Implementing A Framework for Maternity ... - Scottish Government
Implementing A Framework for Maternity ... - Scottish Government
Implementing A Framework for Maternity ... - Scottish Government
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
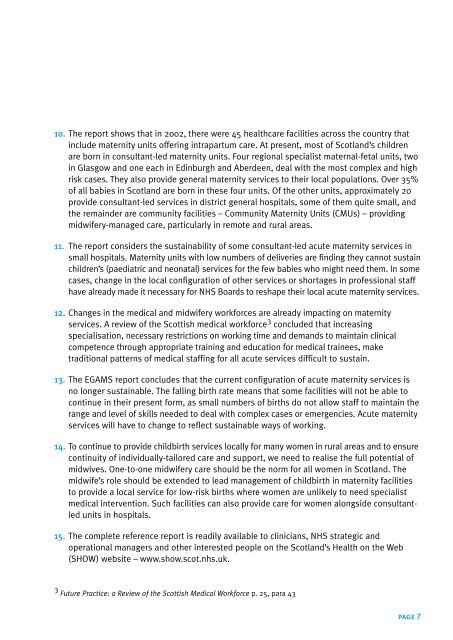
10. The report shows that in 2002, there were 45 healthcare facilities across the country that<br />
include maternity units offering intrapartum care. At present, most of Scotland’s children<br />
are born in consultant-led maternity units. Four regional specialist maternal-fetal units, two<br />
in Glasgow and one each in Edinburgh and Aberdeen, deal with the most complex and high<br />
risk cases. They also provide general maternity services to their local populations. Over 35%<br />
of all babies in Scotland are born in these four units. Of the other units, approximately 20<br />
provide consultant-led services in district general hospitals, some of them quite small, and<br />
the remainder are community facilities – Community <strong>Maternity</strong> Units (CMUs) – providing<br />
midwifery-managed care, particularly in remote and rural areas.<br />
11. The report considers the sustainability of some consultant-led acute maternity services in<br />
small hospitals. <strong>Maternity</strong> units with low numbers of deliveries are finding they cannot sustain<br />
children’s (paediatric and neonatal) services <strong>for</strong> the few babies who might need them. In some<br />
cases, change in the local configuration of other services or shortages in professional staff<br />
have already made it necessary <strong>for</strong> NHS Boards to reshape their local acute maternity services.<br />
12. Changes in the medical and midwifery work<strong>for</strong>ces are already impacting on maternity<br />
services. A review of the <strong>Scottish</strong> medical work<strong>for</strong>ce 3 concluded that increasing<br />
specialisation, necessary restrictions on working time and demands to maintain clinical<br />
competence through appropriate training and education <strong>for</strong> medical trainees, make<br />
traditional patterns of medical staffing <strong>for</strong> all acute services difficult to sustain.<br />
13. The EGAMS report concludes that the current configuration of acute maternity services is<br />
no longer sustainable. The falling birth rate means that some facilities will not be able to<br />
continue in their present <strong>for</strong>m, as small numbers of births do not allow staff to maintain the<br />
range and level of skills needed to deal with complex cases or emergencies. Acute maternity<br />
services will have to change to reflect sustainable ways of working.<br />
14. To continue to provide childbirth services locally <strong>for</strong> many women in rural areas and to ensure<br />
continuity of individually-tailored care and support, we need to realise the full potential of<br />
midwives. One-to-one midwifery care should be the norm <strong>for</strong> all women in Scotland. The<br />
midwife’s role should be extended to lead management of childbirth in maternity facilities<br />
to provide a local service <strong>for</strong> low-risk births where women are unlikely to need specialist<br />
medical intervention. Such facilities can also provide care <strong>for</strong> women alongside consultantled<br />
units in hospitals.<br />
15. The complete reference report is readily available to clinicians, NHS strategic and<br />
operational managers and other interested people on the Scotland’s Health on the Web<br />
(SHOW) website – www.show.scot.nhs.uk.<br />
3 Future Practice: a Review of the <strong>Scottish</strong> Medical Work<strong>for</strong>ce p. 25, para 43<br />
page 7