Hematology - ION Solutions
Hematology - ION Solutions
Hematology - ION Solutions
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
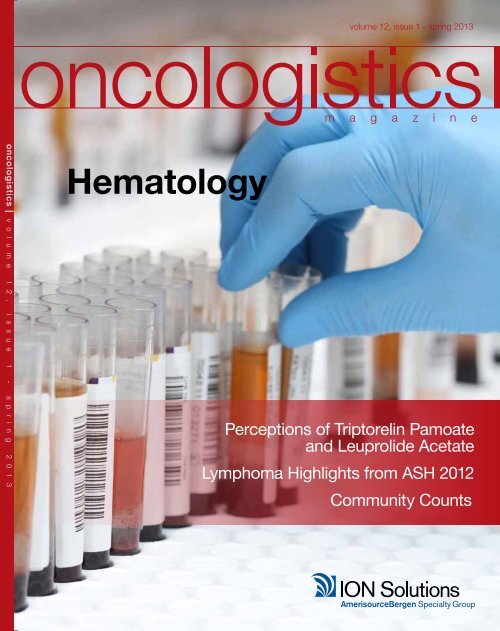
volume 12, issue 1 - spring 2013<br />
oncologistics | v o l u m e 1 2 , i s s u e 1 - s p r i n g 2 0 1 3<br />
<strong>Hematology</strong><br />
Perceptions of Triptorelin Pamoate<br />
and Leuprolide Acetate<br />
Lymphoma Highlights from ASH 2012<br />
Community Counts
oncologistics volume 12, issue 1 - spring 2013<br />
table of contents spring 2013<br />
02<br />
14<br />
34<br />
42<br />
Industry Insight:<br />
Millennium’s Mission in Oncology<br />
By: Melissa Bradbury<br />
Drug Update:<br />
Levo-leucovorin in Colon Cancer<br />
By: Sam E. Mikhail, M.D. and<br />
John Marshall, M.D.<br />
Reimbursement Watch:<br />
New Payment Models in Healthcare Delivery<br />
By: Sara Fernandez, PhD<br />
The Physician-Payer Relationship: Using<br />
Data to Drive the Future Of Oncology Care<br />
By: Barry Fortner, PhD<br />
editorial & design staff:<br />
> Chris Vorce<br />
Director, Marketing & Communications, <strong>ION</strong> <strong>Solutions</strong><br />
> Melissa Bradbury<br />
Manager, Marketing & Communications, <strong>ION</strong> <strong>Solutions</strong><br />
> Amy Migliore<br />
Graphic Designer, Marketing & Communications,<br />
<strong>ION</strong> <strong>Solutions</strong><br />
article and advertising submissions:<br />
Article submissions and suggestions, as well as<br />
advertising inquiries, may be sent to:<br />
Chris Vorce<br />
Managing Editor, Oncologistics<br />
c/o <strong>ION</strong> <strong>Solutions</strong><br />
3101 Gaylord Parkway<br />
Frisco, TX 75034<br />
or by e-mail: chris.vorce@iononline.com<br />
Information presented in Oncologistics is not intended as a substitute<br />
for the personalized advice given by a healthcare provider. The<br />
opinions expressed on the pages of Oncologistics magazine are<br />
those of the authors and do not necessarily reflect the views of<br />
<strong>ION</strong> <strong>Solutions</strong> or AmerisourceBergen Specialty Group. Although<br />
Oncologistics strives to present only current and accurate information,<br />
readers should not consider it as professional advice or endorsement<br />
of any position. Although great care has been taken in compiling and<br />
checking the information given in this publication to ensure accuracy,<br />
the authors, <strong>ION</strong> <strong>Solutions</strong>, and its employees or agents shall not<br />
be responsible or in any way liable for the continued currency of<br />
the information or for any errors, omissions, or inaccuracies in this<br />
magazine, whether arising from negligence or otherwise or for any<br />
consequence arising therefrom. The staff of Oncologistics provides<br />
columns and other editorial support. In no way are they responsible<br />
for the specific views presented in Oncologistics. Oncologistics<br />
magazine is published by <strong>ION</strong> <strong>Solutions</strong>, an AmerisourceBergen<br />
Specialty Group company.<br />
All archived issues of Oncologistics are available online<br />
at www.iononline.com.
oncologistics volume 12, issue 1 - spring 2013<br />
table of contents spring 2013<br />
04<br />
18<br />
30<br />
36<br />
Drug Update:<br />
Patient and Clinician Perceptions of<br />
Triptorelin Pamoate and Leuprolide Acetate<br />
in Patients With Advanced Prostate Cancer<br />
By: Neal D. Shore, MD, FACS, Paul Sieber,<br />
MD, FACS, Leanne Schimke, MSN, CRNP,<br />
FNP-C, CUNP, Adam Perzin, MD, Scott<br />
Olsen, MPH<br />
Industry Insight:<br />
Why Community Counts<br />
By: Chris Vorce<br />
Industry Insight:<br />
Lymphoma Review: Selected Highlights<br />
from ASH 2012<br />
By: Michael E. Williams, MD, ScM<br />
Reimbursement Watch:<br />
Getting Ready For Health Insurance<br />
Exchanges<br />
By: Zachary Bridges<br />
editorial & design staff:<br />
> Chris Vorce<br />
Director, Marketing & Communications, <strong>ION</strong> <strong>Solutions</strong><br />
> Melissa Bradbury<br />
Manager, Marketing & Communications, <strong>ION</strong> <strong>Solutions</strong><br />
> Amy Migliore<br />
Graphic Designer, Marketing & Communications,<br />
<strong>ION</strong> <strong>Solutions</strong><br />
article and advertising submissions:<br />
Article submissions and suggestions, as well as<br />
advertising inquiries, may be sent to:<br />
Chris Vorce<br />
Managing Editor, Oncologistics<br />
c/o <strong>ION</strong> <strong>Solutions</strong><br />
3101 Gaylord Parkway<br />
Frisco, TX 75034<br />
or by e-mail: chris.vorce@iononline.com<br />
oncologistics volume 12, issue 1 - spring 2013 2<br />
Information presented in Oncologistics is not intended as a substitute<br />
for the personalized advice given by a healthcare provider. The<br />
opinions expressed on the pages of Oncologistics magazine are<br />
those of the authors and do not necessarily reflect the views of<br />
<strong>ION</strong> <strong>Solutions</strong> or AmerisourceBergen Specialty Group. Although<br />
Oncologistics strives to present only current and accurate information,<br />
readers should not consider it as professional advice or endorsement<br />
of any position. Although great care has been taken in compiling and<br />
checking the information given in this publication to ensure accuracy,<br />
the authors, <strong>ION</strong> <strong>Solutions</strong>, and its employees or agents shall not<br />
be responsible or in any way liable for the continued currency of<br />
the information or for any errors, omissions, or inaccuracies in this<br />
magazine, whether arising from negligence or otherwise or for any<br />
consequence arising therefrom. The staff of Oncologistics provides<br />
columns and other editorial support. In no way are they responsible<br />
for the specific views presented in Oncologistics. Oncologistics<br />
magazine is published by <strong>ION</strong> <strong>Solutions</strong>, an AmerisourceBergen<br />
Specialty Group company.<br />
All archived issues of Oncologistics are available online<br />
at www.iononline.com.<br />
oncologistics 3
drug update<br />
PATIENT and CLINICIAN<br />
PERCEPT<strong>ION</strong>S of TRIPTORELIN<br />
PAMOATE and LEUPROLIDE<br />
ACETATE in PATIENTS WITH<br />
Advanced PROSTATE CANCER<br />
oncologistics drug update<br />
THE incidence of<br />
PROSTATE cancer<br />
HAS been decreasing<br />
SINCE 2004 in men aged<br />
≥65 yEARS, but has<br />
REMAINED stable in<br />
MEN aged
drug update<br />
oncologistics drug update<br />
THE study protocol was approved by an institutional<br />
REVIEW board and conducted in accordance with<br />
GOOD CLINICAL PRACTICE and all applicable codes<br />
AND regulations.<br />
oncologistics volume 12, issue 1 - spring 2013 6<br />
regarding specific tolerability issues with different<br />
GnRH agonists. This study compares patients’ as well<br />
as clinicians’ perceptions of injection site tolerability<br />
following the IM injection of triptorelin pamoate or SC<br />
injection of leuprolide acetate.<br />
Methods<br />
Patients<br />
Male patients aged ≥18 years with a diagnosis of<br />
advanced prostate cancer for whom treatment with<br />
triptorelin IM or leuprolide SC is indicated were included.<br />
Patients had to have a life expectancy of ≥1 year and<br />
had to be capable of completing study questionnaires<br />
without assistance. Patients with a history of alcohol<br />
or drug abuse within the past year, patients who<br />
required concomitant medications that could affect<br />
study assessments (eg, topical medications used for<br />
pretreatment of injection site pain), and patients with<br />
known hypersensitivity to GnRH or luteinizing hormonerelease<br />
hormone (LHRH) agonists were excluded from<br />
the study.<br />
Study Design and Treatments<br />
This multicenter, randomized, crossover, open-label<br />
study (NCT01161563) consisted of two study periods.<br />
During the first study period, patients were randomized<br />
1:1 to receive a single injection of triptorelin pamoate<br />
22.5 mg mixed with 2 mL sterile water administered<br />
intramuscularly in either buttock or leuprolide acetate<br />
45 mg mixed liquid in a prefilled delivery system<br />
administered subcutaneously in the upper- or midabdominal<br />
area. Block randomization was used to<br />
ensure equal distribution among study centers. During<br />
study period 2, 24 to 26 weeks after the Period 1 clinic<br />
visits, patients crossed over and received the alternate<br />
treatment. Pretreatment of the injection site with topical<br />
anesthetic or analgesic agents was not permitted.<br />
The study protocol was approved by an institutional<br />
review board and conducted in accordance with<br />
Good Clinical Practice and all applicable codes and<br />
regulations. Written informed consent was obtained<br />
from each patient before any study procedure was<br />
initiated.<br />
Patient Perceptions<br />
Questionnaires assessing patient perceptions were<br />
administered 10 to 15 minutes after each injection. The<br />
primary assessment was patient bother from injection<br />
site burning and/or stinging, which was assessed on a<br />
Visual Analog Scale (VAS) from 0 (not bothered at all)<br />
to 10 (extremely bothered). Secondary assessments<br />
included patient bother from each of the following<br />
potential injection site effects: soreness, redness,<br />
bruising, itching, hardening, and swelling. These<br />
assessments also were done on VAS from 0 to 10.<br />
Other patient perceptions were assessed, including:<br />
discomfort experienced (0 [no discomfort] to 10 [worst<br />
discomfort]); anxiety prior to receiving the injection (0<br />
[not at all anxious] to 10 [extremely anxious]); anxiety<br />
about receiving another injection with the same<br />
product (0 [not at all anxious] to 10 [extremely anxious]);<br />
and overall satisfaction with injection experience (0<br />
[completely satisfied] to 10 [not satisfied at all]).<br />
Clinician Perceptions<br />
The clinician who prepared and administered the<br />
medications completed the questionnaire assessing<br />
clinician perceptions after each injection. Clinician<br />
satisfaction with the following aspects of the<br />
medications were assessed on a VAS from 0 (strongly<br />
oncologistics 7
drug update<br />
oncologistics drug update<br />
Table 1: Demographic and Physical Characteristics at Baseline (Per-Protocol Population)<br />
oncologistics volume 12, issue 1 - spring 2013 8<br />
agree) to 10 (strongly disagree): convenience of product<br />
to store prior to administration; simplicity and ease of<br />
understanding the instructions; ease in identifying the<br />
components of the injection device; time required to<br />
set up for the injection was reasonable for the method<br />
of administration; ease in preparing the device prior to<br />
injection; ease in mixing the product using the device;<br />
ease in drawing the product into the syringe and<br />
attaching the needle; time required to prepare product<br />
was reasonable for the method of administration; ease in<br />
injecting the product; feeling protected from accidental<br />
needle sticks following the product administration; and the<br />
time required to administer the product was reasonable<br />
for the method of administration.<br />
Other caregiver assessments included: distress the<br />
patient experienced associated with this injection (0 [no<br />
distress at all] to 10 [extremely distressed]) and overall<br />
satisfaction with injection experience (0 [completely<br />
satisfied] to 10 [not satisfied at all]).<br />
Adverse Events<br />
Adverse events (AEs) were assessed for each study<br />
period for 24 hours after administration of study<br />
medication. An AE was defined as any undesirable<br />
medical event occurring to a patient, regardless of<br />
whether the event was related or unrelated to the study<br />
medication. Exacerbation of a pre-existing medical<br />
condition also was considered an AE.<br />
Statistical Analysis<br />
The study population included all patients who received<br />
injections of both study medications and answered<br />
the primary assessment question on the patient<br />
questionnaires following both study injections. The<br />
clinician population included all study site clinicians<br />
who administered at least 1 injection and completed at<br />
least 1 clinician impression questionnaire. All patients<br />
who received at least 1 dose of study medication were<br />
included in the safety analyses.<br />
It was estimated that a sample size of 81 patients per<br />
treatment group was necessary to provide 90% power to<br />
detect a difference between the groups. In a crossover<br />
study, this means that 81 patients had to complete both<br />
treatments (triptorelin pamoate/leuprolide acetate). The<br />
target was a total of 100 patients enrolled to have at<br />
least 80 who would complete the study. All statistical<br />
comparisons for patient perceptions were conducted<br />
as two-sided tests, with p ≤ 0.05 considered statistically<br />
significant. Primary and secondary assessments were<br />
analyzed using an analysis of variance (ANOVA) model,<br />
adjusting for sequence, patient within sequence, period,<br />
and treatment. Clinician perception and safety data are<br />
summarized descriptively.<br />
results<br />
Patients<br />
A total of 118 patients were randomized, with 63<br />
randomized to receive triptorelin IM first and 55 to receive<br />
leuprolide SC first. Of the 107 patients who completed<br />
the study, 58 patients received triptorelin IM first and 49<br />
patients received leuprolide SC first. Demographic and<br />
physical characteristics of patients at baseline generally<br />
were similar between the two groups (Table 1).<br />
Patient Perceptions<br />
Patients reported significantly less post-injection burning<br />
and/or stinging with triptorelin IM than with leuprolide SC<br />
(p < 0.0001; Figure 1). In addition, significantly less postinjection<br />
soreness and less discomfort was reported with<br />
triptorelin IM than with leuprolide SC (both p < 0.0001;<br />
Figure 2). Results from other secondary assessments are<br />
reported in Table 2. Triptorelin IM versus leuprolide SC<br />
was associated with significantly less bother by redness,<br />
itching, and hardening (p ≤ 0.04), numerically less bother<br />
from bruising and swelling, and significantly greater<br />
satisfaction with overall injection experience (p = 0.0009).<br />
Significantly more anxiety prior to injection (p = 0.0271)<br />
and significantly more anxiety about a future injection<br />
with the same product (p = 0.0006) were reported with<br />
leuprolide SC than with triptorelin IM.<br />
Clinician Perceptions<br />
Clinicians reported less patient distress with triptorelin<br />
IM versus leuprolide SC (Figure 3). Clinicians also<br />
reported greater overall satisfaction with triptorelin IM<br />
Characteristic<br />
Age, y<br />
Mean (SD)<br />
Range<br />
Race, n (%)<br />
White<br />
African American<br />
Asian<br />
American Indian/Alaska Native<br />
Native Hawaiian/Pacific Islander<br />
Ethnicity, n (%)<br />
Hispanic or Latino<br />
Not Hispanic or Latino<br />
Previous GnRH therapy, n (%)<br />
Leuprolide (IM)<br />
Leuprolide (SC)<br />
Triptorelin<br />
Triptorelin First<br />
(n=58)<br />
73.2 (9.6)<br />
57-91<br />
44 (76)<br />
12 (21)<br />
1 (2)<br />
1 (2)<br />
0<br />
2 (3)<br />
56 (97)<br />
38 (66)<br />
9 (16)<br />
22 (38)<br />
7 (12)<br />
Leuprolide First<br />
(n=49)<br />
75.0 (9.6)<br />
56-91<br />
38 (78)<br />
10 (20)<br />
0<br />
0<br />
1 (2)<br />
3 (6)<br />
46 (94)<br />
31 (63)<br />
9 (18)<br />
18 (37)<br />
4 (8)<br />
Overall<br />
(N=107)<br />
74.0 (9.7)<br />
56-91<br />
82 (77)<br />
22 (21)<br />
1 (1)<br />
1 (1)<br />
1 (1)<br />
5 (5)<br />
102 (95)<br />
69 (64)<br />
18 (17)<br />
40 (37)<br />
11 (10)<br />
Height, cm<br />
Mean (SD) 176.9 (7.6) 174.8 (7.2) 175.9 (7.5)<br />
Weight, kg<br />
Mean (SD)<br />
Range<br />
89.5 (17.6)<br />
57.6–163<br />
89.9 (22.8)<br />
49.1–165<br />
––<br />
Notes: GnRH = gonadotropin-releasing hormone, IM = intramuscular, SC = subcutaneous.<br />
Figure 1. Figure 2.<br />
How much were you bothered by burning and/or stinging How much discomfort did you<br />
experience from the injection<br />
Leuprolide<br />
Triptorelin<br />
Not bothered<br />
at all<br />
VAS Score<br />
Extremely<br />
bothered<br />
0 20 40 60 80 100<br />
Adjusted mean score indicating how much<br />
patients were bothered by burning and/or<br />
stinging on a VAS.<br />
Leuprolide<br />
Triptorelin<br />
No<br />
discomfort<br />
Worst<br />
discomfort<br />
0 20 40 60 80 100<br />
VAS Score<br />
89.7 (20.0)<br />
49.1–165<br />
How much were you bothered by soreness<br />
Leuprolide<br />
Triptorelin<br />
Not<br />
bothered<br />
at all<br />
Extremely<br />
bothered<br />
0 20 40 60 80 100<br />
VAS Score<br />
Adjusted mean scores indicating how much patients were bothered<br />
by soreness and how much discomfort patients experienced from the<br />
injection on a VAS.<br />
oncologistics 9
drug update<br />
oncologistics drug update<br />
Figure 3.<br />
In your opinion, how much distress do<br />
you think you patient experienced<br />
associated with this injection<br />
How satisfied are you overall with the<br />
injection experience<br />
Figure 4.<br />
I felt protected from accidental needle<br />
stickes following product administration<br />
The injection of the product was easy<br />
Leuprolide<br />
Leuprolide<br />
Leuprolide<br />
Leuprolide<br />
Triptorelin<br />
Triptorelin<br />
Triptorelin<br />
Triptorelin<br />
No distress<br />
at all<br />
Extremely<br />
distressed<br />
0 20 40 60 80 100<br />
VAS Score<br />
Completely<br />
satisfied<br />
Not satisfied<br />
at all<br />
0 20 40 60 80 100<br />
VAS Score<br />
Mean scores indicating how much distress<br />
clinicians thought patient experienced<br />
associated with the injection and clinicians’<br />
overall satisfaction with the injection<br />
experience on a VAS.<br />
Strongly<br />
agree<br />
Strongly<br />
disagree<br />
0 20 40 60 80 100<br />
VAS Score<br />
Strongly<br />
agree<br />
Strongly<br />
disagree<br />
0 20 40 60 80 100<br />
VAS Score<br />
Mean scores indicating clinicians’<br />
satisfaction with the injection process<br />
and device disposal on the VAS.<br />
Table 2: Results From Secondary Assessments of Patient Perceptions<br />
oncologistics volume 12, issue 1 - spring 2013 10<br />
Characteristic<br />
Bother from redness<br />
Adjusted mean (95% CI)<br />
Range<br />
Bother from bruising<br />
Adjusted mean (95% CI)<br />
Range<br />
Bother from itching<br />
Adjusted mean (95% CI)<br />
Range<br />
Bother from hardening<br />
Adjusted mean (95% CI)<br />
Range<br />
Bother from swelling<br />
Adjusted mean (95% CI)<br />
Range<br />
Anxiety prior to injection<br />
Adjusted mean (95% CI)<br />
Range<br />
Anxiety post-injection*<br />
Adjusted mean (95% CI)<br />
Range<br />
Dissatisfaction with overall<br />
injection experience<br />
Adjusted mean (95% CI)<br />
Range<br />
Triptorelin Injection<br />
(n=107)<br />
3.39 (1.57–5.22)<br />
0–28<br />
2.95 (1.12–4.77)<br />
0–31<br />
2.70 (1.49–3.91)<br />
0–17<br />
3.47 (1.62–5.31)<br />
0–34<br />
3.04 (1.41–4.68)<br />
0–18<br />
12.42 (7.38–17.46)<br />
0–99<br />
6.65 (2.11–11.19)<br />
0–94<br />
5.21 (1.47–8.96)<br />
0–91<br />
––<br />
*Anxiety post-injection about getting another injection with the same product.<br />
Leuprolide Injection<br />
(n=107)<br />
6.26 (4.43–8.09)<br />
0–87<br />
4.90 (3.08–6.73)<br />
0–96<br />
5.14 (3.93–6.34)<br />
0–47<br />
6.16 (4.31–8.00)<br />
0–99<br />
5.01 (3.37–6.64)<br />
0–98<br />
19.05 (14.00–24.09)<br />
0–100<br />
17.27 (12.73–12.81)<br />
0–100<br />
13.44 (9.70–17.19)<br />
0–100<br />
Difference<br />
2.87 (0.28–5.45)<br />
p = 0.0302<br />
1.96 (-0.61–4.52)<br />
p = 0.1331<br />
2.43 (0.74–4.13)<br />
p = 0.0052<br />
2.69 (12.60–23.46)<br />
p = 0.0386<br />
1.96 (-0.29–4.21)<br />
p = 0.0869<br />
6.62 (0.76–12.48)<br />
p = 0.0271<br />
10.62 (4.68–16.56)<br />
p = 0.0006<br />
8.23 (3.47–12.99)<br />
p = 0.0009<br />
than leuprolide SC (Figure 3). In addition, clinicians reported<br />
more ease of injection with triptorelin IM versus leuprolide<br />
SC and felt more protected from accidental needle sticks<br />
after administering triptorelin versus leuprolide (Figure 4).<br />
Clinicians’ satisfaction assessments with other aspects of<br />
the study medications are reported in Table 3, with greater<br />
satisfaction with individual aspects reported with triptorelin<br />
versus leuprolide.<br />
Adverse Events<br />
Both study medications generally were well tolerated.<br />
Injection site pain was the most commonly reported AE and<br />
was reported by one patient in the triptorelin IM group and<br />
two patients in the leuprolide SC group. Other AEs reported<br />
were cystitis (1 patient in the triptorelin group), diarrhea (1<br />
patient in the leuprolide group), and urinary retention (1<br />
patient in the triptorelin group).<br />
Discussion<br />
In the present study, patients reported that triptorelin IM is<br />
associated with significantly less post-injection burning and/<br />
or stinging than leuprolide SC. In addition, significantly less<br />
post-injection soreness, discomfort, bother by redness,<br />
itching, and hardening, and anxiety were reported with<br />
triptorelin IM versus leuprolide SC. Similarly, patients reported<br />
significantly greater satisfaction with triptorelin IM versus<br />
leuprolide SC. Clinicians reported greater overall satisfaction<br />
and lower perceived patient distress with triptorelin IM versus<br />
leuprolide SC, Clinicians also reported greater convenience,<br />
ease, and satisfaction for all questionnaire parameters,<br />
including injection setup, preparation, administration, and<br />
disposal with triptorelin IM versus leuprolide SC. Both<br />
treatments were well tolerated.<br />
The efficacy and tolerability of triptorelin pamoate IM and<br />
leuprolide acetate SC in patients with advanced prostate<br />
cancer have been previously established (Sanofi-Aventis<br />
US, LLC, 2011; Watson Pharma, Inc., 2001). An earlier<br />
parallel-group, randomized, controlled multicenter study<br />
compared the efficacy and tolerability of triptorelin pamoate<br />
with leuprolide acetate in 284 men with advanced cancer<br />
(Heyns et al., 2003). Notably, however, both medications in<br />
the study were administered intramuscularly (Heyns et al.,<br />
2003). Findings from the study showed that triptorelin and<br />
leuprolide were both effective in maintaining castration and<br />
had similar tolerability (Heyns et al., 2003). When there is<br />
comparable efficacy between treatment options, a patient’s<br />
preference should be considered when making decisions<br />
about treatments (Wennberg, 2002).<br />
Understanding individual patients’ preferences for<br />
medications is important in clinical practice (Blinman, King,<br />
Norman, Viney, & Stockler, 2012). It allows physicians to<br />
tailor cancer treatments to individual patients (Blinman et al.,<br />
2012). Moreover, patient preferences for a medication can<br />
oncologistics 11
drug update<br />
oncologistics drug update<br />
Table 3: Clinicians’ Satisfaction With Various Aspects of the Study Medications<br />
oncologistics volume 12, issue 1 - spring 2013 12<br />
Characteristic Triptorelin Injection Leuprolide Injection<br />
Time required to administer the<br />
product was reasonable<br />
Mean (SD)<br />
Range<br />
Convenience of storage before<br />
administration<br />
Mean (SD)<br />
Range<br />
Instructions simple and easy to<br />
understand<br />
Mean (SD)<br />
Range<br />
All components of injection device<br />
were easy to identify<br />
Mean (SD)<br />
Range<br />
Time required to setup for the<br />
injection was reasonable<br />
Mean (SD)<br />
Range<br />
It was easy to prepare the device<br />
before injection<br />
Mean (SD)<br />
Range<br />
The product was easy to mix using<br />
the device<br />
Mean (SD)<br />
Range<br />
It was easy to draw the product<br />
into the syringe and attach to<br />
the needle<br />
Mean (SD)<br />
Range<br />
Time required to prepare the<br />
product was reasonable<br />
Mean (SD)<br />
Range<br />
5.32 (12.47)<br />
0–98<br />
3.59 (9.61)<br />
0–83<br />
5.04 (10.53)<br />
0–76<br />
4.27 (9.48)<br />
0–79<br />
4.41 (8.92)<br />
0–71<br />
5.29 (10.18)<br />
0–78<br />
6.21 (12.46)<br />
0–80<br />
7.54 (13.83)<br />
0–78<br />
4.88 (9.16)<br />
0–75<br />
15.56 (17.67)<br />
0–60<br />
10.72 (15.6)<br />
0–88<br />
9.73 (13.24)<br />
0–77<br />
11.17 (16.9)<br />
0–97<br />
12.47 (16.94)<br />
0–94<br />
13.16 (16.72)<br />
0–94<br />
15.45 (17.99)<br />
0–93<br />
19.0 (20.28)<br />
0–81<br />
16.88 (19.36)<br />
0–86<br />
affect treatment compliance, and consequently, treatment<br />
outcomes (Cameron, 1996). Treatment tolerability, complexity<br />
and convenience of treatment regimen, and the duration<br />
of treatment also affect patient compliance with treatment<br />
(Anderson, 2003; Cameron, 1996). Additional studies to further<br />
assess perceptions of GnRH agonists and the<br />
effect of these perceptions on treatment compliance are<br />
warranted to identify medication factors that could potentially<br />
improve compliance.<br />
Using VAS questionnaires, this study provided important<br />
information about patients’ and clinicians’ perceptions of two<br />
different GnRH agonist therapies. The VAS questionnaire is<br />
an easy and convenient tool that can be rapidly completed<br />
by patients or clinicians (Torrance, Feeny, & Furlong, 2001;<br />
Wewers & Lowe, 1990). However, there are limitations to<br />
findings obtained with VAS assessments. One limitation is<br />
measurement bias; people tend to avoid choosing the extreme<br />
ends of a continuous scale (Blinman et al., 2012). Comparability<br />
of scores between respondents also is limited (Blinman et al.,<br />
2012), because the VAS is subjective in nature and based on<br />
personal perceptions (Wewers et al., 1990). Moreover, some<br />
patients may not conceptually understand the VAS, which<br />
has been noted with elderly patients (Wewers et al., 1990). An<br />
additional limitation of the study is that AEs were evaluated for<br />
only 24 hours after administration of study medication. Certain<br />
longer-term AEs would not have been captured in this study. A<br />
future study assessing AEs for at least 72 hours post-injection<br />
would further describe the tolerability of GnRH agonists.<br />
Despite the study’s limitations, the present findings provide<br />
important information regarding patients’ perceptions<br />
of triptorelin IM versus leuprolide SC. The differences in<br />
perceptions between these medications may be attributable<br />
to the different routes of administration. In general, advantages<br />
of SC injections include a greater area for target injection sites<br />
and injections can be more easily self-administered (Prettyman,<br />
2005). In addition, the patient’s muscle mass does not need to<br />
be considered, and SC injections generally have a better safety<br />
profile (Prettyman, 2005). On the other hand, IM injections<br />
allow for a greater volume of medication to be delivered, and<br />
medications that are irritating to SC tissues may be less so<br />
when administered intramuscularly (Prettyman, 2005).<br />
Findings from the present study suggest that patients may<br />
prefer the IM GnRH agonist injection over the SC injection.<br />
Few studies of patients’ preferences for IM or SC injections<br />
have been published. To our knowledge, perceptions of<br />
the tolerability of GnRH agonists have not been previously<br />
evaluated. However, results from a study conducted in patients<br />
with diabetes demonstrated that seven out of eight patients<br />
reported equal pain when injecting insulin IM versus SC (Vaag,<br />
Pedersen, Lauritzen, Hildebrandt, & Beck-Nielsen, 1990).<br />
Findings from a previous randomized, open-label, parallelgroup<br />
study of 620 men with prostate cancer suggest that<br />
SC injections may be associated with more frequent injectionsite<br />
reactions than IM injections (Klotz et al., 2008). In the<br />
study, 40% of patients given SC degarelix, a GnRH receptor<br />
antagonist, reported injection-site reactions, compared with<br />
oncologistics volume 12, issue 1 - spring 2013 14<br />
drug update<br />
studies are needed to better understand how the route of<br />
administration affects patients’ and clinicians’ preferences<br />
for medications.<br />
Conclusion<br />
Triptorelin IM and leuprolide SC were both well tolerated,<br />
but patients reported less post-injection burning and/<br />
or stinging, soreness, discomfort, and anxiety with<br />
triptorelin IM versus leuprolide SC. Similarly, clinicians<br />
reported greater overall satisfaction, convenience,<br />
ease, as well as greater patient satisfaction and lower<br />
perceived patient distress with triptorelin IM versus<br />
leuprolide SC. Although the present study had limitations,<br />
many inherent to the limitations of VAS questionnaires<br />
in general, it is the first study to provide important<br />
information regarding preference for GnRH agonists.<br />
Future studies are warranted to further determine factors<br />
that may contribute to and affect patient preferences and<br />
treatment compliance.<br />
ACknowledgement<br />
Anny Wu, PharmD, Marsha Hall, BA, and Matthew<br />
Dougherty, BA (Scientific Connexions, Newtown, PA)<br />
provided medical writing and editorial assistance,<br />
supported by Watson Pharma, Inc.<br />
Neal D. Shore, MD, FACS, is managing partner,<br />
Atlantic Urology Clinics and Director, CPI, the Carolina<br />
Urologic Research Center, Myrtle Beach, SC.<br />
Paul Sieber, MD, FACS, is a urologist, Lancaster<br />
Urology, Lancaster, PA.<br />
Leanne Schimke, MSN, CRNP, FNP-C, CUNP, is a<br />
nurse practitioner, Lancaster Urology, Lancaster, PA.<br />
Adam Perzin, MD, is president of Delaware Valley<br />
Urology, Voorhees, NJ.<br />
Scott Olsen, MPH, is associate director, Clinical<br />
Affairs, Watson Pharmaceuticals, Salt Lake City, UT.<br />
References<br />
1. American Cancer Society (2012). Cancer Facts & Figures 2012.<br />
Retrieved from http://www.cancer.org/acs/groups/content/@<br />
epidemiologysurveilance/documents/document/acspc-031941.pdf<br />
2. Anderson, J. (2003). The role of antiandrogen monotherapy in<br />
the treatment of prostate cancer. BJU Int, 91(5), 455-461. doi.<br />
org/10.1046/j.1464-410X.2003.04026.x<br />
3. Blinman, P., King, M., Norman, R., Viney, R., & Stockler, M.R.<br />
(2012). Preferences for cancer treatments: an overview of methods<br />
and applications in oncology. Ann Oncol, 23(5), 1104-1110. doi.<br />
org/10.1093/annonc/mdr559<br />
4. Cameron, C. (1996). Patient compliance: recognition of factors<br />
involved and suggestions for promoting compliance with<br />
therapeutic regimens. J Adv Nurs, 24(2), 244-250. doi.org/10.1046/<br />
j.1365-2648.1996.01993.x<br />
5. Heyns, C.F., Simonin, M.-P., Grosgurin, P., Schall, R., Porchet, H.C.,<br />
for the South African Triptorelin Study Group. (2003). Comparative<br />
efficacy of triptorelin pamoate and leuprolide acetate in men with<br />
advanced prostate cancer. BJU Int, 92(3), 226-231. doi.org/10.1046/<br />
j.1464-410X.2003.04308.x<br />
6. Klotz, L., Boccon-Gibod, L., Shore, N.D., Andreou, C., Persson,<br />
B.E., Cantor, P., Schröder, F.H. (2008). The efficacy and safety<br />
of degarelix: a 12-month, comparative, randomized, open-label,<br />
parallel-group phase III study in patients with prostate cancer. BJU<br />
Int 102(11), 1531-1538. doi.org/10.1111/j.1464-410X.2008.08183.x<br />
7. National Comprehensive Cancer Network (NCCN). (2012). Clinical<br />
guidelines in oncology. Prostate cancer. Version 3.2012. Retrieved<br />
from http://www.nccn.org/professionals/physician_gls/pdf/<br />
prostate.pdf<br />
8. Prettyman, J. (2005). Subcutaneous or intramuscular Confronting<br />
a parenteral administration dilemma. Medsurg Nurs. 14(2), 93-98.<br />
9. Sanofi-Aventis US, LLC. (2011). Eligard: Highlights of prescribing<br />
information. Retrieved from http://products.sanofi.us/eligard/<br />
eligard_75.html<br />
10. Schulman, C. (2007). Assessing the attitudes to prostate cancer<br />
treatment among European male patients. BJU Int 100(suppl 1),<br />
6-11. doi.org/10.1111/j.1464-410X.2007.6976.x<br />
11. Torrance, G.W., Feeny, D., & Furlong, W. (2001). Visual Analog<br />
Scales: do they have a role in the measurement of preferences<br />
for health states Med Decis Making 21(4), 329-334. doi.<br />
org/10.1177/0272989X0102100408<br />
12. vaag, A., Pedersen, K.D., Lauritzen, M., Hildebrandt, P., & Beck-<br />
Nielsen, H. (1990). Intramuscular versus subcutaneous injection<br />
of unmodified insulin: consequences for blood glucose control in<br />
patients with type 1 diabetes mellitus. Diabet Med 7(4), 335-442.<br />
doi.org/10.1111/j.1464-5491.1990.tb01401.x<br />
13. Watson Pharma, Inc. (2001). Trelstar: Highlights of prescribing<br />
information. Available at: http://pi.watson.com/data_stream.<br />
aspproduct_group=1684&p=pi&language=E. Accessed<br />
September 4, 2012.<br />
14. Wennberg, J.E. (2002). Unwarranted variations in healthcare<br />
delivery: implications for academic medical centres. BMJ 325(7370),<br />
961-964. doi.org/ 10.1136/bmj.325.7370.961<br />
15. Wewers, M.E., & Lowe, N.K. (1990). A critical review of visual<br />
analogue scales in the measurement of clinical phenomena. Res<br />
Nurse Health 13(4), 227-236. doi.org/10.1002/nur.4770130405<br />
In Men With Advanced Prostate Cancer<br />
DEPENDABLE TESTOSTERONE<br />
SUPPRESS<strong>ION</strong><br />
Few castration escapes with<br />
Trelstar® therapy occurred<br />
during months 2 to 9 1,2 *<br />
• 4 patients (5 occurrences) in the<br />
Trelstar® 3.75 mg group<br />
• 11 patients (18 occurrences) in the<br />
active comparator group<br />
Convenient, well-tolerated delivery<br />
• Simple IM injection with MIXJECT®—<br />
no refrigeration necessary<br />
• Well-tolerated IM administration—injection<br />
site pain occurred in 2 patients (1.7%)<br />
with Trelstar® 22.5 mg (N=120) 3<br />
• Trelstar® is available for 1-month<br />
(3.75 mg), 3-month (11.25 mg), and<br />
6-month (22.5 mg) administration<br />
Mean Testoster<br />
stosterone one Level (ng/dL)<br />
50<br />
20<br />
Trelsta<br />
elstar ® 3.75 mg (n=137) †<br />
Active comparator (n=140) †<br />
50 ng/dL castrate level<br />
0<br />
29 57 85 113 141 169 197<br />
225 253<br />
Days<br />
Based on a 9-month, multicenter, parallel group, blindly randomized, controlled<br />
clinical trial comparing Trelstar® 3.75 mg to an active comparator in patients<br />
with advanced (stage C/D) prostate cancer (N=284). Mean testosterone<br />
concentrations were calculated from months 2 through 9.<br />
* The clinical benefi ts of maintaining testosterone levels
oncologistics volume 12, issue 1 - spring 2013 16<br />
BRIEF SUMMARY<br />
For full Prescribing Information, see package insert.<br />
INDICAT<strong>ION</strong>S AND USAGE<br />
TRELSTAR is indicated for the palliative treatment of advanced prostate cancer.<br />
CONTRAINDICAT<strong>ION</strong>S<br />
Hypersensitivity<br />
TRELSTAR is contraindicated in individuals with a known hypersensitivity to triptorelin or<br />
any other component of the product, or other GnRH agonists or GnRH [see Warnings and<br />
Precautions].<br />
Pregnancy<br />
TRELSTAR may cause fetal harm when administered to a pregnant woman. Expected hormonal<br />
changes that occur with TRELSTAR treatment increase the risk for pregnancy loss and fetal<br />
harm when administered to a pregnant woman [see Use in Specific Populations]. TRELSTAR<br />
is contraindicated in women who are or may become pregnant. If this drug is used during<br />
pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be<br />
apprised of the potential hazard to the fetus.<br />
WARNINGS AND PRECAUT<strong>ION</strong>S<br />
Hypersensitivity Reactions<br />
Anaphylactic shock, hypersensitivity, and angioedema related to triptorelin administration<br />
have been reported. In the event of a hypersensitivity reaction, therapy with TRELSTAR<br />
should be discontinued immediately and the appropriate supportive and symptomatic care<br />
should be administered.<br />
Transient Increase in Serum Testosterone<br />
Initially, triptorelin, like other GnRH agonists, causes a transient increase in serum testosterone<br />
levels. As a result, isolated cases of worsening of signs and symptoms of prostate<br />
cancer during the first weeks of treatment have been reported with GnRH agonists. Patients<br />
may experience worsening of symptoms or onset of new symptoms, including bone pain,<br />
neuropathy, hematuria, or urethral or bladder outlet obstruction.<br />
Metastatic Vertebral Lesions and Urinary Tract Obstruction<br />
Cases of spinal cord compression, which may contribute to weakness or paralysis with<br />
or without fatal complications, have been reported with GnRH agonists. If spinal cord<br />
compression or renal impairment develops, standard treatment of these complications<br />
should be instituted, and in extreme cases an immediate orchiectomy considered.<br />
Patients with metastatic vertebral lesions and/or with upper or lower urinary tract obstruction<br />
should be closely observed during the first few weeks of therapy.<br />
Hyperglycemia and Diabetes<br />
Hyperglycemia and an increased risk of developing diabetes have been reported in men receiving<br />
GnRH agonists. Hyperglycemia may represent development of diabetes mellitus or worsening<br />
of glycemic control in patients with diabetes. Monitor blood glucose and/or glycosylated<br />
hemoglobin (HbA1c) periodically in patients receiving a GnRH agonist and manage with current<br />
practice for treatment of hyperglycemia or diabetes.<br />
Cardiovascular Diseases<br />
Increased risk of developing myocardial infarction, sudden cardiac death and stroke has been<br />
reported in association with use of GnRH agonists in men. The risk appears low based on<br />
the reported odds ratios, and should be evaluated carefully along with cardiovascular risk<br />
factors when determining a treatment for patients with prostate cancer. Patients receiving a<br />
GnRH agonist should be monitored for symptoms and signs suggestive of development of<br />
cardiovascular disease and be managed according to current clinical practice.<br />
Laboratory Tests<br />
Response to TRELSTAR should be monitored by measuring serum levels of testosterone<br />
periodically or as indicated.<br />
Laboratory Test Interactions<br />
Chronic or continuous administration of triptorelin in therapeutic doses results in suppression<br />
of pituitary-gonadal axis. Diagnostic tests of the pituitary-gonadal function conducted during<br />
treatment and after cessation of therapy may therefore be misleading.<br />
ADVERSE REACT<strong>ION</strong>S<br />
Clinical Trials Experience<br />
Because clinical trials are conducted under widely varying conditions, adverse reaction rates<br />
observed in the clinical trials of a drug cannot be directly compared with rates in the clinical<br />
trials of another drug and may not reflect the rates observed in practice.<br />
The safety of the three TRELSTAR formulations was evaluated in clinical trials involving<br />
patients with advanced prostate cancer. Mean testosterone levels increased above baseline<br />
during the first week following the initial injection, declining thereafter to baseline levels or<br />
below by the end of the second week of treatment. The transient increase in testosterone levels<br />
may be associated with temporary worsening of disease signs and symptoms, including bone<br />
pain, neuropathy, hematuria, and urethral or bladder outlet obstruction. Isolated cases of<br />
spinal cord compression with weakness or paralysis of the lower extremities have occurred<br />
[see Warnings and Precautions].<br />
Adverse reactions reported for each of the three TRELSTAR formulations in the clinical trials, are<br />
presented in Table 2, Table 3, and Table 4. Often, causality is difficult to assess in patients with<br />
metastatic prostate cancer. The majority of adverse reactions related to triptorelin are a result<br />
of its pharmacological action, i.e., the induced variation in serum testosterone levels, either<br />
an increase in testosterone at the initiation of treatment, or a decrease in testosterone once<br />
castration is achieved. Local reactions at the injection site or allergic reactions may occur.<br />
The following adverse reactions were reported to have a possible or probable relationship<br />
to therapy as ascribed by the treating physician in at least 1% of patients receiving<br />
Trelstar 3.75 mg.<br />
Table 2. TRELSTAR 3.75 mg: Treatment-Related Adverse Reactions Reported<br />
by 1% or More of Patients During Treatment<br />
TRELSTAR 3.75 mg<br />
N = 140<br />
Adverse Reactions 1<br />
N %<br />
Application Site Disorders<br />
Injection site pain 5 3.6<br />
Body as a Whole<br />
Hot flush<br />
Pain<br />
Leg pain<br />
Fatigue<br />
82<br />
3<br />
3<br />
3<br />
58.6<br />
2.1<br />
2.1<br />
2.1<br />
Cardiovascular Disorders<br />
Hypertension 5 3.6<br />
Central and Peripheral Nervous System Disorders<br />
Headache<br />
Dizziness<br />
Gastrointestinal Disorders<br />
Diarrhea<br />
Vomiting<br />
7<br />
2<br />
2<br />
3<br />
5.0<br />
1.4<br />
1.4<br />
2.1<br />
Musculoskeletal System Disorders<br />
Skeletal pain 17 12.1<br />
Psychiatric Disorders<br />
Insomnia<br />
Impotence<br />
Emotional lability<br />
3<br />
10<br />
2<br />
2.1<br />
7.1<br />
1.4<br />
Red Blood Cell Disorders<br />
Anemia 2 1.4<br />
Skin and Appendages Disorders<br />
Pruritus 2 1.4<br />
Urinary System Disorders<br />
Urinary tract infection<br />
Urinary retention<br />
2<br />
2<br />
1.4<br />
1.4<br />
1 Adverse reactions for TRELSTAR 3.75 mg are coded using the WHO Adverse Reactions<br />
Terminology (WHOART)<br />
The following adverse reactions were reported to have a possible or probable relationship<br />
to therapy as ascribed by the treating physician in at least 1% of patients receiving<br />
Trelstar 11.25 mg.<br />
Table 3. TRELSTAR 11.25 mg: Treatment-Related Adverse Reactions<br />
Reported by 1% or More of Patients During Treatment<br />
TRELSTAR 11.25 mg<br />
N = 174<br />
Adverse Reactions 1<br />
N %<br />
Application Site<br />
Injection site pain 7 4.0<br />
Body as a Whole<br />
Hot flush<br />
Leg pain<br />
Pain<br />
Back pain<br />
Fatigue<br />
Chest pain<br />
Asthenia<br />
Peripheral edema<br />
Cardiovascular Disorders<br />
Hypertension<br />
Dependent edema<br />
Central and Peripheral Nervous System Disorders<br />
Headache<br />
Dizziness<br />
Leg cramps<br />
Endocrine<br />
Breast pain<br />
Gynecomastia<br />
Gastrointestinal Disorders<br />
Nausea<br />
Constipation<br />
Dyspepsia<br />
Diarrhea<br />
Abdominal pain<br />
127<br />
9<br />
6<br />
5<br />
4<br />
3<br />
2<br />
2<br />
7<br />
4<br />
12<br />
5<br />
3<br />
4<br />
3<br />
5<br />
3<br />
3<br />
2<br />
2<br />
73.0<br />
5.2<br />
3.4<br />
2.9<br />
2.3<br />
1.7<br />
1.1<br />
1.1<br />
4.0<br />
2.3<br />
6.9<br />
2.9<br />
1.7<br />
2.3<br />
1.7<br />
2.9<br />
1.7<br />
1.7<br />
1.1<br />
1.1<br />
Liver and Biliary System<br />
Abnormal hepatic function 2 1.1<br />
Metabolic and Nutritional Disorders<br />
Edema in legs<br />
Increased alkaline phosphatase<br />
Musculoskeletal System Disorders<br />
Skeletal pain<br />
Arthralgia<br />
Myalgia<br />
Psychiatric Disorders<br />
Decreased libido<br />
Impotence<br />
Insomnia<br />
Anorexia<br />
Respiratory System Disorders<br />
Coughing<br />
Dyspnea<br />
Pharyngitis<br />
11<br />
3<br />
23<br />
4<br />
2<br />
4<br />
4<br />
3<br />
3<br />
3<br />
2<br />
2<br />
6.3<br />
1.7<br />
13.2<br />
2.3<br />
1.1<br />
2.3<br />
2.3<br />
1.7<br />
1.7<br />
1.7<br />
1.1<br />
1.1<br />
Skin and Appendages<br />
Rash 3 1.7<br />
Urinary System Disorders<br />
Dysuria<br />
Urinary retention<br />
Vision Disorders<br />
Eye pain<br />
Conjunctivitis<br />
1 Adverse reactions for TRELSTAR 11.25 mg are coded using the WHO Adverse Reactions<br />
Terminology (WHOART)<br />
The following adverse reactions occurred in at least 5% of patients receiving TRELSTAR 22.5<br />
mg. The table includes all reactions whether or not they were ascribed to TRELSTAR by the<br />
treating physician. The table also includes the incidence of these adverse reactions that were<br />
considered by the treating physician to have a reasonable causal relationship or for which the<br />
relationship could not be assessed.<br />
Table 4. TRELSTAR 22.5 mg: Adverse Reactions Reported by 5% or More of<br />
Patients During Treatment<br />
8<br />
2<br />
2<br />
2<br />
4.6<br />
1.1<br />
1.1<br />
1.1<br />
TRELSTAR 22.5 mg<br />
N = 120<br />
Treatment-Emergent Treatment-Related<br />
Adverse Reactions 1<br />
N % N %<br />
General Disorders and<br />
Administration Site Conditions<br />
Edema peripheral 6 5.0 0 0<br />
Infections and Infestations<br />
Influenza<br />
Bronchitis<br />
19<br />
6<br />
15.8<br />
5.0<br />
Endocrine<br />
Diabetes Mellitus/Hyperglycemia 6 5.0 0 0<br />
Musculoskeletal and Connective<br />
Tissue Disorders<br />
Back pain<br />
Arthralgia<br />
Pain in extremity<br />
13<br />
9<br />
9<br />
10.8<br />
7.5<br />
7.5<br />
0<br />
0<br />
1<br />
1<br />
1<br />
0<br />
0<br />
0.8<br />
0.8<br />
0.8<br />
Nervous System Disorders<br />
Headache 9 7.5 2 1.7<br />
Psychiatric Disorders<br />
Insomnia 6 5.0 1 0.8<br />
Renal and Urinary Disorders<br />
Urinary tract infection<br />
Urinary retention<br />
Reproductive System and<br />
Breast Disorders<br />
Erectile dysfunction<br />
Testicular atrophy<br />
Vascular Disorders<br />
Hot flush<br />
Hypertension<br />
14<br />
6<br />
12<br />
9<br />
87<br />
17<br />
11.6<br />
5.0<br />
10.0<br />
7.5<br />
72.5<br />
14.2<br />
1 Adverse reactions for TRELSTAR 22.5 mg are coded using the Medical Dictionary for<br />
Regulatory Activities (MedDRA)<br />
0<br />
0<br />
12<br />
9<br />
86<br />
1<br />
0<br />
0<br />
10.0<br />
7.5<br />
71.7<br />
0.8<br />
Changes in Laboratory Values During Treatment<br />
The following abnormalities in laboratory values not present at baseline were observed in 10%<br />
or more of patients:<br />
TRELSTAR 3.75 mg: There were no clinically meaningful changes in laboratory values<br />
detected during therapy.<br />
TRELSTAR 11.25 mg: Decreased hemoglobin and RBC count and increased glucose, BUN,<br />
SGOT, SGPT, and alkaline phosphatase at the Day 253 visit.<br />
TRELSTAR 22.5 mg: Decreased hemoglobin and increased glucose and hepatic transaminases<br />
were detected during the study. The majority of the changes were mild to moderate.<br />
Postmarketing Experience<br />
The following adverse reaction has been identified during post approval use of gonadotropin<br />
releasing hormone agonists. Because this reaction is recorded voluntarily from a population of<br />
uncertain size, it is not always possible to reliably estimate its frequency or establish a causal<br />
relationship to drug exposure.<br />
During postmarketing surveillance, rare cases of pituitary apoplexy (a clinical syndrome<br />
secondary to infarction of the pituitary gland) have been reported after the administration of<br />
gonadotropin-releasing hormone agonists. In a majority of these cases, a pituitary adenoma<br />
was diagnosed with a majority of pituitary apoplexy cases occurring within 2 weeks of the first<br />
dose, and some within the first hour. In these cases, pituitary apoplexy has presented as sudden<br />
headache, vomiting, visual changes, ophthalmoplegia, altered mental status, and sometimes<br />
cardiovascular collapse. Immediate medical attention has been required.<br />
DRUG INTERACT<strong>ION</strong>S<br />
No drug-drug interaction studies involving triptorelin have been conducted.<br />
Human pharmacokinetic data with triptorelin suggest that C-terminal fragments produced by<br />
tissue degradation are either degraded completely within tissues or are rapidly degraded further<br />
in plasma, or cleared by the kidneys. Therefore, hepatic microsomal enzymes are unlikely<br />
to be involved in triptorelin metabolism. However, in the absence of relevant data and as a<br />
precaution, hyperprolactinemic drugs should not be used concomitantly with triptorelin since<br />
hyperprolactinemia reduces the number of pituitary GnRH receptors.<br />
USE IN SPECIFIC POPULAT<strong>ION</strong>S<br />
Pregnancy<br />
Pregnancy Category X [see ‘Contraindications’ section].<br />
TRELSTAR is contraindicated in women who are or may become pregnant while receiving the<br />
drug. Expected hormonal changes that occur with TRELSTAR treatment increase the risk for<br />
pregnancy loss. If this drug is used during pregnancy, or if the patient becomes pregnant while<br />
taking this drug, the patient should be apprised of the potential hazard to the fetus.<br />
Studies in pregnant rats administered triptorelin at doses of 2, 10, and 100 mcg/kg/day<br />
(approximately equivalent to 0.2, 0.8, and 8 times the estimated human daily dose based on<br />
body surface area) during the period of organogenesis demonstrated maternal toxicity and<br />
embryo-fetal toxicities. Embryo-fetal toxicities consisted of pre-implantation loss, increased<br />
resorption, and reduced mean number of viable fetuses at the high dose. Teratogenic effects<br />
were not observed in viable fetuses in rats or mice. Doses administered to mice were 2, 20,<br />
and 200 mcg/kg/day (approximately equivalent to 0.1, 0.7, and 7 times the estimated human<br />
daily dose based on body surface area).<br />
Nursing Mothers<br />
TRELSTAR is not indicated for use in women [see Indications and Usage]. It is not known if<br />
triptorelin is excreted in human milk. Because many drugs are excreted in human milk, and<br />
because of the potential for serious adverse reactions in nursing infants from TRELSTAR, a<br />
decision should be made to either discontinue nursing, or discontinue the drug taking into<br />
account the importance of the drug to the mother.<br />
Pediatric Use<br />
Safety and effectiveness in pediatric patients have not been established.<br />
Geriatric Use<br />
Prostate cancer occurs primarily in an older population. Clinical studies with TRELSTAR have<br />
been conducted primarily in patients ≥ 65 years.<br />
Renal Impairment<br />
Subjects with renal impairment had higher exposure than young healthy males.<br />
Hepatic Impairment<br />
Subjects with hepatic impairment had higher exposure than young healthy males.<br />
OVERDOSAGE<br />
There is no experience of overdosage in clinical trials. In single dose toxicity studies in<br />
mice and rats, the subcutaneous LD 50 of triptorelin was 400 mg/kg in mice and 250 mg/kg<br />
in rats, approximately 500 and 600 times, respectively, the estimated monthly human<br />
dose based on body surface area. If overdosage occurs, therapy should be discontinued<br />
immediately and the appropriate supportive and symptomatic treatment administered.<br />
Distributed By: Watson Pharma, Inc., Parsippany, NJ 07054 USA<br />
Manufactured By: Debio RP, CH-1920 Martigny, Switzerland<br />
For all medical inquiries contact: WATSON Medical Communications, Parsippany, NJ<br />
07054 800-272-5525<br />
MIXJECT is manufactured by and is a registered trademark of: Medimop Medical Projects<br />
Ltd., Ra’anana, Israel<br />
The pre-filled syringe containing sterile water for injection is manufactured by: Solvay<br />
Biologicals BV, Olst, The Netherlands<br />
Rx only Revised: March 2011<br />
oncologistics 17
industry insight<br />
oncologistics industry insight<br />
WHY CommuniTY<br />
Counts<br />
By: Chris Vorce<br />
Community oncology has long been a key component in this nation’s healthcare delivery system.<br />
Despite the implementation of the Medicare Modernization Act, and other measures that have cut<br />
reimbursement and made it more difficult for private practices to operate, community oncologists<br />
continue to treat the majority of patients in the United States. The community oncology model was<br />
essentially created to remove cancer care from the hospital system, where treatments could be<br />
delivered conveniently, directly, efficiently, and at less cost to the patient. Unfortunately, over the<br />
years, Medicare reimbursement cuts have jeopardized this care delivery model. Furthermore, recently<br />
introduced sequestration cuts may push community oncology over the edge, and initiate a major<br />
regression in the way care is currently delivered to patients with cancer.<br />
In response to the changing dynamics of the<br />
These resources can be accessed on<br />
healthcare landscape, and to combat industry<br />
www.ourcommunitycounts.org, and include:<br />
forces that are effectively weakening community<br />
oncology, <strong>ION</strong> <strong>Solutions</strong> has launched the<br />
> Two educational Web cast series that provide<br />
Community Counts campaign.<br />
insight on how to become more efficient and<br />
grow/expand business<br />
This campaign aims to educate providers, payers,<br />
> Informative white papers that quantify the value<br />
oncologistics volume 12, issue 1 - spring 2013 18<br />
and legislators on the issues that are affecting the<br />
viability of community oncology: the above-mentioned<br />
sequestration cuts, SGR cuts, the Affordable Care Act,<br />
etc; provide tools and resources to empower physicians<br />
to be able to advocate on their own behalf; and use<br />
ion <strong>Solutions</strong>’ standing in the market to amplify the<br />
voice of community oncology throughout the nation.<br />
of community oncology and can be used as the<br />
basis for discussions with legislators, payers,<br />
and others<br />
> Archival information on past events: live meetings,<br />
web casts, etc on sequestration<br />
> Site of Care presentation deck, to arm practices<br />
with insight needed to conduct meaningful<br />
discussions with payers and legislators<br />
In response to the changing dynAMiCS of the healTHCARe<br />
lanDSCApe, and to combAT inDUSTRY foRCes that are eFFeCTively<br />
weakening communiTY oncoloGY, <strong>ION</strong> SolUTions has lAUnCHed<br />
THe CommuniTY CounTS campaign.<br />
oncologistics 19
industry insight<br />
> Several practice efficiency resources: “9 Habits<br />
of a Healthy Practice”, survey results, editorials,<br />
talking points<br />
> Patient-facing materials: waiting room posters, call<br />
to action letters, talking points, etc<br />
> An advocacy tool that allows practice personnel to<br />
contact regional legislators in an effort to combat<br />
recent sequestration cuts<br />
ion <strong>Solutions</strong> truly believes that the community setting<br />
provides the best opportunity for convenient, efficient,<br />
and effective cancer care. We are wholly committed<br />
to this space, and will continue to dedicate our time,<br />
energy, and resources to supporting your mission of<br />
providing optimal patient care. As sequestration cuts<br />
begin to influence the way that you are able to treat your<br />
patients and serve your community, please let us know<br />
what we can provide to help.<br />
Contact your <strong>ION</strong> <strong>Solutions</strong> strategic account manager,<br />
or visit www.ourcommunitycounts.org to learn more.<br />
The future of your practice<br />
begins here and now.<br />
oncologistics volume 12, issue 1 - spring 2013 20<br />
Chris Vorce is director, marketing and communications,<br />
at <strong>ION</strong> <strong>Solutions</strong>.<br />
Share your voice with legislators at<br />
CommunityCountsAdvocacy.org<br />
It’s time to demonstrate the real, measurable<br />
value of community oncology.<br />
To ensure the future of community oncology, we must communicate its value today.<br />
Community Counts is a physician-led movement that puts the power in your hands.<br />
Simply register at ourcommunitycounts.org and gain access to information and tools<br />
to help you learn how to navigate this new healthcare environment, and operate<br />
more efficiently in it.<br />
So join the cause and make your voice count. Go to ourcommunitycounts.org today.
2013 Meeting Schedule<br />
For melanoma patients with microscopic<br />
or gross nodal involvement<br />
Meeting Date Meeting Name Location Venue<br />
April 19-21, 2013 LPP National Meeting Washington, DC Renaissance<br />
May 17-19, 2013 Business of Oncology Washington, DC Renaissance<br />
Sept 20-22, 2013 National Healthcare Nashville, TN Loews Vanderbilt<br />
Practitioners Meeting<br />
Sept 27-29, 2013 LPP Select Meeting Dallas, TX Fairmont Dallas<br />
Oct 25-27, 2013 LPP Excel Meeting Dallas, TX Dallas Marriott<br />
City Center<br />
November 8-10, 2013 <strong>ION</strong> National Meeting Phoenix, AZ Sheraton Downtown<br />
A Perspective on Adjuvant Therapy<br />
Significant effect on<br />
relapse-free survival<br />
Based on 696 relapse-free survival (RFS) events, determined by the Independent Review Committee,<br />
median RFS was 34.8 months (95% CI, 26.1–47.4) and 25.5 months (95% CI, 19.6–30.8) in the group<br />
treated with SYLATRON (peginterferon alfa-2b) and the observation group, respectively. The estimated<br />
hazard ratio for RFS was 0.82 (95% CI, 0.71–0.96; unstratified log-rank P=0.011) in favor of SYLATRON.<br />
SYLATRON is indicated for the adjuvant treatment of melanoma with microscopic or gross nodal<br />
involvement within 84 days of definitive surgical resection including complete lymphadenectomy.<br />
SELECT IMPORTANT SAFETY INFORMAT<strong>ION</strong><br />
WARNING: Depression and other Neuropsychiatric Disorders<br />
The risk of serious depression, with suicidal ideation and completed suicides, and other<br />
serious neuropsychiatric disorders are increased with alpha interferons, including SYLATRON.<br />
Permanently discontinue SYLATRON in patients with persistently severe or worsening signs<br />
or symptoms of depression, psychosis, or encephalopathy. These disorders may not resolve<br />
after stopping SYLATRON.<br />
SYLATRON is contraindicated in patients with a history of anaphylaxis to peginterferon alfa-2b or<br />
interferon alfa-2b, in patients with autoimmune hepatitis, and in patients with hepatic decompensation<br />
(Child-Pugh score >6 [Class B and C]).<br />
*Meeting dates subject to change*<br />
Please see the adjacent Brief Summary of the Prescribing Information,<br />
including the Boxed Warning about depression and other<br />
neuropsychiatric disorders.<br />
oncologistics 23
SELECT IMPORTANT SAFETY INFORMAT<strong>ION</strong><br />
• Peginterferon alfa-2b can cause life-threatening or fatal neuropsychiatric reactions. These<br />
include suicide, suicidal and homicidal ideation, depression, and an increased risk of relapse<br />
of recovering drug addicts. Depression occurred in 59% of patients treated with SYLATRON<br />
(peginterferon alfa-2b) and 24% of patients in the observation group. Depression was severe<br />
or life-threatening in 7% of patients treated with SYLATRON compared with
SYLATRON (peginterferon alfa-2b) is indicated for the adjuvant treatment of melanoma<br />
with microscopic or gross nodal involvement within 84 days of definitive surgical resection<br />
including complete lymphadenectomy.<br />
A Perspective on Adjuvant Therapy<br />
Significant effect on<br />
relapse-free survival<br />
• In the pivotal study, the dose of SYLATRON was adjusted to maintain an ECOG Performance Status of 0 or 1.<br />
• Median duration of therapy:<br />
– 6-mcg/kg/wk dose: median 8.0 weeks<br />
– 3-mcg/kg/wk dose: median 14.3 months<br />
• Patients achieved a significant improvement in relapse-free survival.<br />
– Based on 696 RFS events, determined by the Independent Review Committee.<br />
– Median RFS was 34.8 months (95% CI, 26.1–47.4) and 25.5 months (95% CI, 19.6–30.8) in the group<br />
treated with SYLATRON and the observation group, respectively.<br />
– The estimated hazard ratio for RFS was 0.82 (95% CI, 0.71–0.96; unstratified log-rank P=0.011)<br />
in favor of SYLATRON.<br />
SELECT IMPORTANT SAFETY INFORMAT<strong>ION</strong><br />
• There are no adequate and well-controlled studies of SYLATRON in pregnant women. Use SYLATRON<br />
during pregnancy only if the potential benefit justifies the potential risk to the fetus.<br />
• It is not known whether the components of SYLATRON are excreted in human milk. Because of the<br />
potential for adverse reactions from the drug in nursing infants, a decision must be made whether to<br />
discontinue nursing or discontinue treatment with SYLATRON.<br />
• Safety and effectiveness in patients below the age of 18 years have not been established.<br />
• Increase frequency of monitoring for SYLATRON toxicity in patients with moderate and severe renal impairment.<br />
Please see the adjacent Brief Summary of the Prescribing Information,<br />
including the Boxed Warning about depression and other neuropsychiatric disorders.<br />
Copyright © 2012 Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc.<br />
All rights reserved. ONCO-1064624-0000 12/12<br />
Brief Summary of the Prescribing Information<br />
WARNING: DEPRESS<strong>ION</strong> AND OTHER NEUROPSYCHIATRIC DISORDERS<br />
The risk of serious depression, with suicidal ideation and completed suicides,<br />
and other serious neuropsychiatric disorders are increased with alpha interferons,<br />
including SYLATRON. Permanently discontinue SYLATRON in patients with<br />
persistently severe or worsening signs or symptoms of depression, psychosis, or<br />
encephalopathy. These disorders may not resolve after stopping SYLATRON<br />
[see Warnings and Precautions and Adverse Reactions].<br />
INDICAT<strong>ION</strong>S AND USAGE<br />
SYLATRON is an alpha interferon indicated for the adjuvant treatment of melanoma with<br />
microscopic or gross nodal involvement within 84 days of definitive surgical resection including<br />
complete lymphadenectomy.<br />
CONTRAINDICAT<strong>ION</strong>S<br />
SYLATRON is contraindicated in patients with a history of anaphylaxis to peginterferon alfa-2b<br />
or interferon alfa-2b, autoimmune hepatitis, or hepatic decompensation (Child-Pugh score >6 [class<br />
B and C]).<br />
WARNINGS AND PRECAUT<strong>ION</strong>S<br />
Depression and Other Serious Neuropsychiatric Adverse Reactions<br />
Peginterferon alfa-2b can cause life-threatening or fatal neuropsychiatric reactions. These include<br />
suicide, suicidal and homicidal ideation, depression, and an increased risk of relapse of recovering<br />
drug addicts. In the clinical trial, depression occurred in 59% of SYLATRON-treated patients and<br />
24% of patients in the observation group. Depression was severe or life threatening in 7% of<br />
SYLATRON-treated patients compared with
Brief Summary of the Prescribing Information for SYLATRON (peginterferon alfa-2b)<br />
Immunogenicity<br />
As with all therapeutic proteins, there is potential for immunogenicity. The incidence of antibodies<br />
to peginterferon alfa-2b has not been studied in patients with melanoma. In clinical studies<br />
conducted in patients with chronic hepatitis C, the incidence of binding antibodies to peginterferon<br />
alfa-2b was approximately 10% (174/1,759). Among the patients tested positive for binding<br />
antibodies, 18% (32/174) developed neutralizing antibodies.<br />
The incidence of antibody formation is highly dependent on the sensitivity and specificity of the<br />
assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity<br />
in an assay may be influenced by several factors, including assay methodology, sample handling,<br />
timing of sample collection, concomitant medications, and underlying disease. For these reasons,<br />
comparison of the incidence of antibodies to SYLATRON with the incidence of antibodies to other<br />
products may be misleading.<br />
Postmarketing Experience<br />
The following adverse reactions have been identified during postapproval use of peginterferon<br />
alfa-2b as monotherapy and in combination with ribavirin in chronic hepatitis C (CHC) patients.<br />
Because these reactions are reported voluntarily from a population of uncertain size, it is not<br />
always possible to reliably estimate their frequency or establish a causal relationship to drug<br />
exposure.<br />
Blood and Lymphatic System Disorders: pure red cell aplasia, thrombotic thrombocytopenic<br />
purpura<br />
Ear and Labyrinth Disorders: hearing loss, vertigo, hearing impairment<br />
Endocrine Disorders: diabetic ketoacidosis<br />
Eye Disorders: Vogt-Koyanagi-Harada syndrome<br />
Gastrointestinal Disorders: aphthous stomatitis, pancreatitis, colitis<br />
Infusion reactions: angioedema, urticaria, bronchoconstriction<br />
Immune System Disorders: systemic lupus erythematosus, erythema multiforme, thyroiditis,<br />
thrombotic thrombocytopenic purpura, idiopathic thrombocytopenic purpura, rheumatoid arthritis,<br />
interstitial nephritis, and systemic lupus erythematosus<br />
Infections: sepsis<br />
Metabolism and Nutrition Disorders: hypertriglyceridemia<br />
Musculoskeletal and Connective Tissue Disorders: rhabdomyolysis, myositis<br />
Nervous System Disorders: seizures, memory loss, peripheral neuropathy, paraesthesia,<br />
migraine headache<br />
Respiratory, Thoracic, and Mediastinal Disorders: dyspnea, pulmonary infiltrates, pneumonia,<br />
bronchiolitis obliterans, interstitial pneumonitis, sarcoidosis, and pulmonary hypertension<br />
Skin and Subcutaneous Tissue Disorders: Stevens-Johnson syndrome, toxic epidermal<br />
necrolysis, psoriasis<br />
Vascular Disorders: hypertension, hypotension, stroke<br />
DRUG INTERACT<strong>ION</strong>S<br />
In healthy subjects who were administered peginterferon alfa-2b subcutaneously at 1 mcg/kg once<br />
weekly for four weeks with probe drugs of metabolic enzymes administered before the first dose<br />
and after the fourth dose, a measure of CYP2C9 activity increased to 125% of baseline, whereas a<br />
measure of CYP2D6 activity decreased to 51% of baseline.<br />
When administering SYLATRON with medications metabolized by CYP2C9 or CYP2D6, the<br />
therapeutic effect of these drugs may be altered.<br />
The effects of pegylated interferon alfa-2b on the pharmacokinetics of drugs metabolized by<br />
cytochrome P-450 enzymes have not been studied at the higher clinical doses for patients with<br />
melanoma (3 mcg/kg/week and 6 mcg/kg/week).<br />
USE IN SPECIFIC POPULAT<strong>ION</strong>S<br />
Pregnancy<br />
Pregnancy Category C:<br />
There are no adequate and well-controlled studies of SYLATRON in pregnant women.<br />
Nonpegylated interferon alfa-2b was an abortifacient in Macaca mulatta (rhesus monkeys) at<br />
15 and 30 million international units (IU)/kg (estimated human equivalent of 5 and 10 million IU/kg,<br />
based on body surface area adjustment for a 60-kg adult). The estimated INTRON ® A (interferon<br />
alfa-2b) human equivalent dose of 5 to 10 million IU/kg daily is approximately equal to a human<br />
equivalent dose of 79 to 158 mcg/kg/week of SYLATRON. Use SYLATRON during pregnancy only<br />
if the potential benefit justifies the potential risk to the fetus.<br />
Nursing Mothers<br />
It is not known whether the components of SYLATRON are excreted in human milk. Studies in<br />
mice have shown that mouse interferons are excreted in breast milk. Because of the potential<br />
for adverse reactions from the drug in nursing infants, a decision must be made whether to<br />
discontinue nursing or discontinue the SYLATRON treatment, taking into account the importance of<br />
the therapy to the mother.<br />
Pediatric Use<br />
Safety and effectiveness in patients below the age of 18 years have not been established.<br />
Geriatric Use<br />
Clinical studies of SYLATRON did not include sufficient numbers of subjects aged 65 and over<br />
to determine whether they respond differently from younger subjects.<br />
Hepatic Impairment<br />
SYLATRON has not been studied in patients with melanoma who have hepatic impairment.<br />
In patients treated for viral hepatitis, peginterferon alfa-2b treatment is contraindicated in those<br />
with moderate or severe hepatic impairment (Child-Pugh scores >6). Discontinue SYLATRON if<br />
hepatic decompensation (Child-Pugh scores >6) occurs during treatment. [See Contraindications<br />
and Warnings and Precautions.]<br />
Renal Impairment<br />
The mean area under the concentration-time curve (AUC last<br />
) following a single dose of<br />
peginterferon alfa-2b at 1 mcg/kg increased by 1.3-, 1.7- and 1.9-fold in subjects with mild<br />
(creatinine clearance 50–79 mL/min), moderate (creatinine clearance 30–50 mL/min), and severe<br />
(creatinine clearance 10–29 mL/min) renal impairment, respectively. After multiple doses, the<br />
mean AUC tau<br />
increased by 1.3-fold in moderate and 2.1-fold in severe renal impairment. No<br />
clinically meaningful amounts of peginterferon alfa-2b were removed during hemodialysis.<br />
Dose reductions of 25% and 50% are recommended in patients with moderate and severe renal<br />
impairment, respectively, receiving alpha interferons for chronic hepatitis C.<br />
The effect of varying degrees of renal impairment on the pharmacokinetics of peginterferon<br />
alfa-2b at the recommended doses of 3 mcg/kg or 6 mcg/kg for patients with melanoma has not<br />
been studied.<br />
OVERDOSAGE<br />
The experience with overdose of SYLATRON is limited. Patients who were over dosed<br />
experienced the following adverse reactions: severe fatigue, headache, myalgia, neutropenia, and<br />
thrombocytopenia. The highest single dose administered was 14 mcg/kg.<br />
For more detailed information, please read the Prescribing Information.<br />
LRN#054031-SYL-PWi-USPI.14<br />
Copyright © 2012 Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc.<br />
All rights reserved. ONCO-1064624-0000 12/12<br />
MORE PATIENTS. MORE PRESCRIPT<strong>ION</strong>S.<br />
A MORE COMPlETE CONTINuuM Of CARE<br />
wIThIN yOuR PRACTICE.<br />
The SpecialTy OncOlOgy neTwOrk frOm iOn SOluTiOnS.<br />
establishing your own in-practice dispensing service through iOn <strong>Solutions</strong><br />
not only allows your patients more convenient access to medication, but<br />
it also enhances your control and oversight of their therapy. The Specialty<br />
Oncology network (SOn) exists to help community oncology practices<br />
successfully optimize in-practice dispensing services — in fact, 90% of<br />
all dispensing oncology practices are part of SOn. with the largest and<br />
longest-tenured pharmacy program in the market, and eight gpO contracts<br />
currently in place, iOn <strong>Solutions</strong> harnesses the collective power of community<br />
oncology to accelerate practice growth and improve patient care.<br />
For additional information, please visit iononline.com or email<br />
SON@iononline.com.
industry insight<br />
oncologistics industry insight<br />
LyMPHOMA Review:<br />
SELECTED HIGHLIGHTS<br />
FROM ASH 2012<br />
By: Michael E. Williams, MD, ScM<br />
Several interesting updates on investigational lymphoma treatment approaches were presented at the Annual<br />
Meeting of the American Society for <strong>Hematology</strong> (ASH) this past winter.<br />
First, it is worthwhile to begin with some data from the 2012 annual meeting of the American Society of Clinical<br />
Oncology (ASCO). In a Plenary Session at ASCO 2012, Rummel et al. presented data from the prospective,<br />
multicenter, randomized, Phase III StiL NHL1-2003 trial, which compared the combination of bendamustine<br />
(Treanda ® )-rituximab (Rituxan ® ) to R-CHOP (rituximab with cyclophosphamide [Cytoxan ® ], doxorubicin,<br />
vincristine, prednisone) in the first-line treatment of indolent lymphomas and mantle cell lymphoma (MCL) [1].<br />
In this study of 549 patients, bendamustine-rituximab significantly improved progression-free survival (PFS)<br />
and was better tolerated than R-CHOP. The median PFS with this regimen was 69.5 months compared to<br />
A subset analySIS of this trial,<br />
31.2 months with R-CHOP. In addition, the benefit of bendamustine-rituximab was observed in all histologic<br />
PRESENTED at ASH [2], shows<br />
subtypes except marginal zone lymphoma (MZL), including in both low-risk and high risk follicular lymphoma<br />
THAT patients who achievED<br />
(FL). No differences in the rates of secondary malignancies have been observed to date.<br />
a complete response (CR)<br />
FOLLOWING first-LINE treatment<br />
HAD a significantly longer<br />
oncologistics volume 12, issue 1 - spring 2013 30<br />
A subset analysis of this trial, presented at ASH [2],<br />
shows that patients who achieved a complete response<br />
(CR) following first-line treatment had a significantly longer<br />
PFS and overall survival (OS) compared to those who<br />
achieved only a partial response (PR), suggesting an<br />
association between quality of response and outcome.<br />
Overall, the results of StiL NHL1 establish bendamustinerituximab<br />
as a front-line regimen for indolent B cell non-<br />
Hodgkin lymphoma (NHL) and non-transplant-eligible<br />
MCL. More data on OS and potential long-term toxicities,<br />
including risk of myelodysplastic syndromes (MDS) and<br />
second primary cancers, are needed before determining<br />
whether B-R should be the preferred initial treatment.<br />
Detailed results from StiL NHL1 have been recently<br />
published on-line in Lancet Oncology.<br />
Final results from the MCL Younger Trial, conducted by<br />
the European Mantle Cell Lymphoma Network, were<br />
presented at this winter’s meeting by Hermine et al. [3].<br />
This randomized trial compared the following treatments<br />
in previously untreated MCL patients (N=497; stage II-IV)<br />
PFS and ovERALL survivAL<br />
(OS) compared to those<br />
WHO achievED only a partial<br />
RESPONSE (PR), suggesting an<br />
ASSOCIAT<strong>ION</strong> between quality of<br />
RESPONSE and outcome.<br />
oncologistics 31
industry insight<br />
oncologistics industry insight<br />
age 65 and younger:<br />
> 6 courses of R-CHOP followed by myeloablative<br />
radiochemotherapy and autologous stem cell<br />
transplant (ASCT)<br />
> Alternating courses of 3x R-CHOP and 3x R-DHAP<br />
(rituximab plus dexamethasone, high-dose cytarabine<br />
> 79.6% by FDG-PET (n=162) after 4 courses of R-DHAP<br />
(International Harmonization Project [IHP] criteria).<br />
> 89% by FDG-PET (n=121) after ASCT (IHP criteria).<br />
Response rates with R-DHAP followed by ASCT (without total<br />
body irradiation in the conditioning regimen) also compared<br />
Table 1: Phase II Study of Lenalidomide Plus Rituximab in Untreated, Advanced-Stage Indolent Non-Hodgkin<br />
Lymphoma: Response Rates<br />
Response<br />
Histology<br />
Follicular Lymphoma<br />
Marginal Zone<br />
Lymphoma<br />
Small Lymphocytic<br />
Lymphoma<br />
All Evaluable<br />
Patients<br />
[AraC, Cytosar-U ® ], and cisplatin [Platinol®]) followed<br />
by a high-dose cytarabine-containing myeloablative<br />
favorably with other chemotherapy regimens. However, the<br />
impact of this regimen in terms of event-free survival (EFS),<br />
(n=46)<br />
(n=27)<br />
(n=30)<br />
(N=103)<br />
radiochemotherapy regimen and ASCT<br />
The primary endpoint was time to treatment failure (TTF).<br />
PFS, and OS still needs to be investigated, as well as the<br />
role of transplant versus other consolidation strategies and<br />
maintenance therapy<br />
ORR 98% 89% 80% 90%<br />
CR/CRu 87% 67% 27% 64%<br />
PR 11% 22% 53% 25%<br />
ASCT was performed and documented at a similar rate<br />
in both arms (R-CHOP: 83% vs. R-DHAP: 80%), with a<br />
response rate of 98% in both arms after ASCT. In addition,<br />
Taken together, the results of the MCL Younger Trial and<br />
LyMa show that high-dose cytarabine and ASCT are<br />
important components of treatment in younger MCL patients.<br />
SD 2% 11% 13% 7%<br />
PD 0 0 7% 2%<br />
both induction arms achieved a similar rate of complete<br />
––<br />
Abbreviations: ORR=objective response rate; CR=complete response; CRu=complete response, unconfirmed;<br />
response (CR; R-CHOP: 62% vs. R-DHAP: 61%). With<br />
Several studies at ASH focused on the use of lenalidomide<br />
PR=partial response; PD=progressive disease (Source: Fowler et al. Proc ASH 2012; Abstract 901).<br />
a median follow up of 53 months, TTF was significantly<br />
(Revlimid ® ) in the treatment of lymphoma, further<br />
better with alternating courses of R-CHOP/R-DHAP than<br />
demonstrating that it is an active agent in follicular lymphoma<br />
with R-CHOP (88 months vs. 46 months, respectively;<br />
(FL) and MCL.<br />
p=0.0382, Hazard Ratio [HR]: 0.68), with benefits observed<br />
across all prognostic groups. The R-DHAP regimen was<br />
First, Fowler et al. presented the final results of a Phase II<br />
oncologistics volume 12, issue 1 - spring 2013 32<br />
also associated with improvement in overall survival (OS;<br />
not reached [NR] vs. NR, respectively; p=0.0485) and with<br />
achievement of minimal residual disease (MRD) negativity, a<br />
predictor of PFS. It also exhibited an acceptable safety profile.<br />
These final results demonstrate that alternating courses<br />
of R-CHOP/R-DHAP followed by a high dose cytarabinecontaining<br />
myeloablative regimen and ASCT significantly<br />
improves TTF, and that induction regimens containing high<br />
dose cytarabine followed by ASCT should become a new<br />
standard of care in younger MCL patients.<br />
The randomized, open-label, phase III LyMA study was<br />
conducted to evaluate the efficacy of rituximab maintenance<br />
therapy in younger MCL patients (ages 18-66 years)<br />
undergoing first-line treatment with 4 courses of R-DHAP<br />
and exhibiting a response after ASCT. An analysis of clinical,<br />
metabolic and molecular response data from this trial shows<br />
that R-DHAP induction alone prior to ASCT provides a high<br />
CR and CR unconfirmed (CR/CRu) rate, as demonstrated<br />
by both FDG-PET and assessment of MRD [4]. The CR/CRu<br />
rates by assessment criteria were:<br />
> 76.5% in the intent-to-treat population (n=199) after 4<br />
courses of R-DHAP (Cheson 99 criteria).<br />
study investigating lenalidomide plus rituximab for untreated,<br />
advanced-stage indolent non-Hodgkin lymphoma (NHL) [5].<br />
Patient histologies included FL, marginal zone lymphoma<br />
(MZL), and small lymphocytic lymphoma (SLL).<br />
Front-line lenalidomide and rituximab produced high<br />
overall and complete response rates (Table 1) with durable<br />
remissions in the majority of patients and a projected 3-year<br />
PFS of 81% in FL, 89% in MZL, and 66% in SLL.<br />
The toxicity profile of lenalidomide-rituximab was mild, with<br />
manageable hematologic side effects. Grade 3/4 neutropenia<br />
occurred in 41% of patients and thrombocytopenia<br />
occurred in 6% of patients. Five patients developed grade<br />
3 neutropenic fever. The most common grade 3/4 nonhematologic<br />
toxicities included muscle pain (8%), rash (7%),<br />
and fatigue (5%). Five secondary malignancies were reported.<br />
Phase III randomized trials investigating this combination in<br />
untreated FL are underway.<br />
The Phase II, multicenter, single-arm, open-label MCL-001<br />
EMERGE study investigated single-agent lenalidomide (25<br />
mg/d PO on days 1-21 of a 28-day cycle) in MCL patients<br />
who had relapsed on, progressed after, or were refractory<br />
to bortezomib (Velcade®) [6]. The primary endpoints were<br />
overall response rate (ORR) and duration of response.<br />
Lenalidomide demonstrated rapid and durable efficacy<br />
in MCL patients who had failed prior therapies, including<br />
bortezomib. In this heavily pretreated patient population<br />
(N=134; median prior therapies: 4), the ORR to singleagent<br />
lenalidomide was 28%, with a CR/CRu rate of 8% by<br />
independent central review. The median duration of response<br />
was 16.6 months and the median time to response was 2.2<br />
months. The median PFS was 4.0 months, while median OS<br />
was 19.0 months.<br />
The most frequent adverse event (≥ 5% grade 3/4) was<br />
myelosuppression, consistent with the known safety profile<br />
for lenalidomide in NHL.<br />
Based on these and other promising data, lenalidomide will<br />
likely become a standard approach for relapsed disease and<br />
for maintenance or consolidation therapy in MCL.<br />
Emerging data suggests that the addition of lenalidomide<br />
to R-CHOP is feasible and effective. In a Phase II study<br />
presented by Nowakowski et al., the combination of<br />
lenalidomide (25 mg day 1-10 of a 28 day cycle) with R-CHOP<br />
(R2CHOP) was shown to be well tolerated and effective as<br />
initial therapy for aggressive B-cell lymphomas [7]. In adults<br />
with newly diagnosed CD20 positive diffuse large B cell<br />
(DLBCL) or grade 3 FL (n=47), the ORR was 98%, CR was<br />
83%, and PR was 15%, and the addition of lenalidomide to<br />
R-CHOP also appeared to ameliorate the negative effect of<br />
the non-germinal center B-cell phenotype on outcome. The<br />
efficacy of this regimen also appears to be promising when<br />
compared to an R-CHOP treated historical cohort, with a<br />
12-month PFS of 73% for R2CHOP versus 62% for the casematched<br />
R-CHOP controls.<br />
R2CHOP was well tolerated, including in elderly patients.<br />
Grade 3/4 adverse events were mainly hematological.<br />
Although grade 4 neutropenia was common (70%), infectious<br />
complications were rare. Grade 4 thrombocytopenia<br />
occurred in 20% of patients without bleeding complications,<br />
and thrombosis occurred in 1 patient (1%), similar to the<br />
oncologistics 33
industry insight<br />
oncologistics industry insight<br />
risk reported for NHL patients. One death was reported<br />
(perforation/sepsis).<br />
Randomized trials are in progress to further evaluate<br />
R2CHOP in comparison to R-CHOP.<br />
Another interesting agent being investigated for lymphoma<br />
treatment is the orally administered Bruton’s tyrosine kinase<br />
(BTK) inhibitor, ibrutinib (PCI-32765), with several studies<br />
showing that the BCR pathway is highly targetable in B-cell<br />
malignancies. In a report by Fowler et al., long-term followup<br />
from a Phase I study of ibrutinib shows it to be active<br />
and well tolerated in relapsed FL [8]. In 9 patients who<br />
received a dose of 5 mg/kg/day or more, 3 CRs and 2 PRs<br />
were reported. The median duration of response among<br />
this group was 12.3 months and the median PFS was 19.6<br />
months. There was no cumulative toxicity with extended<br />
dosing, and response improved with continued treatment<br />
in some patients. Based on drug occupancy and clinical<br />
responses, a dose of 560 mg daily is recommended for<br />
future FL studies. Phase II studies in FL are currently being<br />
planned.<br />
In relapsed/refractory MCL, interim results from a Phase<br />
II study continue to show that ibrutinib (560mg daily in<br />
continuous 28-day cycles) is highly active in this population<br />
[9]. In the efficacy- evaluable participants (n=51), the<br />
ORR was 69% for all patients and was similar among<br />
both bortezomib-naïve (n=31) and bortezomib-exposed<br />
patients (n=20) (71% vs. 65%, respectively). Few grade 3/4<br />
hematologic adverse events were observed (n=61) included<br />
neutropenia (5%), febrile neutropenia (3%), anemia (3%),<br />
thrombocytopenia (3%), and pancytopenia (2%).<br />
Brentuximab vedotin (Adcetris ® ) is an anti-CD30<br />
monoclonal antibody conjugated by a protease-cleavable<br />
linker to a microtubule-disrupting agent, monomethyl<br />
auristatin E (MMAE). In an open-label, multicenter Phase I<br />
study in Hodgkin lymphoma, this agent was administered<br />
with standard ABVD therapy (doxorubicin [Adrimycin ® ],<br />
bleomycin [Blenoxane ® ], vinblastine [Velban ® ], and<br />
dacarbazine [DTIC-Dome ® ]) or a modified standard<br />
(AVD; adriamycin, vinblastine, and dacarbazine) [10].<br />
This study showed that brentuximab can be combined<br />
with AVD chemotherapy, but cannot be given<br />
concomitantly with bleomycin due to pulmonary toxicity.<br />
Aside from this, AVD combined with brentuximab<br />
appeared to be well tolerated with manageable adverse<br />
effects and a CR rate of 86% at the end of frontline<br />
therapy. The recommended regimen is 1.2 mg/<br />
kg brentuximab every 2 weeks combined with AVD.<br />
A multinational Phase III study is ongoing to assess<br />
brentuximab in combination with AVD compared to ABVD<br />
alone in treatment-naïve Hodgkin lymphoma patients.<br />
References<br />
1. Rummel MJ, Niederle N, Maschmeyer G, et al.<br />
Bendamustine plus rituximab (B-R) versus CHOP plus<br />
rituximab (CHOP-R) as first-line treatment in patients with<br />
indolent and mantle cell lymphomas (MCL): Updated results<br />
from the StiL NHL1 study. J Clin Oncol 30, 2012 (suppl;<br />
abstr 3).<br />
2. Rummel MJ, Niederle N, Maschmeyer G, et al. Subanalysis<br />
of the StiL NHL 1-2003 Study: Achievement of Complete<br />
Response with Bendamustine-Rituximab (B-R) and<br />
CHOP-R in the First-Line Treatment of Indolent and Mantle<br />
Cell Lymphomas Results in Superior Survival Compared to<br />
Partial Response. Proc ASH 2012; Abstract 2724.<br />
3. Hermine O, Hoster E, Walewski J, et al. Alternating Courses<br />
of 3x CHOP and 3x DHAP Plus Rituximab Followed by<br />
a High Dose ARA-C Containing Myeloablative Regimen<br />
and Autologous Stem Cell Transplantation (ASCT)<br />
Increases Overall Survival When Compared to 6 Courses<br />
of CHOP Plus Rituximab Followed by Myeloablative<br />
Radiochemotherapy and ASCT in Mantle Cell Lymphoma:<br />
Final Analysis of the MCL Younger Trial of the European<br />
Mantle Cell Lymphoma Network (MCL net). Proc ASH 2012;<br />
Abstract 151.<br />
4. Le Gouill S, Callanan M, Macintyre E, et al. Clinical,<br />
Metabolic and Molecular Responses After 4 Courses of<br />
R-DHAP and After Autologous Stem Cell Transplantation for<br />
Untreated Mantle Cell Lymphoma Patients Included in the<br />
LyMa Trial, a Lysa Study. Proc ASH 2012; Abstract 152.<br />
5. Fowler NH, Neelapu SS, Hagemeister FB, et al.<br />
Lenalidomide and Rituximab for Untreated Indolent<br />
Lymphoma: Final Results of a Phase II Study. Proc ASH<br />
2012; Abstract 901.<br />
6. Goy A, Sinha R, Williams ME, et al. Phase II Multicenter<br />
Study of Single-Agent Lenalidomide in Subjects with Mantle<br />
Cell Lymphoma Who Relapsed or Progressed After or Were<br />
Refractory to Bortezomib: The MCL-001 “EMERGE” Study.<br />
Proc ASH 2012; Abstract 905.<br />
7. Nowakowski GS, LaPlant BR, Craig Reeder C, et al.<br />
Combination of Lenalidomide with R-CHOP (R2CHOP) Is<br />
Well-Tolerated and Effective As Initial Therapy for Aggressive<br />
B-Cell Lymphomas - A Phase II Study. Proc ASH 2012;<br />
Abstract 689.<br />
8. Fowler NH, Advani RH, Sharman JP, et al. The Bruton’s<br />
Tyrosine Kinase Inhibitor Ibrutinib (PCI-32765) Is Active and<br />
Tolerated in Relapsed Follicular Lymphoma. Proc ASH 2012;<br />
Abstract 156.<br />
9. Wang M, Rule SA, Martin P, et al. Interim Results of an<br />
International, Multicenter, Phase 2 Study of Bruton’s<br />
Tyrosine Kinase (BTK) Inhibitor, Ibrutinib (PCI-32765), in<br />
Relapsed or Refractory Mantle Cell Lymphoma (MCL):<br />
Durable Efficacy and Tolerability with Longer Follow-up.<br />
Proc ASH 2012; Abstract 904.<br />
10. Ansell SM, Connors JM, Park SI, O’Meara MM, Younes A.<br />
Frontline Therapy with Brentuximab Vedotin Combined with<br />
ABVD or AVD in Patients with Newly Diagnosed Advanced<br />
Stage Hodgkin Lymphoma. Proc ASH 2012; Abstract 798.<br />
oncologistics volume 12, issue 1 - spring 2013 34<br />
Michael E. Williams, MD, ScM is byrd s. leavell<br />
professor of medicine chief, Hematologic Malignancies<br />
Section <strong>Hematology</strong>/Oncology Division, University of<br />
Virginia Cancer Center, Charlottesville, VA<br />
Disclosure: Grant support - Celgene, Cephalon,<br />
Genentech, Millennium; Pharmacyclics Consultant -<br />
Celgene, Genentech, Millennium, Pharmacyclics<br />
oncologistics 35
eimbursement watch<br />
oncologistics reimbursement watch<br />
GETTING READy FOR<br />
Health INSURANCE<br />
EXCHANGES<br />
By: Zachary Bridges<br />
Beginning in January of 2014, U.S. residents and small businesses will be able to purchase insurance<br />
coverage through newly created health insurance exchanges. Whether obtaining coverage for the first time or<br />
transitioning from an employer-sponsored insurance plan, patients purchasing coverage through one of the<br />
Qualified Health Plans (QHPs) sold through the exchanges will have a new benefit structure. A major concern<br />
expressed by the cancer community has been whether QHPs will provide access to the most appropriate<br />
oral and physician-administered therapies for individual patients.<br />
oncologistics volume 12, issue 1 - spring 2013 36<br />
Physicians rely on the drug margin revenue to cover<br />
It will be months before exchange plans publish<br />
their coverage criteria, formularies, and cost-sharing<br />
requirements. However, recent regulatory guidance gives<br />
some insights into how this coverage picture will look.<br />
Tracking these developments will give your practice an<br />
advantage in terms of helping your patients to select<br />
exchange plans that will enable them to continue on<br />
needed therapies and avoid obstacles that could impede<br />
access to care.<br />
BACKGROUND ON EXCHAnges<br />
Mandated by the Patient Protection & Affordable Care Act<br />
(ACA), health insurance exchanges are intended to be a<br />
marketplace where patients without access to affordable<br />
employer-sponsored health plans can purchase health<br />
insurance. The ACA requires that all QHPs offered<br />
through exchanges provide patients with a minimum level<br />
of coverage known as “essential health benefits” (EHBs).<br />
The EHB package includes coverage for 10 benefit<br />
categories such as prescription drugs.<br />
The required categories of essential health benefits (EHBs)<br />
for any plans sold through health insurance exchanges<br />
include the following: 1) ambulatory patient services<br />
(2) emergency services (3) hospitalization (4) maternity<br />
and newborn care (5) mental health and substance use<br />
disorder services including behavioral health treatment<br />
(6) prescription drugs (7) rehabilitative and habilitative<br />
services and devices (8) laboratory services (9) preventive<br />
and wellness services and chronic disease management<br />
and (10) pediatric services, including oral and vision care.<br />
THE required categories of essential health benefits<br />
(EHBs) for any plans sold through health insurance<br />
EXCHANGES include the following: 1) ambulatory patient<br />
SERvICES (2) emergency servICES (3) hospitalization (4)<br />
MATERNITy and newborn care (5) mental health and<br />
SUBSTANCE use disorder servICES including behavIORAL<br />
HEALTH treatment (6) prescription drugs (7) rehabilitative<br />
AND habilitative servICES and devICES (8) laboratory<br />
SERvICES (9) prevENTIve and wellness servICES and chronic<br />
DISEASE management and (10) pediatric servICES, including<br />
ORAL and vIS<strong>ION</strong> care.<br />
oncologistics 37
eimbursement watch<br />
oncologistics reimbursement watch<br />
In recent months, states had to select “benchmark plans”<br />
that will act as models for other QHPs operating in<br />
that state. The benchmarks were selected from the<br />
following options:<br />
> Largest plan by enrollment in any of the 3 largest<br />
small-group insurance products in a given state’s<br />
small-group market<br />
> Any of the 3 largest state employee health benefit<br />
plans by enrollment<br />
> Any of the 3 largest national Federal Employees<br />
Health Benefits Program (FEHBP) plan options<br />
> Largest insured commercial non-Medicaid HMO<br />
operating in a state<br />
class listed in the U.S. Pharmacopeia Medicare<br />
Model Guidelines for formularies, or<br />
> The same number of drugs in each category and<br />
class as the state’s benchmark plan<br />
That means there is some potential that an exchange<br />
plan may only have to cover a single therapy in a given<br />
drug class with no special exceptions for oncology<br />
or hematology. This is a significant change from the<br />
requirements for plans offering coverage to Medicare Part<br />
D beneficiaries: Part D plans are required to offer open<br />
access to products in 6 protected therapeutic classes,<br />
which include anti-cancer treatments.<br />
oncologistics volume 12, issue 1 - spring 2013 38<br />
For any states that did not select a benchmark, the U.S.<br />
Department of Health & Human Services (HHS) used the<br />
first criterium listed above as the default for selecting a<br />
plan. A full listing of the benchmark plans can be found<br />
at the Center for Consumer Information and Insurance<br />
website at http://cciio.cms.gov/.<br />
Open enrollment in the exchanges starts October 1,<br />
2013. Oncology and hematology practices may want to<br />
consider reviewing the formularies for the benchmark<br />
plan in their respective states now to gain insights into the<br />
coverage parameters for key therapies.<br />
ehb Final Rule<br />
In February 2013, HHS released additional regulations<br />
about the EHB package of benefits that will be offered<br />
in all QHPs. According to the EHB final rule, access in<br />
exchange plans can be defined in a couple ways, such as<br />
formulary offerings and patient cost sharing. The final rule<br />
established broad parameters to ensure QHPs provide<br />
access to clinically necessary treatments and outlined<br />
limitations on beneficiaries’ maximum deductibles and<br />
yearly out-of-pocket costs.<br />
Prescription Drug Coverage<br />
According to the final rule, exchange plans must cover the<br />
greater of:<br />
> One drug in every therapeutic category and<br />
However, similar to Part D, exchange plans will be<br />
required to implement procedures such as appeals or<br />
exceptions processes that will facilitate patient access to<br />
drugs that are not on a formulary. Additional regulatory<br />
guidance on this subject is pending. In the case of<br />
Medicare Part D plans, this often means that a physician<br />
must submit a letter explaining the clinical need for the<br />
patient to be on a specific, non-covered medication.<br />
Currently, many private insurance plans offer favorable<br />
access to anti-cancer drugs. That could bode well for<br />
coverage of oncology therapies under exchange plans,<br />
since one of the benchmark plan options for states<br />
was to select a popular plan sold in that state with a<br />
high enrollment.<br />
Cost-Sharing Requirements<br />
The limitations on patient cost sharing outlined in the final<br />
rule establish general parameters for annual deductibles<br />
and maximum out-of-pocket limits. However, the final rule<br />
did not address limits for patient out-of-pocket spending<br />
on prescription drugs. Beginning in January 2014, the<br />
maximum deductible an exchange plan can require is<br />
$2,000 for an individual or $4,000 for a family. Limits on<br />
annual out-of-pocket spending are $6,250 for individuals<br />
or $12,500 for families. However, cost-sharing and annual<br />
deductible limits for network benefit plans apply only<br />
for services furnished by participating providers. Costsharing<br />
for benefits furnished by out-of-network providers<br />
will not count towards these annual limitations. Thus,<br />
patients who obtain care from out-of-network providers could<br />
see higher costs.<br />
In not addressing the issue of prescription drug costs,<br />
HHS allowed states the flexibility to establish cost-sharing<br />
limitations within their exchanges. While the EHB final rules<br />
did not provide much insight on this topic, some states such<br />
as California have begun to release-more detailed regulations<br />
for participating QHPs. The regulations released provide<br />
specific benefit design details for plans that are purchased<br />
through the exchange named Covered California, and include<br />
cost-sharing information including, annual deductibles, office<br />
visit copayments, and prescription copayments for brand and<br />
generic drugs.<br />
What This Means for Your PrACtice<br />
and Patients<br />
HHS has left states with a certain level of flexibility to<br />
encourage new and innovative plan benefit designs.<br />
Considering that cost containment is a significant focus for<br />
the health insurance industry as a whole, it is reasonable<br />
to assume that plan structure and benefit designs<br />
available within the exchanges will follow suit. Utilizationmanagement<br />
strategies such as prior authorization, step<br />
therapy requirements, and tiered formularies will continue<br />
to be employed as a tool for managing high-cost specialty<br />
medications. It will be important for oncology and hematology<br />
practices to have an understanding of which oral and<br />
physician-administered therapies are covered under the major<br />
exchange plans in their region and also be familiar with any<br />
“state-required benefits.” One additional provision of the EHB<br />
final rule was that “state-required benefits” enacted on or<br />
before December 31, 2011, must be included in all QHPs. As<br />
2014 approaches, states may release more-clearly defined<br />
regulations for QHPs. Practices should monitor and review<br />
any and all state regulations for how they might impact their<br />
patients’ access to care.<br />
One of the primary goals of the ACA was to provide coverage<br />
options for the 55 million Americans who are currently<br />
uninsured. It is notable that of the 24 million Americans<br />
expected to enroll in exchange plans by 2016, 20 million are<br />
expected to qualify for income-based federal assistance<br />
that, depending on the recipients’ income levels, could range<br />
from tax subsidies to help with premiums; to cost-sharing<br />
assistance with deductibles, co-payments, or co-insurance;<br />
to additional limits on out-of-pocket spending. 1 However, even<br />
though assistance will be available for many if their incomes<br />
fall between 100% and 400% of the federal poverty level<br />
(FPL)* many exchange plan enrollees are still likely going to<br />
oncologistics 39
oncologistics volume 12, issue 1 - spring 2013 40<br />
reimbursement watch<br />
face challenges affording insurance and their share of the exchange plan enrollees, like their Medicare counterparts,<br />
costs of therapy. 2<br />
will have to seek cost-sharing support from independent,<br />
charitable copayment assistance foundations.<br />
*2013 Federal Poverty Guidelines 3<br />
Persons In Household Poverty Guideline<br />
1 $11,490<br />
2 $15,510<br />
3 $19,530<br />
4 $23,550<br />
5 $27,570<br />
6 $31,590<br />
7 $35,610<br />
8 $39,630<br />
1<br />
Congressional Budget Office’s February 2013 Estimate of the<br />
Effects of the Affordable Care Act on Health Insurance Coverage<br />
2<br />
Patient Protection and Affordable Care Act, Pub. L. No. 111-<br />
148, §1401, 124 Stat. 215 (2010).<br />
3<br />
78 Fed. Reg. 5183 (Jan 24, 2013) available at http://www.gpo.<br />
gov/fdsys/pkg/FR-2013-01-24/pdf/2013-01422.pdf.<br />
Just as they do now, underinsured patients will need<br />
access to sources of financial support so that healthcare<br />
costs do not adversely impact their compliance with<br />
therapy. It will be important for practices to keep abreast<br />
of new regulatory developments from bodies like the<br />
Office of the Inspector General (OIG), assistance program<br />
policies among manufacturers, and communications from<br />
charitable copayment foundations. For example, while<br />
many privately insured patients with high deductibles and<br />
copayments currently receive cost-sharing assistance<br />
TIPS FOR PRACTICES<br />
> Monitor new information from HHS, OIG, and your<br />
state regarding exchange plans, required benefits,<br />
cost-sharing, and patient eligibility for manufacturer<br />
assistance programs<br />
> Plan to contact charitable copay foundations,<br />
manufacturer copay card programs, and<br />
manufacturer patient assistance (free drug) programs<br />
toward the end of 2013 to verify whether they are<br />
planning any changes to their program policies and,<br />
in particular, how they plan to support patients who<br />
enroll in exchange plans<br />
> Review information from your specialty societies,<br />
group purchasing organizations, and patient<br />
advocacy groups to keep abreast of critical<br />
information related to healthcare reform<br />
implementation<br />
> Review details about your state’s exchange<br />
benchmark plan now to get a better sense of how<br />
other exchange plans that will be available in your<br />
state will cover key therapies<br />
Once your state selects the qualified health plans that<br />
will be sold in the exchanges, become familiar with those<br />
plans’ formularies, coverage policies, and cost-sharing<br />
requirements so you can be an effective source of<br />
information for your patients who are considering enrolling<br />
in an exchange plan.<br />
from branded copay cards offered by manufacturers,<br />
there has been no regulatory guidance issued on the<br />
subject of whether exchange plan enrollees will be eligible<br />
for such programs. In the absence of regulation, it means<br />
that manufacturers who offer brand copay assistance to<br />
exchange plan enrollees risk the possibility of violating<br />
federal anti-kickback rules. It is possible that underinsured<br />
Zachary Bridges is manager, Xcenda Reimbursement<br />
Strategy & Trends.<br />
CONGRESS:<br />
Fight Cancer.<br />
NOT Cancer Care.<br />
Thanks to advances in cancer care in America, lives are being<br />
saved everyday. But unfortunately, our nation is facing a crisis<br />
in cancer care that could negatively impact patient access, quality<br />
and availability of critical medications and therapies.<br />
Financial pressures resulting from repeated cuts to Medicare<br />
reimbursement for life-saving therapies are forcing some cancer<br />
centers to shut their doors.<br />
These closures have led to patient access challenges,<br />
clinical staff reductions and higher Medicare<br />
costs because of cancer patients seeking<br />
care in more expensive settings.<br />
Sequestration and some deficit reduction<br />
proposals further threaten America’s<br />
community cancer centers, cancer<br />
doctors and their vulnerable patients.<br />
Any more cuts to community cancer<br />
care must be stopped.<br />
While America’s<br />
cancer patients<br />
fight for their<br />
lives, let’s fight<br />
to protect their<br />
community<br />
cancer care.<br />
To learn more, visit www.communityoncology.org