the BRAIN - Shepherd Center
the BRAIN - Shepherd Center
the BRAIN - Shepherd Center
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
As Seen on TV<br />
<strong>Shepherd</strong>TV.org offers<br />
SpinalColumn<br />
videos on <strong>the</strong> Web.<br />
The Magazine of <strong>Shepherd</strong> <strong>Center</strong>: Providing Medical Treatment, Research and Rehabilitation | www.shepherd.org<br />
New<br />
Voice<br />
Technology restores<br />
communication.<br />
Complex<br />
Cases<br />
<strong>Shepherd</strong> resolves<br />
medical complications.<br />
Patient<br />
Profile<br />
Former patient is<br />
flying <strong>the</strong> skies.<br />
Breathing<br />
Easier<br />
System helps patients<br />
brea<strong>the</strong> on <strong>the</strong>ir own.<br />
Fall 2009<br />
HEALING<br />
<strong>the</strong> <strong>BRAIN</strong><br />
<strong>Shepherd</strong> <strong>Center</strong> brain injury programs<br />
include specialized treatment for young<br />
stroke patients, people in semi-comatose<br />
states and soldiers injured in battle.
Letter from James <strong>Shepherd</strong><br />
Dear Friends,<br />
Photo by Gary Meek<br />
As state and federal governments push for improved and more efficient medical<br />
care for citizens, a trend is emerging among a few leading healthcare facilities,<br />
including <strong>Shepherd</strong> <strong>Center</strong>. It’s a trend toward transparency – specifically, <strong>the</strong><br />
readily available publication of data on patient outcomes and satisfaction at<br />
hospitals and o<strong>the</strong>r medical facilities.<br />
<strong>Shepherd</strong> <strong>Center</strong> has begun publishing this information on its Web site (see<br />
<strong>the</strong> Patient Care section of www.shepherd.org) – updating it quarterly – and<br />
is making it available in printed form (see <strong>the</strong> fold-out attachment on page 21<br />
in this issue of Spinal Column) to referring facilities, case managers, payers, and<br />
patients and <strong>the</strong>ir families. A few o<strong>the</strong>r facilities are publishing this information,<br />
but generally, hospitals have been slow to take this proactive step. The time has<br />
come, however, for healthcare facilities to make this information directly available<br />
to <strong>the</strong>ir customers – not relying solely upon any third party to ga<strong>the</strong>r and publish<br />
it. Our customers deserve <strong>the</strong> opportunity to make good, informed healthcare<br />
decisions based upon solid data.<br />
Organizations that publish <strong>the</strong>ir data on patient outcomes and customer<br />
satisfaction – even if it’s not perfect – convey <strong>the</strong> message that <strong>the</strong>ir institution<br />
is one of integrity and progressive thinking. <strong>Shepherd</strong> <strong>Center</strong>’s data also lets you<br />
see what an excellent job our staff does in caring for patients and meeting <strong>the</strong><br />
needs of <strong>the</strong>ir families, as well. For example, <strong>the</strong> numbers show our low, hospitalacquired<br />
infection rates, which we attribute to our dedicated respiratory <strong>the</strong>rapy<br />
and nursing staffs, as well as rigorous quality control measures. Specifically,<br />
<strong>Shepherd</strong> has been able to sustain a no-infection rate in ventilator-associated<br />
pneumonia for more than a year. That’s practically unheard of among hospitals.<br />
Ano<strong>the</strong>r reason <strong>Shepherd</strong> <strong>Center</strong> excels across <strong>the</strong> data measured is our broad<br />
continuum of care. We are one of <strong>the</strong> few places that can provide true continuity<br />
of care across all levels – from <strong>the</strong> intensive care unit to inpatient and outpatient<br />
rehabilitation <strong>the</strong>rapy to adaptive driver training to <strong>the</strong> community reintegration<br />
assistance provided by our Marcus Community Bridge Program.<br />
As our nation engages in a discussion about healthcare reform, it is our hope<br />
that transparency in patient outcomes and customer satisfaction will become <strong>the</strong><br />
norm among medical facilities. <strong>Shepherd</strong> <strong>Center</strong> is proud to be on <strong>the</strong> leading<br />
edge of this trend, which will ultimately benefit every American faced with<br />
making decisions about where to obtain healthcare services.<br />
Warm regards,<br />
SpinalColumn<br />
T h e m a g a z i n e o f S h e p h e r d C e n t e r<br />
Fa l l 2 0 0 9<br />
<strong>Shepherd</strong> <strong>Center</strong><br />
2020 Peachtree Road, NW<br />
Atlanta, Georgia 30309<br />
404-352-2020<br />
spinalcolumn@shepherd.org<br />
www.spinalcolumn.org<br />
Editor<br />
Jane M. Sanders<br />
Design<br />
Soloflight Design<br />
Contributing Writers<br />
Lauren Angelo, Sara Baxter, Larry<br />
Bowie, Pete Collman, Amanda Crowe,<br />
Kayla Eubanks, Caroline Hemingway,<br />
Dean Melcher, Anne Pearce, Bill<br />
Sanders, Scott Sikes<br />
Contributing Photographers<br />
Leita Cowart, Jim Fitts, Anthony Orig,<br />
Eric Schultz, Gary Meek, Owen Riley<br />
Board of Directors<br />
James H. <strong>Shepherd</strong>, Jr., Chairman<br />
Gary Ulicny, Ph.D., President and CEO<br />
Emory A. Schwall, Vice President<br />
William C. Fowler, Treasurer<br />
Stephen B. Goot, Corporate Secretary<br />
Alana <strong>Shepherd</strong>, Recording Secretary<br />
Members<br />
Fred V. Alias, Gregory P. Anderson,<br />
David F. Apple, Jr., M.D., Brock Bowman,<br />
M.D.*, Wilma Bunch*, James M. Caswell,<br />
Jr., Sara S. Chapman, John S. Dryman,<br />
Mitchell J. Fillhaber*, David H. Flint,<br />
Stephen B. Holleman*, Michael L. Jones,<br />
Ph.D.*, Tammy King*, Donald Peck<br />
Leslie, M.D., Bernie Marcus, Joseph R.<br />
Moderow, Julian B. Mohr, Charles T.<br />
Nunnally III, Sally D. Nunnally, Clyde<br />
<strong>Shepherd</strong> III, J. Harold <strong>Shepherd</strong>, Scott<br />
H. Sikes*, James E. Stephenson, James<br />
D. Thompson, Goodloe H. Yancey III<br />
*Ex Officio<br />
Spinal Column is published quarterly by<br />
<strong>Shepherd</strong> <strong>Center</strong>, a private, not-for-profit<br />
hospital specializing in <strong>the</strong> treatment<br />
of people with spinal cord injury and<br />
disease, acquired brain injury, multiple<br />
sclerosis and o<strong>the</strong>r neuromuscular<br />
disorders, and urological problems.<br />
E-mail change of address information or<br />
request to be removed from our mailing<br />
list to spinalcolumn@shepherd.org, or<br />
by mail to <strong>Shepherd</strong> <strong>Center</strong>, Attn: Spinal<br />
Column Mailing List, 2020 Peachtree<br />
Road, NW, Atlanta, Georgia, 30309.<br />
Please include mailing label. Spinal<br />
Column accepts no advertising. Spinal<br />
Column is a registered trademark of<br />
<strong>Shepherd</strong> <strong>Center</strong>.<br />
James H. <strong>Shepherd</strong>, Jr.<br />
Chairman of <strong>the</strong> Board
Fall2009Contents<br />
Photo by Leita Cowart<br />
SpinalColumn<br />
The Magazine of <strong>Shepherd</strong> <strong>Center</strong>:<br />
Providing Medical Treatment, Research and Rehabilitation<br />
12<br />
14<br />
Features<br />
Breathing Easier:<br />
Pacing system gives ventilator-dependent<br />
patients hope for improved quality of life.<br />
Eye Control:<br />
<strong>Shepherd</strong> evaluates vision-based<br />
communication system.<br />
15<br />
Building Professional Relationships:<br />
<strong>Shepherd</strong> <strong>Center</strong> emphasizes outreach to<br />
referring facilities and physicians.<br />
16<br />
Uncomplicating SCI Complications:<br />
<strong>Shepherd</strong> has success in resolving associated<br />
health problems in people with SCI.<br />
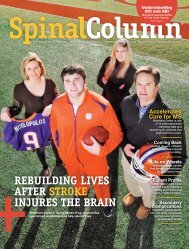
Cover<br />
Story<br />
19<br />
On <strong>the</strong> Net:<br />
“Catch Me on <strong>Shepherd</strong>TV.org” message<br />
debuts during Peachtree Road Race.<br />
Healing <strong>the</strong> Brain<br />
<strong>Shepherd</strong> <strong>Center</strong> brain injury<br />
programs include specialized<br />
treatment for young stroke patients,<br />
people in semi-comatose states and<br />
soldiers injured in battle.<br />
Departments<br />
2 Short Takes<br />
20 Research: Addressing Barriers to a Cure<br />
21 Managed Care Corner<br />
22 Patient Profile: Mal Zackery<br />
24 Ask <strong>the</strong> Doc Q & A<br />
25 Medical Staff Profile: John Lin, M.D.<br />
26 <strong>Shepherd</strong> Alums<br />
28 Foundation Features<br />
38 Loving Tributes<br />
About <strong>the</strong> cover:<br />
Lauren Rushen, 25, of Hartselle, Ala., experienced a<br />
stroke in September 2008. She has made tremendous<br />
progress and continues to work toward a full recovery<br />
with <strong>the</strong> help of <strong>Shepherd</strong> <strong>Center</strong>'s Acquired Brain Injury<br />
Program. Photo by Gary Meek<br />
Photo by Credit Here<br />
Photo by Leita Cowart<br />
22<br />
If you would like to make a gift to support <strong>the</strong> work<br />
you have read about, please contact Scott Sikes at <strong>the</strong><br />
<strong>Shepherd</strong> <strong>Center</strong> Foundation at 404-350-7305 or visit<br />
shepherd.org.
ShortTakes<br />
<strong>Shepherd</strong> Snapshots: A Look at News and O<strong>the</strong>r Notes<br />
Dr. Keith Tansey Appointed<br />
to ASIA Board of Directors<br />
Keith Tansey, M.D., Ph.D.,<br />
director of spinal cord injury research<br />
at <strong>Shepherd</strong> <strong>Center</strong>, has been<br />
appointed to <strong>the</strong> prestigious Board<br />
of Directors of <strong>the</strong> American Spinal<br />
Injury Association (ASIA).<br />
ASIA’s Board of Directors consists<br />
of 11 representatives, each serving<br />
a two-year term. A director is eligible to be reappointed twice<br />
following his/her initial term, for a maximum of six years. This is<br />
Dr. Tansey's first term.<br />
He has been a member of ASIA for some time and recently<br />
served as chairman of <strong>the</strong> Membership Committee. His primary<br />
board assignment for <strong>the</strong> next year will be to co-chair an effort to<br />
upgrade <strong>the</strong> ASIA Web site at www.asia-spinalinjury.org.<br />
Dr. Tansey joins two o<strong>the</strong>r <strong>Shepherd</strong> <strong>Center</strong> physicians –<br />
David Apple, Jr., M.D., and Bruce G. Green, M.D. – who have<br />
also served as ASIA board members in <strong>the</strong> past,. The National<br />
Office of ASIA is located within <strong>the</strong> Crawford Research<br />
Institute at <strong>Shepherd</strong> <strong>Center</strong>. — Caroline Hemingway<br />
Photo by Leita Cowart<br />
<strong>Shepherd</strong> <strong>Center</strong> Conducts<br />
Inpatient Satisfaction Surveys<br />
<strong>Shepherd</strong> <strong>Center</strong> is now conducting inpatient satisfaction surveys<br />
on a regular basis through a company called NRC Picker.<br />
Former patients will receive a call from Discovery Research<br />
Group on behalf of <strong>Shepherd</strong> <strong>Center</strong>. The caller will request a<br />
few minutes of time to complete a set of prepared questions.<br />
Discovery Research makes five call attempts starting about<br />
two weeks after <strong>the</strong> month of <strong>the</strong> patient’s discharge.<br />
The goal of <strong>the</strong> survey is to obtain feedback, information<br />
and opinion on <strong>the</strong> inpatient experience at <strong>Shepherd</strong> <strong>Center</strong>,<br />
and to establish and execute improvements and changes<br />
moving forward.<br />
<strong>Shepherd</strong> <strong>Center</strong> has taken previous survey results into<br />
consideration, and will implement a number of improvements,<br />
including a comprehensive handbook for <strong>the</strong><br />
families of patients, white boards in patients’ rooms<br />
to improve <strong>the</strong> level of communication, an indepth<br />
injury explanation on <strong>Shepherd</strong> <strong>Center</strong>’s<br />
site at www.shepherd.org and a permanent<br />
notebook in each Woodruff Family Residence<br />
<strong>Center</strong> apartment with information relevant<br />
to housing needs. — Caroline Hemingway<br />
Hurry and register! All Sports Camp<br />
Scheduled for Oct. 16-18<br />
<strong>Shepherd</strong> <strong>Center</strong>’s annual All Sports Camp is scheduled for<br />
Oct. 16-18 at Roosevelt Warm Springs Camp Dream in Warm<br />
Springs, Ga. The camp includes hands-on adaptive sports<br />
instruction in wheelchair basketball, quad rugby, swimming,<br />
wheelchair tennis, canoeing and kayaking, handcycling, track,<br />
field, scuba, wheelchair football and wheelchair team handball.<br />
The camp is open to adults ages 18 and up. The cost of $150<br />
includes lodging and meals. For more information, contact<br />
Matt Edens at 404-367-1287 or matt_edens@shepherd.org.<br />
Register online at: www.shepherd.org/allsportscamp.<br />
<strong>Shepherd</strong> <strong>Center</strong> File Photo<br />
<strong>Shepherd</strong> <strong>Center</strong> Physical<br />
Therapist Named Emerging Leader<br />
<strong>Shepherd</strong> <strong>Center</strong> spinal cord injury<br />
physical <strong>the</strong>rapist Joy Bruce recently<br />
received <strong>the</strong> American<br />
Physical Therapy Association’s<br />
Emerging Leader Award for 2008.<br />
This honor is given to one PT who<br />
demonstrates extraordinary service<br />
and makes exceptional contributions<br />
to APTA and <strong>the</strong> physical<br />
<strong>the</strong>rapy profession.<br />
Aside from her role as a PT, Bruce conducts clinical<br />
research with <strong>Shepherd</strong> <strong>Center</strong>’s new Spinal Cord Injury<br />
Research Laboratory. Studies she’s coordinating include a<br />
project with <strong>the</strong> Georgia Institute of Technology investigating<br />
<strong>the</strong> Tongue Drive wheelchair navigation system for people<br />
with quadriplegia and a project with <strong>the</strong> University of Georgia<br />
on <strong>the</strong> effects on muscle plasticity and glucose tolerance of<br />
an electrically stimulated streng<strong>the</strong>ning program.<br />
“It is an honor to be recognized by my peers,” Bruce says.<br />
“We cannot overestimate <strong>the</strong> importance of having strong<br />
leaders to guide research and education, and to advocate for<br />
patients and <strong>the</strong> profession.”<br />
Bruce praises <strong>the</strong> mentorship she receives from <strong>Shepherd</strong>’s<br />
clinicians and managers as a guiding force in her ability to<br />
emerge as a leader in her profession. — Kayla Eubanks<br />
Photo by Kayla Eubanks<br />
2 Spinal Column<br />
w w w. s h e p h e r d . o r g
Newly Integrated Sip-and-Puff System<br />
Gives Patients More Independence<br />
When <strong>Shepherd</strong> patient James Brown wants a little more light in his<br />
room, it’s as easy as a simple blow into a straw, <strong>the</strong>n a puff, thanks to a<br />
new, integrated sip-and-puff control system developed by <strong>Shepherd</strong>’s<br />
Assistive Technology <strong>Center</strong>.<br />
The system gives James <strong>the</strong> ability to control <strong>the</strong> lights and o<strong>the</strong>r<br />
technology in his room through a single device, which gives quadriplegic<br />
patients like him as much control as possible over <strong>the</strong>ir surroundings,<br />
says Assistive Technology <strong>Center</strong> manager John Anschutz, who<br />
developed <strong>the</strong> system with help from Jiasheng He, a Georgia Institute<br />
of Technology student who interned at <strong>Shepherd</strong> this past summer.<br />
“It gives <strong>the</strong> patient a sense of controlling <strong>the</strong>ir environment, which<br />
is important,” John says. “James told us that 16 years ago, when he<br />
was first injured, he had no control and felt stuck, like he couldn’t do<br />
anything. This system takes that away.”<br />
James helped John and his staff test <strong>the</strong> system, which allows <strong>the</strong><br />
user to adjust lights, control a television’s power and channels, make<br />
phone calls and summon a nurse.<br />
The system represents a huge upgrade, James says.<br />
“Controlling your environment is huge,” he explains. “This is really<br />
cutting-edge technology compared to where we were 16 years ago.<br />
When I was first injured, I had to call my mom all <strong>the</strong> time to do<br />
things for me.”<br />
Ultimately, John and his staff want to provide a cost-effective version<br />
of <strong>the</strong> integrated sip-and-puff system to patients like James for<br />
use in <strong>the</strong>ir homes.<br />
“First, we want to get this system into <strong>the</strong> hospital rooms of all<br />
patients who need <strong>the</strong>m, and <strong>the</strong>n get systems into <strong>the</strong>ir homes,” John<br />
says. “We have some steep hills to climb to get <strong>the</strong>re. We want to keep it<br />
simple and cheap and fill a niche where <strong>the</strong>re isn’t a lot out <strong>the</strong>re that is<br />
inexpensive.” — Bill Sanders<br />
Above: <strong>Shepherd</strong> <strong>Center</strong> Assistive Technology <strong>Center</strong> manager John<br />
Anschutz and Georgia Tech student Jiasheng He developed a new,<br />
integrated sip-and-puff control system with input from patient James<br />
Brown of Conyers, Ga.<br />
Photo by Gary Meek<br />
<strong>Shepherd</strong> <strong>Center</strong> and SkiMore Tours<br />
Offer Annual Adaptive Skiing Trip<br />
<strong>Shepherd</strong> <strong>Center</strong> and SkiMore Tours have planned<br />
a trip to Breckenridge, Colo., this winter for adaptive<br />
snow skiing for beginners to advanced skiers<br />
with physical disabilities.<br />
The trip, scheduled for Jan. 17-22, 2010,<br />
includes private adaptive skiing lessons, lift tickets,<br />
equipment, hotel accommodations, transportation<br />
from <strong>the</strong> airport to <strong>the</strong> hotel and two group dinners.<br />
People of all abilities are welcome, as well as<br />
<strong>the</strong>ir families and friends. Advance registration<br />
is required.<br />
For more information, contact <strong>Shepherd</strong> <strong>Center</strong><br />
<strong>the</strong>rapeutic recreation <strong>the</strong>rapist Katie Murphy at<br />
404-350-7488 or katie_murphy@shepherd.org. Or,<br />
go to www.skimoretours.com.<br />
<strong>Shepherd</strong> Launches<br />
New Web Site<br />
<strong>Shepherd</strong> <strong>Center</strong> has a new home on <strong>the</strong> Internet.<br />
This fall, <strong>the</strong> <strong>Center</strong> launched a redesigned Web<br />
site to keep pace with <strong>the</strong> overwhelming number<br />
of people who visit <strong>the</strong> site each day to learn more<br />
about <strong>the</strong> <strong>Shepherd</strong> experience.<br />
The new site, at www.shepherd.org, features<br />
several new features, including an updated overview<br />
of care programs, patient and program videos, and<br />
new online functions for submitting a referral or<br />
joining a research study.<br />
More and more people are now using <strong>the</strong> Internet<br />
when choosing a rehabilitation facility for <strong>the</strong>ir loved<br />
one. The new site is geared<br />
to helping people who are<br />
considering <strong>Shepherd</strong> as a<br />
rehabilitation option.<br />
In addition, a number<br />
of o<strong>the</strong>r types of visitors<br />
will find something of<br />
interest on <strong>the</strong> new site,<br />
including people interested<br />
in <strong>Shepherd</strong>’s research<br />
programs, clinical trials,<br />
volunteering or giving<br />
opportunities. There is<br />
also information available for download on injury<br />
prevention tips and resources related to disabilities.<br />
<strong>Shepherd</strong> <strong>Center</strong> expects to continue upgrading<br />
and improving <strong>the</strong> site. If you have any feedback<br />
about something you’d like to see, please contact<br />
Larry Bowie at larry_bowie@shepherd.org.<br />
Fall 2009 3
CoverStory<br />
Photo by Gary Meek<br />
Lauren Rushen, 25, of Hartselle, Ala.,<br />
experienced a stroke in September 2008. She<br />
completed <strong>Shepherd</strong> <strong>Center</strong>'s Young Stroke<br />
Rehabilitation Program. Recently, she returned<br />
to visit with several of her <strong>the</strong>rapists, left to right,<br />
Erin Mattingly, Jane Woodward and Lora Harvey.<br />
4 Spinal Column<br />
w w w. s h e p h e r d . o r g
HEALING<br />
<strong>the</strong> brain<br />
<strong>Shepherd</strong> <strong>Center</strong> brain injury programs include specialized treatment for young stroke<br />
patients, people in semi-comatose states and soldiers injured in battle. By Bill Sanders<br />
Twenty-five-year-olds aren’t supposed to have strokes, particularly those in good<br />
health and with few, if any, risk factors.<br />
And nei<strong>the</strong>r should 20-year-olds spend five weeks in a coma, nor should 22-<br />
year-olds experience <strong>the</strong> death and destruction of war.<br />
But, in reality, <strong>the</strong>se things happen, and that’s why <strong>Shepherd</strong> <strong>Center</strong>’s Acquired<br />
Brain Injury (ABI) Program has designed three unique, specialized programs<br />
among <strong>the</strong> many in its broad continuum of care.<br />
<strong>Shepherd</strong>’s Young Stroke Program treats stroke patients in <strong>the</strong>ir 20s, 30s and<br />
40s, helping <strong>the</strong>m with parenting skills, work re-entry or academic skills if <strong>the</strong>y are<br />
still in school.<br />
“For just about all of <strong>the</strong>m, <strong>the</strong>re is a change in lifestyle,” says ABI program director<br />
Susan Johnson, MA, CCC, CCM. “We teach <strong>the</strong>m strategies to live to <strong>the</strong>ir highest<br />
level of independence while focusing on re-integrating into <strong>the</strong>ir community.”<br />
<strong>Shepherd</strong>’s Pre-Rehabilitation and Education Program (PREP) admits patients who<br />
are semi-comatose or in a minimally conscious state for a five-week program that<br />
focuses on medical, pharmacological and equipment needs, while optimizing <strong>the</strong>ir<br />
recovery for emergence from <strong>the</strong>ir coma. The program also focuses on educating<br />
<strong>the</strong> patient’s family on how to take care of <strong>the</strong>ir loved one once he or she goes home.<br />
Patients who emerge from <strong>the</strong>ir coma go directly into <strong>Shepherd</strong>’s intensive rehabilitation<br />
program. Those who do not are discharged to <strong>the</strong>ir home or an alternative setting<br />
that supports <strong>the</strong>ir ongoing needs until <strong>the</strong>y are ready for more intensive <strong>the</strong>rapy.<br />
“We started PREP nine years ago because managed care policies were forcing<br />
families to take 18- or 19-year-old semi-comatose or minimally conscious patients to<br />
nursing homes because <strong>the</strong>re were little to no o<strong>the</strong>r alternatives,” Johnson explains.<br />
Fall 2009 5
“<strong>Shepherd</strong> brought her<br />
back from <strong>the</strong> dead.<br />
Had God not led us<br />
to <strong>Shepherd</strong>, Lauren<br />
wouldn’t have gotten well.”<br />
—Donna Rushen, mo<strong>the</strong>r of<br />
patient Lauren Rushen<br />
“Initially, only a few insurance companies agreed to pay for this level<br />
of care. In time, many insurance companies began to see <strong>the</strong> benefits<br />
with fewer rehospitalizations down <strong>the</strong> road.”<br />
And <strong>Shepherd</strong>’s SHARE Initiative, which began in early 2008,<br />
provides additional care to U.S. soldiers who sustain brain and/or<br />
spinal cord injuries while serving in Iraq or Afghanistan. SHARE is a<br />
partnership between <strong>Shepherd</strong>, <strong>the</strong> military’s healthcare services provider<br />
and Atlanta philanthropist Bernie Marcus, whose gift started <strong>the</strong><br />
program. SHARE funds cover needs and services outside <strong>the</strong> scope of<br />
benefits provided by <strong>the</strong> Department of Veterans Affairs and Humana<br />
Military Healthcare Services. Examples include personal support<br />
services, transportation, housing for family members, groceries and<br />
<strong>Shepherd</strong>’s Beyond Therapy activity-based <strong>the</strong>rapy program.<br />
Photo by Eric Schultz<br />
Above: After more than a year since her<br />
stroke, Lauren Rushen is working part<br />
time and living with her family, enjoying<br />
<strong>the</strong>ir horses, dogs and pond that sit on<br />
<strong>the</strong> family's 40-acre farm southwest<br />
of Huntsville. Her mo<strong>the</strong>r, Donna,<br />
thanks God that Lauren came to<br />
<strong>Shepherd</strong> for rehabilitation.<br />
Young Stroke Program<br />
Fortunately for Lauren Rushen, 25, of Hartselle, Ala., <strong>Shepherd</strong> <strong>Center</strong><br />
has a subspecialty program designed specifically for patients like her.<br />
On Sept. 17, 2008, Lauren got a bad headache – or toothache, she<br />
thought. She couldn’t specify exactly where <strong>the</strong> pain originated. But it<br />
was bad. And <strong>the</strong> timing for it was bad, too. Lauren, a case manager at<br />
<strong>the</strong> North Central Alabama Mental Retardation Authority in Decatur,<br />
Ala., was preparing for a visit <strong>the</strong> next day by Medicaid reviewers, who<br />
routinely examine <strong>the</strong> agency’s files.<br />
“I woke up Sept. 18 and couldn’t go to work,” Lauren recalls. “And on<br />
that day, it was a big deal. I had gone to <strong>the</strong> dentist <strong>the</strong> day before, and<br />
he thought maybe I needed a root canal, and he gave me some penicillin<br />
and Percocet. Then on this day, I got up and went to <strong>the</strong> chiropractor,<br />
thinking it might be TMJ (a jaw condition that causes pain).<br />
“I went to my mom’s house, and she was sick with a stomach virus, and<br />
we were both kind of reclining, her on <strong>the</strong> couch, me on a chair. I tried to<br />
get up and slid into <strong>the</strong> floor as my left side just collapsed. I couldn’t get<br />
up. My mom called 911, which we all thought was an overreaction.”<br />
But Lauren’s mom, Donna Rushen, wasn’t overreacting.<br />
Lauren had experienced a stroke that was severe enough for doctors<br />
in Huntsville, Ala., to put her in an induced paralytic state for 12 days<br />
and perform a craniotomy to help relieve <strong>the</strong> swelling of her brain.<br />
Initially, doctors were unable to offer <strong>the</strong> Rushen family any hope for<br />
Lauren’s recovery.<br />
But now, a year later, Lauren is home, working part time and living<br />
with her family, enjoying <strong>the</strong>ir horses, swimming pool and pond that<br />
sit on <strong>the</strong>ir 40-acre farm southwest of Huntsville. Mom and daughter<br />
bicker a bit at one ano<strong>the</strong>r: “She calls me Attila,” Donna says. But it’s<br />
good-natured ribbing – born from relief and fed by <strong>the</strong> reality that<br />
<strong>the</strong>y came close to losing one ano<strong>the</strong>r. Recalling Lauren’s initial prognosis<br />
still brings tears to Donna’s eyes.<br />
“When we left Huntsville for <strong>Shepherd</strong> <strong>Center</strong>, I had no idea she’d<br />
be like she is now,” Donna recalls as she makes iced tea in her kitchen.<br />
“We’d never heard of <strong>Shepherd</strong>, but while we were at <strong>the</strong> hospital in<br />
Huntsville, we heard from nurses who told us, ‘Don’t go anywhere but<br />
<strong>Shepherd</strong>.’ God took us <strong>the</strong>re. I’m sure of that.”<br />
6 Spinal Column w w w. s h e p h e r d . o r g
ain injury statistics<br />
<strong>Shepherd</strong> <strong>Center</strong> Brain Injury Inpatient<br />
Admissions by Injury Type, Fiscal Year 2009<br />
<strong>Shepherd</strong> Pathways Post-Acute<br />
Admissions by Injury Type, Fiscal Year 2009 SHARE Initiative Admissions, March 2008-July 2009<br />
144<br />
ATV<br />
Falls<br />
Automobile<br />
Traumatic Brain Injury<br />
Anoxia,<br />
Encephalopathies<br />
21<br />
Traumatic<br />
Brain Injury<br />
Non-Traumatic<br />
25<br />
= 143<br />
Brain Injury<br />
34<br />
Non-Traumatic Brain Injury<br />
Stroke<br />
43<br />
Clinical<br />
Population:<br />
Brain<br />
63%<br />
Spinal Cord<br />
Injury<br />
30%<br />
Pain<br />
Management<br />
7%<br />
For statistics on patient outcomes, see <strong>the</strong> “Why <strong>Shepherd</strong>?” tear-out information<br />
attached to page 21 in this issue of Spinal Column.<br />
Patient Military Service Status:<br />
53% = active duty<br />
47% = separated<br />
94<br />
Total<br />
Lauren’s treatment at <strong>Shepherd</strong> was nothing out of <strong>the</strong> ordinary<br />
by <strong>Shepherd</strong> standards. But try telling that to a mom who had visited<br />
a couple of general rehabilitation facilities that were potential<br />
alternatives for her daughter.<br />
“<strong>Shepherd</strong> – I’m going to start crying now – brought her back<br />
from <strong>the</strong> dead,” Donna says. “When she got <strong>the</strong>re, her voice wasn’t<br />
even a whisper. She couldn’t swallow, hadn’t sat up in 34 days, and<br />
we walked in <strong>the</strong>re, and on <strong>the</strong> first day, <strong>the</strong>y had her sitting up. I<br />
was afraid <strong>the</strong>y were hurting her, but <strong>the</strong>y knew what <strong>the</strong>y were<br />
doing. Then <strong>the</strong>y had her standing, and she’d feel ligh<strong>the</strong>aded and<br />
nauseated, and I’d worry. But again, <strong>the</strong>y knew best. Had God not<br />
led us to <strong>Shepherd</strong>, Lauren wouldn’t have gotten well.”<br />
Trauma doctors told Donna and her family that Lauren was<br />
brain damaged. At <strong>Shepherd</strong>, <strong>the</strong> staff told her that Lauren had<br />
a brain injury. Subtle difference? Maybe. But to Donna, it meant<br />
hope versus despair, dignity versus stigma. Even today, saying ‘brain<br />
damaged versus a brain injury’ brings tears to Donna’s eyes.<br />
As for Lauren, she returned to work part time in spring 2009,<br />
and she believes she’s almost 100 percent back to her former life.<br />
In reality, she’s not yet, but she may be soon, Donna says. Young<br />
stroke patients who rehabilitate at <strong>Shepherd</strong> often continue<br />
recovering for years.<br />
“They say my reaction time is still a bit slow and that my reasoning<br />
and judgment and problem-solving abilities are still affected,”<br />
Lauren says. “I don’t see that, don’t really believe it. But <strong>the</strong>y tell me<br />
that denial is part of it. So maybe it is.”<br />
Today, Lauren walks with a slight limp in her left leg, and she<br />
has perhaps <strong>the</strong> slightest droop on one side of her mouth. But that<br />
disappears when Lauren smiles, which is often, and in time, it will<br />
probably disappear altoge<strong>the</strong>r.<br />
Lauren has not returned to driving or living alone yet, but just<br />
about every o<strong>the</strong>r part of her life is back to how it used to be.<br />
Her boss, Earl Brightwell, says it was a delight to have Lauren<br />
return to work and that her responsibilities will increase in time.<br />
“She’s assisting with office chores, and it is great to see how<br />
much recovery she has made,” he adds. “We are looking forward<br />
to her continued recovery. She is a great asset to us as we serve<br />
people with intellectual disabilities. She is an excellent coordinator<br />
and has a sincere interest in <strong>the</strong> people she serves. They are all very<br />
excited to have her back.”<br />
PREP Program<br />
Joel Rodriguez, 20, of Gulf Breeze, Fla., sustained a traumatic<br />
brain injury in a T-bone automobile crash on April 1, 2009. The<br />
crash, which was caused by a drunk driver, killed one of his best<br />
friends and left Joel in a semi-comatose state. He came to<br />
<strong>Shepherd</strong> as a PREP patient.<br />
“The PREP program helps medically stabilize semi-comatose<br />
or minimally conscious patients and prepare <strong>the</strong>m for <strong>the</strong> intensity<br />
of a full rehabilitation program,” explains Darryl Kaelin,<br />
M.D., medical director of <strong>the</strong> Acquired Brain Injury Program.<br />
Fall 2009 7
“Sixty to 70 percent of <strong>the</strong>se patients end up getting into a regular<br />
rehabilitation program.”<br />
PREP also addresses <strong>the</strong> patient’s family’s concerns about caring<br />
for <strong>the</strong>ir loved one. “The physicians and ABI staff involve <strong>the</strong> family<br />
and educate <strong>the</strong>m about caring for <strong>the</strong> patient from <strong>the</strong> beginning,”<br />
Dr. Kaelin says.<br />
“From <strong>the</strong> first day we got <strong>the</strong>re, I was shocked to see a team<br />
here waiting for us,” recalls Joel’s mom, Nancy Rodriguez. “It was<br />
amazing. They checked him out and started to explain things to me.<br />
It was so calming <strong>the</strong> way <strong>the</strong> doctors talked to me, how thorough<br />
<strong>the</strong>y were in giving me test results, telling me everything <strong>the</strong>y were<br />
going to do.”<br />
After about two weeks in <strong>the</strong> PREP program, Joel emerged<br />
from <strong>the</strong> semi-comatose state he was in. Then he underwent<br />
<strong>the</strong>rapy in <strong>Shepherd</strong>’s inpatient program and continued rehabilitation<br />
in <strong>the</strong> post-acute residential program at <strong>Shepherd</strong> Pathways.<br />
Joel does not remember much of <strong>the</strong> first few weeks he spent at<br />
<strong>Shepherd</strong>. His perception of <strong>the</strong> time he spent in <strong>the</strong>rapy at<br />
<strong>Shepherd</strong> is skewed, and just a week or so into his <strong>the</strong>rapy at<br />
Pathways, he felt like he was ready to return home. Like many braininjured<br />
patients, Joel’s lack of insight into his injuries caused him to<br />
doubt his need for continued cognitive <strong>the</strong>rapy, Dr. Kaelin notes.<br />
But Joel’s mom knew it was best for her son to complete <strong>the</strong><br />
full continuum of care that <strong>Shepherd</strong> offers for people with brain<br />
injuries. “I have faith in this place,” Nancy says. “I wanted what was<br />
best for Joel, so we stayed until he was ready to be released. The<br />
people at <strong>Shepherd</strong> knew <strong>the</strong>re was still healing that needed to<br />
happen inside Joel’s brain.”<br />
At Pathways, Joel attended classes that challenged him to use<br />
cognitive reasoning and problem-solving skills. He also continued<br />
physical, occupational and speech <strong>the</strong>rapy, and participated in<br />
group and individual counseling. Joel worked to regain function<br />
in his paralyzed left arm and leg. He can walk short distances<br />
with some assistance now, but continues to use a wheelchair for<br />
longer walks.<br />
One thing he particularly enjoyed during his <strong>the</strong>rapy was<br />
playing Wii video games that helped improve his eye-hand<br />
coordination. He also kept in touch with his friends back home,<br />
some of whom visited him at <strong>Shepherd</strong>. And Joel imagined <strong>the</strong><br />
things he’ll do as he continues to recover.<br />
“I could dance really good,” Joel says. “I ought to get out of this<br />
chair and show you how good. I could run fast and liked playing<br />
basketball and football. I can’t play those now. Maybe later. I<br />
hope in a year or so. I think I’ll have everything back.”<br />
Sary Newman, a physical <strong>the</strong>rapist at Pathways, believes Joel<br />
will indeed be back to his old self in time.<br />
“From a physical standpoint, his prognosis is good,” she says.<br />
“But he’s not seeing <strong>the</strong> big picture right now and is frustrated.<br />
That can take a while – maybe a couple of years. But he’s got a<br />
great family who loves him, and he’s getting good care.”<br />
SHARE Initiative<br />
Smiles don’t flow easily from <strong>the</strong> face of 22-year-old U.S.<br />
Army Specialist Greg Hutchinson – even now, with his whole<br />
life ahead of him. The horrors of war are still very much a part<br />
of him. But thanks to <strong>the</strong> SHARE Initiative at <strong>Shepherd</strong><br />
<strong>Center</strong>, <strong>the</strong>y are no longer <strong>the</strong> sole defining statement of who<br />
he is or who he can become.<br />
“Six months ago, I couldn’t make it out to lunch,” Greg says.<br />
“I’m a totally different person now. I have a different outlook.<br />
Six months ago, if you were wearing a jacket, I’d be wondering<br />
Photos by Gary Meek<br />
8 Spinal Column w w w. s h e p h e r d . o r g
what you had underneath <strong>the</strong> jacket. My physical pain was<br />
through <strong>the</strong> roof, but I was also hyper-alert, hyper-sensitive,<br />
paranoid, isolated.”<br />
Today, Greg is none of those things. But he knows he’s still<br />
a work in progress. The difficult task of putting his life back<br />
toge<strong>the</strong>r is not done – not by a long shot. But <strong>the</strong>re is hope<br />
where <strong>the</strong>re once was only fear and despair.<br />
Greg doesn’t talk about his combat experience in Iraq. But<br />
he was injured in a blast explosion in October 2007 – one<br />
that damaged his brain, back and legs. He came back home a<br />
broken and battered man.<br />
“His lingering effects included PTSD (post-traumatic<br />
stress disorder), headaches, memory problems, dizziness,<br />
multiple musculo-skeletal pains and insomnia,” Dr. Kaelin<br />
says. “We look at this kind of patient as an onion with many<br />
layers that you have to peel back one at a time.<br />
“Greg was one of <strong>the</strong> more affected or impaired patients of<br />
anyone we’d seen,” Dr. Kaelin adds. “But he decided we knew<br />
what we were doing and jumped on board with us and gave it<br />
his all. He’s gotten better control of his pain and his emotional<br />
state – with less medication. He more independently<br />
manages his stressors and is emotionally stable.”<br />
Greg gives all <strong>the</strong> credit for his improvement to <strong>the</strong><br />
SHARE Initiative.<br />
“I’ve been to all <strong>the</strong> big places that <strong>the</strong>y tend to send<br />
patients like me,” Greg says. “Nothing has come close to this<br />
place. I came here thinking I was weird, that something was<br />
not right with me. What I learned here, through group sessions<br />
and informal talks with o<strong>the</strong>r patients, was that what I<br />
was feeling was normal for someone who had gone through<br />
what I had gone through.”<br />
Photo by Gary Meek<br />
“From <strong>the</strong> first day we got <strong>the</strong>re, I was shocked to see a<br />
team here waiting for us. It was amazing. They checked him<br />
out and started to explain things to me. It was so calming<br />
<strong>the</strong> way <strong>the</strong> doctors talked to me”<br />
—Nancy Rodriguez, mo<strong>the</strong>r of patient Joel Rodriguez<br />
Far Left: Darryl Kaelin, M.D., is medical director of <strong>Shepherd</strong>'s Acquired Brain Injury Program. Left: Even though<br />
her son Joel Rodriguez thought he was ready to return home after a couple of weeks at <strong>Shepherd</strong> Pathways,<br />
Nancy Rodriguez decided her son should stay until he completed <strong>the</strong> full continuum of care <strong>Shepherd</strong> offers for<br />
brain injury patients.<br />
Above: Sary Newman, right, one of Joel Rodriguez' <strong>the</strong>rapists at <strong>Shepherd</strong> Pathways, says his physical prognosis<br />
is good, and she thinks he will recover cognitively in time.<br />
Fall 2009 9
Photo by Gary Meek<br />
Photo by Leita Cowart<br />
Below: Greg Hutchinson discharged from <strong>the</strong><br />
SHARE Initiative at <strong>Shepherd</strong> <strong>Center</strong> this past<br />
summer. His treatment team believes he is<br />
prepared to face <strong>the</strong> challenges ahead. While<br />
in <strong>the</strong> program, he participated in equestrian<br />
<strong>the</strong>rapy at Chastain Horse Park in Atlanta.<br />
In <strong>the</strong> SHARE program, soldiers are housed<br />
toge<strong>the</strong>r near <strong>Shepherd</strong> – much like <strong>the</strong>y would<br />
be when on active duty – and go through <strong>the</strong> long<br />
process of healing toge<strong>the</strong>r. The military-like setup<br />
is part of <strong>the</strong> reason <strong>the</strong> program is so effective, Dr.<br />
Kaelin says.<br />
“Wounded soldiers tend to be more comfortable if<br />
<strong>the</strong>y are left in a military environment,” he explains.<br />
“So we house <strong>the</strong> patients toge<strong>the</strong>r instead of mixing<br />
<strong>the</strong>m into <strong>the</strong> civilian patient population. They get to<br />
be around o<strong>the</strong>r patients who are in similar situations,<br />
and that helps <strong>the</strong>m in <strong>the</strong>rapy – even informally.”<br />
Greg’s healing began once he realized he could<br />
let his guard down around staff and o<strong>the</strong>r patients –<br />
including ones who outranked him, he says.<br />
“You had to practice what you were learning, and<br />
that’s hard to do <strong>the</strong> first few weeks,” Greg recalls.<br />
“When you’re in <strong>the</strong> Army, you are taught to always<br />
have your dukes up. Once you figure out that you can<br />
let your hands down and trust people, and that <strong>the</strong>re<br />
were no ranks in <strong>the</strong> groups, <strong>the</strong>n you could start<br />
healing. I’ve been able to help o<strong>the</strong>rs go through that<br />
process. Most of us don’t have anyone else. I might<br />
have had experiences in combat and working through<br />
those issues that can help someone else. Or <strong>the</strong>y might<br />
have strategies that can help me. The PTSD – and all<br />
of <strong>the</strong> emotions – is <strong>the</strong> hardest thing to get fixed.”<br />
Greg discharged from <strong>the</strong> SHARE Initiative this<br />
past summer – feeling both eager and apprehensive<br />
about leaving <strong>the</strong> program. He has no long-term<br />
goals yet. Instead, he focuses on <strong>the</strong> more immediate<br />
future. He expects to be medically discharged from<br />
<strong>the</strong> Army soon.<br />
“I’m moving to Wisconsin with an Army buddy<br />
and starting life over <strong>the</strong>re,” Greg says. “It’s a<br />
Catch-22 because I want to get out and go on with<br />
my life so badly, but I also know that this part of my<br />
support will be missing, and that’ll be scary. Every<br />
transition is tough, but <strong>the</strong> transition out of<br />
<strong>Shepherd</strong> will be very scary. Being on my own,<br />
where I can’t just go knock on someone’s door and<br />
talk, and have <strong>the</strong>m understand what’s going on,<br />
that’s intimidating.”<br />
Terri Kohn, LPC, Greg’s counselor at <strong>Shepherd</strong>,<br />
knows, maybe even more than Greg does, just how<br />
far he has come. “He has had several bumps in <strong>the</strong><br />
road and will continue to face challenges that might<br />
set him back,” Kohn says. “But he definitely makes<br />
use of <strong>the</strong> strategies he has learned to get through<br />
<strong>the</strong> more difficult times.”<br />
It’s a challenge Greg appears prepared to take on<br />
and one he is now better equipped to face.<br />
1 0 Spinal Column w w w. s h e p h e r d . o r g
+<br />
CoverStorySidebar<br />
Praise on<br />
Peachtree<br />
Former Young Stroke Program patient gives thanks for<br />
his recovery during Atlanta’s Peachtree Road Race.<br />
By Bill Sanders<br />
This year, while everyone else celebrated Independence Day on<br />
July 4th, Wes Varda celebrated Thanksgiving.<br />
As he ran up Cardiac Hill in Atlanta’s Peachtree Road Race,<br />
he stopped to thank staff and supporters of <strong>Shepherd</strong> <strong>Center</strong>. He<br />
wanted <strong>the</strong>m to know how grateful he was to be alive – much less<br />
running again.<br />
In December 2008, 32-year-old Wes had a stroke so severe<br />
that doctors and Wes’ parents thought he was dying. Taken to<br />
Northside Hospital in Atlanta, Wes was unable to speak or move,<br />
but could see, hear and understand. He knew a priest was coming<br />
to give him Last Rites.<br />
But doctors performed a two-hour, life-saving surgery in which<br />
a ca<strong>the</strong>ter carrying a clot-busting chemical was threaded from<br />
Wes’ groin into his brain stem. The chemical worked, <strong>the</strong> clot<br />
dissolved and Wes was soon admitted to <strong>Shepherd</strong> <strong>Center</strong> for<br />
rehabilitation. Staff in <strong>the</strong> hospital’s Young Stroke Program set<br />
out to help Wes put his life back toge<strong>the</strong>r.<br />
“When admitted, Wes was weak in all of his extremities,”<br />
recalls Payal Fadia, M.D., Wes’ physician at <strong>Shepherd</strong>. “His<br />
ability to communicate was limited, and he required a feeding<br />
tube for nutrition due to difficulty swallowing. In addition, he had<br />
difficulty with balance, dizziness and coordination of movements.<br />
The sort of stroke Wes had is life-threatening and can have a very<br />
poor prognosis if not immediately treated.”<br />
Wes did not realize his prognosis when he first came to<br />
<strong>Shepherd</strong>. But he did sense he was in <strong>the</strong> right place to get <strong>the</strong><br />
help he needed.<br />
“When I got <strong>the</strong>re, I was still wondering what was going on,<br />
but I knew enough to know that it was a great hospital, so my<br />
spirits were a little better because of that,” Wes recalls. “I was out<br />
of <strong>the</strong> woods as far as living or dying, but I still had some major<br />
health concerns. I couldn’t walk and could barely talk.”<br />
But things soon began to improve for Wes.<br />
“Everyone was so warm and nice <strong>the</strong>re,” he says. “They were<br />
patient with me. I didn’t really have many expectations when I<br />
got <strong>the</strong>re because I was still so dazed. But <strong>the</strong> recovery has been<br />
much greater than I could have expected. Just nine months<br />
after my stroke, I am almost fully functioning. All of my doctors<br />
are optimistic.”<br />
Wes deserves a lot of <strong>the</strong> credit for his recovery, says Kendra<br />
Moon, his case manager at <strong>Shepherd</strong>.<br />
Above: Wes Varda, 32, of Atlanta had a severe<br />
stroke in December 2008. Today, he is back to<br />
running and now volunteers at <strong>Shepherd</strong> <strong>Center</strong>.<br />
“Wes was open and willing to acknowledge <strong>the</strong> differences in his<br />
condition, both physically and cognitively, as a result of his brain<br />
injury,” she explains. “When he got here, he was in a wheelchair<br />
and required physical assistance and supervision with his personal<br />
care. He had visual and speech difficulties, and he had lost a lot of<br />
strength, coordination, and fluidity of movement in his arms and<br />
legs. He required 24-hour supervision and care.”<br />
After completing <strong>the</strong> inpatient Young Stroke Program at<br />
<strong>Shepherd</strong>, Wes moved on to <strong>the</strong> post-acute day program at<br />
<strong>Shepherd</strong> Pathways. It included physical, occupational, speechlanguage-cognitive<br />
<strong>the</strong>rapies, <strong>the</strong>rapeutic recreation, counseling and<br />
vocational services. After two months, he transitioned to Pathways’<br />
outpatient <strong>the</strong>rapy program, where he participated in rehabilitation<br />
<strong>the</strong>rapy twice a week.<br />
By July 4th, Wes was ready to say thanks publicly. He chose <strong>the</strong><br />
Peachtree Road Race for his mission because it takes participants<br />
past <strong>Shepherd</strong> <strong>Center</strong>. Patients and staff line <strong>the</strong> sidewalk to cheer<br />
participants as <strong>the</strong>y pass by, but on this day, Wes cheered <strong>the</strong>m.<br />
“That was truly one of <strong>the</strong> highlights of my recovery,” Wes recalls.<br />
“Getting to run past <strong>Shepherd</strong> and talk to patients in wheelchairs<br />
and tell <strong>the</strong>m I was where <strong>the</strong>y are just a few months ago, that made<br />
me very happy. I didn’t get emotional, like fighting back tears, but I<br />
felt very blessed.”<br />
Wes is not sure what <strong>the</strong> future holds for him. He is volunteering<br />
at <strong>Shepherd</strong> – now as a greeter in <strong>the</strong> cafeteria and later with a peer<br />
volunteer group. O<strong>the</strong>r than that: “The future is wide open,” he says.<br />
And Wes knows he’ll have plenty of support from friends and<br />
family, which is vital in rehabilitation.”<br />
Dr. Fadia says Wes’ recovery has surprised everyone, even at<br />
<strong>Shepherd</strong> – a place where incredible recoveries often occur.<br />
“His stroke is extremely rare in a person of Wes’ age and good<br />
general health,” Dr. Fadia says. “And as for where he is now, I did<br />
not expect this. Wes has made an unbelievably remarkable recovery<br />
in an extremely short period of time.”<br />
Photo by Gary Meek<br />
Fall 2009 1 1
PacingSystemFeature<br />
Breathing<br />
NeuRx Diaphragmatic Pacing System<br />
gives ventilator-dependent patients hope<br />
for an improved quality of life.<br />
By Bill Sanders<br />
For Jenny Sorenson, not having a voice with which to speak<br />
meant it was hard to have a voice in how she would raise her<br />
children, how she would keep friends informed, and how<br />
she would thank her husband for his faithful support.<br />
Thanks to new technology being implemented at <strong>Shepherd</strong><br />
<strong>Center</strong>, Jenny – and o<strong>the</strong>r patients who are dependent upon<br />
a ventilator to make <strong>the</strong>m brea<strong>the</strong> – can now wean off <strong>the</strong><br />
ventilator and instead use an implantable device called <strong>the</strong><br />
NeuRx Diaphragmatic Pacing System (DPS). The system<br />
has made all <strong>the</strong> difference in <strong>the</strong> world for Jenny, who no<br />
longer has to rely upon her friends and family to read her<br />
lips.“They had gotten pretty good at it,” she says. “But that<br />
wasn’t a solution long-term.”<br />
Now, Jenny uses <strong>the</strong> NeuRx DPS most of <strong>the</strong> time, but<br />
still relies upon a ventilator occasionally. Dual dependency is<br />
normal for a while, but eventually, Jenny expects <strong>the</strong> ventilator<br />
to be a thing of <strong>the</strong> past in her life.<br />
The NeuRx DPS, which was developed by researchers at<br />
Case Western Reserve University and is licensed by Synapse<br />
Biomedical Inc., works like this: Four small wires are surgically<br />
attached to <strong>the</strong> diaphragm, <strong>the</strong> breathing muscle in <strong>the</strong><br />
chest. This procedure requires minimally invasive laparoscopic<br />
surgery. These wires exit <strong>the</strong> chest wall and are attached to an<br />
external stimulator, <strong>the</strong> NeuRx DPS. The stimulator provides<br />
electrical stimulation through <strong>the</strong> wires to <strong>the</strong> diaphragm and<br />
nerves that run through <strong>the</strong> diaphragm. When stimulated, <strong>the</strong><br />
diaphragm contracts, mimicking natural breathing. Air is allowed<br />
to fill <strong>the</strong> upper and lower parts of <strong>the</strong> lungs ra<strong>the</strong>r than<br />
forcing air in with a mechanical ventilator.<br />
Following clinical trials of NeuRx DPS in patients at<br />
<strong>Shepherd</strong> <strong>Center</strong> and elsewhere, <strong>the</strong> FDA approved <strong>the</strong> use of<br />
<strong>the</strong> device in June 2008. After that approval, Jenny was <strong>the</strong> first<br />
patient in <strong>the</strong> nation to undergo <strong>the</strong> procedure and begin using<br />
<strong>the</strong> pacing system, says Cathy Gragg, <strong>the</strong> <strong>Shepherd</strong> program<br />
coordinator for NeuRx DPS. Since <strong>the</strong>n, <strong>Shepherd</strong> <strong>Center</strong><br />
physicians have implanted <strong>the</strong> device in 10 patients with spinal<br />
cord injury (SCI). Most are now in various stages of weaning<br />
from <strong>the</strong> ventilator.<br />
Jenny’s success with <strong>the</strong> NeuRx DPS stems from<br />
determination and hard work on her part, as well as her<br />
caregivers, which include family members. She has come a long<br />
way since <strong>the</strong> diagnosis of <strong>the</strong> medical condition that left her a<br />
quadriplegic in early 2008. Doctors at Johns Hopkins Hospital<br />
in Baltimore determined <strong>the</strong>re was an abnormal tangle of<br />
vessels in Jenny’s spinal cord, which cut off blood supply to her<br />
cord. She underwent surgery and transferred to <strong>Shepherd</strong> for<br />
rehabilitation in May 2008.<br />
While she was undergoing rehabilitation, Andrew Zadoff,<br />
M.D., medical director of <strong>Shepherd</strong>’s Intensive Care Unit (ICU)<br />
and Pulmonary Services, screened Jenny as a potential candidate<br />
for <strong>the</strong> NeuRx DPS.<br />
“I had been at <strong>Shepherd</strong> for two months, and Johns Hopkins<br />
before that, so when <strong>the</strong>y first suggested <strong>the</strong> pacing system, I just<br />
wanted to go home and see my family,” Jenny recalls. “But after<br />
getting home and clearing my head a little, I realized I really<br />
needed to do this.<br />
“For <strong>the</strong> first four months on <strong>the</strong> ventilator, all I did was lie in<br />
bed,” Jenny says. “I didn’t speak clearly with a voice until I got to<br />
1 2 Spinal Column<br />
w w w. s h e p h e r d . o r g
Photo by Owen Riley<br />
Photo by Leita Cowart<br />
“Now, with <strong>the</strong> pacing system, my voice is much stronger. Even if<br />
I’m not strictly on <strong>the</strong> pacer, I have it on, and my breathing is a<br />
lot stronger. It’s just easier to brea<strong>the</strong>.” — Jenny Sorenson<br />
<strong>Shepherd</strong>. People had learned to read my lips, but trying to communicate<br />
with my kids (twin 10-year-olds and a 7-year old) was<br />
very hard at times.<br />
“Now, with <strong>the</strong> pacing system, my voice is much stronger,” she<br />
adds. “Even if I’m not strictly on <strong>the</strong> pacer, I have it on, and my<br />
breathing is a lot stronger. It’s just easier to brea<strong>the</strong>.”<br />
Dr. Zadoff, who screens all <strong>Shepherd</strong> ventilator-dependent<br />
SCI inpatients and outpatients to see if <strong>the</strong>y are medically appropriate<br />
for <strong>the</strong> NeuRx DPS, attributes Jenny’s success with<br />
<strong>the</strong> device to several factors – most importantly her desire to<br />
make a change that would improve her quality of life.<br />
“First of all, <strong>the</strong> patient has to have a willingness to get off<br />
<strong>the</strong> ventilator,” Dr. Zadoff says. “It is hard work that begins<br />
within 24 hours after <strong>the</strong> procedure. Vent-weaning can <strong>the</strong>n<br />
take up to seven weeks after that. In <strong>the</strong>ory, <strong>the</strong>re’s no reason<br />
why <strong>the</strong>y cannot be completely weaned off <strong>the</strong> ventilator and use<br />
<strong>the</strong> pacing system 24 hours a day. But some patients feel more<br />
comfortable continuing to use <strong>the</strong> ventilator at night, even after<br />
<strong>the</strong> procedure is done.”<br />
Ano<strong>the</strong>r requirement for NeuRx DPS patients and caregivers<br />
are pre- and post-operative training sessions. “We want<br />
patients to have a good understanding of how <strong>the</strong> pacing system<br />
works and what we’re trying to do,” Dr. Zadoff notes.<br />
Once <strong>the</strong> screening process indicates a patient is a good<br />
candidate for <strong>the</strong> NeuRx DPS, <strong>Shepherd</strong> <strong>Center</strong> consulting<br />
surgeon Saeid Khansarinia, M.D., performs an exploratory<br />
laparoscopy on <strong>the</strong> patient at neighboring Piedmont Hospital.<br />
In that procedure, he attaches electrodes to <strong>the</strong> patient’s phrenic<br />
nerve, which helps control breathing, to see if it can cause <strong>the</strong><br />
diaphragm to be stimulated. If so, <strong>the</strong>n <strong>the</strong> surgery is done, and<br />
soon <strong>the</strong>reafter, <strong>the</strong> vent-weaning process begins.<br />
Dr. Khansarinia says <strong>the</strong> NeuRx DPS can make a significant<br />
and dramatic change in patients’ lives. He looks forward<br />
to future generations of <strong>the</strong> device that may make it entirely<br />
implantable, thus eliminating <strong>the</strong> need for any external wires<br />
and machines, he adds.<br />
Inpatients who are interested in <strong>the</strong> NeuRx DPS can<br />
initiate <strong>the</strong> screening process by simply asking <strong>the</strong>ir doctor.<br />
Outpatients are asked to contact <strong>Shepherd</strong> <strong>Center</strong> case manager<br />
Brenna Blocker at 404-367-1253 or brenna_blocker@shepherd.<br />
org. More information is available at www.shepherd.org/dps.<br />
For Jenny, <strong>the</strong> decision to get <strong>the</strong> NeuRx DPS was a good<br />
one, she says. Though she’s not sure when, if ever, things will get<br />
back to normal for her, she’s thrilled to have a voice again and to<br />
have a family that loves her so much.<br />
“My husband has been wonderful,” Jenny says. “I couldn’t get<br />
through it without him. My kids want <strong>the</strong> old mom back, but<br />
we’ve adapted how we do things, such as hugs and going places.<br />
They put <strong>the</strong>ir hand on my hand when we’re out. It’s not by any<br />
means normal for <strong>the</strong>m, but <strong>the</strong>y like it that I can come to <strong>the</strong>ir<br />
swim practices, can go out to eat and not just be in a bed. So<br />
that’s some normalcy.”<br />
Above: Jenny Sorenson, her husband Scott and <strong>the</strong>ir children are<br />
returning to some normalcy in <strong>the</strong>ir lives in Irmo, S.C., since Jenny<br />
started using <strong>the</strong> NeuRx DPS system to help her brea<strong>the</strong>.<br />
Andrew Zadoff, M.D., screens all ventilator-dependent SCI patients<br />
to see if <strong>the</strong>y are appropriate for <strong>the</strong> pacing system.<br />
Fall 2009 1 3
AssistiveTechnologyFeature<br />
Photo by Gary Meek<br />
Edge with appropriate <strong>Shepherd</strong> patients to see how it can<br />
help <strong>the</strong>m and <strong>the</strong>n determine if it’s an affordable solution<br />
for <strong>the</strong>m. Results elsewhere indicate <strong>the</strong>re is reason to be<br />
optimistic, John notes.<br />
Eyegaze Edge appears to be a promising piece of<br />
technology for improving patients’ quality<br />
of life and restoring some of <strong>the</strong>ir independence.<br />
Eye Control<br />
<strong>Shepherd</strong>’s Assistive Technology <strong>Center</strong> evaluates<br />
vision-based communication and control system<br />
for patients who cannot speak.<br />
By Bill Sanders<br />
<strong>Shepherd</strong> <strong>Center</strong> patient Julius Singleton struggled a bit <strong>the</strong><br />
first time he stared at a computer screen and tried to type out<br />
his name, using nothing but his eyes.<br />
But, with a little practice using a vision-based communication and<br />
control technology called Eyegaze Edge, Julius, a college professor from<br />
Burnsville, W.Va., made progress.<br />
“This technology has <strong>the</strong> potential to transform <strong>the</strong> lives of quadriplegics<br />
whose high-level injuries make it difficult for <strong>the</strong>m to speak and<br />
communicate,” says John Anschutz, director of <strong>the</strong> Assistive Technology<br />
<strong>Center</strong> at <strong>Shepherd</strong> <strong>Center</strong>.<br />
The technology, developed by LC Technologies Inc., gives users numerous<br />
functions including: speech generation, environmental control<br />
(lights, appliances), typing, and running both mouse- and keyboardcontrolled<br />
applications on <strong>the</strong> company’s Edge screen. Also, <strong>the</strong> Edge<br />
can serve as a keyboard and mouse interface for a user’s own computer.<br />
Users make selections by looking at boxes or “keys” displayed on <strong>the</strong><br />
Edge screen. The system uses a pupil-center/corneal-reflection method<br />
to determine where a user is looking on <strong>the</strong> screen. An infrared-sensitive<br />
video camera, mounted beneath <strong>the</strong> system’s screen, takes 60 pictures per<br />
second of <strong>the</strong> user’s eye. The Edge calculates <strong>the</strong> person’s gazepoint (i.e.,<br />
<strong>the</strong> coordinates of where he is looking on <strong>the</strong> screen) based on <strong>the</strong> relative<br />
positions of <strong>the</strong> pupil center and corneal reflection within <strong>the</strong> video<br />
image of <strong>the</strong> eye.<br />
The technology isn’t new to <strong>the</strong> market, but it’s new to <strong>Shepherd</strong><br />
<strong>Center</strong> and its patient population. Ruth Fierman, an occupational<br />
<strong>the</strong>rapist in <strong>the</strong> Assistive Technology <strong>Center</strong>, is testing <strong>the</strong> Eyegaze<br />
If Ruth determines <strong>the</strong>re is potential for <strong>the</strong> Eyegaze Edge<br />
system to be a good match for a patient, one of <strong>Shepherd</strong>’s<br />
speech and language pathology <strong>the</strong>rapists determines if <strong>the</strong><br />
system will provide efficient communication for <strong>the</strong> patient.<br />
As a technology demonstration with Julius shows, Eyegaze<br />
requires practice. Users must learn how to focus on a letter or<br />
statement, such as “I am thirsty,” for <strong>the</strong> right amount of time.<br />
“It can be intimidating until you are familiar with it,” John<br />
says. “Once <strong>the</strong>y get <strong>the</strong> hang of it, though, <strong>the</strong>y want us to<br />
speed it up.”<br />
Physicians expect Julius to regain his voice, but some<br />
o<strong>the</strong>r high-level quadriplegics do not regain that function.<br />
And if <strong>the</strong>y are unable to use a mouse stick in <strong>the</strong>ir mouth,<br />
<strong>the</strong>y have virtually no ability to communicate, John notes.<br />
So Eyegaze Edge appears to be a promising technology for<br />
improving patients’ quality of life and restoring some of <strong>the</strong>ir<br />
independence.<br />
“If someone can’t communicate at all, it is amazingly<br />
frustrating for that person,” John explains. “So, once we finish<br />
evaluating <strong>the</strong> Eyegaze Edge system we have at <strong>Shepherd</strong><br />
now, we hope to get some funding through grants to help<br />
more people. The price of <strong>the</strong>se units has come down from<br />
about $18,000 to $9,000, so we hope, in time, that we can get<br />
<strong>the</strong>m into some homes of people who need <strong>the</strong>m.”<br />
Above: Ruth Fierman, center, an occupational <strong>the</strong>rapist<br />
in <strong>Shepherd</strong> <strong>Center</strong>'s Assistive Technology <strong>Center</strong> (ATC),<br />
evaluates whe<strong>the</strong>r <strong>the</strong> Eyegaze Edge system is appropriate for<br />
quadriplegics who have lost use of <strong>the</strong>ir voice. John Anschutz,<br />
manager of <strong>the</strong> ATC, assists with a demonstration for patient<br />
Julius Singleton of Burnsville, W. Va.<br />
Photo by Gary Meek<br />
1 4 Spinal Column<br />
w w w. s h e p h e r d . o r g
OutreachFeature<br />
Building<br />
Professional<br />
Relationships<br />
<strong>Shepherd</strong> <strong>Center</strong> emphasizes outreach to referring<br />
facilities and physicians.<br />
By Kayla Eubanks<br />
The <strong>Shepherd</strong> <strong>Center</strong> Marketing and Public Relations<br />
departments have teamed up to create a special outreach<br />
plan to <strong>the</strong> hundreds of referring facilities and physicians<br />
who work with <strong>the</strong> hospital each year.<br />
To build better relationships and improve communications,<br />
<strong>the</strong> team created new strategies to effectively communicate<br />
news at <strong>Shepherd</strong> and update referring physicians on how <strong>the</strong>ir<br />
patients are doing in rehabilitation, explains Mitch Fillhaber, vice<br />
president of marketing and managed care. The goal is to improve<br />
access to <strong>Shepherd</strong> <strong>Center</strong> physicians for <strong>the</strong> trauma physicians<br />
and neurosurgeons who initiate life-saving interventions at <strong>the</strong><br />
facilities that refer patients to <strong>Shepherd</strong>.<br />
Fillhaber outlines <strong>the</strong> details of <strong>the</strong> plan:<br />
MD-to-MD Communication<br />
As part of <strong>the</strong> new plan, <strong>Shepherd</strong> <strong>Center</strong> doctors call referring<br />
physicians to provide insight into <strong>the</strong>ir patient’s transition and rehabilitation<br />
plan following admission. Although most physicians<br />
already call <strong>the</strong> referring hospital or physician once a patient has<br />
arrived, <strong>Shepherd</strong> created an internal standard to ensure that this<br />
happens regularly.<br />
If a patient is admitted to <strong>the</strong> ICU, <strong>the</strong> admitting physician<br />
will contact <strong>the</strong> referring physician within 24 hours to confirm<br />
<strong>the</strong> patient arrived. The physician also will provide information<br />
on <strong>the</strong> patient’s medical status and immediate plan of care. If a<br />
patient is admitted on a Friday, <strong>the</strong> referring physician will be<br />
contacted by Monday.<br />
For acute rehabilitation patients, <strong>the</strong> standard is to call <strong>the</strong><br />
referring physician within 24 hours of <strong>the</strong> first team meeting,<br />
which is typically held during <strong>the</strong> patient’s first week at<br />
<strong>Shepherd</strong>. Team meetings involve <strong>the</strong> patient’s physician, case<br />
manager, <strong>the</strong>rapists and nurses. The team discusses <strong>the</strong> patient’s<br />
plan of care, including anticipated <strong>the</strong>rapies and any medical issues<br />
<strong>the</strong> patient may be having. Referring physicians will be told<br />
<strong>the</strong> medical status, care plan and anticipated length of stay.<br />
Enhancing Discharge Summaries<br />
Ano<strong>the</strong>r way <strong>Shepherd</strong> <strong>Center</strong> is intent on improving its direct<br />
communication with outside physicians is through enhanced<br />
Above: <strong>Shepherd</strong> <strong>Center</strong> physicians, including<br />
Medical Director Donald Peck Leslie, M.D., call referring<br />
physicians to provide insight into <strong>the</strong>ir patient’s transition<br />
and rehabilitation plan following admission.<br />
information in its discharge summaries. The hospital’s 13 admissions<br />
liaisons have been meeting with referring physicians from<br />
trauma centers to determine what additional information would be<br />
beneficial for <strong>the</strong>m to have in anticipation of serving patients upon<br />
<strong>the</strong>ir return to <strong>the</strong> community.<br />
New Newsletters<br />
<strong>Shepherd</strong> <strong>Center</strong> also will be expanding its physician publications<br />
to include two new newsletters that will complement Consulting<br />
Physician, a newsletter <strong>the</strong> hospital started earlier this year. The two<br />
new bi-annual newsletters include one written for neurosurgeons<br />
and trauma physicians and <strong>the</strong> o<strong>the</strong>r for physiatrists. The newsletters<br />
provide information on hospital practices, ICU processes,<br />
research trials, continuing education opportunities and more. The<br />
first issue of Consulting Physician is available at www.shepherd.org/<br />
publications. The o<strong>the</strong>rs are under development.<br />
Photo and Video Updates<br />
A great way to understand <strong>Shepherd</strong> <strong>Center</strong> practices is to see<br />
firsthand how a patient is improving. For a visual update, referring<br />
facilities can receive a photo or video of <strong>the</strong>ir former patient. Photos<br />
are taken during <strong>the</strong>rapy sessions to demonstrate something <strong>the</strong><br />
patient is working to improve, such as lifting <strong>the</strong>ir arms or writing<br />
<strong>the</strong>ir name. The photos also give <strong>the</strong> patient an opportunity to say<br />
thank you to <strong>the</strong> referring team.<br />
Video updates include recorded messages from <strong>the</strong> patient, his<br />
or her physician and sometimes even family members. It shows<br />
<strong>the</strong> patient in multiple <strong>the</strong>rapy sessions and tells <strong>the</strong> story of <strong>the</strong>ir<br />
recovery since arriving at <strong>Shepherd</strong>. The admissions team can take<br />
<strong>the</strong>se to referring hospitals when <strong>the</strong>y visit to show physicians and<br />
case managers how <strong>the</strong>ir prior referrals improved.<br />
Photo by Gary Meek<br />
Fall 2009 1 5
ICUFeature<br />
Photos by Gary Meek<br />
Above and Right: <strong>Shepherd</strong><br />
<strong>Center</strong> ICU nurses, such as Kim<br />
Whitlock, have training in both<br />
critical care and rehabilitation.<br />
Acquired Brain Injury Program<br />
Medical Director Darryl Kaelin,<br />
M.D., left, discusses a case wtih<br />
Whitlock and Emory University<br />
resident Dionne Cas<strong>the</strong>ly, M.D.<br />
1 6 Spinal Column<br />
w w w. s h e p h e r d . o r g
Un-<br />
Adapting to life after a spinal cord injury is no easy task.<br />
Unlike o<strong>the</strong>r less severe injuries, spinal cord injury (SCI) often<br />
comes with a host of o<strong>the</strong>r complications – a cascade of health issues<br />
that can result from damaged nerves, sudden immobility, loss<br />
of sensation and paralysis of <strong>the</strong> breathing muscles, among o<strong>the</strong>rs.<br />
Some of <strong>the</strong> most common problems patients may encounter<br />
include skin sores, ventilator-assisted pneumonia, and bowel and<br />
bladder control issues.<br />
It’s important for people with SCI and <strong>the</strong>ir loved ones to<br />
remember that many of <strong>the</strong>se health issues are not inevitable<br />
and can be controlled or managed. Knowing how to recognize,<br />
anticipate and treat complications early on is essential for quality<br />
patient care and recovery – and has long been a major priority for<br />
treatment teams at <strong>Shepherd</strong> <strong>Center</strong>.<br />
<strong>Shepherd</strong>’s acute-care capabilities and expert medical staff help<br />
resolve SCI-related complications quickly – often simultaneously<br />
to starting patients in a coordinated rehabilitation program to<br />
maximize recovery and avoid delays.<br />
Keys to Success<br />
“We spend a lot of time making sure our staff understand <strong>the</strong><br />
physiology and anatomy of catastrophic injuries,” says Tammy<br />
King, RN, chief nurse executive at <strong>Shepherd</strong> <strong>Center</strong>.<br />
That’s because what appears as “normal” body functioning for<br />
any o<strong>the</strong>r person is not for someone with a spinal cord injury.<br />
“Their bladder functions differently, <strong>the</strong> skin is at risk for breakdown,<br />
and patients who appear normal may actually be cognitively<br />
impaired, which means <strong>the</strong>y can’t be relied upon for medical<br />
histories,” she says.<br />
The sheer volume of patients cared for means <strong>Shepherd</strong> is<br />
accustomed to assessing complications early on and determining<br />
what is <strong>the</strong> “norm” for neurological problems.<br />
“One marker of success is our ability to wean patients from <strong>the</strong><br />
ventilator, a machine that helps <strong>the</strong>m brea<strong>the</strong>,” King says. “It’s <strong>the</strong><br />
difference between a patient going around with a machine every<br />
day and being able to brea<strong>the</strong> on his or her own, which is a huge<br />
quality-of-life issue – not to mention <strong>the</strong> additional medical and<br />
financial burdens that come with using a ventilator.”<br />
In 2008, nearly 86 percent of <strong>Shepherd</strong> SCI patients with injuries<br />
ranging from C-4 to C-7 or T-1 to T-12 were weaned from<br />
<strong>Shepherd</strong> has success in resolving associated health problems<br />
in people with spinal cord injury. By Amanda Crowe, MA, MPH<br />
complicating<br />
SCI<br />
<strong>the</strong> ventilator during <strong>the</strong>ir inpatient stay<br />
at <strong>the</strong> hospital in an average of 20 days.<br />
The hospital also prides itself on low,<br />
hospital-acquired infection rates thanks<br />
to its dedicated respiratory <strong>the</strong>rapy and<br />
nursing staff and rigorous quality control<br />
measures, which track <strong>the</strong> incidence of complications.<br />
<strong>Shepherd</strong> has been able to sustain<br />
a no-infection rate in ventilator-associated<br />
pneumonia for more than a year. Efforts to<br />
prevent <strong>the</strong> transmission of o<strong>the</strong>r hospitalacquired<br />
infections (for example, MRSA, a<br />
virulent staph infection, and ca<strong>the</strong>ter-related<br />
bloodstream infections) are taken very seriously.<br />
These include education of staff on hand<br />
hygiene, proper disinfection of equipment and<br />
adhering to protocols to isolate infected patients,<br />
among o<strong>the</strong>r evidence-based precautions.<br />
The intensive care unit (ICU) staff also pays<br />
careful attention to <strong>the</strong> use of antibiotics, which<br />
can kill <strong>the</strong> good bacteria in <strong>the</strong> body and cause<br />
a c. difficile infection in a patient’s intestines.<br />
Staff minimizes use of antibiotics to avoid <strong>the</strong>se<br />
infections.<br />
A Central Resource for O<strong>the</strong>rs<br />
Because of <strong>Shepherd</strong>’s success, ICUs and trauma<br />
centers at o<strong>the</strong>r facilities often call on <strong>Shepherd</strong> for<br />
assistance and best practices to identify complications<br />
and prevent common problems. Managing hospitalacquired<br />
infections or problems among SCI patients<br />
has become increasingly important to o<strong>the</strong>r facilities<br />
amid new policies by <strong>the</strong> <strong>Center</strong>s for Medicare &<br />
Medicaid Services and managed care organizations.<br />
These policies are aimed at reducing “never events,”<br />
which are considered serious, preventable and costly<br />
Fall 2009 1 7
medical errors. Medicare and o<strong>the</strong>r plans<br />
no longer pay for <strong>the</strong> treatment of <strong>the</strong>se<br />
complications, and several states have<br />
enacted laws requiring <strong>the</strong> disclosure of<br />
“never events” at hospitals.<br />
Possible Complications from SCI<br />
• Skin breakdown or “pressure sores”<br />
• Urinary tract and bowel management<br />
problems, including loss of bladder or<br />
bowel control that increases <strong>the</strong> risk of<br />
urinary tract infections<br />
• Respiratory problems, including pneumonia<br />
or ventilator dependence<br />
• Muscle spasms<br />
• Blood clots<br />
• Weight loss and muscle atrophy<br />
• Pain<br />
• Increased likelihood of new injuries, especially<br />
where <strong>the</strong>re is impaired sensation<br />
“<strong>Shepherd</strong> is both a teacher and an asset<br />
for hospitals worried about never-event costs<br />
because it’s all we do,” says Mitch Fillhaber, vice<br />
president of marketing and managed care at<br />
<strong>Shepherd</strong>. “Our acute-care capabilities provide<br />
added value for <strong>the</strong> patient, facilitate earlier referrals<br />
and also can help trauma centers turn over<br />
beds more quickly and help transition patients<br />
into rehab more quickly.”<br />
The rehabilitative environment at <strong>Shepherd</strong> gives<br />
patients – even <strong>the</strong> most severely injured – a sense<br />
of control over <strong>the</strong>ir situation. Even in <strong>the</strong> ICU,<br />
aggressive physical <strong>the</strong>rapy is started at some level,<br />
and patients are often helped out of bed and into a<br />
wheelchair.<br />
“<strong>Shepherd</strong> <strong>Center</strong> appears to have one of <strong>the</strong> most<br />
advanced programs for early treatment and strategic<br />
planning for spinal cord injury management, including<br />
having <strong>the</strong>ir own ICU,” says Julian E. Bailes,<br />
M.D., chairman of <strong>the</strong> Department of Neurosurgery<br />
at West Virginia University School of Medicine.<br />
King is most proud of <strong>the</strong> careful attention<br />
<strong>Shepherd</strong> clinicians give to every body system, from<br />
<strong>the</strong> heart and bladder to <strong>the</strong>ir sexuality and spirituality.<br />
“Our long-term outcomes are a reflection of everything<br />
we’ve done throughout <strong>the</strong> continuum of care,”<br />
she says. “And we don’t consider only acute medical or<br />
physical issues. We also take time to focus on patients’<br />
spiritual and emotional well-being.”<br />
Ahead of Its Time<br />
<strong>Shepherd</strong>’s on-site intensive care unit ensures continuity of care.<br />
Even though <strong>Shepherd</strong> <strong>Center</strong> was established 34 years ago, its founders had <strong>the</strong> foresight to<br />
structure <strong>the</strong> hospital’s care model so every aspect of spinal cord injury care would be available<br />
under one roof.<br />
In doing so, patients receive seamless, comprehensive care – from acute medical services<br />
and cutting-edge interventions that maximize rehabilitation and recovery to bridge programs that<br />
help <strong>the</strong>m transition back to <strong>the</strong>ir communities.<br />
“The founders developed a hospital for <strong>the</strong> future, where catastrophically injured patients<br />
wouldn’t have to be transferred and <strong>the</strong>re would be no disruption in care,” says Mitch Fillhaber,<br />
vice president of marketing and managed care at <strong>Shepherd</strong> <strong>Center</strong>. “Such early intervention and<br />
coordinated rehabilitation are critical for long-term recovery.”<br />
Beginning a rehabilitation regimen within two weeks of injury can lead to increases in<br />
functional improvement and more cost-effective care for people with spinal cord injury (SCI),<br />
experts say. Today, <strong>Shepherd</strong> <strong>Center</strong> remains one of only a few facilities that has an on-site<br />
intensive care unit (ICU). <strong>Shepherd</strong> accepts patients directly from a trauma center’s emergency<br />
department and aggressively starts rehabilitation from day one.<br />
“This capability allows us to admit patients earlier in <strong>the</strong> acute stage and possibly shorten<br />
<strong>the</strong>ir hospital stay by reducing <strong>the</strong> number of complications,” says Andrew Zadoff, M.D.,<br />
medical director of <strong>Shepherd</strong>’s 10-bed ICU. “We can start patients in rehabilitation even<br />
while <strong>the</strong>y’re still in <strong>the</strong> ICU. We get <strong>the</strong>m out of <strong>the</strong> bed, and that improves <strong>the</strong>ir mobility.”<br />
A team of rehabilitation and medical professionals – including orthopedists, internists<br />
and urologists – who have extensive experience in catastrophic care address individual<br />
patient needs and establish short- and long-term rehabilitation goals from <strong>the</strong> start. The<br />
ICU staff works alongside physical, occupational and speech <strong>the</strong>rapists to begin rehab as<br />
soon as possible and can draw upon <strong>the</strong> expertise of o<strong>the</strong>r specialists as needed.<br />
Dr. Zadoff is proud of <strong>Shepherd</strong>’s dedicated respiratory <strong>the</strong>rapy and nursing staffs that<br />
work collaboratively to minimize SCI-related complications (for example, skin, bladder<br />
and bowel problems, blood clots, nutritional deficiencies) and have helped contribute to<br />
low, hospital-acquired infection rates.<br />
“Our ICU nurses have both rehabilitation and critical care training, so <strong>the</strong>y look at both<br />
medical issues (<strong>the</strong> injury itself, as well as related complications) at <strong>the</strong> same time, and<br />
that benefits patients greatly,” he says. “For example, our ventilator-associated pneumonia<br />
rate is next to zero. That’s because of <strong>the</strong> way we wean patients and our careful<br />
attention to secretion control. A rate this low is unheard of in an ICU environment.”<br />
This is important because such infections can cost an extra $40,000 per episode<br />
and greatly leng<strong>the</strong>n a patient’s stay in <strong>the</strong> ICU, potentially hindering <strong>the</strong>ir rehabilitation.<br />
Having an on-site ICU has clear clinical benefits for patients. Much of <strong>the</strong> care that<br />
starts in <strong>the</strong> ICU will continue as <strong>the</strong> patient moves to a regular room and through<br />
rehabilitation to ensure seamless care for patients – and provides reassurance for<br />
patients and families who already have enough to worry about. — Amanda Crowe<br />
Photo by Gary Meek<br />
Left: <strong>Shepherd</strong> ICU<br />
charge nurse Anneka<br />
Maguigan checks on<br />
patient Tyler Epps<br />
of Lincolnton, Ga.<br />
Patients benefit from<br />
<strong>the</strong> depth and breadth<br />
of experience of<br />
<strong>Shepherd</strong> nurses like<br />
Maguigan.<br />
1 8 Spinal Column<br />
w w w. s h e p h e r d . o r g
<strong>Shepherd</strong>TVFeature<br />
<strong>Shepherd</strong> asked KPKi to incorporate <strong>the</strong> videos into a<br />
Web site linked to <strong>Shepherd</strong>’s main site. <strong>Shepherd</strong>TV.org<br />
went live in late January and has garnered nearly 1 million<br />
hits with 12,700 unique visitors from across <strong>the</strong> world.<br />
In addition, KPKi produces videos for <strong>Shepherd</strong>TV.org,<br />
following <strong>Shepherd</strong> patients during <strong>the</strong>ir stays and once<br />
<strong>the</strong>y are back home. In <strong>the</strong> past two months, <strong>the</strong> company<br />
has traveled to Lake Martin, Ala.; Nashville, Tenn.; and<br />
Boca Raton and Delray Beach, Fla., to create Stories of<br />
Hope on <strong>Shepherd</strong> graduates.<br />
Some “Stories of Hope” featured on <strong>Shepherd</strong>TV.org<br />
include:<br />
On <strong>the</strong> Net<br />
“Catch Me on <strong>Shepherd</strong>TV.org” message debuts on<br />
wheelchair sweeper vans during Peachtree Road Race.<br />
<strong>Shepherd</strong> <strong>Center</strong> has rolled out <strong>the</strong> first of several vans<br />
in its transportation fleet that are slated for a cosmetic<br />
update with colorful vehicle wraps promoting <strong>Shepherd</strong><br />
<strong>Center</strong>’s people and programs.<br />
Peachtree Road Race enthusiasts lining <strong>the</strong> race route were<br />
<strong>the</strong> first to see <strong>Shepherd</strong>’s sweeper van during <strong>the</strong> July 4 race.<br />
The vehicle wrap features messages about <strong>the</strong> <strong>Center</strong> and its<br />
video Web site, <strong>Shepherd</strong>TV.org.<br />
The van is wrapped in large photographs of <strong>Shepherd</strong><br />
Wheelchair Division Peachtree Road Race participants, along<br />
with <strong>the</strong> message “Catch Me on <strong>Shepherd</strong>TV.org.” The sweeper<br />
van travels alongside wheelchair racers competing in <strong>the</strong> race in<br />
case any of <strong>the</strong>m need help or don’t clear <strong>the</strong> course in <strong>the</strong> time<br />
allotted before foot racers begin.<br />
<strong>Shepherd</strong>TV.org was launched earlier this year to put<br />
<strong>Shepherd</strong> <strong>Center</strong>’s messages and patient success stories –<br />
called “Stories of Hope” – online with compelling, feature-style<br />
videos about <strong>Shepherd</strong> and its patients.<br />
“Online video has become an important tool to introduce a<br />
facility such as ours to families whose loved one may have just<br />
sustained a catastrophic injury or been diagnosed with a chronic<br />
illness,” says Larry Bowie, public relations director for <strong>Shepherd</strong><br />
<strong>Center</strong>. “Seeing <strong>the</strong> facility in quality HD video and hearing<br />
from our patients, <strong>the</strong>ir families, our founders, staff and physicians<br />
offers a firsthand, realistic look at a place that may become<br />
a ‘home away from home.’”<br />
<strong>Shepherd</strong>TV.org was created by KPKinteractive (KPKi) after<br />
<strong>the</strong> company completed a series of nine videos for <strong>Shepherd</strong> in<br />
2008. Because of enthusiastic reception to <strong>the</strong> videos,<br />
<strong>Shepherd</strong> <strong>Center</strong> File Photo<br />
• Stephanie Beard of Adams, Tenn., who sustained a<br />
spinal cord injury in an automobile crash in April 2007<br />
and now walks unassisted and limp-free, is a college<br />
student in Nashville, Tenn.<br />
• Jennifer Lindquist of Sussex, Wis., who sustained a<br />
spinal cord injury in a skiing accident in January 2007,<br />
can now walk with forearm crutches.<br />
• Parker King of Atlanta, who sustained brain and spinal<br />
cord injuries when he was hit by a truck in August<br />
2003, is now a student at <strong>the</strong> University of Georgia.<br />
• Alex Vazquez of Boca Raton, Fla., who sustained a<br />
severe brain injury when he was hit by a car in August<br />
2007, is now pursuing a career in video production.<br />
O<strong>the</strong>r content available on <strong>Shepherd</strong>TV.org includes videos<br />
on <strong>Shepherd</strong>’s spinal cord and brain injury rehabilitation<br />
programs, research, special events such as patients reunions,<br />
<strong>the</strong> annual Adventure Skills Workshop and <strong>the</strong> Wheelchair<br />
Division of <strong>the</strong> Peachtree Road Race.<br />
Above: <strong>Shepherd</strong> <strong>Center</strong> vans are getting a cosmetic update<br />
with colorful vehicle wraps that promote <strong>Shepherd</strong>'s people and<br />
programs, including video content posted at <strong>Shepherd</strong>TV.org.<br />
Fall 2009 1 9
Research<br />
It’s an exciting time for neuroscience, including <strong>the</strong> hope for<br />
new <strong>the</strong>rapies to treat spinal cord injury (SCI). While basic<br />
scientists and clinicians are making important advances, <strong>the</strong>y<br />
face daunting challenges when it comes to moving promising<br />
research from <strong>the</strong> bench to <strong>the</strong> bedside.<br />
To identify and address <strong>the</strong>se barriers, leading experts in neuroscience<br />
and stem cells recently came toge<strong>the</strong>r for <strong>the</strong> one-day<br />
workshop at <strong>the</strong> University of Georgia.<br />
“The concept of this workshop grew out of a need for better<br />
communication between stem cells scientists, who dared to use<br />
<strong>the</strong> term ‘cure’ for spinal cord injury, and care providers, who are<br />
worried about raising ‘false hopes’ and setting unrealistic goals<br />
for people with spinal cord injury,” says Ann Kiessling, Ph.D.,<br />
associate professor of surgery at Harvard Medical School and<br />
director of <strong>the</strong> Bedford Stem Cell Research Foundation, which<br />
organized <strong>the</strong> second annual ga<strong>the</strong>ring in cooperation with<br />
<strong>Shepherd</strong> <strong>Center</strong>. “Both groups clearly have <strong>the</strong> patient’s best<br />
interest at heart, but were not hearing each o<strong>the</strong>r’s concerns.”<br />
A key challenge for people with SCI is <strong>the</strong> concern among<br />
clinicians that any direct intervention at <strong>the</strong> site of <strong>the</strong> injury<br />
could impose fur<strong>the</strong>r damage and additional loss of function,<br />
Dr. Kiessling says. “They are understandably reluctant to expose<br />
<strong>the</strong>ir patients to <strong>the</strong> risk of fur<strong>the</strong>r spinal cord damage for<br />
research purposes,” she adds.<br />
There is also a lack of infrastructure within <strong>the</strong> SCI research<br />
community to support multi-center studies, and to define how<br />
studies in SCI can be made safe and relevant to human patients.<br />
Keith Tansey, M.D., Ph.D., director of spinal cord injury research<br />
at <strong>Shepherd</strong>, spoke to <strong>the</strong> group about <strong>the</strong> need to ensure<br />
animal studies are more relevant to humans.<br />
“Humans aren’t necessarily just big rats, and we need to better<br />
understand how and why animals are recovering from SCI<br />
because <strong>the</strong> mechanisms may not be <strong>the</strong> same in humans,”<br />
Dr. Tansey says. “Studies of animals and humans with incomplete<br />
injuries reveal a bias toward spinal plasticity in animals<br />
and brain plasticity in humans as <strong>the</strong> reason for functional<br />
recovery, so treatments may need to be different. In complete<br />
injuries, spinal circuits in rodents can regain stepping, but<br />
humans can’t, so we need to learn how to make human spinal<br />
cords function like rats’.”<br />
Dr. Kiessling agrees, adding that animal model research needs<br />
to be more carefully aligned with human injuries and <strong>the</strong> outto<br />
Bedside<br />
From Bench<br />
Leading experts in basic science and clinical care discuss barriers to a “cure”<br />
for spinal cord injury. By Amanda Crowe, MA, MPH<br />
come goals for human <strong>the</strong>rapies. “If walking is <strong>the</strong> outcome<br />
measure, animal models need to reflect that. But if bladder<br />
control is what’s important, a different animal model may be<br />
needed,” she says.<br />
Researchers and clinicians must gain a better understanding<br />
of how much recovery is due to re-establishment of brainspinal<br />
cord connections versus improvements in interpreting<br />
and using sensory information in <strong>the</strong> spinal cord below <strong>the</strong><br />
level of injury. Dr. Tansey challenged <strong>the</strong> traditional view of<br />
translational research in which discoveries at <strong>the</strong> cellular level<br />
move from <strong>the</strong> lab to clinical practice, arguing that it should<br />
be more of a two-way street. That is, questions that arise in <strong>the</strong><br />
clinical setting can go back to <strong>the</strong> lab to find answers. O<strong>the</strong>r<br />
attendees said this model could help inspire greater communication<br />
and partnership, as well.<br />
A memorable highlight of <strong>the</strong> workshop was a tour of<br />
<strong>Shepherd</strong> <strong>Center</strong>, <strong>the</strong> only specialty rehabilitation center in<br />
<strong>the</strong> country that combines intensive medical care, rehabilitation<br />
and a clinical research program under one roof. This visit<br />
gave basic scientists a chance to see what <strong>the</strong>ir work can do at<br />
<strong>the</strong> human level, well beyond studying cell biology in <strong>the</strong> lab.<br />
“We could have held this workshop anywhere in <strong>the</strong><br />
country, but we were impressed by <strong>the</strong> clear enthusiasm and<br />
determination of <strong>Shepherd</strong>’s leadership, particularly Alana<br />
<strong>Shepherd</strong>, in creating a unique center of excellence in patient<br />
care,” Dr. Kiessling says.<br />
Still, experts say <strong>the</strong> complexity of SCI cannot be overstated,<br />
and <strong>the</strong>re is no silver bullet – no single cell, no single<br />
surgery, no single nerve-growth factor that will solve <strong>the</strong><br />
whole riddle. “The more realistic expectation is that a combination<br />
of incremental steps is needed to improve recovery and<br />
maximize function,” Dr. Tansey says. “There is huge potential<br />
with stem cell biology and cell-replacement <strong>the</strong>rapies, but<br />
<strong>the</strong>re’s also a long distance between where we are today and<br />
where we need to be to find a ‘cure.’”<br />
Collaborations among <strong>the</strong>se leading experts will help<br />
forge <strong>the</strong> path forward. In <strong>the</strong> meantime, patients and <strong>the</strong>ir<br />
families should be encouraged by <strong>the</strong> progress made thus far,<br />
experts say. Prevention and early intervention, regeneration<br />
<strong>the</strong>rapies at <strong>the</strong> cellular and extra-cellular levels and aggressive<br />
rehabilitation are all contributing to significant neurological<br />
recovery after SCI.<br />
2 0 Spinal Column<br />
w w w. s h e p h e r d . o r g
ManagedCareCorner<br />
Why <strong>Shepherd</strong><br />
By Colleen McCrory, <strong>Shepherd</strong> <strong>Center</strong> Director of Marketing and Managed Care<br />
Photo by Gary Meek<br />
I am continually challenged by<br />
managed care payers, referring hospital<br />
systems, patients and families<br />
with <strong>the</strong> question “Why <strong>Shepherd</strong>?”<br />
when <strong>the</strong>y are considering rehabilitation<br />
options.<br />
While I try to verbalize our<br />
strengths, outcomes, and earlyintervention<br />
ICU and o<strong>the</strong>r levels<br />
along our continuum of care, <strong>the</strong><br />
message sometimes isn’t conveyed or<br />
received – as compelling as I think <strong>the</strong> verbal “evidence” might be.<br />
Showcasing <strong>Shepherd</strong> <strong>Center</strong>’s specialization in <strong>the</strong> treatment of<br />
spinal cord and brain injuries and multiple traumas in a conversation<br />
just isn’t enough.<br />
Working in conjunction with our Quality, Resources and<br />
Outcomes Department, we’ve assembled a compelling outcomes<br />
scorecard. It illustrates why we are not a general rehabilitation<br />
hospital like <strong>the</strong> majority of facilities you encounter or consider for<br />
<strong>the</strong> care of your member, patient, client or loved one. Here’s why:<br />
<strong>Shepherd</strong> <strong>Center</strong> is ranked by U.S. News and World Report<br />
as one of <strong>the</strong> top 10 best rehabilitation hospitals in <strong>the</strong> nation.<br />
This is <strong>the</strong> type of news<br />
you expect to hear about<br />
<strong>Shepherd</strong> <strong>Center</strong>. After all,<br />
we’re <strong>the</strong> only rehabilitation<br />
facility in <strong>the</strong> nation with an<br />
intensive care unit and acute<br />
medical component on site,<br />
allowing us to begin <strong>the</strong> rehabilitation process sooner than o<strong>the</strong>r<br />
rehabilitation hospitals.<br />
Our specialization has enabled our staff to develop higher levels<br />
of expertise and achieve better results and outcomes for our<br />
patients. When it comes to independence, functional improvement<br />
and prevention of secondary complications, our patients are<br />
more independent and have better outcomes than <strong>the</strong> national<br />
average. In fact our patient outcomes are among <strong>the</strong> best in <strong>the</strong><br />
United States.<br />
As part of <strong>Shepherd</strong> <strong>Center</strong>’s efforts and a growing trend<br />
among hospitals to be transparent in terms of patient outcomes,<br />
Transparency of data can help families,<br />
referral sources and <strong>the</strong> medical community<br />
make more informed decisions on <strong>the</strong> care<br />
of <strong>the</strong>ir loved ones and patients.<br />
we have included our data in this issue of Spinal Column in a<br />
removable fact sheet attached to this page. So when you ask,<br />
“Why <strong>Shepherd</strong>?,” you have documentation of <strong>the</strong> evidence.<br />
The fact sheet is composed of four sections – data on early<br />
intervention, independence, prevention and evidence.<br />
Early intervention focuses on <strong>Shepherd</strong> <strong>Center</strong>’s ventilatorweaning<br />
rates with respect to clinical acuity, secondary<br />
diagnoses and co-morbidities. The prevention data reflects<br />
<strong>the</strong> “never-event” occurrences and an approximate cost of<br />
such occurrences, which highlights potential cost-savings<br />
associated with admissions to <strong>Shepherd</strong> <strong>Center</strong>.<br />
All rehabilitation hospitals measure patient results in terms<br />
of “functional improvement” as measured by <strong>the</strong> FIM rating<br />
scale. The independence section of outcomes showcases<br />
<strong>Shepherd</strong> <strong>Center</strong>’s average FIM change for both spinal<br />
cord and brain injuries, as well as <strong>the</strong> percentage of patients<br />
returned to <strong>the</strong>ir home community ra<strong>the</strong>r than a long-term<br />
care facility.<br />
Finally, <strong>the</strong> evidence quadrant focuses on <strong>Shepherd</strong>’s<br />
dedication to a unique patient population, <strong>the</strong> specialization<br />
associated with more than 33 years of care for <strong>the</strong>se patients,<br />
<strong>the</strong> volume of patients seen and <strong>the</strong>ir average age. And, as <strong>the</strong><br />
only free-standing rehabilitation<br />
facility in <strong>the</strong> country<br />
with an ICU level-of-care,<br />
<strong>Shepherd</strong> <strong>Center</strong>’s average<br />
length-of-stay in ICU and <strong>the</strong><br />
number of admissions to our<br />
ICU quarterly fur<strong>the</strong>r reflect<br />
<strong>Shepherd</strong> <strong>Center</strong>’s highly specialized continuum of care.<br />
As I am continually challenged by our potential referring<br />
hospitals, payers and patients, I challenge each of you to ask<br />
for <strong>the</strong> same outcomes data from our rehabilitation facility<br />
peers. Transparency of data can help families, referral sources<br />
and <strong>the</strong> medical community make more informed decisions<br />
on <strong>the</strong> care of <strong>the</strong>ir loved ones and patients.<br />
If you have any questions or would like to discuss <strong>the</strong>se<br />
outcomes in more detail, please contact me or Susan Bowen,<br />
director of our Quality, Resources and Outcomes<br />
Department, at 404-352-2020.<br />
Fall 2009 2 1
Early Intervention<br />
Level of Injury<br />
C1 - C2 7<br />
C3<br />
C4<br />
C5 - C7<br />
T1 - T12<br />
L1 - L5<br />
Rancho 1 - 3<br />
Total Volume<br />
6<br />
25<br />
25<br />
6<br />
1<br />
13<br />
2007 2008<br />
Ventilator-weaning data is analyzed<br />
annually by Andrew Zadoff,<br />
M.D., medical director, ICU and<br />
PulmonaryServices.<br />
Data includes patients admitted within<br />
<strong>the</strong> calendar year.<br />
# D/C Home on Vent<br />
4<br />
2<br />
3<br />
3<br />
0<br />
0<br />
3<br />
# Weaned<br />
3<br />
4<br />
22<br />
22<br />
6<br />
1<br />
10<br />
Avg Days to Wean<br />
-<br />
8<br />
23<br />
16<br />
18<br />
8<br />
7<br />
Wean Rate<br />
42.9%<br />
66.7%<br />
88%<br />
88%<br />
100%<br />
100%<br />
76.9%<br />
Level of Injury<br />
C1 - C2<br />
C3<br />
C4<br />
C5 - C7<br />
T1 - T12<br />
Rancho 1 - 3<br />
Total Volume<br />
12<br />
6<br />
27<br />
26<br />
18<br />
6<br />
# D/C Home on Vent<br />
9<br />
4<br />
4<br />
2<br />
2<br />
1<br />
# Weaned<br />
3<br />
2<br />
22<br />
24<br />
15<br />
5<br />
Avg Days to Wean<br />
27<br />
21<br />
24<br />
13<br />
20<br />
12<br />
Wean Rate<br />
25%<br />
33.3%<br />
81.5%<br />
92.3%<br />
83.3%<br />
83.3%<br />
Patients excluded from population:<br />
• Patients with a primary diagnosis<br />
o<strong>the</strong>r than SCI or ABI.<br />
• Patients who have not<br />
discharged by reporting cut-off<br />
date.<br />
• Patients whose injury level is<br />
not complex and are, <strong>the</strong>refore,<br />
“expected” to wean.<br />
SCI/ABI dual diagnosis patients are<br />
reported according to <strong>the</strong>ir spinal<br />
cord injury level.<br />
Independence<br />
90<br />
75<br />
60<br />
45<br />
Discharge Total FIM ®<br />
Total Spinal Cord Injury<br />
85.0<br />
80.1<br />
Q3<br />
2008<br />
83.3<br />
81.6<br />
Q4<br />
2008<br />
88.4<br />
83.2<br />
Q1<br />
2009<br />
85.8<br />
80.9<br />
Q2<br />
2009<br />
40<br />
30<br />
20<br />
10<br />
28.7<br />
28.9<br />
Q3<br />
2008<br />
<strong>Shepherd</strong><br />
Nation<br />
Total FIM ® Change<br />
Total Brain Injury<br />
33.2<br />
29.7<br />
Q4<br />
2008<br />
30.1<br />
26.9<br />
Q1<br />
2009<br />
30.3<br />
29.0<br />
Q2<br />
2009<br />
Story Behind <strong>the</strong> Data<br />
Wean Rates<br />
• Data represents medically complex patients only.<br />
• Influenced by clinical acuity and primary/<br />
secondary diagnoses, <strong>the</strong> following are<br />
considered significant influences in determining<br />
<strong>the</strong> potential capability to wean a patient from<br />
ventilator assistance:<br />
• Level of injury<br />
• Patient age<br />
• Complete vs. incomplete spinal cord injury<br />
• Co-morbidity<br />
Discharge to Community<br />
• Rate is high because of <strong>Shepherd</strong> <strong>Center</strong> family<br />
education programs and continued support of<br />
families in <strong>the</strong>ir homes.<br />
Discharge to Community<br />
100%<br />
75%<br />
50%<br />
25%<br />
Total Spinal Cord Injury<br />
90.1%<br />
74.2%<br />
Q3<br />
2008<br />
92.8%<br />
74.7%<br />
Q4<br />
2008<br />
93.1%<br />
73.1%<br />
Q1<br />
2009<br />
87.8%<br />
74.8%<br />
Q2<br />
2009<br />
100%<br />
75%<br />
50%<br />
25%<br />
Total Brain Injury<br />
Source: UDS Quarterly Trends Report M240_9021 (July 1, 2008 – June 30, 2009) unless o<strong>the</strong>rwise cited.<br />
91.9%<br />
70.0%<br />
Q3<br />
2008<br />
93.5%<br />
68.8%<br />
Q4<br />
2008<br />
92.2%<br />
70.0%<br />
Q1<br />
2009<br />
91.0%<br />
70.7%<br />
Q2<br />
2009<br />
• Discharge Total FIM ® (Total SCI) Published quarterly by UDS.<br />
The functional assessment instrument is composed of 18<br />
items rated on a seven-level scale that represents gradations<br />
in function from independence to complete dependence.<br />
Measured at discharge to <strong>the</strong> rehabilitation program.<br />
• Total FIM ® Change (Total Brain Injury) Published quarterly<br />
by UDS. The difference in FIM ® Score as measured at<br />
discharge to <strong>the</strong> rehabilitation program and admission to <strong>the</strong><br />
rehabilitation program.<br />
• Discharge to Community (Total Spinal Cord Injury and Total Brain<br />
Injury) Published quarterly by UDS. The percentage of patients<br />
who return to a community-based setting, including a home<br />
(of <strong>the</strong> patient, relative or ano<strong>the</strong>r person), transitional living<br />
setting, board and care setting, or assisted living residence.
Why <strong>Shepherd</strong><br />
Evidence<br />
ICU Statistics<br />
General Statistics<br />
6.0<br />
5.0<br />
4.0<br />
3.0<br />
2.0<br />
1.0<br />
0.0<br />
ICU Average LOS<br />
(in days)<br />
5.64<br />
Q3<br />
2008<br />
5.70<br />
Q4<br />
2008<br />
5.60<br />
Q1<br />
2009<br />
5.09<br />
Q2<br />
2009<br />
Source for Both ICU Statistics: <strong>Shepherd</strong> <strong>Center</strong> Internal Databases<br />
Prevention<br />
Raw # Cases/Month<br />
Raw # Cases/Month<br />
Raw # Cases/Month<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
Jul<br />
08<br />
Jul<br />
08<br />
Jul<br />
08<br />
Aug<br />
08<br />
Ventilator-Associated Pneumonia<br />
Oct<br />
08<br />
Wounds Requiring Surgical Intervention<br />
Aug<br />
08<br />
Oct<br />
08<br />
Ca<strong>the</strong>ter-Related Blood Stream Infections<br />
Aug<br />
08<br />
Sept<br />
08<br />
Sept<br />
08<br />
Sept<br />
08<br />
Oct<br />
08<br />
60<br />
40<br />
20<br />
0<br />
Nov<br />
08<br />
Nov<br />
08<br />
Nov<br />
08<br />
57<br />
ICU Admissions<br />
Source for Chart Data Below (Not Cost<br />
Data): <strong>Shepherd</strong> <strong>Center</strong> Internal Databases<br />
Dec<br />
08<br />
Dec<br />
08<br />
Dec<br />
08<br />
Jan<br />
09<br />
Cost = $40,000/infection<br />
Cost = $1,600/day; Patients<br />
three times more likely to D/C to LTCH<br />
Jan<br />
09<br />
Jan<br />
09<br />
Feb<br />
09<br />
Feb<br />
09<br />
Feb<br />
09<br />
Mar<br />
09<br />
Mar<br />
09<br />
Cost = $45,000/infection<br />
Mar<br />
09<br />
Apr<br />
09<br />
Apr<br />
09<br />
Apr<br />
09<br />
May<br />
09<br />
Source: UDS Office of Quality and Performance (10Q). FY 2008, Q1 technical manual for <strong>the</strong><br />
VHA performance measurement system. Washington (DC); 2007 Oct 31. 315 p.<br />
May<br />
09<br />
Source: Russo, C.A. (Thomson Reuters), Steiner, C. (AHRQ) and Spector, W. (AHRQ).<br />
Hospitalizations Related to Pressure Ulcers, 2006. HCUP Statistical Brief #64. December 2008.<br />
Agency for Healthcare Research and Quality, Rockville, MD.<br />
May<br />
09<br />
Source: "An intervention to decrease ca<strong>the</strong>ter-related bloodstream infections in <strong>the</strong> ICU,"<br />
by Dr. Pronovost, Dale Needham, M.D., Ph.D., Sean Berenholtz, M.D., and o<strong>the</strong>rs, in <strong>the</strong><br />
December 28, 2006, New England Journal of Medicine 355(26), pp. 2725-2732.<br />
43<br />
Q3<br />
2008<br />
51<br />
29<br />
Q4<br />
2008<br />
38<br />
25<br />
Q1<br />
2009<br />
57<br />
39<br />
Q2<br />
2009<br />
All Patients Admitted Directly to ICU<br />
ICU Patients Admitted Within 30<br />
Days of Injury<br />
160<br />
140<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
Jun<br />
09<br />
Jun<br />
09<br />
Jun<br />
09<br />
ABI SCI All Patients<br />
300<br />
77<br />
Discharge Volume<br />
216 207 249 249<br />
107<br />
Q3<br />
2008<br />
77<br />
95<br />
Q4<br />
2008<br />
93<br />
96<br />
Q1<br />
2009<br />
91<br />
87<br />
Q2<br />
2009<br />
250<br />
200<br />
150<br />
100<br />
50<br />
Source: <strong>Shepherd</strong> <strong>Center</strong> Internal Databases<br />
0<br />
Average Patient Age/# <strong>Shepherd</strong> Cases<br />
<strong>Shepherd</strong><br />
Total SCI<br />
Nation<br />
Total SCI<br />
<strong>Shepherd</strong><br />
Total Brain<br />
Nation<br />
Total Brain<br />
<strong>Shepherd</strong><br />
Total Stroke<br />
Nation<br />
Total Stroke<br />
Q3<br />
2008<br />
Q4<br />
2008<br />
Q1<br />
2009<br />
Q2<br />
2009<br />
Avg. Age 37.3 38.5 41.2 37.9<br />
# Cases<br />
Avg. Age<br />
Avg. Age<br />
# Cases<br />
Avg. Age<br />
Avg. Age<br />
# Cases<br />
Avg. Age<br />
71 69 72 82<br />
47.1 50.5 52.3 50.4<br />
33.3 32.5 33.4 32.9<br />
37 46 51 67<br />
58.1 56.8 61.1 59.8<br />
45.3 44.8 48.6 42.8<br />
9 15 11 18<br />
67.2 67.7 68.2 67.5<br />
Source: UDS Quarterly Trends Report M240_9021 (July 1,<br />
2008 – June 30, 2009)<br />
Evidence<br />
General Statistics<br />
Discharge Volume<br />
• ABI population includes: Medical and rehabilitation patients with an<br />
impairment code of “ABI” (no dual diagnosis patients).<br />
• SCI population includes: Medical and rehabilitation patients with an<br />
impairment code of “SCI” (no dual diagnosis patients).<br />
• Average Patient Age / # <strong>Shepherd</strong> Cases: Published quarterly by Uniform<br />
Data System (UDS). All <strong>Shepherd</strong> patients are not reported to UDS. UDS<br />
requires patients to receive at least three hours of <strong>the</strong>rapy per day to be<br />
included in <strong>the</strong> dataset.<br />
ICU Statistics<br />
• ICU Average Length of Stay (LOS): Data collected from <strong>Shepherd</strong><br />
financial system. Average number of days <strong>Shepherd</strong> patients stayed in<br />
ICU per episode of care during <strong>the</strong> reporting period.<br />
•ICU Admissions: Data collected from <strong>Shepherd</strong> financial system. All<br />
patients admitted directly to ICU (compares first date of stay in ICU to a<br />
patient’s admission date to see if <strong>the</strong>y were admitted directly to ICU). ICU<br />
patients admitted within 30 days of injury (from <strong>the</strong> above pool of patients<br />
who were admitted directly to ICU; compares date of injury to admission<br />
date to see if <strong>the</strong>y were admitted to <strong>Shepherd</strong> within 30 days of injury).<br />
Prevention<br />
• Ventilator-Associated Pneumonia: Cases reported by <strong>Shepherd</strong> <strong>Center</strong><br />
Infection Control. Figure reflects number of healthcare-associated<br />
infections of patients on ventilators.<br />
• Wounds Requiring Surgical Intervention Cases reported by <strong>Shepherd</strong><br />
<strong>Center</strong> wound nurse. Figure reflects number of<br />
patients with hospital-acquired wounds.<br />
• Ca<strong>the</strong>ter-Related Blood Stream Infection: Cases reported by<br />
<strong>Shepherd</strong> <strong>Center</strong> Infection Control. Figure reflects blood stream infections<br />
where central venous line (CVL) or peripherally inserted central ca<strong>the</strong>ter<br />
(PICC) is <strong>the</strong> primary source of infection.
PatientProfile<br />
Flying<br />
HighBy Bill Sanders<br />
Former patient<br />
overcomes trauma and<br />
tense situation, <strong>the</strong>n<br />
earns a pilot’s license.<br />
Above and Following Page: Mal Zackery, a former<br />
spinal cord injury patient from Atlanta, underwent<br />
flight training through <strong>the</strong> Able Flight scholarship<br />
program in an adapted Sky Arrow 600 LSA with Matt<br />
Hansen of Hansen Air Group based at McCollum<br />
Field in Kennesaw, Ga. Some 38 hours of flying time<br />
later, Mal earned his pilot’s license – but not until<br />
after an emergency landing incident.<br />
Photos by Leita Cowart<br />
Somehow, Mal Zackery doesn’t seem shell-shocked at all. In<br />
<strong>the</strong> course of less than two years, <strong>the</strong> 29-year-old Atlantan was<br />
shot during a robbery and left paralyzed below <strong>the</strong> waist and<br />
was <strong>the</strong>n involved in a harrowing emergency landing of a small<br />
airplane on a busy Georgia highway. The latter captured live<br />
national media coverage.<br />
That Mal lived through those two incidents is miracle enough. That<br />
he came out determined, happy and focused is more than a miracle. It’s<br />
a testament to his inner strength and <strong>the</strong> positive spirit that <strong>Shepherd</strong><br />
<strong>Center</strong> staff reinforced in him every day he spent in rehabilitation at<br />
<strong>the</strong> hospital.<br />
“The care at <strong>Shepherd</strong> was <strong>the</strong> best,” Mal says. “They taught me<br />
how to do <strong>the</strong> things I’d need to do in my everyday life, and <strong>the</strong>y kept<br />
it real upbeat. It’s a hard enough time as it is, and <strong>the</strong> last thing you’d<br />
need is for people to be all heavy and depressing. It wasn’t like that at<br />
all. They informed me of everything I needed to know, but <strong>the</strong>y always<br />
kept it positive.”<br />
Mal came to <strong>Shepherd</strong> after being shot by a gunman in Montgomery,<br />
Ala., who robbed him and a fellow employee as <strong>the</strong>y were making a bank<br />
deposit after hours. The gunman demanded <strong>the</strong> money and Mal’s car.<br />
“The next thing I know, I hear a gunshot and I collapse,” Mal<br />
recalls. “There was no blood really, but I went down and couldn’t move<br />
my legs, had no feeling, and I knew what had happened.”<br />
Mal spent about 10 days at Jackson Hospital in Montgomery.<br />
Almost from <strong>the</strong> beginning, <strong>the</strong> staff <strong>the</strong>re encouraged him to transfer<br />
to <strong>Shepherd</strong> for rehabilitation. “They were very nice, showing me<br />
brochures about <strong>Shepherd</strong>,” he recalls. “When I got to <strong>Shepherd</strong>, it was<br />
<strong>the</strong> best.”<br />
Mal sustained a T-12 to L-1 incomplete spinal cord injury. But it<br />
was <strong>the</strong> worst kind of incomplete injury, Mal says, and he has regained<br />
very little movement in his legs.<br />
During his time as both an inpatient and outpatient, <strong>Shepherd</strong>’s<br />
<strong>the</strong>rapeutic recreation <strong>the</strong>rapists urged Mal to find an activity that<br />
2 2 Spinal Column<br />
w w w. s h e p h e r d . o r g
interested him. They suggested basketball or swimming, but Mal<br />
just wasn’t interested.<br />
“I tried every angle possible to get him involved, and <strong>the</strong>re<br />
wasn’t much that got through,” recalls Ashleigh Koontz, a <strong>the</strong>rapeutic<br />
recreation specialist. “He was resistant to participating in<br />
much more than physical and occupational <strong>the</strong>rapy because he<br />
was not someone who was open to <strong>the</strong> idea of participating in<br />
those things he once loved to do – now from a wheelchair.”<br />
Then someone told him about Able Flight, which provides<br />
flight training scholarships for people with disabilities.<br />
“It was <strong>the</strong> first time I saw a sparkle in his eye, and from what<br />
I can remember, <strong>the</strong> first time in a long time I saw that smile,”<br />
Ashleigh says. “It wasn’t long after hearing about Able Flight that<br />
Mal took <strong>the</strong> necessary steps and applied for <strong>the</strong> scholarship.”<br />
Mal wrote an essay for <strong>the</strong> scholarship application and was<br />
accepted into <strong>the</strong><br />
program. Within a<br />
few weeks, he began<br />
flight training in an<br />
adapted Sky Arrow<br />
600 LSA with Matt<br />
Hansen of Hansen<br />
Air Group based at<br />
McCollum Field<br />
in Kennesaw, Ga.<br />
Some 38 hours of flying time later, Mal earned his pilot’s license<br />
– but not until after <strong>the</strong> emergency landing incident.<br />
Here’s Mal’s recollection, in his words:<br />
“We had some hints that things weren’t perfect. The oil<br />
temperature was high as it had been on <strong>the</strong> previous flight, but<br />
no one thought that was a big deal. So I was flying it, and we’d<br />
climbed to about 2,500 feet when my instructor and I started<br />
smelling smoke.<br />
We looked around to see if <strong>the</strong>re was something burning on<br />
<strong>the</strong> ground, but we saw smoke coming from <strong>the</strong> cockpit.<br />
“The instructor took over and shut off most of <strong>the</strong> electrical<br />
stuff. Then he had me try to turn <strong>the</strong> radio back on, and it<br />
wouldn’t work. He told me to try <strong>the</strong> master switch, and when I<br />
switched it, everything went off. We were flying with no engine,<br />
and <strong>the</strong>re was nowhere to land except Cobb Parkway (a busy<br />
four-lane highway in suburban Atlanta).<br />
“We flew right over two trucks, whose drivers saw what was<br />
happening, and <strong>the</strong>y stopped and blocked traffic behind <strong>the</strong>m.<br />
And we landed <strong>the</strong>re on <strong>the</strong> road. It was a perfect landing. It<br />
really wasn’t that scary because we train for that, and we knew<br />
<strong>the</strong> landing itself would be<br />
easy. It was just a matter of<br />
having a place to land.”<br />
Within a couple weeks<br />
later, Mal was back in<br />
<strong>the</strong> cockpit of <strong>the</strong> same<br />
airplane. “The first time was<br />
a bit tense,” he recalls. “But<br />
after that, all was good.”<br />
Mal’s instructor, Matt<br />
Hansen, praises both Able Flight and Mal, who was <strong>the</strong><br />
organization’s 12th scholarship student.<br />
“We’ve worked with Able Flight from <strong>the</strong> beginning because<br />
it’s something we feel strongly about,” Matt says. “Mal’s done<br />
great. He’s right where he ought to be in his flying schedule.”<br />
“It was <strong>the</strong> first time I saw a sparkle in his eye, and from<br />
what I can remember, <strong>the</strong> first time in a long time I saw<br />
that smile. It wasn’t long after hearing about Able Flight<br />
that Mal took <strong>the</strong> necessary steps and applied for <strong>the</strong><br />
scholarship.” — Ashleigh Koontz, <strong>Shepherd</strong> <strong>Center</strong> recreation <strong>the</strong>rapist<br />
Fall 2009 2 3
Q+A<br />
ask <strong>the</strong> Doc<br />
<strong>Shepherd</strong> <strong>Center</strong> physicians answer medical questions from patients and family members.<br />
Q: What infertility problems are found in people with<br />
spinal cord injury?<br />
A: Most spinal cord injury (SCI) patients with infertility issues<br />
are men. Women may be concerned about obstetrical<br />
issues and complications – depending on whe<strong>the</strong>r <strong>the</strong>y<br />
have lung, kidney, neurologic and clotting problems. If<br />
women are over 35, <strong>the</strong> normal issues with achieving<br />
a pregnancy relate to age, ra<strong>the</strong>r than <strong>the</strong>ir SCI status.<br />
But if <strong>the</strong>re are medical concerns regarding carrying a<br />
pregnancy successfully, a gestational carrier (surrogate)<br />
can be used through in vitro fertilization (IVF).<br />
Men with SCI may have varying types of erectile<br />
dysfunction (ED) that may lead to infertility. It is important<br />
to have a semen analysis (SA) to determine what options<br />
are available for treatment. But many men with more<br />
extensive injuries may need to have electroejaculation<br />
(EEJ) to determine what treatment is indicated for<br />
achieving a pregnancy.<br />
If <strong>the</strong> SA is normal and <strong>the</strong> spouse is under age 35,<br />
ovulation induction with Clomid can be used with<br />
intrauterine inseminations (IUI) with a success rate<br />
of 8 to 12 percent per cycle. If <strong>the</strong> woman is over 35,<br />
medications may need to be more extensive with<br />
injectable drugs that can increase results up to 20<br />
percent. EEJ can cause concern because it may have<br />
to be done under anes<strong>the</strong>sia, and repeated procedures<br />
may irritate <strong>the</strong> rectal mucosa.<br />
Most couples in <strong>the</strong>se situations should do IVF so an EEJ<br />
may be done only once, if possible. The success rate can<br />
be 45 to 50 percent, depending on <strong>the</strong> woman’s age. If<br />
sperm aspiration or testicular sperm extraction (TESE) is<br />
needed due to a failed EEJ or extremely low sperm count,<br />
IVF is <strong>the</strong> only option for achieving a pregnancy.<br />
When a couple is considering a pregnancy with known<br />
issues, <strong>the</strong>y should consult with a urologist specializing<br />
in male infertility. This may be done in combination with<br />
a reproductive endocrinologist and infertility specialist.<br />
Each case is individualized. Overall, pregnancy rates are<br />
excellent, and if IVF is considered, most couples will have<br />
a sufficient number of embryos stored to complete <strong>the</strong>ir<br />
family with one cycle if all factors are optimal.<br />
— Dorothy Mitchell-Leef, M.D.<br />
Q: Do I really need to start one of <strong>the</strong> injectable medications if I've<br />
just been diagnosed with relapsing-remitting MS? Can’t I just<br />
wait and see how things go over <strong>the</strong> next couple of years?<br />
A: There are several reasons to strongly consider starting an injectable<br />
medication soon after a diagnosis of relapsing-remitting MS.<br />
1) Nerve fiber damage may occur early in MS. For years, MS was<br />
thought to involve mainly damage to <strong>the</strong> insulation (myelin) of <strong>the</strong><br />
nerve fibers (axons) in <strong>the</strong> brain and/or spinal cord. This is referred to<br />
as demyelination. In 1998, researchers confirmed that MS also can<br />
damage axons <strong>the</strong>mselves. This damage is permanent and leads to<br />
disability. It has been shown to occur early in MS. Starting<br />
an injectable MS <strong>the</strong>rapy early may help prevent this.<br />
2) MS changes over time. Without treatment, most people with<br />
relapsing-remitting MS will move toward secondary progressive<br />
MS. This form of MS does not respond well to currently approved<br />
<strong>the</strong>rapies and is characterized by a steady accumulation of disability.<br />
Starting treatment early may slow or prevent this move from<br />
relapsing-remitting to secondary progressive MS.<br />
3) While benign forms of MS exist, we are not good at predicting who<br />
might follow a milder course. We have some clues in early MS that<br />
may point toward someone doing well versus someone who’s<br />
going to have a more aggressive course, but most MS healthcare<br />
providers would not feel confident enough in <strong>the</strong>m to recommend<br />
absolutely against starting <strong>the</strong>rapy. — Ben Thrower, M.D.<br />
contributors<br />
Submit your questions for “Ask <strong>the</strong> Doc”<br />
to jane_sanders@shepherd.org or via<br />
fax at 404-350-3145<br />
Dorothy Mitchell-Leef, M.D.,<br />
<strong>Shepherd</strong> consulting physician,<br />
reproductive endocrinologist<br />
and infertility<br />
specialist with Reproductive<br />
Biology Associates<br />
Ben Thrower, M.D., medical<br />
director of <strong>the</strong> Andrew C.<br />
Carlos Multiple Sclerosis<br />
Institute at <strong>Shepherd</strong> <strong>Center</strong><br />
2 4 Spinal Column<br />
w w w. s h e p h e r d . o r g
Q&A<br />
Q+A<br />
with John Lin, M.D., Associate Medical<br />
Director of Post-Acute Services<br />
Interviewed by Kayla Eubanks<br />
Q: How did you come to <strong>Shepherd</strong> <strong>Center</strong> – both as a<br />
patient and a doctor?<br />
A: In 1991, I had an aneurysm-like condition known as epidural<br />
arteriovenous malformation, which left me paralyzed. At <strong>the</strong><br />
time, I was on summer break from college, visiting my parents<br />
in Charleston. A <strong>Shepherd</strong> <strong>Center</strong> admissions liaison came to<br />
my hospital to discuss rehabilitation options. I had never heard<br />
of <strong>Shepherd</strong> <strong>Center</strong> before – like most people who had no<br />
reason to. However, it was apparent to me that <strong>the</strong> <strong>Center</strong> had<br />
<strong>the</strong> expertise I needed since it treated more spinal cord injuries<br />
than <strong>the</strong> average rehabilitation facility.<br />
After my discharge, I wanted to practice medicine. I spoke<br />
with (Medical Director) Dr. Donald Leslie who mentored me<br />
before, during and after medical school. When I completed my<br />
residency, we discussed my joining <strong>Shepherd</strong>, but <strong>the</strong> timing<br />
wasn’t right. I practiced general rehab medicine for a while and<br />
worked at a VA hospital for a few years. Then in 2005, I joined<br />
<strong>the</strong> <strong>Shepherd</strong> medical staff.<br />
Q: What is it like going from patient to doctor? Does that<br />
make your approach unique from o<strong>the</strong>r physicians?<br />
A: It was a transformative process. At first, it was difficult to<br />
readjust my mindset. I found myself getting lost in patients’<br />
tragic stories. It became difficult to hear again and again. To<br />
be emotionally immersed was draining and did not allow me<br />
to be as objective as necessary. As a doctor, you have to<br />
be objective. Today, I am better able to find a balance: Be<br />
empathic when I can, but be objective when possible.<br />
Q: Explain how your experience in internal medicine and<br />
physical medicine and rehabilitation (PM&R) work<br />
toge<strong>the</strong>r to benefit your patients.<br />
A: Internal medicine is <strong>the</strong> prevention, diagnosis and care of<br />
general illness, disease and injury. Having knowledge in both<br />
fields makes it easier to take patients from acute injury to<br />
preventative treatment.<br />
I find myself able to see things happening and prevent it, ra<strong>the</strong>r<br />
than having to deal with <strong>the</strong> consequences. For <strong>the</strong> patient,<br />
it’s better because <strong>the</strong>re are many interactions with <strong>the</strong> various<br />
medications that require deeper knowledge of <strong>the</strong> drugs and<br />
<strong>the</strong>ir effects.<br />
Q: How important is research to patients with SCI? What<br />
expectations should people have about discoveries in<br />
<strong>the</strong> future?<br />
A: Research is critical to advance <strong>the</strong> field and impacts people<br />
worldwide. Without it, we would be stuck in <strong>the</strong> past. With<br />
as many clinical trials as our staff conduct and <strong>the</strong> tremendous<br />
number of patients we see with SCI, we are becoming leaders in<br />
SCI research. Our experience and knowledge in this field goes<br />
beyond what people can get at many o<strong>the</strong>r facilities because <strong>the</strong>y<br />
simply don’t have <strong>the</strong> same volume of cases.<br />
When setting expectations, it’s important for patients and families<br />
to realize <strong>the</strong>re are two types of research – bench research, which<br />
is conducted prior to human trials, and clinical research, which<br />
is <strong>the</strong> phase when studies start being tested on humans. For<br />
research like stem cells, which is moving to <strong>the</strong> clinical phase,<br />
it will take many years to see any impact. However, <strong>the</strong>re will<br />
be a more immediate impact from testing new medications or<br />
<strong>the</strong>rapies. Some of this research will have an effect within months<br />
or a year. But a cure will take many years.<br />
Q: What advice do you give patients and <strong>the</strong>ir family members<br />
when <strong>the</strong>y arrive at <strong>Shepherd</strong>?<br />
A: When patients first arrive, I tell <strong>the</strong>m to keep an open mind. A lot<br />
of things are possible here. Don’t be confined by presumptions of<br />
what your injury will or will not allow you to do. You have <strong>the</strong> chance<br />
to become a person with an SCI, not an SCI person.<br />
When patients return home, it’s important to jump back into life.<br />
The most successful patients are <strong>the</strong> ones who integrate back into<br />
society and do well enough that we only see <strong>the</strong>m every year or so.<br />
INTERESTING FACTS<br />
John Lin, M.D.<br />
<strong>Shepherd</strong> File Photo<br />
Residency:<br />
Internal Medicine and<br />
Rehabilitation Medicine at<br />
Temple University<br />
Medical School:<br />
Medical University of<br />
South Carolina<br />
Undergraduate Degree:<br />
Emory University<br />
Board Certification:<br />
Physical medicine and<br />
rehabilitation, spinal cord injury<br />
medicine and internal medicine<br />
Experience:<br />
Joined <strong>Shepherd</strong> medical staff in<br />
January 2005<br />
Random Facts:<br />
• English was Dr. Lin’s fourth<br />
language. He learned<br />
Taiwanese, Mandarin-Chinese<br />
and Spanish first.<br />
• Dr. Lin is an avid wheelchair<br />
tennis player and competes in<br />
local league tournaments.<br />
• He travels to a new country<br />
every year.<br />
Fall 2009 2 5
<strong>Shepherd</strong>Alums<br />
By sara baxter<br />
John Trimbath,<br />
of Cleveland, Ohio<br />
Susan Gaudet,<br />
of Falmouth, Maine<br />
Traci Pauls, of<br />
Blackville, S.C.<br />
Mike McHale,<br />
of Ruston, La.<br />
Vicki Karnes,<br />
of Atlanta, Ga.<br />
FROM NEAR<br />
AND FAR<br />
Former <strong>Shepherd</strong> <strong>Center</strong> patients<br />
from across <strong>the</strong> nation report on <strong>the</strong>ir<br />
productive lives post-injury.<br />
As a spinal cord injury patient, Susan<br />
Gaudet, of Falmouth, Maine, did<br />
something unusual when she came to<br />
<strong>Shepherd</strong>: She walked in.<br />
“It wasn’t pretty,” she recalls. “I was on<br />
a walker, and I looked like a drunkard.”<br />
Susan was on her way to a doctor’s<br />
appointment in March 2009 when she<br />
slipped on some ice. To prevent herself<br />
from falling, she contorted her body<br />
in a way that herniated two disks. At<br />
<strong>the</strong> doctor’s visit, she was simply given<br />
medication to help <strong>the</strong> pain.<br />
Three days later, Susan woke up and<br />
couldn’t feel her legs and lost bowel and<br />
bladder function.<br />
The swelling in her back had strangulated<br />
a network of peripheral nerves<br />
at <strong>the</strong> lower end of <strong>the</strong> spinal cord.<br />
The condition, known as cauda equina<br />
syndrome, can lead to permanent loss<br />
of bowel and bladder control, as well<br />
as sensation and weakness of <strong>the</strong> legs.<br />
Despite this, Susan is able to walk and is<br />
referred to as a “walking paraplegic.”<br />
After stays at Maine Medical <strong>Center</strong> and<br />
a rehabilitation hospital in Portland, Susan<br />
transferred to <strong>Shepherd</strong> <strong>Center</strong>. Here, she<br />
learned <strong>the</strong> daily living skills of bowel and<br />
bladder management, caring for herself,<br />
and worked on regaining strength in her<br />
legs. She stayed just 12 days.<br />
“My goal was to make it home in time<br />
to spend Easter with my family,” says<br />
Susan, who has a husband and three<br />
daughters.<br />
Susan’s recovery has been slow, but<br />
steady. She can now walk unassisted and<br />
is back at work as a rehabilitation counselor,<br />
helping those with various degrees<br />
of injury.<br />
Though <strong>the</strong> road to recovery has been<br />
rough, Susan remains grateful for her<br />
progress.<br />
“Every step I take, however painful, is<br />
precious,” she says. “I also have a huge<br />
amount of respect and gratitude for all<br />
<strong>the</strong> people who have helped me.” She<br />
also is optimistic on a full recovery: “I’m<br />
not hopeful – I’m expecting it.”<br />
Vicki Karnes, of Atlanta, credits <strong>the</strong> staff<br />
at <strong>Shepherd</strong> <strong>Center</strong>’s Andrew C. Carlos<br />
Multiple Sclerosis Institute for helping prepare<br />
her for new changes – and challenges<br />
– in her life after being diagnosed with MS<br />
in 1998.<br />
“I felt 100 percent supported by my care<br />
team at <strong>Shepherd</strong> <strong>Center</strong> when I decided<br />
to retire from a career as an airline pilot<br />
in 2003,” she says. “It was time to put my<br />
health first.”<br />
Vicki, who had flown for Delta Air Lines<br />
for nearly 20 years, initially found enjoyment<br />
playing <strong>the</strong> mandolin and taking<br />
Spanish classes after retirement. But she<br />
wanted more interaction with people.<br />
“I began volunteering in <strong>Shepherd</strong>’s<br />
Noble Learning Resource <strong>Center</strong> in 2004,”<br />
Vicki says. “Being surrounded by <strong>the</strong><br />
medical books, journals and videos in <strong>the</strong><br />
library reminded me how much I enjoyed<br />
learning and helping o<strong>the</strong>r people to learn.”<br />
After two years of weekly volunteering,<br />
Vicki decided to embark on a new career<br />
as a registered nurse and enrolled in <strong>the</strong><br />
2 6 Spinal Column<br />
w w w. s h e p h e r d . o r g
nursing program at Georgia Perimeter<br />
College.<br />
“I had my concerns about managing<br />
<strong>the</strong> fatigue that comes with living with<br />
MS,” Vicki says. But with <strong>the</strong> support of<br />
her family and her new friends in nursing<br />
school, she completed seven semesters<br />
of nursing school and graduated in May<br />
2009. She even became a mentor to o<strong>the</strong>r<br />
students, developing study guides and<br />
helping <strong>the</strong>m get organized.<br />
After graduating in May 2009, Vicki took<br />
a job in community health, working at a<br />
Snellville, Ga., clinic providing diabetes<br />
education and disease management.<br />
“In helping those with diabetes, I can<br />
draw upon my experience of living with a<br />
chronic illness,” she says. “I feel like I can<br />
make a difference.”<br />
Mike McHale, from Ruston, La., learned<br />
so much from <strong>Shepherd</strong> <strong>Center</strong> about<br />
daily living that he’s often asked for advice<br />
by people in wheelchairs who didn’t go to<br />
<strong>Shepherd</strong>, he says.<br />
“They ask me, ‘What do you do about<br />
this?’ or ‘How did you learn to do that?’”<br />
Mike explains. “<strong>Shepherd</strong> did a wonderful<br />
job of teaching me <strong>the</strong> little things.”<br />
Mike was injured on Sept. 14, 2006 when<br />
he fell 30 feet from a deer stand he had<br />
been building. He severed his spinal cord<br />
at <strong>the</strong> T-12 level and is paralyzed from <strong>the</strong><br />
waist down.<br />
Before his accident, he owned a convenience<br />
store and an adjacent storage facility.<br />
While at <strong>Shepherd</strong>, he realized he was not<br />
going to be able to handle running <strong>the</strong> store<br />
and sold both businesses as a package.<br />
A year after <strong>the</strong> accident, Mike went to<br />
work for a good friend who owns an air<br />
conditioning service company and was looking<br />
for someone to take care of <strong>the</strong> business<br />
side. Mike now calls on new customers<br />
in <strong>the</strong> morning and works on finance and<br />
accounting in <strong>the</strong> afternoon. Thanks to<br />
Mike’s business expertise and his friend’s<br />
knowledge of <strong>the</strong> industry, <strong>the</strong> company is<br />
thriving.<br />
Today, Mike drives an adapted truck and<br />
is accompanied by a service dog who helps<br />
him with daily tasks. He enjoys woodworking<br />
and loves to work in <strong>the</strong> yard. Mike has<br />
a vegetable garden, which he named in<br />
honor of <strong>Shepherd</strong> horticultural <strong>the</strong>rapist<br />
Debi Cziok, who helped show him<br />
how to create a garden.<br />
Mike was active before his accident<br />
and was determined to stay that way.<br />
“Before my accident, I got up at 6 a.m.<br />
and didn’t quit until 9 p.m.,” he says.<br />
“The chair has slowed me down, but my<br />
quality of life has improved thanks to<br />
<strong>the</strong> training I received at <strong>Shepherd</strong>.”<br />
Traci Pauls, of Blackville, S.C., was<br />
so inspired by <strong>the</strong> work of speech<br />
pathologists at <strong>Shepherd</strong> <strong>Center</strong>, she<br />
has decided that one day she will<br />
become one.<br />
Traci was a sophomore at Winthrop<br />
College in Rock Hill, S.C., when she<br />
sustained a T-4 spinal cord injury in a<br />
car accident in 2007. Originally a biology<br />
major, Traci returned to Winthrop<br />
in January 2009 and changed her major.<br />
“Through my own work with <strong>the</strong><br />
speech pathologist and what I saw<br />
<strong>the</strong>m do with o<strong>the</strong>rs, I was inspired,”<br />
Traci says.<br />
Though she was excited about a career<br />
change, she was a little nervous about<br />
returning to school after taking a year<br />
off. “I didn’t know what to expect,” Traci<br />
says, “or how I would get around.” She<br />
credits her mo<strong>the</strong>r with giving her <strong>the</strong><br />
confidence and motivation she needed.<br />
“She told me I could do it and said she’d<br />
be <strong>the</strong>re to help whenever I needed it.”<br />
Also <strong>the</strong>re to help is her twin bro<strong>the</strong>r,<br />
who also is a student at Winthrop and<br />
shares an apartment with her. “He<br />
pushes me to class if I’m running late<br />
and helps in many o<strong>the</strong>r ways,” Traci<br />
says. She also receives a lot of support<br />
from her friends.<br />
Now Traci is turning her attention to<br />
helping o<strong>the</strong>rs in her situation. She has<br />
created Project Live, a campus club for<br />
students with disabilities. “This will be<br />
a place for us to come toge<strong>the</strong>r to share<br />
our experiences and suggest ways to<br />
improve things at Winthrop,” Traci says.<br />
She also hopes <strong>the</strong> organization will<br />
be a place for <strong>the</strong> community to learn<br />
about those with physical disabilities.<br />
As a physician’s assistant, John<br />
Trimbath, of Cleveland, Ohio, knew<br />
something was seriously wrong <strong>the</strong> moment<br />
he was thrown from a mechanical<br />
bull in October 2008.<br />
“I couldn’t feel my arms and legs, and I<br />
had difficulty breathing,” John recalls.<br />
“Being a PA, I knew what was happening.”<br />
When he arrived at <strong>the</strong> hospital, he<br />
asked physicians to put him in traction.<br />
That request was prescient: John had<br />
sustained a C-4 spinal cord injury, which<br />
left him a quadriplegic.<br />
John came to <strong>Shepherd</strong> <strong>Center</strong> on Feb.<br />
10, 2009, and <strong>the</strong> seven weeks he spent as<br />
an inpatient brought a profound change<br />
of perspective. “The surgeons and pulmonologists<br />
saved my life,” he says, “but<br />
<strong>Shepherd</strong> gave me back my will to live.”<br />
One important aspect of his recovery,<br />
John says, was <strong>the</strong> support he received<br />
from both his family and <strong>the</strong> o<strong>the</strong>r patients<br />
– both of which <strong>Shepherd</strong> helped<br />
facilitate.<br />
“<strong>Shepherd</strong> helped with <strong>the</strong> social and<br />
emotional aspects of my recovery,” John<br />
says. “It was so helpful meeting o<strong>the</strong>r<br />
people who had gone through what I had.<br />
The upbeat staff helped me stay motivated<br />
– and learn that <strong>the</strong> hurdles you have to<br />
face aren’t insurmountable.”<br />
John, who worked full time in a hospital<br />
emergency department, hopes to return<br />
to work in some capacity, even if it’s not<br />
direct patient care. He’s also continuing his<br />
volunteer work with American Academy<br />
of Physician’s Assistants, where he just<br />
finished a two-year term on <strong>the</strong> organization’s<br />
board of directors.<br />
John is continuing his rehabilitation<br />
through <strong>the</strong> Cleveland VA hospital and<br />
is regaining movement in his arms and<br />
hands. His short-term goal is to continue<br />
his recovery so he can meet his long-term<br />
goal: celebrating his 20th wedding anniversary<br />
in Egypt with wife Diane in 2012.<br />
What’s New?<br />
We want to stay current on any personal or<br />
professional news in your life. Send us an<br />
update and a photo (we’ll return it to you):<br />
Jane Sanders, Spinal Column Magazine, 2020<br />
Peachtree Rd., N.W., Atlanta, GA, 30309. You can<br />
also e-mail us at spinalcolumn@shepherd.org.<br />
Fall 2009 2 7
FoundationFeatures<br />
Photo by Gary Meek<br />
Fall 2009<br />
“It was an awful year, and I lived through <strong>the</strong> family<br />
trauma of what a devastating diagnosis can do to <strong>the</strong> life of<br />
not just <strong>the</strong> patient, but <strong>the</strong> family as a whole,” Vida says. “I<br />
learned a lot from that experience and felt that I might be a<br />
good fit and useful volunteer at <strong>Shepherd</strong> <strong>Center</strong>.”<br />
Vida volunteers three days a week, dividing her time<br />
between staffing <strong>the</strong> welcome desk, feeding lunches to<br />
patients and assisting with Family Support Services. She<br />
has logged more than 500 volunteer hours in <strong>the</strong> year and<br />
“I’d say some key life lessons are: Don’t take<br />
things for granted, count your blessings –<br />
both big and small – daily, stay focused on<br />
what’s really important and practice humility.<br />
It is a virtue. Adversity can be a lesson, as<br />
well as an opportunity.” — Vida Harmon<br />
Volunteer Profile<br />
Vida Harmon<br />
Former New Yorker finds fulfilling volunteer work<br />
at <strong>Shepherd</strong> <strong>Center</strong>. By Lauren Angelo<br />
When Vida Harmon moved to Atlanta from New York<br />
City two years ago, she had no idea her new home would<br />
be within walking distance of <strong>Shepherd</strong> <strong>Center</strong>, or that her<br />
frequent walks throughout her neighborhood would lead to<br />
such a fulfilling volunteer opportunity.<br />
But after passing <strong>Shepherd</strong> <strong>Center</strong> several times and<br />
learning more about <strong>the</strong> highly specialized care <strong>the</strong> hospital<br />
offers, Vida was impressed and wanted to give her time to<br />
contribute to <strong>the</strong> patients and families at <strong>Shepherd</strong>.<br />
After losing her bro<strong>the</strong>r to a brain tumor in 2001, Vida<br />
says she feels an especially strong connection to families<br />
facing <strong>the</strong> same fear and uncertainty her family experienced.<br />
Her bro<strong>the</strong>r’s struggle with cancer lasted eight months, and<br />
instead of pulling her family closer toge<strong>the</strong>r, <strong>the</strong> tragedy<br />
pushed <strong>the</strong>m fur<strong>the</strong>r apart, she says. He was <strong>the</strong> patriarch of<br />
her family, and <strong>the</strong>y found <strong>the</strong>mselves lost without him.<br />
a half she has been volunteering at <strong>Shepherd</strong>, and Vida<br />
says she has loved every minute of it. Her time with Family<br />
Support Services allows her to meet <strong>the</strong> families of <strong>the</strong><br />
patients and fur<strong>the</strong>r her goal of helping families survive<br />
difficult circumstances and emerge from <strong>the</strong>m even stronger.<br />
She also makes a great effort to answer families’ questions<br />
and help in any way she can during <strong>the</strong> time she spends at<br />
<strong>the</strong> welcome desk.<br />
“It’s a wonderful feeling to know that you can make a<br />
difference in ano<strong>the</strong>r person’s life, even if only for a short<br />
time,” Vida says. “As in any area of life, I believe that a kind<br />
word and a smile can go a long way.”<br />
Jackie Gehner, <strong>Shepherd</strong> <strong>Center</strong>’s former volunteer<br />
manager, says Vida is known for doing favors for people<br />
throughout <strong>the</strong> hospital and is someone <strong>the</strong>y really count on.<br />
Vida says she has learned a lot from volunteering and<br />
believes it is a learning experience on both ends. Through<br />
her own life experiences and her volunteer experience at<br />
<strong>Shepherd</strong>, Vida has a wealth of knowledge to share.<br />
“I’d say some key life lessons are: Don’t take things<br />
for granted, count your blessings – both big and small –<br />
daily, stay focused on what’s really important and practice<br />
humility,” Vida says. “It is a virtue. Adversity can be a lesson,<br />
as well as an opportunity.”<br />
Above: Vida Harmon, left, of Atlanta is a frequent volunteer<br />
at <strong>Shepherd</strong> <strong>Center</strong>. She splits her volunteer time between<br />
staffing <strong>the</strong> welcome desk, feeding lunches to patients and<br />
assisting with Family Support Services. Here, she chats with<br />
patient Keith Champion of Forest City, N.C.<br />
2 8 Spinal Column<br />
w w w. s h e p h e r d . o r g
Partners for<br />
Passengers<br />
<strong>Shepherd</strong>’s relationships with two Atlanta-based airlines<br />
help ease travel woes for patients. By Sara Baxter<br />
Many people find air travel somewhat stressful. But for people<br />
in a wheelchair who travel by plane, that level of stress can take<br />
on a whole new dimension.<br />
That’s why <strong>Shepherd</strong> <strong>Center</strong> has partnered with Delta Air<br />
Lines and AirTran Airways to make it easier for <strong>Shepherd</strong> patients<br />
to readjust to air travel.<br />
“Some patients have to fly home after <strong>the</strong>ir discharge from<br />
<strong>Shepherd</strong>, so <strong>the</strong>y are flying for <strong>the</strong> first time with a wheelchair,”<br />
says Dean Melcher, <strong>Shepherd</strong>’s director of annual giving. “That can<br />
be very stressful.”<br />
The trauma can be mitigated with a lot of knowledge and a<br />
little practice, however. Delta donated airline seats and transfer<br />
chairs to <strong>Shepherd</strong> for occupational and recreational <strong>the</strong>rapists to<br />
help patients learn how to make <strong>the</strong> transition from <strong>the</strong> wheelchair<br />
to <strong>the</strong> aircraft seat. Therapists also take patients on outings<br />
to Atlanta’s Hartsfield-Jackson International Airport, where <strong>the</strong>y<br />
practice checking luggage, going through security and getting to<br />
<strong>the</strong> gate. Then <strong>the</strong>y board an empty Delta jet to become familiar<br />
with <strong>the</strong> transfer and boarding procedures and learn more about<br />
<strong>the</strong> onboard accessibility features on Delta aircraft.<br />
“Delta has been instrumental in this training,” Melcher says.<br />
“Travelers with disabilities have to be comfortable, and <strong>the</strong>y have to<br />
do it correctly so <strong>the</strong>y don’t hurt <strong>the</strong>mselves. These trial runs help<br />
<strong>the</strong>m know what to expect and can take away a lot of <strong>the</strong> anxiety.”<br />
“Delta’s relationship with <strong>Shepherd</strong> <strong>Center</strong>, now entering its<br />
20th year, reflects our commitment to serving people with disabilities<br />
and compliance to federal regulations that protect <strong>the</strong><br />
rights of customers with disabilities in air travel,” says David S.<br />
Martin, Delta’s disabilities program manager. “This relationship<br />
reminds me that what we are providing is not just an educational<br />
experience. We are giving people back <strong>the</strong>ir independence and<br />
hope for <strong>the</strong>ir future.”<br />
To facilitate transferring from a wheelchair to a seat where <strong>the</strong><br />
armrest does not come up (common in older planes), Delta has<br />
developed a hydraulic transfer chair that elevates patients above<br />
<strong>the</strong> armrest. This decreases <strong>the</strong> chance of <strong>the</strong> passenger scraping<br />
<strong>the</strong> armrest, which could cause problems on already sensitive skin.<br />
“This is ano<strong>the</strong>r example of how Delta listens to <strong>the</strong> needs of<br />
<strong>the</strong> disabled community,” says Pete Collman, <strong>Shepherd</strong>’s community<br />
relations coordinator, who also uses a wheelchair and travels<br />
extensively with <strong>the</strong> <strong>Shepherd</strong> fencing team. “They saw this as a<br />
customer service issue and fixed it.”<br />
Like Delta, AirTran is also stepping up its customer service for<br />
travelers with disabilities. The airline is working with <strong>Shepherd</strong><br />
on a training video for its employees on disability awareness. The<br />
video, which will feature <strong>Shepherd</strong> staff members, will give an<br />
overview of how to accommodate disabled travelers, including<br />
how to safely transfer <strong>the</strong>m into a seat.<br />
“A video is so much more helpful and educational than someone<br />
telling <strong>the</strong>m or having <strong>the</strong>m read about it,” Melcher says.<br />
“Staff training is imperative – it’s <strong>the</strong> o<strong>the</strong>r half of <strong>the</strong> equation.”<br />
Aside from training, Melcher says both airlines have generously<br />
provided free tickets and frequent flyer miles to fly<br />
patients and family members to and from Atlanta, as well as<br />
donating tickets for <strong>Shepherd</strong> fundraisers.<br />
Photos by Kayla Eubanks<br />
Above: <strong>Shepherd</strong> <strong>Center</strong> <strong>the</strong>rapists take patients on outings to<br />
Atlanta’s Hartsfield-Jackson International Airport, where <strong>the</strong>y<br />
practice checking luggage, going through security and getting to <strong>the</strong><br />
gate. Then <strong>the</strong>y board an empty Delta jet to become familiar with <strong>the</strong><br />
transfer and boarding procedures and learn more about <strong>the</strong> onboard<br />
accessibility features on Delta aircraft.<br />
Fall 2009 2 9
FoundationFeatures<br />
A Desire to<br />
SHARE<br />
The generosity of individuals and<br />
organizations enables <strong>Shepherd</strong> <strong>Center</strong><br />
to extend its specialty care to military<br />
service personnel. By Sara Baxter<br />
Photo by Anthony Orig<br />
Mat<strong>the</strong>w Sanchez and three friends biked 4,500 miles across <strong>the</strong> country this past summer –<br />
not just for thrills, but to raise awareness and funds for a <strong>Shepherd</strong> <strong>Center</strong> program that serves<br />
active and separated service members.<br />
The program is SHARE – Shaping Hope and Recovery<br />
Excellence – and it extends <strong>Shepherd</strong>’s continuum of care<br />
to U.S. service men and women who have served in Iraq and<br />
Afghanistan. Through <strong>the</strong>ir cross-country odyssey, Mat<strong>the</strong>w<br />
and his team raised $9,625, and donations are still coming in.<br />
“We talked to as many people as we could along <strong>the</strong> way to<br />
let <strong>the</strong>m know about <strong>the</strong> program, what it does and why we<br />
were raising <strong>the</strong> money for it,” Mat<strong>the</strong>w says. “In many cases,<br />
people approached us and asked us about it because we had<br />
car magnets on our support vehicle.”<br />
Mat<strong>the</strong>w’s commitment to bicycle thousands of miles was<br />
born out of a simple desire to give back to those who make<br />
<strong>the</strong> ultimate sacrifice for country.<br />
“I feel that <strong>the</strong> men and women serving our nation should<br />
have access to <strong>the</strong> best treatment available,” he says, “and I<br />
believe this to be at <strong>Shepherd</strong> <strong>Center</strong>.”<br />
Mat<strong>the</strong>w experienced <strong>Shepherd</strong> care first hand: He spent<br />
time at <strong>the</strong> hospital after sustaining an incomplete C-5 spinal<br />
cord injury in a high school football game in 2005.<br />
The Tyrone, Ga., native walked out of <strong>Shepherd</strong> and has<br />
been running, biking and swimming ever since.<br />
Mat<strong>the</strong>w is far from alone in his quest to support<br />
<strong>the</strong> SHARE Initiative. Funded by an initial gift from<br />
philanthropist Bernie Marcus, who also believes <strong>the</strong><br />
men and women fighting for our country should have<br />
<strong>the</strong> best care possible, <strong>the</strong> program has received support<br />
from o<strong>the</strong>r foundations, organizations and individuals.<br />
While <strong>the</strong> bulk of medical payments for service<br />
members is provided through <strong>the</strong> military’s healthcare<br />
benefits provider, SHARE helps service members<br />
cover a wide range of o<strong>the</strong>r expenses associated with<br />
<strong>the</strong>ir injuries.“I see this as <strong>the</strong> vehicle through which<br />
we can help eliminate barriers associated with coming<br />
to <strong>Shepherd</strong> for care,” says Terran Cooper, SHARE<br />
project manager. “The things we pay for are a little off<br />
<strong>the</strong> beaten path.”<br />
3 0 Spinal Column<br />
w w w. s h e p h e r d . o r g
As examples, Cooper cites money for groceries and monthly bills, all<br />
<strong>the</strong> way up to big expenses, such as providing in-home care or airline<br />
tickets. SHARE donations also cover operational costs, such as staff<br />
travel expenses for visits to U.S. Department of Veterans Affairs hospitals,<br />
as well as equipment and items not covered by insurance.<br />
Cooper tells a story of a service member in Florida who wanted to<br />
receive treatment at <strong>Shepherd</strong>, but was hesitant because he had no one<br />
to care for his dog, which he couldn’t afford to board. “We found a kennel<br />
for his dog in Atlanta,” Cooper says. “They gave us a discounted rate,<br />
and <strong>the</strong> dog received veterinary care for no charge.”<br />
Photo by Gary Meek<br />
“We work with each service member on a case-bycase<br />
basis. We help each one establish individual<br />
goals and <strong>the</strong>n give <strong>the</strong>m <strong>the</strong> tools and skills<br />
needed to meet those goals. We want to help <strong>the</strong>m<br />
become as independent as possible, whe<strong>the</strong>r that<br />
means returning to active duty or living back at<br />
home in <strong>the</strong> civilian community.” — Terran Cooper<br />
Ano<strong>the</strong>r service member wanted to receive outpatient care at<br />
<strong>Shepherd</strong>, but couldn’t live on his own in an apartment. SHARE paid<br />
for an attendant so <strong>the</strong> man could come to <strong>the</strong>rapy at <strong>Shepherd</strong>.<br />
“The funding is not so much covering care, but quality-of-life issues,”<br />
says Dean Melcher, director of annual giving for <strong>Shepherd</strong>. “This is a<br />
different group. They need more specialized help.”<br />
In addition to brain and/or spinal cord injuries, injured troops may<br />
be dealing with skeletal issues from carrying <strong>the</strong>ir equipment packs or<br />
suffer from severe headaches, Melcher says. Some have substance abuse<br />
problems, and most suffer from some level of post-traumatic stress<br />
disorder. Service men and women who are not returning to active duty<br />
may need help with re-entering <strong>the</strong> job market, planning <strong>the</strong>ir finances<br />
or related activities.<br />
No matter <strong>the</strong> need, SHARE has an answer. “We work with each service<br />
member on a case-by-case basis,” Cooper says. “We help each one<br />
establish individual goals and <strong>the</strong>n give <strong>the</strong>m <strong>the</strong> tools and skills needed<br />
to meet those goals. We want to help <strong>the</strong>m become as independent as<br />
possible, whe<strong>the</strong>r that means returning to active duty or living back at<br />
home in <strong>the</strong> civilian community.”<br />
Because of <strong>the</strong>ir specialized needs, patients in <strong>the</strong> SHARE<br />
Initiative are treated separately from <strong>the</strong> general patient population.<br />
“They are unique in psychology and temperament,” Melcher says. “They<br />
don’t respond to <strong>the</strong> same <strong>the</strong>rapy and stimulus that o<strong>the</strong>rs do, based on<br />
<strong>the</strong>ir training and demeanor. We found <strong>the</strong>y respond better in <strong>the</strong>ir own<br />
environment.”<br />
Thus, <strong>Shepherd</strong> renovated six apartments at Biscayne Place, which is<br />
near <strong>the</strong> hospital. The apartments had been used in <strong>the</strong> past for family<br />
housing, but now that <strong>Shepherd</strong> has <strong>the</strong> Irene and George Woodruff<br />
Family Residence <strong>Center</strong>, <strong>the</strong> Biscayne apartments are available to<br />
service members and <strong>the</strong>ir families.<br />
Support for SHARE also goes beyond monetary contributions.<br />
Volunteers shop for groceries and run o<strong>the</strong>r errands, and businesses have<br />
donated <strong>the</strong>ir products and services at no charge or for a discounted rate.<br />
“It’s amazing how much <strong>the</strong> whole community wants to help,”<br />
Cooper says. “The support we’ve received has been absolutely wonderful.”<br />
Photo Courtesy of Anthony Orig<br />
Above: Dillon Cannon of Sugar Land, Texas, sustained<br />
a spinal cord injury while serving in Iraq. He received<br />
treatment in <strong>Shepherd</strong>'s SCI Day Program through <strong>the</strong><br />
SHARE Initiative.<br />
Mat<strong>the</strong>w Sanchez, right, and his friends decided to raise<br />
money for SHARE because <strong>the</strong>y believe all soldiers should<br />
have access to <strong>the</strong> best possible care. Left to right are:<br />
Anthony Orig, Jonny Cromwell, Marina Fleming, Peter<br />
Zhang and Mat<strong>the</strong>w.<br />
Previous Page: Former spinal cord injury patient Mat<strong>the</strong>w<br />
Sanchez and some friends, including Marina Fleming,<br />
biked 4,500 miles across <strong>the</strong> United States this past<br />
summer to raise money for military patients being treated<br />
in <strong>Shepherd</strong>'s SHARE Initiative.<br />
Fall 2009 3 1
FoundationFeatures<br />
<strong>Shepherd</strong> Injury Prevention Program<br />
Launches Online Effort to Reach<br />
More Teens and Young Adults<br />
By Pete Collman, <strong>Shepherd</strong> <strong>Center</strong> Community Relations Coordinator<br />
and Think First Director of Georgia<br />
It is said that an ounce of prevention<br />
is worth a pound of cure. This<br />
proverb describes <strong>the</strong> foundation on<br />
which <strong>Shepherd</strong> <strong>Center</strong>’s Think First<br />
and injury prevention programs are<br />
built. For nearly 20 years, <strong>Shepherd</strong><br />
<strong>Center</strong>’s injury prevention message<br />
has been delivered by speakers living<br />
with disabilities, explaining <strong>the</strong>ir<br />
unique stories of injury and teaching<br />
youth on how to avoid brain and<br />
Pete Collman<br />
spinal cord trauma.<br />
Having managed <strong>the</strong> Think First Program at <strong>Shepherd</strong> for<br />
Photo by Leita Cowart<br />
<strong>the</strong> past 10 years, I have found that teens and young adults<br />
don’t easily seek out information on injury prevention. The<br />
challenge lies in getting <strong>the</strong> message to <strong>the</strong>m. That is why we<br />
are creating a new, socially<br />
dynamic outreach program<br />
called YiPES!! (Youth and<br />
Injury Prevention Education<br />
at <strong>Shepherd</strong>).<br />
<strong>Shepherd</strong>’s adolescent team<br />
orthopedic physician, Herndon<br />
Murray, M.D., proposed a<br />
new approach to reach young<br />
people on <strong>the</strong> perils of diving<br />
and o<strong>the</strong>r risky behaviors related to water recreation. “I wanted<br />
to see a specific focus on preventing diving and skim-boarding<br />
injuries in <strong>the</strong> Sou<strong>the</strong>ast,” he says. “What Pete (Collman) and<br />
his team have done has given this injury prevention message a<br />
vehicle to reach even more young people than <strong>the</strong> 13,000 reached<br />
through <strong>Shepherd</strong> <strong>Center</strong>’s current Think First Program.”<br />
YiPES!! is designed to use social networking sites, such as<br />
Facebook, Twitter and YouTube, to get an “edgier” message out to<br />
teens and young adults. This addition to <strong>the</strong> Think First Program<br />
will help in <strong>the</strong> broadening of our audience through <strong>the</strong> World<br />
Wide Web. Activities such as diving, skim boarding, skateboarding,<br />
ATV riding and o<strong>the</strong>r extreme sports will be highlighted. Also, a<br />
special emphasis will be placed upon distracted driving with a preventative<br />
approach to educating drivers on <strong>the</strong> perils of texting and<br />
phone usage while behind <strong>the</strong> wheel.<br />
Video public service announcements (PSAs) will be created to<br />
capture <strong>the</strong> attention of <strong>the</strong> adolescent Web surfer. Those will be<br />
followed by a message from a current <strong>Shepherd</strong> <strong>Center</strong> patient explaining<br />
<strong>the</strong>ir injury and how to avoid spinal cord and brain trauma.<br />
“I feel this is a great effort to get behind and show support for<br />
our injury prevention programs<br />
here at <strong>Shepherd</strong>,” Dr.<br />
Murray says. “I will be<br />
presenting our efforts on<br />
Think First and YiPES!! at<br />
<strong>the</strong> International Spinal Cord<br />
Society Convention this October<br />
in Florence, Italy. I feel<br />
this may just jump-start o<strong>the</strong>r<br />
organizations to follow suit<br />
in decreasing <strong>the</strong>se catastrophic injuries among our young people.”<br />
The YiPES!! Facebook page is active and is linked from <strong>the</strong><br />
<strong>Shepherd</strong> <strong>Center</strong> Facebook homepage at www.facebook.com/shepherd.<br />
The YouTube and Twitter endeavors are under construction.<br />
“I wanted to see a specific focus on preventing diving and<br />
skim-boarding injuries in <strong>the</strong> Sou<strong>the</strong>ast. What Pete (Collman)<br />
and his team have done has given this injury prevention<br />
message a vehicle to reach even more young people than<br />
<strong>the</strong> 13,000 reached through <strong>Shepherd</strong> <strong>Center</strong>’s current<br />
Think First Program.” — Herndon Murray, M.D.<br />
3 2 Spinal Column<br />
w w w. s h e p h e r d . o r g
A Holiday Gift with Meaning<br />
The true spirit of <strong>the</strong> holidays is conveyed through<br />
giving. Many of our friends and supporters plan to give<br />
a personal and special gift to <strong>the</strong>ir friends and family –<br />
<strong>the</strong> gift of hope for <strong>Shepherd</strong> <strong>Center</strong>’s patients –<br />
by making a “Holiday Tribute” gift to <strong>Shepherd</strong> <strong>Center</strong><br />
Foundation in honor of <strong>the</strong>ir family and associates.<br />
The Foundation sends personalized cards with our<br />
donors’ own greetings to <strong>the</strong>ir holiday card mailing lists.<br />
In addition, <strong>the</strong>ir friends and families are included in<br />
Spinal Column’s annual Holiday Tribute listing.<br />
Long-time <strong>Shepherd</strong> <strong>Center</strong> supporters Forrest<br />
Leef and Dorothy Mitchell-Leef and Becca and<br />
Rudy Harrell have a tradition of sharing <strong>the</strong>ir spirit<br />
of philanthropy by making Holiday Tributes for<br />
<strong>the</strong>ir friends and associates. Stan Topol & Associates<br />
was among <strong>the</strong> businesses that chose to honor <strong>the</strong>ir<br />
customers by making gifts to <strong>the</strong> Foundation to help<br />
<strong>Shepherd</strong> in its mission to restore our patients’ lives with<br />
hope, dignity and independence.<br />
For information about <strong>Shepherd</strong>’s Holiday Tribute<br />
program, contact Dean Melcher at 404-350-7306 or<br />
dean_melcher@shepherd.org.<br />
Gritz at <strong>the</strong> Ritz Honors Dell Sikes<br />
The Phoenix Society hosted its annual<br />
Gritz at <strong>the</strong> Ritz fashion show luncheon<br />
at <strong>the</strong> Ritz-Carlton, Buckhead on July 26.<br />
The guests enjoyed a delicious meal featuring<br />
a fashion show from Belk at Phipps<br />
Plaza and an entertaining and enlightening<br />
presentation by <strong>Shepherd</strong> <strong>Center</strong><br />
Chief Nurse Executive Tammy King.<br />
Ty Tippett, Senior Director of Planned<br />
Giving for <strong>Shepherd</strong> <strong>Center</strong> Foundation,<br />
served as master of ceremonies and had<br />
<strong>the</strong> pleasure of recognizing his friend and<br />
mentor, Dell Sikes, who was honorary<br />
chairman of <strong>the</strong> event. Dell served<br />
as vice-president of development for<br />
<strong>Shepherd</strong> <strong>Center</strong> form 1986-2002 and<br />
has been serving as special advisor to <strong>the</strong><br />
Foundation since 2002.<br />
The 2009 Phoenix Debutantes were introduced<br />
and recognized for <strong>the</strong>ir outstanding<br />
efforts in volunteering with <strong>Shepherd</strong><br />
<strong>Center</strong>’s patients and families, and particularly<br />
for <strong>the</strong>ir wonderful work at <strong>the</strong><br />
Wheelchair Division of <strong>the</strong> Peachtree Road<br />
Race. Alli Gombolay was awarded <strong>the</strong> prize<br />
of Debutante of <strong>the</strong> Year for her tireless<br />
volunteerism and outstanding commitment<br />
to <strong>the</strong> Phoenix Society.<br />
This year’s highly successful luncheon<br />
was thanks to <strong>the</strong> hard work and careful<br />
planning of Co-Chairmen Robin<br />
Phillips and Melinda Dabbiere. Leslie<br />
Grace, Connie Kushner, Karen Martin<br />
and Lois Puckett served as planning<br />
committee members. — Dean Melcher<br />
Above: <strong>Shepherd</strong> <strong>Center</strong> Foundation<br />
advisor Dell Sikes, second from right,<br />
was honored by <strong>the</strong> Phoenix Society and<br />
<strong>Shepherd</strong> <strong>Center</strong> for his many years of<br />
service. Also pictured, left to right, are event<br />
Co-Chairman Robin Phillips, Hugh McLeod,<br />
M.D., and Alana <strong>Shepherd</strong>.<br />
<strong>Shepherd</strong> <strong>Center</strong> co-founder Alana<br />
<strong>Shepherd</strong>, left, congratulates Phoenix<br />
Society Debutante of <strong>the</strong> Year Alli Gombolay.<br />
<strong>Shepherd</strong> <strong>Center</strong><br />
Auxiliary Announces<br />
Pecans Fundraiser<br />
The <strong>Shepherd</strong> <strong>Center</strong> Auxiliary’s<br />
annual holiday fundraiser, Pecans<br />
on Peachtree, runs from Nov. 9 to<br />
Dec. 24. This is <strong>the</strong> 26th year for<br />
<strong>the</strong> fundraiser, which has raised<br />
more than $1.3 million for patientrelated<br />
programs and Auxiliary<br />
operations since 1982.<br />
Georgia pecan farmers report<br />
that this year’s pecan crop appears<br />
to be even better than last year’s.<br />
Plus, all of <strong>the</strong> fundraiser’s mouthwatering<br />
pecan varieties will be<br />
available again this year along with<br />
two new products – Sweet & Salty<br />
Pleasures and a Holiday Trio.<br />
The Auxiliary is busy signing up<br />
volunteers to work <strong>the</strong> sales tables<br />
inside <strong>Shepherd</strong> <strong>Center</strong> from 9 a.m.<br />
to 4 p.m. weekdays and to host<br />
“Pecan Parties” in <strong>the</strong>ir homes or<br />
businesses. If you would like to volunteer,<br />
receive a brochure or place<br />
an order, call 404-367-1322 or go to<br />
www.pecansonpeachtree.org.<br />
— Midge Tracy<br />
Fall 2009 3 3
FoundationFeatures<br />
Junior Ball<br />
Promises Great Times<br />
and Great Music<br />
Get ready for a fun-filled night of great times,<br />
good friends and terrific music. On Saturday, Nov.<br />
7, Junior Ball Chairmen Hea<strong>the</strong>r and Eli Flint and<br />
Junior Committee Co-Chairmen Miller Jackson<br />
and Kirk Martin will host “Back to <strong>the</strong> Future,”<br />
<strong>the</strong> annual Junior Ball held in conjunction with<br />
The Legendary Party, <strong>Shepherd</strong> <strong>Center</strong>’s black-tie<br />
gala. While The Legendary Party will celebrate <strong>the</strong><br />
historical dream of Jules Verne, <strong>the</strong> Junior Ball will<br />
party to his visions of time and space travel in a<br />
modern set-up.<br />
Not only is this a great party on its own, but<br />
<strong>the</strong> Junior Ball gives our younger crowd a chance<br />
to sample The Legendary Party and let <strong>the</strong>se two<br />
groups of <strong>Shepherd</strong> supporters mingle and have a<br />
great time for a great cause.<br />
This year’s bash will be at The Ritz-Carlton,<br />
Buckhead and will feature a terrific Atlanta party<br />
band, League of Decency, in <strong>the</strong> Plaza Ballroom.<br />
Guests will also party into <strong>the</strong> late night hours to<br />
DJ-led karaoke in <strong>the</strong> Reform Club.<br />
The party starts at 10 p.m. and ends at 2 a.m.<br />
with late-night buffets featuring The Ritz-<br />
Carlton’s famous waffle bar and a hosted bar.<br />
Tickets are $75 per person and include all festivities.<br />
For more information, please contact Anne<br />
Pearce at (404) 350-7302 or<br />
anne_pearce@shepherd.org. — Dean Melcher<br />
Below: Junior Ball Chairmen Hea<strong>the</strong>r and Eli Flint, center,<br />
along with Junior Committee Chairmen Miller Jackson<br />
and Kirk Martin (not pictured), will host this year's event,<br />
which coincides with The Legendary Party. Pictured with<br />
<strong>the</strong> Flints are party Chairman-elect Dorothy Mitchell-Leef,<br />
M.D., left, and Chairman Cyndae Arrendale.<br />
Photos by Jim Fitts<br />
Legendary Party to<br />
Dazzle and Amaze<br />
Much as Jules Verne’s classic character Phileas Fogg embarked on<br />
an 80-day journey filled with intrigue and excitement, <strong>the</strong> guests<br />
of The Legendary Party 2009 will experience a wondrous adventure<br />
filled with fun and glamour – and perhaps <strong>the</strong> unexpected.<br />
“Around <strong>the</strong> World in 80 Days, The Legend of Jules Verne”<br />
promises to be <strong>the</strong> most imaginative and thrilling gala yet.<br />
Chairman Cyndae Arrendale and her dear friend and<br />
Chairman-elect, Dororthy Mitchell-Leef, M.D., have been<br />
working hard with The Legendary Committee to plan a truly<br />
amazing event to celebrate <strong>the</strong> vision and accomplishments of<br />
Jules Verne and <strong>Shepherd</strong> <strong>Center</strong>.<br />
“Since <strong>Shepherd</strong> has seen patients from all 50 states and 44<br />
countries, what better <strong>the</strong>me for The Legendary Party than<br />
‘Around <strong>the</strong> World in 80 Days’?” Cyndae says. She is also delighted<br />
<strong>the</strong> ball will celebrate <strong>the</strong> devotion and accomplishment<br />
of long-time <strong>Shepherd</strong> <strong>Center</strong> supporter Jane Woodruff, who<br />
serves as honorary chairman.<br />
On Nov. 7, Tony Conway’s A Legendary Event will transform<br />
<strong>the</strong> Ritz-Carlton, Buckhead into a real-life adventure. Guests<br />
will explore <strong>the</strong> cultures of <strong>the</strong> Victorian world while <strong>the</strong>y dine<br />
on scrumptious food and dance <strong>the</strong> night away to Doc Scantlin’s<br />
Imperial Palms Orchestra. The late-night entertainment will<br />
feature DJ-led karaoke. Festivities begin with cocktails at 7 p.m.<br />
and dancing and carousing will continue until 2 a.m.<br />
For sponsorship or ticket information, please contact<br />
Cara Puckett at cara_puckett@shepherd.org or<br />
404-350-7778. — Dean Melcher<br />
Photo by Jim Fitts<br />
Above: Committee leaders for The Legendary Party 2009 are,<br />
left to right, Terri Vawter, Steve Lore, John Woodruff, Cyndae<br />
Arrendale and Dorothy Mitchell-Leef, M.D.<br />
Inset: Cyndae is chairman of <strong>the</strong> 2009 committee, and Dorothy<br />
is chairman-elect for next year's event.<br />
3 4 Spinal Column<br />
w w w. s h e p h e r d . o r g
Junior Committee Preparing for a Memorable Year<br />
Photo by Anne Pearce<br />
The Junior Committee is back from its summer break and ready to start ano<strong>the</strong>r<br />
year of fundraising and fun.<br />
Earlier this year, <strong>the</strong> Junior Committee’s annual fundraiser, Derby Day, raised<br />
$200,000 – an especially impressive figure considering <strong>the</strong> state of <strong>the</strong> economy.<br />
Derby Day 2010 Co-Chairs Miller Jackson and Kirk Martin got started with<br />
planning early this summer with what is sure to be <strong>the</strong> best event yet.<br />
This season’s first Junior Committee meeting was held on Sept.16. The first order<br />
of business was showing appreciation to last year’s co-chairs, Erin Jernigan and<br />
Ryan Hoyt, for all <strong>the</strong> time and hard work <strong>the</strong>y put into making Derby Day 2009<br />
so successful. After hearing from several members of <strong>the</strong> <strong>Shepherd</strong> <strong>Center</strong> staff, <strong>the</strong><br />
committee jumped right in with <strong>the</strong>ir plans for sponsorship, an auction and how to<br />
make Derby Day 2010 <strong>the</strong> best one to date.<br />
For more information on joining <strong>the</strong> Junior Committee or becoming a sponsor of<br />
Derby Day, please contact Anne Pearce at 404-350-7302 or anne_pearce@shepherd.org.<br />
2009-2010<br />
Executive Board:<br />
Derby Day Co-Chairs:<br />
Miller Jackson and Kirk Miller<br />
Sponsorship Co-Chairs:<br />
Dan Lenahan and Scott Tucker<br />
Auction Co-Chairs:<br />
Reagan Michaelis, Lauren Tucker<br />
and Philip Mize<br />
Membership Co-Chairs:<br />
Stuart Griswold and Shannon Shipley<br />
Beverage Co-Chairs:<br />
Brenden Harper and Hunter Ross<br />
Operations Committee:<br />
Hamilton Bridges, Orin Romain,<br />
Wesley Snapp and Trey Wea<strong>the</strong>rly<br />
Treasurer:<br />
Nadine Helal<br />
<strong>Shepherd</strong> <strong>Center</strong> Staff:<br />
Anne Pearce<br />
Above: The 2009-2010 Junior Committee<br />
Executive Board: front row, left to right –<br />
Nadine Helal, Wesley Snapp, Shannon<br />
Shipley, Lauren Tucker, Reagan Michaelis, Kirk<br />
Martin and Miller Jackson; back row: Brenden<br />
Harper, Orin Romain, Hamilton Bridges, Trey<br />
Wea<strong>the</strong>rly, Stuart Griswold, Scott Tucker,<br />
Hunter Ross and Philip Mize. Not pictured are<br />
Dan Lenahan and Anne Pearce.<br />
<strong>Shepherd</strong> <strong>Center</strong> Society Gets Its Second Year Under Way<br />
Photo by Anne Pearce<br />
Above: Daryn Schwartz, left,<br />
and Albie Whitaker are <strong>the</strong><br />
2009-2010 <strong>Shepherd</strong> <strong>Center</strong><br />
Society co-chairmen.<br />
Last summer, 16 individuals, many recent Junior<br />
Committee alumni, formed a new volunteer group<br />
to bridge <strong>the</strong> gap between <strong>the</strong> Junior<br />
Committee and <strong>Shepherd</strong> <strong>Center</strong>’s o<strong>the</strong>r two<br />
volunteer groups, Peach Corps and <strong>the</strong> <strong>Shepherd</strong><br />
<strong>Center</strong> Auxiliary.<br />
<strong>Shepherd</strong> <strong>Center</strong> Society (SCS) was born and<br />
couldn’t have had a more successful first year. Under<br />
SCS Co-Chairs Lauren Hooks and Alex Panos,<br />
<strong>the</strong> group grew to 167 members and raised a net of<br />
more than $10,000 for <strong>Shepherd</strong> <strong>Center</strong>.<br />
This fall, SCS has launched its second year under<br />
<strong>the</strong> guidance of new SCS Co-Chairs Daryn Schwartz and Albie Whitaker. With events<br />
in <strong>the</strong> fall, winter, spring and summer, <strong>the</strong>re’s sure to be something for everyone.<br />
For more information on joining SCS, please contact Anne Pearce at 404-350-7302<br />
or anne_pearce@shepherd.org — Anne Pearce<br />
SCS Leadership<br />
for 2009-2010<br />
SCS Co-Chairs:<br />
Daryn Schwartz and Albie Whitaker<br />
Kick-off Party Co-Chairs:<br />
Lucy King and Meredith Repp<br />
“Big Game” Bash Co-Chairs:<br />
Brandie Miner and Will Lovell<br />
Casino Night Co-Chairs:<br />
Lauren and Mike Imber<br />
Sarah and Jamie <strong>Shepherd</strong><br />
Summer In <strong>the</strong> City Co-Chairs:<br />
Leah Humphries, Caeser Pruett<br />
and Stacey Lucas<br />
Fall 2009 3 5
FoundationFeatures<br />
Photo by Leita Cowart<br />
Notes from Scott Sikes<br />
<strong>Shepherd</strong> <strong>Center</strong> Foundation Executive Director<br />
Giving Thanks!<br />
Dear <strong>Shepherd</strong> <strong>Center</strong> Volunteers and Donor Friends:<br />
I’m writing you this letter in <strong>the</strong> heat and humidity of an<br />
Atlanta summer. By <strong>the</strong> time you see this in print, fall has<br />
returned, and you are busy with all sorts of activities.<br />
Kids are back in school. Young adults are in college. The first<br />
cooler, drier days have arrived in Atlanta. The leaves are changing.<br />
College football is in full swing with many of you intently<br />
following scores nationwide. Those of you who are super-organized<br />
may be ga<strong>the</strong>ring your income tax-related information. Your<br />
meetings with your accountant or o<strong>the</strong>r tax preparer may involve<br />
pre-planning before <strong>the</strong> end of <strong>the</strong><br />
”These aren’t simply monetary<br />
values. Often, <strong>the</strong>y are a guidebook<br />
for living a generous life.”<br />
calendar/tax year. Normally, you consider<br />
accelerating any payments or gifts that<br />
might be deductible into this year and<br />
delaying any income into next year.<br />
Regardless of what you are doing<br />
this fall with family and/or friends or how sophisticated your<br />
tax planning is, consider what one Atlanta family has done for<br />
decades. They hold a family meeting after <strong>the</strong>ir Thanksgiving<br />
dinner and discuss <strong>the</strong> charitable organizations to which <strong>the</strong>y give<br />
and how large to make <strong>the</strong>ir contributions.<br />
Each family member brings with <strong>the</strong>m some of <strong>the</strong> charitable<br />
solicitations <strong>the</strong>y received during <strong>the</strong> year. Even <strong>the</strong> youngest<br />
family members are involved. The family members discuss each of<br />
<strong>the</strong>se charitable organizations: each organization’s return-on-gift<br />
“investment,” <strong>the</strong> impact of <strong>the</strong> organization on society, how<br />
<strong>the</strong> organization has benefited <strong>the</strong> family members’ loved ones<br />
and/or friends, etc. Afterward, family members vote on <strong>the</strong><br />
charitable organizations that will receive gifts and determine<br />
what size <strong>the</strong> contributions will be.<br />
This meeting serves as one way for grandparents and parents<br />
to transfer <strong>the</strong>ir own values and identities to <strong>the</strong>ir children and<br />
o<strong>the</strong>r loved ones at a significant time of year. The Thanksgiving<br />
holiday is a time when one can thank those organizations<br />
doing crucial work for important constituencies. Also, it is an<br />
excellent time to prepare prudently for <strong>the</strong><br />
end of <strong>the</strong> tax year.<br />
Sophisticated financial and estate<br />
planners don’t spend time with clients<br />
simply helping <strong>the</strong> clients transfer <strong>the</strong>ir<br />
money to heirs. Instead, planners spend<br />
time with clients helping <strong>the</strong>m to transfer <strong>the</strong>ir most deeply<br />
held convictions and values to <strong>the</strong> generation that follows.<br />
These aren’t simply monetary values. Often, <strong>the</strong>y are a<br />
guidebook for living a generous life.<br />
If you would like to leave a legacy to <strong>the</strong> next generation<br />
of your family on Thanksgiving Day, please call me, and I can<br />
help you organize a game plan. Thank you for your generous<br />
investments in our work, which helps better <strong>the</strong> lives of<br />
patients and families.<br />
Seasons<br />
of <strong>Shepherd</strong> <strong>Center</strong><br />
Supporters<br />
From season to season, <strong>Shepherd</strong><br />
<strong>Center</strong> supporters combine generous<br />
giving with fun events and<br />
activities to benefit patients and <strong>the</strong>ir<br />
families. From The Legendary Party<br />
to Casino Night to Derby Day, supporters<br />
consistently donate <strong>the</strong>ir time<br />
and money to help patients rebuild<br />
<strong>the</strong>ir lives with hope, dignity and<br />
independence.<br />
3 6 Spinal Column<br />
w w w. s h e p h e r d . o r g
Alyson Roth:<br />
Advocate and Surfing Competitor<br />
Former <strong>Shepherd</strong> <strong>Center</strong> spinal cord<br />
injury patient Alyson Roth of Irvine,<br />
Calif., was crowned Ms. Wheelchair<br />
California in April and placed second<br />
in <strong>the</strong> Ms. Wheelchair America<br />
competition in August. The California<br />
and national pageants are competitions<br />
designed to select <strong>the</strong> most accomplished<br />
and articulate spokeswoman for <strong>the</strong><br />
millions of Americans with disabilities.<br />
Alyson has been involved in advocacy<br />
work for nearly a decade. She is now<br />
<strong>the</strong> development manager for Free<br />
Wheelchair Mission, a non-profit organization that distributes wheelchairs<br />
to poor people with disabilities in 71 countries around <strong>the</strong> world. For more<br />
information on Alyson and <strong>the</strong> pageant, see www.mswheelchairca.org and<br />
www.mswheelchaircalifornia2009.blogspot.com.<br />
Also, in July, Alyson became <strong>the</strong> first woman with a disability to ever<br />
surf in <strong>the</strong> Hurley U.S. Open of Surfing in Huntington Beach, Calif.<br />
More than half a million people attended <strong>the</strong> event to witness this<br />
history-making moment.<br />
“I was truly honored to have been chosen and to represent not only<br />
women, but all people with disabilities and let <strong>the</strong>m know that life<br />
doesn't stop after injury!” Alyson says.<br />
You can read more about <strong>the</strong> event on Alyson’s blog at<br />
http://alysonroth.blogspot.com/2009/07/us-open-of-surfing.html.<br />
Photo Courtesy of Alyson Roth<br />
Above: Former patient Alyson Roth of Irvine, Calif., was crowned<br />
Ms. Wheelchair California and placed second in <strong>the</strong> Ms. Wheelchair<br />
America pageant.<br />
<strong>Shepherd</strong> <strong>Center</strong>’s<br />
2009 Annual Report<br />
Available Online<br />
<strong>Shepherd</strong> <strong>Center</strong>’s 2009 Annual Report is<br />
available both online and in printed format.<br />
The report includes statistical information<br />
about <strong>Shepherd</strong> patients, financial information<br />
about <strong>the</strong> hospital and information about<br />
philanthropic gifts to<br />
<strong>the</strong> <strong>Shepherd</strong> <strong>Center</strong><br />
Foundation.<br />
It also includes features<br />
on <strong>Shepherd</strong>’s programs<br />
in <strong>the</strong>rapeutic recreation<br />
and assistive technology,<br />
<strong>the</strong> Marcus Community<br />
Bridge Program, animalassisted<br />
<strong>the</strong>rapy and <strong>the</strong><br />
Patient Care and Patient<br />
Equipment funds.<br />
Also available both<br />
online and in print is a<br />
separate donor directory<br />
that lists individual and organizational donors,<br />
as well as Bridge Builders and endowed funds.<br />
To request copies, contact Dean Melcher at<br />
404-350-7306 or dean_melcher@shepherd.<br />
org. Also, you can download electronic copies<br />
in PDF format from our Web site at<br />
www.shepherd.org/publications.<br />
Fall 2009 3 7
LovingTributes<br />
Honorariums<br />
Honorees are listed first in bold print followed by <strong>the</strong> names of<br />
those making gifts in <strong>the</strong>ir honor. This list reflects gifts made to<br />
<strong>Shepherd</strong> <strong>Center</strong> between June 1, 2009 and July 31, 2009.<br />
Cyndae Arrendale’s Birthday<br />
Mr. and Mrs. Steve A. Williams<br />
Winkie Arrendale’s Birthday<br />
Mr. and Mrs. Steve A. Williams<br />
Marla Jones Bennett’s Birthday<br />
Mr. and Mrs. Thomas J. Bennett<br />
Irene Berson’s Recovery<br />
Mrs. William Schwartz<br />
Rachel D. Betzler – “Thanks for<br />
C.V. help.”<br />
Dr. David F. Apple, Jr.<br />
Susan Bowen – “Congratulations on<br />
<strong>the</strong> JCAHO results.”<br />
Dr. David F. Apple, Jr.<br />
Richard Brazones’ Birthday<br />
Mr. and Mrs. Patrick T. Hickey, Jr.<br />
Wanda Buckley’s Marriage to<br />
Dr. Steven Morganstern<br />
Mr. and Mrs. Joel K. Isenberg<br />
William F. Bundy<br />
Ms. Susan Gregory<br />
Dr. and Mrs. Christopher Clare – For<br />
<strong>the</strong>ir Unending Love and Support<br />
Ms. Carol A. Clare<br />
Jonathan R. Cromwell – We Ride<br />
for <strong>Shepherd</strong><br />
Mr. R. James Cromwell<br />
Hill Daniel<br />
Mr. Phillip Lee<br />
Mr. and Mrs. Douglas S. Simpson<br />
Jason DiSanto<br />
Mr. and Mrs. Giuseppe Vitulli<br />
Carol Chambers and Col. Jack<br />
Gibson’s Wedding<br />
Mr. and Mrs. Joel K. Isenberg<br />
Kim Harrison<br />
Mr. Dan Chase<br />
Cathy Ellis and Greg Hendrix’s<br />
Wedding<br />
Mr. and Mrs. Jere V. Garde<br />
Steve Holleman – Great CFO of<br />
<strong>the</strong> Year<br />
Dr. David F. Apple, Jr.<br />
Captain Brian Jantzen<br />
Mr. and Mrs. Robert Jantzen<br />
Linda Jones, PT – “Thanks for all<br />
your hard work.”<br />
Dr. David F. Apple, Jr.<br />
Kings County Bicyclists<br />
Mr. Gary Chuba<br />
Joan Latiolais<br />
Mr. Stan Topol<br />
Mae Laverty<br />
Mr. and Mrs. William Laverty<br />
Above: Donor Sydell<br />
Harris, right, founder of Spa<br />
Sydell based in Atlanta,<br />
volunteers her time to provide<br />
makeovers to female patients<br />
at <strong>Shepherd</strong> <strong>Center</strong>.<br />
Donald Peck Leslie, M.D.<br />
Mrs. Morris I. McDonald<br />
Donald Peck Leslie, M.D. – “For<br />
saving lives and changing lives<br />
for <strong>the</strong> better forever”<br />
Ms. Carol A. Clare<br />
Leslie and Hugh McLeod<br />
Dr. and Mrs. William A. Blincoe<br />
Brian Mock’s Recovery<br />
Mr. and Mrs. Ronald L. Mock<br />
Michael Moderow<br />
Mr. and Mrs. Joseph Moderow<br />
Laurence Moore – “Thanks for your<br />
great job.”<br />
Dr. David F. Apple, Jr.<br />
Anthony Orig’s Ride for <strong>Shepherd</strong><br />
Carroll County Nephrology, PC<br />
Mr. Jim LaRocca<br />
Dr. Harry Uy<br />
Carrie Ann Patterson’s Graduation<br />
– Receipt of Doctor of Physical<br />
Therapy Degree<br />
Ms. Teresa L. Little<br />
Libby Pearce<br />
Mrs. Virginia Roe<br />
Matt Sanchez’s Efforts for our Troops<br />
Mr. William E. Barry<br />
Mr. Steve Branigan<br />
Mr. John Brucato<br />
Mtn. View RV, Inc.<br />
Dr. Harry Uy<br />
Janis Sheftel’s Retirement<br />
The UPS Foundation<br />
Beverly and Jack Shields<br />
Mr. John R. Simmerman<br />
Dell Sikes – Gritz at <strong>the</strong> Ritz<br />
Mr. and Mrs. Louie A. Pittman, Jr.<br />
Elizabeth Fowler Smith<br />
Mr. K. Boynton Smith<br />
Nicole Smith and Bryan Wynn’s<br />
Engagement<br />
Mrs. Mary E. Forgione<br />
LTG Stephen Speakes<br />
Captain Brennan Speakes<br />
Smith Wallace’s Birthday<br />
Mr. Harold R. Smith<br />
Phillip Watters<br />
Ms. Christine Lynn<br />
Photo by Gary Meek<br />
Molly Welch<br />
Mrs. Kyle Watzman<br />
Mr. Gerald Welch<br />
The Birth of Audrey Turner Wilson<br />
Mr. and Mrs. James H. <strong>Shepherd</strong> III<br />
Mr. and Mrs. Mark M. Whitney<br />
Above: The fifth floor of <strong>the</strong> Marcus-Woodruff Building is almost complete. Staff and patients from <strong>the</strong><br />
Spinal Cord Injury Unit expect to move in soon.<br />
Hortense B. Wolf<br />
Mr. and Mrs. David D. Wolf<br />
3 8 Spinal Column<br />
w w w. s h e p h e r d . o r g
LovingTributes<br />
Memorials<br />
Deceased friends of <strong>Shepherd</strong> <strong>Center</strong> are listed first in bold<br />
print followed by <strong>the</strong> names of those making gifts in <strong>the</strong>ir<br />
memory. This list reflects gifts made to <strong>Shepherd</strong> <strong>Center</strong><br />
between June 1, 2009 and July 31, 2009.<br />
Craig Alford<br />
Mr. and Mrs. Edwin Cowart<br />
Danforth P. Bearse<br />
Mrs. Frank C. Bowen, Jr.<br />
Mr. and Mrs. Edwin Cowart<br />
Griffin B. Bell<br />
Mr. and Mrs. Geoffrey S. Fishman<br />
Jonathan M. Be<strong>the</strong>l – In Loving<br />
Memory<br />
Mr. and Mrs. Robert M. Slider<br />
Lauren Clark<br />
Mr. and Mrs. William T. Hopkins<br />
David and Billy Foster<br />
Ms. Jane S. Taylor<br />
W. A. Gardner<br />
Mr. and Mrs. Gary Roques<br />
Malissa L. Grady<br />
Mr. and Mrs. Richard W. Sorenson<br />
Silas G. Gurley, Jr.<br />
Mr. and Mrs. Donald Atcheson<br />
Mr. John R. Atcheson<br />
Delree, Annette and Bob Friant<br />
Dr. Aprille Holland<br />
Mr. and Mrs. Jack Julian and Family<br />
McKenney's, Inc.<br />
John Drayton Conley, M.D.<br />
Mr. and Mrs. Larry Anderson<br />
Mrs. Sandra S. Biggs<br />
Mr. and Mrs. Lanny W. Marsh<br />
Suzanne Schilling Doughtie<br />
Mrs. Frank C. Bowen, Jr.<br />
Larry Doyal<br />
Mr. and Mrs. James M. Caswell, Jr.<br />
Mrs. Patricia C. Williams<br />
Paul A. Duke<br />
Mr. and Mrs. Edwin Cowart<br />
Mr. and Mrs. Theodore M. Forbes, Jr.<br />
Mr. and Mrs. Connor F. Nelson, Jr.<br />
Mr. and Mrs. William R. Newton<br />
Mr. and Mrs. Louie A. Pittman, Jr.<br />
Lil Hankey<br />
Elizabeth and Mark Pope<br />
Zuma W. Harris<br />
Mr. and Mrs. Nick Brink<br />
Mr. and Mrs. Grifton Carden<br />
Mrs. Peg Confer<br />
Mr. and Mrs. Paul Corley<br />
Captain and Mrs. James C. Hatch<br />
Mrs. Betty Ann Inman<br />
Mr. and Mrs. Daniel Kuerner<br />
Mr. and Mrs. Benjamin L. Mason<br />
Mr. and Mrs. William D. Morrison<br />
Mr. and Mrs. William H. Schneidewind, Jr.<br />
Ms. Rebecca Shuler<br />
Ms. Nancy B. Thomas<br />
Mr. and Mrs. Almand J. Westbrook, Sr.<br />
Mr. and Mrs. Randolph Wolfe<br />
Above: Players and cheerleaders for <strong>the</strong> Atlanta Falcons visited<br />
<strong>Shepherd</strong> <strong>Center</strong> rehabilitation inpatients at <strong>the</strong> hospital this<br />
past summer.<br />
Paul Bowen<br />
1924-2009<br />
<strong>Shepherd</strong> <strong>Center</strong> celebrates <strong>the</strong> life of beloved<br />
volunteer Paul Bowen, who passed away on Aug.<br />
26. Paul had been a donor and volunteer since<br />
1985. In 2003, Paul was honored as one of <strong>the</strong><br />
11Alive Community Service Award recipients<br />
for founding “The Breakfast Club,” a group of<br />
volunteers who assist with feeding breakfast to our<br />
patients. The Breakfast Club and <strong>Shepherd</strong> <strong>Center</strong><br />
salute his faithful service to volunteering for this<br />
program for many years.<br />
Paul personally recorded more than 3,500<br />
volunteer hours since 1992 and earned himself <strong>the</strong><br />
nickname “The Colonel” by <strong>the</strong> o<strong>the</strong>r Breakfast<br />
Club members for his take-charge, former Marine<br />
approach. In 2002, <strong>Shepherd</strong> <strong>Center</strong> presented Paul<br />
with a Bronze Star for his excellent customer service<br />
to our patients and staff. In 2007, Paul was named<br />
<strong>Shepherd</strong> <strong>Center</strong> Angel of <strong>the</strong> Year to honor his<br />
service to our patients and <strong>the</strong>ir families.<br />
Fall 2009 3 9
LovingTributes<br />
John W. McIntyre, Sr.<br />
Mr. and Mrs. James M. Caswell, Jr.<br />
Mrs. Joan Woodall<br />
Rebecca Cox McKinley<br />
Mr. and Mrs. James M. Caswell, Jr.<br />
Alice Davis McKnight<br />
Mrs. Frank C. Bowen, Jr.<br />
Mr. and Mrs. Edwin Cowart<br />
John O. Mitchell<br />
Mrs. John Jungman<br />
Caleb C. Moffat<br />
Jacksonville Hockey Boosters<br />
Club, Inc.<br />
B. Waldo “Buck” Moore, M.D.<br />
Ms. Marcia J. Hubbard<br />
Ms. Mabel A. Nicholson<br />
Mr. and Mrs. J. Harold <strong>Shepherd</strong><br />
Joseph K. Orr III<br />
Mr. and Mrs. William C. Rawson, Sr.<br />
Ronald Parker<br />
Mrs. John R. Robinson<br />
David C. Patrick II<br />
Dr. and Mrs. C. W. Bolinger<br />
Ms. Jeanne K. Costigan<br />
Mr. and Mrs. William Eller<br />
Mr. and Mrs. Walter P. Ledet<br />
Mrs. Frances F. Outland<br />
Above: Former spinal cord injury patients Mat<strong>the</strong>w Sanchez, left, and Dillon Cannon, center,<br />
were interviewed in August by CNN's Dr. Sanjay Gupta. Mat<strong>the</strong>w and some friends completed<br />
a cross-country bicycle ride this past summer to raise money for <strong>the</strong> SHARE Initiative, which<br />
funds care for soldiers and veterans, such as Dillon.<br />
Alexander Radev<br />
Mr. and Mrs. Skip Foley<br />
Claire Rappaport<br />
Ms. Sally Atwell<br />
Nathan Robertson<br />
Mr. and Mrs. Milton Jacobson<br />
Robert Lee Harvey<br />
Mrs. R. B. Lippincott, Jr.<br />
Charles E. Houswirth, Sr.<br />
Mrs. Lindsey Hopkins III<br />
Ken Hawkins<br />
Mr. Alex Painter<br />
Jennings Hertz, Jr.<br />
Mr. and Mrs. J. Harold <strong>Shepherd</strong><br />
McArba Hunter<br />
Mr. and Mrs. Joel K. Isenberg<br />
Jack Izard<br />
Mr. and Mrs. James M. Caswell, Jr.<br />
Robert Joel<br />
Mrs. Patricia C. Williams<br />
Ralph “RNK” Kelley<br />
Mr. and Mrs. Thomas J. Bennett, Jr.<br />
Dr. John Dudley King, Sr.<br />
Mr. and Mrs. Marshall J. Bachman<br />
Mr. and Mrs. Rhea Bowden<br />
Mr. and Mrs. Lawrence W. Gillespie<br />
Mrs. Frank S. Goodman<br />
Ms. Peggy Hatcher<br />
Mr. and Mrs. William C. Hatcher<br />
Ms. Mary Klein<br />
Pat and Tricia McConathy<br />
Elizabeth and Mark Pope<br />
Mr. Richard F. Romeo<br />
Mr. and Mrs. J. Harold <strong>Shepherd</strong><br />
Mrs. Patricia C. Williams<br />
Tom King<br />
Harp & Callier, LP<br />
O. David Kulman<br />
Dr. and Mrs. David F. Apple, Jr.<br />
Mavis P. Leslie<br />
Dr. and Mrs. David DuBose<br />
Roberta Letton<br />
Mrs. J. Lucian Smith<br />
Tim Lovelace<br />
Ms. Jane S. Taylor<br />
Donald M. Lynch<br />
Mr. and Mrs. Christopher W. Cay<br />
Nathan “Nat” Manning<br />
U.S. Customs Law Enforcement<br />
Explorers Post 4601, Newark, NJ<br />
Elizabeth Deckle Marks<br />
Mr. John Barton Marks, Jr.<br />
Ellen Marrs’ Mo<strong>the</strong>r<br />
Mr. and Mrs. Mark W. Slonaker<br />
Lawrence F. McArdle<br />
Mrs. Barbara McArdle<br />
Madlyn McCollum<br />
Dr. and Mrs. David F. Apple, Jr.<br />
Don McDaniel<br />
Dr. and Mrs. Brock Bowman<br />
Ms. Nora Mangrum<br />
<strong>Shepherd</strong> <strong>Center</strong> Financial<br />
Services and Materials<br />
Management Staff<br />
<strong>Shepherd</strong> <strong>Center</strong> Foundation Staff<br />
Dr. and Mrs. David L. Smith<br />
Dr. Allen McDonough<br />
Mr. and Mrs. Theodore M.<br />
Forbes, Jr.<br />
Harold C. McKenzie<br />
Mr. and Mrs. J. Harold <strong>Shepherd</strong><br />
Mrs. Joan Woodall<br />
Sherri Rudd<br />
Mr. and Mrs. Bruce Barkley<br />
Mr. Gerald Barnes<br />
Benchmark Rehabilitation<br />
Mr. and Mrs. Wayne Cranford<br />
Mr. and Mrs. Lewis J. DiPrima<br />
Ms. Patricia Harwell<br />
Mr. and Mrs. Byrne E. Heninger<br />
Dr. and Mrs. Mark Lobstein<br />
Ms. Betsy McDaniel<br />
Ms. Mary L. Rudd<br />
Ms. Pat Walter<br />
White County Middle School<br />
Mr. and Mrs. Mark Winchester<br />
Dr. Leigh Scott<br />
Mr. and Mrs. James M. Caswell, Jr.<br />
Sallie Sellers<br />
Mr. John M. Tinley<br />
Charles R. <strong>Shepherd</strong><br />
Mr. and Mrs. Louie A. Pittman, Jr.<br />
Captain Sean P. Sims<br />
Mr. Thomas Sims<br />
Wyman P. Sloan, M.D.<br />
Mr. and Mrs. J. Harold <strong>Shepherd</strong><br />
Mrs. Patricia C. Williams<br />
4 0 Spinal Column<br />
w w w. s h e p h e r d . o r g
Anita M. Smith<br />
Mrs. Frank C. Bowen, Jr.<br />
Laura Maddox Smith<br />
Dr. and Mrs. David F. Apple, Jr.<br />
Mr. and Mrs. James M. Caswell, Jr.<br />
Mr. and Mrs. Theodore M. Forbes, Jr.<br />
Mr. and Mrs. J. Harold <strong>Shepherd</strong><br />
Wilfred Sollenberger<br />
Mrs. R. B. Lippincott, Jr.<br />
Mrs. Stark – Ruth Baxter’s Mo<strong>the</strong>r<br />
Mr. and Mrs. T. Ray Logan<br />
Doris Rose Thomas<br />
Mr. and Mrs. James R. Balkcom, Jr.<br />
Mr. and Mrs. Jack J. Berlin<br />
Mr. and Mrs. Ronald B. Bobo<br />
Mr. Broughton Ferguson<br />
Mr. and Mrs. William M. Graves<br />
Governor and Mrs. Joe F. Harris<br />
Mr. and Mrs. Wilder G. Little<br />
Mr. and Mrs. Bryan E. Marshall<br />
Mr. and Mrs. Kenneth W. Miller, Jr.<br />
Mr. and Mrs. James M. Morris<br />
Ms. Ann P. Morriss<br />
Mr. David C. Mulkey<br />
Mr. and Mrs. Arthur J. Schwartz<br />
Mr. and Mrs. Richard W. Taylor<br />
Mr. and Mrs. Ken Thrasher<br />
Mr. Andrew Turner<br />
Mr. Jerry Wi<strong>the</strong>rs<br />
Frank “Bubba” Thurmond<br />
Mr. David G. Hall<br />
Above: Atlanta Falcons players found some fans when <strong>the</strong>y visited <strong>Shepherd</strong> <strong>Center</strong><br />
inpatients this past summer.<br />
Lee Timberlake<br />
Ms. Linda Crowley<br />
Mark P. Tomlinson<br />
Mr. and Mrs. James M. Caswell, Jr.<br />
Hardon McDonald Wade III<br />
Mrs. Virginia Iszard<br />
John Watt<br />
Mr. Spencer W. Smith, Sr.<br />
Walter C. Wattles<br />
Mr. and Mrs. William R. Newton<br />
Elizabeth and Mark Pope<br />
Brenda White<br />
Mr. and Mrs. William T. Hopkins<br />
Tate Wright, Jr.<br />
Mr. and Mrs. C. Alexander Peterson<br />
Margaret <strong>Shepherd</strong> Yates<br />
Cobb Community Foundation<br />
Mr. and Mrs. P. Daniel Yates III<br />
Lawson Yow<br />
Mr. and Mrs. James M. Caswell, Jr.<br />
Mr. and Mrs. J. Harold <strong>Shepherd</strong><br />
Josephine Zachary<br />
Dr. and Mrs. Brock Bowman<br />
Mr. and Mrs. Stephen B. Goot<br />
Mr. and Mrs. J. Harold <strong>Shepherd</strong><br />
The <strong>Shepherd</strong> <strong>Center</strong> Auxiliary<br />
Mr. and Mrs. Dell B. Sikes<br />
Mr. and Mrs. Terrence M. Tracy<br />
Above: Former brain injury patient Brooke Albright of Troy, Tenn., participates in art <strong>the</strong>rapy with<br />
lead Acquired Brain Injury Unit recreation <strong>the</strong>rapist Ashley Haynes.<br />
Fall 2009 4 1
Address Service Requested<br />
Read <strong>the</strong> magazine<br />
online at:<br />
spinalcolumn.org<br />
Photo Courtesy of Brian Waldersen<br />
A Dream No Longer Deferred<br />
Brian Waldersen’s dream to go to medical school was sidelined after a February<br />
2007 car accident injured his C-5 to C-7 vertebrae, leaving him a quadriplegic.<br />
But Brian’s dream is back on track.<br />
This past summer, he moved from Phoenix to Baltimore and began studying<br />
medicine at Johns Hopkins University on Aug. 17. He will be <strong>the</strong> first person in<br />
a wheelchair ever to attend medical school at <strong>the</strong> university.<br />
“It feels good to be focused on something and have a true purpose,” says<br />
Brian, who spent four months at <strong>Shepherd</strong>. “Before <strong>the</strong> accident, I had been<br />
thinking about med school for four or five years. Now it’s here, and I’m ready to<br />
get going.”<br />
While Johns Hopkins held Brian to <strong>the</strong> same standards as all o<strong>the</strong>r applicants,<br />
<strong>the</strong> university is making some adjustments in environment and equipment to accommodate<br />
him. The medical school purchased a specialized power wheelchair<br />
that allows Brian to stand and move around, as well as adapted standard equipment<br />
and instruments such as his stethoscope. Brian plans to review Webcasts<br />
and online class notes and complete assignments using voice-activated software.<br />
“It will definitely be a challenge because I’m not at <strong>the</strong> same physical level as<br />
everyone else,” Brian says. “But I’m up for it.”<br />
Brian is interested in shaping health policy, possibly by working in an academic<br />
setting, although he hasn’t ruled out treating patients. “I’m especially interested<br />
in working to address health disparities within <strong>the</strong> disabled community,” he says.