Steven Miller: When Injury Happens: Imaging the Newborn Brain ...
Steven Miller: When Injury Happens: Imaging the Newborn Brain ...
Steven Miller: When Injury Happens: Imaging the Newborn Brain ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
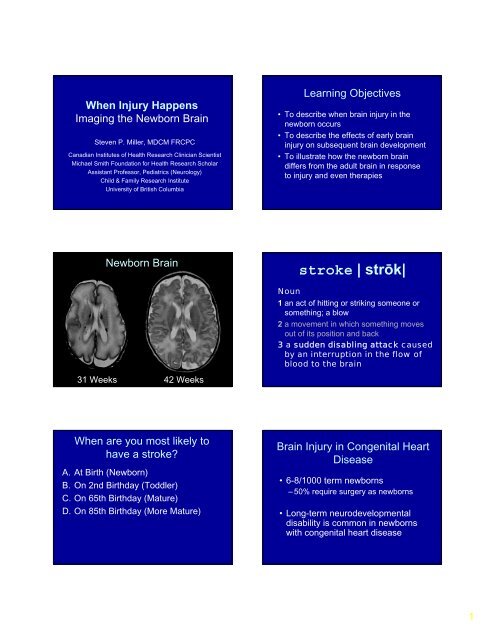
<strong>When</strong> <strong>Injury</strong> <strong>Happens</strong><br />
<strong>Imaging</strong> <strong>the</strong> <strong>Newborn</strong> <strong>Brain</strong><br />
<strong>Steven</strong> P. <strong>Miller</strong>, MDCM FRCPC<br />
Canadian Institutes of Health Research Clinician Scientist<br />
Michael Smith Foundation for Health Research Scholar<br />
Assistant Professor, Pediatrics (Neurology)<br />
Child & Family Research Institute<br />
University of British Columbia<br />
Learning Objectives<br />
• To describe when brain injury in <strong>the</strong><br />
newborn occurs<br />
• To describe <strong>the</strong> effects of early brain<br />
injury on subsequent brain development<br />
• To illustrate how <strong>the</strong> newborn brain<br />
differs from <strong>the</strong> adult brain in response<br />
to injury and even <strong>the</strong>rapies<br />
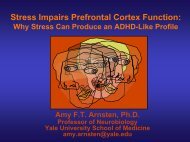
<strong>Newborn</strong> <strong>Brain</strong><br />
stroke | strōk|<br />
Noun<br />
1 an act of hitting or striking someone or<br />
something; a blow<br />
2 a movement in which something moves<br />
out of its position and back<br />
3 a sudden disabling attack caused<br />
by an interruption in <strong>the</strong> flow of<br />
blood to <strong>the</strong> brain<br />
31 Weeks 42 Weeks<br />
<strong>When</strong> are you most likely to<br />
have a stroke<br />
A. At Birth (<strong>Newborn</strong>)<br />
B. On 2nd Birthday (Toddler)<br />
C. On 65th Birthday (Mature)<br />
D. On 85th Birthday (More Mature)<br />
<strong>Brain</strong> <strong>Injury</strong> in Congenital Heart<br />
Disease<br />
• 6-8/1000 term newborns<br />
– 50% require surgery as newborns<br />
• Long-term neurodevelopmental<br />
disability is common in newborns<br />
with congenital heart disease<br />
1
<strong>When</strong> brain injury happens in<br />
newborns with heart disease<br />
<strong>Brain</strong> <strong>Injury</strong> in Congenital Heart<br />
Disease<br />
• Timing Informs Mechanism<br />
• Surprising Patterns of <strong>Brain</strong> <strong>Injury</strong><br />
• Consider <strong>Brain</strong> Development<br />
Bypass<br />
Birth<br />
2000: Neurobehavioral abnormalities in >50% preoperative<br />
Limperopoulos JPediatr (2000) 137<br />
2003-2004: At school age, outcomes of different<br />
bypass strategies (Circulatory Arrest, Low Flow,<br />
Full Flow) not different but whole cohorts below<br />
expectations<br />
Bellinger JTCS(2003)126<br />
Karl JTCS(2004)127<br />
Pre-Operative <strong>Injury</strong>: Stroke<br />
Term<br />
Birth<br />
PreOp<br />
Bypass<br />
PostOp<br />
MRI<br />
MRI<br />
Outcome<br />
McQuillen PS et al. Circulation 2006<br />
2
Pre-operative <strong>Injury</strong><br />
Median (Range) or No <strong>Brain</strong> <strong>Injury</strong> Acquired P<br />
Number (%)<br />
<strong>Brain</strong> <strong>Injury</strong><br />
Number of patients 17 (59%) 12 (41%)<br />
Balloon Atrial 7 (41%) 12 (100%) 0.001<br />
Septostomy<br />
SNAP-PE 14 (9 - 26) 19.5 (9 - 30) 0.1<br />
Lowest O 2 saturation<br />
recorded<br />
70 (26 - 82) 50 (20 - 70) 0.05<br />
Term<br />
Birth<br />
PreOp<br />
MRI<br />
Bypass<br />
PostOp<br />
MRI<br />
Outcome<br />
McQuillen PS et al. Stroke 2007<br />
Perioperative white matter injury is common<br />
WMI Stroke Any<br />
Preoperative<br />
N=62<br />
11 (18%)<br />
13 (21%)<br />
23 (37%)<br />
Postoperative<br />
N=53<br />
Totals<br />
14 (26%)<br />
23 (40%)<br />
5 (9%)<br />
15 (26%)<br />
19 (36%)<br />
32 (56%)<br />
Impaired Global Oxygen Delivery<br />
Median (Range) or Number (%) No Postop New Postop P<br />
<strong>Injury</strong><br />
<strong>Injury</strong><br />
Number of patients 34 19<br />
Preoperative brain injury 13 (38%) 7 (37%) 0.6<br />
Lowest flow ml/kg/min 142 (22 - 229) 85 (17 - 197) 0.05<br />
Bypass Full Flow 26 (76%) 8 (42%)<br />
strategy RCP 2 (6%) 8 (42%)<br />
O<strong>the</strong>r 6 (18%) 3 (16%) 0.01<br />
Postop Day #1 Lowest<br />
MBP<br />
45 (33 - 66) 41 (33 - 63) 0.09<br />
<strong>When</strong> brain injury happens in<br />
newborns with heart disease<br />
• Pre-operative stroke<br />
– Therapeutic ca<strong>the</strong>terization procedures<br />
• Post-operative white matter injury<br />
– Bypass strategy<br />
– Low cardiac output state<br />
• Different modifiable risk factors<br />
3
<strong>Newborn</strong> <strong>Brain</strong><br />
Term<br />
Birth<br />
PreOp<br />
Bypass<br />
PostOp<br />
MRI<br />
MRI<br />
Outcome<br />
31 Weeks 42 Weeks<br />
Normal<br />
Term<br />
Controls<br />
<strong>Miller</strong> SP et al. New England Journal<br />
of Medicine 2007<br />
• 41 <strong>Newborn</strong>s with<br />
CHD<br />
–29 with TGA<br />
– 12 with Single<br />
Ventricle<br />
• 16 Normal Controls<br />
<strong>Newborn</strong>s with 95% CI p-value<br />
CHD relative to<br />
Controls<br />
MRSI<br />
NAA/Choline -10% -15% to -3% 0.003<br />
Lactate/Choline 28% -3% to 68% 0.08<br />
• 3D MRSI<br />
• DTI<br />
–D av<br />
– Fractional<br />
Anisotropy<br />
DTI<br />
Average<br />
Diffusivity<br />
Fractional<br />
Anisotropy<br />
4% 2% to 7%
Opportunities for Intervention<br />
Fractional No Postoperative Preoperative<br />
Anisotropy <strong>Injury</strong> <strong>Injury</strong> <strong>Injury</strong> P<br />
% Increase/week<br />
Median Median<br />
Median<br />
DTT: 4.43 2.44 0.90 0.02*<br />
Ferriero DM NEJM 2006<br />
Neurotoxic Cascade in Hypoxia<br />
Ischemia<br />
Cerebral blood flow<br />
Energy failure<br />
Hypo<strong>the</strong>rmia<br />
Hypo<strong>the</strong>rmia: protects cortex<br />
Glutamate release<br />
Calcium-dependent<br />
‘excitotoxicity’<br />
Apoptotic cell death<br />
Caspase inhibitors<br />
Delayed cell death<br />
Anti-inflammatory agents<br />
NMDA-2nd messenger<br />
modulation<br />
Necrotic cell death<br />
Inflammation<br />
Repair<br />
Restoration<br />
Neurotrophins<br />
Plasticity & Recovery<br />
Stem cells<br />
Normo<strong>the</strong>rmia<br />
Hypo<strong>the</strong>rmia<br />
Inder TE et al. J Pediatr 2004; 145:835-7<br />
Blockade of NMDA Receptor Leads to<br />
Apoptotic Cell Death in Neonatal Rats<br />
• P7 rats<br />
• 3 IP injections of<br />
MK801<br />
• Sacrificed 24 hours<br />
post injection<br />
• Silver stain to detect<br />
apoptotic cells<br />
Conclusions<br />
• Timing informs mechanism<br />
• Surprising patterns of brain injury<br />
• Consider brain development<br />
• <strong>Imaging</strong> important for implementing<br />
brain protection<br />
Ikonomidou, C et. al (1999) Science 283:70-74<br />
5
UBC<br />
Neurology<br />
UCSF<br />
<strong>Steven</strong> <strong>Miller</strong> MD<br />
Vann Chau MD<br />
Wendy Soulikias RN<br />
Vesna Popovska MD<br />
Alan Hill MD PhD<br />
Elke Roland MD<br />
Bruce Bjornson MD<br />
Neonatology<br />
Anne Syness MD<br />
Ruth Grunau PhD<br />
Radiology<br />
Ken Poskitt MD<br />
Michael Sargent MD<br />
PICU/Cardiac Surgery<br />
Andrew Campbell MD<br />
Norbert Froese MD<br />
Neonatal <strong>Brain</strong> Disorders Center<br />
Patrick McQuillen MD<br />
Donna Ferriero MD<br />
A. James Barkovich MD<br />
Shannon Hamrick MD<br />
David V Glidden PhD<br />
MR Science Center<br />
Daniel Vigneron PhD<br />
Pratik Mukherjee MD PhD<br />
Support<br />
CIHR<br />
Michael Smith Foundation<br />
March of Dimes<br />
NIH:NS35902,<br />
RR01271(PCRC)<br />
AHA<br />
Hillblom Foundation<br />
BC Children’s Hospital<br />
Foundation<br />
6