Rehabilitation Care Pathway - East Midlands Cancer Network
Rehabilitation Care Pathway - East Midlands Cancer Network
Rehabilitation Care Pathway - East Midlands Cancer Network
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
National <strong>Cancer</strong> Action Team<br />
<strong>Rehabilitation</strong><br />
<strong>Care</strong> <strong>Pathway</strong><br />
Head & Neck
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Head & Neck<br />
Pre Diagnosis<br />
Drop Down <strong>Pathway</strong>s<br />
Anorexia & cachexia<br />
Dysphagia<br />
Fatigue & energy management<br />
PD1 Assessment<br />
a Assess respiratory, functional & mobility status and<br />
treat as necessary<br />
b Ensure optimum and timely access to specialist<br />
assessment & rehabilitation service for all patients.<br />
PD2 Cognitive & Psychological Factors<br />
a Assess & plan anxiety management programme in<br />
order to provide confidence for patient &/ or carers in<br />
management of condition & lifestyle<br />
PD3 Communication<br />
PD4 Information/Support<br />
a Provide information on role & scope of specific AHPs,<br />
referral process & development of therapeutic<br />
relationship<br />
b Advise on AHP clinic availability for patients requiring<br />
rapid access to supportive care<br />
PD5 Nutrition<br />
a Assess nutritional requirements & factors affecting<br />
potential nutritional status<br />
b Provide practical dietary advice<br />
c Influence organisational approach to provision of food<br />
PD6 Referral/Liaison<br />
a Refer to identified AHP for assessment<br />
b Refer using generic AHP/oncology assessment tool<br />
during assessment by medical/nursing/AHP staff doing<br />
the screening<br />
a As specific cancer symptoms emerge, undertake<br />
swallowing & communication assessment<br />
2
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Head & Neck<br />
Diagnosis & <strong>Care</strong> Planning<br />
Drop Down <strong>Pathway</strong>s<br />
Anorexia & cachexia<br />
Fatigue & energy management<br />
Mobility problems/ loss of function<br />
Dysphagia<br />
D1 Assessment<br />
a Undertake baseline holistic care assessment<br />
considering quality of life, anxiety & depression,<br />
smoking & alcohol use, lifestyle & treat as appropriate<br />
b Integrate with pre-treatment assessment & provide<br />
follow-up clinics<br />
c Support patient consent process<br />
d Ensure understanding of high risk patients & comorbidities<br />
e Assess speech, voice and swallowing<br />
D2 Communication<br />
a Establish case history, current extent of disease &<br />
proposed form of treatment.<br />
b Screen for communication difficulties<br />
c Liaise with previous AHPs, social services, PCT<br />
colleagues & provide AHP differential diagnosis<br />
d Provide pre-treatment AHP clinic<br />
e Assess current communication skills & level of cognitive<br />
functioning<br />
f Ensure onward appropriate referral to colleagues &<br />
other AHPs<br />
g Provide equipment &/ or intervention to support<br />
communication<br />
h Liaise with medical staff on proposed cancer treatment<br />
plan<br />
i surgical voice restoration (SVR) programme – advise<br />
surgeon on appropriate method of rehabilitation of<br />
communication<br />
j Provide prophylactic therapy programme before<br />
treatment starts<br />
k Link with other centres / teams on hand over of care<br />
l Facilitate contact with other patients & make referral<br />
to support groups<br />
m Provide information & ensure patient choice in<br />
decision of treatment (advocate)<br />
D3 Exercise & Physical Well Being<br />
a Optimise physical & respiratory fitness prior to<br />
treatment<br />
3
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Head & Neck<br />
D4 Nutrition<br />
a Influence organisational approach to provision of food<br />
b Implement nutritional screening<br />
c<br />
Assess nutritional requirements & status<br />
d Assess factors affecting nutritional intake<br />
e Assess patient’s circumstances & ability to act on<br />
dietetic and SLT advice<br />
f Provide practical dietary advice, including written<br />
information tailored to individual’s needs, prognosis &<br />
circumstances<br />
g Liaise with other health professionals in the oncology<br />
team<br />
h Provide ongoing monitoring & support to patient,<br />
family & carers<br />
i Draw up & review nutritional care plans to achieve<br />
optimal nutritional status<br />
j Where necessary, consider alternative methods of<br />
nutrition support & provide advice & support for<br />
health care professionals, patients & relatives<br />
D5 Referral/Liaison<br />
a Liaise with MDT on treatment planning and<br />
management of primary disease<br />
b Attend AHP led independent or combined clinic/<br />
appointment<br />
Treatment<br />
Drop Down <strong>Pathway</strong>s<br />
Anorexia / Cachexia<br />
Breathlessness<br />
Dysphagia<br />
Fatigue & energy management<br />
Lymphoedema<br />
Mobility problems/ loss of function<br />
Pain<br />
Intervention<br />
T1 Assessment<br />
a Provide ongoing holistic assessment of function,<br />
quality of life, anxiety & depression as appropriate<br />
b Assess respiratory status, functional status & mobility<br />
status<br />
c Assess mobility & provide treatment<br />
d Undertake musculoskeletal assessment<br />
e Carry out interventional assessments<br />
f Undertake joint dietetic & speech and language<br />
therapy assessments<br />
g Undertake assessment & provide rehabilitation for all<br />
patients with emergence of symptoms/ side effects<br />
affecting independent functional status<br />
4
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Head & Neck<br />
h Undertake pre-surgical assessment in clinic as<br />
appropriate<br />
i<br />
j<br />
Undertake instrumental assessments of communication<br />
& / or swallowing<br />
Carry out holistic communication assessment<br />
k Undertake airway assessment<br />
l<br />
Re assess swallow function & instigate dysphagia<br />
therapy (see dysphagia pathway)<br />
T2 Cognitive & Psychological Factors<br />
a Provide techniques to help manage anxiety and mood<br />
b Provide body image management<br />
T3 Communication<br />
a Re assess communication status<br />
b Work with MDT to ascertain the cause of speech,<br />
language, swallowing or voice difficulty<br />
c<br />
Check & analyse medical & surgical notes & decide on<br />
appropriate treatment plan<br />
d Attend theatre & liaise with surgeons on SVR<br />
techniques<br />
e Support, teach & advise relatives of appropriate<br />
communication channels<br />
f<br />
Provide equipment & materials and teach their use to<br />
patients and carers<br />
g Carry out voice, speech & communication therapy<br />
h Carry out videofluoroscopy X-ray if appropriate for<br />
investigation of poor voicing<br />
i<br />
j<br />
Liaise with family<br />
Liaise with local services<br />
k Liaise with MDT<br />
l Instigate the whole programme for surgical voice<br />
restoration (SVR) and prepare for voice prosthesis<br />
fitting including selection of appropriate prosthesis &<br />
preparation of patient<br />
m Fit voice prosthesis & teach patient, family, carers,<br />
nursing staff as appropriate about care & maintenance<br />
n Trouble shoot re voice prosthesis management & liaise<br />
with MDT<br />
o Give patient appropriate oro-motor range of motion &<br />
strengthening exercises in collaboration with the<br />
medical/surgical teams<br />
T4 Exercise & Physical Well Being<br />
a Teach exercises for neck, shoulder, facial,<br />
temperomandibular joint & any other area affected by<br />
plastic reconstruction to ensure reduction in pain,<br />
recovery of movement & improve function<br />
5
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Head & Neck<br />
b Advise on fibrosis pre treatment & treat if appropriate<br />
with soft tissue massage<br />
c<br />
Undertake musculo-skeletal assessment of neck and<br />
TMJ and treat as appropriate<br />
d Assess/ manage range of movement – assess any other<br />
musculoskeletal problems related to any plastic surgery<br />
e Advise on exercise programme in conjunction with SLT<br />
f<br />
Assess & treat facial nerve palsy<br />
g Advise on symptom control<br />
h Advise on support services<br />
T5 Nutrition<br />
a Manage rehabilitation for feeding tube dependent<br />
patients<br />
b Manage nutritional status<br />
c<br />
Start/continue nutritional support (oral/ enteral/<br />
parenteral nutrition)<br />
d Advise on specific diets<br />
e Provide advice on weaning from enteral tube feeding<br />
to oral diet<br />
f<br />
Provide education regarding feed tube management &<br />
the administration of feed<br />
g Coordinate enteral feeding tube discharges & ensure<br />
referral to community services for continued support<br />
h Provide on-going advice on diet, texture modification<br />
& quantity of food based on treatment side effects &<br />
nutritional status<br />
i Start/continue enteral nutritional support &<br />
management for type of feeding tube & on-going<br />
education regarding care<br />
j Liaise with home enteral feeding team for changes to<br />
feeding regime<br />
k Influence organisational approach to provision of food<br />
T6 Referral/Liaison<br />
a Refer to extended members of the team<br />
b Screen for facial problems & refer to other AHPs for<br />
assessment & management<br />
c Contribute to complex discharge planning as part of<br />
MDT<br />
d Ensure dedicated oncology specialist is made available<br />
for all head & neck patients<br />
e Identify complex discharge needs & instigate discharge<br />
planning in liaison with MDT in Assessment Clinic<br />
T7 Respiratory<br />
a Carry out respiratory assessment<br />
b Assist patient to manage respiratory function including<br />
tracheostomy care & weaning<br />
6
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Head & Neck<br />
c Identify patient with or without pre-existing<br />
respiratory disease if patient is to be referred for<br />
surgery<br />
d Commence chest physiotherapy to suit individual<br />
requirements<br />
e Advise on selection, care and use of laryngectomy<br />
tracheostoma valves<br />
f Advise on selection, use & care of laryngectomy stoma<br />
filters/ heat & moisture exchangers<br />
T8 Work, Leisure & Activities of Daily Living<br />
a Advise, assess, treat & support as indicated to maintain<br />
patient’s independence in all activities of daily living<br />
b Advise on compensatory techniques especially<br />
following major head & neck reconstructions<br />
c Assist patient to manage lifestyle & symptoms<br />
d Provide rehabilitation classes to help improve<br />
functional ability<br />
e Respond to variations in functional status<br />
f Maintain awareness of wider issues of cancer prognosis<br />
& the impact of treatment on self image<br />
g Provide ongoing monitoring<br />
Post Treatment<br />
Drop Down <strong>Pathway</strong>s<br />
Anorexia / Cachexia<br />
Dysphagia<br />
Fatigue & energy management<br />
Lymphoedema<br />
Pain<br />
Intervention<br />
PT1 Assessment<br />
a Provide outreach or locality based multi-disciplinary<br />
AHP team for ongoing monitoring & reassessment of<br />
needs in line with changing clinical condition/<br />
functional status at home<br />
b Undertake ongoing respiratory assessment & manage<br />
respiratory problems including tracheostomy care &<br />
weaning<br />
c Undertake mobility assessment & treat if appropriate<br />
d Assess for timely removal & coordination of procedure<br />
for removal of the feeding tube<br />
e Provide ongoing interventional assessment &<br />
therapeutic intervention for swallowing problems &<br />
communication disorders<br />
f Undertake joint dietetic & speech & language therapy<br />
assessments including communication status<br />
7
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Head & Neck<br />
PT2 Cognitive & Psychological Factors<br />
a Help provide psychological support on side effects of<br />
treatment & refer as necessary to psychological services<br />
PT3 Communication<br />
a Re-assess status of Surgical Voice Restoration<br />
b Change prosthesis when necessary and troubleshoot<br />
problems<br />
c<br />
Undertake assessment (endoscopy) & treat any<br />
identified vocal cord palsy/ dysfunction<br />
d Ensure out-patient follow up with specialist AHP<br />
e Train & provide support to local services<br />
f<br />
Agree protocol with family<br />
g Carry out assessment at X-ray for voice problems with<br />
laryngectomy patients & advise re appropriateness of<br />
Botox injections<br />
h Refer to self-help group<br />
i Continue oromotor range of motion, articulation &<br />
strengthening exercises to facilitate oral<br />
communication<br />
j Provide & maintain equipment and teach patients &<br />
carers appropriate use<br />
k Refer to other health care professionals for assessment<br />
as necessary<br />
l<br />
Advise MDT on signs of recurrence or complications &<br />
provide appropriate advice & interventions<br />
PT4 Exercise & Physical Well being<br />
a Provide exercises for neck, shoulder, facial,<br />
temperomandibular joint & relevant area of plastic<br />
reconstruction to ensure reduction in pain, return of<br />
movement & to improve function<br />
b Provide advice on scar management & posture<br />
PT5 Information/Support<br />
a Provide SLT led clinic session<br />
PT6 Nutrition<br />
a Continue to monitor nutritional status & manage<br />
symptoms secondary to treatment related symptoms<br />
b Provide rehabilitation for feeding tube dependent<br />
patients<br />
c Provide ongoing nutritional support & symptom<br />
control with weaning from enteral tube feeding to<br />
oral diet<br />
d Monitor ongoing changes to home enteral feeding<br />
needs & communicate with relevant individuals<br />
e Undertake joint dietetic & speech & language therapy<br />
assessments<br />
8
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Head & Neck<br />
PT7 Referral/Liaison<br />
a Attend MDT & contribute to discussions re ongoing<br />
treatment plan<br />
b Ensure AHP representation within the MDT Clinic<br />
(acute or community based)<br />
c<br />
Refer to outpatient physiotherapy with specific<br />
physical problems following treatment<br />
d Screen for facial problems & refer to AHPs for<br />
assessment & management<br />
e AHPs to liaise with keyworker<br />
f<br />
Refer to local support team<br />
g Communicate with relevant professionals involved in<br />
patient care<br />
h Ensure joint working between AHPs & CNS for<br />
intensive rehabilitation & ongoing assessment of<br />
quality of life, anxiety & depression as appropriate<br />
PT8 Work, Leisure & Activities of Daily<br />
Living<br />
a Respond to variations in functional status<br />
b Maintain awareness of wider issues of cancer prognosis<br />
& impact of surgery on self image<br />
c Provide ongoing monitoring & support to maintain<br />
patient’s independence in all activities of daily living<br />
Monitoring & Survivorship<br />
Drop Down <strong>Pathway</strong>s<br />
Anorexia / Cachexia<br />
Dysphagia<br />
Fatigue & energy management<br />
Lymphoedema<br />
Pain<br />
Poor Mobility and loss of function<br />
Intervention<br />
M1 Assessment<br />
a Provide ongoing assessment of quality of life, anxiety<br />
& depression as appropriate<br />
b Undertake interventional assessments<br />
c Undertake joint dietetic & speech & language therapy<br />
assessments<br />
M2 Cognitive and Psychological Factors<br />
a Complete holistic initial assessment including social,<br />
psychological, functional, cognitive & perceptual areas<br />
b Assess & plan anxiety management programme in<br />
order to provide confidence for patient &/ or carers in<br />
management of condition<br />
9
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Head & Neck<br />
M3 Communication<br />
a Check for signs of recurrence & deteriorating<br />
symptoms and refer to medical / surgical teams if<br />
concerned<br />
b Liaise with core MDT clinic on regular basis to review<br />
patient progress<br />
c Liaise with work environment re communication needs<br />
and aids<br />
d Select, provide and maintain communication aids<br />
e Liaise to provide financial support as appropriate<br />
f Provide ongoing support to PCT colleagues<br />
g Link with user partnership group<br />
h Undertake re-assessment of needs on a regular basis<br />
i Re-assess status of Surgical Voice Restoration (SVR)<br />
j Change prosthesis when necessary and troubleshoot<br />
problems<br />
k Carry out assessment at X-ray for voice problems with<br />
laryngectomy patients & advise re appropriateness of<br />
Botox injections<br />
l Provide & maintain equipment and teach patients &<br />
carers appropriate use<br />
m Refer to other health care professionals for assessment<br />
as necessary<br />
n Advise MDT on signs of recurrence or complications &<br />
provide appropriate advice & interventions<br />
M4 Information/Support<br />
a Encourage links to support groups<br />
b Manage longer term effects of treatment<br />
M5 Nutrition<br />
a Provide rehabilitation for feeding tube dependent<br />
patients<br />
b Influence organisational approach to provision of food<br />
M6 Referral/ Liaison<br />
a Attend MDT & make recommendations on changing<br />
treatment plan<br />
b Support patients to re-engage in graded social<br />
activities<br />
M7 Work, Leisure & Activities of Daily<br />
Living<br />
a Advise on maintaining role at work or re-engaging in<br />
work place<br />
b Support patients to re-engage in graded social<br />
activities<br />
c Encourage lifestyle modifications<br />
d Assess patients for needs such as psychological support<br />
& other support groups<br />
10
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Palliative & EOL<br />
Palliative <strong>Care</strong><br />
Drop Down <strong>Pathway</strong>s<br />
Anorexia/cachexia<br />
Breathlessness<br />
Communication<br />
Dysphagia<br />
Fatigue<br />
Lymphoedema<br />
Pain<br />
Mobility & loss of function<br />
Spinal cord compression<br />
Intervention<br />
P1 Assessment<br />
a Carry out comprehensive social assessment<br />
b Undertake functional assessment<br />
c Undertake assessment of cognitive & psychological<br />
ability<br />
d Undertake holistic needs assessment<br />
e Provide ongoing assessment of quality of life, anxiety<br />
& depression, psychological & social needs as<br />
appropriate<br />
f Provide ongoing assessment and feedback to multidisciplinary<br />
team about symptoms such as pain,<br />
breathlessness, fatigue, depression, low mood<br />
g Agree patient centred goals<br />
P2 Cognitive & Psychological Factors<br />
a Assess & assist in management of anxiety & refer on to<br />
appropriate specialist<br />
b Provide anxiety management, relaxation & structured<br />
sleep strategies<br />
c Manage mood through compensatory strategies &<br />
engagement in meaningful occupations<br />
d Retrain and/or educate as necessary in order to help<br />
patient with cognitive & perceptual dysfunction<br />
e Identify psychological needs & provide psychological<br />
support to patients & carers<br />
P3 Communication<br />
a Assess communication skills and capacity to make<br />
informed decisions<br />
b Assess ability to communicate/ convey needs relating to<br />
pain, care, place of death & drawing up will<br />
c Educate patient, carers and healthcare professionals on<br />
optimal communication methods for individual patient<br />
d Implement communication strategies to optimise<br />
communication function<br />
e Trial, prescribe and train in use of communication aids<br />
if required<br />
11
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Palliative & EOL<br />
P4 Exercise & Physical Well Being<br />
a Assess current function, mobility, muscle power,<br />
fatigue and general weakness<br />
b Apply restorative or compensatory therapy<br />
interventions where appropriate<br />
c<br />
Advise on pacing, relaxation and controlled exercise<br />
d Provide exercise classes to maintain/improve physical<br />
and psychological functioning and quality of life taking<br />
into account variations in health status<br />
P5 Equipment Provision<br />
a Provide aids/ equipment to support daily living & self<br />
management techniques to optimise management of<br />
activities of daily living<br />
P6 Fatigue<br />
a Assessment and intervention as appropriate with<br />
energy conservation techniques, goal planning, pacing,<br />
diet, exercise and anxiety management<br />
b Ensure treatable causes of fatigue are ruled out by<br />
referral to other disciplines<br />
P7 Information/ Support<br />
a Ensure good communication and coordination<br />
between the various care settings and professions<br />
b Be involved in discussions on preferred priorities and<br />
place of care<br />
c Provide education & support to patient, family & carers<br />
d Provide information prescription & leaflet with links to<br />
charities & support groups<br />
e Enable informed decision making with regards to<br />
treatment & management<br />
f Consider ethical issues & goals of treatment to improve<br />
quality of life<br />
P8 Mobility<br />
a Assess mobility including function, strength, sensation,<br />
joint range, coordination and potential risks (refer to<br />
mobility and loss of function pathway)<br />
b Stabilise/immobilise unstable areas using braces, splints<br />
and positioning<br />
c Help patient to optimise function & assess risk assisting<br />
with activities for the treatment of physical<br />
dysfunction, impaired motor, sensory & self<br />
maintenance skills<br />
d Carry out wheelchair assessment & prescription<br />
including associated pressure relieving cushions<br />
e Assess for specialist & complex seating and/ or<br />
positioning in bed<br />
f Carry out manual handling training & assessment<br />
g Assess the need for and provide hoists at home<br />
12
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Palliative & EOL<br />
P9 Nutrition<br />
a Implement nutritional screening at each outpatient<br />
visit/ inpatient admission & refer on to dietitian as<br />
appropriate<br />
b Assess nutritional status & consider nutritional<br />
requirements if appropriate formulating a nutritional<br />
care plan for the patient<br />
c Assess factors affecting nutritional intake & barriers to<br />
optimising nutritional intake & quality of life<br />
d Provide practical nutritional advice including written<br />
information tailored to individuals needs, prognosis &<br />
circumstances<br />
e Consider modified consistency diet for palliative stents<br />
f Implement dietary adaptations to optimise nutrition<br />
related symptom management<br />
g Advise on symptom management, taste changes,<br />
nausea, vomiting, mouth care etc to help improve<br />
quality of life and liaise with palliative/ medical/<br />
nursing team regarding pharmacological management<br />
of symptoms<br />
h Work with family on understanding of & anxiety about<br />
eating & drinking<br />
i Provide dietetic monitoring & follow up including<br />
discharge planning of enterally fed patients where<br />
appropriate<br />
P10 Pain Management<br />
a Identify pain issues and apply non pharmacological<br />
pain management techniques (refer to pain pathway)<br />
P11 Referral/ Liaison<br />
a Refer on to other members of the team if appropriate<br />
b Signpost to other supportive care services as required<br />
dependent on need<br />
c Liaise with multi-disciplinary team and allocate key<br />
worker<br />
d Issues relating to sexual function and expression should<br />
be referred to the most appropriate local specialist<br />
P12 Respiratory<br />
a Maintain optimal respiratory function<br />
b Provide non-pharmacological management of<br />
breathlessness (refer to breathlessness pathway)<br />
P13 Skin <strong>Care</strong><br />
a Manage sensory impairment and tissue viability,<br />
lymphoedema and lymphorrhoea as appropriate (refer<br />
to lymphoedema pathway)<br />
13
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Palliative & EOL<br />
P14 Swallowing<br />
a Assess swallow function and monitor regularly for<br />
change<br />
b Manage any dysphagia via compensatory strategies<br />
and/or direct intervention (refer dysphagia pathway)<br />
P15 Work, Leisure & Activities of Daily<br />
Living<br />
a Discuss lifestyle adjustment including roles, loss & self<br />
esteem<br />
b Assess impact illness has on occupational pursuits<br />
c Help patient to manage lifestyle including<br />
investigating meaningful hobbies, leisure, occupational<br />
pursuits and driving<br />
d Undertake environmental and functional assessment<br />
e Assess and support patient to carry out personal care<br />
and domestic activities<br />
f Provide aids/ equipment to support daily living, & self<br />
management techniques to optimise independent<br />
activities of daily living<br />
End of Life<br />
Drop Down <strong>Pathway</strong>s<br />
Anorexia/cachexia<br />
Breathlessness<br />
Communication<br />
Dysphagia<br />
Fatigue<br />
Lymphoedema<br />
Pain<br />
Mobility & loss of function<br />
Spinal cord compression<br />
Intervention<br />
E1 Assessment<br />
a Carry out comprehensive social and functional<br />
assessment<br />
b Assess functional & cognitive ability<br />
c Assess & assist in management of anxiety & refer on to<br />
appropriate specialist<br />
d Undertake holistic needs assessment<br />
14
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Palliative & EOL<br />
E2 Cognitive & Psychological Factors<br />
a Identify psychological needs<br />
b Undertake pre bereavement work with family<br />
c<br />
Apply spiritual care taking multi-disciplinary team<br />
approach<br />
d Provide ongoing psychological support with regards to<br />
adjusting to loss, deteriorating function, grief response<br />
e Assist in management of low moods<br />
f<br />
Apply sleep and relaxation techniques<br />
g Apply restorative or compensatory therapy<br />
interventions<br />
E4 Equipment Provision<br />
a Provide mobility aids for safe moving & handling if<br />
appropriate and manage deteriorating function<br />
E5 Fatigue<br />
a Assessment and intervention as appropriate with<br />
energy conservation techniques, goal planning, pacing,<br />
diet, exercise and anxiety management (refer to<br />
fatigue care pathway)<br />
b Ensure treatable causes of fatigue are ruled out by<br />
referral to other disciplines<br />
E3 Communication<br />
a Assess communication skills and capacity to make<br />
informed decisions<br />
b Assess ability to communicate/ convey needs relating to<br />
pain, care, place of death & drawing up will<br />
c<br />
Educate patient, carers and healthcare professionals on<br />
optimal communication methods for individual patient<br />
d Implement communication strategies to optimise<br />
communication function<br />
e Trial, prescribe and train in use of communication aids<br />
if required<br />
E6 Information/ Support<br />
a Ensure good communication and coordination<br />
between the various care settings and professions<br />
b Provide education & support to carers<br />
c Provide information prescription<br />
d Consider sudden events, scenario planning<br />
e Identify and help to facilitate preferred place of care<br />
(preferred place of dying) where this is home<br />
f Attend case conferences when complex discharge is<br />
apparent<br />
g With the MDT/key worker, identify the dying process<br />
and implement Liverpool <strong>Care</strong> <strong>Pathway</strong> ensuring that<br />
unnecessary and invasive treatment is avoided<br />
15
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Palliative & EOL<br />
E7 Mobility<br />
a Carry out risk assessment to optimise comfort (refer to<br />
mobility and loss of function pathway)<br />
b Prevent complications of inactivity<br />
c<br />
Provide seating, position & manual handling advice for<br />
patient & carers<br />
E8 Nutrition<br />
a Influence organisational approach to provision of food<br />
b Assess patients nutritional status, history & recent<br />
history & oral intake<br />
c<br />
Address concerns expressed by patient and their family<br />
regarding food and fluids.<br />
d Implement dietary adaptations to optimise nutrition<br />
related symptom management<br />
e Address feeding & hydration issues with patient, carer<br />
& relatives, MDT in conjunction with palliative care/<br />
medical team<br />
f Advise & encourage on mouth care strategies to<br />
reduce the use of artificial hydration<br />
g Make decisions with multi-disciplinary team around<br />
ethics for feeding & feeding withdrawal<br />
E9 Referral/ Liaison<br />
a Multi-disciplinary team liaison/ referral to other<br />
specialist professions<br />
b Address & support symptom control & quality of life<br />
issues as appropriate on an individual basis in<br />
conjunction with Palliative <strong>Care</strong> MDT, carers, patients &<br />
relatives<br />
c Ensure appropriate withdrawal of intervention in<br />
liaison with multi-disciplinary team<br />
d Show awareness of advance of symptoms, need for<br />
further palliative/ surgical intervention such as<br />
paracentesis, stenting & debulking & how this further<br />
affects quality of life<br />
E10 Respiratory<br />
a Apply breathing strategies (refer to breathlessness<br />
pathway)<br />
b Carry out respiratory & airway management<br />
16
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Palliative & EOL<br />
E11 Skin <strong>Care</strong><br />
a Assess positioning & provide simple<br />
massage/movement/comfort measures<br />
b Identify soft tissue viability & refer on as necessary<br />
c<br />
Assess & manage sensory changes and advise on<br />
suitable clothing<br />
d Manage ascites as appropriate<br />
e Manage lymphorrhoea (refer to lymphoedema<br />
pathway)<br />
E13 Work, Leisure & Activities of Daily<br />
Living<br />
a Undertake environmental and functional assessment<br />
b Manage deteriorating function<br />
c Assess and support patient to carry out personal care<br />
and domestic activities<br />
d Provide aids/ equipment to support daily living, & self<br />
management techniques to optimise independent<br />
activities of daily living<br />
E12 Swallowing<br />
a Assess swallow function and monitor regularly for<br />
change<br />
b Manage any dysphagia via compensatory strategies<br />
and in accordance with patients wishes (refer to<br />
dysphagia pathway)<br />
17
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Head & Neck<br />
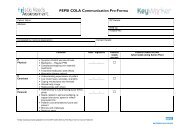
Professional intervention matrix<br />
The rehabilitation interventions listed in the care<br />
pathways can either be carried out by a single profession<br />
or could be carried out by a number of professions. There<br />
is the potential for different professions to be involved in<br />
delivering some of the interventions for a number of<br />
reasons.<br />
• Unique skills are required which are within the scope<br />
of a single allied health profession eg videofluoroscopy<br />
is only carried out by Speech and Language Therapists<br />
• The intervention listed may be approached in different<br />
ways. For example P9b (Assess the factors affecting<br />
nutritional intake and barriers to optimising<br />
nutritional intake and quality of life) could involve:<br />
• the Dietitian focusing of nutritional intake and<br />
physiological barriers.<br />
• the Occupational Therapist focusing on cutlery,<br />
seating position and equipment that may help<br />
during feeding and<br />
• the Physiotherapist looking at postural stability and<br />
physical capacity<br />
SALT – Speech and Language Therapists<br />
OT – Occupational Therapy<br />
Other – Other professions including Clinical Nurse<br />
Specialists, Lymphoedema Practitioners<br />
18
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Head & Neck<br />
AHP<br />
Intervention Number<br />
Physio PD1 (a/ b)<br />
PD4 (a/ b)<br />
PD6 (a/ b)<br />
D1 (a/ b/ c/<br />
d)<br />
D2 (a)<br />
D3 (a)<br />
D5 (a/ b)<br />
T1 (b/ c/ d/ e/<br />
g/ h,k)<br />
T4 (a/ b/ c/ d<br />
/e/ f/ g/ h)<br />
T6 (a/ b)<br />
T7 (a/ b/ c/ d)<br />
T8 (a/ b/ c/ d/<br />
e/ f/ g)<br />
PT1 (a/ b/ c)<br />
PT4 (a/ b)<br />
PT7 (a/ b/ c/ d/<br />
e/ f/ g/ h)<br />
PT8 (a/ b / c)<br />
M1 (a/ b)<br />
M4 (a/ b)<br />
M6 (a)<br />
M7 (c/ d)<br />
P1 (a/ b/ c/ d/ e/ f/ g)<br />
P2 (a/ e)<br />
P4 (a/ b/ c/ d)<br />
P5 (a)<br />
P6 (a/ b)<br />
P7 (a/ b/ c/ d/ e/ f)<br />
P8 (a/ b/ c/ d/ e/ f/ g)<br />
P10 (a)<br />
P11 (a/ b/ c/ d)<br />
P12 (a/ b)<br />
P13 (a)<br />
P15 (d/ e/ f)<br />
E1 (a/ b/ c/ d)<br />
E2 (a/ b/ c/ d/ e/ f)<br />
E3 (a/ b/ c/ d)<br />
E4 (a)<br />
E5 (a/ b)<br />
E6 (a/ b/ c/ d/ e/ f/ g)<br />
E7 (a/ b)<br />
E9 (a/ b/ c/ d)<br />
E10 (a/ b)<br />
E11 (a/ b)<br />
E13 (b/ d)<br />
OT PD1 (a/ b)<br />
PD2 (a)<br />
PD4 (a/ b)<br />
PD6 (a/ b)<br />
D1 (a/ b/ c/<br />
d)<br />
D5 (a/ b)<br />
T1 (a/ c/ e/ g/<br />
h)<br />
T2 (a/ b)<br />
T5 (a)<br />
T6 (a/ c/ d/ e)<br />
T8 (a/ b/ c/ d/<br />
e/ f/ g)<br />
PT1 (a/ c)<br />
PT2 (a)<br />
PT7 (a/ b/ e/ f/<br />
g)<br />
PT8 (a/ b/ c)<br />
M1 (a/ b)<br />
M2 (a/ b)<br />
M4 (a/ b)<br />
M6 (a)<br />
M7 (a/ b/<br />
c/ d)<br />
P1 (a/ b/ c/ d/ e/ f/ g)<br />
P2 (a/ b/ c/ d/ e)<br />
P3 (a)<br />
P4 (a/ b/ c/ d)<br />
P5 (a)<br />
P6 (a/ b)<br />
P7 (a/ b/ c/ d/ e/ f)<br />
P8 (a/ b/ c/ d/ e/ f/ g)<br />
P9 (a/ b/ c/ h)<br />
P10 (a)<br />
P11 (a/ b/ c/ d)<br />
P12 (b)<br />
P13 (a)<br />
P15 (a/ b/ c/ d/ e/ f)<br />
E1 (a/ b/ c/ d)<br />
E2 (a/ b/ c/ d/ e/ f/ g)<br />
E3 (a/ b/ c/ d/ e)<br />
E4 (a)<br />
E5 (a/ b)<br />
E6 (a/ b/ c/ d/ e/ f/ g)<br />
E7 (a/ b/ c)<br />
E8 (c/ e)<br />
E9 (a/ b/ c/ d)<br />
E11 (a/ b/ c/ d)<br />
E13 (a/ b/ c/ d)<br />
19
<strong>Rehabilitation</strong> <strong>Care</strong> <strong>Pathway</strong> Head & Neck<br />
AHP<br />
Intervention Number<br />
Dietetic<br />
PD1 (b)<br />
PD4 (a/ b)<br />
PD5 (a/ b/<br />
c)<br />
PD6 (a/ b)<br />
D1 (a/ b/ c/<br />
d)<br />
D4 (a/ b/ c/<br />
d/ e/ f/ g/<br />
h/ i/ j)<br />
D5 (a/ b)<br />
T1 (e/ f/ h)<br />
T5 (a/ b/ c/ d/<br />
e/ f/ g/ h/ i/ j/<br />
k)<br />
T6 (a/ c/ d)<br />
T8 (a/ b/ c)<br />
PT1 (a/ d/ f)<br />
PT6 (a/ b/ c/ d/<br />
e)<br />
PT7 (a/ b/ e/ f/<br />
g/ h)<br />
PT8 (b)<br />
M1 (a/ b/ c)<br />
M4 (a/ b)<br />
M5 (a/ b)<br />
M6 (a)<br />
P1 (d/ e/ f/ g)<br />
P2 (a/ e)<br />
P5 (a)<br />
P6 (a)<br />
P7 (a/ b/ c/ d/ e/ f)<br />
P9 (a/ b/ c/ d/ e/ f/<br />
g/ h/ i)<br />
P11 (a/ b/ c)<br />
P15 (a/ b/ c)<br />
E1 (b/c)<br />
E2 (a/ b/ c/ d/ e/ f)<br />
E3 (a/b)<br />
E6 (a/ b/ c/ d/ e/ f/ g)<br />
E8 (a/ b/ c/ d/ e/ f/ g)<br />
E9 (a/ b/ c/ d)<br />
E11 (d)<br />
SALT<br />
PD1 (b)<br />
PD3 (a)<br />
PD4 (a/ b)<br />
PD6 (a)<br />
D1 (a,b/ c/<br />
d/ e)<br />
D2 (a/ b/ c/<br />
d/ e/ f/ g/<br />
h/ i/ j/ k/ l/<br />
m)<br />
D4<br />
d,e,g,h,j<br />
D5 (a/ b)<br />
T1 (a, e/ f/ g/<br />
h/ i/ j/ k, l)<br />
T2 a,b<br />
T3 (a/ b/ c/ d/<br />
e/ f/ g/ h/ i/ j/<br />
k/ l/ m/ n/ o)<br />
T4 (e/ f/ g/ h)<br />
T5 a,c,d,e,h<br />
T6 (a/ b/ c/ d/<br />
e)<br />
T7 b,e,f<br />
T8 (a/ e,f,g)<br />
PT1 (a/ b/ d/ e/<br />
f)<br />
PT2 (a)<br />
PT3 (a/ b/ c/ d/<br />
e/ f/ g/ h/ i/ j/ k/<br />
l)<br />
PT4 (a)<br />
PT5 (a)<br />
PT6 (a,b,c/ e)<br />
PT7 (a/ b/ d/ e/<br />
f/ g/ h)<br />
PT8 (a,b,c)<br />
M1 (a/ b/ c)<br />
M2 a<br />
M3 (a/ b/ c/ d/<br />
f/<br />
g,h,i,j,k,l,m,n)<br />
M4 (a/ b)<br />
M5 (a,b)<br />
M6 (a)<br />
M7 (a/ b/ c/ d)<br />
P1 (b/ d/ e/ f/ g)<br />
P2 (a/ e)<br />
P3 (a/ b/ c/ d/ e)<br />
P7 (a/ b/ c/ d/ e/ f)<br />
P9 (a/ c/ g/ h)<br />
P11 (a/ b/ c)<br />
P14 (a/ b)<br />
P15 (a/ b)<br />
E1 (b/ c/ d)<br />
E2 (a/ b/ c/ d/ e/ f/ g)<br />
E3 (a/ b/ c/ d/ e)<br />
E6 (a/ b/ c/ d/ e/ f/ g)<br />
E8 (c/ d/ e/ f/ g)<br />
E9 (a/ b/ c/ d)<br />
E12 (a/ b)<br />
Other<br />
PD1 (b)<br />
PD4 (a/ b)<br />
PD6 (a/ b)<br />
D1 (b/ c/<br />
d)<br />
D5 (a/ b)<br />
T1 (e/ h)<br />
T5 (a/ b)<br />
T7 (a/ c/ e,f)<br />
PT1 (a)<br />
PT7 (a/ b/ e/ f/<br />
g)<br />
PT8 (b)<br />
M1 (b)<br />
M3 (a/ b)<br />
M5 (a)<br />
P1 (d/ e/ f/ g)<br />
P2 (a/ e)<br />
P7 (a/ b/ c/ d/ e/ f)<br />
P8 (h)<br />
P11 (a/ b/ c)<br />
P13 (a)<br />
E1 (a/ b/ c)<br />
E2 (a/ b/ c/ d/ e/ f)<br />
E3 (a/ b/ c/ d)<br />
E6 (a/ b/ c/ d/ e/ f/ g)<br />
E9 (a/ b/ c/ d)<br />
E11 (a/ b/ e)<br />
E13 (b)<br />
20
National <strong>Cancer</strong> Action Team<br />
Designed and produced by Cynergy www.cynergy.co.uk<br />
All rights reserved © Crown Copyright 2009 National <strong>Cancer</strong> Action Team