Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Kentucky</strong> <strong>Medicaid</strong><br />
Spring 2009<br />
Billing Workshop<br />
CMS 1500
Agenda<br />
• Representative List<br />
• Reference List<br />
• CMS Claim Form<br />
• Detailed Billing Instructions<br />
• Forms<br />
• Timely Filing<br />
• FAQ’s<br />
• Did You Know<br />
• Top Denials<br />
• Questions<br />
• Evaluation<br />
Cabinet for Health and Family Services<br />
2
Representative List<br />
Cabinet for Health and Family Services<br />
3
Representative List<br />
Cabinet for Health and Family Services<br />
4
Reference List<br />
Helpful Phone Numbers<br />
EDI Helpdesk<br />
800-205-4696<br />
ky_edi_helpdesk@eds.<strong>com</strong><br />
Provider Billing Inquiry<br />
800-807-1232<br />
ky_provider_inquiry@eds.<strong>com</strong><br />
Web Addresses<br />
EDS Website<br />
www.kymmis.<strong>com</strong><br />
KyHealthnet<br />
http://home.kymmis.<strong>com</strong><br />
KY <strong>Medicaid</strong><br />
www.chfs.ky.gov/dms<br />
Cabinet for Health and Family Services<br />
5
Top Half CMS Claim Form<br />
Cabinet for Health and Family Services<br />
6
Required Information<br />
FIELD NUMBER NAME AND DESCRIPTION<br />
2 Patient’s Name<br />
Enter the member’s last name and first name exactly as it appears on<br />
the Member Identification card.<br />
3 Date of Birth<br />
Enter the date of birth for the member.<br />
9A Other Insured’s Policy Group Number<br />
Enter the 10 digit Member Identification number exactly as it appears<br />
on the current Member Identification card.<br />
10 Patient’s Condition<br />
Check the appropriate block if applicable.<br />
Cabinet for Health and Family Services<br />
7
Required Information<br />
FIELD NUMBER NAME AND DESCRIPTION<br />
10D<br />
Reserved for Local Use<br />
Enter the Physician Assistant’s NPI Number, if applicable.<br />
11 Insured’s Policy Group or FECA Number<br />
Required only if member is covered by Commercial Insurance and<br />
ONLY if a payment is made, otherwise leave blank.<br />
11C<br />
Insurance Plan Name or Program Name<br />
If an insurance <strong>com</strong>pany other than <strong>Medicaid</strong> has issued payment on a<br />
claim, enter the name of the other insurance <strong>com</strong>pany.<br />
Cabinet for Health and Family Services<br />
8
Bottom Half of CMS Claim Form<br />
Cabinet for Health and Family Services<br />
9
Required Information<br />
FIELD NUMBER NAME AND DESCRIPTION<br />
14 Date of Current (Accident Indicator Only)<br />
Enter the appropriate date, if you marked “Yes” in the fields 10A-<br />
10C. (Accident indicator only)<br />
17B<br />
Referring Provider<br />
Enter the KenPAC NPI number.<br />
21 Diagnosis or Nature of Illness or Injury<br />
Enter the required, appropriate ICD-9-CM diagnosis code.<br />
23 Prior Authorization Number<br />
Enter the PA number assigned for these procedures, if<br />
applicable.<br />
24A<br />
24B<br />
Date(s) of Service (Non Shaded Area)<br />
Enter the date or dates of service (s) in month, day, year<br />
numeric format (MMDDYY).<br />
Place of Service (Non Shaded Area)<br />
Enter the appropriate two digit place of service code which<br />
identifies the location where services were rendered.<br />
Cabinet for Health and Family Services<br />
10
Required Information<br />
FIELD NUMBER NAME AND DESCRIPTION<br />
24C<br />
24D<br />
24D<br />
24E<br />
24E<br />
EMG (Shaded Area) School Based Providers only<br />
Enter number of students in the group on the shaded area above EMG. Valid entry is 1-6<br />
Procedures, services or Modifiers<br />
(Shaded Area)<br />
Enter EI for employee ID followed by the three digit employee ID # (School Based Providers)<br />
(Shaded Area)<br />
Enter EI for employee ID followed by the four digit employee ID # (Community Mental Health)<br />
(Shaded Area above modifier)<br />
Enter the appropriate EPSDT Referral code if applicable<br />
(Non-Shaded Area)<br />
Enter appropriate procedure code (non-shaded area)<br />
Modifier (Non-Shaded Area)<br />
Enter appropriate Modifier to identify the procedure.<br />
Diagnosis Pointer (Shaded Area)<br />
Enter Military Time of Pickup (Transportation only)<br />
Diagnosis Pointer (Non-Shaded Area)<br />
Diagnosis Code Indicator Enter 1, 2, 3, or 4<br />
Cabinet for Health and Family Services<br />
11
Required Information<br />
FIELD NUMBER NAME AND DESCRIPTION<br />
24F<br />
24G<br />
Charges<br />
Enter detail charges.<br />
Days or Units<br />
Enter units.<br />
For Anesthesia Billing, Enter the total number of minutes (shaded area, above the units)<br />
24I<br />
EXCEPTION:<br />
24I<br />
24J<br />
EXCEPTION:<br />
24J<br />
ID Qualifier (Shaded area)<br />
Enter ZZ to indicate Taxonomy<br />
ID Qualifier (Shaded area)<br />
Enter a 1D to indicate <strong>Medicaid</strong> Provider (Provider types ONLY: Hands, Commission for<br />
Handicapped Children, Title V, First Steps, Impact Plus and Non Emergency<br />
Transportation)<br />
Rendering Provider ID # (Shaded Area)<br />
The Rendering Provider’s Taxonomy Code<br />
(Non-Shaded Area)<br />
Enter the Rendering Provider’s NPI’s Number<br />
Rendering Provider ID # (Shaded Area)<br />
Enter the <strong>Medicaid</strong> Provider number (Provider types ONLY: Hands, Commission for<br />
Handicapped Children, Title V, First Steps, Impact Plus and Non Emergency<br />
Transportation)<br />
Cabinet for Health and Family Services<br />
12
Required Information<br />
FIELD NUMBER NAME AND DESCRIPTION<br />
26 Patient’s Account No.<br />
Enter the office account number you have assigned to this member, if<br />
desired.<br />
28 Total Charge<br />
Enter the total of all individual charges entered in column 24F. Total<br />
each claim separately.<br />
29 Amount Paid<br />
Enter the amount paid, if any, by a private insurance not Medicare.<br />
30 Balance Due<br />
Enter the balance due if applicable.<br />
EXCEPTION: (If you are a certified Primary Care or Rural Health provider, or<br />
Community Mental Health provider, this field is only used for Medicare<br />
payments)<br />
Cabinet for Health and Family Services<br />
13
Required Information<br />
FIELD NUMBER NAME AND DESCRIPTION<br />
33 Physician/ Supplier’s Billing Name, Address, Zip Code and Phone Number<br />
Enter the provider’s name, address, zip code and phone number (including area<br />
code).<br />
33A<br />
EXCEPTION:<br />
33A<br />
NPI<br />
Enter the appropriate Pay to NPI Number.<br />
Provider types ONLY: Hands, Commission for Handicapped Children, Title V, First<br />
Steps, Impact Plus and Non Emergency Transportation, LEAVE BLANK<br />
33B<br />
EXCEPTION:<br />
33B<br />
(Shaded Area)<br />
Enter ZZ and the Pay to Taxonomy Number.<br />
Enter 1D and the Pay to Provider Number. (Provider types ONLY: Hands,<br />
Commission for Handicapped Children, Title V, First Steps, Impact Plus and Non<br />
Emergency Transportation)<br />
Cabinet for Health and Family Services<br />
14
Forms<br />
• Third Party Liability<br />
• Adjustment and Claim Credit<br />
• Cash Refund<br />
Cabinet for Health and Family Services<br />
15
TPL Lead Form<br />
Cabinet for Health and Family Services<br />
16
TPL Helpful Hints<br />
• When to use the TPL Lead Form:<br />
• When there is no response within 120 days from the insurance<br />
carrier.<br />
When the other health insurance has not responded to a provider’s<br />
billing within 120 days from the date of filing a claim, a provider may<br />
<strong>com</strong>plete a TPL Lead Form.<br />
Mark “no response in 120 days” on the TPL Lead Form.<br />
Attach it to the back of claim and submit it to EDS.<br />
EDS overrides the other health insurance edits and forwards a copy of<br />
the TPL Lead form to the TPL Unit. The TPL staff contacts the<br />
insurance carrier to see why they have not paid their portion of liability.<br />
• Used for Commercial Insurance Only<br />
• Not to be used for Medicare<br />
• Other section is obsolete<br />
• Contact name and phone number is person and phone<br />
number at Commercial Insurance<br />
Cabinet for Health and Family Services<br />
17
Adjustment Claim Credit<br />
Cabinet for Health and Family Services<br />
18
Adjustment, Claim Credit/Void Hints<br />
An adjustment/void is a change to be made to a “PAID” claim.<br />
Please keep the following points in mind when filing an adjustment<br />
request:<br />
• Attach a copy of the corrected claim and the paid remittance<br />
advice page to your adjustment form.<br />
• Do not send refunds on claims for which an adjustment or void<br />
has been filed.<br />
• Be specific. Explain exactly what is to be changed on the claim.<br />
• Claims showing paid zero dollar amounts are considered paid<br />
claims by <strong>Medicaid</strong>.<br />
• If the paid amount of zero is incorrect, the claim requires an<br />
adjustment.<br />
• Do not do a adjustment/void on KyHealth Net and paper. Do one<br />
or the other.<br />
• A claim credit is on paper, a void is on the KyHealth Net. They are<br />
the same.<br />
• Only a void/claim credit will re-set a Prior Authorization<br />
Cabinet for Health and Family Services<br />
19
Cash Refund<br />
Cabinet for Health and Family Services<br />
20
Cash Refund Hints<br />
The Cash Refund Documentation Form is used when refunding<br />
money to KY <strong>Medicaid</strong>.<br />
Please keep the following points in mind when refunding:<br />
• Attach to the Cash Refund Documentation Form a check for<br />
the refund amount made payable to the KY State Treasurer.<br />
• Attach applicable documentation, such as a copy of the<br />
remittance advice showing the claim for which a refund is<br />
being issued.<br />
• Do not send a refund and an adjustment/void on the same<br />
claim.<br />
Cabinet for Health and Family Services<br />
21
Timely Filing<br />
Aged claims (those older than within 12 months from date of service or 6 months<br />
from the Medicare payment or denial date) may be considered for payment only<br />
when documentation is submitted behind the claim to support timely filing.<br />
The ONLY Acceptable documentation will include a copy of one or more of the<br />
following:<br />
• Remittance advices to verify timely filing within each 12 months from date of<br />
service.<br />
• A Screen Print from KYHealth-Net to verify issue date of the eligibility. (this is<br />
the card issuance screen)<br />
• A Screen Print from KYHealth-Net Summary Page, to verify timely filing within<br />
each 12 months from date of service.<br />
• Medicare explanation of benefits (EOMB)<br />
• Commercial Insurance EOB<br />
Cabinet for Health and Family Services<br />
22
Timely Filing Examples<br />
1 Year From Issue Date<br />
Cabinet for Health and Family Services<br />
23
Timely Filing Examples<br />
KyHealth Net<br />
Search Criteria<br />
Screen<br />
Not Acceptable<br />
for timely filing<br />
Cabinet for Health and Family Services<br />
24
Timely Filing Examples<br />
KyHealth Net<br />
Header Screen<br />
Not Acceptable<br />
for timely filing<br />
Cabinet for Health and Family Services<br />
25
Timely Filing Examples<br />
KyHealth Net<br />
Summary<br />
Screen<br />
Acceptable for<br />
timely Filing<br />
Cabinet for Health and Family Services<br />
26
FAQ’s<br />
If you bill Medicare and drop your claim to paper, remember to attach<br />
your coding sheet when Medicare allows a charge. If Medicare denies<br />
a charge, this must be billed paper with the denial EOB attached.<br />
Medicare Replacements follow the same rules as Medicare claims.<br />
The sequence to submit is; Claim, Coding sheet then any other<br />
attachments.<br />
When billing Medicare electronically, you may bill with NPI and<br />
taxonomy and the claim will cross via 837. Medicare’s website about<br />
taxonomy is: www.cms.hhs.gov/manuals/<br />
When submitting a paper claim with attachments, the claim must<br />
always be on top of any attachments. Except, when submitting paper<br />
adjustments, the adjustment form is to be on top of the claim.<br />
Cabinet for Health and Family Services<br />
27
FAQ’s Cont.<br />
<br />
Member Program Codes to watch for<br />
Z-QMB Only-<strong>Medicaid</strong> only allows after Medicare, so if Medicare<br />
denies, <strong>Medicaid</strong> will deny.<br />
ZJ, ZK, ZL, ZQ Buy-In Member-<strong>Medicaid</strong> is only paying the<br />
Medicare Premiums. No <strong>Medicaid</strong> coverage.<br />
<br />
<br />
<br />
For Ambulatory Surgery Centers only:<br />
The 59 modifier is ONLY for implants. These must be billed on<br />
paper with the invoice attached and the billed amount must match<br />
the invoice dollar amounts.<br />
Rendering ARNP/CRNA cannot be billed along with the<br />
physician group.<br />
Billing for a Physician Assistant: In field 10d, enter the PA’s NPI<br />
number. In field 24d enter the U1 modifier. In field 24j, enter the<br />
supervising Physician’s NPI.<br />
Cabinet for Health and Family Services<br />
28
FAQ’S Cont.<br />
Internal Control Number (ICN)<br />
All claims, adjustment and Voids are given a unique number.<br />
First two digits are the Region, Second 2 digits is the Year the<br />
claim was received and the 3 rd three digits are the Julian Date<br />
of receipt.<br />
*Example 2009061123456-Claim received as an electronic claim,<br />
March 2, 2009.<br />
If the ICN begins with:<br />
10-Paper claim with no attachments<br />
11-Paper claim with attachments<br />
20-Electronic claim<br />
22-KyHealth billed claim<br />
50-Adjustment<br />
56-Claim Void<br />
Cabinet for Health and Family Services<br />
29
FAQ’s Cont. Physicans ONLY<br />
• Recently the Department for <strong>Medicaid</strong> Services (DMS) requested a review of the<br />
medical necessity of CT scans performed for <strong>Medicaid</strong> members. The review<br />
revealed that many diagnoses appear unrelated to the medical conditions/reasons for<br />
CT scans. Inaccurate diagnosis coding may result in the denial or recovery of<br />
services because the medical necessity of the scan can not be determined. <strong>Medicaid</strong><br />
funds can only be used for services that are medically necessary.<br />
• Examples of inappropriate brain CT diagnoses include cellulitis of the toe, sunburn,<br />
osteoarthritis, lumbago, trigger finger, joint pain of the shoulder, cough, chest pain,<br />
screening mammogram, removal of sutures, varied fractures and sprains of the<br />
patella, wrist, tibia, fibula, hand and foot.<br />
• Examples of inappropriate spine CT diagnoses include malaise, convulsions,<br />
generalized pain, altered mental status, abdominal pain, ankle and foot fractures and<br />
sprained ankle.<br />
• Examples of inappropriate chest CT diagnoses include panic disorder, anxiety,<br />
hyperlipidemia, appendicitis, pain in the limb, memory loss, headache and diarrhea.<br />
• DMS is requesting all providers review their radiology billing process and bill claims<br />
with the appropriate diagnoses that supports the medical necessity of the procedure<br />
being performed. Future restrictions may be imposed if the medical necessity of CT<br />
scans continues to be unsupported by the diagnosis codes.<br />
Cabinet for Health and Family Services<br />
30
Did You Know<br />
* Coming Soon--Paper checks are going to be mailed from the<br />
KY State Treasurer. Remittance Advices will continued to be<br />
mailed by EDS.<br />
* GO GREEN--Did you know that you can opt not to receive<br />
paper RA's. You can download the RA from the KyHealth Net<br />
and keep an electronic copy.<br />
Cabinet for Health and Family Services<br />
31
Top Denials<br />
<br />
<br />
<br />
<br />
<br />
EOB 0482-Exact duplicate<br />
Resolution: The claim has already paid, a duplicate will not hit against a previously<br />
denied claim.<br />
EOB 1010-Rendering Provider not a member of billing group.<br />
Resolution: Contact provider enrollment at 877-838-5085. Invalid billing NPI and<br />
taxonomy may result in this denial code.<br />
EOB 1955-The billing provider NPI submitted on the claim cannot be used to<br />
uniquely identify the billing provider.<br />
Resolution: Verify billing provider number NPI and taxonomy number billed.<br />
EOB1908-NPI IS NOT ON FILE<br />
Resolution: Contact provider enrollment at 877-838-5085 to update provider file.<br />
EOB2003-Member not eligible for <strong>Medicaid</strong><br />
Resolution: Always check member eligibility.<br />
Cabinet for Health and Family Services<br />
32
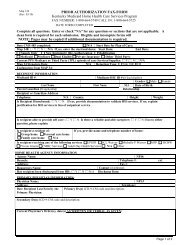
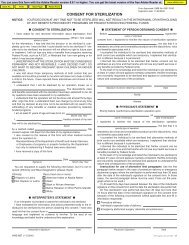
KY MMIS Project<br />
Provider Evaluation – Provider Workshop<br />
Date:<br />
Thank you for attending this session. We’d appreciate your feedback, as well as suggestions on how we can<br />
improve future sessions.<br />
Please answer the following questions, rating them on a scale of 1-5, with 1 being strongly disagree and 5 being<br />
strongly agree.<br />
Strongly<br />
Disagree<br />
Somewhat<br />
Agree<br />
Strongly<br />
Agree<br />
Question 1 2 3 4 5<br />
1. Material was appropriate for the audience.<br />
Comments:<br />
2. Presentation was well-organized and easy to follow.<br />
Comments:<br />
3. Session leader was easy to hear/understand.<br />
Comments:<br />
4. The Session leader was well-versed in their subject area and presented information<br />
in a clear, understandable manner.<br />
Comments:<br />
5. I was given appropriate material/handouts.<br />
Comments:<br />
6. Questions were answered to my satisfaction.<br />
Comments:<br />
7. I was able to see/hear the audiovisual portion with no trouble.<br />
Comments:<br />
If you would like to receive information via e-mail, please provide address below.<br />
Comments:<br />
Optional: if you would like a member of the KY MMIS team to contact you, please provide your contact information below.<br />
Name: Department/Branch:<br />
Phone Number: Email: