BPSD - Devon Partnership NHS Trust
BPSD - Devon Partnership NHS Trust
BPSD - Devon Partnership NHS Trust
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
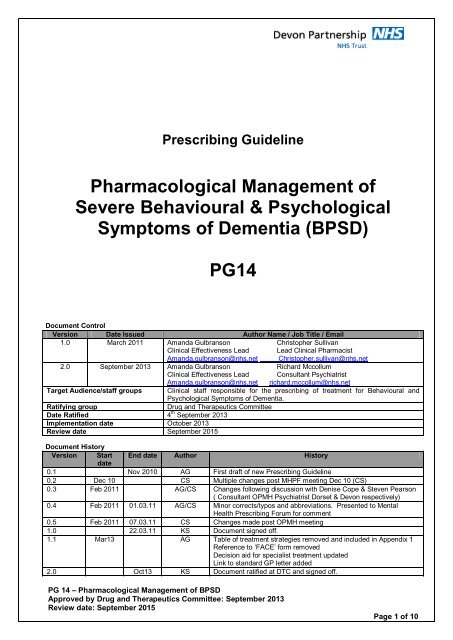
Prescribing Guideline<br />
Pharmacological Management of<br />
Severe Behavioural & Psychological<br />
Symptoms of Dementia (<strong>BPSD</strong>)<br />
PG14<br />
Document Control<br />
Version Date Issued Author Name / Job Title / Email<br />
1.0 March 2011 Amanda Gulbranson Christopher Sullivan<br />
Clinical Effectiveness Lead Lead Clinical Pharmacist<br />
Amanda.gulbranson@nhs.net Christopher.sullivan@nhs.net<br />
2.0 September 2013 Amanda Gulbranson Richard Mccollum<br />
Clinical Effectiveness Lead Consultant Psychiatrist<br />
Amanda.gulbranson@nhs.net richard.mccollum@nhs.net<br />
Target Audience/staff groups Clinical staff responsible for the prescribing of treatment for Behavioural and<br />
Psychological Symptoms of Dementia.<br />
Ratifying group<br />
Drug and Therapeutics Committee<br />
Date Ratified 4 th September 2013<br />
Implementation date October 2013<br />
Review date September 2015<br />
Document History<br />
Version Start End date Author History<br />
date<br />
0.1 Nov 2010 AG First draft of new Prescribing Guideline<br />
0.2 Dec 10 CS Multiple changes post MHPF meeting Dec 10 (CS)<br />
0.3 Feb 2011 AG/CS Changes following discussion with Denise Cope & Steven Pearson<br />
( Consultant OPMH Psychiatrist Dorset & <strong>Devon</strong> respectively)<br />
0.4 Feb 2011 01.03.11 AG/CS Minor corrects/typos and abbreviations. Presented to Mental<br />
Health Prescribing Forum for comment<br />
0.5 Feb 2011 07.03.11 CS Changes made post OPMH meeting<br />
1.0 22.03.11 KS Document signed off.<br />
1.1 Mar13 AG Table of treatment strategies removed and included in Appendix 1<br />
Reference to ‘FACE’ form removed<br />
Decision aid for specialist treatment updated<br />
Link to standard GP letter added<br />
2.0 Oct13 KS Document ratified at DTC and signed off.<br />
PG 14 – Pharmacological Management of <strong>BPSD</strong><br />
Approved by Drug and Therapeutics Committee: September 2013<br />
Review date: September 2015<br />
Page 1 of 10
Pharmacological Management of Severe Behavioural & Psychological<br />
Symptoms of Dementia (<strong>BPSD</strong>)<br />
The aim of these guidelines is to promote evidence based, cost effective prescribing and<br />
support adherence to:<br />
o NICE Clinical Guideline CG42: Dementia (Nov 2006)<br />
o The use of antipsychotic medication for people with dementia: Time for action.<br />
(Banerjee 2009: Department of Health)<br />
o NICE Quality Standard QS01: Dementia (June 2010)<br />
o Alzheimer’s Society (2011): Optimising treatment and care for people with<br />
behavioural and psychological symptoms of dementia- A best practice guide for<br />
health and social care professionals<br />
The guidelines are NOT intended to replace prescribing information contained in the BNF or<br />
Summary of Product Characteristics.<br />
Treatment choice and duration<br />
Behavioural and psychological symptoms occur in about 90% of individuals with dementia,<br />
(frequency increases with severity of dementia), causing considerable distress and/or risk of harm<br />
to the individual, increasing distress to the family/carer and potentially interfering with/preventing<br />
the provision of required care.<br />
The presenting neuropsychiatric symptoms include psychosis, agitation, aggression, mood<br />
disorder and wandering and are collectively referred to as ‘behavioural and psychological<br />
symptoms of dementia’ (<strong>BPSD</strong>).<br />
For people with a diagnosis of dementia, behaviours that challenge are best ‘managed’ by good<br />
nursing care, the correct environment and use of ‘ABC’ (antecedents, behaviours and<br />
consequences) to try and identify causes and possible triggers for the presenting behaviour (e.g.<br />
hunger, pain).<br />
Non-pharmacological approaches must always be considered first<br />
(but are beyond the scope of, and not covered in, this guideline)<br />
Pharmacological treatment is not a substitute for non-pharmacological approaches and these<br />
techniques must always be used concurrently.<br />
Where non-pharmacological interventions have failed or are inappropriate, other possible causes<br />
(i.e. physical illness) should be eliminated prior to considering an individual trial of medication for<br />
the management of <strong>BPSD</strong> using the Pharmacological Treatment Algorithm below.<br />
PG 14 – Pharmacological Management of <strong>BPSD</strong><br />
Approved by Drug and Therapeutics Committee: September 2013<br />
Review date: September 2015<br />
Page 2 of 10
No further intervention needed at this time. Continue to provide care for individual in accordance<br />
with current care-plan<br />
Individual presents with behaviours that challenge (e.g. agitation, wandering, aggression, tearfulness,<br />
sexual disinhibition shouting, hallucinations, delirium)<br />
Identify and document target symptoms, severity and level of distress caused to individual<br />
(Use suitable assessment tool i.e. Cohen–Mansfield Scale or Neuropsychiatric Inventory )<br />
Could presenting<br />
symptoms be a<br />
result of underlying<br />
physical cause<br />
(including pain)<br />
YES<br />
Assess,<br />
diagnose and<br />
provide<br />
appropriate<br />
treatment<br />
Symptoms<br />
resolved<br />
NO<br />
YES<br />
NO<br />
Could<br />
presenting<br />
symptoms be sideeffects<br />
of<br />
concurrently<br />
prescribed<br />
medication<br />
YES<br />
Complete a<br />
medication<br />
review and<br />
rationalise<br />
treatment<br />
Symptoms<br />
resolved<br />
YES<br />
NO<br />
NO<br />
Could presenting<br />
symptoms be<br />
caused by<br />
underlying<br />
depressive illness<br />
and/ or anxiety<br />
disorder<br />
YES<br />
Assess, diagnose<br />
and provide<br />
appropriate<br />
treatment (refer to<br />
local prescribing<br />
guidelines)<br />
Symptoms<br />
resolved<br />
YES<br />
NO<br />
NO<br />
Consider and implement<br />
appropriate nonpharmacological<br />
interventions<br />
(e.g. environmental changes,<br />
psychological therapies,<br />
multisensory stimulation,<br />
massage, aromatherapy)<br />
Symptoms<br />
resolved<br />
YES<br />
Consider, discuss and provide<br />
appropriate pharmacotherapy<br />
in accordance with this<br />
prescribing guidance (PG14)<br />
NO<br />
Symptoms<br />
resolved<br />
NO<br />
YES<br />
Review prescribed<br />
medication regularly. After a<br />
period of 3 months, aim to<br />
reduce and stop medication<br />
when presenting behaviour<br />
has settled.<br />
Advise GP of plan to reduce<br />
and stop medication if still<br />
prescribed medication (after<br />
a trial of reduction) on<br />
discharge from in-patient<br />
unit or community team<br />
Where a medication has been ineffective, always stop it before introducing a subsequent treatment<br />
PG 14 – Pharmacological Management of <strong>BPSD</strong><br />
Approved by Drug and Therapeutics Committee: September 2013<br />
Review date: September 2015<br />
Page 3 of 10
Pharmacological Management:<br />
The expected benefits must outweigh the potential risks/side effects of medication for each individual.<br />
Pharmacological management of severe <strong>BPSD</strong> (agitation and aggression in particular) should only be<br />
considered if behaviours cause severe distress to the individual and/or there is immediate risk of<br />
harm to other patients or carers. Remember- wandering behaviour does NOT respond to medication.<br />
Medication prescribed for the management of <strong>BPSD</strong> should be considered as an individual<br />
therapeutic trail, with the choice of medication based upon an individual risk-benefit analysis.<br />
Always “START LOW AND GO VERY SLOW”.<br />
Treatment choice and duration:<br />
Once a decision has been reached to start medication for the management of <strong>BPSD</strong> the first choice<br />
of treatment considered should be;<br />
Risperidone<br />
Initial dose of 250micrograms twice a day recommended.<br />
This may be increased according to response in steps of 250micrograms twice a day on alternate<br />
days. Usual dose 500micrograms twice a day (but doses up to 1mg twice a day may be beneficial<br />
for some individuals).<br />
Risperidone is the only medication with UK Marketing authorisation for this indication, licensed for<br />
“the short-term treatment (up to 6 weeks) of persistent aggression in patients with moderate to<br />
severe Alzheimer's dementia unresponsive to non-pharmacological approaches and when there is<br />
a risk of harm to self or others”.<br />
Antipsychotic drugs are known to be harmful and can have severe side-effects and it is vital that<br />
any person prescribed risperidone (or other antipsychotic) is monitored for side-effects and<br />
progression of symptoms.<br />
Exercise caution if risperidone is prescribed together with furosemide (higher incident of mortality<br />
observed although mechanism unclear). The risks and benefits of combining risperidone with<br />
furosemide or other potent diuretics must be considered prior to use. Refer to Risperidone SPC for<br />
more information.<br />
The most important adverse effects associated with antipsychotics are parkinsonism, falls,<br />
dehydration, chest infections, ankle oedema, deep vein thrombosis/pulmonary embolism, cardiac<br />
arrhythmia and stroke (highest risk in first four weeks of treatment). Antipsychotics are also<br />
associated with increased mortality in the long term (often related to pneumonia and thromboembolic<br />
events) which can be caused by over-sedation and dehydration.<br />
Complete a cardiac risk assessment prior to initiating treatment.<br />
Weekly monitoring of sedation, fluid intake and early indicators of chest infection is strongly<br />
recommended.<br />
Caution: antipsychotics should not be used in someone with Lewy Body Dementia (LBD)<br />
Where<br />
without<br />
risperidone<br />
specialist<br />
is contraindicated<br />
advice.<br />
or where no clinical benefit is achieved and/or the individual<br />
experiences intolerable side effects, it may be appropriate to consider alternative pharmacological<br />
treatment options (to be initiated by or on the recommendation of a specialist).<br />
The available evidence base is insufficient to support specific recommendations on preferred<br />
choices of medication or the order in which different medicines/different classes of medication<br />
should be prescribed.<br />
Refer to the Decision aid for specialist treatment strategies-Severe <strong>BPSD</strong> (Appendix 1)<br />
PG 14 – Pharmacological Management of <strong>BPSD</strong><br />
Approved by Drug and Therapeutics Committee: September 2013<br />
Review date: September 2015<br />
Page 4 of 10
Initiation of medication (by, or on the recommendation from, a specialist):<br />
Identify, quantify & document target symptoms including severity and level of distress caused<br />
to the individual (and family/carers where appropriate) and set realistic treatment goals.<br />
Suitable assessment tools include Adapted Cohen –Mansfield Agitation Inventory (Adapted<br />
CMAI) or Neuropsychiatric Inventory (NPI).<br />
The Adapted Cohen–Mansfield Agitation Inventory is available here<br />
Document which non-pharmacological interventions have been used and/or offered to the<br />
individual (as appropriate) and level of effectiveness.<br />
Complete baseline physical monitoring, appropriate to the individual drug prescribed.<br />
Complete baseline assessment of cognition.<br />
Clearly record rationale for treatment and choice of medication in the clinical notes, including<br />
agreed start date and initial treatment review date (& person responsible for completion).<br />
It is recognised that when medication is prescribed for the management of <strong>BPSD</strong> it will<br />
generally arise from a ‘best interest decision’. The prescriber must ensure that a formal record<br />
of capacity assessment is completed (using RiO capacity assessment form) and a summary<br />
of multi-professional team discussion and rationale for treatment clearly documents in the<br />
notes (including information provided to family and/or carers where applicable).<br />
Communication of information to family/carers:<br />
The prescriber must discuss the possible treatment options with the individual and/or<br />
family/carers, including the anticipated benefits and potential risks of treatment (in particular,<br />
cerebrovascular risk factors should be assessed and the possible increased risk of<br />
stroke/transient ischaemic attack and possible adverse effects on cognition discussed).<br />
Provide information in an appropriate format to support discussion about expected benefits<br />
and possible risks of treatment (see user-friendly resources).<br />
A summary of the discussion (and note of any additional information provided) must be clearly<br />
documented in the clinical notes.<br />
During treatment:<br />
Regularly monitor response to treatment/changes in target symptoms & document in notes<br />
Assess cognition at regular intervals, and document any required action(s)/treatment plan to<br />
address any deterioration in cognition in the notes<br />
Monitor for emergence of side effects associated with mediation. Discuss with individual<br />
and/or carer and review treatment if side effects intolerable or severe. (NB people with DLB<br />
have increased sensitivity to antipsychotic side effects, including acute & severe physical<br />
deterioration- monitor carefully).<br />
Ensure on-going physical monitoring is carried out appropriate to the medication prescribed.<br />
Document subsequent treatment review dates (& person responsible) in the clinical notes at<br />
each clinical review. Treatment should be time-limited and regularly reviewed.<br />
Reviewing and stopping treatment:<br />
Treatment should be reviewed at 6 and/or twelve weeks (with more frequent review<br />
considered according to clinical need).<br />
Following review, unless there is severe risk or extreme distress, the recommended default<br />
management is to discontinue antipsychotic medication.<br />
When stopping medication, if the daily dose of risperidone is 500micrograms or less<br />
immediate discontinuation is recommended. For higher doses a gradual reduction is<br />
preferable to abrupt withdrawal, i.e. reduce dose by 50% of total daily dose every 1-2 weeks<br />
until dose of 500micrograms or less/day reached, then stop minimum dose after 1-2 weeks.<br />
PG 14 – Pharmacological Management of <strong>BPSD</strong><br />
Approved by Drug and Therapeutics Committee: September 2013<br />
Review date: September 2015<br />
Page 5 of 10
Acute management in an emergency situation:<br />
For individuals, receiving treatment on an in-patient ward only, where physically violent and<br />
aggressive behaviour has or may imminently result in harm to the individual and/or others, it may be<br />
appropriate to consider ‘rapid tranquillisation’ where repeated attempts at non-pharmacological<br />
interventions and oral medication has failed to produce any benefit (or has been refused). Refer to<br />
the <strong>Trust</strong> Policy for Rapid Tranquillisation (C36) and Clinical Protocol (CP11). This protocol states<br />
antipsychotic medication is not suitable for use in rapid tranquilisation in this population.<br />
Communication of information on transfer of care:<br />
Following a treatment review, it may be appropriate for the medication to be continued for an<br />
agreed period of time following discharge from an in-patient unit, or after review by a specialist<br />
in a community team.<br />
Where it is appropriate for treatment to be continued in primary care, the <strong>Trust</strong> prescriber<br />
(Consultant or Associate specialist) will:<br />
o Contact individual’s GP to request that they accept on-going responsibility for<br />
prescribing<br />
o Where prescribing is to be continued by GP- provide them with a clear treatment plan<br />
to cover the reduction and discontinuation of medication for <strong>BPSD</strong> and who to<br />
contact if they need to seek further advice on the clinical management of the<br />
individual (i.e. original symptoms re-emerge on discontinuation of treatment).<br />
o Include a summary of the information documented in the clinical notes regarding<br />
target symptoms and choice of medication and rationale for treatment.<br />
A standard letter template for communicating prescribing information to GPs is available here<br />
User-friendly resources<br />
Patient decision aid (intended to assist healthcare professionals in consultations with people with<br />
dementia and their family/carers) when treatment with antipsychotic drugs is being considered for<br />
<strong>BPSD</strong>: http://www.npci.org.uk/therapeutics/cns/dementia/resources/pda_dementia_antipsychotics.pdf<br />
Leaflets for patients/family/carers on dementia can be found on the Alzheimer’s Society website:<br />
www.alzheimers.org.uk/Facts_about_dementia/factsheets.htm)<br />
PG 14 – Pharmacological Management of <strong>BPSD</strong><br />
Approved by Drug and Therapeutics Committee: September 2013<br />
Review date: September 2015<br />
Page 6 of 10
Appendix 1<br />
Decision aid for specialist treatment strategies: Severe <strong>BPSD</strong><br />
There is a lack of high quality clinical trial evidence to support the effectiveness of medication for <strong>BPSD</strong><br />
(with evidence base generally based on Alzheimer’s dementia rather than vascular/stroke related, frontotemporal<br />
lobe, mixed or DLB), however increasingly there is information which questions their safety. The<br />
table below is designed to provide you with a summary the available evidence for drugs used for the<br />
management of <strong>BPSD</strong> (specific to aggression, agitation and/or psychosis), along with a summary of<br />
possible side effects and precautions required.<br />
ANTIPSYCHOTICS<br />
Evidence of efficacy in <strong>BPSD</strong>, though limited, is greatest for risperidone and olanzapine, however, clinical<br />
efficacy is at best only modest and this must be balanced against elevated risk of cerebrovascular adverse<br />
events, mortality, upper respiratory infections, oedema, extrapyramidal symptoms and an increase in overall<br />
mortality rate which applies to ALL ANTIPSYCHOTICS (first and second generation) and not just<br />
risperidone and olanzapine as originally reported in the Committee of Safety of Medicines alert (2004).<br />
Summary of risks and benefits for treating1000 people with dementia for <strong>BPSD</strong> over a 12 week period with<br />
an second generation antipsychotic would result in;<br />
91-200 people with behavioural disturbance showing clinically significant improvement in symptoms<br />
10 deaths<br />
(Evidence suggests that risk of mortality increases over time, therefore longer term treatment may result in<br />
up to 167 additional deaths over a 2 year period<br />
18 CVAEs of which ~50% would be severe<br />
(Evidence from observational studies suggests increased risk of CVAE may be confined to the 2-3 month<br />
period typically encompassed in RCT follow-up studies, therefore extrapolation of data in the original CSM<br />
alert, 2004, proposing that NNH of 37 would translate to NNH of 6.3 over 1 year, resulting in an additional<br />
159 CVAEs per 1000 people treated, may be an over-estimation).<br />
No additional falls or fractures<br />
58-94 people with gait disturbance<br />
Intervention<br />
Risperidone<br />
Olanzapine<br />
(Off-license use)<br />
Amisulpride<br />
(Off-license use)<br />
Aripiprazole<br />
(Off-license use)<br />
Quetiapine<br />
(Off-license use)<br />
First Generation<br />
antipsychotics<br />
(Off-license use)<br />
Rationale<br />
(Where stated, doses derived from published studies)<br />
Licensed for the short-term treatment (up to 6 weeks) of persistent<br />
aggression in patients with moderate to severe Alzheimer's dementia<br />
unresponsive to non-pharmacological approaches and when there is a risk of<br />
harm to self or others (500micrograms- 2mg/daily).<br />
Significant improvement in aggression & psychosis compared to placebo<br />
Significant improvement in aggression compared to placebo (5-10mg/daily)<br />
ONLY consider as a 2nd line option where risperidone not appropriate/not<br />
tolerated<br />
Reported doses prescribed 200mg/daily. Preliminary observation suggests<br />
that amisulpride may be useful to control agitation and disruptive behaviours.<br />
RCT (open prospective) demonstrated equivalent efficacy to risperidone.<br />
Only small open-label studies available. Evidence weak.<br />
Improvement in psychosis demonstrated with 2-15mg/day compared with<br />
placebo (Schneider et al 2006; NNT=13.8)<br />
Reported doses prescribed: 50-200mg/day. 200mg/day reported superior to<br />
placebo for agitation where 100mg/day not superior to placebo, BUT showed<br />
harm compared with placebo at 26 weeks for severe impairment battery (SIB)<br />
Potential risks outweigh possible benefits: (Associated with increased risk of<br />
CVE and mortality (mortality risk ≥ second generation antipsychotics)<br />
DPT use<br />
approved<br />
YES<br />
YES<br />
NO<br />
NO<br />
NO<br />
NO<br />
PG 14 – Pharmacological Management of <strong>BPSD</strong><br />
Approved by Drug and Therapeutics Committee: September 2013<br />
Review date: September 2015<br />
Page 7 of 10
ACETYL-CHOLINESTERASE INHIBITORS (If not already prescribed for management of AD)<br />
Intervention Rationale (Where stated, doses derived from published studies) DPT use<br />
approved<br />
Donepezil<br />
(Off-license use)<br />
Meta-analysis demonstrated a small by significant overall advantage of<br />
AChEIs over placebo with regard to the treatment of <strong>BPSD</strong> in Alzheimer’s<br />
Disease, although no short term benefit for treatment of clinically significant<br />
agitation with donepezil observed in 12 week RCT.<br />
Current evidence appears to demonstrate that AChEIs have their greatest<br />
effects on depression and dysphoria, apathy, indifference and anxiety and<br />
are probably not an effective treatment for the management of agitation or<br />
aggression in Alzheimer’s dementia.<br />
YES<br />
Galantamine<br />
(Off-license use)<br />
Rivastigmine<br />
(Off-license use)<br />
Evidence equivocal at doses of 16-24mg/day. In placebo controlled trials,<br />
Rockwood et al (2001) reported no statistically significant difference in<br />
behavioural symptoms between groups (n=386). Cummings et al (2004) post<br />
hoc analysis of Tariot et al (2000) reported slight improvement (NPI)<br />
observed with galantamine (p=0.04) at 16 & 24mg/day but not 8mg/d (n=978)<br />
Not approved because available evidence equivocal and increased treatment<br />
cost cannot be justified due to lack of evidence demonstrating increased<br />
efficacy compared with donepezil.<br />
Reported doses prescribed 1.5-4.5mg bd (6-12mg/day). Evidence equivocal<br />
(most studies open-label and behaviour a secondary end-point). Metaanalysis<br />
reported rivastigmine may be tolerated and effective for <strong>BPSD</strong> (6-<br />
12mg/d) (Finkel et al, 2004)<br />
Not approved because available evidence equivocal and increased treatment<br />
cost cannot be justified due to lack of evidence demonstrating increased<br />
efficacy compared with donepezil.<br />
NO<br />
NO<br />
NMDA ANTAGONIST<br />
Memantine Systemic meta- analysis suggested that memantine (10mg bd) decreases<br />
(Off-license use) NPI scores and may have a role in <strong>BPSD</strong> (reducing agitation/aggression) but<br />
effect size small. Could be considered for management of severe symptoms<br />
of agitation/aggression and psychosis in people who have failed to respond<br />
to other medication and who are otherwise prone to a rapid decline.<br />
Maidment et al (2008).<br />
However, a randomised DB PC trial (Fox et al 2012) reported no<br />
improvement in significant agitation in people with moderate to severe AD,<br />
suggesting that memantine should not be routinely prescribed to treatment<br />
agitation in AD.<br />
YES<br />
ANTIDEPRESSANTS<br />
Intervention Rationale (Where stated, doses derived from published studies) DPT use<br />
approved<br />
Mirtazapine<br />
(Off-license use)<br />
Citalopram<br />
(Off-license use)<br />
Trazadone<br />
(Off-license use)<br />
Limited evidence available. One 12 week open-label study reported<br />
mirtazapine (15-30mg/day) could be a well-tolerated treatment option for the<br />
management of agitation in people with Alzheimer’s Disease (AD).<br />
YES<br />
Whilst not clinically effective for the treatment of depression in people with<br />
AD, mirtazapine may act to improve general behavioural and psychological<br />
Banerjee (2013)<br />
symptoms in dementia rather than depression<br />
Limited, but encouraging, evidence available. More studies needed.<br />
Trazadone most widely used antidepressant prescribed for people presenting<br />
with <strong>BPSD</strong> despite lack of robust evidence to support efficacy.<br />
NO<br />
NO<br />
PG 14 – Pharmacological Management of <strong>BPSD</strong><br />
Approved by Drug and Therapeutics Committee: September 2013<br />
Review date: September 2015<br />
Page 8 of 10
BENZODIAZEPINES<br />
Intervention Rationale<br />
(Where stated, doses derived from published studies)<br />
Diazepam 1-2 mg up to 3 times a day (increase if necessary to<br />
(Off-license use) Max 15mg/24 in divided doses) Licensed for anxietyshort<br />
term use only for acute & severe distress<br />
and/or where sedation is required<br />
T1/2 ~32 hours (21-50) longer in older adults<br />
No systemic reviews of RCTs examining the<br />
usefulness of benzodiazepines in the management<br />
symptoms associated with dementia (including<br />
anxiety) were identified.<br />
Lorazepam<br />
(Off-license use)<br />
NB 5mg diazepam ~equiv to 0.5mg lorazepam<br />
Usual max dose= 2mg/24hours (in divided doses)<br />
Short term use for only for acute & severe distress<br />
and/or where sedation is required<br />
Licensed for anxiety<br />
T1/2 ~12 hours (8-25) Similar in older adults<br />
No systemic reviews of RCTs examining the<br />
usefulness of benzodiazepines in the management<br />
symptoms associated with dementia (including<br />
anxiety) were identified<br />
May<br />
cause/hasten<br />
cognitive decline<br />
Paradoxical<br />
disinhibition may<br />
occur<br />
Contribute to falls<br />
and hip fractures<br />
Accumulation<br />
leading to<br />
excessive<br />
sedation/adverse<br />
effects and/or<br />
tolerance over<br />
time<br />
DPT use<br />
approved<br />
YES<br />
ONLY<br />
for short<br />
term use for<br />
acute &<br />
severe<br />
distress<br />
and/or where<br />
sedation is<br />
required<br />
ANTI-CONVULSANTS:<br />
Intervention Rationale<br />
(Where stated, doses derived from published studies)<br />
Carbamazepine Uncontrolled studies & case reports have reported improvement in<br />
(Off-license use) presenting hostility & aggression in people with dementia who had not<br />
responded to antipsychotics as well as short term efficacy for agitation,<br />
however a review of placebo controlled RCTs to date provides equivocal<br />
information about efficacy for <strong>BPSD</strong>, and the safety and tolerability of<br />
therapeutic doses in people with dementia/older adults still needs to be<br />
established.<br />
DPT use<br />
approved<br />
NO<br />
Valproate<br />
(Off-license use)<br />
Adverse effects include: Impairment of balance & increased risk of falls,<br />
Drug interactions, Impaired cognition, Blood dyscraisias, Hyponatraemia,<br />
Hepatic dysfunction, Serious skin reactions<br />
Despite positive treatment responses documented in case reports,<br />
retrospective chart reviews and open-label studies, the existing d/b, p/c,<br />
RCTs do not support the proposal that valproate is effective in the<br />
management of agitation, aggression or other <strong>BPSD</strong> in people with<br />
dementia.<br />
NO<br />
Adverse effects include: GI side effects, Impaired cognition,<br />
Hepatotoxicity- monitor liver function before & during treatment<br />
Oxcarbazepine No evidence to demonstrate efficacy NO<br />
Gabapentin Limited data reporting treatment well tolerated and effective, but<br />
NO<br />
evidence weak (small open-label &case reports only) and incomplete.<br />
Pregabalin No available published evidence reporting use or efficacy for <strong>BPSD</strong> NO<br />
Lamotrigine<br />
Topiramate<br />
Limited data reporting treatment well tolerated and effective, but<br />
evidence very weak (case reports only).<br />
Limited data (non-random retrospective study n=15). Reduction in<br />
Cohen-Mansfield Agitation Inventory noted but evidence very weak.<br />
NO<br />
PG 14 – Pharmacological Management of <strong>BPSD</strong><br />
Approved by Drug and Therapeutics Committee: September 2013<br />
Review date: September 2015<br />
Page 9 of 10
References<br />
Alzheimer’s Society (2011) Optimising treatment and care for people with behavioural<br />
and psychological symptoms of dementia .A best practice guide for health and social<br />
care professionals.<br />
Available at http://www.alzheimers.org.uk/site/scripts/download_info.phpfileID=1163<br />
Ballard C.G.; Gauthier S.; Cummings J.L.; Brodaty H.; Grossberg G.T.; Robert P.;<br />
Lyketsos C.G. Management of agitation and aggression associated with Alzheimer<br />
disease<br />
Nature reviews. Neurology, May 2009, vol./is. 5/5(245-255),<br />
Ballard C.; Corbett A.; Chitramohan R.; Aarsland D. Management of agitation and<br />
aggression associated with Alzheimer's disease: Controversies and possible<br />
solutions Current Opinion in Psychiatry, November 2009, vol./is. 22/6(532-540),<br />
Banerjee S, Hellier J, Romeo R et al (2013) Study of the use of antidepressants for<br />
depression in dementia: the HTA-SADD trial- a multicentre, randomised, DB, PC trial of<br />
the clinical effectiveness and cost-effectiveness of sertraline and mirtazapine. Health<br />
Technol Assess 17(7) DOI: 10.3310/hta17070 www.alzheimers.org.uk/bpsdguide.<br />
Accessed 14 Aug 2013<br />
Bazire S (2012) Psychotropic Drug Directory 2012. Warwickshire.UK<br />
Cakir S, Kulaksizoglu I (2008) The efficacy of mirtazapine in agitated patients with<br />
Alzheimer’s Dementia: A 12 week open label pilot study. Neuropsychiatric Disease and<br />
Treatment 4(5) 963-966<br />
Corbett A.; Smith J.; Creese B.; Ballard C. Treatment of behavioral and psychological<br />
symptoms of Alzheimer's disease Current Treatment Options in Neurology, April<br />
2012, vol./is. 14/2(113-125),<br />
Fox C, Crugel M, Maidment I et al (2012) Efficacy of memantine for agitation in<br />
Alzheimer’s Dementia: A randomised double-blind placebo controlled trial PLoS ONE<br />
7(5): e35185 doi:10.1371/journal.pone.0035185<br />
Konovalov S, Muralee S, Tampi R (2007) Anticonvulsants for the treatment of<br />
behavioural and psychological symptoms of dementia: a literature review. International<br />
Psychogeriatrics 20:2, 293-308<br />
Pollock B.G.; Mulsant B.H.; Rosen J.; Mazumdar S.; Blakesley R.E.; Houck P.R.; Huber<br />
K.A. (2007) A double-blind comparison of citalopram and risperidone for the<br />
treatment of behavioral and psychotic symptoms associated with dementia The<br />
American journal of geriatric psychiatry, vol./is. 15/11(942-952)<br />
Pollock B.G.; Mulsant B.H.; Rosen J.; Sweet R.A.; Mazumdar S.; Bharucha A.; Marin R.;<br />
Jacob N.J.; Huber K.A.; Kastango K.B.; Chew M.L. (2002) Comparison of citalopram,<br />
perphenazine, and placebo for the acute treatment of psychosis and behavioral<br />
disturbances in hospitalized, demented patients American Journal of Psychiatry,<br />
vol./is. 159/3(460-465),<br />
National Institute for Health and Clinical Excellence (2006) Dementia (CG42): Supporting<br />
people with dementia and their carers in health and social care<br />
Seitz DP, Adunuri N, Gill SS, Gruneir A, Herrmann N, Rochon P. Antidepressants for<br />
agitation and psychosis in dementia. Cochrane Database of Systematic Reviews 2011,<br />
Issue 2. Art. No.: CD008191. DOI: 10.1002/14651858.CD008191.pub2<br />
PG 14 – Pharmacological Management of <strong>BPSD</strong><br />
Approved by Drug and Therapeutics Committee: September 2013<br />
Review date: September 2015<br />
Page 10 of 10