IHE Patient Care Coordination Technical Framework Vol I
IHE Patient Care Coordination Technical Framework Vol I
IHE Patient Care Coordination Technical Framework Vol I
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
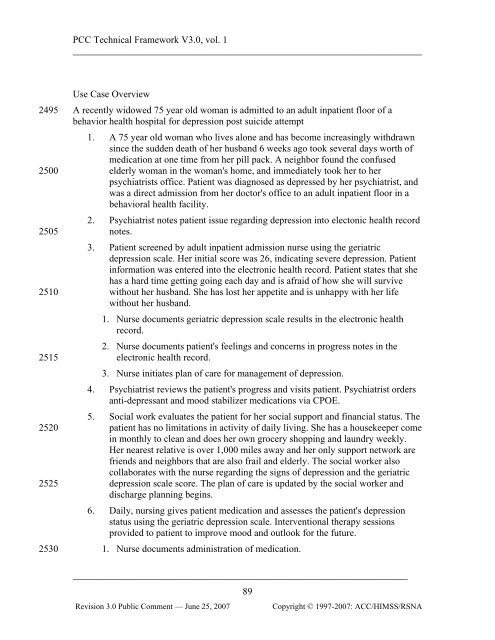
PCC <strong>Technical</strong> <strong>Framework</strong> V3.0, vol. 1<br />
________________________________________________________________________<br />
2495<br />
2500<br />
2505<br />
2510<br />
2515<br />
2520<br />
2525<br />
2530<br />
Use Case Overview<br />
A recently widowed 75 year old woman is admitted to an adult inpatient floor of a<br />
behavior health hospital for depression post suicide attempt<br />
1. A 75 year old woman who lives alone and has become increasingly withdrawn<br />
since the sudden death of her husband 6 weeks ago took several days worth of<br />
medication at one time from her pill pack. A neighbor found the confused<br />
elderly woman in the woman's home, and immediately took her to her<br />
psychiatrists office. <strong>Patient</strong> was diagnosed as depressed by her psychiatrist, and<br />
was a direct admission from her doctor's office to an adult inpatient floor in a<br />
behavioral health facility.<br />
2. Psychiatrist notes patient issue regarding depression into electonic health record<br />
notes.<br />
3. <strong>Patient</strong> screened by adult inpatient admission nurse using the geriatric<br />
depression scale. Her initial score was 26, indicating severe depression. <strong>Patient</strong><br />
information was entered into the electronic health record. <strong>Patient</strong> states that she<br />
has a hard time getting going each day and is afraid of how she will survive<br />
without her husband. She has lost her appetite and is unhappy with her life<br />
without her husband.<br />
1. Nurse documents geriatric depression scale results in the electronic health<br />
record.<br />
2. Nurse documents patient's feelings and concerns in progress notes in the<br />
electronic health record.<br />
3. Nurse initiates plan of care for management of depression.<br />
4. Psychiatrist reviews the patient's progress and visits patient. Psychiatrist orders<br />
anti-depressant and mood stabilizer medications via CPOE.<br />
5. Social work evaluates the patient for her social support and financial status. The<br />
patient has no limitations in activity of daily living. She has a housekeeper come<br />
in monthly to clean and does her own grocery shopping and laundry weekly.<br />
Her nearest relative is over 1,000 miles away and her only support network are<br />
friends and neighbors that are also frail and elderly. The social worker also<br />
collaborates with the nurse regarding the signs of depression and the geriatric<br />
depression scale score. The plan of care is updated by the social worker and<br />
discharge planning begins.<br />
6. Daily, nursing gives patient medication and assesses the patient's depression<br />
status using the geriatric depression scale. Interventional therapy sessions<br />
provided to patient to improve mood and outlook for the future.<br />
1. Nurse documents administration of medication.<br />
_____________________________________________________________________<br />
89<br />
Revision 3.0 Public Comment — June 25, 2007<br />
Copyright © 1997-2007: ACC/HIMSS/RSNA