Field Guide for Supervisors of Medical and Dental ... - Oxford Deanery
Field Guide for Supervisors of Medical and Dental ... - Oxford Deanery
Field Guide for Supervisors of Medical and Dental ... - Oxford Deanery
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Health Education Thames Valley<br />
<strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong> <strong>of</strong> <strong>Medical</strong> <strong>and</strong> <strong>Dental</strong><br />
trainees working in the Ox<strong>for</strong>d Postgraduate <strong>Medical</strong><br />
& <strong>Dental</strong> Education (PGMDE) programmes<br />
(excluding training in General Practice)<br />
Jane Siddall, Associate Dean <strong>for</strong> Educator <strong>and</strong> Faculty Development<br />
John Derry, Director CDU <strong>and</strong> Associate Dean<br />
Tony Jefferis, Deputy Dean<br />
Simon Street, GP Associate Dean<br />
Greg Simons, GP Associate Dean<br />
Chris Morris, Associate Dean <strong>for</strong> Quality<br />
Amit Gupta, Associate Dean <strong>for</strong> International <strong>Medical</strong> Graduates<br />
First Edition April 2013<br />
This edition is valid until September 2013. New editions will be<br />
online at the Ox<strong>for</strong>d PGMDE website.<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v4.indd 1 16/04/2013 09:57
This h<strong>and</strong>book has been produced using material from the Gold <strong>Guide</strong>,<br />
(4th edition, 2010)<br />
GMC guidance (The Trainee Doctor, July 2011 <strong>and</strong> Tomorrow’s Doctors,<br />
Oct 2011)<br />
NACT guidance (Managing the Trainee in Difficulty, 2008),<br />
The Ox<strong>for</strong>d PGMDE workshops <strong>for</strong> both Clinical <strong>and</strong> Educational<br />
<strong>Supervisors</strong><br />
‘Best practice’ from Employment Tribunal experience, (August 2011).<br />
The UK Foundation Programme Reference <strong>Guide</strong>, (July 2012).<br />
Ox<strong>for</strong>d PGMDE Policies (2012)<br />
NHS <strong>Medical</strong> Careers website (2012)<br />
The British Dyslexia Association (2012)<br />
The Equality Act (2010)<br />
This first edition will be updated with feedback from users, <strong>and</strong> whenever<br />
there is a national change <strong>of</strong> significance. The most up to date iteration<br />
will be found on the deanery’s website in the Education section.<br />
If you have any comments about material, which you believe should be<br />
in this h<strong>and</strong>book, but is not, please email me at<br />
jane.siddall@thamesvalley.hee.nhs.uk<br />
Jane Siddall<br />
Associate Dean <strong>for</strong> Educator Faculty Development<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 2 09/04/2013 14:01
Contents<br />
Introduction <strong>and</strong> Background ...................................................................... 4<br />
Chapter 1: Definitions <strong>and</strong> Differences ....................................................... 6<br />
Chapter 2: What are the ‘essential’ responsibilities <strong>of</strong><br />
Clinical <strong>Supervisors</strong>? ...................................................................................... 8<br />
Chapter 3: Feedback on per<strong>for</strong>mance ....................................................... 11<br />
Chapter 4: The International <strong>Medical</strong> Graduate trainee .......................... 14<br />
Chapter 5: ‘Something isn’t right’ .............................................................. 16<br />
Appendices<br />
A: ARCP outcomes<br />
B: Generation Y: what they expect<br />
C: The Ox<strong>for</strong>d PGMDE Descriptors <strong>of</strong> Behaviour<br />
D: Adult checklist <strong>for</strong> Dyslexia<br />
E: Role <strong>of</strong> educational supervisor in the revalidation <strong>of</strong> trainees<br />
Ox<strong>for</strong>d PGMDE polices are accessible from the home page <strong>of</strong> the deanery’s<br />
website at www.ox<strong>for</strong>ddeanery.nhs.uk<br />
Policies that may be especially useful include<br />
• Policy <strong>for</strong> approving <strong>and</strong> recognising medical <strong>and</strong> dental trainers<br />
(covers training requirements, time, duties etc, found in the Educator<br />
Development section)<br />
• Equality <strong>and</strong> Diversity<br />
• Bullying <strong>and</strong> Harassment<br />
• IMG policy<br />
• Less than fulltime training<br />
• Trainee in difficulty / Supporting the Trainee<br />
And can be found in the ‘About Ox<strong>for</strong>d <strong>Deanery</strong> section’ <strong>of</strong> the website<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 3<br />
49087 Ox PGMDE H<strong>and</strong>book v5.indd 3 18/04/2013 12:44
Introduction<br />
Forward by Postgraduate Dean:<br />
“The expectations on those who undertake roles in medical <strong>and</strong> dental<br />
education have increased significantly in the last few years. There is now a<br />
requirement <strong>for</strong> us to properly induct, plan, assess, deliver specific curriculum<br />
objectives <strong>and</strong> vitally, record many aspects <strong>of</strong> doctors/dentists’ per<strong>for</strong>mance<br />
during their training. There is abundant evidence that well-trained <strong>and</strong><br />
supported clinicians work safely; those who are not supported in this manner<br />
are more likely to be involved in adverse events which may damage their<br />
pr<strong>of</strong>essional st<strong>and</strong>ing, the reputation <strong>of</strong> the department, Trust or training<br />
programme as well as result in harm to patients.<br />
I am delighted that our team <strong>of</strong> Associate Deans have produced this field<br />
guide <strong>for</strong> trainers in medical <strong>and</strong> dental practice across our patch. It is<br />
intended to be a ‘Quick Look Book’ to help busy clinical <strong>and</strong> educational<br />
supervisors navigate through an increasingly complex training l<strong>and</strong>scape. It is<br />
not, however, a replacement <strong>for</strong> training in effective supervision.”<br />
Background<br />
Dr Michael Bannon<br />
Postgraduate Dean<br />
There are comprehensive national frameworks <strong>for</strong> Foundation, General Practice<br />
<strong>and</strong> Specialty Trainees, <strong>and</strong> local PGMDE policies, which can be accessed on<br />
the internet. Most, if not all, can be seen by visiting the deanery’s website at<br />
www.ox<strong>for</strong>ddeanery.nhs.uk <strong>and</strong> clicking on the relevant school tab. The new<br />
Foundation h<strong>and</strong>book can be downloaded from the Foundation Programme<br />
NHS website at http://www.foundationprogramme.nhs.uk<br />
Why is training (<strong>and</strong> support) <strong>for</strong> trainers important?<br />
During 2012 the GMC opened a consultation on the recognition <strong>and</strong> approval<br />
<strong>of</strong> non-GP trainers. The outcome <strong>of</strong> the consultation was published in August<br />
2012 as the GMC ‘Approving <strong>and</strong> Recognising Trainers: the Implementation<br />
Plan’. Trainers must have training, <strong>and</strong> have been updated as required under the<br />
PGMDE’s policy <strong>for</strong> Approving <strong>and</strong> Recognising <strong>Medical</strong> <strong>and</strong> <strong>Dental</strong> trainers.<br />
The GMC plan relates to:<br />
• Named educational supervisors in postgraduate training<br />
• Named clinical supervisors in postgraduate training<br />
• Lead co-ordinators <strong>of</strong> undergraduate training at each local education<br />
provider<br />
• Doctors responsible <strong>for</strong> overseeing students’ educational progress<br />
<strong>for</strong> each medical school.<br />
4<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v3.indd 4 12/04/2013 15:54
Other doctors whose practice contributes to the teaching, training or<br />
supervision <strong>of</strong> students or trainee doctors, on a more sessional or occasional<br />
basis, such as senior trainees <strong>and</strong> most specialty doctors who observe practice<br />
are not included in the GMC plan, but the PGMDE has commissioned training in<br />
supervision <strong>for</strong> such staff.<br />
The GMC trainer st<strong>and</strong>ards<br />
The GMC already has existing st<strong>and</strong>ards <strong>for</strong> postgraduate training set out<br />
in The Trainee Doctor (in section 6 <strong>of</strong> the 2011 publication) <strong>and</strong> <strong>for</strong><br />
undergraduate education in Tomorrow’s Doctors. These address<br />
• The differing levels <strong>of</strong> supervision trainees require during the entire<br />
postgraduate training programme, (6.29 to 6.31)<br />
• The expectation that the Postgraduate <strong>Medical</strong> education team will<br />
support the trainer <strong>and</strong> that job plans will factor time <strong>for</strong> the trainer to<br />
facilitate trainee development (6.32-6.36)<br />
• The expectation that trainers underst<strong>and</strong> the structure <strong>and</strong> purpose <strong>of</strong><br />
the training programme, <strong>and</strong> their role in training (6/38- 6.39)<br />
• And <strong>for</strong> GP training, section 6.37 stipulates that GP trainers must be<br />
trained <strong>and</strong> selected in accordance with the <strong>Medical</strong> Act 1983.<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 5<br />
49087 Ox PGMDE H<strong>and</strong>book v3.indd 5 12/04/2013 15:54
Chapter 1<br />
Definitions <strong>and</strong> Differences<br />
Definitions<br />
The GMC has defined the roles <strong>of</strong> both clinical <strong>and</strong> educational<br />
supervisors, which are:<br />
Named clinical supervisor: a trainer who is responsible <strong>for</strong> overseeing a<br />
specified trainee’s clinical work <strong>for</strong> a placement in a clinical environment <strong>and</strong><br />
is appropriately trained to do so. He or she will provide constructive feedback<br />
during that placement, <strong>and</strong> in<strong>for</strong>m the decision about whether the trainee<br />
should progress to the next stage <strong>of</strong> their training at the end <strong>of</strong> that placement<br />
<strong>and</strong>/or series <strong>of</strong> placements.<br />
Named educational supervisor: a trainer who is selected <strong>and</strong> appropriately<br />
trained to be responsible <strong>for</strong> the overall supervision <strong>and</strong> management <strong>of</strong> a<br />
trainee’s trajectory <strong>of</strong> learning <strong>and</strong> educational progress during a placement<br />
<strong>and</strong>/or series <strong>of</strong> placements. Every trainee must have a named educational<br />
supervisor. The educational supervisor’s role is to help the trainee to plan their<br />
training <strong>and</strong> achieve agreed learning outcomes. He or she is responsible <strong>for</strong><br />
the educational agreement <strong>and</strong> <strong>for</strong> bringing together all relevant evidence<br />
to <strong>for</strong>m a summative judgement at the end <strong>of</strong> the placement <strong>and</strong>/or series <strong>of</strong><br />
placements.<br />
It is expected that educational supervisors should have all the attributes<br />
expected <strong>of</strong> trained clinical supervisors. Being an educational supervisor<br />
does not necessarily preclude a trainer from having any other educational<br />
role, <strong>and</strong> is it desirable <strong>for</strong> senior educators to be active educational<br />
supervisors.<br />
PGMDE definitions <strong>of</strong> other key supervisors are:<br />
Academic supervisors are responsible to help the trainee to plan their research<br />
activity <strong>and</strong> achieve agreed outcomes. Even if he or she has a clinical contract,<br />
they should not normally be the trainee’s educational or clinical supervisor. He<br />
or she is required to provide an annual report on a trainee <strong>for</strong> the ARCP panel.<br />
A sessional supervisor is a clinician who supervises a trainee <strong>for</strong> individual<br />
sessions, <strong>and</strong> who may be required to provide <strong>for</strong>mal assessment <strong>and</strong> feedback<br />
on the trainee to their clinical, or educational, supervisor.<br />
6<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 6 09/04/2013 14:01
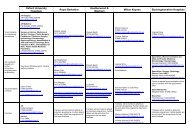
The<br />
The<br />
table<br />
table below,<br />
below,<br />
adapted<br />
adapted<br />
from<br />
from<br />
the<br />
the<br />
Ox<strong>for</strong>d<br />
Ox<strong>for</strong>d<br />
PGMDE<br />
PGMDE<br />
Clinical<br />
Clinical<br />
Supervisor<br />
Supervisor<br />
training workshop <strong>and</strong> RCPsych H<strong>and</strong>book <strong>for</strong> Trainers, summarises the<br />
training workshop <strong>and</strong> RCPsych H<strong>and</strong>book <strong>for</strong> Trainers, summarises the<br />
differences between clinical <strong>and</strong> educational supervisors:<br />
differences between clinical <strong>and</strong> educational supervisors:<br />
Clinical supervisor Attribute Educational supervisor<br />
Operational Vision Strategic<br />
Clinical Experience Depth <strong>and</strong> breadth<br />
Work place based<br />
assessments<br />
(Including feedback on<br />
per<strong>for</strong>mance)<br />
Assessment<br />
Educational/<br />
behavioural (e.g.<br />
multisource feedback)<br />
Clinical competence Curriculum All competencies (i.e.<br />
clinical <strong>and</strong><br />
pr<strong>of</strong>essional<br />
behaviours)<br />
Trainer <strong>and</strong> apprentice<br />
(To include equal<br />
opportunity <strong>and</strong> diversity<br />
awareness <strong>and</strong><br />
awareness <strong>of</strong> ‘trainee in<br />
difficulty’)<br />
Skills, knowledge <strong>and</strong><br />
experience<br />
Specified <strong>and</strong> defined<br />
(may include advice on<br />
suitable courses/ study<br />
leave)<br />
Relationship with<br />
trainee<br />
Evidence<br />
Guidance<br />
Mentor or coach<br />
(To include equal<br />
opportunity <strong>and</strong> diversity<br />
awareness <strong>and</strong><br />
awareness <strong>of</strong> ‘trainee in<br />
difficulty’)<br />
Portfolio <strong>of</strong> training<br />
progress<br />
Broad <strong>and</strong> generic (may<br />
include advice on suitable<br />
courses/ study leave)<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013 7<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 7<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 7 09/04/2013 14:01
Chapter 2<br />
What are the ‘essential’ responsibilities <strong>of</strong> Clinical<br />
<strong>Supervisors</strong>?<br />
It is important to make early contact with the trainees allocated to you, ideally<br />
face to face, but if not, by email to arrange a meeting. A suggested algorithm is<br />
at the end <strong>of</strong> this chapter.<br />
It is important that CSs in<strong>for</strong>m a trainee’s Educational Supervisor <strong>of</strong> anything<br />
which is noteworthy, but should include involvement in Serious Incidents,<br />
complaints from patients <strong>and</strong> health / probity issues (see Chapter 4) as these<br />
events are noted at ARCP <strong>and</strong> in<strong>for</strong>m the revalidation process.<br />
Your knowledge <strong>of</strong> the curriculum<br />
As a clinical supervisor (CS), one is not expected to produce the annual<br />
assessment report <strong>for</strong> the ARCP, but a CS should know what skills the trainee<br />
should develop, or acquire, during the phase <strong>of</strong> training with you. This should<br />
be available on your Royal College website.<br />
CSs do not personally have to sign <strong>of</strong>f every workplace-based assessment, but it<br />
is good practice <strong>for</strong> a proportion to be completed by a consultant. Some colleges<br />
require the final one confirming independent competence <strong>for</strong> a procedure to be<br />
signed by a consultant.<br />
Whilst a clinical supervisor will not be suggesting the likely outcome <strong>of</strong> the<br />
ARCP to a trainee (this is the responsibility <strong>of</strong> the Educational Supervisor), it<br />
is worth being aware <strong>of</strong> the possible outcomes <strong>and</strong> what the trainee needs to<br />
achieve (See Appendix A <strong>for</strong> detail on <strong>for</strong>ms <strong>and</strong> ARCP outcomes).<br />
The e-portfolio<br />
All foundation trainees use an electronic portfolio, <strong>and</strong> increasingly, trainees in<br />
all specialties are being registered through the Royal Colleges. Each specialty<br />
has a slightly different set <strong>of</strong> sections to be completed by trainees <strong>and</strong> their<br />
assessors, which is outside the scope <strong>of</strong> this h<strong>and</strong>book. However, your local<br />
College / Specialty Tutor should have a good underst<strong>and</strong>ing <strong>of</strong> your eportfolio<br />
system, or there may be a member <strong>of</strong> your School Board who has been charged<br />
with ensuring consultants know how to navigate the system. Your specialty<br />
Head <strong>of</strong> School may organise <strong>for</strong>mal training on eportfolio from time to time.<br />
8<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 8 09/04/2013 14:01
Work place based assessments (WPBAs)<br />
All trainees are required to demonstrate their acquisition <strong>of</strong> relevant clinical<br />
skills <strong>and</strong> behaviours in a structured manner, as described in the relevant<br />
specialty curriculum. A clinical supervisor is expected to facilitate this process by<br />
aiding learning using WPBA tools <strong>for</strong>matively, to give constructive feedback on<br />
per<strong>for</strong>mance <strong>and</strong> advice on how to improve further, <strong>and</strong> summatively, when a<br />
trainee is observed carrying out the procedure or consultation independently.<br />
There are three steps in the assessment process:<br />
• Evidence by observation <strong>of</strong> trainee, e.g. ‘I see evidence <strong>of</strong> your findings’<br />
• Relevance by explanation, e.g. ‘if you don’t record your findings, noone<br />
else will know what you did’<br />
• Competence by evaluation, e.g. ‘these notes do not contain enough<br />
in<strong>for</strong>mation’<br />
And finally, giving feedback to trainee.<br />
What sorts <strong>of</strong> work place based assessments are there <strong>and</strong> how can<br />
they be fitted into my job plan?<br />
Fundamentally, there are three types <strong>of</strong> activity that trainees undertake where<br />
a more senior clinician should observe practice, <strong>and</strong> feedback to the trainee,<br />
using <strong>for</strong>ms delivered by the Foundation Programme or relevant medical Royal<br />
College. The <strong>for</strong>ms can be found in the relevant specialty eportfolio <strong>and</strong> / or<br />
college website.<br />
These are:<br />
• One where the trainee carries out a practical procedure, such as a<br />
cannulation, insertion <strong>of</strong> a chest drain or a hysterectomy (DOPs, OSATS<br />
or other acronyms, dependent upon specialty).<br />
• Mini clinical examinations, where the trainee is observed <strong>for</strong> part <strong>of</strong> a<br />
consultation with a patient. The focus <strong>for</strong> assessment may be one <strong>of</strong>:<br />
the presentation <strong>of</strong> the patient’s history, the taking <strong>of</strong> a history, the<br />
examination, proposed management <strong>and</strong> explanation <strong>of</strong> investigations.<br />
• Case-based discussions, where the trainee may discuss a real case, or a<br />
condition which is rare, but <strong>of</strong> which the specialty curriculum dem<strong>and</strong>s<br />
evidence <strong>of</strong> at least some supervised discussion (such as a pregnant<br />
woman with cystic fibrosis).<br />
The first two activities can usually be easily accommodated ‘on the job’ in<br />
theatres, on ward rounds, <strong>and</strong> occasionally in clinic consultations. Casebased<br />
discussions will need some time setting aside, but it is possible to pool resources<br />
<strong>and</strong> invite other trainees <strong>and</strong> run an interactive <strong>and</strong> discursive tutorial session.<br />
These could time tabled <strong>for</strong> a number <strong>of</strong> afternoons a year within the teaching<br />
timetable, with one or two supervisors leading each session.<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 9<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 9 09/04/2013 14:01
A suggested flow chart <strong>for</strong> clinical supervisors supporting all all<br />
trainees is shown below:<br />
At the start <strong>of</strong> the post<br />
• Invite trainee to have a conversation about their clinical training to date.<br />
The meeting should take place within the first two weeks <strong>of</strong> the trainee<br />
taking up the post. Invite them to show you their log <strong>of</strong> work place based<br />
assessments.<br />
• Ideally undertake WPBAs electronically uploading to the trainee’s<br />
eportfolio in real-time. If this is not possible, keep a copy <strong>of</strong> the paper<br />
documents in a secure filing cabinet just in case the trainee loses their<br />
copy.<br />
• Identify clinical skills training goals.<br />
• Ensure that the trainee knows what material should be collated <strong>for</strong> the<br />
period <strong>of</strong> training you are supervising.<br />
• Invite the trainee to make regular, in<strong>for</strong>mal contact with you.<br />
Regularly<br />
• Share good <strong>and</strong> positive feedback from colleagues, as well as any issues <strong>of</strong><br />
concern.<br />
• If there are specific issues or targets to be addressed, write to educational<br />
supervisor <strong>and</strong> other colleagues as necessary. Copy the trainee in to this<br />
letter. This applies to good trainees just as much as those with emerging<br />
issues.<br />
Pre ARCP assessment (month 10)<br />
• Advise trainee to collate all evidence six to eight weeks be<strong>for</strong>e ARCP<br />
scheduled.<br />
• Ensure that you have provided written evidence <strong>of</strong> any outst<strong>and</strong>ing<br />
practice, or concerns, to the ES. This might include written material from<br />
patients, complaints, cases reviewed through clinical governance (good or<br />
bad care / outcomes).<br />
• Ideally, trainee will have all necessary material <strong>for</strong> summative assessment<br />
to be made (sufficient WPBA, mini Cex, CbDs, TO1s) <strong>and</strong> ‘annual<br />
assessment review’ to be written by educational supervisor. Trainee<br />
should submit papers or eportfolio <strong>of</strong> evidence to programme manager at<br />
least two weeks be<strong>for</strong>e ARCP.<br />
It is best practice to<br />
It is (i) best practice Keep copies to <strong>of</strong> invitations sent to trainee by using<br />
(i) Keep copies ‘read receipts’ <strong>of</strong> invitations email sent to trainee by using ‘read<br />
(ii) receipts’ Sign on all email entries made by yourself into any trainee’s<br />
eportfolio<br />
(ii) Sign all entries made by yourself into any trainee’s eportfolio<br />
10<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
10 First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 10 09/04/2013 14:01
Chapter 3<br />
Feedback on per<strong>for</strong>mance<br />
What is effective feedback?<br />
‘In<strong>for</strong>mation about a per<strong>for</strong>mance or behaviour which leads to action to affirm,<br />
or develop, that per<strong>for</strong>mance or behaviour’.<br />
Ideally, feedback should be given close in time to the event, <strong>and</strong> should be in a<br />
private setting (particularly if behaviour modification is mooted). It should also<br />
be clear; avoid s<strong>and</strong>wiching the bit which needs improvement between two<br />
nuggets <strong>of</strong> praise as the trainee will miss hearing the awful bit.<br />
Feedback should increase the trainee’s insight <strong>and</strong> motivate them to either<br />
continue (or modify if necessary) their practice or behaviours. It is helpful to<br />
have a benchmark the level expected <strong>of</strong> the trainee. However, if the goal is<br />
perceived to be unrealistic, trainee motivation will drop <strong>of</strong>f. Thus, feedback<br />
needs to be <strong>of</strong>fered using the Norcini <strong>and</strong> Burch (2007) headings:<br />
S specific<br />
N non-judgemental<br />
B balanced<br />
P promotes reflection<br />
T timely<br />
For example, you have just observed a consultation between a patient with<br />
recurrent episodes <strong>of</strong> cramping abdominal pain <strong>and</strong> a trainee, where the<br />
patient mentioned a fear that the pain may be a symptom <strong>of</strong> cancer, <strong>and</strong><br />
alluded to a relative having been diagnosed with colon cancer a few years<br />
earlier. The trainee did not pick up on this thread <strong>of</strong> concern, simply suggesting<br />
that a colonoscopy would be a useful investigation. As a clinical supervisor,<br />
you might open the feedback conversation with, ‘What do you think was the<br />
patient’s greatest concern today?’<br />
If you are checking a set <strong>of</strong> notes where the trainee has failed to record<br />
important negative findings during an examination, <strong>for</strong> example there being<br />
no weakness in the limbs <strong>of</strong> an elderly patient admitted following a collapse<br />
at home, the feedback should not be ’these notes are useless’, but something<br />
along the lines <strong>of</strong> ‘it is really valuable to state that she did not have any<br />
weakness on admission, so that the team on duty overnight will be aware <strong>of</strong> a<br />
deterioration if this develops’.<br />
It can also be tricky to give feedback to a trainee who is doing well, but finding<br />
something to gently challenge them is educational in a way that the report ’well<br />
you obviously can do that OK’ is not. In these circumstances, open questions<br />
such as ‘is there anything you would do differently next time?’ or ‘have you<br />
considered…’ , or ‘what would you like to do to make this even better?’ might<br />
open a conversation up.<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 11<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 11 09/04/2013 14:01
Other phrases, which could be helpful in a debriefing episode,<br />
Other phrases, which could be helpful in episode,<br />
might include:<br />
might include:<br />
What was going well?<br />
What was ELSE going was well? going well?<br />
Was What there ELSE was anything going you well? found difficult/ what were the difficulties?<br />
Are Was there anything skills you you found think difficult/ need more what development?<br />
were the difficulties?<br />
What Are there were any you skills thinking you think whilst need this more was development?<br />
all going on? (Might be useful after<br />
dealing What were with you an thinking emergency whilst situation) this was all going on? (Might be useful after<br />
What dealing were with you an emergency feeling? situation)<br />
What were would you be feeling? the best role <strong>for</strong> you in that situation?<br />
What would be you the do best next role time? <strong>for</strong> you in that situation?<br />
What would else needs you do to next happen? time?<br />
What else needs to happen?<br />
The Johari Window (Joe Luft <strong>and</strong> Harry Ingram, 1955)<br />
The Johari Window (Joe Luft <strong>and</strong> Harry Ingram, 1955)<br />
This tool was initially developed <strong>for</strong> self help groups, but is commonly<br />
This used tool <strong>for</strong> examining was initially personal developed effectiveness. <strong>for</strong> self The help factors groups, are: but selfdisclosure,<br />
commonly<br />
used openness <strong>for</strong> examining to feedback personal <strong>and</strong> perceptiveness.<br />
effectiveness. The factors are: selfdisclosure,<br />
openness to feedback <strong>and</strong> perceptiveness.<br />
And with a shared dialogue the windowpanes change size<br />
And with a shared dialogue the windowpanes change size<br />
It may be worth remembering that even experienced supervisors<br />
can It may find be worth it challenging remembering to give that even positive experienced feedback supervisors to learners. can find<br />
Frequently, it challenging to there give is positive a mismatch feedback between to learners. teachers’ Frequently, <strong>and</strong> there learners’ is a<br />
perceptions mismatch between <strong>of</strong> the teachers’ adequacy <strong>and</strong> learners’ <strong>and</strong> effectiveness perceptions <strong>of</strong> <strong>of</strong> the feedback. adequacy <strong>and</strong><br />
(Ramani<br />
effectiveness<br />
S <strong>and</strong><br />
<strong>of</strong> feedback.<br />
Krakov SK, Twelve tips <strong>for</strong> giving feedback effectively in<br />
the<br />
(Ramani<br />
clinical<br />
S <strong>and</strong><br />
environment.<br />
Krakov SK, Twelve<br />
<strong>Medical</strong><br />
tips<br />
Teacher,<br />
<strong>for</strong> giving<br />
2012;34:<br />
feedback<br />
787-791)<br />
effectively in the<br />
clinical environment. <strong>Medical</strong> Teacher, 2012;34: 787-791)<br />
12 First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013<br />
12<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 12 09/04/2013 14:01
Effective or or ineffective feedback?<br />
Effective<br />
Ineffective<br />
Good<br />
per<strong>for</strong>mance<br />
Celebratory<br />
Baffled or puzzled<br />
Per<strong>for</strong>mance<br />
improvement<br />
needed<br />
A h<strong>and</strong> up<br />
Dejected<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 13<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013 13<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 13 09/04/2013 14:01
Chapter 4<br />
The International <strong>Medical</strong> Graduate trainee<br />
International medical graduates constitute 32% <strong>of</strong> the medical work<strong>for</strong>ce with<br />
more than one-in-three hospital doctors <strong>and</strong> one-in-five general practitioners<br />
having qualified overseas.<br />
Studies have shown that this group <strong>of</strong> doctors perceive discrimination, which<br />
may be subtle, or overt. This can be due to a limited opportunity to train in a<br />
certain part <strong>of</strong> the UK, entering the specialty at a more junior level than they<br />
had worked at be<strong>for</strong>e arriving in the UK, <strong>and</strong> lack <strong>of</strong> familiarity with assessment<br />
<strong>and</strong> career progression in the NHS. (Chen P, Nunez-smith M, Bernheim SM, Berg<br />
D et al, Pr<strong>of</strong>essional experiences <strong>of</strong> International <strong>Medical</strong> Graduates Practising<br />
primary care in the United States, 2010; J Gen Intern Med 25 (9): 947-953 )<br />
In addition, many <strong>of</strong> these doctors have become voluntarily separated from<br />
family <strong>and</strong> friends in order to gain UK training experience, <strong>and</strong> may not have a<br />
geographically local network <strong>of</strong> contacts from their country <strong>of</strong> origin.<br />
Induction programme<br />
IMGs should attend the Trust run Induction Programme, normally on the first<br />
day or two days at the start <strong>of</strong> the new appointments (in the first week <strong>of</strong><br />
August or February). Attendance at this is compulsory, as it will provide all the<br />
vital local in<strong>for</strong>mation about working in any particular Trust.<br />
Support<br />
The BMA have published a very useful document entitled: “Working <strong>and</strong><br />
Training in the United Kingdom National Health Service - a guide <strong>for</strong><br />
International <strong>Medical</strong> Graduates (IMGs)”, available through its website.<br />
The PGMDE Associate Dean <strong>for</strong> Overseas Doctors (IMGs), Dr Amit Gupta, has<br />
responsibility <strong>for</strong> matters specific to doctors who have qualified outside the UK,<br />
whether in the EEA countries or elsewhere, or whose nationality does not allow<br />
automatic right <strong>of</strong> permanent residence in the UK. These include:<br />
• Guidance regarding visa status<br />
• Career guidance in relation to overseas status<br />
• Advice in connection with training <strong>and</strong> non-training posts<br />
• Assistance with the <strong>Medical</strong> Training Initiative Scheme<br />
• Provision <strong>of</strong> induction <strong>for</strong> IMGs<br />
• Advice to doctors enquiring from overseas about postgraduate training<br />
• Support <strong>for</strong> refugee <strong>and</strong> asylum-seeking doctors in the Ox<strong>for</strong>d area<br />
14<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 14 09/04/2013 14:01
Both IMGs <strong>and</strong> their supervisors can contact Dr. Amit Gupta, the Associate<br />
Dean <strong>for</strong> IMGs through the PGMDE <strong>for</strong> specific advice at<br />
amit.gupta@thamesvalley.hee.nhs.uk<br />
The CDU can also help with mentoring <strong>and</strong> confidential coaching <strong>for</strong><br />
doctors who <strong>for</strong> whatever reason finds they are in personal or career<br />
difficulty. The CDU can be contacted on cdu@thamesvalley.hee.nhs.uk.<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 15<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 15 09/04/2013 14:01
Chapter 5<br />
‘Something isn’t right’<br />
Chapter 5<br />
‘Something isn’t right’<br />
Concerns over per<strong>for</strong>mance during training<br />
Concerns over per<strong>for</strong>mance during training<br />
Concerns about a doctor’s per<strong>for</strong>mance during training arise more<br />
Concerns<br />
commonly<br />
about<br />
than<br />
a doctor’s<br />
one might<br />
per<strong>for</strong>mance<br />
expect, <strong>and</strong><br />
during<br />
educators<br />
training<br />
are<br />
arise<br />
<strong>of</strong>ten<br />
more<br />
not<br />
commonly<br />
sure what<br />
than<br />
to do.<br />
one<br />
Some<br />
might<br />
doctors<br />
expect,<br />
will<br />
<strong>and</strong><br />
have<br />
educators<br />
periods<br />
are<br />
where<br />
<strong>of</strong>ten not<br />
their<br />
sure<br />
per<strong>for</strong>mance<br />
what to do.<br />
‘slips’<br />
Some<br />
from<br />
doctors<br />
a previous<br />
will have<br />
high<br />
periods<br />
st<strong>and</strong>ard,<br />
where<br />
<strong>and</strong><br />
their<br />
some<br />
per<strong>for</strong>mance<br />
doctors exhibit<br />
‘slips’<br />
challenging<br />
from a previous high<br />
st<strong>and</strong>ard, behaviours <strong>and</strong> from some the doctors beginning exhibit <strong>of</strong> challenging a training behaviours placement. from Factors the beginning both inside<br />
<strong>of</strong> <strong>and</strong> a training outside placement. work may Factors be at play. both inside <strong>and</strong> outside work may be at play.<br />
These factors can include:<br />
These factors can include:<br />
Situations<br />
The ‘8 Bs’ mnemonic<br />
Relationships<br />
These could be new ones, or<br />
failing ones, could include<br />
weddings, or pr<strong>of</strong>essional<br />
‘Birds <strong>and</strong> blokes’<br />
‘Bosses’<br />
problems (bullying<br />
/harassment)<br />
Family pressures Parental expectation<br />
Fertility issues<br />
‘Babies’<br />
New parenthood<br />
Financial pressures May be doing locum shifts ‘Broke’<br />
Loss or separation Lack <strong>of</strong> a local supportive<br />
network<br />
Lack <strong>of</strong> cultural reference<br />
points<br />
Death <strong>of</strong> a family member<br />
Being ' bi-lingual’<br />
‘Bereavement’<br />
or other close friend<br />
Exam pressures May impede training<br />
‘Books’<br />
progress<br />
Substance dependency Prescription drugs,<br />
especially analgesics, non<br />
prescription drugs <strong>and</strong><br />
alcohol<br />
‘Booze’<br />
The The symptoms may may manifest manifest as: as:<br />
• Absenteeism:<br />
Absenteeism:<br />
o o Arriving Arriving late late<br />
o o Leaving Leaving early early<br />
o o Not Not answering bleep bleep<br />
• Presenteeism<br />
o o Arriving Arriving very very early early<br />
o<br />
o<br />
Staying<br />
Staying<br />
behind<br />
behind<br />
to finish<br />
to finish<br />
work<br />
work<br />
regularly<br />
regularly<br />
o Volunteering <strong>for</strong> every task <strong>and</strong> project but not completing them<br />
o Volunteering <strong>for</strong> every task <strong>and</strong> project but not completing<br />
them<br />
16<br />
16 First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 16 09/04/2013 14:02
• Lack <strong>of</strong> rapport with peers<br />
• Lack o<strong>of</strong> rapport Nurseswith peers<br />
o oNurses<br />
Colleagues at same level<br />
o oColleagues Junior or at student same level colleagues<br />
• Higher o Junior incidence or student <strong>of</strong> name colleagues appearing in grumbles, <strong>for</strong>mal complaints<br />
• Higher or case incidence reviews <strong>of</strong> than name peers appearing in grumbles, <strong>for</strong>mal complaints or<br />
• case Poor reviews attention than to peers paperwork<br />
• Poor<br />
o<br />
attention<br />
Reviewing<br />
to paperwork<br />
patient’s results <strong>and</strong> following them up<br />
o Reviewing patient’s results <strong>and</strong> following them up<br />
o Uneven accrual <strong>of</strong> WPBAs<br />
o Uneven accrual <strong>of</strong> WPBAs<br />
o Failure to register with NHS e-portfolio<br />
o Failure to register with NHS e-portfolio<br />
Behaviours<br />
Behaviours<br />
It is helpful to characterise behaviours using the seven domains <strong>of</strong> Good<br />
<strong>Medical</strong> It is helpful Practice: to characterise behaviours using the seven domains <strong>of</strong> Good<br />
<strong>Medical</strong> Practice:<br />
• Good clinical care,<br />
• Maintaining • Good good clinical medical care, practice,<br />
• Relationship • Maintaining with patients, good medical practice,<br />
• Working<br />
• Relationship<br />
with colleagues,<br />
with patients,<br />
• Working with colleagues,<br />
• Teaching <strong>and</strong> training,<br />
• Teaching <strong>and</strong> training,<br />
• Probity, <strong>and</strong><br />
• Probity, <strong>and</strong><br />
• Health.<br />
• Health.<br />
A detailed appendix describing incompetence, competence <strong>and</strong><br />
detailed appendix describing incompetence, competence <strong>and</strong> per<strong>for</strong>mance<br />
per<strong>for</strong>mance descriptors (appendix C) is included at the end <strong>of</strong> this<br />
descriptors (appendix C) is included at the end <strong>of</strong> this h<strong>and</strong>book, <strong>and</strong> should be<br />
h<strong>and</strong>book, <strong>and</strong> should be referred to regularly.<br />
referred to regularly.<br />
Personality as a factor<br />
Personality as factor<br />
Human beings do do not not all all per<strong>for</strong>m in in the the same same way, way, nor do nor we do perceive we perceive things<br />
things similarly. similarly. At times At <strong>of</strong> times stress, previous <strong>of</strong> stress, strengths previous may strengths become may overexaggerated<br />
become overexaggerated<br />
<strong>and</strong> metamorphose <strong>and</strong> metamorphose into weaknesses, into or ‘difficult’ weaknesses, behaviours. or ‘difficult’ behaviours.<br />
Enthusiastic<br />
Shrewd<br />
Careful<br />
Independent<br />
Confident<br />
Focused<br />
Charming<br />
Vivacious<br />
Imaginative<br />
Diligent<br />
Dutiful<br />
Volatile<br />
Mistrustful<br />
Cautious<br />
Detached<br />
Arrogant<br />
Passive-aggressive<br />
Manipulative<br />
Dramatic<br />
Eccentric<br />
Perfectionist<br />
Dependent<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013 17<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 17<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 17 09/04/2013 14:02
The Ox<strong>for</strong>d PGMDE policy <strong>for</strong> supporting trainees about whom there are<br />
concerns over per<strong>for</strong>mance during training can be seen on the deanery’s<br />
website.<br />
Although the term “Trainee in Difficulty” has been used commonly as<br />
shorth<strong>and</strong>, the deanery recognises that such labelling <strong>of</strong> individual trainees<br />
is <strong>of</strong>ten unhelpful. The Gold <strong>Guide</strong> refers to “managing concerns over<br />
per<strong>for</strong>mance during training” (see paragraphs 8.19-8.35, Gold <strong>Guide</strong> Fourth<br />
Edition, 2010), <strong>and</strong> the deanery’s policy has been revised to set out how trainees<br />
should be supported where there are such concerns.<br />
NACT (UK) (the National Association <strong>of</strong> Clinical Tutors) has published a useful<br />
guide, updated in July 2012, ‘Managing Trainees in Difficulty: Practical Advice<br />
<strong>for</strong> Educational <strong>and</strong> Clinical <strong>Supervisors</strong>’, which outlines the relationships<br />
between employers, Deaneries <strong>and</strong> the GMC in such circumstances. It can be<br />
downloaded from the NACT website at<br />
http://www.nact.org.uk/documents.<br />
Training workshops are hosted by the deanery <strong>and</strong> are delivered in each Trust<br />
on an annual basis. Please see the website <strong>for</strong> details <strong>of</strong> dates <strong>and</strong> venues.<br />
Any supervisor can attend a session at other Trusts; subject to local study leave<br />
procedures.<br />
It should be evident that where there are concerns about atrainee’s<br />
per<strong>for</strong>mance in training, or achievement <strong>of</strong>competencies, there should be more<br />
frequent reviews <strong>of</strong> progressthan the ‘minimum’ set out by the medical royal<br />
colleges.<br />
Clinical or educational supervisors may need assistance from College Tutors,<br />
Training Programme Directors or School Board <strong>of</strong>ficers. If in any doubt it is<br />
prudent to seek early confidential advice. The PGMDE Career Development Unit<br />
(CDU) can provide educators with advice about the appropriate steps to take<br />
in managing concerns about trainee per<strong>for</strong>mance, as well as personal coaching<br />
<strong>and</strong> mentoring support <strong>for</strong> individual trainees. Further in<strong>for</strong>mation is available<br />
from the CDU website at www.ox<strong>for</strong>ddeanerycdu.org.uk/index.html.<br />
Issues that are related to patient safety should be discussed with<br />
the Director <strong>of</strong> <strong>Medical</strong> Education <strong>and</strong> / or the <strong>Medical</strong> Director <strong>of</strong><br />
your own Trust.<br />
Equality <strong>and</strong> diversity<br />
It is important <strong>for</strong> clinical supervisors, educational supervisors, College Tutors,<br />
Training Programme Directors <strong>and</strong> School Board <strong>of</strong>ficers to treat all trainees<br />
equally <strong>and</strong> without discrimination. This is <strong>of</strong> particular importance when the<br />
trainee’s problems begin to impact on their per<strong>for</strong>mance, as less than equal<br />
treatment might be alleged through either PGMDE appeals panels or even<br />
Employment Tribunals. The same st<strong>and</strong>ards <strong>of</strong> communication <strong>and</strong> support to all<br />
trainees should be applied from the outset. An electronic file is recommended<br />
<strong>for</strong> every trainee with whom you have any dealings, password protected <strong>of</strong><br />
18<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v3.indd 18 12/04/2013 15:59
course, <strong>and</strong> any paper material should be kept securely under lock <strong>and</strong> key.<br />
The Ox<strong>for</strong>d PGMDE policy can be viewed on the website.<br />
Harassment<br />
Harassment can take various <strong>for</strong>ms <strong>and</strong> may be directed against males or<br />
females, ethnic minorities or subgroups, towards people because <strong>of</strong> their age,<br />
sexual orientation, physical or mental disability, or some other characteristic.<br />
It may involve action, behaviour, comment or physical contact which is found<br />
to be objectionable by the recipient or which causes <strong>of</strong>fence <strong>and</strong> can result in<br />
the recipient feeling threatened, humiliated, patronised or isolated. It can also<br />
create an intimidating work environment. Individual perceptions about certain<br />
types <strong>of</strong> behaviour will vary, so what is acceptable <strong>for</strong> one person, may be<br />
inappropriate or unacceptable behaviour to another.<br />
Harassment may be persistent or occur on a single occasion. It may be<br />
intentional or unintentional on the part <strong>of</strong> the perpetrator, but it is the impact<br />
<strong>of</strong> the behaviour on the recipient, <strong>and</strong> the deed itself, which constitutes<br />
harassment.<br />
As be<strong>for</strong>e, this policy can be viewed on the deanery’s website.<br />
Concerns about health<br />
If there are any concerns about an individual’s health affecting training, the<br />
doctor should be encouraged to see their own GP. If there is a possibility that a<br />
doctor’s health may be affecting their work, then the employer may ask <strong>for</strong> an<br />
occupational health assessment. Further in<strong>for</strong>mation <strong>and</strong> guidance is available<br />
from the CDU website <strong>and</strong> from NCAS at http://www.ncas.nhs.uk/resources/<br />
h<strong>and</strong>ling-healthconcerns/<br />
Dyslexia in relation to Postgraduate <strong>Medical</strong> <strong>and</strong> <strong>Dental</strong> Education<br />
<strong>and</strong> Training<br />
Dyslexia is one <strong>of</strong> a group <strong>of</strong> conditions called Specific Learning Difficulties<br />
in Adults, which also includes Dyspraxia or Development Co-ordination<br />
Disorder, Dyscalculia, <strong>and</strong> Attention Deficit Disorder. Further in<strong>for</strong>mation<br />
about these is available on the British Dyslexia Association website – see<br />
http://www.bdadyslexia.org.uk/about-dyslexia. Hereafter in these notes<br />
the term “dyslexia” will be used to refer to all the Specific Learning<br />
Difficulties in Adults.<br />
Specific in<strong>for</strong>mation about dealing with dyslexia in postgraduate medical <strong>and</strong><br />
dental education <strong>and</strong> training is hard to find. There is useful in<strong>for</strong>mation on the<br />
BMA website produced by the BMA <strong>Medical</strong> Students Committee – see http://<br />
bma.org.uk/developing-your-career/studyingmedicine/common-challengeswhile-studying/studying-with-dyslexia<br />
but this does not refer to what happens after qualification.<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 19<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 19 09/04/2013 15:03
The GMC website includes references to dyslexia under its Gateways<br />
guidance – see http://www.gmcuk.org/education/undergraduate/gateways_<br />
guidance.asp <strong>for</strong> general in<strong>for</strong>mation about this guidance. In summary:<br />
• GMC Gateways guidance<br />
• This advisory guidance is aimed primarily at medical schools. It will also<br />
interest organisations involved in postgraduate medical training <strong>and</strong><br />
many individuals, including disabled doctors, students <strong>and</strong> potential<br />
students.<br />
• It provides practical suggestions to help schools ensure that disabled<br />
students do not face unnecessary barriers to successful medical careers.<br />
• The advisory guidance originally resulted from a partnership led by<br />
the GMC <strong>and</strong> financially supported by 11 medical schools. Matched<br />
funding was provided through Gateways to the Pr<strong>of</strong>essions, set up by<br />
the Department <strong>for</strong> Education <strong>and</strong> Skills (Engl<strong>and</strong>), as it then was. The<br />
guidance has been revised to take account <strong>of</strong> developments including<br />
the 2009 edition <strong>of</strong> Tomorrow’s Doctors <strong>and</strong> the Equality Act 2010.<br />
• The guidance does not lay down new requirements, quality assurance<br />
st<strong>and</strong>ards or ‘policies’ from the GMC or any <strong>of</strong> the other organisations<br />
involved.<br />
• Section 4.2 <strong>of</strong> the guidance covers the legal definition <strong>of</strong> ‘a disabled<br />
person’ (copied from GMC guidance – the emphasis is added):<br />
The Equality Act 2010 defines a disabled person as:<br />
‘A person (P) has a disability if P has a physical or mental impairment which has<br />
a:<br />
• Long-term <strong>and</strong><br />
• Substantial adverse effect on P’s ability to carry out normal day-today<br />
activities.’<br />
As this is a legal definition, it is ultimately <strong>for</strong> a court or tribunal to determine<br />
to whom it applies. Where there is doubt about whether an individual will be<br />
covered, it is best practice to assume that they will be <strong>and</strong> focus on identifying<br />
reasonable adjustments that will assist them.<br />
The effect <strong>of</strong> an impairment is long-term if:<br />
• It has lasted <strong>for</strong> at least 12 months<br />
• It is likely to last <strong>for</strong> at least 12 months or<br />
• It is likely to last <strong>for</strong> the rest <strong>of</strong> the life <strong>of</strong> the person affected.<br />
• A ‘substantial’ adverse effect is defined in the Act as one that is<br />
‘more than minor or trivial’.<br />
20<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 20 09/04/2013 14:02
• <strong>Medical</strong> schools, postgraduate deaneries <strong>and</strong> employers should<br />
use this definition when considering how to assess <strong>and</strong> support<br />
disabled applicants, students <strong>and</strong> employees. They should also<br />
encourage a greater underst<strong>and</strong>ing <strong>of</strong> who is protected by the<br />
Act, <strong>and</strong> seek to protect the rights <strong>of</strong> disabled people in their use<br />
<strong>of</strong> all the services at university <strong>and</strong> medical school.<br />
• People with a range <strong>of</strong> impairments <strong>and</strong> long-term health<br />
conditions are included in this definition, such as people who are<br />
hard <strong>of</strong> hearing or have mental health issues, multiple sclerosis,<br />
cancer or HIV. Importantly, others who would not usually describe<br />
themselves as disabled people, such as those with dyslexia, may<br />
be protected by the Act if the effects <strong>of</strong> the impairment are ‘long<br />
term’ ‘adverse’ <strong>and</strong> ‘substantial’ on normal day-today activities.<br />
People with hidden disabilities such as epilepsy are also covered.<br />
• It is not clear from the above to what extent The Equality Act 2010<br />
places any obligation on postgraduate deaneries in relation to doctors<br />
<strong>and</strong> dentists in training that have diagnosed or suspected dyslexia.<br />
There are certainly obligations under the Act <strong>for</strong> the employers <strong>of</strong><br />
doctors <strong>and</strong> dentists in training.<br />
• There is most useful <strong>and</strong> comprehensive guidance <strong>for</strong> employers on the<br />
British Dyslexia Association website (see<br />
http://www.bdadyslexia.org.uk/about-dyslexia/adults-<strong>and</strong>business.<br />
html). For example, there is:<br />
• An Adult Dyslexia Checklist which can be used as a screening tool<br />
<strong>for</strong> adult dyslexia – see<br />
http://www.bdadyslexia.org.uk/files/Adult%20Checklist.pdf This<br />
test is said to be 90% accurate in predicting dyslexia.<br />
Some relevant text copied from the BDA guidance follows:<br />
o There is no legal requirement to disclose a disability. However<br />
once the employer has been in<strong>for</strong>med <strong>of</strong> an employee’s dyslexia<br />
or been given a copy <strong>of</strong> an assessment report, they are on notice<br />
that they have a duty under the Equality Act.<br />
o Disciplinary proceedings around per<strong>for</strong>mance issues are frequently<br />
dyslexia related. Many are <strong>of</strong>f sick with stress as a result. In many<br />
circumstances they could seek redress under the Equality Act in an<br />
Employment Tribunal.<br />
o Assessment. Where an employee has not been previously assessed<br />
<strong>for</strong> dyslexic difficulties (post 16 years), the first step would be<br />
<strong>for</strong> the employer to arrange <strong>for</strong> the employee to have a full<br />
diagnostic assessment:<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 21<br />
49087 Ox PGMDE H<strong>and</strong>book v3.indd 21 12/04/2013 16:00
• This should by carried out by a Chartered Psychologist<br />
specialising in adult dyslexia. The cost could be around £500 or<br />
more.<br />
• However in the case <strong>of</strong> a job not involving significant<br />
paperwork, a screening test such as the one linked to our<br />
website may be sufficient. This test is 90% accurate in predicting<br />
dyslexia.<br />
• Most large employers <strong>and</strong> those in the public sector would be<br />
expected to fund a dyslexia assessment <strong>for</strong> an employee as part<br />
<strong>of</strong> their duty under the Equality Act. A small employer may help<br />
with the cost. For recommendations <strong>of</strong> appropriate psychologists<br />
<strong>for</strong> a diagnostic assessment, contact your nearest Local Dyslexia<br />
Association.<br />
Workplace Need Assessment <strong>for</strong> doctors with dyslexia<br />
Following the diagnostic assessment, (or where an employee is able to show<br />
an existing adult assessment report), a workplace needs assessment should<br />
be arranged with a dyslexia specialist. This will detail the most appropriate<br />
accommodations <strong>and</strong> support, (reasonable adjustments) which would be<br />
successful in mitigating any weak areas <strong>and</strong> reduce stress. This is not something<br />
that either the individual or the employer would be able to work out <strong>for</strong> himself<br />
or herself.<br />
Workplace needs assessments can normally be obtained from Access to<br />
Work, part <strong>of</strong> the Jobcentre organisation.<br />
• The application to Access to Work should be made by the employee.<br />
For in<strong>for</strong>mation on this process see Dyslexia Support in the Workplace.<br />
• Independent dyslexia workplace consultants can also be appointed to<br />
do an assessment. Their report can still be submitted to Access to Work<br />
<strong>for</strong> the grant to the individual <strong>for</strong> items <strong>and</strong> training recommended.<br />
Implementing Reasonable Adjustments.<br />
Reasonable Adjustments should be put in place as soon as possible.<br />
Failure to implement Reasonable Adjustments would be a breach <strong>of</strong> the<br />
Equality Act. Reasonable Adjustments are not a quick overnight remedy.<br />
Depending on the individual circumstances, it may take 2 or 3 months <strong>for</strong><br />
measures to become embedded <strong>and</strong> <strong>for</strong> any associated training <strong>and</strong><br />
learning to become effective.<br />
22<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 22 09/04/2013 14:02
External sources <strong>of</strong> support <strong>for</strong> trainees<br />
There are a number <strong>of</strong> well-regarded external sources <strong>of</strong> support, <strong>and</strong> it is<br />
strongly recommended that supervisors direct trainees to them <strong>and</strong> do not<br />
try to act as, <strong>for</strong> example, marriage guidance counsellors, or ‘doctors’ to<br />
their trainees.<br />
The agencies which may be suitable include:<br />
Medic Support<br />
The CDU<br />
‘Doctors <strong>for</strong> Doctors’<br />
Funded by the Ox<strong>for</strong>d PGMDE to provide a free <strong>and</strong><br />
confidential counselling service <strong>for</strong> doctors <strong>and</strong> dentists<br />
in training. See<br />
http://www.ox<strong>for</strong>ddeanerycdu.org.uk/health/help_<strong>for</strong>_<br />
trainees/medic_support.html<br />
See the CDU website <strong>for</strong> more in<strong>for</strong>mation<br />
A BMA service <strong>for</strong> medical students <strong>and</strong> qualified<br />
doctors. Contact on 08459 200169<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 23<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 23 09/04/2013 14:02
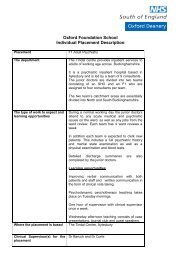
Appendix A: Forms usually collated by the<br />
Educational Supervisor <strong>and</strong> ARCP outcomes<br />
These are described in detail in ‘The Gold <strong>Guide</strong>’. Increasingly these <strong>for</strong>ms<br />
are lodged in the specialty eportfolio. Both trainee <strong>and</strong> Educational<br />
Supervisor normally have access to the same site: other assessors may<br />
be invited by the trainee sending an ‘e ticket’ to login.<br />
The Educational Agreement (EA)<br />
Both the trainee <strong>and</strong> their Educational Supervisor at the start <strong>of</strong> each year<br />
<strong>of</strong> training should sign it. The <strong>for</strong>m looks like this:<br />
The Trainee’s Personal Development Plan (PDP)<br />
This should be written by the trainee at the start <strong>of</strong> the training year, <strong>and</strong><br />
reviewed after each assessment, as a minimum (due at 4, 8 <strong>and</strong> 11+<br />
months)<br />
The Annual Assessment Review Form (AARF)<br />
This document <strong>for</strong>ms the summative assessment <strong>of</strong> a trainee’s progress<br />
during the preceding year <strong>and</strong> is an integral part <strong>of</strong> the evidence required<br />
<strong>for</strong> the ARCP panel review. It will include the domains laid out by the<br />
GMC:<br />
Good clinical care<br />
Developing <strong>and</strong> maintaining good medical practice<br />
24<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
24 First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 24 09/04/2013 14:02
Working with colleagues<br />
Teaching <strong>and</strong> training<br />
Probity<br />
Health<br />
<strong>and</strong> attributes / targets required by the specialty curriculum, including an<br />
overview <strong>of</strong> progress <strong>and</strong> all the work place based assessments.<br />
Confirmation that an audit has been completed, evidence <strong>of</strong> reflective<br />
learning <strong>and</strong>, from 2013, reporting <strong>of</strong> the trainee’s involvement in<br />
complaints or critical incidents are usually required fields on these <strong>for</strong>ms.<br />
An example <strong>of</strong> such a <strong>for</strong>m is shown below (note TO2 is the abbreviation<br />
<strong>for</strong> multisource feedback used by the example specialty)<br />
First First edn. edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> PGMDE Jan Apr 2013 2013 25 25<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 25 09/04/2013 14:02
Action Plans / Improvement Plans<br />
These are <strong>for</strong>mulated to address any concerns about the trainee’s<br />
per<strong>for</strong>mance, should be agreed <strong>and</strong> documented between the educational<br />
supervisor <strong>and</strong> trainee. This is effectively what we call a Pr<strong>of</strong>essional<br />
Improvement Plan (PIP) in the PGMDE ‘Supporting the Trainee Protocol’.<br />
ARCP outcomes<br />
Outcome 1<br />
Outcome 2<br />
Outcome 3<br />
Outcome 4<br />
Outcome 5<br />
Outcome 6<br />
Outcome 7<br />
Outcome 8<br />
The trainee has achieved all the required technical <strong>and</strong><br />
educational targets set <strong>for</strong> the period <strong>of</strong> training under<br />
review<br />
The trainee has almost achieved the targets set, <strong>and</strong><br />
does not need to have the CCT date delayed. This may<br />
be a small shortfall in WPBA numbers. Exam failure may<br />
be such a target, unless the trainee is at a point in<br />
training where continued progress dem<strong>and</strong>s exam<br />
success.<br />
This trainee has not achieved the training targets set <strong>for</strong><br />
the period <strong>of</strong> training <strong>and</strong> will need more time in<br />
programme to achieve these targets.<br />
This trainee is leaving the programme, either with the<br />
required targets having been achieved, or without. Some<br />
trainees choose to leave the specialty because it was the<br />
‘wrong’ choice <strong>for</strong> them, others leave because their<br />
training time has already been prolonged by the<br />
maximum <strong>of</strong> two additional years, but has still not<br />
achieved the educational targets required to progress<br />
further.<br />
This trainee has not submitted the required evidence <strong>of</strong><br />
training to the ARCP panel <strong>and</strong> a decision on their<br />
progress cannot be made. This trainee is expected to<br />
produce the necessary evidence within two weeks <strong>of</strong> the<br />
date <strong>of</strong> the ARCP.<br />
This trainee has completed the entire specialty training<br />
programme <strong>and</strong> can apply <strong>for</strong> the CCT<br />
This prefix is used <strong>for</strong> trainees in LAT or FTSTA posts.<br />
The suffix is .1, .2, .3 as above.<br />
This trainee is currently ‘out <strong>of</strong> programme’. This may be<br />
<strong>for</strong> research, specific clinical experience elsewhere, or as<br />
a career break.<br />
26<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
26 First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v3.indd 26 12/04/2013 16:00
Appendix B: Expectations <strong>of</strong> generation Y<br />
This has been taken from the <strong>Medical</strong> Careers pages <strong>of</strong> the NHS <strong>Medical</strong><br />
Careers website.<br />
People born between 1946 <strong>and</strong> 1964 are <strong>of</strong>ten described as ‘baby<br />
boomers’, those between 1965 <strong>and</strong> 1981 as ‘generation X’ <strong>and</strong> those after<br />
1981 as ‘generation Y’. Whilst these terms are American, the expectations<br />
<strong>and</strong> experiences <strong>of</strong> the groups are transferable to the UK. The<br />
demographic groups have different expectations <strong>and</strong> values when<br />
compared to each other.<br />
There have been several recent studies that have looked into the<br />
differences in attitude between generations <strong>and</strong> how this relates<br />
to the working environment. These studies do not relate strictly to<br />
medicine; however they are relevant as they are valid in any<br />
working environment. This article focuses on the attitudes <strong>of</strong><br />
Generation Y as today the majority <strong>of</strong> medical trainees fall into<br />
this category.<br />
One recent study is the ‘Gen Up’ report, published in September 2008,<br />
which is a joint survey report commissioned by the CIPD <strong>and</strong> Penna. This<br />
study surveyed over 5,500 employees across 6 Western European<br />
countries.<br />
The ‘Gen Up’ report compares attitudes between the above four<br />
generations under the following headings:<br />
• Retention <strong>and</strong> loyalty<br />
According the report ‘Gen X <strong>and</strong> Y may ‘dem<strong>and</strong>’ more flexible hours <strong>and</strong><br />
are less likely to take a long term career view with the organisation’.<br />
However, ‘nearly half <strong>of</strong> Gen Y intend to be with their current employer in<br />
five years time <strong>and</strong> one in four expects to change jobs every two to three<br />
years.... So the commonly held belief that Gen Y is easy to recruit, hard to<br />
retain may not be strictly true.’<br />
• Driving Customer Service<br />
‘Gen Y is more positive about service being recognised than other<br />
generations’, although ‘16% <strong>of</strong> Gen Y are not at all interested in customer<br />
service being part <strong>of</strong> their role.’<br />
• Per<strong>for</strong>mance Management<br />
‘Gen Y is much less tolerant <strong>of</strong> under-per<strong>for</strong>mance. Nearly one in five Gen<br />
Ys believe that the best solution <strong>for</strong> under-per<strong>for</strong>mance is <strong>for</strong> someone to<br />
be fired’.<br />
• Mobile <strong>and</strong> Flexible Working<br />
‘As a generation, Gen Y are the first to truly adopt technology to manage<br />
their life/work balance as the boundaries <strong>of</strong> <strong>of</strong>fice <strong>and</strong> personal life<br />
become blurred.’<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 27<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013 27<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 27 09/04/2013 14:02
• Internal communication<br />
‘Gen Y is actually the most positive generation about communication.<br />
They may be expected to be more dem<strong>and</strong>ing <strong>of</strong> internal communication<br />
given the fact that they are used to ‘in<strong>for</strong>mation at their fingertips’.<br />
• Leadership <strong>and</strong> Management<br />
‘Gen Y may find that older generations demonstrate less trust <strong>for</strong> senior<br />
management. Gen Y are also more likely to rate senior mangers well<br />
including the fact that they make work priorities clear.’ The report also<br />
finds that ‘Gen Y is the most trusting <strong>of</strong> the organisation as they have not<br />
been exposed to significant downsizing or economic uncertainty.’ This<br />
characteristic may now be subject to change, however, with the effects <strong>of</strong><br />
the current recession.<br />
• Career development<br />
‘Gen Y may find some generational conflict in terms <strong>of</strong> career<br />
development’.<br />
’Gen Y may find development conversations with other Gen Y much easier<br />
to manage – conversations are likely to stretch beyond the current<br />
organisation’. The Baby Boomer may be surprised at the ‘self- sufficiency’<br />
<strong>of</strong> Gen Y as they expect to manage their own career development’.<br />
28<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
28 First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 28 09/04/2013 14:02
Appendix C: Good <strong>Medical</strong> Practice: Indicators <strong>for</strong><br />
assessors<br />
1 Good Clinical Care<br />
Incompetent<br />
History Taking<br />
Incomplete, inaccurate <strong>and</strong><br />
confusing history taking from,<br />
<strong>and</strong> communication with,<br />
patients (carers).<br />
Fails to take into account the<br />
patients (carers) concerns,<br />
expectation or underst<strong>and</strong>ing.<br />
May repeatedly upset patients<br />
(carers).<br />
Examination<br />
Regularly fails to elicit physical<br />
signs <strong>of</strong> common clinical<br />
problems. Poor technique<br />
Frequently takes inappropriate<br />
short cuts when examining.<br />
Routinely fails to adequately<br />
explain procedures <strong>for</strong> intimate<br />
examinations.<br />
Cannot get patient co-operation<br />
<strong>for</strong> examination.<br />
Investigations<br />
Regularly fails to order<br />
appropriate basic investigations<br />
Orders inappropriate, r<strong>and</strong>om<br />
unnecessary investigations, no<br />
thought given.<br />
Often fails to per<strong>for</strong>m<br />
investigations requested<br />
Fails to recognise normal <strong>and</strong><br />
abnormal results <strong>of</strong> common<br />
investigations.<br />
Fails to ask <strong>for</strong> help or take<br />
appropriate action thereon.<br />
Competent<br />
History Taking<br />
Clear history taking <strong>and</strong><br />
communication with patients (carers).<br />
Uses open & closed questions<br />
appropriately<br />
Knowledge <strong>of</strong> ‘alarm’ symptoms<br />
Appreciates the importance <strong>of</strong><br />
clinical, psychological <strong>and</strong> social<br />
factors.<br />
Attempts to incorporate the patients<br />
(carers) concerns, expectations <strong>and</strong><br />
underst<strong>and</strong>ing.<br />
Ability to take specialised histories:<br />
mental health, sexual health, from<br />
children / parents.<br />
Examination<br />
Explains the examination procedure<br />
<strong>and</strong> minimises patient discom<strong>for</strong>t.<br />
Uses chaperones appropriately<br />
Can elicit individual clinical signs but<br />
may lack co-ordinated approach <strong>and</strong><br />
sometimes fails to target detailed<br />
examination as suggested from the<br />
patient’s symptoms.<br />
Able to use instruments appropriately.<br />
Investigations<br />
Requests common investigations<br />
appropriately <strong>for</strong> patients’ needs.<br />
Ensures investigations requested by<br />
team are completed.<br />
Discusses risks, possible outcomes<br />
<strong>and</strong> later results with patients (carers)<br />
appropriate to level <strong>of</strong> expertise.<br />
Recognises normal <strong>and</strong> abnormal<br />
results.<br />
Prioritises importance <strong>of</strong> results <strong>and</strong><br />
asks <strong>for</strong> help appropriately.<br />
Underst<strong>and</strong>s local systems <strong>and</strong> asks<br />
<strong>for</strong> help appropriately from the<br />
relevant individuals.<br />
Per<strong>for</strong>mance<br />
History Taking<br />
Accomplished, concise <strong>and</strong><br />
focused (targeted) history<br />
taking <strong>and</strong> communication,<br />
including difficult<br />
circumstances (when<br />
English not the patients first<br />
language; confused patients<br />
or other psychiatric /<br />
psychological problem or<br />
special educational needs;<br />
deaf patients; child abuse /<br />
neglect.<br />
Examination<br />
Elicits signs appropriately<br />
<strong>and</strong> with attention to patient<br />
dignity. Skilled<br />
examination technique<br />
Teaches examination<br />
techniques.<br />
Able to examine children <strong>of</strong><br />
all ages<br />
Investigations<br />
Arranges, completes & acts<br />
on investigations<br />
intelligently, economically<br />
& diligently.<br />
Teaches F1 trainees about<br />
requests <strong>for</strong>, interpretation<br />
<strong>of</strong> <strong>and</strong> action on normal <strong>and</strong><br />
abnormal results, <strong>for</strong><br />
common investigations.<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 29<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013 29<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 29 09/04/2013 14:02
1 Good Clinical Care (2)<br />
Incompetent<br />
Making a diagnosis /<br />
management plan<br />
Decisions frequently<br />
questionable.<br />
Unable to make decisions or<br />
even make a working diagnosis<br />
Seeks help all the time.<br />
Fails to involve patients in<br />
decision making.<br />
Therapeutics<br />
Prescribing regularly shows lack<br />
<strong>of</strong> clarity.<br />
Repeatedly fails to take account<br />
<strong>of</strong> drug history.<br />
Frequently fails to prescribe<br />
according to st<strong>and</strong>ard BNF<br />
recommendations, including<br />
potentially harmful interactions.<br />
Record Keeping<br />
Keeps inaccurate or illegible<br />
notes with key in<strong>for</strong>mation<br />
missing.<br />
Fails to sign entries.<br />
Clinical Risk Management<br />
Lacks knowledge or<br />
underst<strong>and</strong>ing <strong>of</strong> common<br />
complications/side effects <strong>of</strong><br />
treatments / procedures.<br />
Fails to identify signs that might<br />
indicate acute illness.<br />
Does not seek help<br />
appropriately.<br />
Consistently fails to h<strong>and</strong> over.<br />
Competent<br />
Making a diagnosis /<br />
management plan<br />
Decisions generally<br />
satisfactory, though occasional<br />
inadequacies when under work<br />
pressure.<br />
Can make a sound diagnosis &<br />
produce safe, appropriate<br />
management plans.<br />
Involves patients (& other<br />
pr<strong>of</strong>essionals where<br />
appropriate – aware <strong>of</strong> own<br />
skill & competency)<br />
Therapeutics<br />
Takes an accurate drug<br />
history.<br />
Uses the BNF <strong>and</strong> other<br />
sources to access in<strong>for</strong>mation.<br />
Prescribes drugs (including<br />
oxygen, fluids <strong>and</strong> blood<br />
products) clearly <strong>and</strong><br />
unambiguously. Underst<strong>and</strong>s<br />
the implications <strong>of</strong> religious<br />
beliefs.<br />
Describes common drug<br />
interactions <strong>and</strong> allergic<br />
reactions.<br />
Record Keeping<br />
Routinely records accurate,<br />
logical legible history which is<br />
timed, dated <strong>and</strong> clearly<br />
attributable. Medico – legally<br />
sound.<br />
Routinely records patients’<br />
progress including<br />
management plans <strong>and</strong><br />
discussion with relatives <strong>and</strong><br />
other health care pr<strong>of</strong>essionals.<br />
Utilises in<strong>for</strong>mation systems<br />
effectively. Adapts style to<br />
multidisciplinary case record<br />
where appropriate.<br />
Clinical Risk Management<br />
Describes common<br />
complications <strong>and</strong> side effects<br />
<strong>of</strong> treatments/procedures.<br />
Identifies <strong>and</strong> responds<br />
appropriately to patients with<br />
abnormal signs.<br />
Recognises personal<br />
limitations <strong>and</strong> seeks help at<br />
an early stage.<br />
Communicates effectively to<br />
ensure continuity <strong>of</strong> care.<br />
Per<strong>for</strong>mance<br />
Making a diagnosis /<br />
management plan<br />
Decision making satisfactory even<br />
when under pressure.<br />
Shows intelligent interpretation <strong>of</strong><br />
available data to <strong>for</strong>m an effective<br />
hypothesis, underst<strong>and</strong>s the<br />
importance <strong>of</strong> probability in<br />
diagnosis.<br />
Teaches F1 trainees on taking drug<br />
history, obtaining prescribing<br />
in<strong>for</strong>mation <strong>and</strong> unambiguous<br />
prescribing.<br />
Describes the implications <strong>of</strong><br />
pregnancy <strong>for</strong> safe use <strong>of</strong><br />
commonly used drugs.<br />
Therapeutics<br />
Teaches on common drug<br />
interactions <strong>and</strong> management <strong>of</strong><br />
allergic reactions.<br />
Ability to manage adverse drug<br />
reactions<br />
Record Keeping<br />
Teaches record keeping <strong>and</strong><br />
intra/internet access skills to F1<br />
trainees.<br />
Timely sending out <strong>of</strong> letters,<br />
discharge summaries.<br />
Structures letters to communicate<br />
findings <strong>and</strong> outcome <strong>of</strong> episodes<br />
clearly.<br />
Clinical Risk Management<br />
Appropriately discusses potential<br />
advantages <strong>and</strong> disadvantages <strong>of</strong><br />
treatments/procedures with patients<br />
(carers).<br />
Teaches F1 trainees the appropriate<br />
response to patients with abnormal<br />
signs.<br />
Sets example by calling <strong>for</strong> help<br />
from appropriate health care<br />
pr<strong>of</strong>essionals in timely fashion.<br />
Demonstrates good h<strong>and</strong>over to<br />
ensure continuity <strong>of</strong> care.<br />
Involvement in critical incident<br />
analysis.<br />
30<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
30 First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 30 09/04/2013 14:02
Management <strong>of</strong> Acutely Ill patients (1)<br />
(i) Promptly assesses airway, breathing, circulation in the collapsed patient<br />
Incompetent<br />
Fails to respond promptly to<br />
calls <strong>for</strong> help<br />
Slow, incomplete or<br />
unstructured initial<br />
assessment<br />
Competent<br />
Completes initial assessment within 2-<br />
3 minutes<br />
Supports <strong>and</strong> clears airway<br />
Observes respiratory pattern <strong>and</strong> rate,<br />
identifies inadequate ventilation<br />
Assesses pulse rate, rhythm, volume<br />
Measures blood pressure using<br />
automated methods or<br />
sphygmomanometer<br />
Per<strong>for</strong>mance<br />
As preceding, plus…<br />
Makes a clinical assessment <strong>of</strong><br />
adequacy <strong>of</strong> cardiac output &<br />
oxygen delivery<br />
Capable <strong>of</strong> leading multidisciplinary<br />
team<br />
Helps others stay calm<br />
(ii) Identifies & responds to acutely abnormal physiology<br />
Incompetent<br />
Fails to focus on correcting<br />
abnormal physiology as a<br />
priority<br />
Lacks underst<strong>and</strong>ing <strong>of</strong><br />
clinical relevance <strong>of</strong><br />
abnormal vital signs<br />
Uses oxygen or intravenous<br />
fluids in a potentially unsafe<br />
manner<br />
Fails to monitor effect <strong>of</strong><br />
interventions<br />
Competent<br />
Administers oxygen safely, monitors<br />
efficacy<br />
Identifies <strong>and</strong> attempts to correct<br />
hypotension appropriately<br />
Identifies oliguria, checks <strong>for</strong> common<br />
causes, intervenes appropriately<br />
Per<strong>for</strong>mance<br />
Interprets abnormal vital signs<br />
correctly in context<br />
Anticipates <strong>and</strong> prevents<br />
deterioration in vital signs<br />
Recognises patients at risk<br />
Investigates causes <strong>for</strong><br />
abnormal vital signs<br />
(iii) Where appropriate, delivers a fluid challenge safely to an acutely ill patient<br />
Incompetent<br />
Regularly fails to identify<br />
need <strong>for</strong> a fluid challenge<br />
Unable to distinguish<br />
between different fluids<br />
Competent<br />
Selects an appropriate fluid <strong>for</strong><br />
intravenous resuscitation<br />
Sets up fluid administration giving set<br />
correctly<br />
Administers fluid bolus(es), observes<br />
response, ensures continued<br />
administration with monitoring <strong>of</strong><br />
effect to desired endpoints<br />
Identifies hypokalaemia <strong>and</strong> chooses a<br />
safe & effective method <strong>of</strong> potassium<br />
supplementation<br />
Per<strong>for</strong>mance<br />
Reviews impact <strong>of</strong> fluid<br />
administration on organ system<br />
function<br />
Considers additional electrolyte<br />
replacement requirements<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 31<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013 31<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 31 09/04/2013 14:02
Management <strong>of</strong> Acutely Ill patients (2)<br />
(iv) Reassesses acutely ill patients promptly following initiation <strong>of</strong> treatment<br />
Incompetent<br />
Is unreliable in per<strong>for</strong>ming<br />
regular review <strong>of</strong> acutely ill<br />
or unstable patients<br />
Does not pass on in<strong>for</strong>mation<br />
to other members <strong>of</strong> the<br />
health care team to ensure<br />
continued review<br />
Competent<br />
Implements a system <strong>of</strong> regular<br />
checking <strong>of</strong> unstable patients<br />
Calls <strong>for</strong> help if patient does not<br />
respond to initial measures<br />
Makes patient safety a priority<br />
Per<strong>for</strong>mance<br />
Provides clear guidance to<br />
colleagues about monitoring<br />
Supports nursing staff in<br />
designing <strong>and</strong> implementing<br />
monitoring or calling criteria<br />
(v) Requests senior or more experienced help when appropriate<br />
Incompetent<br />
Permits problems to remain<br />
unresolved without seeking<br />
help<br />
Does not make decisions<br />
Seeks help all the time<br />
Over-confident<br />
No insight into own<br />
limitations<br />
Competent<br />
Analyses clinical problems, considers<br />
possible causes & solutions.<br />
Calls <strong>for</strong> help or advice appropriately<br />
Per<strong>for</strong>mance<br />
Prioritises problems<br />
Puts the patient first<br />
Seniors are confident in his/her<br />
judgement<br />
(vi) Undertakes a secondary survey to establish a differential diagnosis<br />
Incompetent<br />
Fails to consider underlying<br />
cause <strong>for</strong> deterioration<br />
Inaccurate examination<br />
technique, mistakes or<br />
overlooks important clinical<br />
signs<br />
Competent<br />
Recognises the importance <strong>of</strong> iterative<br />
review<br />
Competent history taking <strong>and</strong> clinical<br />
examination<br />
Arranges basic laboratory tests<br />
Per<strong>for</strong>mance<br />
Focused further history taking<br />
in difficult circumstances<br />
<strong>and</strong>/or when patient unable to<br />
co-operate (see 1.A)<br />
Rapidly identifies clinical signs,<br />
links them to the history to<br />
<strong>for</strong>m a differential diagnosis<br />
Plans appropriate investigations<br />
to confirm or refute a diagnosis<br />
32<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
32 First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 32 09/04/2013 14:02
Management <strong>of</strong> Acutely Ill patients (3)<br />
(vii) Obtains an arterial blood gas sample safely, interprets results correctly<br />
Incompetent<br />
Fails to underst<strong>and</strong> the need<br />
<strong>for</strong> arterial blood gas<br />
sampling <strong>and</strong> <strong>of</strong>ten omits or<br />
delays taking the sample<br />
Does not know the main<br />
indications <strong>and</strong><br />
contraindications <strong>for</strong><br />
sampling<br />
Fails to attend to patient<br />
com<strong>for</strong>t during the procedure<br />
Competent<br />
Takes an arterial sample safely using a<br />
heparinised syringe<br />
Describes common causes <strong>of</strong> abnormal<br />
values.<br />
Interprets results in context<br />
Documents results clearly in the case<br />
record<br />
Per<strong>for</strong>mance<br />
Communicates significance <strong>of</strong><br />
acid base disturbances to others<br />
in the team<br />
Directs corrective measures<br />
(viii) Manages patients with impaired consciousness including fits<br />
Incompetent<br />
Omits major supportive<br />
measures<br />
Unaware <strong>of</strong> complications <strong>of</strong><br />
anticonvulsant therapy<br />
Fails to provide a safe<br />
environment <strong>for</strong> the patient,<br />
including seeking senior<br />
assistance<br />
Competent<br />
Appreciates urgency<br />
Administers oxygen, protects airway in<br />
unconscious patient<br />
Places unconscious patient in recovery<br />
position<br />
Calls <strong>for</strong> help if fitting does not<br />
respond to immediate measures<br />
Follows local protocols<br />
Per<strong>for</strong>mance<br />
Seeks <strong>and</strong> corrects<br />
abnormalities <strong>of</strong> physiological<br />
signs, particularly hypoxaemia,<br />
hypotension, hypoglycaemia<br />
<strong>and</strong> electrolyte disturbances<br />
Questions <strong>and</strong> discusses<br />
scientific content <strong>of</strong> protocols<br />
in use<br />
Capable <strong>of</strong> leading<br />
multidisciplinary team<br />
(ix) Safely uses common analgesic drugs<br />
Incompetent<br />
Does not routinely seek<br />
in<strong>for</strong>mation about patient<br />
com<strong>for</strong>t<br />
Fails to review patient’s<br />
com<strong>for</strong>t in a timely manner<br />
Lacks knowledge <strong>of</strong> side<br />
effects <strong>of</strong> commonly used<br />
analgesic drugs<br />
Prescribes analgesics<br />
unsafely<br />
Fails to consider interactions<br />
between patient’s condition<br />
<strong>and</strong> side effects <strong>of</strong> commonly<br />
used analgesics<br />
Competent<br />
Evaluates the patient in pain<br />
Prescribes opioid <strong>and</strong> non-opioid<br />
analgesic drugs safely<br />
Re-evaluates the efficacy <strong>of</strong> analgesia<br />
in a timely manner<br />
Monitors patients <strong>for</strong> common side<br />
effects <strong>of</strong> analgesic drugs<br />
Safely uses anti-emetic drugs to treat or<br />
prevent nausea & vomiting<br />
Per<strong>for</strong>mance<br />
Considers the effect <strong>of</strong> hepatic<br />
<strong>and</strong> renal dysfunction on<br />
analgesic pharmacology<br />
Makes patient com<strong>for</strong>t a<br />
priority<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 33<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013 33<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 33 09/04/2013 14:02
Management <strong>of</strong> Acutely Ill patients (4)<br />
(x) Explains the principles <strong>of</strong> managing a patient following self-harm<br />
Incompetent<br />
Fails to consider<br />
possibility <strong>of</strong> self harm as<br />
cause <strong>for</strong> patient’s<br />
presentation<br />
Omits appropriate<br />
investigations in patients<br />
who present after selfpoisoning<br />
Does not identify main<br />
monitoring goals<br />
Competent<br />
Focussed history taking, including<br />
psychosocial causes requiring social<br />
services or police intervention<br />
Can access Toxbase<br />
Recognises need <strong>for</strong> involvement <strong>of</strong><br />
Mental Health or more experienced<br />
personnel<br />
Demonstrates tolerance & underst<strong>and</strong>ing<br />
Per<strong>for</strong>mance<br />
Protects <strong>and</strong> supports<br />
colleagues faced with an<br />
abusive patient<br />
Anticipates necessary steps to<br />
minimise risks to patient<br />
Can per<strong>for</strong>m a mental state<br />
assessment<br />
(xi) Describes the management <strong>of</strong> a patient with an acute psychosis<br />
Incompetent<br />
Fails to recognize features<br />
<strong>of</strong> psychosis<br />
Unaware <strong>of</strong> provisions <strong>of</strong><br />
Mental Health Act<br />
Competent<br />
Recognizes diagnostic features <strong>of</strong> psychosis<br />
Summons experienced help promptly<br />
Can discuss safe administration <strong>of</strong> antipsychotic<br />
drugs<br />
Can discuss provisions <strong>of</strong> Mental Health<br />
Act<br />
Per<strong>for</strong>mance<br />
Protects patient <strong>and</strong><br />
colleagues from harm<br />
Can safely administer antipsychotic<br />
drugs<br />
Can initiate requirements <strong>of</strong><br />
the Mental Health Act<br />
Considers underlying causes<br />
<strong>of</strong> psychosis<br />
(xii) Resuscitation training<br />
Incompetent<br />
No certification or<br />
indication <strong>of</strong> not reaching<br />
the required st<strong>and</strong>ard<br />
Competent<br />
Trained to Intermediate Life Support (ILS)<br />
st<strong>and</strong>ard<br />
Per<strong>for</strong>mance<br />
Trained to Advanced Life<br />
Support (ALS) st<strong>and</strong>ard<br />
(xiii) Discusses Do Not Attempt Resuscitation (DNAR) orders/advance directives appropriately.<br />
Incompetent<br />
Does not underst<strong>and</strong> the<br />
importance <strong>of</strong> timely<br />
DNAR decisions <strong>and</strong> their<br />
discussion with patients,<br />
relations <strong>and</strong>/or colleagues.<br />
Ignores advance directives.<br />
May cause unnecessary<br />
upset<br />
Competent<br />
Underst<strong>and</strong>s the criteria <strong>for</strong> issuing orders<br />
<strong>and</strong> level <strong>of</strong> experience required to issue<br />
them<br />
Can discuss with colleagues including<br />
nurses <strong>and</strong> also relatives.<br />
Facilitates the regular review <strong>of</strong> DNAR<br />
decisions <strong>and</strong> underst<strong>and</strong>s actions required<br />
if decision challenged<br />
Per<strong>for</strong>mance<br />
Discusses the DNAR criteria<br />
<strong>and</strong> their legal framework<br />
with colleagues including<br />
nurses <strong>and</strong> also relatives<br />
Encourages regular review <strong>of</strong><br />
this order <strong>and</strong> takes<br />
appropriate action if<br />
challenged<br />
34<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
34 First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 34 09/04/2013 14:02
Practical procedures<br />
Incompetent<br />
High failure rate <strong>for</strong><br />
simple procedures<br />
Hurts patients<br />
Ignores patients<br />
feeling <strong>and</strong> wishes<br />
Unsafe, prepares<br />
badly<br />
Unclear <strong>and</strong> worrying<br />
consent<br />
Muddled records<br />
Competent<br />
For each procedure consider the following:<br />
1. Knowledge <strong>of</strong> indications &<br />
contraindications<br />
2. Explanation to the patient<br />
3. Skill in gaining in<strong>for</strong>med consent<br />
4. Preparation <strong>of</strong> equipment<br />
5. Preparation <strong>of</strong> the skin where<br />
appropriate<br />
6. Positioning <strong>of</strong> the patient<br />
7. Trainees hygiene where appropriate<br />
8. Sharing <strong>of</strong> in<strong>for</strong>mation <strong>and</strong> aftercare<br />
arrangements<br />
9. Monitoring <strong>of</strong> the patient<br />
10. Disposal <strong>of</strong> equipment<br />
11. Documentation <strong>of</strong> procedure<br />
12. Recording complications<br />
Per<strong>for</strong>mance<br />
A model per<strong>for</strong>mer, seen as<br />
the example to follow.<br />
Contributes to the<br />
improvement <strong>of</strong> this aspect<br />
<strong>of</strong> the service<br />
Procedures<br />
• Venepuncture, cannulation <strong>and</strong> venesection<br />
• Central venous access<br />
• Blood cultures from peripheral <strong>and</strong> central sites<br />
• Intravenous infusions including the prescription <strong>of</strong> fluids, blood <strong>and</strong> blood products<br />
• Per<strong>for</strong>ming an ECG<br />
• Arterial blood sampling<br />
• Injection- subcutaneous, intradermal, intramuscular, intravenous<br />
• Urethral catheterisation, male <strong>and</strong> female<br />
• Airway care, oxygen, nebulisers<br />
• Respiratory function tests – spirometry, peak flow rate<br />
• Nasogastric tube insertion<br />
• Urinalysis<br />
• Proctoscopy<br />
• Pleural aspiration<br />
• Lumbar puncture diagnostic <strong>and</strong> therapeutic<br />
• Skin suturing<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 35<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013 35<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 35 09/04/2013 14:02
2 Maintaining good medical practice<br />
Incompetent<br />
Learning<br />
Lazy<br />
Never turns up to timetabled<br />
teaching sessions<br />
Never voluntarily addresses<br />
gaps in their knowledge.<br />
When assessed <strong>for</strong> a second<br />
time on core knowledge has<br />
made no progress.<br />
Does not learn from mistakes<br />
No use <strong>of</strong> IT<br />
No personal learning plan<br />
No engagement with the e<br />
portfolio<br />
Inadequate number <strong>of</strong><br />
SLEs/WPBAs<br />
Clustering <strong>of</strong> SLEs, over<br />
reliance on other trainees <strong>and</strong><br />
allied health pr<strong>of</strong>essionals<br />
Evidence / audit / guidelines<br />
Fails to show any knowledge<br />
or underst<strong>and</strong>ing <strong>of</strong> the<br />
evidence base in medical care.<br />
Avoids discussions with<br />
colleagues <strong>and</strong> patients<br />
(carers) in this area.<br />
Ignores or unaware <strong>of</strong> local<br />
guidelines/protocols<br />
Has no knowledge <strong>of</strong> the audit<br />
cycle, or any recognition <strong>of</strong> its<br />
relevance to the assessment<br />
<strong>and</strong> improvement <strong>of</strong> clinical<br />
st<strong>and</strong>ards<br />
Competent<br />
Learning<br />
Hard working<br />
Regular <strong>and</strong> active contribution at<br />
organised teaching sessions. (>50%<br />
attendance)<br />
Uses sensible methods to build up their<br />
knowledge <strong>and</strong> skills.<br />
When assessed <strong>for</strong> a second time on<br />
core knowledge has a well-<strong>for</strong>mulated<br />
answer.<br />
Awareness <strong>of</strong> & can access electronic<br />
learning resources, databases, library<br />
Personal learning plan (reflective<br />
learner)<br />
Contemporaneous engagement with the<br />
e portfolio<br />
Prescribed number <strong>of</strong> SLEs/WPBAs<br />
Regular SLEs, mainly by consultants<br />
Evidence / audit / guidelines<br />
Demonstrates a clear ability to<br />
critically appraise evidence base <strong>of</strong><br />
medical care<br />
Willing to discuss with colleagues <strong>and</strong><br />
seeks to in<strong>for</strong>m patients (carers)<br />
appropriately<br />
Applies local guidelines/protocols.<br />
Underst<strong>and</strong>s the audit cycle <strong>and</strong><br />
recognises how it relates to the<br />
improvement <strong>of</strong> clinical st<strong>and</strong>ards<br />
Per<strong>for</strong>mance<br />
Learning<br />
Exemplary<br />
Sets st<strong>and</strong>ards (>75%<br />
attendance at teaching<br />
sessions)<br />
Always has a well<br />
researched <strong>and</strong> organised<br />
approach to medical practice<br />
Reports own errors<br />
unhesitatingly & shows<br />
ability to learn from the<br />
experience<br />
Actively evolving personal<br />
learning plan (reflective<br />
self-directed learner)<br />
E portfolio exemplary<br />
organisation<br />
More than enough SLEs:<br />
with evidence that the<br />
curriculum is being<br />
systematically covered<br />
Evidence / audit /<br />
guidelines<br />
Implements the available<br />
evidence base in most areas<br />
<strong>of</strong> clinical care<br />
Seeks out opportunities to<br />
discuss with colleagues.<br />
Supports patients (carers) in<br />
making sense <strong>of</strong> the<br />
evidence base in terms <strong>of</strong><br />
their personal circumstances<br />
Seeks to refine local<br />
guidelines/protocols<br />
Has been actively involved<br />
in undertaking a clinical<br />
audit, <strong>and</strong> recognises how it<br />
relates to the improvement<br />
<strong>of</strong> clinical st<strong>and</strong>ards <strong>and</strong><br />
addresses the clinical<br />
governance agenda<br />
36<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
36 First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 36 09/04/2013 14:02
3a<br />
Relationship with Patients<br />
Incompetent<br />
A: patient centredness<br />
Discourteous, inconsiderate <strong>of</strong><br />
patients’ views, preferences,<br />
cultural norms, dignity &<br />
privacy<br />
Discusses one patient in front<br />
<strong>of</strong> another<br />
Unable to reassure, subject <strong>of</strong><br />
repeated complaints.<br />
Discriminates against patients<br />
with disabilities<br />
Exploits relationships with<br />
patients to own advantage<br />
Has inappropriate financial or<br />
personal relationships with<br />
patients<br />
B: Communication Skills<br />
Consistently ignores,<br />
interrupts or contradicts<br />
patients<br />
Competent<br />
A: patient centredness<br />
Respects the autonomy, dignity,<br />
confidentiality & privacy <strong>of</strong> the<br />
patient.<br />
Knowledge <strong>of</strong> limits to<br />
confidentiality<br />
Elicits the patients hopes, fears &<br />
expectations<br />
Relates to patients as equal<br />
partners, encourages questions<br />
Knowledge <strong>of</strong> children’s rights<br />
B: Communication Skills<br />
Courteous, polite, communicates<br />
well with patients<br />
Demonstrates active listening &<br />
an ability to establish trust &<br />
rapport<br />
Able to break bad news to<br />
patients sensitively, & avoid<br />
conveying unrealistic optimism<br />
& undue pessimism<br />
Able to h<strong>and</strong>le difficult patient<br />
interactions – reassurance <strong>of</strong> the<br />
‘worried well’, self discharge,<br />
complaints, do not resuscitate<br />
decisions<br />
Avoids jargon<br />
Telephone skills<br />
Per<strong>for</strong>mance<br />
A: patient centredness<br />
Able to anticipate patients emotional<br />
& physical needs & plans to meet<br />
them<br />
Recognises & responds to their health<br />
beliefs<br />
B: Communication skills<br />
Explains clearly & checks<br />
underst<strong>and</strong>ing<br />
Able to apply models <strong>of</strong> the<br />
consultation appropriately<br />
Able to use language (<strong>and</strong><br />
interpreters) appropriately; including<br />
communicating with patients with a<br />
disability e.g. deafness, visual<br />
impairment<br />
Respond to a patients underst<strong>and</strong>ing<br />
when breaking bad news or in<br />
discussion <strong>of</strong> life threatening or<br />
terminal illness<br />
Able to h<strong>and</strong>le difficult patient<br />
interactions –advance directives /<br />
living wills, organ donation,<br />
reporting patients to DVLA,<br />
compulsory detention under a section<br />
<strong>of</strong> the Mental Health Act<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 37<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013 37<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 37 09/04/2013 14:02
3b<br />
Relationship with Patients<br />
Incompetent<br />
C: Patient<br />
Involvement:<br />
Ignores the patients best<br />
interests when deciding<br />
about treatment or<br />
referral<br />
Fails to obtain patients<br />
consent to treatment<br />
Competent<br />
C: Patient Involvement:<br />
Explain the concept <strong>of</strong> risk to a<br />
patient<br />
Knowledge <strong>of</strong> legal framework <strong>of</strong><br />
consent<br />
Apply the rules <strong>of</strong> consent – gain<br />
consent <strong>for</strong> a variety <strong>of</strong> procedures<br />
Able to provide patients with<br />
underst<strong>and</strong>able in<strong>for</strong>mation<br />
Appropriate use <strong>of</strong> leaflets &<br />
written in<strong>for</strong>mation<br />
D: Patient in Context<br />
Underst<strong>and</strong>ing <strong>of</strong> the impact <strong>of</strong> the<br />
patient as a person in a family<br />
E: Relationship with patients<br />
relatives / carers<br />
Can gain consent <strong>for</strong> a postmortem<br />
Able to break bad news to relatives<br />
sensitively<br />
Able to share decision making with<br />
relatives<br />
F: Health Promotion<br />
Give simple health promotion<br />
advice<br />
Per<strong>for</strong>mance<br />
C: Patient Involvement:<br />
Respond to a patients underst<strong>and</strong>ing &<br />
attitude towards risk<br />
Ensure patients are able to make<br />
in<strong>for</strong>med choices in health care<br />
decisions<br />
Respects the rights <strong>of</strong> patients to refuse<br />
treatments or tests<br />
Share an underst<strong>and</strong>ing <strong>of</strong> printed or<br />
internet in<strong>for</strong>mation to enhance the<br />
patients concordance with management<br />
plans & prescriptions<br />
D: Patient in Context<br />
Gain underst<strong>and</strong>ing <strong>of</strong> physical,<br />
psychological, social & cultural<br />
dimensions <strong>of</strong> problems presented<br />
E: Relationship with patients<br />
relatives / carers<br />
Able to deal with patients who cannot<br />
give in<strong>for</strong>med consent<br />
F: Health Promotion<br />
Assess an individual’s risk factors &<br />
tailor make health promotion advice<br />
38<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
38 First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 38 09/04/2013 14:02
4 Working with Colleagues – Team working<br />
Incompetent<br />
a. Communication<br />
Unable / refuses to communicate<br />
with colleagues<br />
Intolerant <strong>of</strong> other pr<strong>of</strong>essional<br />
viewpoint<br />
b. Team Working<br />
Does not know the members <strong>of</strong><br />
the team in which they work<br />
Does not partake in team<br />
meetings<br />
Does not know what skills other<br />
team members have<br />
Delegates tasks to other<br />
members <strong>of</strong> the team <strong>for</strong> which<br />
they don’t have the appropriate<br />
skills<br />
Bullies or harasses her<br />
colleagues<br />
Can’t work to a common goal –<br />
selfish, inflexible<br />
c. Referral <strong>and</strong> h<strong>and</strong>over<br />
Doesn’t pass on in<strong>for</strong>mation to<br />
colleagues about at-risk patients<br />
Dismisses patients requests <strong>for</strong> a<br />
second opinion<br />
Refers patients <strong>for</strong> care which<br />
they should be able to provide<br />
Does not provide in<strong>for</strong>mation in<br />
a referral that enables the second<br />
opinion to give appropriate<br />
advice<br />
Competent<br />
a. Communication<br />
Listens to colleagues, accepts<br />
the views <strong>of</strong> others<br />
Able to communicate<br />
effectively with other<br />
members <strong>of</strong> the team & interpr<strong>of</strong>essional<br />
communication<br />
(nursing staff / social services /<br />
coroner)<br />
Able to communicate<br />
effectively with other teams<br />
(h<strong>and</strong> over)<br />
Able to communicate<br />
effectively with GP colleagues<br />
-(telephone referrals ‘on take’)<br />
-written communication<br />
(discharges)<br />
Able to present a case clearly<br />
b. Team working<br />
Attends & contributes to team<br />
meetings<br />
Knows how to contact team<br />
outside meetings<br />
Ensures satisfactory<br />
completion <strong>of</strong> reasonable tasks<br />
by the end <strong>of</strong> the day / shift<br />
Arranges cover <strong>for</strong> duties with<br />
colleagues<br />
Flexible – ability to change in<br />
the face <strong>of</strong> a valid argument<br />
a. Referral <strong>and</strong> h<strong>and</strong>over<br />
Knowledge <strong>of</strong> roles &<br />
responsibilities <strong>of</strong> team<br />
members & other<br />
pr<strong>of</strong>essionals in patient care,<br />
able to involve them in care<br />
appropriately<br />
Accompanies referrals with<br />
the in<strong>for</strong>mation needed by the<br />
second opinion to make an<br />
appropriate <strong>and</strong> efficient<br />
evaluation <strong>of</strong> the patients<br />
problem<br />
Per<strong>for</strong>mance<br />
a. Communication<br />
Able to bring together views <strong>for</strong> a<br />
common goal<br />
b. Team Working<br />
Anticipates problems <strong>for</strong> next shift<br />
& takes pre-emptive action<br />
Able to lead <strong>and</strong> facilitate team<br />
meetings<br />
Able to facilitate change<br />
Team goal is put be<strong>for</strong>e personal<br />
agenda<br />
Able to facilitate the development<br />
<strong>of</strong> colleagues<br />
c. Referral <strong>and</strong> h<strong>and</strong>over<br />
Where appropriate feeds back to<br />
specialists views on the quality <strong>of</strong><br />
their care<br />
Uses h<strong>and</strong>overs systematically <strong>for</strong><br />
training other doctors <strong>and</strong> nurses.<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 39<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013 39<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 39 09/04/2013 14:02
5 Teaching <strong>and</strong> Training<br />
Incompetent<br />
Teaching<br />
No interest in teaching,<br />
mentoring <strong>and</strong>/or supervising<br />
more junior doctors / medical<br />
students<br />
Few teaching skills<br />
Presentations<br />
Absent themselves at the last<br />
minute, poor preparation <strong>and</strong><br />
structure<br />
Competent<br />
Teaching<br />
Beginning to develop teaching<br />
skills, supervising more junior<br />
doctors & medical students<br />
Presentations<br />
Gives presentations to small<br />
groups e.g. journal club<br />
Per<strong>for</strong>mance<br />
Teaching<br />
Actively involved in teaching,<br />
enthusiastic, able to motivate<br />
Clear demonstration <strong>of</strong> teaching<br />
skills<br />
Presentations<br />
Confident, embraces new<br />
technology<br />
Able to present material using<br />
different media<br />
40<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
40 First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 40 09/04/2013 14:02
6 Probity / pr<strong>of</strong>essional behaviour:<br />
Trustworthiness, honesty, confidentiality, ethics, dress code, manners, punctuality, time<br />
management<br />
Incompetent<br />
Poor attitude / approach in<br />
above areas, possible concerns...<br />
Fails to make care <strong>of</strong> patient first<br />
concern<br />
Own beliefs prejudice care<br />
Abuses position as doctor<br />
Seeks inappropriate personal<br />
gain in pursuit <strong>of</strong> practice<br />
Carelessly attaches her name to<br />
certificates or documents<br />
Provides false in<strong>for</strong>mation on<br />
such documents<br />
Persistently failing to cope with<br />
own work, despite advice,<br />
support <strong>and</strong> extra clinical help<br />
Fails to involve patients in<br />
decision making<br />
Competent<br />
Reasonable approach /<br />
attitudes in above areas…<br />
Recognises own limitations –<br />
seeks advice if unsure<br />
Accepts pr<strong>of</strong>essional<br />
regulation<br />
Punctual<br />
Attends to detail<br />
Respects living wills &<br />
advance directives<br />
Knowledge <strong>of</strong> legal<br />
responsibilities & ability to<br />
complete death certificates<br />
Only shares clinical<br />
in<strong>for</strong>mation, whether spoken<br />
or written, with appropriate<br />
individuals or groups<br />
Needs occasional help with<br />
organisation <strong>and</strong> prioritisation<br />
<strong>of</strong> tasks<br />
Mostly re-prioritises<br />
appropriately <strong>and</strong> usually calls<br />
<strong>for</strong> help when falling behind.<br />
Per<strong>for</strong>mance<br />
Excellent attitude / approach in<br />
above areas, a credit to the<br />
pr<strong>of</strong>ession. Coaches F1 trainees in<br />
these attitudes<br />
Patient care a priority<br />
Seeks constructive criticism &<br />
changes per<strong>for</strong>mance as a result<br />
Fosters trust amongst others &<br />
promotes sensitivity to others<br />
feelings & needs<br />
Prioritises <strong>and</strong> re-prioritises<br />
appropriately<br />
Delegates or calls <strong>for</strong> help in a<br />
timely fashion when he/she is<br />
falling behind<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 41<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013 41<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 41 09/04/2013 14:02
7 Health:<br />
This section should be used if there are any health issues which have influenced<br />
the doctor’s progress in the foundation programme<br />
Concerns<br />
Often <strong>of</strong>f sick<br />
No explanation<br />
Often coincides with duty<br />
Genuine health issues used to justify<br />
underper<strong>for</strong>mance<br />
No concerns<br />
Rarely sick<br />
Always explains <strong>and</strong> apologises<br />
Genuine health issues never used to justify<br />
underper<strong>for</strong>mance<br />
42<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
42 First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 42 09/04/2013 14:02
Appendix D: Checklist <strong>for</strong> Adult Dyslexia<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 43<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013 43<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 43 09/04/2013 14:02
Appendix E:<br />
Role <strong>of</strong> educational supervisor in the revalidation <strong>of</strong> trainees<br />
As ES your role is to support the revalidation <strong>of</strong> trainees by:<br />
• ensuring the ES report <strong>for</strong> ARCP is sufficiently comprehensive <strong>and</strong> clear to be<br />
used in triangulation about fitness to practise<br />
• including a statement in the ES report <strong>for</strong> ARCP about your knowledge <strong>of</strong><br />
their involvement in conduct, capability, serious untoward incidents,<br />
significant event investigation or complaints as a named individual<br />
• helping trainees to underst<strong>and</strong> the PGMDE process <strong>for</strong> revalidation <strong>and</strong> what<br />
is required <strong>of</strong> them (http://www.ox<strong>for</strong>ddeanery.nhs.uk/revalidation.aspx)<br />
• Role model <strong>of</strong> good appraisal<br />
• Encouraging trainees to document their reflection<br />
• Communicating concerns any concerns about fitness to practise in a timely<br />
manner <strong>and</strong> to the appropriate people<br />
44<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
44 First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d <strong>Deanery</strong> Jan 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v3.indd 44 12/04/2013 16:01
Notes<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013 45<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 45 09/04/2013 14:02
Notes<br />
46<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 46 09/04/2013 14:02
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 47 09/04/2013 14:02
Postgraduate <strong>Medical</strong> & <strong>Dental</strong> Education<br />
The Triangle, Roosevelt Drive,<br />
Headington<br />
Ox<strong>for</strong>d<br />
OX3 7XP<br />
Tel: 01865 740601<br />
www.thamesvalley.hee.nhs.uk<br />
www.ox<strong>for</strong>ddeanery.nhs.uk<br />
First edn. <strong>Field</strong> <strong>Guide</strong> <strong>for</strong> <strong>Supervisors</strong>: Ox<strong>for</strong>d PGMDE Apr 2013<br />
49087 Ox PGMDE H<strong>and</strong>book v2.indd 48 09/04/2013 14:02