Download Slides - AATS: American Association for Thoracic Surgery ...
Download Slides - AATS: American Association for Thoracic Surgery ...
Download Slides - AATS: American Association for Thoracic Surgery ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
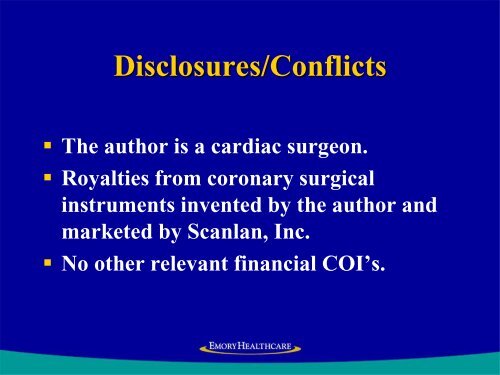
Disclosures/Conflicts<br />
• The author is a cardiac surgeon.<br />
• Royalties from coronary surgical<br />
instruments invented by the author and<br />
marketed by Scanlan, Inc.<br />
• No other relevant financial COI’s.
Whatever Happened to OPCAB<br />
John D. Puskas, MD, FACS, FACC<br />
Professor, Quality Officer and Associate Chief<br />
Division of Cardiothoracic <strong>Surgery</strong>, Emory University<br />
<strong>AATS</strong> Annual Meeting<br />
May 8, 2013<br />
Minneapolis, MN
Why Should OPCAB Be Better<br />
• CABG/CPB entails extracorporeal circulation, aortic<br />
cannulation and clamping, global myocardial<br />
ischemia, hypothermia, hemodilution etc.<br />
• OPCAB avoids these deleterious effects of CPB by<br />
mechanically stabilizing each coronary artery target<br />
individually, while the rest of the heart beats and<br />
supports normal physiologic circulation.<br />
• If a complete revascularization with precise<br />
anastomoses can be accomplished without CPB,<br />
then the patient will benefit.
National Data Sample<br />
• Non-emergent, isolated, primary CABGs<br />
• ONCAB or OPCAB<br />
• North <strong>American</strong> centers which each<br />
per<strong>for</strong>med >100 ONCAB and >100 OPCAB<br />
cases between 1/1/2004 and 12/31/2005<br />
• Time interval included all data available since<br />
introduction of data field <strong>for</strong> conversions
Study Cohort (Intent-to-Treat)<br />
• 42,477 consecutive patients:<br />
16,245 OPCAB vs 26,232 CPB<br />
• 63 North <strong>American</strong> centers, including 8 with<br />
cardiothoracic residency programs<br />
• Of the 16,245 OPCAB cases, 355 (2.2%) were<br />
converted during surgery from an initial OPCAB<br />
approach to ONCAB and were analyzed within the<br />
OPCAB group.
Risk-Adjusted Odds Comparisons<br />
OPCAB vs ONCAB:<br />
Major Adverse Cardiac Events<br />
Outcome Adjusted OR (95% CI) P-value<br />
Death 0.83 (0.69, 0.98) 0.03<br />
Stroke 0.65 (0.52, 0.80)
Risk-Adjusted Odds Comparisons<br />
OPCAB vs ONCAB: Other Outcomes<br />
Outcome Adjusted OR (95% CI) P-value<br />
Renal Failure 0.74 (0.64, 0.86)
Off-Pump Coronary Artery Bypass<br />
Disproportionately Benefits Patients With<br />
Higher Society of <strong>Thoracic</strong> Surgeons Predicted<br />
Risk Of Mortality<br />
John D Puskas MD, Vinod Thourani MD, Patrick Kilgo MS*,<br />
William Cooper MD, Thomas Vassiliades MS, J David Vega MD,<br />
Cullen Morris MD, Edward Chen MD, Brian J Schmotzer BS*,<br />
Robert A Guyton MD, Omar M Lattouf MD PhD<br />
Emory University<br />
Atlanta, USA<br />
Society of <strong>Thoracic</strong> Surgeons<br />
January 27, 2009<br />
San Francisco
Methods<br />
• The Society of <strong>Thoracic</strong> Surgeons (STS) database was<br />
queried <strong>for</strong> all isolated, primary CABG cases between<br />
1/1/97 and 12/31/07 at a US academic center.<br />
• The STS Predicted Risk of Mortality (PROM), based on<br />
30 preoperative risk factors, was used in three ways to<br />
compare 30-day operative mortality between patients<br />
treated with OPCAB versus CPB.
Results (1)<br />
• There were 14766 consecutive patients; 7083<br />
OPCAB (48.0%) and 7683 CPB (52.0%).<br />
• There was no difference in operative mortality<br />
between OPCAB and CPB <strong>for</strong> patients in the<br />
lower two risk quartiles.<br />
• In the higher risk quartiles there was a mortality<br />
benefit <strong>for</strong> OPCAB (odds ratio 0.62 and 0.45 <strong>for</strong><br />
OPCAB in the third and fourth risk quartiles).
Results (2)<br />
• In the highest risk quartile there was a large<br />
mortality benefit <strong>for</strong> OPCAB:<br />
(Odds Ratio 0.45; 95%CI 0.33-0.63; p
Conclusions<br />
• OPCAB is associated with lower operative<br />
mortality than CABG on CPB <strong>for</strong> higher risk<br />
patients.<br />
• This mortality benefit increases with<br />
increasing STS Predicted Risk of Mortality.
Implications (1)<br />
• These findings corroborate the preference of<br />
many surgeons to per<strong>for</strong>m OPCAB <strong>for</strong><br />
patients at high risk <strong>for</strong> mortality with<br />
CABG/CPB.<br />
• Explain why randomized controlled trials<br />
enrolling predominantly low risk patients<br />
have failed to show a mortality benefit <strong>for</strong><br />
OPCAB.
Off-Pump Coronary Artery Bypass<br />
Disproportionately Benefits Higher Risk<br />
Patients After Adjustment <strong>for</strong> Patient Factors,<br />
Center Volume and Surgeon Identity<br />
John D Puskas MD*, Sean S. O’Brien PhD**<br />
and Xia He MS**<br />
*Division of Cardiothoracic <strong>Surgery</strong>, Emory University and<br />
**Duke Clinical Research Institute, Duke University<br />
<strong>American</strong> <strong>Association</strong> <strong>for</strong> <strong>Thoracic</strong> <strong>Surgery</strong><br />
Annual Meeting 2012<br />
San Francisco
Methods<br />
• The STS National Cardiac Database queried <strong>for</strong> all isolated,<br />
primary CABG cases between 1/1/2005 and 12/31/2010<br />
• Of these 876,081 cases (“All Sites”), 210,469 were at<br />
participant sites that per<strong>for</strong>med >300 OPCAB and >300 CPB<br />
cases during the 6-year study period (“High Volume Sites”).<br />
• Operative mortality, stroke, ARF, M+M, and PLOS >=14d were<br />
analyzed with conditional logistic models, stratified by<br />
participant and by surgeon and adjusted <strong>for</strong> all 30 variables<br />
that comprise the STS PROM score.
Results (1)<br />
• OPCAB was associated with significant reduction in risk<br />
of death, stroke, ARF, M+M and PLOS>14d, compared to<br />
CABG/CPB after adjustment <strong>for</strong> 30 patient risk factors in<br />
the overall sample.<br />
• This held true within high volume centers alone, and was<br />
somewhat more pronounced after adjustment <strong>for</strong><br />
surgeon effect.
Results (2)<br />
• In the overall sample, there was a significant (p
Mortality or Major Morbidity For All Patients:<br />
OPCAB vs CPB at Varying Levels of PROM
Results (3)<br />
• In all PROM quartiles, OPCAB was associated with<br />
significantly reduced risk of death and stroke.<br />
• The magnitude of reduction increased with increasing PROM.<br />
• Large volume centers had slightly lower risk of death and<br />
stroke than lower volume centers.<br />
• The relative reduction of risk of death and stroke with<br />
OPCAB vs CPB was similar in high volume centers compared<br />
to all centers.
Whatever Happened to OPCAB
ROOBY Trial Rebuttal<br />
• VA ROOBY trial enrolled low-risk male patients in whom<br />
avoidance of CPB was unlikely to greatly improve the<br />
expected excellent outcomes.<br />
• Most cases per<strong>for</strong>med by residents, supervised by<br />
attendings inexperienced in OPCAB and much more<br />
experienced in ONCAB: 12.4% conversion rate 6x STS!<br />
• Illogical to conduct a RCT comparing outcomes with<br />
alternative surgical techniques among operators who have<br />
grossly asymmetric experience and expertise with the two<br />
techniques being compared.<br />
• Wrong patients; wrong surgeons.
ACC March, 2013<br />
26
CORONARY Trial<br />
Lamy et al, NEJM 2012<br />
• 4752 pts randomized at 79 centers in 19 countries<br />
• Predominantly low and intermediate risk patients<br />
• Primary endpoint: death, stroke, MI, RF<br />
• Intention-to-treat analysis<br />
• No signif difference at 30 days<br />
(OPCAB 9.8% vs CPB 10.3%; HR 0.95, p=0.59)
Benefits of OPCAB in CORONARY<br />
OPCAB associated with significant reduction in:<br />
• Transfusion (50.7% vs 63.3%; RR 0.80; CI 0.75-0.85; p
Primary Outcome (%)<br />
Primary outcome per EuroSCORE<br />
15<br />
HR 1.35<br />
HR 0.87<br />
HR 0.85<br />
12<br />
9<br />
6<br />
3<br />
0<br />
Off-pump On-pump Off-pump On-pump Off-pump On-pump<br />
0-2 3 to 5 >5<br />
P=0.047 interaction<br />
EuroSCORE
Primary Outcome per EuroSCORE<br />
OFF-PUMP<br />
ON-PUMP
Hazard Ratio<br />
Hazard Ratio Off-pump/On-pump<br />
ROOBY<br />
CORONARY<br />
37
1 st Co-Primary Outcome (30 Days)<br />
(830 patients)<br />
Off Pump<br />
%<br />
On Pump<br />
%<br />
Hazard<br />
Ratio<br />
95% CI<br />
p<br />
value<br />
Primary Outcome<br />
Death, Stroke, MI, Renal Failure<br />
Components<br />
9.2 13.7 0.66 0.44-1.00 0.049<br />
Death 1.4 1.4 1.01 0.33-3.13 0.98<br />
Stroke 1.2 1.7 0.72 0.23-2.27 0.57<br />
Non Fatal MI 7.5 10.6 0.70 0.44-1.11 0.13<br />
New Renal Failure 0.2 1.0 0.25 0.03-2.25 0.22<br />
* Not a pre-specified sub-group<br />
38
CORONARY: The Coronary Artery Bypass<br />
Grafting <strong>Surgery</strong> Off or On Pump<br />
Revascularization Study<br />
Results at 1 Year<br />
André Lamy<br />
Population Health Research Institute<br />
Hamilton Health Sciences<br />
McMaster University<br />
Hamilton, CANADA<br />
on behalf of the CORONARY Investigators<br />
Disclosures: CORONARY was funded by a grant from the Canadian Institutes<br />
of Health Research (CIHR).
1 st Co-Primary Outcome (1 Year)<br />
Off Pump<br />
%<br />
On Pump<br />
%<br />
Hazard<br />
Ratio<br />
95% CI<br />
p<br />
value<br />
Primary Outcome<br />
Death, Stroke, MI, Renal Failure<br />
Components<br />
12.1 13.3 0.91 0.77-1.07 0.24<br />
Death 5.1 5.0 1.03 0.80-1.32<br />
Stroke 1.5 1.7 0.90 0.57-1.41<br />
Non Fatal MI 6.8 7.5 0.90 0.73-1.12<br />
New Renal Failure 1.3 1.3 0.97 0.59-1.60<br />
40
Cumulative Event Rate<br />
0.0 0.05 0.10 0.15 0.20<br />
Death/MI/Stroke/New Renal Failure<br />
at 1 Year<br />
On Pump CABG<br />
Off Pump CABG<br />
HR 0.91<br />
95% CI 0.77-1.07<br />
p value 0.24<br />
0 3 6 9 12<br />
41
CORONARY:<br />
Why No Difference in Stroke<br />
• Surgeons opted to convert CPB patients<br />
to OPCAB when they found a calcified<br />
aorta (102 patients)
Etiology of Stroke in CABG<br />
• AORTIC ATHEROEMBOLISM<br />
• OTHER:<br />
• Intraop hypotension, esp in setting of cerebrovascular disease<br />
• Periop atrial fibrillation causing thromboembolism<br />
• Postoperative hypotension or arrest<br />
• Hemorrhagic stroke, esp associated with hypertension or<br />
cerebral aneurysm (Bad Luck)
Etiology of Aortic Atheroembolism<br />
• AORTIC MANIPULATION:<br />
• Cannulation and De-cannulation<br />
• Clamping<br />
• Un-clamping<br />
• Proximal anastomoses<br />
• Late thromboembolism from aortic intimal<br />
clamp injury<br />
• OTHER:<br />
• Bad luck
How Can We Reduce Aortic<br />
Manipulation<br />
• Limit or eliminate aortic clamping<br />
• On-Pump CABG:<br />
• Single clamp<br />
• No clamp<br />
• OPCAB:<br />
• clampless OPCAB<br />
• All-arterial with BITA inflow<br />
• Clampless aortic proximals
Clampless OPCAB:<br />
State of the Art CABG<br />
Borgermann et al, Circulation 2012; 126:S176-182<br />
• 395 consecutive clampless OPCAB (310 PAS-Port; 85 all-arterial<br />
without proximals)<br />
• Propensity Score matching on 15 preop risk variables to compare<br />
outcomes among 394 pairs of clampless OPCAB vs cCABG:<br />
In-hospital death<br />
Stroke<br />
Death or Stroke<br />
(OR 0.25; 95% CI 0.05-1.18; p=0.08)<br />
(OR 0.36; 95% CI 0.13-0.99; p=0.048)<br />
(OR 0.27; 95% CI 0.11-0.67; p=0.005)<br />
• 2 years F/U: death (OR 0.39; 95% CI 0.19-0.80; p=0.01), death or<br />
stroke (OR 0.58; 95% CI 0.34-1.00; p=0.05)<br />
• MACCE (OR 0.62; 95% CI 0.37-1.02; p=0.06)<br />
• Repeat revascularization (OR 0.74; 95% CI 0.40-1.38; p=0.35)
Aortic No-Touch Technique Makes the<br />
Difference in OPCAB<br />
Emmert et al JTCCVS 2011; 142:1499-506.<br />
• 2004-2009: 4314 patients, OPCAB 2203, cCABG 2111.<br />
• Propensity-adjusted regression, OPCAB vs cCABG:<br />
Composite respir/renal/bleed (OR 0.46; CI 95% 0.35-0.91; p
Aortic No-Touch Technique Makes the<br />
Difference in OPCAB<br />
Emmert et al JTCCVS 2011; 142:1499-506.<br />
• Two OPCAB groups: PC n=567 vs HS n=1365<br />
• Propensity-adjusted regression, HS vs PC:<br />
Stroke<br />
MACCE<br />
(0.7% vs 2.3%; OR 0.39; CI 95% 0.16-0.90; p=0.04)<br />
(6.7% vs 10.8%; OR 0.55; CI 95% 0.38-0.79; p=0.001)<br />
• Stroke rate similar between cCABG and PC OPCAB
OPCAB Can Be Better Than<br />
Conventional CABG on CPB<br />
• Operator dependent procedure<br />
• Different skill set, physically and psychologically<br />
• It matters how you do it!<br />
• Avoid aortic clamping to optimize benefit<br />
• Multiple arterial grafts to optimize longevity<br />
• Not <strong>for</strong> every patient or every surgeon.
Conclusions<br />
• SYNTAX and FREEDOM 5-yr results demonstrate that<br />
CABG is superior to PCI <strong>for</strong> most patients with complex<br />
CAD, especially those with diabetes<br />
• Outcomes with LM PCI in pts with low Syntax score are<br />
favorable and have inspired the EXCEL trial.<br />
• BITA grafting may be the single most effective therapy most<br />
commonly denied patients with CAD<br />
• OPCAB is operator-dependent and benefits high-risk patients<br />
most; clampless OPCAB with multiple arterial grafts
Clampless CABG—How<br />
• All inflow from ITAs (BITA grafting as a<br />
strategy <strong>for</strong> reducing stroke)<br />
• Clampless proximal anastomoses on the<br />
ascending aorta<br />
• Heartstring<br />
• Novare<br />
• PAS-port<br />
• Cyclone
Conclusions<br />
• SYNTAX and FREEDOM 5-yr results demonstrate that<br />
CABG is superior to PCI <strong>for</strong> most patients with complex<br />
CAD, especially those with diabetes, but stroke remains the<br />
Achilles Heal of CABG<br />
• Reducing stroke in CABG should be a high priority<br />
• BITA grafting may be the single most effective therapy most<br />
commonly denied patients with CAD<br />
• OPCAB is operator-dependent and benefits high-risk patients<br />
most; clampless OPCAB with multiple arterial grafts<br />
• Multiple grafting techniques that avoid aortic clamping are<br />
available and should become routine.
Whatever Happened to OPCAB<br />
• To truly exploit the potential benefit of OPCAB<br />
aortic manipulation should be minimized: no<br />
partial clamp<br />
• To optimize long-term benefit of CABG, BITA<br />
and all-arterial grafting should be more<br />
commonly practiced.<br />
• We can and should do better OPCAB!