Spring 2013 - Tufts University School of Dental Medicine
Spring 2013 - Tufts University School of Dental Medicine
Spring 2013 - Tufts University School of Dental Medicine
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
leading-edge science<br />
regeneration<br />
multipurpose cells could act as biological repair<br />
kits, treating diseases that won’t get better on<br />
their own by David Levin<br />
for most <strong>of</strong> us, minor<br />
wounds are just an inconvenience.<br />
We endure the minor<br />
pain <strong>of</strong> a cut or scrape, stick on<br />
a bandage and within a week,<br />
our skin looks like nothing ever<br />
happened.<br />
In some cases, though,<br />
healing isn’t so simple.<br />
Somewhere along the way,<br />
the complex chain <strong>of</strong> events<br />
that lets the body repair itself<br />
breaks down, and a wound<br />
remains open, raw. Such is<br />
the case with those who suffer<br />
from chronic foot ulcers, a<br />
nonhealing wound common<br />
in diabetics.<br />
“For these foot ulcers,<br />
there are a variety <strong>of</strong> therapies,<br />
but they are only successful<br />
in roughly half the cases,<br />
and [the ulcers] have a high<br />
recurrence rate,” says Jonathan<br />
Garlick, head <strong>of</strong> the Division<br />
<strong>of</strong> Cancer Biology and Tissue<br />
Engineering at <strong>Tufts</strong> <strong>School</strong> <strong>of</strong><br />
<strong>Dental</strong> <strong>Medicine</strong>. If the wound<br />
doesn’t heal, sometimes the<br />
only recourse is to amputate<br />
the limb.<br />
Garlick’s research could one<br />
day help patients avoid that<br />
kind <strong>of</strong> traumatic outcome.<br />
He studies pluripotent stem<br />
cells—a type <strong>of</strong> all-purpose<br />
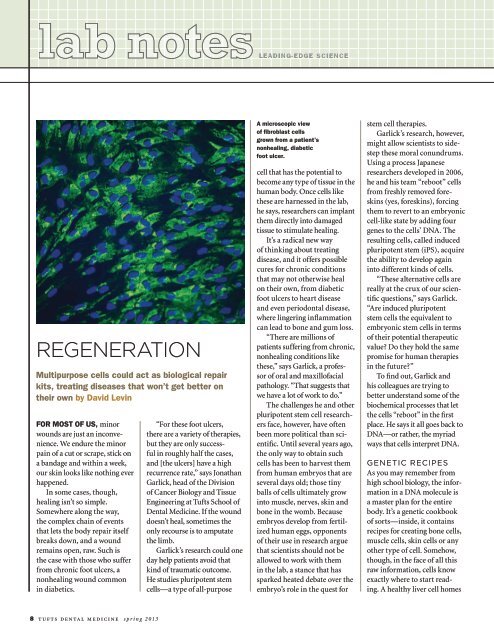
A microscopic view<br />
<strong>of</strong> fibroblast cells<br />
grown from a patient’s<br />
nonhealing, diabetic<br />
foot ulcer.<br />
cell that has the potential to<br />
become any type <strong>of</strong> tissue in the<br />
human body. Once cells like<br />
these are harnessed in the lab,<br />
he says, researchers can implant<br />
them directly into damaged<br />
tissue to stimulate healing.<br />
It’s a radical new way<br />
<strong>of</strong> thinking about treating<br />
disease, and it <strong>of</strong>fers possible<br />
cures for chronic conditions<br />
that may not otherwise heal<br />
on their own‚ from diabetic<br />
foot ulcers to heart disease<br />
and even periodontal disease,<br />
where lingering inflammation<br />
can lead to bone and gum loss.<br />
“There are millions <strong>of</strong><br />
patients suffering from chronic,<br />
nonhealing conditions like<br />
these,” says Garlick, a pr<strong>of</strong>essor<br />
<strong>of</strong> oral and maxill<strong>of</strong>acial<br />
pathology. “That suggests that<br />
we have a lot <strong>of</strong> work to do.”<br />
The challenges he and other<br />
pluripotent stem cell researchers<br />
face, however, have <strong>of</strong>ten<br />
been more political than scientific.<br />
Until several years ago,<br />
the only way to obtain such<br />
cells has been to harvest them<br />
from human embryos that are<br />
several days old; those tiny<br />
balls <strong>of</strong> cells ultimately grow<br />
into muscle, nerves, skin and<br />
bone in the womb. Because<br />
embryos develop from fertilized<br />
human eggs, opponents<br />
<strong>of</strong> their use in research argue<br />
that scientists should not be<br />
allowed to work with them<br />
in the lab, a stance that has<br />
sparked heated debate over the<br />
embryo’s role in the quest for<br />
stem cell therapies.<br />
Garlick’s research, however,<br />
might allow scientists to sidestep<br />
these moral conundrums.<br />
Using a process Japanese<br />
researchers developed in 2006,<br />
he and his team “reboot” cells<br />
from freshly removed foreskins<br />
(yes, foreskins), forcing<br />
them to revert to an embryonic<br />
cell-like state by adding four<br />
genes to the cells’ DNA. The<br />
resulting cells, called induced<br />
pluripotent stem (iPS), acquire<br />
the ability to develop again<br />
into different kinds <strong>of</strong> cells.<br />
“These alternative cells are<br />
really at the crux <strong>of</strong> our scientific<br />
questions,” says Garlick.<br />
“Are induced pluripotent<br />
stem cells the equivalent to<br />
embryonic stem cells in terms<br />
<strong>of</strong> their potential therapeutic<br />
value Do they hold the same<br />
promise for human therapies<br />
in the future”<br />
To find out, Garlick and<br />
his colleagues are trying to<br />
better understand some <strong>of</strong> the<br />
biochemical processes that let<br />
the cells “reboot” in the first<br />
place. He says it all goes back to<br />
DNA—or rather, the myriad<br />
ways that cells interpret DNA.<br />
Genetic Recipes<br />
As you may remember from<br />
high school biology, the information<br />
in a DNA molecule is<br />
a master plan for the entire<br />
body. It’s a genetic cookbook<br />
<strong>of</strong> sorts—inside, it contains<br />
recipes for creating bone cells,<br />
muscle cells, skin cells or any<br />
other type <strong>of</strong> cell. Somehow,<br />
though, in the face <strong>of</strong> all this<br />
raw information, cells know<br />
exactly where to start reading.<br />
A healthy liver cell homes<br />
8 tufts dental medicine spring <strong>2013</strong>