PEPSI COLA Aide Memoire - East Midlands Cancer Network
PEPSI COLA Aide Memoire - East Midlands Cancer Network
PEPSI COLA Aide Memoire - East Midlands Cancer Network
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Document History<br />
Document Location<br />
This document is only valid on the day it was printed.<br />
The source of the document will be found at this location –<br />
www.eastmidlandscancernetwork.nhs.uk<br />
Revision History<br />
Date of this revision: 25 August 2010<br />
Date of next revision: December 2011<br />
Revision Previous Summary of Changes<br />
date revision date<br />
25/08/10 First issue<br />
Changes<br />
marked<br />
Approvals<br />
This document requires the following approval.<br />
Name Title Date of Version<br />
Issue<br />
Mr T Rideout Chief Executive NHS Leicester City 01/09/10 1.0<br />
Distribution<br />
This document has been distributed to:<br />
Group Name Location Date of Issue Version<br />
Primary Care Trust <strong>East</strong> <strong>Midlands</strong> 01/09/10 1.0<br />
Acute Trust <strong>East</strong> <strong>Midlands</strong> 01/09/10 1.0<br />
General Practitioners <strong>East</strong> <strong>Midlands</strong> 01/09/10 1.0<br />
Lead <strong>Cancer</strong> Nurses <strong>East</strong> <strong>Midlands</strong> 01/09/10 1.0<br />
Allied Health Protection <strong>East</strong> <strong>Midlands</strong> 01/09/10 1.0<br />
Leads<br />
Voluntary Sector <strong>East</strong> <strong>Midlands</strong> 01/09/10 1.0<br />
Hospices <strong>East</strong> <strong>Midlands</strong> 01/09/10 1.0<br />
EMCN NSSG Boards <strong>East</strong> <strong>Midlands</strong> 01/09/10 1.0<br />
Lead Nurses in <strong>East</strong> <strong>Midlands</strong> 01/09/10 1.0<br />
Community<br />
Long Term Conditions <strong>East</strong> <strong>Midlands</strong> 01/09/10 1.0<br />
Managers<br />
Social Services <strong>East</strong> <strong>Midlands</strong> 01/09/10 1.0<br />
This list is not exhaustive as further dissemination will take place by the above groups
Content<br />
1. Introduction ........................................................................................... 4<br />
2. Key Evidence ........................................................................................ 5<br />
3. Purpose of Guidelines........................................................................... 6<br />
4. Who should be Assessed.................................................................... 6<br />
5. Who should be the Assessor............................................................... 6<br />
6. Competencies ....................................................................................... 7<br />
7. Education & Training............................................................................. 9<br />
8. When should you Assess.................................................................. 10<br />
9. How to Assess .................................................................................... 11<br />
10. Recording, storing and sharing information from the assessment....... 14<br />
11. Taking Action ...................................................................................... 15<br />
12. Patient Information.............................................................................. 15<br />
13. Minimum Standards and Outcome Measures ..................................... 16<br />
14. Summary............................................................................................. 16<br />
15. References and bibliography............................................................... 18<br />
16. Acknowledgements............................................................................. 18<br />
Appendix A – <strong>Cancer</strong> Patient Pathway..................................................................... 20<br />
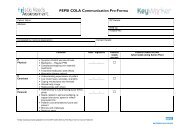
Appendix B – <strong>PEPSI</strong> <strong>COLA</strong> Communication Pro-Forma .......................................... 21<br />
Appendix C – Holistic Needs Assessment Template................................................ 23<br />
Appendix D – <strong>PEPSI</strong> <strong>COLA</strong> <strong>Aide</strong> <strong>Memoire</strong>............................................................... 29<br />
Appendix E – Distress Thermometer........................................................................ 31<br />
Appendix E continued............................................................................................... 33<br />
Appendix F – Patient Leaflet..................................................................................... 35<br />
Appendix G – Priority 2 – Holistic Assessment of Patient Supportive & Palliative Care<br />
Needs.................................................................................................. 37<br />
3
1. Introduction<br />
The aim of this document is to be a guide for the Holistic Needs Assessment (HNA)<br />
for the Supportive and Palliative Care of adults with cancer and their carers; this can<br />
support practitioners and managers providing or co-ordinating the care. The<br />
guidance has been prepared in response to recommendations from the National<br />
Institute for Health and Clinical Excellence Guidance on Improving Supportive and<br />
Palliative Care for Adults with <strong>Cancer</strong> (NICE 2004). It can be used to check if current<br />
documentation records the information listed in this guide. It can help with updating<br />
patient records, and can be used as the standard to audit documentation against. It<br />
is designed for healthcare teams to use as a benchmark against which current local<br />
processes of assessment can be audited. It is recommended that an audit of practice<br />
is completed 2 yearly. The results should be acted upon to enable improvements to<br />
be made and to inform future commissioning.<br />
Being clear about the kind of information we should be gathering on patients and<br />
their carers is fundamental to the delivery of high quality care. When done well a<br />
Holistic Needs Assessment (HNA) is helpful in not only gathering useful information<br />
but can also be therapeutic in its own right.<br />
A good Holistic Needs Assessment depends on well developed communication skills.<br />
In recent years, throughout the <strong>East</strong> <strong>Midlands</strong> <strong>Cancer</strong> <strong>Network</strong> (EMCN), Advanced<br />
Communication Skills courses have been delivered to senior health care<br />
professionals. These courses, and the research they are based on, emphasise the<br />
importance of having a patient-centred rather than just a disease-centred approach in<br />
assessing patients.<br />
A Holistic Needs Assessment tool, defined by The Kings College London (2005), is a<br />
collection of questions, scales and other means of obtaining information which<br />
provides a consistent and comprehensive system through which patient’s needs for<br />
support and care can be explored. In addition, to assisting professionals to<br />
determine appropriate care for a patient, the information might also be used for audit<br />
and service planning.<br />
The need for robust care planning and coordination of care is highlighted in the End<br />
of Life Care Strategy (DOH 2008). Undertaking a Holistic Needs Assessment helps<br />
achieve this both at the end of life and also at all stages of the pathway. By clearly<br />
identifying and documenting patient’s needs care can be planned accordingly.<br />
Living with and beyond cancer (survivorship) has been recognised in the <strong>Cancer</strong><br />
Reform Strategy (DOH 2007). It is therefore important for the assessor to assist the<br />
patient to adapt to normal life following their treatment phase. Prevention and health<br />
promotion are also key priorities within the strategy and the assessor needs to use<br />
the assessment process not only to encourage patients to live more healthily but also<br />
to help their carers.<br />
4
Advance Care Planning discussions can be undertaken during a Holistic Needs<br />
Assessment but should not be forced upon an individual.<br />
The Mental Capacity Act came into force in 2005. Important elements include<br />
Advance Decisions to Refuse Treatment and the personal welfare Lasting Power of<br />
Attorney. There should be a clear record if a patient has these, including what has<br />
been discussed and acted upon. It should also be clearly documented if a patient has<br />
already used these processes to guide their choice of care.<br />
2. Key Evidence<br />
The requirement to offer people with cancer a range of physical, emotional, spiritual<br />
and social support was one of the key recommendations in the NICE guidance on<br />
Supportive and Palliative care:<br />
Key Recommendation 2: Assessment and discussion of patients’ needs for<br />
physical, psychological, social, spiritual and financial support should be<br />
undertaken at key points (such as at diagnosis; at commencement, during, and<br />
at the end of treatment; at relapse; and when death is approaching). <strong>Cancer</strong><br />
<strong>Network</strong>s should ensure that a unified approach to assessing and recording<br />
patients’ needs is adopted, and that professionals carry out assessments in<br />
partnership with patients and carers.<br />
From Improving Supportive and Palliative Care for Adults with <strong>Cancer</strong>, published by<br />
the National Institute for Clinical Excellence, (NICE) March 2004<br />
The NICE guidance, (2004), also gave further specific recommendations with respect<br />
to assessment:<br />
• Patients should be offered support to help them to assess their own needs<br />
• They should not be subjected to unnecessary repeated assessments from<br />
different professionals aiming to elicit similar information<br />
• Assessments should encompass all aspects of Supportive and Palliative care<br />
• A structured assessment should be undertaken and recorded (in an agreed<br />
format) at key points in the patient pathway with mechanisms developed for<br />
sharing the data among the multidisciplinary team<br />
• Following each assessment, potential interventions should be discussed with<br />
patients and carers and a mutually agreed action plan formulated<br />
• Health and social care professionals who undertake assessment should have<br />
received training in assessing patients’ and carers’ needs (see section 7)<br />
In January 2007 the National <strong>Cancer</strong> Action Team published a specification for the<br />
holistic common assessment of Supportive and Palliative care needs for adults with<br />
cancer. The specification outlined 5 domains of assessment:<br />
• Background information and assessment preferences<br />
• Physical needs<br />
• Social and occupational needs<br />
• Psychological well-being<br />
• Spiritual well-being<br />
5
3. Purpose of Guidelines<br />
The <strong>East</strong> <strong>Midlands</strong> <strong>Cancer</strong> <strong>Network</strong> guidelines are intended to assist teams in<br />
implementing the Holistic Needs Assessment in any setting. (This is likely to be done<br />
by the Key Worker). The key stages of the cancer patient’s journey have been<br />
identified to indicate where a HNA should be undertaken to ensure and identify any<br />
Holistic Care Needs and co-ordinate the patient’s care (see Appendix A). Where<br />
teams use this guidance for other disease pathways, the stages may vary slightly.<br />
4. Who should be Assessed<br />
All patients with a diagnosis of cancer and/or receiving care in any setting should be<br />
offered this assessment.<br />
It is not expected that this Holistic Needs Assessment will be offered routinely to<br />
patients with suspected cancer. However, assessment should always be offered to<br />
any individual with suspected cancer who has supportive care needs.<br />
The guidance is for the assessment of patients needs and has not been designed to<br />
assess the needs of carers. However, it is recognised that carers’ needs might be<br />
identified during the course of the patient assessment, and this may in itself raise a<br />
need for further assessment of the carer and acted upon.<br />
5. Who should be the Assessor<br />
The patient’s healthcare team at each stage of the pathway is responsible for<br />
ensuring that the assessment takes place at that key point. The patient’s Key Worker<br />
is ideally placed for undertaking the Holistic Needs Assessment with the patient. In<br />
the Acute setting, the Key Worker will be a Clinical Nurse Specialist (CNS) where<br />
one is in post. In the absence of a CNS a senior nurse or other health care<br />
professional may be allocated as a Key Worker. The HNA may also be undertaken<br />
by other competent health professionals or in primary care by an appropriate<br />
member of the healthcare team.<br />
Teams should use the following principles when selecting an assessor:<br />
• The assessor should have reached an agreed level of competence in key<br />
aspects of the assessment process<br />
• The assessor should be a clinical professional with an appropriate level of<br />
knowledge of the disease, its symptoms, treatment and likely prognoses<br />
• The selection should be in accordance with any patient preferences for<br />
communicating with a particular professional<br />
• The assessor should have access to up-to-date information about local<br />
service providers, referral criteria and support services<br />
6
6. Competencies<br />
The competencies have been adapted from Department of Health Core<br />
Competencies for End of Life Care (June 2009) and Marie Curie Spiritual & Religious<br />
Competencies for Specialist Palliative Care.<br />
Communication Skills<br />
• Communicate with a range of people on a range of matters in a form that is<br />
appropriate to them and the situation<br />
• An ability to develop a rapport with patients and carers<br />
• An ability to elicit the patient’s key concerns at a pace directed by the patient<br />
• Develop and maintain communication with people about difficult and complex<br />
matters<br />
• Present information in a range of formats, including written and verbal, as<br />
appropriate to the circumstances<br />
• Understand the importance and impact of non-verbal and verbal<br />
communication recognising the importance of active listening<br />
• Utilise all forms of patient information to enable the patient to have a better<br />
understanding of their diagnosis and treatment plan (see section 12)<br />
• Listen to individuals, their families and friends about their concerns and<br />
provide information and support<br />
• Work with individuals, their families and friends in a sensitive and flexible<br />
manner, demonstrating awareness of the impact of a cancer diagnosis, and<br />
recognising that their priorities and ability to communicate may vary over time<br />
• Act as an advocate for the patient who has or may have had cancer<br />
• Initiate and participate in MDT discussion and case conferences with all<br />
professionals involved in the delivery of patient care<br />
• Understand confidentiality with regard to the patients/carers personal<br />
information and what may be shared within the MDT<br />
• Act as a communication resource and co-ordinator for other members of the<br />
multi-professional team in the care of the patient<br />
• Ensure accurate follow-up documentation is maintained including any changes<br />
in the named Key Worker<br />
• Have sufficient knowledge and links with national/local support groups and be<br />
able to provide/record information relating to these groups to guide and advise<br />
patients<br />
Assessment and Care Planning<br />
• Recognition of their own personal limits<br />
• Documents patient/carer information in a way that respects confidentiality of<br />
individuals and of the MDT<br />
7
• Understand the range of assessment tools, and ways of gathering information,<br />
and their advantages and disadvantages<br />
• Document the assessment, intervention, outcomes and referrals for<br />
patients/carers<br />
• Assess pain and other symptoms using assessment tools, pain history,<br />
appropriate physical examination and relevant investigation<br />
• Undertake/contribute to multi-disciplinary assessment and information sharing<br />
• Ensure that all assessments are holistic, including:<br />
o Background information<br />
o Current physical health and prognosis<br />
o Social/occupational well-being<br />
o Psychological and emotional well-being<br />
o Religion and/or spiritual well-being, where appropriate<br />
o Culture and lifestyle aspirations, goals and priorities<br />
o Risk and risk management<br />
o The needs of families and friends, including carer’s assessments<br />
• Regularly review assessments to take account of changing needs, priorities<br />
and wishes, and ensure information about changes is properly communicated<br />
• Co-ordinate the onward referral of patient and/or family members to<br />
appropriate clinical or support services<br />
• Utilise all available support strategies and interventions<br />
• Initiate appropriate referrals when caring for patients with Complex needs, e.g.<br />
patients exhibiting denial/anger following cancer diagnosis, adverse reactions<br />
to altered body image<br />
• Understand the ethical issues relating to treatment in advanced disease<br />
Symptom management, maintaining comfort and well being<br />
• Be aware that symptoms have many causes, including the disease itself, its<br />
treatment, a concurrent disorder, including depression or anxiety, or other<br />
psychological or practical issues<br />
• Understand the significance of the individual’s own perception of their<br />
symptoms to any intervention<br />
• Understand that the underlying causes of a symptom will have an impact upon<br />
how care should be delivered<br />
• Understand the range of therapeutic options available, including drugs,<br />
hormone therapy, physical therapies, counselling or other psychological<br />
interventions, complementary therapies, surgery, community or practical<br />
support<br />
• In partnership with others, including the individual, their family and friends,<br />
develop a care plan which balances disease-specific treatment with other<br />
interventions and support that meet the needs of the individual<br />
• In partnership with others, implement, monitor and review the care plan<br />
8
• Awareness of cultural issues that may impact on symptom management<br />
• Be aware of local contact arrangements in the event of patients experiencing<br />
unwanted side effects.<br />
Advance Care Planning<br />
• Demonstrate awareness and understanding of Advance Care Planning, and<br />
the times at which it would be appropriate<br />
• Demonstrate awareness and understanding of the legal status and<br />
implications of the Advance Care Planning process in accordance with the<br />
provisions of the Mental Capacity Act 2005<br />
• Show understanding of Informed Consent, and demonstrate the ability to give<br />
sufficient information in an appropriate manner<br />
• Use effective communication skills when having Advance Care Planning<br />
discussions as part of ongoing assessment and intervention<br />
• Work sensitively with families and friends to support them as the individual<br />
decides upon their preferences and wishes during the Advance Care Planning<br />
process<br />
• Where appropriate, ensure that the wishes of the individual, as described in an<br />
Advance Care Planning statement, are shared (with permission) with other<br />
workers.<br />
Spirituality & Religion<br />
• Recognise that everyone has a spiritual dimension, and that some people will<br />
have a religious element to their spirituality<br />
• Recognise their personal boundaries in spiritual care and know when to refer<br />
on for more experienced assistance whilst understanding the skills that other<br />
members of the Multi-Disciplinary Team (MDT) possess in relation to spiritual<br />
care<br />
• Understand the nature of spiritual assessment including religious and ethical<br />
dimensions<br />
• An ability to describe and evidence a working definition of spiritual and<br />
religious needs<br />
7. Education & Training<br />
It is necessary for individuals who perform the Holistic Needs Assessment to identify<br />
their training needs in their KSF Development Review; the individual must ensure<br />
that they meet the standard of competence necessary to be able to undertake<br />
Holistic Needs Assessment, i.e.<br />
9
• The professional carrying out the Holistic Needs Assessment should<br />
have experience in cancer care and up-to-date information on local<br />
service providers, referral criteria and support services<br />
• All professionals carrying out the Holistic Need Assessment should have postregistration<br />
training and education in intermediate/advanced communication<br />
and/or counselling skills, and for core MDT members within secondary care, to<br />
have undertaken the National Advanced Communication Skills Training<br />
course<br />
• All staff should have basic cancer awareness – able to recognise the impact of<br />
diagnosis and treatment and consider practical, financial and emotional effects<br />
• The line manager should ensure appropriate clinical supervision is available<br />
for those undertaking this role<br />
• The individual carrying out the Holistic Needs Assessment must be either a<br />
recognised core-member of the relevant cancer or palliative care local or<br />
specialist MDT, or a member of the patient’s primary health care team and/or<br />
Hospice staff<br />
• The individual performing the Holistic Needs Assessment is responsible for<br />
identifying any other personal training needs required in relation to fulfilling this<br />
role<br />
• Training in the use and application of the Distress Thermometer is<br />
recommended.<br />
8. When should you Assess<br />
The NICE Supportive and Palliative Care Guidance (2004) states that whilst<br />
assessment should be an ongoing process, structured assessments of patients’<br />
needs should be undertaken at key points in their cancer journey, (Appendix A), and<br />
should supplement day-to-day appraisal of individual patients.<br />
An assessment can be carried out in any setting that ensures comfort and privacy<br />
and will be determined by the patient’s care setting at that point in their pathway.<br />
Assessment is likely to be needed at:<br />
• Around the time of diagnosis<br />
• Commencement of treatment (if appropriate for patient care)<br />
• Completion of primary treatment plan<br />
• Each new episode of disease recurrence<br />
• The point of recognition of incurability / Palliative Care (Gold Standard<br />
Framework may be a trigger)<br />
• The point at which dying is recognised (Liverpool Care Pathway may be<br />
commenced)<br />
• At any other time the patient requests it<br />
• At any other time that a professional carer may judge necessary<br />
• Survivorship (a Holistic Needs Assessment may be needed to produce<br />
individualised self care plans to form part of the discharge process)<br />
10
Whilst best practice suggests that a full assessment should be completed in a single<br />
session, this might not always be practical or appropriate. The assessment should<br />
follow these principles:<br />
• The timing and pace of the assessment is patient sensitive<br />
• Priority needs are identified at an early stage<br />
• The whole assessment is completed within a reasonably short time<br />
• If the assessment is to be completed by a different assessor communication<br />
must take place with the appropriate healthcare professional. An example of a<br />
communication tool is the <strong>PEPSI</strong> <strong>COLA</strong> Communication pro-forma (Appendix<br />
B)<br />
9. How to Assess<br />
All patients should have an assigned Key Worker at each stage of their care pathway<br />
(please see the EMCN ‘Policy for the Key Worker role in the management of adult<br />
patients with cancer (2010)). The most appropriate health care professional to act as<br />
Key Worker is dependent on individual patient’s needs.<br />
Best practice recommends that a HNA can be completed at any point of the patient’s<br />
pathway. An example of the minimum information that must be recorded is shown in<br />
Appendix C.<br />
A HNA may already be embedded within your organisation. Otherwise examples are<br />
shown in the appendices. The <strong>PEPSI</strong> <strong>COLA</strong> <strong>Aide</strong> <strong>Memoire</strong> compliments the process<br />
as a practical guide for staff (Appendix D).<br />
Using the Distress Thermometer as part of the HNA will help the assessor to<br />
evaluate if a patient requires referral to other agencies or the need to escalate to<br />
level 3 or 4 of the psychological support pathway. Staff will need training in the use<br />
of the Distress Thermometer before using this particular assessment tool (Appendix<br />
E).<br />
Before doing a full assessment of a patient and carer’s needs, it is useful to start by<br />
finding out as much information as possible from previous notes or letters and<br />
colleagues before seeing the patient. When seeing the patient it is useful for the<br />
consultation to follow a structure. This helps to ensure as much appropriate<br />
information is gathered as possible. It also has been shown to increase the<br />
usefulness of the consultation to the patient.<br />
This guide can be used not just as a structure in assessing patients but can also be<br />
used to inform what should be recorded. For example it is helpful to ask about and<br />
record patients’ concerns, expectations and feelings as well a history of the illness<br />
and a list of drugs. The five main parts to this structure are:<br />
1. Initiating the session<br />
2. Gathering information<br />
3. Building the relationship<br />
4. Explanation and planning<br />
11
5. Closing the session<br />
When initiating the session it is important to be clear about whom you are and what<br />
your role is, and also to check what the patient likes to be called. Gathering<br />
information is about listening to the patient’s narrative to see what they know and<br />
what currently are their concerns and feelings.<br />
For this part of the consultation it is useful to start off with an open question such as<br />
‘Could you tell me what has been happening to you since the beginning of this<br />
illness’ or ‘How did all this start’ The assessor can pick up on various points and<br />
cover information that has not yet been addressed. Summarising shows the patient<br />
you have been listening carefully and helps the patient come up with any other<br />
concerns they may have.<br />
The history also usually provides a basis on which to construct a list of problems and<br />
concerns from the patient's point of view. Acknowledging the patient’s views and<br />
feelings and being empathic, ‘It sounds to me like you’ve had a tough year’, helps to<br />
build the relationship.<br />
Many patients leave consultations without understanding things so explanation and<br />
planning is important.<br />
Closing the session involves checking if there is an understanding of the discussion<br />
and if there are any other concerns and then making plans for follow up.<br />
Assessments can be more complex than this but generally follow the above<br />
structure.<br />
Patients who are ill and tired may not be able to partake in a prolonged Holistic<br />
Needs Assessment (HNA). The reality of working in a busy clinical environment also<br />
means that staff time is limited. To get the best out of the assessment and to make<br />
things more effective for everyone, including patients and carers, there are a number<br />
of things that can be done:<br />
• Being clear about what information is discussed / required. This guidance<br />
outlines what information should be collected<br />
• Documentation needs to be well designed. It is important that paperwork is<br />
well designed so that it can be quick and easy to fill in. (See Appendix C for<br />
suggested content)<br />
• Information should be shared. The NICE Supportive and Palliative Care<br />
Guidelines (2004) recommend that patients should not be subjected to<br />
unnecessary repeated assessment from different professionals aiming to elicit<br />
similar information. Sharing information saves staff, patients’ and carers’ time.<br />
It is important that the paperwork and electronic systems allow relevant<br />
information to flow easily between the various teams an example of this is the<br />
adapted <strong>PEPSI</strong> <strong>COLA</strong> communication pro-forma (Appendix B)<br />
• Have similar ways of recording information. Family trees can be recorded<br />
in the same way for example using the same types of genogram graphics as<br />
in Appendix C<br />
• Remove obsolete documentation. It is worth reviewing paperwork from time<br />
to time, for example when documentation is being audited. It is relatively easy<br />
12
to add extra bits of paperwork to be filled in but more difficult to remove bits of<br />
paperwork that have become obsolete<br />
• Use the same documentation across departments. Using the same<br />
paperwork across different departments and providers can also save time<br />
• Communication skills training helps healthcare professionals carry out<br />
holistic assessments that more accurately identify patients’ concerns and is<br />
more likely to lead to better patient satisfaction<br />
<strong>PEPSI</strong> <strong>COLA</strong> Communication tool / <strong>Aide</strong> <strong>Memoire</strong> for undertaking the HNA<br />
The <strong>PEPSI</strong> <strong>COLA</strong> can be used as an aide memoire to ensure patient’s holistic needs<br />
are assessed.<br />
The aide memoir was adaptation from the Gold Standard Framework (GSF) by<br />
Mount Vernon <strong>Cancer</strong> <strong>Network</strong> (Appendix D). It is a tool to support practitioners<br />
carrying out assessments and can be used with current assessment tools and<br />
documentation. It promotes communication, support between professionals and<br />
patients, and provides a framework to consider patients holistic needs.<br />
The aide memoir encompasses all the domains of a Holistic Needs Assessment<br />
through the acronym <strong>PEPSI</strong> <strong>COLA</strong>:<br />
P<br />
E<br />
P<br />
S<br />
I<br />
C<br />
O<br />
L<br />
A<br />
Physical<br />
Emotional<br />
Personal<br />
Social Support<br />
Information and Communication<br />
Control and Autonomy<br />
Out of Hours<br />
Living with your Illness<br />
Aftercare<br />
In each domain the tool identifies:<br />
• Consider - Potential anticipated patient issues and concerns<br />
• Resources - Cue questions to ask patients and carers<br />
• Refer on if Appropriate - Resources for professionals to signpost to.<br />
The <strong>PEPSI</strong> <strong>COLA</strong> Communication Pro-forma is an adaptation to aid clear<br />
communication pathways.<br />
To avoid patients having repeated assessments, the communication pro-forma<br />
allows the assessor to acknowledge information gained and to communicate this to<br />
the most appropriate healthcare professional as follows:<br />
• If there are no problems identified record in the Patient’s needs met column<br />
that there are no issues at that particular assessment (it needs to be<br />
acknowledged that this assessment is only valid as per the date and will need<br />
to be reviewed and evaluated at subsequent assessments)<br />
13
• If there is a problem identified, the assessor will document this in the<br />
Patient’s needs not met column, with a detailed action plan<br />
A copy of every assessment must be filed in the patients notes for continuity of care.<br />
However if an onward referral is an outcome for example secondary to primary care<br />
a copy of the document with the patient’s consent will be sent to the appropriate<br />
healthcare professional. (If requested a copy can be given to the patient)<br />
10. Recording, storing and sharing information from the assessment<br />
The healthcare team should agree standard processes for the recording, storage,<br />
and sharing of assessment information.<br />
Each assessment should be recorded. An assessment record should capture:<br />
• Information obtained through the use of the Distress Thermometer. This will<br />
form the basis for future assessments<br />
• All identified needs documented and referrals documented as appropriate<br />
• Relevant discussion relating to identified needs<br />
• Overall conclusions of the assessment and the evidence behind them<br />
(Conclusions should be agreed with the patient and any major difference of<br />
opinion recorded)<br />
• A summary record of the principal findings, and actions agreed with the patient<br />
It must be recorded in all the patient’s notes that the patient has been offered a<br />
Holistic Needs Assessment and if they have accepted or subsequently declined.<br />
The Distress Thermometer needs to be held in the patient’s medical notes. (The<br />
patient may also request a copy). Detailed information from the assessment should<br />
be held in electronic or paper files, as a ‘full record’ of the assessment activity at that<br />
point in time. It is imperative that, where electronic systems exist, a record of<br />
assessment is recorded. As a minimum, the use of a paper-based system for sharing<br />
the record of assessment e.g. a patient-held record may be used. The record of<br />
assessment should support sharing both within and across the teams and agencies<br />
involved in the care of the patient.<br />
Supportive and Palliative care may be provided by care teams from organisations<br />
outside the NHS, e.g. social services. Where it is in the best interest of the patient’s<br />
care for the assessment record to be shared with organisations outside the NHS, the<br />
assessor should discuss and agree this with the patient beforehand. In instances<br />
where the patient does not agree the assessor should discuss with the patient the<br />
possible effect this may have on their care and the alternatives available to them.<br />
This needs to be documented in the patient’s notes.<br />
Generally speaking, the HNA should be shared between multi-professional teams<br />
and across agencies as required, subject to the patient’s consent.<br />
14
Assessors should have routine access to the details of any previous assessments<br />
and, on request to the team(s) responsible for them, access to further information<br />
from the full records of such assessments where these may be relevant to the current<br />
care of the patient. This information may include any other pertinent assessments,<br />
including specialist assessments. This is all with the consent of the patient.<br />
11. Taking Action<br />
The assessor should work with the patient to identify solutions or actions and to plan<br />
care. Where possible the assessor should focus on what the patient can do for<br />
himself or herself. If more help is needed the assessor should establish whether this<br />
can be provided by the patient’s current care package.<br />
If referral is needed, the assessor should be aware of local services and their referral<br />
criteria. Where referral is necessary the assessor should:<br />
• Agree the referral with the patient and seek their agreement to appropriate<br />
information sharing with the agency<br />
• Discuss the assessment and referral with the receiving agency including, if<br />
appropriate, agreeing a lead professional<br />
• Where there is agreement, share the content of HNA with the agency<br />
• Communicate with the patient’s Key Worker (if they are not the person<br />
undertaking the assessment)<br />
12. Patient Information<br />
Offering information throughout the patient journey is an integral part of holistic care,<br />
and must not be seen as a ‘one-off’ task. Information needs change over time, and<br />
differ markedly between patients, so assumptions of need should not be made<br />
without sensitively questioning the patient about their wish for information, their<br />
background knowledge, and the type and depth of information they would like.<br />
Information provision should normally be recorded on an Information Prescription,<br />
which can be updated with subsequent assessments, and, with the patient’s<br />
permission, be shared as part of continuing care when the Key Worker changes.<br />
If a patient refuses information this should be documented. However information<br />
should still be offered at each assessment, and at any other stage when requested<br />
by the patient.<br />
Information should be offered in three main areas:<br />
i. Disease related - depending on the patient’s wishes, this may be on cancer,<br />
the tumour type, prognosis, inheritable factors, treatments, effectiveness,<br />
alternative therapies, self care<br />
ii. Support - support groups (local and national), reliable websites, voluntary<br />
services, appropriate help lines<br />
iii. Appropriate services - NHS, benefits advice, social services<br />
15
The assessor should remain alert to signs that the patient does not understand the<br />
information provided, or that they may have unanswered questions, and use<br />
advanced communication skills to ensure that the patient can ask for the information<br />
they need.<br />
The assessor should have information available through the Information Prescription<br />
Generator and/or local resources. The assessor should also seek expert guidance<br />
from information centres or other appropriate specialists whenever required.<br />
An example of a Patient information leaflet in relation to the Holistic Needs<br />
Assessment is included as Appendix F.<br />
13. Minimum Standards and Outcome Measures<br />
The IOG recommends that audits are completed against EMCN guidance.<br />
The following measures are recommended:<br />
• It must be recorded in all the patients notes that the patient has been offered<br />
an Holistic Needs Assessment with reference to their choice<br />
• The Distress Thermometer is completed and held within the patient notes<br />
• 50% should be offered assessment using network agreed approach and rising<br />
to 100% by December 2011 to meet core deliverables as per Appendix G<br />
• All identified needs documented and referrals documented as appropriate<br />
• Relevant discussion relating to identified needs<br />
• Evidence of the review of the physical, social, psychological, emotional and<br />
spiritual beliefs of the patient is evident<br />
• The training and competencies of assessors are appropriate as per this<br />
guidance - section 6 and 7<br />
• Processes in place for both offering an assessment and the uptake of<br />
assessment documented in the patient’s notes<br />
Each provider organisation should take responsibility for auditing the effectiveness of<br />
the Holistic Need Assessment. This audit should take place at least two yearly.<br />
Documentation mentioned to be read as both paper and electronic documentation.<br />
14. Summary<br />
Assessment forms an integral part of patient care and should be seen as a<br />
continuous process. Undertaking a Holistic Needs Assessment at key points forms<br />
part of this continuous process, and should supplement day-to-day appraisal of<br />
individual patient needs.<br />
The assessor should take account of any patient needs identified in previous<br />
assessments.<br />
16
The patient is at the heart of assessment and care planning. The process of<br />
assessment should be one of partnership between patient and professional.<br />
Assessment should be patient ‘concerns-led’. Helping patients to assess their own<br />
needs should be central to the process. The assessment should mainly follow a<br />
conversational style.<br />
Self-assessment is a useful way to identify issues of particular concern to the patient,<br />
for subsequent discussion with the assessor. Patients should therefore be offered the<br />
opportunity to self-assess. Self-assessment is widely seen as acceptable for many<br />
aspects of the physical, social and occupational well-being domains. Caution should<br />
be exercised in relation to the psychological well being domain and not pursued in<br />
relation to the spiritual well-being domain since the latter in particular does not lend<br />
itself to self-assessment.<br />
Healthcare teams may wish to utilise one or more existing tools as part of a Holistic<br />
Needs Assessment; however, in all cases it must be ensured that the assessment<br />
covers the full range of needs listed in this guidance. An example of a suitable tool<br />
would be the <strong>PEPSI</strong> <strong>COLA</strong> documents (Appendix C). The <strong>East</strong> <strong>Midlands</strong> <strong>Cancer</strong><br />
<strong>Network</strong> also supports the use of the Distress Thermometer.<br />
All Holistic Needs Assessments should be documented and evidenced in the<br />
patient’s notes. This process should then be audited and the results acted upon to<br />
ensure care delivery is monitored and improved for safe effective delivery of patient<br />
care across the whole pathway as outlined in Appendix A.<br />
My learning space (www.mylearningspace.me.uk) has electronic competencies for<br />
both Key Worker and Holistic Needs Assessment and these can be accessed by the<br />
End of Life Care hub.<br />
For further information and access to downloadable documents please visit the <strong>East</strong><br />
<strong>Midlands</strong> <strong>Cancer</strong> <strong>Network</strong> website www.eastmidlandscancernetwork.co.uk<br />
17
15. References and bibliography<br />
Calman Hine (1995) A policy framework for commissioning cancer services: A report<br />
by the Expert Advisory Group on <strong>Cancer</strong> to the Chief Medical Officers of England<br />
and Wales. London: DOH<br />
<strong>Cancer</strong> Action Team (2007) Holistic Common Assessment of Supportive and<br />
Palliative Care Needs for Adults with <strong>Cancer</strong>: Assessment Guidance. London:<br />
<strong>Cancer</strong> Action Team<br />
Department of Health (2007) <strong>Cancer</strong> Reform Strategy. London: DOH<br />
<strong>East</strong> <strong>Midlands</strong> <strong>Cancer</strong> <strong>Network</strong> (2010) Policy for the Key Worker role in the<br />
management of adult patients with cancer<br />
National Institute for Clinical Excellence (2004). Guidance on cancer services:<br />
improving supportive and palliative care for adults with cancer. The manual.<br />
London: National Institute for Clinical Excellence<br />
Keri Thomas (2003) Caring for the Dying at Home<br />
Richardson A, Sitzia J, Brown V, Mediana A, (2005) Patients Needs Assessment<br />
Tools in <strong>Cancer</strong> Care; Principals and Practice. London. Kings College London<br />
16. Acknowledgements<br />
<strong>East</strong> <strong>Midlands</strong> <strong>Cancer</strong> <strong>Network</strong> Patient Partnership groups<br />
<strong>East</strong> <strong>Midlands</strong> <strong>Cancer</strong> <strong>Network</strong> Supportive and Palliative Care Service Improvement<br />
Facilitators<br />
<strong>East</strong> <strong>Midlands</strong> <strong>Cancer</strong> <strong>Network</strong> Supportive and Palliative Care group<br />
18
Appendices<br />
Appendix A - <strong>Cancer</strong> Patient Pathway<br />
Appendix B - <strong>PEPSI</strong> <strong>COLA</strong> Communication Pro-Forma<br />
Appendix C - Holistic Needs Assessment Template<br />
Appendix D - <strong>PEPSI</strong> <strong>COLA</strong> <strong>Aide</strong> <strong>Memoire</strong><br />
Appendix E - Distress Thermometer<br />
Appendix F - Patient Leaflet<br />
Appendix G - Priority 2 - Holistic Assessment of Patient Supportive & Palliative Care<br />
Needs<br />
19
Appendix A – <strong>Cancer</strong> Patient Pathway<br />
Key<br />
Secondary Care<br />
Primary Care<br />
information<br />
prescription discussed<br />
Key Worker<br />
CANCER PATIENTS PATHWAY<br />
RECOMMENDED STAGES FOR ALLOCATION OF KEY WORKER &<br />
HOLISTIC ASSESSMENT<br />
Holistic Needs Assessment<br />
Minimum Requirements<br />
Documented in relevant Medical, Nursing Notes / Verbal & Written Name & Contact Details of Key Worker<br />
Key Worker / Holistic Needs Assessment Information Leaflet<br />
+/- Consultant / G.P / District Nurses / Community Matron / Allied Health Care Professional / Macmillan Palliative Care CNS (if complex symptom management or<br />
other palliative care needs)<br />
DIAGNOSTIC<br />
INVESTIGATIONS<br />
Highly suspicious<br />
of cancer<br />
Key Worker = GP<br />
AROUND THE<br />
TIME OF<br />
DIAGNOSIS<br />
Key Worker = Site<br />
Specific CNS<br />
COMMENCEMENT<br />
OF TREATMENT<br />
Key Worker = Site<br />
Specific CNS<br />
COMPLETION OF<br />
TREATMENT<br />
Key Worker = GP /<br />
DN or Site Specific<br />
CNS if ongoing<br />
rehabilitation needed<br />
SURVIVORSHIP<br />
Key Worker = GP<br />
DISEASE<br />
RECURRENCE<br />
Key Worker = Site<br />
Specific CNS / GP /<br />
Community Nurse<br />
PALLIATIVE CARE<br />
(point of<br />
recognition of<br />
incurability)<br />
Key Worker = GP<br />
*Consider GSF &<br />
Advanced Care<br />
Planning<br />
END OF LIFE<br />
CARE<br />
Key Worker =<br />
Community /<br />
Hospice Nurse /<br />
Hospital Palliative<br />
Care CNS / GP<br />
‘Non-clinical’ information applies throughout the pathway as a minimum.<br />
For further information on these pathways see:<br />
<strong>East</strong> <strong>Midlands</strong> <strong>Cancer</strong> <strong>Network</strong> Guidelines for The Holistic Needs Assessment for adult patients with cancer (2010)<br />
<strong>East</strong> <strong>Midlands</strong> <strong>Cancer</strong> <strong>Network</strong> Policy for the Key Worker role in the management of adult patients with cancer (2010)<br />
NB: The patient can request without any explanation a change of their Key Worker<br />
This chart is designed to guide clinicians on the most appropriate healthcare professionals to act as the patients Key Worker at all stages in the cancer patients care pathway. In most cases the hospital site specific<br />
Clinical Nurse Specialist will be the Key Worker during the acute treatment stages. The GP, working in collaboration with other professionals, may be the Key Worker when patients are in the community. At the<br />
End Of Life the Key Worker may change depending on which care setting the patient is in i.e. home, hospice, hospital.<br />
20
Appendix B – <strong>PEPSI</strong> <strong>COLA</strong> Communication Pro-Forma<br />
<br />
Patient Name: GP Details:<br />
Address:<br />
NHS No:<br />
Hospital No:<br />
Completed by (name & designation) Contact Details:<br />
P<br />
Physical<br />
E<br />
Emotional<br />
P<br />
Personal<br />
Consider Date / Signature Patients<br />
needs<br />
are met<br />
• Symptom Control and use of tools<br />
• Medication – Regular/PRN<br />
• Compliance/stopping non essential<br />
treatments<br />
• Treatment/medication side effects<br />
• Alternative therapy referral<br />
• Understanding expectations of patient<br />
• Low mood, fears, anxieties, strengths<br />
• Coping mechanisms and interests<br />
• Altered body image<br />
• Relationships with others<br />
• Patient/family’s cultural background/ ethnic<br />
group<br />
• Needs related to spiritual wellbeing, ie:<br />
support structures, space to reflect/<br />
pray/quiet time<br />
• Patient’s concerns/desires future and<br />
present<br />
• Worries and challenges<br />
• Religious items<br />
____/____/____<br />
____/____/____<br />
____/____/____<br />
<br />
<br />
<br />
Kindly reproduced and adapted from the GSF toolkit 2004 by The Mount Vernon <strong>Cancer</strong> <strong>Network</strong><br />
Patients needs not met<br />
(what needs doing Action Plan)<br />
21
S<br />
Social<br />
Support<br />
Consider Date / Signature Patients<br />
needs<br />
are met<br />
• Care for carers<br />
• Practical/family support<br />
• Occupational/financial welfare support<br />
services<br />
• Social & recreational activities<br />
____/____/____<br />
<br />
I<br />
Information<br />
Communication<br />
• Identify the key team as per EMCN MDT<br />
policy<br />
• Liaison with MDT/PHCT or the receiving<br />
health care worker<br />
• Appropriate patient information leaflets<br />
____/____/____<br />
<br />
C<br />
Control<br />
O<br />
Out of Hours<br />
• Discussion around patient choice<br />
• Patient dignity<br />
• Treatment options/plans discussed<br />
• Preferred place of care documented<br />
• Advanced care planning<br />
• Communication to out of hours service<br />
(OOH)<br />
• Access to drugs/equipment<br />
• Ensure continuity of care<br />
____/____/____<br />
____/____/____<br />
<br />
<br />
L<br />
Living with<br />
your illness<br />
A<br />
After Care<br />
• Follow up care<br />
• Rehabilitation support<br />
• Patient/carer expectations<br />
• End of life care planning (if appropriate)<br />
• Liverpool Care Pathway<br />
• GSF register<br />
• Future support - family/patient<br />
• Discharge planning<br />
• Reassessment<br />
• Bereavement follow up<br />
____/____/____<br />
____/____/____<br />
<br />
<br />
Kindly reproduced and adapted from the GSF toolkit 2004 by The Mount Vernon <strong>Cancer</strong> <strong>Network</strong><br />
Patients needs not met<br />
(what needs doing Action Plan)<br />
22
Appendix C – Holistic Needs Assessment Template<br />
Holistic Needs Assessment Template<br />
Assessment information and preferences<br />
Date of last assessment<br />
The assessor should have copies of previous holistic<br />
assessments on file, should be aware of the needs identified in<br />
previous assessments, and should be aware of actions taken<br />
to address those needs<br />
Date of this assessment<br />
Name, role and contact details of assessor<br />
Key point / trigger<br />
Key point at which the assessment is being undertaken<br />
or the trigger for assessment (e.g. professional concerns,<br />
patient initiated, carer initiated)<br />
Site of this assessment<br />
Patient’s ability to participate in<br />
face-to-face assessment<br />
Sensitivities regarding assessment<br />
Willingness for assessment and consent<br />
Preference for family member or<br />
carer to be present at assessment<br />
The assessor should determine the patient’s:<br />
• Communication ability (hearing, vision, speech / voice /<br />
oral communication, use of alternative communication,<br />
language issues)<br />
• Cognitive ability (understanding, memory)<br />
Cultural sensitivities<br />
Current health/fatigue<br />
The assessor should determine the patient’s willingness to<br />
take part in assessment and also the patient’s willingness to<br />
‘self report’ where possible. This discussion should identify any<br />
cultural sensitivities regarding assessment, identify any<br />
reservations the patient might have, and generally identify any<br />
other barriers to assessment<br />
Demographic Information<br />
NHS number and other<br />
numbers<br />
Patient title (Mr, Ms, Mrs, Miss,<br />
Dr, Fr) other - specify<br />
Patient name<br />
Address - house number, road,<br />
locality, town, county, and<br />
postcode<br />
Preferred name<br />
Date of birth Age Gender<br />
Telephone numbers (land line<br />
and mobile)<br />
Marital status<br />
Religion<br />
Ethnicity<br />
Occupation (current or<br />
previous)<br />
23
Next of kin<br />
Relationship<br />
Address<br />
Telephone numbers (home, work, mobile)<br />
Other contacts (relationship,<br />
address, and telephone<br />
numbers)<br />
Identify who to call first in case<br />
of a crisis and whether they<br />
want to be contacted at night<br />
This has a legal meaning as well as a practical one - the next<br />
of kin may not be the person nominated by the patient to be<br />
telephoned first in case of crisis<br />
GP, practice address, telephone and fax<br />
number<br />
District Nurse, address, telephone and fax<br />
number<br />
Consultants (names and hospitals)<br />
Specialist palliative care nurses (hospital and<br />
community)<br />
Specialist nurses<br />
Social worker<br />
Other key professionals<br />
Clinical History<br />
Medical<br />
Diagnosis<br />
Primary site<br />
Site of metastases<br />
Month and year of diagnosis<br />
Tissue diagnosis (yes/no)<br />
Histology<br />
History of current illness<br />
(With dates/details of any surgery,<br />
chemotherapy, radiotherapy or endocrine<br />
therapy and response or adverse effects of<br />
these treatments)<br />
Past medical history<br />
Previous and current illnesses<br />
Drug history<br />
Allergies<br />
Resuscitation status<br />
This will need updating with each assessment<br />
Include all significant conditions e.g. non insulin dependent<br />
diabetes, ischemic heart disease.<br />
An accurate drug history that is regularly updated is essential.<br />
It is important to check what is and is not working and to go<br />
through patient’s concerns about their medication<br />
Teams have different ways of assessing this - a common way<br />
is for a doctor first to assess whether CPR would be futile, with<br />
a reason; if it is considered futile then many units do not go on<br />
to discuss it with the patient, unless they are known to want<br />
involvement in all clinical decisions. Often the question of CPR<br />
is raised within other discussions about future management<br />
and the aims of all treatments. The notes should say whether<br />
the matter has been directly discussed with the patient and/or<br />
their relatives (who should be named)<br />
24
Current problems<br />
Patient’s current problems discussed,<br />
including physical, psychological, social and<br />
spiritual problems.<br />
Specific tools such as pain assessment tools may be used<br />
Information needs<br />
Preferred language - need for interpreter<br />
‘Would it be helpful for you to have an interpreter from the<br />
hospital or community when we come to talk with you’ 'Are<br />
you comfortable with X from the family translating for you’<br />
Any aids to communication needed e.g.<br />
hearing aid, Light writer.<br />
Current insight<br />
‘What do you know about your illness at the moment’<br />
Amount of information wanted<br />
How information should be conveyed and with<br />
whom present<br />
As a rule do you like to have a lot of information about your<br />
illness, or just really general information “<br />
Are you the sort of person who likes to know everything about<br />
your illness or are you the sort of person who likes to leave<br />
things up to the doctors and nurses’<br />
‘How do you like to get information about your illness - face to<br />
face like this, or written down’ ‘Is there anyone you usually<br />
like to be with you if we have to tell you the results of tests or<br />
discuss treatments’<br />
Wants / does not want copies of treatment<br />
plans<br />
‘Would you like copies of the letters we write to your GP’<br />
Preferred amount of involvement in decisionmaking<br />
and management planning<br />
‘How much do you usually like to be involved in making<br />
decisions about your treatment”<br />
Consent for sharing information with<br />
family/carers<br />
‘Are you happy for your family to know details of your illness or<br />
treatments Is it all right if we answer their questions without<br />
you’<br />
Consent for sharing information with other<br />
professionals/ entering on patient record<br />
system.<br />
‘Are you happy for what we’ve discussed to be shared with<br />
other members of the team/other professionals such as your<br />
GP or District Nurse’<br />
Need to make sure they understand the extent the notes are<br />
shared.<br />
Social<br />
Practical living arrangements<br />
Work<br />
Finances<br />
Type of accommodation(house, flat), access (access to<br />
entrance, stairs), toilet and bathroom (upstairs,<br />
downstairs),transport, mobility in and out of house<br />
Whether in nursing home or residential home, or staying with<br />
relatives<br />
Ability to carry out household duties e.g. preparing food,<br />
shopping, cleaning, laundry, manage pets<br />
Any issues around work<br />
Any concerns about finances<br />
25
Benefits<br />
Legal arrangements<br />
Services involved<br />
Interests<br />
Patient receiving appropriate benefits Including DLA or Carer<br />
Allowance (under the special rules if prognosis less than 6<br />
months)<br />
E.g. Will made or not, Advance Decision to Refuse Treatment,<br />
Lasting Power of Attorney, plans for care/guardianship of<br />
children<br />
This should include all agencies involved when at home and<br />
some detail about the level of services provided. Does the<br />
patient attend day care Are patient and carer aware of the<br />
out of hour services available locally e.g. Rapid Response<br />
Services<br />
Identify things patient has had to give up because of illness<br />
Identify things patient would still like to do<br />
Habits<br />
Psychological<br />
Mood –Depression, anxiety, anger, despair<br />
Coping mechanism for illness<br />
Effect of illness – body image, on<br />
relationships, on interests.<br />
Spiritual<br />
Spiritual needs<br />
Religious needs<br />
Restrictions related to culture or belief system<br />
Rehabilitation needs<br />
Impact of illness on activities of daily living<br />
Smoking, drinking<br />
‘How are you feeling about all this’<br />
Use of the Distress thermometer)<br />
The distress thermometer adapted for EMCN attached as<br />
Appendix E can be used to measure distress but should only<br />
be used by health care professionals who have undertaken<br />
level 2 training<br />
‘How are you coping with all of this’<br />
‘How do you feel when you see yourself in the mirror’<br />
Consider using a spiritual need assessment proforma<br />
Start assessment with an introductory, exploratory<br />
question to determine patient’s existing faith/belief<br />
Someone to speak to: faith leader or minister e.g. chaplain,<br />
vicar, priest, imran, rabbi, church leader or other person<br />
Religious items e.g. religious texts, prayer mat, religious<br />
objects, holy water<br />
Things to help you practice e.g. chapel, prayer room, quiet<br />
room, ablution<br />
‘Do you belong to any church’<br />
Diet. Medicines. Treatment products e.g. blood products<br />
Consider using a scale such as Modified extended Activities of<br />
Daily Living<br />
Ability to carry out personal care e.g. wash and dress,<br />
personal hygiene, manage medication<br />
Dietary needs/preferences<br />
Ability to carry out key transfers e.g. get in and out of bed, on<br />
and off chairs, on and off toilet, in and out of bath/shower<br />
Mobility around house and outside<br />
Does the patient have specific dietary needs e.g. diabetic,<br />
gluten free, kosher, halal, vegetarian<br />
Specific tools may be helpful e.g. nutrition screening<br />
26
Complementary therapies<br />
Complementary therapies patients enjoys.<br />
Physical assessment of the patient<br />
Appropriate assessment by doctor, nurse and<br />
other<br />
health care professionals at the appropriate<br />
times<br />
Carer and family needs<br />
Name and relationship<br />
Insight into illness<br />
Any specific worries or concerns<br />
Level of involvement in care<br />
How other members of the family are coping<br />
e.g. children, elderly parents<br />
Needs – practical, emotional<br />
Sexual relations<br />
Bereavement needs<br />
Goals/Expectations<br />
Summary of problems and plans<br />
Advance care plans<br />
Advance statement<br />
Advance decision to refuse treatment<br />
Personal Welfare Lasting Power of Attorney<br />
See Appendix C for how to draw a genogram. The genogram<br />
should include family, children, and 'any significant others'<br />
Conflicts/communication issues within family<br />
Is help needed talking to children about cancer, does the<br />
school know of child’s relative’s illness, children coping<br />
Sexual difficulties caused by illness or treatment<br />
Patient’s concerns or desires regarding a goal they may want<br />
to achieve e.g attending a family wedding, going on holiday<br />
Expectations during the admission or visit should be checked<br />
regularly<br />
When you think it is appropriate, it is helpful to ask where the<br />
patient would like to die, then to record this and let other<br />
healthcare professionals know<br />
This should be a list of the major concerns of the patient - the<br />
things that are stopping them living in the way they would like.<br />
It is usual to list them in the patient's order of importance.<br />
Need to summarize plans to help with each problem<br />
A statement of wishes and preferences<br />
about their future management or place of care<br />
A specific refusal of treatment(s) in a predefined potential<br />
future situation<br />
Where another person has been given authority to make<br />
health and welfare decisions for a patient when they lose<br />
mental capacity<br />
End of Life care tools<br />
End of life care tools should be implemented as necessary –<br />
Gold Standards Framework, Liverpool Care Pathway<br />
27
GENOGRAMS<br />
Male ( died)<br />
Pregnancy<br />
Female (<br />
died)<br />
X or X Patient<br />
Married<br />
Separated<br />
Twins<br />
Divorced<br />
Cohabitng<br />
Homosexual<br />
Relationship<br />
Adoption<br />
1 st 2 nd 3 rd<br />
X<br />
1st, 2 nd and 3 rd Marriages<br />
Parents<br />
Ron Elsie Sam Tom Jim Mary Jack Joan<br />
X<br />
Live in<br />
Peter Ann Kim Joanna John James Sheila Emma Paul<br />
same house<br />
18 16 14 7 6 22 18 18 14<br />
It is important to keep each generation on its own line<br />
28
Appendix D – <strong>PEPSI</strong> <strong>COLA</strong> <strong>Aide</strong> <strong>Memoire</strong><br />
<strong>PEPSI</strong> <strong>COLA</strong> <strong>Aide</strong> <strong>Memoire</strong><br />
Consider Resources Refer on if Appropriate<br />
Symptom Control and use of tools<br />
Medication – Regular/PRN<br />
Compliance/stopping non essential<br />
treatments<br />
Treatment/medication side effects<br />
Alternative therapy referral<br />
Cue questions<br />
Elicit a description of problem<br />
Ascertain the effect<br />
History of management<br />
Ask patient if treatment is helping<br />
Has a pain chart been commenced<br />
Is a medication summary available Is it updated<br />
Specialist clinician<br />
Pharmacist<br />
Accredited therapist<br />
Specialist Palliative care team<br />
Hospice<br />
P<br />
Physical<br />
Understanding expectations of patient<br />
Low mood, fears, anxieties, strengths<br />
Coping mechanisms and interests<br />
Altered body image<br />
Relationships with others<br />
Cue questions:<br />
Is anything worrying you<br />
During the last month have you lost interest in things you<br />
usually enjoyed<br />
How do you normally cope in stressful situations<br />
Consider NICE – psychological levels of intervention and<br />
refer on appropriately<br />
Recommendation: level 2 practitioners to use an approved<br />
distress thermometer tool<br />
Have psychological/quality of life/genogram assessment<br />
tools been completed<br />
Follow the EMCN psychological<br />
competency pathway.<br />
Refer on to identified level, 3, 4<br />
practitioners if necessary.<br />
E<br />
Emotional<br />
Patient/family’s cultural background/<br />
ethnic group<br />
Needs related to spiritual wellbeing, ie:<br />
personal support structures, space to<br />
reflect/ pray/quiet time<br />
Patient’s concerns/desires both future<br />
and present<br />
Their worries and challenges<br />
Religious needs<br />
Cue questions (adapted from Peter Speck, questions<br />
2005)<br />
How do you make sense of what is happening to you<br />
What sources of strength do you look to when life is<br />
difficult<br />
Would you find it helpful to talk to someone who could help<br />
you explore the issues of spirituality/faith<br />
Awareness of Marie Curie spirituality competency<br />
framework<br />
Contact local spirituality lead if<br />
requested by patient<br />
Acute trust/hospice chaplains<br />
Palliative out of hours advice line if<br />
available locally<br />
<strong>Cancer</strong> patient information centre if<br />
available locally<br />
P<br />
Personal<br />
Care for carers<br />
Practical/family support<br />
Occupational/financial welfare support<br />
services<br />
Social & recreational activities<br />
Cue questions<br />
How are things in relation to:<br />
Managing at home etc, work and finance, family and close<br />
relationships, social and recreation<br />
Social services<br />
Local welfare rights advisor via<br />
local cancer patient information<br />
centres if available locally<br />
Citizens Advice Bureau<br />
S<br />
Social<br />
Support<br />
Kindly reproduced and adapted from the GSF toolkit 2004 by The Mount Vernon <strong>Cancer</strong> <strong>Network</strong><br />
29
<strong>PEPSI</strong> <strong>COLA</strong> <strong>Aide</strong> <strong>Memoire</strong><br />
Identify the key team as per EMCN<br />
MDT policy<br />
Liaison with MDT/PHCT or the<br />
receiving health care worker<br />
Appropriate patient information leaflets<br />
Have the key-worker/team details been informed to the<br />
patient and recorded in the patient held records<br />
Has a transfer of care form been completed<br />
Notification of the Key Worker sent to relevant Teams as<br />
appropriate<br />
Has the patient been informed of relevant information that<br />
is appropriate at this stage<br />
Has the patient been informed of any local support groups<br />
I<br />
Information<br />
Communication<br />
Discussion around patient choice<br />
Patient dignity<br />
Treatment options/plans discussed<br />
Preferred place of care documented<br />
Advanced care planning<br />
Consent form completed if appropriate<br />
Preferred place of care or advanced care planning tools<br />
used<br />
Kindly reproduced and adapted from the GSF toolkit 2004 by The Mount Vernon <strong>Cancer</strong> <strong>Network</strong><br />
<strong>Cancer</strong> patient information centres<br />
Patient information prescriptions<br />
Communication to Primary Health<br />
Care Team and entered on GSF<br />
register if appropriate<br />
O<br />
Out of Hours<br />
C<br />
Control<br />
Communication to out of hours service<br />
(OOH)<br />
Access to drugs/equipment<br />
Ensure continuity of care<br />
Are all emergency/out of hour’s numbers available to the<br />
patient/family<br />
Does the patient/family know what to do OOH<br />
Has a transfer of care form been forwarded to the OOH<br />
service If appropriate to your area<br />
Have the recommended anticipatory drugs been prescribed<br />
and dispensed<br />
Follow up care<br />
Rehabilitation support<br />
Patient/carer expectations<br />
End of life care planning (if<br />
appropriate)<br />
Liverpool Care Pathway<br />
GSF register<br />
Is the patient aware of the next steps<br />
Has the patient been informed of the rehabilitation support<br />
services available<br />
Has the patient had an opportunity to discuss their<br />
future/expectations<br />
Has the patient been considered to be registered on the<br />
GSF or LCP (if appropriate)<br />
Out of Hours Service<br />
Palliative care advice line centres,<br />
if available<br />
Liverpool Care Pathway<br />
commenced and symptom<br />
guidelines used appropriately<br />
Specialist allied health<br />
professionals<br />
Intermediate care services<br />
Palliative care teams<br />
Local cancer information and<br />
support services<br />
A<br />
After Care<br />
L<br />
Living with<br />
your illness<br />
Future support - family/patient<br />
Discharge planning<br />
Reassessment<br />
Bereavement follow up<br />
Has the patient/family relevant contact numbers<br />
Is the patient aware of how to re-establish contact<br />
Has the family been told of bereavement services<br />
available<br />
Contact patient information centres<br />
for further information<br />
30
Appendix E – Distress Thermometer<br />
Distress Thermometer<br />
1. PATIENT DETAILS INSTRUCTIONS<br />
Addressograph<br />
This tool is a simple method of identifying patient distress<br />
With the patient’s verbal consent and agreement please help to complete this<br />
form and the relevant action plan (see over) then file this in their notes.<br />
This is not intended to replace clinical assessment and discretion but is a guide to<br />
assisting/managing psychological/psychiatric distress related to cancer.<br />
The NICE guidelines for supportive and palliative care in cancer recommend<br />
screening patients at; diagnosis, commencement / completion of treatment,<br />
survivorship, disease recurrence, palliative care and end of life care as a minimum.<br />
Please indicate at what stage assessment completed<br />
Diagnosis Commencement of<br />
Treatment<br />
Completion of Treatment Survivorship<br />
DOB __/__/____<br />
2. DISTRESS THERMOMETER<br />
Male/Female<br />
Disease recurrence Palliative and end of life<br />
Instructions<br />
Please ask the patient to circle the number (0-10) that best describes how much distress in general<br />
they have been experiencing over the past week<br />
Does this represent a significant deterioration from ‘normal’<br />
Deteriorating No Change Improving<br />
3. CONCERNS CHECKLIST<br />
Instructions<br />
Please ask the patient to tick any of the following that has been a cause of distress over the past<br />
week, including today.<br />
Also ask the patient to identify the most pressing difficulties and to rank these in order of concern<br />
(1 st would be the biggest problem 4 th would be their fourth biggest concern).<br />
Practical Concerns Personal Concerns Emotional Concerns Physical Concerns<br />
Family Issues Appearance Anger / Irritability Breathing<br />
Issues with Health Staff Self-care Nervousness / Anxiety Eating / Weight<br />
Finances / Bills Loss of Independence Low in Mood Toileting<br />
Lack of Information Loss of Role Worry about <strong>Cancer</strong> Fatigue / Exhaustion<br />
Problems with Medication Sexual/Intimacy Issues Odd Experience Sleep Problems<br />
Spiritual Issues Memory / Concentration Nausea<br />
Others Self-esteem / Confidence Headaches<br />
Fears about Dying Pain<br />
MOST PRESSING CONCERNS<br />
(1 st ) (2 nd ) (3 rd ) (4 th )<br />
4. ACTION TAKEN FOR EACH CONCERN<br />
No Action No Action No Action No Action<br />
Declined Help Declined Help Declined Help Declined Help<br />
Help Given Help Given Help Given Help Given<br />
Referral Referral Referral Referral<br />
Other (state) Other (state) Other (state) Other (state)<br />
Clinician Name Designation Specialty Date<br />
Outcome/Referred to (describe)<br />
Please file with additional information in notes<br />
*Note – Practitioners using this tool must have the appropriate competencies and training in its use.<br />
31
1<br />
2<br />
3<br />
4<br />
Key Concerns / brief description<br />
TO BE COMPLETED BY STAFF<br />
Who is already helping Plan of Action Date Signature<br />
32
Appendix E continued<br />
33
Appendix F – Patient Leaflet<br />
What is it, and how will<br />
it affect my care<br />
Key Worker<br />
35
They might ask the following:<br />
How is the treatment going (if you<br />
are having treatment)<br />
What symptoms are bothering you<br />
How are you getting on with any<br />
medicines you’re taking<br />
How are you feeling, and are you<br />
worried about anything<br />
Have you got the support you need<br />
How are the family coping<br />
Your spiritual needs – are you<br />
managing to make sense of what’s<br />
happening Do you need to talk to<br />
someone If you have a religious faith,<br />
are you able to practice your faith<br />
Practical help: do you have money<br />
worries<br />
What will be done with the information<br />
First, you’ll develop a plan together saying<br />
what will happen next<br />
The plan could include a referral to another<br />
service, or information on benefits or support<br />
services, or some ideas to think through<br />
You should be given a summary of what<br />
you talked about, what you agreed<br />
and things that you or the healthcare<br />
professional will do<br />
The full discussion will be written down<br />
and kept safe in your personal NHS<br />
records, with your medical notes<br />
Sometimes, they will need to share<br />
information, so they can ask other services<br />
to help you, such as Social Services<br />
The healthcare professional will make sure you<br />
are happy about this before they pass on the<br />
information.<br />
© <strong>East</strong> <strong>Midlands</strong> <strong>Cancer</strong> <strong>Network</strong> 2010<br />
36
Appendix G – Priority 2 – Holistic Assessment of Patient Supportive &<br />
Palliative Care Needs<br />
(To be read in line with EMCN Holistic Needs Assessment guideline/core<br />
deliverables)<br />
NICE Recommendation: Assessment and discussion of patients’ needs for physical,<br />
psychological, social, spiritual and financial support should be undertaken at key<br />
points (such as at diagnosis; at commencement, during, and at the end of treatment;<br />
at relapse; and when death is approaching). <strong>Cancer</strong> <strong>Network</strong>s should ensure that a<br />
unified approach to assessing and recording patients’ needs is adopted, and that<br />
professionals carry out assessments in partnership with patients and carers.<br />
Core Deliverables<br />
<strong>Network</strong> level guidance in place, based on the national HNA specification, including<br />
identifying who (role) is the most appropriate person to undertake assessment in each care<br />
setting<br />
Agreed network-wide paper based (or electronic) tool in place for undertaking assessment.<br />
Note – many networks are using SPARC, Distress Thermometer, <strong>PEPSI</strong> <strong>COLA</strong><br />
Clear communication policy developed for information sharing following the assessment.<br />
Patients and carers are given written information on the holistic needs assessment process<br />
(how and who undertakes it) and also how/when to request one<br />
Process of offering assessment and uptake of assessment documented in patient notes<br />
Competencies in place for roles required to undertake assessment – EOLC assessment<br />
competencies developed by Skills for Health/Care recommended.<br />
Education and training strategy developed for HNA<br />
Education and training programme in place to ensure staff receive training in assessment in<br />
line with competencies<br />
<strong>Network</strong> wide audits, based on agreed HNA guidance, undertaken.<br />
Action plans in place as a result of the audits, (plans should be used to inform service<br />
developments)<br />
50 % of patients in secondary care offered assessment using network agreed approach<br />
(evidenced by audit being undertaken)<br />
By December 2009<br />
85-100% patients in secondary care offered assessment using network agreed approach<br />
(evidenced by audit being undertaken)<br />
Underpinning Processes:<br />
• The national holistic specification benchmarked against local assessment<br />
tools/frameworks<br />
• The network holistic needs assessment guidance/specification shared with all<br />
provider organisations and communicated to all relevant teams<br />
Keeping abreast of the National Common Assessment Framework and the<br />
implications arising out of that<br />
Improving the Supportive and Palliative Care of Adults with <strong>Cancer</strong> (2004)<br />
37