LB2882MaternalNutriti+ - Mead Johnson Nutrition
LB2882MaternalNutriti+ - Mead Johnson Nutrition
LB2882MaternalNutriti+ - Mead Johnson Nutrition
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
MATERNAL NUTRITION<br />
bY<br />
Elizabeth M. Ward, M.S., R.D.<br />
EDITED bY<br />
Anna Maria Siega-Riz, Ph.D., R.D.<br />
WITH<br />
Julia Boettcher, M.Ed., R.D.<br />
Elisha London, R.D.<br />
Brittney Drone, B.S.
IFC
TAbLE OF CONTENTS<br />
EXECUTIVE SUMMARY . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3<br />
INTRODUCTION . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5<br />
NUTRITION BEFORE PREGNANCY . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6<br />
Pre-pregnancy Body Weight and Pregnancy Outcome . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6<br />
Preconception Diabetes and Pregnancy Outcome. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6<br />
Preconception Care. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7<br />
NUTRITION DURING PREGNANCY AND LACTATION . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7<br />
Pregnancy Weight Gain Guidelines . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7<br />
Nutrient Needs during Pregnancy and Lactation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9<br />
Energy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9<br />
Carbohydrate . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10<br />
Protein . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10<br />
Fat . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11<br />
Vitamins . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13<br />
Folate and Folic Acid . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15<br />
Vitamin B12 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15<br />
Choline . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15<br />
Vitamin A . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16<br />
Vitamin D . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17<br />
Minerals . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17<br />
Iron . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19<br />
Calcium . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20<br />
Zinc . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20<br />
Iodine . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21<br />
Multivitamin Use during Pregnancy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21<br />
DESIGNING HEALTHY LIFESTYLE PLANS FOR WOMEN IN THE CHILDBEARING YEARS . . . . . . . . . . . . . . . . . 22<br />
Guides to Healthy Eating . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 22<br />
Guidelines for Physical Activity during Pregnancy and Lactation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 23<br />
ALCOHOL, CAFFEINE, AND OTHER FOOD SAFETY ISSUES IN WOMEN OF CHILDBEARING AGE . . . . . . . . . . 24<br />
Alcohol . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 24<br />
Caffeine . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 24<br />
FOOD SAFETY ISSUES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 25<br />
Fish and Seafood . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 25<br />
Foodborne Pathogens . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 25<br />
PREGNANCY-ASSOCIATED CONDITIONS AND POSSIBLE DIET AND LIFESTYLE INTERVENTIONS . . . . . . . . . 26<br />
Nausea, Vomiting, and Hyperemesis Gravidarum . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26<br />
Hypertensive Disease . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26<br />
Gestational Diabetes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 27<br />
Preterm Birth . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28<br />
1
CONCLUSION . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28<br />
REFERENCES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 30<br />
LIST OF FIGURES<br />
Figure 1. Differences in Vitamin Intake Recommendations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14<br />
Figure 2. Differences in Mineral Intake Recommendations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18<br />
LIST OF TAbLES<br />
Table 1. Criteria for Classifi cations of Pre-pregnancy Weight Status BMI (kg/m 2 ). . . . . . . . . . . . . . . . . . . . . . . . . . 8<br />
Table 2. Recommended Weight Gain for Pregnant Women . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8<br />
Table 3. Recommended Weekly Rate of Weight Gain for Singleton Pregnancies, 2nd and 3rd Trimesters . . . . . . . 8<br />
Table 4. Recommendations for Additional Daily Calorie Intake during Pregnancy and Lactation . . . . . . . . . . . . . 10<br />
Table 5. Protein Recommendations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11<br />
Table 6. Recommended Intakes for LCPUFA during Pregnancy and Lactation . . . . . . . . . . . . . . . . . . . . . . . . . . 12<br />
Table 7. Selected Food Sources of DHA . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13<br />
Table 8. Recommended Vitamin Intakes for Women during Pregnancy and Lactation, Ages 19 to 50 years . . . . 14<br />
Table 9. Recommended Mineral Intakes for Women during Pregnancy and Lactation, Ages 19 to 50 years . . . . 18<br />
Table 10. WHO Recommended Nutrient Intakes for Zinc during Pregnancy and Lactation . . . . . . . . . . . . . . . . . . 21<br />
Table 11. Selected Sources of Caffeine . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 24<br />
Table 12. Selected Foodborne Pathogens and Risks to Maternal and Fetal Health . . . . . . . . . . . . . . . . . . . . . . . . 26<br />
MATERNAL NUTRITION 2
EXECUTIVE SUMMARY<br />
A mother’s nutritional status, diet and lifestyle influence pregnancy and lactation outcomes and can have lasting<br />
effects on her offspring’s health. This monograph reviews current nutrition and nutrition-related recommendations for<br />
women during pregnancy and lactation. The goal in highlighting these recommendations is to increase familiarity with<br />
nutrients and nutrition-related issues that can have an important impact during pregnancy, lactation, and beyond.<br />
Experts around the world increasingly emphasize the importance of providing preconception health services that<br />
include screening for health risks that could affect the outcome of a future pregnancy. 1,2 Women should be counseled<br />
regarding the benefits of achieving a healthy weight prior to pregnancy, regular physical activity, consuming a<br />
balanced diet with adequate folic acid, and controlling preexisting medical conditions, such as diabetes, along with<br />
other factors that influence pregnancy outcome. 2<br />
To help optimize conception and pregnancy outcomes, women should strive to enter pregnancy with a Body Mass<br />
Index (BMI) within the normal range (18.5 to 24.9 kg/m 2 ). 3 Weight-gain and weight-monitoring recommendations<br />
during pregnancy vary around the world 4 and women should follow recommendations endorsed by experts in their<br />
countries. In 2009, the Institute of Medicine (IOM) in the United States updated its pregnancy weight gain guidelines<br />
as a result of rising obesity rates, the large proportion of women with high gestational weight gain, and the strength<br />
of the evidence linking gestational weight gain to certain adverse outcomes. 3 The recommended weight gain ranges<br />
vary significantly according to a woman’s pre-pregnancy BMI. Women within the normal BMI range should gain<br />
between 25 and 35 pounds. Overweight and obese women are encouraged to gain less (15 to 25 pounds for<br />
overweight women; 11 to 20 pounds for obese women). 3<br />
Recommended intakes for energy and the macronutrients, carbohydrate and protein, increase during pregnancy<br />
and are easily achieved by most women who are eating a balanced diet. 5-7 Recommended intake for total fat, as a<br />
percentage of energy, does not increase during pregnancy and lactation. 5,8 However, the importance of consuming<br />
long chain polyunsaturated fatty acids (LCPUFA), particularly docosahexaenoic acid (DHA), during pregnancy and<br />
lactation has received increased emphasis in recent years. Exact requirements for DHA during pregnancy and<br />
lactation have not been determined but in 2010 three groups published recommendations on DHA intakes. The<br />
minimum amount of DHA recommended during pregnancy and lactation by these groups is 200 mg per day. 8-10<br />
Recommended intakes of several vitamins and minerals also increase during pregnancy and lactation and many of<br />
these recommendations can be met with a balanced diet. While appropriate intake of all vitamins and minerals is<br />
important, some deserve particular attention with pregnancy. For example, adequate folic acid intake prior to and<br />
during the first few weeks of pregnancy is associated with a reduced risk of neural tube defects (NTDs) 11,12 and<br />
observational studies suggest that adequate choline intake during early pregnancy may positively influence neural<br />
tube closure, independent of folate. 13,14 Emerging evidence indicates that vitamin D may play an important role<br />
in immunity and neurocognitive development in addition to its roles in calcium homeostasis and bone health. 15,16<br />
Inadequate intakes of vitamin A, iron and iodine are associated with night-blindness, anemia, and brain damage,<br />
respectively. 17-19 While adequate intakes of vitamins and minerals during pregnancy are essential, excessive intakes of<br />
some can have negative consequences and should be avoided. For example, excessive intake of preformed vitamin<br />
A (retinoids) during pregnancy increases the risk of birth defects. 20,21<br />
Food guides can be used by women and their health care providers to design balanced eating plans before<br />
pregnancy for achieving desirable weight, and to support a healthy pregnancy and lactation. Some countries around<br />
the world have adopted food guides based on those developed in the US while others have developed their own<br />
specific guides that are based on the country’s food supply, food consumption patterns, nutrition issues and nutrition<br />
standards. 22 Women should use food guides that are adopted by the countries in which they live.<br />
3
Research indicates that the risk of an adverse pregnancy outcome associated with moderate-intensity physical<br />
activity, such as brisk walking, is very low for healthy pregnant women. 23 Physical activity can be benefi cial in<br />
controlling blood glucose levels and promoting weight gain within target ranges. Women with uncomplicated<br />
pregnancies should participate in at least 150 minutes (2 hours, 30 minutes) of moderate-intensity aerobic activity a<br />
week which may be divided up into fi ve, 30-minute walks per week or into bouts of 10-minutes of physical activity<br />
at a time. 3,23-25 Most women with uncomplicated pregnancies and deliveries can begin exercising a few weeks<br />
after delivery; others will need to wait longer. A gradual return to a pre-pregnancy level of physical activity is most<br />
prudent, 26 especially for women who have cesarean deliveries and those on bed rest during pregnancy. Gradual<br />
weight loss resulting from exercise and calorie restriction does not appear to compromise lactation performance. 27,28<br />
Women should be counseled to avoid all alcohol during pregnancy since there is no known safe intake. 29,30 Research<br />
studies linking caffeine intake to pregnancy complications are confl icting but it is prudent to limit intake of caffeine to<br />
200 mg/day during pregnancy. 31-34 Methyl mercury, found in high levels in certain species of fi sh, is neurotoxic 35 and<br />
women of childbearing age should avoid fi sh with high concentrations of methyl mercury. 36,37 Levels of neurotoxic<br />
contaminants in fi sh vary widely among regions of the world. Therefore, it is important to check with national and<br />
regional authorities for information on the levels of contaminants found in fi sh consumed in that region and for<br />
recommendations on fi sh consumption. 35<br />
Pregnant women are also more susceptible to foodborne illnesses and their effects. 38 Women in the childbearing<br />
years should be educated about how best to handle and prepare food, and about which foods are particularly<br />
risky due to possible contamination with micro-organisms including Taxoplasma gondii, Listeria monocytogenes,<br />
Escherichia coli and salmonella.<br />
Some conditions and complications associated with pregnancy, such as nausea and vomiting, and hypertensive<br />
disease, may potentially benefi t from diet and lifestyle interventions. 3,39 In addition, women with gestational diabetes<br />
will benefi t from glycemic control and should be counseled about a balanced diet that fosters normal blood glucose<br />
and meets pregnancy nutrient needs. 40<br />
There is no doubt about the strong connection between maternal health habits and fetal and infant well-being. Eating<br />
a balanced diet, ensuring adequate micronutrient intakes, getting regular physical activity, and avoiding noxious<br />
substances are increasingly regarded as strategies for achieving good pregnancy and lactation outcomes.<br />
MATERNAL NUTRITION 4
INTRODUCTION<br />
A mother’s nutritional status, diet and lifestyle influence pregnancy and lactation outcomes and can have lasting<br />
effects on her offspring’s health. For example, inadequate intakes of certain micronutrients during pregnancy,<br />
such as folic acid and iodine, can contribute to birth defects and/or the inability of the child to develop to his or<br />
her full cognitive potential. In addition, maternal overweight and obesity are increasing globally and present major<br />
challenges for health care providers and their clients since overweight and obesity are associated with several<br />
adverse pregnancy outcomes including birth defects, gestational diabetes, pre-eclampsia and cesarean section. 41,42<br />
Undernutrition and overconsumption during fetal life may also influence the infant’s cognition and future risk of<br />
coronary heart disease, type 2 diabetes, stroke, obesity, and hypertension. 3,43-45 A mother’s consumption of potentially<br />
harmful substances, such as alcohol, during pregnancy can also have irreversible negative consequences.<br />
With the growing body of evidence indicating that a woman’s nutritional status and health-related behaviors both<br />
prior to and during pregnancy influence pregnancy outcomes and the child’s future health, experts are placing more<br />
emphasis on preconception and inter-pregnancy care. This includes screening for health risks that could affect the<br />
outcome of a future pregnancy. Many of those risks, such as poorly-controlled diabetes, hypertension, obesity, and<br />
a poor quality diet, are amenable to positive lifestyle changes. Women are encouraged to achieve and remain at a<br />
healthy body weight prior to pregnancy. 3 They should also be counseled regarding the benefits of physical activity,<br />
avoiding food faddism, consuming adequate folic acid and maintaining good control of medical conditions. 2 After<br />
conception has occurred, a balanced diet that supports appropriate maternal weight gain and meets maternal and<br />
fetal micronutrient needs contributes to creating a favorable intrauterine environment to support optimal pregnancy<br />
outcomes. 5 Good nutrition continues to be important after birth since a diet with insufficient levels of critical nutrients<br />
during lactation can deplete maternal stores and may lower nutrient levels in breast milk. Furthermore, breastfeeding<br />
beyond 6 months, regular physical activity and a balanced diet with an appropriate amount of energy help hasten the<br />
return to pre-pregnancy weight. 27<br />
Many countries around the world have issued diet and nutrient intake recommendations for their populations,<br />
including pregnant and lactating women, which are based on the countries’ food supply, food consumption patterns,<br />
and specific nutrition-related issues. 22 Other countries have adopted recommendations (Dietary Reference Intakes<br />
[DRI]) issued by the Institute of Medicine (IOM) of the National Academies in the United States or The World Health<br />
Organization (WHO). This monograph reviews current nutrition recommendations for women during pregnancy and<br />
lactation primarily from the renowned IOM and WHO. The goal in highlighting these nutrition recommendations is to<br />
increase familiarity with nutrients and nutrition-related issues that can have an important impact during pregnancy,<br />
lactation, and beyond.<br />
5
NUTRITION bEFORE PREGNANCY<br />
Pre-pregnancy body Weight and Pregnancy Outcome<br />
A mother’s nutritional status prior to pregnancy can affect reproduction and pregnancy outcomes, and pre-pregnancy<br />
weight is a common indicator of a woman’s nutritional status. 46 Body Mass Index (BMI) describes body weight in<br />
relation to height and is commonly used in nutrition assessments. It is defi ned as an individual’s body weight (mass)<br />
divided by the square of his or her height (kg/m 2 ). A BMI of less than 18.5 is defi ned as underweight while a BMI ≥ 25<br />
indicates overweight. Obesity is defi ned as a BMI ≥ 30. 3<br />
A low pre-pregnancy BMI may indicate chronic nutritional insuffi ciency 47 and women with a low BMI may have<br />
delayed conception. 48 Women with a low pre-pregnancy BMI are also at increased risk for having an infant with low<br />
birth-weight, or an infant that is small for gestational age or born preterm. 47 Increasingly, however, women around<br />
the world are entering pregnancy overweight or obese. For example, in 2006 it was reported that of women 20<br />
years of age or older in the United States, about 62% had a BMI ≥ 25 and approximately 33% of those women were<br />
considered obese (BMI ≥ 30). 49 Consequently, health experts are placing increased emphasis on the relationship<br />
between overweight and obesity and the potential for sub-optimal reproductive and pregnancy outcomes.<br />
Excess adiposity can hinder a woman’s ability to have regular menstruation and subsequently lead to diffi culty in<br />
conceiving. 48,50 In addition, obesity at the time of conception is associated with many pregnancy complications<br />
including gestational diabetes, hypertension, pre-eclampsia, cesarean delivery, macrosomia, and perintatal<br />
mortality. 3,46 Infants born to obese women also have a higher incidence of congenital defects 4 and greater fat mass<br />
and subsequent overweight in childhood. 3,51 Pre-pregnancy weight status may have implications for infant feeding,<br />
too. Research indicates that women who begin pregnancy obese are also less likely to initiate breastfeeding 52,53 and<br />
to continue full breastfeeding at one month and three months when compared with normal-weight counterparts. 52<br />
They are also more likely to have shorter duration of any breastfeeding. 53<br />
While BMI is a useful, easy screening tool for predicting excess body fat, it does have limitations. For example, very<br />
muscular, fi t women may be considered overweight by BMI standards, even though they are healthy and free of<br />
chronic conditions; other women with body weights within the healthy weight range may have undesirable lipid and/<br />
or blood glucose profi les or poor nutritional reserves, including low iron reserves, which could affect the outcome of a<br />
future pregnancy. A very low BMI, however, is a reliable indicator of low levels of fat and lean tissue due to inadequate<br />
intake. 47<br />
Preconception Diabetes and Pregnancy Outcome<br />
The incidence of diabetes mellitus around the world is on the rise. For example, an estimated 12.6 million (10.8%)<br />
women in the US age 20 and older have diabetes, but many are unaware of their condition. Most cases of diabetes<br />
in adults are type 2 diabetes which is related to obesity. 54<br />
Women with poorly controlled type 1 or type 2 diabetes or those with pre-gestational diabetes are more likely to<br />
deliver an infant with a birth defect than women without diabetes or those who enter pregnancy with normal glucose<br />
levels. 55 Results from the seven-year Hyperglycemia and Adverse Pregnancy Outcomes study demonstrated a<br />
positive relationship between elevated maternal blood glucose levels between weeks 24 and 32 of gestation and<br />
birth-weight above the 90th percentile for gestational age, primary cesarean delivery, neonatal hypoglycemia, and<br />
cord-blood serum C-peptide level above the 90th percentile. Five secondary outcomes – premature delivery, shoulder<br />
dystocia or birth injury, intensive neonatal care, hyperbilirubinemia, and pre-eclampsia – also showed continuous<br />
positive linear associations with blood glucose levels. These data illustrate that the higher the maternal blood glucose<br />
concentrations, the greater the likelihood of these pregnancy complications. 56<br />
MATERNAL NUTRITION 6
Preconception Care<br />
In 2005, the WHO’s World Report 2005: Make Every Mother and Child Count detailed the importance of<br />
preconception care and indicated that reproductive health is an essential element of the continuum of maternal and<br />
child health. It called for reform of programs and interventions at the country and international level. 1 Since 2005, a<br />
number of programs and guidelines have been revised or developed but they vary in scope and content due to a<br />
number of factors including the type of health care system, level of economic support, political, cultural, and religious<br />
beliefs of the locale. Despite the differences in the programs and guidelines, the concept of preconception care<br />
remains a critical component of maternal and child health promotion globally. 57<br />
The US Centers for Disease Control and Prevention has issued recommendations on preconception care for<br />
women. 2,58 The recommendations include screening for health risks that could affect the outcome of a future<br />
pregnancy. Many of those risks, such as obesity, poorly-controlled diabetes, and inadequate diet are amenable to<br />
positive lifestyle changes. Women should be counseled regarding the benefits of physical activity, achieving a healthy<br />
weight prior to pregnancy, avoiding food faddism, consuming adequate folic acid, and controlling preexisting medical<br />
conditions, such as diabetes, along with other factors that influence pregnancy outcome. 2 Pregnancy preparedness<br />
is wise even when a woman does not plan to conceive since many pregnancies are unintended. For example, in the<br />
United States, an estimated 50% of pregnancies are unintended or mistimed. 59 During the first seven to eight weeks<br />
of pregnancy, when women may not realize they are pregnant, a developing fetus is highly susceptible to congenital<br />
anomalies and other adverse outcomes as a result of exposure to alcohol, tobacco and other drugs, workplace<br />
hazards, and inadequate intake of essential nutrients, such as folic acid. 60<br />
NUTRITION DURING PREGNANCY AND LACTATION<br />
Pregnancy Weight Gain Guidelines<br />
Starting pregnancy with a healthy weight and gaining appropriately during pregnancy typically translates into a lower<br />
risk of complications for mother and child. 3 However, women who are attempting to lose weight prior to conception<br />
should stop once pregnancy has occurred.<br />
Weight-gain and weight-monitoring recommendations during pregnancy vary around the world. 4 Many countries<br />
in Europe, for example, do not weigh pregnant women after their first antenatal visit, 4 while others have developed<br />
population-specific pregnancy weight-gain curves based on research of weight gain and pregnancy outcomes in their<br />
countries. 61,62 In 2004, the Report of a Joint FAO/WHO/UNU Expert Consultation on human energy requirements 6<br />
stated,<br />
“This consultation endorsed the WHO recommendation that healthy, well-nourished women should gain 10 to<br />
14 kg [22 to 30.8 pounds] during pregnancy, with an average of 12 kg [26.4 pounds], in order to increase the<br />
probability of delivering full-term infants with an average birth weight of 3.3 kg, and to reduce the risk of foetal<br />
and maternal complications.”<br />
According to the Expert Consultation, underweight women (with a BMI 25 may benefit with weight gains near the lower end of the range. 6<br />
In 2009, the Institute of Medicine (IOM) in the United States updated its guidelines for weight gain during pregnancy<br />
as a result of rising obesity rates in women, the large proportion of women with high gestational weight gain, and the<br />
strength of the evidence linking gestational weight gain to certain adverse outcomes. 3 The 2009 recommendations<br />
are an attempt to balance the risks and benefits associated with gestational weight gain for both the mother and<br />
child. The IOM stated that while the guidelines are intended for use in the United States, “They may be applicable to<br />
7
women in other developed countries.” 3 For example, Canada has adopted the IOM guidelines. 63 The IOM guidelines,<br />
however, are “not intended for use in areas of the world where women are substantially shorter or thinner than<br />
American women or where adequate obstetric services are unavailable.” 3 The IOM guidelines are reviewed here.<br />
The 2009 IOM recommendations adopted the World Health Organization (WHO) BMI categories to classify women’s<br />
weight. The WHO categories make the 2009 weight gain recommendations for pregnancy congruent with those of<br />
the non-pregnancy state (Table 1) and set an upper limit of weight gain for obese women (Table 2). The weight gain<br />
range for obese women in the IOM’s latest recommendations was primarily based on data for women with BMIs in<br />
the range of 30 to 34.9 kg/m. 2 Thus, women with higher BMIs are encouraged to gain at the lower end of the range. 3<br />
TAbLE 1. CRITERIA FOR CLASSIFICATIONS OF PRE-PREGNANCY WEIGHT STATUS bMI (kG/M 2 ) 3<br />
bMI<br />
Underweight
Nutrient Needs during Pregnancy and Lactation<br />
A balanced diet that supports appropriate maternal weight gain and meets maternal and fetal nutrient needs<br />
contributes to creating a favorable intrauterine environment. 5 However, for a variety of reasons, pregnant and<br />
lactating women often do not consume the recommended amounts of essential nutrients. Inadequate micronutrient<br />
intake during pregnancy and lactation has been attributed to factors such as increased nutritional needs, maternal<br />
age, geography, and socioeconomic status. 21,65<br />
In the following sections, recommended intakes for energy, macro- and micronutrients during pregnancy and<br />
lactation are summarized.<br />
Energy<br />
The energy cost of pregnancy (measured in calories or kilojoules) includes energy needed for accretion of maternal,<br />
fetal and placental tissues, increases in the mother’s basal metabolism, and the mother’s physical activity level.<br />
Table 4 summarizes recommendations for additional daily calorie intakes during pregnancy and lactation. The FAO/<br />
WHO/UNU Expert Consultation on human energy requirements recommended an additional intake of 85, 285 and<br />
475 kcal/d during the first, second and third trimesters of pregnancy, respectively. 6 The IOM Dietary Reference<br />
Intakes do not recommend an increase in daily calorie intake during the first trimester of singleton pregnancies. 5<br />
Women are advised to increase their daily calorie intakes during pregnancy according to their pre-pregnancy body<br />
weight, physical activity level, and weeks gestation. The suggested calorie increase for women who conceive at a<br />
body weight in the normal range is 340 calories a day in the second trimester and 450 calories a day in the third<br />
trimester. 5 It has been suggested that in the US, women pregnant with multiple fetuses need about 500 calories a<br />
day beyond what is required for a singleton pregnancy starting in the first trimester. 66<br />
The amount of milk that a woman produces and secretes as well as the milk’s energy content influence the energy<br />
cost of lactation. 67 The FAO/WHO/UNU Expert Consultation on human energy requirements recommended<br />
that well-nourished lactating women consume an additional 505 kcal/d during the first 6 months of lactation.<br />
Undernourished women should consume more: an additional 675 kcal/d. The expert consultation did not make<br />
recommendations for the second 6 months of lactation since milk production is more highly variable during this<br />
time. 67 The IOM daily calorie intake recommendations for lactating women are based on pre-pregnancy calorie<br />
requirements for weight maintenance for women within the normal weight range. The IOM recommends that women<br />
in the normal weight range consume 330 additional calories per day for the first six months after delivery and 400<br />
additional calories each day for months six through 12 of their infant’s life. 5 Overweight and obese women and<br />
women who gained too much weight during pregnancy may not need to consume additional energy. Research<br />
indicates that once lactation is established, breastfeeding women with a post-pregnancy BMI >25 may restrict their<br />
intake by 500 kilocalories per day and exercise to promote weight loss without affecting infant growth. 27,68<br />
9
TAbLE 4. RECOMMENDATIONS FOR ADDITIONAL DAILY CALORIE INTAkE DURING PREGNANCY AND<br />
LACTATION 5,6,67<br />
Pregnancy IOM FAO/WHO/UNU<br />
1 st Trimester 0 85<br />
2 nd Trimester 340 285<br />
3 rd Trimester 450 475<br />
Lactation<br />
1 st 6 Months 330 505 a<br />
2 nd 6 Months 400 Varies depending on milk output<br />
a For women with adequate gestational weight gain. The recommendations for undernourished women and those with insuffi cient gestational<br />
weight gain is 675 kcal/d.<br />
Carbohydrate<br />
The primary role of dietary carbohydrate is to provide energy to cells. Sugars and starches supply energy in the<br />
form of glucose, which is the only energy source for red blood cells and is the preferred energy source for the brain,<br />
central nervous system, and fetus. 5 The U.S. Dietary Reference Intake (DRI) for carbohydrate for a pregnant woman<br />
19 to 50 years of age is a minimum of 175 grams of carbohydrate daily to provide adequate glucose for her body<br />
and for a single fetus. 5 This represents a daily increase of 45 grams above the non-pregnancy state and is easily<br />
achieved by most pregnant women who are eating a balanced diet. The DRI for lactation is higher (210 grams daily)<br />
to compensate for the carbohydrate secreted in breast milk. 5<br />
Fiber is non-digestible carbohydrate and lignin found in plant foods. 5 Benefi ts of dietary fi bers include feelings of<br />
fullness and improved laxation, which could help reduce the chances for hemorrhoids during pregnancy. Some<br />
types of dietary fi ber are also associated with lower postprandial blood glucose levels and reduced blood cholesterol<br />
concentrations. The Adequate Intake (AI) for fi ber during pregnancy and lactation is 14 grams per 1,000 calories. 5<br />
Thus, a pregnant woman with an estimated energy requirement of 2,400 calories should consume about 34 grams of<br />
fi ber daily. Most women do not consume enough fi ber and require counseling about including high-fi ber foods in their<br />
diet, such as dried beans and peas, vegetables, fruits, nuts, and whole grains, to meet the suggested intake.<br />
Protein<br />
Protein is a constituent of all cells and a component of enzymes, membranes, transport carriers, and many<br />
hormones. The amino acids from dietary proteins are utilized by the body for endogenous synthesis of structural<br />
proteins as well as enzymes, numerous hormones, immune factors and a plethora of other vital mediators of<br />
physiological function. 5 Pregnancy signifi cantly increases protein needs due to the increase in hormone production<br />
and plasma volume expansion, along with increased tissue formation for the placenta, fetus and breasts. During<br />
lactation, additional protein intake compensates for protein and non-protein nitrogen output in breast milk. 5<br />
The U.S. Dietary Reference Intakes recommended 0.8 g/kg/day of dietary protein for non-pregnant women. Starting<br />
in the second trimester, the recommended protein intake for pregnancy is 1.1 g/kg/day or about 25 g of additional<br />
protein per day. An additional 50 grams a day of protein is suggested for twin pregnancies beginning in the second<br />
trimester. 5 The WHO recommends that pregnant women consume 1, 9 and 31 g of additional protein daily during the<br />
fi rst, second and third trimesters, respectively. 7<br />
MATERNAL NUTRITION 10
During lactation, the U.S. Dietary Reference Intakes recommend that women consume 1.3 g/kg/d or about 25 g of<br />
additional protein daily. 5 The WHO recommends 19 and 12.5 g of additional protein daily for lactating women during<br />
the first and second 6 months, respectively (Table 5). 7<br />
With the exception of soy and quinoa, animal foods, such as meat, poultry, seafood, eggs, and dairy, are the only<br />
choices that provide all of the indispensable amino acids in a single food. Vegetarian diets that feature a mixture of a<br />
variety of plant foods in adequate amounts are capable of satisfying indispensable amino acid needs, too. Generally<br />
speaking, it is possible for vegetarian women to meet the recommended protein intake during pregnancy and<br />
lactation by eating a balanced diet.<br />
Table 5. Protein Recommendations 5,7<br />
Additional Daily Protein<br />
(g/day)<br />
IOM<br />
WHO<br />
Pregnancy<br />
1st Trimester 0 1<br />
2nd Trimester 25 9<br />
3rd Trimester 25 31<br />
Lactation<br />
1st 6 months 25 19<br />
2nd 6 months 25 12.5<br />
Fat<br />
Dietary fat provides energy (calories) and the essential fatty acids (EFA), linoleic acid and alpha-linolenic acid. Linoleic<br />
acid (LA; 18:2n-6; an 18-carbon, 2-double bond fatty acid) is the parent fatty acid of the n-6 (or omega-6) family of<br />
fats, including the long-chain polyunsaturated fatty acid (LCPUFA) arachidonic acid (ARA; 20:4n-6). Alpha-linolenic<br />
acid (ALA; 18:3n-3; an 18-carbon, 3-double bond fatty acid) is the precursor of the n-3 (or omega-3) family of fatty<br />
acids including LCPUFAs eicosapentaenoic acid (EPA; 20:5n-3) and docosahexaenoic acid (DHA; 22:6n-3). Dietary<br />
fat is also necessary for the absorption of the fat-soluble vitamins A, D, E, and K and participates in the transport of<br />
these and other fat-soluble compounds to cells and tissues.<br />
Daily total fat intake recommendations are related to energy requirements; fat should supply 20% to 35%<br />
of a woman’s total energy needs during pregnancy and lactation. 5,8 There are no dietary requirements for<br />
monounsaturated fatty acids, saturated fatty acids, or trans fatty acids. 5 The recommended daily limit for saturated<br />
fatty acids does not change during pregnancy and lactation and is less than 10% of total energy needs. 8,37 Trans fatty<br />
acid intakes, primarily from partially hydrogenated vegetable oils, should be as low as possible. 8,37<br />
LCPUFA intakes during pregnancy and lactation have received increased attention in recent years. The LCPUFA<br />
DHA is the predominant n-3 fatty acid in brain cells and comprises as much as 65% of the total fatty acids in certain<br />
phospholipids of the retina. 69 The metabolic demand for DHA increases during pregnancy. The mother requires more<br />
DHA to support expanded red blood cell mass and the placenta. In addition, the fetal brain and nervous system rapidly<br />
accumulate DHA during the last trimester of pregnancy. 70 The increased metabolic need for DHA is met by synthesis<br />
from the precursor ALA, maternal stores, and maternal DHA intake. 70 Intake of DHA by pregnant women in industrialized<br />
11
countries varies considerably (mean 70 to 200 mg/day) and the median intake (30-50 mg/day) 70 is lower than the<br />
estimated amount that the fetus accrues daily during the last trimester (~75mg/day of n-3 LCPUFA, mostly DHA). 71<br />
DHA supplementation during pregnancy has been linked to benefi cial outcomes, including slightly longer gestation<br />
(within the normal range of gestation) and slightly higher infant birth-weight. 70,72 There is some evidence to suggest<br />
that maternal DHA supplementation during pregnancy improves infants’ visual acuity, cognitive development, and<br />
immune outcomes. 72,73 Emerging evidence suggests that maternal DHA supplementation may affect infant body<br />
composition later in life by lowering adiposity. 70<br />
After delivery, DHA continues to rapidly accumulate in the infant brain during the fi rst 18 to 24 months of life. 74 Human<br />
milk contains DHA but the amount varies with maternal intake. 72 Brenna and colleagues 75 reported the worldwide<br />
average level of DHA in mature human milk as 0.32 ± 22% (% fatty acids ± SD) with a wide range of 0.06% to 1.4%.<br />
Coastal or island populations with high intakes of marine foods had the highest breast milk DHA levels while inland<br />
populations and developed countries had the lowest. Supplementing DHA intake of lactating women increases breast<br />
milk DHA content but supplementation with the DHA precursor, ALA, does not. 72<br />
Observational studies and intervention trials of breastfed infants indicate that DHA levels in human milk infl uence<br />
infant outcomes. 72 In observational studies, higher DHA levels in human milk and/or infant blood have been<br />
associated with better infant visual acuity when compared with lower levels. 76 In addition, several intervention trials<br />
have found that maternal DHA or DHA+EPA supplementation positively affects neural development of breastfed<br />
infants. 76,77<br />
Exact requirements for DHA during pregnancy and lactation have not been determined but in 2010 three groups<br />
published recommendations on DHA intakes. The Joint FAO/WHO Expert Consultation on Fats and Fatty Acids in<br />
Human <strong>Nutrition</strong> recommended that pregnant and lactating women consume at least 200 mg DHA per day (Table<br />
6). 8 In addition, the French Agency for Food, Environmental and Occupational Health & Safety (ANSES) 9 considered<br />
DHA to be an essential fatty acid in their update of the French population reference intakes (Apports nutritionnels<br />
conseillés or ANCs); they established ANCs for DHA of 250 mg DHA per day for pregnant and lactating women. 9<br />
Also in 2010, the European Food Safety Authority (EFSA), in their Scientifi c Opinion on Dietary Reference Values<br />
for Fats and Fatty Acids, established an adequate intake (AI) of 250 mg of EPA + DHA per day for adults. EFSA<br />
recommended that 100 to 200 mg of preformed DHA be added to this daily intake during pregnancy and lactation. 10<br />
Previously (2007), a Consensus Statement from the Perinatal Lipid Intake Working Group (on behalf of the European<br />
Commission Perinatal Lipid Metabolism [PeriLip] and Early <strong>Nutrition</strong> Programming [EARNEST] research projects,<br />
jointly with representatives of seven other international nutrition or medical organizations) recommended that pregnant<br />
and lactating women consume at least 200 mg DHA per day. 78<br />
Experts have concluded that there is no evidence indicating that intake of dietary n-6 fatty acids, including ARA,<br />
should be increased during pregnancy and lactation. 72 In addition, no recommendation for EPA intake alone during<br />
pregnancy and lactation has been made since EPA has only been studied with DHA as a component of fi sh or a fi sh<br />
oil preparation 72 (Table 6).<br />
TAbLE 6. RECOMMENDED INTAkES FOR LCPUFA DURING PREGNANCY AND LACTATION 8<br />
Recommended Intake Upper Intake Limit<br />
DHA 200 mg/day 1.0 g/day<br />
DHA + EPA 300 mg/day 2.7 g/day<br />
ARA No recommendation 800 mg/day<br />
MATERNAL NUTRITION 12
The United States has not established recommended intakes for DHA. The US Dietary Guidelines for Americans<br />
2010, however, recognized the importance of DHA during pregnancy and lactation. 37 The Guidelines state,<br />
“Moderate evidence indicates that intake of omega-3 fatty acids, in particular DHA, from at least 8 ounces<br />
of seafood per week for women who are pregnant or breastfeeding is associated with improved infant health<br />
outcomes, such as visual and cognitive development. Therefore, it is recommended that women who are<br />
pregnant or breastfeeding consume at least 8 and up to 12 ounces of a variety of seafood per week, from<br />
choices that are lower in methyl mercury.”<br />
Cold water, ocean-faring fatty fish, such as salmon and tuna, are among the richest natural sources of DHA. DHA is<br />
present naturally in lesser amounts in organ meats, poultry and eggs and is found in DHA-fortified foods (Table 7).<br />
The presence of methyl mercury and other neurotoxic chemicals in fish and shellfish is a potential concern for women<br />
in their childbearing years. 36 The US Dietary Guidelines for Americans 2010 state that women who are pregnant or<br />
breastfeeding should not eat tilefish, shark, swordfish and king mackerel because they are high in mercury. 37 Fortified<br />
foods and dietary supplements containing DHA, either derived from single-cell organisms or fish oil that have been<br />
processed to remove potential contaminants, are also sources of preformed DHA for pregnant and lactating women<br />
who do not eat enough DHA-rich foods.<br />
Table 7. Selected Food Sources of DHA<br />
Food<br />
DHA (mg)<br />
Salmon, coho, farmed, 3 oz, cooked 706<br />
Tuna, light, canned, drained, 3 oz 190<br />
Catfish, 3 oz, cooked 116<br />
Blue crab, 3 oz, cooked 57<br />
Fortified eggs, 1 large 57<br />
Chicken, roasted, dark meat, 3 oz 45<br />
Eggs, 1 large 29<br />
Sources: www.nal.usda.gov/fnic/foodcomp/search/. Accessed 09/12<br />
Fortified Eggs: www.egglandsbest.com. Accessed 09/12<br />
Vitamins<br />
Recommended intakes of several vitamins increase during pregnancy and lactation. Figure 1 compares<br />
recommended intakes of select vitamins for non-pregnant women (19 to 30 years old) with those of pregnant or<br />
lactating women of the same age.<br />
13
FIGURE 1. DIFFERENCES IN VITAMIN INTAkE RECOMMENDATIONS<br />
200%<br />
180%<br />
160%<br />
140%<br />
120%<br />
100%<br />
80%<br />
60%<br />
40%<br />
20%<br />
0%<br />
Vitamin C<br />
Vitamin D<br />
Vitamin E<br />
Vitamin K<br />
Thiamin<br />
Riboflavin<br />
Vitamin A<br />
Niacin<br />
Vitamin B6<br />
Pantothenic Acid<br />
Pregnancy, 19-30 years<br />
Lactation, 19-30 years<br />
Biotin<br />
Choline<br />
Folate<br />
Vitamin B12<br />
100% represents the DRI for non-pregnant and<br />
non-lactating women ages 19-30 years. The<br />
bar graphs illustrate the percentage of the nonpregnant/non-lactating<br />
DRI recommended for<br />
pregnant and lactating women.<br />
Specifi c recommendations for pregnancy and<br />
lactation are provided in Table 8. It is important<br />
for pregnant women to consume adequate<br />
amounts of all essential vitamins. Some vitamins<br />
that deserve special attention during pregnancy<br />
and/or lactation are highlighted.<br />
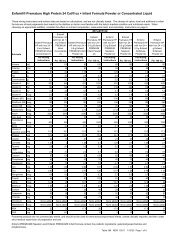
TAbLE 8. RECOMMENDED VITAMIN INTAkES FOR WOMEN DURING PREGNANCY AND LACTATION,<br />
AGES 19 TO 50 YEARS 21,79,80<br />
Nutrient<br />
Vitamin A ac , µg RAE<br />
Vitamin C ac , mg<br />
Pregnancy<br />
Lactation<br />
IOM WHO/FAO IOM WHO/FAO<br />
770<br />
(2541 IU)<br />
85<br />
800<br />
1300<br />
(4290 IU)<br />
850<br />
55 120 70<br />
250%<br />
200%<br />
150%<br />
100%<br />
50%<br />
0%<br />
Vitamin D ac , µg<br />
15<br />
(600 IU)<br />
MATERNAL NUTRITION 14<br />
5<br />
(200 IU)<br />
15<br />
(600 IU)<br />
5<br />
(200 IU)<br />
Vitamin E a , mg 15 - 19 -<br />
Vitamin K bc , ug 90 55 90 55<br />
Vitamin B1 ac (thiamin), mg 1.4 1.4 1.4 1.5<br />
Vitamin B2 ac (riboflavin), mg 1.4 1.4 1.6 1.6<br />
Vitamin B3 ac (niacin), mg 18 18 17 17<br />
Vitamin B6 ac , mg Pregnancy, 1.9 19-30 years 1.9 2.0 2.0<br />
Pantothenic Acid bc , mg Lactation, 6 19-30 years 6 7 7<br />
Biotin bc , µg 30 30 35 35<br />
Choline b , mg 450 - 550 -<br />
Folate ac , µg 600 600 500 500<br />
Vitamin B12 ac , µg 2.6 2.6 2.8 2.8<br />
a Recommended Dietary Allowance (RDA)<br />
b Adequate Intake (AI)<br />
c Recommended Nutrient Intake (RNI)<br />
Intakes are per day, unless otherwise noted.<br />
Calcium<br />
Chromium<br />
Copper<br />
Fluoride<br />
Iodine<br />
Iron<br />
Magnesium<br />
Manganese<br />
Molybdenum<br />
Phosphorus<br />
Selenium<br />
Zinc<br />
Potassium<br />
Sodium<br />
Chloride
Folate and Folic Acid<br />
Folate is a generic term for a B-complex vitamin. Folate is found naturally in plant foods while folic acid is its synthetic<br />
counterpart that is added to enriched grains and dietary supplements. 81 Folate is central in the production of cells,<br />
particularly red blood cells, for nucleic acid synthesis, cell division, and for normal serum homocysteine levels. 81,82<br />
Adequate folic acid intake prior to conception and during the first 28 to 30 days of pregnancy is associated with<br />
a reduced risk of neural tube defects (NTDs). 11,12 Women with pre-gestational diabetes and obese women are at<br />
increased risk of having a pregnancy affected by a NTD and they may benefit from higher intakes of folic acid, though<br />
the exact mechanism as to why this occurs and the actual amount needed are uncertain. 83<br />
Due to the importance of folate in fetal development, various approaches have been implemented around the world<br />
in an attempt to increase the folate status for women of childbearing age. These approaches include voluntary or<br />
mandatory fortification of foods and/or recommendations for folic acid supplementation for women of childbearing<br />
age with associated public health campaigns. 84 Mandatory food fortification programs are in place in many countries 85<br />
and reports have demonstrated a decrease in the prevalence of neural tube defects associated with folic acid<br />
fortification in the US, Canada, Chile, South Africa, Costa Rica, Argentina, and Brazil. 85 The U.S. Preventive Services<br />
Task Force recommends that women of childbearing age with no history of a NTD-affected pregnancy consume 400<br />
to 800 µg of folic acid daily from foods and/or vitamin supplements before and during early pregnancy, while women<br />
with a history of a NTD-affected pregnancy should consult with their physician about taking 4 mg of folic acid daily to<br />
prevent a recurrence. 11 Similar recommendations are in place in various countries around the world. 86<br />
The health benefits of folic acid intake during pregnancy may go beyond those associated with preventing structural<br />
birth defects. 87,88 Periconceptionally, and throughout pregnancy, low dietary folate intake and low circulating blood<br />
folate concentrations have been associated with higher risks of preterm delivery, low birth weight, and fetal growth<br />
restriction. 82,89,90<br />
The IOM recommends 600 µg of dietary folate equivalents (DFE) daily for pregnant women of all ages, and during<br />
lactation, 500 µg/day DFE is recommended. 81 The WHO adopted the IOM’s recommendations for pregnant and<br />
lactating women. 21 Multiparous pregnancies may require more folate but there is no established DRI for women<br />
carrying more than one fetus. 81<br />
Vitamin B12<br />
Vitamin B12 is necessary for healthy nerve and red blood cells and for the production of nucleic acids. 81 Vitamin B12 is<br />
found naturally only in animal foods. Vegans and others who consume few or no animal foods and insufficient vitamin<br />
B12 fortified foods may be at risk of vitamin B12 deficiency. 81 The IOM established recommended intakes for vitamin<br />
B12 during pregnancy at 2.6 µg and 2.8 µg during lactation. 81 The WHO adopted the IOM’s recommendations for<br />
pregnant and lactating women. 21<br />
Maternal vitamin B12 deficiency can result in deficiency in the nursing infant within months after birth. Infantile vitamin<br />
B12 deficiency may cause lasting neurodisability. 91 Women at risk for vitamin B12 deficiency should include fortified<br />
foods such as breakfast cereals, soy and other plant-based beverages, nutrition bars, meat substitutes, and fortified<br />
brewer’s yeast in their eating plan, as well a vitamin B12 supplement to achieve the suggested amounts.<br />
Choline<br />
Choline is an organic compound that is usually grouped within the vitamin B complex. Choline is found in cell<br />
membrane lipids; in sphingomyelin, a component of the myelin sheath surrounding nerve fibers; and as part of the<br />
neurotransmitter acetylcholine, necessary for muscle control, memory, and other functions. Choline is also present in<br />
high concentrations in the liver. 81,92<br />
Adequate choline intake during early pregnancy is important as availability of dietary choline during early pregnancy<br />
may influence neural tube closure, independent of folate. 13,14,93 Experimental animals supplemented with choline (in<br />
15
utero or during the second week of life) experienced lifelong memory enhancement, which appeared to be a result of<br />
the development of the hippocampus (memory center) in the brain. 13<br />
The IOM’s recommendation for choline intake for ages is 19 to 50 is 425 mg/day; during pregnancy, the suggested<br />
intake is 450 mg/day; and during lactation, it is 550 mg/day. 81 The WHO does not establish recommended intakes<br />
for choline. Most women consume inadequate dietary choline. 94 Over-the-counter multivitamins and mineral<br />
supplements and prenatal prescription supplements typically lack adequate choline for women at all stages of life.<br />
Maternal choline requirements should be satisfi ed with choline-rich foods as part of balanced diet. Egg yolks, liver,<br />
meat, poultry, and seafood are particularly rich in choline. Choline is also found in lesser amounts in foods such as<br />
broccoli, peanuts and peanut butter, and milk. 95<br />
Vitamin A<br />
Vitamin A designates a group of compounds essential to growth, cellular differentiation and proliferation, vision,<br />
reproduction, and immunity. 20 Preformed vitamin A (retinoids) is found largely in animal foods, such as liver and<br />
fortifi ed milk, and in dietary supplements. The carotenoids (beta-carotene, alpha-carotene, and beta-cryptoxanthin)<br />
can be converted to vitamin A by the body and are found in vegetables, fruits and oils. 20<br />
Adequate maternal vitamin A status is essential to fetal growth and development since vitamin A status in the fetus<br />
and neonate is dependent upon maternal status. Vitamin A is important for cell division, organ and skeletal growth<br />
and maturation, immune system maintenance, and visual development of the fetus. 17<br />
Maternal vitamin A defi ciency appears to be associated with decreased birth weight, preterm birth and low neonatal<br />
liver stores. 65 Worldwide, vitamin A defi ciency remains a concern among women. It is reported to affect an estimated<br />
19 million pregnant women with the highest prevalence of defi ciency occurring in Africa and Southeast Asia. Night<br />
blindness as a consequence of vitamin A defi ciency is reported to affect 9.8 million pregnant women worldwide. 17<br />
Maternal vitamin A defi ciency most commonly occurs in the third trimester due to the increase in blood volume<br />
and accelerated fetal development. In vitamin A defi cient areas, it may be diffi cult for pregnant women to meet<br />
the recommended intakes of vitamin A through diet alone. The WHO convened an expert group to establish<br />
guidelines on vitamin A supplementation during pregnancy. In areas where the prevalence of night blindness is 5%<br />
or higher in pregnant women and/or children 24-59 months of age, the WHO expert group recommends vitamin A<br />
supplementation during pregnancy for the prevention of night blindness. 17 If supplementation is recommended, betacarotene<br />
is not known to cause birth defects. 17<br />
Conversely, in areas where vitamin A defi ciency is not a public health problem, maternal vitamin A supplementation<br />
as retinoids may lead to toxicity. The WHO Expert Group advises that maternal vitamin A intakes of 10,000 IU daily<br />
or 25,000 IU weekly may lead to vitamin A toxicity for the mother and fetus. Symptoms of vitamin A toxicity include<br />
dizziness, nausea, vomiting, headaches, blurred vision, vertigo, skin exfoliation, reduced muscle coordination, weight<br />
loss and fatigue. 17 Excessive intake of preformed vitamin A during early pregnancy, a time when a woman may not<br />
realize that she has conceived, increases the risk of fetal malformations. 20,21 Maternal vitamin A supplementation<br />
is not recommended by the WHO for prevention of maternal morbidity and mortality unless vitamin A defi ciency<br />
presents a severe public health problem. 17 Dietary intake of vitamin A in the US appears to be adequate in women of<br />
childbearing age, 96 and there is no evidence of the need for routine supplementation which may prove harmful.<br />
The IOM’s recommendation for daily vitamin A intake for pregnant women ages 19 to 50 is 770 µg Retinol Activity<br />
Equivalents (RAE) or 2564 IU. 20 The Tolerable Upper Intake Level (UL) for vitamin A established by the IOM is 3,000<br />
µg RAE (10,000 IU) a day for 19 to 50 year-olds. 20 The WHO established levels of safe intake for vitamin A. The level<br />
of safe intake during pregnancy is 800 µg RAE a day while the level of safe intake during lactation is 850 µg RAE a<br />
day. 21 The WHO does not establish a tolerable upper intake level, however, it does refer to the WHO Expert Group<br />
recommendations as stated above. 21<br />
MATERNAL NUTRITION 16
Vitamin D<br />
Vitamin D’s principal role in the human body is to maintain serum calcium and phosphorus concentrations within the<br />
range that supports cellular processes, proper neuromuscular function, and bone ossification. 97 Vitamin D enhances<br />
calcium absorption in the gut and mobilizes calcium and phosphorus stores from bone to maintain a healthy blood<br />
calcium level. 97 Emerging evidence indicates that vitamin D has important roles in immunity and neurocognitive<br />
development in addition to its roles in calcium homeostasis and bone health. 15,16 Research conducted with female<br />
experimental animals suggests vitamin D plays a role in fertility. 98<br />
Vitamin D is formed in response to strong ultraviolet light (UV) from the sun that initiates the production of vitamin D<br />
in skin. Dietary and endogenously synthesized vitamin D are activated to 1,25-Dihydroxy-Vitamin D (1,25-OH-D) via<br />
two sequential hydroxylation reactions, first by the liver, and second by the kidneys. 97 Healthy humans with sufficient<br />
sunlight exposure can make the vitamin D they need to meet short-term needs, and store vitamin D in fat tissue for<br />
future use. Serum 25 Hydroxyvitamin D (25-OH-D) is an indicator of vitamin D status but optimal levels of 25-OH-D<br />
have not been established. 80<br />
Vitamin D insufficiency and deficiency in women of childbearing age is common throughout the world and is<br />
influenced by the woman’s lifestyle, degree of skin pigmentation, location, time of year, and sun exposure. 15 NHANES<br />
data from 2001-2006 indicated that 26% and 12% of women 19-30 years in the US were at risk for vitamin D<br />
inadequacy or deficiency, respectfully. When considering women who were pregnant or lactating, the risk for<br />
inadequacy was 21%, while the risk for deficiency was 7%. 99 Living at latitudes above 40° N or below 40° S, where<br />
there is relatively weak sunshine for about half a year, is a risk factor for vitamin D deficiency. The use of sunscreen<br />
with a sun protection factor of 8 and above significantly reduces cutaneous production of previtamin D3. 97 Women of<br />
color who live in northern climates may also be at particular risk for low vitamin D levels, because darker skin contains<br />
more melanin which blocks vitamin D production. 100 Overweight women, in particular, run a greater risk of midpregnancy<br />
vitamin D deficiency. 101<br />
Maternal vitamin D insufficiency or deficiency during pregnancy has been linked to adverse pregnancy outcomes<br />
including intrauterine growth restriction, pre-eclampsia, pre-term birth, and gestational diabetes, as well as recurrent<br />
wheeze, reduced bone mineral accrual, and increased rate of language impairment in infants. 16,65,102,103 In addition,<br />
maternal vitamin D deficiency during pregnancy has been associated with several disorders of calcium metabolism<br />
in the mother and infant (neonatal hypocalcemia and tetany, infant hypoplasia of tooth enamel, and maternal<br />
osteomalacia). Since vitamin D deficiency or insufficiency is thought to be common among pregnant women, a<br />
recent meta-analysis evaluated vitamin D supplementation during pregnancy. 104 The results show that vitamin D<br />
supplementation during pregnancy improves maternal vitamin D levels at term. Quality data on the clinical significance<br />
of this finding is too limited to draw conclusions. However, data suggest that pregnant women who consume vitamin<br />
D in supplement form are at lower risk for giving birth to babies who weigh below 2500 grams. 104<br />
The DRI for vitamin D before, during, and after pregnancy, including during lactation, is 600 IU/day for women ages<br />
19-50. 80 The WHO established a RNI for vitamin D at 5 mg/day (200 IU) during pregnancy and lactation. 21 According<br />
to The American College of Obstetricians and Gynecologists, “When vitamin D deficiency is identified during<br />
pregnancy, most experts agree that 1,000 to 2,000 international units per day of vitamin D is safe.” 105 The Tolerable<br />
Upper Intake Level (UL) for vitamin D established by the IOM is 4,000 IU per day. 80<br />
Minerals<br />
Similar to vitamins, recommended intakes of several minerals increase during pregnancy and lactation. Figure 2<br />
compares recommended intakes of select minerals for non-pregnant women (19 to 30 years old) with those of<br />
pregnant or lactating women of the same age.<br />
17
FIGURE 2. DIFFERENCES IN MINERAL INTAkE RECOMMENDATIONS<br />
250%<br />
200%<br />
150%<br />
100%<br />
Calcium<br />
Chromium<br />
Copper<br />
Fluoride<br />
Iodine<br />
Iron<br />
Magnesium<br />
Manganese<br />
Molybdenum<br />
Phosphorus<br />
Selenium<br />
Zinc<br />
50%<br />
0%<br />
Pregnancy, 19-30 years<br />
Lactation, 19-30 years<br />
Potassium<br />
Sodium<br />
Chloride<br />
100% represents the DRI for nonpregnant<br />
and non-lactating women ages<br />
19-30 years. The bar graphs illustrate<br />
the percentage of the non-pregnant/nonlactating<br />
DRI recommended for pregnant<br />
and lactating women.<br />
Specifi c recommendations for pregnancy<br />
and lactation are provided in Table 9. It is<br />
important for pregnant women to consume<br />
adequate amounts of all essential minerals.<br />
Some minerals that deserve special<br />
attention during pregnancy and/or lactation<br />
are highlighted below.<br />
TAbLE 9. RECOMMENDED MINERAL INTAkES FOR WOMEN DURING PREGNANCY AND LACTATION,<br />
AGES 19 TO 50 YEARS 21,79,80<br />
Pregnancy<br />
Lactation<br />
Nutrient<br />
IOM WHO/FAO IOM WHO/FAO<br />
1200<br />
Calcium ac , mg 1000<br />
1000 1000<br />
3rd Trimester<br />
Chromium b , µg 30 - 45 -<br />
Copper a , µg 1000 - 1300 -<br />
Flouride b , mg 3 - 3 -<br />
Iodine ac , µg 220 200 290 200<br />
Iron ac , mg 27 Not specified 9 10-30<br />
Magnesium ac , mg 350-360 220 310-320 270<br />
Manganese b , mg 2 - 2.6 -<br />
Molybdenum a , µg 50 - 50 -<br />
Phosphorus a , mg 700 - 700 -<br />
Selenium a , µg 60 - 70 -<br />
Zinc a , mg 11 4.2-20 12 4.3-17.5<br />
Potassium b , g 4.7 - 5.1 -<br />
Sodium b , g 1.5 - 1.5 -<br />
Chloride b , g 2.3 - 2.3 -<br />
a Recommended Dietary Allowance (RDA)<br />
b Adequate Intake (AI)<br />
c Recommended Nutrient Intake (RNI)<br />
Intakes are per day, unless otherwise noted.<br />
MATERNAL NUTRITION 18
Iron<br />
Iron is vital to the production of hemoglobin, (which is necessary for oxygen transport), and energy production,<br />
fetal immunity, and development of the central nervous system. 106 Iron deficiency affects more than 2 billion people<br />
globally, making it the most common nutrient deficiency in the world. Iron deficiency is more common in developing<br />
countries but continues to be a significant problem in developed countries despite near elimination of other forms<br />
of malnutrition. 107 An estimated eight million women of childbearing age in the US have iron-deficiency anemia, 2 and<br />
it is reasonable to expect that a large number of women are also iron-deficient. Low-income, less than 12 years of<br />
education and increased parity are all associated with a greater risk of iron deficiency and iron-deficiency anemia. 42,108<br />
The global prevalence of iron-deficiency anemia is estimated to be 47.4% in pregnant women. 18<br />
The recommended iron intakes established by the IOM increase from 18 mg/day to 27 mg/day during pregnancy<br />
for women ages 19 to 50 years 20 while the WHO has established different recommended intakes based on the<br />
bioavailability of dietary iron consumed. In developing countries, it is reasonable to use iron bioavailability levels of 5%<br />
and 10% translating into recommended nutrient intakes for lactating women of 30 and 15 mg/day respectively. In<br />
developed countries consuming a more Western diet, it is more appropriate to use bioavailability levels of 12% and<br />
15%, translating into recommended nutrient intakes for lactating women of 12.5 and 10 mg/day of iron, respectively.<br />
The WHO establishes no recommended nutrient intakes for iron in pregnant women because the iron balance in the<br />
diet depends on amounts of stored iron in addition to the bioavailability of dietary iron. 21<br />
Iron stores at the time of conception are a strong indicator of risk for iron-deficiency anemia later in pregnancy. 42<br />
Serum ferritin levels are a measure of stored iron in the body and can be used with a hematocrit to confirm irondeficiency<br />
anemia when there is no evidence of inflammation 108 before and during pregnancy. Iron-deficiency anemia<br />
during pregnancy has been associated with an increased risk for preterm birth, low birth weight, and perinatal<br />
mortality. 109-111 However, results of recent studies on the effects of maternal iron status and supplementation during<br />
pregnancy on fetal growth have been inconsistent. In a recent review on iron supplementation and pregnancy<br />
outcome, studies starting supplementation in mid- or late pregnancy found an increase in maternal iron markers,<br />
but no effect on fetal growth with the exception of one study where high-dose supplementation showed a<br />
positive association with birth length (not with birth weight) in a low-income setting. However, in studies starting<br />
supplementation in early pregnancy, maternal iron status did not improve, but there was a beneficial effect on fetal<br />
growth. 112<br />
Iron absorption during pregnancy is determined by several factors including the amount and bioavailability of<br />
dietary iron as well as the changes in iron absorption that occur during pregnancy. Although there is an increase in<br />
iron absorption, it is difficult for the mother to consume enough dietary iron to meet her iron requirements during<br />
pregnancy. 21 The typical American diet provides inadequate iron to meet the recommendations for the pregnancy<br />
state. 113 In addition, the endogenous iron stores of women may be insufficient to provide for the increased iron<br />
demands of pregnancy. 65<br />
In the US, the CDC recommends that all pregnant women take 30 mg of supplemental elemental iron every day<br />
to prevent anemia 2 and 60 to 120 mg of elemental iron daily to treat anemia once it is diagnosed. 2,113 In the UK,<br />
prophylactic iron supplementation is not recommended for pregnant women. However, pregnant women are<br />
monitored throughout pregnancy for iron-deficiency anemia and recommendations for supplementation based on iron<br />
status tests are established. 107 There is some concern that such prophylactic iron supplementation in women without<br />
anemia or iron-deficiency anemia may increase the risk of pregnancy complications. 42 However, iron supplementation<br />
during pregnancy has merit, as a large proportion of women have difficulty maintaining iron stores during pregnancy<br />
and are at risk for anemia. 113 The WHO recommends that pregnant women be supplemented with 60 mg iron in<br />
conjunction with 400 µg of folic acid daily. 18<br />
19
Calcium<br />
Calcium has structural and metabolic functions. The skeleton and teeth serve as reservoirs for about 99% of the<br />
body’s calcium; the remainder is found in blood, extracellular fl uid, muscle, and other tissues, where it plays a role in<br />
vascular contraction and vasodilation, muscle contraction, and nerve transmission. 97<br />
The recommended intake established by the IOM for calcium in pregnant and lactating women ages 19 to 50 is<br />
1,000 mg/day, 80 which does not represent an increase from the non-pregnant state. The recommended intake for<br />
calcium established by WHO for pregnant and lactating women is also 1000 mg/day, but increases to1200 mg/day<br />
during the last trimester of pregnancy. 21<br />
During pregnancy, adaptive maternal responses to fetal calcium needs include an enhanced effi ciency in absorption.<br />
Many women in their childbearing years do not consume adequate calcium. Multivitamins, including prescription<br />
and over-the-counter prenatal supplements, typically lack enough calcium to meet a woman’s daily needs. Women<br />
who cannot satisfy their calcium needs through food should take separate supplements. The UL for calcium<br />
established by the IOM is 2,500 mg/day. 80 The WHO establishes an upper limit on calcium intake of 3,000 mg/day. 21<br />
The WHO studied the effects of calcium supplementation on pre-eclampsia in pregnant women with low calcium<br />
intake. Calcium supplementation did not prevent preeclampsia, however it did reduce the severity, maternal<br />
morbidity, and neonatal mortality. 114 In 2011, the WHO published 23 recommendations for the prevention and<br />
treatment of pre-eclampsia. 39 The WHO guidelines recommend calcium supplementation (1.5 to 2.0 g elemental<br />
calcium per day) for pregnant women residing in areas where dietary calcium intake is low to help prevent preeclampsia.<br />
Zinc<br />
Zinc performs many functions and is a part of every cell in the body. Zinc is essential for growth and development,<br />
as well as reproduction and immunity. 20 The primary function of zinc is to promote cell reproduction and tissue<br />
growth and repair. It serves as a part of more than 70 enzymes including alcohol dehydrogenase, alkaline<br />
phosphatase, and ribonucleic acid (RNA) polymerases. Zinc also provides a structural function for copper-zinc<br />
superoxide dismutase. 115<br />
Because zinc plays a critical role in embryogenesis and fetal growth, as well as being secreted in breast milk, the<br />
body’s need for zinc is greater during pregnancy and lactation. 116 The recommended intakes for zinc established by<br />
the IOM for women ages 19 to 50 during pregnancy and lactation are 11 and 12 mg/day respectively. 20<br />
The WHO considered the bioavailability of zinc in food sources consumed when establishing recommendations. 21<br />
The bioavailability of zinc varies widely depending on a number of factors. Some zinc is more bioavailable from<br />
foods for absorption. Substances that can decrease zinc bioavailability include iron, calcium, phosphorus, amount<br />
and type of protein, phytates and fi ber. 117<br />
In addition to bioavailability, the WHO considers the variable needs during each trimester of pregnancy and stage of<br />
lactation by establishing different recommended zinc intakes for each. The recommended nutrient intakes for zinc<br />
during pregnancy and lactation can be found in Table 10.<br />
MATERNAL NUTRITION 20
Table 10. WHO Recommended Nutrient Intakes for Zinc during Pregnancy<br />
and Lactation 21<br />
Group<br />
High bioavailability<br />
(mg/day)<br />
Moderate<br />
bioavailability<br />
(mg/day)<br />
Low bioavailability<br />
(mg/day)<br />
Pregnancy<br />
First trimester 3.4 5.5 11<br />
Second trimester 4.2 7 14<br />
Third trimester 6 10 20<br />
Lactation<br />
0 to 3 months 5.8 9.5 19<br />
3 to 6 months 5.3 8.8 17.5<br />
6 to 12 months 4.3 7.2 14.4<br />
Iodine<br />
Iodine, a mineral often added to table salt, is a critical component of thyroid hormones. Thyroid hormones regulate<br />
many key metabolic processes and are particularly important for myelination of the central nervous system during<br />
fetal and early prenatal development. 20 Iodine deficiency from the fetal stage to about 3 months after birth leads to<br />
irreversible alterations in brain function. 19 The World Health Organization stated, “iodine deficiency is the greatest<br />
cause of preventable brain damage in childhood…” 19 Iodine deficiency in mothers also increases the risk of infant<br />
mortality, miscarriage and stillbirth. 118<br />
Iodine intakes vary around the world and within countries. Iodine content of foods is affected by iodine content of soil.<br />
Snow, heavy rainfall, and water can leach iodine from the soil lowering iodine content of crops grown in that soil. 19<br />
Many countries add iodine to table salt as an inexpensive yet effective way to increase iodine intakes. 19 According<br />
to the IOM, “Most foods provide 3 to 75 mg iodine per serving.” 20 Processed foods may contain significant amounts<br />
of iodine if iodized salt or other ingredients containing iodide are added (i.e. calcium iodate, potassium iodate,<br />
potassium iodide, cuprous iodide). 20 Food manufacturers, however, may use salt without added iodide, so it is<br />
important to read ingredient labels.<br />
The recommended intakes established by the IOM for iodine by pregnant and lactating women ages 19 to 50 are<br />
220 and 290 µg/day respectively. 20 The WHO established the recommended dietary intake of iodine for pregnant and<br />
lactating women at 3.5 µg/kg/day or about 200 µg/day. 21<br />
Multivitamin Use during Pregnancy<br />
Women in low income countries often consume inadequate amounts of micronutrients due to a limited food supply<br />
as well as limited intake of fortified foods. Micronutrient deficiencies that result from inadequate intakes are intensified<br />
during pregnancy and can lead to adverse effects for the mother and infant. 119 In developed countries such as<br />
the US, many women in their childbearing years are at risk for inadequate intakes of several nutrients. 42 Although<br />
vitamin and mineral supplements (multivitamins) are not suitable substitutes for a healthy diet at any time during<br />
the reproductive years, they are useful for filling nutrient gaps for nutrients that could affect pregnancy outcomes,<br />
including folic acid and iron.<br />
21
A meta-analysis evaluated the use of multiple-micronutrient supplementation for women during pregnancy. Multiple<br />
micronutrient supplementation was associated with reductions in maternal anemia, low birth-weight babies, and<br />
small-for-gestational-age (SGA) babies. However, the analysis revealed no additional benefi t when compared to a<br />
combination of iron and folic acid supplementation. The authors concluded that the results are limited by the small<br />
number of studies available and further research is needed related to the maternal and fetal benefi ts of multiplemicronutrient<br />
supplementation. 119 The WHO Commentary associated with this meta-analysis reported that the<br />
results are most likely applicable to under-resourced areas since all of the trials included in the meta-analysis were<br />
conducted in low-income countries. 120 Emerging evidence indicates that multiple micronutrient supplements may<br />
provide additional benefi ts when compared to iron or iron and folate supplementation, including reduction in risk of<br />
low birth-weight and SGA as well as an increase in mean birth-weight. 121<br />
Taking a daily multiple-micronutrient supplement containing modest levels of nutrients and eating a balanced diet that<br />
includes foods rich in folic acid and iron may satisfy vitamin and mineral intake recommendations during pregnancy<br />
and lactation. Dietary supplements containing DHA can help pregnant and lactating women who do not eat enough<br />
DHA-rich foods achieve recommended intakes of this important fatty acid.<br />
DESIGNING HEALTHY LIFESTYLE PLANS FOR WOMEN IN THE<br />
CHILDbEARING YEARS<br />
Guides to Healthy Eating<br />
Food guides can be used by women and their health care providers to design balanced eating plans before<br />
pregnancy for losing, gaining or maintaining weight, and to support a healthy pregnancy and lactation. In 1992, the<br />
United States Department of Agriculture issued the Food Guide Pyramid as a guide for healthy eating. Balance,<br />
variety, and moderation are the basic tenets of the Food Guide Pyramid, which gave guidance on how much to eat<br />
from each of fi ve foods groups including grains, vegetables, fruits, dairy, and protein foods and from the fats and oils<br />
category. In 2011, the US replaced the Food Guide Pyramid with MyPlate, a new guide to healthy eating for most<br />
people ages two years and older. As part of MyPlate, the Daily Food Plan for Moms provides dietary guidance for<br />
pregnant and lactating women, suggesting what women should eat on a daily basis. MyPlate and MyPlate Daily Food<br />
Plan for Moms can be found at www.choosemyplate.gov/.<br />
Some countries around the world have adopted food guides similar to the US Food Guide Pyramid while others have<br />
developed their own specifi c guides for healthy eating that are based on the country’s food supply, food consumption<br />
patterns, nutrition issues and nutrition standards. 22 In addition to pyramids, food guide illustrations from around the<br />
world include pagodas, rainbows, circles and plates. 22 Food groups and recommended numbers of servings from<br />
each food group vary somewhat among international food guides. Most guides, however, encourage individuals to<br />
consume more grains, vegetables, and fruits and less meat and dairy products. 22 Women and healthcare providers<br />
should use food guides specifi cally designed for and/or adopted by their countries or regions of the world when<br />
planning diets for pregnancy and lactation. A web site of the FAO provides information on food guides that it has<br />
received from around the world. The food guides can be accessed at http://www.fao.org/ag/humannutrition/<br />
nutritioneducation/fbdg/en/.<br />
Although food guides provide reliable templates for balanced eating plans, it may be necessary for women to<br />
receive additional dietary advice from a knowledgeable nutritional professional, such as a registered dietitian (RD). A<br />
registered dietitian can tailor food plans to meet individual needs and promote appropriate weight gain. Women who<br />
do not eat the suggested number of servings from each of the food groups, adolescents who need higher amounts<br />
of some nutrients, and those who need to amend their diets to manage chronic conditions during pregnancy will<br />
benefi t from additional dietary advice from a registered dietitian.<br />
MATERNAL NUTRITION 22
Guidelines for Physical Activity during Pregnancy and Lactation<br />
Exercise is beneficial for weight control during pregnancy and for weight loss or maintenance during the<br />
preconception, postpartum, and intrapartum periods. During pregnancy, regular physical activity may improve the<br />
possibility of gaining weight within the targeted ranges, 3 help decrease minor aches and pains, lessen constipation,<br />
improve energy level, reduce stress, and improve sleep. 77 Exercise has also been shown to improve glucose<br />
tolerance, and help prevent the development of gestational diabetes. 122,123 Research indicates that infant birth-weight<br />
is not negatively affected by moderate-intensity exercise in women who have adequate energy intake. 26,124<br />
Research indicates that the risk of an adverse pregnancy outcome associated with moderate-intensity physical<br />
activity, such as brisk walking, is very low for healthy pregnant women. 23 The US Department of Health and Human<br />
Services states, “Unless a woman has medical reasons to avoid activity during pregnancy, she can begin or continue<br />
moderate-intensity aerobic physical activity during her pregnancy and after the baby is born.” 23 The World Health<br />
Organization suggests that pregnant and postpartum women seek medical advice on how to achieve their physical<br />
activity goals. 25<br />
Women with uncomplicated pregnancies should participate in at least 150 minutes (2 hours, 30 minutes) of<br />
moderate-intensity aerobic activity a week which may be divided up into five, 30-minute walks per week or into bouts<br />
of 10-minutes of physical activity at a time. 3,23-25 Pregnant women just beginning to exercise should start slowly and<br />
gradually increase over time. 23 Exercise is not indicated for women with certain medical or obstetrical complications<br />
such as significant heart disease, restrictive lung disease or pre-eclampsia, among others. 28<br />
Certain activities are not recommended during pregnancy, including any activity involving pressure changes that could<br />
deprive the fetus of oxygen, such as scuba diving, and any activity with a high risk of falling or abdominal trauma<br />
such as downhill skiing, horseback riding, soccer, basketball, and anything with jumping or jarring motions such as<br />
high-impact aerobics classes. 23,28,77 Pregnant women should also avoid exercising while lying on their backs after the<br />
first trimester, 26,28 as it compresses the vena cava possibly causing a sudden drop in blood pressure, dizziness, or a<br />
loss of consciousness.<br />
To avoid dehydration, pregnant women need about 10 eight-ounce cups of fluid daily. 125 While there are no<br />
recommendations for fluid intake in pregnant exercisers, they will likely need more to account for losses.<br />
Most women with uncomplicated pregnancies and deliveries can begin exercising a few weeks after delivery; others<br />
will need to wait longer. A gradual return to a pre-pregnancy level of physical activity is most prudent, 26 especially for<br />
women who have cesarean deliveries and those on bed rest during pregnancy. Women should be encouraged to get<br />
regular physical activity in the post-partum period and beyond, even when weight loss is not a goal. 37<br />
Gradual weight loss resulting from exercise and calorie restriction does not appear to compromise lactation<br />
performance. 27,28,68 Severe calorie deficits, however, may impair milk production. 126 Lactating mothers should try<br />
to nurse just before exercising for prolonged periods (thirty minutes or more) to avoid discomfort 26 and should be<br />
encouraged to drink fluids before, during, and after exercise to stay hydrated. Experts recommend that lactating<br />
women consume 13 eight-ounce cups of fluid daily; 125 exercise will likely increase their fluid needs.<br />
23
ALCOHOL, CAFFEINE, AND OTHER FOOD SAFETY ISSUES IN WOMEN OF<br />
CHILDbEARING AGE<br />
Alcohol<br />
Prenatal alcohol use is a preventable cause of birth defects. The term Fetal Alcohol Spectrum Disorders (FASDs)<br />
refers to the problems that arise in infants from mothers who consumed alcohol during pregnancy including<br />
facial abnormalities, intellectual disabilities, heart defects, and learning and emotional problems. The most severe<br />
effect attributed to prenatal alcohol intake is Fetal Alcohol Syndrome, a combination of physical and mental birth<br />
defects. 29,30 The effects of gestational alcohol intake are more pronounced in the offspring of heavy drinkers, but<br />
lesser amounts of alcohol intake during pregnancy have also proven to be problematic. 127-129 Pregnant women should<br />
be counseled to avoid all alcohol during pregnancy since there is no known safe intake. 29,30<br />
The effects of alcohol on the breastfeeding infant are directly related to maternal consumption. Moderate to heavy<br />
drinking (2 or more alcoholic drinks per day) can interfere with let-down and milk ejection. 130 Alcohol is transferred into<br />
breast milk and is capable of slowing infant growth. 130 An occasional drink when lactating probably presents little risk<br />
to a nursing child but mothers should discuss alcohol consumption with their health care provider. 131<br />
Caffeine<br />
Caffeine is present in a variety of beverages and foods (Table 11). Studies evaluating the risk of caffeine consumption<br />
and pregnancy complications have been confl icting in their fi ndings. 31-33 Some authors of observational studies<br />
have concluded that caffeine contributes to miscarriage, growth restriction, reduced birth-weight, preterm birth or<br />
stillbirth but authors of a 2009 review concluded that there is insuffi cient evidence “from randomized controlled trials<br />
to support any benefi ts from avoiding caffeine during pregnancy.” 33 Given the potential for pregnancy complications<br />
seen in observational studies, it is prudent to advise women to limit caffeine intake to 200 mg/day or less when<br />
trying to conceive a child and during pregnancy. 34 A small amount of caffeine is transferred into breast milk, but the<br />
American Academy of Pediatrics considers caffeine consumption safe for breastfeeding women. 130 Women who<br />
consume more than 2-3 cups of coffee per day, however, may fi nd that their babies become irritable or have diffi culty<br />
sleeping. 34,130<br />
TAbLE 11. SELECTED SOURCES OF CAFFEINE<br />
beverage or Food Amount Caffeine (mg)<br />
Coffee, drip brewed 12 ounces 98-180<br />
Energy drinks 8 ounces Varies. Several contain ~80<br />
Cappuccino 12 ounces 113<br />
Energy mints 1 piece 100<br />
Espresso 1 ounce 75<br />
Cola soft drinks 12 ounces 36-69<br />
Tea, Black, brewed 8 ounces 38-58<br />
Tea, green, brewed 8 ounces 23-35<br />
Bottled iced tea 12 ounces 25-45<br />
Sources: www.pepsiproductfacts.com/caffeine.php; www.starbucks.com; www.redbull.com.; www.vroomfoods.com; http://www.cspinet.org/<br />
new/cafchart.htm. Accessed 9/12 and 10/12.<br />
MATERNAL NUTRITION 24
FOOD SAFETY ISSUES<br />
Fish and Seafood<br />
Seafood is an easy-to-prepare food that is rich in protein, vitamins, and minerals, and relatively low in total and<br />
saturated fat. Fish and shellfish also supply LCPUFA, most notably DHA, that play a role in the development of the<br />
fetal and infant brain and retina.<br />
Fish and shellfish, however, are also potential sources of methyl mercury and other neurotoxic contaminants. 35<br />
Exposure to high levels of such contaminants during gestation increases the risk for suboptimal neurodevelopment of<br />
children. Levels of neurotoxic contaminants in fish vary widely among regions of the world. Therefore, it is important<br />
to check with national and regional authorities for information on the levels of contaminants found in fish consumed in<br />
that region and for recommendations on fish consumption. 35<br />
According to the US Food and Drug Administration (FDA) and the US Dietary Guidelines for Americans 2010, women<br />
in their childbearing years should avoid swordfish, tilefish, king mackerel, and shark because of their high methyl<br />
mercury content. In addition, women should eat no more than 12 ounces (about 340 grams) of low-mercury fish and<br />
shellfish weekly, such as trout, salmon, pollock, catfish, canned light tuna, canned sardines, shrimp, crab, scallops,<br />
and herring, and limit albacore (“white”) tuna intake to 6 ounces weekly as part of the 12-ounce limit. 36,37 Women who<br />
eat fish caught for sport should first check the safety of the rivers, lakes, and streams where the fish has been caught<br />
with local or state health authorities.<br />
Even with all the caveats, it is likely that the benefits of consuming low-risk seafood outweigh the potential harm to<br />
a developing fetus and to maternal health. 132 Maternal intake of low-risk seafood during pregnancy helps to optimize<br />
neurodevelopment in children. 132-134<br />
Foodborne Pathogens<br />
Pregnant women run a greater risk for foodborne illness from pathogens that can threaten maternal and fetal health. 38<br />
For example, pregnant women are more likely to develop listeriosis if exposed to Listeria monocytogenes. 135 Infection<br />
with Toxoplasma gondii from eating undercooked, contaminated meat and/or from contact with contaminated<br />
cat feces can be transmitted to a fetus and can cause severe illness. 136 Table 12 summarizes common foodborne<br />
pathogens that may harm a pregnant woman or her fetus.<br />
Adequate hand washing and proper food handling can significantly reduce the risk of foodborne illness. 38 There is<br />
no evidence to suggest that organic foods, which are produced with no synthetic pesticides, synthetic fertilizers,<br />
antibiotics, growth hormones and other drugs, offer complete protection from foodborne pathogens.<br />
25
TAbLE 12. SELECTED FOODbORNE PATHOGENS AND RISkS TO MATERNAL AND FETAL HEALTH<br />
Organism May result in To reduce risk, avoid<br />
Listeria monocytogenes Miscarriage, preterm<br />
delivery, infant death<br />
Hot dogs, luncheon meats, foods made<br />
with unpasteurized milk and cheese,<br />
refrigerated pate, meat spreads, and<br />
smoked seafood<br />
Escherichia coli<br />
Abdominal cramps, bloody<br />
diarrhea, vomiting<br />
Undercooked beef, contaminated<br />
bean sprouts, fresh leafy greens,<br />
unpasteurized milk and juice<br />
Salmonella Diarrhea, fever, cramps Undercooked animal foods,<br />
unpasteurized milk, raw eggs<br />
Toxoplasma gondii<br />
Vision loss, mental disability<br />
in offspring<br />
Undercooked meat, dust, contaminated<br />
kitty litter boxes, and outdoor areas<br />
where cat feces found<br />
Source: CDC.gov. Accessed 09/12<br />
PREGNANCY–ASSOCIATED CONDITIONS AND POSSIbLE DIET AND<br />
LIFESTYLE INTERVENTIONS<br />
Nausea, Vomiting, and Hyperemesis Gravidarum<br />
Rapidly rising blood levels of human chorionic gonadotropin (HCG) may be culpable for so-called “morning sickness”<br />
that includes nausea or vomiting in the fi rst trimester that may signifi cantly reduce a woman’s appetite. 137,138<br />
Management of nausea and vomiting typically involves avoiding offending foods and eating small, frequent meals<br />
and snacks. 3 Hyperemesis gravidarum is persistent, extreme nausea and vomiting that may result in dehydration and<br />
poor weight gain. 138 It is distinguished from morning sickness by weight loss (> 5% of weight) and development of<br />
dehydration and ketoacidosis. 138 Hyperemesis gravidarum requires medical supervision to monitor maternal and fetal<br />
well-being. 137<br />
Hypertensive Disease<br />
About 10% of pregnant women worldwide develop hypertensive disorders of pregnancy. These disorders include preeclampsia<br />
and eclampsia, gestational hypertension and chronic hypertension. Pre-eclampsia, which is characterized<br />
by hypertension and proteinuria, is a primary cause of maternal and perinatal morbidity and mortality worldwide. 39<br />
In addition to gestational hypertension, risk factors for pre-eclampsia include being pregnant with more than one<br />
child, maternal obesity, a history of pre-eclampsia, and pre-existing diabetes. 139,140 An increase in pre-pregnancy BMI<br />
between pregnancies poses a risk for pre-eclampsia in the second pregnancy for women with no previous history of<br />
the condition. 140<br />
Managing hypertensive disease during pregnancy is critical for reducing infant mortality and maternal morbidity and<br />
mortality. 39 In 2011, The World Health Organization published 23 recommendations for prevention and treatment of<br />
pre-eclampsia and eclampsia. The target audience was health care providers, particularly those in under-resourced<br />
settings. 39 While the guidelines are not intended as a comprehensive guide on treatment of pre-eclampsia and<br />
eclampsia, they do review the evidence of important topics related to the management of these disorders. Four of<br />
MATERNAL NUTRITION 26
the recommendations, summarized below, are related to micronutrient intakes and/or supplementation. In general,<br />
the group that developed the guidelines agreed that “healthy dietary practices should be promoted in the general<br />
population, including among pregnant women.” 39<br />
The WHO guidelines recommend calcium supplementation for pregnant women residing in areas where dietary<br />
calcium intake is low. The recommendation states, “ In areas where dietary calcium intake is low, calcium<br />
supplementation during pregnancy (at doses of 1.5-2.0 g elemental calcium/day) is recommended for the prevention<br />
of pre-eclampsia in all women, but especially in those at high risk of developing pre-eclampsia.” Additional<br />
calcium supplementation, however, does not improve outcomes related to pre-eclampsia and pregnancy- related<br />
hypertensive disorders for populations with adequate calcium intake. 39<br />
The expert group agreed that avoiding excessive dietary salt intake is a healthy dietary practice. However, restricting<br />
dietary salt intake during pregnancy to prevent pre-eclampsia was not recommended. The group did not define<br />
“excessive salt intake.” (Sodium intake recommendations during pregnancy are provided in Table 9). In addition,<br />
supplementation with vitamin D and supplementation with the antioxidant vitamins C and E, individually or in<br />
combination, are not recommended to prevent pre-eclampsia and its complications since research data available at<br />
the time did not support a beneficial effect. 39<br />
Gestational Diabetes<br />
Gestational diabetes mellitus (GDM) affects about 4% of all pregnancies worldwide. 141 Risk factors for GDM include<br />
having an immediate family member with diabetes, being overweight, having pre-diabetes, or having a history of<br />
GDM in a past pregnancy. Women with GDM have an increased risk of developing hypertension during pregnancy<br />
and are more likely to have a cesarean delivery, as infants born to mothers with poorly controlled GDM may be larger<br />
at birth, and macrosomic neonates are more prone to birth injury. 142 Children born to mothers with poorly controlled<br />
GDM are at greater risk for breathing problems and other serious illnesses in the newborn period, and they are more<br />
likely to become overweight in childhood or as adults. All pregnant women should be screened for GDM risk at their<br />
first prenatal visit. 40<br />
Women with GDM should receive nutritional counseling about a balanced diet that meets pregnancy nutrition needs,<br />
promotes appropriate weight gain, and fosters blood glucose control. 40 Appropriate weight gain may lessen risk of<br />
undesirable pregnancy outcomes. For example, women with singleton pregnancies diagnosed with GDM who gained<br />
more than the suggested amounts during pregnancy had higher risk of preterm delivery, delivering macrosomic<br />
neonates, and cesarean delivery. 143 In obese women with GDM, moderate caloric restriction may improve glycemic<br />
control without inducing ketonuria. 123 Women should also be made aware of the glucose-lowering benefits of physical<br />
activity. Programs of moderate physical exercise have been shown to lower maternal glucose concentrations in<br />
women with GDM and those without medical or obstetrical contraindications should be encouraged to start or<br />
continue a program of moderate exercise as a part of treatment for GDM. 144<br />
Women with GDM should be aware that they have a much higher risk (about 7 times higher) for developing type 2<br />
diabetes after delivery than women without GDM. 145 Therefore, in the US, the National Diabetes Education Program<br />
recommends that women with GDM be screened for type 2 diabetes 6 to 12 weeks after delivery. If initial blood<br />
glucose concentrations are normal, these women should be screened for type 2 diabetes every 3 years. 145 Women<br />
who had GDM can help lower their risk for developing type 2 diabetes by losing weight, increasing physical activity<br />
and making healthy food choices. Children born to women with GDM are also more likely to become obese and<br />
develop type 2 diabetes. Children’s risk is also lower if they stay at a healthy weight, consume a healthy diet and<br />
incorporate daily physical activity. 145<br />
27
Preterm birth<br />
Preterm birth—live birth before thirty-seven completed weeks of gestation—is a daunting obstetrical problem. An<br />
estimated 15 million babies are born preterm worldwide every year. 146 Preterm babies are at greater risk of death<br />
and disability, including cerebral palsy, sensory impairments, intellectual disabilities, and vision and hearing loss. 147<br />
Most preterm births occur between 32 and 36 weeks of gestation. Babies born before 34 weeks of pregnancy<br />
generally experience more health consequences that affect their ability to properly grow and develop, such as<br />
respiratory distress syndrome (RDS), necrotizing enterocolitis (NEC), and anemia, than do those born further along in<br />
gestation. 148<br />
The cause of preterm birth is unidentifi able in many cases but it is more common in women with a past history of<br />
preterm birth, multiparity, abnormalities of the cervix or uterus, and autoimmune diseases. 148 Maternal diabetes,<br />
hypertension, pre-eclampsia, gestational alcohol consumption, maternal stress and anxiety, smoking cigarettes<br />
during pregnancy, 148 pre-pregnancy underweight, and gaining an inadequate amount of weight during pregnancy 149<br />
are also associated with preterm birth risk.<br />
Some nutrient defi ciencies, such as folate and vitamin A defi ciencies, have been linked to preterm birth. 65,82,89 Several<br />
studies have investigated the relationship between maternal n-3 LCPUFA intake and duration of gestation and some<br />
suggest that consuming n-3 LCPUFA slightly increases duration of gestation (within the normal range). 72 In 2010,<br />
Makrides and colleagues reported the results of the large randomized DOMINO (DHA to Optimize Mother Infant<br />
Outcomes) trial with 2399 women. In this study, the group of women who received 800 mg DHA per day during<br />
pregnancy had signifi cantly fewer very preterm births (
Women are encouraged to enter pregnancy at a desirable body weight and with good control of chronic medical<br />
conditions, such as diabetes, to help optimize pregnancy outcomes. Once pregnancy is achieved, appropriate<br />
weight gain should be encouraged. In the United States, the IOM has issued detailed recommendations on<br />
pregnancy weight gain that are based on a woman’s pre-pregnancy BMI. Women with pre-pregnancy BMIs indicating<br />
overweight or obesity are encouraged to gain less weight than women with low or normal BMIs. Physical activity is<br />
encouraged for all women except those with specific obstetric and/or medical conditions.<br />
Recommended intakes for energy, protein and carbohydrate increase during pregnancy and lactation.<br />
Recommended intakes for total fat as a percentage of total energy do not change, but the importance of<br />
consuming the fatty acid DHA should be emphasized since it supports a healthy pregnancy and visual and cognitive<br />
development of the infant. The IOM and WHO also recommend higher intakes for several vitamins and minerals<br />
during pregnancy and lactation. It is important for pregnant and lactating women to consume adequate levels of all<br />
essential vitamins and minerals. Folic acid intakes during the first few weeks of pregnancy and iodine intakes during<br />
pregnancy and early infancy are particularly important since deficiencies of these nutrients can have irreversible<br />
negative consequences for an infant. Diet, nutrient, and lifestyle modifications may also prove helpful if pregnancyassociated<br />
conditions arise.<br />
The goal in highlighting these recommendations is to increase familiarity with nutrients and nutrition-related<br />
issues that play important roles in supporting healthy pregnancies and lactation. Eating a safe, balanced diet with<br />
appropriate levels of energy, macronutrients and micronutrients, getting regular physical activity, and avoiding noxious<br />
substances are increasingly recognized at strategies for achieving good pregnancy and lactation outcomes.<br />
29
REFERENCES<br />
1. World Health Organization. The world health report 2005 : make every mother<br />
and child count. Geneva: World Health Organization; 2005.<br />
2. <strong>Johnson</strong> K, Posner SF, Biermann J, Cordero JF, Atrash HK, Parker CS, Boulet S,<br />
Curtis MG. Recommendations to improve preconception health and health care -<br />
United States. A Report of the CDC/ATSDR Preconception Care Work Group and<br />
the Select Panel on Preconception Care. MMWR. 2006:1-23.<br />
3. Committee to Reexamine IOM Pregnancy Weight Guidelines, Institute of<br />
Medicine, National Research Council. Weight gain during pregnancy: reexamining<br />
the guidelines. Washington, D. C. : The National Academies Press; 2009.<br />
4. Poston L, Harthoorn LF, Van Der Beek EM. Obesity in pregnancy: implications<br />
for the mother and lifelong health of the child. A consensus statement. Pediatric<br />
Research. 2011 Feb;69:175-80.<br />
5. Institute of Medicine. Dietary Reference Intakes for energy, carbohydrate, fi ber,<br />
fat, fatty acids, cholesterol, protein, and amino acids. Washington, D. C. : The<br />
National Academies Press; 2005.<br />
6. FAO/WHO/UNU. Energy requirements of pregnancy. Report of a Joint FAO/WHO/<br />
UNU Expert Consultation: Human energy requirements. Rome: FAO; 2004.<br />
7. World Health Organization. Protein and amino acid requirements in human<br />
nutrition. Geneva: WHO; 2007.<br />
8. FAO. Fats and fatty acids in human nutrition: report of an expert consultation.<br />
Rome: FAO; 2010. p. 1-189.<br />
9. ANSES. Opinion of the French Food Safety Agency on the update of French<br />
population reference intakes (ANCs) for for fatty acids; 2010. Report No.: 2006-<br />
SA-0359.<br />
10. EFSA Panel on Dietetic Products <strong>Nutrition</strong> and Allergies. Scientifi c opinion on<br />
dietary reference values for fats, including saturated fatty acids, polyunsaturated<br />
fatty acids, monounsaturated fatty acids, trans fatty acids, and cholesterol. EFSA<br />
Journal. 2010;8.<br />
11. U.S. Preventive Services Task Force. Folic acid for the prevention of neural tube<br />
defects: U.S. Preventive Services Task Force recommendation statement. Ann<br />
Intern Med. 2009 May 5;150:626-31.<br />
12. Berry RJ, Li Z, Erickson JD, Li S, Moore CA, Wang H, Mulinare J, Zhao P, Wong<br />
LY, et al. Prevention of neural-tube defects with folic acid in China. China-U.S.<br />
Collaborative Project for Neural Tube Defect Prevention. N Engl J Med. 1999 Nov<br />
11;341:1485-90.<br />
13. Shaw GM, Carmichael SL, Yang W, Selvin S, Schaffer DM. Periconceptional<br />
dietary intake of choline and betaine and neural tube defects in offspring. Am J<br />
Epidemiol. 2004 Jul 15;160:102-9.<br />
14. Zeisel SH, Niculescu MD. Perinatal choline infl uences brain structure and function.<br />
Nutr Rev. 2006 Apr;64:197-203.<br />
15. Wagner CL, Taylor SN, Dawodu A, <strong>Johnson</strong> DD, Hollis BW. Vitamin D and its role<br />
during pregnancy in attaining optimal health of mother and fetus. Nutrients. 2012<br />
Mar;4:208-30.<br />
16. Whitehouse AJ, Holt BJ, Serralha M, Holt PG, Kusel MM, Hart PH. Maternal<br />
serum vitamin D levels during pregnancy and offspring neurocognitive<br />
development. Pediatrics. 2012 Feb 13;129:485-93.<br />
17. World Health Organization. Guideline: Vitamin A supplementation in pregnant<br />
women. Geneva: World Health Organization; 2011.<br />
18. World Health Organization. Weekly iron-folic acid supplementation (WIFS) in<br />
women of reproductive age: its role in promoting optimal maternal and child<br />
health. Position statement. 2009 [cited 15 June 2012]; Available from: http://www.<br />
searo.who.int/LinkFiles/<strong>Nutrition</strong>_for_Health_and_Development_WHO_weekly_<br />
iron_folic_acid.pdf<br />
19. de Benoist B, Andersson M, Egli I, Takkouche B, Allen H, editors. Iodine status<br />
worldwide: WHO Global Database on Iodine Defi ciency. Geneva: World Health<br />
Organization; 2004.<br />
20. Institute of Medicine. Dietary Reference Intakes for vitamin A, vitamin K, arsenic,<br />
boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon,<br />
vanadium, and zinc. Washington, D.C.: The National Academies Press; 2001.<br />
21. FAO/WHO. Vitamin and Mineral Requirements in Human <strong>Nutrition</strong>. Geneva: The<br />
World Health Organization and The Food and Agricultural Organization of the<br />
United Nations; 2004.<br />
22. Painter J, Rah JH, Lee YK. Comparison of international food guide pictorial<br />
representations. J Am Diet Assoc. 2002 Apr;102:483-9.<br />
23. U.S. Department of Health and Human Services. Chapter 7: Additional<br />
considerations for some adults. Physical activity guidelines for Americans.<br />
2008 [cited 3 April 2012]; Available from: http://www.health.gov/PAGuidelines/<br />
guidelines/chapter7.aspx<br />
24. Centers for Disease Control and Prevention. Physical activity for everyone. Healthy<br />
pregnant or postpartum women. 2011 [cited 3 April 2012]; Available from: http://<br />
www.cdc.gov/physicalactivity/everyone/guidelines/pregnancy.html<br />
25. World Health Organization. Global recommendations on physical activity for<br />
health. Geneva: World Health Organization; 2010.<br />
26. Artal R, O’Toole M. Guidelines of the American College of Obstetricians and<br />
Gynecologists for exercise during pregnancy and the postpartum period. Br J<br />
Sports Med. 2003 Feb;37:6-12; discussion<br />
27. Lovelady C. Balancing exercise and food intake with lactation to promote postpartum<br />
weight loss. Proc Nutr Soc. 2011 May;70:181-4.<br />
28. ACOG Committee on Obstetric Practice. ACOG Committee Opinion Number 267:<br />
Exercise during pregnancy and the postpartum period. Obstet Gynecol. 2002<br />
Reaffi rmed 2009 Jan;99:171-3.<br />
29. March of Dimes. Drinking alcohol during pregnancy. 2012 [cited 10 August 2012];<br />
Available from: http://www.marchofdimes.com/pregnancy/alcohol_indepth.html<br />
30. National Institutes of Health. Fetal alcohol syndrome. 2012 [cited 22 October<br />
2012]; Available from: http://www.nlm.nih.gov/medlineplus/ency/article/000911.<br />
htm<br />
31. Weng X, Odouli R, Li DK. Maternal caffeine consumption during pregnancy and<br />
the risk of miscarriage: a prospective cohort study. Am J Obstet Gynecol. 2008<br />
Mar;198:279 e1-8.<br />
32. Savitz DA, Chan RL, Herring AH, Howards PP, Hartmann KE. Caffeine and<br />
miscarriage risk. Epidemiology. 2008 Jan;19:55-62.<br />
33. Jahanfar S, Sharifah H. Effects of restricted caffeine intake by mother on<br />
fetal, neonatal and pregnancy outcome. Cochrane Database Syst Rev.<br />
2009:CD006965.<br />
34. March of Dimes. Caffeine in pregnancy. 2010 [cited 10 October 2012]; Available<br />
from: http://www.marchofdimes.com/pregnancy/nutrition_caffeine.html<br />
35. FAO/WHO. Report of the Joint FAO/WHO Expert Consultation on the risks and<br />
benefi ts of fi sh consumption. Rome: Food and Agriculture Organization of the<br />
United Nations. Geneva: World Health Organization; 2011.<br />
36. U.S. Environmental Protection Agency, U.S. Food and Drug Administration.<br />
Consumption Advice: Joint Federal Advisory for Mercury in Fish. Backgrounder for<br />
the 2004 FDA/EPA consumer advisory: What you need to know about mercury in<br />
fi sh and shellfi sh. 2004 [cited 22 October 2012]; Available from: http://water.epa.<br />
gov/scitech/swguidance/fi shshellfi sh/outreach/factsheet.cfm<br />
37. U.S. Department of Agriculture, U.S. Department of Health and Human<br />
Services. Dietary Guidelines for Americans 2010. 7th ed. Washington, DC: U.S.<br />
Government Printing Offi ce; 2010.<br />
38. U. S. Food and Drug Administration, Center for Food Safety and Applied <strong>Nutrition</strong>.<br />
Food safety for moms-to-be. 2012 [cited 05 September 2012]; Available from:<br />
http://www.fda.gov/food/resourcesforyou/healtheducators/ucm081785.htm<br />
39. World Health Organization. WHO recommendations for prevention and treatment<br />
of pre-eclampsia and eclampsia. Geneva: World Health Organization; 2011.<br />
40. Expert Committee on the Diagnosis and Classifi cation of Diabetes Mellitus. Report<br />
of the Expert Committee on the Diagnosis and Classifi cation of Diabetes Mellitus.<br />
Diabetes Care. 1997 Jul;20:1183-97.<br />
41. Waller DK, Shaw GM, Rasmussen SA, Hobbs CA, Canfi eld MA, Siega-Riz AM,<br />
Gallaway MS, Correa A. Prepregnancy obesity as a risk factor for structural birth<br />
defects. Arch Pediatr Adolesc Med. 2007 Aug;161:745-50.<br />
42. Kaiser L, Allen LH. Position of the American Dietetic Association: nutrition and<br />
lifestyle for a healthy pregnancy outcome. J Am Diet Assoc. 2008 Mar;108:553-<br />
61.<br />
43. Barker DJ. Fetal origins of coronary heart disease. BMJ. 1995 Jul 15;311:171-4.<br />
44. Barker DJ. The developmental origins of adult disease. J Am Coll Nutr. 2004<br />
Dec;23:588S-95S.<br />
45. Walker SP, Wachs TD, Grantham-McGregor S, Black MM, Nelson CA, Huffman<br />
SL, Baker-Henningham H, Chang SM, Hamadani JD, et al. Inequality in early<br />
childhood: risk and protective factors for early child development. Lancet. 2011<br />
Oct 8;378:1325-38.<br />
46. Siega-Riz AM, King JC. Position of the American Dietetic Association and<br />
American Society for <strong>Nutrition</strong>: obesity, reproduction, and pregnancy outcomes.<br />
J Am Diet Assoc. 2009 May;109:918-27.<br />
47. World Health Organization. Physical Status: The use and interpretation of<br />
anthropometry. Report of a WHO Expert Committee. Geneva: World Health<br />
Organization; 1995.<br />
48. Gesink Law DC, Maclehose RF, Longnecker MP. Obesity and time to pregnancy.<br />
Hum Reprod. 2007 Feb;22:414-20.<br />
49. Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM.<br />
Prevalence of overweight and obesity in the United States, 1999-2004. JAMA.<br />
2006 Apr 5;295:1549-55.<br />
50. Wang JX, Davies M, Norman RJ. Body mass and probability of pregnancy<br />
during assisted reproduction treatment: retrospective study. BMJ. 2000 Nov<br />
25;321:1320-1.<br />
51. Oken E, Taveras EM, Kleinman KP, Rich-Edwards JW, Gillman MW. Gestational<br />
weight gain and child adiposity at age 3 years. Am J Obstet Gynecol. 2007<br />
Apr;196:322 e1-8.<br />
52. Mok E, Multon C, Piguel L, Barroso E, Goua V, Christin P, Perez MJ, Hankard R.<br />
Decreased full breastfeeding, altered practices, perceptions, and infant weight<br />
change of prepregnant obese women: a need for extra support. Pediatrics. 2008<br />
May;121:e1319-24.<br />
MATERNAL NUTRITION 30
53. Viswanathan M, Siega-Riz AM, Moos M-K, Deierlein A, Mumford S, Knaack J,<br />
Thieda P, Lux LJ, Lohr KN. Outcomes of maternal weight gain, Evidence Report/<br />
Technology Assessment No. 168. Rockville, MD: AHRQ; 2008.<br />
54. Centers for Disease Control and Prevention. National diabetes fact sheet. 2011<br />
[cited 29 October 2012]; Available from: http://www.cdc.gov/diabetes/pubs/pdf/<br />
ndfs_2011.pdf<br />
55. Correa A, Gilboa SM, Besser LM, Botto LD, Moore CA, Hobbs CA, Cleves MA,<br />
Riehle-Colarusso TJ, Waller DK, Reece EA. Diabetes mellitus and birth defects.<br />
Am J Obstet Gynecol. 2008 Sep;199:237 e1-9.<br />
56. HAPO Study Cooperative Research Group, Metzger BE, Lowe LP, Dyer AR,<br />
Trimble ER, Chaovarindr U, Coustan DR, Hadden DR, McCance DR, et al.<br />
Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008 May<br />
8;358:1991-2002.<br />
57. Boulet SL, Parker C, Atrash H. Preconception care in international settings.<br />
Matern Child Health J. 2006 Sep;10:S29-35.<br />
58. Centers for Disease Control and Prevention. Preconception care and health care.<br />
Information for health professionals. Clinical content of care for women. 2012<br />
[cited 4 September 2012]; Available from: http://www.cdc.gov/preconception/<br />
careforwomen/index.html<br />
59. Centers for Disease Control and Prevention, Department of Health and Human<br />
Services. Unintended pregnancy prevention. 2012 [cited 22 October 2012];<br />
Available from: http://www.cdc.gov/reproductivehealth/UnintendedPregnancy/<br />
index.htm<br />
60. National Institutes of Health, National Library of Medicine. Medical Encyclopedia.<br />
Fetal development. 2011 [cited 22 October 2012]; Available from: http://www.<br />
nlm.nih.gov/medlineplus/ency/article/002398.htm<br />
61. Wong W, Tang NL, Lau TK, Wong TW. A new recommendation for maternal<br />
weight gain in Chinese women. J Am Diet Assoc. 2000 Jul;100:791-6.<br />
62. Kac G, Nucci LB, Spyrides MH, Duncan BB, Schmidt MI. Evaluation of the<br />
ability of a Latin-American gestational weight curve to predict adverse pregnancy<br />
outcomes. International journal of gynaecology and obstetrics: the official organ of<br />
the International Federation of Gynaecology and Obstetrics. 2009 Sep;106:223-6.<br />
63. Health Canada. Canadian gestational weight gain recommendations. 2010 [cited<br />
25 April 2012]; Available from: www.hc-sc.gc.ca/fn-an/nutrition/prenatal/qa-gestgros-qr-eng.php<br />
64. Yaktine A. Calculating estimates for total gestational weight gain for normal and<br />
overweight women based on first trimester gains. Personal communication to AM<br />
Siega-Riz, October 8, 2012.<br />
65. Berti C, Biesalski HK, Gartner R, Lapillonne A, Pietrzik K, Poston L, Redman<br />
C, Koletzko B, Cetin I. Micronutrients in pregnancy: current knowledge and<br />
unresolved questions. Clin Nutr. 2011 Dec;30:689-701.<br />
66. Marcason W. What are the calorie requirements for women having twins J Am<br />
Diet Assoc. 2006 Aug;106:1292.<br />
67. FAO/WHO/UNU. Energy requirements of lactation. Report of a Joint FAO/WHO/<br />
UNU Expert Consultation: Human energy requirements. Rome: FAO; 2004.<br />
68. Lovelady CA, Garner KE, Moreno KL, Williams JP. The effect of weight loss in<br />
overweight, lactating women on the growth of their infants. N Engl J Med. 2000<br />
Feb 17;342:449-53.<br />
69. Neuringer M, Anderson GJ, Connor WE. The essentiality of n-3 fatty acids for the<br />
development and function of the retina and brain. Ann Rev Nutr. 1988;8:517-41.<br />
70. Makrides M. Is there a dietary requirement for DHA in pregnancy Prostaglandins<br />
Leukot Essent Fatty Acids. 2009 Aug-Sep;81:171-4.<br />
71. Lapillonne A, Jensen CL. Reevaluation of the DHA requirement for the premature<br />
infant. Prostaglandins Leukot Essent Fatty Acids. 2009 Aug-Sep;81:143-50.<br />
72. Brenna JT, Lapillonne A. Background paper on fat and fatty acid requirements<br />
during pregnancy and lactation. Ann Nutr Metab. 2009;55:97-122.<br />
73. Koletzko B, Lien E, Agostoni C, Bohles H, Campoy C, Cetin I, Decsi T,<br />
Dudenhausen JW, Dupont C, et al. The roles of long-chain polyunsaturated<br />
fatty acids in pregnancy, lactation and infancy: review of current knowledge and<br />
consensus recommendations. J Perinat Med. 2008;36:5-14.<br />
74. Martinez M. Tissue levels of polyunsaturated fatty acids during early human<br />
development. J Pediatr. 1992 Apr;120:S129-38.<br />
75. Brenna JT, Varamini B, Jensen RG, Diersen-Schade DA, Boettcher JA, Arterburn<br />
LM. Docosahexaenoic and arachidonic acid concentrations in human breast milk<br />
worldwide. Am J Clin Nutr. 2007;85:1457-64.<br />
76. Hoffman DR, Boettcher JA, Diersen-Schade DA. Toward optimizing vision and<br />
cognition in term infants by dietary docosahexaenoic and arachidonic acid<br />
supplementation: a review of randomized controlled trials. Prostaglandins Leukot<br />
Essent Fatty Acids. 2009 Aug-Sep;81:151-8.<br />
77. March of Dimes. Pregnancy. 2012 [cited 15 Nov 2012] Available from http://<br />
www.marchofdimes.com/pregnancy/nutrition_omega3.html and http://www.<br />
marchofdimes.com/pregnancy/physicalactivity_indepth.html<br />
78. Koletzko B, Cetin I, Brenna JT. Dietary fat intakes for pregnant and lactating<br />
women. Br J Nutr. 2007 Nov;98:873-7.<br />
79. Otten JJ, Pitzi Hellwig J, Meyers LD, editors. Dietary Reference Intakes: The<br />
Essential Guide to Nutrient Requirements. Washington, D. C.: National Academies<br />
Press; 2006.<br />
80. Institute of Medicine. Dietary Reference Intakes for calcium and vitamin D.<br />
Washington, D.C: The National Academies Press; 2011.<br />
81. Institute of Medicine. Dietary Reference Intakes for thiamin, riboflavin, niacin,<br />
vitamin B6, folate, vitamin B12, pantothenic acid, biotin, and choline. Washington,<br />
D. C.: The National Academies Press;1998.<br />
82. Scholl TO, <strong>Johnson</strong> WG. Folic acid: influence on the outcome of pregnancy. Am J<br />
Clin Nutr. 2000 May;71:1295S-303S.<br />
83. ACOG. ACOG Practice Bulletin. Clinical Management Guidelines for Obstetrician-<br />
Gynecologists. Number 60, March 2005. Pregestational diabetes mellitus. Obstet<br />
Gynecol. 2005;105:675-85.<br />
84. Buttriss J. Strategies designed to increase awareness about folates and health,<br />
and to increase folate intake: A review. Trends in Food Science & Technology.<br />
2005;16:246-52.<br />
85. Crider KS, Bailey LB, Berry RJ. Folic acid food fortification-its history, effect,<br />
concerns, and future directions. Nutrients. 2011 Mar;3:370-84.<br />
86. Heseker HB, Mason JB, Selhub J, Rosenberg IH, Jacques PF. Not all cases of<br />
neural-tube defect can be prevented by increasing the intake of folic acid. Br J<br />
Nutr. 2009 Jul;102:173-80.<br />
87. Siega-Riz AM, Savitz DA, Zeisel SH, Thorp JM, Herring A. Second trimester folate<br />
status and preterm birth. Am J Obstet Gynecol. 2004 Dec;191:1851-7.<br />
88. Wen SW, Chen XK, Rodger M, White RR, Yang Q, Smith GN, Sigal RJ, Perkins<br />
SL, Walker MC. Folic acid supplementation in early second trimester and the risk<br />
of preeclampsia. Am J Obstet Gynecol. 2008 Jan;198:45 e1-7.<br />
89. Furness DLF, Yasin N, Dekker GA, Thompson SD, Roberts CT. Maternal red blood<br />
cell folate concentration at 10-12 weeks gestation and pregnancy outcome.<br />
Journal of Maternal-Fetal and Neonatal Medicine. 2012;25:1423-7.<br />
90. Timmermans S, Jaddoe VWV, Hofman A, Steegers-Theunissen RPM, Steegers<br />
EAP. Periconception folic acid supplementation, fetal growth and the risks of<br />
low birth weight and preterm birth: The Generation R Study. British Journal of<br />
<strong>Nutrition</strong>. 2009;102:777-85.<br />
91. von Schenck U, Bender-Gotze C, Koletzko B. Persistence of neurological damage<br />
induced by dietary vitamin B-12 deficiency in infancy. Arch Dis Child. 1997<br />
Aug;77:137-9.<br />
92. Zeisel SH. Choline: an essential nutrient for humans. <strong>Nutrition</strong>. 2000 Jul-<br />
Aug;16:669-71.<br />
93. Shaw GM, Finnell RH, Blom HJ, Carmichael SL, Vollset SE, Yang W, Ueland<br />
PM. Choline and risk of neural tube defects in a folate-fortified population.<br />
Epidemiology. 2009 Sep;20:714-9.<br />
94. Chester DN, Goldman JD, Ahuja JK, Moshfegh AJ. Dietary intakes of choline:<br />
what we eat in America, NHANES 2007-2008. Food Surveys Research Group<br />
Dietary Data Brief No 9. 2011 [cited 29 October 2012]; Available from: http://<br />
www.ars.usda.gov/SP2UserFiles/Place/12355000/pdf/DBrief/9_choline_<br />
intakes_0708.pdf<br />
95. U.S. Department of Agriculture. USDA database for the choline content of<br />
common foods. 2008 . Available from: http://www.ars.usda.gov/services/docs.<br />
htmdocid=6232<br />
96. Ervin RB, Wright JD, Wang CY, Kennedy-Stephenson J. Dietary intake of selected<br />
vitamins for the United States population: 1999-2000. Advance Data from Vital<br />
and Health Statistics. 2004 Mar 12:1-4.<br />
97. Institute of Medicine. Dietary Reference Intakes for calcium, phosphorus,<br />
magnesium, vitamin D, and fluoride. Washington, D. C. : The National Academies<br />
Press; 1997.<br />
98. <strong>Johnson</strong> LE, DeLuca HF. Reproductive defects are corrected in vitamin<br />
D-deficient female rats fed a high calcium, phosphorus and lactose diet. J Nutr.<br />
2002 Aug;132:2270-3.<br />
99. Looker AC, <strong>Johnson</strong> CL, Lacher DA, Pfeiffer CM, Schleicher RL, Sempos CT.<br />
Vitamin D status: United States, 2001-2006. NCHS data brief. 2011 Mar:1-8.<br />
100. Bodnar LM, Simhan HN, Powers RW, Frank MP, Cooperstein E, Roberts JM. High<br />
prevalence of vitamin D insufficiency in black and white pregnant women residing<br />
in the northern United States and their neonates. J Nutr. 2007 Feb;137:447-52.<br />
101. Bodnar LM, Catov JM, Roberts JM, Simhan HN. Prepregnancy obesity predicts<br />
poor vitamin D status in mothers and their neonates. J Nutr. 2007 Nov;137:2437-<br />
42.<br />
102. Robinson CJ, Wagner CL, Hollis BW, Baatz JE, <strong>Johnson</strong> DD. Association of<br />
maternal vitamin D and placenta growth factor with the diagnosis of early onset<br />
severe preeclampsia. Am J Perinatol. 2012;In Press.<br />
103. Thorne-Lyman A, Fawzi WW. Vitamin D during pregnancy and maternal, neonatal<br />
and infant health outcomes: a systematic review and meta-analysis. Paediatric<br />
and Perinatal Epidemiology. 2012;26:75-90.<br />
104. De-Regil LM, Palacios C, Ansary A, Kulier R, Pena-Rosas JP. Vitamin D<br />
supplementation for women during pregnancy. Cochrane Database Syst Rev.<br />
2012;2:CD008873.<br />
31
105. ACOG Committee on Obstetric Practice. ACOG Committee Opinion No. 495:<br />
Vitamin D: Screening and supplementation during pregnancy. Obstet Gynecol.<br />
2011 Jul;118:197-8.<br />
106. National Institutes of Health, Offi ce of Dietary Supplements. Dietary Supplement<br />
Fact Sheet: Iron. 2007 [cited 22 October 2012]; Available from: http://ods.od.nih.<br />
gov/factsheets/iron/<br />
107. Pavord S, Myers B, Robinson S, Allard S, Strong J, Coppenheimer C. UK<br />
guidelines on the management of iron defi ciency in pregnancy. London: British<br />
Society for Haematology; 2011.<br />
108. Scholl TO. Iron status during pregnancy: setting the stage for mother and infant.<br />
Am J Clin Nutr. 2005 May;81:1218S-22S.<br />
109. Centers for Disease Control and Prevention. Recommendations to prevent and<br />
control iron defi ciency in the United States. MMWR. 1998:RR-3.<br />
110. Ramakrishnan U, Grant F, Goldenberg T, Zongrone A, Martorell R. Effect of<br />
women’s nutrition before and during early pregnancy on maternal and infant<br />
outcomes: A systematic review. Paediatric and Perinatal Epidemiology.<br />
2012;26:285-301.<br />
111. Scholl TO. Maternal iron status: Relation to fetal growth, length of gestation, and<br />
iron endowment of the neonate. <strong>Nutrition</strong> Reviews. 2011;69:S23-S9.<br />
112. Rodriguez-Bernal CL, Rebagliato M, Ballester F. Maternal nutrition and fetal<br />
growth: the role of iron status and intake during pregnancy. <strong>Nutrition</strong> and Dietary<br />
Supplements 2012;4:25-37.<br />
113. Siega-Riz AM, Hartzema AG, Turnbull C, Thorp J, McDonald T, Cogswell ME.<br />
The effects of prophylactic iron given in prenatal supplements on iron status<br />
and birth outcomes: a randomized controlled trial. Am J Obstet Gynecol. 2006<br />
Feb;194:512-9.<br />
114. Villar J, Abdel-Aleem H, Merialdi M, Mathai M, Ali MM, Zavaleta N, Purwar M,<br />
Hofmeyr J, thi Nhu Ngoc N, et al. World Health Organization randomized trial of<br />
calcium supplementation among low calcium intake pregnant women. Am Journal<br />
of Obstet Gynecol. 2006;194:639-49.<br />
115. Mahan K, Escott-Stump, S. Krause’s Food, <strong>Nutrition</strong>, and Diet Therapy. 11 ed.<br />
Philadelphia: Elsevier; 2004.<br />
116. Donangelo CM, King JC. Maternal zinc intakes and homeostatic adjustments<br />
during pregnancy and lactation. Nutrients. 2012;4:782-98.<br />
117. Taylor CJ, Moore G, Davidson DC. The effect of treatment on zinc, copper and<br />
calcium status in children with phenylketonuria. J Inherit Metab Dis. 1984;7:160-<br />
4.<br />
118. UNICEF. Delivering essential micronutrients: Iodine. Micronutrients - iodine, iron<br />
and vitamin A 2003 [cited 6 June 2012]; Available from: http://www.unicef.org/<br />
nutrition/index_iodine.html<br />
119. Haider BA, Bhutta ZA. Multiple-micronutrient supplementation for women during<br />
pregnancy. Cochrane Database Syst Rev. 2006:CD004905.<br />
120. Lumbiganon P. Multiple-micronutrient supplementation for women during<br />
pregnancy: RHL commentary The WHO Reproductive Health Library. 23 August<br />
2007 [cited 26 June 2012]; Available from: http://apps.who.int/rhl/pregnancy_<br />
childbirth/antenatal_care/nutrition/plcom2/en/index.html<br />
121. Ramakrishnan U, Grant FK, Goldenberg T, Bui V, Imdad A, Bhutta ZA. Effect of<br />
multiple micronutrient supplementation on pregnancy and infant outcomes: A<br />
systematic review. Paediatric and Perinatal Epidemiology. 2012;26:153-67.<br />
122. Dempsey JC, Sorensen TK, Williams MA, Lee IM, Miller RS, Dashow EE, Luthy<br />
DA. Prospective study of gestational diabetes mellitus risk in relation to maternal<br />
recreational physical activity before and during pregnancy. Am J Epidemiol. 2004<br />
Apr 1;159:663-70.<br />
123. Bantle JP, Wylie-Rosett J, Albright AL, Apovian CM, Clark NG, Franz MJ,<br />
Hoogwerf BJ, Lichtenstein AH, Mayer-Davis E, et al. <strong>Nutrition</strong> recommendations<br />
and interventions for diabetes: a position statement of the American Diabetes<br />
Association. Diabetes Care. 2008 Jan;31 Suppl 1:S61-78.<br />
124. Clapp JF, 3rd, Kim H, Burciu B, Lopez B. Beginning regular exercise in early<br />
pregnancy: effect on fetoplacental growth. Am J Obstet Gynecol. 2000<br />
Dec;183:1484-8.<br />
125. Institute of Medicine. Dietary Reference Intakes for water, potassium, sodium,<br />
chloride, and sulfate. Washington, D. C.: The National Academies Press; 2005.<br />
126. McCrory MA, Nommsen-Rivers LA, Mole PA, Lonnerdal B, Dewey KG.<br />
Randomized trial of the short-term effects of dieting compared with dieting plus<br />
aerobic exercise on lactation performance. Am J Clin Nutr. 1999 May;69:959-67.<br />
127. Day NL, Leech SL, Richardson GA, Cornelius MD, Robles N, Larkby C. Prenatal<br />
alcohol exposure predicts continued defi cits in offspring size at 14 years of age.<br />
Alcohol Clin Exp Res. 2002 Oct;26:1584-91.<br />
128. Sood B, Delaney-Black V, Covington C, Nordstrom-Klee B, Ager J, Templin T,<br />
Janisse J, Martier S, Sokol RJ. Prenatal alcohol exposure and childhood behavior<br />
at age 6 to 7 years: I. dose-response effect. Pediatrics. 2001 Aug;108:E34.<br />
129. Kesmodel U, Wisborg K, Olsen SF, Henriksen TB, Secher NJ. Moderate alcohol<br />
intake during pregnancy and the risk of stillbirth and death in the fi rst year of life.<br />
Am J Epidemiol. 2002 Feb 15;155:305-12.<br />
130. American Academy of Pediatrics Committee on Drugs. Transfer of drugs and<br />
other chemicals into human milk. Pediatrics. 2001 Sep;108:776-89.<br />
131. National Institutes of Health and National Library of Medicine. Medical<br />
Encyclopedia. Breastfeeding - self-care. 2011 [cited 10 August 2012]; Available<br />
from: http://www.nlm.nih.gov/medlineplus/ency/article/002454.htm<br />
132. Mozaffarian D, Rimm EB. Fish intake, contaminants, and human health: evaluating<br />
the risks and the benefi ts. JAMA. 2006 Oct 18;296:1885-99.<br />
133. Oken E, Osterdal ML, Gillman MW, Knudsen VK, Halldorsson TI, Strom M,<br />
Bellinger DC, Hadders-Algra M, Michaelsen KF, Olsen SF. Associations of<br />
maternal fi sh intake during pregnancy and breastfeeding duration with attainment<br />
of developmental milestones in early childhood: a study from the Danish National<br />
Birth Cohort. Am J Clin Nutr. 2008 Sep;88:789-96.<br />
134. Hibbeln JR, Davis JM, Steer C, Emmett P, Rogers I, Williams C, Golding J.<br />
Maternal seafood consumption in pregnancy and neurodevelopmental outcomes<br />
in childhood (ALSPAC study): an observational cohort study. Lancet. 2007 Feb<br />
17;369:578-85.<br />
135. Bakardjiev AI, Theriot JA, Portnoy DA. Listeria monocytogenes traffi cs from<br />
maternal organs to the placenta and back. PLoS Pathog. 2006 Jun;2:e66.<br />
136. Lopez A, Dietz VJ, Wilson M, Navin TR, Jones JL. Preventing congenital<br />
toxoplasmosis. MMWR Recomm Rep. 2000 Mar 31;49:59-68.<br />
137. U.S. National Library of Medicine, National Institutes of Health. Hyperemesis<br />
gravidarum. 2010 [cited 15 May 2012]; Available from: http://www.nlm.nih.gov/<br />
medlineplus/ency/article/001499.htm<br />
138. The Merck Manuals Online Medical Library. Hyperemesis Gravidarum. 2010 [cited<br />
22 October 2012]; Available from: http://www.merckmanuals.com/professional/<br />
gynecology_and_obstetrics/abnormalities_of_pregnancy/hyperemesis_<br />
gravidarum.html<br />
139. Duckitt K, Harrington D. Risk factors for pre-eclampsia at antenatal booking:<br />
systematic review of controlled studies. BMJ. 2005 Mar 12;330:565.<br />
140. Getahun D, Ananth CV, Oyelese Y, Chavez MR, Kirby RS, Smulian JC. Primary<br />
preeclampsia in the second pregnancy: effects of changes in prepregnancy body<br />
mass index between pregnancies. Obstet Gynecol. 2007 Dec;110:1319-25.<br />
141. International Diabetes Federation. Types of diabetes. 2011 [cited 8 May 2012];<br />
Available from: http://www.idf.org/types-diabetes<br />
142. ADAM Medical Encyclopedia. Gestational diabetes: Glucose intolerance during<br />
pregnancy. 2012 [cited 8 May 2012]; Available from: http://www.ncbi.nlm.nih.gov/<br />
pubmedhealth/PMH0001898/<br />
143. Cheng YW, Chung JH, Kurbisch-Block I, Inturrisi M, Shafer S, Caughey AB.<br />
Gestational weight gain and gestational diabetes mellitus: perinatal outcomes.<br />
Obstet Gynecol. 2008 Nov;112:1015-22.<br />
144. American Diabetes Association. Position Statement: Gestational diabetes mellitus.<br />
Diabetes Care. 2004 Jan;27 Suppl 1:S88-90.<br />
145. National Diabetes Education Program. Diabetes risk after gestational diabetes;<br />
2011 [cited 22 October 2012]; Available from: http://ndep.nih.gov/am-i-at-risk/<br />
gdm/index.aspx<br />
146. World Health Organization. Preterm birth. 2012 [cited 9 May 2012]; Available<br />
from: http://www.who.int/mediacentre/factsheets/fs363/en/<br />
147. March Of Dimes. Premature birth. 2012 [cited 31 October 2012]; Available from:<br />
http://www.marchofdimes.com/baby/premature_indepth.html<br />
148. Institute of Medicine Committee on Understanding Premature Birth and Assuring<br />
Healthy Outcomes, Board on Health Sciences Policy. Preterm birth: causes,<br />
consequences, and prevention. Washington, D. C.: The National Academies<br />
Press; 2007.<br />
149. Schieve LA, Cogswell ME, Scanlon KS. Maternal weight gain and preterm<br />
delivery: differential effects by body mass index. Epidemiology. 1999 Mar;10:<br />
141-7.<br />
150. Makrides M, Gibson RA, McPhee AJ, Yelland L, Quinlivan J, Ryan P. Effect<br />
of DHA supplementation during pregnancy on maternal depression and<br />
neurodevelopment of young children: a randomized controlled trial. JAMA. 2010<br />
Oct 20;304:1675-83.<br />
MATERNAL NUTRITION 32
XXXXXX NEW 12/12 ©2012 <strong>Mead</strong> <strong>Johnson</strong> & Company, LLC