Your Baby's Birth - Pregnancy & Childbirth Home
Your Baby's Birth - Pregnancy & Childbirth Home
Your Baby's Birth - Pregnancy & Childbirth Home
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Congratulations!<br />
It is wonderful that you are expecting a child and have decided to<br />
share this special experience with us. Our doctors, nurses<br />
and staff look forward to caring for you and making your upcoming<br />
hospital stay very comfortable and pleasant.<br />
<strong>Your</strong> Baby’s <strong>Birth</strong> is designed to help you and your family prepare for the birth of your child. We<br />
have included tips on how you can stay healthy, what items you may need for your nursery, signs<br />
of labor and how families can make the most of this wonderful event. To help you through your<br />
pregnancy, we have divided the information into four chapters: “All the Help You Need;” “You and<br />
<strong>Your</strong> Baby’s Health;” “<strong>Your</strong> Hospital Stay;” and “<strong>Your</strong> Going <strong>Home</strong> Guide.”<br />
<strong>Your</strong> Baby’s <strong>Birth</strong> is yours to keep and can be a helpful way to organize the information most new<br />
parents gather when preparing for a child. Remember to bring <strong>Your</strong> Baby’s <strong>Birth</strong> with you to your<br />
childbirth education classes and the hospital to add information that you may receive.<br />
<strong>Your</strong> Baby’s <strong>Birth</strong> is not meant to replace the advice of a healthcare provider. We are always<br />
available to help, so please call us with your questions. Turn to the section “All the Help You Need”<br />
for important phone numbers.<br />
The birth of a baby is a special event. At PinnacleHealth we have a team of dedicated healthcare<br />
professionals who specialize in the care of mothers and babies. Our team includes nurses,<br />
obstetricians, midwives, perinatologists, pediatricians,<br />
neonatologists, social workers, childbirth educators, lactation<br />
consultants and Nursing Mothers Counselors to care for<br />
you and your baby. Together, we are committed to<br />
making your pregnancy and birth the positive<br />
experience we believe every birth should be.<br />
Again, thank you for allowing PinnacleHealth<br />
WomanCare at Harrisburg Campus to be a<br />
part of this special time in your life.<br />
1<br />
Y O U R B A B Y ’ S B I R T H
2<br />
Y O U R B A B Y ’ S B I R T H
You and <strong>Your</strong> Baby’s Health
You and <strong>Your</strong> Baby’s Health<br />
You are responsible for your baby’s health and nutrition, right from the start. Here are some topics<br />
you should think about now that you are pregnant.<br />
<strong>Your</strong> growing body and baby<br />
MONTH 1<br />
<strong>Your</strong> Baby<br />
• Tiny limb buds, which will grow into arms<br />
and legs, appear.<br />
• The heart and lungs begin to form. By the<br />
22nd day, the heart starts to beat.<br />
• The neural tube, which becomes the brain<br />
and spinal cord, begins to form.<br />
• At the end of the first month, your baby is<br />
about 1/4 inch long.<br />
<strong>Your</strong> Body<br />
• <strong>Your</strong> body is making lots of hormones needed<br />
to grow a baby.<br />
• <strong>Your</strong> breasts are slightly bigger and sore and<br />
may tingle.<br />
• You may have morning sickness. Try eating<br />
crackers.<br />
• You may crave some foods or hate foods you<br />
usually like.<br />
Prenatal Care Guide<br />
• Visit your healthcare provider for your first<br />
prenatal care checkup as soon as you think<br />
you are pregnant.<br />
• Take a multivitamin with at least 400<br />
micrograms of the B vitamin folic acid every<br />
day to help reduce the risk of birth defects<br />
of the brain and spinal cord.<br />
• Ask your healthcare provider before taking<br />
any prescription drugs, over-the-counter<br />
products or herbal products.<br />
• Stop smoking, drinking alcohol and taking<br />
street drugs.<br />
Body before pregnancy<br />
3<br />
Y O U R B A B Y ’ S B I R T H
MONTH 2<br />
<strong>Your</strong> Baby<br />
• All major body organs and systems are formed<br />
but not completely developed.<br />
• Early stages of the placenta, which exchanges<br />
nutrients from your body for waste products<br />
produced by the baby, are visible and working.<br />
• Ears, ankles and wrists are formed. Eyelids<br />
form and grow but are sealed shut.<br />
• Fingers and toes are developed.<br />
• By the end of the second month, your baby<br />
is about 1 inch long and still weighs less than<br />
1/3 ounce.<br />
<strong>Your</strong> Body<br />
• <strong>Your</strong> breasts are still sore and are enlarging;<br />
your nipples and the area around them begin<br />
to darken.<br />
• You will urinate more often because your<br />
growing uterus is pressing on your bladder.<br />
• Morning sickness may continue.<br />
• You may feel tired and need to rest more as<br />
your body adjusts to being pregnant.<br />
• The total amount of blood in your body<br />
increases.<br />
Prenatal Care Guide<br />
• Visit your healthcare provider for one prenatal<br />
care checkup.<br />
• Eat a variety of healthy foods from the five<br />
major food groups: grains; fruit; vegetables;<br />
dairy products; and meats and proteins.<br />
• <strong>Your</strong> healthcare provider probably will<br />
prescribe prenatal vitamins. <strong>Your</strong> prenatal<br />
vitamin should contain at least 400<br />
micrograms of folic acid.<br />
• Drink at least six to eight glasses of water,<br />
juice or milk every day.<br />
• Do not smoke, drink alcohol or take street<br />
drugs.<br />
MONTH 3<br />
<strong>Your</strong> Baby<br />
• Fingers and toes have soft nails.<br />
• The mouth has 20 buds that will become baby<br />
teeth.<br />
• Fine hairs begin to form on the baby’s skin.<br />
• You can hear your baby’s heartbeat for the first<br />
time (10 to 12 weeks) using a special<br />
instrument called a doptone.<br />
• For the rest of pregnancy, all body organs will<br />
mature and the baby will gain weight.<br />
• By end of this month, the baby is about 2 1/2 to<br />
3 inches long and weighs about 1 ounce.<br />
<strong>Your</strong> Body<br />
• You may still feel tired and have morning<br />
sickness.<br />
• You may have headaches and get lightheaded<br />
or dizzy. If these symptoms persist or are<br />
severe, tell your healthcare provider.<br />
• <strong>Your</strong> clothes may begin to feel tight around<br />
your waist and breasts. Try pullover tops and<br />
skirts or pants with elastic waists.<br />
6 & 7 weeks pregnant<br />
4<br />
Y O U R B A B Y ’ S B I R T H
MONTH 4<br />
<strong>Your</strong> Baby<br />
• The baby moves, kicks and swallows.<br />
• The skin is pink and transparent.<br />
• The umbilical cord continues to carry<br />
nourishment from mother to baby—but it also<br />
can pass along hazards like alcohol, nicotine<br />
and other drugs.<br />
• By the end of the fourth month, your baby is 6<br />
to 7 inches long and weighs about 4 to 5<br />
ounces.<br />
12 weeks pregnant<br />
Prenatal Care Guide<br />
• Visit your healthcare provider for one prenatal<br />
checkup.<br />
• You have a slightly increased need for almost<br />
all vitamins and minerals to nourish your baby.<br />
A healthy diet helps to meet these needs.<br />
• You may have gained 2 to 4 pounds by now. A<br />
woman who starts pregnancy at a normal<br />
weight should gain 25 to 35 pounds during<br />
pregnancy. Ask your healthcare provider how<br />
much weight you should gain.<br />
• Exercise can be beneficial. Walking is a good<br />
choice. Check with your healthcare provider<br />
before starting an exercise program.<br />
• If your healthcare provider recommends<br />
prenatal testing using chorionic villus<br />
sampling (CVS), you can have the test now.<br />
• Do not smoke, drink alcohol or take street<br />
drugs.<br />
<strong>Your</strong> Body<br />
• <strong>Your</strong> appetite increases as morning sickness<br />
goes away. You should begin to feel more<br />
energetic.<br />
• Toward the end of the fourth month (16 to 20<br />
weeks), you might feel your baby move for the<br />
first time; tell your healthcare provider.<br />
• <strong>Your</strong> belly begins to show—you probably will<br />
need maternity clothes and bigger bras now.<br />
Prenatal Care Guide<br />
• Visit your healthcare provider for one prenatal<br />
care checkup.<br />
• Pregnant women need extra iron—more than<br />
even a good diet can supply. <strong>Your</strong> doctor may<br />
recommend iron supplements.<br />
• You’ll probably gain about a pound a week, or<br />
12 to 14 pounds, during the second trimester<br />
(months 4 to 6).<br />
• Do not smoke, drink alcohol or take street<br />
drugs.<br />
• If your healthcare provider recommends<br />
prenatal testing using amniocentesis or a<br />
blood test called a triple screen for Down<br />
syndrome and neural tube defects, you can<br />
have them at 15 to 18 weeks.<br />
5<br />
Y O U R B A B Y ’ S B I R T H
MONTH 5<br />
<strong>Your</strong> Baby<br />
• The baby becomes more active, turning from<br />
side to side and sometimes head over heels.<br />
• Finger and toe prints can be seen.<br />
• The baby sleeps and wakes at regular<br />
intervals.<br />
• This is a month of rapid growth. At the end of<br />
the fifth month, your baby is about 10 inches<br />
long and weighs 1/2 to 1 pound.<br />
<strong>Your</strong> Body<br />
• If you haven't already, you will begin to feel<br />
your baby moving. Tell your healthcare<br />
provider.<br />
• <strong>Your</strong> uterus has grown to the height of your<br />
belly button.<br />
• <strong>Your</strong> heart beats faster.<br />
• You may need eight or more hours of sleep<br />
each night. During the day, take rest breaks if<br />
tired. Don't push yourself.<br />
Prenatal Care Guide<br />
• Visit your healthcare provider for one prenatal<br />
care checkup.<br />
• <strong>Your</strong> baby's growth and weight gain can be<br />
affected if you're smoking, drinking or taking<br />
drugs. It's never too late to quit.<br />
• Eat a healthy, nutritious diet and drink lots of<br />
juice, water and milk every day.<br />
• Do not smoke, drink alcohol or take street<br />
drugs.<br />
MONTH 6<br />
<strong>Your</strong> Baby<br />
• The skin is red and wrinkled and covered with<br />
fine, soft hair.<br />
• Eyelids begin to part and the eyes open.<br />
• The baby continues to grow rapidly. At end of<br />
the sixth month, the baby is about 12 inches<br />
long and weighs 1-1/2 to 2 pounds.<br />
<strong>Your</strong> Body<br />
• You may feel the baby kicking strongly now.<br />
• The skin on your growing belly may start to<br />
itch.<br />
• <strong>Your</strong> back may hurt. Wear low-heeled shoes or<br />
flats. Don’t stand for long periods of time.<br />
Exercise can help. You may feel pain down the<br />
sides of your belly as your uterus stretches the<br />
ligaments that support it.<br />
Prenatal Care Guide<br />
• Visit your healthcare provider for one prenatal<br />
care checkup.<br />
• You may be constipated. Drink more water or<br />
fruit juice, eat more foods with fiber (like<br />
fruits and vegetables) and get some exercise<br />
(with your healthcare provider's approval).<br />
• To help with heartburn, try eating four or five<br />
smaller meals during the day.<br />
• Do not take laxatives or antacids without<br />
asking your healthcare provider.<br />
• Do not smoke, drink alcohol or take street<br />
drugs.<br />
20 weeks pregnant<br />
6<br />
Y O U R B A B Y ’ S B I R T H
MONTH 7<br />
<strong>Your</strong> Baby<br />
• The baby can open and close her eyes and<br />
suck her thumb.<br />
• The baby exercises by kicking and stretching.<br />
• The baby responds to light and sound.<br />
• The baby is now about 15 to 16 inches long<br />
and weighs about 2-1/2 to 3 pounds.<br />
<strong>Your</strong> Body<br />
• If your ankles and feet swell from standing, lie<br />
down with your feet raised. If your hands<br />
and face swell suddenly, call your healthcare<br />
provider.<br />
• Stretch marks may appear on the abdomen<br />
and breasts as they get bigger.<br />
• You may have contractions. This is normal, but<br />
call your healthcare provider if you have more<br />
than five contractions in one hour.<br />
• As your belly gets bigger, you may lose your<br />
sense of balance. This makes it easier to fall.<br />
Be careful!<br />
Prenatal Care Guide<br />
• After the 28th week, visit your healthcare<br />
provider every two weeks for prenatal care.<br />
• Eat a variety of foods that are good for you.<br />
You should gain 1 pound a week this month.<br />
• Get plenty of rest—your body is working hard.<br />
• Do not smoke, drink alcohol or take street<br />
drugs.<br />
• Start childbirth education classes if you<br />
haven't already done so.<br />
• Most healthcare providers do a blood test for<br />
gestational diabetes (diabetes during<br />
pregnancy) at 24 to 28 weeks.<br />
28 weeks pregnant<br />
7<br />
Y O U R B A B Y ’ S B I R T H
MONTH 8<br />
<strong>Your</strong> Baby<br />
• Rapid brain growth continues.<br />
• The baby is too big to move around much, but<br />
he can kick strongly and roll around.<br />
• You may notice the shape of an elbow or heel<br />
against your abdomen.<br />
• Bones of the head are soft and flexible to<br />
make it easier for the baby to fit through the<br />
birth canal.<br />
• Fingernails have grown to tips of fingers.<br />
• Lungs may still be immature.<br />
• <strong>Your</strong> baby is now about 18 to 19 inches long<br />
and weighs about 4 to 5 pounds.<br />
• Call your healthcare provider right away if<br />
you have:<br />
- Bleeding or a gush of fluid from your vagina<br />
- Cramps, stomach pains or a dull backache<br />
- Blurry vision, or spots before your eyes<br />
- A feeling that the baby is pushing down<br />
- A noticeable decrease in the baby’s<br />
movements<br />
- More than five contractions in one hour<br />
<strong>Your</strong> Body<br />
• You may feel stronger contractions this month.<br />
• You may have some leakage of colostrum<br />
(the fluid that will feed your baby until your<br />
milk comes in) from your breasts.<br />
• You may have trouble sleeping because it is<br />
hard to get comfortable. Try putting several<br />
pillows under your head.<br />
• You may have shortness of breath as the baby<br />
crowds your lungs.<br />
• The baby may crowd your stomach. Try eating<br />
five or six smaller meals during the day.<br />
• The top of your uterus lies just under your rib<br />
cage.<br />
Prenatal Care Guide<br />
• Visit your healthcare provider every two weeks<br />
for prenatal care checkups.<br />
• You should gain 1 pound a week this month.<br />
• Do not smoke, drink alcohol or take street<br />
drugs.<br />
36 weeks pregnant<br />
8<br />
Y O U R B A B Y ’ S B I R T H
MONTH 9<br />
<strong>Your</strong> Baby<br />
• At 37 to 40 weeks, your baby is full term.<br />
• The baby’s lungs are mature and ready to<br />
function on their own.<br />
• The baby gains about 1/2 pound a week.<br />
• The baby usually drops into a head-down<br />
position and rests lower in your abdomen.<br />
• By the end of the ninth month, the baby is 19<br />
to 21 inches long and weighs 6 to 9 pounds.<br />
<strong>Your</strong> Body<br />
• <strong>Your</strong> belly button may stick out.<br />
• <strong>Your</strong> breathing should be easier once the baby<br />
drops, but you’ll have to urinate more often<br />
because the baby is pressing on your bladder.<br />
• Swelling of ankles and feet may increase.<br />
• <strong>Your</strong> cervix will open up (dilate) and thin out<br />
(efface) as it prepares for birth.<br />
• You may be uncomfortable because of the<br />
pressure and weight of the baby. Rest often.<br />
Prenatal Care Guide<br />
• After the 36th week, visit your healthcare<br />
provider once a week for prenatal care<br />
checkups.<br />
• You may not gain any weight at all this month;<br />
you may even lose 1 or 2 pounds.<br />
• Do not smoke, drink alcohol or take street<br />
drugs.<br />
• Decide if you are going to breastfeed or<br />
formula-feed your baby.<br />
• Time your contractions. You are in labor if your<br />
contractions:<br />
- Are regular or evenly spaced apart (every<br />
seven minutes, for example)<br />
- Happen more than five times an hour<br />
- Last for 30 to 70 seconds<br />
- Get worse as you move around<br />
- Call your healthcare provider if you think you<br />
are in labor.<br />
*Information and photos provided by the March of Dimes<br />
and <strong>Childbirth</strong> Connection<br />
40 weeks pregnant<br />
9<br />
Y O U R B A B Y ’ S B I R T H
10<br />
Y O U R B A B Y ’ S B I R T H
Early <strong>Pregnancy</strong><br />
Prenatal Tests<br />
As part of your healthcare, your physician, nurse practitioner or midwife will order a number of tests.<br />
Some tests are routine for all expectant mothers; others are ordered in selected cases. <strong>Your</strong><br />
physician, nurse practitioner or midwife can provide you with more information regarding these<br />
tests or the results of your tests.<br />
Common Tests for <strong>Your</strong> First Visit<br />
• Blood Tests:<br />
- Blood Type (A, B, O), and antibody screen Rh; to identify possible problems between<br />
mother and baby with different blood sugar types or antibody screens.<br />
- Iron Level: screen for low iron in blood.<br />
- Rubella Immunity (German Measles): prevent birth defects from rubella exposure.<br />
- HIV: If you are HIV positive, medication can be given to decrease the chance of the virus<br />
being passed to the baby.<br />
- Hepatitis B and Hepatitis C testing<br />
- Sickle Cell Trait<br />
• Sexually Transmitted Diseases (chlamydia, syphilis, gonorrhea, trich or bacterial vaginosis) —<br />
If you have a sexually transmitted disease, medication can be given to decrease the chance of the<br />
diseases being passed to the baby.<br />
• Urine Tests (tested throughout pregnancy): detects protein in the urine to screen for<br />
preeclampsia.<br />
• Culture and Sensitivity (C&S): to check for bacteria in the urinary tract.<br />
• Pelvic Exam: to measure the pelvic size and detect infections or certain problems.<br />
• Cervical Tests:<br />
- Pap Smear: checks for signs of cervical cancer.<br />
- Culture: screens for sexually transmitted disease.<br />
• Blood Pressure: a baseline will be obtained to watch for changes as the pregnancy progresses.<br />
• Body Mass Index (BMI): A standard for determining obesity using your weight and height.<br />
A BMI between 19 and 29 is ideal. If your BMI is less than 19, you may meet with a dietitian for<br />
teaching and meal planning. If your BMI is over 30, you may meet with a dietitian and have<br />
additional testing for diabetes and the well-being of your baby.<br />
11<br />
Y O U R B A B Y ’ S B I R T H
Tests for Later in the <strong>Pregnancy</strong><br />
• Ultrasound: Some physicians routinely order ultrasound; others use it as needed. Ultrasound can<br />
be done to determine:<br />
- Due date: This test can be performed as early as the 5th week<br />
- Baby’s size<br />
- Number of babies in the uterus<br />
- Certain birth defects<br />
- Fetal well-being<br />
• Blood Glucose Tests: to determine the amount of sugar in the blood. A routine test is done<br />
between 24 and 28 weeks. Screens for gestational (pregnancy) diabetes. If positive, dietary<br />
changes can be started to reduce the complications of diabetes.<br />
• Alpha Feto Protein: screens for spina bifida or other problems with the baby’s brain or spine.<br />
Results are sometimes inconclusive.<br />
• Quad Marker Screen: measures alpha feto protein (above) and two other hormones (estriol and<br />
HCG) at 15-20 weeks. Screens for the possibility of genetic disorders, such as spina bifida or<br />
Down’s syndrome.<br />
• Amniocentesis*: tests for genetic disorders. This is often done between the 15th and 18th<br />
week but can be done earlier. Amniotic fluid around the baby is withdrawn by a needle. This can<br />
also be used to determine if baby’s lungs are mature in the third trimester.<br />
• Beta Strep Test: a culture of the vagina done to detect beta strep bacteria. Many providers test<br />
for beta strep in the last month of pregnancy and give antibiotics if the test is positive. All<br />
mothers with a positive test will receive antibiotics through an IV line during labor.<br />
*Other tests for fetal well-being that may be done in the last trimester are described later in this<br />
section (“Later <strong>Pregnancy</strong>”).<br />
Warning Signs<br />
The following warning signs may indicate that there is a problem. Contact your healthcare provider<br />
immediately if you experience any of these:<br />
• Vaginal bleeding<br />
• Fluid leaking from the vagina<br />
• Severe headache or problems with your vision<br />
• Decrease in baby’s movements once they have been felt<br />
• No fetal movement felt by 22 weeks<br />
• Vaginal itching or burning<br />
• Weight gain of more than one pound per day<br />
Also look under “Premature Labor” later in this chapter.<br />
12<br />
Y O U R B A B Y ’ S B I R T H
Exercise and <strong>Pregnancy</strong><br />
Exercise helps the muscles, joints, heart and lungs meet the changes of pregnancy. In addition,<br />
keeping physically fit helps the mother feel good about herself and her pregnancy. Exercise is great<br />
for you and the baby. It increases your strength and energy, feels good physically, relieves stress<br />
and decreases joint pain.<br />
There are a few important guidelines to follow when beginning an exercise program while<br />
pregnant.<br />
• Talk with your healthcare provider before beginning any new exercise program. There are a few<br />
high-risk situations in which your healthcare provider may advise against exercise.<br />
• Exercise at least three times a week or every other day.<br />
• Warm up for at least five minutes before exercising.<br />
• Drink plenty of liquids before, during and after exercise. A simple rule to follow is to drink a glass<br />
of water for every half-hour of strenuous activity and drink more during warmer weather.<br />
• Eat a light snack about an hour before you exercise.<br />
• Dress appropriately: loose, stretchy clothes, supportive shoes and a supportive bra.<br />
• <strong>Your</strong> heartbeat should not exceed 140 beats/minute.<br />
• Never exercise until the point of exhaustion, always keep your workout at a mild to moderate pace.<br />
• Avoid jerky, bouncy movements and be sure to exercise on a wooden floor or tightly carpeted<br />
surface to reduce shock and provide better footing.<br />
• Listen to your body. Stop exercising if you have pain, cramps, dizziness, racing heartbeat,<br />
breathlessness, difficulty walking, headache or increased swelling.<br />
Massage During <strong>Pregnancy</strong><br />
Massage during pregnancy helps to relieve symptoms of many of the uncomfortable conditions<br />
caused by pregnancy. The overall goals for pregnancy massage are to help minimize stress, promote<br />
relaxation, and prepare the muscles for childbirth. In addition, there are specific techniques and<br />
movements which are designed to help relieve particular conditions, including: low back pain,<br />
swelling of hands and feet, headaches, calf cramps, insomnia, sciatic pain and sinus congestion.<br />
Massage can also help to restore your muscles after delivery.<br />
In most instances, pregnancy massage can be received safely. At times, there are reasons not to<br />
receive massage or precautions that your massage therapists should take. Talk with your<br />
healthcare provider before getting a pregnancy massage. Do not get a massage if you have the<br />
following: heavy vaginal discharge, pre-eclampsia, diabetes, high blood pressure, contagious<br />
illness, morning sickness, fever, abdominal pain, vomiting and/or diarrhea, any malignant condition<br />
or unusual pain.<br />
13<br />
Y O U R B A B Y ’ S B I R T H
Working and <strong>Pregnancy</strong><br />
Evaluate any hazards you may be exposed to at your job, including X-rays, lead, lifting heavy objects<br />
or exposure to chemicals.<br />
Tips for working during pregnancy:<br />
• Alternate sitting and standing every half-hour. Either sitting or standing for long periods of time<br />
will cause soreness and increased swelling in your legs.<br />
• When sitting, make sure your chair is the correct height for your legs, so that your feet rest<br />
on the floor.<br />
• When standing for a while, stand with one foot on a ledge or a small box so one foot is higher than<br />
the other and alternate your feet.<br />
• Stretching occasionally helps to relieve stiffness in muscles and joints.<br />
• Most jobs are safe to continue until the birth of your baby. Some mothers may be advised by<br />
their healthcare provider to discontinue work if they develop high blood pressure, risk of premature<br />
labor or other complications.<br />
Sex and <strong>Pregnancy</strong><br />
Sexual intimacy is important to your relationship throughout the pregnancy. <strong>Pregnancy</strong> is a good time<br />
to find new ways of giving pleasure to each other. Many couples enjoy cuddling, fondling and trying<br />
new positions as the abdomen enlarges. Sexual intercourse is safe throughout pregnancy UNLESS you<br />
experience any of the following:<br />
• Bleeding from the vagina<br />
• Clear fluid from the vagina (indicates the bag of water has broken)<br />
• High risk for premature labor (more than four contractions in one hour before 37 weeks)<br />
• Placenta previa or low-lying placenta (afterbirth partially or completely covers the opening<br />
of the cervix)<br />
• <strong>Your</strong> physician or midwife advises against sexual intercourse<br />
14<br />
Y O U R B A B Y ’ S B I R T H
Nutrition and <strong>Pregnancy</strong><br />
Eating for a Healthy Baby<br />
Good nutrition during pregnancy and breastfeeding is important for the growth and development<br />
of your baby as well as for your own health. By making wise choices about what you eat during<br />
pregnancy, you can improve your chance of having a healthy baby and healthy pregnancy.<br />
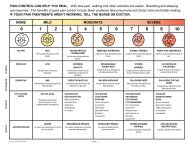
What Counts As One Serving<br />
Grains & Cereals Vegetable Fruit Dairy Protein Fluid<br />
6-11 servings 3-5 servings 2-4 servings 4-6 servings 2-3 servings 8-10 cups<br />
Make at least half Include dark green, Make most Choose low fat Choose lean meat<br />
your choices whole orange and starchy choices fresh, or fat free most and poultry.<br />
grain. vegetables. frozen or canned often. Include nuts, fish<br />
without sugar.<br />
and beans.<br />
1 slice bread 1 cup raw, l medium l cup milk or 2-3 ounces l cup water,<br />
leafy vegetables piece of fruit yogurt cooked lean mineral water,<br />
meat, poultry diluted juice,<br />
¾ cup cereal or fish lemonade<br />
½ cup cooked ½ cup other ½ cup canned 1 ½ ounces 1 cup cooked,<br />
cereal vegetables cooked fruit cheese dry beans<br />
or chopped raw<br />
½ cup cooked 1 cup chopped 1 ½ cup soup<br />
rice or pasta raw fruit made with milk<br />
6 crackers ½ baked potato ¼ cup dried fruit 2 eggs<br />
1 tortilla 2 Tbsp. peanut butter<br />
or 1/3 cup nuts = 1 oz. meat<br />
15<br />
Y O U R B A B Y ’ S B I R T H
Weight Gain<br />
The amount of weight you should gain during your pregnancy to have a healthy baby depends<br />
on your pre-pregnancy weight. If you are at a normal weight before pregnancy you should gain<br />
25-35 pounds; underweight before pregnancy should gain 28-40 pounds; and overweight<br />
before pregnancy should gain 15-25 pounds. Most of the weight should be gained in the second<br />
and third trimesters. Eating about 300 calories more than your usual intake in the last trimesters<br />
should allow gradual weight gain.<br />
If you are gaining too much weight, here are some ways to cut back on calories without<br />
decreasing your intake of vitamins and minerals:<br />
• Do not skip meals.<br />
• Use low-fat dairy products like skim or low-fat yogurt and cottage cheese.<br />
• Substitute water for sodas or other sweetened drinks and juices.<br />
• Trim fat from meat before cooking. Drain off fat after cooking.<br />
• Bake, broil, roast and stew meats and other foods. Limit frying.<br />
• Limit chips, cookies, cake, pastry and candy.<br />
• Decrease the amount of butter, margarine, oil, cream cheese, sour cream, salad dressing and<br />
cream sauce.<br />
• When eating out at a fast food restaurant, choose salads, small sandwiches, baked potatoes and<br />
low-fat milk.<br />
If you are not gaining enough weight, here are some strategies to increase your calories<br />
and nutritional intake:<br />
• Eat small, more frequent meals throughout the day.<br />
• Decrease liquids taken with meals, which make you feel full<br />
more rapidly.<br />
• Add margarine or butter to vegetables and potatoes.<br />
• Use whole milk, ice cream and cheese.<br />
• Drink high-calorie drinks during the day like milkshakes,<br />
Carnation Instant Breakfast, hot chocolate or chocolate milk.<br />
• Use margarine, butter, mayonnaise, sour cream, cream cheese,<br />
oil, salad dressing, gravy, cream sauce and cream soup.<br />
16<br />
Y O U R B A B Y ’ S B I R T H
Protecting <strong>Your</strong> Baby<br />
Prenatal Supplements<br />
<strong>Your</strong> diet may not meet the increased vitamin and mineral needs of pregnancy, especially if you are<br />
not eating a variety of foods from the food guide pyramid. A prenatal vitamin supplement including<br />
folic acid is usually recommended. Folic acid before and during pregnancy helps reduce the risk of<br />
neural tube defects (brain and spine). Iron supplements are sometimes needed to prevent anemia.<br />
Remember, supplements do not replace eating a healthy diet.<br />
Alcohol<br />
Just like smoking or street drugs, alcohol can cause serious birth defects in your child if you drink<br />
while you are pregnant. Fetal Alcohol Spectrum Disorder (FASD) is a permanent condition that<br />
results in brain damage and physical abnormalities. Alcohol is NOT safe during pregnancy.<br />
Artificial Sweeteners<br />
During pregnancy, the best sweeteners are natural and nutritious fruits and fruit juices. Saccarine<br />
(Sweet’n’Low) is not recommended during pregnancy, and aspartame (Equal, Nutrasweet) and<br />
sucralose (Splenda) should only be consumed in limited amounts.<br />
Caffeine<br />
Beverages such as coffee, tea, chocolate and cola contain caffeine, which passes into the placenta<br />
and enters your baby’s circulation. A cup or two a day of caffeinated beverages shouldn’t be a<br />
problem, but if you can, cutting out caffeine makes for a healthier diet.<br />
Cats and Kitty Litter<br />
Cats may carry a harmful infection called toxoplasmosis that may harm your baby. Wash your<br />
hands after handling cats and have someone else change the kitty litter.<br />
Dieting<br />
In short, don’t diet. You should never try to lose weight once you are pregnant, no matter what your<br />
weight was before you became pregnant.<br />
Hair Color and Other Chemical Treatments<br />
Avoid use of chemicals on your body, especially in the first trimester of pregnancy. If you color,<br />
straighten, or perm your hair, discuss your concerns with your healthcare provider and hair stylist.<br />
Hot Tubs/Saunas/Tanning Beds<br />
Raising the mother’s body temperature even a small amount increases the risk of damage to the<br />
baby’s nervous system. Don’t use hot tubs, saunas or tanning beds until your care provider tells<br />
you it is safe.<br />
Lead<br />
Lead can be found in water in lead pipes and old paint in older homes. Lead poisoning can cause<br />
brain damage and learning problems.<br />
Medications<br />
Do not take any over-the-counter or prescription medications while you are pregnant without<br />
talking to your healthcare provider. <strong>Your</strong> doctor can provide you with a list of safe, over-the-counter<br />
medications.<br />
RhoGam<br />
When a mother’s blood is Rh negative, a medicine needs to be given to prevent blood problems<br />
with your baby both in this pregnancy and any future pregnancies.<br />
17<br />
Y O U R B A B Y ’ S B I R T H
Smoking<br />
Smoking during pregnancy is hazardous to the health of your baby. It can cause many birth<br />
defects, low birth weight infants, increased miscarriage, stillbirth and sudden infant death<br />
syndrome. Give your baby the best possible start and quit! For more information on smoking<br />
cessation, visit www.pinnaclehealth.org or call the PA Quitline at 1-877-724-1090.<br />
Street Drugs<br />
Street drugs can cause serious birth defects, premature birth or sick infants. Street drugs can also<br />
cause the baby to be stillborn (born dead), or to die after birth.<br />
Unprotected Sex<br />
Unprotected sex can lead to sexually transmitted diseases that can be passed to the baby. Latex<br />
condoms help prevent transmission of STDs.<br />
Vaccines<br />
A vaccine to prevent influenza (flu) can be taken during pregnancy. Vaccines to prevent measles,<br />
mumps, rubella, hepatitis, chickenpox and pertusses (TDAP), can be taken either before or after<br />
pregnancy.<br />
Viral Infections<br />
Exposure to some viral infections can harm your baby. Some infections can be prevented by<br />
vaccination. Please call your healthcare provider if you have symptoms or exposure to any of the<br />
following infections: Rubella, chickenpox, Hepatitis A, B or C, CMV, Herpes and/or HIV.<br />
Common Discomforts<br />
In addition to the joys of pregnancy, many women experience common complaints. Below are some<br />
common discomforts and ways that may help you feel better.<br />
Backache<br />
Lower back muscle strain is brought on by changes in how you sit and stand. Exercising, wearing<br />
supportive shoes with low heels and supportive panty hose, maintaining good posture, applying<br />
moist heat, and receiving back rubs may help you to feel better.<br />
Bleeding Gums<br />
An increase in your body’s hormones may cause tenderness and bleeding of your gums. Eat foods<br />
high in vitamin C, use an antiseptic mouthwash, and be sure to brush and floss your teeth every<br />
day to help maintain good dental health. Visit your dentist regularly.<br />
Breast Changes<br />
As your breasts get bigger, they may be tender and sensitive. To help ease overall discomfort, wear<br />
a supportive cotton bra or a maternity/nursing bra. As your pregnancy progresses, you may begin<br />
to leak colostrum or pre-milk. If this becomes a problem, tuck a handkerchief or gauze pad into<br />
each bra cup.<br />
Constipation<br />
To avoid or relieve constipation, increase the fiber in your diet by eating more fresh fruits,<br />
vegetables, beans, whole grains, high fiber cereal and drink plenty of water or juice. Also increase<br />
your physical activity.<br />
18<br />
Y O U R B A B Y ’ S B I R T H
Fainting or Dizziness<br />
Lowered blood pressure may cause you to feel faint when standing for extended periods of time or<br />
lying on your back. Sleeping on your side, when possible, eating frequent small meals, avoiding<br />
sweets, and moving around while standing should help.<br />
Hand Pain and Numbness<br />
Increased fluid and pressure on the carpal tunnel nerve in the wrist may cause numbness, tingling,<br />
burning and/or pain in the hand, wrist and arm. The discomfort may increase at night. Wearing a<br />
wrist splint, vigorously shaking your hands at the onset of pain and avoiding sleeping on your<br />
hands may help you feel better.<br />
Headaches<br />
Increased stress and hormone changes can cause frequent headaches. Reducing stress or relaxing<br />
in a dark or pleasant room may help decrease the intensity and frequency of headaches. If you<br />
experience severe headaches or problems with your vision, contact your healthcare provider<br />
immediately.<br />
Hemorrhoids<br />
To ease hemorrhoid discomfort, take a 15-20 minute bath three or four times a day or apply a cotton<br />
ball soaked with cold witch hazel, a Tucks pad or ice directly to the hemorrhoid.<br />
Indigestion or Heartburn<br />
Because of the hormonal and physical changes in pregnancy, food sometimes moves more slowly<br />
through your system, which causes bloating and indigestion. To help lessen your discomfort and<br />
heartburn, follow the tips for nausea (below) and also:<br />
• Remain upright for 30 minutes after eating and don’t exercise for 45 minutes after a meal.<br />
• Stop eating 2-3 hours before going to bed to give your stomach time to settle.<br />
• Cut back on coffee, tea, soda and other high acidic foods and beverages.<br />
Leaking Urine<br />
As your abdomen enlarges, pressure is continually placed on your bladder and can lead to urine<br />
leakage. Practice kegel exercise several times per day to prevent leakage.<br />
Leg Cramps<br />
You may get leg cramps that come and go for no apparent reason. Increasing calcium intake and<br />
exercising may help prevent leg cramps. To ease the pain, push away from your body with your heel<br />
while pointing your toes toward your head, gently massage the cramped area, and take a warm bath.<br />
Nausea and Vomiting<br />
These unpleasant problems occur most often during the early months of pregnancy. There are many<br />
causes of nausea, including hormonal changes. If vomiting and nausea continue for a longer period<br />
of time, you may have weight loss and loss of appetite. To help you cope with this common problem,<br />
you might try to:<br />
• Eat crackers before you get out of bed, and get out of bed slowly.<br />
• Eat several small meals instead of a few large meals.<br />
• Only eat when you are truly hungry, and take your time with each bite.<br />
• Avoid spicy or greasy foods.<br />
• Try to drink fluids in between meals instead of during meals.<br />
• Take your prenatal vitamins with meals.<br />
• Get fresh air.<br />
• Stop smoking.<br />
19<br />
Y O U R B A B Y ’ S B I R T H
Shortness of Breath<br />
<strong>Your</strong> growing uterus takes up part of your breathing space causing shortness of breath. To temporarily<br />
relieve symptoms, raise your arms over your head and stretch.<br />
Swollen Legs, Hands and Feet<br />
Many women retain fluid while pregnant, which causes swelling. You can help decrease swelling by<br />
eating plenty of protein, drinking eight glasses of water a day and eating low sodium foods.<br />
Vaginal Discharge<br />
<strong>Pregnancy</strong> hormones cause the vagina to increase its normal secretions. Yeast infections are also<br />
more common among pregnant women. To help ease discomfort, wear skirts and dresses rather than<br />
pants, avoid wearing panty hose when possible, and wear cotton undergarments and/or a minipad.<br />
Call your doctor if you think you have a yeast infection or other infection. Do not take over-the-counter<br />
medications before talking with your doctor.<br />
Varicose Veins<br />
Varicose veins may ache or hurt in your thigh, calf, pelvic area or groin. Help improve your<br />
circulation by putting on support stockings before getting out of bed in the morning, avoiding<br />
crossing your legs, and keeping your legs elevated when seated.<br />
Conditions of special concern<br />
Anemia<br />
Anemia results from having low iron and folic acid levels in your body. Most pregnant women have<br />
a difficult time getting the iron and folic acid they need. Prenatal vitamins help, but make sure<br />
your diet is high in iron and rich in folic acid and vitamin C. Orange juice is an excellent source of<br />
both folic acid and vitamin C. Vitamin C, taken with vitamins, increases iron absorption.<br />
Group B Streptococcus (GBS) and <strong>Pregnancy</strong><br />
During pregnancy, your healthcare provider will take a vaginal culture to test for group B<br />
streptococcus. GBS is a bacteria that usually does not cause problems for women, but may cause<br />
problems for your baby. Babies can be infected with GBS during labor or delivery.<br />
While your baby is in the hospital, the nurses and doctors will monitor your baby for signs of GBS<br />
infection. Early signs occur within six hours of birth and may include problems breathing, problems<br />
with temperature, low heart rate, seizures, vomiting, diarrhea, or abdominal swelling. However, a<br />
baby may be infected with GBS and not show any signs for days or even weeks after birth. This is<br />
called late-onset GBS infection and has many of the same signs as infections that occur earlier.<br />
Both early and late-onset GBS infections are very serious and need to be treated as soon as possible.<br />
Not all babies born to mothers with GBS become infected with the bacteria. A mother with GBS<br />
can be treated with antibiotics during labor to decrease the risk of infection to the baby. After<br />
being admitted to Newborn Nursery, the baby will be observed for signs of infection. The baby’s<br />
blood may also be tested. Babies whose mothers did not receive the recommended antibiotics<br />
prior to delivery may need to stay in the hospital for at least 48 hours after birth so that they can be<br />
observed for signs of infection and other problems and for treatment if necessary.<br />
GBS is common in pregnant women. Not all babies of women with GBS will have problems<br />
related to the infection. It is important to call your baby’s healthcare provider with any concerns<br />
after leaving the hospital.<br />
20<br />
Y O U R B A B Y ’ S B I R T H
Preeclampsia<br />
Preeclampsia is a group of changes that can occur after the 20th week of your pregnancy. The most<br />
common change is high blood pressure. Not all women have the same symptoms, and many<br />
symptoms are mild. That is why seeing your healthcare provider for blood pressure and urine checks,<br />
is so important. Warning signs of preeclampsia include:<br />
• Sudden weight gain of more than one pound a day<br />
• Changes in your vision (blurred vision or spots before your eyes)<br />
• Headaches that won’t go away<br />
• Pain under the upper right part of your rib cage<br />
Call your healthcare provider immediately if you have any of these discomforts.<br />
Gestational Diabetes<br />
Gestational diabetes mellitus (GDM) is a temporary condition that results in high blood sugar levels.<br />
Screening for GDM occurs between 24 and 28 weeks of pregnancy. If you are at high risk for GDM, you<br />
may be screened early in your pregnancy and rescreened if early testing was normal. Risk factors for<br />
GDM are:<br />
• Previous history of GDM<br />
• Glucose in urine<br />
• Strong family history of diabetes<br />
• Obesity<br />
• Previous history of large babies<br />
• Previous pregnancy loss<br />
• Ethnic background (Hispanic, African, Native American, South or East Asian or<br />
Pacific Island ancestry)<br />
If you are diagnosed with GDM, your healthcare provider will recommend a special diet, blood testing<br />
and exercise and lifestyle changes to keep your blood sugar levels in normal ranges. Insulin may<br />
also be required. A diabetes educator and dietician are available to help you learn how to manage your<br />
gestational diabetes and have a healthy pregnancy.<br />
Ultrasounds and non-stress tests may be done to check the health of your baby. Women with GDM may<br />
have large babies and/or babies with low blood sugar after birth. If you have GDM, your baby will have<br />
blood sugar testing after she/he is born.<br />
Women with gestational diabetes have a higher risk of developing diabetes later in life and should<br />
receive follow-up care by their primary care provider within the first year after delivery.<br />
21<br />
Y O U R B A B Y ’ S B I R T H
Premature Labor<br />
Preterm or premature labor is labor that begins after 20 weeks and before 37 weeks. About<br />
10 percent of infants are born more than three weeks before the due date. The uterine contractions<br />
may feel like menstrual-type cramps, dull backache or pelvic pressure. Drinking fluids and lying<br />
on your side may make the contractions go away. If there are more than four contractions in one<br />
hour, immediately call your physician or midwife. It is important to know the difference between<br />
preterm labor and the normal growing pains of pregnancy.<br />
Normal Discomforts of <strong>Pregnancy</strong><br />
• Contractions occurring three or fewer per hour.<br />
• Backache as the baby grows.<br />
• Pressure as the baby presses on your pubic bone and legs.<br />
• Pulling and stretching of muscles causing localized pain.<br />
Signs of Preterm/Premature Labor and Warning Signs<br />
Signs of preterm labor may be easily apparent or very subtle. Call your caregiver if you have<br />
any of the following symptoms:<br />
• Regular contractions or uterine tightening, more than four per hour. These contractions may<br />
be painless or feel like the baby is “balling up.”<br />
• Rhythmic, lower abdominal cramps - with or without diarrhea, nausea or indigestion.<br />
• Lower back pain or pressure.<br />
• Achiness or pressure in the pelvis, thighs, groin or lower abdomen.<br />
• Increase or change in vaginal discharge (watery, pinkish or brownish) sometimes preceded<br />
by the passage of a mucus plug.<br />
• Bleeding (more than one inch of spotting on your undergarments).<br />
If you think you are having preterm labor, call your healthcare provider right away. Treatment can<br />
often stop or postpone premature labor and increase the baby’s chance of survival. Limiting physical<br />
and sexual activity, bed rest, and sometimes hospitalization may be needed to stop preterm labor.<br />
Emergency signs for contacting your healthcare provider<br />
Other problems can also occur later in pregnancy. Call your healthcare provider if any of the<br />
following occur.<br />
• Trickle or flow of amniotic fluid from the vagina.<br />
• Bleeding—more than one inch of spotting on your undergarments.<br />
• Green or tarry color (meconium) when your water breaks.<br />
• Decreased fetal movements.<br />
22<br />
Y O U R B A B Y ’ S B I R T H
Later <strong>Pregnancy</strong><br />
Now that you are in your second trimester, you should continue to see your care provider, exercise<br />
and eat right for a healthy pregnancy and begin planning your baby’s birth.<br />
Things to Arrange<br />
• Tour<br />
Consider touring Harrisburg Campus Maternity Center before delivering your baby. Tours are<br />
included in childbirth classes if your class meets at the Brady Building next to Harrisburg<br />
Hospital or the Fredricksen Outpatient Center in Mechanicsburg. Call the Learning Institute<br />
at 221-6255 for other community tour information.<br />
• Baby’s Healthcare Provider<br />
You must choose a healthcare provider for your baby before you deliver. Make sure the caregiver<br />
you choose accepts your insurance. To find a pediatrician in your area go to<br />
www.pinnaclehealth.org and click on Find a Doctor.<br />
Circumcision<br />
Circumcision is a choice. Only you can decide whether it is right for your baby boy. Circumcision<br />
is a surgical procedure that cuts away the foreskin, which is the skin covering the glans (head of the<br />
penis). Remember, as with any surgical procedure, you will need to sign a consent form and there<br />
are possible complications. Talk with your obstetrician for more information about circumcision.<br />
Check with your insurance provider to be sure the cost of circumcision is covered by your policy.<br />
Breastfeeding or Bottlefeeding<br />
Deciding whether to feed your baby by breast or bottle is one of the most important decisions you<br />
will make concerning the care of your baby. The best decision is one that you feel most comfortable<br />
with. Read books that offer objective information. Friends and family may offer advice that<br />
reflects good or bad experiences with newborn feeding. Keep this in mind when making your own<br />
personal decision.<br />
Attend a breastfeeding class that offers accurate, up-to-date information. PinnacleHealth Learning<br />
Institute has a lactation center staffed by registered nurses who are board-certified lactation<br />
consultants. The lactation consultants teach breastfeeding classes, offer guidance to moms<br />
experiencing difficulty with breastfeeding, and provide assistance to moms returning to work who<br />
wish to continue breastfeeding. See the section “All the Help You Need” for more information about<br />
the Learning Institute.<br />
Benefits of breastfeeding include:<br />
For baby:<br />
• Breast milk is easier for baby to digest<br />
• Protection against gastrointestinal infections<br />
• Protection against ear infections<br />
• Reduced incidence of childhood lymphoma<br />
• Reduced incidence of childhood onset diabetes<br />
• Reduced incidence of Crohn’s Disease<br />
• Reduced incidence of allergies<br />
For mother:<br />
• Reduces blood loss after birth and helps the uterus return to its normal size<br />
• Produces hormones that help keep mother calm<br />
• Decreases risk of osteoporosis<br />
• Protects against ovarian and breast cancer<br />
Y O U R B A B Y ’ S B I R T H<br />
23
Planning <strong>Your</strong> Baby’s Healthcare<br />
<strong>Your</strong> prenatal care has helped to provide the best possible start for your baby. Now is the time to<br />
make preparations to continue that care after your baby is born. One of the first steps is to choose a<br />
healthcare provider for your newborn. (Note: the physician who delivers your baby does not provide<br />
newborn care.) This decision must be made prior to your baby’s birth.<br />
Types of providers:<br />
• Pediatrician - a doctor specializing in the care of children<br />
• Family Practice Physician- a doctor who can care for the entire family. If the baby develops a<br />
serious illness, he would probably refer you to a pediatrician or other specialist<br />
• Pediatric Nurse Practitioner<br />
Find a provider:<br />
Check with your insurance company to get a list of participating providers. Some people like to talk<br />
to friends, family and their own healthcare provider to get recommendations. Once you have<br />
identified a potential provider, call their office to ask:<br />
• Is the practice accepting new patients<br />
• Does the practice accept your insurance coverage<br />
• Does the healthcare provider see patients at PinnacleHealth If not, does the provider refer to a<br />
practice that takes care of newborns at the hospital<br />
• Request an appointment before your baby is born, if possible, to allow you to meet the provider<br />
and the office staff.<br />
Make a list of questions that you would like to have answered at your visit, or by phone. Here are<br />
some suggestions:<br />
• What are your office hours<br />
• What type of on-call and after-hours coverage do you have<br />
• Do you offer phone support for questions that may not require an appointment When is that<br />
available<br />
• Who takes the calls and answers the questions Does the provider return phone calls if requested<br />
• What is your recommended well-baby visit schedule and immunization schedule<br />
• Do you support breastfeeding<br />
If you plan to breastfeed your baby, here are some questions you may wish to ask the provider.<br />
Hearing their responses will help you determine whether or not they support your thoughts and<br />
feelings about breastfeeding. Be aware of enthusiastic responses versus a sense of indifference.<br />
This can tell you a lot.<br />
• When do you have breastfed babies come to the office for their first weight check<br />
(The American Academy of Pediatrics recommends two days.)<br />
• Do you recommend routine formula supplementation for breastfed babies<br />
• If someone is having difficulty breastfeeding, what support is available within the practice<br />
or by referral<br />
• To what age do most of your patients breastfeed their babies<br />
24<br />
Y O U R B A B Y ’ S B I R T H
If the provider you have selected does not see patients at PinnacleHealth, you should ask that the<br />
baby’s physical exam report be sent to your provider’s office or that a copy be given to you before<br />
you are discharged.<br />
Be sure to have the name, address and phone number of the provider you have chosen for your<br />
baby available at the time of your hospital admission. Use the checklist at the front of this book to<br />
record this information.<br />
<strong>Childbirth</strong> and parenting classes<br />
If you are interested in registering for a class, or want more information, call 221-6255.<br />
Adoptive Parent<br />
A single evening class designed for couples or individuals who plan to adopt a child within the<br />
next year. Class discussion is individualized to the type of adoption that is being planned. Content<br />
focusing on adopting an infant includes baby care, necessary supplies, travel with baby, as<br />
well as the emotional and social aspects of adoption. Content focusing on adopting an older child<br />
includes facilitating attachment, finding local support services, as well as addressing unique<br />
concerns, such as maintaining sibling contact.<br />
Baby Care Basics<br />
In this two-week series, expectant parents learn how to care for a newborn. Discussion,<br />
demonstration and class participation are used to teach basic information about baby’s bath, cord<br />
care, diapering, safety and feeding. Other topics include normal newborn behaviors, symptoms of<br />
illness, how to stimulate learning, parenting and issues around returning to work.<br />
<strong>Birth</strong> Center Tour<br />
This tour provides an opportunity to visit the Labor and Delivery, Neonatal Intensive Care and<br />
Maternity Units. You may tour the facility at any phase of your pregnancy. Due to the areas being<br />
toured, we are not able to accommodate children on this tour. There is no fee for this tour.<br />
Becoming a Grandparent<br />
This single evening class focuses on the experience of the grandparent. Discussion includes<br />
supporting the new family, and recent changes in medical practices and infant care.<br />
Breastfeeding Basics<br />
This class for expectant parents focuses on the joys and common concerns of breastfeeding.<br />
Information includes the benefits for mothers and babies, initiating feedings, maintaining a milk<br />
supply and other practical considerations. Discussion includes combining breastfeeding and<br />
working, expression and storage of breast milk and use of breast pumps. Expectant fathers are<br />
encouraged to attend.<br />
Cesarean <strong>Birth</strong><br />
A single class designed for expectant parents who are anticipating a cesarean birth. Focus is on<br />
the physical and emotional aspects of a cesarean birth experience. Class includes information<br />
about the reasons for cesarean birth, medications and anesthesia, and discussion regarding the<br />
role of the support person before, during and after the birth.<br />
<strong>Childbirth</strong> Refresher<br />
This class is a three-week series for expectant parents who have previously attended a childbirth<br />
education program. Class includes review of relaxation, breathing patterns and comfort measures<br />
for labor. This class does not include a <strong>Birth</strong> Center tour.<br />
25<br />
Y O U R B A B Y ’ S B I R T H
First Aid for Parents<br />
This one-day non-certification class for parents and other caregivers of infants and children<br />
includes basic first aid, emergencies common to babies and children, and Infant/Child CPR.<br />
Instructors are certified by the American Heart Association. “Family and Friends First Aid for<br />
Children” and “Family and Friends CPR” participation cards will be received in this class.<br />
Individualized <strong>Childbirth</strong> Classes<br />
This class is available to expectant parents who request individualized instruction. Course content<br />
includes phases of labor, comfort techniques medical interventions, and more. This class will<br />
enhance your understanding of labor and birth. A certified childbirth educator will address your<br />
specific needs and concerns. Two class sessions, two hours each.<br />
Infant/Child Cardiopulmonary Resuscitation (CPR)<br />
This one evening non-certification class focuses on Infant/Child CPR and obstructed airway<br />
techniques taught in a “watch and practice” format. Instructors are certified by the American Heart<br />
Association. A “Family and Friends CPR” participation card will be received in this class.<br />
Lamaze ® <strong>Childbirth</strong> Classes<br />
This six-week series provides information on the phases of labor, common medical options and<br />
comfort techniques, including support, positioning, breathing and relaxation. Brief overviews of<br />
postpartum and newborn are presented. These classes promote the Lamaze ® Philosophy of <strong>Birth</strong><br />
and the Six Care Practices of the Lamaze ® Institute for Normal <strong>Birth</strong>. Additional time is spent<br />
practicing comfort measures, as these classes are a half-hour longer than Prepared <strong>Childbirth</strong><br />
classes. They are taught by childbirth educators certified by Lamaze ® International. A tour of the<br />
Harrisburg Hospital <strong>Birth</strong> Center is included.<br />
Prepared <strong>Childbirth</strong><br />
This six-week series focuses on preparation for childbirth, emphasizing the experience of labor and<br />
birth and the supportive role of the partner. A variety of comfort measures are taught and practiced<br />
in class, including relaxation and breathing techniques. Medical options are discussed, as well as<br />
a brief overview of postpartum and newborn. Taught by certified childbirth educators, these<br />
classes will enhance your understanding of labor and birth and provide valuable information to help<br />
you prepare for your birth experience. A tour of the Harrisburg Hospital <strong>Birth</strong> Center is included.<br />
Siblings: A New Baby at Our House — Babies and Big Kids<br />
This class, designed for children four to nine years of age, includes discussion and a children’s<br />
video about birth and becoming a big brother or sister. Children also have the opportunity to<br />
practice holding dolls and learn how newborn babies look and behave. Class includes a child’s tour<br />
of the Maternity Center and Newborn Nursery.<br />
Siblings: A New Baby at Our House — Babies and Toddlers<br />
This group is designed for two and three-year-olds who are about to become big brothers or sisters.<br />
Each child should bring a favorite doll or teddy bear for the play activities. There will also be a short<br />
tour, but no video will be shown.<br />
The Happiest Baby<br />
Join the growing number of parents using Dr. Harvey Karp’s method to calm their crying babies. In<br />
a single class you will learn Dr. Karp’s secrets for making babies happy. Practice the 5 S’s used to<br />
engage your baby’s “calming reflex.” These techniques are most beneficial for babies from birth to<br />
two months of age. Instructors teaching this class have completed The Happiest Baby Certification<br />
Program. Class fee includes “The Happiest Baby on the Block” DVD and “Soothing Sounds” CD.<br />
26<br />
Y O U R B A B Y ’ S B I R T H
Tiny-Touch Infant Massage<br />
Loving, nurturing touch between parent<br />
and infant has a positive effect on the<br />
child’s development. Bring your baby<br />
(six weeks to six months old) and learn<br />
the techniques and benefits of massaging<br />
your infant. This four-week series also<br />
offers time to meet with other new parents.<br />
Massage oil is provided in the class.<br />
Twins, Triplets or More<br />
This class, for parents expecting multiples,<br />
is recommended for the second trimester.<br />
The class is intended to supplement the<br />
regular childbirth class with information<br />
specific to your family’s unique needs.<br />
A tour of the Neonatal Intensive Care Unit<br />
(NICU) is included.<br />
Vaginal <strong>Birth</strong> After Cesarean (VBAC)<br />
Individualized or small class instruction<br />
for parents who previously had a cesarean<br />
and want a vaginal birth for this pregnancy.<br />
Guidelines for a vaginal birth and the<br />
additional needs of a VBAC mother are<br />
discussed. Parents are also encouraged to attend a refresher class to learn confort techniques<br />
and medical options.<br />
Weekend <strong>Childbirth</strong> Seminar<br />
This seminar condenses the material taught in the six-week Prepared <strong>Childbirth</strong> course.<br />
There is a one-hour lunch break on Saturday. This class does not include a <strong>Birth</strong> Center tour.<br />
Weekend Lamaze ® Seminar<br />
This seminar condenses the material taught in the six-week Lamaze ® <strong>Childbirth</strong> course.<br />
There is a one-hour lunch break on Saturday. This class does not include a <strong>Birth</strong> Center tour.<br />
27<br />
Y O U R B A B Y ’ S B I R T H
Tests for <strong>Your</strong> Baby’s Well-Being<br />
There are different tests your physician may order during the later part of pregnancy to determine the<br />
condition of the baby. Some of these will not be covered by insurance unless the physician indicates<br />
there is a condition requiring the test.<br />
Fetal Kick Count<br />
The fetal kick count is a no cost, no risk test that every mother can use. Starting in the 28th week, the<br />
mother chooses a time each day to begin the fetal kick count. It should be the same time every day.<br />
She counts the baby’s movements and determines how long it takes for the baby to move 10 times. If<br />
the baby is not moving, or is moving much less than usual, the mother should rest and direct her<br />
attention to the infant’s movements. If she notes less than five movements in 30 minutes, the<br />
physician or midwife should be called. Other tests can then be used to evaluate the baby’s condition.<br />
Non-Stress Test<br />
A non-stress test is a safe, painless way to check your baby’s well-being before it is born. An external<br />
monitor will be placed onto the mother’s abdomen using elastic straps. One part will record fetal heart<br />
rate. One part will record contractions, if you are having any. <strong>Your</strong> healthcare provider will look at the<br />
baby’s heart rate. Normally when a baby moves, his heart rate speeds up. That is a sign of good health.<br />
The test can take up to 60 minutes to complete.<br />
Biophysical Profile<br />
A biophysical profile is another safe test to check your baby’s health before it is born. It is an<br />
ultrasound study that looks at your baby’s movement, body tone, breathing and the amount of fluid<br />
around the baby. It is often done in addition to the non-stress test.<br />
Oxytocin Challenge Test<br />
This test measures how your baby’s heart rate responds to contractions. An external monitor will be<br />
placed onto the mother’s abdomen using elastic straps. One part will record fetal heart rate. One part<br />
will record contractions. A catheter will be placed into a vein (IV) and a medicine called Oxytocin<br />
(Pitocin) will be given through that catheter. The medicine will be run on a pump and will be increased<br />
slowly to create contractions. <strong>Your</strong> healthcare provider will look at your baby’s heart rate during and<br />
after contractions. A baby that can handle the stress of labor will not have any slowing of the heart rate<br />
associated with contractions.<br />
28<br />
Y O U R B A B Y ’ S B I R T H
Y O U R B A B Y ’ S B I R T H<br />
29
30<br />
Y O U R B A B Y ’ S B I R T H
Choosing and Using a Car Seat<br />
Pennsylvania’s Child Passenger Safety Law requires that all children under age 4 must be<br />
properly restrained and transported in a federally approved car seat that is appropriate<br />
for the child’s age, height and weight. Children ages 4-8 must use a booster seat if they are<br />
no longer in a car seat. Children ages 8-18 must use a vehicle seatbelt.<br />
In addition to compliance with the law, the use of a car seat also has the following benefits:<br />
• Prevents your infant’s body from acting as a missile in the event of an accident.<br />
• Reduces the incidence of death or injury by spreading the impact along the strongest part of the<br />
infant’s body.<br />
• Reduces discipline problems of toddlers in the car, since they are used to sitting securely<br />
fastened in their seat.<br />
When installed and used properly, a safety seat can reduce a child’s chances of being killed or<br />
injured in a crash by 71%.<br />
In March/April 2011, The American Academy of Pediatrics (AAP) and the National Highway<br />
Traffic Safety Administration (NHTSA) revised their child restraint guidelines in order to<br />
keep pace with the latest scientific and medical research and the development of new child<br />
restraint technologies. They are now advising parents and caregivers to keep children in<br />
each restraint type, including rear-facing, forward-facing and booster seats, for as long as<br />
possible before moving them up to the next type of seat.<br />
Types of car seats<br />
Rear Facing Seats<br />
• Keeping your child rear-facing as long as possible is the best way to keep him or her safe.<br />
• In a policy published in the April 2011 issue of Pediatrics, the American Academy of Pediatrics<br />
(AAP) advises parents to keep their children in rear-facing car seats from birth until the age<br />
of 2, or until they reach the maximum height and weight allowed by their car seat’s manufacturer.<br />
• In the event of a collision, the impact is spread along the back. A rear-facing child safety seat<br />
does a better job of supporting the head, neck and spine of infants and toddlers in a crash,<br />
because it distributes the force of the collision over the entire body.<br />
• Newborns must be reclined at a 45 degree angle to prevent their head from dropping forward and<br />
blocking their airway. As the neck becomes stronger, the car seat may be more upright.<br />
• Many rear facing car seats can also be used as infant carriers.<br />
• Harness straps should come out at or below the shoulder level.<br />
Convertible Seat<br />
• Designed by the manufacturer to be both a rear-facing seat and a forward-facing seat.<br />
• Not used as an infant carrier, due to larger size.<br />
• There are usually two different belt paths for the car seat belts, depending on whether the seat is<br />
facing forward or backward.<br />
• When the seat is facing forward, it is essential to move the harness straps to the upper shoulder<br />
slots, so they come out at or above your child’s shoulder level.<br />
31<br />
Y O U R B A B Y ’ S B I R T H
Forward Facing Seats<br />
• Children face forward when they reach the maximum height and weight for their rear-facing car<br />
seat. A forward-facing seat with a harness and tether is the next step. It is safer than a booster<br />
seat. It limits your child’s forward movement during a crash.<br />
• In the event of a collision, the impact is spread across the shoulder, breast and hip bones.<br />
• Adjust the harness snugly so you cannot pinch the webbing together between your fingers at the<br />
baby’s shoulders. Only one finger should fit snugly beneath the harness and your baby.<br />
• The harness clip should be at the armpit level, so it lies across the breastbone.<br />
• Harness straps should come out at or above the shoulder level.<br />
Combination Seat<br />
• Designed by the manufacturer to be both a forward facing seat with a harness and belt<br />
positioning booster.<br />
• When the child is ready for the booster, the harness straps are removed, and the car lap and<br />
shoulder belt are used to secure the child in the car.<br />
Belt Positioning Boosters<br />
• The belt-positioning booster seat positions an older child so that the vehicle shoulder belt fits<br />
snug across the middle of the shoulder bone and middle of the breastbone, and the lap portion<br />
rides low across the thigh area.<br />
• Used with both the lap and shoulder belts.<br />
• A belt-positioning booster seat provides better protection than a seat belt alone, until the seat<br />
belt fits correctly.<br />
• The AAP advises that children must ride in belt-positioning booster seats until they have reached<br />
4’ 9” tall and are between 8 and 12 years of age. Ideally they should also weigh 80 pounds.<br />
• Keep your child in a booster seat until he or she is big enough to fit in a seat belt properly.<br />
- <strong>Your</strong> child’s legs should be long enough so the knees bend at the front edge of the seat.<br />
- <strong>Your</strong> child should be able to sit with their back straight against the vehicle seat back cushion.<br />
- The vehicle lap belt fits low and snug across the upper thighs (hips), not the stomach.<br />
- The shoulder belt should cross the collar bone and center of the child’s chest. It should lie snug<br />
across the shoulder and chest and not cross the neck or face.<br />
Children should ride in the back seat of a vehicle until they are 13 years old.<br />
32<br />
Y O U R B A B Y ’ S B I R T H
Selecting your car seat<br />
• Consider if you would prefer a rear facing only seat (which can be used as an infant carrier),<br />
or a convertible seat (which can also be used forward facing when the infant is older). Shop and<br />
compare prices, as well as the pros and cons of each option.<br />
• Keep in mind that, because of its size, convertible seats often do not fit newborns properly;<br />
especially smaller newborns. The convertible seat for newborns is also less convenient, because<br />
baby must be wrapped and unwrapped when getting in and out of the car, especially in cold<br />
weather.<br />
• Keep in mind that rear-facing only seats must be replaced with a forward-facing seat when your<br />
baby outgrows the manufacturer’s height and weight restrictions.<br />
Installing your car seat<br />
Be willing to invest the time to learn to use your car seat properly. Many people spend hours, days<br />
or even weeks picking out a vehicle, but don’t think of taking the time to get acquainted with a car<br />
safety seat.<br />
• Read the instruction booklet that comes with the car seat.<br />
Correct<br />
• Check your car owner’s manual for special instructions on the<br />
use of car safety seats.<br />
• Infants should never travel behind an airbag.<br />
• Put your weight into the car seat as you fasten it. It should<br />
move no more than one inch side to side at the seat belt.<br />
• To be sure your baby is safe, it is best to have your car seat<br />
checked by a Certified Child Passenger Safety Technician<br />
before you are admitted to the hospital.<br />
Call Dauphin County SAFE KIDS at (717) 531-SAFE (7233)<br />
Incorrect<br />
or South Central PA Highway Safety at (717) 766-1616<br />
or 1-800-822-2358 for an appointment.<br />
Additional car seat check points, recall information, and other<br />
child safety seat information can be accessed by contacting:<br />
- The National Highway Traffic Safety Administration<br />
www.nhtsa.gov or call 1-888-327-4236.<br />
- Traffic Injury Prevention Project (TIPP)<br />
www.paaap.org or call 1-800 CAR BELT (227-2358)<br />
- www.carseatdata.org<br />
- www.seatcheck.org or call 1-866-SEAT CHECK<br />
33<br />
Y O U R B A B Y ’ S B I R T H
Car seat safety<br />
Head Support Cushions<br />
• Do not put a head support cushion in your baby’s car seat, unless it came with the seat from the<br />
manufacturer. Head support cushions put padding behind your baby’s head and may cause his<br />
head to tip too far forward, possibly blocking his airway or changing the fit of the harness,<br />
making it unsafe in an accident. Manufacturers who have head supports in their car seats have<br />
done safety tests with them in place.<br />
• Bring three to four extra blankets to the hospital. The blankets may be used to support your baby’s<br />
head properly in the car seat if the car seat head support is too big for your baby’s head.<br />
Outerwear and Carrier Bunting<br />
Do not use outerwear or carrier bunting (the type<br />
that lay in the car seat and your baby lays on top<br />
of). Fabric on or under your baby pushes down<br />
during an accident and may change the harness<br />
fit. Put your baby in the car seat with one layer<br />
of clothing; secure him in the seat with the<br />
harness snug, and then place blankets over the<br />
harness system for warmth. Use a hat, mittens<br />
and booties if needed. Remember to bring three to<br />
four extra blankets or a carrier cover to keep your<br />
baby warm when going home from the hospital.<br />
Correct<br />
Incorrect<br />
Carrier Toys, Baby Mirrors and Baby Window Shades<br />
Toys, baby mirrors and window shades may be thrown loose during an accident and injure your<br />
baby. Anything loose in your car, including groceries, pets, sports equipment, etc., can become a<br />
projectile during an accident and cause serious injury to passengers, including your baby. Use a<br />
cargo cover or your trunk to store loose items. Note: a projectile’s weight is multiplied by the<br />
speed of your vehicle at the time it becomes airborne. For example, if a one pound window shade<br />
loosens from the window when your car is traveling 50 miles per hour, its weight on impact will<br />
be 50 pounds!<br />
Fitting your baby in a child safety seat<br />
• Place your baby flush against the car seat in one layer of clothing.<br />
• Adjust the harness snugly so you cannot pinch the webbing together between your fingers at the<br />
baby’s shoulders. Only one finger should fit snugly beneath the harness and your baby.<br />
• Position the retainer clip on your baby’s upper chest (armpit level), about one inch from his neck<br />
so it does not press on his airway.<br />
• Check that the harness straps are not rubbing on the sides of your baby’s neck. Pull your baby’s<br />
collar out over the shoulder straps, or pull up the fabric on his clothes alongside his neck.<br />
• If your car seat did not come with a head support, or did, but it is too big for your baby’s head,<br />
fold a blanket in half and roll it into a tube. Mold the rolled blanket around your baby’s head or<br />
inside the existing head support, and then tuck the remaining length along side of the baby’s ears.<br />
• Layer blankets as appropriate for warmth.<br />
34<br />
Y O U R B A B Y ’ S B I R T H
Car Seat Challenge Testing<br />
Some babies who are born prematurely (early) or small may have breathing problems when sitting<br />
in a semi-reclined car safety seat. The breathing problems usually go away as the baby grows<br />
during the next month. If your baby was born at less than 37 weeks gestation, he will be tested in<br />
the newborn nursery to be sure that he can breathe well while sitting in an upright car seat. It is<br />
important to bring your car seat to your hospital room immediately following transfer to the<br />
maternity unit so that your baby can be tested.<br />
If your baby was born prematurely or small and has not passed the car seat challenge testing, this<br />
information will help you transport your baby safely:<br />
• <strong>Your</strong> baby will need to use a car bed if any of the following occur while in a car safety seat:<br />
- a decrease in oxygen levels<br />
- slow heart rate<br />
- apnea (breathing stops for a moment or two)<br />
• Car beds can be rented from PinnacleHealth.<br />
• Car beds that meet Federal Motor Vehicle Safety Standards allow babies to travel while lying<br />
down. Some reasons why a baby may need to travel in a car bed include:<br />
- problems breathing when sitting up or semi-reclined<br />
- decreased muscle control<br />
- bones that break very easily<br />
- recent surgery on the spine<br />
- wearing a cast<br />
• It is important to use the car bed every time your baby travels in the car, and monitor baby<br />
at all times.<br />
• Position your baby on his or her back in the car bed.<br />
• Use the car bed ONLY in the vehicle to prevent injury to your baby. DO NOT use in your home or<br />
on a shopping cart.<br />
• When you return home, make an appointment to bring your baby to be retested in the car safety<br />
seat. The test can be done in 3-4 weeks at PinnacleHealth Pulmonary Function Lab. You must<br />
bring your car seat and paperwork with you. For more information, please call (717) 782-3684.<br />
• If your baby has outgrown the car bed before he is scheduled for the retest, please call the<br />
Pulmonary Function Lab for an earlier appointment.<br />
• When your baby passes the retest, the Pulmonary Function Lab will return the car bed. <strong>Your</strong><br />
deposit, less $10, will be mailed to you.<br />
Until your baby passes the retest, DO NOT place him in the infant chair, swing or other upright<br />
position. Upright positions may cause breathing problems.<br />
For more information on child safety seats or to schedule an appointment for car seat installation<br />
visit www.carseatdata.org, www.nhtsa.dot.gov, www.seatcheck.org, or call 1-800-CARBELT or<br />
Dauphin County SAFE KIDS at (717) 531-SAFE, or South Central PA Highway Safety at (717) 766-1616.<br />
35<br />
Y O U R B A B Y ’ S B I R T H
36<br />
Y O U R B A B Y ’ S B I R T H
All the Help You Need
All the Help You Need<br />
In this section we have listed resources and programs that may be useful during and after<br />
your pregnancy.<br />
PinnacleHealth Resources<br />
Adoption Information<br />
<strong>Birth</strong> parents and adoptive parents can obtain<br />
individual information and support from the<br />
Maternity clinical nurse specialist (782-5906)<br />
and social workers (231-8896).<br />
Behavioral Health | 231-8360<br />
Counseling and support services are provided<br />
for individuals and families needing<br />
psychological or emotional support, especially<br />
with postpartum depression.<br />
<strong>Childbirth</strong> Education | 221-6255<br />
A variety of classes including childbirth,<br />
breastfeeding, baby care, infant/child CPR, first<br />
aid and sibling preparation are available<br />
through our Parent/Child Education department.<br />
Childhood Lead Poisoning<br />
Prevention Center | 782-6442<br />
Children under six years of age and pregnant<br />
women are screened for lead exposure.<br />
Diabetes Education | 221-6250<br />
Provides education on all aspects of diabetes<br />
management.<br />
Doula Services | 221-6268<br />
A doula is a specially trained labor companion<br />
who provides physical and emotional support<br />
for women and their partners during labor<br />
and birth. A list of certified doulas who attend<br />
births at Harrisburg Hospital is available for<br />
interested families. Call for additional<br />
information if you are looking for a doula or are<br />
interested in becoming a certified doula.<br />
Children’s and Teen Center | 782-4650<br />
Provides well and sick healthcare for children<br />
0-21 years. Specialty clinics include lead,<br />
neurology, asthma and pulmonology, family<br />
planning and neonatal follow-up.<br />
Lactation Consultants | 782-5372<br />
Professional support, education and counseling<br />
for breastfeeding mothers are provided in the<br />
hospital by certified lactation consultants.<br />
One-on-one counseling and assistance is also<br />
available by appointment or by phone after<br />
discharge. A variety of breastfeeding aids,<br />
including rental of breast pumps, are available.<br />
Learning Institute | 221-6250<br />
PinnacleHealth Learning Institute offers a<br />
variety of programs for groups and individuals<br />
with a focus on wellness and prevention. Our<br />
team includes health educators, dietitians,<br />
nurses, childbirth educators, diabetes educators<br />
and lactation consultants.<br />
Mothers and Children (MAC) | 231-8900<br />
This group provides an opportunity for moms<br />
and tots to interact socially.<br />
New Mom Network | 231-8900<br />
An informal time of sharing for new mothers.<br />
This group is facilitated by an experienced<br />
nurse in maternal/child health, infant massage<br />
and lactation. Join other new moms and their<br />
infants, 0-9 months old and older babies age<br />
10-16 months for discussion about the physical<br />
and emotional adjustments to motherhood.<br />
No older children please.<br />
Nursing Mothers Counselors | 221-6250<br />
A team of dedicated volunteers with<br />
breastfeeding experience who are available to<br />
give support and answer questions/concerns<br />
about breastfeeding.<br />
Nutrition Education | 221-6250<br />
A registered dietician is available to provide<br />
individualized nutrition education on healthy<br />
eating while pregnant or breastfeeding.<br />
37<br />
Y O U R B A B Y ’ S B I R T H
The Parent Review<br />
PinnacleHealth offers a free weekly email for<br />
expectant and new parents to help guide you<br />
through pregnancy, labor and birth, and the<br />
first year of your baby’s life. Receive customized<br />
information, including tips, support, news,<br />
advice and resources. Register online at<br />
www.pinnaclehealth.org and click on the icon.<br />
Perinatal Bereavement Services | 231-8844<br />
Education and support services provided to<br />
those dealing with grief and loss related to<br />
pregnancy or childbirth. A support group meets<br />
monthly at Community Campus. Please call<br />
782-5906 or 221-6268 for more information.<br />
Perinatology | 231-8472<br />
Perinatalogists provide care for high-risk<br />
mothers through pregnancy and delivery. They<br />
may be the primary care provider or consult<br />
with a woman’s obstetrician.<br />
PinnacleHealth <strong>Home</strong> Care | 231-6363<br />
At home follow-up care by a registered nurse is<br />
covered by some insurance plans.<br />
PinnacleHealth Internet Site<br />
Providing health information on the Internet at<br />
www.pinnaclehealth.org. Look for directions,<br />
physician finder, events calendar and specific<br />
information about hospital and outpatient<br />
services, and several e-newsletters on a variety<br />
of topics.<br />
PinnacleHealth Library Services<br />
We offer professionally staffed medical libraries<br />
open to the public. Consumer health library<br />
services provide health information sources,<br />
Internet access and research to meet individual<br />
needs. <strong>Childbirth</strong> and Parenting DVDs are<br />
available for home viewing. Located at<br />
PinnacleHealth Community Campus (657-7247),<br />
Harrisburg Campus (782-5510).<br />
PinnacleHealth Psychological Associates<br />
231-8360<br />
An outpatient psychotherapy practice offering<br />
services to adults, older adults, children and<br />
adolescents. Licensed, masters level, Psy.D.<br />
and Ph.D. clinicians provide individual, family<br />
or marital evaluations, therapy as needed.<br />
We also offer group therapy should you and your<br />
therapist determine it would be helpful.<br />
REACCH | 782-2363<br />
A comprehensive care program for HIV positive<br />
mothers and their HIV-exposed infants and<br />
affected children.<br />
Social Services | 782-5574<br />
Referrals for help with financial problems, those<br />
who need help with drug/alcohol or domestic<br />
violence, adoption questions, or other stressors.<br />
Tours | 221-6255<br />
Tours of the <strong>Birth</strong> Center are available on an<br />
ongoing basis.<br />
WomanCare Resource Center | 231-8975<br />
WomanCare Resource Center promotes healthy<br />
lifestyles for women at every age and stage of<br />
their lives. We understand the delicate balance<br />
women seek to achieve in this demanding<br />
world of careers, personal interests, home and<br />
family. It’s common that the needs of aging<br />
parents, young children, maturing teens,<br />
spouses, partners and grandchildren<br />
often take precedence over your own.<br />
We are committed to you. Registered<br />
nurses are available onsite and by<br />
telephone to answer questions and<br />
provide individual health consultations.<br />
Visit www.pinnaclehealth.org/womancare<br />
for more information.<br />
Women’s Outpatient<br />
Health Center | 782-4700<br />
Hospital based gynecological,<br />
prenatal care and family<br />
planning are provided regardless<br />
of ability to pay.<br />
Please call the PinnacleHealth OneLine at 231-8900 if you would<br />
like a free copy of our Look Inside service brochure.<br />
38<br />
Y O U R B A B Y ’ S B I R T H
Healthcare Provider Resources<br />
More than 60 obstetrician/gynecologists, family<br />
practice physicians, midwives, nurse<br />
practitioners and pediatricians provide care for<br />
their patients at PinnacleHealth. This enables<br />
you to choose the caregiver that’s right for you.<br />
When choosing a caregiver, be sure to find out if<br />
the practice philosophy, areas of special interest<br />
and qualifications meet your needs. Each<br />
caregiver’s office staff can answer your specific<br />
questions about hours of operation, location and<br />
insurance accepted. For additional help in<br />
choosing a physician that meets your family’s<br />
healthcare needs, visit www.pinnaclehealth.org<br />
and click on Find a Doctor, or call PH Oneline at<br />
(717) 231-8900 or 1-877-499-3299.<br />
Family practice: The medical specialty which<br />
provides continuing and comprehensive<br />
healthcare for the individual and family. The<br />
scope of family practice includes all ages, both<br />
sexes, and every disease entity.<br />
Midwife: A registered nurse trained to assist a<br />
woman during childbirth. Many nurse midwives<br />
also provide prenatal care for pregnant women,<br />
birth education for women and their partners,<br />
and care for mothers and newborn babies after<br />
the birth. A midwife may be a man or a woman.<br />
Midwives may deliver babies in the mother’s<br />
home, in a special birthing center or clinic, or in<br />
a hospital.<br />
Neonatologist: A specialist in the care of the<br />
newborn with complications.<br />
Nurse practitioner (NP): A registered nurse<br />
(RN) who has completed an advanced training<br />
program in a medical specialty such as<br />
women’s health, family practice, pediatrics,<br />
neonatal or internal medicine. A NP may<br />
function as a primary direct healthcare provider<br />
and prescribe medications.<br />
Obstetrician/gynecologist: A physician who<br />
both delivers babies and treats diseases of the<br />
female reproductive organs.<br />
Pediatrician: The medical specialty which<br />
provides continuing and comprehensive<br />
healthcare for the individual and children from<br />
birth to adulthood. The scope of pediatricians<br />
encompasses both sexes and every disease<br />
entity.<br />
Perinatologist: An obstetrical subspecialist<br />
physician concerned with the care of the<br />
mother and fetus at higher-than-normal risk for<br />
complications.<br />
Community Resources<br />
Contact Help Line | 652-4400<br />
Crisis Intervention<br />
Eastern Cumberland & Perry counties -<br />
763-2222<br />
Western Cumberland & Perry counties -<br />
243-6005<br />
Dauphin county - 232-7511<br />
York county - 851-5320<br />
Dauphin County Social Services for<br />
Children and Youth | 782-7200<br />
The department is responsible for protecting<br />
the health and safety of children and youth.<br />
Services range from in-home services including<br />
prevention, intake/assessment and<br />
counseling/intervention and placement services<br />
including foster family care, group home,<br />
adoption and residential placement. Referrals<br />
may be made by phone, in writing or in person.<br />
Emergency services are provided 24-hours a<br />
day, seven days a week.<br />
Dauphin County Department of Drug<br />
and Alcohol Services | 635-2254<br />
This program implements alcohol and drug<br />
abuse prevention, intervention and treatment<br />
programs.<br />
Dauphin County SAFE KIDS<br />
(car seat installation) | 531-SAFE<br />
39<br />
Y O U R B A B Y ’ S B I R T H
Domestic Violence Services<br />
Provides shelter services, counseling, support<br />
groups, accompaniment services, legal services,<br />
and preventative education program.<br />
Domestic Violence Services of Cumberland<br />
& Perry Counties: 800-852-2101<br />
YWCA/Domestic Violence Services serving<br />
Dauphin County: 800-654-1211<br />
Domestic Violence Intervention of Lebanon<br />
County: 866-686-0451<br />
ACCESS-York serving York County: 24-hour<br />
hotline: 800-262-8444<br />
Domestic Violence Services of Lancaster<br />
County: 800-932-4632<br />
La Leche League | 1-800-LaLeche;<br />
1-846-519-7730<br />
This organization offers community support<br />
groups for breastfeeding mothers. www.llli.org<br />
PA Department of Health<br />
1-877-PA-HEALTH<br />
This state-run service provides programs for<br />
women, children and families for the prevention<br />
and suppression of disease and injury. Visit<br />
them on the Web at www.health.state.pa.us.<br />
PA Quitline (smoking cessation)<br />
1-877-724-1090<br />
Secret Safe Place for Newborns<br />
1-866-347-4287<br />
“A Secret Safe Place for Newborns” program is<br />
offered at the Harrisburg and Community<br />
General Hospital Emergency Departments.<br />
The mission of this service is to rescue<br />
newborn infants, who would otherwise be<br />
abandoned, from injury or death by providing<br />
confidential emergency care and shelter.<br />
Of special note is a promise by the Dauphin<br />
County District Attorney not to prosecute a<br />
mother as long as the baby is unharmed.<br />
A special toll-free number has been established<br />
to provide information.<br />
South Central PA Highway Safety<br />
(car seat installation) | 717-766-1616<br />
WIC (Women, Infants and Children)<br />
1-800-942-9467<br />
Provides healthy foods at no cost; health<br />
nutrition information; health and immunization<br />
screenings; breastfeeding information and<br />
support; recipes, newsletters and educational<br />
materials; one-to-one nutrition counseling;<br />
referrals to community services.<br />
40<br />
Y O U R B A B Y ’ S B I R T H
<strong>Childbirth</strong> Education<br />
and Parenting Programs
<strong>Childbirth</strong> Education<br />
and Parenting Programs<br />
Welcome to Parent/Child Education!<br />
The birth of a baby is one of the most treasured experiences in life. To help families prepare<br />
for this meaningful event, PinnacleHealth offers comprehensive childbirth education and parenting<br />
programs. All sessions are taught by certified instructors, at a variety of times and locations for<br />
your convenience.<br />
Our classes help you take responsibility for your health and the health of your child. We want<br />
to hear about your expectations and concerns, and we want to share knowledge that will help you<br />
approach this experience with confidence. The information you receive may prove helpful when<br />
making medical decisions with your healthcare provider. Our classes offer an opportunity to<br />
ask questions and get answers. They also allow you to connect with others who are going through<br />
a similar experience.<br />
We are committed to making your pregnancy and birth the most memorable and rewarding<br />
experience it can be. Thank you for allowing us to be a part of this special time in your life.<br />
Questions about our programs can be answered by calling the PinnacleHealth Learning Institute<br />
at (717) 221-6255.<br />
Table of Contents<br />
Preparation for <strong>Childbirth</strong><br />
Page 42 Lamaze ® <strong>Childbirth</strong> Series<br />
Page 42 Weekend Lamaze ® Seminar<br />
Page 43 Prepared <strong>Childbirth</strong> Series<br />
Page 44 Weekend <strong>Childbirth</strong> Seminar<br />
Page 44 <strong>Childbirth</strong> Refresher<br />
Page 45 Cesarean <strong>Birth</strong><br />
Page 45 Twins, Triplets & More<br />
Page 46 Online <strong>Childbirth</strong> Education Program<br />
Page 47 <strong>Birth</strong> Center Tours<br />
Individualized Classes<br />
Page 48 <strong>Childbirth</strong> Preparation<br />
Page 48 Vaginal <strong>Birth</strong> After Cesarean (VBAC)<br />
Parenting<br />
Page 49 Baby Care Basics<br />
Page 50 Breastfeeding Basics<br />
Page 50 Pediatric First Aid<br />
Page 51 Heartsaver AED/CPR<br />
Page 51 CPR for Family & Friends<br />
Page 52 Prenatal Infant Massage<br />
Page 52 Postpartum Infant Massage<br />
Page 52 The Happiest Baby<br />
Family<br />
Page 53 Siblings: “Big Brothers and Big Sisters”<br />
Page 53 Becoming a Grandparent<br />
Other Services<br />
Page 54 Doula Services<br />
Page 54 The Parent Review<br />
Page 54 Wellness Phone Calls to New Moms<br />
Page 54 Perinatal Bereavement Services<br />
Page 55 New Mom Network I<br />
Page 55 New Mom Network II<br />
Page 55 New Mom Network III<br />
Page 55 Working Moms Network (Evening)<br />
Page 55 Moms Navigating Through Life<br />
Page 57 Lactation Services<br />
Class Registration<br />
Page 58 Registration Information<br />
Page 59 Registration Form<br />
PinnacleHealth Locations<br />
Page 60 Map & Directions<br />
Page 60 Harrisburg Area Map<br />
41<br />
Y O U R B A B Y ’ S B I R T H
Preparation for <strong>Birth</strong><br />
Lamaze ® <strong>Childbirth</strong> Classes<br />
This six-week series provides information on the process of labor and birth, common medical<br />
interventions and options, and the important role of the dad/partner. Comfort techniques, including<br />
positioning, breathing and relaxation will be taught and practiced. A brief overview of cesarean<br />
birth, postpartum, and newborn are presented. These classes promote the Lamaze ® Philosophy<br />
of <strong>Birth</strong> and the Six Care Practices of the Lamaze ® Institute for Normal <strong>Birth</strong>. Additional time is<br />
spent practicing comfort measures, so these classes are a half-hour longer than Prepared <strong>Childbirth</strong><br />
classes. They are taught by childbirth educators certified by Lamaze ® International. A tour of the<br />
Harrisburg Hospital <strong>Birth</strong> Center is included.<br />
Registration fee: $100 (includes partner)<br />
PinnacleHealth Harrisburg Campus,<br />
Brady Building<br />
205 South Front Street, Harrisburg, PA 17104<br />
Mondays, 6:30-9 p.m.<br />
January 3 – February 7<br />
March 7 – April 11<br />
May 2 – June 13*<br />
*(No Class – May 30)<br />
July 11 – August 15<br />
September 12 – October 17<br />
November 7 – December 12<br />
PinnacleHealth Cumberland Campus,<br />
Fredricksen Outpatient Center,<br />
2015 Technology Parkway, Mechanicsburg, PA<br />
17050<br />
Thursdays, 6:30-9 p.m.<br />
February 3 – March 10<br />
April 7 – May 12<br />
June 23 – July 28<br />
August 11 – September 15<br />
October 6 – November 17*<br />
*(No Class – October 27)<br />
Weekend Lamaze ® Seminar<br />
This seminar condenses the material taught in the six-week Lamaze ® <strong>Childbirth</strong> course. There is<br />
a one-hour lunch break on Saturday. This class does not include a tour. <strong>Birth</strong> Center tour dates are<br />
listed on page 47 of this booklet.<br />
Registration fee: $110 (includes partner)<br />
The Community Center at Camp Hill<br />
GIANT Super Food Store<br />
3301 Trindle Road, Camp Hill, PA 17011<br />
Friday, 6-9:30 p.m. and<br />
Saturday, 9 a.m.-5:30 p.m.<br />
January 21 – January 22<br />
March 25 – March 26<br />
April 22 – April 23<br />
June 24 – June 25<br />
July 22 – July 23<br />
September 23 – September 24<br />
October 21 – October 22<br />
December 16 – December 17<br />
The Community Center at Linglestown<br />
GIANT Super Food Store<br />
2300 Linglestown Road, Harrisburg, PA 17110<br />
Friday, 6-9:30 p.m. and<br />
Saturday, 9 a.m.-5:30 p.m.<br />
February 25 – February 26<br />
May 20 – May 21<br />
August 26 – August 27<br />
November 18 – November 19<br />
42<br />
Y O U R B A B Y ’ S B I R T H
Prepared <strong>Childbirth</strong> Classes<br />
This six-week series focuses on preparation for childbirth, emphasizing the experience of labor and<br />
birth and the important role of the dad/partner. A variety of comfort measures are taught and<br />
practiced in class, including relaxation and breathing techniques. Medical interventions and<br />
options are discussed, as well as a brief overview of cesarean birth, postpartum, and newborn.<br />
Taught by certified childbirth educators, these classes will provide valuable information to help you<br />
prepare for your birth experience. A tour of the Harrisburg Hospital <strong>Birth</strong> Center is included.<br />
Registration fee: $85 (includes partner)<br />
PinnacleHealth Harrisburg Campus, Brady Building<br />
205 South Front Street, Harrisburg, PA 17104<br />
Evenings, 6:30-8:30 p.m.<br />
Tuesdays<br />
February 15 – March 22<br />
March 1 – April 5<br />
April 19 – May 24<br />
May 3 – June 7<br />
June 14 – July 19<br />
July 26 – August 30<br />
August 23 – September 27<br />
September 13 – October 18<br />
October 4 – November 8<br />
October 25 – November 29<br />
Wednesdays<br />
January 5 – February 9<br />
February 16 – March 23<br />
April 20 – June 1*<br />
*(No Class – May 4)<br />
June 8 – July 13<br />
August 17 – September 28*<br />
*(No Class – September 7)<br />
September 14 – October 19<br />
October 5 – November 9<br />
Thursdays<br />
January 6 – February 10<br />
March 3 – April 7<br />
May 12 – June 16<br />
July 28 – September 1<br />
September 15 – October 20<br />
November 3 – December 15*<br />
*(No Class – November 24)<br />
PinnacleHealth Cumberland Campus<br />
Fredricksen Outpatient Center<br />
2015 Technology Parkway, Mechanicsburg, PA 17050<br />
Mondays, 6:30-8:30 p.m.<br />
January 3 – February 7<br />
March 7 – April 11<br />
May 2 – June 13*<br />
*(No Class – May 30)<br />
July 11 – August 15<br />
September 12 – October 17<br />
November 7 – December 12<br />
43<br />
Y O U R B A B Y ’ S B I R T H
Weekend <strong>Childbirth</strong> Seminar<br />
This seminar condenses the material taught in the six-week Prepared <strong>Childbirth</strong> course. There is a<br />
one-hour lunch break on Saturday. This class does not include a tour. <strong>Birth</strong> Center tour dates are<br />
listed on page 47 of this booklet.<br />
Registration fee: $100 (includes partner)<br />
The Community Center at Camp Hill<br />
GIANT Super Food Store<br />
3301 Trindle Road, Camp Hill, PA 17011<br />
Friday, 6-9 p.m. and Saturday, 9 a.m.-5 p.m.<br />
January 7 – January 8<br />
February 11 – February 12<br />
April 8 – April 9<br />
May 13 – May 14<br />
July 8 – July 9<br />
August 12 – August 13<br />
October 7 – October 8<br />
November 4 – November 5<br />
The Community Center at Linglestown<br />
GIANT Super Food Store<br />
2300 Linglestown Road, Harrisburg, PA 17110<br />
Friday, 6-9 p.m. and Saturday, 9 a.m.-5 p.m.<br />
March 11 – March 12<br />
June 10 – June 11<br />
September 9 – September 10<br />
December 2 – December 3<br />
<strong>Childbirth</strong> Refresher<br />
This class is for expectant parents who have previously attended a childbirth education program.<br />
Class includes a review of labor and birth, medical interventions, and comfort measures, including<br />
positions, relaxation, and breathing patterns. A brief overview of cesarean birth, postpartum,<br />
and newborn will be presented. The important role of the dad/partner and preparing siblings for<br />
your hospital stay are also discussed. This class does not include a tour. <strong>Birth</strong> Center tour dates<br />
are listed on page 47 of this booklet.<br />
Registration fee: $40 (includes partner)<br />
The Community Center at Camp Hill GIANT Super Food Store<br />
3301 Trindle Road, Camp Hill, PA 17011<br />
Tuesdays, 6-9 p.m.<br />
January 11<br />
April 5<br />
July 12<br />
October 11<br />
44<br />
Y O U R B A B Y ’ S B I R T H
Cesarean <strong>Birth</strong><br />
A single class designed for expectant parents who are anticipating a cesarean birth. Focus is on<br />
the physical and emotional aspects of a cesarean birth experience and touches on relaxation as a<br />
coping skill. Class includes information about the reasons for cesarean birth, medications and<br />
anesthesia, postpartum recovery and newborn appearance and procedures. The important role of<br />
the dad/partner before, during, and after birth will be discussed.<br />
Registration fee: $35 (includes partner)<br />
The Community Center at Camp Hill GIANT Super Food Store<br />
3301 Trindle Road, Camp Hill, PA 17011<br />
Wednesdays, 6:30-9 p.m.<br />
February 9<br />
May 11<br />
August 10<br />
November 9<br />
Twins, Triplets & More<br />
This two-evening class for parents expecting multiples is recommended for the second trimester.<br />
The class is intended to supplement a regular childbirth class, with information specific to your<br />
family’s unique needs. It is also for parents expecting multiples who already have children.<br />
Class includes information about the different types of twinning, the process of labor and birth with<br />
multiples, what you need “two or more” of, feeding multiple babies, and ways of supporting the<br />
new family postpartum. A tour of the Neonatal Intensive Care Unit (NICU) and Newborn Nursery<br />
is included.<br />
Registration fee: $45 (includes partner)<br />
PinnacleHealth Harrisburg Campus, Brady Building<br />
205 South Front Street, Harrisburg, PA 17104<br />
Tuesdays, 6:30-8:30 p.m.<br />
February 8 and February 15<br />
May 10 and May 17<br />
August 23 and August 30<br />
November 8 and November 15<br />
45<br />
Y O U R B A B Y ’ S B I R T H
Online <strong>Childbirth</strong> Education Program<br />
In Addition To A Traditional <strong>Childbirth</strong> Class:<br />
PinnacleHealth Parent/Child Education is offering a special addition to our face-to-face childbirth<br />
classes. A new online program, based on The Gift of Motherhood book which you will receive in<br />
class, is now available for a minimal fee to those registering for a Lamaze ® <strong>Childbirth</strong> or Prepared<br />
<strong>Childbirth</strong> Class, or a Weekend Lamaze ® or Weekend <strong>Childbirth</strong> Seminar.<br />
This web-based eLearning program is interactive and includes animated illustrations, videos,<br />
voice-overs, and games. This additional resource can be used as an enhancement to your<br />
childbirth class, as a review, and to reinforce what you have learned. Should you have any<br />
questions, you will continue to have access to your childbirth educator, with whom you have<br />
established a relationship, even after your classes have ended.<br />
When you attend your first childbirth class, you will receive The Gift of Motherhood book. When<br />
you register for the online program, you will receive a personal access code. This program will be<br />
available to you for three months after initial log-on. You decide when to first access the online<br />
materials. Some parents benefit from having the information available to review at home between<br />
childbirth classes. Others prefer to complete their childbirth classes and access the online program<br />
closer to their due date. This allows them to review what they have previously learned and have<br />
the information available for a period of time after their baby arrives.<br />
Register for one of the childbirth classes mentioned above and take advantage of this additional<br />
resource at a special reduced fee.<br />
Registration fee: $20 in addition to the in-person childbirth class fee<br />
As An Alternative To A Traditional <strong>Childbirth</strong> Class:<br />
The PinnacleHealth Online <strong>Childbirth</strong> Education Program is also available as an alternative for<br />
parents who cannot attend a conventional childbirth class due to bed rest, scheduling conflicts,<br />
or time constraints.<br />
When you register and pay for the course, an<br />
access code will be mailed to you with your<br />
confirmation letter. This code will be valid for a<br />
period of three months after initial log-on. You<br />
will also receive a copy of The Gift of Motherhood<br />
book in the mail. With this option, you will<br />
have access to a certified childbirth educator,<br />
who will answer any questions you may have.<br />
Registration fee: $120<br />
46<br />
Y O U R B A B Y ’ S B I R T H
<strong>Birth</strong> Center Tours<br />
This tour provides the expectant mother and father/support person an opportunity to visit Labor<br />
and Delivery, the Neonatal Intensive Care Unit (NICU), the Maternity Center and the Newborn<br />
Nursery. This will allow you to become familiar with Harrisburg Hospital and get answers to any<br />
questions you may have. You may tour the <strong>Birth</strong> Center at any phase of your pregnancy.<br />
Due to the areas being toured, we are not able to accommodate children on this tour.<br />
A tour especially suited for children is provided in the Siblings class.<br />
Pre-registration is required. There is no fee.<br />
PinnacleHealth Harrisburg Campus, Harrisburg Hospital Lobby<br />
111 South Front Street, Harrrisburg, PA 17101<br />
Wednesdays, 1-2 p.m.<br />
January 5<br />
February 2<br />
March 2<br />
April 6<br />
May 4<br />
June 1<br />
July 6<br />
August 3<br />
September 7<br />
October 5<br />
November 2<br />
December 7<br />
Evenings, 6-7 p.m. OR 7:15-8:15 p.m.<br />
Tuesdays<br />
Thursdays<br />
January 13<br />
January 25<br />
February 10<br />
February 22<br />
March 10<br />
March 22<br />
April 14<br />
April 26<br />
May 12<br />
May 24<br />
June 9<br />
June 21<br />
July 14<br />
July 26<br />
August 11<br />
August 23<br />
September 8<br />
September 20<br />
October 13<br />
October 25<br />
November 10<br />
November 22<br />
December 8<br />
December 13<br />
A Virtual Tour of the <strong>Birth</strong> Center is available online at www.pinnaclehealth.org. Click on<br />
“Women’s Health,” then “<strong>Pregnancy</strong> and <strong>Childbirth</strong>.” A “Quick Link” will take you to the <strong>Birth</strong><br />
Center Virtual Tour.<br />
47<br />
Y O U R B A B Y ’ S B I R T H
Individualized Classes<br />
The following classes can be scheduled individually for expectant parents who need one-on-one<br />
instruction due to special circumstances. To schedule individualized classes, call the<br />
PinnacleHealth Learning Institute at (717) 221-6255.<br />
<strong>Childbirth</strong> Preparation<br />
This class focuses on preparing you for your birth experience. Course content includes information<br />
about the physical and emotional changes during labor, the important role of the dad/partner,<br />
relaxation and comfort techniques, common medical interventions and options, as well as a brief<br />
overview of cesarean birth, postpartum, and the newborn. <strong>Your</strong> instructor will address your specific<br />
needs and concerns. A certified childbirth educator will contact you to schedule two class sessions<br />
of two hours each.<br />
Registration fee: $150 (includes partner)<br />
Vaginal <strong>Birth</strong> After Cesarean (VBAC)<br />
Instruction is available for parents who have previously had a cesarean and want a vaginal<br />
birth for this pregnancy. Guidelines for a vaginal birth and the additional needs of a VBAC<br />
mother are discussed. Parents are also encouraged to attend a refresher class (see page 44) to learn<br />
comfort techniques and medical options.<br />
Registration fee: $50 (includes partner)<br />
48<br />
Y O U R B A B Y ’ S B I R T H
Parenting<br />
Baby Care Basics<br />
In this two-week series, expectant parents learn how to care for a newborn. Discussion,<br />
demonstration and class participation are used to teach basic information about baby’s bath, cord<br />
care, diapering, safety and feeding. Other topics include normal newborn behaviors, symptoms of<br />
illness, how to stimulate learning, parenting and issues around returning to work. Our Pediatric<br />
First Aid class (see page 50) compliments this series by providing instruction on health and safety<br />
issues.<br />
Registration fee: $45 (includes partner)<br />
The Community Center at Camp Hill GIANT Super Food Store<br />
3301 Trindle Road, Camp Hill, PA 17011<br />
Mondays, 6:30-8:30 p.m.<br />
January 3 and January 10<br />
January 17 and January 24<br />
January 31 and February 7<br />
February 14 and February 21<br />
February 28 and March 7<br />
March 14 and March 21<br />
March 28 and April 4<br />
April 11 and April 18<br />
April 25 and May 2<br />
May 9 and May 16<br />
June 6 and June 13<br />
June 20 and June 27<br />
July 11 and July 18<br />
July 25 and August 1<br />
August 8 and August 15<br />
August 22 and August 29<br />
September 12 and September 19<br />
September 26 and October 3<br />
October 10 and October 17<br />
October 24 and October 31<br />
November 7 and November 14<br />
November 21 and November 28<br />
December 5 and December 12<br />
49<br />
Y O U R B A B Y ’ S B I R T H
Breastfeeding Basics<br />
This two-week series for expectant parents focuses on the joys and common concerns of<br />
breastfeeding. Information includes the benefits for mothers and babies, initiating feedings,<br />
maintaining a milk supply and other practical considerations. Discussion includes combining<br />
breastfeeding and working, expression and storage of breast milk, and use of breast pumps.<br />
Expectant fathers are encouraged to attend. Saturday sessions meet for one 3-1/2 hour class.<br />
Registration fee: $45 (includes partner)<br />
PinnacleHealth Harrisburg Campus, Brady Building<br />
205 South Front Street, Harrisburg, PA 17104<br />
Mondays, 6:30-8:30 p.m.<br />
January 17 and January 24<br />
February 14 and February 21<br />
March 14 and March 21<br />
April 18 and April 25<br />
May 16 and May 23<br />
June 20 and June 27<br />
July 18 and July 25<br />
August 15 and August 22<br />
September 19 and September 26<br />
October 17 and October 24<br />
November 14 and November 21<br />
December 12 and December 19<br />
The Community Center at Camp Hill GIANT Super Food Store<br />
3301 Trindle Road, Camp Hill, PA 17011<br />
Thursdays, 6:30-8:30 p.m.<br />
Saturdays, 9-12:30 p.m.<br />
January 6 and January 13<br />
February 3 and February 10<br />
March 3 and March 10<br />
April 7 and April 14<br />
May 5 and May 12<br />
June 2 and June 9<br />
July 7 and July 14<br />
August 4 and August 11<br />
September 1 and September 8<br />
October 6 and October 13<br />
November 3 and November 10<br />
December 1 and December 8<br />
February 19<br />
May 21<br />
August 20<br />
October 22<br />
Pediatric First Aid<br />
This four-hour certification course for parents and other caregivers of infants and children includes<br />
basic first aid and medical, injury, and environmental emergencies, such as choking, asthma,<br />
bleeding, burns, poisoning, etc. Instructors are certified by the American Heart Association.<br />
A certification card will be mailed to your home address approximately 30 days after completion<br />
of the course.<br />
Registration fee: $55/person<br />
The above fee includes a Pediatric First Aid textbook, which will be mailed to you approximately<br />
two weeks before the class date. We strongly suggest that you read this book prior to class.<br />
The Community Center at Camp Hill GIANT Super Food Store<br />
3301 Trindle Road, Camp Hill, PA 17011<br />
Saturdays, 8:30 a.m.-12:30 p.m.<br />
February 19<br />
April 9<br />
June 18<br />
August 20<br />
October 15<br />
December 17<br />
50<br />
Y O U R B A B Y ’ S B I R T H
Heartsaver AED/CPR<br />
This four-hour certification course focuses on use of an automated external defibrillator (AED),<br />
Adult/Child/Infant CPR, and techniques to use on a person who is choking. Individual skill testing<br />
with an instructor must be successfully completed for certification. Instructors are certified<br />
by the American Heart Association. An AED/CPR certification card will be mailed to your home<br />
address approximately 30 days after completion of the course.<br />
Registration fee: $55/person<br />
The above fee includes a Heartsaver AED/CPR textbook which will be mailed to you approximately<br />
two weeks before the class date. We strongly suggest that you read this book prior to class.<br />
The Community Center at Linglestown GIANT Super Food Store<br />
2300 Linglestown Road, Harrisburg, PA 17110<br />
Saturdays, 8:30 a.m.-12:30 p.m.<br />
January 15<br />
March 19<br />
May 21<br />
July 16<br />
September 17<br />
November 19<br />
CPR for Family & Friends<br />
This non-certification class focuses on Adult/Child/Infant CPR and techniques to use on a person<br />
who is choking. This course is taught in a “watch and practice” format.<br />
Instructors are certified by the American Heart Association. A Family & Friends CPR participation<br />
card will be received in this class.<br />
Registration fee: $35/person; $50/couple<br />
<strong>Your</strong> CPR book will be mailed to you approximately two weeks prior to the class date for review.<br />
The Community Center at Camp Hill GIANT Super Food Store<br />
3301 Trindle Road, Camp Hill, PA 17011<br />
Wednesdays, 6:30-9 p.m.<br />
January 5<br />
March 2<br />
May 4<br />
July 6<br />
September 7<br />
November 2<br />
The Community Center at Linglestown GIANT Super Food Store<br />
2300 Linglestown Road, Harrisburg, PA 17110<br />
Wednesdays, 6:30-9 p.m.<br />
February 2<br />
April 6<br />
June 1<br />
August 3<br />
October 5<br />
December 7<br />
51<br />
Y O U R B A B Y ’ S B I R T H
52<br />
Prenatal Infant Massage<br />
This is a program of early touch experiences using the World Institute for Nurturing<br />
Communication’s (WINC) “Welcome Baby Massage” as the basis for the class. Parents will learn the<br />
value of touch to the newborn, as well as the connection between touch and baby’s adjustment to<br />
life outside the womb. How to interpret your baby’s behavior and identify his/her cues will be<br />
discussed. Why, when, and how to add touch strokes to early infant care, and the father’s important<br />
role will be covered in this two-session class.<br />
Registration fee: $35 (includes partner)<br />
The Community Center at Camp Hill GIANT Super Food Store<br />
3301 Trindle Road, Camp Hill, PA 17011<br />
Tuesdays, 6:30-8 p.m.<br />
April 19 and April 26<br />
October 18 and October 25<br />
Postpartum Infant Massage<br />
Loving, nurturing touch between parent and infant has a positive impact on the child’s<br />
development. Bring your baby (six weeks to six months old) and learn the techniques and benefits<br />
of infant massage. This three-week series also offers an opportunity to meet with other new<br />
parents. Massage oil is provided in the class.<br />
Registration fee: $50 (includes parent and baby)<br />
The Community Center at Camp Hill GIANT Super Food Store<br />
3301 Trindle Road, Camp Hill, PA 17011<br />
Saturdays, 10-11:30 a.m.<br />
February 5, February 12, and February 19<br />
July 30, August 6, and August 13<br />
Although some of the course information overlaps, each program stands on its own. The prenatal<br />
sessions focus on the immediate postpartum time period, and the postpartum sessions focus on the<br />
older infant (6 weeks to 6 months) with the growing child in mind. It is highly recommended that<br />
both programs be taken, but it is not required to reap the wonderful benefits of infant massage.<br />
Register for both Prenatal and Postpartum Infant Massage together and receive a $10<br />
discount! Both classes for $75!<br />
The Happiest Baby<br />
Join the growing number of parents using Dr. Harvey Karp’s method to calm their crying babies. In a<br />
single class you will learn Dr. Karp’s secrets for making babies happy. Practice the 5 S’s used to engage<br />
your baby’s “calming reflex”. These techniques are most beneficial for babies birth to two months of<br />
age. Educators teaching this class have completed the Happiest Baby Certification Program. Class fee<br />
includes “The Happiest Baby on the Block” DVD and “Soothing Sounds” CD.<br />
Registration fee: $35<br />
The Community Center at Camp Hill GIANT Super Food Store<br />
3301 Trindle Road, Camp Hill, PA 17011<br />
Wednesdays, 6:30-8:30 p.m.<br />
January 19<br />
March 16<br />
Y O U R B A B Y ’ S B I R T H<br />
May 18<br />
July 20<br />
September 14<br />
November 16
Family<br />
Siblings: “Big Brothers and Big Sisters”<br />
“Babies and Toddlers”<br />
This class is designed for two and three-year-olds who are about to become big brothers or sisters.<br />
Children will learn about newborns and how to interact with them. Some safety lessons will be<br />
shared. There will be a celebration of their role as big brothers and big sisters. A short tour of the<br />
Maternity Center and Newborn Nursery is included, but no video will be shown.<br />
Registration fee: $10/child<br />
PinnacleHealth Harrisburg Campus, Brady Building<br />
205 South Front Street, Harrisburg, PA 17104<br />
Fridays, 6:30-7:30 p.m.<br />
January 7<br />
March 11<br />
May 13<br />
July 8<br />
September 9<br />
November 11<br />
“Babies and Big Kids”<br />
This class, designed for children four to nine years of age, includes discussion and a children’s<br />
video about birth and becoming a big brother or sister. Children also have the opportunity to<br />
practice holding dolls and learn how newborn babies look and behave. Class includes a child’s tour<br />
of the Maternity Center and Newborn Nursery.<br />
Registration fee: $10/child<br />
PinnacleHealth Harrisburg Campus, Brady Building<br />
205 South Front Street, Harrisburg, PA 17104<br />
Fridays, 6:30-8 p.m.<br />
January 7<br />
February 11<br />
March 11<br />
April 8<br />
May 13<br />
June 10<br />
July 8<br />
August 12<br />
September 9<br />
October 7<br />
November 11<br />
December 9<br />
Becoming a Grandparent<br />
This single evening class focuses on the experience of the grandparent. New trends in medical<br />
practices and current recommendations for infant care and safety will be discussed. Suggestions<br />
on how grandparents can support the new family and play a valuable role in the lives of their<br />
grandchildren will be shared. A tour of the Harrisburg Hospital <strong>Birth</strong> Center is offered following the<br />
class. Participation is optional.<br />
Registration fee: $10/person<br />
PinnacleHealth Harrisburg Campus, Brady Building<br />
205 South Front Street, Harrisburg, PA 17104<br />
Tuesdays, 6:30-8 p.m.<br />
January 11<br />
April 5<br />
July 12<br />
October 11<br />
53<br />
Y O U R B A B Y ’ S B I R T H
Other Services<br />
Doula Services<br />
<strong>Birth</strong> doulas are trained professionals who provide continuous physical and emotional support,<br />
encouragement, and wisdom to moms and their partners during labor and birth. Postpartum doulas<br />
provide emotional and practical support to families as they transition to life with their new baby.<br />
The Parent/Child Education office maintains a list of certified birth doulas who provide services at<br />
PinnacleHealth, as well as general information about birth and postpartum doulas.<br />
To request this information, or if you have other questions regarding doulas, please call<br />
the PinnacleHealth Learning Institute at (717) 221-6255.<br />
The Parent Review<br />
PinnacleHealth offers a free weekly email for expectant and new parents to help guide you through<br />
pregnancy, labor and birth, and the first year of your baby’s life. Receive customized information,<br />
including tips, support, news, advice and resources.<br />
Register online at www.theparentreview.com/pinnacle.<br />
Wellness Phone Calls to New Moms<br />
A registered nurse from the WomanCare Resource Center will call new moms approximately<br />
two weeks following their discharge from Harrisburg Hospital. She will talk to you about your<br />
physical and emotional health, as well as the health of your baby. She will answer any questions<br />
that you may have and offer support in your new role as a parent.<br />
Perinatal Bereavement Services<br />
Education and support services are provided to those dealing with grief and loss related to<br />
pregnancy or childbirth. Call (717) 231-8844 for assistance.<br />
“Heartstrings”<br />
“Heartstrings” is a perinatal bereavement support group for those who have experienced a<br />
pregnancy loss or newborn death. You are welcome to come no matter where you are in your grief,<br />
or how long it has been since your loss. You may choose to talk or just listen. Some meetings<br />
include brief presentations, as well as time for sharing. Two registered nurses, who are also<br />
perinatal bereavement counselors, will facilitate the meetings.<br />
PinnacleHealth Community Campus<br />
4300 Londonderry Road, Harrisburg, PA 17109<br />
Fourth Tuesday of each month, 7-8:30 pm - Second floor, Conference Room 3<br />
December meeting is third Tuesday<br />
There is no charge and no registration is required. Call (717) 782-5906 or (717) 221-6268<br />
for more information.<br />
54<br />
Y O U R B A B Y ’ S B I R T H
New Mom Networks<br />
An informal time of sharing and support for new mothers. These groups are facilitated by an<br />
experienced nurse in maternal/child health, infant massage and lactation. Join other new moms<br />
and parents for one of these groups. No older children please.<br />
New Mom Network I<br />
For new mothers and their 0-9 month-olds<br />
1-2:30 p.m. FREE<br />
Every Monday: Linglestown GIANT Super Food Store Community Center<br />
Every Tuesday: Camp Hill GIANT Super Food Store Community Center<br />
New Mom Network II<br />
For mothers and their 10-16 month-olds<br />
1-2:30 p.m. FREE<br />
Every Monday: Linglestown GIANT Super Food Store Community Center<br />
New Mom Network III<br />
For new mothers and their 18-24 month-olds<br />
10-11:30 a.m. FREE<br />
Every Monday: Linglestown GIANT Super Food Store Community Center<br />
Working Moms Network (Evenings)<br />
Informally discuss the challenges of returning to the workplace, along with some tips on how to<br />
adjust. For moms who work outside the home and their babies. Facilitated by working moms.<br />
6-7 p.m. FREE<br />
Fourth Wednesday/month:<br />
Linglestown GIANT Super Food Store Community Center<br />
For more information about PinnacleHealth classes, programs and upcoming events,<br />
please call (717) 231-8900.<br />
Moms Navigating Through Life<br />
This is a therapy group dealing with the transition into and through all stages of motherhood.<br />
Dealing with role adjustments in relationships within the family and at work will be addressed. It<br />
will offer problem solving solutions to the demands of mothering at different stages from birth<br />
through the terrible teens. It is an opportunity to connect with others and realize that you are not<br />
alone. This group is facilitated by a licensed professional counselor.<br />
PinnacleHealth Psychological Associates, Harrisburg Campus, Brady Building $45/session.<br />
Most insurance plans cover the cost of group therapy.<br />
To register or for more information, call (717) 231-8360.<br />
55<br />
Y O U R B A B Y ’ S B I R T H
56<br />
Y O U R B A B Y ’ S B I R T H
Lactation Services<br />
PinnacleHealth promotes breastfeeding as a baby’s<br />
best start in life. We offer central Pennsylvania’s most<br />
comprehensive breastfeeding support services to<br />
help new moms initiate and maintain breastfeeding.<br />
Here are some of the key services provided:<br />
• Our Maternity Center nursing staff has specialized<br />
breastfeeding training, and is available 24 hours<br />
a day to evaluate, assist, and support breastfeeding<br />
moms and their babies.<br />
• Lactation consultants, professionally trained in the<br />
technique and science of breastfeeding, are available<br />
upon referral by the Maternity Center nursing staff,<br />
to assist mothers having difficulty breastfeeding or<br />
dealing with special needs. Our lactation consultants<br />
are certified by the International Board of Lactation<br />
Consultant Examiners (IBLCE).<br />
Additional Lactation Services<br />
at PinnacleHealth<br />
• Breastfeeding classes<br />
• In-hospital assistance and support<br />
• Information and assistance for new families with<br />
sick or premature babies in the Neonatal Intensive<br />
Care Unit (NICU)<br />
• Electric breast pump rentals and sales, call (717) 782-5372<br />
• At home information and support available by telephone<br />
• Outpatient visits, by appointment only, at the Harrisburg Hospital Lactation Center<br />
• Corporate lactation program<br />
• Professional lactation education<br />
Additional Information about Breastfeeding<br />
• Lactation Consultants at Harrisburg Hospital - (717) 782-5372<br />
• Breastfeeding Education - (717) 221-6255<br />
57<br />
Y O U R B A B Y ’ S B I R T H
Registration Information<br />
Early registration is suggested. Some classes fill quickly.<br />
Please contact your insurance company before you register to find out if they will<br />
reimburse you for classes.<br />
Full payment is required upon registration.<br />
By Telephone:<br />
• Contact the PinnacleHealth Learning Institute at: (717) 221-6255<br />
Monday through Friday, 8 a.m. – 3:30 p.m.<br />
• Credit Card payment will be accepted at time of registration<br />
OR<br />
• Check should be mailed upon completion of phone registration.<br />
By Mail:<br />
• Complete registration form.<br />
• Make check payable to: PinnacleHealth<br />
• Mail registration form and payment to:<br />
Parent/Child Education<br />
PinnacleHealth<br />
P.O. Box 8700<br />
Harrisburg, PA 17105-8700<br />
• Registration confirmation will be sent to you upon receipt of payment.<br />
Note<br />
• Full payment is required for all classes upon registration.<br />
• Cancellations prior to scheduled class will be given a full refund or rescheduled.<br />
• No-shows will forfeit one-half the class fee.<br />
• There will be a $20 charge for checks returned for insufficient funds.<br />
58<br />
Y O U R B A B Y ’ S B I R T H
Registration Form<br />
Please register early, as some classes fill quickly. Contact your insurance company before<br />
registering to find out if they will reimburse you for classes.<br />
Name<br />
<strong>Home</strong> Phone<br />
Partner’s Name<br />
Child(ren)’s Name and Age<br />
(For Sibling Class)<br />
Address<br />
City State Zip<br />
Phone (Work or cell)<br />
Doctor<br />
Email<br />
Due Date<br />
Program Starting Date Location<br />
❑ Baby Care Basics ____________________________ ___________________________<br />
❑ Becoming a Grandparent ____________________________ ___________________________<br />
❑ <strong>Birth</strong> Center Tour ____________________________ ___________________________<br />
❑ Breastfeeding Basics ____________________________ ___________________________<br />
❑ Cesarean <strong>Birth</strong> ____________________________ ___________________________<br />
❑ <strong>Childbirth</strong> Refresher ____________________________ ___________________________<br />
❑ CPR for Family & Friends ____________________________ ___________________________<br />
❑ Heartsaver AED/CPR ____________________________ ___________________________<br />
❑ Individualized <strong>Childbirth</strong> Class ____________________________ ___________________________<br />
❑ Individualized VBAC ____________________________ ___________________________<br />
❑ Lamaze ® <strong>Childbirth</strong> ____________________________ ___________________________<br />
❑ Pediatric First Aid ____________________________ ___________________________<br />
❑ Prepared <strong>Childbirth</strong> ____________________________ ___________________________<br />
❑ Prenatal Infant Massage ____________________________ ___________________________<br />
❑ Postpartum Infant Massage ____________________________ ___________________________<br />
❑ Siblings: “Babies and Toddlers” ____________________________ ___________________________<br />
❑ Siblings: “Babies and Big Kids” ____________________________ ___________________________<br />
❑ The Happiest Baby ____________________________ ___________________________<br />
❑ Twins, Triplets & More ____________________________ ___________________________<br />
❑ Weekend <strong>Childbirth</strong> Seminar ____________________________ ___________________________<br />
❑ Weekend Lamaze ® Seminar ____________________________ ___________________________<br />
❑ Online <strong>Childbirth</strong> Education Program ____________________________ ___________________________<br />
FULL PAYMENT IS REQUIRED UPON REGISTRATION.<br />
Payment Date: ____________________Enclosed Check #: ___________Amount:_________________<br />
Y O U R B A B Y ’ S B I R T H<br />
59
PinnacleHealth Locations<br />
PinnacleHealth Harrisburg Campus<br />
Brady Building<br />
205 South Front St., Harrisburg, PA 17104<br />
Park in the Visitor’s Parking Garage on Mary Street<br />
and follow signs to the Brady Building for classes.<br />
Tours meet in the Hospital Lobby.<br />
PinnacleHealth Cumberland Campus<br />
Fredricksen Outpatient Center<br />
2015 Technology Parkway,<br />
Mechanicsburg, PA 17050<br />
Exit onto Wertzville Road from I-81.<br />
Go to the first light and turn right on to<br />
Technology Parkway. Turn left at the sign<br />
for Fredricksen Outpatient Center.<br />
Make first right into parking lot by the<br />
Physician Office Building. Enter building<br />
and proceed to Conference Room G08,<br />
the first room on the left.<br />
The Community Center at Camp Hill<br />
GIANT Super Food Store<br />
3301 Trindle Road, Camp Hill, PA 17011<br />
Take I-83 to 581West. Take 581 West to<br />
exit 5A- North 11 & 15/Camp Hill.<br />
Camp Hill Shopping Center is on the left.<br />
GIANT Super Food Store is at the end<br />
near the intersection of Trindle Road.<br />
The classrooms are located on the second floor in The Community Center. As you enter the GIANT Super Food Store,<br />
bear left, passing Bucks County Coffee and the Marketplace Café. You will see the Cooking School to the right and stairs<br />
and an elevator to the left, which will take you to the second floor.<br />
The Community Center at Linglestown GIANT Super Food Store<br />
2300 Linglestown Road, Harrisburg, PA 17110<br />
Take I-83 to I-81. Take I-81 to Exit 69, Progress Avenue. Turn left onto Progress Avenue at the bottom of the exit ramp.<br />
Follow Progress Avenue North to Linglestown Road (Route 39). Turn left onto Linglestown Road. The GIANT Super Food<br />
Store is on the right in the Blue Mountain Commons Shopping Center. The classrooms are located on the second floor in<br />
The Community Center.<br />
60<br />
Y O U R B A B Y ’ S B I R T H
<strong>Your</strong> Hospital Stay
Checklist for Delivery<br />
Please complete the following information and place<br />
with your belongings to bring with you when you come<br />
to the hospital:<br />
❑ Insurance cards<br />
❑ Name and phone number of pediatrician or family<br />
practice physician who practices at PinnacleHealth<br />
and accepts your insurance to care for your baby in the hospital:<br />
❑ Any changes in your name, address, telephone number, or insurance information<br />
to give to Patient Access (717-782-5734) when you are admitted:<br />
❑ Information for your baby’s Social Security number:<br />
Mother<br />
Social Security number<br />
Date of birth<br />
Father<br />
Social Security number<br />
Date of birth<br />
❑ Infant car seat: Bring to your room after you are transferred to the postpartum floor.<br />
❑ Personal items needed after delivery. Please keep your suitcase and car seat<br />
in your car when you are in Labor and Delivery. <strong>Your</strong> support person<br />
can bring your suitcase and car seat to your room when you are transferred<br />
to the postpartum floor.<br />
61<br />
Y O U R B A B Y ’ S B I R T H
62<br />
Y O U R B A B Y ’ S B I R T H
<strong>Your</strong> Hospital Stay<br />
PinnacleHealth Harrisburg Campus<br />
Labor and Delivery is located on the eighth floor. Use the North Elevators (overhead sign) at the<br />
end of the hallway. Please press the button on the call box outside the doors and a nurse will let you<br />
in the unit.<br />
If you are not in labor and do not need assistance and arrive at the hospital<br />
between 5 a.m. and 8 p.m.:<br />
Park in the patient/physician garage, enter the hospital through the lobby, proceed through the<br />
main hallway and take the North elevators (at the end of the hall near the Emergency Department)<br />
to Labor and Delivery on the 8th floor.<br />
If you are in labor and need assistance and arrive at the hospital between 8 p.m. and 5 a.m.:<br />
<strong>Your</strong> labor partner may temporarily park at the Emergency Department drop-off. He or she may<br />
escort you to the labor and delivery suite on the 8th floor and then re-park in the patient/physician<br />
garage, which is accessible from Front Street.<br />
If you need assistance at any time, please come to the Emergency Department.<br />
63<br />
Y O U R B A B Y ’ S B I R T H
Prenatal Checklist<br />
❏ Check with your insurance company to find out what costs will and will not be covered.<br />
❏ Mail your pre-admission forms to the hospital as soon as possible, but no later than your sixth<br />
month of pregnancy. Please notify Patient Access (782-5734) if there are any changes in your<br />
name, address, phone number or insurance information as soon as possible.<br />
❏ Register for a childbirth class. PinnacleHealth offers six different types of childbirth classes at a<br />
variety of times and locations, in addition to classes on the care of your baby and new family.<br />
Some community organizations also offer classes.<br />
❏ Choose a pediatrician or family practice physician to care for your baby. Make sure he/she<br />
accepts your insurance and practices at PinnacleHealth.<br />
❏ Decide if you want your baby circumcised if he is a male, and check with your insurance<br />
company to find out if the procedure is covered.<br />
❏ Consider if you and your partner would like to have a doula with you through your labor.<br />
❏ Pack your suitcase prior to labor. See the list on the next page under “What to Bring.”<br />
❏ Bring all insurance cards with you to the hospital.<br />
❏ For the baby’s social security<br />
number, you will need the<br />
following information about both<br />
the mother and father of the<br />
baby: social security number,<br />
date of birth and place of birth.<br />
A paternity acknowledgement is<br />
also needed if the mother and<br />
father of the baby are not married.<br />
Fill out the birth certificate<br />
information and return it to your<br />
nurse or unit secretary before you<br />
leave the hospital.<br />
❏ Get a car seat that is new or less than six years old and have it installed in your car before<br />
coming to the hospital (call 1-800-SAFE-KIDS or log onto www.seatcheck.org to find a<br />
car seat technician in your area). If you have a used car seat, make sure it has never been in an<br />
accident. Bring your car seat to your hospital room after transfer to the Maternity Center.<br />
64<br />
Y O U R B A B Y ’ S B I R T H
What to Bring<br />
Whether you pack your bags weeks before your due date or right before you leave for Harrisburg<br />
Hospital, it is easy to forget important items. We encourage you to bring anything that will<br />
make you feel comfortable during your stay. However, we don’t recommend bringing valuable items.<br />
Here are a few items to keep in mind when packing your bags:<br />
• <strong>Your</strong> Baby’s <strong>Birth</strong> notebook<br />
• Camera and /or hand-held video camera<br />
• Heavy socks or slippers<br />
• Bed pillows<br />
• Snacks for labor partner (coffee shop and cafeteria are available with limited day and<br />
evening hours)<br />
• Bottle of bubbly cider to toast the new baby<br />
• Robe or nightgowns and underwear (keep in mind these may become permanently stained)<br />
• Hard candy or sour lollipops—sugarless will keep you from getting thirsty<br />
• Tennis ball in sock<br />
• Lip balm<br />
• Talcum powder<br />
• iPod (music)<br />
• Shower cap<br />
• Toiletries: mouth wash, shampoo, toothbrush, toothpaste, lotion, bar of soap, deodorant,<br />
hairbrush, make-up, hair dryer, curling iron, along with any other beauty and hygiene items<br />
you use regularly<br />
• Small amount of change<br />
• Going-home outfit for mom: loose, baggy clothes will feel most comfortable, nursing bra if<br />
you are breastfeeding<br />
• Going-home outfit for baby: stretchy suit, T-shirt, booties/socks, hat, 3-4 receiving blankets,<br />
warm blanket in cold weather, and/or outfit for baby’s first photo taken at the hospital<br />
• Snow suits, sweaters, blanket sleepers and buntings are not safe to use with car seats.<br />
• Infant car seat (PA law states babies cannot ride in a car without a federally approved car seat) —<br />
have your car seat installed before coming to the hospital in the back seat of the car<br />
(center position is safest) facing backwards. You may call the State Police or Safe Kids at<br />
(717) 531-SAFE to schedule your appointment for car seat installation on Tuesday or Thursday.<br />
Leave your suitcase and car seat in your car until after you have given birth and are moved to<br />
the maternity floor. Take only what you need for labor and delivery. Bring your car seat and suitcase<br />
to the room once you are transferred to the Maternity Unit.<br />
65<br />
Y O U R B A B Y ’ S B I R T H
Call <strong>Your</strong> Physician/Midwife When:<br />
• If you are a first time mother—when contractions are five minutes apart, last longer than a<br />
minute and have been this way for at least one hour.<br />
• If you’ve already delivered a baby—when your contractions are seven minutes apart and have<br />
been that way for one hour<br />
• <strong>Your</strong> membranes (bag of waters) rupture—note the color.<br />
• You have bright red bleeding<br />
• <strong>Your</strong> baby is moving less than normal<br />
• You have sharp, steady abdominal pain that does not come or go<br />
• You have fever, chills, backache and/or burning when you empty your bladder<br />
• You have nausea and vomiting lasting more than 24 hours<br />
• You have a headache or blurred vision<br />
Signs of Labor<br />
• Contractions (labor pains) may feel like cramping or back discomfort with a tightening of the<br />
abdomen<br />
• You may feel contractions in the abdomen, lower back or both<br />
• The pain from the contractions will come and go<br />
• Ruptured membranes is a loss of fluid from the vagina as a gush or slow leak—note the color of<br />
fluid and the time rupture of membranes<br />
• If you are already having contractions, when they become stronger, walking and talking will<br />
be difficult<br />
• You may have spotting in early labor if you have had a vaginal exam<br />
• Bleeding like a period is not normal and you should notify your physician or midwife immediately<br />
Coming To Labor And Delivery<br />
<strong>Your</strong> partner(s) is welcome to stay with you the entire time. When you arrive, the nurse will ask<br />
about your health history and the onset of labor. The baby’s heart rate and contractions will be<br />
monitored by electronic fetal monitoring. <strong>Your</strong> blood pressure, temperature and pulse will be<br />
checked, and a pelvic exam will be done to determine cervical dilation. You will have a chance to<br />
discuss your pain management preferences and ask questions during this time.<br />
Parking<br />
Park in the Patient/Physician Garage, off of Front Street or Second Street. The main support person<br />
with the white bracelet can get in and out of the parking garage without charge.<br />
66<br />
Y O U R B A B Y ’ S B I R T H
Visitation Policy For Labor And Delivery<br />
Antepartum Assessment Center:<br />
• Each patient in the Assessment Center is allowed one family/visitor/support person with her.<br />
• This family/visitor/support person will be given a “Labor & Delivery Visitor Pass.”<br />
• The family/visitor/support person is responsible for keeping the people in the waiting room informed<br />
of the patient’s condition.<br />
• The family/visitor/support person may “trade off” their pass to allow another person to see the<br />
patient. “Trading off” is to be done only with the patient’s permission.<br />
Labor/Delivery/Recovery Rooms (LDRs):<br />
• Each patient in an LDR is allowed three (3) family/visitor/support persons, at a time.<br />
• Each family/visitor/support person will be given a “Labor & Delivery Visitor Pass.” Any<br />
family/visitors/support persons beyond three will be directed to the waiting room and given the<br />
phone number for the patient’s room.<br />
• Family/visitors/support persons are responsible for keeping the people in the waiting room<br />
informed of the patient’s condition.<br />
• “Labor & Delivery Visitor Passes” may be “traded off” to allow different people to visit the patient.<br />
“Trading off” is to be done only with the patient’s permission.<br />
Postpartum Maternity Unit (delivered mothers and babies)<br />
• Visitors are welcome to visit from noon until 8 p.m., grandparents from 10 a.m. - 8 p.m.<br />
• All visitors should enter Maternity on the 9th floor through the secured access north entrance.<br />
This can be accessed by utilizing the visitor elevators in the North Elevator Lobby. There is no<br />
public access from the main entrance elevators to the 9th floor.<br />
• One support person (father of the baby or another adult) is allowed to remain after visiting<br />
hours and may also stay overnight.<br />
Children under the age of twelve (12) are not permitted to visit unless they are the patient’s<br />
own children.<br />
Recording <strong>Your</strong> Labor, <strong>Birth</strong>, Baby<br />
• Recording/Broadcasting any part of your labor, delivery or infant care is allowed if you get written<br />
permission from everyone who will be present during the birth, including your doctor/midwife<br />
and nurses. Ask your nurse for a permission form. Due to Federal Privacy Rules (HIPAA), you may<br />
take pictures or videotape your baby only. Taking pictures of other babies is not allowed.<br />
67<br />
Y O U R B A B Y ’ S B I R T H
Guide To Labor<br />
What To Expect<br />
Early Labor<br />
What is happening with your body:<br />
• Contractions are five minutes apart or longer<br />
• Cervical dilation progresses to about three or four centimeters<br />
The healthcare team will:<br />
• Encourage you to labor at home unless your water has broken or complications were identified in<br />
your pregnancy<br />
• Have you come to the hospital when contractions are five minutes apart<br />
• Admit you to the hospital and orient you to your birth room<br />
You and your partner can:<br />
• Enjoy walking together while you are at home<br />
• Use relaxation and breathing techniques<br />
• Eat light foods and drink fluids<br />
• Rock in rocking chair or walk<br />
• Bathe (if the bag of water has not broken) or shower<br />
Active Labor and Transition<br />
What is happening with your body:<br />
• Contractions will be stronger and five minutes apart or less<br />
• Cervix dilates to a maximum of 10 centimeters<br />
The healthcare team will:<br />
• Assist you with comfort measures and emotional support<br />
• Monitor contractions and progress of labor<br />
• Watch for problems with you or the baby<br />
• Use medical interventions as needed (see descriptions later in this section)<br />
• Offer pain medication if desired (see descriptions later in this section)<br />
You and your partner can:<br />
• Change positions frequently<br />
• Use relaxation/breathing<br />
• Apply comfort techniques learned in class<br />
68<br />
Y O U R B A B Y ’ S B I R T H
Second Stage - Pushing<br />
What is happening with your body:<br />
• Once the cervix is fully dilated, the baby comes down into the vagina as mother bears down with<br />
the contractions.<br />
The healthcare team will:<br />
• Adjust bed for your comfort<br />
• Clean perineum and inner thighs with warm water<br />
• Prepare for delivery<br />
You and your partner can:<br />
• Work with the contractions to bear down effectively<br />
• Adjust your position<br />
• Use the squatting bar<br />
Second Stage - <strong>Birth</strong><br />
What is happening to your body:<br />
• Baby’s head emerges first, then the shoulders and body are delivered.<br />
The healthcare team will:<br />
• Put the baby on your abdomen at birth<br />
• Monitor the baby’s condition<br />
You and your partner can:<br />
• Enjoy the birth of your baby<br />
• Take time to bond with the baby<br />
Third Stage - <strong>Birth</strong> of the Placenta<br />
What is happening to your body:<br />
• Contractions continue but milder than before.<br />
• You will push with contractions until the placenta is passed, usually within 30 minutes following<br />
the baby’s birth.<br />
The healthcare team will:<br />
• Guide you to push with contractions.<br />
• Examine the placenta to be sure all was passed.<br />
• Repair your perineum if necessary.<br />
• Clean perineum and make you comfortable.<br />
• Assist with breastfeeding.<br />
You and your partner can:<br />
• Celebrate your baby’s birth.<br />
• Bond as a family.<br />
• You are encouraged to breastfeed within the first hour and to have your baby skin-to-skin<br />
with you.<br />
69<br />
Y O U R B A B Y ’ S B I R T H
Medical Interventions<br />
There are a variety of medical interventions that may be ordered during your labor. Because we<br />
never know in advance exactly what procedures may be needed for your labor, it is helpful to discuss<br />
with your physician or midwife their thoughts about the need for these common procedures.<br />
IV<br />
An IV is inserted in the hand or arm to provide fluids and medication during labor. A pump is often<br />
used to control the exact amount given.<br />
Electronic Fetal Monitor (EFM)<br />
The External EFM is attached to the mother’s abdomen. One part of the monitor tracks the fetal<br />
heart rate and the other tells when the mother is having a contraction. This information is<br />
transmitted through wires to the main part of the monitor and printed on a graph. The Internal<br />
EFM is sometimes used instead of External EFM. The bag of water must be broken and the<br />
monitoring device inserted through the vagina to the uterus. There is a fetal scalp monitor, which<br />
attaches to the baby to monitor his/her heart rate. A separate catheter can monitor the strength<br />
of the mother’s contractions.<br />
Pitocin or “Pit”<br />
Pitocin is the synthetic form of the hormone oxytocin, which causes the contractions of labor.<br />
It is administered through an IV line. It is used to induce (or start) labor, to augment (strengthen)<br />
labor or given after delivery to keep the uterus firm.<br />
Episiotomy<br />
An incision may be made in the perineum between the vagina and the rectum at the time of birth.<br />
It is made by the physician or midwife to enlarge the vaginal opening and will be repaired with<br />
stitches after the baby and placenta are delivered.<br />
Vacuum Extractor<br />
A small suction cup can be placed on the baby’s head during the pushing stage. The physician<br />
applies pressure during the contraction to bring the head down for delivery.<br />
Forceps<br />
A metal “spoon-like” instrument can be applied on either side of the baby’s head by the physician,<br />
which can then be positioned and brought down for delivery.<br />
70<br />
Y O U R B A B Y ’ S B I R T H
Pain Management<br />
PinnacleHealth uses a pain scale (see picture below) to measure your pain levels. Pain relief is<br />
available to you during labor, including both medication and medication-free comfort techniques.<br />
Some women prefer the advantages of using pain medications, while others prefer the advantages<br />
of natural childbirth (without using drugs). Be aware that pain medications are not usually given<br />
until labor has progressed to a certain point. Discuss your options with your healthcare provider<br />
and labor partner before your labor begins to find out what pain relief may be best for you.<br />
Advantages of pain medications:<br />
• Provides significant pain relief<br />
• Allows you to rest or sleep late in labor<br />
• Promotes muscular relaxation<br />
• Pitocin can be given to strengthen contractions without increasing your discomfort<br />
Advantages of natural childbirth:<br />
• Allows you to move and position freely<br />
• Decreases use of other medical procedures which may be used with pain medications<br />
• Provides sense of personal accomplishment<br />
• Enhances early breastfeeding with the delivery of a more alert baby<br />
Medication Options<br />
• Pain Medication<br />
Medicine can be given through an IV once you are in active labor and your cervix is progressively<br />
dilating. Giving the medication too early may cause contractions to slow down and affect the<br />
progress of your labor. Many women find that a dose of medication, such as Stadol, can provide<br />
just enough relief to “take the edge off” the contractions and give them a rest period.<br />
• Epidural Anesthesia<br />
An epidural will provide numbing from your waist down so the contractions will not feel as<br />
painful, although you may still feel some pelvic pressure. This type of anesthesia, given only by a<br />
doctor called an anesthesiologist, is administered by inserting a catheter into the epidural space<br />
in your spinal column. Again, your labor must be progressing to receive this type of pain relief.<br />
The epidural may be allowed to “wear off” when you are fully dilated so that you can feel your<br />
contractions and know when to push. Once you’ve received an epidural, you must stay in bed. If<br />
you have an epidural for labor and are unable to deliver vaginally, the epidural can be used as<br />
anesthesia for your cesarean section.<br />
71<br />
Y O U R B A B Y ’ S B I R T H
Medication-free Pain Management<br />
There are many comfort measures you can use to relieve pain throughout your labor. <strong>Your</strong> labor<br />
support partner and/or a Doula can be very effective in helping to keep you focused and in<br />
control, despite the pain of the contractions. Here are some techniques which are especially helpful<br />
in easing the discomforts of labor.<br />
• Relaxation and breathing<br />
• Supportive labor partner<br />
• Walking<br />
• Shower or jacuzzi<br />
• Rocking chair<br />
• Massage<br />
• Counter pressure<br />
• Soothing music<br />
• Position changes<br />
• <strong>Birth</strong> ball<br />
• Aromatherapy (candles are not allowed in the hospital)<br />
Cesarean Delivery<br />
Sometimes a cesarean section is planned during the pregnancy and scheduled in advance. Other<br />
times, it may occur as a result of conditions that happen during labor. In either case, it is valuable<br />
for the mother to be fully informed of the reasons for the cesarean and be aware of what will happen<br />
during this procedure. Some common reasons for cesarean sections include: fetal stress, extended<br />
length of labor, unusual position of the baby or maternal conditions.<br />
A cesarean section is a surgical delivery of the baby through the abdominal wall and uterus.<br />
It occurs in approximately one in four deliveries and is done by an obstetrician in a surgical room in<br />
the Labor and Delivery suite. One labor partner will usually be able to stay with you during the<br />
surgery. Cesareans are usually done with spinal anesthesia while the mother is awake. In some<br />
cases (usually emergencies), general anesthesia may be used and the mother will not be awake.<br />
A neonatologist/CNP and obstetrical nurse will be available to care for the baby at delivery.<br />
After the delivery, the mother will be transferred to the obstetric recovery room for about one hour.<br />
The baby will stay with the mother as long as the baby is stable. The hospital stay after a cesarean<br />
is three to four days.<br />
Vaginal <strong>Birth</strong> After a Cesarean (VBAC)<br />
If you had a cesarean section with a previous delivery, you may be able to deliver vaginally with<br />
this pregnancy. This should be discussed early in pregnancy to be sure your physician is supportive.<br />
You will need to sign a specific consent form if you plan to attempt a VBAC.<br />
72<br />
Y O U R B A B Y ’ S B I R T H
<strong>Your</strong> <strong>Birth</strong> Plan<br />
Are you in the early weeks of your pregnancy, thinking about baby names, or nearing the home<br />
stretch of your pregnancy, getting your nursery ready Now is the time to be thinking about your<br />
birth preferences.<br />
What is a <strong>Birth</strong> Plan<br />
The term birth plan can actually be misleading. It’s less an exact plan than a list of your preferences<br />
concerning your labor, birth and hospital stay. A birth plan isn’t a binding agreement, but rather a<br />
guideline of your wishes for your healthcare providers.<br />
Why have a <strong>Birth</strong> Plan<br />
A birth plan isn’t a must, and it is fine if you don’t want to write one. Many couples don’t bother<br />
with a birth plan because they are comfortable trusting their healthcare providers to help them<br />
make appropriate choices as the need arises. Other couples have strong opinions and expectations<br />
they want to share with their caregivers.<br />
Where to start<br />
Spend some time together thinking about and prioritizing what you want. Consider the options<br />
available to you that may be discussed in your childbirth class or hospital tour. While forming a birth<br />
plan, you will also obtain more knowledge regarding the labor and birth process.<br />
What questions does a <strong>Birth</strong> Plan answer<br />
1. What are your preferences during a normal labor and delivery<br />
2. What are your wishes for your baby’s care in the first few days after birth<br />
3. What would you like to happen in case of unexpected events<br />
While in labor, be flexible and keep an open mind. Remember, a birth plan isn’t a guarantee that<br />
your birth will go just as you planned it. By educating yourselves in advance, you will be less fearful<br />
and more empowered to make the best choices for you and your baby.<br />
You may choose to use the following birth plan (on next page).<br />
73<br />
Y O U R B A B Y ’ S B I R T H
74<br />
Y O U R B A B Y ’ S B I R T H
My <strong>Birth</strong> Plan<br />
Date:<br />
I, ______________________, am creating this birth plan prior to my labor to make my wishes clear<br />
to my doctor/midwife, and the nurses at the hospital. These are the items I feel are important<br />
regarding the birth of my unborn baby, and would like them to be followed as closely as possible<br />
whenever possible. I understand a circumstance might come up where either I may want to<br />
change my mind, or my doctor/midwife suggests that it is in my best interest to deviate from my<br />
birth plan. I will be flexible, however request to be kept informed of every aspect of my labor<br />
My name:<br />
My due date:<br />
My provider’s name:<br />
My birth partners’ names:<br />
Environment: (Check all that are your requests)<br />
❏ To control the temperature, lighting and sounds/music in my labor room<br />
❏ Please allow all visitors to come and go as they please (up to three at a time)<br />
❏ I only want visitors during the early stages of labor<br />
❏ No visitors except for my birth partner(s)<br />
❏ Do not allow these people:__________________<br />
❏ My doula/childbirth educator will be present.<br />
Comfort Measures:<br />
❏ Ice chips/clear liquids by mouth<br />
❏ Position changes/walking for comfort<br />
❏ Shower/jet tub to relieve pain<br />
❏ Massage/breathing techniques<br />
Pain Management:<br />
❏ No medication at all: I want a drug-free birth<br />
❏ Shots through the IV of medications such as Stadol<br />
❏ An epidural when in active labor<br />
Delivery:<br />
❏ To use the birthing position of my choice<br />
❏ To use self-directed pushing<br />
❏ To used coached/directed pushing techniques<br />
❏ An episiotomy only if necessary<br />
75<br />
Y O U R B A B Y ’ S B I R T H
Immediately After Delivery:<br />
❏ Lay my baby on my abdomen/chest immediately<br />
❏ Clean up my baby before placing him/her on my chest<br />
❏ Delay cord clamping until pulsation stops<br />
❏ My partner wants to cut the umbilical cord<br />
❏ We are banking the cord blood<br />
❏ To breastfeed my baby as soon as possible in Labor and Delivery<br />
❏ Delay antibiotic eye ointment up to one hour<br />
❏ I want visitors to see us in Labor and Delivery<br />
❏ Just the new family in Labor and Delivery<br />
Cesaerean Section:<br />
❏ I want to be awake for my C/S<br />
❏ _______________will be my partner for my C/S (one only)<br />
❏ Want to see/hold my baby in the operating room<br />
❏ Have my baby skin-to-skin in the recovery room so I may bond/breastfeed<br />
❏ Wait until I am situated in my room before my baby is brought to me<br />
Postpartum Care:<br />
❏ I__________________will be staying overnight in my room (one only)<br />
Newborn Care:<br />
❏ Breastfeeding only<br />
❏ Breastfeeding and supplementing with formula<br />
❏ Formula feeding only<br />
❏ No pacifiers or artificial nipples given to my breastfed baby<br />
❏ Circumcise my newborn son<br />
❏ No circumcision<br />
Other:<br />
Thank you for taking the time to read my birth plan, which I have shared with my healthcare provider.<br />
Please keep me informed of anything that comes up that might cause me to deviate from it.<br />
Sign<br />
Date<br />
76<br />
Y O U R B A B Y ’ S B I R T H
Care for You & <strong>Your</strong> Baby Following <strong>Birth</strong><br />
After months of waiting, your baby is finally here and eager to adjust in his new world. Our doctors<br />
and nurses will do everything possible to make sure your baby’s adjustment to life after birth is a<br />
smooth and healthy one.<br />
Newborn Care in Labor and Delivery<br />
The first few hours of life are known as transition. After your baby is born, he will be placed<br />
skin-to-skin with you to help him during transition as he adjusts his breathing, heartbeat,<br />
blood sugar and body temperature after birth. You and your baby will snuggle and have the<br />
opportunity to breastfeed for the first time. You and your family can begin to bond to your baby<br />
and get to know him as you welcome him.<br />
While in Labor and Delivery, your nurse will continue to care for your baby including:<br />
• Assess baby’s transition to life after delivery<br />
• Weigh and measure baby<br />
• Help with breastfeeding<br />
• Test baby’s blood sugar, if needed<br />
Newborn Care on the Postpartum Unit<br />
You and your baby will be transferred to the Maternity Center on the 9th floor about two hours after<br />
birth to continue transition. <strong>Your</strong> nurse will care for both you and your baby.<br />
<strong>Your</strong> baby will complete his transition in your room and will remain with you until the time of<br />
discharge. There are many benefits of uninterrupted contact between baby and family:<br />
• Supports family centered maternity care<br />
• Nurtures baby’s transition to life after delivery<br />
• Supports skin-to-skin care<br />
• Helps baby and mother learn to breastfeed successfully, learn feeding cues, and feed baby as<br />
soon as he is hungry, especially at night<br />
• Allows mother and father get to know their baby, bond and develop their role as parents<br />
• Increases your self-confidence in caring for your baby<br />
• Provides quality time to learn how to care for yourself and your baby<br />
• Prepares you to go home and continue your life as a family<br />
After you and your baby are transferred to postpartum, your baby will have assessments, routine<br />
care supported by your nurse and his first bath in your room. Within 24 hours, your baby will have a<br />
physical exam done by your pediatrician. One benefit of your baby transitioning in your room is<br />
that your baby will remain skin-to-skin with your or your support person. In addition to helping your<br />
baby regulate his breathing, heart rate, body temperature and blood sugar, a baby who is skin to<br />
skin often cries less and can breastfeed when he is ready to eat.<br />
• Until you can walk independently, it is helpful to have a support person with you<br />
• It is important that you or your support person hold your baby skin-to-skin to maintain his body<br />
temperature<br />
• You or the person holding your baby skin-to-skin will need to be awake<br />
• <strong>Your</strong> visitors will be able to hold your baby once transition is complete<br />
77<br />
Y O U R B A B Y ’ S B I R T H
While you are in the hospital, your baby’s care will be done in your room. This allows you to watch,<br />
participate, and learn about his care without being separated from him. You can maintain<br />
skin-to-skin contact with your baby during rest, feeding, assessments and care as much as possible.<br />
Some care that we will provide in your room includes:<br />
- Newborn assessment<br />
- Monitoring of vital signs and adaptation to life after delivery<br />
- Promotion and support for breastfeeding<br />
- Newborn bath when his temperature is stable, and he has had at least one successful breastfeeding<br />
- Continued skin-to-skin after bath to keep him warm<br />
- Blood sugar monitoring, if indicated<br />
- Collection of newborn screen and other specimens<br />
- Hepatitis B vaccine<br />
- Promotion of parent-infant bonding<br />
Sleep is important for both parents and baby. We encourage you to sleep when your baby is<br />
sleeping, both in the hospital and after you go home. The Safe Sleep Initiative recommends that<br />
your baby sleeps on his back in the bassinet or crib. Anyone who becomes drowsy while holding<br />
your baby should place him in the bassinet to prevent injury and keep your baby safe.<br />
We encourage you to keep your baby with you throughout your hospital stay to help you to bond<br />
with your baby, know him, learn his routines and how to care for him. However, if either you or<br />
your baby has a problem at any time during your hospital stay, your baby may need to be cared for<br />
in the Newborn Nursery or in the Neonatal Intensive Care Unit (NICU). <strong>Your</strong> nurse will assist<br />
you to spend time with your baby in the NICU. <strong>Your</strong> baby will be brought to your room when the<br />
problem improves.<br />
Congratulation on the birth of your baby and becoming parents!<br />
78<br />
Y O U R B A B Y ’ S B I R T H
Visiting Hours on Postpartum<br />
Try to keep visitors to a minimum so that you and your partner can get some rest and get to know<br />
and care for your baby.<br />
Length of Stay<br />
The average length of stay is two days for vaginal delivery or three to four days for cesarean. If you<br />
are interested in going home before 24 hours, discuss early discharge with your physician or<br />
midwife and pediatrician in advance. You would need to arrange for help at home. A home visit<br />
from a nurse can be arranged through the agency of your choice. Some insurance plans may cover<br />
this. Check with your insurance company.<br />
<strong>Your</strong> Baby’s Stay<br />
Now that your baby is born, your baby is depending on you to care for his/her every need. Not only<br />
is this a time to bond with your baby, but also a time to learn your baby’s personality and to<br />
develop routines that work well for both of you.<br />
<strong>Your</strong> support person, with the white ID band, may visit any time. Brothers and sisters of the baby,<br />
grandparents and other visitors can come to see you and your baby between noon and 8 p.m.<br />
Visitors and family should use the elevators in the North Lobby of the hospital (near the Emergency<br />
Department) when they come to visit. Family or friends who are ill or have a cold should not visit.<br />
Remind your visitors to wash their hands before holding your baby. Children, other than brothers<br />
and sisters of the baby, who visit must be 12 years of age or older.<br />
Infant Treatments and Screenings<br />
There are a number of treatments that are done in the first hours or days after birth for every baby.<br />
Eye Prophylaxis<br />
Medication is placed in the infant’s eyes to prevent infection or blindness from gonorrhea and<br />
chlamydia infections.<br />
Foot Printing and Identification Bands<br />
This is done in the birth room or delivery room for the identification of the infant.<br />
Vitamin K<br />
An injection into the baby’s thigh muscle is given to prevent internal bleeding.<br />
Hepatitis B Vaccination<br />
Many pediatricians recommend starting Hepatitis B vaccine in the hospital. This is a series of<br />
three injections to immunize the child against Hepatitis B. The other two injections will be given at<br />
the pediatric visit at two and six months.<br />
Newborn Metabolic Screening<br />
A small amount of blood is taken from the infant’s heel and applied to a special card. It tests for<br />
these conditions: phenylketonuria (PKU), hypothyroidism, sickle cell, galacosemia and congenital<br />
adrenal hyperplasia, Maple Syrup Urine Disease and other genetic disorders. Many of these<br />
diseases can be treated before problems occur.<br />
79<br />
Y O U R B A B Y ’ S B I R T H
Bilirubin Screening<br />
At 24 hours of age, your baby will be screened for newborn jaundice. In the first two to five days<br />
after birth, some babies may develop a yellow to orange color in their skin and whites of their eyes.<br />
This color is caused by bilirubin, the normal product of the breakdown of red blood cells, which is<br />
usually harmless. Babies have extra red blood cells before they are born to make sure they get<br />
enough oxygen. After they are born, they do not need the extra red blood cells. When their bodies<br />
break down the extra red blood cells, their livers may not be able to excrete the extra bilirubin that<br />
colors their skin (jaundice). Sometimes jaundice is also caused by a difference in blood types<br />
between mom and baby or by illness.<br />
The physicians and nurses will watch for jaundice and will test your baby for her bilirubin level.<br />
They may use a light test on your baby’s forehead and/or may prick your baby’s heel for a blood test.<br />
If bilirubin builds up too high in the body, your baby will be treated with special blue lights<br />
(phototherapy) or a “bili-bed” and extra fluids to prevent damage to nerve cells in her brain. This<br />
treatment usually lasts a few days. If your baby needs light treatment, your physician and nurse will<br />
give you more information.<br />
If your baby goes home with jaundice, he should be seen by a pediatrician within one to two days.<br />
<strong>Your</strong> physician will tell you what to watch for and when to call the office. You should always call<br />
your physician if your baby seems sick, more yellow, or seems too sleepy to wake for feedings every<br />
two to four hours.<br />
Hearing Screening<br />
Some babies are born with hearing problems. The only way to detect a problem is through<br />
screening. <strong>Your</strong> baby will be screened in the nursery before leaving the hospital. If your baby<br />
passes the hearing screening, you do not need to do any more testing at this time. A small number<br />
of babies who pass the screening at birth can lose their hearing before one year of age or older.<br />
Some babies develop hearing loss later as a child. If you are concerned about your child’s hearing,<br />
talk with your child’s doctor. If your baby does not pass the hearing screening, you should get<br />
another screening. There may be several reasons why your baby does not pass the screening: she<br />
may have permanent or temporary hearing loss; she may be too active or awake during the<br />
screening; or the nursery may be too noisy to get good results. If you have any questions or<br />
concerns or need another screening for your baby, talk with your baby’s doctor.<br />
NICU<br />
A Neonatal Intensive Care Unit (NICU) is available for premature and ill infants. Neonatologists,<br />
specially trained nurses and respiratory therapists care for babies in the NICU. The family is given<br />
individual attention from a caring staff in a friendly atmosphere. Parents are encouraged to spend<br />
time with the baby, and mothers are encouraged to breastfeed. Breast pumps are available for<br />
nursing mothers. Skin-to-skin kangaroo care may be provided by parents, depending on the infant’s<br />
condition. You will be given more information about the NICU if your baby needs to stay there for any<br />
length of time. For more information about the NICU, call the clinical nurse specialist at 782-5282.<br />
80<br />
Y O U R B A B Y ’ S B I R T H
<strong>Your</strong> Going <strong>Home</strong> Guide
<strong>Your</strong> Going <strong>Home</strong> Guide<br />
Discharge Plans<br />
Discharge planning begins with the birth of your baby. Our healthcare team will work with you and<br />
your family to identify your needs to provide a smooth homecoming.<br />
On the Day of Delivery<br />
Infant Car Seat<br />
• Bring your car seat to your hospital room following transfer to the Postpartum Maternity Unit.<br />
• Make sure you are familiar with the operation and/or adjustment of your car seat before you come<br />
to the hospital.<br />
• Bring a baby outfit for your baby’s pictures.<br />
Day Before Discharge<br />
• Take home as many belongings as possible (flowers and gifts, etc.).<br />
• Turn in birth certificate and paternity papers, (if applicable).<br />
• Verify with your nurse that all baby’s blood work and vaccinations have been done (NeoGen and<br />
PKU screening, Hepatitis B vaccine). Make sure your baby’s hearing test is done.<br />
• A photographer will stop by your room with information about baby pictures. Please have your<br />
baby dressed in the outfit you want for the picture.<br />
Day Of Discharge<br />
• <strong>Your</strong> doctor will come to your room to discharge you. <strong>Your</strong> pediatrician will discharge your baby.<br />
• <strong>Your</strong> nurse will review discharge instructions with you. You will need to sign the instruction<br />
sheet, and your baby’s bracelet will be removed to keep with his hospital records.<br />
• <strong>Your</strong> support person will take the last of your belongings to the car. Once you are discharged,<br />
your support person may bring the car around to the main entrance of the hospital and wait for<br />
the nurse to bring you and your baby down in a wheelchair.<br />
General Information<br />
• The average discharge time is between 10 a.m.<br />
and noon. Please ask your support person<br />
to be at the hospital by 9 a.m.<br />
• Remember, FREE parking is only<br />
available for the support person<br />
wearing an ID bracelet. All other<br />
visitors must pay for parking<br />
upon leaving the parking garage.<br />
81<br />
Y O U R B A B Y ’ S B I R T H
Layette and Nursery Needs<br />
The following list of items should only be used as a guideline. <strong>Your</strong> baby can get by with fewer<br />
than the number of clothing and bedding pieces listed. Keep in mind, fewer articles just mean more<br />
frequent laundering.<br />
Layette Needs:<br />
• 4-6 undershirts<br />
• 4-6 bodysuits (onesies)<br />
• 4-6 sleeping gowns<br />
• 2-3 pairs of booties or socks<br />
• 2-3 sweaters or sweatshirts<br />
• 4 bibs<br />
• 1 or 2 hats or bonnets<br />
Bath Supplies:<br />
• 4 washcloths<br />
• 2-3 hand towels<br />
• 2-3 bath towels<br />
• Brush and comb<br />
• Emory board for nail filing<br />
Toiletries:<br />
• Q-tips or cotton balls<br />
• Mild baby soap and shampoo<br />
• Petroleum jelly<br />
• Diaper rash ointment<br />
Diapers:<br />
A newborn needs to be changed 10-12 times a<br />
day for the first month. Be sure to cleanse your<br />
baby’s bottom with diaper wipes or a washcloth<br />
and warm water with every diaper change.<br />
• Cloth Diapers: four or more dozen. If you use<br />
a diaper service or combine with disposables,<br />
you will need half this amount.<br />
• Disposables: about 300 for the first month if<br />
you mainly use disposables.<br />
Layette and Nursery Needs<br />
For the safety of your baby, DO NOT use pillows, quilts, bumper pads and stuffed animals in the crib<br />
or bassinette.<br />
•Crib (if using an older crib, make sure the crib<br />
slats are no more than 2-3/8 inches apart and<br />
that it is painted with lead-free paint)<br />
• Mattress (make sure it fits snugly in the crib)<br />
- Do not use bumper pads<br />
- Do not place toys or stuffed animals in<br />
crib/bassinette<br />
• 2-3 crib sheets<br />
• 6 small waterproof pads<br />
• 4-6 receiving blankets<br />
• Dressing or changing table<br />
• Laundry hamper<br />
• Diaper pail<br />
• Infant carrier seat<br />
• Electronic thermometer<br />
• Diaper bag<br />
• Chest of drawers<br />
• An infant car seat that meets the Federal<br />
Motor Vehicle Safety Standard 213<br />
Miscellaneous extras include:<br />
• Record book<br />
• Nursery lamp<br />
• Crib mobile<br />
• Toys<br />
• Wall pinups<br />
• <strong>Birth</strong> announcements<br />
• Stroller or carriage<br />
• Portable baby bed<br />
• Baby carrier (sling/snugly)<br />
• Feeding equipment for the first few months:<br />
- If breastfeeding and planning to return to work,<br />
plastic containers and lids to store breast milk.<br />
- If formula feeding, eight bottles, nipples and<br />
bottle covers, bottle and nipple brush, and<br />
formula. Check with your pediatrician about<br />
which formula to buy.<br />
Please see Resource Section in the back<br />
of this manual for safe sleep practices for<br />
your infant.<br />
82<br />
Y O U R B A B Y ’ S B I R T H
How to Care for <strong>Your</strong> Baby<br />
Remember, your baby’s body is adjusting to its new environment outside the womb. Everything is<br />
new. Expect it to take time for your baby’s body to adapt to both you and its new surroundings.<br />
Eyes: Shortly after birth, babies can focus at a distance of 10-12 inches. At birth your baby’s eye<br />
muscles are not coordinated and so his/her eyes may appear crossed. By three months, muscle<br />
coordination and strength will improve, and your baby will be able to focus quickly.<br />
Sleep: Babies sleep an average of 15-18 hours a day in the first few months. A day and night<br />
schedule will be developed in about five to six weeks. When putting your newborn down to sleep,<br />
position her on her back. After about four to seven months when your baby can roll over on her<br />
own, she will select her own sleeping position. To help your baby adjust to the difference between<br />
day and night, keep late night feedings as low-key as you can. During the day if your baby naps<br />
longer than three or four hours, it is okay to wake your baby up to play or eat.<br />
Newborn Skin: Dry skin is normal for newborns. A small amount of mild soap may be used. Do not<br />
use baby oil. Many babies develop a “newborn rash” which goes away in seven to 10 days and<br />
needs no treatment. Some babies may have milia, tiny white bumps, usually on baby’s nose,<br />
cheeks or chin. These will disappear without treatment. Do NOT squeeze them or use acne<br />
medicine.<br />
Cradle Cap: This is a yellow, flaky, waxy buildup that sometimes develops on a baby’s head. It is<br />
usually prevented by shampooing two to three times a week and combing your baby’s hair.<br />
Stools: For the first few days your baby will pass thick, dark, tarry “meconium” stools. Stools will<br />
change to a greenish color and then to a normal yellow. If your baby is breastfeeding, stools will<br />
most likely be frequent and “seedy yellow.”<br />
Newborn Behavior: <strong>Your</strong> baby is born with natural reflexes that improve as she grows and develops<br />
better muscle tone and coordination.<br />
• Grasp: Most babies have a strong grasp reflex and will eagerly grip your finger.<br />
• Startle: <strong>Your</strong> baby may throw her hands up whenever there is a loud noise, sudden movement or<br />
flash of light.<br />
• Rooting: When you touch your baby’s cheek, he may turn his head in that direction. When<br />
breastfeeding, stroke his cheek with your nipple to get him to turn his head in the direction of<br />
your breast.<br />
• Crying: All babies communicate by crying. After checking to see if your baby is hungry, wet or<br />
tired, there are a few tips that can help calm a crying baby.<br />
- Hold your baby skin-to-skin, covered by a warm blanket<br />
- Rock your baby<br />
- Gently pat your baby’s back or stroke her head<br />
- Wrap or “swaddle” your baby snugly in a receiving blanket<br />
- Sing a song or tell your baby a story<br />
- Play soft music<br />
- Take your baby for a walk or drive<br />
- Burp your baby<br />
- Give your baby a warm, relaxing bath<br />
Babies tend to cry less when their needs are met quickly. Try to remain calm and relaxed,<br />
because babies can sense your emotions. Never shake or hit your baby. If you need a break<br />
from a fussy baby, call a friend or relative for help.<br />
83<br />
Y O U R B A B Y ’ S B I R T H
• Sneezing: all babies sneeze because they are unable to blow or scratch their noses. Dust, lint or<br />
mucus may be the cause.<br />
• Stepping: Newborns push their feet against surfaces their feet touch. This produces a “creeping”<br />
motion, allowing your baby to creep to your breast after delivery.<br />
The time you spend holding, bathing, feeding and diapering your baby will provide many wonderful<br />
opportunities to bond. Holding your baby correctly helps your baby feel safe and comfortable.<br />
Holding<br />
It is important for your baby to feel comfortable, secure and supported when held. There are many<br />
ways to hold your baby. You may want to try the following techniques:<br />
• The traditional cradle hold may help your baby fall asleep. Support your baby’s head by resting<br />
it in the crook of your elbow.<br />
• Snuggle your baby near your heart. Hold your baby so his/her body faces yours and his/her head<br />
is turned sideways. Use one hand to support his/her neck and the other to hold his/her bottom.<br />
• You may want to try the “sitting” position by supporting the baby’s back with your forearms and<br />
holding his/her head in your hands, resting his/her legs against your chest. This will let you stare<br />
eye-to-eye with your baby.<br />
• The “football” hold can also be used. Sit in an upright position, placing the back of your baby’s<br />
head in your hand and your forearm supporting the spine. The baby is bent at her hips with her<br />
legs behind your back.<br />
Bathing<br />
• Wash baby in warm water in a room without drafts. Test temperature before placing baby in water.<br />
• Bathe baby every 1-2 days.<br />
• Use plain water on face and eyes.<br />
• Wash with a mild, fragrance-free and lanolin-free mild soap.<br />
• Wash hair by rubbing gently with baby shampoo or mild soap.<br />
• It is not necessary to use lotions or oils on baby’s skin.<br />
• The use of baby powder and cornstarch is not recommended.<br />
Diapering<br />
Every baby needs to have his diaper changed often. The average baby needs his diaper changed<br />
about 10 times a day. Frequent changing helps reduce the chance of diaper rash and keeps your<br />
baby happier. Never leave your baby alone while changing him. Gather all needed materials before<br />
you begin.<br />
As a new parent, you must decide if you want to use cloth or disposable diapers. Cloth diapers are<br />
softer against a baby’s skin, are less expensive, and are less harmful to the environment.<br />
Disposable diapers are more convenient and their plastic liners do a good job of protecting your<br />
baby’s bedding and clothing.<br />
• Cloth Diapers: if you use a diaper service, you can have your dirty diapers picked up and clean<br />
ones dropped off on a weekly or biweekly basis. Individual services have different rules to<br />
follow. If you wash the diapers yourself, separate them from the rest of your laundry, wash them<br />
in soap instead of detergent, don’t use fabric softeners and double rinse each load.<br />
• Disposable Diapers: be sure to change your baby’s diapers often and dispose of the diapers in<br />
the trash or in a diaper pail.<br />
84<br />
Y O U R B A B Y ’ S B I R T H
To change a diaper, first remove baby’s dirty diaper and gently clean diaper area with a diaper<br />
wipe or warm, wet washcloth. Be sure to wipe from front to back to reduce the risk of infection.<br />
Apply Vaseline, cream or ointment when needed. Place a diaper on your baby and fasten it so it is<br />
snug, but not pinching. Do not use baby powder, since your baby may breathe in the powder. It is<br />
important to wash your hands after each diaper change.<br />
• Diaper rash: if your baby has small, red bumps on her bottom, genitals, thigh folds or lower<br />
tummy near her diaper, she may have a diaper rash. Use an over-the-counter ointment<br />
or lotion that contains zinc oxide to help clear up the rash and keep your baby’s diaper loosely<br />
fastened, sometimes letting her “air-out” without a diaper. Call your baby’s doctor if the rash<br />
does not get better.<br />
Umbilical Cord Care<br />
Keep your baby’s umbilical cord clean and dry. If the cord becomes soiled with urine or stool,<br />
cleanse it with water. Do not use alcohol or other materials on the cord.<br />
Be sure to fold the diaper away from the umbilical cord to allow air movement. Normal healing of<br />
the cord may have a “mucky” or mucus appearance. If the skin around the umbilical cord is red, the<br />
cord begins to drain, or the cord has a bad odor, it may be infected. Take your baby’s temperature<br />
and call your doctor.<br />
Special Care for <strong>Your</strong> Baby Boy<br />
Uncircumcised Boy<br />
Be sure to wash the penis with soap and water every day including the underside of the scrotum.<br />
No special attention is needed, so don’t use cotton swabs or special cleansers, and don’t probe<br />
under the foreskin or try to push the foreskin back during cleaning.<br />
Circumcised Boy<br />
• Comfort measures include swaddling, rocking, holding, feeding and sucking<br />
• Observe for signs of infection: redness and swelling towards the shaft of the penis, or greenish<br />
yellow discharge. Call your baby’s doctor if you see any of these signs or if your baby does not<br />
urinate for 12 hours.<br />
• If your baby has a plastibell circumcision, wash his penis with water only for 3-4 days.<br />
Do not use petroleum jelly (Vaseline).<br />
• If your baby has a surgical method circumcision, apply petroleum jelly (Vaseline) around the<br />
penis. Gently wash penis with water only for 3-4 days.<br />
85<br />
Y O U R B A B Y ’ S B I R T H
Is <strong>Your</strong> Baby Sick<br />
Risk of Infection<br />
During the first 6-8 weeks of your baby’s life, she is at higher risk for infections. Help reduce your<br />
baby’s risk by asking everyone who holds your baby to first wash their hands. Try to limit your baby’s<br />
visitors. Friends or family who have been exposed to chicken pox in the last 7-21 days or have had<br />
a cold or flu should not visit. It is also best to keep your baby away from large crowds.<br />
Paying close attention to your baby’s behavior will help you know when she isn’t feeling well. If you<br />
notice any of these symptoms, call your baby’s doctor:<br />
• Fever of 100.4°F (under the arm) or higher<br />
• Vomiting<br />
• Refusing food several times in a row<br />
• Excessive crying<br />
• Listlessness<br />
• Loose running bowel movements with mucus or foul odor<br />
• Rash<br />
• Persistent coughing<br />
How to Take Baby’s Temperature<br />
The ability to take your baby’s temperature accurately will help you determine when your baby is<br />
sick. You can take your baby’s temperature under the arm (axillary).<br />
A normal range for an under the arm temperature is 97.6°F to 99.6°F. Place the tip of the<br />
thermometer under the baby’s arm while holding her arm to her side. Wait the appropriate amount<br />
of time, then remove the thermometer and read your baby’s temperature. If you do not have a<br />
digital thermometer, wait one to two minutes before removing the thermometer.<br />
86<br />
Y O U R B A B Y ’ S B I R T H
Feeding <strong>Your</strong> Baby<br />
How you feed your baby, whether by breast or by bottle, is your choice. Research the issue with an<br />
open mind, and make your decision based on what is best for you, your baby and your lifestyle.<br />
Breastfeeding Baby<br />
Breastfeeding is recommended by the American Academy of Pediatrics for at least one year.<br />
Benefits of Breastfeeding<br />
• Healthier babies<br />
• Fewer colds, ear infections and diarrhea<br />
• Fewer allergies<br />
• Promotes brain development and higher IQ<br />
• Promotes close bond with mother<br />
• Convenient—milk is always ready<br />
• Saves money—breast milk is free<br />
The Basics:<br />
PinnacleHealth offers a prenatal breastfeeding course which will answer your questions and<br />
provide accurate information on getting started breastfeeding. Call (717) 221-6250.<br />
Breastfeeding is the natural way for baby to feed. Here are some simple steps that will help you and<br />
baby get off to a good start:<br />
• Put your baby to breast as soon as possible after birth. The nurses in Labor and Delivery can<br />
help. Babies who go to the breast during the first hour of life do not always latch on but seem to<br />
have an easier time learning to feed.<br />
• Provide lots of skin-to-skin contact the first few days. This helps reduce stress hormones in<br />
baby’s body and encourages breastfeeding<br />
• The first three to five days baby will get colostrum which contains substances that prevent<br />
infection.<br />
• Baby may be very sleepy the first day and then do many small feedings at night. This is normal.<br />
Feeding at night helps your body produce more milk.<br />
• Keep baby with you as much as possible. Baby will give feeding cues, smacking his lips,<br />
hands to mouth or rooting when he needs to breastfeed.<br />
• Most babies lose weight the first few days. A loss of 8 to 10 percent of body weight is usually<br />
all right.<br />
• The more you breastfeed, the more milk you will make. Do not give formula unless ordered by<br />
your baby’s doctor.<br />
• Ask for help when needed. The nursing staff will help you learn to breastfeed.<br />
• Board certified lactation consultants are available and may visit during your hospital stay. If you<br />
have questions or problems, ask your nurse to notify them.<br />
• You may call the breastfeeding telephone warm-line with questions or concerns either before<br />
baby’s arrival or after discharge from the hospital at (717) 782-5372.<br />
Avoid use of alcoholic beverages because alcohol is concentrated in breast milk and its use can<br />
inhibit milk production. An occasional celebratory single, small alcoholic drink is acceptable, but<br />
breastfeeding should be avoided for two hours after the drink.<br />
87<br />
Y O U R B A B Y ’ S B I R T H
Feeding Baby:<br />
The time you spend breastfeeding your baby should be comfortable for both of you. Find a position<br />
that allows your baby to feed easily and for you to relax.<br />
• Cradle Hold: Sit comfortably with baby’s head in the crook of your arm and support your baby<br />
with your forearm. <strong>Your</strong> baby will lie tummy to tummy against you with her ear, shoulder and<br />
hip in alignment.<br />
• Football Hold: This is the best position for C-section moms. Sit in an upright position placing the<br />
back of your baby’s head in your hand with your forearm supporting her spine. The baby is bent<br />
at the hip with her legs behind your back. You may wish to use pillows to support baby.<br />
• Lying on Side: Lie on your side, supporting your head, knees and back with pillows. Lie your<br />
baby on her side facing you belly to belly. Place a blanket roll behind your baby’s back for support<br />
and either place your baby’s head on the bed or in the crook of your arm for support.<br />
Formula-feeding Baby<br />
Each baby develops different feeding habits. Don’t expect your baby to follow a textbook schedule<br />
and drink the same amount of formula, at the same time, every day.<br />
The Basics:<br />
• On average, after the first week, your newborn will take about 6-8 bottles a day with about 2 to 4<br />
ounces of formula in each.<br />
• There are several kinds of bottles and nipples on the market. Try different kinds until your baby<br />
finds one she likes best. Try to choose a nipple that matches your baby’s mouth size and level<br />
of development. The formula should be easy for your baby to suck without flowing too fast for<br />
your baby to keep up.<br />
Preparing Formula:<br />
• There are several recipes for formula. Check with your baby’s doctor to be sure that you’re giving<br />
your baby the best kind of formula for his digestive system. Be sure to follow the formula’s<br />
preparation and storage instructions carefully. Always wash your hands before preparing formula.<br />
It is best to boil clean bottles, nipples and equipment for five minutes to sanitize them before the<br />
first use. Boil water (including bottle or spring water) before using it to make formula from powder<br />
or concentrate; let it cool to 100°F. Be sure to accurately follow mixing instructions. Shake the<br />
bottle well before feeding. Warm the formula by placing the bottle in a cup or pan with warm<br />
water and be sure to test its temperature before feeding your baby. Never microwave prepared<br />
formula. Throw away any formula left in the bottle after your baby has eaten. Bottles at room<br />
temperature should be thrown away after one hour.<br />
Feeding Baby<br />
• Hold your baby close and cuddle during feedings. Rest your baby’s head in the bend of your<br />
elbow, facing your baby toward you. Touch the middle of your baby’s lower lip with the nipple of<br />
the bottle until she starts sucking. Tilt the bottle so the formula fills the nipple, to prevent excess<br />
air bubbles. Make sure your baby’s head stays slightly higher than her tummy, preventing the<br />
formula from draining into the ears and possibly causing an infection. Never prop the bottle<br />
in your baby’s mouth, because she can choke. Never put your baby to sleep with a bottle. The<br />
formula will stay in your baby’s mouth and cause damage to her teeth.<br />
88<br />
Y O U R B A B Y ’ S B I R T H
Burping Baby<br />
• Air bubbles may get trapped in your baby’s stomach. You may need to burp your baby once or<br />
twice during feedings and again when finished. Use gentle patting and rubbing motions when<br />
burping your baby and don’t forget a burp cloth — babies frequently spit-up while burping.<br />
There are three common ways to burp your baby. Try them all, and if one doesn’t work, switch.<br />
• The “classic” burping position is to hold your baby on your shoulder with her body facing yours.<br />
Gently pat and rub your baby’s back to burp.<br />
• Lay your baby facedown on your lap and gently rub her back.<br />
• Set your baby on your lap, supporting her chest and chin with one hand and lightly pat her back<br />
with the other.<br />
• Sometimes babies do not burp at every feeding.<br />
Spit-Up<br />
It is common and normal for babies to spit-up a little of their food with a burp. Babies will begin to<br />
hold down their food as they grow. If you think your baby is spitting up whole feedings or if her<br />
spit-up becomes forceful, call your baby’s doctor.<br />
Cereal and Solid Food<br />
Introducing cereal too soon can increase the chance of your baby developing allergies. DO NOT<br />
give your baby any cereal, solid food or liquids other than breast milk or formula until your<br />
pediatrician tells you. Most pediatricians begin babies on cereal at four to six months.<br />
Caring for Mom’s Body<br />
Follow-up Care<br />
You will need to schedule a follow-up appointment with your doctor or midwife between four and<br />
six weeks after delivery. Depending on your needs, your healthcare provider may check your blood<br />
pressure, weight, breasts for abnormalities, and your reproductive system to be sure your body is<br />
healing properly.<br />
<strong>Your</strong> Healing Body<br />
<strong>Your</strong> body has been through many changes during pregnancy. As your body heals after delivery, it<br />
will slowly return to how you remember it. It is important to remember that everyone’s body heals<br />
from pregnancy and birth at a different pace. Don’t expect too much, too fast. Keep in touch with<br />
your healthcare provider to be sure your body is healing properly.<br />
• Episiotomy or Tear Resulting from Vaginal <strong>Birth</strong><br />
It takes several weeks for your episiotomy sutures to be absorbed into your body. To help promote<br />
healing, relieve discomfort and keep your perineum clean, sit in a tub of warm water twice a day<br />
for 10-15 minutes at a time.<br />
• Abdominal Incision Following a Cesarean <strong>Birth</strong><br />
If you have staples in your incision, your healthcare provider will remove them from 4-7 days after<br />
delivery. If you have stitches, they will become less noticeable in 1-2 weeks and can take up to<br />
two months to absorb into your body. The steri-strips that may cover your incision will fall off on<br />
its own. To help keep the incision area dry and clean, wash gently with soap and water, rinse<br />
well, and carefully pat dry.<br />
89<br />
Y O U R B A B Y ’ S B I R T H
• Vaginal Bleeding<br />
Bleeding may last anywhere from less than one week to six weeks or more. Small clots (up to<br />
thumb size) are okay. The amount of bleeding should lessen each week and fade in color from red<br />
to pink then brown, tan and then white. Use sanitary napkins for the first six weeks. Do not use<br />
tampons during this time. Increased activity will cause increased vaginal drainage. If this flow<br />
persists and you soak two or more pads in an hour, call your doctor immediately. If your discharge<br />
becomes foul smelling or accompanied by a fever greater than 100.4°F, notify your doctor.<br />
• Menstruation<br />
<strong>Your</strong> body is going through a lot of changes. It may take time for you to adjust to your prepregnancy<br />
cycle. If you are bottle feeding, you will probably get your period 4-8 weeks after<br />
delivery. If you are breastfeeding your baby, you may get your period anywhere from six weeks to<br />
three months after delivery. It may take as many as 18 months for your body to return to a normal<br />
menstrual cycle. Keep in mind that your first menstrual period may be heavier and last longer<br />
than your pre-pregnancy cycle.<br />
• Constipation<br />
The following suggestions may help you avoid constipation:<br />
• Drink eight glasses of water a day.<br />
• Take dietary fiber (whole grain cereal, whole wheat bread) or supplemental fiber<br />
(Citrucel, Metamucil).<br />
• Eat citrus fruits, dates and prunes.<br />
• Avoid harsh laxatives. Laxatives such as Doxidan, Senokot and Milk of Magnesia may be<br />
taken as needed.<br />
Resuming Normal Activities<br />
Now that you have delivered your baby, you may be starting to feel better and want to resume<br />
your normal activity level. Don’t feel like you have to tackle the world again right away. It will<br />
take time for your body to return to your regular activity level (about four weeks after a vaginal<br />
birth and six weeks after a Cesarean birth).<br />
Avoiding the “Superwoman Syndrome”<br />
Gradually resume your household activities. Avoid lifting anything heavier than your baby.<br />
Avoid excessive stair climbing, bending and stooping. Accept offers of help from family and<br />
friends to prepare meals and help with housework.<br />
Slowing Down the Social Butterfly<br />
• Make a new message for your telephone and let callers know that you are resting and will return<br />
their calls later.<br />
• Put a note on the door saying that you are sleeping and to please call to set up a time to visit.<br />
• You may drive one week after a vaginal birth and two weeks after a Cesarean birth and are no<br />
longer taking narcotic pain relievers.<br />
• Avoid driving and traveling for long periods.<br />
90<br />
Y O U R B A B Y ’ S B I R T H
Time to Rest, Relax and Heal<br />
• Try to take naps when your baby is sleeping<br />
• Get plenty of rest during the first 30 days. Complete rest for these first few weeks will allow your<br />
body to recover more quickly and naturally.<br />
• Don’t feel hesitant to ask your doctor for pain relief if necessary.<br />
• Contact WomanCare Resource Center for information about perinatal massage to help you rest,<br />
relax and heal.<br />
Personal Care<br />
• You may find that the best time for personal care is after your baby’s first morning feeding.<br />
• You may take showers immediately after delivery.<br />
• You may take 15-minute baths following a vaginal birth and two weeks after a Cesarean delivery.<br />
Healthy Living<br />
Nutrition<br />
Maintaining good nutrition after delivery is important in helping your body return to normal and<br />
promote healing. Do not diet during the first six weeks. Eat a well-balanced diet including meats,<br />
fruits, vegetables, dairy products and breads. Try to limit sweets and high-calorie foods, but feel<br />
free to snack on nutritious foods if you get hungry between meals. Continue taking prenatal<br />
vitamins because they provide your body with the vitamins and minerals it needs to recover.<br />
Breastfeeding moms should continue taking prenatal vitamins until the baby is weaned. Bottle<br />
feeding moms should discuss with the doctor how long to continue taking prenatal vitamins.<br />
Postpartum Weight Loss<br />
• Wait six weeks before attempting to drop pounds - your body needs time to recover, and you<br />
need the energy to keep up with the needs of a new baby. You may lose some of the weight in<br />
these weeks without intentional dieting.<br />
• Follow the food guide pyramid - it will guide you to getting all the nutrients you need. If you are<br />
breastfeeding, be careful not to be too restrictive — your baby is depending on you. A drastic<br />
reduction in your intake may decrease your milk supply. Breastfeeding can require 500 calories or<br />
more per day, so you are likely to see weight loss without cutting back.<br />
• Focus on fruits and vegetables - these foods are a key to a healthy diet. They provide maximum<br />
nutrients with minimum calories.<br />
• Choose non or low fat dairy products and whole grain breads - these foods will meet your<br />
nutritional needs and help you to feel satisfied without empty calories.<br />
• Stay hydrated, drink water - your body needs at least eight cups of fluid per day, and water is a<br />
great choice. If you are nursing, it is likely you will need more, so let your thirst be your guide,<br />
and always keep a glass of ice water by your side when breastfeeding.<br />
• Avoid extra sweet and fatty foods - these foods are high in calories and low in nutrients.<br />
Use them as a treat rather than part of your everyday routine.<br />
• Eat four to five small meals per day - this may help you to keep your energy up with the new<br />
baby. <strong>Your</strong> schedule may be irregular and avoiding extreme hunger is wise. Frequent small meals<br />
can help you to avoid a binge during your baby’s nap. Keep healthy snacks on hand for a quick<br />
energy boost.<br />
91<br />
Y O U R B A B Y ’ S B I R T H
• Get active - when your doctor says you are ready, try to get regular physical activity into your<br />
routine. Take your baby for walks outside or at a local mall. Look for classes that include healthy<br />
postpartum exercises that can be done with your baby.<br />
• Ask about a supplement - your doctor may suggest that you continue taking your prenatal<br />
vitamin after delivery, especially if you plan to breastfeed.<br />
• Focus on health - remember that a healthier you should be the focus. <strong>Your</strong> body was pregnant for<br />
nine months, and you can’t expect to be back in those favorite jeans right away. You need the<br />
energy and strength to provide the best care for you and the new arrival.<br />
Exercise<br />
Exercise will help tone your muscles that were stretched and weakened with pregnancy, improve<br />
circulation and help you return to your normal weight. If an exercise causes you pain, stop<br />
exercising and check with your doctor. The following exercises are listed from the easiest to the<br />
most strenuous. You can do the first three (deep breathing, head lifts, and pelvic tilt) immediately<br />
after a vaginal delivery. Wait until 10 days after delivery to start the others (straight curl-ups,<br />
diagonal curl-ups and knees-to-chest).<br />
Deep breathing<br />
You can do this exercise standing, sitting or lying on your back with knees bent and feet flat<br />
on the floor.<br />
• Place your hands on your abdomen and take a deep breath through your nose.<br />
• Breathe out very slowly through your mouth, pulling in your abdomen towards your back, until<br />
you feel you’ve completely emptied your lungs.<br />
• Repeat five times, progressing to doing one repetition 10 times a day by the end of the first week.<br />
Head lifts<br />
This exercise helps prepare your abdomen for the later, more strenuous exercises.<br />
• Lie on your back with knees bent and arms crossed over your chest or at your sides.<br />
• Breathe in.<br />
• Slowly breathe out and raise your head until you can see your knees. Hold for a count of three.<br />
• Slowly lower your head.<br />
• Repeat five times, every four hours, increasing to 30 head lifts a day by the end of the first week.<br />
Pelvic Tilt<br />
• Start by doing this exercise lying on your back with your knees bent. Use other variations in a<br />
few days as you feel comfortable.<br />
• Lie on your back on a firm surface, knees bent, feet flat on the floor.<br />
• Tighten your buttocks and slowly flatten the small of your back. (With your hands on your hips,<br />
you should feel your pelvis tilt.)<br />
• Hold for a slow count of three, then relax.<br />
• Gradually increase the hold to five seconds and progress to doing one exercise 8-10 times a day<br />
by the tenth day.<br />
92<br />
Y O U R B A B Y ’ S B I R T H
Knees-to-chest<br />
• Lie on your back, knees bent and feet raised.<br />
• Tilt your pelvis to make sure your lower back is flat. You can help the tilt by placing your hands<br />
or fists palm down under both sides of buttocks.<br />
• Breathe in.<br />
• Slowly breathe out while slowly bringing your knees as close to your chest as possible.<br />
• Slowly breathe out and return to starting position. Repeat three times the first day gradually<br />
increasing to 10 times a day.<br />
Straight curl-ups<br />
• Lie on your back with knees bent and feet flat on the floor, about 12 inches apart, arms reaching<br />
toward knees.<br />
• Take a deep breath.<br />
• Slowly breathe out while flattening the small of your back (pelvic tilt) and curling your head and<br />
shoulders slowly forward, towards your knees. Reach as far as you comfortably can.<br />
• Hold this position for a slow count of five, then slowly roll down to your starting position. Relax<br />
the pelvic tilt.<br />
• Start with 4-6 repetitions the first day, gradually increasing to 8-12.<br />
Diagonal curl-ups<br />
• Start in the same position as for straight curl-ups.<br />
• As you breathe out, slowly curl up, reaching diagonally. (Reach your right hand to the outside of<br />
your left knee.)<br />
• Slowly return to starting position as you breathe in.<br />
• Repeat, reaching left hand toward outside of right knee.<br />
• Start with 4-6 repetitions the first day, gradually increasing to 8-12.<br />
• More advanced: lift knee to opposite elbow with hands clasped behind head.<br />
Intimate Issues<br />
<strong>Your</strong> body is still healing from your delivery. Although it takes at least four weeks for your body to<br />
heal, your hormones may not have returned to normal. Now that you have given birth to your baby,<br />
you probably aren’t getting as much sleep as you used to, your hormones and energy levels are all<br />
changing, and your sexual drive may or may not have returned. Here are some general guidelines<br />
to follow when considering resuming sexual activity.<br />
• It usually takes about four to six weeks for your body to heal enough to resume sexual relations.<br />
Check with your healthcare provider to make certain the lochia from the placental site has<br />
cleared before having sexual intercourse.<br />
• You may notice vaginal dryness. A water soluble lubricant like K-Y Jelly may help.<br />
• Sex may be uncomfortable. If you have had an episiotomy or a laceration there may be painful<br />
discomfort for weeks to months after delivery. If you had a normal vaginal delivery or a Cesarean<br />
delivery you may also feel discomfort. <strong>Your</strong> doctor may be able to prescribe an estrogen cream to<br />
lessen the pain and tenderness.<br />
To prevent pregnancy you should decide on a method of birth control before having sex. There are<br />
several methods to choose from so choose one that best fits your lifestyle. Remember that women who<br />
breastfeed and women who have not resumed a regular menstrual cycle may still become pregnant.<br />
93<br />
Y O U R B A B Y ’ S B I R T H
Abstinence<br />
This means that you do not resume having sexual intercourse. This method is 100% reliable.<br />
<strong>Birth</strong> Control Pills/Oral Contraceptives<br />
<strong>Birth</strong> control pills are made of artificial hormones that stop the ovaries from releasing eggs each<br />
month. You must have a doctor’s prescription. The pills must be taken every day to be effective. If<br />
you are taking antibiotics, this may affect the reliability of birth control pills. Talk with your doctor<br />
so that you can avoid an unplanned pregnancy. This method is 97-99% reliable.<br />
Condom<br />
A latex condom is the most reliable condom. Condoms fit over the penis and prevent the sperm<br />
from entering the woman’s body. This method is 80% reliable when used alone and up to 95%<br />
reliable when used with contraceptive foam. Female condoms are another option.<br />
Contraceptive Foam, Cream or Jelly<br />
Contraceptive foams, creams and jellies work by killing sperm. These methods are 80-95% reliable<br />
if used with a condom.<br />
Depo-Provera<br />
A medication given by a shot every three months containing a hormone that prevents the ovaries<br />
from releasing eggs and changes the lining of the uterus. This method is 99% reliable after the first<br />
two weeks.<br />
Diaphragm<br />
A diaphragm is a small, rubber cap that fits over the cervix, keeping the sperm from entering the<br />
uterus. A diaphragm should be used with a contraceptive jelly or cream. <strong>Your</strong> doctor will fit you for<br />
a diaphragm. This method is 82-97% effective.<br />
IUD<br />
An IUD is a small device inserted into the uterus or womb. It prevents the fertilized egg from<br />
implanting into the uterus and growing. This method is 95-99% reliable.<br />
Natural Family Planning<br />
A woman must track vaginal mucous, days of menstrual cycle, and temperature daily to help<br />
predict when she is most fertile. Partners abstain from sexual relations during the fertile period.<br />
This method is 95% reliable. Detailed information on this method is available from books or your<br />
healthcare provider.<br />
NuvaRing<br />
A flexible ring inserted in the vagina once a month. The ring releases a continuous low dose of<br />
hormone to prevent pregnancy. The ring stays in place for three weeks and is then removed. One<br />
week later, insert a new ring. This method is as effective as the pill.<br />
Patch<br />
The patch is a thin stick-on medicated square that allows hormones to enter the bloodstream. The<br />
hormones stop your body from releasing an egg and provides protection from pregnancy. A new<br />
patch is used once per week for three weeks. On the fourth week, when no patch is used, you will<br />
get your period.<br />
94<br />
Y O U R B A B Y ’ S B I R T H
Caring for Mom and Dad’s Spirits<br />
Coping<br />
It is easy to become overwhelmed as a new parent. It is also completely normal to feel overwhelmed<br />
and exhausted. You may find comfort in talking with other new parents or joining a weekly parents’<br />
group, like the New Mom Network, to meet parents who are experiencing the same joys and<br />
challenges of parenthood.<br />
Don’t be afraid to ask for help. It takes a first-time mother six months to a year to adjust to<br />
postpartum changes. And it takes new fathers just as long to adjust to parenthood. Let your family<br />
and friends know how they can help you around the house, with your baby or other children, or just<br />
to have someone to talk with and support you. Asking a friend or relative to watch your baby for a<br />
short time can help you recharge and gain some perspective.<br />
Parents should also take some time to spend with each other. Going out for the evening or even for<br />
a short walk can help you connect as a couple while adjusting to parenthood.<br />
Understanding <strong>Your</strong> Emotions<br />
From pregnancy to the birth of your baby you may experience a wide range of emotions from joy<br />
and excitement to anxiety and worry. After your baby arrives it is common to feel overwhelmed,<br />
uncertain and frustrated. Regardless of how prepared you were or how much you looked forward to<br />
your baby’s birth, you may experience some unexpected “highs” and “lows” after your baby is<br />
born. You may find time, patience and support from family and friends helpful during this period of<br />
adjustment. However, sometimes in spite of help and support, your feelings may overwhelm and<br />
concern you.<br />
If you are experiencing new and unpredictable emotions, you are not alone. Most women have<br />
never experienced anything like this at any other time in their lives. Any woman who is pregnant,<br />
had a baby within the past year or so, miscarried or recently weaned a child from breastfeeding<br />
can be affected regardless of how many previously uncomplicated pregnancies and/or postpartum<br />
adjustments she has made.<br />
The “baby blues” are the most common, least severe and the most well-known postpartum reaction<br />
and occur in 50-75% of all new mothers after delivery. Symptoms of the baby blues last a short time<br />
and usually disappear on their own (crying for no apparent reason, impatience, irritability,<br />
restlessness and anxiety).<br />
At least one in 10 new mothers experience various degrees of postpartum depression. Postpartum<br />
depression can occur within days of delivery or may appear gradually, sometimes taking up to a<br />
year. <strong>Your</strong> symptoms may make you feel either depressed or anxious depending on how your body<br />
is coping. Each symptom may come and go to varying degrees, and you may alternate between<br />
good and bad days.<br />
95<br />
Y O U R B A B Y ’ S B I R T H
Common Signs of Depression:<br />
• Sluggishness, fatigue, exhaustion<br />
• Sadness, depression, hopelessness<br />
• Appetite and sleep disturbances<br />
• Poor concentration, confusion, memory loss<br />
• Over concern for the baby<br />
• Uncontrollable crying, irritability<br />
• Lack of interest in the baby<br />
• Feelings of guilt, inadequacy, worthlessness<br />
• Fear of harming the baby<br />
• Fear of harming yourself<br />
• Exaggerated highs and/or lows<br />
Common Signs of Anxiety:<br />
• Intense anxiety and/or fear<br />
• Rapid breathing<br />
• Fast heart rate<br />
• Sense of doom<br />
• Hot or cold flashes<br />
• Chest pain<br />
• Shaking<br />
• Dizziness<br />
To help physical and emotional recovery after childbirth, you should get enough rest, eat a<br />
nutritious diet, and have help and support from family and friends. Consider participating in the<br />
New Mom Network, an informal time of sharing for new moms and their babies. This group is<br />
facilitated by a nurse experienced in maternal/child health, infant massage and lactation. Join other<br />
new moms and their babies in one of two groups—ages 0 – 9 months and 10 – 16 months—for<br />
discussion about the physical and emotional adjustments to motherhood. Please call WomanCare at<br />
(717) 231-8975.<br />
If you have any signs of depression and/or anxiety, talk with others about how you’re feeling.<br />
Treatment for postpartum depression and postpartum anxiety varies depending on the type and<br />
severity of symptoms. All symptoms, whether mild or severe, are temporary and treatable with<br />
skilled professional help and support. If you are having symptoms of postpartum depression and/or<br />
anxiety, talk with your healthcare provider to begin receiving medical treatment. Treatment may<br />
include medication and/or psychotherapy. Many antidepressants have been used by women who<br />
are breastfeeding. If you are breastfeeding and antidepressants are recommended to treat<br />
depression, talk with your healthcare provider, your pediatrician and a lactation consultant.<br />
Counseling is available through PinnacleHealth Psychological Associates (PHPA) at (717) 231-8360.<br />
If you need immediate help, contact Crisis Intervention Services in your county:<br />
Western Cumberland and Perry Counties 243-6005<br />
Dauphin County Crisis 232-7511<br />
Eastern Cumberland and Perry Counties 763-2222<br />
York County Crisis 851-5352<br />
96<br />
Y O U R B A B Y ’ S B I R T H
Baby Bonding<br />
As parents, the time you spend taking part in daily loving contact will help you bond with your<br />
baby. So take advantage of the time you spend changing diapers, giving baths, feeding, cuddling,<br />
singing lullabies, and holding your baby.<br />
Moms and dads can nurture their child’s emotional growth by giving her plenty of comfort, helping<br />
her feel secure by holding her when she cries, feeding her when she’s hungry, keeping her warm,<br />
and avoiding jarring movements and sounds.<br />
Engage your baby’s natural curiosity by providing lots of interesting stimulation. Babies love<br />
exaggerated expressions and gestures. Make funny faces by sticking out your tongue or smiling<br />
broadly. You can make your baby gurgle and smile by pitching your voice at different levels. <strong>Your</strong><br />
baby likes to be touched, so gently stroke different parts of her body, starting with her legs and<br />
moving up. <strong>Your</strong> baby will let you know what she likes, so watch her expressions.<br />
Fathers, Too!<br />
At PinnacleHealth, fathers are important. Now that your baby has arrived, you have a special<br />
opportunity to get to know your baby, care for him, and become “daddy” as you bond as a family.<br />
There are many special ways that the bond between dad and baby can grow. Here are some<br />
suggestions for dads:<br />
• Talk and sing to your baby. <strong>Your</strong> deep voice can be soothing. Babies often relax when they<br />
hear a deep voice.<br />
• Skin-to-skin contact. Babies love being close to you. <strong>Your</strong> skin feels good to baby. Hold your baby<br />
on your chest and relax.<br />
• Bath time. Make this a special “daddy” time with baby. Bathing can be done anytime during<br />
the day to fit into your schedule.<br />
• Holding. <strong>Your</strong> strong arms and hands are great for holding, swaying, rocking, or dancing<br />
with baby.<br />
• Hanging out. Going for walks or car rides, watching TV, listening to music are all ways of<br />
spending time with your baby.<br />
• Play time. Playing with your baby can help baby’s motor skills, physical development and social<br />
interactions.<br />
• Reading time. Reading stories can be a special time for dads and babies. Babies love hearing<br />
the words and voice changes during a story. They also enjoy the pictures in the books. Reading<br />
with dad from an early age can help baby develop a life-long love of reading as well as a close<br />
father-child relationship.<br />
• Special dad-and-baby time. Just the two of you to look at each other, play and get to know one<br />
another. Have fun!<br />
Congratulations on the birth of your child and on becoming a dad!<br />
97<br />
Y O U R B A B Y ’ S B I R T H
Making Childcare Decisions<br />
When choosing childcare, it is important to find someone you trust, you can depend on, and with<br />
whom you feel comfortable. Start your search early. It may take a couple of months to find the<br />
right childcare provider and you may have to place your baby on a waiting list. Before you begin<br />
your search, ask your baby’s doctor or other parents for recommendations.<br />
There are several kinds of childcare settings to consider. So choose one that works best with your<br />
lifestyle, personality, budget and schedule.<br />
Group Day Care<br />
A group day care is often a licensed center featuring rooms and staff specifically trained to care for<br />
your baby’s age group. It is important to make sure the center is licensed, has a trained,<br />
experienced and healthy staff, a good caregiver-to-baby ratio, a loving and stimulating atmosphere,<br />
and strict health and safety rules.<br />
Family <strong>Home</strong> Day Care<br />
A family home day care setting provides a family setting in a private home, usually with only a few<br />
other children. Costs of home day care are usually lower than those of a center, and scheduling is<br />
often more flexible. <strong>Home</strong> day cares may or may not be licensed by the state. When your caregiver<br />
or her children become ill, you may have to find a back-up caregiver. Look for a family home day<br />
care that is certified by the state, meets health and safety regulations, and whose providers share<br />
similar parenting philosophies.<br />
In-<strong>Home</strong> Care<br />
Choosing a nanny or college student to care for your baby keeps your baby in familiar surroundings.<br />
Keep in mind that if your caregiver is sick or decides to quit, you will need to find another<br />
caregiver. In-home care is almost always more expensive, especially if you hire a nanny. Once you<br />
decide who your best candidates are, interview them and check references. Find out why the<br />
person is interested in caring for your baby and “test” his/her child care skills with questions<br />
about what he/she would do with your baby all day and how he/she plans to discipline your child<br />
as he/she gets older. It may also be a good idea to arrange a trial period to determine if you, your<br />
caregiver and your baby make a good team.<br />
Questions to Guide <strong>Your</strong> Search<br />
When looking for a childcare center, there are several topics to consider that can help guide your<br />
search.<br />
• The People<br />
Consider the personality and values of the child care provider. Do you agree on discipline,<br />
weaning, feeding and toilet training issues How does the caregiver(s) handle conflict<br />
How much one-on-one time will the caregiver(s) spend with your child and will his/her special<br />
needs be accommodated<br />
• The Place<br />
Are you comfortable with the environment where your child will spend a significant portion<br />
of his/her days Is the center/home sanitary, safe and well lit Are toys appropriate for your<br />
child’s age What is the caregiver-to-child ratio and group size for your child’s age group<br />
What is the procedure if your child becomes ill or hurt<br />
98<br />
Y O U R B A B Y ’ S B I R T H
• The Convenience<br />
The convenience of your childcare provider is important when determining if the provider<br />
matches your schedule and lifestyle. Is the location of the childcare provider convenient to your<br />
home or work Are the hours convenient to your schedule What happens if you pick up your<br />
child either early (partial day) or late What happens if the childcare provider goes on vacation or<br />
gets sick Are there days the center is closed<br />
• The Credentials<br />
It is also important to consider childcare provider’s accreditations. Is the program accredited by<br />
the National Association for the Education of Young Children or the National Association of<br />
Family Child Care Are the caregivers certified by the Council for Early Childhood Professional<br />
Recognition or do they have any post-secondary education credentials Does the caregiver have<br />
documentation of a criminal background check and/or child abuse clearance Does the caregiver<br />
have CPR and first aid training<br />
Once again, thank you for choosing PinnacleHealth.<br />
We hope this book has been helpful to you during this time.<br />
We welcome your feedback and suggestions.<br />
Call our Marketing and Public Relations Department at 231-8900.<br />
99<br />
Y O U R B A B Y ’ S B I R T H
100<br />
Y O U R B A B Y ’ S B I R T H
Resources
Y O U R B A B Y ’ S B I R T H<br />
101
102<br />
Y O U R B A B Y ’ S B I R T H
Sign up today and your name will automatically be entered into a drawing<br />
on Labor Day to win FREE DIAPERS for a year!