Childhood Immunisation Policy - Halton and St Helens PCT
Childhood Immunisation Policy - Halton and St Helens PCT
Childhood Immunisation Policy - Halton and St Helens PCT
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
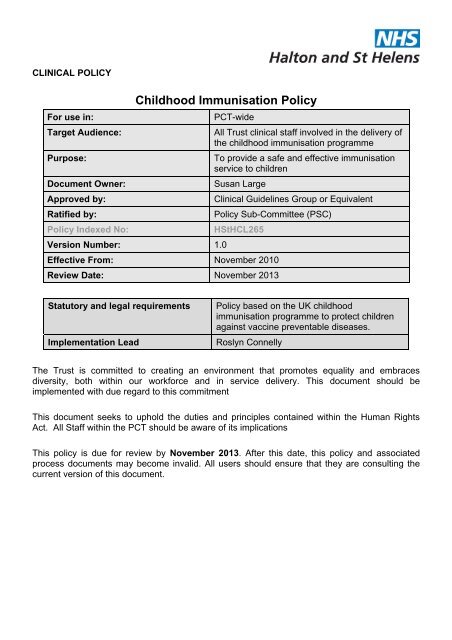
CLINICAL POLICY<br />
<strong>Childhood</strong> <strong>Immunisation</strong> <strong>Policy</strong><br />
For use in:<br />
<strong>PCT</strong>-wide<br />
Target Audience:<br />
All Trust clinical staff involved in the delivery of<br />
the childhood immunisation programme<br />
Purpose:<br />
To provide a safe <strong>and</strong> effective immunisation<br />
service to children<br />
Document Owner:<br />
Susan Large<br />
Approved by:<br />
Clinical Guidelines Group or Equivalent<br />
Ratified by:<br />
<strong>Policy</strong> Sub-Committee (PSC)<br />
<strong>Policy</strong> Indexed No:<br />
H<strong>St</strong>HCL265<br />
Version Number: 1.0<br />
Effective From: November 2010<br />
Review Date: November 2013<br />
<strong>St</strong>atutory <strong>and</strong> legal requirements<br />
Implementation Lead<br />
<strong>Policy</strong> based on the UK childhood<br />
immunisation programme to protect children<br />
against vaccine preventable diseases.<br />
Roslyn Connelly<br />
The Trust is committed to creating an environment that promotes equality <strong>and</strong> embraces<br />
diversity, both within our workforce <strong>and</strong> in service delivery. This document should be<br />
implemented with due regard to this commitment<br />
This document seeks to uphold the duties <strong>and</strong> principles contained within the Human Rights<br />
Act. All <strong>St</strong>aff within the <strong>PCT</strong> should be aware of its implications<br />
This policy is due for review by November 2013. After this date, this policy <strong>and</strong> associated<br />
process documents may become invalid. All users should ensure that they are consulting the<br />
current version of this document.
Key individuals involved in developing the document (Internal <strong>St</strong>aff Only)<br />
Name(s)<br />
Sue Large<br />
Roslyn Connelly<br />
Lynne Shaw<br />
Lin Charlesworth<br />
Designation<br />
Lead Nurse Child Health Service Development<br />
Assistant Director Children’s Services<br />
<strong>St</strong>.<strong>Helens</strong><br />
<strong>Immunisation</strong> trainer<br />
<strong>Immunisation</strong> trainer<br />
Distributed to the following for approvals <strong>and</strong> comments<br />
Committee(s)<br />
Members of the <strong>Policy</strong> Sub Committee (PSC)<br />
Members of the Clinical Policies Guidelines<br />
Group (CPG)<br />
Members of the <strong>Immunisation</strong> Committee<br />
Individual(s)<br />
Julie Banat<br />
Karen Worthington<br />
Lesley Brownlow<br />
Pat Byrne<br />
Michelle Bradshaw<br />
Health visitors, school nurses, community<br />
nurses<br />
Gill Clare<br />
Dot Keates<br />
<strong>St</strong>ephen McDowell<br />
Michelle Falconer<br />
<strong>Halton</strong> staff<br />
Fiona Johnson<br />
Jeannette Owens<br />
Carmel Farmer<br />
Linda Spooner<br />
Designation<br />
Service Manager Health Visiting <strong>St</strong>.<strong>Helens</strong><br />
Service Manager Health Visiting <strong>Halton</strong><br />
Service Manager School Nursing <strong>St</strong>.<strong>Helens</strong><br />
Service Manager School Nursing <strong>Halton</strong><br />
Assistant Director Children’s Services <strong>Halton</strong><br />
Skill mix teams<br />
Senior Pharmacist (Medicines Governance)<br />
Professional Development Lead<br />
CPR/First Aid Training Manager<br />
<strong>Immunisation</strong> Coordinator<br />
Practice Nurses<br />
Director of Public Health<br />
Infection Control Nurse Specialist<br />
Lead Nurse Safeguarding Children<br />
Professional Development Manager<br />
Page 2 of 46
Revision History <strong>and</strong> Version Control<br />
Revision<br />
Date<br />
Reason for Change Version No. By Who Version No.<br />
25.05.10 Anaphylaxis updated S.Large 0.1<br />
27.05.10 Document review 0.1 S.Large 0.2<br />
01.06.10 Document review 0.2 S.Large 0.3<br />
18.06.10 Document review 0.3 S.Large 0.4<br />
22.06.10 Document review 0.4 S.Large 0.5<br />
01.07.10 Document review 0.5 S.Large 0.6<br />
06.07.10 Document review 0.6 S.Large 0.7<br />
07.07.10 Document review 0.7 S.Large 0.8<br />
20.07.10 Review at V&I Group 0.8 S.Large 0.9<br />
04.08.10 Document review 0.9 S.Large 0.10<br />
12.08.10 Document review 0.10 S.Large 0.11<br />
05.10.10 Review from CGG 0.11 S.Large 0.12<br />
22.11.10 Final Version published 0.12 1.0<br />
Page 3 of 46
Table of Contents<br />
Introduction ..................................................................................................................................6<br />
Purpose........................................................................................................................................6<br />
Objectives .................................................................................................................................6<br />
Outcome....................................................................................................................................6<br />
Scope...........................................................................................................................................7<br />
<strong>Childhood</strong> <strong>Immunisation</strong>...............................................................................................................7<br />
Access to <strong>Immunisation</strong> ...............................................................................................................7<br />
Patient Group Directions..............................................................................................................8<br />
Training Requirements.................................................................................................................9<br />
Consent......................................................................................................................................10<br />
Parents Who Decline <strong>Immunisation</strong> ...........................................................................................11<br />
Therapeutic Holding of Children.................................................................................................11<br />
Risk Assessment of Premises....................................................................................................11<br />
Cold Chain .................................................................................................................................12<br />
Infection Control.........................................................................................................................12<br />
Administration of Vaccines.........................................................................................................12<br />
Anaphylaxis................................................................................................................................12<br />
<strong>Childhood</strong> <strong>Immunisation</strong> Procedural Guidelines ........................................................................13<br />
Equipment Required ..................................................................................................................13<br />
Referral to Secondary Care .......................................................................................................14<br />
Record Keeping .........................................................................................................................14<br />
Patient Safety.............................................................................................................................15<br />
Management of Adverse Effects ................................................................................................15<br />
Adverse Incident Reporting........................................................................................................15<br />
Domiciliary <strong>Immunisation</strong> ...........................................................................................................16<br />
Duties <strong>and</strong> Responsibilities ........................................................................................................17<br />
Duties within the Organisation.................................................................................................17<br />
Document <strong>St</strong>orage <strong>and</strong> Filing.....................................................................................................18<br />
References.................................................................................................................................19<br />
Appendix 1 .................................................................................................................................21<br />
Glossary of Terms ...................................................................................................................21<br />
Appendix 2 .................................................................................................................................22<br />
Appendix 3 .................................................................................................................................24<br />
Page 4 of 46
Process Map for <strong>Childhood</strong> <strong>Immunisation</strong>s Preschool ............................................................24<br />
Appendix 4 .................................................................................................................................25<br />
Looked after Children ..............................................................................................................25<br />
Appendix 5 .................................................................................................................................26<br />
Appendix 6a ...............................................................................................................................27<br />
Appendix 6b ...............................................................................................................................28<br />
Risk Assessment of an Environment for <strong>Immunisation</strong> Sessions............................................28<br />
Appendix 7 .................................................................................................................................29<br />
<strong>Childhood</strong> <strong>Immunisation</strong> Procedural Guidelines......................................................................29<br />
Appendix 8 .................................................................................................................................32<br />
Appendix 9 .................................................................................................................................33<br />
Appendix 10 ...............................................................................................................................36<br />
<strong>Immunisation</strong> data is recorded according to local requirements..............................................41<br />
Appendix 11 ...............................................................................................................................43<br />
Appendix 12 ...............................................................................................................................44<br />
Appendix 13 ...............................................................................................................................45<br />
Equality Impact Assessment Tool ...........................................................................................45<br />
Appendix 14 ...............................................................................................................................46<br />
Dissemination <strong>and</strong> Training Plan.............................................................................................46<br />
Page 5 of 46
INTRODUCTION<br />
<strong>Immunisation</strong> is the most effective method of preventing disease <strong>and</strong> maintaining the public<br />
health of the population (DH 2006).<br />
The World Health Organisation recommends that the national target for uptake of antigens in<br />
the <strong>Childhood</strong> <strong>Immunisation</strong> programme is 95% by age 24 months for completed courses of<br />
each of the primary programmes. NHS <strong>Halton</strong> <strong>and</strong> <strong>St</strong>.<strong>Helens</strong> recorded a 96% uptake of<br />
DTaP/IPV/Hib <strong>and</strong> 90% uptake of MMR during the year 2008-09. (NHS Imms <strong>St</strong>atistics,<br />
Engl<strong>and</strong> 2008-09)<br />
The Department of Health’s (DH) immunisation programme is described in ‘<strong>Immunisation</strong><br />
Against Infectious Disease’ (2006), also known as ‘The Green Book’. All immunisations must be<br />
in line with the Green Book (2006) <strong>and</strong> any subsequent recommendations from the Department<br />
of Health (DH), Joint Committee for Vaccination <strong>and</strong> <strong>Immunisation</strong> (JCVI) <strong>and</strong> other relevant<br />
bodies, e.g. NICE. The ‘Green Book’ should be accessed on line to ensure updated<br />
recommendations <strong>and</strong> guidelines are followed<br />
This policy is to be read in conjunction with relevant <strong>PCT</strong> policies, ‘Maintenance of the Cold<br />
Chain <strong>Policy</strong> 2008’, ‘Resuscitation <strong>Policy</strong> 2010’, ‘Health Record <strong>Policy</strong> 2010’, ‘Consent to<br />
treatment <strong>Policy</strong> 2009’, ‘Medicine <strong>and</strong> controlled drugs policy 2010’ <strong>and</strong> associated st<strong>and</strong>ard<br />
operating procedures <strong>and</strong> service specifications.<br />
PURPOSE<br />
This policy provides a framework to support professional practice to safely achieve the<br />
maximum uptake <strong>and</strong> delivery of the <strong>Childhood</strong> <strong>Immunisation</strong> Programme<br />
The aim of this policy is to ensure that all practitioners who administer childhood immunisations<br />
practice in accordance with national <strong>and</strong> local policies <strong>and</strong> guidance for evidence based<br />
practice, thus minimising the risk of errors.<br />
Objectives<br />
To provide a guide to good practice in the delivery of the <strong>Childhood</strong> <strong>Immunisation</strong><br />
Programme<br />
To develop a clinical governance framework to support service delivery<br />
To identify roles <strong>and</strong> responsibilities of all staff who deliver the <strong>Childhood</strong><br />
<strong>Immunisation</strong> Programme<br />
Outcome<br />
A safe <strong>and</strong> effective delivery of the <strong>Childhood</strong> <strong>Immunisation</strong> Programme.<br />
Improved vaccine uptake rates for children in the Trust<br />
Reduction in vaccine preventable diseases<br />
Page 6 of 46
SCOPE<br />
The scope of this policy applies to all staff members who are involved in the provision of<br />
immunisation advice or the preparation, administration <strong>and</strong> documentation of immunisations<br />
given to children aged 0-18 years. This will include all practitioners <strong>and</strong> staff involved in the<br />
delivery of the <strong>Childhood</strong> <strong>Immunisation</strong> Programme.This procedure excludes the administration<br />
of travel vaccines<br />
Healthcare professionals involved in any aspect of immunisation are accountable for their own<br />
actions <strong>and</strong> as such, have a responsibility to acquire <strong>and</strong> maintain their necessary skills <strong>and</strong><br />
competencies in order to demonstrate their capability to offer safe <strong>and</strong> effective care. (NMC<br />
2008)<br />
CHILDHOOD IMMUNISATION<br />
<strong>Childhood</strong> immunisation is the schedule of vaccines offered to every child from the ages of 8<br />
weeks to 18 years (see appendix 2) This policy includes all childhood immunisations that are<br />
prescribed individually by a GP, or hospital consultant or included as part of a Patient Group<br />
Direction (PGD).<br />
The process for pre school childhood immunisation is detailed in appendix 3a <strong>and</strong> school age<br />
children process in appendix 3b<br />
Any practitioner who has concerns or queries regarding immunisation should refer primarily to<br />
the guidance in the ‘Green book’ or updated DH guidance on immunisation. Unanswered<br />
enquiries should be directed to the <strong>Immunisation</strong> Coordinator.<br />
<strong>Immunisation</strong> programmes should be based on a multi-professional team approach, where each<br />
member’s skills <strong>and</strong> knowledge contribute to improving the public health of the local population.<br />
The <strong>Immunisation</strong> Programme should be delivered flexibly to enable new vaccines to be<br />
included.<br />
Only practitioners with additional training in Vaccination <strong>and</strong> <strong>Immunisation</strong> approved by the<br />
Primary Care Trust (<strong>PCT</strong>) may administer vaccines. All child health staff should endeavour<br />
when appropriate, to either immunise children who have not completed the programme or<br />
arrange for them to attend an immunisation session.<br />
ACCESS TO IMMUNISATION<br />
The <strong>PCT</strong> is responsible to ensure that all children have access to the immunisation programme,<br />
namely:<br />
<br />
<br />
<br />
All children resident within <strong>Halton</strong> or <strong>St</strong>.<strong>Helens</strong> boroughs<br />
All children registered with a GP whose practice forms part of the <strong>PCT</strong><br />
Children attending local authority maintained schools in <strong>Halton</strong> <strong>and</strong> <strong>St</strong>.<strong>Helens</strong>,<br />
independent schools <strong>and</strong> all school age children resident elsewhere but attending<br />
schools in the two boroughs.<br />
Page 7 of 46
‘At risk’ groups determined by the Health Protection Agency (HPA) <strong>and</strong> national<br />
campaigns.<br />
Some children are more at risk of low take up of immunisation <strong>and</strong> staff in Health Visiting <strong>and</strong><br />
School Nursing teams should ensure that these groups have equitable access to<br />
immunisations. These children include:<br />
Children in care<br />
Young people who missed previous immunisations<br />
Children with physical or learning difficulties<br />
Children of lone parents<br />
Children not registered with a general practitioner<br />
Children in larger families<br />
Minority ethnic groups <strong>and</strong> non English speaking families<br />
Vulnerable children e.g. travellers, asylum seekers or homeless families<br />
Children in hospital or have a chronic illness<br />
PATIENT GROUP DIRECTIONS<br />
(Patient Group Direction <strong>Policy</strong><br />
<strong>Halton</strong> <strong>and</strong> <strong>St</strong>.<strong>Helens</strong> NHS 2010)<br />
The Trust’s Patient Group Direction <strong>Policy</strong> 2010 <strong>and</strong> Medicine <strong>and</strong> Controlled Drugs policy 2010<br />
contains information <strong>and</strong> guidance on Patient Group Directions.<br />
For nurse led sessions, vaccines are administered under Patient Group Directions (PGDs),<br />
which are drawn together locally by the <strong>PCT</strong> PGD Development Group. The PGD is then<br />
approved by The Trust.<br />
The Service Lead or designated Authorising Manager is responsible for ensuring that fully<br />
competent, qualified <strong>and</strong> trained professionals operate within the PGDs <strong>and</strong> have their own<br />
current authorised PGDs. They must maintain a list of the practitioners they have authorised to<br />
use specific PGDs <strong>and</strong> a copy forwarded <strong>and</strong> retained by the Clinical Governance Department<br />
All immunisers must have read <strong>and</strong> signed their personal PGD <strong>and</strong> these documents are<br />
retained safely <strong>and</strong> be easily accessible to the individual <strong>and</strong> relevant others.<br />
Before using a PGD it is the individual nurse’s responsibility to ensure that they are competent<br />
to deal with each patient under its terms <strong>and</strong> comply fully with the details in the PGD. See The<br />
Trust’s Patient Group Direction <strong>Policy</strong> 2010 <strong>and</strong> Medicine <strong>and</strong> Controlled Drugs <strong>Policy</strong> 2010.<br />
.<br />
The practitioner must ensure:<br />
They have read <strong>and</strong> understood the PGD<br />
They have signed the PGD<br />
The authorising manager has signed the PGD<br />
Page 8 of 46
Has attended an immunisation update within the last twelve months<br />
The PGD is stored safely <strong>and</strong> readily accessible to both the practitioner <strong>and</strong><br />
relevant others<br />
The PGD is available for reference before the administration of vaccines to the<br />
individual or groups at immunisation sessions<br />
Nurses may administer vaccines with a written instruction signed <strong>and</strong> dated by a doctor, under<br />
Patient Specific Direction.<br />
TRAINING REQUIREMENTS<br />
Only practitioners with additional training in Vaccination <strong>and</strong> <strong>Immunisation</strong> approved by the <strong>PCT</strong><br />
may administer vaccines.<br />
All registered nurses are accountable for their practice <strong>and</strong> must ensure that they undertake the<br />
appropriate training to perform the task in a professional <strong>and</strong> competent manner. Competency<br />
must be maintained in accordance with current Nursing <strong>and</strong> Midwifery Council (NMC)<br />
guidelines.<br />
<br />
<br />
<br />
<br />
Initial immunisation training programme approved by the <strong>PCT</strong><br />
Medicines management training, including Patient Group Directions<br />
Attend yearly immunisation updates.<br />
Undertake annual Basic Life Support <strong>and</strong> Anaphylaxis training<br />
All health professionals should follow the guidelines set out in the The Green Book (D.O.H.<br />
<strong>Immunisation</strong> against Infectious Disease 2006) with updated chapters available at<br />
www.dh.gov.uk All who administer or advise about immunisation should be well informed <strong>and</strong><br />
up to date about vaccines, their benefits, possible reactions, <strong>and</strong> rare contraindications, <strong>and</strong><br />
also informed about the diseases against which they offer protection <strong>and</strong> the risks of not<br />
immunising.<br />
All who administer, or give advice about immunisations must be proficient <strong>and</strong> competent in the<br />
following areas of core knowledge (HPA 2005), or know where to obtain the relevant<br />
information.<br />
Aims of immunisation: national policy <strong>and</strong> schedules<br />
Immune system <strong>and</strong> how vaccines work<br />
Vaccine preventable disease<br />
Different types of vaccine used <strong>and</strong> their composition<br />
Current issues <strong>and</strong> controversies regarding immunisation<br />
Communication with patients <strong>and</strong>/or parents<br />
Legal aspects of immunisation<br />
<strong>St</strong>orage <strong>and</strong> h<strong>and</strong>ling of vaccines<br />
Correct administration of vaccines<br />
Anaphylaxis <strong>and</strong> other adverse events<br />
Documentation, record keeping <strong>and</strong> reporting<br />
<strong>St</strong>rategies for improving immunisation rates<br />
Page 9 of 46
CONSENT<br />
All staff should practice in accordance with the current <strong>PCT</strong> Consent <strong>Policy</strong>, the Mental Capacity<br />
Act <strong>and</strong> the Mental Capacity Act code of Practice. Consent must be obtained before each <strong>and</strong><br />
every immunisation.<br />
The practitioner who is to administer the vaccine should obtain valid consent or authorisation<br />
from the individual or parent/guardian. The explanation of the options available to the individual,<br />
guardian or relevant others should be given. This involves facilitating an underst<strong>and</strong>ing of the<br />
advantages, disadvantages, benefits <strong>and</strong> potential complications of the procedure <strong>and</strong><br />
vaccines. Practitioners gaining consent must adhere to the consent for immunisation guidelines<br />
in the Consent to Examination or Treatment <strong>Policy</strong>.<br />
Initial written intent for the child to be invited to be immunised must be sought <strong>and</strong> is primarily<br />
gained by the health visitor at the visit shortly after the child’s birth. The signed intent form must<br />
be returned to the correct Child Health Department. The details will be inputted onto the<br />
computer, which in turn will generate the appropriate appointments <strong>and</strong> clinic lists.<br />
In cases where young children are not competent to either give or withhold consent, such<br />
consent must be given by a person with parental responsibility. If a child is in the care of the<br />
Local Authority, see appendix 4 for arrangements within the two boroughs.<br />
Where immunisations are routinely offered in the school setting, older children are seldom<br />
accompanied by parent/s or carer/s for immunisations <strong>and</strong> teachers do not have parental<br />
powers<br />
Young people aged 16 or 17 are presumed, in law, to be able to consent to their own medical<br />
treatment. Younger children who underst<strong>and</strong> fully what is involved in the proposed procedure,<br />
referred to as ‘meeting the Fraser Guidelines’ or ‘Gillick’ competent, can also give consent<br />
although ideally their parents will be involved <strong>and</strong> the immuniser should attempt to make contact<br />
with the parents to gain a verbal consent. (DH 2006). Practitioners should use the checklist to<br />
assess competency (Fraser competency checklist appendix 5)<br />
If the health professional giving the immunisation feels a child does not meet the Fraser<br />
’competence’, then the consent of someone with parental responsibility must be sought. The<br />
immuniser should document any consent or refusal obtained, on the consent form.<br />
Should a child wish, or present, for immunisation, <strong>and</strong> there is no written or verbal consent, but<br />
the child meets the ‘Fraser Guidelines’ (appendix 5), then the immunisation can be given<br />
(Fraser competence, Consent to Examination or Treatment <strong>Policy</strong> 2009) The immuniser must<br />
ensure that the young person signs the consent form. An attempt should be made to contact the<br />
person with parental responsibility to obtain verbal consent.<br />
School Nurses may obtain verbal consent where possible from the parents/carers <strong>and</strong> record<br />
this in the child’s case notes. Immunisers who are immunising in a school setting should also<br />
follow the clinical guidelines in appendix 10.<br />
An interpreter or other suitable person should be available (where required) to enable the<br />
patient, client or parent to make an informed consent.<br />
Page 10 of 46
PARENTS WHO DECLINE IMMUNISATION<br />
If parents decline any of the immunisations due, explore the reasons why <strong>and</strong> offer further<br />
information <strong>and</strong> advice on risks <strong>and</strong> benefits of protecting against disease. Whilst,<br />
parents/guardians should not be unduly pressured, they need to be given sufficient information<br />
to make an informed decision. When two parents with parental responsibility, do not agree on<br />
vaccines to be given, advice should be sought from the <strong>Immunisation</strong> Coordinator; in some<br />
cases legal advice might be required.<br />
THERAPEUTIC HOLDING OF CHILDREN<br />
This predominately applies to three to four year old children. Therapeutic holding is, by<br />
definition, applied without a child’s consent however; safe holding by the parent reduces the risk<br />
of needle stick injury to the child. Therapeutic holding of children means immobilisation by the<br />
use of limited force. Parents/Carers are guided by nursing staff on how to hold the child in a<br />
safe position. The child should sit on the parent/carer’s lap who will immobilise the relevant limb<br />
of the child in readiness for the immunisation. Nurses should not hold the child routinely, unless<br />
requested by the parent/carer. Clinical judgment on what advice to give parents will always be<br />
on a case by case basis, the child’s welfare <strong>and</strong> safety will always be paramount. (RCN<br />
guidance 2010)<br />
RISK ASSESSMENT OF PREMISES<br />
A basic risk assessment should be undertaken in premises where immunisations are<br />
administered (appendix 6a) <strong>and</strong> updated annually or reviewed when there is a change in<br />
circumstances.<br />
It is essential that the criteria is met <strong>and</strong> where premises are found to be unsuitable or<br />
inadequate, the risk assessment is discussed with the service lead or line manager.<br />
When other services are using the same premises to immunise, only one risk assessment is<br />
required <strong>and</strong> shared with the relevant staff. The assessor will liaise with other teams <strong>and</strong> a copy<br />
of the risk assessment is stored at the premises by the clerical officer or GP practice manager.<br />
Assessments completed on external premises will be stored at the nearest clinic <strong>and</strong> copies<br />
sent to the service manager.<br />
A more detailed risk assessment is undertaken in the school setting (appendix 6b). It is<br />
essential to meet this criteria in order to deliver a session. Advice of the line manager is to be<br />
sought where environments do not meet the criteria.<br />
<strong>Immunisation</strong> should only take place in premises or homes where emergency assistance can be<br />
summoned immediately. The practitioner should ensure that a telephone is available <strong>and</strong> there<br />
is a second responsible adult who is able to summon emergency assistance if required<br />
<strong>St</strong>aff must be able to adhere to <strong>PCT</strong> Infection Control Policies <strong>and</strong> the <strong>PCT</strong> Cold Chain <strong>Policy</strong><br />
whilst at the premises<br />
Page 11 of 46
COLD CHAIN<br />
<strong>St</strong><strong>and</strong>ards around vaccine storage, transportation <strong>and</strong> the maintenance of the cold chain are in<br />
accordance with the Trusts Medicine <strong>Policy</strong> <strong>and</strong> Cold Chain <strong>Policy</strong>.<br />
INFECTION CONTROL<br />
Equipment required in maintaining st<strong>and</strong>ard precautions in infection control must be available at<br />
each vaccination session:<br />
<br />
<br />
<br />
<br />
<br />
Disposable roll<br />
Gloves for spillages or bleeds-<br />
Infection control procedures should be followed as per policy.<br />
Clinical waste bags<br />
Sharps disposal-<br />
Sharps to be disposed of into a sharps box, directly after use<br />
Sharps boxes replaced when two thirds full<br />
Access to h<strong>and</strong> decontamination facilities-<br />
Alcohol gel should be available <strong>and</strong> used after every patient. H<strong>and</strong>s will also need<br />
to be washed with running water after 3 to 4 uses of gel to prevent a build up of<br />
residue.<br />
In the event of any needle stick injury, infection control procedures should be followed as per<br />
policy.<br />
ADMINISTRATION OF VACCINES<br />
Health care professionals should follow the guidelines set out in ‘The Green Book’ (DH 2006).<br />
Health professionals should endeavour to ensure that each child under their care is fully<br />
immunised, unless there is a true contraindication.<br />
Vaccines should either have been dispensed to the patient on prescription, or administered from<br />
stock held at the practice premises or health centre. The correct authorisation to administer<br />
must be in place e.g. PGD or Patient Specific Direction.<br />
Immunisers must underst<strong>and</strong> <strong>and</strong> practice in accordance with the <strong>PCT</strong> Medicine <strong>and</strong><br />
Controlled Drugs <strong>Policy</strong> <strong>and</strong> the NMC <strong>St</strong><strong>and</strong>ards for Medicine Management 2010.<br />
Registered healthcare professionals should ensure the drug Adrenaline (Epinephrine) 1:1000<br />
(1mg/1ml) is available for use in the treatment of anaphylaxis. (See the current Trust<br />
Resuscitation <strong>Policy</strong> <strong>and</strong> the <strong>PCT</strong> PGD for Adrenaline)<br />
ANAPHYLAXIS<br />
It is the policy of the Trust that all professional staff who administers medications <strong>and</strong>/or<br />
vaccinations is able to recognise <strong>and</strong> treat anaphylaxis. Such members of staff are to receive<br />
Page 12 of 46
annual training in the recognition <strong>and</strong> management of anaphylaxis; this is in addition to<br />
resuscitation training. (Resuscitation <strong>Policy</strong> 2010).<br />
The Resuscitation <strong>Policy</strong> states:<br />
Adrenaline Injection BP 1 in 1000 solution (1mg/ml) 2 x 1ml ampoules.<br />
The PGD for the administration of adrenaline (epinephrine) 1:1000 (1mg/mL) states:<br />
Frequency of administration<br />
The dose may be repeated, if necessary, if there is no improvement in the patient’s<br />
condition after a 5-minute interval.<br />
Monitor individual patient’s response: blood pressure, pulse <strong>and</strong> respiratory function.<br />
Further doses can be given at about 5-minute intervals according to the patient’s<br />
response. This is in accordance with advice given by the Resuscitation Council,<br />
‘Emergency treatment of anaphylactic reactions. Guidelines for healthcare providers’<br />
(2008)<br />
Resuscitation Council (UK)<br />
Intramuscular Adrenaline dosage<br />
IM doses of 1:1000 adrenaline (repeat after 5 min if no better)<br />
• Adult 500 micrograms IM (0.5 mL)<br />
• Child more than 12 years: 500 micrograms IM (0.5 mL)<br />
or 300 micrograms (0.3mL) if child is small or prepubertal<br />
• Child 6 -12 years: 300 micrograms IM (0.3 mL)<br />
• Child less than 6 years: 150 micrograms IM (0.15 mL)<br />
Equipment required <strong>and</strong> appropriate dosage is listed at appendix 8<br />
CHILDHOOD IMMUNISATION PROCEDURAL GUIDELINES<br />
These guidelines apply to all practitioners whose duties involve the prescribing, administration<br />
or h<strong>and</strong>ling of vaccines.<br />
The basic procedural guidelines are to be followed when administering any childhood vaccine.<br />
(appendix 7). Practitioners will need to also refer to more detailed guidelines that are available<br />
for specific situations <strong>and</strong> areas e.g. School Nursing <strong>Immunisation</strong>s in Schools (appendix 10),<br />
<strong>and</strong> Guidelines for Intramuscular <strong>and</strong> Subcutaneous Injections 2010.<br />
EQUIPMENT REQUIRED<br />
Vaccine supply including the manufacturer’s information leaflet<br />
Patient Documentation, as required by your employer<br />
Copy of PGD, if relevant<br />
H<strong>and</strong> gel<br />
Page 13 of 46
Blue roll<br />
Kidney dish or appropriate receiver<br />
Non sterile gauze squares<br />
Micro pore tape or plasters if required<br />
Sharps disposal bin <strong>and</strong> transportation carrier<br />
Selection of syringes – 1ml or 2ml<br />
Selection of needles-<br />
-Green 21 gauge – 38 mm long - use for drawing up of vaccine<br />
only<br />
-Blue 23 gauge – 25 mm long – use to administer vaccines suitable<br />
for all ages<br />
-A 25G 16mm length needle (orange) is suitable for IM injection in pre- term or very<br />
small infants ONLY.<br />
16mm long, only to be used on pre-term or very small infants<br />
Anaphylaxis pack (appendix 8)<br />
REFERRAL TO SECONDARY CARE<br />
In incidences, where there has been a previous adverse reaction to a vaccine or there is a<br />
contraindication to the vaccine (The Green Book), the professional may refer to secondary care<br />
when they feel the child cannot be safely immunised in a community clinic. The referral pathway<br />
is to be followed (appendix 9).<br />
RECORD KEEPING<br />
Accurate records of vaccines given or reason for not giving are important for patient safety,<br />
monitoring immunisation uptake <strong>and</strong> facilitating recall of recipients of vaccines, if required.<br />
The following information must be recorded:<br />
See checklist for Health Visiting services appendix 11<br />
Assessment process indicating information about the child’s fitness for immunisation <strong>and</strong><br />
verbal informed parental consent given.<br />
Name of patient, address, date of birth <strong>and</strong> GP<br />
Vaccine name, product name, batch number <strong>and</strong> expiry date.<br />
Dose administered<br />
Site(s) used – including clear description of which injection was administered in each site.<br />
Date immunisation given.<br />
Details of any ADRs <strong>and</strong> action taken<br />
Advice given <strong>and</strong> action to be taken if vaccine deferred or declined.<br />
Name, designation <strong>and</strong> signature of immuniser.<br />
Page 14 of 46
If following assessment <strong>and</strong> discussion the vaccine is not given, the reason for this must be<br />
recorded. This should also include any relevant follow-up advice provided.<br />
This information is recorded in the most appropriate notes at the time of administration. These<br />
include:<br />
Personal Child Health Record (PCHR) for children<br />
Child clinical records (Contact sheets are completed <strong>and</strong> one copy sent to the named<br />
health professional <strong>and</strong> one copy given to the parent)<br />
GP computerised record system<br />
School nurse sessional documentation (see procedures in appendix 10)<br />
I.T. systems<br />
Scheduled data collection form <strong>and</strong> unscheduled data forms, as required, are completed <strong>and</strong><br />
returned to the Child Health Information System<br />
PATIENT SAFETY<br />
The safety of patients involved in the immunisation programme is paramount<br />
All immunisers must:<br />
Ensure the safety <strong>and</strong> efficacy of vaccines in accordance with the <strong>PCT</strong>’s Medicine <strong>and</strong><br />
Controlled Drugs <strong>Policy</strong> 2010 <strong>and</strong> Maintaining the Cold Chain <strong>Policy</strong> 2008<br />
Work within the Nursing <strong>and</strong> Midwifery Council (NMC) The Code <strong>and</strong> The Guidelines for<br />
the Administration of Medicines<br />
Have access to emergency anaphylaxis <strong>and</strong> resuscitation equipment <strong>and</strong> drugs when<br />
undertaking <strong>Immunisation</strong> sessions<br />
Have available <strong>and</strong> adhere to the guidelines within the Department of Health<br />
‘<strong>Immunisation</strong> Against Infectious Disease’ (the Green Book) 2006<br />
Report incidents in accordance with the <strong>PCT</strong>’s Accident <strong>and</strong> Incident Reporting<br />
Procedures (Health <strong>and</strong> Safety <strong>Policy</strong> 2009)<br />
MANAGEMENT OF ADVERSE EFFECTS<br />
If an error is made, the immuniser must take any action to prevent any potential harm to the<br />
patient <strong>and</strong> report as soon as possible to the prescriber, line manager or employer (according to<br />
local policy) <strong>and</strong> document actions. (NMC <strong>St</strong><strong>and</strong>ard 24 2010)<br />
ADVERSE INCIDENT REPORTING<br />
In the event of a suspected or actual adverse incident the healthcare professional should:<br />
<br />
<br />
<br />
<br />
Inform <strong>and</strong> seek guidance <strong>and</strong> advice from the Service Lead<br />
Inform <strong>and</strong> seek clinical advice from the <strong>Immunisation</strong> Trainer or <strong>Immunisation</strong><br />
Coordinator<br />
Inform the patient, client or parent of the error <strong>and</strong> action to be taken<br />
Report all errors or suspected errors in accordance with Trust Accident <strong>and</strong> Incident<br />
Reporting procedures (Health <strong>and</strong> Safety <strong>Policy</strong> 2009)<br />
Page 15 of 46
Clearly document action <strong>and</strong> outcomes in the recipient’s clinical records.<br />
Complete an incident form [IR1] <strong>and</strong> send to the Governance Department the same day.<br />
Report to the MHRA (Medicines <strong>and</strong> Healthcare Products Regulatory Agency), via the<br />
Yellow Card Scheme, any unwanted or harmful reactions following the administration of a<br />
vaccine ( The Green Book Chapter 9)<br />
use the NHS no. as an identifier<br />
If a patient experiences an adverse drug reaction to a medication, immediate action must be<br />
taken to remedy harm caused by the reaction. Actions are recorded in the patient’s notes, notify<br />
the prescriber (if you did not prescribe the drug) <strong>and</strong> notify via the Yellow Card Scheme<br />
immediately (<strong>St</strong><strong>and</strong>ard 25 NMC 2010)<br />
All incidents <strong>and</strong>/or breeches in patient safety must be reported to the Governance Department<br />
using the incident form (IR1).<br />
DOMICILIARY IMMUNISATION<br />
Children <strong>and</strong> families are routinely offered appointments to attend immunisation sessions,<br />
however in exceptional circumstances, home immunisations may be offered.<br />
Criteria:<br />
Failure to attend two appointments<br />
Mitigating domestic circumstances rendering parents unable to attend a session, e.g.<br />
multiple births, children with complex or additional needs.<br />
Looked after children <strong>and</strong> those on a child protection plan<br />
This criterion is not definitive <strong>and</strong> should only be used as a guide. Immunisers should use their<br />
own discretion <strong>and</strong> professional judgement.<br />
Source of referrals<br />
Health Visitors<br />
GP via health visiting team<br />
Children Centre staff<br />
Recommendations from LAC review or case conferences<br />
Parents (if fulfil criteria)<br />
Foster carers<br />
The following information must accompany each referral:<br />
Name of child<br />
Address <strong>and</strong> contact number<br />
Date of birth<br />
GP<br />
Named Health visitor<br />
Reason for referral<br />
Procedures<br />
The guidelines for domiciliary immunisation to be followed (appendix 12)<br />
Page 16 of 46
DUTIES AND RESPONSIBILITIES<br />
Duties within the Organisation<br />
Chief Executive<br />
The Chief Executive is responsible for ensuring compliance with the Policies <strong>and</strong> Guidelines,<br />
legislation, NHS guidance <strong>and</strong> for ensuring the policy is effective.<br />
Trust Board<br />
The Trust board is responsible for overall responsibility for ensuring the provision of effective<br />
clinical services within the organisation, <strong>and</strong> to ensure that the Trust complies with its statutory<br />
obligations.<br />
Assistant Directors Child Health<br />
Assistant Directors Child Health Services are responsible for ensuring effective implementation<br />
of this policy across their areas of responsibility. Assistant Directors will support <strong>and</strong> enable the<br />
operational service leads <strong>and</strong> clinical leads to fulfil their responsibilities <strong>and</strong> ensure the effective<br />
implementation of this policy within their speciality<br />
Assistant Directors will ensure that an effective audit is in place to identify that the policy is<br />
being adhered to.<br />
Child services lead<br />
Child service leads will ensure that:<br />
All relevant training needs are addressed to ensure there is full adherence to the policy.<br />
Practitioners have read <strong>and</strong> signed the appropriate <strong>Childhood</strong> <strong>Immunisation</strong> Patient<br />
Group Directions <strong>and</strong> send a copy to the Governance team<br />
Maintain a current list of practitioners using active PGDs.<br />
Any new employee completes the relevant training <strong>and</strong> is assessed as competent as<br />
soon as possible after joining the organisation.<br />
All <strong>Halton</strong> & <strong>St</strong> <strong>Helens</strong> <strong>St</strong>aff<br />
All <strong>St</strong>aff are responsible for adhering to <strong>and</strong> complying with the requirements of the policies,<br />
guidelines, protocols <strong>and</strong> <strong>St</strong><strong>and</strong>ard Operating Procedures (SOPs) contained within <strong>and</strong><br />
applicable to their area of operation, particularly those stated in this policy<br />
All relevant practitioners have a responsibility to ensure they are authorised <strong>and</strong> competent to<br />
administer <strong>and</strong>/or advise on childhood immunisations <strong>and</strong> they have a responsibility to ensure<br />
that they read, underst<strong>and</strong> <strong>and</strong> follow this policy at all times.<br />
Immunisers will have read <strong>and</strong> signed the appropriate Patient Group Directions <strong>and</strong> have<br />
access to an authorised up to date copy.<br />
Page 17 of 46
Temporary <strong>and</strong> Agency <strong>St</strong>aff, Contractors <strong>and</strong> Subcontractors<br />
All <strong>St</strong>aff are responsible for adhering to <strong>and</strong> complying with the requirements of the policies,<br />
guidelines, protocols <strong>and</strong> <strong>St</strong><strong>and</strong>ard Operating Procedures (SOPs) contained within <strong>and</strong><br />
applicable to their area of operation.<br />
DOCUMENT STORAGE AND FILING<br />
The approved <strong>and</strong> ratified corporate document will be uploaded to the document portal. Follow<br />
the link below to view the policy document <strong>and</strong> its related pages:<br />
http://sharepointcompliance/default.aspx<br />
Page 18 of 46
REFERENCES<br />
Reference<br />
<strong>Immunisation</strong> against Infectious Disease (The Green<br />
Book) Salisbury D (Ed) The <strong>St</strong>ationery Office, 2006<br />
NHS Imms <strong>St</strong>atistics,<br />
Engl<strong>and</strong> 2008-09<br />
Consent to Examination or Treatment <strong>Policy</strong><br />
<strong>Halton</strong> <strong>and</strong> <strong>St</strong>.<strong>Helens</strong> NHS 2009<br />
The Code<br />
NMC 2008<br />
<strong>St</strong><strong>and</strong>ards for Medicines Management<br />
NMC 2010<br />
Medicine <strong>and</strong> Controlled Drugs <strong>Policy</strong><br />
(Patient Group Directions)<br />
<strong>Halton</strong> <strong>and</strong> <strong>St</strong>.<strong>Helens</strong> NHS 2010<br />
Patient Group Direction <strong>Policy</strong><br />
<strong>Halton</strong> <strong>and</strong> <strong>St</strong>.<strong>Helens</strong> NHS 2010<br />
Maintaining the Cold Chain <strong>Policy</strong><br />
<strong>Halton</strong> <strong>and</strong> <strong>St</strong>.<strong>Helens</strong> NHS 2008<br />
Referral Pathway for <strong>Childhood</strong> <strong>Immunisation</strong>s in<br />
Secondary Care<br />
<strong>Halton</strong> <strong>and</strong> <strong>St</strong>.<strong>Helens</strong> NHS 2009<br />
Resuscitation <strong>Policy</strong><br />
<strong>Halton</strong> <strong>and</strong> <strong>St</strong>.<strong>Helens</strong> NHS 2010<br />
Infection Prevention <strong>and</strong> Control <strong>Policy</strong><br />
<strong>Halton</strong> <strong>and</strong> <strong>St</strong>.<strong>Helens</strong> NHS 2009<br />
UK Guidance on Best Practice in Vaccine<br />
Administration<br />
The Vaccine Administration Taskforce 2001<br />
Mental Capacity Act<br />
DH 2005<br />
Prevention <strong>and</strong> management of exposure to BBV<br />
including prevention of sharps injuries<br />
<strong>Halton</strong> <strong>and</strong> <strong>St</strong>.<strong>Helens</strong> NHS 2009<br />
Emergency treatment of anaphylactic reactions.<br />
Guidelines for healthcare providers<br />
Resuscitation Council, 2008<br />
Restrictive Physical Intervention <strong>and</strong> Therapeutic<br />
Holding For Children <strong>and</strong> Young People<br />
RCN 2010<br />
Health <strong>and</strong> Safety <strong>Policy</strong><br />
<strong>Halton</strong> <strong>and</strong> <strong>St</strong>.<strong>Helens</strong> NHS 2009<br />
Relevance<br />
(whole<br />
document or<br />
section,<br />
please state)<br />
Whole<br />
document<br />
Appendices<br />
Whole<br />
document<br />
Whole<br />
document<br />
Whole<br />
document<br />
Whole<br />
document<br />
Whole<br />
document<br />
Whole<br />
document<br />
Whole<br />
document<br />
Whole<br />
document<br />
Whole<br />
document<br />
Whole<br />
document<br />
Whole<br />
document<br />
Needle stick<br />
injury<br />
Whole<br />
document<br />
Whole<br />
document<br />
Accident <strong>and</strong><br />
Incident<br />
Evidence Grade<br />
National<br />
directives/guidelines<br />
National statistics<br />
Trust <strong>Policy</strong><br />
Professional<br />
Document<br />
Professional<br />
Document<br />
Trust <strong>Policy</strong><br />
Trust <strong>Policy</strong><br />
Trust <strong>Policy</strong><br />
Trust Guidelines<br />
Trust <strong>Policy</strong><br />
Trust <strong>Policy</strong><br />
Professional<br />
Document<br />
National legislation<br />
Trust policy<br />
National<br />
directives/guidelines<br />
Professional<br />
Document<br />
Trust <strong>Policy</strong><br />
Page 19 of 46
Guidelines for Intramuscular <strong>and</strong> Subcutaneous<br />
Injections<br />
<strong>Halton</strong> <strong>and</strong> <strong>St</strong>.<strong>Helens</strong> NHS 2010<br />
reporting<br />
procedures<br />
Whole<br />
document<br />
Trust guidelines<br />
Page 20 of 46
APPENDIX 1<br />
Glossary of Terms<br />
DTaP……………………………………………Diphtheria, Tetanus, Pertussis Vaccines<br />
DtaP<br />
(reconstituted with other vaccines)<br />
dTaP<br />
IPV………………………………………….. Inactivated Polio Vaccine<br />
PCV…………………………………………….Pneumococcal vaccine<br />
Hib…………………………………………….. Haemophilus influenzae Vaccine<br />
MMR……………………………………….......Measles, Mumps <strong>and</strong> Rubella vaccine<br />
MenC…………………………………………..Meningitis C vaccine<br />
BCG………………………………………….. .Bacillus Calmette-Guérin vaccine<br />
Td………………………………………………Tetanus <strong>and</strong> Diphtheria Vaccine<br />
Hep B…………………………………………..Hepatitis B Vaccine<br />
PGD…………………………………………....Patient Group Direction<br />
IM……………………………………………….Intra muscular<br />
LAC……………………………………………..Looked After Children (children in care)<br />
MHRA…………………………………………. Medicines <strong>and</strong> Healthcare Products Regulatory<br />
Agency<br />
ADR……………………………………………Adverse Drug Reaction<br />
Page 21 of 46
APPENDIX 2<br />
CHILDHOOD IMMUNISATION PROGRAMME<br />
When to<br />
immunise<br />
Diseases protected against<br />
Vaccine given<br />
Two months old<br />
Diphtheria, tetanus, pertussis<br />
(whooping cough), polio <strong>and</strong><br />
Haemophilus influenzae type b<br />
(Hib)<br />
Pneumococcal infection<br />
DTaP/IPV/Hib<br />
+ Pneumococcal conjugate<br />
vaccine, (PCV)<br />
Three months old<br />
Diphtheria, tetanus, pertussis, polio<br />
<strong>and</strong> Haemophilus influenzae type b<br />
(Hib)<br />
Meningitis C<br />
DTaP/IPV/Hib<br />
+ MenC<br />
Four months old<br />
Diphtheria, tetanus, pertussis, polio<br />
<strong>and</strong> Haemophilus influenzae type b<br />
(Hib)<br />
Meningitis C<br />
Pneumococcal infection<br />
DTaP/IPV/Hib<br />
+ MenC + PCV<br />
Around 12 months<br />
Haemophilus influenza type b (Hib)<br />
Meningitis C<br />
Hib/MenC<br />
Around 13 months<br />
old<br />
Measles, mumps <strong>and</strong> rubella<br />
Pneumococcal infection<br />
MMR<br />
+ PCV<br />
Three years <strong>and</strong><br />
four months or<br />
soon after<br />
Diphtheria, tetanus, pertussis <strong>and</strong><br />
polio<br />
Measles, mumps <strong>and</strong> rubella<br />
DTaP/IPV or dTaP/IPV<br />
+MMR<br />
Girls aged 12 to<br />
13 years<br />
13 to 18<br />
years old<br />
Cervical cancer caused by human<br />
papillomavirus<br />
types 16 <strong>and</strong> 18.<br />
Diphtheria, tetanus, polio<br />
HPV<br />
Td/IPV<br />
Page 22 of 46
When to immunise<br />
Diseases protected against<br />
Vaccine<br />
given<br />
At birth<br />
(to babies who have an<br />
increased risk of coming<br />
into contact with TB)<br />
Tuberculosis<br />
BCG<br />
At birth<br />
(to babies whose mothers<br />
are hepatitis B positive)<br />
Hepatitis B<br />
Hep B<br />
Page 23 of 46
APPENDIX 3<br />
Process Map for <strong>Childhood</strong> <strong>Immunisation</strong>s Preschool<br />
Labour<br />
ward<br />
notify<br />
CHCS of<br />
birth.<br />
CHCS<br />
send birth<br />
notificatio<br />
n to HV.<br />
Birth<br />
visit<br />
conducte<br />
d by<br />
Health<br />
Visitor<br />
between<br />
10 -14<br />
Intent form<br />
from Red<br />
Book<br />
completed<br />
Form<br />
returned to<br />
CHCS (Child<br />
Health<br />
Computer<br />
S t )<br />
Appointments sent by CHCS to child for<br />
scheduled immunisations (Pre-school)<br />
If Intent form is not<br />
returned to CHCS, the<br />
child does not receive any<br />
immunisation<br />
appointments. Within 3<br />
weeks of birth, CHCS<br />
chase up outst<strong>and</strong>ing<br />
intents with HV<br />
Child attends<br />
clinic <strong>and</strong><br />
receives<br />
scheduled<br />
immunisations<br />
Clinic clerk /<br />
immuniser<br />
returns<br />
scheduled<br />
sheet to CHCS,<br />
enters details<br />
in red book<br />
<strong>and</strong> onto GP<br />
computer<br />
system /<br />
yellow card<br />
Clinic details<br />
sent to CHCS<br />
via internal<br />
mail system<br />
within 24<br />
Child attends<br />
clinic<br />
opportunistically<br />
<strong>and</strong> receives<br />
unscheduled<br />
Clinic clerk or<br />
immuniser returns<br />
unscheduled sheet<br />
to CHCS, enters<br />
details in red book<br />
<strong>and</strong> onto GP<br />
computer system /<br />
yellow card<br />
Clinic details<br />
sent to CHCS via<br />
internal mail<br />
system within 24<br />
hours<br />
Child does not<br />
attend clinic<br />
but parent /<br />
carer calls to<br />
cancel<br />
Clerk /<br />
immuniser<br />
records non<br />
attendance (A)<br />
on scheduled<br />
h t<br />
Clinic details<br />
sent to CHCS via<br />
internal mail<br />
system within 24<br />
h<br />
New<br />
appointment<br />
sent to child<br />
Child does not<br />
attend<br />
Clerk / immuniser<br />
records non attendance<br />
(B) on scheduled sheet<br />
Clinic details<br />
sent to CHCS via<br />
internal mail<br />
system within 24<br />
hours<br />
New<br />
appointment sent<br />
to child (report<br />
sent to GP<br />
practices to list<br />
Child suspended if<br />
2 x DNAs<br />
Missed 2 appt list sent monthly<br />
by CHCS to HVs to initiate<br />
face to face contact with parent<br />
Page 24 of 46
APPENDIX 4<br />
Looked after Children<br />
Consent for looked after children seems complex as different councils use different people to<br />
sign for consent but the basis for consent is the same.<br />
For children who are accommodated by the local authority, the parent with parental<br />
responsibility is the only person who should sign. Where the parent is not contactable, the<br />
local authority will have a designated person to sign.<br />
<strong>St</strong> <strong>Helens</strong> - the Service Manager on the rota<br />
<strong>Halton</strong> - the parent will have completed a card which the carer should have with<br />
them.<br />
NB Arrangements with <strong>Halton</strong> LA are to be revised. If a carer is not in<br />
possession of a card, then contact Christine Taylor LA Service Manager<br />
who will arrange for consent to be given.<br />
For children who are on an interim or full care order, the local authority share parental<br />
responsibility <strong>and</strong> so can make decisions. Where the parent is not available or disagrees with<br />
care, the local authority will have a designated person to sign. In <strong>St</strong> <strong>Helens</strong>, this designated<br />
person will be the carer for day to day routine care <strong>and</strong> the Service Manager for planned<br />
invasive treatment or blood tests. For <strong>Halton</strong> the card system is used as above<br />
The named nurse for children in care should know the arrangements for those on his/her<br />
caseload. In the case of <strong>St</strong> <strong>Helens</strong> he/she will be sent a notification of consent by the LAC<br />
administrator (health). This is currently under review in <strong>Halton</strong><br />
Children who are on Residence Orders, Special Guardianship Orders or Adoption Orders are<br />
not in care. Their carers/adoptive parents can sign as parents sign.<br />
Where there are queries please contact the LAC health team 01744 671245/25 or<br />
S<strong>and</strong>ra.campbell2@hsthpct.nhs.uk<br />
Page 25 of 46
APPENDIX 5<br />
Assessing Fraser Competence Checklist<br />
This form is to be used by Health Professionals assessing young persons (ages 11-16) consent to<br />
treatment in the absence of a person with responsibility or refusal to consent.<br />
Name of Child/Young Person………………………………. Venue/ School ….……………………<br />
D.O.B………………………………………..<br />
Yes No<br />
Parent/Guardian has provided consent<br />
Parent/Guardian has refused consent to this treatment/procedure<br />
Has the young person refused to tell the Parent/Guardian or to allow<br />
the health professional to discuss it with their parents<br />
If answered “yes” to any of the above points, what actions have been taken <strong>and</strong> what evidence do<br />
you have to support this (Please write all relevant evidence in the space provided).<br />
……………………………………………………………………………………………………………………<br />
……………………………………………………………………………………………………………………<br />
……………………………………………………………………………………………<br />
The Young Person:<br />
<br />
Underst<strong>and</strong>s the benefits of proposed treatment<br />
<br />
Underst<strong>and</strong>s the risks of proposed treatment<br />
<br />
Underst<strong>and</strong>s what the treatment involves<br />
<br />
Underst<strong>and</strong>s the implications of not having the treatment<br />
<br />
Underst<strong>and</strong>s the alternatives available<br />
<br />
Underst<strong>and</strong>s what effects on their lives of having or not<br />
having the treatment will be<br />
<br />
Underst<strong>and</strong>s the language <strong>and</strong> clinical terms<br />
<br />
Underst<strong>and</strong>s the procedure to be carried out<br />
<br />
Demonstrates the ability to communicate a choice<br />
Name of Professional Completing this form………………………………………………….<br />
Signature……………….. ………………….<br />
Date………………………<br />
Designation………………………………….<br />
Page 26 of 46
APPENDIX 6A<br />
Date:<br />
BASIC CHECKLIST OF PREMISES USED FOR IMMUNISATION SESSIONS<br />
Assessor:<br />
Location<br />
Contact Person:<br />
(<strong>St</strong>aff member with responsibility for organising immunisation sessions)<br />
ESSENTIAL CRITERIA Not suitable Adequate Good<br />
Is there sufficient clinical work<br />
space for nurses to work<br />
effectively including management<br />
of anaphylaxis<br />
Are there h<strong>and</strong>-washing facilities<br />
available in the room or<br />
nearby<br />
Is the room lit well enough to<br />
perform the task<br />
Are the noise levels low enough to<br />
enable full concentration<br />
Are the table <strong>and</strong> chairs of<br />
suitable height <strong>and</strong> suitable for<br />
the purpose<br />
Is there a telephone access<br />
available<br />
Is there a suitable space for<br />
patients/clients to wait with<br />
minimal disturbance<br />
Is there a private area for<br />
patients/clients who feel ill<br />
Does the room meet <strong>PCT</strong> health<br />
<strong>and</strong> safety requirements<br />
Are the premises suitable to be used for immunisations sessions<br />
If any part of this checklist is classed as unsuitable, discuss with line manager Yes No<br />
Further action required Yes No<br />
Details<br />
Date for review:<br />
Page 27 of 46
APPENDIX 6B<br />
Risk Assessment of an Environment for <strong>Immunisation</strong> Sessions<br />
RISK ASSESSMENT FOR: ______________________________ (school, community setting)<br />
PRIOR TO IMMUNISATION SESSION ON: __________________________<br />
ROOM: ________________ School Reception direct phone number: __________________<br />
Number of pupils: ________<br />
Requirement Y/N Comments Checked on<br />
day of<br />
immunisation<br />
session<br />
1. Is there an identified waiting area, with an agreement that<br />
pupils arrive at the session at regular intervals<br />
2. Has it been agreed that a member of staff who is not<br />
actively involved with teaching a class can be available at<br />
the session to oversee the pupil’s behaviour<br />
3. Has an appropriate room been agreed <strong>and</strong> confirmed for<br />
the prearranged date/s (Please identify room above) This<br />
needs to be confirmed with the Head of Year or member of<br />
the Senior Management Team.<br />
4. Is the room well ventilated <strong>and</strong> of optimal temperature.<br />
5. Is the room of adequate size for the number of immunisers<br />
<strong>and</strong> pupils that will be attending for their immunisation<br />
6. Is there adequate lighting in all areas<br />
7. Is the room free from hazards, e.g. equipment, trailing<br />
electrical wiring etc<br />
8. Is there an identified recovery area with gym mats,<br />
preferably screened from other pupils to preserve their<br />
privacy <strong>and</strong> dignity<br />
9. Will there be sufficient free-st<strong>and</strong>ing tables/desks with flat<br />
surfaces for the immunisation equipment <strong>and</strong> for nurses to<br />
immunise safely<br />
10. Is the room easily accessible for emergency services,<br />
preferably on the ground floor<br />
11. Can 2 desks/chairs need to be positioned near the<br />
entrance of the room for clerks<br />
12. Has the member of school staff confirmed that there are<br />
no pupils on work experience, no college visits, no exams<br />
<strong>and</strong> no school trips<br />
If any part of the assessment is unacceptable, discuss with line manager or service lead<br />
The above requirements have been agreed between School <strong>and</strong> the School Health Nursing Service to ensure that<br />
pupils receive their immunisations safely. These arrangements must not be changed without discussion with the<br />
named nurse for the school.<br />
Signature of Assessor: ....................................... Date: ...........................<br />
Agreed by School Health Nurse: ..........................................<br />
Date: …........................<br />
Signature of Head of Year: .................................. Date: ..........................<br />
Copy to Head Teacher Copy to immunisation file Date to be reviewed:<br />
Page 28 of 46
APPENDIX 7<br />
<strong>Childhood</strong> <strong>Immunisation</strong> Procedural Guidelines<br />
NB.<br />
Practitioners are to arrive at the premises 15 minutes before the start of the session in<br />
order to prepare themselves <strong>and</strong> the room. Adequate time should be allocated to<br />
check/review all information necessary for the safe administration of vaccines.<br />
Preparation<br />
Action<br />
Rationale<br />
1. Ensure safe <strong>and</strong> suitable environment for clinic <strong>and</strong><br />
appropriate equipment is available<br />
2. Check immunisation schedules <strong>and</strong> clinic lists to identify<br />
vaccines required<br />
3. Ensure suitable vaccines are available, checking expiry<br />
date <strong>and</strong> cold chain has been maintained.<br />
4. Ensure Patient Group Directives authorisation in place or<br />
individual prescription if immunisation not covered by<br />
Patient Group Directive.<br />
5. There is immediate access to adrenaline (epinephrine)<br />
pack in the event of an anaphylactic reaction <strong>and</strong> there<br />
is a means to call for assistance e.g. telephone should<br />
emergency help be required (check mobile reception).<br />
Check expiry date of adrenaline<br />
1. Invite <strong>and</strong> welcome child/parent into area<br />
Pre administration of vaccine<br />
2. Confirm the correct identity with the child/carer <strong>and</strong> with<br />
clinical or electronic records<br />
3. Confirm which vaccine is to be given with the<br />
child/parent <strong>and</strong> the clinical or electronic records. If<br />
there are any anomalies in the schedule or history,<br />
contact the informatics department to confirm<br />
4. Check individual child’s vaccine history against the<br />
child’s records, immunisation schedule <strong>and</strong> parent held<br />
record (red book). Where there are concerns or<br />
discrepancies, the GP practice <strong>and</strong>/or information<br />
services are to be contacted to discuss.<br />
5. When delivering an immunisation session within the<br />
school setting, if the immunisation history is not<br />
available, the immunisation can proceed if the parent or<br />
young person confirms that the immunisation has not<br />
previously been given. If the parent or young person<br />
has any doubt regarding previous immunisations the<br />
immunisation should be postponed.<br />
6. If have unanswered concerns, refer to the ‘Green Book’,<br />
immunisation coordinator or <strong>Immunisation</strong> Trainer<br />
7. Check for contra-indication especially with regard to<br />
pregnancy, illness, medication, allergies, fever, previous<br />
adverse reaction <strong>and</strong> any recent vaccinations.<br />
To ensure patient safety <strong>and</strong> minimise the<br />
risk of drug errors<br />
To aid in emergency assistance<br />
To establish the correct identity <strong>and</strong><br />
immunisation schedule<br />
To gain informed consent<br />
Page 29 of 46
8. Ensure the child/parent is aware of common adverse<br />
reactions <strong>and</strong> action to take if they have any concerns<br />
9. Explain the procedure<br />
10. Ensure that the child/parent underst<strong>and</strong>s about the<br />
vaccines to be given <strong>and</strong> gain verbal informed consent<br />
11. Establish current health status to assess if child is fit for<br />
immunisation<br />
To assess if fit for immunisation<br />
12. Immediately prior to immunising the child, having<br />
assessed fitness to be immunised, select the correct<br />
vaccine, check dosage, expiry date <strong>and</strong> prepare.<br />
Reconstitute if necessary according to the<br />
manufacturer’s instructions<br />
Immunisers must not prepare substances for injection in<br />
advance of their immediate use or administer<br />
medication drawn into a syringe or container by another<br />
practitioner when not in their presence.(NMC 2010)<br />
13. Be aware of the dose of adrenaline that may be<br />
required for the individual child. Adrenaline must not be<br />
pre-drawn<br />
Administration of vaccine<br />
Action<br />
1. Check the route of administration <strong>and</strong> be familiar with<br />
the method of delivery<br />
2. Ensure safe positioning of child <strong>and</strong> administer vaccine<br />
at correct site using appropriate equipment <strong>and</strong><br />
technique<br />
Note<br />
Medical <strong>and</strong> nursing staff must give routine vaccines by<br />
the intra-muscular or deep subcutaneous route only.<br />
The sites which can be used are the middle third, upper<br />
outer aspect of the thigh or arm according to the<br />
manufacturers recommendations. BCG vaccine is given<br />
by intradermal injection.<br />
Where two or more injections need to be administered<br />
at the same time, they should be given at separate<br />
sites, preferably in a different limb. If more than 1<br />
injection is to be given in the same limb, they should be<br />
administered at least 2.5cm apart <strong>and</strong> documented<br />
accordingly<br />
Only the outer aspect of the thigh is to be used in a<br />
child under 1 year old<br />
3. Dispose of equipment as per policy.<br />
Post administration of vaccine<br />
To minimise the risk of drug errors<br />
Rationale<br />
To decide on appropriate route <strong>and</strong><br />
treatment<br />
To offer evidence based practice<br />
Action<br />
1. Observation of a patient following immunisation<br />
The Department of Health does not state a specific<br />
Rationale<br />
(See <strong>Immunisation</strong> against Infectious<br />
Diseases 2006 page 31).<br />
Resuscitation Council (UK) 2008 (updated<br />
Page 30 of 46
time <strong>and</strong> does not recommend long periods of<br />
observation. The risk of severe life-threatening<br />
reactions after immunisation is extremely small. A<br />
short period of observation (5-10 minutes), whilst<br />
completing documentation, should be used to detect<br />
immediate problems.<br />
2. Patients (<strong>and</strong> carers) should be provided with verbal or<br />
written advice on possible local <strong>and</strong> systemic reactions<br />
<strong>and</strong> what to do if they occur.<br />
3. Inform parent/care to contact GP or NHS direct in the<br />
event of adverse events or concerns<br />
4. Inform of timeframe of next vaccines due (if appropriate)<br />
5. Record the administration of the vaccines to include<br />
date of administration, name of vaccine, dose, the batch<br />
number, the site, the route of administration, expiry date<br />
<strong>and</strong> manufacturer.<br />
Enter details in the child’s records <strong>and</strong> immunisation<br />
schedule<br />
Enter on GP electronic patient record in scheduled<br />
clinics where in operation<br />
Unscheduled immunisation forms completed <strong>and</strong> copy<br />
sent to GP <strong>and</strong> Information Services<br />
Write the date <strong>and</strong> vaccine given in the parent’s red<br />
book<br />
6. Inform the child’s GP <strong>and</strong> named professional (if<br />
appropriate)<br />
2008, 2009)<br />
To offer advice, support <strong>and</strong> aftercare<br />
To maintain good st<strong>and</strong>ards of record<br />
keeping <strong>and</strong> documentation<br />
To liaise with extended health care teams<br />
7. Complete data collection for Child Health Information<br />
system <strong>and</strong> return to informatics within 24 hours.<br />
Page 31 of 46
APPENDIX 8<br />
ANAPHYLAXIS<br />
Equipment required for the treatment of anaphylaxis<br />
Practitioners must have attended anaphylaxis training within the last 12 months <strong>and</strong> be<br />
competent in the administration of adrenaline. Although adrenaline may be administered in<br />
anaphylaxis emergencies, practitioners should preferably have a PGD for the administration of<br />
adrenaline.<br />
<br />
<br />
<br />
Mobile phone or l<strong>and</strong>line access for emergency calls<br />
Laerdal or equivalent pocket mask or face shield for adults <strong>and</strong> children<br />
Adrenaline kit containing-<br />
-2 ampoules of Adrenaline (Epinephrine) 1:1000 (1mg/ml) injection<br />
- 4 x 23G (blue) needle (suitable for all ages).<br />
-A 21G (green) needle may be needed for obese patients.<br />
-A 25G 16mm length needle (orange) is suitable for IM injection in pre-term or very<br />
small infants ONLY.<br />
-4 x 1ml syringes (calibrated to 0.01ml)<br />
Adrenaline (epinephrine) dosage<br />
Adrenaline (epinephrine) 1 : 1000 (1mg/ml) solution<br />
The appropriate dose of adrenaline should be administered immediately by intramuscular (IM)<br />
injection (see table below). Treatment should be administered in accordance with advice given<br />
by the Resuscitation Council, Emergency treatment of anaphylactic reactions. Guidelines for<br />
Healthcare Providers (January 2008). A <strong>PCT</strong> Adrenaline PGD is available for practitioners to be<br />
signed up to use.<br />
Dose of adrenaline by age<br />
Child less than 6 years<br />
AGE<br />
DOSE OF ADRENALINE<br />
INTRAMUSCULAR (IM)<br />
(epinephrine) 1: 1000 (1mg/ml)<br />
150 micrograms 0.15ml route IM*<br />
Child 6-12 years 300 micrograms 0.3ml route IM<br />
Child over 12 years including adults 500 micrograms 0.5ml route IM<br />
*Use suitable syringe for measuring small volume<br />
Adrenaline must not be pre drawn<br />
300 microgram 0.3ml if child is small or<br />
prepubertal<br />
Page 32 of 46
APPENDIX 9<br />
Referral Pathway for <strong>Childhood</strong> <strong>Immunisation</strong>s in<br />
Secondary Care<br />
Rationale: To prevent inappropriate referrals to secondary care<br />
Please ensure you have prior discussion with an <strong>Immunisation</strong> Trainer or the <strong>Immunisation</strong> Co-ordinator<br />
before referring to secondary care.<br />
Page 33 of 46
Contraindications to <strong>Immunisation</strong><br />
All vaccines are contraindicated in those who have had:<br />
A confirmed anaphylactic reaction to a previous dose of a vaccine containing the same<br />
antigens, or<br />
A confirmed anaphylactic reaction to another component contained in the relevant<br />
vaccine, e.g. neomycin, streptomycin or polymixin B (which may be present in trace<br />
amounts in some vaccines).<br />
Live vaccines may be temporarily contraindicated in individuals who are:<br />
Immunosuppressed or Pregnant (see The Green Book)<br />
The following are NOT contraindications to immunisation<br />
Family history of any adverse reactions following immunisation<br />
Previous history of the disease (with the exceptions of BCG for people who have<br />
evidence of past exposure to tuberculosis)<br />
Contact with an infectious disease<br />
Premature birth<br />
<strong>St</strong>able neurological conditions such as cerebral palsy <strong>and</strong> Down’s syndrome<br />
Asthma, eczema or hay fever<br />
Mild self-limiting illness without fever, e.g. runny nose<br />
Treatment with antibiotics or locally acting (e.g. topical or inhaled) steroids<br />
Child’s mother or someone in the household being pregnant<br />
Currently breast-feeding or being breast-fed<br />
History of jaundice after birth<br />
Under a certain weight<br />
Being over the age recommended in the routine childhood immunisation schedule<br />
Personal history of febrile convulsions or epilepsy<br />
Close family history (parent or sibling) of febrile convulsions or epilepsy<br />
Being a sibling or close contact of an immunosuppressed individual<br />
Recent or imminent elective surgery<br />
Imminent general anaesthesia<br />
Unknown or inadequately documented immunisation history<br />
Egg Allergy<br />
Individuals with a confirmed anaphylactic reaction to egg should not receive influenza or yellow<br />
fever vaccines. MMR vaccine can be safely given to most children with a previous history<br />
of allergy after ingestion of egg or egg-containing food, <strong>and</strong> vaccination with MMR can<br />
be performed under normal circumstances.<br />
For the small number of individuals who have a history of confirmed anaphylactic reaction after<br />
any egg containing food, specialist advice should be sought with a view to <strong>Immunisation</strong> under<br />
controlled conditions.<br />
Anaphylaxis<br />
The following statement relating to a definition of anaphylaxis is taken from the ‘Emergency<br />
treatment of anaphylactic reactions: Guidelines for healthcare providers (January 2008)<br />
produced by the Resuscitation Council (UK)<br />
Page 34 of 46
“A precise definition of anaphylaxis is not important for the emergency treatment of an<br />
anaphylactic reaction. There is no universally agreed definition. The European Academy<br />
of Allergology <strong>and</strong> Clinical Immunology Nomenclature Committee proposed the following<br />
broad definition: ‘Anaphylaxis is a severe, life-threatening, generalised or systemic<br />
hypersensitivity reaction’. This is characterised by rapidly developing life-threatening<br />
airway <strong>and</strong>/or breathing <strong>and</strong>/or circulation problems usually associated with skin <strong>and</strong><br />
mucosal changes.”<br />
Ref:<br />
Department of Health<br />
2006 <strong>Immunisation</strong> against infectious disease<br />
(The Green Book),<br />
Resuscitation Council UK 2008 Emergency treatment of anaphylactic reactions.<br />
Guidelines for healthcare providers<br />
Page 35 of 46
APPENDIX 10<br />
PROCEDURES FOR MASS IMMUNISATION OF SCHOOL AGE CHILDREN IN<br />
THE SCHOOL NURSING SERVICE<br />
These procedures are to be read in conjunction with relevant <strong>PCT</strong> policies, <strong>Childhood</strong><br />
<strong>Immunisation</strong> <strong>Policy</strong>, ‘Maintenance of the Cold Chain <strong>Policy</strong>’, ‘Mass Vaccination <strong>Policy</strong>’,<br />
‘Resuscitation <strong>Policy</strong>’, ‘Health Records <strong>Policy</strong>’, ‘Consent <strong>Policy</strong>’, ‘<strong>St</strong><strong>and</strong>ards for Medicine<br />
Management’ <strong>and</strong> associated st<strong>and</strong>ard operating procedures.<br />
Procedures<br />
ACTION RATIONALE PERSON<br />
RESPONSIBLE<br />
1. An up to date school year list is to be<br />
acquired from school.<br />
2. Parent/ guardians immunisation written<br />
consent forms to be ordered<br />
3. An appropriate number of verbal<br />
consent forms is printed to be used<br />
when initial consent forms have not<br />
been returned<br />
4. The correct amount of immunisation<br />
leaflets are ordered from DH or Library<br />
Resource Officer<br />
5. The immunisation timetable is agreed<br />
by the school nurse <strong>and</strong> the school<br />
health team for the next academic<br />
year.<br />
6. <strong>Immunisation</strong> dates agreed with each<br />
school’s senior leadership team.<br />
7. A risk assessment of the environment<br />
used for immunisation session to be<br />
completed<br />
8. An immunisation team is identified for<br />
each immunisation session.<br />
PREPARATION<br />
To identify the accurate cohort of<br />
pupils who require immunisation.<br />
To ensure there are an<br />
appropriate number of consent<br />
forms.<br />
To ensure that adequate stocks<br />
are available<br />
To ensure there are an<br />
appropriate number of<br />
immunisation information leaflets<br />
to send to young people,<br />
parents/guardians.<br />
To ensure that immunisations are<br />
offered within an optimal<br />
timescale.<br />
To ensure that immunisations are<br />
organised at an appropriate time<br />
within the school calendar.<br />
To ensure that immunisations are<br />
given in a safe environment<br />
To maintain adequate cover for<br />
sickness, safeguarding, holidays.<br />
<strong>St</strong> <strong>Helens</strong> - Named<br />
Immuniser for each<br />
school<br />
<strong>Halton</strong> – Admin<br />
<strong>and</strong> Clerical team<br />
A designated<br />
person from the<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Team Co-ordinator<br />
Team Coordinators<br />
School Health<br />
Teams<br />
Immuniser<br />
Immuniser<br />
Team Co-ordinator<br />
9. A reserve nurse immuniser is identified To maintain adequate cover in Team Co-ordinator<br />
Page 36 of 46
for each session.<br />
10. The names <strong>and</strong> location of young<br />
people who are educated ‘otherwise’<br />
<strong>and</strong> require immunisations are<br />
coordinated by a named nurse.<br />
11. The availability of an Admin Officer <strong>and</strong><br />
a reserve clerk, is negotiated with the<br />
clinic clerical staff for each session<br />
including the sessions in the special<br />
schools.<br />
12. Sufficient number of vaccines ordered<br />
4 weeks prior to a session<br />
13. Year group <strong>and</strong> parent education<br />
sessions agreed with school as<br />
appropriate.<br />
14. <strong>Immunisation</strong> packs to be prepared:-<br />
HPV<br />
Information letter<br />
HPV Consent Form<br />
Q/A leaflet for parents / carers<br />
(Year 8)<br />
Information leaflet for young person<br />
Pre addressed return envelope<br />
marked private <strong>and</strong> confidential<br />
case of sickness<br />
To ensure that all school aged<br />
young people have the opportunity<br />
to be immunised.<br />
To ensure each session is<br />
supported by an Admin Officer.<br />
To ensure that the required<br />
amount of vaccine is available for<br />
each session.<br />
To ensure that young people <strong>and</strong><br />
parents / guardians can make<br />
decisions based on informed<br />
consent.<br />
To ensure parents / guardians <strong>and</strong><br />
young people have enough<br />
information to make an informed<br />
decision before completing <strong>and</strong><br />
returning a signed consent form.<br />
Team Co-ordinator<br />
Immuniser<br />
Immuniser<br />
Immuniser<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Td/IPV<br />
Information letter<br />
DTP/MMR Consent Form<br />
Information leaflet<br />
Pre addressed return envelope<br />
marked private <strong>and</strong> confidential<br />
15. A written action plan is agreed by<br />
immuniser <strong>and</strong> the school lead which<br />
outlines the date that consent forms<br />
will be delivered <strong>and</strong> collected.<br />
16. The appropriate number of information<br />
packs is taken to school at least 3<br />
weeks prior to the immunisation<br />
session<br />
17. A labelled box file is available in each<br />
school for returned envelopes<br />
containing the consent forms.<br />
18. Returned consent forms will be<br />
collected from school on a pre-<br />
To ensure that the consent forms<br />
are transported by a member of<br />
the school health team. To avoid<br />
multiple visits to school to collect<br />
forms <strong>and</strong> to avoid loss of forms.<br />
To ensure that each parent /<br />
guardian receive a consent form<br />
<strong>and</strong> enough information to make<br />
an informed decision.<br />
For risk minimisation.<br />
To allow enough time for the<br />
consent forms to be processed<br />
Immuniser<br />
<strong>St</strong> <strong>Helens</strong> - School<br />
Nurses<br />
<strong>Halton</strong> – School<br />
Health Nursing<br />
Assistant<br />
Immuniser<br />
<strong>St</strong> <strong>Helens</strong> -<br />
Immuniser<br />
Page 37 of 46
arranged date at least one week before<br />
the immunisation session<br />
19. Returned consent forms logged<br />
against the school’s year list.<br />
20. Where consent has been refused the<br />
forms to be identified as a ‘consent<br />
refusal’ <strong>and</strong> filed separately.<br />
21. In the event of a consent form being<br />
lost, a second consent form is sent to<br />
the parent/ guardians. This second<br />
form must state the pupil’s name <strong>and</strong><br />
date of birth <strong>and</strong> be clearly marked<br />
DUPLICATE.<br />
22. A list to be made of the outst<strong>and</strong>ing<br />
consent forms.<br />
23. When consent forms are not returned,<br />
the parent / guardians to be contacted<br />
by the Immuniser to obtain verbal<br />
consent in accordance with consent<br />
guidelines <strong>and</strong> the <strong>Childhood</strong><br />
<strong>Immunisation</strong> <strong>Policy</strong>.<br />
24. Consent forms checked for parental<br />
concerns <strong>and</strong> discrepancies.<br />
25. The immunisation equipment is cross<br />
checked with the agreed list <strong>and</strong><br />
prepared for the session<br />
26. <strong>St</strong> <strong>Helens</strong> <strong>and</strong> Widnes<br />
The correct number of vaccines<br />
required for the session is removed<br />
from the fridge in the clinic setting. The<br />
temperature of the fridge checked as<br />
per Cold Chain <strong>Policy</strong>.<br />
Runcorn<br />
The correct number of vaccines is<br />
collected from North Cheshire Hospital<br />
(<strong>Halton</strong>) pharmacy.<br />
<strong>PCT</strong> wide<br />
Vaccines are transported to the school<br />
in an approved vaccine carrier<br />
1. Equipment laid out onto each<br />
immunisation table.<br />
Adrenalin boxes <strong>and</strong> packs are to be<br />
before the immunisation sessions. <strong>Halton</strong> – School<br />
Health Nursing<br />
Assistant<br />
To identify those young people<br />
who require immunisation <strong>and</strong><br />
those who do not consent to the<br />
immunisation being given.<br />
To minimise risk of immunisation<br />
without consent.<br />
To ensure that the correct form is<br />
issued to the correct pupil. To<br />
avoid immunisations being given<br />
twice.<br />
To enable the Immuniser to<br />
contact parents / guardians to<br />
facilitate verbal consent if<br />
appropriate.<br />
To facilitate verbal consent safely<br />
To extract issues / questions<br />
which need addressing.<br />
To ensure that the correct<br />
equipment is taken into school.<br />
To take the correct amount of<br />
vaccine to the session at the<br />
correct<br />
temperature<br />
To maintain the cold chain.<br />
PRE ADMINISTRATION OF VACCINE<br />
To ensure that each nurse has<br />
access to everything she needs<br />
<strong>and</strong> is adequately prepared should<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Immuniser<br />
Immuniser<br />
Immuniser<br />
Immuniser<br />
Immuniser<br />
Page 38 of 46
easily accessible. a young person have an<br />
anaphylactic reaction.<br />
2. Pupils present themselves to the clerk,<br />
who verifies name, date of birth <strong>and</strong><br />
address of the child <strong>and</strong> the completed<br />
consent form is given to the child<br />
3. Children / young people who do not<br />
have written consent to be seen by an<br />
Immuniser <strong>and</strong> be assessed for their<br />
ability to give verbal consent as per<br />
consent policy<br />
4. The Immuniser confirms the correct<br />
identity with the child<br />
5. Confirm which vaccine is to be given<br />
with the child/parent. If there are any<br />
anomalies in the schedule or history,<br />
contact the informatics department.<br />
6. If there are unanswered concerns,<br />
refer to immunisation coordinator or<br />
specialist lead immunisation<br />
coordinator<br />
7. Check for contra-indication especially<br />
with regard to pregnancy, illness,<br />
medication, allergies, fever, previous<br />
adverse reaction <strong>and</strong> any recent<br />
vaccinations.<br />
8. Ensure the child/parent is aware of<br />
common adverse reactions <strong>and</strong> action<br />
to take if they have any concerns<br />
9. Explain the procedure, ensuring that<br />
the child/parent underst<strong>and</strong>s about the<br />
vaccines to be given<br />
10 Establish current health status to<br />
assess if child is fit for immunisation<br />
To ensure that the right person<br />
receives the right immunisation<br />
To ensure that all young people<br />
are given equal opportunity to<br />
receive their immunisation.<br />
To establish the correct identity<br />
<strong>and</strong> immunisation schedule<br />
To explain the procedure<br />
To assess if fit for immunisation<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Immuniser<br />
Immuniser<br />
Immuniser<br />
Immuniser<br />
ADMINISTRATION OF VACCINE<br />
1 In the presence of the child/parent, To minimise the risk of drug errors Immuniser<br />
select the correct vaccine, check<br />
dosage, expiry date <strong>and</strong> prepare<br />
immediately prior to immunising the<br />
child. Reconstitute if necessary<br />
according to the manufacturer’s<br />
instructions<br />
2 Be aware of the dose of adrenaline<br />
that may be required for the individual<br />
child. Adrenaline must not be predrawn<br />
3 Check the route of administration <strong>and</strong> To decide on appropriate route<br />
be familiar with the method of delivery <strong>and</strong> treatment<br />
Immuniser<br />
4 Ensure safe positioning of child <strong>and</strong> To offer evidence based practice Immuniser<br />
Page 39 of 46
administer vaccine at correct site using<br />
appropriate equipment <strong>and</strong> technique<br />
Note<br />
Medical <strong>and</strong> nursing staff must give<br />
routine vaccines by the intra-muscular<br />
or deep subcutaneous route only. The<br />
sites which can be used are the middle<br />
third, upper outer aspect of the thigh or<br />
arm according to the manufacturers<br />
recommendations<br />
5 Each immunisation carried out in<br />
accordance with the appropriate PGD<br />
as per <strong>PCT</strong> Patient Group Direction<br />
(PGD) <strong>Policy</strong><br />
6 Dispose of equipment as per Infection<br />
Prevention <strong>and</strong> Control policy.<br />
To ensure that each immunisation<br />
is given correctly <strong>and</strong> safely in<br />
accordance with local <strong>and</strong> national<br />
guidance.<br />
Immuniser<br />
POST ADMINISTRATION OF VACCINE<br />
1 Record the administration of the<br />
vaccines to include date of<br />
administration, name of vaccine, dose,<br />
the batch number, the site, the route of<br />
administration, expiry date <strong>and</strong><br />
manufacturer. Immuniser to print <strong>and</strong><br />
sign name <strong>and</strong> designation. This<br />
completed consent form to be given to<br />
the Admin <strong>and</strong> Clerical team<br />
2 In the case of HPV, a record card to be<br />
completed for each pupil after each<br />
immunisation <strong>and</strong> given to the pupil<br />
after dose 3<br />
3 After the immunisation, each pupil be<br />
given a post immunisation letter to take<br />
home<br />
To maintain good st<strong>and</strong>ards of<br />
record keeping <strong>and</strong><br />
documentation<br />
To provide each pupil with a<br />
complete record of their HPV<br />
immunisation.<br />
To inform parents / guardians<br />
that the immunisation has been<br />
given <strong>and</strong> to provide them with<br />
information about possible side<br />
effects.<br />
Immuniser<br />
Immuniser<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Immuniser<br />
Admin <strong>and</strong> Clerical<br />
team<br />
4 Observation of a patient following<br />
immunisation<br />
The Department of Health does not<br />
state a specific time <strong>and</strong> does not<br />
recommend long periods of<br />
observation. The risk of severe lifethreatening<br />
reactions after<br />
immunisation is extremely small. A<br />
short period of observation (5-10<br />
In the case of HPV the letter will<br />
tell the young person, parent /<br />
carer which dose they have<br />
received <strong>and</strong> when the next one<br />
is due.<br />
(See <strong>Immunisation</strong> against<br />
Infectious Diseases 2006 page<br />
31).<br />
Resuscitation Council (UK) 2008<br />
(updated 2008, 2009)<br />
Page 40 of 46
minutes), whilst completing<br />
documentation, should be used to<br />
detect immediate problems.<br />
5 2 immunisers to remain on school site<br />
for approximately 30 minutes following<br />
the last immunisation to support school<br />
staff<br />
To ensure that any clinical<br />
incidents after the immunisation<br />
session are dealt with<br />
appropriately<br />
School nursing team<br />
AFTER THE SESSION AT BASE<br />
1 <strong>Immunisation</strong> data is recorded<br />
according to local requirements<br />
HPV consent forms are photocopied<br />
<strong>and</strong> sent to informatics after dose 1<br />
<strong>and</strong> 2. The original consent form be<br />
sent after dose 3.<br />
2 A HPV tally sheet for each year is<br />
completed after each HPV<br />
immunisation session<br />
3. Unused vaccines are returned promptly<br />
to the fridge as per Cold Chain <strong>Policy</strong><br />
4. A letter is sent to the parents /<br />
guardians of pupils who did not receive<br />
their immunisation explaining the<br />
reasons for non immunisation <strong>and</strong> what<br />
action the parent/guardian should now<br />
take.<br />
Any pupil who does not receive their<br />
immunisation in school may be offered<br />
the immunisation in a future clinic in<br />
school or the community<br />
5. Once the consent forms are returned<br />
from informatics, the consent form is<br />
filed in each pupil’s records. If any of<br />
the child health records are unavailable<br />
follow the records management policy.<br />
6. All admin <strong>and</strong> clerical officers will<br />
check that the same number of<br />
consent forms that were sent to<br />
informatics are returned to the clinic.<br />
7. Following HPV <strong>Immunisation</strong> Sessions<br />
consent forms <strong>and</strong> immunisation<br />
record cards are stored securely at<br />
base, between each session.<br />
To enable data to be entered<br />
onto the Child Health Computer<br />
in a timely manner.<br />
To ensure that the monthly<br />
returns for HPV are accurate<br />
<strong>and</strong> available to the Department<br />
of Health<br />
To store vaccines safely<br />
To ensure that parents /<br />
guardians are kept informed<br />
about their child’s immunisation<br />
needs <strong>and</strong> to ensure that all<br />
young people will be given equal<br />
opportunity to receive their<br />
immunisation.<br />
To ensure the <strong>PCT</strong> holds health<br />
information for every pupil.<br />
To enable practitioners to cross<br />
reference immunisation dates<br />
with each young person’s<br />
consent form <strong>and</strong> to ensure that<br />
consent forms are appropriately<br />
filed in each pupil’s records.<br />
To ensure that the original<br />
consent form is available for the<br />
next stage of the programme.<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Immuniser<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Admin <strong>and</strong> Clerical<br />
team<br />
8. Young people who are educated To ensure that all young people Team Co-ordinator<br />
Page 41 of 46
‘otherwise’ are invited to a community<br />
session or offered the immunisation at<br />
home.<br />
9 If any pupil relocates to another school<br />
during the immunisation programme,<br />
their consent form <strong>and</strong> immunisation<br />
record card to be included in the child<br />
health record prior to booking out to<br />
new clinic/<strong>PCT</strong>. Transfer out data will<br />
be recorded.<br />
are given equal opportunity to<br />
receive their immunisation.<br />
To ensure that pupils are<br />
included in the correct<br />
immunisation session <strong>and</strong> thus<br />
receive their immunisation in a<br />
timely manner.<br />
Admin <strong>and</strong> Clerical<br />
team<br />
Page 42 of 46
APPENDIX 11<br />
HEALTH VISITING TEAM PRE IMMUNISATION CHECK LIST<br />
Childs Name:<br />
Yes<br />
Date of Birth:<br />
Location:<br />
No<br />
Date:<br />
Checked client details with relevant documentation<br />
Discussed vaccines to be administered<br />
Informed verbal consent obtained<br />
Identify if child is well today<br />
Has the child had a temperature in last 48 hours<br />
Are they on any medication<br />
Did the child have any problems with any previous vaccinations<br />
Has the child ever had an allergic reaction to anything<br />
Has the child received another vaccine in last 4 weeks<br />
If yes document what they are; when & where given.<br />
Was vaccination deferred<br />
Has the child had this vaccine(s) anywhere else<br />
If yes document <strong>and</strong> inform information services & GP<br />
Post vaccination advice/ 2009 leaflet given.<br />
Information services & GP surgery informed of vaccines administered.<br />
Signed:<br />
Page 43 of 46
APPENDIX 12<br />
Guidelines for Domiciliary <strong>Immunisation</strong><br />
These guidelines are intended to support all staff who administer immunisations, within a<br />
domiciliary setting.<br />
These guidelines should be used in conjunction with the current volume<br />
<strong>and</strong> updated chapters of <strong>Immunisation</strong> against Infectious Disease (2006), (The Green<br />
Book)<br />
Immunisers must adhere to all process <strong>and</strong> procedures in the Trust’s <strong>Childhood</strong><br />
<strong>Immunisation</strong> <strong>Policy</strong> (2010),<br />
In the event of a failed visit, one further appointment may be made <strong>and</strong> the referrer<br />
notified.<br />
Action<br />
Rationale<br />
Referral received <strong>and</strong> immunisation status checked<br />
with GP <strong>and</strong> information services<br />
Immuniser to contact the family to arrange an<br />
appointment<br />
Immuniser to practice in accordance with the<br />
<strong>Childhood</strong> <strong>Immunisation</strong> <strong>Policy</strong> 2010 when offering<br />
immunisations in the home setting<br />
Vaccines transported according to the Cold Chain<br />
<strong>Policy</strong><br />
Immuniser <strong>and</strong> a second staff member to attend visit<br />
To prevent immunisation<br />
duplication/drug errors<br />
To maintain time management<br />
To ensure evidence based practice is<br />
followed.<br />
To maintain the cold chain<br />
To aid in emergency assistance<br />
Mobile phone available <strong>and</strong> accessible during visit<br />
<strong>Childhood</strong> <strong>Immunisation</strong> Procedural Guidelines to be<br />
followed in the preparation, administration <strong>and</strong><br />
documentation of immunisation<br />
Unused vaccines returned as per Cold Chain <strong>Policy</strong><br />
To offer evidence based practice<br />
To maintain the cold chain<br />
Page 44 of 46
APPENDIX 13<br />
Equality Impact Assessment Tool<br />
To be completed with the corporate document when submitted to the appropriate committee for<br />
consideration, approval <strong>and</strong> ratification.<br />
1. Does the corporate document affect one group<br />
less or more favourably than another on the basis<br />
of:<br />
Yes/No<br />
Race N<br />
Ethnic origins (including gypsies <strong>and</strong> travellers) N<br />
Nationality N<br />
Gender N<br />
Culture N<br />
Religion or belief N<br />
<br />
Sexual orientation including lesbian, gay <strong>and</strong><br />
bisexual people<br />
Comments<br />
Age Y Children 0-18 years<br />
<br />
Disability - learning disabilities, physical disability,<br />
sensory impairment <strong>and</strong> mental health problems<br />
2. Is there any evidence that some groups are<br />
affected differently<br />
3. If you have identified potential discrimination, are<br />
there any exceptions valid, legal <strong>and</strong>/or<br />
justifiable<br />
4. Is the impact of the policy/guidance likely to be<br />
negative<br />
5. If so can the impact be avoided<br />
6. What alternative are there to achieving the<br />
policy/guidance without the impact<br />
7. Can we reduce the impact by taking different<br />
action<br />
N<br />
N<br />
N<br />
Y<br />
N<br />
As above<br />
If you have identified a potential discriminatory impact of this corporate document, please refer it<br />
to [insert name of appropriate person], together with any suggestions as to the action required<br />
to avoid/reduce this impact. For advice in respect of answering the above questions, please<br />
contact [insert name of appropriate person <strong>and</strong> contact details].<br />
Page 45 of 46
APPENDIX 14<br />
Dissemination <strong>and</strong> Training Plan<br />
To be completed with the corporate document when submitted to the appropriate committee for<br />
consideration, approval <strong>and</strong> ratification. The status column must be given a Red, Amber or<br />
Green rating with evidence to demonstrate an action has been completed.<br />
DISSEMINATION PLAN<br />
Title of document:<br />
<strong>Childhood</strong> Vaccination <strong>and</strong> <strong>Immunisation</strong><br />
Dissemination Lead: (Print name <strong>and</strong><br />
contact details)<br />
Proposed action to retrieve out-of-date<br />
copies of the document:<br />
Date finalised: 02.11.10<br />
Previous document already being used no<br />
If yes, in what format <strong>and</strong> where Electronic/Intranet<br />
Withdraw from the internet/intranet/portal<br />
To be disseminated to:<br />
Disseminated<br />
by whom<br />
Timescale<br />
(Date)<br />
<strong>St</strong>atus<br />
R A G<br />
Paper<br />
or<br />
Electronic<br />
Comments<br />
Trust Times<br />
Team Brief<br />
Training sessions (Give Details Below)<br />
Other (Give Details Below) /<br />
Child Health<br />
Service leads<br />
Within 3<br />
months<br />
electronic<br />
IMPLEMENTATION PLAN<br />
Training Timescale Owner <strong>St</strong>atus<br />
R A G<br />
Training Event (Please provide details of available training venues/dates<br />
to educate staff about this document)<br />
Training Plan Lead (Please provide details of staff who will be<br />
responsible for overseeing this training) Team leaders child health<br />
Within 3<br />
months<br />
Service<br />
leads<br />
Compliance Monitoring Timescale Owner <strong>St</strong>atus<br />
R A G<br />
<br />
Methodology to be used for monitoring/audit (please include <strong>PCT</strong><br />
Audit Proposal Form)<br />
12 months Service<br />
lead<br />
Responsibilities for conducting monitoring/audit Team<br />
leaders<br />
Frequency of monitoring/audit (e.g. annually, 6 monthly etc) annual Team<br />
leaders<br />
Process for reviewing/reporting results essential training<br />
PDR process<br />
Denotes: Action not yet taken or deadline for action not met. Action plan to address this must be provided.<br />
Denotes: Action partially implemented.<br />
Denotes: Action complete.<br />
Page 46 of 46