Preventing Suicide - SPINZ
Preventing Suicide - SPINZ
Preventing Suicide - SPINZ
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
S u i c i d e P r e v e n t i o n I n f o r m a t i o n N e w Z e a l a n d<br />
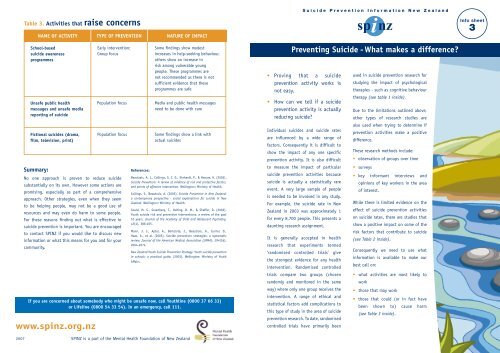
Table 3. Activities that raise concerns<br />
NAME OF ACTIVITY TYPE OF PREVENTION NATURE OF IMPACT<br />
Info sheet<br />
3<br />
School-based<br />
suicide awareness<br />
programmes<br />
Unsafe public health<br />
messages and unsafe media<br />
reporting of suicide<br />
Fictional suicides (drama,<br />
film, television, print)<br />
Summary:<br />
No one approach is proven to reduce suicide<br />
substantially on its own. However some actions are<br />
promising, especially as part of a comprehensive<br />
approach. Other strategies, even when they seem<br />
to be helping people, may not be a good use of<br />
resources and may even do harm to some people.<br />
For these reasons finding out what is effective in<br />
suicide prevention is important. You are encouraged<br />
to contact <strong>SPINZ</strong> if you would like to discuss new<br />
information or what this means for you and for your<br />
community.<br />
Early intervention;<br />
Group focus<br />
Population focus<br />
Population focus<br />
References:<br />
Beautrais, A. L., Collings, S. C. D., Ehrhardt, P., & Henare, K. (2005).<br />
<strong>Suicide</strong> Prevention: A review of evidence of risk and protective factors,<br />
and points of effective intervention. Wellington: Ministry of Health.<br />
Collings, S., Beautrais, A. (2005). <strong>Suicide</strong> Prevention in New Zealand:<br />
a contemporary perspective - social explanations for suicide in New<br />
Zealand. Wellington: Ministry of Health.<br />
Gould, M. S., Greenberg, T., Velting, D. M., & Shaffer, D. (2003).<br />
Youth suicide risk and preventive interventions: a review of the past<br />
10 years. Journal of the Academy of Child and Adolescent Psychiatry,<br />
42(4), 386-405.<br />
Mann, J. J., Apter, A., Bertolote, J., Beautrais, A., Currier, D.,<br />
Haas, A., et al. (2005). <strong>Suicide</strong> prevention strategies: a systematic<br />
review. Journal of the American Medical Association (JAMA), 294(16),<br />
2064-2074.<br />
New Zealand Youth <strong>Suicide</strong> Prevention Strategy: Youth suicide prevention<br />
in schools: a practical guide. (2003). Wellington: Ministry of Youth<br />
Affairs.<br />
Some findings show modest<br />
increases in help-seeking behaviour,<br />
others show an increase in<br />
risk among vulnerable young<br />
people. These programmes are<br />
not recommended as there is not<br />
sufficient evidence that these<br />
programmes are safe<br />
Media and public health messages<br />
need to be done with care<br />
Some findings show a link with<br />
actual suicides<br />
If you are concerned about somebody who might be unsafe now, call Youthline (0800 37 66 33)<br />
or Lifeline (0800 54 33 54). In an emergency, call 111.<br />
www.spinz.org.nz<br />
<strong>Preventing</strong> <strong>Suicide</strong> - What makes a difference?<br />
• Proving that a suicide<br />
prevention activity works is<br />
not easy.<br />
• How can we tell if a suicide<br />
prevention activity is actually<br />
reducing suicide?<br />
Individual suicides and suicide rates<br />
are influenced by a wide range of<br />
factors. Consequently it is difficult to<br />
show the impact of any one specific<br />
prevention activity. It is also difficult<br />
to measure the impact of particular<br />
suicide prevention activities because<br />
suicide is actually a statistically rare<br />
event. A very large sample of people<br />
is needed to be involved in any study.<br />
For example, the suicide rate in New<br />
Zealand in 2003 was approximately 1<br />
for every 8,700 people. This presents a<br />
daunting research assignment.<br />
It is generally accepted in health<br />
research that experiments termed<br />
‘randomised controlled trials’ give<br />
the strongest evidence for any health<br />
intervention. Randomised controlled<br />
trials compare two groups (chosen<br />
randomly and monitored in the same<br />
way) where only one group receives the<br />
intervention. A range of ethical and<br />
statistical factors add complications to<br />
this type of study in the area of suicide<br />
prevention research. To date, randomised<br />
controlled trials have primarily been<br />
used in suicide prevention research for<br />
studying the impact of psychological<br />
therapies - such as cognitive behaviour<br />
therapy (see table 1 inside).<br />
Due to the limitations outlined above,<br />
other types of research studies are<br />
also used when trying to determine if<br />
prevention activities make a positive<br />
difference.<br />
These research methods include:<br />
• observation of groups over time<br />
• surveys<br />
• key informant interviews and<br />
opinions of key workers in the area<br />
of interest.<br />
While there is limited evidence on the<br />
effect of suicide prevention activities<br />
on suicide rates, there are studies that<br />
show a positive impact on some of the<br />
risk factors that contribute to suicide<br />
(see Table 2 inside).<br />
Consequently we need to use what<br />
information is available to make our<br />
best call on:<br />
• what activities are most likely to<br />
work<br />
• those that may work<br />
• those that could (or in fact have<br />
been shown to) cause harm<br />
(see Table 3 inside).<br />
2007 <strong>SPINZ</strong> is a part of the Mental Health Foundation of New Zealand
A programme is most likely to be safe and make a positive difference if it is aligned with research evidence<br />
that shows this type of activity is effective. This is an important consideration with suicide prevention<br />
because of the potential to do harm.<br />
<strong>SPINZ</strong> has used the evidence from recent extensive reviews of the research literature to compile a summary<br />
of what the international evidence shows us as at January 2006.<br />
Note on Tables: Activities / interventions generally fit along a continuum from promoting<br />
wellbeing and healthy development to early identification through to clinical services.<br />
Activities / interventions are aimed at individuals, groups, or whole populations.<br />
Table 2. Activities which have some evidence of effectiveness<br />
Population Focus<br />
NAME OF ACTIVITY TYPE OF PREVENTION NATURE OF IMPACT<br />
Media education and guidelines Reducing risk Can limit suicide contagion (e.g. copycat<br />
suicides)<br />
Public awareness of depression/mental<br />
health literacy (e.g. destigmatisation of<br />
mental illness, depression recognition<br />
programmes)<br />
Promoting wellbeing<br />
May increase help-seeking<br />
Improving the control of alcohol Reducing risk May reduce problem alcohol use which is<br />
a risk factor for suicide<br />
Whanau, hapu, iwi, taitamariki<br />
development<br />
Promoting wellbeing<br />
Recognises international best practice<br />
and also subscribes to unique Maori<br />
values, processes and social institutions<br />
Telephone hotlines and crisis centres Early identification Some impact on risk factors<br />
Table 1. Activities with good evidence of effectiveness<br />
NAME OF ACTIVITY<br />
Psychological therapies<br />
(e.g. Cognitive Behavioural<br />
Therapy, Problem Solving<br />
Therapy, Dialectic Behavioural<br />
Therapy, Interpersonal<br />
Psychotherapy)<br />
Restriction of access to<br />
means (e.g. control of<br />
guns and toxic substances,<br />
removing hanging points<br />
in prisons or mental health<br />
inpatient units)<br />
TYPE OF PREVENTION<br />
Clinical services;<br />
Individual focus<br />
Reducing risk;<br />
Population focus<br />
NATURE OF IMPACT<br />
Reduction in depression and<br />
some reductions in suicidal<br />
behaviour among specific<br />
high risk groups<br />
Reduction in suicide<br />
attempts using that means<br />
and sometimes reduction in<br />
total suicides<br />
Group Focus<br />
Internet/computer based tools Promoting wellbeing May improve help-seeking skills<br />
Interventions which strengthen families<br />
and individuals (e.g. decreasing family<br />
violence, child abuse, improving opportunities,<br />
improving problem solving & social skills,<br />
building resiliency or protective factors)<br />
Skills training (e.g. improving individuals or<br />
groups problem solving and coping skills)<br />
Targeted programmes (e.g. programmes<br />
that target substance abuse, depressive<br />
symptoms, anxiety & conduct disorders)<br />
Befriending, mentoring or volunteer<br />
support programmes<br />
Screening programmes - screening young<br />
people or groups who are at increased risk<br />
(such as those in social welfare care) for<br />
depression or suicide risk<br />
Reducing risk;<br />
Promoting wellbeing<br />
Promoting wellbeing<br />
Early identification;<br />
Reducing risk<br />
Early intervention<br />
Early identification<br />
This may limit risk factors or the impact<br />
of risk factors<br />
Some reduction in risk factors<br />
Often some improvement regarding<br />
targeted risk factor<br />
Where the programmes are well run there<br />
can be some impact on risk factors<br />
Can identify high-risk individuals. Needs<br />
to be a quality screening programme,<br />
with follow up for those who need it<br />
Postvention (support after a suicide) Reducing risk May decrease depressive symptoms<br />
amongst bereaved family. Addresses<br />
potential risks within affected people<br />
Education of doctors and<br />
other health professionals<br />
in recognition and treatment<br />
of depression<br />
Gatekeeper training (e.g.<br />
training of caregivers,<br />
military or prison personnel,<br />
school staff, pastors or others<br />
in recognising warning signs,<br />
getting assessment and<br />
treatment)<br />
Early identification<br />
Early identification<br />
Increases recognition and<br />
treatment of depression with<br />
some reductions in suicide<br />
Where gatekeepers are able<br />
to identify risk and facilitate<br />
access to treatment this<br />
can be effective and is a<br />
promising strategy to reduce<br />
suicide<br />
Individual Focus<br />
Co-ordinated follow up programmes<br />
Programmes which focus on pro-active,<br />
regular, co-ordinated follow-up of people<br />
who are at increased risk, e.g. managed care,<br />
collaborative case management or wrap around<br />
programmes for those with depression, those<br />
whom have attempted suicide, or who have<br />
recently been discharged from psychiatric care<br />
Primary health care and mental health<br />
care - programmes that make it easier for<br />
people to access or use primary health care<br />
or mental health care; provide training for<br />
staff and implement systems for recognising<br />
and treating depression and other mental<br />
health problems and assessing & managing<br />
suicide risk<br />
Clinical<br />
Clinical<br />
Can monitor and address current suicidal<br />
risk & promote wellbeing; likely to be an<br />
important strategy in reducing suicides<br />
Increase opportunity for early detection<br />
and management of suicide risk factors;<br />
likely to be an important strategy in<br />
reducing suicide<br />
Psychopharmacological interventions<br />
(e.g. medications for depression and other<br />
specific mental illnesses)<br />
Clinical<br />
Effective in treating the specific<br />
disorders, this may be an important<br />
strategy for reducing suicide