Differential Diagnosis - Pacific University
Differential Diagnosis - Pacific University
Differential Diagnosis - Pacific University
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
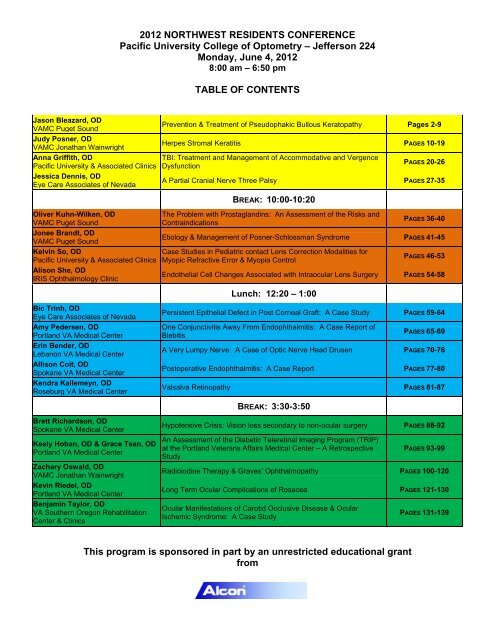
2012 NORTHWEST RESIDENTS CONFERENCE<br />
<strong>Pacific</strong> <strong>University</strong> College of Optometry – Jefferson 224<br />
Monday, June 4, 2012<br />
8:00 am – 6:50 pm<br />
TABLE OF CONTENTS<br />
Jason Bleazard, OD<br />
VAMC Puget Sound<br />
Judy Posner, OD<br />
VAMC Jonathan Wainwright<br />
Anna Griffith, OD<br />
<strong>Pacific</strong> <strong>University</strong> & Associated Clinics<br />
Jessica Dennis, OD<br />
Eye Care Associates of Nevada<br />
Oliver Kuhn-Wilken, OD<br />
VAMC Puget Sound<br />
Jonee Brandt, OD<br />
VAMC Puget Sound<br />
Kelvin So, OD<br />
<strong>Pacific</strong> <strong>University</strong> & Associated Clinics<br />
Alison She, OD<br />
IRIS Ophthalmology Clinic<br />
Prevention & Treatment of Pseudophakic Bullous Keratopathy Pages 2-9<br />
Herpes Stromal Keratitis PAGES 10-19<br />
TBI: Treatment and Management of Accommodative and Vergence<br />
Dysfunction<br />
PAGES 20-26<br />
A Partial Cranial Nerve Three Palsy PAGES 27-35<br />
BREAK: 10:00-10:20<br />
The Problem with Prostaglandins: An Assessment of the Risks and<br />
Contraindications<br />
PAGES 36-40<br />
Etiology & Management of Posner-Schlossman Syndrome PAGES 41-45<br />
Case Studies in Pediatric contact Lens Correction Modalities for<br />
Myopic Refractive Error & Myopia Control<br />
PAGES 46-53<br />
Endothelial Cell Changes Associated with Intraocular Lens Surgery PAGES 54-58<br />
Lunch: 12:20 – 1:00<br />
Bic Trinh, OD<br />
Eye Care Associates of Nevada<br />
Amy Pedersen, OD<br />
Portland VA Medical Center<br />
Erin Bender, OD<br />
Lebanon VA Medical Center<br />
Allison Coit, OD<br />
Spokane VA Medical Center<br />
Kendra Kallemeyn, OD<br />
Roseburg VA Medical Center<br />
Persistent Epithelial Defect in Post Corneal Graft: A Case Study PAGES 59-64<br />
One Conjunctivitis Away From Endophthalmitis: A Case Report of<br />
Blebitis<br />
PAGES 65-69<br />
A Very Lumpy Nerve: A Case of Optic Nerve Head Drusen PAGES 70-76<br />
Postoperative Endophthalmitis: A Case Report PAGES 77-80<br />
Valsalva Retinopathy PAGES 81-87<br />
BREAK: 3:30-3:50<br />
Brett Richardson, OD<br />
Spokane VA Medical Center<br />
Keely Hoban, OD & Grace Tsan, OD<br />
Portland VA Medical Center<br />
Zachary Oswald, OD<br />
VAMC Jonathan Wainwright<br />
Kevin Riedel, OD<br />
Portland VA Medical Center<br />
Benjamin Taylor, OD<br />
VA Southern Oregon Rehabilitation<br />
Center & Clinics<br />
Hypotensive Crisis: Vision loss secondary to non-ocular surgery PAGES 88-92<br />
An Assessment of the Diabetic Teleretinal Imaging Program (TRIP)<br />
at the Portland Veterans Affairs Medical Center – A Retrospective<br />
Study<br />
PAGES 93-99<br />
Radioiodine Therapy & Graves’ Ophthalmopathy PAGES 100-120<br />
Long Term Ocular Complications of Rosacea PAGES 121-130<br />
Ocular Manifestations of Carotid Occlusive Disease & Ocular<br />
Ischemic Syndrome: A Case Study<br />
PAGES 131-139<br />
This program is sponsored in part by an unrestricted educational grant<br />
from
Coursebook Page 1 of 139
5/29/2012<br />
Prevention, <strong>Diagnosis</strong>, and Management.<br />
Jason Bleazard, O.D.,<br />
American Lake Veterans’ Association, Tacoma, WA<br />
Five Layers<br />
(anterior to<br />
posterior)<br />
◦ Epithelium<br />
◦ Bowman’s<br />
Layer<br />
◦ Stroma<br />
◦ Descemet’s<br />
Membrane<br />
◦ Endothelium<br />
Endothelial cells are connected by gap<br />
junctions and macular occludens and thus<br />
make up a very slightly permeable membrane<br />
between the stroma and aqueous humor.<br />
Recall that the corneal endothelium is in fact a<br />
specialized epithelial layer. The base of the<br />
cells attach to Decemet’s, while the apices face<br />
the anterior chamber.<br />
• Water follows large molecules such as amino<br />
acids and glucose into the stroma.<br />
• The endothelial cells pump water out of the<br />
cornea via Sodium/Potassium ATP-ase pumps<br />
and aquaporins.<br />
• A compromised endothelium may lead to<br />
stroma edema<br />
• The endothelial cells of the cornea do not<br />
replicate.<br />
• It follows that adult corneas have a lower<br />
endothelial cell density than youngsters.<br />
• Damage to the endothelium further decrease<br />
endothelial cells counts.<br />
Coursebook Page 2 of 139<br />
1
5/29/2012<br />
Normal Endothelial<br />
Mosaic<br />
Corneal guttata<br />
Depositions of basement membrane in<br />
Descemet’s, cause thickening and bulging<br />
into the anterior chamber.<br />
Peripherally, these are termed Hassall-Henle<br />
bodies<br />
Centrally, the areas of thickening are called<br />
guttata<br />
Guttata represent thinning of the<br />
endotheilum as well as a thickened basement<br />
membrane.<br />
Guttata – “Spotted, speckled, or drop-like”<br />
Direct illumination of<br />
advanced Corneal<br />
guttata<br />
Elaphe<br />
Guttata<br />
A damaged endothelium has a reduced ability<br />
to pump water out of the stroma<br />
Fluid accumulates between the fibrils of the<br />
stroma, resulting in edema<br />
Stromal edema results in blurry vision and a<br />
painful eye<br />
Guttata alone do not warrant a diagnosis of<br />
Fuch’s, stromal edema must be present<br />
Endothelial cell density<br />
is critical in<br />
maintaining a properly<br />
hydrated cornea.<br />
In children, the<br />
average density is<br />
3,000-4,00/mm 2<br />
In adults, cell density<br />
ranges from 1,000-<br />
2,000/mm 2<br />
In order to maintain a<br />
functioning<br />
endothelium, 500<br />
cells/mm 2 are needed<br />
The exact mechanism of endothelial cell loss is<br />
unknown, however, there are a number of<br />
theories:<br />
◦ Histology has shown increasing amounts of apoptotic<br />
endothelial cells in Fuch’s patients. These corneas<br />
also show decreased anti-apoptosis gene expression.<br />
◦ UV light (gets blamed for everything) has been shown<br />
to induce DNA damage to endothelial cells. The longer<br />
you live, the more UV you will have been exposed to.<br />
◦ Fuch’s corneas have shown to have reduced<br />
expression of the aquaproin-1 protein. This is an<br />
integral protein in pumping fluid out of the cornea.<br />
• Mouse models have shown that decreased aquaporin-1<br />
expression results in slower recovery times in edematous<br />
corneas<br />
Coursebook Page 3 of 139<br />
2
5/29/2012<br />
Other factors that result in decreased endothelial<br />
cell numbers (occur in otherwise normal eyes):<br />
◦ Age<br />
◦ Previous ocular surgery<br />
◦ Ocular trauma or infection<br />
◦ Angle closure glaucoma<br />
◦ Pseudoexfoliation<br />
◦ Long-term contact lens wear<br />
◦ Sex- Filipino men had lower endothelial cells counts than<br />
women<br />
◦ Diabetes<br />
• 10 years or more results in decreased endothelial cell<br />
numbers and morphological changes.<br />
• Endothelial cell loss after phacoemulsification is higher in<br />
diabetics than normals<br />
While not all Fuch’s patients progress to<br />
bullous keratopathy, the risk for significant<br />
corneal damage such as that in PBK is real.<br />
Swelling of the cornea as a result of<br />
iotrogenic trauma to ocular tissues.<br />
PBK results in an extremely painful eye with<br />
significant reduction in visual function.<br />
Edema can be present in the stroma and the<br />
epithelium<br />
◦ Epithelial edema results<br />
in bullae, which are<br />
essentially corneal<br />
blisters.<br />
Subjective<br />
◦ Decreased vision<br />
◦ Pain<br />
◦ Epiphora<br />
◦ Foreign body sensation<br />
◦ Photophobia<br />
◦ Recent cataract surgery<br />
Patients with PBK can present with mild to<br />
severe findings on physical examination<br />
Corneal findings:<br />
◦ Corneal guttata<br />
◦ Folds in Descemet’s Membrane<br />
◦ Stromal edema<br />
◦ Stromal haze<br />
◦ Epithelial edema<br />
◦ Bullae- may be ruptured<br />
◦ Corneal neovascularization<br />
Coursebook Page 4 of 139<br />
3
5/29/2012<br />
Other Ocular Findings:<br />
◦ Cells/flare in anterior<br />
chamber<br />
◦ Subluxed IOL<br />
◦ Shunt tube w/ current or<br />
previous endothelial touch<br />
◦ Elevated IOP<br />
◦ Cystoid macular edema (CME)<br />
has been associated with PBK,<br />
especially in patients with an<br />
anterior chamber IOL<br />
As is the case with most conditions,<br />
treatment depends on the severity of the<br />
disease in each patient.<br />
Mild cases may respond to medical therapy,<br />
while moderate to severe cases often require<br />
surgery.<br />
Mild<br />
◦ Edema<br />
• Muro 128 (NaCl 5%) gtts QID<br />
• Muro 128 (NaCl 5%) ung QHS<br />
◦ Elevated IOP<br />
• Antiglacuoma medications<br />
• Avoid prostaglandin analogues to reduce risk of CME<br />
◦ CME<br />
• Treat as with other cases of CME<br />
Surgical procedures are dependent on the<br />
severity of the patient’s condition as well as<br />
their visual potential.<br />
Penetrating Keratoplasty Diagram<br />
If a patient is a cataract surgery candidate<br />
and has Fuch’s, measures must be taken to<br />
protect the cornea.<br />
For healthy corneas with guttata, viscoelastic<br />
should be used<br />
◦ Most surgeons use the soft-shell technique<br />
• Combines cohesive and dispersive viscoelastic<br />
◦ Viscoelastic protects the endothelium from the<br />
energy released during phacoemulsification as well<br />
as the trauma that is incurred during surgery<br />
Corneas with stromal edema take special care<br />
and consideration when cataract surgery is to<br />
be performed.<br />
If CCT is greater than 640um, a “Triple”<br />
procedure may be considered<br />
◦ Triple= Phacoemulsification+IOL implantation+cornea transplant<br />
If the patient elects for CE without a<br />
transplant, they MUST be educated that they<br />
will likely need one in the future.<br />
Coursebook Page 5 of 139<br />
4
5/29/2012<br />
For patients that qualify, the triple procedure<br />
is preferred-<br />
◦ One trip to operating room<br />
• Reduces cost<br />
• Less discomfort for patient<br />
• Low risk for future corneal decompensation<br />
◦ Cataract removed<br />
◦ Surgery is the only true definitive treatment for<br />
Fuch’s<br />
Penetrating Keratoplasty (PKP) is a full-thickness<br />
corneal transplant. Previously, it was the only<br />
surgical treatment for patients with advanced<br />
Fuch’s or PBK.<br />
PKP may be indicated in a plethora of conditions:<br />
• Fuch’s<br />
• PBK<br />
• Keratoconus<br />
• Failed grafts<br />
• Scarring<br />
• Corneal thinning<br />
• Corneal perforations<br />
While more surgeons are familiar with PKP,<br />
there are a fair amount of downsides to it…<br />
• Even in uncomplicated cases, Post-op is very<br />
involved -<br />
• Topical corticosteroids<br />
• QID*1mo<br />
• QD*6mo<br />
• Q o D *6mo<br />
• This may be altered (usually increased)<br />
• Systemic steroids or other immunosuppressants may<br />
be warranted as well<br />
• Endophthalmitis- most dreaded complication<br />
• Treated aggressively<br />
• Epithelial downgrowth<br />
• Wound Leak- requires immediate intervention<br />
• Epithelial defects (usually resolve w/ lubrication after a<br />
few weeks)<br />
• Glaucoma due to:<br />
• Infectious keratitis<br />
• Crystalline keratitis – usually 2’ streptococcus near suture<br />
• Graft rejection<br />
• 50% of rejection occurs w/in 6 mo<br />
• The rest usually occur w/in the next 6 mo<br />
• Most common type is also the most serious: Endothelial<br />
rejection<br />
• Tx= Repeat transplant<br />
• 10% are epithelial<br />
Nowadays, PKP is not always considered firstline<br />
treatment, and is more of a last-resort<br />
for PBK patients in the U.S.<br />
Newer techniques are proving to be quite<br />
effective and tend to have fewer side effects<br />
and less severe complications<br />
We will review some of the well-established<br />
procedures and introduce a few new ones as<br />
well<br />
DALK = Deep Anterior Lamellar Keratoplasty<br />
DSEK= Descemet Stripping Endothelial<br />
Keratoplasty<br />
◦ DSAEK= Descemet Stripping Automated Endothelial<br />
Keratoplasty<br />
◦ FS-DSEK= Femtosecond DSEK<br />
DMEK= Descemet Membrane Endothelial<br />
Keratoplasty<br />
◦ Transplantation of Decemet’s membrane and<br />
endothelium only<br />
PTK = Phototherapeutic Keratectomy<br />
Coursebook Page 6 of 139<br />
5
5/29/2012<br />
Began in 2003<br />
Descemet’s Membrane and endothelium is<br />
removed from the host cornea<br />
Small portion of posterior stroma along with<br />
Descemet’s and endothelium are harvested<br />
and transplanted on posterior surface of host<br />
cornea<br />
DSEK<br />
No corneal surface incisions<br />
Little post-op astigmatism<br />
Fewer suture related problems<br />
Less wound dehiscence<br />
Better, less variable visual<br />
outcomes<br />
Low rates of graft rejection<br />
Usually done after cataract surgery<br />
Higher endothelial density longterm<br />
PKP<br />
Significant corneal incisions<br />
High and variable astigmatism<br />
High rates of suture problems<br />
Wound dehiscence<br />
Variable, poor visual outcomes<br />
Higher (double) graft rejection<br />
rates<br />
Done before cataract surgery<br />
Lower cell denisty<br />
In Koenig’s study, patients went from an<br />
average of 20/100 preoperatively to 20/40<br />
postoperatively @ 6 months.<br />
DSEK and DSAEK have shown promising longterm<br />
outcomes.<br />
◦ Li’s study showed steady improvement in BCVA<br />
from 6-12 months, from 12-24 months, and from<br />
24-36 months, with a mean BCVA of 20/25.<br />
◦ Ratanasit et al. showed 75% of patients were<br />
20/20-20/40 @ 5 years, and not one patient lost<br />
vision.<br />
Successful In vitro<br />
Descemet’s Membrane<br />
transplantation in 1998,<br />
2002<br />
Descemet’s and<br />
endothelium removed<br />
from both host and<br />
donor.<br />
Both Descemet’s and<br />
endothelium are<br />
transplanted to host<br />
cornea<br />
No stroma<br />
In vivo DMEK in 2006<br />
◦ Single case- 20/20 vision<br />
one week post-op<br />
DMEK carries most of the same risks as DSEK<br />
DMEK patients are more likely to experience a<br />
graft dislocation.<br />
◦ Over 50% of patients had a dislocation<br />
◦ In DMEK, dislocations are partial<br />
◦ Partial dislocations require re-bubbling and are<br />
relatively simple to correct<br />
Price et al (60 eyes, two surgeons, both were<br />
brand new to DMEK)<br />
◦ Mean BCVA was 20/30 @ one month<br />
• 84% were 20/40 or better<br />
◦ Mean BCVA @ 3 months was 20/25<br />
• 94% were 20/40 or better<br />
• 63% were 20/25 or better<br />
Coursebook Page 7 of 139<br />
6
5/29/2012<br />
DMEK<br />
Better refractive predictability<br />
DSEK<br />
Fair predictability – Host stroma<br />
adds to corneal thickness<br />
Thinner post-op CCT (528um) Thicker post-op CCT (650um)<br />
Endothelial cell density equal ---<br />
Tearing of donor tissue<br />
Less likely to tear<br />
Can use one donor cornea for<br />
DMEK + DALK<br />
No hyaluronic acid- lower<br />
host/donor interface issues<br />
Lower start-up cost<br />
Can only use donor cornea for<br />
DSEK<br />
Need to use hyaluronic acid<br />
Higher start-up cost<br />
(microkeratom)<br />
Done by many corneal surgeons<br />
Fewer experienced surgeons<br />
Partial graft detachments common Graft detachment rare (2-3%)<br />
Using 20/40 or better @ 6-12 months<br />
post-op as a benchmark:<br />
38-100% of DSEK pts<br />
◦ Few reach 20/25<br />
40% of PKP pts<br />
95% of DMEK pts<br />
◦ 75% reached 20/25<br />
◦ Most are 20/40 on the day of surgery<br />
Post-op endothelial cell density is reduced in<br />
both DSEK and DMEK. This is due to (1) cell loss<br />
during dissection and (2) endothelial damage<br />
while the graft is being handled before and<br />
during surgery.<br />
DMEK and DSEK are comparable in cell counts<br />
◦ 25-54% loss 6 mo Post op in DSEK<br />
◦ 24-61% 1 yr post op in DSEK<br />
◦ 30% loss at 1 yr in DMEK<br />
◦ 40% 1 yr post op in PKP<br />
Even with all the cell loss, most corneas are well<br />
above the 500/mm 2 cutoff.<br />
For patients with limited visual potential<br />
unrelated to the cornea, phototherapuetic<br />
keratectomy (PTK) is a good option for pain<br />
management.<br />
Collagen cross-linking has shown some<br />
potential for pain management, but longterm<br />
results are lacking.<br />
It may be possible to inject prepared<br />
endothlial cells into the anterior chamber as<br />
they have shown the ability to migrate onto<br />
the posterior surface of the cornea.<br />
PKP is well-established, but has more serious<br />
and frequent complications and poorer visual<br />
outcomes<br />
DSEK/DSAEK provides for predictable<br />
outcomes but requires a long wait-time<br />
before visual acuity is optimal<br />
DMEK is new and looks promising, however<br />
there are few surgeons who will do it and<br />
graft dislocations are common.<br />
PBK causes painful vision loss<br />
It is largely avoidable<br />
Careful examination, proper patient<br />
education, and appropriate surgical care are<br />
necessary to avoid PBK<br />
DSEK is the most common option for<br />
treatment of PBK or use in a tirple procedure<br />
DMEK has shown very promising results and<br />
will be implemented in many surgical centers<br />
Coursebook Page 8 of 139<br />
7
5/29/2012<br />
Ehlers, Justis P., et al. The Wills Eye Manual: Office and Emergency Room <strong>Diagnosis</strong><br />
and Treatment of Eye Disease, Fifth Edition. Baltimore, Lippincott Williams &<br />
Wilkins, 2008.<br />
Ghanem, Santhiago, Berti, Thomaz, Netto “Collagen crosslinkin with riboflavin and<br />
ultraviolet-A in eyes with pseudophakic bullous keratopathy.” Journal of Cataract<br />
& Refractive<br />
Surgery. 36.2. (2010).<br />
Kanski, Jack J. Clinical Opthalmology: A Sytematic Approach, Seventh Edition.<br />
Elsevier Saunders, 2011.<br />
Koenig, Steven B., Covert, Douglas J., Dupps, William J., Meisler, Daivd M. “Visual<br />
Acuity, Refractive Error, and Endothelial Cell Density Six Months After Descemet<br />
Stripping and Automated Endothelial Keratoplasty (DSAEK).” Cornea. 26.6 (2007).<br />
Li, Jennifer Y., Terry, Mark A., Goshe, Jeffrey, Davis-Boozer, David, Shamie, Neda. “<br />
Three-Year Visual Acuity Outcomes after Descemet’s Stripping Automated<br />
Endothelial Keratoplasty.” Ophthalmology. March 2012.<br />
Lin, Pei-Yu, Wu, Chih-Chiau, Lee, Shui-Mei. “Combined phototherapeutic<br />
keratectomy and therapeutic contact lens for recurrent erosions in bullous<br />
keratopathy. British Journal of Ophthalmology. 85 (2001).<br />
Milla, Elena, Verges, Carlos, Cipres, Maricruz. “Corneal Endothelium Evaluation<br />
After Phacoemulsification With Continuous Anterior Chamber Infusion.”Cornea.<br />
24.3 (2005).<br />
Price, Marianne O., Giebel, Arthur W., Fairchild, Kelly M., Price, Francis W.<br />
“Descemet’s Membrane Endothelial Keratoplasty: Prospective Multicenter Study of<br />
Visual and Refractive Outcomes and Endothelial Survival.” Ophthalmology. 116.12<br />
(2009).<br />
Ratanasit, Arlene, Gorovoy, Mark S. “Long-term Results of Decemet Stripping<br />
Automated Endothelial Keratoplasty.” Cornea. 30.12 (2011).<br />
Rosado-Adames, Noel, Afshari, Natalie A. Current Opinion in Ophthalmology. 23.1<br />
(2012).<br />
Remington, Lee Ann. Clinical Anatomy of the Visual System, Second Edition. T.<br />
Louis. Elsevier, 2005.<br />
Ruggeri, A, Grisan, E., Jaroszeski, J. “A new system for the automatic estimation of<br />
endothelial cell density in donor corneas.” British Journal of Ophthalmology. 89<br />
(2005).<br />
Seitzman, Gerami D. “Cataract Surgery in Fuch’s Dystrophy.” Current Opinion in<br />
Ophthalmology. 16 (2005).<br />
Wollensak, Aurich, Wirbelauer, Pham. “Potential Use of Riboflavin/UVA Cross-<br />
Linking in Bullous Keratopathy.” Ophthalmic Research. 41.2 (2009).<br />
Coursebook Page 9 of 139<br />
8
5/29/2012<br />
A Case Presentation<br />
Case Presentation<br />
Introduction to Stromal keratitis<br />
• Immune Stromal Keratitis (ISK) defined<br />
• Necrotizing versus Non-necrotizing<br />
Pathophysiology of the disease<br />
Epidemiology<br />
Workup<br />
Landmark Studies – HEDS I and II<br />
Current therapies<br />
• Including surgery<br />
Conclusion/Clinical Pearls<br />
65 YOWM new patient presented for a<br />
consult for a CVE<br />
The consult was placed by their PCP for<br />
vision changes thought to be related to<br />
hyperbaric O2 treatments 2/2 a bleeding<br />
bladder from radiation cystitis<br />
• Vet was initially given radiation therapy for<br />
prostate cancer<br />
• Last tx received 04/11- total of 40 tx that started<br />
in 02/11<br />
Overview: Hyperbaric oxygen therapy<br />
(HBOT) is breathing 100% oxygen while<br />
under increased atmospheric pressure<br />
HBOT is generally performed daily for a<br />
minimum of 30 treatments<br />
• Treatment is typically at 2 to 2.4 ATA for a total<br />
of 90 minutes<br />
• ATA = atmosphere absolute<br />
• 1 ATA= atmospheric pressure at sea level<br />
Delayed radiation injury (soft tissue and<br />
bony necrosis) **<br />
Diabetic retinopathy<br />
Diabetic foot<br />
Carbon monoxide poisoning<br />
Decompression sickness<br />
Selected problem wounds<br />
Coursebook Page 10 of 139<br />
1
5/29/2012<br />
Increase in myopia*<br />
Improvement in hyperopia<br />
Vision changes more common after 20<br />
treatments and in patients >40 years old<br />
This is usually temporary and in the<br />
majority of patients, vision returns to its<br />
pre-treatment level about six weeks after<br />
the cessation of therapy<br />
CC: Decreased vision at distance OU, that<br />
occurred suddenly after receiving O2 treatments<br />
LEE: ~ 08/11 with Dr. X (a non-VA provider);<br />
07/13/11 CVE at the Portland VAMC<br />
Current Ocular Medications: Prednisone TID OS<br />
prescribed initially by Dr. X for an “abrasion”<br />
and a “viral infection” that he has been using<br />
intermittently since ~08/11 (renewed by his PCP)<br />
– had been off for 1 month and was about to<br />
restart<br />
Personal OHx: corneal abrasion OS with a<br />
viral infection dx ~8/11<br />
Family OHx: Unremarkable<br />
Pertinent Medical Conditions: DM II,<br />
COPD, Vitamin D deficiency, prostate<br />
cancer<br />
Autorefractor:<br />
• RE:-1.25-0.75x091 LE:-1.75-1.00x013<br />
Current Spec Rx: Bifocals<br />
• RE:-0.50DS 20/60 PH:20/40<br />
• LE:-0.25-0.75x033 20/150 PH:20/80<br />
• ADD:+2.50<br />
Pupils: PERRL (-)APD OU<br />
EOMS:FROM OU<br />
CF:FTFC OU<br />
SLE:<br />
• L/L: BE: flakes, lower lid laxity w/ mild proptosis<br />
• Conj: BE: Ping N&T LE:1+ diffuse injection temp<br />
• Cornea:BE: arcus 360 w/ krukenberg spindles<br />
• LE: central areas of white patchy stromal haze<br />
• Sectoral deep stromal NV from ~3:00-5:00<br />
• Central folds and SEI, bullae superior cornea<br />
• (+)staining over the neo with stromal filling<br />
• A/C: Deep and Quiet OU<br />
• Iris: Normal w/o NVI OU<br />
• Tonomtery by Applanation: 15/16 @ 15:48<br />
Coursebook Page 11 of 139<br />
2
5/29/2012<br />
DFE:<br />
Periphery: Attached 360 w/o holes/tears<br />
Lens: RE: 1+ milky NS w/ vacuoles LE:1-2+<br />
milky NS<br />
Vitreous: BE: syneresis<br />
Optic Nerve C/D ratio: RE:0.35 rd HRT<br />
LE:0.40 shallow HRT<br />
Macula: Flat and Dry OU LE: hazy view 2/2<br />
cornea<br />
Vessels:1:2 with moderate tortuosity and<br />
threadlike arterioles<br />
1)Left Eye Stromal Keratitis with stromal<br />
edema – likely related to Herpes virus<br />
per patient history with Dr. X<br />
2)Bilateral Nuclear Sclerotic Cataracts<br />
3)Diabetes Type II without retinopathy<br />
OU<br />
4)Bilateral Retinal Vascular Changes –<br />
likely related to hyperbaric treatments<br />
received back in April<br />
Coursebook Page 12 of 139<br />
3
5/29/2012<br />
1)Prescribed oral Acyclovir 800mg 5X/day<br />
for 1 month<br />
• Viroptic 5x/day OS<br />
• Pred acetate 1% q2h OS<br />
• A referral to Portland VAMC for a corneal consult<br />
• Vet from Astoria, OR and would not be able to f/u in<br />
Walla Walla<br />
2-4)Baseline photos were taken, will<br />
monitor.<br />
HPI: Vet reports symptoms started a year ago, with blurry<br />
vision, pain and redness in the left eye<br />
He was treated for an eye infection with numerous gtts (he<br />
thinks herpes)<br />
He denies any rash or eyelid lesions at the time<br />
He had a recurrence after 3 months. He was seen in Walla<br />
Walla, and was treated for HSV keratitis<br />
His symptoms resolved after 2 weeks of treatment<br />
Today he is pain free, but noted continued blurry vision in<br />
both eyes. He was referred for evaluation by corneal<br />
specialist to r/o interstitial keratitis OS<br />
Habitual Rx Acuity:<br />
• RE:20/100+1 PH:20/40-2 LE:20/400 PH:20/80<br />
Pupils: Dilated OU<br />
EOMS: FROM OU<br />
Cover Test: No tropia<br />
CF: FTFC OU<br />
Ocular Medications: PF OS 5x per day,<br />
Ocuflox TID OS, viroptic 5x/day OS,<br />
acyclovir 800mg po 5x/day<br />
SLE:<br />
• L/L: No lesions OU<br />
• Cornea: RE: WNL, +KS<br />
• LE: trc PEE, IT pannus 1mm beyond limbus<br />
• 1+ subepi haze<br />
• 1+ diffuse stromal haze most prominent IT extending centrally<br />
• Deep stromal NV IT<br />
• Conj: 1+ diffuse injection<br />
• AC: Deep and quiet<br />
• Iris: WNL (-)NVI<br />
• Tonometry: 14/14 @<br />
DFE: Same as previous exam<br />
OCT Scan: RE:261, no IRF/SRF LE:267, no IRF/SRF<br />
1)Corneal Opacity, OS<br />
• With extension to visual axis, and poor visual acuity (20/80)<br />
• Possible interstitial keratitis, in the setting of presumed HSV keratitis, and<br />
history of atopy (exzema)<br />
• PPD negative<br />
• Reports history of risk factors for syphillis<br />
• Check RPR, ANA, RF, Lyme, EBV, ESR<br />
• Continue PF, viroptic, ofloxacin, acyclovir<br />
• F/U with cornea fellow next week<br />
2)DM II, no retinopathy OU<br />
• No CSME<br />
• Continue good glycemic index<br />
• Continue annual exams<br />
3)Pigment Dispersion Syndrome, OU<br />
• Stable IOP, nerves intact<br />
4)Cataract OU<br />
• Monitor.<br />
Habitual RX Acuity:<br />
RE:20/60-2 PH:20/30-2, LE:20/80-2 PH:20/40-2<br />
Pupils: 2/3 (-)APD<br />
SLE:<br />
• L/L: No lesions OU<br />
• Cornea:<br />
• RE: Epi intact, trc subepi haze, +KS<br />
• LE: Decreased corneal sensation, +KS<br />
• Conj: White and Quiet OU<br />
• A/C: deep and quiet OU<br />
• Iris: TIDs peripherally OU<br />
• Tonometry: 15/14 @ <br />
Coursebook Page 13 of 139<br />
4
5/29/2012<br />
1)presumed HSV stromal keratitis OS.<br />
Clincal appearance consistent. RPR, ANA,<br />
RF, EBV, ESR, wnl.<br />
• h/o atopy<br />
• Continue PF qid<br />
• Reduce acyclovir to 400mg po bid<br />
• d/c viroptic<br />
• d/c ocuflox<br />
• Return 4 wks, MRx next visit<br />
Herpes Simplex Type I and Type II<br />
Cytomegalovirus<br />
Epstein-Barr Virus<br />
VZV<br />
Ocular herpes affects each corneal layer differently<br />
and can vary in presentation as categorized below:<br />
• Corneal epithelial disease<br />
• Dendritic keratitis<br />
• Geographic (ameboid) ulcer<br />
• Marginal keratitis (limbitis)<br />
• Corneal Stromal Disease**<br />
• Necrotizing<br />
• Non-Necrotizing<br />
• Disciform, immune rings, limbal vasculitis<br />
• Endothelitis<br />
• Neurotrophic keratopathy 4,5<br />
Management depends on the layer affected<br />
By definition - “Immune” refers to the fact that<br />
typically at this corneal level, the virus has been<br />
reactivated and the patient has developed an<br />
immunity/humoral response<br />
The immune reaction represents a delayed<br />
hypersensitivity reaction by T lymphocytes to<br />
viral antigen<br />
There are two types of ISK that may occur during<br />
herpes infection:<br />
• Necrotizing and Non-necrotizing<br />
Presenting signs and symptoms:<br />
• Reduced vision<br />
• Pain<br />
• Photophobia<br />
• Lacrimation<br />
• Blepharospasm<br />
• Decreased corneal sensation<br />
Presentation may be either unilateral or<br />
bilateral<br />
A history of prior episodes in patients with<br />
recurrent disease may exist<br />
There may be single or multiple patches of infiltration and inflammation<br />
within the corneal stroma<br />
<br />
Typically concurrent stromal edema<br />
Stromal neovascularization may be present but is not necessary for the<br />
diagnosis<br />
<br />
The overlying epithelium is usually intact<br />
If there is epithelial disruption, it will be much smaller in area than the<br />
underlying inflammation<br />
The inflammatory deposits are thought to represent complexes of viral<br />
antigen with antibodies and complement – may take the form of a ring<br />
infiltrate (Wessely ring)<br />
<br />
<br />
Secondary anterior uveitis may be present<br />
Endothelial folds and keratic precipitates are common<br />
Coursebook Page 14 of 139<br />
5
5/29/2012<br />
Corneal thinning - secondary to chronic<br />
inflammation<br />
Corneal Scarring – secondary to stromal<br />
neovascularization that can result in<br />
profound vision loss**<br />
Fibrosis, pannus, and lipid deposits from<br />
stromal neovascularization<br />
Occurs in 20-60% of eyes with recurrent HSV, and<br />
90% of recurrent stromal keratitis 3,4<br />
It does not usually move toward ulceration and<br />
perforation<br />
Untreated non-necrotizing ISK runs a self-limiting<br />
course over several months; however if left<br />
untreated severe vascularization and scarring<br />
can result in profound vision loss thus treatment<br />
is indicated 7<br />
More severe form of herpetic stromal keratitis<br />
• Manifests as dense, cheesy, yellow-white stromal infiltration<br />
• Epithelial ulceration<br />
• Stromal edema<br />
• Dense vascularization<br />
• Profound corneal thinning<br />
• Possible perforation (major complication)**<br />
The use of topical corticosteroids without antiviral<br />
coverage may be a possible risk factor for its<br />
development<br />
It is much less common than the non-necrotizing type<br />
Coursebook Page 15 of 139<br />
6
5/29/2012<br />
Occurs mainly by 2 mechanisms:<br />
1) Reactivation of the virus in the trigeminal<br />
ganglion<br />
• Migrates down the nerve axon to replicate and<br />
infect ocular tissue<br />
2) The cornea itself<br />
• The virus may subsist latently within corneal tissue<br />
(stromal keratocytes) and reactivate<br />
• May also cause donor-derived HSV disease in<br />
transplanted corneas<br />
Conditions causing ISK include:<br />
• Herpes simplex and zoster<br />
• Epstein-Barr virus<br />
• Syphillis<br />
• Tuberculosis<br />
• Lyme disease<br />
• Mumps and measles<br />
• Acanthamoebe<br />
• Sarcoidosis<br />
• Onchocerciasis<br />
• Idiopathic<br />
The most common cause of active ISK is the herpes<br />
simplex virus, accounting for 70% of unilateral<br />
cases 2<br />
Frequency<br />
• United States<br />
• 80-90% of the US population has been infected with the<br />
herpes virus – many with no history of clinical herpes<br />
• ~ 20,000 new cases of ocular HSV occur annually<br />
• >28,000 reactivations occur annually<br />
• ~24% - 36% of patients with ocular disease will<br />
experience recurrence within 2-5 years after the first<br />
episode***<br />
• International<br />
• An estimated 1/3 of the population worldwide suffers<br />
from recurrent infections 7<br />
Mortality/Morbidity<br />
• HSV keratitis IS THE MOST FREQUENT cause of corneal<br />
blindness in the United States<br />
• A leading indication for corneal transplantation<br />
• Most common cause of infectious blindness in the<br />
Western world<br />
Age<br />
• Affects mainly adults, and occurs many years after the<br />
primary infection<br />
• In children it involves the corneal epithelium<br />
• Risk of binocular disease<br />
• A high recurrence rate<br />
• Amblyopia<br />
Corneal Abrasion<br />
Recurrent Corneal Erosion<br />
Herpes Zoster<br />
Bacterial Keratitis<br />
Fungal Keratitis<br />
Interstitial Keratitis<br />
Keratoconjunctivitis Sicca<br />
Corneal Ulcer<br />
Coursebook Page 16 of 139<br />
7
5/29/2012<br />
<strong>Diagnosis</strong> is primarily made based<br />
on clinical features of the corneal<br />
lesion **<br />
Epithelial scrapings with Giemsa<br />
stain:<br />
• Show multinucleated giant cells<br />
• Which are coalesced infected<br />
corneal epithelial cells and<br />
intranuclear viral inclusions 7<br />
viral DNA can be detected in the:<br />
• Corneal epithelium<br />
• Conjunctiva<br />
• Skin<br />
• Anterior chamber tap<br />
Negative cytology results do not<br />
exclude HSV infection<br />
Classic case of a multinucleated herpes simplex virus-infected cell 17<br />
Enzyme-linked virus inducible system<br />
(ELVIS)<br />
• Very specific for detecting herpes virus<br />
• Results in 24hrs!<br />
ELVIS test result is negative<br />
• Cell culture for confirmation is recommended<br />
Cultures obtained within several days of onset, prior to<br />
antiviral therapy give a sensitivity of up to 70%<br />
Enzyme immunoassay (EIA) tests can be<br />
performed in the office<br />
• HerpChek<br />
The Captia test (Trinity Biotech) is a<br />
blood test to detect antibodies to the HSV<br />
• Unlike other tests it can differentiate between<br />
HSV -1 and HSV-2<br />
Combined CORTICOSTEROID and antiviral therapy –<br />
• Viroptic or Zirgan and Pred acetate 1%<br />
• Acyclovir 3% ophthalmic ointment is available in Europe but not in the US<br />
• Cycloplegia and topical lubricants are used to ease patient discomfort<br />
Dosing<br />
• Viroptic (trifluridine 1%) dosing – q2h up to a maximum 9x/day for 7-14 days, then QID for<br />
1-2 days after complete epitheliazation (not to exceed 21 days due to toxicity)<br />
<br />
• Zirgan (ganciclovir 0.15%)- q3h up to 5x/day typically 7-10 days–then taper to 1-3x/day<br />
for 7 days<br />
• Pred acetate 1% q1-2h initially then tapered<br />
One common recommendation is:<br />
• Equal frequency of topical antiviral with a corticosteroid<br />
Conducted by the National Eye Institute<br />
Herpetic Eye Disease Study (HEDS) I – 1996<br />
• Focused on stromal keratitis treatment<br />
• Anti-viral alone<br />
• Anti-viral + corticosteroid<br />
• Anti-viral + corticosteroid + acyclovir<br />
Herpetic Eye Disease Study (HEDS) II- 1998<br />
• Focused on epithelial disease<br />
• Looked at early treatment with acyclovir if it prevented progression to stromal<br />
disease<br />
• Patients with previous HSV disease not active within 30 days, if longterm<br />
low dose treatment with acyclovir prevented recurrence<br />
Focused on stromal keratitis (3 groups)<br />
• Anti-viral alone<br />
• Anti-viral + corticosteroid<br />
• Anti-viral + corticosteroid + acyclovir<br />
Results<br />
1. Duration of inflammation and risk of progression were<br />
significantly reduced in patient’s receiving prednisolone<br />
2. The rate of epithelial HSV recurrence was not increased<br />
3. The addition of oral acyclovir to topical corticosteroid and<br />
topical antivirals provided no additional benefit**<br />
• The role of external factors in triggering recurrence<br />
Coursebook Page 17 of 139<br />
8
5/29/2012<br />
<br />
3 Main Studies:<br />
1. Acute Epithelial HSV Keratitis<br />
Study:<br />
• Early tx with oral acyclovir<br />
prevented progression to stromal<br />
disease<br />
2. Acyclovir Prevention Trial:<br />
• If long-term tx with low dose oral<br />
acyclovir (400mg BIDx1yr)<br />
prevented recurrence<br />
3. Ocular HSV Recurrence Factor<br />
Study – looked at triggers<br />
• Patients filled out questionnaires<br />
every week for 52 weeks to track<br />
acute and chronic stressors<br />
<br />
Results:<br />
1. There was no benefit from<br />
addition of oral acyclovir to<br />
preventing progression to<br />
stromal keratitis<br />
2. 41% reduction that any ocular<br />
herpetic disease would recur<br />
• 50% reduction in stromal keratitis<br />
3. There are no results available<br />
yet<br />
Topical cyclosporin A 0.05% showed some<br />
effectiveness in cases of HSK resistant to<br />
corticosteroids<br />
• It improves visual acuity<br />
• Reduces inflammation and lesion size<br />
• Regression of corneal stromal neovascularization 12<br />
• Contraindicated with active epithelial herpes keratitis<br />
Antiangiogenic agents, such as Avastin<br />
A therapeutic vaccine designed to boost<br />
protective CD8 T-cell population within HSV<br />
latently affected ganglia<br />
A triple-drug therapy targeting viral<br />
replication with:<br />
• Oral acyclovir<br />
• Topical cyclosporin A<br />
• Anti-VEGF<br />
Randomized clinical trials needed<br />
Penetrating Keratoplasty (PK)*<br />
Deep Anterior Lamellar Keratoplasty<br />
(DALK)<br />
• Assumes healthy endothelium intact<br />
• Not preferred secondary to viral latency in stromal<br />
keratocytes<br />
Conjunctival flap<br />
• Still performed on select patients, not as common<br />
• Helps quiet down an inflamed eye<br />
• PK may still be performed through the flap<br />
During active HSV infection AVOID<br />
transplantation<br />
• Unless perforation is eminent<br />
Corneal neovascularization is the main<br />
risk factor for immune rejection<br />
• Recent studies show that topical and<br />
subconjunctival bevacizumab (Avastin) is<br />
effective in regressing neovascularization in<br />
these patients 12<br />
Prophylaxis with oral acyclovir<br />
• Improves corneal graft survival<br />
• Famciclovir and valacyclovir may be as effective<br />
but have not been studied<br />
Topical treatment with Zirgan given it’s<br />
safety profile<br />
Coursebook Page 18 of 139<br />
9
5/29/2012<br />
Non-Necrotizing ISK<br />
• Treat with topical anti-viral (Viroptic or Zirgan) and Pred<br />
Acetate 1% with equal frequency until the steroid is<br />
tapered down to BID or QD<br />
• Add oral acyclovir AFTER the virus is inactive without<br />
treatment for 30 days – 400mg BID x 1 year<br />
Necrotizing ISK<br />
• Perforation likely eminent requiring a corneal transplant<br />
• Use oral acyclovir to prevent graft rejection<br />
• Zirgan should also be considered to prevent rejection<br />
• Restasis and Avastin are new treatments to consider as<br />
well<br />
1. Latham , Emi. "Hyperbaric Oxygen Therapy." Medscape Reference.<br />
WebMD LLC, 19052010. Web. 27 Apr 2012.<br />
.<br />
2. Onofrey B, Skorin L, Holdeman N. Ocular Therapeutics Handbook: A<br />
Clinical Manual. 3. Philadelphia; Lippincott Williams & Wilkins, 2011.<br />
198-204. Print.<br />
3. Sugar, Alan. "Herpes Simplex Keratitis." UpToDate. N.p., 11/11/2011.<br />
Web. 30 Apr 2012. .<br />
4. Schwartz GS, Harrison AR, Holland EJ. “Etiology of immune stromal<br />
(interstitial) keratitis.” Cornea. 1998; 17(3):278-81<br />
5. Krachmer J, Mannis M, Holland E. Cornea. 2. 1. Philadelphia: Elsevier<br />
Mosby, 2005. 1048-1066. Print.<br />
6. Dr. Hetrick’s book<br />
7. Sowka J, Gurwood A, Kabat A. “Immune Stromal (Interstital) Keratitis.”<br />
Handbook of Ocular Disease Management. N.p.; n.d. Web. 4 March 2012.<br />
.<br />
8. Wang, J. “Ophthalmologic Manifestations of Herpes Simplex Keratitis.”<br />
Medscape Reference. WebMD LLC., 18 Nov 2010. Web. 3 March 2012.<br />
.<br />
9. Wilhelmus KR, Gee L, Hauck WW, et al. “Herpetic Eye Disease Study. A controlled trial<br />
of topical corticosteroids for herpes simplex stromal keratitis.” Ophthalmology.<br />
1994;101(12):1883-95.<br />
10. Barron BA, Gee L, Hauck WW, et al. “Herpetic Eye Disease Study. A controlled trial of<br />
oral acyclovir for herpes simplex stromal keratitis.” Ophthalmology.<br />
1994;101(12):1871-82.<br />
11. Herpetic Eye Disease Study Group. “Predictors of recurrent herpes simplex virus<br />
keratitis.” Cornea. 2001;20(2):123-8.<br />
12. Herpetic Eye Disease Study Group. “Oral acyclovir for herpes simplex virus eye<br />
disease: effect on prevention of epithelial keratitis and stromal keratitis.” Arch<br />
Ophthalmol. 2000;118(8):1030-6.<br />
13. Herpetic Eye Disease Study Group. “Acyclovir for the prevention of recurrent herpes<br />
simplex virus eye disease.” N Engl J Med. 1998;339(5):300-6.<br />
14. Knickelbein J, Buela K, Hendricks R. “Herpes Stromal Keratitis: Erosion of Ocular<br />
Immune Privilege by Herpes Simplex Virus.” Future Virology, 5.6 (2010):699-708. Print.<br />
15. Saxena S, Sinha N. Keratoplasties- Surgical techniques and complications.<br />
Shanghai:InTech, 2012. 127-134. Print.<br />
16. Wilhelmus KR, Dawson CR, Barron BA, et al. “Risk factors for herpes simplex virus<br />
epithelial keratitis recurring during treatment of stromal keratitis or iridocyclitis.” Br J<br />
Ophthalmol 1996; 80:969-72.<br />
1-3) Latham , Emi. "Hyperbaric Oxygen Therapy." Medscape<br />
Reference. WebMD LLC, 19052010. Web. 27 Apr 2012.<br />
.<br />
4-8) Photos obtained from Wainwright Memorial VAMC Walla Walla,<br />
WA 03/24/12<br />
9-12)Photos obtained from various cartoon monster websites<br />
13,14)Photos obtained from <strong>Pacific</strong> Cataract and Laser Institute<br />
Kennewick, WA 03/14/12<br />
15)Herpes Simplex Stromal Necrotizing Keratitis- American<br />
Academy of Ophthalmology<br />
16)Trigeminal Nerve- wikipedia<br />
17)Multinucleated giant cells-<br />
<br />
18)Elvis photo- <br />
19) Conjunctival Flap photo-<br />
<br />
Coursebook Page 19 of 139<br />
10
5/31/2012<br />
Anna Griffith, O.D.<br />
<strong>Pacific</strong> <strong>University</strong> College of Optometry<br />
Resident in Vision Therapy, Rehabilitation and Pediatrics<br />
TBI Case<br />
• 33 y.o.<br />
• Involved in 9 blasts during combat<br />
• CC: Intermittent blur<br />
• HPI<br />
▫ OD>OS<br />
▫ All distances<br />
▫ Lasts 2 seconds - 1 minute<br />
▫ Eyestrain on the computer after 2-3 hours<br />
▫ Cannot see 3-D in movies, also cause nausea<br />
• Goals<br />
▫ Read again<br />
▫ Return to School for Electrical Engineering<br />
TBI Case<br />
• Other complaints<br />
▫ Difficulty finding things<br />
in crowded drawers or<br />
shelves<br />
▫ Extreme photosensitivity,<br />
some days much worse<br />
than others<br />
TBI Case: Medical History<br />
• Brain Contusion and<br />
Blood Clots seen on MRI<br />
• PTSD<br />
• HTN<br />
• GERD<br />
• Quitting Smoking<br />
0.5 pack/day x 10 years<br />
• Care giver<br />
• Acetaminophen prn<br />
• Diazepam<br />
• Docusate<br />
• Hydrocodone<br />
10/Acetaminophen<br />
• Mirtazapine<br />
• Nicotine Patch and Resin<br />
Complex<br />
• Omeprazole<br />
• Promethazine<br />
• Sumatriptan<br />
• Verapamil<br />
TBI Case: Exam Findings<br />
• OD: -2.50-0.75 x 030 OS: -2.50 DS<br />
• Distance Visual Acuity<br />
▫ OD: 20/20-1<br />
▫ OS: 20/20-1<br />
• Near Visual Acuity<br />
▫ OD: 20/25<br />
▫ OS: 20/20<br />
• EOMs: Full, unrestricted VF: FTFC<br />
• Pupils: PERRL-APD<br />
• Saccades: Quick and Accurate<br />
• Pursuits: Smooth and Accurate<br />
TBI Case: Exam Findings<br />
• Distance Cover Test: Ortho<br />
• Near Cover Test: 2 Exophoria<br />
• In-Phoropter Vertical Phoria: 1 BU OS<br />
• Red lens test: Fusion<br />
• Vertical Maddox Rod: (-) Vertical deviation<br />
• Fixation Disparity:<br />
▫ Horizontal: Type IV curve<br />
▫ Vertical Associated Phoria: 1^BU OS<br />
• Stereo: 30” Stereo with 1^BU OS: 20”<br />
Coursebook Page 20 of 139<br />
1
5/31/2012<br />
TBI Case: Accommodative Findings<br />
• Amplitude:<br />
▫ OD: 5.25/4.75D<br />
▫ OS: 5.00/4.75D<br />
• Accuracy: MEM (+0.50)<br />
• Facility: +/-2.00 flippers<br />
▫ 2.00D too difficult<br />
▫ 1.50D OD: 4.5cpm<br />
▫ 1.50D OS: 11cpm<br />
▫ 1.50D OU: Suppression<br />
• Binocular Cross-Cyl: +0.75 (varied +0.25 to+1.00)<br />
• NRA, PRA<br />
▫ +3.50/+2.75, -1.50/-1.25<br />
Accommodation/Vergence Relationship<br />
• Low PRA<br />
▫ Decreased accommodative amplitude and/or<br />
decreased negative fusional vergence (BI)<br />
• Low NRA<br />
▫ Reduced ability to relax accommodation and/or<br />
decreased positive fusional vergence (BO)<br />
TBI Case: Vergence Findings<br />
• Gross Convergence<br />
▫ 18 inches<br />
• Near Vergence Ranges<br />
▫ Phoropter: smooth, in-instrument<br />
• BO: 34/34/18<br />
• BI: 24/28/15<br />
▫ Prism bar: jump vergence, free-space<br />
• BO: 20/14<br />
• BI: 10/8<br />
TBI Case: Other Testing<br />
• Visual Midline Shift:<br />
Negative<br />
• DEM (Developmental Eye<br />
Movement test) Tests for<br />
Saccadic Dysfunction:<br />
H/V ratio: 7 th percentile<br />
TBI Case: Other Testing<br />
• Motor-Free Visual Perceptual Test, Edition 3<br />
(MVPT-3): Age equivalent: 18 years. Most<br />
difficulty with figure ground and form constancy<br />
TBI Case: Assessment and<br />
Recommendations<br />
• Assessment<br />
▫ Accommodative Insufficiency and Infacility<br />
▫ Gross Convergence Insufficiency (possibly<br />
secondary to accommodative dysfunction)<br />
▫ Decreased Visual Perceptual Skills<br />
• Recommendations<br />
▫ Vision therapy to improve visual efficiency and<br />
reduce symptoms<br />
▫ Re-evaluate vertical deviation<br />
Coursebook Page 21 of 139<br />
2
5/31/2012<br />
Accommodative Therapy:<br />
Near-Far Hart Chart<br />
• Monocular<br />
• Push up with near chart<br />
• Many variations<br />
• Can also be used for<br />
saccadic training<br />
• Goal: Accuracy, then<br />
speed<br />
Accommodative Therapy:<br />
Loose Lens Rock<br />
• Monocular<br />
• Target: sheet of words<br />
or groups of letters<br />
• Alternate viewing<br />
between (-) and (+)<br />
lens<br />
• Goal: -6.00/+2.50<br />
Accommodative Therapy:<br />
HTS (Home Therapy System)<br />
• Red/Blue Glasses<br />
create monocular<br />
fixation in a<br />
binocular field<br />
(MFBF)<br />
Accommodative Therapy:<br />
Binocular Accommodative Rock<br />
• Binocular: Bar readers<br />
and red/green or<br />
polaroid glasses for<br />
monitoring<br />
suppression<br />
• Use lens flipper<br />
Accommodative Therapy:<br />
Prolonged Reading<br />
• Monocular or Binocular<br />
• Bar readers<br />
• 2 minute adaptation<br />
period<br />
Convergence Therapy:<br />
Gross Convergence<br />
• Brock String<br />
▫ Push up<br />
▫ Bug on a String<br />
▫ Bead Jumps<br />
▫ Different FOG<br />
• Barrel Card<br />
http://www.flickr.com/photos/xooorx/6264870613/<br />
http://www.bernell.com/category/skeyword=barrel+card<br />
Coursebook Page 22 of 139<br />
3
5/31/2012<br />
Convergence Therapy:<br />
Smooth Vergence<br />
• Variable Vectogram<br />
• Variable Tranaglyph<br />
Convergence Therapy: Smooth<br />
Vergence<br />
• Computer Programs<br />
(HTS, VTS, Vision<br />
Builder)<br />
• Tromboning with<br />
Stereoscope<br />
http://www.visiontherapysolutions.net/co.php#7<br />
http://www.bernell.com<br />
Convergence Therapy:<br />
Jump Vergence<br />
• Fixed Tranaglyphs<br />
• Fixed Tranaglyphs<br />
• HTS, VTS, or Vision<br />
Builder<br />
Convergence Therapy:<br />
Jump Vergence<br />
• Loose Prism Rock<br />
• Look-aways with any<br />
vergence activity<br />
http://www.bernell.com<br />
• Computer Program<br />
Jump Vergence (HTS,<br />
VTS, Vision Builder<br />
http://www.bernell.com<br />
http://www.bernell.com<br />
Convergence Therapy:<br />
Free Space<br />
Eccentric Circles<br />
• Can be done in<br />
different fields of<br />
gaze and with<br />
motion<br />
Life Savers<br />
Accommodation Progress Chart<br />
Accomm.<br />
Amplitude<br />
(break /<br />
recovery)<br />
2/2/12 5.25/4.75D<br />
5.00/4.75D<br />
2/9/23 6.00/4.75 D<br />
7.75/6.00 D<br />
Facility +/-<br />
2.00<br />
(OD/OS)<br />
7cpm/7cpm<br />
Facility<br />
+/-2.00<br />
(OU)<br />
suppression<br />
both sides<br />
Near Far<br />
Rock Hart<br />
Chart<br />
OD/OS<br />
3:28/not<br />
timed<br />
2/23/12 18cpm/18cpm 2:31/2:35<br />
3/1/12 +/-0.75<br />
flippers:<br />
intermittent<br />
suppression<br />
3/15/12 6.5, 8cpm<br />
5/17/12 18cpm/19cpm 9cpm 2:15/2:12<br />
Coursebook Page 23 of 139<br />
4
5/31/2012<br />
Vergence Progress Chart<br />
Developmental Eye Movements Test<br />
Clown Vecto<br />
2/2 BO: 4/2<br />
BI: 2/0<br />
Spirangle<br />
Vecto<br />
2/9 BO: 10/4<br />
BI: 10/9<br />
3/1 BO: 21/13<br />
BI: 13/8<br />
5/17 BO: 20/17<br />
BI: 14/7<br />
BO: 35/24<br />
BI: 21/14<br />
Quoit Vecto<br />
BO: 2/0<br />
BI: 2/0<br />
BO: 2/0<br />
BI: 2/0<br />
BO: 25/23<br />
BI: 13/8<br />
BO: 29/23<br />
BI: 11/7<br />
Brock<br />
String<br />
6 inches<br />
w/effort<br />
7cm<br />
Stereoscope<br />
BO: 7<br />
BI: 3<br />
Vergence<br />
Facility<br />
8pd: 3cpm<br />
6pd: 6cpm<br />
8pd:<br />
8.5cpm<br />
• February 9 th<br />
▫ Vertical: 77 th percentile<br />
▫ Horizontal: 53 rd percentile<br />
▫ H/V: 7 th percentile<br />
▫ 1-2 errors<br />
• March 15 th<br />
▫ Vertical: 72 nd percentile<br />
▫ Horizontal: 69 th percentile<br />
▫ H/V: 47 th percentile<br />
▫ No errors<br />
Stereo Acuity<br />
• Initial Evaluation: 70”<br />
• After 2 wks of therapy: 30”<br />
Treatment Summary<br />
Initial Evaluation<br />
OD Monocular Facility +/-1.50: 4.5 cpm<br />
OS Monocular Facility +/-1.50: 11 cpm<br />
Post Therapy<br />
Evaluation<br />
+/-2.00: 18 cpm<br />
+/-2.00: 19cpm<br />
Binocular Facility +/-0.75: unable +/-2.00: 9 cpm<br />
• 3 months later: 20”<br />
Near BI range 24/28/15 x/12/5<br />
Near BO range 34/34/18 >40/30<br />
Vergence Facility unable 8BI/BO: 8.5 cpm<br />
NPC 18 inches 6 cm<br />
Stereopsis 70” 20”<br />
DEM H/V ratio 7 th percentile 47 th percentile<br />
Subjective Improvements<br />
Reading again<br />
More visually aware/less blur<br />
Feels more ready to start<br />
school for Electrical<br />
Engineering<br />
Sees 3-D in movies<br />
Treatment Summary<br />
• Evaluations and initial treatment: Dec, Jan. 26<br />
• 5 training sessions: Feb. 2 nd , 9 th , 23 rd , March 1 st<br />
and 15 th<br />
• Progress Visual Efficiency Eval: April 12 th (not<br />
feeling well and very dim illumination needed)<br />
• Progress: MVPT3, DEM, FD: April 19 th<br />
• CL fit: May 3 rd<br />
• CL check and repeat Visual Efficiency Progress<br />
Evaluation: May 17 th<br />
Coursebook Page 24 of 139<br />
5
5/31/2012<br />
Special Considerations for VT patient<br />
with TBI<br />
• Usually takes longer<br />
• Other factors, speech, cognitive impairment, etc.<br />
• Mild TBI often most successful cases<br />
• More variation in performance, good and bad<br />
days<br />
• Be aware of nausea<br />
• Vision Therapy can make a difference<br />
Traumatic Brain Injury<br />
• 1.4 million brain injuries each year 1<br />
• 5.3 million Americans (2% of population) need<br />
help performing activities of daily living 2<br />
• In combat, at least 14-20% of casualties have<br />
TBI that require acute and long term care 3<br />
• Mild TBI cases are not being identified. 40% of<br />
these patients experience vision problems. 3<br />
Biochemical Basis of Neuro-Disruption 4<br />
Breakdown of intimate<br />
association of cerebral<br />
blood flow (CBF) and<br />
cerebral glucose<br />
metabolism (CMGL)<br />
Cell<br />
toxicity<br />
Ischemia and<br />
hypoxia<br />
Metabolic<br />
imbalances<br />
Change<br />
neuronal cell<br />
membrane<br />
permeability<br />
Most Common Visual Diagnoses<br />
Following TBI<br />
• Convergence Insufficiency<br />
• Strabismus<br />
• Accommodative Insufficiency<br />
• Accommodative Infacility<br />
• Ocular Motility Disorders<br />
• Visual Field Defects<br />
• Photosensitivity<br />
• Dry Eye<br />
Case History<br />
• Did you lose consciousness Did you feel heat or pressure during blast<br />
• Did the blast affect your hearing<br />
• Are you more sensitive to light Noise<br />
• Blurry or double vision<br />
• Headaches<br />
• Balance problems<br />
• Feel dizzy Do you feel this way when you move your eyes<br />
• Bump into things<br />
• Miss objects when first reach Have difficulty judging depth of stairs<br />
• Poor concentration, memory, or attention<br />
• Difficulty thinking or solving problems Identifying objects<br />
• Trouble with speech<br />
• Overstimulated Overwhelmed Do things that didn’t bother you, now do<br />
• Change of emotions Short-tempered<br />
• Anxious Depressed Dreams of traumatic past events Fatigue easily<br />
• Are there things you used to be able to do and can’t anymore<br />
• Does the floor look tilted Do walls or floor shift and move<br />
• Cranial nerve questions<br />
BIVSS SYMPTOM CHECKLIST<br />
Please check the most appropriate box, or circle the item number that best matches your observations. Alll<br />
information will be held in confidence. Circle a number below. Please rate each behavior.<br />
How often does each behavior occur (circle a number) Never Seldom Occasionally Frequently Always<br />
EYESIGHT CLARITY<br />
Distance vision blurred and not clear -- even with lenses 0 1 2 3 4<br />
Near vision blurred and not clear -- even with lenses 0 1 2 3 4<br />
Clarity of vision changes or fluctuates during the day 0 1 2 3 4<br />
Poor night vision / can’t see well to drive at night 0 1 2 3 4<br />
VISUAL COMFORT<br />
Eye discomfort / sore eyes / eyestrain 0 1 2 3 4<br />
Headaches or dizziness after using eyes 0 1 2 3 4<br />
Eye fatigue / very tired after using eyes all day 0 1 2 3 4<br />
Feel “pulling” around the eyes 0 1 2 3 4<br />
DOUBLING<br />
Double vision -- especially when tired 0 1 2 3 4<br />
Have to close or cover one eye to see clearly 0 1 2 3 4<br />
Print moves in and out of focus when reading 0 1 2 3 4<br />
Coursebook Page 25 of 139<br />
6
5/31/2012<br />
BIVSS SYMPTOM CHECKLIST<br />
LIGHT SENSITIVITY<br />
Normal indoor lighting is uncomfortable – too much glare 0 1 2 3 4<br />
Outdoor light too bright – have to use sunglasses 0 1 2 3 4<br />
Indoors fluorescent lighting is bothersome or annoying 0 1 2 3 4<br />
DRY EYES<br />
Eyes feel “dry” and sting 0 1 2 3 4<br />
“Stare” into space without blinking 0 1 2 3 4<br />
Have to rub the eyes a lot 0 1 2 3 4<br />
DEPTH PERCEPTION<br />
Clumsiness / misjudge where objects really are 0 1 2 3 4<br />
Lack of confidence walking / missing steps / stumbling 0 1 2 3 4<br />
Poor handwriting (spacing, size, legibility) 0 1 2 3 4<br />
PERIPHERAL VISION<br />
Side vision distorted / objects move or change position 0 1 2 3 4<br />
What looks straight ahead--isn’t always straight ahead 0 1 2 3 4<br />
Avoid crowds / can’t tolerate “visually-busy” places 0 1 2 3 4<br />
READING<br />
Short attention span / easily distracted when reading 0 1 2 3 4<br />
Difficulty / slowness with reading and writing 0 1 2 3 4<br />
Poor reading comprehension / can’t remember what was read 0 1 2 3 4<br />
Confusion of words / skip words during reading 0 1 2 3 4<br />
Lose place / have to use finger not to lose place when reading 0 1 2 3 4<br />
Home Training Kit $325<br />
• 1-patch, 1-Brock String (large), 1-Marsden Ball<br />
• R/G glasses<br />
• 2-Lifesaver cards (Clear and Opaque)<br />
• 10-loose lenses (+.50, +1.00, +1.50, +2.00, +2.50, -.1.00, -2.00,<br />
-3.00, -4.00, -5.00)<br />
• 4-flipper lenses: (+/- 1.00, +/- 1.50, +/- 2.00, +/- 2.50)<br />
• Loose Prisms: 4, 6, 8, 12 pd<br />
• Tranaglyphs:<br />
6-one-piece fixed:<br />
BC 71, BC 72 vertical<br />
BC 51, BC 52, BC 53, BC 54<br />
3-two-piece variable: BC 920H (horizontal mini), BC 520, BC 802<br />
• Tranaglyph holder<br />
• Reading Bars for suppression monitoring<br />
Resources<br />
• DVBIC (Defense and Veterans Brain Injury<br />
Center)www.dvbic.org<br />
• NORA (Neuro-Optometric Rehabilitation<br />
Association)www.nora.cc<br />
• Resources for returning Veterans:<br />
http://www.oefoif.va.gov<br />
• www.Bernell.com<br />
• http://oep.excerpo.com/<br />
References<br />
1. Langlois JA, Rutland-Brown W, Thomas KE.Traumatic brain injury in the United States:<br />
emergency department visits, hospitalizations and deaths. Atlanta GA: Centers for Disease<br />
Control and Prevention, National Center for Injury Prevention and Control, 2004.<br />
2. Thurmann D, Alverson C, Dunn K, Guerro J,Sniezek J. Traumatic brain injury in the United<br />
States: a public health perspective. J Head Trauma Rehab 1999;14:602-15.<br />
3. Traumatic Brain Injury, Veterans Health Initiative: Department of Veterans Affairs,<br />
Employee Education System; January 2004.<br />
4. Center for Neuro Skills. http://www.neuroskills.com/brain-injury/the-neuro-biochemicalbasis-of-post-trauma-vision-syndrome.php<br />
5. Scheiman and Wick. Clinical Management of Binocular Vision: Heterophoric,<br />
Accommodative, and Eye Movement Disorders<br />
6. Griffin and Grisham. Binocular Anomalies: <strong>Diagnosis</strong> and Vision Therapy<br />
7. NORA meeting notes. Atlanta 2011.<br />
8. Medscape: Epidemiology and Classification of Traumatic Brain Injury<br />
Thank you!<br />
Coursebook Page 26 of 139<br />
7
5/29/2012<br />
Overview<br />
CASE STUDY:<br />
THE EVOLUTION AND RESOLUTION OF AN<br />
OCULOMOTOR NERVE PALSY<br />
PRESENTER: JESSICA DENNIS - JNDMAIL@YAHOO.COM<br />
INSTRUCTOR: DOUGLAS DEVRIES - EMAIL<br />
Case presentation<br />
<strong>Differential</strong> diagnoses and assessment<br />
Pathway and function of oculomotor nerve<br />
Plan<br />
Referrals<br />
Follow ups<br />
Additional information<br />
Questions<br />
Eye Care Associates of Nevada - 2285 Green Vista- Sparks, NV 89431<br />
Ring ring<br />
Presentation (11/14/2012)<br />
ER doctor calls Saturday night<br />
CC: dull eye ache/pain OS<br />
• Stable VAs<br />
Reports normal eye examination including<br />
• Full EOMs, no pain/diplopia<br />
• Pupils normal, no APD<br />
• No AC reaction<br />
• Normal CT scan<br />
Initial assessments…<br />
Follow up with Ophthalmologist Monday<br />
Demographics-<br />
54 year old<br />
African American male<br />
Medical history:<br />
• Heart disease<br />
• High blood pressure<br />
• Diabetes, type II<br />
• Insulin dependent<br />
• Peripheral diabetic neuropathy<br />
• Hemodialysis secondary to diabetic nephropathy<br />
ROS:<br />
• Hearing loss, chronic cough, arthritis, easy fatigability, depression, kidney failure<br />
Current medications:<br />
• Alprazolam, amlodipine, aspirin, Coreg, gabapentin, insulin, Prevacid, nitroglycerine,<br />
Coumadin, Zovirax<br />
Ocular history:<br />
• Cataract extraction OU (5/2011)<br />
Presentation (11/14/2012)<br />
Examination (11/14/2012)<br />
CC: “Worried implant moved”<br />
HPI:<br />
Constant dull ache OS<br />
• No jaw claudication or temporal pain<br />
• Trace photophobia<br />
(+) diplopia for 2 days, goes away if OD covered<br />
• Vertical and horizontal, distance and near<br />
• Stable, constant<br />
Slight blur/fuzzy VA OS<br />
Reports blood glucose in the low 100’s<br />
<br />
<br />
<br />
<br />
<br />
VA(sc)<br />
OD: 20/20<br />
OS: 20/25- , PH 20/25+<br />
CVF:<br />
full OD, OS<br />
EOMs:<br />
full OD<br />
Normal primary gaze- no exotropia or hypotropia<br />
Adduction and infraduction gaze restrictions OS, (+) diplopia<br />
Pupils:<br />
Aniso OS>OD in light and dim illuminations<br />
Slow reaction to light OS<br />
Normal near response<br />
No APD<br />
Hertel:<br />
21>-----
5/29/2012<br />
Examination (11/14/2012)<br />
Anterior segment<br />
Ptosis OS<br />
Trace SPK OU<br />
PCIOL OU<br />
1+ PCO OS<br />
Examination (11/14/2012)<br />
Posterior segment<br />
Questionable mild pallor ONH OS<br />
Tortuous vessels OU<br />
(+) trace cellophane changes OU<br />
Scattered dot/blot hemes in all four quadrants OU<br />
• possible IRMA/NVE superotemporal arcades OS<br />
Abnormal findings…<br />
DDx<br />
Abnormal EOMs OS<br />
Pupil OS<br />
Ptosis OS<br />
Diabetic/heart conditions…<br />
DDx<br />
Partial oculomotor nerve palsy<br />
Strabismus<br />
Decompensated phoria<br />
Myasthenia Gravis<br />
Grave’s<br />
Orbital fracture<br />
Internuclear ophthalmoplegia<br />
Duane’s type II<br />
Brown’s<br />
Strabismus and Decompensated Phorias<br />
Perform cover test in different fields of gaze<br />
Results comitant or non-comitant<br />
Non-comitant considered greater then 5 prism diopters<br />
of difference between<br />
Non-comitant generally implies cranial nerve palsies<br />
Comitant usually indicates strabismus<br />
Paretic or mechanical<br />
Ductions (monocular eye movement)<br />
Versions (binocular eye movement, physiologic H)<br />
Ductions>Versions<br />
Paretic<br />
Ductions=Versions<br />
Mechanical<br />
Forced duction testing<br />
Drop the suspected eye with anesthetic<br />
Grab conjunctiva with toothless forceps near limbus and attempt to move eye in<br />
direction opposite that mechanical restriction is thought<br />
+ forced duction means eye did NOT move<br />
Indicates mechanical restriction<br />
- forced duction means eye DID move<br />
Indicates paretic in nature<br />
Coursebook Page 28 of 139<br />
2
5/29/2012<br />
History is key…<br />
Myasthenia Gravis<br />
Grave’s<br />
Orbital fracture<br />
Review<br />
Internuclear ophthalmoplegia<br />
Lesion of MLF<br />
Ipsilateral adduction deficit with abducting nystagmus is<br />
opposite eye<br />
Duane’s type II<br />
Adduction deficit<br />
No globe retraction<br />
Brown’s<br />
Superior oblique tendon sheath syndrome<br />
Limited elevation in adduction<br />
Assessment<br />
1. Left partial CN III palsy, relative pupil sparing<br />
2. IDDM with moderate to severe NPDR OD<br />
IDDM with likely NPDR OS<br />
Oculomotor nerve review<br />
Origination and pathway<br />
Efferent pupillary pathway<br />
OM nerve functions<br />
Partial, complete, isolated<br />
3. Pseudophakic OU<br />
4. PCO OS<br />
Origin<br />
Oculomotor nuclear complex<br />
http://www.neuroanatomy.wisc.edu/virtualbrain/BrainStem/21CNIII.html<br />
Coursebook Page 29 of 139<br />
3
5/29/2012<br />
Origin<br />
Pathway<br />
http://radiologymri.blogspot.com/2010/12/oculomotor-infarct.html<br />
http://www.medrounds.org/ocular-pathology-study-guide/uploaded_images/cwmr-768439.jpg<br />
Pathway<br />
Pathway<br />
http://bestpractice.bmj.com/best-practice/monograph/956/basics/pathophysiology.html<br />
http://legacy.owensboro.kctcs.edu/gcaplan/anat/notes/api%20notes%20m%20%20peripheral%20nerves.htm<br />
Functions<br />
Edinger-Westphal (Efferent pupillary pathway review)<br />
Superior division:<br />
levator palpebrae superioris*<br />
superior rectus<br />
Inferior division:<br />
medial rectus*<br />
inferior rectus*<br />
inferior oblique<br />
- preganglionic parasympathetic to ciliary ganglion<br />
(innervation of sphincter pupillae* and ciliary muscle)<br />
http://brains.oxfordmedicine.com/cgi/content-nw/full/12/1/med-9780198569381-chapter-002/FIG002037<br />
Coursebook Page 30 of 139<br />
4
5/29/2012<br />
Types<br />
Recall assessment<br />
<br />
Pupil involving<br />
Aneurysm, tumor, trauma, cavernous sinus mass, pituitary<br />
apoplexy, herpes zoster<br />
1. Isolated left partial CN III palsy<br />
-relative pupil sparing<br />
<br />
<br />
<br />
<br />
Relative pupil sparing<br />
Ischemic microvascular disease*<br />
Pupil sparing<br />
Ischemic microvascular disease, GCA<br />
Isolated<br />
Partial or complete<br />
2. IDDM with moderate to severe NPDR OD<br />
IDDM with likely NPDR OS<br />
3. Pseudophakic OU<br />
4. PCO OS>OD<br />
Plan<br />
1. Order MRI of brain/orbits****<br />
- Request CT scan<br />
- Neuro-ophthalmic consult<br />
2. Retina specialist consult for likely PDR<br />
3. Yag laser OS<br />
Treatment options for diplopia:<br />
Patching (remember not to patch patients
5/29/2012<br />
11/30/2012 continued<br />
MRI w/o contrast<br />
<br />
Examination continued…<br />
Anisocoria OS>OD<br />
OS down and to the left<br />
EOMs OS<br />
• Supraduction, infraduction, adduction restricted<br />
• normal abduction<br />
Negative forced ductions**<br />
Complete ptosis OS<br />
Maxillofacial CT scan (11/12/11) – normal<br />
MRI (11/15/2011)<br />
Brain<br />
Findings<br />
No mass effects or shift of midline structures<br />
No hemorrhagic lesions<br />
No evidence of acute cerebral infarction<br />
Impression<br />
Minimal age related cortical atrophy<br />
Microvascular ishemic gliosis<br />
Wedge shaped area of chronic infarction, left occipital lobe<br />
11/30/2012 continued<br />
12/22/2011<br />
Assessment:<br />
Pupillary involving left oculomotor palsy…<br />
Diabetic (ischemic microvascular) third nerve palsies spare pupil…<br />
Order MR angiogram of head and neck to r/o posterior communicating artery aneurysm<br />
Left occipital infarct<br />
HVF<br />
Diabetic retinopathy OU<br />
Ordered the following lab studies:<br />
• CBC<br />
• ESR/CRP<br />
• ACE level<br />
• ANA<br />
• PRP<br />
Trial dispense of celebrex for pain<br />
RTC 1 month<br />
Patient reports slight increase on inward eye movement and<br />
complete relief of pain with celebrex<br />
Examination:<br />
Slightly improved motilities on supraduction and adduction<br />
HVF 30-2:<br />
Scattered defects<br />
Lab results:<br />
CBC: normal<br />
Metabolic panel: elevated glucose level<br />
ANA, ACE, ESR, RPR, vit B12, folate: normal<br />
MR angiogram (12/9/2011):<br />
Circle of Wilis: normal<br />
Neck: normal carotid arteries<br />
12/22/2012 continued<br />
Assessment:<br />
<br />
1. Marginally improved pupillary involving left<br />
oculomotor palsy<br />
**Importantly “no clear-cut evidence of posterior<br />
communicating artery aneursym”<br />
2. Left occipital lobe infarction<br />
- No HVF defects<br />
3. Bilateral diabetic retinopathy<br />
RTC 1 month<br />
03/01/2012<br />
Missed appointments… things must be better<br />
Yes! No double vision, pain and ptosis improved<br />
EOMs, pupils<br />
Examination showed full recovery of adduction,<br />
supraduction and infraduction!<br />
Pupils showed slight aniso (4.5 OD, 5.0 OS)<br />
Coursebook Page 32 of 139<br />
6
5/29/2012<br />
Summary of Retinal Appointments<br />
Retinal Consultation<br />
Dr. Jarl Nielsen<br />
Nevada Retina Associates<br />
610 Sierra Rose Drive<br />
Reno, NV 89511<br />
11/15/2011 (OD 20/20, OS 20/25)<br />
NPDR OD, Early PDR OS<br />
12/20/2011 (OD 20/20, OS 20/40)<br />
IVFA performed<br />
PDR OS>OD<br />
PRP OS performed<br />
01/10/2012 (OD 20/20, OS 20/40)<br />
PRP OS<br />
1/31/2012 (OD 20/20, OS 20/30)<br />
PRP OS<br />
RTC for DFE OD, possible PRP<br />
Summary of Retinal Appointments<br />
Summary of Retinal Appointments<br />
02/07/2012 (OD 20/20, OS 20/30)<br />
DFE OD minimally active NVE<br />
Stable OS<br />
Follow up in 2-4 weeks, PRP OD<br />
02/28/2012<br />
PRP OD<br />
03/20/2012<br />
PRP OD<br />
05/08/2012<br />
Involuting NVE OD<br />
No active NVE OS<br />
RTC 1 month<br />
04/10/2012<br />
PRP OD<br />
03/05/2012<br />
Back to Eye Care Associates…<br />
<br />
<br />
<br />
<br />
Referred back by Dr. Hershewe for possible conjunctivitis<br />
SLE:<br />
2+ injected nasal and temporal pinguecula<br />
Trace to 1+ diffuse SPK<br />
PCO OS>OD<br />
Assessment:<br />
Pingueculitis OD>OS<br />
Dry eye syndrome<br />
Plan:<br />
Continue FML qid (as dispensed by Dr. Hershewe)<br />
add artificial tear use<br />
RTC for YAG OS 1 st , then OD<br />
Coursebook Page 33 of 139<br />
7
5/29/2012<br />
03/14/2012<br />
Lastly, addressing “slight blur OS”<br />
VA post laser treatment<br />
• OD: 20/20<br />
• OS: 20/20-<br />
Additional information<br />
Possible CN III locations of involvement<br />
Aberrant regeneration<br />
Food for thought<br />
And full motilities!<br />
RTC annually<br />
Follow up with Dr. Nielsen as scheduled<br />
Location of palsy<br />
Midbrain damage<br />
All or part of nucleus may be affected<br />
• More commonly entire nucleus<br />
If entire nucleus<br />
• Ipsilateral muscles involved: MR, IR IO<br />
• Contralateral muscles involved: SR<br />
• Both: levators<br />
CN IV nucleus close by…<br />
• Is contralateral superior oblique involved<br />
Location of palsy<br />
Intracranial<br />
As previously discussed, posterior communicating artery<br />
common location for aneurysm to affect oculomotor<br />
nerve<br />
Less common are posterior cerebral and superior<br />
cerebellar arteries<br />
Location of palsy<br />
Cavernous sinus<br />
Ipsilateral CN IV involvement possible<br />
Ophthalmic division of V<br />
Maxillary division of V<br />
Eye would be out (only LR working) and facial anesthesia<br />
would be present<br />
Orbital<br />
Retrobulbar tumor or inflammation<br />
• CN VI and nasociliary nerves involved secondary to close location<br />
in muscle cone<br />
Eye would be down, slightly out (only SO working)<br />
http://www.oculist.net/downaton502/prof/ebook/duanes/pages/v1/v1c003.html<br />
Coursebook Page 34 of 139<br />
8
5/29/2012<br />
CN III aberrant regeneration<br />
Fibers making incorrect connections<br />
Can occur from the following<br />
Congenital<br />
Primary<br />
Acquired… damage or compression<br />
• During recovery<br />
• NOT ISCHEMIC!!!<br />
CN III aberrant regeneration<br />
1. Pseudo graefe sign<br />
levator superioris and inferior rectus<br />
2. Eyelid dyskinesis<br />
levator superioris and medial rectus<br />
3. Pupil dyskinesis<br />
parasympathetic fibers and medial rectus<br />
Food for thought<br />
86% of pupil involved are from aneurysms<br />
23% of pupil involved are vascular/ischemic<br />
14% of pupil sparing are from aneurysms<br />
77% of pupil sparing are vascular/ischemic<br />
Food for thought<br />
95% of painful CN III palsies are caused by<br />
aneurysms<br />
80% of painful CN III palsies are ischemic/vascular<br />
Pain not a very good differential<br />
Kissel JT. Ann Neurol 1983<br />
Goldstein JE, et al. Arch Ophthalmol 1960<br />
Clinical Pearls<br />
Questions<br />
<br />
<br />
<br />
<br />
<br />
Case history<br />
Investigate the double vision<br />
• Monocular or binocular<br />
• Vertical or horizontal<br />
• Distance or at near<br />
Comitant or non-comitant<br />
Forced duction testing!<br />
Photo document<br />
Don’t forget imaging guidelines<br />
Can be an ocular emergency!!<br />
Send for proper referrals<br />
Atypical cases… not all are textbook<br />
Special thanks to:<br />
Curtis Manning, MD<br />
Paul W Hiss, MD<br />
Douglas Devries, OD<br />
Gerard L Hershewe, DO<br />
Jarl Nielsen, MD<br />
Coursebook Page 35 of 139<br />
9
5/29/2012<br />
Oliver<br />
Oliver<br />
Kuhn-Wilken,<br />
Kuhn-Wilken,<br />
O.D.<br />
O.D.<br />
Jeffery Hiett, O.D. and Irene Yang, O.D.<br />
Drs. Jeffery Hiett and Irene Yang<br />
Jonee Brandt, O.D. and Jason Bleazard, O.D.<br />
Drs. Jonee Brandt American and Lake Jason VA Bleazard Hospital<br />
American Lakewood, VA Washington Hospital<br />
Lakewood, Washington<br />
The Problem with<br />
Prostaglandins<br />
Case #1: BW<br />
• 71 yo white male<br />
• CC: vision OD is “like spots on a shower door” x 6 months,<br />
gradual onset, now constant, am = pm, distance = near.<br />
• POHx: POAG treated with TravatanZ qhs OU<br />
cataract extraction with PCIOL (2006) and YAG OU<br />
• PMHx: COPD<br />
sleep apnea with CPAP cannulas<br />
• VAs sc: OD 20/50-2 PHNI, OS 20/20-1<br />
• Tap OD 11 mmHg, OS 13 mmHg @ 0900<br />
• SLE: ONH: c/d ratio OD 0.65 with pallor, OS 0.30<br />
macula: OD elevation at fovea, OS normal<br />
Case #1: BW<br />
• Stratus OCT:<br />
foveal thickness<br />
OD 541 um,<br />
OS 214 um<br />
Case #1: BW<br />
• Assessment: cystoid macular edema OD<br />
• Plan: discontinue TravatanZ<br />
Rx dorzolamide 2% bid OU<br />
Rx ketorolac 0.4% qid OD<br />
Case #1: BW<br />
Exam Date Foveal thickness OD BCVA OD IOP OD<br />
8/19/2011 541um 20/50-2 11<br />
8/30/2011 475um 20/40-2 15<br />
9/13/2011 298um 20/40 17<br />
9/27/2011 252um 20/30+1 18<br />
10/27/2011 275um 20/40 19<br />
CME fundus appearance<br />
OCT<br />
OD:10/27/2<br />
011<br />
CME fundus<br />
appearance<br />
Coursebook Page 36 of 139<br />
1
5/29/2012<br />
CME<br />
Cystic spaces<br />
on OCT:<br />
CME can follow<br />
ant. seg. inflammation<br />
• Anterior uveitis<br />
• Cataract surgery (Irvine-Gass Syndrome) or YAG<br />
Late-phase petalloid appearance on FA:<br />
CME can follow<br />
post. seg. inflammation<br />
• Retinal venous occlusions<br />
• Epiretinal membrane<br />
• Diabetic retinopathy<br />
• ARMD<br />
Edema<br />
of<br />
Müller<br />
cells<br />
Edema<br />
of the<br />
Edema optic<br />
of nerve the<br />
optic<br />
nerve<br />
The Prostaglandin Analogs<br />
• First line glaucoma therapy<br />
• Possible pro-inflammatory effect<br />
• Relative contraindications: cataract surgery<br />
uveitis<br />
herpes simplex keratitis<br />
epiretinal membrane<br />
pregnancy<br />
Coursebook Page 37 of 139<br />
2
5/29/2012<br />
The Inflammatory Cascade<br />
The Hidden Cost of CME<br />
• 1-2% of CE patients diagnosed with “clinical CME.”<br />
• 20% of patients have “angiographic CME.”<br />
0.8<br />
LogMAR vision versus time following cataract extraction<br />
ETDRS vision in LogMAR units<br />
0.7<br />
0.6<br />
0.5<br />
0.4<br />
0.3<br />
0.2<br />
0.1<br />
No CME<br />
CME at 8 weeks<br />
0<br />
Pre-op Day 1 Day 14 Day 30 Day 60<br />
Ursell PG, Spalton DJ, Whitcup SM, et al.<br />
CME and cataract surgery<br />
• The biggest risk factors:<br />
uncontrolled diabetes or hypertension<br />
CME following CE in the fellow eye<br />
CE with breach of the posterior capsule<br />
retinal venous disease<br />
epiretinal membrane<br />
PGs and cataract surgery<br />
• There is no Gold Standard.<br />
• Recommendation: cover with an NSAID<br />
qid for 2-7 days prior to surgery.<br />
• Do not discontinue or replace a<br />
prostaglandin.<br />
Management of CME<br />
• NSAID qid<br />
• Pred Forte qid<br />
• Consider replacing a prostaglandin<br />
• Referral if not improving: consider sub-<br />
Tenon’s injection, intravitreal injection, or<br />
vitrectomy<br />
PGs<br />
and<br />
uveitis<br />
• Uveitis is an inflammatory disease<br />
• PGs may have a pro-inflammatory effect<br />
• Therefore PGs are relatively<br />
contraindicated in uveitic patients.<br />
• Contraindication is rarely observed<br />
Coursebook Page 38 of 139<br />
3
5/29/2012<br />
PGs and uveitis<br />
Study No. of eyes Time Uveitic response<br />
Warwar 1998 163 normals 1 year 6.4%<br />
Smith 1999 505 normals 1 year 1.0%<br />
Smith 1999 13 uveitics 1 year 23.1% Mostly mild cases<br />
Chang 2008 163 uveitics 3 mos.<br />
Markomichelakis<br />
2008 58 uveitics 6 mos.<br />
equal to<br />
control<br />
equal to<br />
control<br />
Control = fellow eye, non PG<br />
glaucoma medication<br />
Control =<br />
dorzolamide/timolol<br />
medication<br />
PGs and uveitis<br />
• Case studies describe patients in whom<br />
uveitis occurs in the ipsilaterally treated<br />
eye, and patients in whom the uveitis<br />
improves after cessation and recurs after<br />
rechallenge.<br />
• Latanoprost may not lower IOP during a<br />
uveitic flare.<br />
Goldberg 2008 5,856 normals 5 years OD<br />
laser burns OS peripheral retina, no tear<br />
Case #2: HF<br />
• Assessment: herpes simplex keratitis OS.<br />
• Plan: Rx Viroptic q2h OS, acyclovir<br />
400mg bid po, and erythromycin ung qhs<br />
OS.<br />
Case #2: HF<br />
Date VA OS Assessment Current medications<br />
10/25/07 20/200 Acute HSK OS TravatanZ qhs OU, timolol 0.5%<br />
GFSqam OU (continued)<br />
10/29/07 20/200 “Improving” Viroptic q2hr OS, erythromycin ung<br />
qhs OS (continued)<br />
11/02/07 20/200 “Improving” Viroptic 5x/day OS with taper,<br />
acyclovir 400 mg po bid<br />
11/09/07 4/300 “No improvement” Viroptic 5x/day OS, acyclovir 400mg<br />
po bid (continued)<br />
11/13/07 5/200-1 “Improving” Taper Viroptic over 4 days<br />
11/16/07 5/200-1 “Slowly improving” Viroptic qd x 2 days then d/c<br />
11/19/07 5/200- “Resolving” Refresh tears qid OS<br />
11/26/07 5/250 “Resolving” no change<br />
11/30/07 5/200 “no improvement” Replace erythro with bacitracin ung<br />
12/3/07 5/200- “Resolving” no change<br />
12/7/07 5/225 “Resolved” Replace baci with erythro ung qhs OU<br />
Case #2: HF<br />
Date VA OS Assessment Plan<br />
12/14/07 4/160 “Resolving” TravatanZ qhs OU, timolol 0.5% GFSqam<br />
OU, acyclovir 400 mg po bid (continued)<br />
12/31/07 4/160 “Resolving” no change<br />
2/5/08 5/700 Active disciform<br />
HSK<br />
Viroptic 5x/day OS,<br />
acyclovir 400 mg po bid (continued)<br />
2/8/08 2/125 “Resolving” Viroptic 5x.day OS<br />
2/11/08 2/125 “Resolving” Viroptid qid OS<br />
2/15/08 3/400 “Resolving” Viroptic qd OS x 1 day then d/c<br />
2/20/08 3/350 “Improving” D/c Viroptic. D/c TravatanZ OS<br />
2/25/08 3/350 “Improving” no change<br />
3/4/08 5/350 “improvement” D/c TravatanZ OD<br />
3/7/08 5/350 “continued<br />
no change<br />
improvement”<br />
3/14/08 5/300 “stable” no change<br />
Coursebook Page 39 of 139<br />
4
5/29/2012<br />
PGs and herpes simplex keratitis<br />
PGs and herpes simplex keratitis<br />
Study Patients Time HSK rate Caveat<br />
Bean 2004 39,174 normals<br />
on PG therapy<br />
6 years 0.11% Only counted 1 st occurrence<br />
Only counted if within 7<br />
days of PG start<br />
Lead researcher employed<br />
by Pfizer<br />
Research paid for by Pfizer<br />
• Case studies: HSK reported to recur after<br />
up to 10 years of inactivity upon<br />
commencement of latanoprost use, and be<br />
unresponsive to anti-viral therapy until<br />
the latanoprost is discontinued.<br />
• No other large studies<br />
References<br />
Prostaglandin take-homes<br />
1. Cover with an NSAID prior to CE if there<br />
are any risk factors.<br />
2. Uveitis or HSK due to PGs is very rare.<br />
3. Strongly consider discontinuing PGs<br />
once CME, uveitis, or HSK occurs.<br />
• Giuffre G. The effects of prostaglandin F2 in the human eye. Graefes Arch Clin Exp Ophthalmol<br />
1985;222:139-41.<br />
• Benitah, Nicole R. MD; Arroyo, Jorge G. MD. Pseudophakic Cystoid Macular Edema. International<br />
Ophthalmology Clinics: Winter 2010 - Volume 50 - Issue 1 - pp 139-153. doi:<br />
10.1097/IIO.0b013e3181c551da. extraction: a fluorescein funduscopic and angiographic study. Arch<br />
Ophthalmol. 1966;76:646.<br />
• Yanoff M, Fine BS, Brucker AJ, et al. Pathology of Human Cystoid Macular Edema. Surv Opthalmol 28<br />
(Suppl): 505-511, 1984.<br />
• Miyake K, Ibaraki N. Prostaglandins and Cystoid Macular Edema. Surv Opthalmol 47 (Supplement 1):<br />
S203-S218, 2002.<br />
• Warren K. Current Concepts in the Etiology and Treatment of Pseudophakic Cystoid Macular Edema.<br />
Retinal Physician: http://www.retinalphysician.com/printarticle.aspxarticle=103062, 6/1/2009.<br />
Accessed 03/06/2012.<br />
• Ursell PG, Spalton DJ, Whitcup SM, et al. Cystoid macular edema after phacoemulsification: relationship<br />
to blood-aqueous barrier damage and visual acuity. J Cataract Refract Surg. 1999; 25:1492-1497.<br />
• Ngyuen, Q. The role of prostaglandin analogs in the treatment of glaucoma in the 21 st century. Int.<br />
Ophthalmol Clin 2004;44:2:15-27.<br />
• Arcieri ES, Santana A, Rocha FN, et al. Blood-aqueous barrier changes after the use of prostaglandin<br />
analogues in patients with pseudophakia and aphakia. Arch Ophthalmol. 2005;123:186-192.<br />
• Miyake K, Ota I, Maekubo K, et al. Latanoprost accelerates disruption of the blood-aquous barrier and<br />
the incidence of angiographic cystoid macular edema in early postoperative pseudophakias. Arch<br />
Ophthalmol. 199;117:34-40.<br />
References<br />
• Shrivastava A. Prostaglandins, cataract surgery and CME. Review of Ophthalmology. 07/22/2009.<br />
• Camras CB, Bhuyan KC, Podos SM, et al. Multiple dosing of prostaglandin F2 or epinephrine on<br />
cynomolgus monkey eyes. Invest Ophthalmol Vis Sci 1987;28:921-6.<br />
• Arcieri ES, Pierre Filho PT, Wakamatsu TH. The effects of prostaglandin analogues on the blood aqueous<br />
barrier and corneal thickness of phakic patients with primary open-angle glaucoma and ocular<br />
hypertension. Eye (Lond). 2008 Feb; 22(2):179-183.<br />
• Warner RE, Bullock JD, Ballal D. Cystoid macular edema and anterior uveitis associated with latanoprost<br />
use: experience and incidence in a retrospective review of 94 patients. Opthalmology. 1998;105:263-268.<br />
• Chang JK, McCluskey P, Missotten T, et al. Use of ocular hypotensive prostaglandin analogues in<br />
patients with uveitis: does their use increase anterior uveitis and cystoid macular edema Br J<br />
Ophthalmol. 2008 Jul;92(7):916-21.<br />
• Goldberg I, Li XY, Selaru P, et al. A 5-year, randomized, open-label safety study of latanoprost and usual<br />
care in patients with open-angle glaucoma or ocular hypertension. Eur J Ophthalmol. 2008;18(3):408-416.<br />
• Wand M, Gilbert CM Liesegang Tj. Latanoprost and herpes simplex keratitis. Am J Ophthalmol<br />
1999:127(5):602-604.<br />
• Bean G, Reardon G, Zimmerman TJ. Association between ocular herpes simplex virus and topical ocular<br />
hypotensive therapy. J Glaucoma. 2004;13(5):361-364.<br />
Coursebook Page 40 of 139<br />
5
*<br />
<strong>Diagnosis</strong> and Management of<br />
Posner-Schlossman Syndrome<br />
Jonee Brandt O.D.<br />
VA Puget Sound Health Care System: American Lake<br />
Division<br />
jonee.brandt@gmail.com<br />
What is Posner-Schlossman<br />
Syndrome<br />
• First described in 1948 by Abraham Schlossman and Adolf Posner<br />
who had a series of 9 patients with similar symptoms and<br />
characteristics of both glaucoma and uveitis.<br />
• Uncommon inflammatory eye condition, classically unilateral, with<br />
elevated intraocular pressures and minimal inflammation.<br />
• Recurrent<br />
• Tends to occur in young-middle aged adults, male>female, with no<br />
racial predilection.<br />
• Accounts for about 4% of all anterior uveititis.<br />
Typical Presentation<br />
*Acute intermittent history of mild blurred vision and minimal unilateral<br />
discomfort<br />
*Mild conjunctival injection, minimal anterior chamber reaction, small to<br />
medium keratitic precipitates, NO posterior synechiae, possible iris<br />
heterochromia/sectoral atrophy, and markedly elevated IOP.<br />
*Acute attacks will resolve spontaneously in a matter of days-weeks<br />
*Recurrence of attacks can vary greatly from patient to patient<br />
<strong>Differential</strong> Diagnoses<br />
• Herpes Simplex Trabeculitis<br />
- Viral infection of endothelial cells of TM, cellular swelling and lysis 2’ to<br />
immune attacks<br />
- Management: IOP control, antivirals, and concurrent topical steroid tx<br />
- May also present with: corneal endotheliitis and 2’ edema<br />
- (+)HSV, possible h/o keratitis<br />
●<br />
<strong>Differential</strong> Diagnoses<br />
Fuch's Heterochromic Iridocyclitis<br />
● Iris heterochromia<br />
● Chronic mild unilateral anterior uveitis which does<br />
NOT respond to steroid treatment<br />
● Triad of heterochromia, cataract, and glaucoma<br />
<strong>Differential</strong> Diagnoses<br />
• Pigmentary Glaucoma<br />
-Krukenberg’s spindle, iris TID’s,<br />
pigment in TM<br />
-glaucomatous changes to optic nerve<br />
head<br />
• Angle Closure/Angle<br />
Closure Glaucoma<br />
-closed angle on gonioscopy<br />
-likely more severe symptoms:<br />
including nausea/vomiting, facial<br />
pain, haloes around lights<br />
Coursebook Page 41 of 139<br />
1
*<br />
<strong>Differential</strong> Diagnoses<br />
• Ankylosing Spondylitis<br />
– Lower back pain<br />
– X-Ray of sacral spinal region and<br />
HLA-B27<br />
• Reiter’s Syndrome<br />
– Triad of arthritis, conjunctivitis,<br />
urethritis<br />
– HLA-B27<br />
• Behcet’s Disease<br />
– Mouth, skin, and/or genital ulcers<br />
– Mediterranean descent<br />
– HLA-B5<br />
<strong>Differential</strong> Diagnoses<br />
• Juvenile Rheumatoid<br />
Arthritis<br />
– Children<br />
– Girls>Boys<br />
– ANA<br />
• (Granulomatous)-<br />
Syphillis/Sarcoidosis<br />
– RPR/VDRL if suspect syphilis (quick<br />
nonspecific), reflect disease activity vs<br />
FTA-ABS and MHA-TP remain<br />
positive for life, even after active<br />
disease<br />
Indicated Testing<br />
• Complete eye examination, including gonioscopy to rule out angle<br />
closure glaucoma/pigmentary glaucoma<br />
• As Posner Schlossman patients present with markedly elevated IOP<br />
during these recurrent attacks monitor closely for developing<br />
glaucomatous changes: RNFL OCT, Threshold Visual Fields<br />
• Appropriate lab testing to rule out systemic causes of inflammation:<br />
– CRP/ANA/HLA-B27<br />
– HLA-B5<br />
– PPD/Chest X-Ray to rule out TB<br />
– CBC with differential: to determine if bacterial or viral<br />
– RPR/VDRL, FTA-Abs, MHA-TP<br />
Possible Etiologies<br />
• Posner and Schlossman first theorized an infectious<br />
etiology due to episodic nature.<br />
• Viral favored due to intermittence of attacks<br />
• Trabeculitis<br />
• Elevated prostaglandin E<br />
Possible Etiologies<br />
Possible Etiologies<br />
• Cytomegalovirus<br />
– Various small scale studies have found that aqueous aspirates of PSS patients<br />
(+)CMV<br />
– Chee et al had first large scale study with 24/105 anterior uveitis pts (+)CMV, but<br />
18 out of those 24 were found to have PSS. 11/18 (+)CMV reverse transciptase on<br />
PCR, during inactive periods pts were (-)CMV<br />
– HOWEVER, seropositivity testing reveals CMV is common in the general<br />
population (87% seropositivity in Singapore, 60-80% in US)<br />
●<br />
Helicobacter Pylori<br />
– Choi et al examined 40 PSS vs 73 normals<br />
– 80% of PSS pts were (+)H. Pylori by ELISA, vs 56.2% normals<br />
– Postulated theory of direct infection to the eye or that H. Pylori increases host<br />
susceptibility for ocular inflammation, possibly through damage to blood vessels<br />
• Herpes Simplex Virus<br />
– 3 patients with active PSS had PCR on aqueous draws<br />
(+)HSV, (-)CMV, (-)VZV<br />
– Subsequent studies have failed to replicate these results<br />
– Treatment of PSS with Acyclovir has been shown to be<br />
ineffective<br />
Varicella Zoster Virus<br />
– 1985 Varicella skin testing revealed that 5/7 pts had PSS<br />
attacks when immune response to varicella was low on skin<br />
testing, and the other 2 with a high immune response<br />
showed no PSS attacks in a 2 year follow up<br />
– Small sample size<br />
Coursebook Page 42 of 139<br />
2
*<br />
Is Posner Schlossman Syndrome<br />
Benign<br />
• CASE PP: 37 yo AM<br />
1 st exam in 09/2007: Pt at that time reports recurrent uveitic<br />
attacks OD x 5-6x/year and reports he felt he was having an attack at<br />
that time: discomfort and slight blurred vision OD.<br />
VA 20/20- OD, OS<br />
IOP 22 OD, 14 OS mmHg<br />
C/D ratio 0.5 H/V OD, 0.4 H/V OS<br />
Assessment: Recurrent non-granulomatous anterior uveitis OD<br />
Plan: Scopolamine bid, Cosopt bid, Pred Forte q2hr OD, RTC 3<br />
weeks for follow up<br />
Date<br />
Acute<br />
Attack<br />
vs<br />
Follow<br />
Up<br />
Visual Acuity<br />
OD, OS<br />
9/29/2007 AA 20/20‐ OD,<br />
OS<br />
IOP<br />
OD, OS<br />
Present<br />
ocular meds<br />
Plan<br />
22, 14 None PF q2hr,<br />
scop bid,<br />
cosopt bid<br />
OD. RTC 3<br />
days<br />
10/1/07 FU 20/25 OD, OS 12, 12 PF q2hr, scop<br />
bid, cosopt<br />
bid OD<br />
10/5/2007 FU 20/25 OD<br />
20/20 OS<br />
10, 14 PF qid, Scop<br />
bid, Cosopt<br />
bid OD<br />
PF qid,<br />
continue<br />
Scop/coso<br />
pt bid OD<br />
RTC 4<br />
days<br />
Taper PF,<br />
d/c<br />
Cosopt<br />
and scop<br />
OD<br />
RTC 3<br />
weeks<br />
Additional<br />
Recurrent<br />
NG<br />
Anterior<br />
Uveitis<br />
“”<br />
“”<br />
Date AA vs FU Visual<br />
Acuity<br />
OD, OS<br />
1/30/12 AA 20/15,<br />
20/20<br />
2/10/12 FU 20/15,<br />
20/20<br />
3/5/12 FU with<br />
AA:<br />
symptoms<br />
presented<br />
yesterday<br />
20/15,<br />
20/20<br />
3/19/12 FU 20/20 OD,<br />
OS<br />
IOP<br />
OD, OS<br />
Present ocular meds<br />
27, 11 Self initiated PF 1day<br />
ago OD<br />
Plan<br />
PF qid and Brimonidine<br />
bid OD, RTC 10 days<br />
8, 11 PF qid, Brim bid OD Taper PF, continue<br />
Brim bid OD<br />
RTC 3 weeks for<br />
DFE/OCT<br />
32, 12 None Begin PF qid x 2 weeks,<br />
Brim bid OD. RTC 2<br />
weeks.<br />
7, 14 PF qid and Brim qd<br />
OD<br />
Taper PF slowly,<br />
continue brimonidine<br />
bid OD. Begin trial IBU<br />
200mg po tid. F/U in 1<br />
mo.<br />
03/05/12<br />
RNFL thickness OCT<br />
Impression:<br />
Good symmetry in a triple<br />
hump pattern OD, OS.<br />
No glaucomatous RNFL<br />
thinning OD, OS.<br />
Is Posner Schlossman Syndrome<br />
Benign<br />
• Case 2: NH 67 yo AAM<br />
– 2007: OS red with 8/10 pain, photophobia, and cloudy vision. Pt<br />
reports several occurrences over past few years. Last occurrence<br />
3-4 mos ago and reports it usually resolves in 1 week.<br />
• VA 20/20 OD, 20/30- OS<br />
• Pupils: (+)APD OS<br />
• SLE: +KP’s and 1+ cells OS<br />
• IOP 16 OD/48 OS mmHg<br />
• C/D 0.4 OD, 0.6 OS<br />
• Assessment: Trabeculitis OS<br />
• Plan: Alphagan tid OS, Levobunolol bid OS, Dorzolamide bid OS, IOP check<br />
1 day<br />
Date VA IOP Current ocular meds Plan<br />
4/27/07 20/20, 20/25‐ 16, 36 Brim tid, levo bid, dorz bid, PF<br />
qid<br />
5/2/07 20/20, 20/25 16, 15 Brim tid, levo bid, dorz bid, PF<br />
taper<br />
CPM, RTC 5<br />
days<br />
Taper PF, RTC 2<br />
weeks for<br />
CEE/IOP check<br />
6/5/07 20/20, 20/25 18, 18 Self D/C all meds Start Cosopt tx<br />
bid OS, RTC 6<br />
mos for<br />
HVF/OCT/IOP<br />
12/6/07 20/20, 20/25 18, 22 Cosopt bid OS<br />
RTC 6 weeks<br />
for IOP check.<br />
***FDT at this date showed<br />
nasal step and early inferior<br />
arcuate defect OS. C/D 0.4<br />
OD, 0.6 OS<br />
LOST TO FOLLOW UP<br />
4/10/09 20/20, 20/30‐ 19,54 D/C cosopt bid OS<br />
C/D : 0.45 OD, 0.95 OS<br />
***OCT today<br />
Cosopt bid,<br />
Brim bid, PF qid<br />
OS<br />
Coursebook Page 43 of 139<br />
3
*<br />
Date<br />
Visual Acuity<br />
OD, OS<br />
IOP<br />
OD, OS<br />
Current Ocular<br />
Meds<br />
03/2011 20/20, 20/25 17, 18 Cosopt and<br />
Brimonidine<br />
bid OU, PF bid<br />
OS<br />
04/11 20/20, 20/25 20, 25 Cosopt only bid<br />
OU<br />
06/11 20/20, 20/40 16, 15 Cosopt bid,<br />
Brim bid OU<br />
Plan<br />
CPM, D/C PF.<br />
RTC 1 mo with<br />
glaucoma<br />
specialists<br />
Reinitiate<br />
brimonidine<br />
bid OU. RTC 1<br />
mo<br />
RTC 3 mos with<br />
GLC specialists<br />
08/11 20/20, 20/40 16, 15 “ RTC 3 mos for<br />
HVF/IOP<br />
11/22/11** 20/20, 20/40 18, 35 “ Add PF qid OS,<br />
RTC 2 days<br />
11/24/11** 20/20, 20/40 12, 28 “+PF qid OS RTC 1 week<br />
Date DVA IOP Current ocular meds Plan Additional<br />
01/11/12 20/20,<br />
20/50<br />
02/08/12 20/20,<br />
20/50<br />
03/08/12 20/20,<br />
20/50<br />
04/10/12 20/20,<br />
20/50<br />
4/17/12 20/20,<br />
20/50<br />
05/3/12 20/20,<br />
20/50<br />
14, 20 Cosopt, Brim bid OU Add PF qid x 10 days<br />
OS. Begin<br />
Latanoprost qhs OS.<br />
RTC 10 days<br />
12, 13 Cosopt, Brim bid OU, RTC 4 mos HVF<br />
Latanoprost qhs and PF<br />
tid OS<br />
13, 34 “” without PF OS Add PF qid OS. RTC 1<br />
week<br />
8, 26 Cosopt bid, Brim bid<br />
OU, Latanoprost qhs OS<br />
Add Rimexolone qid<br />
OS, RTC 1 week<br />
11, 15 “” +Rimexolone qid OS RTC for previously<br />
scheduled F/U with<br />
GLC specialists 2‐3<br />
weeks<br />
12, 16 “” RTC 2‐3 mos for HVF.<br />
Still no improvement<br />
of Bell’s Palsy R side.<br />
Dx Pituitary<br />
Microadenoma<br />
Recent onset<br />
Bell’s Palsy R<br />
side<br />
Hold HVF until<br />
Bell’s Palsy<br />
improved R<br />
side.<br />
Failed to<br />
follow up in<br />
GLC clinic.<br />
04/10/2009<br />
Impression:<br />
OD: no glaucomatous<br />
RNFL thinning<br />
OS: severe RNFL<br />
thinning S/I/T and<br />
borderline nasal. Avg<br />
thickness 93 OD, 43<br />
OS<br />
03/24/2011 HVF 24-2<br />
OD: GHT ONL, MD -9.06dB, PSD 10.96dB. Great Reliability<br />
OS: GHT ONL, MD -32.05dB, PSD 1.81dB. Great Reliability<br />
Impression:<br />
OD: Avg thickness 81 (from 93), with mild flattening of curves overall. New borderline<br />
nasal thinning since last<br />
OS: Avg thickness 35 (from 43), overall flattening, severe thinning.<br />
Is Posner Schlossman Syndrome<br />
Benign<br />
• Retrospective review of all patients with PSS seen at Uveitis Clinic of<br />
Singapore National Eye Center: 53 eyes of 50 patients<br />
– Mean age at onset: 35<br />
– 22 Female/28 Male<br />
– Mean duration of disease: 7 years<br />
– No patients had steroids or antiglaucoma tx between attacks<br />
– 14/53 eyes developed glaucomatous damage 2’ to repeated attacks (26.4%)<br />
– 11/14 eyes had normal discs/fields initially, but over a mean of 10 years had<br />
disc/field damage<br />
– Only predictive factor in development of glaucoma is duration of disease<br />
– Risk of glaucoma developing after 10 years of exposure is 2.8x higher than in
*<br />
• 9/14 glaucomatous eyes underwent glaucoma filtering surgery: 1<br />
trabeculectomy with MMC and 8 trabeculectomy with 5-FU<br />
• Mean post op F/U 37 mos, with a mean IOP at last visit of 10mmHg<br />
• 1/9 required glaucoma medications, all of the rest did not<br />
• In the year prior to surgery these 9 eyes had 3-4 iritis attacks each. After<br />
surgery, 6 of these eyes had no further attacks. In the 3 eyes with<br />
further attacks, 2 did not have an increase in IOP, and 1 had 15 attacks<br />
with elevated IOP causing failure of the bleb and progression of<br />
glaucomatous damage.<br />
• PROBLEMS OF STUDY: followed at 6 mo intervals, with instructions<br />
to return earlier if experiencing an attack (reliable pts)<br />
Management<br />
• Treatment doesn’t shorten length of attack<br />
• During an attack inflammation responds well to<br />
topical steroids: prednisolone acetate 1% qid<br />
• IOP control: ocular hypotensive agents<br />
• Careful monitoring of glaucomatous changes with<br />
RNFL OCT and HVF<br />
Possible Treatments<br />
Surgical Options<br />
• Topical Ganciclovir for possible CMV etiology<br />
– Chee et al 10 pts with (+)CMV PSS began oral gancyclovir, oral<br />
valgancyclovir, or intravitreal gancyclovir. All had decrease in attack<br />
frequency and duration of inflammation.<br />
– A follow up study found that systemic gancyclovir for 12 weeks had<br />
cessation of episodes and normalized IOP during treatment in 91%,<br />
topical 64%. But topical had lower recurrence rate (only 57%, vs 80%<br />
systemic)<br />
– Shortcoming of study: PSS recurrence can be separated by months-years.<br />
Treatment success could have been normal time period between<br />
exacerbations<br />
• Not enough evidence to prove efficacy at this time<br />
• Oral or topical NSAID Not enough research<br />
Trabeculectomy Valve/Shunt Implantation<br />
• No study found directly related to valve success in PSS patients<br />
• Stavrou and Murray: 32 eyes with 20 types of uveitis found that 71.9% of eyes had<br />
a reduction in severity of inflammation and the number of relapses after<br />
trabeculectomy<br />
– None of the operations failed as a result of inflammation<br />
– Pattern of uveitis may be related to success rate<br />
– Improved aqueous outflow may allow inflammatory mediators out of the<br />
anterior chamber<br />
●<br />
●<br />
●<br />
●<br />
●<br />
●<br />
In conclusion...<br />
Posner Schlossman Syndrome is a recurrent unilateral mild anterior<br />
uveitis with marked elevation in intraocular pressures.<br />
Management of an acute attack includes ocular hypotensive agents and<br />
topical steroids<br />
Studies have found that 26.4% of PSS patients will develop<br />
glaucomatous changes in the affected eye.<br />
Most important factor in glaucoma risk analysis is duration of the disease<br />
and likely frequency of attacks.<br />
Importance of careful follow up including optic nerve head OCT/VF<br />
Not enough evidence at this point to determine if filtering surgery for<br />
IOP control or topical antivirals to prevent recurrence are viable<br />
treatment options<br />
References<br />
1. Chee, S. Jap, A. Presumed Fuch’s Heterochromic Iridocyclitis and Posner-Schlossman<br />
Syndrome. Comparison of Cytomegalovirus-Positive and Negative Eyes. American<br />
Journal of Ophthalmology. 2008. 883-889<br />
2. DaMata, A. et al.Management of Uveitic Glaucoma with Ahmed Glaucoma Valve<br />
Implantation. Ophthalmology. 106. 1999. 2168-2172.<br />
3. Green, R. Posner Schlossman Syndrome. Clinical and Experimental Optometry. 2007.<br />
53-56<br />
4. Jap, A. et al. Is Posner-Schlossman Syndrome Benign Ophthalmology. 2001. 913-<br />
918.<br />
5. Siveroj, C. et al. <strong>Diagnosis</strong> and Management of Herpetic Anterior Uveitis. 43-47.<br />
6. Takusagawa, H. et al. Infectious Theories of Posner-Schlossman Syndrome.<br />
International Ophthalmology Clinics. 2011. 105-115.<br />
7. Towler, H. et al. Long-term follow up of Trabeculectomy with Intraoperative 5-FU for<br />
Uveitis related Glaucoma. Ophthalmology. 2000. 1822-1828.<br />
8. Stavrou, P. Murray, P. Does trabeculecomy influence the course of uveitis Ocular<br />
Immunology and Inflammation. 1999. 103-108.<br />
Coursebook Page 45 of 139<br />
5
5/29/2012<br />
Learning Objectives<br />
Case Studies in Contact Lens Correction<br />
for Myopic Refractive Error & Myopia Control<br />
Kelvin So, OD<br />
<strong>Pacific</strong> <strong>University</strong> College of Optometry<br />
Review theories of myopia progression and treatment<br />
options<br />
Understand application of gas permeable (GP) and soft<br />
contact lenses (SCL) for myopia correction and control<br />
Review cases of Orthokeratology and Multifocal Soft<br />
Contact Lens correction for myopia<br />
Clinical Pearls for Orthokeratology and Multifocal Soft<br />
Contact Lens fits<br />
Discuss current research in GP and SCL for myopia<br />
control<br />
Myopia Etiology<br />
9.2% of US children<br />
18.5% in Asian Americans<br />
6.6% in African Americans<br />
80% in Taiwan<br />
Theories of Myopia Progression<br />
Near Work<br />
Near-work induced accommodation causes prolate changes<br />
shape of the globe and axial elongation<br />
Support treatment of using progressive addition lenses<br />
Support treatment of inhibiting accommodation or effecting<br />
ocular physiology with the use of cycloplegic agents including<br />
Atropine and Pirenzepine<br />
Ostrow G, Kirkeby L. Update on myopia and myopic progression in children. International Ophthalmology Clinics 2010; 50: 87-93<br />
Waler TW, Mutti DO. The effect of accommodation on ocular shape. Optometry and Vision Science. 2002; 70:424-430.<br />
Smith EL III, Kee C-S. Ramamirtham R, Qiao-Grider Y, Hung L-F. Peripheral vision can influence eye growth and refractive development in<br />
infant monkeys. Invest Ophthalmol Vis Sci 2005; 46: 3965-3972.<br />
Theories of Myopia Progression<br />
Peripheral Image Shell Theory<br />
Foveal image has no effect on emmetropization<br />
Animal studies using chicks and infant monkeys have shown<br />
peripheral hyperopic retinal stimulus to cause axial elongation<br />
Support treatment of shifting peripheral image shell in front of<br />
the retina with the use of concentric multifocal optics<br />
Waler TW, Mutti DO. The effect of accommodation on ocular shape. Optometry and Vision Science. 2002; 70:424-430.<br />
Smith EL III, Kee C-S. Ramamirtham R, Qiao-Grider Y, Hung L-F. Peripheral vision can influence eye growth and refractive development in<br />
infant monkeys. Invest Ophthalmol Vis Sci 2005; 46: 3965-3972.<br />
Efficacy of Treatment Options<br />
Progressive Addition Lenses<br />
Limited effects in 5 years (COMET Study)<br />
Most significant effects in children with poor accommodation<br />
and esophoric at near (COMET II Study)<br />
Atropine<br />
Toxicity, photophobia, myopia rebound to normal after<br />
treatment cessation<br />
Pirenzepine<br />
Limited follow-up data<br />
Concentric Multifocal Optics<br />
Significant slowing in axial elongation<br />
Gwiazda J, Hyman L, Hussein M, et al. A randomized clinical trial of progressive addition lenses verses single vision lenses on the progression<br />
of myopia in children. Invest Ophthalmol Vis Sci. 2003; 44: 1492-1500.<br />
Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopic progression. Br J Ophthalmol. 2009;93:1181–1185<br />
Tong L, Huang XL, Koh AL, et al. Atropine for the treatment of childhood myopia: effect on myopia progression after cessation of atropine.<br />
Ophthalmology. 2009;116:572–579<br />
Coursebook Page 46 of 139<br />
1
5/29/2012<br />
Concentric Multifocal Optics<br />
Orthokeratology (Ortho-K)<br />
Over-night wear of reverse-geometry GP lens<br />
Hydrodynamic forces compress central corneal epithelial cells,<br />
and create mid-peripheral epithelial cells hyperplasia<br />
Central corneal flattening corrects for myopia by placing image<br />
at fovea while maintaining myopic peripheral image shell<br />
Concentric Multifocal Optics<br />
Orthokeratology (Ortho-K)<br />
Hydrodynamic forces compress central corneal epithelial cells,<br />
and create mid-peripheral epithelial cells hypertrophy<br />
Choo J, Caroline P, et al. Changes in Cat Epithelium Following Overnight Lens Wear with the Paragon CRT Lens for Corneal Reshaping.<br />
Poster presented at <strong>Pacific</strong> Univeristy. Forest Grove, Oregon.<br />
Concentric Multifocal Optics<br />
Orthokeratology (Ortho-K)<br />
Orthokeratology<br />
Effective for mild to moderate myopia correction<br />
Conventional correction up to -6.00D, maximum correction<br />
beyond -10.00D<br />
Pros<br />
No lens wear during waking hours<br />
Durable lens with years of effective use<br />
Parents responsible for handling lenses<br />
Higher safety profile<br />
Cons<br />
Adaptation period<br />
Potential for corneal abrasion<br />
Reduced treatment zone size with higher myopia correction<br />
Forister JFY et al, Prevalence of contact lens-related complications: UCLA contact lens study. Eye Contact Lens 2009 July;35(4):176-180.<br />
Wagner H, et al (CLAY Group), Risk factors for interruption to soft contact lens wear in children and young adults, Optom Vis Sci, Aug<br />
2011;88(8):973-980.<br />
Concentric Multifocal Optics<br />
Multifocal SCL<br />
Daily wear of SCL with center-distance multifocal optics<br />
Focused foveal image with myopic peripheral image shell<br />
Multifocal Soft Contact Lenses<br />
Effective for mild to high myopia correction<br />
Correction from -0.25D to -20.00D with off-the-shelf lenses<br />
Custom multifocal soft lenses available<br />
Pros<br />
Minimal adaptation period<br />
Cons<br />
Patient also needs to learn application and removal<br />
Potential for infection<br />
Potential for variable optics due to lens centration, movement,<br />
and material<br />
Coursebook Page 47 of 139<br />
2
5/29/2012<br />
Orthokeratology<br />
Fitting Process<br />
Corneal topography<br />
Simulated Keratometry readings<br />
Evaulation of corneal astigmatism<br />
Manifest refraction<br />
Most recent spectacle Rx<br />
Best corrected visual acuity<br />
Orthokeratology<br />
Fitting Process<br />
Consult fitting chart for appropriate lens<br />
Order based on sliding rule<br />
Orthokeratology<br />
Fitting Process<br />
Upload topography and manifest refraction data to lens fit<br />
simulator<br />
Adjust lens parameters to optimize fit prior to ordering lenses<br />
Orthokeratology<br />
Fit evaluation<br />
“Bullseye” NaFl pattern<br />
Approximately 0.5mm movement<br />
Vision corrected to best spectacle corrected visual acuity<br />
Dispense lens if all three criteria are met and patient/parent<br />
can successfully apply and remove lens<br />
Orthokeratology<br />
Follow-up<br />
One night follow-up the next morning to evaluate lens fit and<br />
myopia correction<br />
Tangential difference display on topographer to evaulate<br />
centration<br />
“Smiley face” crescent suggest high riding lens<br />
“Frowny face” crecsent suggest low riding lens, often better visual<br />
outcome<br />
Axial difference display on topographer to evaluate correction<br />
Correction over visual axis is key<br />
Followed by one week, one month, then three months followup<br />
schedule.<br />
Evaluate vision and corneal integrity at each appointment<br />
Orthokeratology<br />
Case Study: RF<br />
9 YOAM<br />
Both parents myopic<br />
Approximately 0.50D myopia progression every 6 months<br />
Spectacle correction for myopia<br />
Attempted Ortho-K lens dispense 1/2011, patient unable to<br />
keep lids open for safe lens application and removal<br />
Parents and patient practiced artificial tears instillation at home<br />
RTC 8/2011 to attempt Ortho-K again<br />
MRx:<br />
OD: -6.00-0.50x180 20/20<br />
OS: -6.25-0.75x180 20/20<br />
Coursebook Page 48 of 139<br />
3
5/29/2012<br />
Orthokeratology<br />
Case Study: RF<br />
Topography<br />
Orthokeratology<br />
Case Study: RF<br />
CRT Dual Axis Lens Simulator<br />
Orthokeratology<br />
Case Study: RF<br />
CRT Dual Axis Lens Simulator<br />
Orthokeratology<br />
Case Study: RF<br />
CRT Dual Axis Lens Simulator<br />
Orthokeratology<br />
Case Study: RF<br />
CRT Dual Axis Lens Simulator<br />
Orthokeratology<br />
Case Study: RF<br />
Initial lens ordered and dispensed 9/2011:<br />
OD: Paragon CRT Dual Axis 8.9/550/600/35/11.0<br />
OS: Paragon CRT Dual Axis 8.8/550/600/34/11.0<br />
Slightly high riding lens<br />
Lens rest on lower lid due to tight lid architecture<br />
Expect improved centration with lid closure<br />
Dispensed for over-night wear<br />
Coursebook Page 49 of 139<br />
4
5/29/2012<br />
Orthokeratology<br />
Case Study: RF<br />
One-night follow-up the next morning<br />
Slightly high correction zone (smiley face)<br />
Uncorrected VA 20/50- OU<br />
Good corneal integrity<br />
Orthokeratology<br />
Case Study: RF<br />
One-night follow-up difference display<br />
Continue lens wear for one week<br />
Orthokeratology<br />
Case Study: RF<br />
One-week follow-up<br />
Slightly high correction zone<br />
Uncorrected VA 20/50- OU<br />
Good corneal integrity<br />
Topography shows residual myopia OU<br />
Adjust lens parameters to increase corneal flattening using simulator<br />
Orthokeratology<br />
Case Study: RF<br />
New Parameters ordered and dispensed 10/2011<br />
OD: Paragon CRT Dual Axis 9.1/575/34/600/36/11.0<br />
OS: Paragon CRT Dual Axis 9.0/575/34/600/36/11.0<br />
Flattened Base Curve to increase central corneal flattening<br />
Adjusted individual axis to improve lens centration<br />
Flatten base curve to enhance central corneal flattening<br />
Steepen Landing Zone Angle at one meridian to match steeper<br />
vertical corneal meridian<br />
Orthokeratology<br />
Case Study: RF<br />
Follow-up with flatter base curve dual-axis lenses<br />
Central corneal staining with mild irritation and conj injection OD<br />
Uncorrected VA 20/25 OU<br />
Wider, slightly higher treatment area<br />
Axial difference display reveal residual myopia OS<br />
Orthokeratology<br />
Case Study: RF<br />
Discontinue lens wear<br />
Moxeza ophthalmic solution 1gtt bid x 5 days OD<br />
Nevanac ophthalmic suspension 1 gtt tid x 5 days OD<br />
Consider Multifocal SCL at follow-up<br />
Coursebook Page 50 of 139<br />
5
5/29/2012<br />
Orthokeratology<br />
Case Study: RF<br />
Completely healed corneal abrasion with no scarring on f/u<br />
Parent motivated to continue Ortho-K due to convenience of<br />
no lens wear during waking hours, was educated on corneal<br />
complications due to high myopia, agreed to try SCL.<br />
Multi-focal Soft Lenses<br />
Ordered and dispensed 11/2011<br />
OD: Proclear Multifocal 8.7/-5.50/14.4/+2.50Add/D Lens 20/20<br />
OS: Proclear Multifocal 8.7/-6.00/14.4/+2.50Add/D Lens 20/20<br />
Tangential difference display shows centered treatment zone<br />
Axial difference display shows full myopia correction over<br />
visual axis, with +1.50 D add at pupil margin.<br />
Multi-focal Soft Lenses<br />
Increase Add to reduce peripheral myopia correction:<br />
OD: Proclear Multifocal 8.7/-5.50/14.4/+3.00Add/D Lens 20/20<br />
OS: Proclear Multifocal 8.7/-6.00/14.4/+3.00Add/D Lens 20/20<br />
Multi-focal Soft Lenses<br />
Increase Add to reduce peripheral myopia correction:<br />
OD: Proclear Multifocal 8.7/-5.50/14.4/+3.00Add/D Lens 20/20<br />
OS: Proclear Multifocal 8.7/-6.00/14.4/+3.00Add/D Lens 20/20<br />
Clinical Pearls<br />
Orthokeratology<br />
Practice Makes Perfect<br />
Have patient and parents practice artificial tears instillation to improve lid<br />
manipulation and facilitate corneal de-sensitization prior to fitting.<br />
Sleep It Off<br />
Adaptation takes place rapidly in children, especially in over-night wear.<br />
Take It Step by Step<br />
When correcting high myopia, strive for lens centration first with partial<br />
correction and SCL wear during the day, and progressively increase<br />
corneal flattening to achieve full correction.<br />
Be a Boy Scout (Be Prepared!)<br />
Corneal abrasions do happen, and are easily treated with antibiotic cover,<br />
as well as NSAID to improve comfort and control healing process. Have<br />
these medications ready in-office.<br />
Clinical Pearls<br />
Multi-focal Soft Lenses<br />
Topography over SCLs<br />
Difference map comparing baseline topography and topography over<br />
SCL will show effective power over visual axis, and peripheral add<br />
Angle Lambda<br />
Centered lens on cornea does NOT mean centered optics over visual<br />
axis, perform corneal topography prior to fitting to predict success<br />
Foveal Image Clarity is KEY<br />
If lenses are decentered, it is possible that the foveal image is overplused,<br />
consider adding minus to distance power to achieve optimal<br />
distance vision<br />
High Add<br />
Start with minimum of +2.50 Add, increase to +3.00 Add if needed<br />
Maldonado-Codina et al. Comparative clinical performance of rigid versus soft hyper Dk contact lenses used for continuous wear. Optom Vis<br />
Sci, 2005;82(6):536-548.<br />
Coursebook Page 51 of 139<br />
6
5/29/2012<br />
Research Findings<br />
How Much Add<br />
Peripheral image shell have increasing effectiveness with<br />
increase in add<br />
Ortho-K patients perform best if baseline refractive error is<br />
high<br />
Multi-focal soft lenses allow increase in peripheral add even in<br />
low myopes<br />
Case Study<br />
JS & GS<br />
Twins with low myopia<br />
OD fitted with +2.50D add, OS fitted with +3.00D add<br />
At 1 year follow-up, OD showed myopia progression in both twins<br />
while OS stabilized<br />
Lampa M, So K, et al. Assessing Soft Multifocal Contact Lens Centration with the Aid of Corneal Topography. Poster presented at Global<br />
Specialty Lens Symposium. Las Vegas, NV. 2012.<br />
Research Findings<br />
Aspheric ortho-k lens design<br />
Aspheric back surface to induce more mid-peripheral<br />
steepening compared to conventional design<br />
Attempts to induce higher mid-peripheral myopia to increase<br />
myopia control effectiveness<br />
Traditional OK Design<br />
Base Curve: 8.23 mm 41.00 D.<br />
Research Findings<br />
Aspheric ortho-k lens design<br />
Aspheric back surface to induce more mid-peripheral<br />
steepening compared to conventional design<br />
Attempts to induce higher mid-peripheral myopia to increase<br />
myopia control effectiveness<br />
Traditional OK Design<br />
Base Curve: 8.23 mm 41.00 D.<br />
Aspheric OK Design<br />
Base Curve: 8.23 mm 41.00 D.<br />
Aspheric OK Design<br />
Base Curve: 8.23 mm 41.00 D.<br />
Adjunct Therapies<br />
Time outdoors<br />
Sydney Myopia Study in2008 showed sig reduction in myopia<br />
prevalent in children with more time spent outdoors. Light<br />
intensity may play a larger role when outdoor due to<br />
decreased image blur and increased depth of field.<br />
Low-dose atropine<br />
Compared to 1.0% atropine, 0.1% atropine has been reported<br />
to have similar effects on controlling axial elongation but<br />
without the side effects.<br />
Rose KR, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115:1279–1285.<br />
Cooper J. Using Atropine as A Primary or As An Adjunctive Treatment to Control Myopia. Lecture Presented at Vision by Design 2012<br />
converence . Scottsdale, AZ. 2012.<br />
Closing Remarks<br />
Both ortho-keratology and multifocal soft lenses are non-pharmaceutical<br />
options for myopia control.<br />
Corneal topography is essential in ortho-keratology, and can greatly<br />
enhance multi-focal soft lens fitting.<br />
Ortho-keratology provides convenient vision correction for children<br />
without need for daytime lens wear.<br />
Multi-focal soft lenses can provide additional peripheral add for low<br />
myopes, while research is underway for ortho-k lenses to provide similar<br />
optics.<br />
Myopia controlling optics should be standard of care for myopic patients.<br />
Coursebook Page 52 of 139<br />
7
5/29/2012<br />
References<br />
Cooper J. Using Atropine as A Primary or As An Adjunctive Treatment to Control Myopia. Lecture Presented at Vision by<br />
Design 2012 converence . Scottsdale, AZ. 2012.<br />
Forister JFY et al, Prevalence of contact lens-related complications: UCLA contact lens study. Eye Contact Lens 2009<br />
July;35(4):176-180.<br />
Gwiazda J, Hyman L, Hussein M, et al. A randomized clinical trial of progressive addition lenses verses single vision lenses on<br />
the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003; 44: 1492-1500.<br />
Hom MM, Bruce AS, Consider lid geometry when fitting RGP lenses, Ocular Surgery News, US Edition, June 1, 2000<br />
Lampa M, So K, et al. Assessing Soft Multifocal Contact Lens Centration with the Aid of Corneal Topography. Global Contact<br />
Lens Symposium, Las Vegas, NV. 2012.<br />
Maldonado-Codina et al. Comparative clinical performance of rigid versus soft hyper Dk contact lenses used for continuous<br />
wear. Optom Vis Sci, 2005;82(6):536-548.<br />
Rose KR, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology.<br />
2008;115:1279–1285.<br />
Siatkowski RM, Cotter SA, Crockett RS, et al. Two-year multicenter, double-masked, placebo-controlled, parallel safety and<br />
efficacy study of 2% pirenzepine ophthalmic gel in children with myopia. Ophthalmology. 2008;12:332–339.<br />
Stapleton F, Keay L, Edwards K et al. The Incidence of Contact Lens-Related Microbial Keratitis in Australia. Ophthalmology.<br />
2008. 115 (10): 1655-62.<br />
Tong L, Huang XL, Koh AL, et al. Atropine for the treatment of childhood myopia: effect on myopia progression after cessation<br />
of atropine. Ophthalmology. 2009;116:572–579.<br />
Tan DTH, Lam DS, Chua WH, et al. One-year multicenter, double-masked, placebocontrolled, parallel safety and efficacy study<br />
of 2% pirenzepine ophthalmic gel in children with myopia. Ophthalmology. 2005;112:84–91.<br />
Wagner H, et al (CLAY Group), Risk factors for interruption to soft contact lens wear in children and young adults, Optom<br />
Vis Sci, Aug 2011;88(8):973-980.<br />
Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopic progression. Br J Ophthalmol. 2009;93:1181–1185.<br />
Coursebook Page 53 of 139<br />
8
5/29/2012<br />
OVERVIEW<br />
ENDOTHELIAL CHANGES<br />
ASSOCIATED WITH INTRAOCULAR<br />
LENS SURGERY<br />
Benefits and risks.<br />
Corneal responses.<br />
Specular microscopy as a clinical tool.<br />
Research study: endothelial cell<br />
densities/structure after IOL surgeries.<br />
Future directions.<br />
Alison She, OD<br />
IRIS Ophthalmology Clinic, Langley, BC<br />
Primary Care/Ocular and refractive surgery<br />
INTRAOCULAR LENS IMPLANTS<br />
Benefits:<br />
• Vision.<br />
• Efficiency.<br />
• Clear lens exchange.<br />
Risks:<br />
• Post-op side effects.<br />
• Worst case scenarios.<br />
SIGNIFICANCE OF THE ENDOTHELIUM<br />
Barrier that regulates fluid uptake into cornea.<br />
Transport nutrients into corneal tissue.<br />
Endothelium disruption of cell membrane pumps<br />
affects fluid balance, causing …<br />
• corneal edema,<br />
• haze,<br />
• scarring.<br />
From: Baker Eye Institute<br />
ENDOTHELIAL HEALING<br />
Cornea endothelium does not regenerate well after<br />
damage.<br />
Endothelium self-repairs by existing cells migrating<br />
to fill gaps.<br />
• Perimeter cells around injury site enlarge and move to<br />
fill in damaged areas.<br />
• Cell densities generally decrease with age.<br />
• Natural rate of cell density decrease: 0.5%/year<br />
If the cell density drops too low:<br />
• affects fluid barrier stability.<br />
Coursebook Page 54 of 139<br />
1
5/29/2012<br />
WHAT CAUSES ENDOTHELIAL DAMAGE<br />
DURING SURGERY<br />
Energy from phacoemulsification<br />
Air bubble pressure behind cornea<br />
Turbulence from fluid and lens<br />
fragments during surgery<br />
SURGICAL VARIABLES<br />
VISCOELASTIC SOLUTIONS<br />
More<br />
advanced<br />
cataract<br />
Greater<br />
phaco<br />
energy<br />
Longer<br />
surgical<br />
time<br />
Definition: Protective solution injected into anterior<br />
chamber during cataract surgery.<br />
Purpose:<br />
• Protects endothelium from instruments and<br />
phacoemulsification pressure.<br />
• Maintains anterior chamber depth.<br />
• Opens capsular space to insert IOL.<br />
• Keeps incisions closed when instruments removed from<br />
anterior chamber<br />
Greater<br />
endothelial<br />
loss<br />
Viscoelastic can affect surgical outcome.<br />
PROPERTIES OF DUOVISC ®<br />
PROVISC ® VISCOAT ® KONAN non-contact<br />
SPECULAR MICROSCOPY<br />
specular microscope.<br />
Cohesive<br />
High M.W.<br />
Sodium hyaluronate<br />
Dispersive<br />
Medium M.W.<br />
Sodium hyaluronate +<br />
sodium chondroitin<br />
Parameters measured:<br />
• Cell density<br />
• Cell morphology<br />
Historical significance.<br />
Coursebook Page 55 of 139<br />
2
5/29/2012<br />
SPECULAR MICROSCOPY APPLICATIONS<br />
ENDOTHELIAL CELL COUNT NORMS<br />
Age Average Cell Count (cells/mm 2 )<br />
Diagnose endothelial<br />
dystrophies<br />
Child 3000-4000<br />
20s 2700-3600<br />
30s 2550-3400<br />
Diagnose contact lens<br />
related disorders<br />
40s 2400-3200<br />
50s 2250-3000<br />
60s 2100-2800<br />
70s 1950-2600<br />
Monitor ocular surgery<br />
outcomes<br />
80s 1800-2400<br />
Reference: KONAN microscopy manual FRM-012 Rev. A.<br />
ENDOTHELIUM PROPERTIES<br />
ENDOTHELIUM COMPARISONS<br />
Hexagonality<br />
• Cell shape.<br />
• % cells that are six-sided.<br />
• Normal corneas > 50-60%.<br />
Polymegathism<br />
• Cell size variation.<br />
• Unit of measure: Coefficient of variation (CV).<br />
• Normal range: 0.21-0.33.<br />
1.0 = extremely disrupted cornea.<br />
0 = each cell is precisely identical.<br />
46 year old female 82 year old male<br />
RESEARCH STUDY: CHANGES IN<br />
ENDOTHELIAL CELLS AFTER IOL SURGERY<br />
RESEARCH STUDY<br />
Purpose: evaluate changes in endothelial<br />
cell properties pre & post IOL surgery.<br />
Parameters:<br />
• Cell density.<br />
• Cell hexagonality (shape).<br />
• Cell size variation.<br />
All surgeries at IRIS Ophthalmology<br />
Clinic by same surgeon,<br />
All surgeries used Duovisc ® viscoelastic<br />
solution.<br />
All patients fitted with foldable IOLs.<br />
Coursebook Page 56 of 139<br />
3
5/29/2012<br />
PATIENT SELECTION<br />
Patient age range: 46 to 82 years.<br />
No restrictions on race or gender.<br />
Non-candidates:<br />
• diabetic retinopathy,<br />
• uncontrolled diabetes mellitus,<br />
• diagnosed endothelial dysfunction.<br />
Patient consent for educational photos and data<br />
collection.<br />
METHODS<br />
n=28 eyes of 17 patients.<br />
• 19 eyes with cataract extraction.<br />
• 9 eyes with clear lens exchange.<br />
Specular microscopy taken post-op:<br />
• 1 day.<br />
• 1 week.<br />
• 1 month.<br />
• 3 months.<br />
Cataracts removed via “stop-and-chop”<br />
phacoemulsification.<br />
RESULTS: CELL DENSITIES<br />
3500<br />
CELL DENSITY: PRE-OP TO 3 MONTHS POST-OP<br />
20<br />
15<br />
CELL DENSITY: % CHANGE FROM PRE-OP<br />
CELLS/MM²<br />
3000<br />
2500<br />
2000<br />
1500<br />
1000<br />
PERCENTAGE<br />
10<br />
5<br />
0<br />
-5<br />
-10<br />
-15<br />
-20<br />
-25<br />
500<br />
0<br />
Pre‐op 1d post 1 wk 1 mth 3 mths<br />
TIME AFTER SURGERY<br />
-30<br />
1 day post‐op 1 wk 1mth 3 mths<br />
TIME AFTER SURGERY<br />
HEXAGONALITY OF CELLS<br />
70<br />
PERCENTAGE OF HEXAGONAL CELLS<br />
CELL VARIANCE<br />
0.6<br />
CELL SIZE VARIATION (POLYMEGATHISM)<br />
PERCENTAGE<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
COEFFICIENT OF VARIATION<br />
0.5<br />
0.4<br />
0.3<br />
0.2<br />
0.1<br />
0<br />
Pre‐op 1 day post‐op 1 wk 1 mth 3 mths<br />
TIME AFTER SURGERY<br />
0<br />
Pre‐op 1 day post‐op 1 wk 1 mth 3 mths<br />
TIME AFTER SURGERY<br />
Coursebook Page 57 of 139<br />
4
5/29/2012<br />
RESEARCH STUDY SUMMARY<br />
Cell density has a larger decrease at 1 day post-op<br />
then gradually recovers over the next 90 days.<br />
High variability at 1 week post op reflects dynamic<br />
nature of endothelium reorganization.<br />
Hexagonality: No statistically significant change pre<br />
vs post surgery long-term.<br />
Polymegathism: No statistically significant change<br />
pre vs post surgery long-term.<br />
FUTURE DIRECTIONS:<br />
PHAKIC IOL SURGERY<br />
Anterior chamber IOL<br />
• AcrySof ® Cachet ® (Alcon)<br />
• Surgical correction for high<br />
refractive errors > 6 D.<br />
Guidelines:<br />
• Specular microscopy at<br />
Pre-op.<br />
6 months post-op.<br />
1 year post-op.<br />
FUTURE RESEARCH DIRECTIONS<br />
Monitor at 1-2 + years post-surgery.<br />
Evaluate systemic factors in endothelial healing:<br />
• Diabetes.<br />
• Inflammatory conditions (arthritis, lupus, etc).<br />
Compare cell loss in:<br />
• Clear lens exchange vs. cataract extraction.<br />
• Long-term monitoring after phakic IOL surgery.<br />
SUMMARY<br />
REFERENCES<br />
Mencucci, R., Ponchietti, C., Virgili, G., Giansanti, F., Menchini, U. “Corneal endothelial damage after cataract surgery:<br />
Microincision versus standard technique.” J Cataract Refract Surg. 2006; 32:1351-1354.<br />
Hengerer, F.H., Dick, H.B., Buchwald, S., Hütz, W.W., Conrad-Hengerer, I. “Evaluation of corneal endothelial cell loss<br />
and corneal thickness after cataract removal with light-adjustable intraocular lens implantation: 12-month follow-up.” J<br />
Cataract Refract Surg. 2011; 37:2095-2100.<br />
Albert, D.M., Jakobiec, F.A. Principles and Practice of Ophthalmology. 1994. W.B. Saunders Company: Philadelphia.<br />
Van den Bruel, A., Gailly, J., Devrieses, S., Welton, N.J., Shortt, A.J., Vrijens, F. The protective effect of ophthalmic<br />
viscoelastic devices on endothelial cell loss during cataract surgery: a meta-analysis using mixed treatment<br />
comparisons. Br J Ophthal. 2011; 95:5-10.<br />
Remington, L. Clinical Anatomy of the Visual System, 2 nd Edition. 2005. Elsevier: Missouri.<br />
Kiss, B., Findl, O., Menapace, R., Petternel, V., Wirtitsch, M., Lorang, T., Gengler, M., Drexler, W. “Corneal endothelial<br />
cell protection with a dispersive viscoelastic material and an irrigating solution during phacoemulsification. Low cost<br />
versus expensive combination.” J Cataract Refract Surg. 2003; 29: 733-740.<br />
Pereira, ACA., Porfirio, F., Freitas, LL., Belfort, R. “Ultrasound energy and endothelial cell loss with stop-and-chop and<br />
nuclear preslice phacoemulsification.” J Cataract Refract Surg. 2006; 32:1661-1666.<br />
Gogate, P., Ambardekar, P., Kulkarni, S., Deshpande, R., Joshi, S., Deshpande, M. “Comparison of endothelial cell<br />
loss after cataract surgery: Phacoemulsification versus manual small-incision cataract surgery. Six week results of a<br />
randomized control trial.” J Cataract Refract Surg. 2010; 36:247-253.<br />
Daly, L., Bourke, J. Interpretation and Uses of Medical Statistics, Fifth Edition. 2000. Blackwell Sciences: UK.<br />
Rainer, G., Stifter, E., Luksch, A., Menapace, R. “Comparison of the effect of Viscoat ® and DuoVisc ® on Postoperative<br />
intraocular pressure after small-incision cataract surgery.” J Cataract Refract Surg. 2008; 34:253-257<br />
Baryanovits, P. “Stabilisation of refraction following cataract surgery.” Br J Ophthal. 1988; 72 815-819<br />
Thomas, Craig. The Specular Microscopy Primer. KONAN Medical.<br />
Kanski, J. Clinical Ophthalmology, 6 th Edition. 2007. Butterworth Heinemann: Toronto.<br />
Duovisc product insert, Alcon.<br />
THANK YOU!<br />
QUESTIONS<br />
Coursebook Page 58 of 139<br />
5
5/29/2012<br />
Objective<br />
• Corneal infections are a common and sight-threatening condition which<br />
can progress very quickly, leading to extensive corneal tissue<br />
destruction and possible perforation.<br />
BIC TRINH O.D<br />
EYECARE ASSOCIATES OF NEVADA<br />
Case Report: Persistent epithelial defect<br />
in post-corneal graft<br />
• Being able to recognize and appropriately treat these conditions is<br />
critical in preserving vision. Today we will review the different etiologies,<br />
appropriate work up and management of different corneal infections.<br />
J.G 57 yo male<br />
Entrance testing<br />
• Patient<br />
◦ 57 Y.O Hispanic Male<br />
◦ Hx of longstanding corneal ulcer, OS<br />
• HPI<br />
◦ (+) mild watery discharge, photophobia, foreign body sensation<br />
◦ No h/o contact lens wear, outdoor activity, trauma<br />
• Gtts<br />
◦ Durezol tid OS x 3 mo<br />
• Oc Hx<br />
◦ Penetrating keratoplasty OS x 20 years<br />
• Medical Hx:<br />
◦ Heart disease<br />
◦ Arthritis<br />
◦ NIDDM<br />
◦ Elevated cholesterol<br />
• VA (sc)<br />
◦ OD 20/30-<br />
◦ OS 20/100+ PH/60<br />
• Tonometry<br />
◦ Deferred<br />
• MR:<br />
◦ OD +2.75-1.00x115 20/20<br />
◦ OS +4.00 DS 20/60<br />
Exam<br />
<strong>Differential</strong> diagnosis<br />
• Anterior segment<br />
◦ OS:<br />
Conjunctiva: 2 + injection<br />
Cornea:<br />
Graft intact<br />
1 mm epithelial defect with surrounding infiltrate, 6:00<br />
60-70% stromal thinning<br />
Diffuse corneal haze<br />
Anterior Chamber<br />
D/ 2+ mixed cell<br />
1 mm hypopyon<br />
Lens<br />
3 +NSC<br />
◦ Bacterial keratitis<br />
Gram (-)<br />
Pseudomonas<br />
Gram (+)<br />
S. Epidermis, S. Aureus,<br />
S. Pneumoniae<br />
◦ Herpetic eye disease<br />
Herpes Simplex Keratitis<br />
◦ Fungal keratitis<br />
Fusarium, Aspergillus,<br />
Candida<br />
◦ Persistent epithelial defect<br />
Toxicity<br />
Autoimmune<br />
Ocular surface disease<br />
◦ Acanthomoeba<br />
Coursebook Page 59 of 139<br />
1
5/29/2012<br />
Impression<br />
1 day follow up<br />
• Impression<br />
◦ Bacterial keratitis vs. Persistent epithelial defect, OS<br />
◦ S/p PKP, OS<br />
• Plan<br />
◦ Culture<br />
◦ D/C Durezol<br />
◦ Fortified vancomycin, fortified tobramycin q1h OS<br />
◦ Erythromycin ung qid OS<br />
◦ F/u 1 day<br />
• HPI: improved pain<br />
• Anterior segment<br />
◦ Cornea<br />
(+) graft edema<br />
1mm ED, 60-70% thinning<br />
Haze improved<br />
◦ Anterior chamber<br />
1+ cell<br />
Hypopyon resolved<br />
• Culture<br />
◦ Gram stain: No organisms observed<br />
◦ Media: No growth<br />
• Impression<br />
◦ Non-healing epithelial defect, OS<br />
◦ Graft failure, OS<br />
• Plan<br />
◦ Vancomycin, Tobramycin q3h OS<br />
◦ Erythromycin ung qid OS<br />
Follow up<br />
Follow up<br />
• 5 day f/u<br />
• 1 week f/u<br />
• 2 week f/u<br />
• 6 week f/u<br />
• Anterior segment<br />
• Anterior segment<br />
• Anterior segment<br />
• Anterior segment<br />
◦ Cornea<br />
◦ Cornea<br />
◦ Cornea<br />
◦ Cornea<br />
0.6mm ED, 50% thinning<br />
◦ Anterior chamber<br />
• Plan<br />
D/Q<br />
◦ Vancomycin, Tobramycin,<br />
Erythromycin ung qid<br />
No ED, 50% thinning<br />
1.5 mm V x 1.2 mm H stromal<br />
opacity<br />
• Plan<br />
◦ D/C Vancomycin, Tobramycin<br />
◦ Erythromycin ung qid OS<br />
◦ Lotemax qid OS<br />
1.5 mm V x 1.2 mm H stromal<br />
opacity, 10% thinning<br />
Microcystic edema<br />
Pachs 777 microns<br />
IOP 13/13<br />
• Plan<br />
◦ PF qid OS<br />
Stromal opacity<br />
Microcystic edema<br />
IOP 14/17<br />
• Plan<br />
◦ Taper PF slowly<br />
◦ Possible repeat graft with<br />
phacoemulsification OS to<br />
improve vision<br />
Persistent epithelial defect<br />
Persistent ED: Causes<br />
• Presentation<br />
◦ Foreign body sensation,<br />
photophobia, corneal<br />
hypoesthesia<br />
◦ Central/paracentral or<br />
inferior/inferonasal<br />
◦ Epithelial defect with heaped<br />
edges<br />
◦ Underlying stromal<br />
inflammation<br />
◦ Resistant to maximum<br />
therapy<br />
Topical agents<br />
Auto-immune<br />
Ocular surface disease<br />
Neurotrophic keratitis<br />
Trauma<br />
Aminoglycosides, trifluoridine,<br />
antimetabolites<br />
Sjogren’s syndrome, RA, graft-versushost<br />
disease<br />
Dry eye, exposure keratopathy, atopy,<br />
rosacea, ocular pemphigoid, mooren’s<br />
ulcer, limbal stem cell deficiency, RCE,<br />
bullous keratopathy<br />
Anesthetic abuse, acanthomoeba<br />
keratitis, HSK, HZO<br />
Underlying foreign body, local<br />
irradiation, contact lens use<br />
Coursebook Page 60 of 139<br />
2
5/29/2012<br />
Management<br />
Management<br />
• Obtain corneal culture<br />
• Cycloplegic agent<br />
• Treatment aimed towards surface healing and preventing stromal melt<br />
◦ Stop/ taper medications toxic to epithelium<br />
◦ Lubrication (non-preserved)<br />
◦ BCL<br />
◦ Orals<br />
Omega-3 FA<br />
Doxycycline<br />
• Poor response to previous therapy<br />
◦ Autologous serum<br />
◦ Oral acyclovir<br />
◦ Systemic evaluation<br />
The use of autologous serum tears in persistent corneal epithelial defects<br />
Eye (2004) 18, 609–614 A L Young, A C O Cheng, H K Ng, L Cheng, G Y S Leung and D S C Lam<br />
Healing within<br />
Current series=10<br />
2 weeks (effective) 6 (60%)<br />
1 month (partially effective) 0 (0%)<br />
>1 month (ineffective) 2 (20%)<br />
Defaulted 2 (20%)<br />
ADEs 0 (0%)<br />
Management<br />
AMT with tarsorraphy<br />
• Surgical options<br />
◦ Punctal occlusion<br />
◦ Total tarsorrhaphy<br />
◦ AMT graft with tarsorraphy<br />
◦ PKP<br />
• Amniotic membrane graft<br />
◦ (Amniograft® 2.5x 2.0 cm) placed in<br />
layers<br />
◦ Larger piece of AM placed (stromal<br />
side down) placed over layers<br />
◦ BCL<br />
◦ Tarsorraphy<br />
• ProKera<br />
• Prospective studies<br />
◦ Lee et al (Bascom Palmer), 1997: AMT<br />
performed in 11 pts with PED. 10 pts<br />
healed in 2-6wks without recurrence for 3-<br />
15 mos<br />
◦ Pachigolla et al (<strong>University</strong> of Texas SW),<br />
2009: 20 eyes with ProKera implant for<br />
avg of 25.3 days. 12 eyes noticed<br />
increase in acuity. 5 eyes noticed PED<br />
with removal of device<br />
Bacterial keratitis<br />
Bacterial keratitis<br />
◦ S. Epidermis, S. Aureus, S.<br />
Pneumoniae<br />
◦ Gram (+) cocci<br />
◦ S. Aereus binds to exposed<br />
components of Bowman’s and<br />
stroma<br />
◦ Pseudomonas aeruginosa<br />
◦ Gram (-) rod<br />
◦ P aeruginosa binds to molecular<br />
receptors on exposed epithelial cells<br />
• Presentation<br />
◦ Pain, decreased vision, redness, suppuration<br />
◦ Sharply demarcated epithelial defect<br />
◦ Stromal edema<br />
◦ A/C reaction<br />
◦ Stromal thinning/necrosis<br />
• Risk factors<br />
◦ Contact lens*<br />
◦ Trauma<br />
◦ Medications<br />
◦ Impaired defense mechanisms<br />
Coursebook Page 61 of 139<br />
3
5/29/2012<br />
Management<br />
Management<br />
• Initial therapy<br />
◦ D/C contact lens<br />
◦ Small (
5/29/2012<br />
Fungal keratitis<br />
Fungal keratitis<br />
• 5-10% of keratitis are fungal in<br />
nature<br />
• More common warmer, humid<br />
climate<br />
• Aspergillus, Candida, and<br />
Fusarium<br />
• Risk Factors<br />
◦ Ocular trauma from plant<br />
◦ Contact lens wear<br />
◦ Immunosuppression<br />
◦ Medications<br />
◦ Penetrating keratoplasty<br />
• Presentation<br />
◦ Gray-white infiltrate<br />
◦ Satellite or branching lesions<br />
◦ A/C reaction<br />
◦ May invade iris or posterior chamber<br />
Fungal keratitis<br />
Acanthamoeba<br />
• Management<br />
◦ Topical:<br />
natamycin 5% suspension: effective against most cases<br />
amphotericin B 0.15%-0.30%<br />
◦ Oral: Effect on keratitis is limited secondary to poor penetration and systemic<br />
side effects<br />
ketoconazole 200-600 mg/day<br />
fluconazole 200-400 mg/day<br />
◦ Typical treatment time is 1 month but can be used for several months<br />
◦ Repeat smears may be necessary<br />
• Protozoa<br />
• Highly resistant<br />
• 70% of cases related to contact lens use<br />
Acanthamoeba<br />
Acanthamoeba<br />
• Presentation<br />
◦ Severe pain, photophobia, decreased vision<br />
◦ Epithelial defect<br />
◦ Ring shaped infiltrate<br />
◦ Keratoneuritis<br />
◦ A/C reaction<br />
• Management<br />
◦ Mechanical debridement<br />
◦ Topical therapy (must be compounded)<br />
Biguanides:<br />
Chlorhexidine gluconate 0.02%(CHG) q1h<br />
Polyhexamethylene biguanide 0.02%(PHMB) (Bacquicil) q1h<br />
Diamidines:<br />
Brolene<br />
Desmodine<br />
Coursebook Page 63 of 139<br />
5
5/29/2012<br />
Microbiology<br />
Microbiology<br />
• When is laboratory evaluation by culture<br />
recommended<br />
◦ Size<br />
◦ Depth<br />
◦ Chronic in nature<br />
◦ Atypical features/ history<br />
• How to obtain sample<br />
◦ Topical anesthetic (proparacaine hydrocholoride)<br />
◦ Scrape material from border as well as base of ulcer<br />
◦ Inoculate onto solid media by streaking rows of C’s<br />
Media/Smear<br />
Culture<br />
Chocolate agar<br />
Most bacteria, Haemophilus,<br />
Neisseria, Moraxella<br />
Blood agar<br />
Most bacteria, yeast, fungi<br />
Sabourad’s agar<br />
Non-nutrient agar<br />
Gram stain<br />
Most fungi, yeast<br />
Acanthamoeba<br />
Bacteria<br />
Pearls<br />
References<br />
• Careful history<br />
◦ Systemic history<br />
◦ Prior ocular history<br />
◦ Medications<br />
• Examination<br />
◦ Documentation of defect<br />
◦ Observe structures around eye<br />
◦ Take notice of unique features<br />
• Treatment<br />
◦ Initiate aggressive therapy<br />
◦ Have complete list of DDx<br />
◦ Remember guidelines for culturing<br />
• Price F.W, Price M.O, Letko E. Curbside Consultation in Cornea and External Disease. Indianapolis,<br />
IN: Slack Incorporated;2010: 119-130.<br />
• Cohen EJ, Rapuano CJ. Bacteria keratitis, fungal keratitis, Acanthamoeba, herpes simplex virus,<br />
herpes zoster virus. In Kunimoto DY, Kanitkar KD, Maker MS, Friedberg MA, Rapuano CJ, eds. The<br />
Wills Eye Manual: Office and Emergency Room <strong>Diagnosis</strong> and Treatment of Eye Disease. 4 th ed.<br />
Philadelphia, PA: Lippencott Williams and Wilkins. 2004:52-65.<br />
• Sutphin JE, Dana MR, Florakis GJ. Basic and Clinical Science Course: External Disease and Cornea.<br />
Singapore; 2007: 113-189.<br />
• KrachmerJH, Mannis M, III. Holland EJ. Cornea: Fundamentals, <strong>Diagnosis</strong> and Management. Vol 1.<br />
China;1997:277-307.<br />
• Pachigolla G, Prasher P, Di Pascuale MA. Evaluation of the role of ProKera in the management of<br />
ocular surface and orbital disorders. Eye Contact Lens. 2009 Jul;35(4):172-5.<br />
• Lee SH, Tseng SC. Amniotic membrane transplantation for persistent epithelial defects with ulceration.<br />
Am J Ophthalmology. 1997 Mar; 123(3):303-12.<br />
• Seitz B, Das S, Saur R. Amniotic membrane transplantation for persistent corneal epithelial defects in<br />
eyes after penetrating keratoplasty. Eye (London). 2009 Apr;23(4):840-8<br />
Coursebook Page 64 of 139<br />
6
5/29/2012<br />
Chief Complaint<br />
Blebitis<br />
• Amy Pedersen, OD<br />
• Portland VA Medical Center<br />
• “Rust colored film over my eye”<br />
– Present for 2 days, stable, (‐)pain and (‐)discharge<br />
– Secondary Complaint<br />
• Mild upper left lid tenderness<br />
• Present for the past 3 days, stable<br />
• Self treating with tobramycin QID x 2 days with no<br />
resolution or decrease in symptoms<br />
Ocular History<br />
– Advanced primary open angle glaucoma OU<br />
– S/P trabeculectomy 1991 OU ( UC Davis), revision for<br />
leak in 1995 at PVAMC OD<br />
– Non‐exudative age related macular degeneration<br />
OS>OD, AREDS category 2<br />
– Diabetes mellitus type 2 with mild non‐proliferative<br />
diabetic retinopathy OS only<br />
– Pseudophakia OU s/p cataract extraction at PVAMC<br />
Medications<br />
– Amlodipine besylate, Aspirin (81mg), Insulin (aspart),<br />
Insulin (glargine), Lisinopril, Metoprolol succinate,<br />
Ranitidine, Simvastatin<br />
– Glaucoma: timolol maleate 0.5% oph soln, 1 gtt OU bid<br />
Medical History<br />
– Diabetes mellitus type 2, diagnosed in 1998 (Last A1C 8.1<br />
on 09/13/11)<br />
– Hypertension<br />
– Hyperlipidemia<br />
– GERD<br />
Pertinent Findings‐ 09/16/11<br />
• Visual Acuity: 20/25 OD, 20/30‐2 (PH: 20/25‐2) OS<br />
• Anterior Segment<br />
– Lids/ Lashes: 1+ MGD OU<br />
– Cornea: temporal incisional scar OU<br />
– Conjunctiva:<br />
• OD: temporal pinguecula, trab scar at 12 o'clock<br />
• OS: 1+ injection, trab scar with partial opacity at 12<br />
o'clock with surrounding 2+ injection<br />
– Cornea: temporal incisional scar OU<br />
– Ant. Chamber: OD: Deep & Quiet, OS: trace cells, (‐)flare<br />
– Iris: Normal OU, (‐)NVI<br />
• GAT @4:31pm OD: 17mmHg OS: 8mmHg (Seidel testing<br />
questioned pinpoint leak)<br />
Coursebook Page 65 of 139<br />
1
5/29/2012<br />
Pertinent Findings Contd…<br />
• Posterior Segment<br />
– Lens: PC IOL OU<br />
– Vitreous: OD: Clear OS: PVD; (‐)VH OU<br />
– Optic disc:<br />
• OD: 0.9/0.9; advanced cupping with 3+ pallor; (‐)NVD<br />
• OS: 0.7/0.7; cupping with 2+ pallor; (‐)NVD<br />
– Macula: scattered pinpoint drusen, trace‐1+ RPE changes ; (‐<br />
)CSME OU<br />
– Vitreous: OD: Clear OS: PVD; (‐)VH OU<br />
– Vessels: Normal OU<br />
– (+)Dot/blot heme OS inferior nasally, (‐)Dot/blot heme OD;<br />
(+)MA's OS inferior nasal to disc, (‐)MAs OU; (‐)Hard Exudates<br />
OU; (‐)CWS OU; (‐)IRMA OU; (‐)VB OU; (‐)NVE OU<br />
– Posterior Pole and Periphery:<br />
• OS: chorodial detachment ora to equator 360, (‐)vit cells<br />
• OD: no rips, holes or tears 360 OU<br />
Assessment/Plan<br />
• Blebitis with choridal detachment OS, reduced pressure OS<br />
• Instill 1gtt Vigamox OS q15min in office immediately as<br />
loading dose<br />
• Admit as inpatient‐ Moxifloxacin 1gtt q1h overnight<br />
• RTC tomorrow morning in Eye Medical Retina<br />
Follow Up #1 (9/17/11)<br />
– Relevant Findings<br />
• Visual Acuity: 20/25‐1 OD, 20/70‐2 (PH: 20/70‐1) OS<br />
• Conjunctiva OS: significant superior 2‐3+ bleb injection, Seidel<br />
positive centrally, purulent appearance<br />
• Ant. Chamber: OS: 1+ cell with trace pigmented cell<br />
• GAT@9:00am OD: 21 mmHg OS: 2 mmHg<br />
• Choroidal detachment 360 degrees OS, (‐)vitreous cell and flare<br />
– Assessment/Plan<br />
• Blebitis OS ‐ appears to be clinically improving, with no evidence<br />
of endopthalmitis.<br />
• Continue Vigamox q1h during daytime, q3h at night; intiate 1gtt<br />
atropine qd OS, timolol 0.5% bid OD only<br />
• RTC 2 days in Eye Medical Retina<br />
Follow Up #2 (9/19/11)<br />
– Chief Complaint: Follow up of blebitis OS. Soreness same as before.<br />
Feels that OS is blurry. Moxifloxacin q1h in daytime, q3‐4 h at night<br />
OS, 1% Atropine qd OS, 0.5% timolol bid OD.<br />
– Relevant Findings<br />
• Visual Acuity: 20/25‐2 OD, 20/150 (PH 20/50‐2) OS<br />
• Cornea: OS mild superior thinning and vascularization near the blebitis, some<br />
Descemets folds, bleb has infiltration in the center, Seidel positive in center of<br />
the bleb, 2+conj injection superiorly<br />
• Anterior Chamber: OS rare cells<br />
• GAT@3:33pm OD: 12 mmHg OS: 0 mmHg<br />
• Posterior Pole & Peripheral Retina: 360 degree choroidal detachment OS<br />
– Assessment/Plan<br />
• Blebitis with leak OS, resolving anterior chamber reaction with hypotony and<br />
choroidal detachment OS<br />
• Cont Moxifloxacin q1h in the day and q3‐4h at night,1% Atropine eye drops OS<br />
qd and 0.5% timolol bid OD<br />
• Will schedule for bleb revision , tomorrow if possible<br />
Bleb Revision Surgery‐ 1 day post‐op<br />
– Relevant Findings<br />
• VA: 20/200 OS; PH not performed<br />
• Superior bleb revision, (‐)Seidel with intact sutures<br />
• GAT@9:45am OS: 23 mmHg with distorted mires<br />
– Assessment/Plan<br />
• One day post bleb revision with patch graft OS‐ good<br />
closure with no leaks, mild ocular HTN today<br />
• Start Pred Forte q2‐3 hours OS and Vigamox QID OS and<br />
Cosopt BID OS, continue timolol bid OD<br />
1 week post‐op (9/26/11)<br />
– Relevant Findings<br />
• VA OD: 20/25‐ OS: 20/50‐2; PH not performed<br />
• Conjunctivia OS‐ Seidel negative with 1 pair of nylon suture<br />
ends that are mildly exposed, all other suture ends are<br />
vicryls<br />
• GAT@9:37am OD: 16 OS: 14<br />
– Assessment/Plan<br />
• One week post bleb revision with patch graft OS, good<br />
closure with no leaks. Nylon suture ends cut at slit lamp.<br />
• Improved IOP with topical Cosopt, taper Pred to QID OS, D/C<br />
Cosopt OS; continue 0.5% timolol bid OD<br />
• RTC 1 week<br />
Coursebook Page 66 of 139<br />
2
5/29/2012<br />
2 week post‐op (10/3/11)<br />
– Relevant Findings<br />
• VA: 20/25 OD, 20/40 OS; PH not performed<br />
• Conjunctivia OS‐ Seidel positive with slow leak along<br />
perilimbal bleb, otherwise intact<br />
• GAT@11:15am OD: 18 mmHg OS: 11 mmHg<br />
– Assessment/Plan<br />
• Bandage Contact Lens OS<br />
• Taper Pred BID OS, restart Vigamox with bandage CL;<br />
continue 0.5% timolol bid OD<br />
• RTC 10/07/11<br />
2.5 week post‐op (10/7/11)<br />
– Relevant Findings<br />
• VA: 20/25‐1 OS<br />
• Conjunctivia OS‐ trace injection of superior conj with<br />
white bled, Seidel negative even with pressure applied<br />
• GAT@2:41pm OS: 18 mmHg<br />
• Choroid attached 360 OS<br />
– Assessment/Plan<br />
• Removed Bandage Contact Lens OS<br />
• Continue Pred Forte BID, D/C Vigmaox OS, start 0.5%<br />
timolol qAM OS; continue 0.5% timolol bid OD<br />
• RTC 2 weeks<br />
1 month post‐op (10/24/11)<br />
– Relevant Findings<br />
• VA: 20/30 OD, 20/50 OS; PH not performed<br />
• Conjunctivia OS‐ trace injection of superior conj with white<br />
bleb, Seidel negative even with pressure applied<br />
• GAT@10:55pm OD: 15mmHg OS: 16 mmHg<br />
– Assessment/Plan<br />
• Post bleb revision with patch graft OS, IOP trending up<br />
though bleb is filtering, currently on 0.5% timolol qAM OS<br />
• 5‐FU subconj OS injection today<br />
• Increase Pred Forte to QID OS, continue 0.5% timolol qAM<br />
OS; continue 0.5% timolol bid OD<br />
• RTC 11/09/11 and PRN<br />
6 week post‐op (11/9/11)<br />
– Relevant Findings<br />
• VA: 20/40 OS; PH not performed<br />
• Conjunctivia OS‐ quiet with nice diffuse bleb, sutures intact,<br />
negative Seidel<br />
• GAT @10:00am OS: 14mmHg<br />
– Assessment/Plan<br />
• Post bleb revision with patch graft OS, good IOP control<br />
(with adjunctive medical therapy‐ patient is on 0.5% timolol<br />
qAM OS); s/p 5 FU on 10/24/11<br />
• 5‐FU subconj OS injection today (2 nd injection)<br />
• Continue Pred Forte to QID OS, discontinue 0.5% timolol<br />
qAM OS to encourage filtration<br />
• RTC 11/28/11 and PRN<br />
9 week post‐op (11/28/11)<br />
– Relevant Findings<br />
• VA: 20/40 OS, PH 20/30+2<br />
• Conjunctivia OS‐ quiet with nice diffuse bleb, sutures<br />
intact, Seidel negative<br />
• GAT@3:17pm OS: 16mmHg<br />
– Assessment/Plan<br />
• Post bleb revision with patch graft OS, good IOP control<br />
WITHOUT glaucoma drops; s/p 5‐FU injection x 2<br />
• 5 FU subconj OS injection today (3 rd injection)<br />
• Continue Pred Forte QID OS<br />
• RTC 3 weeks and PRN.<br />
3 month post‐op (12/19/11)<br />
– Relevant Findings<br />
• VA: 20/40 OD, 20/40 OS; PH: not performed<br />
• Refraction: +0.50 OD (20/25) ‐0.75 OS (20/25) +2.50 add<br />
OU<br />
• Conjunctivia OS‐ nicely elevated scarred bleb OS, Seidel<br />
negative<br />
• GAT@1:25pm OD: 15mmHg OS: 13mmHg<br />
– Assessment/Plan<br />
• Post bleb revision with patch graft OS, good IOP control<br />
WITHOUT glaucoma drops; s/p 5‐FU injection x 3<br />
• Taper Pred Forte TID OS<br />
• Order VA issued bifocal spectacles<br />
• RTC 4 weeks and PRN.<br />
Coursebook Page 67 of 139<br />
3
5/29/2012<br />
4 month post‐op (4/30/12)<br />
<strong>Differential</strong> Diagnoses<br />
– Relevant Findings<br />
• VA: 20/25 OD, 20/25 OS<br />
• Conjunctivia OS‐ nicely elevated scarred bleb OS, Seidel<br />
negative<br />
• GAT@12:35pm OD: 17mmHg OS: 11mmHg<br />
– Assessment/Plan<br />
• Post bleb revision with patch graft OS, good IOP<br />
control; s/p 5 FU injection x 3<br />
• Taper Pred Forte BID OS<br />
• RTC 2 months in glaucoma clinic and PRN<br />
– Blebitis<br />
– Endophthalmitis<br />
– Episcleritis<br />
– Conjunctivitis<br />
– Anterior uveitis<br />
– Ischemic bleb<br />
– Choroidal Detachment<br />
– Retinal Detachment<br />
– Melanoma of ciliary<br />
body<br />
– Melanoma of the<br />
choroid<br />
Presentation<br />
– Serious complication of trabeculectomy that<br />
requires immediate and aggressive treatment<br />
– “White on Red” appearance with white bleb and<br />
surrounding conjunctival hyperemia<br />
– Patients will typically present with mild discomfort<br />
and redness<br />
– May be associated with mild anterior chamber<br />
reaction but no vitritis is present<br />
Risk Factors<br />
• Use of antimetabolites such as mitomycin C and 5‐<br />
fluorouracil in surgery greatly increase the success rate<br />
of the surgery by inhibiting fibroblast proliferation;<br />
however, risk of infection increases because the<br />
procedure is more likely to result in a thin avascular<br />
bleb<br />
• Younger age<br />
• African American race<br />
• Inferiorly placed blebs<br />
• Chronic blepharitis<br />
TRUE EMERGENCY<br />
– Potential Complications‐ hyptonous maculopathy,<br />
choroidal detachment, endophthalmitis<br />
– An infected bleb with severe anterior chamber<br />
reaction with or without hypopyon, vitritis or a<br />
positive vitreous culture is endophthalmitis; signs<br />
and symptoms include severe pain and reduction<br />
of vision, redness and discharge<br />
• If visibility is limited perform a B‐scan ultrasound to<br />
determine the presence of vitiritis<br />
Serous Choroidal Detachment<br />
– Caused by hypotony<br />
– Swelling of the suprachoroidal space limited by<br />
firm attachment of the choroid at the vortex veins<br />
• treat the underlying cause<br />
– Choroid will spontaneously reattach as pressure<br />
increases and stabilizes<br />
– Verhoeff streaks can be present after<br />
reattachment<br />
Coursebook Page 68 of 139<br />
4
5/29/2012<br />
Bleb Revision<br />
– Increased risk of re‐infection after initial blebitis;<br />
significant risk of bleb revision failure<br />
– If leak persists after treating the infection, send for<br />
revision<br />
• Post Bleb Revision Leak<br />
– Bandage contact lens‐ restart topical antibiotics<br />
for prophylactic coverage<br />
Clinical Pearls<br />
• Blebitis is a SERIOUS complication‐ treat immediately and<br />
aggressively to prevent endophthalmitis (admission to hospital is<br />
often indicated)<br />
• Priority #1‐ Treat the Infection before addressing the hypotony: do<br />
not send for an operation until you sterilize the area, otherwise the<br />
infection could worsen<br />
– Many leaks have continuous outflow and very few bacteria can swim<br />
upstream (be more concerned if fluid is moving in and out, consider<br />
monitoring twice a day or hospitalization<br />
• Be a painter‐ Seidel testing with multiple stacked fluorescein strips<br />
• Patient education is critical‐ Instruct patients with blebs to seek<br />
help IMMEDIATELY in the event of any redness, discharge,<br />
decreased vision or photophobia<br />
References<br />
• Ordan JL, Catey B, Melville MM, et al. Risk factors for development of post trabeculectomy<br />
endophthalmitis. Br J Ophthalmol 2000:84:1349‐1353.<br />
• Muckley ED, Lehrer RA. Late‐onset blebitis and endophthalmitis:incidence and outcomes with<br />
mitomycin C. Optom VisSci. 2004;81:499–504.<br />
• Soltau JB, Rothman RF, Budenz DL, Greenfield DS, Feuer W, Liebmann JM, Ritch R. Risk factors for<br />
glaucoma filtering bleb infections. Arch Ophthalmol 2000;118:338‐42.<br />
• Kanski, J. (2006). Clinical ophthalmology: A systemic approach, Sixth edition. New York: Butterworth<br />
Heinemann Elsevier.<br />
• Bartlett, J.D., & Janus,S.D. (2008). Clinical Ocular Pharmacology. St Lousi: Butterworth Heinman<br />
Elsevier.<br />
• Kais, P. K., & Friedman, N.J. (2004). The Massachusetts eye and ear infirmary illustrated manual of<br />
ophthalmology, Second edition. Philadelphia: Saunders.<br />
• Rhee, Douglas J. The fine art of managing blebitis. Review of ophthalmology online. May 2, 2011.<br />
Coursebook Page 69 of 139<br />
5
5/29/2012<br />
Case Presentation<br />
• 83 year old Caucasian male<br />
• Presented for routine exam 9/2011<br />
• ONH asymmetry noted<br />
◦ FDT screening visual field performed<br />
ERIN J. BENDER<br />
NORTHWEST RESIDENTS CONFERENCE<br />
JUNE 4, 2012<br />
My Initial Visit<br />
• Patient asymptomatic to field loss<br />
• Systemic History:<br />
◦ Impaired fasting glucose<br />
• Ocular History:<br />
◦ Past examinations reveal:<br />
No h/o of diabetic retinopathy OU<br />
Early lens changes OU<br />
Presbyopia OU<br />
Examination Results<br />
Posterior Segment<br />
• VA sc OD 20/20-1 OS 20/25-1<br />
• EOMs full and smooth OU<br />
• CF FTFC OU<br />
• Anterior segment remarkable for 1+ NS OU<br />
• IOP OD 15 mmHg OS 15 mmHg<br />
• +APD OS<br />
◦ Pt reports 50% brightness OS compared to OD<br />
OD: Blurred disc margins with elevation,<br />
greatest N<br />
Macula flat and intact<br />
Peripheral retina: scattered hard drusen<br />
and reticular degeneration<br />
OS: Blurred disc margins with elevation,<br />
greatest N, SN and IN<br />
Macula flat and intact<br />
Peripheral retina: scattered hard drusen<br />
and reticular degeneration<br />
Coursebook Page 70 of 139<br />
1
5/29/2012<br />
Is this Papilledema<br />
Did You KNOW<br />
• Papilledema<br />
◦ Increased intracranial pressure<br />
• Pseudopapilledema<br />
◦ Congenital anomalous disc<br />
◦ Peripapillary myelinated NFL<br />
◦ Crowded disc with hypermetropia<br />
◦ OPTIC DISC DRUSEN<br />
• “Druse” is a German word<br />
• It means a crystal-lined hollow space in a rock<br />
• Was widely used in the mining industry in the 16 th<br />
century.<br />
Clinical Presentation: Optic Disc Drusen<br />
• Blurred disc margins<br />
• Scalloped disc borders<br />
• NO obscuration of surrounding vasculature<br />
• Non-hyperemic disc, no dilated capillaries<br />
• Multi-lobulated refractile bodies (if visible)<br />
• Trifurcations of the blood vessels<br />
• No elevation to surrounding NFL<br />
Incidence<br />
Demographic Presentation<br />
• ~1% of general population<br />
• Increases to ~3.4% in patients with relatives of the<br />
same diagnosis<br />
• Questionable AD inheritance pattern, described as<br />
“irregular dominant fashion”<br />
• 75 to 85% BILATERAL presentation<br />
• Equality in sex distribution<br />
• Caucasians higher incidence<br />
◦ Theory: African Americans tend to have larger scleral canal<br />
sizes as compared to Caucasians<br />
Coursebook Page 71 of 139<br />
2
5/29/2012<br />
Histology<br />
Pathophysiology<br />
• Acellular<br />
◦ Mucopolysaccharides<br />
◦ Amino acids<br />
◦ Ribonucleic and desoxyribonucleic acid<br />
◦ Calcium<br />
◦ Small amounts of iron<br />
• Range from 5 to 1000 microns in diameter<br />
• Deposits anterior to the lamina cribrosa, in 90%<br />
behind the level of Bruch’s membrane<br />
3 THEORIES OF FORMATION OF ODD<br />
Congenital Dysplasia of the optic nerve head<br />
and blood supply<br />
Axoplasmic stasis secondary to crowded disc<br />
Small scleral canal size<br />
Or an amalgamation<br />
Tso’s Theory<br />
Development and Progression<br />
Theory: ABNORMAL<br />
AXONAL METABOLISM<br />
LEADING TO<br />
INTRACELLULAR<br />
MITOCHONDRIAL<br />
CALCIFICATION<br />
Axonal rupture<br />
Mitochondrial extrusion<br />
into extracellular space<br />
Calcium continues to<br />
deposit into extracellular<br />
mitochondria<br />
(Ca2+ concentration<br />
higher than within cell)<br />
Small calcified<br />
microbodies produced<br />
Calcium continue to be<br />
deposited on the surface,<br />
forming drusen<br />
• Labeled as “buried” in young children and adults.<br />
Visibility increases with age secondary to axonal<br />
atrophy and continuing calcium deposition.<br />
• Tend to present or become “unburied” on INFERIOR<br />
NASAL portion of ONH.<br />
• 75% of ODD patients will develop some form of<br />
visual field loss.<br />
• Visual acuity tends to be well preserved.<br />
End Stage<br />
Associated Conditions<br />
• Gradual worsening and compromise to vasculature<br />
and nerve fiber layer can result in:<br />
◦ Anterior Ischemic Optic Neuropathy<br />
Related to mechanical forces<br />
Patients tend to be in mid 20s or younger<br />
Without systemic cardiovascular disease<br />
◦ Compressive CRVO/CRAO<br />
Secondary to impairment of blood flow<br />
◦ Juxtapapillary Choroidal Neovascularization<br />
Secondary to chronic ischemia<br />
• Pseudoxanthoma elasticum<br />
◦ Range from 1.4 to 3.6% association with ODD<br />
◦ Elastin lines the insertion of lamina cribrosa<br />
◦ Abnormal accumulation of polyanions with high calcium<br />
affinity acts as triggering factor for mineralization<br />
• Angioid streaks<br />
◦ Theory that a common defect of abnormal mineralization<br />
predisposes for ODD and angioid streaks<br />
• Retinitis Pigmentosa<br />
◦ Range from 0 to 10% association with ODD<br />
◦ Deposits often found ADJACENT to normal sized disc<br />
Coursebook Page 72 of 139<br />
3
5/29/2012<br />
Diagnostic Testing<br />
Our Case: Visual Field 24-2<br />
• Visual Field<br />
◦ Typically arcuate defects on VF<br />
◦ Enlarged blind spot (less common)<br />
◦ Visible drusen tend to show higher mean deviation<br />
◦ Patients tend to be unaware of visual field defect<br />
VF defects do NOT have direct correlation<br />
with location of drusen!!<br />
Diagnostic Testing<br />
Our Case: Auto fluorescent Photos<br />
• Fluorescein Angiography<br />
◦ Faint diffuse hyper fluorescence of ONH early with late well<br />
defined hyper fluoresce without leakage<br />
OD<br />
OS<br />
• Auto fluorescent Photography<br />
◦ Hyper-reflective lesions within the ONH on photo<br />
◦ Are NOT bi-refringent<br />
◦ Higher sensitivity for detecting buried drusen than<br />
ophthalmoscopy but lower than Bscan<br />
Diagnostic Testing<br />
• Optical Coherence Tomography<br />
◦ Monitor NFL loss<br />
◦ Eyes with buried disc drusen often do NOT show NFL loss<br />
◦ Reveals irregular and discontinuous elevations at ONH<br />
◦ Rounded HYPO-reflectant appearance<br />
• B-scan ultrasonography<br />
◦ STANDARD OF CARE<br />
◦ Hyper reflectance at ONH that persists at low gain settings.<br />
Coursebook Page 73 of 139<br />
4
5/29/2012<br />
OUR CASE:<br />
OCT<br />
FINDINGS<br />
OD and OS elevated<br />
NRR thickness<br />
Sup and Inf NFL<br />
loss OS<br />
Diagnostic Testing<br />
• Optical Coherence Tomography<br />
◦ Monitor NFL loss<br />
◦ Eyes with buried disc drusen often do NOT show NFL loss<br />
◦ Reveals irregular and discontinuous elevations at ONH<br />
◦ Rounded HYPO reflectant appearance<br />
• B-scan ultrasonography<br />
◦ STANDARD OF CARE<br />
◦ Hyper fluorescence at ONH that persists at low gain settings<br />
Our Case: Bscan<br />
OS Bscan at Low Gain<br />
OD at medium gain<br />
OS at medium gain<br />
Treatment<br />
Papilledema versus Pseudopapilledema<br />
• Most cases managed with serial VF testing, IOP<br />
monitoring and NFL analysis.<br />
• No definitive treatment. Not all cases are treated.<br />
• Intraocular pressure lowering agents may be used<br />
with goal of protecting the remaining NFL.<br />
◦ If due to mechanical compression, lowering IOP may alleviate<br />
the process.<br />
◦ Blood flow to ONH may be improved with use of antihypertensives,<br />
potentially reducing chance of vascular events.<br />
• Save healthcare dollars: Diagnostic testing is<br />
expensive and sometimes unnecessary.<br />
• Unduly stress for the patient: Reassurance against<br />
potential morbid outcome.<br />
Coursebook Page 74 of 139<br />
5
5/29/2012<br />
MRI<br />
To scan or not to scan<br />
$$$$$$<br />
36 YO WF referral with “asymptomatic<br />
bilateral disc edema”.<br />
Remote h/o HA and previous work-up.<br />
Past imaging revealed pineal cyst.<br />
Visual Field Results<br />
Fundus Exam<br />
Bscan Results<br />
Bumps in the Nerve<br />
OD: at high and low gains<br />
OS: at high and low gains<br />
• What is the true mechanism<br />
◦ Is scleral size really a risk factor<br />
• What are the genetics<br />
• Is IOP lowering truly beneficial<br />
• Is there an unknown modifiable risk<br />
• Research opportunities abound…<br />
Coursebook Page 75 of 139<br />
6
5/29/2012<br />
TAKE HOME POINTS<br />
References<br />
• Visual field defects common<br />
◦ Often do NOT correlate with ODD location<br />
• B – scan is standard of care<br />
◦ Consider prior to imaging studies<br />
• AF photography<br />
• OCT role TBD<br />
◦ May help in differentiating NFL defects in ODD versus<br />
glaucoma<br />
◦ Perhaps useful to monitor progression<br />
1. Grippo, T. Rogers, S. Optic Disc Drusen. Glaucoma Today. 19-24. Jan/Feb 2012.<br />
2. Antcliff, R. Spalton, D. Are Optic Disc Drusen Inherited Ophthalmology 106: 1278-1281. 1999.<br />
3. Floyd, M. Katz, B. Measurement of Scleral Canal Using Optical Coherence Tomography in patients with Optic<br />
Disc Drusen. Ophthalmology 139: 664-669. 2005.<br />
4. Miller, Newman. Pseudopapilledema associated with Optic Disc Drusen. Clinical Neuro-ophthalmology. 6 th<br />
edition, volume 1. 178-187. 2005.<br />
5. Auw-Haedrick, C. Stauback, F. Optic Disc Drusen. Survey of Ophthalmology. 47: 515-532. Nov/Dec 2002.<br />
6. Golnik, C. Congenital anomalies and acquired abnormalities of the optic nerve. Up to Date. 8/2011.<br />
7. Bienfang, D. Overview and <strong>Differential</strong> diagnosis of papilledema. Up to Date. 6/2010.<br />
8. Slotnik, S. Sherman, J. Buried Disc Drusen Have Hyporeflective Appearance on Spectral Domain Optical<br />
Coherence Tomography. Optometry and Vision Science 89:5. May 2012.<br />
9. Murthy, R. Storm, L. In-vivo high resolution imaging of optic nerve head drusen using spectral domain optical<br />
coherence tomography. BMC Medical Imaging 10:11. 2010.<br />
10. Wilkins, J. Pomeranz, H. Visual Manifestations of Visible and Buried Optic Disc Drusen. Journal of Neuroophthalmology<br />
24. Nov 2004.<br />
11. Katz, B. Pomeranz, H. Visual field Defects and Retinal Nerve Fiber Layer Defects in Eyes with Buried Optic<br />
Nerve Drusen. American Journal of Ophthalmology: 141: 248-253. 2006.<br />
12. Tatlipinar, S. Bozkurt, B. Polarimetric Nerve Fiber Analysis in Patients with Visible Optic Nerve Head Drusen.<br />
Journal of Neuro-ophthalmology: 21: 245-249. 2001.<br />
13. Ocakoglu, O. The investigation of Retinal Nerve Fiber layer thickness in eye with optic nerve head drusen.<br />
Neuro-ophthalmology: 28: 205-214. 2004.<br />
14. Kawa, P. Nowomiejska, K. Glaucoma and Drusen of the Optic Nerve Head. Neuro-ophthalmology: 33: 77-83.<br />
2009.<br />
15. Thurtell, M. Biousse, V. Optic Nerve Head Drusen in Black Patients. Journal of Neuro-ophthalmology: 0: 1-4.<br />
2011.<br />
Coursebook Page 76 of 139<br />
7
5/29/2012<br />
Exam of H.T.<br />
Allison Coit<br />
Spokane VA Resident<br />
June 2012<br />
• Chief Concern:<br />
• Dozed off Friday afternoon and woke himself up when<br />
he jammed his thumb in his right eye<br />
• After incident noticed flash of light and snowstorm of<br />
black floaters<br />
• (‐)curtain over vision<br />
• No new flashes since initial incident<br />
• Immediately after poking eye, flushed eye out with<br />
water<br />
Exam…<br />
**S/p Cataract Extraction/PCIOL OD 2 weeks ago<br />
• DVA: w/o specs<br />
• OD: 20/400‐<br />
• OS: 20/50+<br />
• Pupils: PERRL, (‐)APD<br />
• EOMS: FULL<br />
• CT: No Tropia<br />
• CF: FTFC<br />
• Anterior Segment:<br />
• Lids: Clr OU<br />
• Conj:<br />
• OD: 2+ hyperemia<br />
• OS: Clr<br />
• Cornea: Clr OU<br />
• AC:<br />
• OD: 3+ pigment/cell<br />
• OS: D/Q<br />
• Iris: Flat OU<br />
• Lens:<br />
• OD: PCIOL – clear/centered<br />
• OS: 1+ NS, Tr PSC inferior to visual Axis<br />
Posterior Segment OD<br />
• Vitreous: Dense<br />
Hemorrhage<br />
• C/D: 0.15 , distinct margins<br />
• Macula: Flat<br />
• Posterior Pole:<br />
unremarkable<br />
• A/V: 2/3<br />
• Periphery: Flat<br />
Assessment/Plan<br />
Retina Evaluation<br />
• Assessment:<br />
• Vitreous Hemorrhage OD<br />
• Possible Retinal Detachment<br />
• B‐scan not working so unable to confirm<br />
• Rebound Inflammation OD<br />
• Plan:<br />
• Refer to Retina Specialist<br />
• Rx:<br />
• Scopolamine 1gtt qpm OD and qAM tomorrow OD<br />
• Prednisolone Acetate Q2hr OD only<br />
• DVA: w/o specs<br />
• OD: 5/100<br />
• Pupils: (+)APD<br />
• EOMS: FULL<br />
• CT: No Tropia<br />
• CF: FTFC<br />
• Anterior Segment (OD )<br />
• Lids: ClR<br />
• Conj: Clr<br />
• Cornea: Clr<br />
• AC: 2‐3+ cell<br />
• Iris: Flat<br />
• Lens: PCIOL – clear/centered<br />
• Gonio:<br />
• Small hypopyon<br />
Coursebook Page 77 of 139<br />
1
5/29/2012<br />
Retina Evaluation…<br />
• Posterior Segment ‐<br />
OD only<br />
• Vitreous Hemorrhage<br />
• Vitreous: 3+ vitritis, 3‐4+<br />
vitreous haze, clumps of<br />
vitreous cells and a “string<br />
of pearls”<br />
• Retina: break at 11 o’clock<br />
No Case of No Cataract<br />
Surgeries Years Rate per 1000 Surgeries<br />
Author Country Data Source Endophthalmitis<br />
West et al United States Medicare, US 1026 447,627 1994‐2001 2.15<br />
Taban et al United Kingdom Meta‐analysis >3,000,000 1963‐2003 1.28<br />
Kamalaraajah et al United Kingdom<br />
Estimations from<br />
databases &<br />
questionnaires ~230,000 1999‐2000 1.4<br />
Admin and clinical<br />
Li et al<br />
Australia<br />
databases 210 117,083 1980‐2000 1.79<br />
Admin and clinical<br />
databases 102 57,123 1995‐2000 1.79<br />
Ng et al<br />
Australia<br />
National cataract<br />
registry 112 118,151 1999‐2001 0.6<br />
Wejde et al<br />
Sweden<br />
National cataract<br />
registry 109 225,471 2002‐2004 0.48<br />
Lundstrom et al Sweden<br />
Krummenauer et al Germany Questionnaire 291 404,356 2000 0.72<br />
Moshirfar et al United States 14 20,013 2003‐2005 0.7<br />
Bascom Palmer 1984‐1989 0.7<br />
Bascom Palmer 1990‐1994 0.9<br />
Bascom Palmer 1995‐1999 0.6<br />
Miller et al<br />
Clear Corneal<br />
Incision 6 15, 920 2000‐2004 0.5<br />
other methods 1 0.2<br />
Risk Factors<br />
• Pre‐Operative<br />
• Blepharitis/Conjunctivitis<br />
• Lacrimal Duct Obstruction<br />
• Contact Lens Wear<br />
• Ocular prosthesis in fellow<br />
orbit<br />
• Male>Female<br />
• >85 years old (2 nd risk group<br />
was 20‐64 years)<br />
• Diabetes<br />
• Immunosuppression<br />
• Upper Respiratory Infection<br />
• Intraoperative<br />
• Capsular Rupture<br />
• Secondary IOL<br />
• Inadequate eyelid/conjunctival<br />
disinfection<br />
• Prolonged surgery (>60min)<br />
• Vitreous loss<br />
• Prolene haptic IOLs<br />
• Postoperative<br />
• Wound leak/dehiscence<br />
• Inadequate buried sutures<br />
• Suture removal<br />
• Presence of filtering bleb<br />
Decreased Vision<br />
(+)APD<br />
Loss of red reflex<br />
Corneal Infiltrate<br />
Wound abnormality<br />
Hypopyon<br />
Pain<br />
Corneal Edema<br />
Fibrinoid AC response<br />
Vitreous Inflam<br />
Retinitis<br />
Keratic precipitates<br />
• External Signs<br />
• Ciliary injection<br />
• Chemosis<br />
• Eyelid edema<br />
• Orbital Infection<br />
• Restriction of EOMs<br />
• Proptosis<br />
Delayed Clinical Signs/Symptoms<br />
• Capsular plaques (89%)<br />
• White plaque on posterior capsules<br />
• Fungal or bacterial<br />
• Keratic precipitates (81%)<br />
• Hypopyon (31%)<br />
• Small, do gonio<br />
• Low grade uveitis (may initially respond to steroids)<br />
• Granulomatous<br />
• Vitritis<br />
• Beaded fibrin strand in aqueous<br />
• White “string of pearls” infiltrate in vitreous or aqueous<br />
• fungal<br />
• No pain initially (27%)<br />
Coursebook Page 78 of 139<br />
2
5/29/2012<br />
• Immediate (withinin 2 days of surgery)<br />
Could be any organism!<br />
• Pseudomonas** Streptococcus**<br />
• Early (214 days after surgery)<br />
Could be any organism!<br />
Top Suspects:<br />
•Staphylococcus (coagulase negative) &<br />
•Staphylococcus aureus<br />
**most virulent<br />
<strong>Differential</strong> <strong>Diagnosis</strong><br />
• Delayed (>14 days after surgery)<br />
• Most common:<br />
• Staphylococcus<br />
• Propionibacterium acnes<br />
• Fungi<br />
• Ex: Candida, Aspergillus<br />
• Immediate<br />
• Toxic Anterior Segment Syndrome<br />
• Clinical Findings:<br />
• Fibrin formation<br />
• Corneal Edema<br />
• Anterior Chamber inflammation<br />
• Mid‐dilated and irregular pupil<br />
• Low IOP<br />
• Vs Endophthalmitis<br />
• Usually less prominent redness<br />
• Less pain<br />
• Less severe anterior chamber reaction<br />
• Little or no vitreous inflammation<br />
<strong>Differential</strong> <strong>Diagnosis</strong><br />
• Early (2 14 days)<br />
• Retained Lens Material<br />
• Increased inflammation with time<br />
• Amount of retained lens + amount of time in eye<br />
• Perform gonio<br />
<strong>Differential</strong> <strong>Diagnosis</strong><br />
• Early<br />
• Proliferative Diabetic Retinopathy<br />
• PDR greater disturbance of blood aqueous barrier<br />
• History of Uveitis<br />
• Greatest risk of excessive post‐op inflam and complications<br />
when uveitis not under control<br />
• Most specialists require 6 months of inflamm control<br />
• Increased risk: HLA‐B27 uveities, sarcoidosis, granulomatous<br />
uveitis, children<br />
Coursebook Page 79 of 139<br />
3
5/29/2012<br />
Treatment<br />
• Intravitreal<br />
• Ceftazidime (gram ‐, including P. aeruginosa and H. influenzae)<br />
• 2.25mg in 0.1ml<br />
• Vancomycin (gram +, including MRSA)<br />
• 1.0mg in 0.1mL<br />
• Subconjunctival<br />
• Vancomycin<br />
• 25mg in 0.5mL<br />
• Ceftazidime<br />
• 100mg in 0.5mL<br />
• Steroids<br />
Topical<br />
Vancomycin<br />
50mg in 1.0mL<br />
Ceftazidime<br />
100mg in 1.0mL<br />
• Oral prednisolone 1mg/kg po Qam x 3‐5 days<br />
• Intravitreal dexamethasone<br />
• Topical Pred Acetate 1% q1‐2 hours<br />
Vitrectomy<br />
Goal:<br />
Removing the infecting organisms and toxins<br />
Removing vitreous membranes<br />
Which could lead to retinal detachments<br />
Improve distribution of antibiotics<br />
Cons:<br />
Increase drug toxicity<br />
Endophthalmitis Vitrectomy<br />
Treatment Study (EVS)<br />
• 420 patients<br />
• Endophthalmitis within 6 weeks of cataract surgery<br />
or secondary IOL<br />
• Results<br />
• Systemic antibiotics made no difference in final visual<br />
acuity<br />
• VA of Hand Motion or better<br />
• Vitrectomy made no difference in outcome<br />
• VA of Light Perception only<br />
• Improved outcome with immediate vitrectomy<br />
Prophylaxis<br />
• 5% Povidone Iodine<br />
• Significantly decreases the risk<br />
• Effective against bacteria, fungi, virus, protozoa, and<br />
spores<br />
• Surgeons place 1gtt of Betadine in eye at surgery<br />
• Pre‐op Antibiotics<br />
• Limit pre‐op drops to 1‐3 days to decrease risk of antibiotic<br />
resistance<br />
• Post‐op Subconj Antibiotics<br />
• Inconclusive<br />
• Not always effective because of sub‐therapeutic<br />
intraocular concentration<br />
Special Thanks to:<br />
Thomas Riley, OD, FAAO<br />
References<br />
1. Doshi, Rishi R., J. Fernando Arevalo, Harry W. Flynn, and Emmett T. Cunningham, Jr. "Evaluating<br />
Exaggerated, Prolonged, or Delayed Postoperative Intraocular Inflammation." American Journal of<br />
Ophthalmology 150 (2010): 295‐304. Print.<br />
2. Endophthalmitis Vitrectomy Treatment Group, comp. "Results of the Endophthalmitis Vitrectomy Study."<br />
Arch Ophthalmology 113 (1995): 1479‐496. Print.<br />
3. Hatch, Wendy V., Geta Cernat, David Wong, Robert Devenyi, and Chaim M. Bell. "Risk Factors for Acute<br />
Endophthalmitis after Cataract Surgery: A Population‐based Study." Ophthalmology 116.3 (2009): 425‐30.<br />
Print.<br />
4. Kresloff, Michael S., Alessandro A. Castellarin, and Marco A. Zarbin. "Endophthalmitis." Survey of<br />
Ophthalmitis 43.3 (1998): 193‐224. Print.<br />
5. Lalwani, Geeta A., Harry W. Flynn Jr, Ingrid U. Scott, Carolyn M. Quinn, Audina M. Berrocal, Janet L. Davis,<br />
Timothy G. Murray, William E. Smiddy, and Darlene Miller. "Acute‐Onset Endophthalmitis after Clear<br />
Corneal Cataract Surgery (1996–2005)Clinical Features, Causative Organisms, and Visual Acuity<br />
Outcomes." Ophthalmology 115.3 (2008): 473‐76. Print.<br />
6. Moshirfar, M., V. Feiz, A. Vitale, J. Wegelin, S. Basavanthappa, and D. Wolsey. "Endophthalmitis after<br />
Uncomplicated Cataract Surgery with the Use of Fourth‐Generation FluoroquinolonesA Retrospective<br />
Observational Case Series." Ophthalmology 114.4 (2007): 686‐91. Print.<br />
7. Scott, I., H. Flynnjr, W. Smiddy, J. Newton, and D. Miller. "Acute‐onset Endophthalmitis After Cataract<br />
Surgery (2000–2004): Incidence, Clinical Settings, and Visual Acuity Outcomes After Treatment." American<br />
Journal of Ophthalmology 139.6 (2005): 983‐87. Print.<br />
Coursebook Page 80 of 139<br />
4
5/29/2012<br />
Case History<br />
VALSALVA RETINOPATHY<br />
Kendra Kallemeyn, OD<br />
Roseburg, OR VAMC<br />
65yowm presents with CC of “black spot blocking<br />
the vision in right eye. “<br />
Onset – sudden, 5 days ago<br />
Activity during time of onset – was helping daughter<br />
move an entertainment center the night before and<br />
when he woke up in the middle of the night he could not<br />
see out of his right eye<br />
Change in vision does not appear to be worsening or<br />
improving since time of onset.<br />
No symptoms like this have been noted previously in<br />
either eye.<br />
Ocular History<br />
(-) prior ocular disease, injury or surgery<br />
LEE 4-5yrs ago at commercial practice<br />
Patient’s wife reports he was told to get his blood<br />
pressure checked, because “something is wrong with the<br />
blood vessels in the eye(s).”<br />
No follow-up appointment with PCP was made<br />
Medical History<br />
No prior healthcare with any VA system prior to<br />
today<br />
Medications<br />
Unknown blood pressure medication<br />
started by outside provider in ~2009<br />
patient reports medication is NOT controlling BP<br />
NKDA<br />
Baseline Exam 11/1/11<br />
Visual Acuities cc<br />
OD: CF w/EF PHNI<br />
OS: 20/40 PHNI<br />
Pupils: equal, round, reactive to light, (+)APD OD<br />
EOMs: full and smooth OU<br />
Confrontation Fields: full to finger counting OU<br />
Anterior Seg: unremarkable OU<br />
Tonometry by GAT: 16/16 @ 1:21pm<br />
BP recorded as 174/99 at check-in to ER<br />
Coursebook Page 81 of 139<br />
1
5/29/2012<br />
Baseline Exam Continued…<br />
OD<br />
Posterior Segment<br />
Lens: trace nuclear sclerosis OU<br />
Vitreous: clear OU<br />
C/D Ratio : 0.65/0.65 OD, 0.5/0.5 OS<br />
Vessels: arterial attenuation OU, A/V crossing changes OS<br />
Macula<br />
• OD: 5DDx5DD subretinal and intraretinal hemorrhage<br />
w/preretinal heme inferior<br />
• OS: flat, mild RPE changes, (-)heme/MA<br />
Periphery: intact 360 OU<br />
SUBRETINAL<br />
--green/gray<br />
INTRARETINAL<br />
--dark red<br />
PRERETINAL<br />
(Subhyaloid or sub-ILM)<br />
--boat shape or<br />
horizontal blood line<br />
OS<br />
Assessment/Plan<br />
--arterial attenuation with<br />
no retinal hemorrhages<br />
Assessment<br />
Subretinal hemorrhage OD<br />
Plan<br />
Refer for retinal consult; Portland VA Ophthalmology<br />
<strong>Differential</strong> <strong>Diagnosis</strong><br />
<br />
<br />
Primary <strong>Diagnosis</strong><br />
Valsalva retinopathy<br />
Secondary <strong>Diagnosis</strong><br />
Retinal Artery Macroaneurysm<br />
Terson’s Syndrome<br />
Trauma – Choroidal Rupture<br />
High Altitude Retinopathy<br />
Neovascular Macular Degeneration – CNV<br />
Retinopathy in Blood Disorders<br />
Purtscher Retinopathy<br />
Hypertensive retinopathy<br />
Diabetic retinopathy<br />
Choroidal Melanoma<br />
http://www.sightnation.com/eye-disorders/otherpage=3<br />
http://www.nature.com/eye/journal/v20/n9/fig_tab/6702068f6.html#figure-title<br />
Retinal Artery Macroaneurysm (hemorrhage)<br />
• Aneurysmal dilation of arteriole, most commonly at bifurcation or A/V crossing, along temporal arcades<br />
and is associated with multilayer retinal hemorrhage in 50% of cases.<br />
• Hard exudates may also be present due to chronic leakage<br />
• Most commonly seen with unilateral presentation in hypertensive, elderly women.<br />
•Preretinal and vitreous hemorrhage may block underlying lesion and/or make FA difficult which can<br />
result in misdiagnosis.<br />
Coursebook Page 82 of 139<br />
2
5/29/2012<br />
http://savesightcentre.com/diagnostic-testing.html<br />
http://www.sarawakeyecare.com/Atlasofophthalmology/posteriorsegment/posteriorsegmentpictur5tersonsyndrome.htm<br />
http://www.revoptom.com<br />
Terson’s Syndrome<br />
• Intraocular hemorrhage (typically bilateral) associated with acute intracranial hemorrhage<br />
• Most common cause – subarachnoid bleeding from aneurysm of the anterior communicating artery<br />
• Mechanism -- increased intracranial pressure at the time of an acute intracranial bleed may lead to<br />
acute obstruction of the retinal venous circulation which results in rupture of superficial retinal vessels<br />
• Patient typically presents to ER Physician with significant systemic signs/symptoms after suffering a<br />
spontaneous or trauma-induced subarachnoid hemorrhage<br />
Trauma: Choroidal Rupture<br />
• Involves the choroid, Bruch’s membrane, and RPE<br />
• Overlying subretinal hemorrhage may obscure view of fresh rupture<br />
• rupture will appear as a white, crescent shaped, vertical streak of exposed sclera<br />
http://www.nejm.org/doi/pdf/10.1056/NEJMicm0909506<br />
http://www.eyedefectsresearch.org/mac-degen.html<br />
http://www.ncbi.nlm.nih.gov.proxy.lib.pacificu.edu:2048/pmc/a<br />
rticles/PMC3040733/pdf/pone.0011532.pdftool=pmcentrez<br />
http://www.rustoneyeinstitute.com/index.cfm/PageID/3788<br />
High Altitude Retinopathy<br />
• Acquired retinopathy which typically occurs at elevations above 16,000ft<br />
• Delayed onset of retinal hemorrhages on descent from high altitudes is common<br />
• Triad of dilated retinal veins, retinal hemorrhages and optic disc edema<br />
• Part of a spectrum of conditions associated with high altitude/hypoxic conditions<br />
• Acute Mountain Sickness, High Altitude Cerebral Edema, High Altitude Pulmonary Edema<br />
Neovascular (Wet) Macular Degeneration: CNV<br />
• Non-exudative (dry) Macular Degeneration<br />
• drusen, RPE pigment changes, geographic atrophy<br />
• Exudative (wet) Macular Degeneration<br />
• Choroidal neovascularization (CNV)<br />
http://www.djo.harvard.edu<br />
www.redatlas.org<br />
http://www.retinamaculainstitute.com/ocular-education/ocular-trauma<br />
http://webeye.ophth.uiowa.edu<br />
http://legacy.revoptom.com/handbook/sect7e.htm<br />
Retinopathy in Blood Disorders<br />
• Sickle Cell Retinopathy, Anemia, Leukemia, etc<br />
• salmon patch intraretinal hemorrhages, black sunbursts (RPE hyperplasia), seafan<br />
neovascularization, vitreal hemorrhage, CWS, Roth spots<br />
Purtscher Retinopathy<br />
• Associated with head trauma, compressive chest injuries, long bone fracture, acute<br />
pancreatitis, retrobulbar anesthesia, or systemic disorders (ie. Lupus)<br />
• Typically presents bilaterally with presence of CWS, peri-papillary retinal<br />
whitening, dilated retinal venous system, and retinal hemorrhages<br />
Coursebook Page 83 of 139<br />
3
5/29/2012<br />
http://www.mrcophth.com/retinalvasculardisorders/proliferativediabetic.html<br />
http://www.nature.com/nrrheum/journal/v2/n8/fig_tab/ncprheum0268_F6.html<br />
Hypertensive Retinopathy<br />
• Arterial attenuation, vascular leakage leading to retinal edema and deposition<br />
of hard exudates, macular star, CWS, subretinal hemorrhages, ONH swelling<br />
http://www.rustoneyeinstitute.com/index.cfm/PageID/3796<br />
Diabetic Retinopathy<br />
• NPDR: multiple MA and dot/blot hemes, CWS, HE, IRMA, NVD, NVI, NVE<br />
• progressive: mildmoderatesevere<br />
• PDR<br />
http://www.jhu.edu/wctb/coms/general/about-mm/coms1a.htm<br />
http://www.sightnation.com/casephotos/choroidal-melanoma<br />
Initial Presentation<br />
2 weeks<br />
2 months<br />
Choroidal Melanoma<br />
http://www.kellogg.umich.edu/theeyeshaveit/non-trauma/choroidal-melanoma.html<br />
• Present with varying amounts of pigmentation or amelanotic<br />
• If the tumor breaks through Bruch’s membrane, intrinsic blood vessels and<br />
hemorrhages may also be visible<br />
Valsalva Retinopathy<br />
http://webeye.ophth.uiowa.edu/eyeforum/cases/67-Valsalva-Retinopathy-Vision-Loss-Asthma.htm<br />
• Classically presents as a sudden loss of central vision in a healthy individual that is<br />
caused by premacular hemorrhage secondary to Valsalva stress.<br />
• Valsalva maneuver (stress) is defined as “increasing intrathoracic or intraabdominal<br />
pressure against a closed glottis which slows venous return to the heart, decreases stroke<br />
volume and subsequently increases venous system pressure”<br />
Valsalva maneuver: pathophysiology<br />
Causes of Valsalva Stress<br />
2. Diminished<br />
cardiac filling<br />
lowers the arterial<br />
pressure, slows the<br />
pulse and leads to<br />
reflex tachycardia<br />
and peripheral<br />
vasoconstriction.<br />
3. Release of the<br />
strain causes<br />
sudden reduction<br />
of intrathoracic<br />
pressure, further<br />
lowering the<br />
blood pressure<br />
and increasing<br />
the cardiac<br />
pressure.<br />
4. Abrupt<br />
increase in blood<br />
pressure occurs as<br />
blood surges<br />
back to the heart<br />
which induces<br />
reflex<br />
tachycardia.<br />
1. Sudden<br />
increase in<br />
intrathoracic<br />
pressure<br />
decreases venous<br />
return to the heart.<br />
Valsalva<br />
Retinopathy<br />
5. As the sudden rise<br />
in intraocular venous<br />
pressure occurs,<br />
retinal capillaries<br />
spontaneously rupture<br />
which can lean to…<br />
Coursebook Page 84 of 139<br />
4
5/29/2012<br />
Valsalva retinopathy: Benefits of OCT<br />
Treatment vs Observation<br />
Valsalva retinopathy has a tendency to appear at<br />
the macula.<br />
Visual prognosis and treatment options depend on<br />
the size and anatomical level of the hemorrhage.<br />
Use of the SD-OCT can localize the hemorrhage as<br />
sub-ILM and/or subhyaloid.<br />
Researchers continue to<br />
dispute if the plane of the<br />
hemorrhage is truly sub-ILM,<br />
subhyaloid, or if the ILM and<br />
hyaloid membrane are in fact fused.<br />
Why Consider Treatment<br />
<br />
<br />
<br />
Patient may have profound vision<br />
loss for up to 6mo if left untreated.<br />
Longstanding macular hemorrhages<br />
(even 10DD in area with bullous<br />
intraretinal hemorrhage overlying<br />
• OS: flat<br />
Periphery: attached 360 OU<br />
Macular OCT<br />
OD: large subretinal elevation with large intraretinal cyst<br />
OS: flat<br />
Coursebook Page 85 of 139<br />
5
5/29/2012<br />
Assessment/Plan:<br />
Assessment<br />
Subretinal hemorrhage OD – large, >10DD in area,<br />
prominently elevated<br />
• Given history of patient moving entertainment unit by himself this<br />
likely represents Valsalva retinopathy<br />
Plan<br />
Request patient be sent to Casey Eye Institute for FA and<br />
photos to evaluate for alternative underlying etiology.<br />
Counseled patient only course of action is observation.<br />
Monocular precautions.<br />
RTC 4mo for f/u.<br />
Follow-Up<br />
Attempt #1 (1/23/12)<br />
2mo f/u at Roseburg VAMC – cancelled by patient<br />
Attempt #2 (3/27/12)<br />
4mo f/u at Roseburg VAMC – wife reports they will not be<br />
able to make it to any f/u appointments<br />
*Note: Review of patient chart shows high no-show and<br />
cancel rate for lab work and PCP appointments as well.<br />
Chart notes or test results from Casey Eye Institute were not<br />
available.<br />
Valsalva Retinopathy vs Retinal Artery Macroaneurysm (RAM)<br />
http://savesightcentre.com/diagnostic-testing.html<br />
<br />
Dx: Valsalva Retinopathy<br />
based on case history<br />
OCT would typically show sub-ILM<br />
hemorrhage<br />
<br />
Dx: RAM<br />
hemorrhage present at multiple layers<br />
OCT shows subretinal and intraretinal<br />
elevation<br />
patient is >60yrs old and has h/o<br />
uncontrolled hypertension<br />
RAM “idiopathic, acquired dilation of<br />
a major retinal arteriole typically<br />
occurring at the first three bifurcations<br />
or an area of A/V crossing”<br />
Conclusions and Clinical Pearls<br />
References<br />
<br />
<br />
<br />
<strong>Diagnosis</strong> of Valsalva retinopathy or hemorrhage as a<br />
complication of RAM would not change the plan or outcome in this<br />
patient.<br />
Multi-layer retinal hemorrhages would not benefit from Nd:YAG<br />
membranotomy. Direct or indirect laser treatment for macroaneurysm is<br />
controversial.<br />
Remember to consider your patient’s occupation or recreational<br />
demands. Is binocular vision needed as a work requirement How<br />
is the vision in the other eye<br />
As always, patients need to be presented with all treatment<br />
options and educated on expected timelines for possible visual<br />
recovery.<br />
Al-Mujaini AS, Montana CC. Valsalva retinopathy in pregnancy: a case report. Journal of Medical Case Reports.<br />
2008. 2:101.<br />
De Maeyer K, et al. Sub-inner limiting membrane haemorrhage: causes and treatment with vitrectomy. British Journal<br />
of Ophthalmology. 2007. 91:869-872.<br />
Duane TD. Valsalva hemorrhagic retinopathy. Trans Am Ophthalmol Soc. 1972. 70: 298-313.<br />
Kaiser, Friedman. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 2 nd edition. 2004.<br />
Kanski J. Clinical Ophthalmology, A Systemic Approach. 6 th edition, 2007.<br />
Khan M.T., et al. Nd:YAG laser treatment for Valsalva premacular hemorrhages: 6 month follow up. Alternative<br />
management options for preretinal premacular hemorrhages in Valsalva retinopathy. International Ophthalmology.<br />
2008. 28:325-327.<br />
Kwok AK, Lai TY, Chan NR. Epiretinal membrane formation with internal limiting membrane wrinkling after Nd:YAG<br />
lasaer membranotomy in Valsalva retinopathy. American Journal of Ophthalmology. Oct 2003. 136(4):763-766.<br />
Mumcuoglu T, Durukan A, et al. Outcomes of Nd:YAG Laser Treatment for Valsalva Retinopathy Due to Intense<br />
Military Exercise. Ophthalmology Surgery, Lasers and Imaging. Jan/Feb 2009. Vol 40:19-24.<br />
Sabella P, Bottoni, F, Staurenghi, G. Spectral-domain OCT evaluation of Nd:YAG laser treatment for Valsalva<br />
retinopathy. Graefe’s Arch Clinical and Experimental Ophthalmology. 2010. 248:599-601.<br />
Shukla D, Naresh K, Kim R. Optical coherence tomography findings in Valsalva retinopathy. American Journal of<br />
Ophthalmology. July 2005. 140:134-136.<br />
Tatlipinar S, et al. Optical coherence tomography features of sub-internal limiting membrane hemorrhage and<br />
preretinal membrane in Valsalva retinopathy. Canadian Journal of Ophthalmology. 2007. 42:129-130.<br />
Coursebook Page 86 of 139<br />
6
5/29/2012<br />
Thank you!<br />
Roseburg VA Eye Care Team<br />
• Dr. Bryan Deck, OD<br />
• Dr. Dirk Dittemore, OD<br />
• Dr. Duva Appleman, MD<br />
Coursebook Page 87 of 139<br />
7
Objectives<br />
Perioperative Vision Loss from<br />
Non‐Ophthalmic Surgery<br />
Brett Richardson, O.D.<br />
Spokane VAMC<br />
509.434.7032<br />
• My goal for this presentation is for you to<br />
understand that<br />
– Non‐ophthalmic surgeries can result in<br />
Perioperative Vision Loss (POVL)<br />
– Altered vascular supply is the primary cause<br />
Objectives<br />
• I will be discussing<br />
– Common surgeries that result in Perioperative<br />
vision loss (POVL)<br />
• Cardiac<br />
• Spine<br />
– Most common types of POVL<br />
• Ischemic Optic Neuropathy<br />
• Retinal Vascular Occlusion<br />
• Cortical Blindness<br />
Case<br />
• 65 y.o. WM<br />
• POHx<br />
– Mild Hypertensive Retinopathy OU<br />
– RPE mottling OU<br />
• PMHx<br />
– Malignant Hypertension (as high as 267/158)<br />
– Hypercholesterolemia<br />
– Coronary Artery Disease<br />
– Myocardial Infarction with Angioplasty and stent 2007<br />
– Renal failure<br />
– Angioplasty and stent 2011 (2 weeks ago)<br />
Case<br />
• CC: “During angioplasty and stent surgery 2<br />
weeks ago, my blood pressure shot way up<br />
and my vision has been blurry and distorted<br />
ever since.”<br />
Case<br />
• VA<br />
– od: 20/80 ‐>> ph70, very slow<br />
– os: 20/150 ‐>> phni, very slow<br />
• BCVA<br />
– od: 20/40<br />
– os: 20/100<br />
• PERRLA (‐) APD<br />
• Tonometry<br />
– od: 13<br />
– os: 14<br />
Coursebook Page 88 of 139
Case<br />
• Ant Seg: Unremarkable<br />
• Fundus<br />
– Nerve ou: 0.4rd, (‐) pallor<br />
– Macula: Mild Mottling OS>OD<br />
– Vasculature ou: 2/3, mild nicking<br />
– Posterior Pole: unremarkable ou<br />
– Periphery: flat ou<br />
Case<br />
• Additional Testing<br />
– OCT: macular<br />
• od: 176microns centrally, normal contour<br />
• os: 176microns centrally, normal contour<br />
– BP: 120/72<br />
– Visual Field<br />
Case ‐ Visual Fields #1<br />
Case ‐ CT Scan<br />
• Unremarkable<br />
Homonymous Macular Quadronopsia<br />
Case – Follow Up<br />
Case –Visual Fields #2<br />
• 4 Months later<br />
– VA<br />
• od: 20/60+ phni<br />
• os: 20/100 phni<br />
– Fundus: No significant changes<br />
• (‐) Optic Nerve Pallor<br />
– Visual Field<br />
Generalized Depression OU!!<br />
Coursebook Page 89 of 139
Case – Follow Up<br />
Case –Visual Fields #3<br />
• 8 months later<br />
– VA<br />
• od:20/30<br />
• os:20/100<br />
– Fundus: No Significant changes<br />
– Optic Nerve: (‐) pallor ou<br />
– Visual Field:<br />
Imaging<br />
Fundus Photos<br />
• MRI<br />
– Chronic small right occipital infarct<br />
– Chronic small vessel ischemic changes and chronic<br />
lacunar infarcts<br />
• MRA<br />
– Unremarkable<br />
<strong>Diagnosis</strong><br />
• Angioplasty with stent surgery causing<br />
occipital lobe infarction resulting in<br />
homonymous macular quadranopsia leading<br />
to cortical blindness secondary to cerebral<br />
ischemia<br />
• CARDIAC SURGERY CORTICAL BLINDNESS<br />
Study<br />
• 10 Year study from 1996‐2005 by Nationwide<br />
Inpatient Sample (NIS).<br />
• 74 million patients<br />
– 5.7 million relevant surgical patients<br />
• 8 most common surgeries in U.S.<br />
• Monitoring for Perioperative visual loss<br />
– Ischemic Optic Neuropathy (ION)<br />
– Retinal Vascular Occlusion (RVO)<br />
– Cortical Blindness (CB)<br />
Coursebook Page 90 of 139
Study<br />
• Incidence of POVL<br />
– Cardiac Surgery: 8.64/10,000<br />
– Spine Surgery: 3.09/10,000<br />
– Appendectomy: 0.12/10,000<br />
– Total: 2.35/10,000 (all 8 surgery types)<br />
• POVL in Cardiac Surgery<br />
– RVO 77%<br />
– ION 16%<br />
– CB 8%<br />
• POVL in Spine Surgery<br />
– CB 49%<br />
– ION 28%<br />
– RVO 23%<br />
Study<br />
• Findings<br />
– Highest rate of POVL is found in cardiac and spine<br />
surgeries<br />
– Prevalence: Males vs. Females 2:1<br />
– ION highest in patients 50‐64 y/o<br />
– RVO highest in patients > 65 y/o<br />
– CB highest in patients < 18 y/o<br />
– Highest prevalence in patients < 18 y/o (4.37/10,000)<br />
– POVL remains unpredictable and is not related to any<br />
particular hospital or degree of surgical experience<br />
Literature Review Reveals:<br />
• Ischemic Optic Neuropathy<br />
– 3 Forms<br />
• Perioperative, Arteritic, Non‐arteritic,<br />
– Hypotension ION<br />
– Anemia ION<br />
• > 1L (average 5L)<br />
– Hypothermia ION<br />
• blood viscosity<br />
• 1 o Cdecrease = 6‐7% decrease in cerebral blood flow<br />
– Ocular Hypertension (prone position)<br />
– Surgical Time (> 6 hours)<br />
Literature Review Reveals:<br />
• Central Retinal Artery Occlusion (CRAO)<br />
– Spine Surgeries (933 cases)<br />
• Declined Prone position venous stasis in capillary<br />
beds<br />
– 70% secondary to ocular trauma<br />
• Ocular compression from head rest can raise IOP to<br />
sufficient level to cause ischemia<br />
Literature Review Reveals:<br />
• Cortical Blindness<br />
– Destruction or denervation of 1 o Visual Cortex<br />
(Occipital Lobe) or Optic Radiations<br />
– Highest incidence in cardiac surgery (CABG)<br />
– Results from embolism, stroke<br />
– Risk Factors<br />
• HTN, DM, Renal insufficiency, Smoking, PVD, COPD<br />
Summary<br />
• Perioperative Vision Loss Likely to occur:<br />
– Cardiac Surgery > Spine Surgery > all others<br />
– ION > CRAO > Cortical Blindness<br />
– High Risk patients<br />
• DM, Smoking, HTN, Vascular disease<br />
– High Risk Intraoperative Complications<br />
• Blood loss > 5L<br />
• Hypotension < 90 mmHg<br />
• Long Operating Times (> 6 hours)<br />
Coursebook Page 91 of 139
Coursebook Page 92 of 139
5/31/2012<br />
Diabetic Teleretinal Imaging<br />
Program:<br />
An Assessment of the Diabetic Teleretinal Imaging Program (TRIP) at<br />
the Portland Veterans Affairs Medical Center (PVAMC) - A Retrospective Study<br />
Diabetes Statistics<br />
• 24 million people in the US have DM<br />
• 78% have retinopathy if DM >15yrs<br />
Keely L. Hoban, O.D.<br />
Grace L. Tsan, O.D.<br />
Portland VA Medical Center<br />
June 4, 2012<br />
• 28.5 % of people with diabetes ages >40 years<br />
have diabetic retinopathy<br />
Burden of Diabetic Eye Disease<br />
• #1 cause of blindness in working‐aged adults<br />
in the US<br />
What does this mean for<br />
optometry<br />
Health<br />
Care<br />
System<br />
Burden<br />
Eye Care<br />
Providers<br />
Patients<br />
PVAMC Research Team<br />
• Weon Jun, O.D., FAAO<br />
• Keely L. Hoban, O.D.<br />
• Steve Mansberger, M.D., MPH<br />
• Amy L. Pedersen, O.D.<br />
• Kevin J. Riedel, O.D.<br />
• Grace L. Tsan, O.D.<br />
Objectives<br />
• Advantages and disadvantages of Diabetic Teleretinal Imaging<br />
Program (TRIP).<br />
• Types of clinical settings that may benefit from TRIP.<br />
• Effectiveness of TRIP at the PVAMC.<br />
• Identify program improvements for TRIP at the PVAMC<br />
Coursebook Page 93 of 139<br />
1
5/31/2012<br />
What is Telemedicine<br />
Store‐and‐Forward Telehealth<br />
http://www.telehealth.va.gov/<br />
Annual vs. Biennially<br />
DFE<br />
TRIPDFE<br />
Teledermatology Teleretinal Imaging Teleradiology<br />
How does TRIP work<br />
Four Non‐Mydriatic Images<br />
Cavallerano AA, Conlin PR. Teleimaging to screen for diabetic retinopathy in the Veterans Health Administration. J Diabetes Sci Technol 2(1): 33-9, 2008.<br />
Referral Guidelines for<br />
Diabetic Eye Exam<br />
Who may benefit from TRIP<br />
• Target Patients:<br />
– DM patients with low risk for retinopathy<br />
• i.e. Newly diagnosed DM patients, patients w/ well controlled A1c<br />
– DM patients with diabetic retinopathy that have been lost to follow‐up<br />
• Other Uses:<br />
– Identify co‐morbid eye conditions<br />
• Providers:<br />
– Hospitals<br />
– Academic Institutions<br />
– Group Practice Settings<br />
Cavallerano AA, Conlin PR. Teleimaging to screen for diabetic retinopathy in the Veterans Health Administration. J Diabetes Sci Technol 2(1): 33-9, 2008.<br />
Coursebook Page 94 of 139<br />
2
5/31/2012<br />
Goals for TRIP<br />
CASE #1<br />
• Increase compliance with diabetic eye exams<br />
• Improve patient education on importance of diabetic<br />
eye exam<br />
• Early intervention to treat and manage diabetic<br />
retinopathy<br />
Retrospective Chart Review<br />
• Inclusion Criteria:<br />
– Reviewed CPRS medical records of 200 patients from 1757<br />
diagnosed diabetic patients<br />
– Teleretinal imaging performed between<br />
January 1, 2010 and January 1, 2011<br />
• Exclusion Criteria<br />
PVAMC TRIP Locations<br />
Data<br />
Vancouver<br />
• Quality image:<br />
90% adequate<br />
• Male: 97%<br />
• Average age: 64.7 yrs (std dev 10.2)<br />
• Race:<br />
91% Caucasian<br />
• Avg Height/Weight: 70 inches/230 lbs<br />
• Avg BMI: 33.8 kg/m 2 (obesity >30)<br />
• Avg lab glucose:<br />
155 mg/dL<br />
• Avg HbA1c: 7.3%<br />
• Average duration of DM: 9 yrs<br />
Coursebook Page 95 of 139<br />
3
5/31/2012<br />
Co‐morbid Conditions<br />
• Fasting Cholesterol: 166 (normal
5/31/2012<br />
Efficiency of TRIP at PVAMC<br />
Efficiency of TRIP at PVAMC<br />
• Reader<br />
(Optometrist)<br />
Schedule<br />
appointment<br />
(80%)<br />
•Eye Clinic<br />
Redundancy<br />
11%<br />
6 months<br />
Duplicate Recall<br />
37%<br />
1 year<br />
Refer to eye<br />
clinic (99%)<br />
•Imager<br />
(at PCP dept)<br />
Dilated eye<br />
exam<br />
Eye<br />
Exam<br />
Teleretinal<br />
Imaging<br />
Teleretinal<br />
Recall<br />
TRIP Research Trends<br />
Good referral into eye clinic from readers<br />
Low redundancy by imagers<br />
Majority of patients had no DR<br />
Good compliance for referrals from imagers<br />
• High teleretinal imaging recall within one year<br />
of imaging<br />
Suggested Program Improvements<br />
to TRIP<br />
• Future recall for teleretinal imaging should be based<br />
on reader’s recommendation.<br />
• Increase awareness of all eye care providers to check<br />
future scheduled eye clinic appointments to reduce<br />
duplicated eye clinic and TRIP appointments<br />
Comparison to other VA TRIP<br />
Comparison to Non‐VA Populations<br />
Mansberger SL, Gleitsmann K, Gardine S, Sheppler C, Demirel S, Becker TM. The Comparative Effectiveness of Telemedicine for Providing Diabetic<br />
Retinopathy Screening Exams: A Randomized Controlled Trial<br />
Coursebook Page 97 of 139<br />
5
5/31/2012<br />
Improved Compliance with TRIP<br />
Sensitivity and Specificity of TRIP<br />
Mansberger SL, Gleitsmann K, Gardine S, Sheppler C, Demirel S, Becker TM. The Comparative Effectiveness of Telemedicine for Providing Diabetic<br />
Retinopathy Screening Exams: A Randomized Controlled Trial<br />
Benefits of TRIP<br />
Case #4<br />
Increased referrals for comprehensive eye exams<br />
Improved patient awareness and compliance<br />
Initiated timely treatment<br />
TRIP overcomes barriers for annual eye exams<br />
34‐64% of patients with DM in private and public sectors have<br />
annual eye exams, VA excels in this area<br />
Treatment is 90% effective in preventing severe vision loss<br />
Patient Satisfaction<br />
• Universally Positive<br />
• Efficient<br />
• Less time sensitive<br />
• More convenient for pt to be undilated<br />
• Pt Ed, improved understanding/awareness<br />
• Comfortable<br />
• Improved Compliance!!<br />
Economic Benefits<br />
• DM vision loss = $132 billion<br />
• Detecting proliferative diabetic retinopathy<br />
• Averting cases of severe vision loss<br />
• More time efficient<br />
• Improves adherence<br />
• TRIP may help utilize eye doctors time more<br />
effectively<br />
Cavallerano AA, Conlin PR. Teleimaging to screen for diabetic retinopathy in the Veterans Health Administration. J Diabetes Sci Technol 2(1): 33-9, 2008.<br />
Cavallerano AA, Conlin PR. Teleimaging to screen for diabetic retinopathy in the Veterans Health Administration. J Diabetes Sci Technol 2(1): 33-9, 2008.<br />
Coursebook Page 98 of 139<br />
6
5/31/2012<br />
Practical Implications: How to Bill<br />
Reimbursement<br />
PCP Site<br />
Specialist<br />
Review<br />
Diabetic<br />
Screening<br />
Encounter<br />
• Medicare<br />
– CPT 92227: remote imaging for detection of<br />
retinal disease<br />
– CPT 92228: remote imaging for monitoring and<br />
management of active retinal disease<br />
• Private and commercial carriers<br />
– CPT 92250/S0625<br />
Summary<br />
REFERENCES<br />
• TRIP fulfills the goals of screening low risk diabetic<br />
patients<br />
• Occasionally will miss some findings, or findings may<br />
be worse or improved as it is a “static image”<br />
• Helps patients to maintain quality of life and<br />
independence<br />
1. Huang ES, Basu A, O'Grady M, Capretta JC. Projecting the future diabetes population size and related costs for<br />
the U.S. Diabetes Care 32(12):2225‐2229, 2009.<br />
2. Diabetic Retinopathy. Preferred Practice Patterns. San Francisco: American Academy of Ophthalmology, 2008.<br />
3. Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin epidemiologic study of diabetic retinopathy. III.<br />
Prevalence and risk of diabetic retinopathy when age at diagnosis is 30 or more years. Arch Ophthalmol<br />
102(4):527‐532, 1984.<br />
4. Ferris FL, 3rd, Davis MD, Aiello LM. Treatment of diabetic retinopathy. N Engl J Med 341(9):667‐678, 1999.<br />
5. Garg S, Davis R. Diabetic retinopathy screening update. Clinical Diabetes: A publication of the American<br />
Diabetes Association 27:140‐145, 2009.<br />
6. Conlin PR, Fisch BM, Orcutt JC, Hetrick BJ, Darkins AW. Framework for a national teleretinal imaging program to<br />
screen for diabetic retinopathy in Veterans Health Administration patients. J Rehabil Res Dev 43(6): 741‐8, 2006.<br />
7. Cavallerano AA, Conlin PR. Teleimaging to screen for diabetic retinopathy in the Veterans Health Administration.<br />
J Diabetes Sci Technol 2(1): 33‐9, 2008.<br />
8. Lin DY, Blumenkranz MS, Brothers RJ, Grosvenor DM. The sensitivity and specificity of single‐field nonmydriatic<br />
monochromatic digital fundus photography with remote image interpretation for diabetic retinopathy<br />
screening: a comparison with ophthalmoscopy and standardized mydriatic color photography. Am J Ophthalmol<br />
134(2):204‐213, 2002.<br />
9. Farley TF, Mandava N, Prall FR, Carsky C. Accuracy of primary care clinician in screening for diabetic retinopathy<br />
using single‐image retinal photography. Ann Fam Med 6(5): 428‐34, 2008.<br />
10. Mansberger SL, Gleitsmann K, Gardine S, Sheppler C, Demirel S, Becker TM. The Comparative Effectiveness of<br />
Telemedicine for Providing Diabetic Retinopathy Screening Exams: A Randomized Controlled Trial<br />
THANK YOU!<br />
Portland VA Medical Center<br />
&<br />
<strong>Pacific</strong> <strong>University</strong> College of Optometry<br />
Coursebook Page 99 of 139<br />
7
5/29/2012<br />
Radioiodine Therapy and<br />
Graves’ Ophthalmopathy<br />
ZACHARY OSWALD, O.D.<br />
RESIDENT AT<br />
WALLA WALLA VA MEDICAL CENTER &<br />
PACIFIC CATARACT AND LASER INSTITUTE –<br />
KENNEWICK<br />
MAY 29, 2012<br />
Disclosure<br />
• Zachary Oswald, O.D., developed this course<br />
material and information independently without any<br />
relevant financial interests or influence of<br />
commercial interest.<br />
• Consent was given by the patient to present the<br />
photographs and personal information included in<br />
this course.<br />
Learning Objective<br />
Course Outline<br />
• By the end of this presentation, attendees will be able<br />
to:<br />
◦ 1. Understand, evaluate, and treat Graves’ Ophthalmopathy<br />
with more confidence.<br />
◦ 2. Recognize that using radioiodine therapy to treat<br />
hyperthyroidism can cause the development or worsening<br />
Graves’ Ophthalmopathy.<br />
◦ 3. Better understand the process of co-management with the<br />
other members of a patient’s health care provider team.<br />
• Case Presentation<br />
• Radioiodine in the treatment of hyperthyroidism<br />
• Graves’ Ophthalmopathy Overview<br />
• Possible Treatments of Graves’ Ophthalmopathy<br />
• Explore contraindications and possible side effects of<br />
oral prednisone.<br />
• Co-management Tips<br />
11/18/09 1 st Visit at WWVAMC<br />
11/18/09 1 st Visit at WWVAMC<br />
• 75 yowm<br />
• Comprehensive Exam<br />
• Personal Ocular History<br />
◦ Followed as glaucoma suspect due to larger C/D ratios for 35<br />
years, has never been prescribed glaucoma medication.<br />
◦ 2007 Cataract Extraction at PCLI - Lewiston: phaco with pc iol<br />
both eyes.<br />
◦ Last eye exam was in 2007 in Lewiston, ID.<br />
◦ Was told he had some signs of macular degeneration at last eye<br />
exam.<br />
◦ Wears Bifocals<br />
• Problem List:<br />
◦ Coronary Artery Disease<br />
◦ Congestive Heart Failure<br />
◦ Pulmonary Hypertension<br />
◦ Chronic Obstructive Pulmonary Disease<br />
◦ Dependence on supplemental oxygen<br />
◦ Gout<br />
◦ Dermatitis<br />
◦ Tinnitus<br />
◦ Sensorineural hearing loss<br />
◦ MI 12/21/91, stopped smoking then<br />
Coursebook Page 100 of 139<br />
1
5/29/2012<br />
11/18/09 1 st Visit at WWVAMC<br />
11/18/09 1 st Visit at WWVAMC<br />
• Medications:<br />
◦ Bosentan 125mg bid<br />
◦ Calcium Carbonate 650mg tab qd<br />
◦ Citalopram 20mg ½ tab qd<br />
◦ Clopidogrel Bisulfate 75mg tab qd<br />
◦ Colchicine 0.6mg tab qd<br />
◦ Digoxin 0.125mg tab qd<br />
◦ Flunisolide inhaler bid<br />
◦ Furosemide 40mg tab bid<br />
◦ Hydrocodone 5 / Acetaminopthen 500mg tid prn<br />
◦ Levothyroxine 0.175mg tab qd<br />
• Medications Continued<br />
◦ Magnesium Oxide 400mg tab qd<br />
◦ Potassium Chloride 10meq 2 tab bid<br />
◦ Ranitidine HCL 150mg tab bid<br />
◦ Sildenafil Citrate 50mg ½ tab tid<br />
◦ Simvastatin 10mg tab qhs<br />
◦ Sprionolactone 2 tab qAM, 1 tab afternoon<br />
◦ Tiotropium 1 tab in inhaler qd<br />
◦ Warfarin 5mg tab qd<br />
11/18/09 1 st Visit at WWVAMC<br />
11/18/09 A & P<br />
• +1.00-2.25 x 090 20/25<br />
• +1.00-2.25 x 090 20/20-2<br />
• Add: 2.50 20/20<br />
• Cover Test Distance 4^ exophoria<br />
• ASSESSMENT:<br />
◦ 1) Glaucoma Suspect due to larger C/D ratios (RE 0.55/0.55, LE 0.5/0.5). IOP<br />
18mmHg RE, LE today.<br />
◦ 2) Macular pigment changes BE<br />
◦ 3) Pseudophakia BE with trace PCO<br />
◦ 4) Hyperopia, Astigmatism, Presbyopia BE<br />
• PLAN:<br />
◦ 1&2) Fundus photos taken today. Monitor pt. in one year with a comprehensive<br />
exam watch for changes in ONH, pressure check, and macular changes.<br />
◦ 3) Monitor in 1 year at comprehensive exam.<br />
◦ 4) No glasses ordered today. Pt. satisfied with vision and condition of current<br />
glasses.<br />
• Return to clinic in 1 year for comprehensive examination c FDT to monitor<br />
macular pigment changes and ONH cupping.<br />
01/20/11 Fee Basis Exam at Private Office<br />
06/27/11 WWVAMC – Age 76<br />
• +1.00-1.75 x 089 20/40<br />
• +1.50-2.00 x 086 20/30-<br />
• Add: 2.50<br />
• BE 1-2+ PCO encroaching centrally<br />
• YAG performed in March 2011 at PCLI – Lewiston.<br />
• Binocular Diplopia reported as starting in February<br />
2011.<br />
• Veteran has been working with private doctor in<br />
Lewiston. Last appointment with private doctor<br />
about a week ago.<br />
• Unsure what is causing diplopia.<br />
• Has glasses with prism that help, but eyes still feel<br />
like they are not working together.<br />
• Would like to start coming to VA again because it<br />
will be more cost effective.<br />
Coursebook Page 101 of 139<br />
2
5/29/2012<br />
06/27/11 WWVAMC<br />
06/27/11 WWVAMC<br />
◦ Problem List same as initial visit.<br />
◦ Medication additions since initial visit in 2009:<br />
Albuterol 2 puffs qid prn<br />
Bacitracin ung apply to affected area tid prn (dermatitis)<br />
Carboxymethylcellulose 0.5% qid BE prn<br />
Loratadine 10mg qd<br />
Losartan Potassium 50mg ½ tab qd<br />
Mometasone Furoate 1-2 sprays qd<br />
Mupirocin 2% ung affected areas bid (dermatitis)<br />
Ocular Lubricant Pres Free ung qhs BE<br />
Nitrofurantoin 100mg cap bid<br />
◦ Medications no longer taking since initial visit 2009:<br />
Colchicine<br />
Flunisolide<br />
Simvastatin<br />
Spironolactone<br />
• Hab Rx from Fee Basis Dr.<br />
◦ +1.25-2.00*088 3-4^BD 20/40+2<br />
◦ +1.25-2.50*087 3^BU 20/50+2<br />
◦ Base Curve<br />
RE 6.2<br />
LE 5.8<br />
• EOMs<br />
◦ Sup. right gaze, right eye appears underacting.<br />
◦ Inf. left gaze, left eye appears underacting.<br />
Which muscles are affected<br />
Actions of extraocular muscles<br />
LR<br />
SR<br />
IO<br />
MR<br />
IO<br />
MR<br />
SR<br />
LR<br />
Muscle Primary Action Secondary Tertiary<br />
Superior Rectus Elevation Intorsion Adduction<br />
Inferior Rectus Depression Extorsion Adduction<br />
Medial Rectus Adduction<br />
Inferior Oblique Excyclotorsion Elevation Abduction<br />
Superior Oblique Incyclotorsion Depression Abduction<br />
Lateral Rectus Abduction<br />
IR<br />
SO<br />
SO<br />
IR<br />
Right Eye<br />
Left Eye<br />
06/27/11 WWVAMC<br />
• Cover Test c older Rx (without prism):<br />
◦ Dist: 7^BD RE neutralizes vert movement, residual 2^ BO<br />
◦ Near: 7^BD RE, 8^ BI<br />
• Cover Test c habitual Rx (prism):<br />
◦ Dist: ortho vert and horiz<br />
◦ Near: ortho vert and horiz<br />
06/27/11 WWVAMC<br />
• Refraction:<br />
◦ +0.75-1.50*090 3^BD 20/25+1<br />
◦ +1.75-2.50*081 2^BU 20/25-2 BE:20/25-2<br />
◦ ADD: 2.50 20/25-<br />
• Binocular Testing:<br />
◦ Distance<br />
Horiz Phoria: 5^ BO<br />
Vergences: BI: x/-2/-5, BO: x/20/9<br />
Vert Phoria: 7^ BU LE<br />
Vergences (with 3^BO otherwise no fusion):<br />
LE BU 9/5, BD -2/NA<br />
◦ Near:<br />
Horiz: 10^ BI<br />
Vert 6^ BU LE<br />
Coursebook Page 102 of 139<br />
3
5/29/2012<br />
06/27/11 WWVAMC<br />
• Trial Framed the refraction:<br />
◦ +0.75-1.50*090 3^BD 20/25+1<br />
◦ +1.75-2.50*081 2^BU 20/25-2 BE:20/25-2<br />
◦ ADD: 2.50 20/25-<br />
• Patient reports the letters feel like they are trying to<br />
pull apart, but 5^ BU LE was preferred to 4^ BU or<br />
6^BU. No prism preferred horizontally.<br />
06/27/11 WWVAMC<br />
• Assessment:<br />
◦ 1. Right hypertropia causing diplopia – several muscles may be<br />
involved causing prism combinations to not totally correct the<br />
diplopia.<br />
◦ 2. Dry Eye Syndrome – causing some fluctuation of vision.<br />
◦ 3. Dry AMD BE – at most is minimally affecting vision.<br />
◦ 4. Glaucoma suspect secondary to larger c/d ratios (0.45/0.45 BE)<br />
pressures up from before (21/19), sloping discs.<br />
◦ 5. Bilateral pseudophakia s/p YAG BE<br />
• Plan:<br />
◦ 1. Ordered new bifocals.<br />
◦ 2. Encouraged to continue artificial tears 4x day and ointment at<br />
night.<br />
◦ 3-5. Monitor in one year with full exam.<br />
09/09/11 WWVAMC – Age 77<br />
09/09/11 WWVAMC<br />
• Vet reports that he received his new spectacles about<br />
2 weeks ago. They function better than previous<br />
spectacles, but he reports continued diplopia with<br />
and without them. Sometimes in the afternoon he<br />
sees singly. Right eye reported as much blurrier than<br />
the left with new spectacles.<br />
• External Exam:<br />
◦ Patient uses oxygen by nasal cannula tank with tank set to a 5<br />
or 6 and his lips have a blue hue (vet has pulmonary<br />
hypertension). Right eye possibly proptotic.<br />
• Visual Acuities<br />
• Current Spec Rx:<br />
◦ +1.25-1.25*092 3^BD 20/50 PH: 20/40<br />
◦ +1.75-2.50*082 2^BU 20/25+1<br />
◦ Add:2.25<br />
• Refraction:<br />
◦ RE: +0.75-2.00*092 20/25-2<br />
09/09/11 WWVAMC<br />
09/09/11 WWVAMC<br />
• EOMs:<br />
◦ Restricted RE sup/temp, LE inf/temp, Possible restriction LE<br />
sup/temp as well. (+) forced duction test.<br />
• Pupils: PERRL (-) APD 5-3, 2+ reaction light.<br />
• Cover Test over new specs:<br />
◦ Distance: 3^BD RE neutralizes vertical movement.<br />
◦ Near: 3^BD RE neutralizes vertical movement. 6^exo after<br />
vertical prism correction.<br />
• Red Cap Test: = saturation BE<br />
• Amsler Grid: BE (-) metamorphopsia, (-) scotomas<br />
• Exophthalmometry: 22/21 @ 110 (avg is 15-17)<br />
• SLE:<br />
• Lids, Lashes, Adnexa: BE: edematous upper lids, 2+<br />
dermatochalasis, 2+ MG inspissation, 1+ scalloped<br />
lid margins, 1+ debris along lashes.<br />
• Cornea: BE: Tr-1+ arcus 360*, 1+ diffuse SPK cent to<br />
inf.<br />
Coursebook Page 103 of 139<br />
4
5/29/2012<br />
Suspect Graves’ Ophthalmopathy<br />
• Pertinent medical history:<br />
◦ Veteran has a history of hyperthyroidism that was treated with<br />
radioiodine ablation.<br />
◦ Veteran is currently taking one 0.175mg tablet of levothyroxine<br />
once a day for thyroid.<br />
• Labs<br />
◦ 05/05/08: Thyroid Stimulating Hormone (TSH) 0.85 (o.3-<br />
6.0)<br />
◦ 03/25/09: Free T-4: 1.7 (0.6-2.0)<br />
TSH: 3.76 (0.3-6.0)<br />
◦ 03/18/10: TSH: 2.10 (0.3-6.0)<br />
◦ 08/17/11: TSH: 1.64 (0.3-6.0)<br />
09/09/11 WWVAMC<br />
• Assessment:<br />
◦ 1. Binocular diplopia with right eye hypertropia.<br />
◦ 2. Bilateral dry eye syndrome.<br />
• Plan:<br />
◦ 1. Ordered CT scan of both eyes from orbit to chiasm without<br />
contrast enhancement to review in clinic to rule out Graves, Thyroid,<br />
or compressive sources. Discussed diplopia as possibly related to<br />
thyroid problems and possible treatment options. Dispensed and<br />
applied 3^ BD Fresnel prism on the right lens which allowed single<br />
vision today. Dispensed patch to use as needed to prevent diplopia.<br />
Will call patient following review of CT results to schedule follow up<br />
appointment.<br />
◦ 2. Patient education. Encouraged patient to continue artificial tears 4<br />
times a day and lubricating ointment once at night both eyes.<br />
Monitor.<br />
What do you notice<br />
CT Results<br />
09/09/2011<br />
• Findings:<br />
◦ “The patient has rather marked enlargement identified of the right<br />
superior rectus muscle and the left inferior rectus muscle. There is a<br />
lesser degree of enlargement of the right inferior rectus muscle and<br />
the left superior rectus muscle. There is some stranding identified<br />
surrounding the right superior rectus and left inferior rectus muscle.<br />
This appears to infiltrate the whole muscle body itself with regards to<br />
the right superior and left inferior rectus muscles. The remainder<br />
appear to be infiltrating the mid body of the muscle itself.<br />
◦ Optic nerves appear to be grossly normal. The remainder of the<br />
extraocular muscles are normal.<br />
◦ There is is diffuse cerebral atrophy noted. Some mild mucosal<br />
thickening in both maxillary sinuses.<br />
CT Results<br />
CT Scan Coronal<br />
• Impression:<br />
◦ “The patient has findings most compatible with Grave’s<br />
Ophthalmopathy.”<br />
Coursebook Page 104 of 139<br />
5
5/29/2012<br />
CT Scan Coronal<br />
Treatment Options<br />
• Researched treatment options that would work best<br />
for this patient.<br />
• Decided that oral prednisone would be best with<br />
goals of:<br />
◦ 1. Reducing periorbital edema.<br />
◦ 2. Reducing amount of exophthalmos.<br />
◦ 3. Reducing diplopia.<br />
• Who should manage this treatment plan<br />
Co-management with PCP<br />
Called clinical pharmacist at the VA<br />
• We called the patient’s PCP at 12:15pm on 09/27/11 to<br />
update her with the status of this condition and ask if she<br />
would feel more comfortable handling the Prednisone<br />
treatment.<br />
• She responded that she would prefer that someone with<br />
more experience in this field handled the treatment, and<br />
she would be happy to coordinate follow up for systemic<br />
side effects with Mr. Parks' primary care health team.<br />
• Primary health team includes VA PCP, VA clinical<br />
pharmacist, private PCP, pulmonologist, and<br />
cardiologist.<br />
• Asked him to review the patient’s medications and<br />
relate any concerns with starting oral prednisone.<br />
◦ Patient is already taking Ranitidine.<br />
◦ No major contraindications after reviewing problem list and<br />
medications.<br />
Prednisone versus Prednisolone<br />
Watch Liver Function<br />
WWVAMC 10/12/11<br />
• "Though prednisone and prednisolone are used in the same manner<br />
and equally as effective, they should not be confused with each<br />
other. Prednisone is activated by the liver into prednisolone. For<br />
this reason and because it is more easily absorbed, prednisolone is<br />
the drug of choice when hepatic disease or insufficiency is present."<br />
They are both intermediate strength synthetic corticosteroids.<br />
"Prednisone and prednisolone are synthetic members of the<br />
glucocorticoid class of hormones. They are an intermediate acting,<br />
broad antiinflammatory, medication. They have less activity than<br />
dexamethasone or betamethasone, but exhibit greater activity than<br />
hydrocortisone."<br />
From http://patients.uptodate.com/topic.aspf…<br />
• 77 yo WHITE MALE c Graves ophthalmopathy<br />
(Thyroid Eye Disease = TED) presents for follow up.<br />
• Patient reports no diplopia in straight ahead gaze<br />
since addition of 3^BD RE fresnel prism at last<br />
appointment, but image feels like it is "trying to pull<br />
apart."<br />
• Vet reports diplopia at times when looking to the<br />
side, up, or down.<br />
• Vet reports no pain or irritation BE. No dryness or<br />
tearing or redness. Vet reports that sunlight is<br />
bothersome BE.<br />
Coursebook Page 105 of 139<br />
6
5/29/2012<br />
10/12/11<br />
• EOMS: smooth pursuits. LE: restricted sup/temp,<br />
sup, and sup/nas<br />
◦ Diplopia reported in all field of gaze, worse with sup and<br />
sup/left gaze.<br />
◦ Pain Rating 0/10 in all gazes<br />
10/12/11<br />
• VISUAL ACUITY:<br />
• Current Spec Rx & lens type: St 28, 3^bd Fresnel over RE<br />
• RE:+1.25-1.25*092 3^ BD 20/50 PH: 20/40<br />
• LE:+1.75-2.50*082 2^ BU 20/25+1<br />
• Add:2.25<br />
• Refraction:<br />
• Right:+0.75-2.00*092 20/25-2<br />
• COLOR VISION/RED CAP (RE%/LE%): Equal saturation<br />
• AMSLER GRID: No metamorphopsia in either eye<br />
• SLE:<br />
• LIDS, LASHES, ADNEXA: BE: 2-3+ edematous upper lids, 2+<br />
dermatochalasis, 2+ MG inspissation, scalloped lid margins, 1+ debris<br />
10/12/11<br />
10/12/11<br />
• TONOMETRY BY iCare:<br />
• straight ahead: 18/15<br />
• up: 21/18<br />
• left: 15/14<br />
• right: 17/13<br />
• Blood pressure 146/68 pulse measurement 68<br />
• Weight: 212.5 lbs<br />
• Exophthalmometry: 22/21 @ 110<br />
• Interpalpebral distance measured vertically:<br />
• straight ahead: 10/10 mm<br />
• up: 12/13 mm<br />
10/12/11 10/12/11<br />
Coursebook Page 106 of 139<br />
7
5/29/2012<br />
10/12/11 Posterior Pole<br />
WWVAMC 10/12/11<br />
Non-VA Physicians<br />
• ASSESSMENT(S):<br />
• 1) Graves Ophthalmopathy (Thyroid Eye Disease) with incomitant strabismus and<br />
• near constant diplopia, partially relieved by Fresnel prism. Veteran already<br />
• on ranitidine.<br />
• PLAN(S):<br />
• 1) Veteran is unable to withstand surgical management and steroid<br />
• immunosuppression is the best/only option - patient education. Before<br />
• prescribing prednisone, non-VA providers will be contacted for consensus on<br />
• treatment. 20 mg/day oral prednisone to be started for 1 week with patient<br />
• monitoring his blood pressure, pulse, and weight - with plan to increase to 40<br />
• mg/day if well-tolerated. Return to Walla Walla after 4 weeks of treatment;<br />
• fasting labs: Chem, UA, CBC.<br />
• PATIENT EDUCACTION:<br />
• Reviewed common side effects of Prednisone with patient and his spouse<br />
• including: osteoporosis, irritability/depression, and heartburn/GI tract<br />
• disorders. We also discussed the increased risk of exacerbation of<br />
• hypertension and congestive heart failure.<br />
• Pulmonology: Spokane<br />
• Cardiology: Spokane<br />
• Primary Care: Lewiston<br />
• All gave the okay for to start oral Prednisone.<br />
• Pulmonologist said if anything, it would help his<br />
pulmonary hypertension.<br />
• Everyone offered to help monitor for side effects and<br />
help with the taper when finished.<br />
How to prescribe Prednisone (Up-to-date) 18<br />
Started Prednisone<br />
• “The optimal dose of prednisone is uncertain. Some<br />
clinicians initiate therapy with a high dose, such as 100<br />
mg/day. However, doses of 30 to 40 mg/day appear to be<br />
as effective and have fewer side effects. Improvement<br />
usually occurs within four weeks. About one-half of<br />
patients have a good response to prednisone by the end<br />
of six months; those patients with less muscle swelling<br />
are more likely to respond [19]. However, given the many<br />
side effects of prolonged high-dose prednisone<br />
treatment, other treatments should be considered if the<br />
patient does not respond in four to six weeks. IF a good<br />
response occurs, the daily dose should be decreased to<br />
the lowest dose at which improvement is maintained.”<br />
• 10/18/11 20mg po once a day<br />
• 10/25/11 40mg po once a day<br />
Coursebook Page 107 of 139<br />
8
5/29/2012<br />
WWVAMC 11/21/11 – 1 month of treatment<br />
• REASON FOR EXAM//CC:<br />
• 77 yo WHITE MALE c Graves ophthalmopathy (Thyroid<br />
Eye Disease = TED) presents for follow up.<br />
• Vet reports that the double vision has gradually<br />
improved as he has taken the prednisone and that he<br />
feels his vision has cleared up a little bit. He feels the<br />
prednisone is helping. Vet reports that the right eye has<br />
become a little more fuzzy when looking through his<br />
glasses.<br />
• Vet reports no pain or irritation BE. No dryness or<br />
tearing or redness. Vet reports that sunlight is<br />
bothersome BE.<br />
11/21/11<br />
• EOMS: smooth pursuits. RE: sup restriction; LE:<br />
restricted sup/temp, sup, and sup/nas<br />
◦ With correction no diplopia straight ahead gaze or straight<br />
right or straight left, diplopia reported sup and inf gazes.<br />
◦ Pain Rating 0/10 in all gazes<br />
• Tried taking Fresnel prism off right lens - vet<br />
reported diplopia in straight ahead gaze as a<br />
"shadow trying to pull off the letters“<br />
• Amsler Grid:<br />
• RE: (-) scotoma, (-) metamorphopsia<br />
• LE: (-) scotoma, (-) metamorphopsia<br />
11/21/11<br />
11/21/11<br />
• Refraction:<br />
• Right: Plano-1.00*088 20/25-2 4^ base down<br />
• Left: +1.25-2.50*088 20/25 3^ base up<br />
• Vertical Vergences at distance and near: 7 right hyper<br />
• Vet reported single vision with 7^ BD RE, Diplopia with 6^<br />
BD<br />
• Adjustable Maddox Rod s correction:<br />
• Horizontal: 5-6 XP'<br />
• Vertical: 14 right hyper<br />
• SLE:<br />
◦ LIDS, LASHES, ADNEXA: BE: 2-3+ edematous upper lids, 2+ dermatochalasis, 2+ MG<br />
inspissation, scalloped lid margins, 1+ debris<br />
◦ CONJ: Tr ping N&T BE.<br />
• TONOMETRY BY iCare:<br />
• straight ahead: 21/18 @ 1319<br />
• up: 27/21<br />
• left: 20/21<br />
• right: 19/15<br />
• Blood pressure 153/59 pulse measurement 61<br />
• Weight: 210.1 lbs<br />
• Exophthalmometry: 21/20 @ 110<br />
• Interpalpebral distance measured vertically:<br />
• straight ahead: 09/09 mm<br />
• up: 07/09 mm<br />
11/21/11<br />
WWVAMC 11/21/11 – 1 month treatment<br />
• DFE: SLE: +78<br />
• DILATED PUPIL SIZE: 8 mm<br />
• LENS: BE PCIOL s/p YAG, clear and centered<br />
• VITREOUS: BE PVD and ant syneresis<br />
• OPTIC NERVE C/D RATIO: RE: 0.5/0.5v; LE:<br />
0.45/0.45v<br />
• MACULAE: BE Flat & dry. RE>LE pigment clumps/RPE<br />
changes, similar to photos 11/18/09<br />
• POSTERIOR POLE (vascular arcades to mid-periphery):<br />
intact BE<br />
• VESSELS: A:V = 2:3,mild crossing changes<br />
• ASSESSMENT(S):<br />
• 1) Graves Ophthalmopathy (Thyroid Eye Disease) with incomitant<br />
strabismus and<br />
• diplopia relieved by prism and dry eye.<br />
• 2) Mild dry macular degeneration, bilateral<br />
• 3) Pseduophakia, bilateral<br />
• 4) Glaucoma suspect due to large cup-to-disc ratios<br />
• 5) Bilateral posterior vitreous detachment<br />
• 6) Presbyopia, right eye simple myopic astigmatism, left eye mixed<br />
astigmatism<br />
Coursebook Page 108 of 139<br />
9
5/29/2012<br />
WWVAMC 11/21/11 – 1 month of Treatment<br />
WWVAMC 12/19/11 – 2 months treatment<br />
• PLAN(S):<br />
• 1) Veteran has noticed a decrease in the frequency of diplopia. No diplopia<br />
• noted with straight ahead gaze with the aid of prisms today, which is an<br />
• improvement from previous exam 10/12/11. Continue oral prednisone 40mg/day.<br />
• Veteran will continue to monitor his blood pressure, pulse, and weight. Continue<br />
• to use artificial tears four times a day as needed both eyes. Return<br />
• to Walla Walla clinic 12/19/11 for follow up appointment.<br />
• 2) Patient education. Continue to use Amsler grid at home to monitor for<br />
• distortion. Monitor.<br />
• 3)4)5) Patient education. Monitor.<br />
• 6) Continue to wear habitual spectacles with 3^ base down Fresnel prism on right<br />
• lens. Right eye prescription has changed. Will wait on new glasses since amount<br />
• of prism could change while on Prednisone. Final spectacle prescription today:<br />
• Right: Plano-1.00*088 20/25-2 4^ base down<br />
• Left: +1.25-2.50*088 20/25 3^ base up<br />
• 77 yo WHITE MALE c Graves ophthalmopathy<br />
presents for follow up appointment. Vet reports that<br />
his right eye is still a little blurry (has the Fresnel<br />
prism on it). Vet reports no diplopia with the glasses<br />
and Fresnel prism on.<br />
• Vet reports compliance taking oral Prednisone<br />
40mg/day.<br />
• Subjective Symptoms: Vet reports no pain or<br />
irritation BE. No dryness, tearing, or redness. Vet<br />
reports that sunlight is bothersome BE.<br />
12/19/11 – 2 mos treatment<br />
12/19/11<br />
• External Exam, Chair Skills, Slit Lamp<br />
◦ Improved periorbital edema BE<br />
◦ Tr-1+ diffuse SPK<br />
◦ Stable compared to previous exam<br />
• Refraction:<br />
• Right:Plano-1.25*088 20/30+1 6^ base down<br />
• Left: +1.25-2.25*088 20/25 6^ base up<br />
• Add: 2.50 20/25<br />
• BINOCULAR TESTING:<br />
• Horiz phoria @ distance: 3.5 BO<br />
• Vertical phoria @ distance: 15 left hypo<br />
• Horiz phoria @ near:<br />
• Vertical phoria @ near: 9 BI<br />
• Vertical phoria @ distance: 15 left hypo<br />
• Adjustable Maddox Rod s correction:<br />
• Horizontal: 5 XP'<br />
• Vertical: 14 right hyper<br />
12/19/11<br />
WWVAMC 12/19/11 – 2 mos treatment<br />
• TONOMETRY BY iCare:<br />
• straight ahead: 18/15 @ 1044<br />
• up: 23/18<br />
• left: 18/15<br />
• right: 17/16<br />
• Blood pressure 160/60 pulse measurement 69<br />
• Weight: 210.4 lbs<br />
• ASSESSMENT(S):<br />
• 1) Graves Ophthalmopathy (Thyroid Eye Disease)<br />
with incomitant strabismus and diplopia relieved by<br />
prism and dry eye.<br />
• 2) Presbyopia, right eye simple myopic astigmatism,<br />
left eye mixed astigmatism.<br />
• Exophthalmometry: 20/20 @ 110<br />
• Interpalpebral distance measured vertically:<br />
• straight ahead: 09/09 mm<br />
• up: 10/11 mm<br />
Coursebook Page 109 of 139<br />
10
5/29/2012<br />
WWVAMC 12/19/11 – 2 months treatment<br />
WWVAMC 01/24/12 – 3 months treatment<br />
• PLAN(S):<br />
• 1) Patient education. No apparent change in the level of diplopia. Eye comfort and edema of<br />
upper lids have both improved since oral predisone therapy began 2 months ago. Continue to<br />
take one 20mg tablet of prednisone by mouth twice a day. If no improvement of diplopia is<br />
noted at next exam we will discuss tapering off the prednisone. Continue to use Refresh Plus<br />
artificial tears four times a day as needed, and ocular lubricant ointment once at night both<br />
eyes. Veteran will call if any changes in vision or overall health. Monitor in one month.<br />
• 2) Patient picked out a new frame today to use in case new lenses are ordered with prism<br />
ground in at a future date. Veteran did not report any diplopia when the Fresnel prism was<br />
removed from the right spectacle lens. The right spectacle lens in over-plussed, which causes<br />
the patient to use his left eye for the majority of his vision, thereby, reducing the symptoms of<br />
double vision. Fresnel prism was cleaned and placed in an envelope for Mr. Parks, so he can reapply<br />
it if needed at a future date. Continue to use habitual prescription, full-time wear. Final<br />
spectacle prescription today:<br />
Right:Plano-1.25*088 20/30+1 6^ base down<br />
Left: +1.25-2.25*088 20/25 6^ base up<br />
Add: 2.50<br />
• REASON FOR EXAM//CC:<br />
• 77 yo WHITE MALE c Graves ophthalmopathy presents<br />
for follow up appointment. Vet reports that his right eye<br />
is still a little blurry (has the Fresnel prism on it). Vet<br />
reports no diplopia with the glasses and Fresnel prism<br />
on. Vet reports that he did try using the glasses without<br />
the Fresnel prism, but experienced diplopia without it.<br />
• Vet reports compliance taking oral Prednisone<br />
40mg/day.<br />
• Subjective Symptoms: Vet reports no pain or irritation<br />
BE. No dryness or tearing or redness. Vet reports that<br />
sunlight is bothersome BE.<br />
01/24/12 – 3 mos treatment<br />
01/24/12<br />
• External Exam, Chair Skills, Slit Lamp<br />
◦ Improved periorbital edema BE<br />
◦ Tr-1+ diffuse SPK BE<br />
◦ Stable compared to previous exam<br />
• Refraction:<br />
• Right:Plano-1.25*090 20/30+2 6^ base down<br />
• Left: +1.00-2.00*095 20/25 6^ base up<br />
• Add: 2.50 20/25<br />
• Trial Frame: had patient wear this prescription for 10-15 minutes as he walked<br />
• around the clinic and tried reading. Mr. Parks reported comfortable, clear,<br />
• single vision.<br />
• BINOCULAR TESTING:<br />
• Horiz phoria @ distance: 3 BO<br />
• Vertical phoria @ distance: 15-16 left hypo<br />
• Horiz phoria @ near:<br />
• Vertical phoria @ near: 6-7 BI<br />
• Vertical phoria @ distance: 13-14 left hypo<br />
• Adjustable Maddox Rod s correction:<br />
• Horizontal: 4 XP'<br />
• Vertical: 14 right hyper<br />
01/24/12<br />
WWVAMC 01/24/12 – 3 mos treatment<br />
• TONOMETRY BY Tpen:<br />
• straight ahead: 25/24 @ 1012<br />
• up: 28/24<br />
• left: 26/25<br />
• right: 25/24<br />
• Blood pressure 159/75 pulse measurement 71<br />
• Weight: 216.5 lbs<br />
• Exophthalmometry: 21/20 @ 110<br />
• ASSESSMENT(S):<br />
• 1) Graves Ophthalmopathy (Thyroid Eye Disease)<br />
with incomitant strabismus and diplopia relieved by<br />
prism and dry eye.<br />
• 2) Presbyopia, right eye simple myopic astigmatism,<br />
left eye mixed astigmatism<br />
• Interpalpebral distance measured vertically:<br />
• straight ahead: 09/09 mm<br />
• up: 11/13 mm<br />
Coursebook Page 110 of 139<br />
11
5/29/2012<br />
WWVAMC 01/24/12 – 3 mos treatment<br />
Telephone Visits – 4 mos treat, 1 mo of taper<br />
• PLAN(S):<br />
• 1) Patient education. No apparent change in the level of diplopia. Eye<br />
• comfort and edema of upper lids have both improved since oral predisone therapy<br />
• began 3 months ago. Start taper of oral prednisone. Reduce from 40mg to 30mg for<br />
• one month. Called Mr. Parks primary care physician, Dr. Celso Chavez, who will<br />
• then see Mr. Parks for follow up to reduce travel for veteran. Then reduce to<br />
• 20mg for one month. Return to eye clinic in 2 months for follow up with<br />
• tonometry. Continue to use Refresh Plus artificial tears four times a day as<br />
• needed, and ocular lubricant ointment once at night both eyes. Veteran will call<br />
• if any changes in vision or overall health.<br />
• 2) Order final spectacle prescription full-time wear with high-index transition<br />
• lenses (thyroid eye disease), a rush put on the order:<br />
• Right:Plano-1.25*090 20/30+2 6^ base down<br />
• Left: +1.00-2.00*095 20/25 6^ base up<br />
• Add: 2.50 20/25<br />
• PATIENT EDUCATION:<br />
• Reviewed common side effects of Prednisone with patient including: osteoporosis,<br />
• irritability/depression, and heartburn/GI tract disorders. We also discussed the<br />
• increased risk of exacerbation of hypertension and congestive heart failure.<br />
• 02/28/11: I called veteran to see how he was doing on. He was<br />
not home, but I spoke with his wife who said he was doing<br />
well, but still waiting for his glasses.<br />
• 03/01/11: I received a phone message from veteran saying<br />
that he was in the hospital and wanted to talk with me about<br />
the glasses that were ordered.<br />
• 03/02/11: Veteran reported that he felt dizzy and passed out<br />
on Wednesday of this week. He was getting ready to be<br />
discharged from the hospital when I was speaking with him<br />
on the phone. Veteran reports that the doctors told him that<br />
he was low on oxygen, and they think that may be why he<br />
passed out. He has increased his oxygen to a 7 or 8.<br />
03/02/12 Telephone<br />
03/14/12 Telephone<br />
• Veteran reports that he is doing well the the prednisone<br />
taper, and that his primary care physician has been<br />
seeing him and ensuring that the taper is going well.<br />
Veteran is currently down to 20mg a day and is<br />
scheduled to reduce to 10mg a day starting March 24th.<br />
• Veteran has an appointment scheduled at the eye clinic<br />
on March 20th. He reported that he was not sure if he<br />
would be up to traveling yet by that time. I told him to<br />
call and let me know. If he can't make it, we can continue<br />
to work with his PCP with his follow ups concerning the<br />
tapering of the Prednisone.<br />
• Veteran at nursing home to help with recovery.<br />
• Veteran reports compliance with the taper of the Prednisone.<br />
He will continue to take 20mg once a day until March 24th.<br />
He will then start taking 10mg once a day until April 24 th .<br />
• Veteran reports he needs a prescription written out for<br />
Prednisone so the nursing home can continue to give it to<br />
him.<br />
• I suggested that veteran speak with his private primary care<br />
doctor who signed the paperwork needed to stay at the<br />
nursing home to see if he could provide the prescription.<br />
Veteran spoke with his PCP and reports he was able to provide<br />
the prescription.<br />
04/12/12 – 6 mos treatment, 3 mos taper<br />
04/12/12<br />
• 77 yo MALE c Graves ophthalmopathy presents for follow up<br />
appointment.<br />
• Vet received his new glasses yesterday and reports that he can<br />
see much better with them. No diplopia and clearer vision<br />
with the spectacles.<br />
• Current ocular medications:<br />
◦ Refresh AT q2-4 hrs BE<br />
◦ Ocular lubricant at night BE<br />
◦ Prednisone 10mg po qd.<br />
• Veteran is using a battery operated 4-wheel scooter that he<br />
said has greatly improved his independence and mobility and<br />
allows him to enjoy being outdoors again. Doctors<br />
discontinued Sildenafil.<br />
• Subjective Symptoms: Veteran reports no pain or irritation<br />
BE. Veteran reports that his eye do not feel as puffy and that<br />
they do not feel dry.<br />
Coursebook Page 111 of 139<br />
12
5/29/2012<br />
• VISUAL ACUITY:<br />
04/12/12<br />
• Current Spec Rx & lens type: ST 28<br />
• Right:Plano-1.25*090 20/30 6^ base down<br />
• Left: +1.00-2.00*095 20/30 6^ base up<br />
• Add: 2.50 20/25<br />
04/12/12<br />
• External Exam: Negative for head tilt/turn, ptosis, abnormal<br />
symmetry, skin disorders.<br />
• PERRL(-)APD: 5-3, 2+ RL<br />
• EOMS:LE restricted sup/temp, RE restricted inf, (+) diplopia<br />
sup/temp and inf gazes, Pain Rating 0/10 in all gazes.<br />
• Cover Test cc: Distance: ortho<br />
• Near: 3-4 exo<br />
• Confrontation VF: Full to finger counting<br />
• AMSLER GRID: No metamorphopsia in either eye<br />
• Adjustable Maddox Rod c correction:<br />
• Horizontal: ortho<br />
• Vertical: ortho<br />
04/12/12<br />
• Blood pressure: 114/66 Pulse: 80<br />
• Weight: 211.1 lbs<br />
• Exophthalmometry: 19/19 @ 110<br />
◦ (22/21 @ 110 on 09/09/11)<br />
•<br />
• Interpalpebral distance measured vertically:<br />
• straight ahead: 10/10 mm<br />
◦ Right eye hyper, lid at upper part of non-dilated pupil, left eye lid<br />
2mm above upper edge of non-dilated pupil.<br />
• up: 14/14 mm<br />
04/12/12<br />
• SLE:<br />
• LIDS, LASHES, ADNEXA: RE: 1+ edematous upper lid;<br />
LE: 1+ edematous upper lid; BE<br />
• 1+ dermatochalasis, 1+ MG inspissation, scalloped lid<br />
margins<br />
• CONJ: Tr ping N&T BE.<br />
• CORNEA: Tr-1+ arcus 360 BE, Tr diffuse SPK cent to inf<br />
BE<br />
• A/C: Deep & quiet without cell or flare<br />
• IRIS: Normal, without NVI<br />
• LENS: BE: PCIOL centered, s/p YAG<br />
• Tears: Mid volume with breakup time >10 sec BE<br />
04/12/12<br />
04/12/12<br />
• TONOMETRY BY Tpen:<br />
• straight ahead: 15/13 @ 0934<br />
• up: 20/14<br />
• left: 15/15<br />
• right: 15/14<br />
• down: 17/17<br />
• DFE: SLE: +78<br />
• Stable compared to previous exams.<br />
• (-) optic neuropathy<br />
Coursebook Page 112 of 139<br />
13
5/29/2012<br />
04/12/12, 6 mos treatment, 3 mos taper<br />
• ASSESSMENT:<br />
• 1) Graves Ophthalmopathy (Thyroid Eye Disease) with<br />
dry eye, incomitant strabismus, and diplopia relieved by<br />
prism.<br />
• PLAN:<br />
• 1) Discussed that diplopia is stable and veteran reports<br />
that he feels better and that new spectacles are working<br />
great. Eye comfort and edema of upper lids have both<br />
improved since oral prednisone therapy began. Continue<br />
to taper prednisone. Continue to use Refresh Plus<br />
artificial tears four times a day as needed, and ocular<br />
lubricant ointment once at night both eyes. Veteran will<br />
call if any changes in vision or overall health. Monitor.<br />
Taper Schedule<br />
• 4/24 - 5/14 7.5 mg daily (3 weeks)<br />
• 5/15 - 6/04 5.0 mg daily (3 weeks)<br />
• 6/11 - 6/24 4 mg daily (2 weeks)<br />
• 6/25 - 7/08 3 mg daily (2 weeks)<br />
• 7/09 - 7/22 2 mg daily (2 weeks)<br />
• 7/23 - 7/30 1.5 mg daily (1 week)<br />
• 7/30 - 8/06 1 mg daily (1 week)<br />
• 8/07 - 8/13 0.5 mg daily (1 week)<br />
• 8/14, 8/16, 8/18 0.5 mg every other day for 3 doses<br />
then stop<br />
Goals<br />
04/12/12<br />
9/9/11 10/13 10/18 11/21 12/19 1/24/12 4/12/12<br />
Proptosis 22/21 22/21 Start 21/20 20/20 21/20 19/19<br />
Tx<br />
Prism 8^ 8^ 7^ 12^ 12^ 12^<br />
Reduce<br />
Periorbit<br />
al Edema<br />
See<br />
photos<br />
04/12/12 04/12/12<br />
Coursebook Page 113 of 139<br />
14
5/29/2012<br />
04/12/12 Reduction in edema around eyes<br />
10/12/11 04/12/12<br />
Radioiodine in the treatment of Hyperthyroidism<br />
Risk of worsening or new onset ophthalmopathy<br />
• 69% of North American thyroid specialists chose<br />
radioiodine for a hypothetical patient with Graves’<br />
hyperthyroidism in a survey from 1990 1 .<br />
• There is increasing evidence that radioiodine<br />
therapy can cause the development or worsening of<br />
Graves’ ophthalmopathy more often than antithyroid<br />
drug therapy or surgery.<br />
TRIAL<br />
Radio<br />
iodine<br />
Methi<br />
mazole<br />
Surg<br />
ery<br />
Radio + Pred (3 mos) n New<br />
Onset<br />
Tallstedt 2 33% 10% 16% 168 13%<br />
Traisk 3 39% 21% 313 24%<br />
Bartalena 4 15% 4% 0% + 67% of patients who 443<br />
already had<br />
ophthalmopathy<br />
improved.<br />
Ponto 5 20% 5%<br />
Radioiodine in the treatment of Hyperthyroidism<br />
Lower vs. higher doses of Radioiodine<br />
• In patients with initially mild ophthalmopathy,<br />
worsening after radioiodine therapy may be prevented by<br />
the concurrent administration of glucocorticoids 4 .<br />
• An alternative option for patients with moderate to<br />
severe eye disease is to delay treatment with radioiodine<br />
until the eye disease has been stable for at least one<br />
year 6 .<br />
• In addition, radioiodine should be used with caution in<br />
patients with risk factors for ophthalmopathy, including<br />
smoking, or a high baseline serum concentration of<br />
triiodothyronine 6 .<br />
• Patients are left hypothyroid and supplements such<br />
as Levothyroxine are then used after Radioiodine<br />
therapy. Why not try to leave patients euthyroid after<br />
Radioiodine treatment<br />
◦ 1. Low-dose radioiodine therapy is more likely to result in<br />
treatment failure, necessitating another dose in 6 to 24<br />
months 7,8 .<br />
◦ 2. Less than one-third of patients are euthyroid 10 years after<br />
therapy 9 .<br />
◦ 3. Many patients have chronic subclinical hyperthyroidism,<br />
with its associated risks of atrial fibrillation and reduced bone<br />
density.<br />
Coursebook Page 114 of 139<br />
15
5/29/2012<br />
Graves’ Ophthalmopathy Review<br />
Graves’ Ophthalmopathy Review<br />
• Thyroid eye disease is a heterogeneous autoimmune<br />
orbital reaction 10 .<br />
• The overwhelming majority (90%) of thyroid eye<br />
disease cases are associated with hyperthyroidism,<br />
while the rest are either euthyroid or hypothyroid 11 .<br />
• Approximately half of Graves’ disease patients<br />
experience ophthalmic manifestations, with sightthreatening<br />
disease in 3% to 5% of cases 12 .<br />
• It is the most common orbital disorder in adults 13 .<br />
• Different terms:<br />
◦ Graves’ orbitopathy<br />
◦ Thyroid-associated ophthalmopathy<br />
◦ Thyroid-related ophthalmopathy<br />
◦ Graves’ ophthalmopathy<br />
◦ Thyroid eye disease<br />
◦ Thyroid orbitopathy<br />
◦ Endocrine exophthalmos<br />
◦ Malignant exophthalmos<br />
◦ Infiltrative ophthalmopathy<br />
Risk Factors<br />
Risk Factors<br />
• 1. Hyperthyroidism<br />
◦ The highest risk factor, although there is a subset of patients<br />
who are euthyroid or hypothryroid 11 .<br />
• 2. Smoking<br />
◦ Once a patient has Grave’s disease, the major clinical risk<br />
factor for developing thyroid eye disease is smoking 14 .<br />
◦ Patients with thyroid eye disease are four times more likely to<br />
be smokers or former smokers than never smokers 14 .<br />
◦ The greater the number of cigarettes smoked per day, the<br />
greater the risk 15 .<br />
◦ Also increases the risk for progression of ophthalmopathy after<br />
radioiodine therapy 16 .<br />
• 3. Sex<br />
◦ Women are five to eight times more likely to be affected by<br />
thyroid eye disease than men, but this largely reflects the<br />
increased incidence of Graves’ disease in women 15,19 .<br />
◦ Once someone has Graves’ disease, his or her sex has little<br />
effect on the risk 15 .<br />
◦ Men older than 60 may be at increased risk may be more<br />
severe disease 17 .<br />
• 4. Radioiodine<br />
Risk Factors<br />
Graves’ Ophthalmopathy Review<br />
• 5. Genetics<br />
◦ Multiple genes are likely to be involved in the development of<br />
thyroid eye diseases, and these interact with multiple<br />
environmental risk factors 15 .<br />
◦ An immunological predisposition is likely based on the<br />
increased incidence in certain HLA (DR, B8, and DW) types<br />
and recent genetic mapping of loci for Graves’ disease in some<br />
patients to chromosome 14 11 .<br />
This genetic localization to chromosome 14 is in the area of the<br />
gene for the TSH receptor, but to date no mapping to the area of<br />
the HLA region has been found 11 .<br />
• Possible Symptoms 19 :<br />
◦ Red eye<br />
◦ Foreign-body sensation<br />
◦ Tearing<br />
◦ Decreased vision<br />
◦ Dyschromatopsia<br />
◦ Binocular diplopia<br />
◦ Prominent (“bulging”) eyes<br />
Coursebook Page 115 of 139<br />
16
5/29/2012<br />
Graves’ Ophthalmopathy Review<br />
Graves’ Ophthalmopathy Review<br />
• Signs 19 :<br />
◦ Eyelid retraction<br />
◦ Edema<br />
◦ Lagophthalmos<br />
◦ Lid lag (von Graefe’s sign)<br />
◦ Reduced blinking<br />
◦ Superficial keratopathy<br />
◦ Conjunctival injection<br />
◦ Exophthalmos<br />
◦ Limitation of extraocular movements<br />
Supraduction most common reflecting inferior rectus involvement<br />
• Signs 19 :<br />
◦ Positive forced ductions<br />
◦ Resistance to retropulsion of globe<br />
◦ Decreased visual acuity<br />
◦ Decreased color vision<br />
◦ Relative afferent papillary defect<br />
◦ Visual field defect<br />
◦ Acute congestion of the socket and periocular tissues<br />
Graves’ Ophthalmopathy Review<br />
Graves’ Ophthalmopathy Review<br />
• Werner Classification of Eye Findings 19 :<br />
◦ No signs or symptoms.<br />
◦ Only signs.<br />
◦ Soft tissue involvement (signs and symptoms).<br />
◦ Proptosis.<br />
◦ Extraocular muscle involvement.<br />
◦ Corneal involvement.<br />
◦ Sight loss (optic nerve compression).<br />
• American Thyroid Association Grading System 20 :<br />
◦ Class I<br />
Solely involves lid retraction and stare<br />
◦ Class II<br />
Soft tissue symptoms and signs (chemosis/edema)<br />
◦ Class III<br />
Proptosis<br />
◦ Class IV<br />
Decreased motility and/or diplopia<br />
◦ Class V and Class VI<br />
Corneal exposure symptoms/signs<br />
◦ Class VI<br />
Optic neuropathy<br />
Treatment of Graves’ Orbitopathy<br />
Treatment of Graves’ Orbitopathy<br />
• Treatment of patients has 3 components:<br />
◦ Reversal of hyperthyroidism, if present<br />
◦ Symptomatic treatment<br />
◦ Treatment with a glucocorticoid, and/or orbital irradiation,<br />
and/or orbital decompression surgery to reduce inflammation<br />
in the periorbital tissues.<br />
• Symptomatic Treatment<br />
◦ Sunglasses<br />
◦ Prisms for diplopia<br />
◦ Artificial Tears and Ointments<br />
◦ Lid taping or moisture chamber goggles at nighttime<br />
Wiley X sunglasses with gasket.<br />
◦ Punctal occlusion<br />
◦ Avoid “dry eye environments”<br />
◦ Avoid sleeping on face<br />
◦ Raising the head of the bed at night<br />
◦ Cold packs<br />
◦ Smokers should stop smoking<br />
◦ Selenium 100mcg twice daily 18<br />
Coursebook Page 116 of 139<br />
17
5/29/2012<br />
Selenium 21<br />
Treatment of Graves’ Orbitopathy<br />
• “Graves' disease (GD) and ophthalmopathy (GO) are<br />
organ-specific autoimmune-inflammatory disorders<br />
characterized by a complex pathogenesis.<br />
• The inflammatory process is dominated by an imbalance<br />
of the antioxidant-oxidant mechanism, increased<br />
production of radical oxygen species (ROS), and<br />
cytokines which sustain the autoimmune process and<br />
perpetuate the disease.<br />
• Recently, selenium, which is a powerful antioxidant, has<br />
been successfully applied in patients with mild GO,<br />
slowing the progression of disease, decreasing the clinical<br />
activity score, and appreciably improving the quality of<br />
life.”<br />
• Glucocorticoid Therapy<br />
◦ Primary treatment for moderate to severe Graves’<br />
◦ Oral<br />
◦ Intravenous<br />
◦ Retrobulbar or subconjunctival injections have been found to<br />
be less effective, but can be used if oral or intravenous routes<br />
are contraindicated 20 .<br />
◦ Should monitor liver function and watch for possible side<br />
effects such as hyperglycemia and increased blood pressure.<br />
Contraindications and possible side effects of<br />
Prednisone from Micromedex.<br />
Contraindications and possible side effects of<br />
Prednisone from Micromedex.<br />
• Common<br />
• Cardiovascular:<br />
• Hypertension<br />
◦ All corticosteroids cause sodium retention which results in FLUID RETENTION.<br />
◦ Older patients or those with a history of hypertension are more likely to develop HIGH BLOOD<br />
PRESSURE during treatment with corticosteroids.<br />
• Dermatologic:<br />
• Acne, Ecchymosis, Atrophic condition of skin, Impaired healing.<br />
• Endocrine metabolic:<br />
• Body fluid retention, Decreased body growth, Hypernatremia<br />
• Gastrointestinal:<br />
• Gastrointestinal perforation, Gastrointestinal ulcer, Pancreatitis, Superinfection<br />
• Immunologic:<br />
• Superinfection: At higher risk for infection<br />
• Musculoskeletal: Osteoporosis<br />
• Psychiatric: Depression, Euphoria<br />
• -Serious<br />
• Endocrine metabolic:<br />
• Cushing's syndrome, Hyperglycemia, Primary<br />
adrenocortical insufficiency<br />
• Ophthalmic:<br />
• Cataract (2.5-60% incidence), Glaucoma (more likely<br />
after 1 year or more of therapy), increased IOP (decreases<br />
the outflow), central serous retinopathy, optic nerve<br />
damage<br />
• Respiratory:<br />
• Pulmonary tuberculosis, abscess of lung, aspergillosis,<br />
interstitial pneumonia, pulmonary nocardiosis.<br />
Prednisone Possible Drug Interactions<br />
Prednisone Possible Drug Interactions<br />
• Acenocoumarol<br />
Alatrofloxacin<br />
Alcuronium<br />
Aldesleukin<br />
Alfalfa<br />
Amobarbital<br />
Amphotericin B Liposome<br />
Anthrax Vaccine Adsorbed<br />
Aprobarbital<br />
Asparaginase<br />
Aspirin<br />
Atracurium<br />
Bacillus of Calmette and Guerin Vaccine,<br />
Live<br />
Balofloxacin<br />
Bupropion<br />
Butabarbital<br />
Butalbital<br />
Carbamazepine<br />
Cinoxacin<br />
Ciprofloxacin<br />
Cisatracurium<br />
Clarithromycin<br />
Clinafloxacin<br />
• Cyclosporine<br />
Desogestrel<br />
Dicumarol<br />
Dienogest<br />
Diphtheria Toxoid, Adsorbed<br />
Doxacurium<br />
Drospirenone<br />
Echinacea<br />
Enoxacin<br />
Estradiol Cypionate<br />
Estradiol Valerate<br />
Ethinyl Estradiol<br />
Ethynodiol Diacetate<br />
Etonogestrel<br />
Fleroxacin<br />
Fluconazole<br />
Fluindione<br />
Flumequine<br />
Fosphenytoin<br />
Gallamine<br />
Gatifloxacin<br />
Gemifloxacin<br />
Grepafloxacin<br />
Haemophilus B Vaccine<br />
• Hepatitis A Vaccine, Inactivated<br />
Hexafluorenium<br />
Hydrochlorothiazide<br />
Indinavir<br />
Influenza Virus Vaccine<br />
Isoniazid<br />
Itraconazole<br />
Ketoconazole<br />
Levofloxacin<br />
Levonorgestrel<br />
Licorice<br />
Lomefloxacin<br />
Lyme Disease Vaccine (Recombinant<br />
OspA)<br />
Ma Huang<br />
Measles Virus Vaccine, Live<br />
Medroxyprogesterone Acetate<br />
Meningococcal Vaccine<br />
Mephobarbital<br />
Mestranol<br />
Metocurine<br />
• Mivacurium<br />
Montelukast<br />
Moxifloxacin<br />
Mumps Virus Vaccine, Live<br />
Nateglinide<br />
Neostigmine<br />
Nimodipine<br />
Norelgestromin<br />
Norethindrone<br />
Norfloxacin<br />
Norgestimate<br />
Norgestrel<br />
Ofloxacin<br />
Pancuronium<br />
Pefloxacin<br />
Pentobarbital<br />
Pertussis Vaccine<br />
Phenobarbital<br />
Phenprocoumon<br />
Phenytoin<br />
Pipecuronium<br />
Plague Vaccine<br />
Coursebook Page 117 of 139<br />
18
5/29/2012<br />
Prednisone Possible Drug Interactions<br />
Warfarin/Aspirin (Micromedex)<br />
• Pneumococcal Vaccine, Diphtheria<br />
Conjugate<br />
Pneumococcal Vaccine Polyvalent<br />
Poliovirus Vaccine, Live<br />
Primidone<br />
Prulifloxacin<br />
Pyridostigmine<br />
Quetiapine<br />
Rabies Vaccine<br />
Rifampin<br />
Rifapentine<br />
Ritonavir<br />
Rocuronium<br />
Rosoxacin<br />
Rotavirus Vaccine, Live<br />
Rubella Virus Vaccine, Live<br />
Rufloxacin<br />
Saiboku-To<br />
• Secobarbital<br />
Smallpox Vaccine<br />
Somatropin<br />
Sparfloxacin<br />
Succinylcholine<br />
Telaprevir<br />
Temafloxacin<br />
Tetanus Toxoid<br />
Tosufloxacin<br />
Tretinoin<br />
Trovafloxacin Mesylate<br />
Tuberculin<br />
Tubocurarine<br />
Typhoid Vaccine<br />
Varicella Virus Vaccine<br />
Vecuronium<br />
Warfarin<br />
Yellow Fever Vaccine<br />
• “Summary: The concomitant use of corticosteroids<br />
and anticoagulants has been associated with both<br />
enhanced and diminished anticoagulant effects.<br />
Monitoring of coagulation indices is recommended<br />
when prednisone is co-administered with an<br />
anticoagulant, such as warfarin.”<br />
Treatment of Graves’ Orbitopathy<br />
Treatment of Graves’ Orbitopathy<br />
• External orbital radiation<br />
◦ The role of orbital radiotherapy is controversial 15 .<br />
◦ Effective in up to 70% of patients 11 .<br />
◦ Has been used in the treatment of Graves’ Orbitopathy for more than<br />
90 years 20 .<br />
◦ Used for anti-inflammatory effects and radiosensitivity of activated<br />
orbital T-cells and fibroblasts 20 .<br />
◦ A common cumulative dose of radiation is 20 Gy per eye,<br />
fractionated over a 2-week period 20 .<br />
◦ Known complications are fortunately rare, but may include radiation<br />
retinopathy and cataract 20 .<br />
◦ Also theoretic concerns of cancer induction which is estimated at<br />
0.39% 20 .<br />
◦ Can be used as adjunct to steroids, decompression, or both for<br />
recalcitrant disease 20 .<br />
◦ Contraindicated in diabetic patients with pre-existing retin0pathy 15 .<br />
• Surgical interventions are deferred until a 9-12 month<br />
stable interval is recorded, except in cases of optic<br />
neuropathy or extreme proptosis causing severe<br />
exposure keratopathy 19 .<br />
• Surgery (order is stepwise posterior to anterior):<br />
◦ Orbital decompression surgery<br />
Traditional indications for decompression involved predominantly<br />
optic neuropathy and severe exposure keratopathy 10 .<br />
◦ Fat decompression surgery<br />
Removal of intraconal fat reduces congestive orbitopathy, proptosis,<br />
and may improve preoperative diplopia 10 .<br />
◦ Strabismus surgery<br />
◦ Eyelid reconstruction as indicated<br />
Optic Neuropathy 19<br />
Treatment of Graves’ Orbitopathy<br />
• “Immediate treatment with oral steroids (prednisone<br />
100mg po qd for 2-14 days).<br />
• The use of external beam irradiation (15-30Gy) is<br />
controversial and falling out of favor.<br />
• Orbital decompression for compressive optic<br />
neuropathy should be performed by an oculplastic<br />
surgeon. A balanced approach with decompression<br />
of the medial and lateral orbital walls is most<br />
commonly employed. Removal of the inferior wall is<br />
avoided if possible due to higher incidence of<br />
induced diplopia.”<br />
• Rituximab 18<br />
◦ A number of reports have indicated that some patients with<br />
severe GO may respond dramatically to B cell depletion<br />
induced by Rituximab, which is a monoclonal antibody<br />
directed against the B cell CD20 molecule.<br />
◦ Rituximab induces a fall in TSH receptor antibody levels and<br />
depletion of B cells in the retro orbital tissues, not just the<br />
periphery.<br />
◦ Currently undergoing larger trials; preliminary results from<br />
these trials suggest efficacy in some, but not all, patients.<br />
◦ Used in cases of lymphomas, leukemia, transplant rejection<br />
and some autoimmune disorders.<br />
Coursebook Page 118 of 139<br />
19
5/29/2012<br />
Treatment of Graves’ Orbitopathy<br />
Prognosis 19<br />
• Somatostatin analogs 18<br />
◦ “Have been explored as potential therapy for GO, based upon<br />
the observations that orbital fibroblasts have somatostatin<br />
receptors and the activity of orbitopathy correlates with<br />
activity on octreotide scintigrams.”<br />
• “Diplopia and ocular surface disease are common;<br />
6% develop optic nerve disease. Despite surgical<br />
rehabilitation, which may require multiple<br />
procedures, patients are often left with functional<br />
and cosmetic defects.”<br />
Quality of Life and Occupational Disability in<br />
Endocrine Orbitopathy<br />
Quality of Life and Occupational Disability in<br />
Endocrine Orbitopathy<br />
• Background<br />
◦ “In endocrine orbitopathy (EO), disfiguring proptosis and<br />
diplopia impair patients quality of life both at home and at<br />
work.”<br />
• Methods<br />
◦ “From late 2006 to the beginning of 2008, 250 outpatients in<br />
an interdisciplinary thyroid and eye clinic filled out a<br />
questionnaire about their quality of life, occupational<br />
disability, and use of psychotherapy. 400 physicians who<br />
referred their EO patients to the clinic also participated in a<br />
survey on these issues.”<br />
• Patient Results<br />
◦ 45% of the patients complained of restrictions in their daily<br />
activities.<br />
◦ 38% reported impaired self-perception.<br />
◦ 36% were on sick leave because of EO.<br />
◦ 28% were disabled.<br />
◦ 5% had retired early.<br />
◦ 3% had lost their jobs.<br />
◦ 21% underwent psychotherapy.<br />
Quality of Life and Occupational Disability in<br />
Endocrine Orbitopathy<br />
Co-management Tips<br />
• Physician results<br />
◦ 75% stated that they were taking care of temporarily disabled<br />
patients.<br />
◦ 34% stated that they were taking care of permanently disabled<br />
patients.<br />
◦ 38% stated that they were treating EO patients who were<br />
undergoing psychotherapy.<br />
• Golden Rule: “Do unto others as you would have<br />
them do unto you.”<br />
• Take the time to fully understand the case and<br />
prepare for questions the other health care<br />
professional might ask.<br />
• Have the patient’s chart with you during all<br />
communication with others.<br />
• Always look for opportunities to learn something<br />
new and build relationships with others.<br />
Coursebook Page 119 of 139<br />
20
5/29/2012<br />
Sources<br />
Sources<br />
• 1. Wartofsky L, Glinoer D, Solomon B, et al. Differences and<br />
similarities in the diagnosis and treatment of Graves’ disease<br />
in Europe, Japan, and the United States. Thyroid 1991; 1:129.<br />
• 2. Tallstedt L, Lundell G, Torring O, et al. Occurrence of<br />
ophthalmopathy after treatment for Graves’ hyperthyroidism.<br />
The Thyroid Study Group. N Engl J Med 1992; 326:1733.<br />
• 3. Traisk F, Tallstedt L, Abraham-Nordling M, et al. Thyroidassociated<br />
ophthalmopathy after treatment of Graves’<br />
hyperthyroidism with antithyroid drugs or iodine-131. J Clin<br />
Endocrinol Metab 2009; 94:3700.<br />
• 4. Bartalena L, Marcocci C, Bogazzi F, et al. Relation between<br />
therapy for hyperthyroidism and the course of Graves’<br />
ophthalmopathy. N Engl J Med 1998; 338:73.<br />
• 5. Ponto KA, Zang S, Kahaly GJ. The tale of radioiodine and<br />
Graves’ orbitopathy. Thyroid 2010 Jul; 20(7):785-93.<br />
• 6. Mariotti S, Martino E, Francesconi M, et al. Serum thyroid<br />
autoantibodies as a risk factor for development of<br />
hypothyroidism after radioactive iodine therapy for single<br />
thyroid ‘hot’ nodule. Acta Endocrinol (Copenh) 1986; 113:500.<br />
• 7. Rapoport B, Caplan R, DeGroot LJ. Low-dose sodium<br />
iodide I 131 therapy in Graves disease. JAMA 1973; 224:1610.<br />
• 8. Goolden AW, Stewart JS. Long-term results from graded<br />
low dose radioactive iodine therapy for thyrotoxicosis. Clin<br />
Endocrinol (Oxf) 1986; 24:217.<br />
• 9. Sridama V, McCormick M, Kaplan EL, et al. Long-term<br />
follow-up study of compensated low-dose 131I therapy for<br />
Graves’ disease. N Engl J Med 1984; 311:426.<br />
Sources<br />
Sources<br />
• 10. Bothun, ED, Scheurer RA, Harrison AR, et al. Update<br />
on thyroid eye disease and management. Clinical<br />
Ophthalmology 2009; 3:543-51.<br />
• 11. Burch HB, Wartofsky L. Graves’ ophthalmopathy:<br />
current concepts regarding pathogenesis and<br />
management. Endocr Rev. 1993; 14(6):747-93.<br />
• 11. Liu, GT, Volpe NJ, Galetta SL. Thyroid-associated<br />
ophthalmopathy. Neuro-ophthalmopathy: <strong>Diagnosis</strong><br />
and Mangement. Philadelphia: Saunders, 2001. 661-72.<br />
Print.<br />
• 12. Bartalena L, Pinchera A, Marcocci C. Management of<br />
Graves’ ophthalmopathy: reality and perspectives.<br />
Endocr Rev 2000;21(2):168-99.<br />
• 13. Ponto KA, Pitz S, Pfeiffer N, et al. Quality of life and<br />
occupational disability in endocrine orbitopathy. Dtsch<br />
Arztebl Int 2009; 106(17):283-9.<br />
• 14. Vestergaard, P. Smoking and thyroid disorders—a<br />
meta-analysis. Eur J Endocrinol 2002; 146:153-61.<br />
• 15. Cawood T, Moriarty P, O’Shea D. Recent<br />
developments in thyroid eye disease. BMJ 2004;<br />
329:385-90.<br />
• 16. Bartalena L, Marcocci C, Tanda ML, et al. Cigarette<br />
smoking and tretment outcomes in Graves<br />
ophthalmopathy. Ann Intern Med 1998; 129:632-5.<br />
Sources<br />
• 17. Perros P, Crombie AL, Matthews JN, Kendall-Taylor P. Age and<br />
gender influence the severity of thyroid-associated ophthalmopathy:<br />
a study of 101 patients attending a combined thryroid-eye clinic.<br />
Clin Endocrinol (Oxf) 1993; 38:367-72.<br />
• 18. Davies TF. Treatment of graves’ orbitopathy (ophthlamopathy).<br />
www.uptodate.com 20 Jun 2011.<br />
• 19. Friedman NJ, Kaiser PK, Pineda R. Thyroid-related<br />
ophthalmopathy. The Massachusetts Eye and Ear Infirmary<br />
Illustrated Manual of Ophthalmology. Saunders 2009. 15-19.<br />
• 20. Griepentrop GJ, Garrity JA. Update on the medical treatment of<br />
Graves’ ophthalmopathy. Int J of Gen Med 2009; 2:263-9.<br />
• 21. Duntas, LH. The evolving role of selenium in the treatment of<br />
graves’ disease and ophthalmopaty. J Thyroid Res 2012; Published<br />
online 2012 January 19. doi: 10.1155/2012/736161.<br />
Coursebook Page 120 of 139<br />
21
5/29/2012<br />
ACNE ROSACEA<br />
LONG TERM COMPLICATIONS OF OCULAR<br />
ROSACEA<br />
Kevin Riedel, O.D.<br />
Portland VA Medical Center<br />
Optometry Resident, PGY-1<br />
<strong>Pacific</strong> <strong>University</strong> NW Resident’s Conference<br />
June 4, 2012<br />
• Idiopathic, chronic dermatologic<br />
condition<br />
• Characterized by erythema of<br />
the skin<br />
• Primarily affecting skin of the<br />
cheeks, forehead, chin, and<br />
nose<br />
• Signs/symptoms vary<br />
DERMATOLOGIC FEATURES<br />
• Subtype 1<br />
• “Erythematotelangiectatic”<br />
• Often asymptomatic<br />
• Characterized by flushing (erythema) and telangiectasia<br />
DERMATOLOGIC FEATURES<br />
• Subtype 2<br />
• “Papulopustular”<br />
• Often asymptomatic, but can have burning sensation of the<br />
skin especially during exacerbations<br />
• Characterized by papules and pustules<br />
DERMATOLOGIC FEATURES<br />
• Subtype 3<br />
• “Phymatous”<br />
• ‘Phyma’ – Greek for swollen or bulbous mass<br />
• More likely to be symptomatic<br />
• Classically characterized by extreme sebaceous gland<br />
hypertrophy and rhinophyma<br />
Coursebook Page 121 of 139<br />
1
5/29/2012<br />
Gnathophyma<br />
Metophyma<br />
Otophyma<br />
TRIGGERS<br />
• Environmental factors can cause an outbreak of symptoms (taken from survey of<br />
1,066 patients by the National Rosacea Society)<br />
• Sun exposure (81%)<br />
• Emotional stress (79%)<br />
• Hot weather (75%)<br />
• Wind (57%)<br />
• Strenuous exercise (56%)<br />
• Alcohol consumption (52%)<br />
• Hot bath/shower (51%)<br />
• Others: spicy foods, hot beverages, cigarette smoke, caffeine<br />
EPIDEMIOLOGY<br />
• More common in:<br />
• Adults (acne vulgaris more common<br />
in adolescents)<br />
• Women, however usually more<br />
severe in men (phymatous rosacea<br />
seen less often in females)<br />
• Fair skin (less common in darkly<br />
pigmented races)<br />
• Northern European descent<br />
• Irish<br />
• English<br />
• Scandanavian<br />
• Dutch<br />
• German<br />
TREATMENT<br />
• Topical antibiotics<br />
• Usually erythromycin or metronidazole<br />
• Oral tetracyclines<br />
• Tetracycline or doxycycline<br />
• Surgical treatment<br />
• Typically for severe phymatous rosacea that does not respond to<br />
oral/topical therapy<br />
• Electrosurgery<br />
• Laser (CO2)<br />
• Dermabrasion<br />
Coursebook Page 122 of 139<br />
2
5/29/2012<br />
BEFORE<br />
AFTER<br />
PATHOPHYSIOLOGY – THEORIES<br />
• Climate exposure<br />
• Chemical/food exposure<br />
• Microbial trigger<br />
• Impaired iron metabolism<br />
• Affects of reactive oxygen species and free radical exposure<br />
• Vascular endothelial growth factor and other angiogenic factors<br />
• Antimicrobial peptides<br />
PATHOPHYSIOLOGY – THEORIES<br />
• Climate exposure<br />
• Chemical/food exposure<br />
• Microbial trigger<br />
• Impaired iron metabolism<br />
• Affects of reactive oxygen species and free radical exposure<br />
• Vascular endothelial growth factor and other angiogenic factors<br />
• Antimicrobial peptides<br />
CLIMATE EXPOSURE<br />
• Harsh ultraviolet exposure can cause damage to superficial<br />
blood vessels and connective tissue in the dermis<br />
• This theoretically can lead to chronic increased vascular<br />
permeability and dermatitis<br />
• Could explain why rosacea is typically seen on sun exposed<br />
areas<br />
• Sunlight is believed to be a possible trigger of outbreaks<br />
PATHOPHYSIOLOGY – THEORIES<br />
• Climate exposure<br />
• Chemical/food exposure<br />
• Microbial trigger<br />
• Impaired iron metabolism<br />
• Affects of reactive oxygen species and free radical exposure<br />
• Vascular endothelial growth factor and other angiogenic factors<br />
• Antimicrobial peptides<br />
Coursebook Page 123 of 139<br />
3
5/29/2012<br />
CHEMICAL/FOOD EXPOSURE<br />
• Spicy food, hot beverages, & alcohol known to cause<br />
exacerbations<br />
• Medications can also cause exacerbations<br />
(topical/intranasal steroids, high dose vitamin B6/B12,<br />
amiodarone)<br />
• No evidence that these are the underlying cause of the<br />
disease<br />
PATHOPHYSIOLOGY – THEORIES<br />
• Climate exposure<br />
• Chemical/food exposure<br />
• Microbial trigger<br />
• Impaired iron metabolism<br />
• Affects of reactive oxygen species and free radical exposure<br />
• Vascular endothelial growth factor and other angiogenic factors<br />
• Antimicrobial peptides<br />
MICROBIAL TRIGGER<br />
• Demodex (parasitic mites that live in & around human hair follicles)<br />
• Prefer skin of nose and cheeks<br />
• Some research shows that helper T-cell infiltration occurs adjacent<br />
to known Demodex infestation in patients with rosacea<br />
• Demodex is also found in many healthy individuals without rosacea<br />
Bonnar E, Eustace P, Powell FC. The Demodex mite population in rosacea. J Am Acad Dermatol. Mar<br />
1993;28(3):443-8.<br />
• Helicobacter pylori (bacterium associated with peptic ulcer disease)<br />
• Incidentally, patients with rosacea have been found to have higher<br />
incidence of serological evidence of H. pylori<br />
PATHOPHYSIOLOGY – THEORIES<br />
• Climate exposure<br />
• Chemical/food exposure<br />
• Microbial trigger<br />
• Impaired iron metabolism<br />
• Affects of reactive oxygen species and free radical exposure<br />
• Vascular endothelial growth factor and other angiogenic factors<br />
• Antimicrobial peptides<br />
IMPAIRED IRON METABOLISM<br />
• Iron catalyzes conversion of hydrogen peroxide to free radicals, which<br />
cause tissue injury<br />
• Unmetabolized iron is stored as ferritin<br />
• “Oxidative stress and ferritin expression in the skin of patients with<br />
rosacea.” J Am Acad Dermatol. Feb 2009<br />
• Amount of ferritin in histological skin analysis significantly higher in<br />
patients with rosacea<br />
• Higher ferritin was associated with more advanced stages of rosacea<br />
Tisma VS, Basta-Juzbasic A, Jaganjac M, et al. Oxidative stress and ferritin expression in the skin of patients with<br />
rosacea. J Am Acad Dermatol. Feb 2009;60(2):270-6<br />
PATHOPHYSIOLOGY – THEORIES<br />
• Climate exposure<br />
• Chemical/food exposure<br />
• Microbial trigger<br />
• Impaired iron metabolism<br />
• Affects of reactive oxygen species<br />
• Vascular endothelial growth factor and other angiogenic factors<br />
• Antimicrobial peptides<br />
Coursebook Page 124 of 139<br />
4
5/29/2012<br />
REACTIVE OXYGEN SPECIES<br />
• Released early in inflammatory process by<br />
neutrophils<br />
• Cause tissue damage and cause the release of<br />
inflammatory mediators from damaged cells<br />
PATHOPHYSIOLOGY – THEORIES<br />
• Climate exposure<br />
• Chemical/food exposure<br />
• Microbial trigger<br />
• Impaired iron metabolism<br />
• Affects of reactive oxygen species and free radical exposure<br />
• Vascular endothelial growth factor and other angiogenic<br />
factors<br />
• Antimicrobial peptides<br />
VEGF & ANGIOGENESIS<br />
• Studies show increased VEGF expression in skin with<br />
rosacea lesions vs. skin without rosacea lesions (within<br />
the same patient)<br />
• “Therapeutic response of rosacea to dobesilate”. Eur J<br />
Med Res. Oct 18 2005<br />
• Topical dobesilate (used in Europe) improved<br />
erythema and telangiectasia in rosacea<br />
Cuevas P, Arrazola JM. Therapeutic response of rosacea to dobesilate. Eur J Med Res.<br />
Oct 18 2005;10(10):454-6.<br />
PATHOPHYSIOLOGY – THEORIES<br />
• Climate exposure<br />
• Chemical/food exposure<br />
• Microbial trigger<br />
• Impaired iron metabolism<br />
• Affects of reactive oxygen species and free radical exposure<br />
• Vascular endothelial growth factor and other angiogenic factors<br />
• Antimicrobial peptides<br />
ANTIMICROBIAL PEPTIDES<br />
• Part of the innate immune response<br />
• Cathelicidin<br />
• Abnormally high levels in rosacea patients vs.<br />
normals<br />
• Stimulates angiogenesis and modulates expression<br />
of VEGF<br />
• When injected into mice it induces inflammation,<br />
erythema, and telangiectasia<br />
Schauber J, Gallo RL. Antimicrobial peptides and the skin immune defense system. J Allergy<br />
Clin Immunol. Aug 2008;122(2):261-6<br />
OCULAR ROSACEA (SUBTYPE 4)<br />
• Meibomian glands are sebaceous glands and<br />
are often affected by acne rosacea<br />
• Ocular rosacea is very common (prevalent in up<br />
to 50% of patients with rosacea) and very<br />
commonly ignored by patients and their doctors<br />
Coursebook Page 125 of 139<br />
5
5/29/2012<br />
FEATURES OF OCULAR ROSACEA<br />
• Mild ocular rosacea<br />
• Signs<br />
• Meibomian gland dysfunction<br />
• Lid margin telangiectasia<br />
• Reduced tear stability<br />
(decreased TBUT)<br />
• Symptoms<br />
• Can be asymptomatic<br />
• **Fluctuating vision**<br />
• Mild foreign body sensation<br />
FEATURES OF OCULAR ROSACEA<br />
• Moderate ocular rosacea<br />
• Signs<br />
• Recurrent hordeola &<br />
chalazia<br />
• Corneal disruptions<br />
• Non-central punctate<br />
epithelial erosions<br />
• Conjunctival hyperemia<br />
• Symptoms<br />
• Constant blurred vision<br />
• Persistent epiphoria<br />
• **Burning sensation**<br />
FEATURES OF OCULAR ROSACEA<br />
• Severe ocular rosacea<br />
• Signs<br />
• Severe keratitis<br />
• Coalescent PEE affecting central<br />
cornea<br />
• Corneal ulcers<br />
• Corneal edema<br />
• Corneal neovascularization<br />
• Symptoms<br />
• Blurred vision<br />
• Eye pain<br />
TREATMENT OF OCULAR ROSACEA<br />
• Mild stages<br />
• Preservative free artificial tears QID/PRN<br />
• Eyelid hygiene -- VERY important part of the management<br />
• Avoidance of triggers<br />
• Avoidance of over-the-counter medications that dry out mucous membranes<br />
• Decongestants<br />
• Anti-histamines<br />
• Avoidance of over-the-counter eye drops with preservatives<br />
• Visine and other ocular decongestants<br />
• Artificial tears with preservative<br />
EYELID HYGIENE<br />
• What is a warm compress<br />
• Temperature Not warm…you want HOT<br />
• Duration Needs to be at least 5 minutes, if not 10-15<br />
• Digital massage is essential – breaks up stagnant material in meibomian<br />
glands<br />
• Lid scrubs<br />
• Commercial preparations vs. baby shampoo<br />
• Either works fine, but warm compress with digital massage is more<br />
important<br />
• Better for anterior blepharitis, in ocular rosacea the disease process<br />
is occurring in the meibomian glands<br />
TREATMENT OF OCULAR ROSACEA<br />
• Moderate Stages<br />
• Night-time lubrication<br />
• Celluvisc or lubricating<br />
ointment qHS<br />
• Eyelid hygiene<br />
• Topical steroids for<br />
symptomatic exacerbations<br />
• Lotemax or<br />
fluorometholone<br />
• Topical cyclosporine for longterm<br />
control of inflammation<br />
Coursebook Page 126 of 139<br />
6
5/29/2012<br />
TREATMENT OF OCULAR ROSACEA<br />
• Moderate Stages<br />
• Low dose oral doxycycline<br />
• Start 50-100mg bid then taper<br />
to as low as 50mg qd or qod<br />
• Judicious use of punctal plugs<br />
• Must treat lid<br />
disease/inflammation first or<br />
else you are keeping a pool of<br />
inflammatory tears on the<br />
ocular surface<br />
• Consider referral to dermatologist<br />
depending on individual<br />
presentation and symptomology<br />
NOTES ON DOXYCYCLINE<br />
• Not appropriate for pregnant/breastfeeding women or for children<br />
• Use with caution in patients on chronic anticoagulation (coumadin)<br />
• Increases the INR, an indicator of increased bleeding risk<br />
• Primary care physician or clinical pharmacist should always be consulted<br />
• Use caution in liver/kidney disease<br />
• Consult with primary care physician in patients with complicated medical<br />
histories<br />
• Instructions<br />
• Take on empty stomach<br />
• Take separate from dairy products, calcium supplements, & iron supplements<br />
• Side effects<br />
• Photosensitivity<br />
• GI upset/diarrhea<br />
ANTI-INFLAMMATORY PROPERTIES OF<br />
DOXYCYCLINE<br />
• Inhibits interleukin-1 in cultured human corneal epithelium<br />
Solomon, A et al. Invest Ophthalmol Vis Sci. 2000 Aug;41(9):2544-57.<br />
• Inhibits MMP-13 & MMP-8 in vitro<br />
Smith GN Jr et al. Arthritis Rheum. 1999 Jun;42(6):1140-6.<br />
• Accepted treatment for dermatologic manifestations of rosacea for many<br />
years<br />
RESTASIS & OCULAR ROSACEA<br />
• Cyclosporine is an immunosuppressant that is used systemically to combat<br />
rejection in organ transplants<br />
• Reduces inflammation by inhibition of T-lymphocyte activation and migration<br />
• Topical cyclcosporine (Restasis) BID shown to be more effective than<br />
artificial tears BID in some studies<br />
• Statistically significant improvement in Schirmer scores, symptoms<br />
(OSDI questionaire), tear breakup time, & corneal staining scores.<br />
Schechter B. Adv Ther (2009) 26(6)<br />
TREATMENT OF OCULAR ROSACEA<br />
• Severe Stages<br />
• Consider referral to corneal specialist<br />
• May need corneal transplantation if corneal neovascularization<br />
or ulcer causing central corneal scarring<br />
TREATMENT OF OCULAR ROSACEA<br />
• Emerging Therapy – Anti-VEGF agents<br />
• Commonly used for retinal conditions<br />
• Choroidal neovascularization<br />
• Diabetic macular edema<br />
• Cystoid macular edema associated with retinal vascular<br />
occlusions<br />
• Now being used in subconjunctival injection by<br />
ophthalmologists to induce recession of neovascular vessels<br />
in the cornea and increase chances of successful corneal<br />
grafts<br />
Coursebook Page 127 of 139<br />
7
5/29/2012<br />
FUNCTIONAL TREATMENT FOR ADVANCED<br />
CASES<br />
• Modest magnification<br />
• Increased add power with proper education<br />
• Low power hand held magnifiers<br />
• Low power Optivisor for hands-free near<br />
tasks<br />
• **Glare Control**<br />
• These patients will be VERY light sensitive<br />
• Wrap-around tint<br />
• Gray/Plum for bright days<br />
• Amber/Yellow for cloudy days<br />
Benayoun Y et al. “Effects of Subconjunctival Bevacizumab on Corneal<br />
Neovascularization: Results of a Prospective Study.” Cornea, online ahead of print 2012.<br />
CASE PRESENTATION – A LESSON TO BE<br />
LEARNED<br />
• 9/23/2011 – Portland VAMC Optometry Clinic<br />
• 57yo white male, presenting for consult from PCP for baseline<br />
DM exam (recently diagnosed)<br />
• CC: Decreased vision and eye pain, both gradually progressing<br />
for 3 months<br />
• Eyes feel very dry and scratchy, and pain is constant and sharp,<br />
especially on blink<br />
• Vision “foggy”, like “looking through water”<br />
• LEE: August 2010<br />
OCULAR HISTORY<br />
• Chronic dry eye syndrome secondary to ocular rosacea and ectropion<br />
• Chronic ocular allergies<br />
• Refractive error & presbyopia<br />
• Ocular Medications<br />
• PFAT several times daily<br />
• Cromolyn sodium QID OU<br />
• FML once daily OU (ran out several months ago)<br />
MEDICAL HISTORY<br />
• Recently diagnosed type 2 diabetes mellitus<br />
• Last A1c: 13.4<br />
• Patient taking metformin, reports recent improvement in home blood glucose levels since<br />
starting<br />
• Depression/anxiety associated with post-traumatic stress disorder<br />
• Chronic allergies<br />
• HTN/HLD/CAD<br />
• Systemic medications<br />
• Oral doxycycline (for ocular rosacea)<br />
• Oral antihistamine qd<br />
• Oral anti-depressant<br />
• Metformin<br />
• Lisinopril/Simvastatin/Metoprolol<br />
INITIAL FINDINGS<br />
• Visual Acuity (with correction)<br />
OD: 20/200 PH 20/150<br />
OS: 20/100+2 PH 20/70<br />
• Pupils ERRL, no APD noted OD or OS<br />
• Visual field FTFC OD & OS<br />
• EOM intact OU, no additional pain on movement<br />
Coursebook Page 128 of 139<br />
8
5/29/2012<br />
ANTERIOR SEGMENT FINDINGS<br />
CORNEA OS 20/100 (20/70 BCVA)<br />
• External: (+)flushed cheeks & prominent blood vessels on cheeks/forehead/nose<br />
• Lids/Lashes:<br />
• Significant meibomian gland stasis on digital expression<br />
• Severe lid margin telangiectasia<br />
• Generalized erythema with prominent eyelid fullness<br />
• Very poor lower eyelid snapback<br />
• Conjunctiva: significant, diffuse conjunctival injection 360<br />
• Cornea<br />
CORNEA OD 20/200 (20/150 BCVA)<br />
ASSESSMENT:<br />
1. Extensive Corneal Neovascularization OD>OS related to multifactorial ocular surface<br />
disease<br />
Coursebook Page 129 of 139<br />
9
5/29/2012<br />
TREATMENT<br />
• Pred Forte QID OU<br />
• Cyclosporine BID OU<br />
• PFAT q1hr OU<br />
• Celluvisc qHS OU<br />
• Eyelid hygiene BID OU<br />
• d/c Cromolyn sodium<br />
• Oral NSAID for pain<br />
• Avoid oral antihistamine<br />
• Referral to Cornea Clinic<br />
LESSONS<br />
• Something that is common and often relatively benign (like<br />
ocular rosacea) with the right circumstances & factors can<br />
cause vision loss and blindness<br />
• Early treatment is key because advanced ocular rosacea is very<br />
challenging to control<br />
Coursebook Page 130 of 139<br />
10
5/29/2012<br />
Benjamin Taylor, OD<br />
White City VA SORCC<br />
• 59 year old Caucasian male presented to clinic for his<br />
annual diabetic eye exam<br />
• Patient complaints were:<br />
• 1. Blurred vision at distance<br />
• 2. For the last year he has been noticing “stars” in his<br />
peripheral vision 2‐3 times a week, greater in the left eye.<br />
He reported that this generally lasted for 5‐10 minutes<br />
but never lasted more than an hour and then would just<br />
fade away.<br />
• Type II Diabetes<br />
• Last A1c‐‐>6.7<br />
• Congestive Heart Failure<br />
• Patient has pacemaker<br />
• Chronic Obstructive Pulmonary Disease<br />
• Sleep Apnea<br />
• Anemia secondary to kidney failure<br />
• Hyperlipidemia<br />
• Cholesterol‐‐>205<br />
• LDL‐‐>could not be accurately calculated because triglycerides were<br />
greater than 400<br />
• HDL‐‐>29<br />
• Triglycerides‐‐>674<br />
• Hyperuricemia<br />
• Albuterol<br />
• Carvedilol<br />
• Digoxin<br />
• Furosemide<br />
• Glipizide<br />
• Hydralazine HCl<br />
• Omeprazole<br />
• Simvastatin<br />
• Valsartan<br />
• Warfarin—patient reported starting this just two months<br />
earlier<br />
• Visual Acuities without Correction<br />
• OD: 20/40<br />
• OS: 20/25+2<br />
• Pupils: errl, (‐)apd ou<br />
• EOM’s: full/no restrictions<br />
• CVF: ftfc od, os<br />
• Cover Test: orthophoria at 6m<br />
• Refraction<br />
• OD: +0.50‐1.50x079 VA: 20/20<br />
• OS: plano‐1.00x085 VA: 20/20‐1<br />
• Add +2.50 20/20 OU<br />
• Slit lamp findings<br />
• Lids/Lashes: Mild Meibomian capping<br />
• Conjunctiva: Pinguecula OU<br />
• Cornea: Clear OU<br />
• Anterior Chamber: Deep and Quiet OU<br />
• Iris: Normal OU, (‐)NVI OU<br />
• Lens: 1+ NS OU, trace ACC OU<br />
• Intraocular Pressure<br />
• OD: 15mmHg<br />
• OS: 16mmHg<br />
Coursebook Page 131 of 139<br />
1
5/29/2012<br />
• C/D Ratio<br />
• OD: 0.45v/0.40h<br />
• OS: 0.35 round, flame shaped hemorrhage on inferior temporal rim<br />
• Blood Vessels<br />
• Mild tortuosity, (‐)venous engorgement<br />
• Posterior Pole<br />
• OD: one blot heme inf/temp at the edge of arcades<br />
• OS: two large blot hemes superior to the macula within 1DD with<br />
foveal thickening. Extensive blot hemes all 4 quadrants throughout<br />
the arcades.<br />
• Macular thickening OU per OCT<br />
• Periphery<br />
• OD: few scattered mid‐peripheral blot hemes<br />
• OS: extensive mid‐peripheral blot hemes all 4 quadrants<br />
• (‐)holes, tears, retinal detachments OU<br />
• Assessment/<strong>Differential</strong>s<br />
• Central Retinal Vein Occlusion OS<br />
• Diabetic Retinopathy with possible CSME<br />
• Asymmetric OS>OD<br />
• Carotid Occlusive Disease secondary to greater hemorrhaging<br />
in the left eye<br />
• Warfarin induced retinopathy OS<br />
• Since patient recently started this medication 2 months earlier<br />
• Plan<br />
• Patient was sent to lab for ProtimeINR<br />
• Ordered Carotid Doppler Ultrasound<br />
• Also placed consult to Portland VAMC for fluorescein<br />
angiography<br />
• ProtimeINR came back slightly low at 1.9<br />
• Carotid Ultrasound results were estimated to have 90‐<br />
99% stenosis for both the right and left internal<br />
carotid arteries<br />
Coursebook Page 132 of 139<br />
2
5/29/2012<br />
• Patient then decided not to pursue further optometric<br />
testing until the stenosis was addressed<br />
• VA Physician referred patient to local Vascular<br />
Surgeon<br />
• Patient chose to pursue<br />
bilateral carotid<br />
endarterectomy done by<br />
a local vascular surgeon<br />
in Medford. The left side<br />
first on 11/16/2011 then<br />
the right on 12/28/2011.<br />
http://www.primehealthchannel.com/carotid‐endarterectomy.html<br />
• After endarterectomies patient was referred to local<br />
Ophthalmologist in Medford for a fluorescein<br />
angiography<br />
• Results are as follows:<br />
Taken 1/11/2012 Taken 10/31/2011<br />
Coursebook Page 133 of 139<br />
3
5/29/2012<br />
• Window defect associated<br />
with pigmentary change in<br />
drusen<br />
• One fine microaneurysm<br />
without leakage<br />
• The left side had multiple<br />
microaneurysms in the<br />
temporal macula and<br />
periphery without<br />
significant leakage.<br />
• There was also blockage<br />
from dot and blot<br />
hemorrhages.<br />
• There was no significant<br />
filling delay of the choroid<br />
or retina for either eye.<br />
• Probable ocular ischemic syndrome, left eye<br />
• Non‐proliferative diabetic retinopathy, left eye greater<br />
than right<br />
• History of carotid occlusive disease status post<br />
bilateral carotid endarterectomy<br />
• Cataracts<br />
• The patient was placed under observation and was<br />
scheduled for follow up with Ophthalmology in 3<br />
months.<br />
• Patient was seen again on 4/23/2012 and the findings<br />
below were described by the Ophthalmologist:<br />
• The right retinal periphery has one or two small<br />
intraretinal hemorrhages. In the left periphery, there<br />
are several intraretinal hemorrhages in each of the four<br />
quadrants of the periphery. This represents a significant<br />
decrease in hemorrhages from when I last saw him in<br />
January.<br />
• Epidemiology<br />
• Average age of 65 years, rare before 50<br />
• Men affected 2x more than women<br />
• No racial predilection<br />
• Bilateral involvement in approximately 22% of cases<br />
• 7.5 cases per 1 million people per year<br />
• May be an underestimation as OIS may be misdiagnosed as<br />
other vascular diseases<br />
• 29% of patients with Symptomatic carotid occlusion<br />
manifest retinal vascular changes that are usually<br />
Asymptomatic, and 1.5% of them per year will progress<br />
to symptomatic OIS<br />
• Pathogenesis<br />
• OIS develops primarily in patients<br />
with poor collateral circulation<br />
between the internal and external<br />
carotid arteries or between the two<br />
internal carotid arteries<br />
• People with well developed<br />
collateral circulation may not<br />
develop OIS even with total<br />
occlusion of the internal carotid<br />
artery<br />
• Those with poor collateral<br />
circulation can develop OIS with<br />
less than 50% stenosis of the<br />
internal carotid artery<br />
http://medicaldictionary.thefreedictionary.com/_/viewer.aspxpath=mosbyC<br />
AM&name=500069‐fx30.jpg<br />
Coursebook Page 134 of 139<br />
4
5/29/2012<br />
• Symptoms: patients may have the following<br />
complaints<br />
• Vision Loss<br />
• Can be described as loss of vision anywhere from suddenly to<br />
gradually over the course of a month<br />
• Pain<br />
• Patients will sometimes describe it as a dull, constant ache in<br />
the affected eye. Dull pain also felt over the orbit, upper face,<br />
and temple. This pain may worsen when patient is upright.<br />
• Lying down either can relieve or lessen the pain.<br />
• Episcleral Injection<br />
http://www.aafp.org/afp/2002/0915/p991.html<br />
• Corneal Edema<br />
• Rubeosis Iridis<br />
• Can lead to:<br />
• Hyphema<br />
• Neovascular Glaucoma<br />
http://arapaho.nsuok.edu/~fulk/kanski.html<br />
• Iridocyclitis<br />
• Lead to anterior or<br />
posterior synechiae<br />
• Other Anterior Segment findings:<br />
• Corneo‐scleral Melting<br />
• Iris Atrophy<br />
• Fixed semi‐dilated or sluggish pupil<br />
• Uveal Ectropion<br />
• Asymmetric Cataract<br />
http://disorders.eyes.arizona.edu/disorders/corneal‐dystrophycongenital‐endothelial‐1<br />
http://www.musculoskeletalnetwork.com/rheumatoidarthritis/content/article/1145622/1517642<br />
Coursebook Page 135 of 139<br />
5
5/29/2012<br />
• Cherry Red Spot<br />
• Neovascularization of the disc<br />
http://content.lib.utah.edu/cdm4/item_viewer.phpCISOROO<br />
T=/EHSL‐WFH&CISOPTR=850<br />
http://www.southcoasteye.com/whatsnew.html<br />
• Choroidal Neovascular<br />
Membrane<br />
• Cholesterol Emboli<br />
• Hollenhorst Plaque<br />
http://www.kenteyesurgery.co.uk/a‐z‐of‐eyes‐view.php/amd‐‐<br />
‐age‐related‐macular‐degeneration<br />
• Dilated Retinal Veins<br />
• Narrowed Retinal Arteries<br />
http://www.aao.org/theeyeshaveit/optic‐fundus/hollenhorstplaque.cfm<br />
http://content.lib.utah.edu/cdm4/item_viewer.phpCISOROOT=/EHSL‐<br />
WFH&CISOPTR=524<br />
• Other Posterior Segment Findings<br />
• Retinal hemorrhages<br />
• More prominent in the mid‐periphery<br />
• Microaneurysms<br />
• Macular capillary telangiectasia<br />
• Retinal arteriovenous communication<br />
• Cotton‐wool spots<br />
• Neovascularization elsewhere<br />
• Vitreous Hemorrhage<br />
• Spontaneous Retinal Arterial Pulsations<br />
• Anterior Ischemic Optic Neuropathy<br />
Coursebook Page 136 of 139<br />
6
5/29/2012<br />
• <strong>Differential</strong> <strong>Diagnosis</strong><br />
• Diabetic Retinopathy and Central Retinal Vein<br />
Occlusion are the two most likely conditions to be<br />
confused with OIS<br />
• One way to differentiate is light digital pressure on the eyelid.<br />
Doing this on eyes with OIS will induce retinal arterial<br />
pulsations. (Ophthalmodynamometry)<br />
• Diabetic retinopathy may coexist with OIS.<br />
• It is recommended that those patients with unilateral<br />
retinopathy or large asymmetry of retinopathy be examined<br />
for carotid occlusive disease<br />
• Systemic Associations<br />
• A study by Mizener et al in 1988 of 32 patients showed<br />
the following associated systemic diseases<br />
• Diabetes mellitus (56%)<br />
• Hypertension (50%)<br />
• Coronary Artery Disease (38%)<br />
• Previous Cerebral Infarction or Transient Ischemic Attack<br />
(31%)<br />
• The study also showed that OIS was the initial<br />
manifestation of carotid occlusive disease in 69% of the<br />
patients.<br />
• Other Systemic Associations with OIS:<br />
• Giant Cell Arteritis<br />
• Aortic Arch Syndrome<br />
• Takayasu Arteritis<br />
• <strong>Diagnosis</strong> techniques<br />
• Fluorescein Angiography<br />
• Indocyanine Green Angiography<br />
• Electroretinography<br />
• Visual‐Evoked Potentials<br />
• Ophthalmodynamometry<br />
• Ocular Plethysmography<br />
• Imaging Methods<br />
• Carotid Duplex Ultrasound<br />
• Color Doppler Imaging of Retrobulbar Vessels<br />
• Magnetic Resonance Angiography<br />
• Carotid Arteriography<br />
• Fluorescein Angiography<br />
• Delayed choroidal filling time<br />
• Staining of the retinal vessels<br />
• Indocyanine Green Angiography<br />
• Delayed choroidal filling time<br />
• Slow filling of the watershed zones of the choroid<br />
• Electroretinography<br />
• The a wave corresponds to photoreceptor activity<br />
• The b wave corresponds to bipolar cells<br />
• OIS results in decreased amplitude of a and b waves<br />
• Visual‐Evoked Potentials<br />
• Recovery time after photostress is prolonged in patients<br />
whom have severe carotid artery stenosis<br />
Coursebook Page 137 of 139<br />
7
5/29/2012<br />
• Ophthalmodynamometry<br />
• Used to estimate the pressure in the<br />
Ophthalmic Artery, approximately at the<br />
origin of the Central Retinal Artery.<br />
• Apply pressure to globe to increase IOP, when<br />
artery pulsations are observed this reflects<br />
the ophthalmic artery diastolic pressure.<br />
• In OIS the Central Retinal Artery perfusion<br />
pressure is low meaning less pressure is<br />
necessary for artery pulsations to appear.<br />
• Ocular Plethysmography<br />
• Measures indirectly the Ophthalmic Artery pressure by<br />
recording variations in the size and volume of the eye or<br />
ocular pulsations<br />
• http://bjo.bmj.com/content/87/3/361.2.full<br />
• Imaging Methods<br />
• Carotid Duplex Ultrasound<br />
• Probably will be most ordered diagnostic test by Optometrist<br />
when OIS is suspected<br />
• Color Doppler Imaging of Retrobulbar Vessels<br />
• Magnetic Resonance Angiography<br />
• Carotid Arteriography<br />
• Management<br />
• Carotid Endarterectomy<br />
• http://www.youtube.com/watchv=8rPwO‐093Lo<br />
• Carotid Artery Stenting<br />
• http://www.youtube.com/watchv=6nyNLQUUmOQ&feature=related<br />
• Study from the New England Journal of Medicine called the CREST trial<br />
• 4 year rate of stroke or death was 6.4% with stenting and 4.7% with<br />
endarterectomy.<br />
• The overall results of this study showed that stenting and endarterectomy were<br />
associated with similar primary composite outcomes<br />
• Periprocedural stroke<br />
• Myocardial infarction<br />
• Death and subsequent ipsilateral stroke<br />
• Stroke was more likely after stenting and myocardial infarction was more likely<br />
after endarterectomy. Also worth noting was that younger patients had slightly<br />
fewer problems after stenting and older patients had fewer problems after<br />
endarterectomy<br />
• Management Continued<br />
• Treatment is directed toward control of anterior segment<br />
inflammation, retinal ischemia, increased IOP and<br />
neovascular glaucoma<br />
• Topical Therapy<br />
• Steroid<br />
• Cycloplegic<br />
• Beta blockers<br />
• Alpha Agonists<br />
• Prostaglandins should be avoided because they can increase ocular<br />
inflammation<br />
• When neovascular glaucoma develops surgery or<br />
cycloablation is often needed<br />
• Trabeculectomy with antimetabolites<br />
• Aqueous shunt implants or diode laser cyclophotocoagulation<br />
• Management Continued<br />
• Panretinal Photocoagulation may be effective in some<br />
patients with ocular neovascularization caused from carotid<br />
occlusive disease<br />
• PRP caused regression of iris neovascularization in 36% of the<br />
treated eyes<br />
• Intravitreal Anti VEGF has been used to treat iris<br />
neovascularization and macular edema<br />
• 2 cases reported by Amselem et al of Intravitreal Avastin injection<br />
when carotid endarterectomy was contraindicated<br />
• One week after injection there was a regression of NVI in both cases<br />
and at three months there was no NVI<br />
• One case had a recurrence of NVI at 4 months and was reinjected<br />
and at seven months remained without NVI<br />
Coursebook Page 138 of 139<br />
8
5/29/2012<br />
• Conclusion<br />
• Signs and symptoms of carotid artery occlusive disease<br />
may occur before cerebrovascular and cardiovascular<br />
complications. As a result, optometrists may be the first<br />
to deal with patients suffering from carotid artery<br />
occlusive disease and should be aware of the clinical<br />
presentation of OIS.<br />
• Amselem L, Montero J, et al. Intravitreal Bevacizumab (Avastin) Injection in Ocular<br />
Ischemic Syndrome. American Journal of Ophthalmology 2007;144:122‐124.<br />
• Brott T, Hobson R, et al. Stenting versus Endarterectomy for Treatment of Carotid‐Artery<br />
Stenosis. The New England Journal of Medicine 2010;363(1):11‐23<br />
• Brown GC, Magargal LE. The ocular ischemic syndrome. Clinical, fluorescein<br />
angiographic and carotid angiographic features. Int Ophthalmol. 1988;11 (4):239‐51<br />
• Cohen R, Padilla J, et al. Carotid artery occlusive disease and ocular manifestations:<br />
Importance of identifying patients at risk. Optometry (2010)81, 359‐363.<br />
• Ferguson G, Eliasziw M, et al. The North American Symptomatic Carotid<br />
Endarterectomy Trial: Surgical Results in 1415 patients. Stroke, Journal of the American<br />
Heart Association 1999, 30: 1751‐1758.<br />
• Groschel K, Ernemann U, et al. Incidence and risk factors for medical complications after<br />
carotid artery stenting. Journal of Vascular Surgery 2005; 42: 1101‐1107.<br />
• McCullough H, Reinert C, et al. Ocular findings as predictors of carotid artery occlusive<br />
disease: Is carotid imaging justified Journal of Vascular Surgery 2004; 40: 279‐286.<br />
• Mendrinos E, Machinis T, Pournaras C. Ocular Ischemic Syndrome. Survey of<br />
Ophthalmology 2010; 55(1): 2‐34.<br />
Coursebook Page 139 of 139<br />
9