2012 â Acute Lung Injury - Department of Medicine - University of ...
2012 â Acute Lung Injury - Department of Medicine - University of ...
2012 â Acute Lung Injury - Department of Medicine - University of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
The Division <strong>of</strong> Pulmonary,<br />
Allergy, and Critical Care<br />
<strong>Medicine</strong> at UPMC<br />
In This Issue<br />
2 <strong>2012</strong> Pittsburgh International <strong>Lung</strong> Conference<br />
3 The <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong> Center <strong>of</strong> Excellence<br />
4 Severe ARDS Secondary to H1N1 Infection<br />
5 Educational Opportunities<br />
6 <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong> MSC<br />
7 Transfusion-Associated Complications in the ICU<br />
Summer <strong>2012</strong><br />
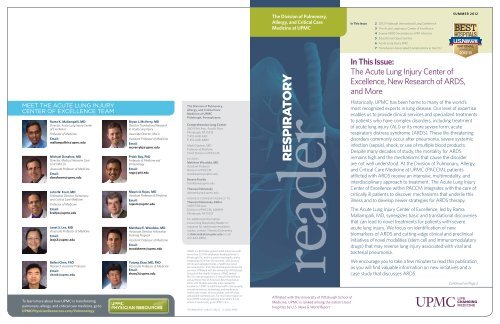
Meet the <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong><br />
Center <strong>of</strong> Excellence Team<br />
Rama K. Mallampalli, MD<br />
Director, <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong> Center<br />
<strong>of</strong> Excellence<br />
Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong><br />
Email:<br />
mallampallirk@upmc.edu<br />
Michael Donahoe, MD<br />
Director, Medical Intensive Care<br />
Unit (MICU)<br />
Associate Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong><br />
Email:<br />
donahoem@upmc.edu<br />
John W. Kreit, MD<br />
Fellowship Director, Pulmonary<br />
and Critical Care <strong>Medicine</strong><br />
Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong><br />
Email:<br />
kreitjw@upmc.edu<br />
Janet S. Lee, MD<br />
Associate Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong><br />
Email:<br />
leejs3@upmc.edu<br />
Beibei Chen, PhD<br />
Research Assistant Pr<strong>of</strong>essor<br />
Email:<br />
chenb@upmc.edu<br />
To learn more about how UPMC is transforming<br />
pulmonary, allergy, and critical care medicine, go to<br />
UPMCPhysicianResources.com/Pulmonology<br />
Bryan J. McVerry, MD<br />
Director, Translational Research<br />
in <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong><br />
Associate Director, MICU<br />
Assistant Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong><br />
Email:<br />
mcverrybj@upmc.edu<br />
Prabir Ray, PhD<br />
Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong> and<br />
Immunology<br />
Email:<br />
rayp@pitt.edu<br />
Mauricio Rojas, MD<br />
Assistant Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong><br />
Email:<br />
rojasm@upmc.edu<br />
Matthew E. Woodske, MD<br />
Associate Director, Fellowship<br />
Training Program<br />
Assistant Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong><br />
Email:<br />
woodskeme@upmc.edu<br />
Yutong Zhao, MD, PhD<br />
Associate Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong><br />
Email:<br />
zhaoy3@upmc.edu<br />
The Division <strong>of</strong> Pulmonary,<br />
Allergy, and Critical Care<br />
<strong>Medicine</strong> at UPMC<br />
Pittsburgh, Pennsylvania<br />
Comprehensive <strong>Lung</strong> Center<br />
3601 Fifth Ave., Fourth Floor<br />
Pittsburgh, PA 15213<br />
T: 412-648-6161<br />
F: 412-648-6869<br />
Mark Gladwin, MD<br />
Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong><br />
Chief, Division <strong>of</strong> PACCM<br />
Editors<br />
Matthew Woodske, MD<br />
Assistant Pr<strong>of</strong>essor<br />
Division <strong>of</strong> PACCM<br />
woodskeme@upmc.edu<br />
Breann Fiorillo<br />
fiorillobm@upmc.edu<br />
Theresa Dobransky<br />
dobranskyta@upmc.edu<br />
Address correspondence to:<br />
Theresa Dobransky, Editor<br />
3459 Fifth Ave.<br />
Division <strong>of</strong> PACCM, 628NW<br />
Pittsburgh, PA 15213<br />
For additional information<br />
concerning Respiratory Reader or<br />
requests for additional newsletter<br />
copies, contact Theresa Dobransky<br />
at dobranskyta@upmc.edu or call<br />
412-624-8856.<br />
UPMC is a $10 billion global health enterprise with<br />
more than 55,000 employees headquartered in<br />
Pittsburgh, Pa., and is transforming health care by<br />
integrating more than 20 hospitals, 400 doctors’<br />
<strong>of</strong>fices and outpatient sites, a health insurance<br />
services division, and international and commercial<br />
services. Affiliated with the <strong>University</strong> <strong>of</strong> Pittsburgh<br />
Schools <strong>of</strong> the Health Sciences, UPMC ranked<br />
No. 10 in the prestigious U.S. News & World Report<br />
annual Honor Roll <strong>of</strong> America’s Best Hospitals in<br />
<strong>2012</strong>, with 15 adult specialty areas ranked for<br />
excellence. UPMC is redefining health care by using<br />
innovative science, technology, and medicine to<br />
invent new models <strong>of</strong> accountable, cost-efficient,<br />
and patient-centered care. For more information on<br />
how UPMC is taking medicine from where it is to<br />
where it needs to be, go to UPMC.com.<br />
TRANS405937 JAB/CS 08/12<br />
© <strong>2012</strong> UPMC<br />
reader<br />
respiratory<br />
Affiliated with the <strong>University</strong> <strong>of</strong> Pittsburgh School <strong>of</strong><br />
<strong>Medicine</strong>, UPMC is ranked among the nation’s best<br />
hospitals by U.S. News & World Report.<br />
In This Issue:<br />
The <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong> Center <strong>of</strong><br />
Excellence, New Research <strong>of</strong> ARDS,<br />
and More<br />
Historically, UPMC has been home to many <strong>of</strong> the world’s<br />
most recognized experts in lung disease. Our level <strong>of</strong> expertise<br />
enables us to provide clinical services and specialized treatments<br />
to patients who have complex disorders, including treatment<br />
<strong>of</strong> acute lung injury (ALI) or its more severe form, acute<br />
respiratory distress syndrome (ARDS). These life-threatening<br />
disorders commonly occur after pneumonia, severe systemic<br />
infection (sepsis), shock, or use <strong>of</strong> multiple blood products.<br />
Despite many decades <strong>of</strong> study, the mortality for ARDS<br />
remains high and the mechanisms that cause the disorder<br />
are not well understood. At the Division <strong>of</strong> Pulmonary, Allergy,<br />
and Critical Care <strong>Medicine</strong> at UPMC (PACCM), patients<br />
afflicted with ARDS receive an intensive, multimodality, and<br />
interdisciplinary approach to treatment. The <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong><br />
Center <strong>of</strong> Excellence within PACCM integrates with the care <strong>of</strong><br />
critically ill patients to discover mechanisms that underlie this<br />
illness and to develop newer strategies for ARDS therapy.<br />
The <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong> Center <strong>of</strong> Excellence, led by Rama<br />
Mallampalli, MD, synergizes basic and translational discoveries<br />
that can lead to novel treatments for patients with severe<br />
acute lung injury. We focus on identification <strong>of</strong> new<br />
biomarkers <strong>of</strong> ARDS and cutting-edge clinical and preclinical<br />
initiatives <strong>of</strong> novel modalities (stem cell and immunomodulatory<br />
drugs) that may reverse lung injury associated with viral and<br />
bacterial pneumonia.<br />
We encourage you to take a few minutes to read this publication,<br />
as you will find valuable information on new initiatives and a<br />
case study that discusses ARDS.<br />
Continued on Page 2
2 Respiratory Reader<br />
Division <strong>of</strong> Pulmonary, Allergy, and Critical Care <strong>Medicine</strong> at UPMC 3<br />
In This Issue: (continued)<br />
As always, for your convenience, we have<br />
included a referral chart <strong>of</strong> our specialists with<br />
contact information.<br />
UPMCPhysicianResources.com <strong>of</strong>fers even<br />
more information on our latest treatments and<br />
techniques for diagnosing and treating those<br />
affected by ARDS. This site houses continuing<br />
medical education programs, case studies,<br />
newsletters, videos, and more.<br />
We welcome any suggestions or comments on<br />
how we might support you in the care <strong>of</strong> your<br />
patients, and we are happy to arrange a consult<br />
or provide more information. Please enjoy this<br />
issue <strong>of</strong> Respiratory Reader.<br />
<strong>2012</strong> Pittsburgh International<br />
<strong>Lung</strong> Conference<br />
<strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong>: New Mechanisms,<br />
Future PITTSBURGH Therapies, and INTERNATIONAL<br />
the Translation<br />
to Clinical LUNG Care CONFERENCE<br />
PERSONALIZED MEDICINE OF LUNG DISEASE<br />
Oct. 5 - Oct. 6, <strong>2012</strong><br />
October 28 – 29, 2011 | Pittsburgh, Pennsylvania<br />
<strong>University</strong> Center, Oakland Campus<br />
The 11th Annual Pittsburgh International <strong>Lung</strong> Conference<br />
will be held Oct. 5 - Oct. 6, <strong>2012</strong>, and will focus on <strong>Acute</strong> <strong>Lung</strong><br />
<strong>Injury</strong>: New Mechanisms, Future Therapies and the Translation<br />
to Clinical Care.<br />
More than 40 worldwide leaders will speak over the course <strong>of</strong><br />
the two-day conference. Day one will focus on clinical features<br />
<strong>of</strong> ARDS, including phenotypes, limitations <strong>of</strong> the consensus<br />
definition, the relationship <strong>of</strong> phenotype to disease outcome, as<br />
well as protocols for clinical management and relevant outcomes<br />
for pre-clinical and clinical studies. Presentations and panel<br />
With great enthusiasm and respect,<br />
Mark T. Gladwin, MD<br />
Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong><br />
Chief, Division <strong>of</strong> Pulmonary,<br />
Allergy, and Critical Care <strong>Medicine</strong><br />
Director, Vascular <strong>Medicine</strong> Institute<br />
Rama K. Mallampalli, MD<br />
Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong><br />
Director, <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong> Center <strong>of</strong><br />
Excellence<br />
discussions will focus on evidence-based practices for the care<br />
<strong>of</strong> patients who are critically ill with ARDS and also sepsis<br />
and pneumonia.<br />
Day two spotlights research into novel mediators <strong>of</strong> acute lung<br />
injury, cell death and cytoprotection, as well as mechanisms <strong>of</strong><br />
stem cell therapy, and the role <strong>of</strong> lung innate immunity. Scientific<br />
discussions will include symposia, panel discussions, and a<br />
scientific poster session highlighting junior investigators in<br />
the field.<br />
The educational sessions will enhance the knowledge <strong>of</strong> attendees<br />
on definitions, diagnosis, and clinical management <strong>of</strong> acute<br />
lung injury; pre-clinical and clinical investigations; and new<br />
discoveries about the basic science behind acute lung injury.<br />
A maximum <strong>of</strong> 14 CME credits will be available for attendees.<br />
For more information, please visit the conference website at<br />
Pittsburgh<strong>Lung</strong>Conference.com.<br />
The <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong> Center <strong>of</strong> Excellence<br />
By Bryan McVerry, MD<br />
Director, Translational Research in <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong><br />
Associate Director, Medical Intensive Care Unit<br />
Associate Fellowship Director for Translational Science<br />
<strong>Acute</strong> lung injury (ALI), and its most severe form, acute respiratory<br />
distress syndrome (ARDS), represent life-threatening complications <strong>of</strong><br />
inflammatory disorders, including sepsis, trauma, pancreatitis, and<br />
pneumonia. ALI causes a significant disease burden, affecting 150,000 to<br />
200,000 people in the United States each year and leading to death in as<br />
many as 35% <strong>of</strong> patients. Because only one large clinical investigation has<br />
demonstrated improved mortality benefit, current and future research is<br />
critically important to advance treatment options for this devastating<br />
syndrome. The <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong> Center <strong>of</strong> Excellence at UPMC aims to<br />
provide state-<strong>of</strong>-the-art treatment to optimize chances <strong>of</strong> survival for<br />
these complex patients, to discover new and promising therapies to<br />
improve survival, to <strong>of</strong>fer comprehensive follow-up, to promote long-term<br />
functional recovery for survivors, and to understand the recovery process.<br />
State-<strong>of</strong>-the-Art Care for Every Patient<br />
At UPMC, we <strong>of</strong>fer the most current therapies for patients with ARDS.<br />
Optimal provision <strong>of</strong> supportive care includes low tidal volume mechanical<br />
ventilation, conservative fluid management, attention to control <strong>of</strong><br />
hyperglycemia, and conservative use <strong>of</strong> blood product transfusions. A<br />
subset <strong>of</strong> patients with ARDS will experience severe and refractory<br />
impairment in their ability to oxygenate the blood, placing them at<br />
significantly increased risk <strong>of</strong> death from the disorder. Several interventions<br />
have been recommended as “rescue” therapies for patients with severe<br />
disease. These so-called rescue therapies include muscle relaxation, inhaled<br />
nitric oxide (iNO), high-frequency oscillatory ventilation (HFOV), prone<br />
positioning, and extracorporeal membrane oxygenation (ECMO). Ideally,<br />
these interventions are provided in specialized centers for the treatment <strong>of</strong><br />
ARDS. Because predicting those who will fare poorly is not possible at the<br />
onset <strong>of</strong> disease, early referral to a tertiary center with expertise delivering<br />
these modalities is essential to optimize the chances <strong>of</strong> survival. At UPMC,<br />
we have extensive experience with provision <strong>of</strong> each <strong>of</strong> these life-sustaining<br />
measures to the appropriate patients.<br />
In recent years, much attention has been dedicated to long-term<br />
functional outcomes <strong>of</strong> survivors <strong>of</strong> critical illness and specifically ARDS.<br />
Physical and psychological debility may persist for years following<br />
hospitalization with ARDS. In accordance with recent literature support,<br />
we have developed and initiated a protocol for reduced sedation and early<br />
mobilization <strong>of</strong> critically ill patients. This has been shown in multiple<br />
studies to improve functionality <strong>of</strong> patients at discharge and to facilitate<br />
their return to normal activity. In addition to our inpatient services, the<br />
UPMC Comprehensive <strong>Lung</strong> Center is staffed with experts who provide<br />
comprehensive, long-term outpatient follow-up to recognize and alleviate<br />
complications from an ICU stay.<br />
Clinical Research and Novel Therapeutics<br />
ALI likely represents a constellation <strong>of</strong> different inflammatory disease<br />
states, thus complicating the design <strong>of</strong> studies and limiting our ability to<br />
interpret and apply data from clinical investigations. At UPMC, we have<br />
developed the <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong> Registry and Biospecimen Repository in<br />
order to better understand the natural history and varying phenotypic<br />
presentation <strong>of</strong> ALI and ARDS. This will help in the development <strong>of</strong><br />
targeted therapeutics in the future and ultimately enable clinicians to<br />
personalize the approach to treatment <strong>of</strong> patients with ALI. Patients who<br />
participate in this registry will help future patients by providing data for<br />
planning and piloting potential therapeutic studies.<br />
In the <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong> Center <strong>of</strong> Excellence, we are involved in<br />
large-scale clinical trials for the treatment <strong>of</strong> ARDS. We previously<br />
recruited subjects for the ARDS Network Fluid and Catheter Treatment<br />
Trial (FACTT), and we are currently enrolling patients in the multi-center<br />
randomized, double-blinded, placebo-controlled Ganciclovir/<br />
Valganciclovir for Prevention <strong>of</strong> Cytomegalovirus Reactivation in <strong>Acute</strong><br />
<strong>Injury</strong> <strong>of</strong> the <strong>Lung</strong> (GRAIL) study. In addition to clinical trials, we are<br />
developing partnerships with industry and designing pilot therapeutic and<br />
observational studies to take bench-top science to the bedside.<br />
Cutting-Edge Translational Research<br />
At the <strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong> Center <strong>of</strong> Excellence, we have an experienced<br />
team <strong>of</strong> scientists exploring the mechanisms <strong>of</strong> disease at the bench in<br />
search <strong>of</strong> novel therapeutic targets and strategies for future translation to<br />
the bedside. Our investigators are well-funded by the National Institutes <strong>of</strong><br />
Health and represent leaders in the fields <strong>of</strong> lipid biology, alveolar barrier<br />
regulation, pulmonary vascular physiology, and inflammation. This<br />
provides a unique and collaborative approach to mechanistic exploration<br />
at the bench and translation to the bedside.<br />
With advances in critical care medicine and refinements in supportive care<br />
modalities, survival from acute lung injury has been improving, but it<br />
remains a significant public health problem and cause <strong>of</strong> death. However,<br />
targeted treatments for this complex disorder remain elusive. This is in part<br />
due to incomplete understanding <strong>of</strong> disease phenotypes and<br />
pathophysiology. At UPMC, we are uniquely positioned to provide<br />
state-<strong>of</strong>-the-art clinical care and access to clinical and preclinical trials, and<br />
to mold future therapeutics through progressive translational research.<br />
Affiliated with the <strong>University</strong> <strong>of</strong> Pittsburgh School <strong>of</strong> <strong>Medicine</strong>, UPMC is ranked among the nation’s best hospitals by U.S. News & World Report. www.dept-med.pitt.edu/PACCM Consults and referrals: Please call the UPMC Comprehensive <strong>Lung</strong> Center at 412-648-6161.
4 Respiratory Reader<br />
Division <strong>of</strong> Pulmonary, Allergy, and Critical Care <strong>Medicine</strong> at UPMC 5<br />
Case Presentation:<br />
Severe ARDS Secondary to H1N1 Infection<br />
By Matthew Synan, MD<br />
Fellow<br />
Pulmonary, Allergy, and Critical Care <strong>Medicine</strong><br />
A 45-year-old obese female with an unsubstantiated diagnosis <strong>of</strong> chronic<br />
obstructive pulmonary disease (COPD) initially presented to the<br />
emergency department (ED) for worsening dyspnea in December 2009.<br />
She had been seen in the ED one week prior for similar respiratory<br />
symptoms (cough and dyspnea) and had completed a course <strong>of</strong><br />
antibiotics, inhaled bronchodilators, and oral corticosteroids with marginal<br />
improvement. She then developed a high fever and worsening dyspnea<br />
and thus returned to the ED. Chest x-ray on the second presentation<br />
revealed new bilateral multifocal infiltrates consistent with pneumonia.<br />
She was admitted and antibiotics were initiated with ceftriaxone and<br />
azithromycin. Over the following two days, she appeared to improve,<br />
however she developed a high-grade fever on day three accompanied by<br />
worsening dyspnea. After consultation with infectious disease specialists,<br />
antibiotics were changed to vancomycin and piperacillin/tazobactam.<br />
Unfortunately she deteriorated further, requiring intubation for hypoxemic<br />
respiratory failure. She was then transferred to UPMC Presbyterian.<br />
Upon arrival to the hospital, she was found to have significant hypoxemia<br />
and bilateral infiltrates on chest x-ray (Figure A), consistent with acute<br />
respiratory distress syndrome (ARDS). There was no evidence <strong>of</strong> heart<br />
failure on exam or by echocardiogram. She was placed on low tidal volume<br />
ventilation with high levels <strong>of</strong> PEEP to maintain oxygenation. Soon after<br />
transfer, her outside hospital cultures returned positive for influenza,<br />
subtype H1N1. She was continued on antibiotics and started on peramivir<br />
(an investigational intravenous neuraminidase inhibitor with anti-H1N1<br />
activity) immediately. Within 24 hours, her oxygenation worsened while<br />
on maximum ventilatory settings, and thus she was commenced on prone<br />
positioning, heavy sedation, and paralytics. She continued to have<br />
desaturations despite this, thus the decision was made to place the patient<br />
on venovenous extracorporeal membrane oxygenation (VV-ECMO). She<br />
remained on VV-ECMO for nine days while her ARDS improved. She was<br />
able to be extubated three days after ECMO decannulation and 17 days<br />
after initial intubation.<br />
Table 1<br />
By Matthew Woodske, MD<br />
Assistant Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong><br />
After a short rehabilitation stay for very mild deconditioning and mild<br />
critical illness polymyopathy, the patient was discharged home. She has<br />
been followed in the UPMC Comprehensive <strong>Lung</strong> Center for more than a<br />
year. Her pulmonary function testing and CXR (Figure B) have now<br />
returned to normal (Table 1).<br />
ARDS is a common clinical entity which is associated with a high<br />
mortality. ARDS and ALI are clinical syndromes defined by non-specific<br />
clinical features including: (1) severe hypoxemia (PaO2/FiO2 ratio<br />
6 Respiratory Reader<br />
Division <strong>of</strong> Pulmonary, Allergy, and Critical Care <strong>Medicine</strong> at UPMC 7<br />
<strong>Acute</strong> <strong>Lung</strong> <strong>Injury</strong> MSC<br />
Transfusion-Associated Complications in the ICU<br />
By Mauricio Rojas, MD<br />
Assistant Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong><br />
By Janet Lee, MD<br />
Associate Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong><br />
ARDS is a condition in which the lungs sustain severe widespread injury,<br />
interfering with their ability to take up oxygen. The pathologic hallmark <strong>of</strong><br />
ARDS is tissue injury to one or both sides <strong>of</strong> the alveolar-capillary<br />
interface, including the endothelial cells and the airway epithelium. For<br />
example, sepsis may cause injury to the vascular endothelium, while<br />
gastric aspiration or pneumonia may cause injury to the epithelial alveolar<br />
lining. However, both injuries lead to a final common pathway in early<br />
ARDS: markedly increased alveolar-capillary permeability leading to an<br />
influx <strong>of</strong> protein rich fluid into the alveoli and hypoxemia.<br />
When lung injury does occur, the effectiveness <strong>of</strong> the repair response is<br />
dependent on many factors. Emerging evidence suggests that endogenous<br />
stem cells may play a role in the repair process in ARDS. In addition, recent<br />
studies suggest that intravenously infused exogenous mesenchymal stem<br />
cells can potentially mitigate lung injury and induce repair. Conversely,<br />
abnormalities in stem cell repair processes may explain susceptibility to<br />
ARDS. For example, aged patients are increasingly susceptible to the<br />
development <strong>of</strong> ARDS, and advancing age has been associated with<br />
abnormal recruitment <strong>of</strong> stem cells to the lung in particular.<br />
Bone-marrow derived stem cells can be divided in two groups:<br />
hematopoietic stem cells (HSC) and mesenchymal stem cells (B-MSC).<br />
B-MSCs were first described in the early 1970s as clonal, plastic adherent<br />
cells capable <strong>of</strong> differentiating into several cell types. Recently it has been<br />
demonstrated that B-MSC can transform into cells representing all three<br />
embryological layers: endoderm, mesoderm, and ectoderm. These cells<br />
also support hematopoiesis providing extracellular matrix, cytokines, and<br />
growth factors to the HSC. The ability <strong>of</strong> B-MSC to create a tolerogenic<br />
niche by direct interaction with immune cells and by secretion <strong>of</strong><br />
regulatory molecules makes them attractive therapeutic candidates in the<br />
regulation <strong>of</strong> the inflammatory response to infection and injury.<br />
Publications from our group have demonstrated compelling benefits from<br />
the administration <strong>of</strong> B-MSC in animal models <strong>of</strong> lung injury. In a mouse<br />
model <strong>of</strong> ALI, initiated by the administration <strong>of</strong> bacterial endotoxin,<br />
infusion <strong>of</strong> mouse-derived B-MSC prevents the systemic inflammatory<br />
response, attenuates lung injury, and protects against pulmonary edema, a<br />
hallmark <strong>of</strong> ALI. Histological examination <strong>of</strong> lung sections demonstrated<br />
that B-MSC infusion completely attenuated neutrophil infiltration and<br />
B-MSC infusion also decreased the plasma levels <strong>of</strong> pro-inflammatory<br />
cytokines after endotoxin, further supporting a protective role in ALI.<br />
Since stem cells suppress inflammation in the mouse model by regulating<br />
the immune response, we expanded our observations to study humanderived<br />
B-MSC. Traditional methods <strong>of</strong> stem cell extraction and<br />
proliferation have used a bone marrow aspirate from a live donor as the<br />
main source <strong>of</strong> cells from which MSCs are purified. Because <strong>of</strong> the low<br />
number <strong>of</strong> cells that are recovered from the biological sample, extensive<br />
manipulation <strong>of</strong> recovered cells must be performed in order to obtain a<br />
large enough sample for use. These limitations are an important obstacle<br />
to translate B-MSCs into clinical applications as they may result in<br />
chromosomal abnormalities and cellular dysfunction.<br />
To overcome these limitations, Albert Donnenberg, from the <strong>University</strong> <strong>of</strong><br />
Pittsburgh, created a unique protocol to isolate and expand human MSCs.<br />
Demonstrating the therapeutic effect <strong>of</strong> these cells, we inoculated our<br />
mouse ALI/ARDS model with human B-MSCs and demonstarted<br />
decreased pulmonary edema and inflammation, similar to prior observations<br />
with mouse derived-stem cells.<br />
These and other experimental data support using B-MSC-based therapy<br />
to mitigate or reverse the deadly consequences <strong>of</strong> ALI and ARDS. This<br />
type <strong>of</strong> novel therapeutic strategy may have far-reaching implications<br />
for the future treatment <strong>of</strong> ARDS and other inflammatory conditions,<br />
including acute myocardial infartion, graft versus host disease, and<br />
Crohn’s disease. Phase I and II clinical trials have provided important<br />
evidence that B-MSCs are well tolerated and elicit no increased incidence<br />
<strong>of</strong> acute side effects when compared to placebo. We hope to advance the<br />
therapeutic niche <strong>of</strong> B-MSC to include ARDS in the near future.<br />
Often in discussing transfusion-associated complications in the intensive<br />
care setting, we focus upon transfusion-related acute lung injury (TRALI).<br />
But, what is TRALI TRALI is defined as acute lung injury <strong>of</strong> new onset<br />
with symptoms during or within six hours <strong>of</strong> transfusion <strong>of</strong> blood<br />
products[1]. The acute lung injury cannot be attributed to other wellestablished<br />
risk factors for acute lung injury (ALI), such as pneumonia,<br />
aspiration, pancreatitis, or sepsis. Although this definition appears<br />
straight-forward, its application can be challenging in some real-life<br />
situations, particularly in the ICU. For example, in cases where a major risk<br />
factor for ALI is concurrent but transfusion precipitates onset <strong>of</strong><br />
symptoms within the pre-defined time frame, the event is referred to as<br />
“possible” TRALI[1,2]. In addition, transfusion-associated cardiac overload<br />
(TACO) can present similarly, but the definition is applied to cases where<br />
left atrial hypertension is the primary explanation for acute pulmonary<br />
edema in the setting <strong>of</strong> transfusion[3].<br />
From 2005 to 2010, TRALI accounted for the highest number <strong>of</strong><br />
transfusion-related fatalities reported to the U.S. Food and Drug<br />
Administration[4]. In addition, TACO has received increasing recognition,<br />
possibly accounting for increased reporting <strong>of</strong> TACO-related fatalities<br />
between 2005 and 2010. TRALI is uncommon, but is more frequently<br />
observed with plasma containing blood components, such as fresh, frozen<br />
plasma (FFP) or whole blood-derived platelet products, although packed<br />
red blood cell (PRBC) transfusion can certainly promote TRALI.<br />
The mechanism <strong>of</strong> injury is not completely understood, but most experts<br />
would agree that TRALI requires two hits: (1) a susceptible recipient with<br />
1. Kleinman S, Caulfield T, Chan P, Davenport R, McFarland J, McPhedran S,<br />
Meade M, Morrison D, Pinsent T, Robillard P, Slinger P: Toward an understanding<br />
<strong>of</strong> transfusion-related acute lung injury: Statement <strong>of</strong> a consensus panel.<br />
Transfusion 2004;44:1774-1789.<br />
2. Shaz BH, Stowell SR, Hillyer CD: Transfusion-related acute lung injury:<br />
From bedside to bench and back. Blood 2011;117:1463-1471.<br />
3. Toy P, Gajic O, Bacchetti P, Looney MR, Gropper MA, Hubmayr R, Lowell CA,<br />
Norris PJ, Murphy EL, Weiskopf RB, Wilson G, Koenigsberg M, Lee D, Schuller R,<br />
Wu P, Grimes B, Gandhi MJ, Winters JL, Mair D, Hirschler N, Sanchez Rosen R,<br />
Matthay MA: Transfusion-related acute lung injury: Incidence and risk factors.<br />
Blood <strong>2012</strong>;119:1757-1767.<br />
primed neutrophils and (2) transfusion <strong>of</strong> biologic response modifiers that<br />
activates the recipient’s primed neutrophils[5]. In the majority <strong>of</strong> cases,<br />
the biologic response modifier that is identified is human leukocyte<br />
antigen (HLA) Class II antibody or human neutrophil antigen (HNA)<br />
antibody. Consistent with this observation, recent data suggest that<br />
donor-based TRALI mitigation strategies widely adopted in the U.S. since<br />
2009, such as supply <strong>of</strong> plasma from primarily male or never-pregnant<br />
female donors, appear to be reducing the risk <strong>of</strong> TRALI[5].<br />
While transfusion risk factors have been widely studied, recipient risk<br />
factors are now being increasingly recognized, and these include positive<br />
fluid balance prior to transfusion, shock prior to transfusion, current<br />
cigarette smoking, chronic alcohol abuse, liver surgery, high-peak<br />
pressures if mechanically ventilated, and higher plasma IL-8<br />
concentrations[5].<br />
If there is concern that a patient is having a transfusion reaction, such as<br />
TRALI or TACO, the transfusion must be stopped immediately and<br />
supportive measures, such as oxygen therapy, be given in an intensive<br />
care setting. Reporting the event to the local blood center is necessary so<br />
that a full assessment can be performed, if possible, to determine the<br />
cause. In challenging cases where TRALI is suspected, acute lung injury is<br />
severe or likely to be protracted, and early referral to UPMC Presbyterian is<br />
recommended for further evaluation and management. In one referral in<br />
which transfusion was suspected to be a contributing factor, acute<br />
exacerbation <strong>of</strong> subclinical pulmonary fibrosis was diagnosed[6].<br />
4. U.S. Food and Drug Administration: Fatalities reported to fda following<br />
blood collection and transfusion: Annual summary for fiscal year 2010.<br />
http://wwwfdagov/biologicsbloodvaccines. Accessed Feb 21, <strong>2012</strong>.<br />
5. Kleinman SH, Triulzi DJ, Murphy EL, Carey PM, Gottschall JL, Roback JD,<br />
Carrick D, Mathew S, Wright DJ, Cable R, Ness P, Gajic O, Hubmayr RD,<br />
Looney MR, Kakaiya RM: The leukocyte antibody prevalence study-ii (laps-ii):<br />
A retrospective cohort study <strong>of</strong> transfusion-related acute lung injury in recipients<br />
<strong>of</strong> high-plasma-volume human leukocyte antigen antibody-positive or -negative<br />
components. Transfusion 2011;51:2078-2091.<br />
6. Woodske M, Donahoe MP, Yazer M, Lee JS: <strong>Acute</strong> exacerbation <strong>of</strong> subclinical<br />
pulmonary fibrosis after red blood cell transfusion: A case report. Transfusion.<br />
2011 Aug 9. doi: 10.1111/j.1537-2995.2011.03296.x.<br />
Affiliated with the <strong>University</strong> <strong>of</strong> Pittsburgh School <strong>of</strong> <strong>Medicine</strong>, UPMC is ranked among the nation’s best hospitals by U.S. News & World Report. www.dept-med.pitt.edu/PACCM Consults and referrals: Please call the UPMC Comprehensive <strong>Lung</strong> Center at 412-648-6161.