Case Report Invasive Mucinous Adenocarcinoma of the Lung ç ä¾ ...
Case Report Invasive Mucinous Adenocarcinoma of the Lung ç ä¾ ...
Case Report Invasive Mucinous Adenocarcinoma of the Lung ç ä¾ ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
台 灣 癌 症 醫 誌 (J. Cancer Res. Pract.) 28(2),94-98, 2012<br />
<strong>Case</strong> <strong>Report</strong><br />
journal homepage:www.cos.org.tw/web/index.asp<br />
<strong>Invasive</strong> <strong>Mucinous</strong> <strong>Adenocarcinoma</strong> <strong>of</strong> <strong>the</strong> <strong>Lung</strong><br />
Han-Tsung Liu 1,2 , Shiou-Fu Lin 3 , Yuh-Ming Chen 4 *<br />
1 Division <strong>of</strong> Hematology and Oncology, Department <strong>of</strong> Medicine, Taipei Veterans General Hospital, Taipei, Taiwan<br />
2 Division <strong>of</strong> Hematology and Oncology, Department <strong>of</strong> Internal Medicine, Taipei City Hospital Zhongxiao Branch,<br />
Taipei, Taiwan<br />
3 Department <strong>of</strong> Pathology and Laboratory Medicine, Taipei Veterans General Hospital, Taipei, Taiwan<br />
4 Department <strong>of</strong> Chest Medicine, Taipei Veterans General Hospital, Taipei, Taiwan<br />
Abstract.<br />
<strong>Invasive</strong> mucinous adenocarcinoma <strong>of</strong> <strong>the</strong> lung is a rare disease with distinct pathological<br />
features and uncommon biological manifestations. We report a 50 year-old woman who initially<br />
presented with increasing shortness <strong>of</strong> breath and progressive facial swelling. She was diagnosed<br />
with invasive mucinous adenocarcinoma <strong>of</strong> <strong>the</strong> lung with its immunohistochemistry revealed<br />
as CK7 (+), CK20 (+), CDX2 (+), TTF-1 (-), CK5/6 (-), and P63 (-). We also describe<br />
how <strong>the</strong> patient initially had a good response to chemo<strong>the</strong>rapy with paclitaxel and cisplatin.<br />
病 例 報 告<br />
Keywords : invasive mucinous adenocarcinoma, diagnosis, treatment<br />
侵 襲 性 黏 液 性 肺 腺 癌<br />
劉 瀚 聰<br />
1,2<br />
林 脩 涪<br />
3<br />
陳 育 民<br />
4 *<br />
1<br />
台 北 榮 民 總 醫 院 內 科 部 血 液 腫 瘤 科<br />
2<br />
台 北 市 立 聯 合 醫 院 忠 孝 院 區 血 液 腫 瘤 科<br />
3<br />
台 北 榮 民 總 醫 院 病 理 部<br />
4<br />
台 北 榮 民 總 醫 院 胸 腔 部<br />
中 文 摘 要<br />
侵 襲 性 黏 液 性 肺 腺 癌 是 一 種 罕 見 的 疾 病 , 它 的 病 理 特 徵 很 特 殊 , 而 且 生 物 表 現 也 不<br />
同 於 一 般 的 肺 腺 癌 。 我 們 要 報 告 一 個 侵 襲 性 黏 液 性 肺 腺 癌 的 個 案 , 她 的 病 理 免 疫 細 胞 學<br />
染 色 呈 現 CK7 (+)、CK20 (+)、CDX2 (+)、TTF-1 (-)、CK5/6 (-) 以 及 P63 (-)。 這 個 病 人 一<br />
開 始 對 太 平 洋 紫 杉 醇 加 上 順 鉑 的 化 學 治 療 有 很 好 的 反 應 。<br />
關 鍵 字 : 侵 襲 性 黏 液 性 肺 腺 癌 、 診 斷 、 治 療<br />
INTRODUCTION<br />
In 2011, <strong>the</strong> International Association for <strong>the</strong><br />
Study <strong>of</strong> <strong>Lung</strong> Cancer (IASLC), <strong>the</strong> American Thoracic<br />
Society (ATS) and <strong>the</strong> European Respiratory Society<br />
(ERS) developed a new classification <strong>of</strong> adenocarcinoma<br />
<strong>of</strong> lung. In <strong>the</strong> new classification, use <strong>of</strong> <strong>the</strong><br />
term “bronchioloalveolar carcinoma” (BAC) describing<br />
certain variants <strong>of</strong> lung cancer has been discon-
H. T. Liu et al./JCRP 28(2012) 94-98 95<br />
tinued [1]. Unlike adenocarcinoma in situ (AIS) and<br />
minimally invasive adenocarcinoma (MIA), which<br />
both have nearly 100% 5-year survival rates, invasive<br />
mucinous adenocarcinoma (formerly mucinous BAC)<br />
has a comparatively poorer prognosis. Within <strong>the</strong> criteria<br />
for <strong>the</strong> new staging system, <strong>the</strong>re is no collected<br />
survival data that has been fully presented for mucinous<br />
adenocarcinoma <strong>of</strong> <strong>the</strong> lung. However, prior literature<br />
shows that <strong>the</strong> disease has unusual clinical<br />
presentation and distinct immunohistochemical features.<br />
CASE REPORT<br />
A 50-year-old woman was transferred to our hospital.<br />
One month before admission, she had increasing<br />
shortness <strong>of</strong> breath and progressive facial swelling.<br />
She visited a local hospital for medical assistance,<br />
where a subsequent chest X-ray showed massive right<br />
pleural effusion and widening <strong>of</strong> <strong>the</strong> upper mediastinum.<br />
Thoracentesis yielded bloody exudative effusion,<br />
and a pig-tail tube was inserted for drainage. The<br />
drainage volume was 400-500 ml per day. Subsequently,<br />
<strong>the</strong> pig-tail tube was <strong>the</strong>n replaced by a chest<br />
tube due to blood clot occlusion. Cytological examination<br />
indicated adenocarcinoma. The patient’s chest<br />
CT scan depicted massive right pleural effusion, a<br />
thrombus at <strong>the</strong> superior vena cava, and a 3 x 3 cm<br />
mass at <strong>the</strong> anterior mediastinum. The thrombus was<br />
thought to be tumor-related. CT-guided biopsy <strong>of</strong> <strong>the</strong><br />
anterior mediastinum mass revealed metastatic adenocarcinoma<br />
with immunohistochemical stain as CK7<br />
(-), TTF-1 (-), CK20 (+) and CDX2 (+), suggesting<br />
metastatic adenocarcinoma <strong>of</strong> <strong>the</strong> lower gastrointestinal<br />
tract. The patient underwent esophagogastroduo-<br />
*Corresponding author: Yuh-Min Chen, M.D., Ph.D.<br />
* 通 訊 作 者 : 陳 育 民 醫 師<br />
Tel: +886-2-28757563<br />
Fax: +886-2-28763466<br />
E-mail: ymchen@vghtpe.gov.tw<br />
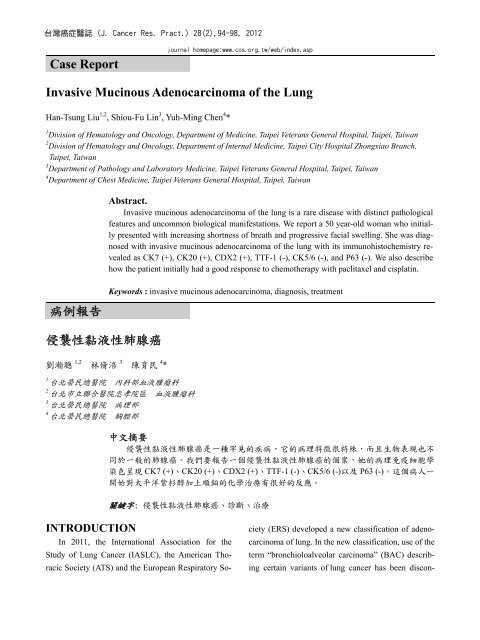
Figure 1. <strong>Mucinous</strong> pools contain poorly differentiated<br />
adenocarcinoma cells (200X)<br />
denoscopy (EGD endoscopy) and colonoscopy, with<br />
resulting negative findings. PET/CT scan revealed uptake<br />
in <strong>the</strong> patient’s anterior mediastinum and <strong>the</strong> right<br />
lower lung, and she was <strong>the</strong>n treated as metastatic adenocarcinoma<br />
<strong>of</strong> lower gastrointestinal origin. After this<br />
diagnosis, <strong>the</strong> patient came to our hospital for a second<br />
opinion, where additional diagnostic tests were performed.<br />
Similar to her previous results, <strong>the</strong> patient’s<br />
brain MRI and mammography were negative; gynecological<br />
ultrasound exam revealed myomas only. We<br />
repeated <strong>the</strong> chest CT scan and performed biopsy to <strong>the</strong><br />
pleural lesions. The pathology report showed metastatic<br />
adenocarcinoma with immunohistochemistry noted as<br />
CK7 (+), CK20 (+), CDX2 (+), TTF-1 (-), CK5/6 (-),<br />
and P63 (-) (Figures 1, 2). EGFR sequencing reported<br />
no mutation. Because <strong>of</strong> <strong>the</strong> discordance <strong>of</strong> immunochemistry<br />
pr<strong>of</strong>iles between <strong>the</strong> pleural sample and <strong>the</strong><br />
anterior mediastinal tumor, we discussed this case in<br />
our lung cancer multidisciplinary conference. The<br />
members concluded that <strong>the</strong> tumor was compatible with<br />
invasive mucinous adenocarcinoma <strong>of</strong> lung, and we<br />
treated <strong>the</strong> patient with paclitaxel plus cisplatin. Three<br />
days later, her pleural effusion markedly decreased, and<br />
chest film indicated widening <strong>of</strong> <strong>the</strong> anterior mediastinum.<br />
We maintained this regimen for 2 months, but<br />
unfortunately her disease progressed (Figure 3).
96 H. T. Liu et al./JCRP 28(2012) 94-98<br />
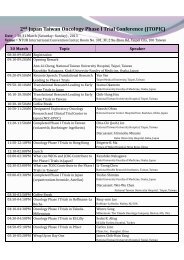
CK7(+)<br />
CK20(+)<br />
TTF‐1(‐)<br />
CDX2(+)<br />
Figure 2. The immunohistochemical stains show CK7 (+), CK20 (+), TTF-1 (-) and CDX2 (+) (400X)<br />
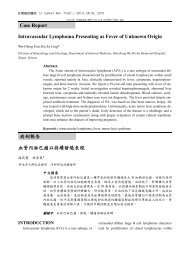
Figure 3. The chest CT shows anterior mediastinal<br />
tumor (black arrow) and pleural seeding<br />
(white arrows)<br />
DISCUSSION<br />
The characteristics <strong>of</strong> invasive mucinous adenocarcinoma<br />
were reported to be predominantly found in<br />
female (58%), non-smoker (55%), positive CK7<br />
(~88%), CK20 (~54%) and negative TTF-1 (~83%) in<br />
immunohistostain. The genotypes <strong>of</strong> invasive mucinous<br />
adenocarcinoma have frequent KRAS mutation<br />
(~76%) and almost no EGFR mutation (~3%) [2]. The<br />
radiographic appearance <strong>of</strong> <strong>the</strong>se tumors are characterized<br />
by majority consolidation, air bronchogram,<br />
and frequent multifocal and multilobar presentation.<br />
Mazziotta et al. also reported ten <strong>of</strong> 84 primary lung<br />
carcinomas (12%) were immunoreactive for CDX2<br />
expression (a gastrointestinal marker) [3]. They concluded<br />
that primary lung adenocarcinoma can also
H. T. Liu et al./JCRP 28(2012) 94-98 97<br />
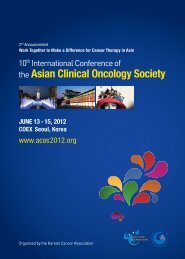
A<br />
B<br />
Figure 4. (A) Series <strong>of</strong> chest films show initial response to a course <strong>of</strong> chemo<strong>the</strong>rapy with paclitaxel<br />
and cisplatin, and (B) progressive disease two months later<br />
express CDX2, which was previously thought to be a<br />
specific marker for tumors with intestinal differentiation.<br />
Due to <strong>the</strong> introduction <strong>of</strong> <strong>the</strong> new classification<br />
system and rare disease incidence rate, <strong>the</strong>re were lim-
98 H. T. Liu et al./JCRP 28(2012) 94-98<br />
ited studies that had mentioned <strong>the</strong> treatment <strong>of</strong> invasive<br />
mucinous adenocarcinoma. According to WHO<br />
2004 classification, research has shown that surgery<br />
for resectable disease remains <strong>the</strong> mainstay treatment<br />
<strong>of</strong> BAC [4]. However, for invasive mucinous adenocarcinoma,<br />
<strong>the</strong>re was no study which demonstrated an<br />
optimum treatment response.<br />
Some reports showed a good treatment response to<br />
tyrosine kinase inhibitor (TKI) in MIA patients harboring<br />
<strong>the</strong> EGFR mutation [5,6]. However, <strong>the</strong> EGFR<br />
mutation represents a relatively low percentage <strong>of</strong> total<br />
cases in comparison with o<strong>the</strong>r types <strong>of</strong> adenocarcinoma.<br />
For this patient, comprehensive studies had been<br />
done to exclude various metastatic origins. Ultimately,<br />
she was diagnosed with stage IV primary lung cancer.<br />
Because <strong>of</strong> <strong>the</strong> wild type EGFR sequencing, we chose<br />
paclitaxel (175 mg/m 2 ) plus cisplatin (50 mg/m 2 ) (TC)<br />
as first line chemo<strong>the</strong>rapy. Although <strong>the</strong> patient’s initial<br />
response to this course <strong>of</strong> treatment was good, her<br />
disease progressed after three cycles <strong>of</strong> TC regimen<br />
(Figure 4). The clinical course implied that <strong>the</strong> disease<br />
had aggressive behavior, which <strong>of</strong>ten leads to a poor<br />
prognosis as occurred in this case.<br />
The valuable information we obtained from this<br />
case was that invasive mucinous adenocarcinoma can<br />
have unusual presentation and distinct pathological<br />
features, highlighting <strong>the</strong> importance <strong>of</strong> multidisciplinary<br />
cooperation for accurate diagnosis and treatment.<br />
Although we have found no strong evidence <strong>of</strong> a particularly<br />
efficacious, long-term treatment, we suggest<br />
paclitaxel plus cisplatin as an option for <strong>the</strong> first line<br />
chemo<strong>the</strong>rapy.<br />
REFERENCES<br />
1. Travis WD, Brambilla E, Noguchi M, et al. International<br />
association for <strong>the</strong> study <strong>of</strong> lung cancer/american<br />
thoracic society/european respiratory<br />
society international multidisciplinary classification<br />
<strong>of</strong> lung adenocarcinoma. J Thorac Oncol<br />
6: 244-285, 2011.<br />
2. Morency E, Rodriguez Urrego PA, Szporn AH, et<br />
al. The “drunken honeycomb” feature <strong>of</strong> pulmonary<br />
mucinous adenocarcinoma: a diagnostic pitfall<br />
<strong>of</strong> bronchial brushing cytology. Diagn Cytopathol:<br />
n/a–n/a, 2011.<br />
3. Mazziotta RM, Borczuk AC, Powell CA, et al.<br />
CDX2 immunostaining as a gastrointestinal<br />
marker: expression in lung carcinomas is a potential<br />
pitfall. Appl Immunohistochem Mol Morphol<br />
13: 55-60, 2005.<br />
4. Whitson BA, Groth SS, Andrade RS, et al. <strong>Invasive</strong><br />
adenocarcinoma with bronchoalveolar features:<br />
a population-based evaluation <strong>of</strong> <strong>the</strong> extent<br />
<strong>of</strong> resection in bronchoalveolar cell carcinoma. J<br />
Thorac Cardiovasc Surg 143(3):591-600,2012 .<br />
5. Kitazaki T, Fukuda M, Kohno S, et al. Novel effects<br />
<strong>of</strong> gefitinib on mucin production in bronchioloalvelar<br />
carcinoma; two case reports. <strong>Lung</strong><br />
Cancer 49(1):125-8, 2005.<br />
6. Popat N, Raghavan N, McIvor RA. Severe bronchorrhea<br />
in a patient with bronchioloalveolar carcinoma.<br />
CHEST 141(2): 513-514, 2012.