Differential Diagnosis - Pacific University
Differential Diagnosis - Pacific University
Differential Diagnosis - Pacific University
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
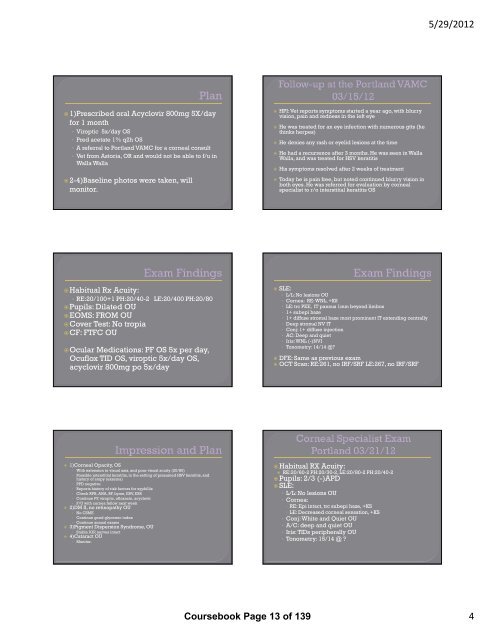
5/29/2012<br />
1)Prescribed oral Acyclovir 800mg 5X/day<br />
for 1 month<br />
• Viroptic 5x/day OS<br />
• Pred acetate 1% q2h OS<br />
• A referral to Portland VAMC for a corneal consult<br />
• Vet from Astoria, OR and would not be able to f/u in<br />
Walla Walla<br />
2-4)Baseline photos were taken, will<br />
monitor.<br />
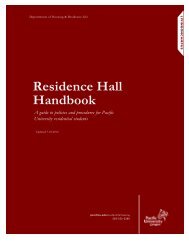
HPI: Vet reports symptoms started a year ago, with blurry<br />
vision, pain and redness in the left eye<br />
He was treated for an eye infection with numerous gtts (he<br />
thinks herpes)<br />
He denies any rash or eyelid lesions at the time<br />
He had a recurrence after 3 months. He was seen in Walla<br />
Walla, and was treated for HSV keratitis<br />
His symptoms resolved after 2 weeks of treatment<br />
Today he is pain free, but noted continued blurry vision in<br />
both eyes. He was referred for evaluation by corneal<br />
specialist to r/o interstitial keratitis OS<br />
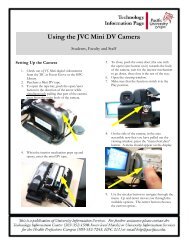
Habitual Rx Acuity:<br />
• RE:20/100+1 PH:20/40-2 LE:20/400 PH:20/80<br />
Pupils: Dilated OU<br />
EOMS: FROM OU<br />
Cover Test: No tropia<br />
CF: FTFC OU<br />
Ocular Medications: PF OS 5x per day,<br />
Ocuflox TID OS, viroptic 5x/day OS,<br />
acyclovir 800mg po 5x/day<br />
SLE:<br />
• L/L: No lesions OU<br />
• Cornea: RE: WNL, +KS<br />
• LE: trc PEE, IT pannus 1mm beyond limbus<br />
• 1+ subepi haze<br />
• 1+ diffuse stromal haze most prominent IT extending centrally<br />
• Deep stromal NV IT<br />
• Conj: 1+ diffuse injection<br />
• AC: Deep and quiet<br />
• Iris: WNL (-)NVI<br />
• Tonometry: 14/14 @<br />
DFE: Same as previous exam<br />
OCT Scan: RE:261, no IRF/SRF LE:267, no IRF/SRF<br />
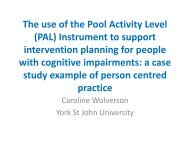
1)Corneal Opacity, OS<br />
• With extension to visual axis, and poor visual acuity (20/80)<br />
• Possible interstitial keratitis, in the setting of presumed HSV keratitis, and<br />
history of atopy (exzema)<br />
• PPD negative<br />
• Reports history of risk factors for syphillis<br />
• Check RPR, ANA, RF, Lyme, EBV, ESR<br />
• Continue PF, viroptic, ofloxacin, acyclovir<br />
• F/U with cornea fellow next week<br />
2)DM II, no retinopathy OU<br />
• No CSME<br />
• Continue good glycemic index<br />
• Continue annual exams<br />
3)Pigment Dispersion Syndrome, OU<br />
• Stable IOP, nerves intact<br />
4)Cataract OU<br />
• Monitor.<br />
Habitual RX Acuity:<br />
RE:20/60-2 PH:20/30-2, LE:20/80-2 PH:20/40-2<br />
Pupils: 2/3 (-)APD<br />
SLE:<br />
• L/L: No lesions OU<br />
• Cornea:<br />
• RE: Epi intact, trc subepi haze, +KS<br />
• LE: Decreased corneal sensation, +KS<br />
• Conj: White and Quiet OU<br />
• A/C: deep and quiet OU<br />
• Iris: TIDs peripherally OU<br />
• Tonometry: 15/14 @ <br />
Coursebook Page 13 of 139<br />
4