L8 Ceramics NOTES.pdf
L8 Ceramics NOTES.pdf
L8 Ceramics NOTES.pdf
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
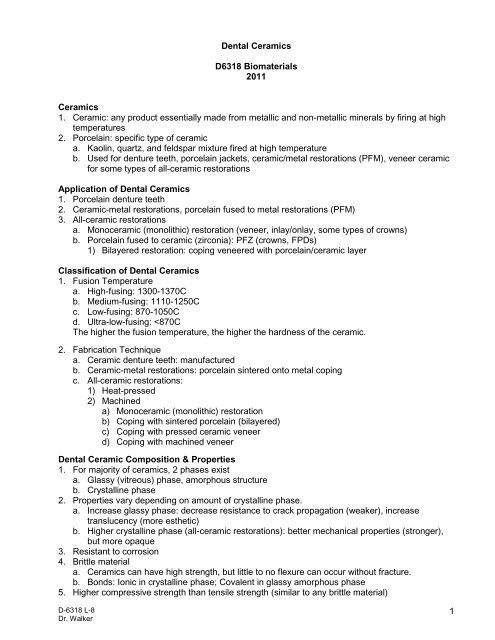
Dental <strong>Ceramics</strong><br />
D6318 Biomaterials<br />
2011<br />
<strong>Ceramics</strong><br />
1. Ceramic: any product essentially made from metallic and non-metallic minerals by firing at high<br />
temperatures<br />
2. Porcelain: specific type of ceramic<br />
a. Kaolin, quartz, and feldspar mixture fired at high temperature<br />
b. Used for denture teeth, porcelain jackets, ceramic/metal restorations (PFM), veneer ceramic<br />
for some types of all-ceramic restorations<br />
Application of Dental <strong>Ceramics</strong><br />
1. Porcelain denture teeth<br />
2. Ceramic-metal restorations, porcelain fused to metal restorations (PFM)<br />
3. All-ceramic restorations<br />
a. Monoceramic (monolithic) restoration (veneer, inlay/onlay, some types of crowns)<br />
b. Porcelain fused to ceramic (zirconia): PFZ (crowns, FPDs)<br />
1) Bilayered restoration: coping veneered with porcelain/ceramic layer<br />
Classification of Dental <strong>Ceramics</strong><br />
1. Fusion Temperature<br />
a. High-fusing: 1300-1370C<br />
b. Medium-fusing: 1110-1250C<br />
c. Low-fusing: 870-1050C<br />
d. Ultra-low-fusing:
Ceramic denture teeth<br />
1. Disadvantages:<br />
a. Higher fracture rate<br />
b. No bond to PMMA denture resin base: Mechanical retention (pegs or holes in teeth)<br />
c. More difficult to adjust<br />
d. Abrade tooth structure and other non-ceramic restorations<br />
2. Advantages<br />
a. Minimal denture tooth wear with max/mand complete denture, as opposed to polymer<br />
denture teeth.<br />
Vertical dimension changes are related to what factors<br />
Historical background ceramic restorations<br />
1. 1900’s, porcelain jackets; Low strength, limited to anterior teeth<br />
2. 1960’s, porcelain fused to metal restorations<br />
a. Higher strength due to metal framework<br />
b. Better match of coefficient of thermal expansion between alloy & ceramic<br />
3. Late 1990’s all-ceramic restorations<br />
a. Glass ceramics (monoceramic-no coping/framework)<br />
b. Porcelain fused to alumina (ceramic coping/framework)<br />
c. Porcelain fused to zirconia (ceramic coping/framework)<br />
<strong>Ceramics</strong> for ceramo-metal restorations (PFM)<br />
1. Low and ultra-low fusing ceramics<br />
a. Melting temperature of the alloy must not be exceeded during ceramic firing process<br />
b. Coefficient of thermal expansion (CTE) of alloy slightly greater than ceramic<br />
c. Ultra-low fusing ceramics are less abrasive than low fusing.<br />
1) Important consideration when ceramic restorations are used in anterior mandible and will<br />
occlude with maxillary natural dentition.<br />
2) In contrast, less of a problem with anterior maxillary restorations, because can have<br />
lingual metal occluding with anterior mandibular natural dentition.<br />
d. UMKC ceramic: Ceramco 3, Low-fusing.<br />
2. Feldspathic dental porcelain<br />
a. Composition: Feldspar 75-85%; Kaolin ~5%; Silica 15%; Metallic Oxides ≤ 3%<br />
b. Powder contains glass components and crystals (leucite)<br />
1) Metallic oxides (pigments/opaquers) added to powder<br />
c. Sintering (Firing)<br />
1) Used in crown/FPD fabrication process; porcelain sintered onto the metal framework<br />
2) Powder particles sintered together to form a continuous mass<br />
a) Glassy matrix with leucite crystals = Porcelain<br />
3) Although porcelain is a glass matrix with crystals, it is not a true “Glass Ceramic”<br />
a) Glass ceramic: during heating process, some glass is converted into crystal.<br />
3. Microstructure feldspathic porcelain<br />
a. Glassy matrix surrounding leucite crystals (10-20% crystalline)<br />
4. Ceramic adhesion to metal<br />
a. Chemical bonding of ceramic metallic oxides with oxides of alloy structure<br />
b. Micro-mechanical interlock<br />
c. Macro-mechanical interlock<br />
D6318 L-8 2
All-ceramic restorations<br />
1. All-ceramic materials<br />
a. Glass ceramics<br />
1) Start with glass to form restoration and crystalline phase forms during processing (heatpressing).<br />
a) Final material has higher crystalline percentage than dental porcelain.<br />
2) Can be monoceramic/monolithic restoration: no separate framework, no porcelain<br />
veneering step<br />
3) Some too opaque and must be veneered with porcelain<br />
b. Glass-infiltrated ceramics<br />
1) Molten glass is infused into porous, crystalline ceramic<br />
2) Higher crystallinity than glass ceramic<br />
3) Serve as a framework that is veneered with porcelain<br />
c. Glass-free, Polycrystalline ceramics<br />
1) 100% crystalline material<br />
2) Framework material that must be veneered with porcelain<br />
2. All-ceramic processing techniques<br />
a. Heat-pressed: Glass ceramics<br />
b. Machined (CAD/CAM):<br />
1) Glass ceramics, Glass-infiltrated ceramics, Polycrystalline (glass-free) ceramics<br />
Current All-Ceramic Systems<br />
1. Heat-pressed all-ceramic restoration<br />
a. Lost-wax technique, injection molding of ceramic<br />
b. Glass ceramics used<br />
1) Leucite-based ceramic<br />
a) 35-55% crystalline (higher crystalline % than feldspathic porcelain,10-20%)<br />
b) Options:<br />
(1) Used alone—monolithic (must be stained)<br />
(2) Veneered with CTE compatible ceramic<br />
c) Examples: Empress (Ivoclar); OPC (Pentron), Cerinate (DenMat)<br />
d) Flexural strength: ~110-140 MPa<br />
e) Applications: Anterior crowns, onlays, inlays, veneers (Single units)<br />
Lumineers (Cerinate, www.cerinate.com)<br />
1. Veneering system which can be fabricated so thin that tooth reduction may not be necessary.<br />
2. 0.3-0.7 mm thick veneers, returned to the dental office etched and ready for bonding to uncut,<br />
etched tooth structure<br />
3. Cerinate porcelain composition is a closely guarded trade secret.<br />
a. Apparently, contains a high proportion of leucite crystalline inclusions<br />
b. Crystals contact each other and form a nearly contiguous internal skeleton to support and<br />
strengthen the surrounding glass matrix<br />
c. Microstructural examination showed leucite crystals clusters (1.5 microns) in Empress.<br />
Cerinate porcelain exhibited a uniform distribution of fine leucite crystals (1 micron).<br />
(Cattell et al 1997)<br />
4. Flexural strength (MPa): Cerinate 110; Empress 135; Feldspathic porcelain 75<br />
2) Lithium disilicate-based ceramic<br />
a) ~60-70% crystalline: stronger, more opaque than leucite-based heat-pressed<br />
b) Examples: IPS e.max (Ivoclar); OPC 3G (Pentron)<br />
c) Options:<br />
(1) Monolithic restoration<br />
(2) Ceramic core with CTE compatible porcelain<br />
d) Flexural strength: 350 MPa<br />
e) Applications: Crowns and FPDs<br />
D6318 L-8 3
2. Machined all-ceramic restoration<br />
a. Computer-aided manufacturing (CAM) (most dental applications use machining process)<br />
Typically linked to computer-aided design (CAD), restoration design<br />
b. Depending on the material and application, can be machined as a monolithic restoration or<br />
as a coping/framework that is veneered with a CTE compatible porcelain<br />
c. In-office CAD/CAM systems, such as CEREC, machined single-unit monolithic/monoceramic<br />
restorations (not crown coping or FPD framework).<br />
d. Only specific materials are appropriate for copings/frameworks with added porcelain layer<br />
(bilayered restorations).<br />
1) Zirconia is commonly used today as framework material, but must be machined with an<br />
in-lab CAM system (not in-office)<br />
2) *Y-TZP = Yttria stabilized-tetragonal zirconia polycrystals<br />
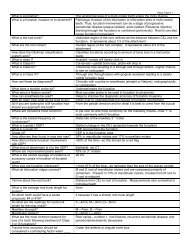
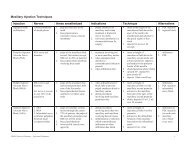
3. All-ceramic materials flexural strength comparisons<br />
Product Material Application Flexural Strength (MPa)<br />
Coping/Framework:<br />
Zirconia (Y-TZP)*<br />
for crowns,<br />
950<br />
(Polycrystalline, Glass-free)<br />
anterior/posterior FPDs<br />
Lava, Cercon,<br />
Procera AllZirkon<br />
e.maxZirCAD<br />
Procera AllCeram<br />
inCoris Al (Cerec)<br />
inCeram Zirconia<br />
e.Max CAD<br />
Empress<br />
Vita Mark II<br />
Alumina<br />
(Polycrystalline, Glass-free)<br />
Alumina/Zirconia<br />
(Glass-infilitrated)<br />
Lithium disilicate<br />
Leucite-based<br />
(Glass ceramic)<br />
Feldspar-based<br />
(Glass ceramic)<br />
Coping/Framework:<br />
for crowns, anterior FPDs<br />
Coping/Framework:<br />
for crowns, post FPDs<br />
Coping/Framework:<br />
for crowns, ant FPDs<br />
OR Crowns, onlays<br />
Restorations: Crowns,<br />
veneers, onlays, inlays<br />
Restorations: Crowns,<br />
veneers, onlays, inlays<br />
650<br />
600<br />
350<br />
150<br />
100<br />
4. Zirconia properties<br />
a. Zirconia = Zirconium dioxide (ZrO 2 ) Key Properties<br />
1) High density, High wear resistance, High fracture toughness, High hardness<br />
b. Ceramic strength differences related to differences in crystallinity. Higher crystallinity, higher<br />
strength. Crystals inhibit crack/fracture propagation. However, with increased strength, also<br />
increased opacity and typically requires a porcelain veneer.<br />
c. Polycrystalline materials exhibit the highest strength. Takes more energy for the<br />
crack/fracture to go around the crystals.<br />
1) Although both alumina and zirconia are polycrystalline higher strength ceramics, zirconia<br />
exhibits the highest fracture resistance, which is related to load-induced phase<br />
transformation. Cracks that might form during loading are closed due to a load-induced<br />
change in the crystalline structure, i.e. smaller crystals become larger with loading and<br />
close the crack. (Rose 1987)<br />
D6318 L-8 4
5. All-ceramic, zirconia-based restoration (PFZ) considerations<br />
a. CAD software: coping/framework is automatically designed to be 0.5 mm thick.<br />
1) However, in situations where excess tooth structure has been lost, a 0.5 mm thick<br />
coping/framework results in thick, unsupported veneer porcelain that is susceptible to<br />
fracture.<br />
2) Most systems have been modified to allow override for coping/framework design.<br />
b. Very thin coping<br />
c. Internal adjustments<br />
6. All-ceramic restoration overview<br />
a. Monoceramic/monolithic restoration (does not include high-strength core/framework)<br />
1) VitaMark II (machined feldspar glass ceramic)<br />
2) Empress (pressed or machined (CAD) leucite glass ceramic)<br />
3) e.max (Press or CAD) lithium disilicate ceramic)<br />
b. Ceramic core veneered with compatible porcelain/ceramic veneer<br />
1) Empress (see above, can also be used as single material)<br />
2) e.max (lithium disilicate glass ceramic)<br />
3) InCeram (machined Glass-infilitrated ceramics)<br />
4) AllCeram (machined Polycrystalline alumina)<br />
5) Lava; Cercon; AllZirkon, e.maxZirCAD (machined polycrystalline zirconia)<br />
Clinical Performance of Ceramo-metal and All-Ceramic Restorations<br />
1. Ceramo-metal crowns and FPD (PFM)<br />
a. High strength; less translucent due to metal coping<br />
b. FPD survival: 96% at 5 yrs, 87% at 10 yrs; 85% at 15 yrs (Walton et al 2002)<br />
c. Failure modes: Tooth fracture, 38%; Perio breakdown, 27%; retention loss, 13%;<br />
caries, 11%. Small percentage, loss of veneer porcelain.<br />
d. When less than optimal occlusal clearance, can modify coping/framework to have partial<br />
metal occlusion.<br />
2. All-ceramic restorations<br />
a. More esthetic<br />
b. Improved strength with newer systems (PFZ)<br />
c. No long-term (>10 yrs) survival studies:<br />
d. Crowns<br />
1) Greatest survival with incisors<br />
2) Decreases progressively to a maximum failure level (fracture) with 2nd molars<br />
3) ProCera AllCeram crowns (6-year study, 60 anterior, 46 posterior crowns):<br />
a) Survival: anterior, 96%; posterior, 91%, does not include fractured posterior crowns<br />
repaired with composite and not replaced (Walter et al 2006)<br />
4) Empress: 95% survival 5-10 years (Update on All-Ceramic Products, JADA supplement Sept 2008)<br />
e. All-ceramic FPD less successful than all-ceramic crowns<br />
1) Empress 2 (e. Max), 30-50% fracture within 2 years (Marquardt & Strub 2006; Taskonak & Sertgoz 2005)<br />
2) InCeram Alumina, 88-90% survival, 3-5 years (vonSteyern et al 2001; Olsson et al 2003)<br />
3) InCeram Zirconia (35%ZrO/65%AlO), 95% survival, 3 yrs (Suarez et al 2004)<br />
4) Lava (PFZ), 100% frame work survival, 3-6 yrs (Dental Advisor 2009-Blackboard)<br />
5) Catastrophic failure mode: fracture at connector<br />
a) Critical factors: material strength and connector size<br />
6) Other failures, porcelain/veneer chipping<br />
D6318 L-8 5
f. All-ceramic FPD failures<br />
1) Posterior FPD require higher strength material<br />
a) Occlusal forces: Anterior 150-300 N vs Posterior 400-800 N<br />
b) Most potential for posterior FPD success: using machined polycrystalline zirconia<br />
framework veneered with compatible ceramic (PFZ)<br />
2) Connector size (height) very critical (height > width)<br />
a) Measure space available from interproximal papilla to incisal edge or marginal ridge<br />
b) Anterior: need 5 mm; Posterior: need 4-5 mm depending on material used<br />
Material<br />
e.Max CAD<br />
InCeram alumina<br />
InCeram zirconia<br />
Procera AllCeram<br />
Application<br />
c) Is there adequate space for the connector Important clinical decision in treatment<br />
planning.<br />
(1) How do you measure the space<br />
(2) Which dimension is more critical<br />
3. Considerations: Zirconia-based restorations<br />
a. Veneer porcelain chipping is a problem with PFZ restorations.<br />
1) Initially used porcelain for PFMs; coefficient of thermal expansion mismatch resulted in<br />
porcelain fracture<br />
2) Porcelain reformulated, specific for ZrO-based restorations (PFZ)<br />
3) Veneer fracture related to CAD software issues<br />
a) Coping/framework automatically designed 0.5 mm thick.<br />
b) Problem if thick unsupported porcelain<br />
c) System override to design as needed<br />
b. Porcelain veneer options for PFZ restorations<br />
1) Powdered, sintered veneer on CAD/CAM ZrO framework<br />
(same porcelain process as PFM)<br />
2) Pressed ceramic veneer on ZrO framework<br />
a) e.max ZirCAD (ZrO): CAD/CAM frame<br />
b) e.max ZirPress: ceramic veneer pressed onto the ZrO frame<br />
3) CAD-on veneer<br />
a) e.max ZirCAD (ZrO): CAD/CAM framework<br />
b) e.max CAD (lithium disilicate): CAD/CAM (machined) ceramic veneer<br />
c) Glass sintering ‘cement’ is used to fuse the framework and the veneer together<br />
c. Despite updates, chipping continues to be a problem with PFZ.<br />
d. PFZ adequate occlusal clearance required<br />
1) Occlusion on ZrO framework not recommended. Why<br />
Connector Dimensions<br />
Occlusal x Buccal<br />
Total area (mm 2 )<br />
(mm)<br />
3-unit Anterior FPD 4-5 x 3-4 12-20<br />
3-unit Posterior FPD<br />
(not adequate esthetics for anterior)<br />
3-unit Anterior FPD<br />
(Maximum 11-mm edentulous space)<br />
4-5 x 3-4 12-20<br />
3 x 3 9<br />
Lava, Cercon<br />
3-unit<br />
3 x 3<br />
9<br />
Procera AllZirkon,<br />
4-unit (2 pontics)<br />
4 x 3 (min)<br />
12 (min)<br />
e.max ZirCAD Anterior or Posterior FPD<br />
Ceramo-metal FPD connectors: Occl/Bucc dimensions, 2.5X2.5 mm=6.25mm 2 (Raigrodski 2004; Ivoclar 2009)<br />
2) With PFM, framework can be in occlusion, if limited occlusal clearance.<br />
e. Full-contour zirconia restorations now available<br />
1) No porcelain veneer (eliminate porcelain chipping problem)<br />
2) ZrO high hardness, concern for wear of opposing dentition<br />
3) Applications: ZrO opposing ZrO restorations; Bruxers (BruxZir Brand)<br />
D6318 L-8 6
All-ceramic crown/abutment preparation (See 3M ESPE LAVA Handout Bb)<br />
1. Anterior: Incisal reduction: 1.5-2.0 mm; Labial/Lingual reduction: 1.0-1.5mm; Chamfer/shoulder<br />
margin: 1.0 mm<br />
2. Posterior: Occlusal reduction: 1.5-2.0 mm; Axial reduction: 1.0-1.5 mm; Chamfer/shoulder<br />
margin: 1.0 mm<br />
All-ceramic restoration cementation procedures<br />
1. Glass and glass-infiltrated ceramics (Ex: VitaMark II, Empress, e.max, InCeram)<br />
a. After restoration fit adjustments, clean internal surface, etch with hydrofluoric acid (HF),<br />
rinse, and place silanating agent<br />
1) Why use HF with these materials What’s etched<br />
b. Conventional resin cement (shades) with dentin bond agent (DBA) (not an adhesive RC)<br />
1) These are typically dual-cure, light-cure initially and any deeper areas will cure over time.<br />
2) Due to restoration translucency, cements with shade options are beneficial especially for<br />
crowns in the anterior/esthestic zone. (High bond strength not a requirement, so<br />
adhesive RCs, which are not as esthetic, not required)<br />
3) Example cement options:<br />
a) Calibra/NT Prime & Bond (Dentsply)<br />
b) Variolink II/Syntac (Ivoclar)<br />
c) RelyX ARC/Single Bond (3M ESPE)<br />
4) RMGI problems with causing fracture of glass/glass infiltrated ceramic restorations<br />
c. Excess cement cleaned, then light cure<br />
d. With lower strength materials, occlusal adjustments after cementation<br />
1) Increased strength from bonding to tooth<br />
2. Polycrystalline Alumina or Zirconia coping/framework restorations (most are PFZ)<br />
(AllCeram, Lava, Cercon, AllZirkon, e.maxZirCAD)<br />
a. After restoration fit adjustments<br />
1) Clean internal surface with phosphoric acid (remove saliva proteins), rinse and dry<br />
2) Dehydrate with isopropyl alcohol, air dry<br />
3) These restorations are NOT etched with HF and silane is NOT used. Why not<br />
b. Cement Options:<br />
1) GI (Ketac), RMGI (RelyX)<br />
2) Adhesive resin cement/ no DBA (Panavia, RelyX Unicem)<br />
a) Adhesive RC will bond to AlO or ZrO.<br />
b) RMGI not cause fracture of high strength polycrystalline coping/framework<br />
Clinical Studies<br />
1. 640 Lava restorations (Dental Advisor 2009-Bb)<br />
a. 42% molars<br />
b. 39% premolars<br />
c. 12% anterior<br />
d. 6% bridges<br />
e. 1% implants<br />
Most cemented with RelyX Unicem cement<br />
2. 100 posterior FPDs (3- or 4-unit), 4-yr study a<br />
(Roediger et al. 2010)<br />
3. 15 posterior FPDs (3- or 4-unit), 51 individual units,<br />
4-yr study b<br />
(Schmitt et al. 2010)<br />
D6318 L-8 7
Reference materials:<br />
Craig’s Restorative Dental Materials, 12 th ed, 2006, Ch 18 <strong>Ceramics</strong><br />
Blackboard Resources:<br />
Lava All-Ceramic System Clinical Preparation, 3M ESPE<br />
Dental Advisor 2009, 3M ESPE Lava Crowns and Bridges 6-year Clinical Performance<br />
Objectives and Study Questions:<br />
1. Know dental ceramic applications.<br />
2. Understand the basic dental ceramic composition and properties.<br />
a. For example,<br />
1) What are the phases present in most ceramics<br />
2) How does the percentage of each phase affect the ceramic properties<br />
3. Be familiar with ceramo-metal porcelains that are less abrasive and situations when those<br />
materials are more appropriate.<br />
4. Understand the differences in crystallinity, strength, and translucency between feldspathic<br />
porcelain, glass ceramics, glass-infiltrated ceramics, and polycrystalline ceramics.<br />
5. Understand the importance of the coefficient of thermal expansion (CTE) for porcelain-fused to<br />
metal (PFM) restorations and porcelain-fused to zirconia restorations (PFZ).<br />
6. Have a basic understanding of the different fabrication techniques for all-ceramic restorations.<br />
7. Compare flexural strength of materials used for PFM and various types of all-ceramic<br />
restorations.<br />
8. Be able to identify which current all-ceramic materials appear to be most appropriate for various<br />
applications.<br />
a. Understand the difference between a monoceramic/monolithic restoration (no porcelain<br />
veneer) and an all-ceramic restoration with a ceramic framework that must be veneered with<br />
porcelain.<br />
b. What materials are appropriate for Single crowns vs FPD applications<br />
c. Which material appears to be most appropriate for posterior FPD use<br />
d. What are common complications associated with all-ceramic restorations<br />
1) Understand why despite using high strength zirconia as a coping or framework for allceramic<br />
crowns or FPDs, the CAD-CAM restorations can be susceptible to veneer<br />
ceramic fracture.<br />
9. Discuss advantages and disadvantages of ceramo-metal versus all-ceramic FPDs.<br />
a. What are differences related to occlusal clearance between preparation and opposing<br />
dentition and restoration occlusion for PFM and PFZ<br />
b. Zirconia restorations with no porcelain veneer are now available. What potential problem<br />
could occur when these restorations oppose natural dentition or other non-zirconia<br />
materials Why For what applications could these restorations be considered<br />
c. Besides using high strength material, what is the most critical fabrication factor for allceramic<br />
FPD success How does this differ from a ceramo-metal FPD How is this factor<br />
evaluated<br />
10. Be familiar with cements and procedures for the different types of all-ceramic materials.<br />
a. Which materials should be etched with hydrofluoric acid (HF) and silanated<br />
1) Understand what component can be etched.<br />
b. Which materials are not HF etched and why not<br />
D6318 L-8 8