAPTER 11 <br />
<strong>Pain</strong> during the puerperium is common <strong>and</strong> <strong>of</strong> multiple aetiologies, most <strong>of</strong>ten being perineal <br />
or uterine cramping <strong>pain</strong> initially <strong>and</strong> breast <strong>pain</strong> from the fourth postpartum day. Women are <br />
<strong>of</strong>ten inadequately warned <strong>and</strong> remain ill informed <strong>of</strong> the best available treatments for <br />
postnatal <strong>pain</strong>. In the first 6 months postpartum, backache was reported by 44% <strong>of</strong> women <br />
<strong>and</strong> perineal <strong>pain</strong> by 21%, <strong>and</strong> many indicated they would have liked more help or advice <br />
(Brown & Lumley, 1998). Severe perineal <strong>and</strong> uterine <strong>pain</strong> limited mobility during maternalinfant bonding, <strong>and</strong> perineal trauma <strong>and</strong> <strong>pain</strong> was associated with delayed resumption <strong>of</strong> <br />
sexual relations after birth (Williams et al, 2007 Level IV). Breast, especially nipple, <strong>pain</strong> may <br />
result in ab<strong>and</strong>onment <strong>of</strong> breastfeeding (Morl<strong>and</strong>‐Schultz & Hill, 2005). <br />
Perineal <strong>pain</strong><br />
A number <strong>of</strong> obstetric <strong>and</strong> surgical factors contribute to perineal <strong>pain</strong> following delivery. After <br />
adjusting for parity, perineal trauma, <strong>and</strong> length <strong>of</strong> labour, women with instrumented versus <br />
unassisted vaginal deliveries reported more perineal <strong>pain</strong> (Thompson et al, 2002 Level IV). <br />
Restrictive use versus routine mediolateral episiotomy reduced the rate <strong>of</strong> episiotomy from <br />
75% to 28% <strong>and</strong> reduced the risk <strong>of</strong> severe perineal trauma <strong>and</strong> the requirement for suturing, <br />
but did not influence the incidence or degree <strong>of</strong> perineal <strong>pain</strong> (Carroli & Mignini, 2009 Level I). In <br />
comparison with interrupted suturing methods, continuous suturing (particularly <strong>of</strong> all layers <br />
rather than skin only) was associated with reductions in <strong>pain</strong> <strong>and</strong> analgesic use (Kettle et al, <br />
2007 Level I). <br />
Non-pharmacological treatments<br />
There is only limited evidence to support the effectiveness <strong>of</strong> local cooling treatments (ice <br />
packs, cold gel pads, cold/iced baths) for relieving <strong>pain</strong> from perineal trauma sustained during <br />
childbirth, <strong>and</strong> pulsed electromagnetic energy was more effective than ice packs (East et al, <br />
2007 Level I). Although improvement in perineal <strong>pain</strong> has been reported with ultrasound, there <br />
is insufficient evidence to fully evaluate efficacy (Hay‐Smith, 2000 Level I). <br />
For women without prior vaginal delivery, antenatal perineal massage (from 35 weeks <br />
gestation) reduced the incidence <strong>of</strong> perineal trauma requiring suturing (NNT 14; CI 9 to 35) <br />
<strong>and</strong> the requirement for episiotomy (NNT 23; CI 13 to 111), but values for NNT were high. <br />
394 <strong>Acute</strong> <strong>Pain</strong> Management: Scientific Evidence