Issue 1 - San Antonio Breast Cancer Symposium
Issue 1 - San Antonio Breast Cancer Symposium
Issue 1 - San Antonio Breast Cancer Symposium
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
1 <strong>Issue</strong> 1<br />
December 10, 2009<br />
“An international scientific symposium for interaction and exchange among basic scientists and clinicians in breast cancer.”<br />
ear Colleagues:<br />
Welcome to the 32nd annual <strong>San</strong> <strong>Antonio</strong> <strong>Breast</strong> <strong>Cancer</strong> <strong>Symposium</strong>, and to our second year in<br />
collaboration with the American Association for <strong>Cancer</strong> Research (AACR). This year’s program<br />
will be bigger and more exciting than ever, with a combination of cutting-edge research, training<br />
opportunities for young researchers, and a comprehensive review of the state of breast cancer<br />
research today.<br />
The plenary lecturers this year will offer up-to-the-minute assessments in the areas of epidemiology, tumor<br />
immunotherapy, and molecular pathways associated with breast cancer. There will be 51 oral presentations in<br />
the General Sessions and over 1100 posters, as well as daily mini-symposia covering nanotechnology, the role of<br />
host-related factors, and the relationship between local control and long-term survival. Four major awards will<br />
honor clinicians and scientists who have made special contributions to the field of breast cancer research.<br />
Yesterday afternoon, continuing a highly successful program that was initiated last year, we featured a variety<br />
of basic education programs, offering additional background in important aspects of breast cancer research,<br />
including RNA interference, breast cancer prevention, and epigenetics, among others. Starting today, we will<br />
also be bringing back the immensely popular lunchtime sessions, with basic science panel discussions in areas of<br />
active controversy, as well as clinical case discussions.<br />
We will be introducing a new feature this year on Sunday morning. Instead of the usual handful of research<br />
presentations to close out the meeting, you are invited to attend a program called “The Year in Review.” This program<br />
will feature expert summaries of the symposium and assessments of developments over the last year in basic research,<br />
translational research, early breast cancer, and metastatic breast cancer.<br />
It should be an exciting week for everyone. We welcome you to <strong>San</strong> <strong>Antonio</strong>, and hope that your time here will<br />
be fruitful and enjoyable.<br />
Charles A. Coltman Jr, MD<br />
C. Kent Osborne, MD<br />
32nd Annual<br />
December 9-13, 2009<br />
Henry B. Gonzalez Convention Center<br />
<strong>San</strong> <strong>Antonio</strong>, Texas, USA<br />
The 32nd Annual <strong>San</strong> <strong>Antonio</strong> <strong>Breast</strong> <strong>Cancer</strong> <strong>Symposium</strong>
2<br />
Your Health During the <strong>Symposium</strong><br />
For the safety of our symposium participants, vendors, and staff we have implemented several steps to help limit the spread<br />
of influenza-like illnesses at the convention center:<br />
• Anti-bacterial foam soap in all restrooms<br />
• Hand sanitizing stations at all time clocks for employees to use before and after clocking in or out<br />
• All staff to use disposable gloves and to change them often<br />
• Containers of hand sanitizer in common areas<br />
• Refreshing and spraying disinfectant in restroom areas<br />
• Wiping all surfaces often, such as escalator hand rails, door knobs/handles, etc<br />
If you feel unwell while attending the symposium, please visit one of our medical services locations. We have designated areas<br />
where you can view the symposium sessions in a more comfortable setting while limiting contagion. All symposium hotels also<br />
have programs in place to assist you.<br />
Please take the following precautions recommended by the Centers for Disease Control and Prevention (CDC) to stay healthy:<br />
• Cover your nose and mouth with a tissue when you cough or sneeze. Throw the tissue in the trash after you use it.<br />
• Wash your hands often with soap and water, especially after you cough or sneeze. Alcohol-based hand cleaners are<br />
also effective.<br />
• Avoid touching your eyes, nose, or mouth. Germs spread that way.<br />
• Stay home if you get sick. Limit contact with others to keep from infecting them.<br />
• Try to avoid close contact with sick people.<br />
When in <strong>San</strong> <strong>Antonio</strong>, if you will not be attending the symposium due to illness, please contact the “call out” number on the back<br />
of your badge to enable us to track health-related issues for the protection of all symposium participants.<br />
The CDC suggests you seek urgent medical care if you are experiencing any of the following symptoms:<br />
• Difficulty breathing or shortness of breath<br />
• Pain or pressure in the chest or abdomen<br />
• Sudden dizziness<br />
• Confusion<br />
• Severe or persistent vomiting
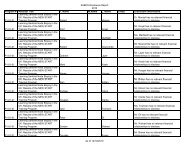
Speaker & Schedule Changes<br />
Thursday, December 10: 12:30–1:45 pm<br />
Basic Science Panel Discussions: Controversies in <strong>Breast</strong> <strong>Cancer</strong> Models for Drug Development<br />
Pre-clinical models for development of marker guided therapy in breast cancer<br />
Laura J. van ‘t Veer, PhD<br />
The Netherlands <strong>Cancer</strong> Institute, Amsterdam<br />
Revised Schedule<br />
Saturday afternoon 12/12/09<br />
12:25–1:25 pm CASE DISCUSSION 2 – Ballroom A<br />
12:25–1:25 pm BASIC SCIENCE FORUM – Ballroom B<br />
1:30–3:00 pm MINI-SYMPOSIUM 3 – Exhibit Hall D<br />
Local Control and Long-term Survival<br />
Moderators: Jay Harris, MD, Dana-Farber <strong>Cancer</strong> Institute, Boston, MA and Monica Morrow, MD, FACS,<br />
Memorial Sloan-Kettering <strong>Cancer</strong> Center, New York, NY<br />
1:30 pm Overview of the randomized trials of radiotherapy in early breast cancer<br />
Sarah Darby, PhD<br />
CTSU Oxford University, Oxford<br />
2:00 pm How the ‘4:1 ratio’ will likely change with increasingly effective systemic therapy<br />
Jay Harris, MD<br />
Dana-Farber <strong>Cancer</strong> Institute, Boston, MA<br />
2:30 pm Minimizing local recurrence: what’s proven, what’s not<br />
Monica Morrow, MD, FACS<br />
Memorial Sloan-Kettering <strong>Cancer</strong> Center, New York, NY<br />
3:00–5:30 pm GENERAL SESSION 6 – Exhibit Hall D<br />
3:00 pm 80. Results of chemotherapy alone, with sequential or concurrent addition of trastuzumab in the NCCTG<br />
N9831 HER2-positive adjuvant breast cancer trial<br />
Perez EA, Suman VJ, Davidson NE, Gralow J, Kaufman PA, Ingle JN, Dakhil SR, Pisansky TM, Jenkins<br />
RB. Mayo Clinic, Jacksonville, FL; Mayo Clinic, Rochester, MN; University of Pittsburgh, Pittsburgh,<br />
PA; Seattle <strong>Cancer</strong> Center Alliance, Seattle, WA; Dartmouth Hitchcock Medical Center, Hanover,<br />
MD; <strong>Cancer</strong> Center of Kansas, Wichita, KS; National <strong>Cancer</strong> Institute, Bethesda, MD<br />
Posters Rescheduled<br />
The following posters will be presented outside of their originally scheduled times:<br />
4028 Thursday 12/10/09 5:30–7:30 pm<br />
5077 Thursday 12/10/09 5:30–7:30 pm<br />
5109 Thursday 12/10/09 5:30–7:30 pm<br />
6033 Friday 12/11/09 5:30–7:30 pm<br />
6091 Friday 12/11/09 5:30–7:30 pm<br />
6125 Friday 12/11/09 5:30–7:30 pm<br />
Poster 5090 has been renumbered and rescheduled as:<br />
710 Saturday 12/12/09 7:00–9:00 am Poster Discussion Session 7<br />
Posters Withdrawn<br />
702, 810, 1003, 1029, 1073, 3018, 3169, 4028, 4030, 4069, 6059, 6060, 6121<br />
3
4<br />
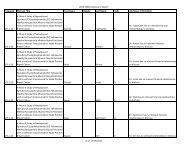
Late-Breaking Abstracts<br />
The following abstracts were received and accepted too late for inclusion in the SABCS abstract book. They will be published<br />
in the January issue of <strong>Cancer</strong> Research.<br />
Abstract 80<br />
Results of chemotherapy alone, with sequential or concurrent addition of 52 weeks of trastuzumab in the NCCTG N9831<br />
HER2-positive adjuvant breast cancer trial<br />
Perez EA, Suman VJ Davidson NE, Gralow J, Kaufman PA, Ingle JN, Dakhil SR, Zujewski JA, Pisansky TM, Jenkins RB. Mayo<br />
Clinic, Jacksonville, FL; Mayo Clinic, Rochester, MN; University of Pittsburg, Pittsburg, PA; Seattle <strong>Cancer</strong> Center Alliance, Seattle,<br />
WA; Dartmouth Hitchcock Medical Center, Hanover, MD; <strong>Cancer</strong> Center of Kansas, Wichita, KS; National <strong>Cancer</strong> Institute,<br />
Bethesda, MD<br />
Background: N9831 is the only randomized phase 3 trial comparing safety and efficacy of the addition of trastuzumab (H) to<br />
doxorubicin and cyclophosphamide then paclitaxel (Arm A: AC T) either following (Arm B: AC T H) or starting concurrently<br />
with paclitaxel (Arm C: AC T+H H) for women with resected Stage I-III invasive HER2+ breast cancer. The 3-y cumulative<br />
incidence of NYHA class III or IV congestive heart failure or sudden cardiac death was previously reported: 3.3% in Arm C, 2.8% in<br />
Arm B (Perez EA et al, JCO 2008). The comparison of AC T to AC T+H H was reported in a joint analysis of N9831 and NSABP<br />
B-31 in 2005 and updated in 2007, demonstrating a 52% reduction in risk of a disease event (Romond E et al, NEJM 2005; Perez<br />
EA et al, ASCO 2007).<br />
Materials and Methods: Primary endpoint is disease-free survival (DFS). At the second planned interim analysis of Arm A vs<br />
Arm B, the O’Brien-Fleming boundary (OFB) was crossed. NCCTG Independent Data Safety Monitoring Committee approved<br />
the release of these data, as well as the data pertaining to Arm B vs Arm C, due to slow pace of events [expected 647 events in<br />
4-y follow-up period (f/u) vs actual 334 events in 4.5-y f/u]. Shortly thereafter, there were sufficient events to perform the first<br />
planned interim analysis of B vs C. We present the results of each of these pairwise comparisons taking into account the potential<br />
for crossover to Arm C after the release of the joint analysis findings in 2005.<br />
Results: From 5/2000 to 4/2005, 2448 eligible women were enrolled for the Arm A (n=1087) vs Arm B (n=1097) comparison.<br />
Median f/u is 5.5 y, with 386 events. The addition of trastuzumab sequentially to AC T significantly improved DFS univariately<br />
[HR(Arm B/Arm A)=0.70; 95% CI, 57-86, logrank P=0.0005] and after adjusting for age, tumor size, number of positive nodes, and<br />
ER [PPH: HR adj =0.67; 95% CI, 0.55-0.82]. 5-y DFS was increased from 72% with AC T to 80% with AC T H.<br />
From 5/2000 to 4/2005, 1903 eligible women were enrolled for the Arm B (n=954) vs Arm C (n=949) comparison. Median f/u is<br />
5.3 y, with 312 events. The log-rank P value testing whether DFS differs with respect to starting time of trastuzumab was 0.019<br />
(not crossing pre-specified OFB for statistical significance). After adjusting for tumor size, number of positive nodes, and ER,<br />
[HR adj (Arm C/Arm B)=0.75; 95% CI, 0.60-0.94]. 5-y DFS was increased from 80% with AC T H to 84% for AC T+H H.<br />
Conclusions: DFS is significantly improved with the addition of 52 weeks of H (sequentially or concurrently) to AC T. There<br />
is a statistically significant 33% reduction in the risk of an event with the sequential addition of H following AC T. There is<br />
a strong trend for a 25% reduction in the risk of an event with starting H concurrently with T relative to sequentially after T.<br />
Therefore, based on a positive risk/benefit ratio, we recommend that trastuzumab be incorporated in a concurrent fashion with<br />
T chemotherapy.<br />
Acknowledgements: NIH CA25224, <strong>Breast</strong> <strong>Cancer</strong> Research Foundation, Genentech
Abstract 112<br />
Prediction of 10-year chemotherapy benefit and breast cancer-specific survival by the 21-gene Recurrence Score (RS) assay in<br />
node-positive, ER-positive breast cancer—An update of SWOG-8814 (INT0100)<br />
Albain KS, Barlow WE, Shak S, Hortobagyi GN, Livingston RB, Yeh I-T, Ravdin P, Bugarini R, Baehner FL, Davidson NE, Sledge<br />
GW, Winer EP, Hudis C, Ingle JN, Perez EA, Pritchard KI, Shepherd L, Gralow JR, Yoshizawa C, Allred DC, Osborne CK, and<br />
Hayes DF for The <strong>Breast</strong> <strong>Cancer</strong> Intergroup of North America. Loyola University Chicago Cardinal Bernardin <strong>Cancer</strong> Center,<br />
Maywood, IL.<br />
Background: A low 21-gene RS identifies patients with ER-positive breast cancer who do not appear to benefit from anthracyclinebased<br />
chemotherapy (CAF) added to tamoxifen (T) despite positive axillary lymph nodes (Albain KS et al, Lancet Oncology, in<br />
press). However, in the low RS group, the lack of improvement by CAF in the 64% disease-free survival (DFS) at 10 years is not<br />
considered definitive evidence against the use of chemotherapy for conventionally identified high-risk patients. We conducted<br />
new DFS prediction analyses within nodal categories by RS over 10 years and assessed whether the assay has predictive utility for<br />
breast cancer specific survival (BCSS).<br />
Methods: RT-PCR analyses for the 21 gene RS assay were feasible in 148 patients on T from the parent trial and 219 on CAF<br />
followed by T, as previously described. In this update, we conducted 10-year DFS analyses within nodal categories 1-3+ and 4+<br />
by the linear RS. For the exploratory analysis of BCSS, only deaths due to breast cancer were counted as events, censoring deaths<br />
due to other causes (such as late cardiovascular events), as well as patients alive at the last follow-up visit. The clinically utilized<br />
(trichotomized) RS categories of low (
6<br />
Revised Abstracts<br />
Revisions of the following abstracts were received and accepted too late for inclusion in the SABCS abstract book. They will<br />
be published in the January issue of <strong>Cancer</strong> Research.<br />
Abstract 41<br />
Final overall survival (OS) results from the randomized, double-blind, placebo-controlled, phase 3 AvADO study of<br />
bevacizumab (Bv) plus docetaxel (D) compared with placebo (PL) plus D for the first-line treatment of locally recurrent<br />
(LR) or metastatic breast cancer (mBC)<br />
Miles DW, Chan A, Romieu G, Dirix LY, Cortés J, Pivot X, Tomczak P, Juozaityte E, Harbeck N, Steger GG, the BO17708 study<br />
group. Mount Vernon <strong>Cancer</strong> Centre, Middlesex, United Kingdom; Mount Hospital, Mount <strong>Breast</strong> Group, Perth, Australia; CRLCC Val<br />
d’Aurelle, P. Lamarque Service Chimioimmunotherapie, Montpellier, France; Algemeen Ziekenhuis St. Augustinus, Wilrijk, Belgium;<br />
University Hospital Vall d’Hebron Oncology, Barcelona, Spain; University Hospital of Besancon, France; Klinika Onkologii Oddzial<br />
Chemioterapii, Poznań, Poland; Kaunas Medical University Hospital, Oncology Clinic, Kaunas, Lithuania; <strong>Breast</strong> Centre, University of<br />
Cologne, Cologne, Germany; Medical University of Vienna, Department of Internal Medicine I-Oncology, Vienna, Austria<br />
Background: Anti-VEGF monoclonal antibody BV significantly improves efficacy in combination with standard therapies in<br />
multiple tumor types, with limited impact on toxicity. Three randomized phase 3 trials (E2100, AVADO, and RIBBON-1) in mBC<br />
have demonstrated that BV + 1st-line chemotherapy (CTx) significantly improves progression-free survival (PFS) and overall<br />
response rates (ORR). We present mature OS data from AVADO.<br />
Methods: Patients (pts) with HER2-negative LR/mBC were randomized to D 100 mg/m 2 + PL, D + BV 7.5 mg/kg or D + BV 15 mg/kg.<br />
D was given q3w for ≤9 cycles. BV or PL was given q3w until disease progression/unacceptable toxicity. After progression, pts were<br />
offered BV with 2nd-line anticancer therapy in a post-study treatment phase. The primary endpoint was PFS; secondary endpoints<br />
included OS, time to treatment failure, ORR, duration of response and safety. An exploratory analysis conducted in pts receiving<br />
post-progression CTx compared OS in pts receiving 2nd-line BV with those who did not.<br />
Results: 736 pts were enrolled March 2006–April 2007. The primary analysis (data cut-off October 2007; median follow-up 10.2<br />
months) showed significant improvements in PFS and ORR for both BV-containing arms compared with PL + D. Mature OS data<br />
(data cut-off April 2009; median follow-up 25 months) are shown (Table). There was no difference in median OS between the<br />
study arms (range 30–32 months). Recognizing the limitations of the non-randomized comparison in exploratory analyses, results<br />
suggest that use of BV with 2nd-line therapy is a possible reason for lack of OS difference. Updated PFS and ORR were superior for<br />
the 15 mg/kg BV arm compared with PL + D. Results for the 7.5 mg/kg BV arm also indicated a less pronounced treatment benefit.<br />
BV had limited impact on the safety profile of docetaxel. Increased SAEs in the 15 mg/kg BV arm may be due to more pts receiving<br />
9 cycles of D than in the PL arm (51% vs 42%).<br />
Conclusions: There was no difference in OS between study arms. Exploratory analyses suggest that use of 2nd-line BV with CTx<br />
may influence OS. These mature data confirm the improvement in PFS and ORR with BV 15 mg/kg combined with D compared<br />
with PL + D.
Abstract 41<br />
PL + D<br />
(n=241)<br />
BV 7.5 mg/kg + D<br />
(n=248)<br />
BV 15 mg/kg + D<br />
(n=247)<br />
Deaths, % 44.8 47.6 47.0<br />
OS<br />
HR 1.05 1.03<br />
95% CI 0.81–1.36 0.79–1.33<br />
P value<br />
P value<br />
P value<br />
0.7198 0.8528<br />
Median 31.9 30.8 30.2<br />
Stratified PFS*<br />
HR 0.80 0.67<br />
95% CI 0.65–1.00 0.54–0.83<br />
P value † 0.0450 0.0002<br />
Median 8.1 9.0 10.0<br />
ORR ‡ , % 46.4 55.2 64.1<br />
0.0739 0.0003<br />
1-y survival, % 76 81 84<br />
PL + D<br />
(n=231)<br />
0.198 0.02<br />
BV 7.5 mg/kg + D<br />
(n=252)<br />
BV 15 mg/kg + D<br />
(n=247)<br />
SAEs, % 32.5 37.3 42.9<br />
Pts discontinuing<br />
treatment due to<br />
AE, %<br />
BV/PL 11.7 8.7 13.8<br />
D 24.7 20.6 24.3<br />
AEs leading to<br />
death, %<br />
2.6 1.6 1.6<br />
*Pts were censored if they had started non-protocol therapy before disease progression.<br />
† Exploratory.<br />
‡ Pts with measurable disease at baseline.<br />
NR, not reached.
8<br />
Abstract 44<br />
A double-blind, randomized, placebo-controlled, phase 2b study evaluating the efficacy and safety of sorafenib (SOR) in combination<br />
with paclitaxel (PAC) as a first-line therapy in patients (pts) with locally recurrent or metastatic breast cancer (BC)<br />
William J. Gradishar, Feinberg School of Medicine, Northwestern University, Chicago, IL; Virginia Kaklamani, Northwestern<br />
University, Chicago, IL; Tarini Prasad Sahoo, Jawaharlal Nehru <strong>Cancer</strong> Hospital, Bhopal-1, M.P, India; D. Lokanatha, Kidwai Institute<br />
of Oncology, Bangalore, India; Vinod Raina, Institute Rotary <strong>Cancer</strong> Hospital, New Delhi, India; Shailesh Bondarde, Shatabadi<br />
Hospital, Nashik, India; Minish Jain, Ruby Hall Clinic, Pune, India; Lee Schwartzberg, West Clinic, Memphis, TN<br />
Introduction: SOR is a targeted therapeutic agent indicated for advanced renal cell carcinoma and hepatocellular carcinoma.<br />
SOR targets multiple kinases involved in tumor growth and angiogenesis. The TIES (Trials to Investigate the Effects of Sorafenib<br />
in BC) program includes 4 phase 2b randomized, double-blind, placebo-controlled screening trials in HER2-negative BC. Recently,<br />
the first of these trials, SOR+capecitabine (CAP) vs placebo (PL)+CAP demonstrated a significant progression-free survival (PFS)<br />
benefit in pts with advanced BC. Here we present initial results from the second of the 4 trials. This study evaluated the efficacy<br />
and safety of SOR in combination with PAC as a first-line regimen for pts with advanced BC.<br />
Methods: Pts with HER2-negative, locally recurrent or metastatic BC were eligible for first-line treatment for advanced BC.<br />
Previous cytotoxic (non-metastatic), endocrine, or radiation therapy was allowed. Pts were randomized 1:1 (stratified by visceral<br />
vs non-visceral metastatic disease) to SOR (400 mg, orally, twice daily, continuously) or PL in combination with PAC (90 mg/m 2<br />
weekly, IV, 3 weeks on/1 week off). The primary endpoint was PFS. Secondary endpoints included overall survival (OS), time to<br />
progression (TTP), overall response rate (ORR), and safety. A sample size of 220 pts was planned to detect a targeted HR of 0.65<br />
(90% power and 1-sided a=0.14). The study is registered at ClinicalTrials.gov (NCT00499525).<br />
Results: From January 2008 to January 2009, 237 pts were randomized to SOR+PAC (n=119) vs PL+PAC (n=118), with 170<br />
pts in India (74% vs 69%), 52 pts in the United States (21% vs 23%), and 15 pts in Brazil (5% vs 8%). Treatment groups were<br />
balanced for age (mean, 51.9 y), ECOG performance 0 (45%) and 1 (53%), stage IV disease (85%), visceral metastatic disease<br />
(75%), and previous non-metastatic chemo (58%). Results of the study were as follows for SOR+PAC vs PL+PAC: median<br />
PFS 6.9 vs 5.6 mos (HR 0.788; 95% CI, 0.558-1.112; 1-sided log rank P=0.0857), median TTP 8.1 vs 5.6 mo (HR 0.674; 95% CI,<br />
0.465-0.975; 1-sided log rank P=0.0171), and ORR of 67% vs 54% (1-sided Cochran-Mantel-Haenszel P=0.0234). OS data<br />
are pending. Discontinuation of study treatment due to adverse events occurred in 23 pts (19%) in the SOR+PAC vs 5 pts<br />
(4%) in the PL+PAC. Grade 3/4 toxicities (SOR+PAC vs PL+PAC) included hand-foot skin reaction (30% vs 3%), asthenia<br />
(7% vs 3%), peripheral neuropathy (6% vs 7%), neutropenia (13% vs 7%), and anemia (11% vs 6%). Treatment-related deaths<br />
occurred in 2 pts (malaria and liver dysfunction), both in the SOR+PAC arm.<br />
Conclusions: Results of the primary endpoint, PFS, demonstrated a trend favoring SOR+PAC over PL+PAC in the treatment of<br />
advanced BC (HR 0.788; P=0.0857). In addition, significant improvements in TTP and ORR were observed. OS data are pending.<br />
There were no new toxicities observed with the combination and AEs were manageable. These data indicate that SOR provides<br />
added benefit when combined with PAC compared with single-agent PAC in the first-line treatment of advanced BC.
Abstract 710<br />
A phase 2 study of trastuzumab-DM1 (T-DM1), a novel HER2 antibody–drug conjugate, in HER2+ metastatic breast cancer (MBC)<br />
patients previously treated with conventional chemotherapy, lapatinib and trastuzumab<br />
Ian Krop, Dana Farber <strong>Cancer</strong> Institute, Boston, MA; Patricia LoRusso, Karmanos <strong>Cancer</strong> Institute, Detroit, MI; Kathy D. Miller,<br />
Indiana University Melvin-Bren Simon <strong>Cancer</strong> Center, Indianapolis, IN; Shanu Modi, Memorial Sloan-Kettering <strong>Cancer</strong> Center, New<br />
York, NY; Denise Yardley, Sarah Cannon Research Institute, Nashville, TN; George Rodriguez, South Texas Oncology/Hematology,<br />
<strong>San</strong> <strong>Antonio</strong>, TX; Sam Agresta, BioOncology, Genentech, South <strong>San</strong> Francisco, CA; Maoxia Zheng, BioOncology, Genentech, South<br />
<strong>San</strong> Francisco, CA; Lukas Amler, BioOncology, Genentech, South <strong>San</strong> Francisco, CA; Hope Rugo, UCSF Comprehensive <strong>Cancer</strong><br />
Center, <strong>San</strong> Francisco, CA<br />
Background: T-DM1 combines the HER2-inhibiting properties of trastuzumab with targeted delivery of the anti-microtubule<br />
agent DM1. In a prior phase 2 study, single agent T-DM1 was well tolerated and had significant activity (objective response rate<br />
[ORR] of 26% by independent review [IRF]) in 112 patients (pts) with pre-treated HER2+ MBC (Vogel CL et al, J Clin Oncol, 27:15s,<br />
2009 [suppl; abstr 1017]). To confirm and extend these findings, we conducted a phase 2 study that enrolled a more homogenous<br />
population of HER2+ MBC pts who had all received prior anthracycline, taxane, capecitabine, trastuzumab, and lapatinib therapy<br />
and progressed on the last regimen received (at least 2 HER2-directed regimens had to be given for metastatic disease).<br />
Methods: This is an open-label, single-arm study of T-DM1 given at 3.6 mg/kg IV q3w. Primary objectives are to assess ORR by<br />
IRF and evaluate the safety of T-DM1. Key secondary objectives assess the clinical benefit rate (CBR = ORR + stable disease [SD]<br />
at 6 months), duration of response (DoR) and progression-free survival (PFS). Pts remain on study until disease progression<br />
or unmanageable toxicity. Key exploratory objectives were the assessment of ORR and clinical benefit rate (CBR) by IRF in<br />
retrospectively tested, centrally confirmed HER2+ patients.<br />
Results: The study completed enrollment of 110 patients. This analysis has a median follow-up of 8.3 months (range 0.7-13.1).<br />
Median age was 52.5 y (range 34–77). Pts received a median of 7 agents for metastatic disease (range 1–15). Median<br />
durations of prior trastuzumab and lapatinib treatment in metastatic setting were 19.4 and 6.9 months respectively. The<br />
ORR was 32.7% and the CBR was 44.5% by IRF. Median DoR and PFS have not reached maturity. In retrospectively tested,<br />
centrally confirmed HER2+ patients, the ORR was 39.5% and the CBR was 52.6% by IRF. T-DM1 was well tolerated, with no<br />
dose-limiting cardiotoxicity. One pt with pre-existing non-alcoholic fatty liver disease died with hepatic dysfunction. The<br />
most common adverse events were fatigue (59.1% of pts), nausea (37.3%), and thrombocytopenia (29.1%); 41.8% of pts<br />
experienced at least one grade 3 or above adverse event.<br />
Conclusions: In this study, single agent T-DM1 demonstrates a 32.7% ORR with an acceptable safety profile in a well defined,<br />
homogeneous, and extensively pretreated population that has not been previously studied. Centrally confirmed HER2 positivity<br />
strongly correlated with objective response. These results confirm the activity of T-DM1 in treatment resistant HER2+ MBC. An<br />
ongoing global randomized phase 23 study is evaluating T-DM1 compared with lapatinib plus capecitabine in pts with advanced<br />
HER2+ who have been previously treated with a taxane and trastuzumab.<br />
9
10<br />
Revised Author Credits<br />
2132<br />
validated 3 gene signature predicts response to neo-adjuvant chemotherapy in luminal breast cancer—results from<br />
GeparTrio and Geparquattro<br />
von Minckwitz G, Budczies J, Loibl S, Darb-Esfahani S, Kaufmann M, Huober J, Engels K, Denkert C, Kronenwett R, von<br />
Toerne C. German <strong>Breast</strong> Group, Neu-Isenburg, Germany; University of Frankfurt, Frankfurt/Main, Germany; University of<br />
Tuebingen, Tuebingen, Germany; Charité, Berlin, Germany<br />
6139<br />
Gene transcripts in the tumor suppressor region of chromosome 3 (3p21)<br />
Reefy S, Al Sarakbi W, Sasi W, Jiang WG, Roberts T, Newbold RF, Mokbel K. St George’s University of London, London, United<br />
Kingdom; University, Wales College of Medicine, Cardiff University, Cardiff, United Kingdom; Institute of <strong>Cancer</strong> Genetics and<br />
Pharmacogenomics, Brunel University, Middlesex, Uxbridge, United Kingdom
SABCS Scholarship Recipients<br />
This year, 5 programs provided scholarships designed to promote the education and professional development of earlycareer<br />
scientists who are actively pursuing research in breast cancer by facilitating their attendance at SABCS. Scholarships<br />
were awarded to graduate students, medical students, residents, and clinical and postdoctoral fellows whose abstracts were<br />
accepted for presentation, based on the quality of the abstracts. This year’s awardees, by program, are:<br />
SABCS Clinical Scholars: For clinical scientists-in-training who are actively pursuing clinical or clinical/translational<br />
research in breast cancer.<br />
Young Kwang Chae Helen Heneghan Derek McHaffie<br />
Elizabeth Comen Catherine Kelly Erin Cobain<br />
Ghada Farhat Laura Kenny Huaying Liu<br />
Luca Fumagalli<br />
SABCS Basic Science Scholars: For laboratory-based investigators-in-training whose work focuses on the biology of<br />
breast cancer and preclinical models of its development and progression.<br />
Rachel Atkinson David Gyorki Cornelia Liedtke<br />
Kyle Covington Cameron Johnstone Beate Litzenburger<br />
Joan Garrett Alexandra Leary Ryan Hartmaier<br />
Ritwik Ghosh<br />
Avon Foundation-AACR International Scholars: For abstract presenters traveling from countries with emerging<br />
economies.<br />
Soo Ahn Mikiya Ishihara Yuri Urata<br />
Pablo Arrieta-Joffe Osvaldo Pontiggia Benlong Yang<br />
Mateus Barros Filho Mika Shirasu Jae Kyo Yi<br />
Pradeep Chaluvally-Raghavan A. Marcell Szasz Guochen Zhang<br />
Hirokuni Ikeda Satoru Tanaka<br />
AACR Translational Research Scholars, funded by Susan G. Komen for the Cure®: For presenters of highly related<br />
abstracts focused on translational breast cancer research.<br />
Phillipe Bedard Melanie Seal Dipika Misra<br />
Hui Gao Adel Tabchy Sarah Andres<br />
Michail Ignatiadis Rinat Yerushalmi Michal Mego<br />
Chann Lagadec Brent Rexer Amir Eitan<br />
Todd Miller Xing Li Mi-Ran Choi<br />
Ciara O’Brien Christina Yau Zhi Hu<br />
Esther Reijm Tracey Martin Karsten Pilones<br />
Dave Bhuvanesh Oleg Gluz Beatrix Elsberger<br />
AACR Minority Scholars, funded by Susan G. Komen for the Cure®: For abstract presenters working within<br />
the United States and within minority groups defined by the National <strong>Cancer</strong> Institute as being traditionally<br />
underrepresented in cancer and biomedical research.<br />
Mariana Chavez-MacGregor Kavitha Raj<br />
Laura Gonzalez-Malerva Cesar <strong>San</strong>chez<br />
11
12<br />
AACR Outstanding Investigator Award<br />
The AACR Outstanding Investigator Award for <strong>Breast</strong> <strong>Cancer</strong> Research is presented to an investigator no more than 50 years<br />
of age whose novel and significant work has had, or may have, a far-reaching impact on the etiology, detection, diagnosis,<br />
treatment, or prevention of breast cancer. This award, now in its second year, is funded by Susan G. Komen for the Cure®.<br />
Therapeutic Implications of the Molecular Portraits of <strong>Breast</strong> <strong>Cancer</strong><br />
Thursday, December 10, 11:30 am<br />
Charles Perou, PhD<br />
Lineberger <strong>Cancer</strong> Center, Chapel Hill, NC<br />
Charles Perou, PhD, is an Associate Professor of Genetics and Pathology & Laboratory Medicine at the University<br />
of North Carolina at Chapel Hill. Dr Perou is a member of the Lineberger Comprehensive <strong>Cancer</strong> Center, the<br />
Carolina Center for Genome Sciences, and the Scientific Director of the UNC Genomics and Bioinformatics<br />
Core Facility. He received his PhD in Cellular and Molecular Biology from the Department of Pathology at the<br />
University of Utah (1996) where he cloned and characterized the human Chediak-Higashi syndrome gene. He<br />
next performed his postdoctoral training in the laboratory of David Botstein at Stanford University (1997-2000)<br />
where he began his genomic studies of human tumors using DNA microarrays. These genomic analyses resulted<br />
in the identification of novel subtypes of human breast tumors that predict patient survival times and response<br />
to therapy. Dr Perou’s laboratory at UNC is focused on using genomics, genetics, and animal models to decipher<br />
the underlying biology of the molecular subtypes of breast cancer, and then using this biological information<br />
to develop therapies that are specifically targeted against each of these distinct subtypes of breast cancer. He has identified at least<br />
5 biologically distinct subtypes of breast tumor that are predictive of relapse, overall survival, and responsiveness to chemotherapy.<br />
Dr Perou will receive his award and present a lecture entitled Therapeutic Implications of the Molecular Portraits of <strong>Breast</strong> <strong>Cancer</strong><br />
this morning at 11:30 am.<br />
Brinker Awards Go to Researchers in Endocrine Therapy<br />
Susan G. Komen for the Cure® Brinker Awards for Scientific Distinction<br />
The Susan G. Komen for the Cure® Brinker Awards for Scientific Distinction are presented to basic and clinical researchers who<br />
have made seminal advances in the fight against breast cancer. This year, the Brinker Awards will be presented to 1 clinical<br />
researcher and 2 basic science researchers who have made significant contributions in the area of endocrine therapy.<br />
Understanding SERM Actions in <strong>Breast</strong> <strong>Cancer</strong><br />
Thursday, December 10, 4:30 pm<br />
Geoffrey L. Greene, PhD<br />
The University of Chicago, Chicago, IL<br />
Dr Green will receive an award for basic science research. Geoffrey L. Greene earned a PhD in chemistry<br />
from Northwestern University in 1974, and came to the University of Chicago the same year as a<br />
postdoctoral trainee in the Ben May Laboratory for <strong>Cancer</strong> Research. He joined the faculty as an assistant<br />
professor in 1980 and became a professor in 1991. Currently, Dr Greene is the Virginia and D.K. Ludwig<br />
Professor and associate director of the Ben May Department for <strong>Cancer</strong> Research, chair of the Committee<br />
on <strong>Cancer</strong> Biology, associate director of the <strong>Cancer</strong> Research Center, and co-director of the Ludwig Center<br />
for Metastasis Research at the University of Chicago. The overall goal of his research is to determine the<br />
molecular mechanisms by which female steroid hormones regulate development, differentiation, cellular<br />
proliferation, and survival in hormone-responsive tissues and cancers. Dr Greene has received a number<br />
of prestigious awards for his research contributions, and serves on several national committees, as well as<br />
journal editorial boards.
<strong>Issue</strong> 1, December 10, 2009<br />
Brinker Awards Go to Researchers in Endocrine Therapy<br />
Susan G. Komen for the Cure® Brinker Awards for Scientific Distinction (continued)<br />
Genomics of Estrogen Receptor Signaling in <strong>Breast</strong> <strong>Cancer</strong> and Endocrine Resistance<br />
Thursday, December 10, 4:45 pm<br />
Benita katzenellenbogen, PhD<br />
University of Illinois-Urbana Champaign, Urbana, IL<br />
Benita S. Katzenellenbogen, PhD, will also receive an award for basic science research.<br />
Dr Katzenellenbogen, PhD, is the Swanlund Professor of Molecular and Integrative Physiology,<br />
Cell and Developmental Biology at the University of Illinois Urbana-Champaign. She is a world expert<br />
on nuclear hormone receptors, especially on estrogen receptors and their actions in breast cancer.<br />
Her work has elucidated fundamental aspects of structure-function relationships and mechanisms of<br />
action of the estrogen receptors, and has provided a framework for the development of anti-hormonal<br />
treatments that are used in breast cancer treatment and prevention. Dr Katzenellenbogen has trained<br />
many young investigators who have gone on to successful careers, and she has served on many important<br />
committees and review panels and as President of the Endocrine Society from 2000-2001. Her research<br />
contributions have been recognized by multiple prestigious awards and honors from professional<br />
societies and foundations.<br />
Getting the Best Out of Neoadjuvant Therapy<br />
Thursday, December 10, 5:00 pm<br />
Professor Ian Smith<br />
Royal Marsden Hospital, London, United Kingdom<br />
Professor Ian Smith is Professor of <strong>Cancer</strong> Medicine at the Institute of <strong>Cancer</strong> Research and the Royal<br />
Marsden Hospital, London, where he is also the Head of the <strong>Breast</strong> Unit. His principal research interests<br />
have been in the biology and treatment of breast cancer and lung cancer, and in new drug development. He<br />
was involved in the early clinical development of several successful anti-cancer drugs, including letrozole<br />
and carboplatin. One of his main interests is in neoadjuvant and short-term preoperative treatments<br />
and in the molecular changes associated with these therapies. He is Chief Investigator of 2 international<br />
neoadjuvant endocrine therapy trials, IMPACT and IRESSA 223, and the UK Principal Investigator for<br />
several international multicenter adjuvant trials, including HERA (trastuzumab), BIG1-98 (letrozole), and<br />
ALTTO (lapatinib). He is the first chairman of the recently formed UK <strong>Breast</strong> Trials Intergroup and recent<br />
past chairman of the British <strong>Breast</strong> Group. He has also been Chairman of several national professional<br />
bodies, including the Association of the <strong>Cancer</strong> Physicians, the Royal College of Physicians Specialist Advisory Committee for<br />
Medical Oncology, and the NCRI Lung <strong>Cancer</strong> Clinical Studies Group. He is a member of numerous international cancer societies<br />
and has over 300 peer-reviewed publications.<br />
13
14<br />
Plenary Lectures to Address Epidemiology,<br />
Molecular Biology, Immunology<br />
Each day of the SABCS traditionally begins with a plenary lecture featuring a world-renowned researcher presenting a<br />
definitive update on his or her field of interest. This year is no exception, with invited speakers who offer a very good reason<br />
to get up early each morning.<br />
On Thursday morning at 8:45 am, Valerie Beral, MD, will speak on An Epidemiological Perspective on the Causes and Prevention<br />
of <strong>Breast</strong> <strong>Cancer</strong>. Dr Beral is the director of the <strong>Cancer</strong> Epidemiology Unit and a professor of epidemiology at the University<br />
of Oxford. Her research has focused on the role of reproductive, hormonal, and infectious agents in cancer. She is principal<br />
investigator for the Million Women Study, the largest study in the world investigating how a woman’s reproductive history can<br />
affect her health.<br />
On Friday at 9:00 am, William Sellers, MD, will discuss the role of the PI3K/Akt/mTOR pathway in cancer. Dr Sellers is currently<br />
the vice president and global head of oncology for the Novartis Institute of BioMedical Research in Cambridge, Massachusetts.<br />
mTOR is a cytoplasmic protein kinase that acts as a central regulator in cell proliferation, angiogenesis, and cell metabolism. It<br />
represents an exciting potential therapeutic target because it is a key intracellular point of convergence for many important<br />
signaling pathways located upstream from it. These pathways can be activated by various signaling proteins, including cell surface<br />
growth factor receptors such as VEGFR, a number of which are abnormally activated in cancer.<br />
Tyler Curiel, MD, will speak on Saturday at 9:00 am, assessing new paradigms in cancer immunology. Dr Curiel is the former<br />
executive director of the <strong>Cancer</strong> Therapy & Research Center at the University of Texas Health Science Center at <strong>San</strong> <strong>Antonio</strong>.<br />
In a landmark paper published in Nature Medicine in 2004, Dr Curiel and his team made the first definitive identification<br />
of an “off switch” in human cancer, the specific recruitment of regulatory T cells to mediate the suppression of tumorassociated<br />
antigen-reactive lymphocytes. He is considered one of the leading researchers in the study of immunopathological<br />
mechanisms in human cancer.
<strong>Issue</strong> 1, December 10, 2009<br />
Supporters<br />
We are proud to acknowledge the following for their contributions to and generous support of<br />
our program (at press time).<br />
ANGEL PLUS<br />
Abraxis Bioscience<br />
Genentech BioOncology<br />
GlaxoSmithKline<br />
Lilly USA, LLC<br />
Novartis Oncology<br />
sanofi-aventis<br />
ANGEL<br />
Genomic Health, Inc.<br />
Pfizer<br />
PATRON PLUS<br />
Amgen<br />
AstraZeneca<br />
Bristol-Myers Squibb<br />
Merck Oncology<br />
MAJOR SUPPORTER PLUS<br />
Wyeth Pharmaceuticals<br />
MAJOR SUPPORTER<br />
Monogram Biosciences<br />
Onyx<br />
CONTRIBUTOR<br />
bioTheranostics, Inc.<br />
Carl Zeiss Meditec, Inc.<br />
Eisai, Inc.<br />
EMD Serono<br />
Halo <strong>Breast</strong> Pap Test (Neomatrix)<br />
HistoRx<br />
Imclone Systems<br />
IOS Press<br />
CONTRIBUTOR (continued)<br />
Ipsogen<br />
Myriad Genetic Laboratories, Inc.<br />
Research To Practice<br />
SenoRx<br />
Ventana Medical Systems, Inc.<br />
A Member of the Roche Group<br />
DONOR<br />
Agendia, Inc.<br />
American Express OPEN<br />
AmeriPath, Inc.<br />
Amoena USA Corporation<br />
Aurora Imaging Technology, Inc.<br />
Biocare Medical<br />
Biopsy Sciences<br />
Caris Diagnostics<br />
Clarient, Inc.<br />
Clinical Care Options<br />
Clinical Oncology News<br />
Combimatrix Molecular Diagnostics<br />
CuraScript<br />
CVS Caremark/CarePlus<br />
Cytori Therapeutics, Inc.<br />
Dako North America, Inc.<br />
deCODE genetics<br />
Diplomat Specialty Pharmacy<br />
DXS Ltd<br />
Endomagnetics Ltd<br />
Faxitron X-Ray LLC<br />
Gamma Medica-Ideas<br />
Hologic<br />
ImpediMed, Inc<br />
Informed Medical Decisions, Inc.<br />
SABCS gratefully acknowledges Susan G. Komen for the Cure® for generous support of AACR Outstanding Investigator Award for<br />
<strong>Breast</strong> <strong>Cancer</strong> Research , CTCR-AACR <strong>San</strong> <strong>Antonio</strong> <strong>Breast</strong> <strong>Cancer</strong> <strong>Symposium</strong> Educational Sessions, AACR Translational Research<br />
Scholars, and Minority Scholar Awards for <strong>Breast</strong> <strong>Cancer</strong> Research.<br />
SABCS wishes to thank Avon Foundation for support of the Avon Foundation-AACR International<br />
Scholar-In-Training Grants.<br />
DONOR (continued)<br />
IntraOp Medical Corporation<br />
Leica Microsystems<br />
Lippincott Williams & Wilkins<br />
Medtronic<br />
Milestone<br />
Onco Inc.<br />
Patient Advocate Foundation<br />
PhenoPath Laboratories, PLLC<br />
Physicians’ Education Resource<br />
PRIME Oncology<br />
R&D Systems, Inc.<br />
RadPharm, Inc.<br />
Siemens Healthcare Diagnostics<br />
Springer<br />
Sysmex America, Inc.<br />
US Labs<br />
US Oncology<br />
Varian Medical Systems<br />
Xceed Molecular<br />
CONFERENCE GRANTS<br />
American <strong>Cancer</strong> Society, Texas Division<br />
National <strong>Cancer</strong> Institute<br />
SERvICE IN kIND<br />
Adjuvant, Inc.<br />
AlphaMed Press/The Oncologist<br />
Elsevier<br />
Inter-American <strong>Breast</strong> <strong>Cancer</strong> Conference<br />
The Oncology Group<br />
15
Contributing Faculty Editor:<br />
Gary C. Chamness, PhD<br />
This newsletter is made possible with support from<br />
Abraxis BioScience<br />
The 2009 <strong>San</strong> <strong>Antonio</strong> <strong>Breast</strong> <strong>Cancer</strong> <strong>Symposium</strong><br />
(SABCS) is presented by the CTRC, AACR, and the<br />
Baylor College of Medicine. The driving force behind<br />
this collaboration is the shared mission of the organizations<br />
to advance progress against breast cancer.<br />
By combining their respective strengths, the <strong>San</strong><br />
<strong>Antonio</strong> <strong>Breast</strong> <strong>Cancer</strong> <strong>Symposium</strong> encompasses<br />
the full spectrum of breast cancer research and facilitates<br />
the rapid transition of new knowledge into<br />
improved care for breast cancer patients.<br />
<strong>Issue</strong> 1, December 10, 2009<br />
Exhibitors<br />
The following information was received too late for inclusion in the SABCS<br />
Pocket Program.<br />
Exhibitors Added<br />
Clinical Oncology News .................................259<br />
IOS Press .................................................................456<br />
Patient Advocate Foundation ....................442<br />
Exhibitor Correction<br />
Lilly Oncology ............................................300/308<br />
Lilly .............................................................................309<br />
Created by:<br />
M2 Communications, Inc.<br />
10524 Moss Park Road<br />
Suite 204-310<br />
Orlando, FL 32832