Issue 1 - San Antonio Breast Cancer Symposium
Issue 1 - San Antonio Breast Cancer Symposium
Issue 1 - San Antonio Breast Cancer Symposium
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
6<br />
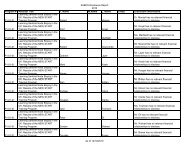
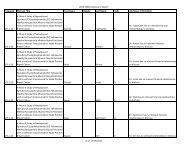
Revised Abstracts<br />
Revisions of the following abstracts were received and accepted too late for inclusion in the SABCS abstract book. They will<br />
be published in the January issue of <strong>Cancer</strong> Research.<br />
Abstract 41<br />
Final overall survival (OS) results from the randomized, double-blind, placebo-controlled, phase 3 AvADO study of<br />
bevacizumab (Bv) plus docetaxel (D) compared with placebo (PL) plus D for the first-line treatment of locally recurrent<br />
(LR) or metastatic breast cancer (mBC)<br />
Miles DW, Chan A, Romieu G, Dirix LY, Cortés J, Pivot X, Tomczak P, Juozaityte E, Harbeck N, Steger GG, the BO17708 study<br />
group. Mount Vernon <strong>Cancer</strong> Centre, Middlesex, United Kingdom; Mount Hospital, Mount <strong>Breast</strong> Group, Perth, Australia; CRLCC Val<br />
d’Aurelle, P. Lamarque Service Chimioimmunotherapie, Montpellier, France; Algemeen Ziekenhuis St. Augustinus, Wilrijk, Belgium;<br />
University Hospital Vall d’Hebron Oncology, Barcelona, Spain; University Hospital of Besancon, France; Klinika Onkologii Oddzial<br />
Chemioterapii, Poznań, Poland; Kaunas Medical University Hospital, Oncology Clinic, Kaunas, Lithuania; <strong>Breast</strong> Centre, University of<br />
Cologne, Cologne, Germany; Medical University of Vienna, Department of Internal Medicine I-Oncology, Vienna, Austria<br />
Background: Anti-VEGF monoclonal antibody BV significantly improves efficacy in combination with standard therapies in<br />
multiple tumor types, with limited impact on toxicity. Three randomized phase 3 trials (E2100, AVADO, and RIBBON-1) in mBC<br />
have demonstrated that BV + 1st-line chemotherapy (CTx) significantly improves progression-free survival (PFS) and overall<br />
response rates (ORR). We present mature OS data from AVADO.<br />
Methods: Patients (pts) with HER2-negative LR/mBC were randomized to D 100 mg/m 2 + PL, D + BV 7.5 mg/kg or D + BV 15 mg/kg.<br />
D was given q3w for ≤9 cycles. BV or PL was given q3w until disease progression/unacceptable toxicity. After progression, pts were<br />
offered BV with 2nd-line anticancer therapy in a post-study treatment phase. The primary endpoint was PFS; secondary endpoints<br />
included OS, time to treatment failure, ORR, duration of response and safety. An exploratory analysis conducted in pts receiving<br />
post-progression CTx compared OS in pts receiving 2nd-line BV with those who did not.<br />
Results: 736 pts were enrolled March 2006–April 2007. The primary analysis (data cut-off October 2007; median follow-up 10.2<br />
months) showed significant improvements in PFS and ORR for both BV-containing arms compared with PL + D. Mature OS data<br />
(data cut-off April 2009; median follow-up 25 months) are shown (Table). There was no difference in median OS between the<br />
study arms (range 30–32 months). Recognizing the limitations of the non-randomized comparison in exploratory analyses, results<br />
suggest that use of BV with 2nd-line therapy is a possible reason for lack of OS difference. Updated PFS and ORR were superior for<br />
the 15 mg/kg BV arm compared with PL + D. Results for the 7.5 mg/kg BV arm also indicated a less pronounced treatment benefit.<br />
BV had limited impact on the safety profile of docetaxel. Increased SAEs in the 15 mg/kg BV arm may be due to more pts receiving<br />
9 cycles of D than in the PL arm (51% vs 42%).<br />
Conclusions: There was no difference in OS between study arms. Exploratory analyses suggest that use of 2nd-line BV with CTx<br />
may influence OS. These mature data confirm the improvement in PFS and ORR with BV 15 mg/kg combined with D compared<br />
with PL + D.