HP Enterprise Services - DHHR
HP Enterprise Services - DHHR
HP Enterprise Services - DHHR
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>HP</strong>ES Response to West Virginia MMIS Re-procurement RFP<br />
4.1.10 Solution Alignment with BMS’ Business and Technical Needs<br />
the new policies through the online application, reducing reliance on technical staff members and accelerating the<br />
implementation time line. Multiple programs, plans, and payer features are supported in interChange through the user interface,<br />
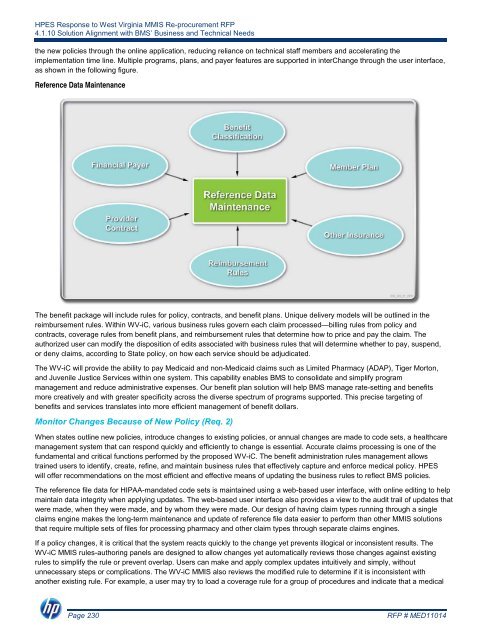
as shown in the following figure.<br />
Reference Data Maintenance<br />
The benefit package will include rules for policy, contracts, and benefit plans. Unique delivery models will be outlined in the<br />
reimbursement rules. Within WV-iC, various business rules govern each claim processed—billing rules from policy and<br />
contracts, coverage rules from benefit plans, and reimbursement rules that determine how to price and pay the claim. The<br />
authorized user can modify the disposition of edits associated with business rules that will determine whether to pay, suspend,<br />
or deny claims, according to State policy, on how each service should be adjudicated.<br />
The WV-iC will provide the ability to pay Medicaid and non-Medicaid claims such as Limited Pharmacy (ADAP), Tiger Morton,<br />
and Juvenile Justice <strong>Services</strong> within one system. This capability enables BMS to consolidate and simplify program<br />
management and reduce administrative expenses. Our benefit plan solution will help BMS manage rate-setting and benefits<br />
more creatively and with greater specificity across the diverse spectrum of programs supported. This precise targeting of<br />
benefits and services translates into more efficient management of benefit dollars.<br />
Monitor Changes Because of New Policy (Req. 2)<br />
When states outline new policies, introduce changes to existing policies, or annual changes are made to code sets, a healthcare<br />
management system that can respond quickly and efficiently to change is essential. Accurate claims processing is one of the<br />
fundamental and critical functions performed by the proposed WV-iC. The benefit administration rules management allows<br />
trained users to identify, create, refine, and maintain business rules that effectively capture and enforce medical policy. <strong>HP</strong>ES<br />
will offer recommendations on the most efficient and effective means of updating the business rules to reflect BMS policies.<br />
The reference file data for HIPAA-mandated code sets is maintained using a web-based user interface, with online editing to help<br />
maintain data integrity when applying updates. The web-based user interface also provides a view to the audit trail of updates that<br />
were made, when they were made, and by whom they were made. Our design of having claim types running through a single<br />
claims engine makes the long-term maintenance and update of reference file data easier to perform than other MMIS solutions<br />
that require multiple sets of files for processing pharmacy and other claim types through separate claims engines.<br />
If a policy changes, it is critical that the system reacts quickly to the change yet prevents illogical or inconsistent results. The<br />
WV-iC MMIS rules-authoring panels are designed to allow changes yet automatically reviews those changes against existing<br />
rules to simplify the rule or prevent overlap. Users can make and apply complex updates intuitively and simply, without<br />
unnecessary steps or complications. The WV-iC MMIS also reviews the modified rule to determine if it is inconsistent with<br />
another existing rule. For example, a user may try to load a coverage rule for a group of procedures and indicate that a medical<br />
Page 230<br />
RFP # MED11014