The Role of the Respiratory Therapist in Organ Donation The ...
The Role of the Respiratory Therapist in Organ Donation The ...
The Role of the Respiratory Therapist in Organ Donation The ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>The</strong> <strong>Role</strong> <strong>of</strong> <strong>the</strong> <strong>Respiratory</strong><br />
<strong>The</strong>rapist <strong>in</strong> <strong>Organ</strong> <strong>Donation</strong><br />
Presented by<br />
Oscar Colon, RN CPTC<br />
In-house Cl<strong>in</strong>ical <strong>Donation</strong> Specialist III<br />
<strong>The</strong> Shar<strong>in</strong>g Network<br />
• Private non-pr<strong>of</strong>it service organization<br />
• Federal designation to provide recovery<br />
services<br />
• State licensed<br />
• Available 24 hours/7 days a week<br />
• Arrange for <strong>the</strong> recovery <strong>of</strong> all organs and<br />
tissues<br />
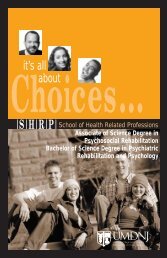
<strong>Organ</strong> Transplant<br />
Wait<strong>in</strong>g Lists<br />
January 2010<br />
105,000Total Wait<strong>in</strong>g <strong>in</strong> U.S.<br />
3,100 Total Wait<strong>in</strong>g In NJ<br />
1
Hospitals<br />
Conditions <strong>of</strong> Participation<br />
1. Refer all deaths to <strong>the</strong><br />
OPO. Referral must be<br />
“timely” and<br />
“imm<strong>in</strong>ent.”<br />
2. Hospitals must<br />
participate with <strong>the</strong>ir<br />
approved OPO <strong>in</strong><br />
Medical Reviews.<br />
3. Only staff tra<strong>in</strong>ed or<br />
employed by an OPO<br />
may <strong>of</strong>fer families <strong>the</strong><br />
options <strong>of</strong> donation<br />
4. All request for donation<br />
must be a collaborative<br />
effort between OPO and<br />
hospital.<br />
5. Develop cooperative<br />
relationships with eye<br />
and tissue banks.<br />
6. <strong>The</strong> OPO must<br />
determ<strong>in</strong>e donor<br />
suitability.<br />
Current Cl<strong>in</strong>ical Triggers:<br />
When to Refer<br />
Imm<strong>in</strong>ent Death Referrals<br />
Regardless <strong>of</strong> age, diagnosis, cause <strong>of</strong> death, sedation or religious beliefs<br />
call on all vented patients<br />
with<strong>in</strong> 1 hour <strong>of</strong> meet<strong>in</strong>g any <strong>of</strong> <strong>the</strong> follow<strong>in</strong>g cl<strong>in</strong>ical triggers:<br />
• Glasgow coma scale (GCS) 5 or less<br />
• Absence <strong>of</strong> 2 or more <strong>of</strong> <strong>the</strong> follow<strong>in</strong>g reflexes:<br />
Cough Reflex<br />
Gag Reflex<br />
Pupillary response to light Corneal Reflex<br />
Response to Pa<strong>in</strong><br />
Loss <strong>of</strong> Respirations<br />
• Call when contemplat<strong>in</strong>g discussions <strong>of</strong> <strong>the</strong> follow<strong>in</strong>g:<br />
Before withdrawal <strong>of</strong> life support, mak<strong>in</strong>g End <strong>of</strong> Life Decisions -<br />
while organs for transplant are still viable<br />
How <strong>the</strong> staff sees us:<br />
2
Incidence <strong>of</strong> Bra<strong>in</strong> Death<br />
• About 75,000 deaths per year <strong>in</strong> N.J.<br />
• 32,000 – 34,000 <strong>of</strong> those deaths <strong>in</strong> hospitals<br />
• Only 275-325 are bra<strong>in</strong> dead and medically<br />
suitable<br />
• That is less than .01% <strong>of</strong> all deaths<br />
<strong>Organ</strong> <strong>Donation</strong><br />
One organ donor can save up to 8 lives<br />
• Heart<br />
• Lungs<br />
• Liver<br />
• Kidneys<br />
• Pancreas<br />
• Small Intest<strong>in</strong>e<br />
Tissue <strong>Donation</strong><br />
(50 or more potential recipients)<br />
• Bone - orthopedic surgeries such as sp<strong>in</strong>al, knee<br />
replacements, hip revisions and dental procedures.<br />
• S<strong>of</strong>t tissue – for sport <strong>in</strong>juries such as Achilles tendon<br />
replacement<br />
• Corneas – restores sight<br />
• Heart valves – used for heart valve replacement<br />
surgery<br />
• Blood vessels – for bypass surgery<br />
• Sk<strong>in</strong> – used for wound and burn graft<strong>in</strong>g<br />
3
Steps <strong>in</strong> <strong>the</strong> <strong>Donation</strong> Process<br />
• 1. Referral<br />
• 2. Evaluation<br />
• 3. Consent<br />
• 4. Ma<strong>in</strong>tenance<br />
• 5. Recovery<br />
• 6. Follow-up<br />
<strong>The</strong> Referral<br />
• Report all deaths –mandated by COP<br />
• Cardiac deaths – Call with<strong>in</strong> 1 hour after <strong>the</strong><br />
patient expires<br />
• Potential organ donor – Call with<strong>in</strong> 1 hour<br />
when <strong>the</strong> patient meets cl<strong>in</strong>ical triggers at or<br />
<strong>in</strong>itiation <strong>of</strong> bra<strong>in</strong> death protocol, Glasgow<br />
Coma Scale <strong>of</strong> 5 or less<br />
<strong>The</strong> Evaluation<br />
• Response –on sight transplant<br />
coord<strong>in</strong>ator<br />
• Donor suitability-lab data, current<br />
status<br />
• Requirements for declaration <strong>of</strong> death<br />
• Medical and social history thru chart<br />
review<br />
4
<strong>The</strong> Consent<br />
• Family assessment-legal NOK and decision<br />
makers<br />
• Decoupl<strong>in</strong>g <strong>in</strong>formation<br />
• Presentation <strong>of</strong> donation options by<br />
“Effective Requestor”<br />
• Legal consent<br />
• Test<strong>in</strong>g -<strong>in</strong>fectious disease screen<strong>in</strong>g<br />
• Medical exam<strong>in</strong>er<br />
Ma<strong>in</strong>tenance<br />
• Ma<strong>in</strong>ta<strong>in</strong> optimal organ function<br />
• Maximize on number <strong>of</strong> recipients<br />
• Ma<strong>in</strong>ta<strong>in</strong> hemodynamic stability<br />
• Adequate oxygenation<br />
<strong>Organ</strong> Shar<strong>in</strong>g<br />
• All recipients listed with UNOS (United<br />
Network for <strong>Organ</strong> Shar<strong>in</strong>g)<br />
• Match run lists from donor <strong>in</strong>formation<br />
• Each organ has separate list<br />
• OPO mandated to share organs by list<br />
• Local centers get greatest priority<br />
5
<strong>The</strong> Recovery<br />
• Use <strong>of</strong> operat<strong>in</strong>g room at donor hospital<br />
• Surgical recovery and preservation <strong>of</strong><br />
organs<br />
• Tissue recovery after organs recovered<br />
• Reconstruction <strong>of</strong> body<br />
• Body released – to medical exam<strong>in</strong>er or<br />
funeral home<br />
Follow up<br />
• Family - provide follow up letter<br />
• Hospital staff - outcomes and appreciation<br />
• Family aftercare support<br />
• Communication - donor family and<br />
recipient(s)<br />
When are you dead<br />
6
New Jersey Legal Def<strong>in</strong>ition<br />
• “An <strong>in</strong>dividual who has susta<strong>in</strong>ed ei<strong>the</strong>r (1)<br />
IRREVERSIBLE cessation <strong>of</strong> circulatory and<br />
respiratory functions, or (2) IRREVERSIBLE<br />
cessation <strong>of</strong> ALL functions <strong>of</strong> <strong>the</strong> bra<strong>in</strong> <strong>in</strong>clud<strong>in</strong>g<br />
<strong>the</strong> bra<strong>in</strong> stem, is dead.<br />
A determ<strong>in</strong>ation <strong>of</strong> death must be made <strong>in</strong><br />
accordance with accepted medical standards.”<br />
State Regulations for Bra<strong>in</strong> Death<br />
• Board <strong>of</strong> Medical Exam<strong>in</strong>ers took law and<br />
passed regulations<br />
• Assure consistent practice<br />
• Create standard <strong>of</strong> care<br />
• Provided level <strong>of</strong> authority to develop new<br />
standards as time progressed<br />
Bra<strong>in</strong> Death: Board Of ME<br />
Appropriate Observation Period<br />
Age<br />
Cause <strong>of</strong> Injury<br />
Cl<strong>in</strong>ical Exams:<br />
M<strong>in</strong>imum<br />
Period <strong>of</strong><br />
Observation<br />
Confirmatory<br />
Test<br />
Any age Any cause One exam only Yes<br />
< 2 months Any cause 48 hours No<br />
2 to 12<br />
months<br />
Any cause 24 hrs No<br />
> 12 months Any cause 6 hrs No<br />
7
Ascerta<strong>in</strong> Irreversibility<br />
• Known etiology<br />
• Rule out <strong>in</strong>toxication<br />
• Rule out abnormal metabolic states<br />
• Rule out pr<strong>of</strong>ound hypo<strong>the</strong>rmia<br />
• Temporal space between exams<br />
Ascerta<strong>in</strong> Totality<br />
• Unresponsiveness GCS <strong>of</strong> 3<br />
• Absence <strong>of</strong> bra<strong>in</strong> stem reflexes<br />
• Apnea<br />
• Acceptance <strong>of</strong> sp<strong>in</strong>al reflexes<br />
• Cerebral Doppler<br />
Confirmatory Tests<br />
• Nuclear Cerebral Blood Flow Study<br />
• Cerebral Vessel Angiography / MRI<br />
8
<strong>The</strong> Apnea Test<br />
• A method to determ<strong>in</strong>e absolute apnea<br />
• Based on a f<strong>in</strong>d<strong>in</strong>g that apnea cannot be<br />
reliably diagnosed unless it occurs <strong>in</strong> a<br />
sett<strong>in</strong>g <strong>of</strong> adequate hypercarbic stimulation<br />
<strong>of</strong> <strong>the</strong> bra<strong>in</strong>stem.<br />
• A PaCO2 <strong>of</strong> 60 mmHG or more is generally<br />
considered adequate hypercarbic<br />
stimulation <strong>of</strong> <strong>the</strong> respiratory centers.<br />
Perform<strong>in</strong>g <strong>the</strong> Apnea Test<br />
• Obta<strong>in</strong> a basel<strong>in</strong>e ABG<br />
• Make necessary ventilator changes to achieve a<br />
PaCO2 <strong>of</strong> 40 mmHG and a pH
Perform<strong>in</strong>g <strong>the</strong> Apnea Test<br />
• If spontaneous breath<strong>in</strong>g does not occur and<br />
patient is hemodynamically stable; after 10<br />
m<strong>in</strong>utes draw an ABG<br />
• If PaCO2 is greater than 60 mmHG or 20<br />
po<strong>in</strong>ts above basel<strong>in</strong>e PaCO2 and <strong>the</strong>re<br />
have been no spontaneous respirations; <strong>the</strong><br />
test is positive and <strong>the</strong> patient is considered<br />
to be apneic<br />
How can you help<br />
• Notify MD/RN <strong>of</strong> changes <strong>in</strong> patients<br />
ventilatory status<br />
• Inquire if <strong>the</strong> referral has been made to<br />
NJSN – If not call us 1800-541-0075<br />
• Please do not mention <strong>Donation</strong>!!!!<br />
• Be an active part <strong>of</strong> <strong>the</strong> healthcare team;<br />
jo<strong>in</strong> <strong>in</strong> our huddles<br />
• Provide aggressive pulmonary support<br />
Someth<strong>in</strong>g to th<strong>in</strong>k about..<br />
• “What’s good for <strong>the</strong> Lungs is<br />
good for <strong>the</strong> Body”<br />
10
How can you help<br />
• Help overcome atelectasis<br />
• Ma<strong>in</strong>ta<strong>in</strong> HOB at 30 degrees<br />
• Turn patient every 2 hours<br />
• Frequent suction<strong>in</strong>g and good mouth care<br />
• Chest PT every 4 hours<br />
• Hyper <strong>in</strong>flate ETT cuff; which reduces aspiration<br />
and protects <strong>the</strong> lungs<br />
• Bronchodilators every 4 hours<br />
• Pulmonary toilet<br />
• Lung Recruitment<br />
Pulmonary Management Goal<br />
is to<br />
Ensure adequate ventilation<br />
• Pressure - Control Ventilation<br />
• TV 10-15ml/kg<br />
• Peep 5-10cm<br />
• ABG’s every 2-3 hours adjust sett<strong>in</strong>gs accord<strong>in</strong>gly to<br />
ma<strong>in</strong>ta<strong>in</strong> optimal parameters<br />
– pH 7.35 -7.45<br />
– PaCO2 35-45<br />
– PaO2 >100<br />
– HCO3 22-26<br />
– O2 Sat 95-100%<br />
• PIP < 30 cm H2O<br />
Requirements for Lung <strong>of</strong>fers<br />
• O 2 Challenge (pO2 > 300mmHg)<br />
• Arterial Blood Gases<br />
• Sputum Culture<br />
• Chest X-rays<br />
• Bronchoscopy<br />
• Lung measurements<br />
• Pulmonary Consult<br />
11
O2 Challenge<br />
• Place patient on 100% FIO2 with 5cm<br />
PEEP for 30 m<strong>in</strong>utes<br />
• After 30 m<strong>in</strong>utes draw an ABG & switch<br />
FIO2 back to orig<strong>in</strong>al sett<strong>in</strong>g<br />
• Lung Transplant Surgeons are look<strong>in</strong>g for<br />
PaO2 >300<br />
What is DCD<br />
• Formerly called Non-Heart-Beat<strong>in</strong>g-<strong>Donation</strong>, <strong>Donation</strong> After<br />
Cardiac Death has been an end-<strong>of</strong>-life option for patients and<br />
families for than 30 years.<br />
• After <strong>the</strong> decision has been made that <strong>the</strong> patient has no chance <strong>of</strong><br />
survival and <strong>the</strong> family has decided to withdraw life support, <strong>the</strong><br />
Shar<strong>in</strong>g Network is contacted and evaluates <strong>the</strong> patient for<br />
medical suitability. If patient is suitable, <strong>the</strong> family is <strong>of</strong>fered <strong>the</strong><br />
option <strong>of</strong> DCD.<br />
• It is <strong>the</strong> recovery <strong>of</strong> organs from those patients who do not meet<br />
<strong>the</strong> criteria <strong>of</strong> bra<strong>in</strong> death. Usually, <strong>the</strong>se patients have suffered a<br />
severe, irreversible bra<strong>in</strong> <strong>in</strong>jury, but reta<strong>in</strong> some bra<strong>in</strong> stem<br />
activity<br />
DCD is Not a New Process……<br />
• Kidney transplants began <strong>in</strong> <strong>the</strong> 1950s<br />
• Early recoveries were from DCD donors<br />
• Bra<strong>in</strong> death criteria established <strong>in</strong> 1960s<br />
• Recent renewed <strong>in</strong>terest <strong>in</strong> DCD-<strong>the</strong> wait<strong>in</strong>g<br />
list is ever grow<strong>in</strong>g!<br />
12
SCORE:<br />
8-12 High Risk for cont<strong>in</strong>u<strong>in</strong>g to brea<strong>the</strong> after extubation<br />
13-18 Moderate Risk for cont<strong>in</strong>u<strong>in</strong>g to brea<strong>the</strong> after extubation<br />
19-24 Low Risk for cont<strong>in</strong>u<strong>in</strong>g to brea<strong>the</strong> after extubation<br />
DCD TOOL<br />
• Prior to <strong>the</strong> test record <strong>the</strong> BP, Pulse, O2 sat<br />
• Disconnect <strong>the</strong> patient from <strong>the</strong> ventilator<br />
• After 5 m<strong>in</strong>utes and 10 m<strong>in</strong>utes record <strong>the</strong><br />
follow<strong>in</strong>g:<br />
– BP, Pulse, O2 sat, respiratory effort (yes or no),<br />
respiratory rate, Tidal volume, NIF<br />
• If patient becomes unstable (O2 sat 40 3<br />
2 – Tidal Volume<br />
Tidal Volume > 200ml 1<br />
Tidal Volume < 200ml 3<br />
3 – Negative Inspiratory Force (NIF)<br />
NIF > -20cmH2O 1<br />
NIF -1 to -20cmH2O 3<br />
****No Spontaneous Respirations automatic 9<br />
5 - BMI<br />
30 3<br />
6 - Vasopressors<br />
No Vasopressors 1<br />
S<strong>in</strong>gle Vasopressor 2<br />
Multiple Vasopressors 3<br />
7 - Patient Age<br />
0-30 1<br />
31-50 2<br />
51 + 3<br />
8 - Intubation<br />
Endotracheal Tube 3<br />
Tracheostomy 1<br />
9 - Oxygenation After 10 M<strong>in</strong>utes<br />
O2 Sat. > 90% 1<br />
O2 Sat. 80-89% 2<br />
O2 Sat. < 79% 3<br />
10- Leak Test: Present Absent Total Score →<br />
Date <strong>of</strong> Extubation:<br />
Date <strong>of</strong> Expiration:<br />
Time <strong>of</strong> Extubation:<br />
Time <strong>of</strong> Expiration:<br />
Total Time:<br />
Formula for Calculat<strong>in</strong>g BMI<br />
BMI = (_________weight <strong>in</strong> pounds__________) X 703<br />
(Height <strong>in</strong> <strong>in</strong>ches) X (Height <strong>in</strong> <strong>in</strong>ches)<br />
13
<strong>Respiratory</strong> <strong>The</strong>rapist’s <strong>Role</strong> <strong>in</strong><br />
<strong>the</strong> OR<br />
Bra<strong>in</strong> Dead – pulmonary management, help transport <strong>the</strong><br />
patient, preferably on a portable vent<br />
- hand <strong>of</strong>f to anes<strong>the</strong>sia<br />
DCD - help transport <strong>the</strong> patient, preferably on a portable<br />
vent<br />
- assist <strong>the</strong> attend<strong>in</strong>g physician and <strong>the</strong><br />
ICU nurse with extubation <strong>in</strong> <strong>the</strong> O.R. as<br />
per standard ICU procedure (suction,<br />
extubate etc.)<br />
Families<br />
give <strong>the</strong> gift<br />
<strong>of</strong> life...<br />
if only we give<br />
<strong>the</strong>m <strong>the</strong><br />
opportunity.<br />
Thank You !!!<br />
Disclaimer<br />
All lecture materials will be posted for 30 days after <strong>the</strong> date <strong>of</strong><br />
<strong>the</strong> conference. <strong>The</strong> material is <strong>in</strong>tended for educational<br />
purposes only, public distribution or use <strong>of</strong> this material is not<br />
allowed without <strong>the</strong> speaker's permission. For more<br />
<strong>in</strong>formation please contact:<br />
http://shrp.umdnj.edu/programs/rspth/UH_conference.htm<br />
Terrence Shenfield<br />
Program Coord<strong>in</strong>ator<br />
shenfite@umdnj.edu<br />
(973) 972-8825<br />
14