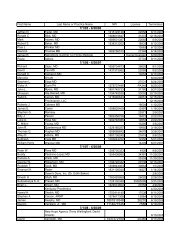
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
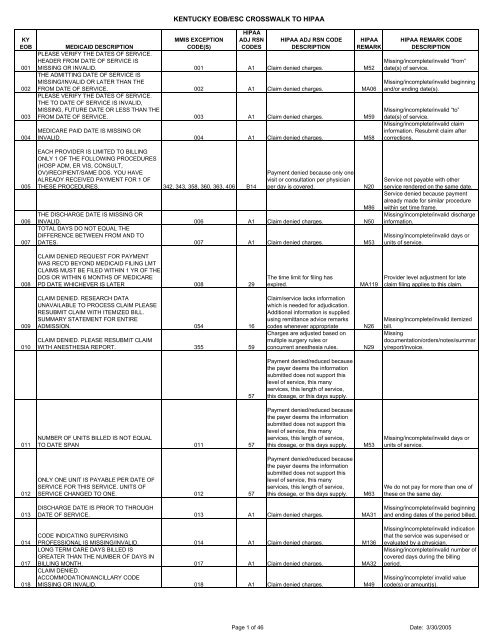
KY<strong>EOB</strong>001002003004KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAHIPAAADJ RSNCODESMEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKPLEASE VERIFY THE DATES OF SERVICE.HEADER FROM DATE OF SERVICE ISMISSING OR INVALID. 001 A1 Claim denied charges. M52THE ADMITTING DATE OF SERVICE ISMISSING/INVALID OR LATER THAN THEFROM DATE OF SERVICE. 002 A1 Claim denied charges. MA06PLEASE VERIFY THE DATES OF SERVICE.THE TO DATE OF SERVICE IS INVALID,MISSING, FUTURE DATE OR LESS THAN THEFROM DATE OF SERVICE. 003 A1 Claim denied charges. M59MEDICARE PAID DATE IS MISSING ORINVALID. 004 A1 Claim denied charges. M58HIPAA REMARK CODEDESCRIPTIONMissing/in<strong>com</strong>plete/invalid “from”date(s) of service.Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong>/or ending date(s).Missing/in<strong>com</strong>plete/invalid “to”date(s) of service.Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.005006007EACH PROVIDER IS LIMITED TO BILLINGONLY 1 OF THE FOLLOWING PROCEDURES(HOSP ADM, ER VIS, CONSULT,OV)/RECIPIENT/SAME DOS. YOU HAVEALREADY RECEIVED PAYMENT FOR 1 OFTHESE PROCEDURES. 342, 343, 358, 360, 363, 406 B14Payment denied because only onevisit or consultation per physicianper day is covered.M86THE DISCHARGE DATE IS MISSING ORINVALID. 006 A1 Claim denied charges. N50TOTAL DAYS DO NOT EQUAL THEDIFFERENCE BETWEEN FROM AND TODATES. 007 A1 Claim denied charges. M53N20Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Missing/in<strong>com</strong>plete/invalid dischargeinformation.Missing/in<strong>com</strong>plete/invalid days orunits of service.008CLAIM DENIED REQUEST FOR PAYMENTWAS REC'D BEYOND MEDICAID FILING LMTCLAIMS MUST BE FILED WITHIN 1 YR OF THEDOS OR WITHIN 6 MONTHS OF MEDICAREPD DATE WHICHEVER IS LATER 008 29The time limit for filing hasexpired.MA119Provider level adjustment for lateclaim filing applies to this claim.009010CLAIM DENIED. RESEARCH DATAUNAVAILABLE TO PROCESS CLAIM PLEASERESUBMIT CLAIM WITH ITEMIZED BILL.SUMMARY STATEMENT FOR ENTIREADMISSION. 054 16CLAIM DENIED. PLEASE RESUBMIT CLAIMWITH ANESTHESIA REPORT. 355 59Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriateCharges are adjusted based onmultiple surgery rules orconcurrent anesthesia rules.N26N29Missing/in<strong>com</strong>plete/invalid itemizedbill.Missingdocumentation/orders/notes/summary/report/invoice.57Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this days supply.011NUMBER OF UNITS BILLED IS NOT EQUALTO DATE SPAN 011 57Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this days supply.M53Missing/in<strong>com</strong>plete/invalid days orunits of service.012ONLY ONE UNIT IS PAYABLE PER DATE OFSERVICE FOR THIS SERVICE. UNITS OFSERVICE CHANGED TO ONE. 012 57Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this days supply.M63We do not pay for more than one ofthese on the same day.013014017018DISCHARGE DATE IS PRIOR TO THROUGHDATE OF SERVICE. 013 A1 Claim denied charges. MA31CODE INDICATING SUPERVISINGPROFESSIONAL IS MISSING/INVALID. 014 A1 Claim denied charges. M136LONG TERM CARE DAYS BILLED ISGREATER THAN THE NUMBER OF DAYS INBILLING MONTH. 017 A1 Claim denied charges. MA32CLAIM DENIED.ACCOMMODATION/ANCILLARY CODEMISSING OR INVALID. 018 A1 Claim denied charges. M49Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong> ending dates of the period billed.Missing/in<strong>com</strong>plete/invalid indicationthat the service was supervised orevaluated by a physician.Missing/in<strong>com</strong>plete/invalid number ofcovered days during the billingperiod.Missing/in<strong>com</strong>plete/ invalid valuecode(s) or amount(s).Page 1 of 46 Date: 3/30/2005
KY<strong>EOB</strong>019MEDICAID DESCRIPTIONKENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESCLAIM/DETAIL DENIED. PROCEDURE/NDCMISSING/INVALID. 019 B18HIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTIONPayment denied because thisprocedure code/ modifier wasinvalid on the date of service orclaim submission. M20 Missing/in<strong>com</strong>plete/invalid HCPCS.020021022Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedMEDICARE DOCUMENTATION NOTATTACHED. 020, 256 16using remittance advice remarkscodes whenever appropriate. N29CLAIM DENIED. PHYSICIAN ON REPORT ANDPHYSICIAN BILLING DO NOT MATCH. 355 A1 Claim denied charges. M29A1 Claim denied charges. MA102COVERED DAYS ARE NOT EQUAL TOACCOMMODATION UNITS. 022 A1 Claim denied charges. MA32M53MA31Missingdocumentation/orders/notes/summary/report/invoice.Missing/in<strong>com</strong>plete/invalid operativereport.Missing/in<strong>com</strong>plete/invalid name orprovider identifier for therendering/referring/ordering/supervising provider.Missing/in<strong>com</strong>plete/invalid number ofcovered days during the billingperiod.Missing/in<strong>com</strong>plete/invalid days orunits of service.Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong> ending dates of the period billed.023024025026027Missing/in<strong>com</strong>plete/invalid indicationCLAIM DENIED. NO PHYSICIAN PATIENTCONTACT. 355 A1 Claim denied charges. M136that the service was supervised orevaluated by a physician.THE DETAIL BILLED AMOUNT IS MISSING ORINVALID. 024 A1 Claim denied charges. M79 Missing/in<strong>com</strong>plete/invalid charge.Informational notice. No paymentissued for this claim with this notice.Payment issued to the hospital by itsCLAIM SUBMITTED FOR INFORMATIONALintermediary for all services for thisPURPOSE ONLY. NO PAYMENT IS TO BENewborn's services are covered inencounter under a demonstrationMADE. 025 128 the mother's Allowance.MA80 project.Claim/service denied because theCLAIM DENIED. LONG TERM CARErelated or qualifying claim/serviceSUPPLEMENTAL BILLING MUST BEwas not previously paid orSUBMITTED AS AN ADJUSTMENT. 026 107 identified on this claim. N34 Incorrect claim form for this service.Missing/in<strong>com</strong>plete/invalid claimCLAIM DENIED. RESUBMIT AN ADJUSTMENTinformation. Resubmit claim afterON RELATED PAID CLAIM. 480, 490 A1 Claim denied charges. M58 corrections.028CLAIM/DETAIL DENIED. DATA ILLEGIBLE.PLEASE RESUBMIT. 355 A1 Claim denied charges. M58N34Incorrect claim form for this service.Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.029CLAIM REQUIRES DOCUMENTATION.PLEASE RESUBMIT ON PAPER. DEPENDENT 180, 181, 182, 183, 232, 256,ON SPECIFIC PROCEDURE CODE ANDCRITERIA SET FOR REVIEW.355, 374, 654, 846, 858, 860,861, 862, 883, 884, 885, 886 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N29Missingdocumentation/orders/notes/summary/report/invoice.030CLAIM/DETAIL DENIED. DETAIL NUMBER OFSERVICES MISSING. 030 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.M53Missing/in<strong>com</strong>plete/invalid days orunits of service.Claim/service lacks informationwhich is needed for adjudication.Additional information is supplied031CLAIM DENIED. LEVEL OF CARE MISSING.PLEASE CORRECT AND RESUBMIT. 031 16using remittance advice remarkscodes whenever appropriate. M58NUMBER OF UNITS BILLED LESS THAN 30033 FOR INSULIN SYRINGES 033 A1 Claim denied charges. M53034 DENIED BY MEDICARE. 034 96 Non-covered charge(s).DETAIL DENIED. THIS SERVICE NOTThis (these) service(s) is (are) not035 PAYABLE ON THIS DATE OF SERVICE 035 46 covered.N2003603703896 Non-covered charge(s). MA66CLAIM DENIED. ONLY 1 DATE OF SERVICEALLOWED PER CLAIM FORM. 036 A1 Claim denied charges. N20MODEL WAIVER 1 RECIPIENT LIMITED TO 24HOURS OF NURSING SERVICES PER DATEBenefit maximum for this timeOF SERVICE. 682 119 period has been reached.M139CLAIM DETAIL DENIED. REVENUE CODEINVALID FOR PLACE OF SERVICE 038 96 Non-covered charge(s). M77Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/invalid days orunits of service.Service not payable with otherservice rendered on the same date.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Service not payable with otherservice rendered on the same date.Denied services exceed the coveragelimit for the demonstration.Missing/in<strong>com</strong>plete/invalid place ofservice.Page 2 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>039040041042MMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESMEDICAID DESCRIPTIONTHIS PROCEDURE CODE IS LIMITED TOTWO UNITS OF SERVICE PER DATE OFSERVICE. 630, 672 119CLAIM/DETAIL DENIED. TYPE OF BILLINVALID OR MISSING. 040, 050, 480 5DRUG MANAGEMENT AND MEDICALPSYCHOTHERAPY NOT ALLOWED FORSAME DATE OF SERVICE, PROVIDER,RECIPIENT. 331, 403 97CLAIM DENIED. COINSURANCE AND/ORDEDUCTIBLE GREATER ON CLAIM THANEOMB. 042 45HIPAA ADJ RSN CODEDESCRIPTIONBenefit maximum for this timeperiod has been reached.The procedure code/bill type isinconsistent with the place ofservice.Payment is included in theallowance for anotherservice/procedure.Charges exceed your contracted/legislated fee arrangement.HIPAAREMARKM53MA30N20M86N4HIPAA REMARK CODEDESCRIPTIONMissing/in<strong>com</strong>plete/invalid days orunits of service.Missing/in<strong>com</strong>plete/invalid type ofbill.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Missing/in<strong>com</strong>plete/invalid priorinsurance carrier <strong>EOB</strong>.043044CLAIM DENIED. VOUCHER NUMBER MISSINGOR INVALID. 043 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N29CLAIM DETAIL DENIED. REVENUE CODEMISSING OR INVALID 044 96 Non-covered charge(s). M50045 TYPE OF BILL INVALID FOR PROVIDER TYPE. 355 A1 Claim denied charges. MA30CLAIM DENIED. HCPCS CODE BILLEDINVALID/OBSOLETE. RESUBMIT WITH046 CORRECT CODE. 046 A1 Claim denied charges. M51N27Missing/in<strong>com</strong>plete/invalid treatmentnumber.Missingdocumentation/orders/notes/summary/report/invoice.Missing/in<strong>com</strong>plete/invalid revenuecode(s).Missing/in<strong>com</strong>plete/invalid type ofbill.Missing/in<strong>com</strong>plete/invalid procedurecode(s) <strong>and</strong>/or rates.047048PROFESSIONAL COMPONENT BILLED. CLAIMMANUALLY PRICED TO MAXIMUMALLOWABLE 047 42CLAIM DENIED. MEDICARE PAID PATIENT,REFER TO DMS PROVIDER SERVICESMANUAL AND RESUBMIT. 048 100Charges exceed our fee scheduleor maximum allowable amount.Payment made topatient/insured/responsible party.N14N13M58Payment based on a contractualamount or agreement, fee schedule,or maximum allowable amount.Payment based on professional/technical <strong>com</strong>ponent modifier(s).Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.049129CLAIM/DETAIL DENIED. MEDICARE PAIDAMOUNT GREATER THAN OR EQUAL TOTOTAL BILLED AMOUNT. 049 23Payment denied - Prior processinginformation appears incorrect.Payment adjusted becausecharges have been paid byanother payer.05005105205305405505605705842Charges exceed our fee scheduleor maximum allowable amount.CLAIM DENIED. PLEASE CORRECT COVEREDDAYS FIELD AND RESUBMIT 050 A1 Claim denied charges. MA32MA31PATIENT CONDITION/STATUS CODEMISSING, INVALID, OR INVALID FOR TYPE OFBILL. 051 A1 Claim denied charges. M44ERROR ON CLAIM RELATED TO DOLLARAMOUNTS -CLAIM IN PROCESS. 052 133The disposition of thisclaim/service is pending furtherreview.CLAIM/DENIED. NET BILLED NOT EQUAL TOTOTAL BILLED MINUS OTHER INSURANCE. 053 A1 Claim denied charges.CLAIM DENIED. OTHER INSURANCE AMOUNTMUST BE MANUALLY COMPUTED FOR THISCLAIM 054 A1 Claim denied charges.CLAIM DENIED TOTAL DETAIL CHARGESNOT EQUAL TO TOTAL BILLED. 055 A1 Claim denied charges. M54CLAIM/DETAIL DENIED. ASSISTANTSURGEON SERVICES NOT PAYABLE FOR AMultiple physicians/ assistants areVAGINAL DELIVERY. 179 54 not covered in this case.N55INVALID TYPE OF BILL FOR CORF/ORFPROVIDER SPECIALTY. 015 A1 Claim denied charges. MA30CLAIM/DETAIL DENIED. ONLY ONE DATE OFSERVICE ALLOWED PER DETAIL. 011 A1 Claim denied charges. N63N4M53Missing/in<strong>com</strong>plete/invalid priorinsurance carrier <strong>EOB</strong>.Missing/in<strong>com</strong>plete/invalid number ofcovered days during the billingperiod.Missing/in<strong>com</strong>plete/invalid days orunits of service.Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong> ending dates of the period billed.Missing/in<strong>com</strong>plete/invalid conditioncode.Missing/in<strong>com</strong>plete/invalid totalcharges.Missing/in<strong>com</strong>plete/invalid totalcharges.Procedures for billing withgroup/referring/performing providerswere not followed.Missing/in<strong>com</strong>plete/invalid type ofbill.Rebill services on separate claimlines.Page 3 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION059CLAIM/DETAIL DENIED. NET BILLED CHARGEMISSING OR INVALID. 059 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.060 CLAIM DENIED. LOCATION CODE INVALID. 060 A1 Claim denied charges. N79061 PAID IN FULL BY MEDICAID. 061 92 Claim Paid in full. MA125M54M58Missing/in<strong>com</strong>plete/ invalid totalcharges.Service billed is not campatible withpatient location information.Missing/in<strong>com</strong>plete/ invalid claiminformation. Resubmit claim aftercorrections.Per legislation governing thisprogram, payment constitutespayment in full.062063CLAIM DENIED. THE HOUR OF ADMISSION ISMISSING OR INVALID. 062 16CLAIM DENIED. AN 8-DIGIT LONG TERMCARE FACILITY NUMBER MUST BE ENTEREDIN FORM LOCATOR #11. 063 62Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.N46N77Missing/in<strong>com</strong>plete/ invalidadmission hour.Missing/in<strong>com</strong>plete/ invaliddesignated provider number.064Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarks16 codes whenever appropriate.THE TIME OF PICK UP IS BEFORE THE TIMEOF CALL IN. 064 A1 Claim denied charges.065 DESTINATION CODE IS MISSING/INVALID. 065 A1 Claim denied charges. N157Payment denied/reduced forPRO STICKER/INDICATOR MISSING ORabsence of, or exceeded, precertification066 INVALID 066 62/authorization.M49067 FAMILY PLANNING INDICATOR INVALID. 067 A1 Claim denied charges. M49068M58AM/PM PICK-UP INDICATOR MISSING ORINVALID. 068 A1 Claim denied charges. M49069 TIME OF CALL IN MISSING/INVALID. 069 A1 Claim denied charges. M125070 TIME OF PICK UP IS MISSING OR INVALID. 070 A1 Claim denied charges.071MORE THAN 10 ERRORS AT THE HEADERLEVEL 071 A1 Claim denied charges.072PICK-UP LOCATION CODE MISSING ORINVALID. 072 A1 Claim denied charges. N53073 REFERRED TO "OTHER" CODE INVALID. 073 A1 Claim denied charges. M49M58M58M58Transportation to <strong>and</strong> from thisdestination is not covered.Missing/in<strong>com</strong>plete/ invalid valuecode(s) or amount(s).Missing/in<strong>com</strong>plete/ invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/ invalid valuecode(s) or amount(s).Missing/in<strong>com</strong>plete/ invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/ invalid valuecode(s) or amount(s).Missing/in<strong>com</strong>plete/ invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/ invalidinformation on the period of time forwhich the service/supply/ equipmentwill be needed.Missing/in<strong>com</strong>plete/invalid point ofpick-up address.Missing/in<strong>com</strong>plete/ invalid valuecode(s) or amount(s).Missing/in<strong>com</strong>plete/ invalid claiminformation. Resubmit claim aftercorrections.074076077078ANCILLARY CHARGES NOT PAYABLE INCONJUNCTION WITH VENTILATOR ORBRAIN INJURY PROGRAM REIMBURSEMENT. 074 B597Payment adjusted becauseoverage/ program guidelines werenot met or were exceeded.Payment is included in theallowance for anotherservice/procedure.OTHER MEANS OF TRANSPORTATION CODEMISSING OR INVALID. 076 A1 Claim denied charges. M58CLAIM DETAIL/DENIED. TIME OF CALL-INAM/PM INDICATOR MISSING 077 A1 Claim denied charges. M58CLAIM/DETAIL DENIED. BASE RATE OR RATEPER MILE MISSING OR INVALID. 078 A1 Claim denied charges. M51M2Not paid separately when the patientis an inpatientMissing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/ invalidprocedure code(s) <strong>and</strong>/or rates.Page 4 of 46 Date: 3/30/2005
KY<strong>EOB</strong>079080081082083084KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAHIPAAADJ RSNCODESMEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKCLAIM/DETAIL DENIED. DETAIL TOTAL BILLNOT=(RATE PER MILE X EXTRA MILES). 079 A1 Claim denied charges. M54PROVIDER TYPE INVALID FOR CATEGORYOF SERVICE. 080 A1 Claim denied charges. N95CLAIM DENIED. NUMBER OF PERSONSSHARING RIDE INVALID. 081 A1 Claim denied charges. N76CLAIM DENIED. TYPE OF TRIP MISSING ORINVALID. 082 A1 Claim denied charges.CLAIM DENIED. SECONDARY SURGERYDATE MISSING/INVALID 083 A1 Claim denied charges. MA06CLAIM DENIED. PRIMARY SURGERY DATEMISSING/INVALID. 084 A1 Claim denied charges. MA06CLAIM DENIED. EPSDT DISPOSITION CODEMISSING OR INVALID. 090 A1 Claim denied charges. M58CLAIM DENIED. YOU MUST INDICATE INBLOCK 15 IF THIS WAS A PARTIAL,COMPLETE, OR COMPLETION OF A PARTIALEXAM FOR PROCESSING. 091 A1 Claim denied charges.THIS SERVICE DENIED. PLEASE RESUBMITCLAIM WITH COPY OF PATHOLOGYREPORT. 182 A1 Claim denied charges. M30HIPAA REMARK CODEDESCRIPTIONMissing/in<strong>com</strong>plete/ invalid totalcharges.This provider type/ provider specialtymay not bill this service.Missing/in<strong>com</strong>plete/invalid number ofriders.Missing/in<strong>com</strong>plete/ invalid beginning<strong>and</strong>/or ending date(s).Missing/in<strong>com</strong>plete/ invalid beginning<strong>and</strong>/or ending date(s).Missing/in<strong>com</strong>plete/invalidprescribing/referring/attendingprovider license number.085CLAIM DENIED/INVALID LINE ITEM PROVIDERLICENSE NUMBER 085 A1 Claim denied charges. N31PROVIDER INELIGIBLE FOR DATE OFSERVICE. PLEASE CONTACT PROVIDERENROLLMENT AT (877) 838-5085 FOR NF ORMissing/in<strong>com</strong>plete/ invalid086 ICF/MR. 086 A1 Claim denied charges. N77 designated provider number.Missing/in<strong>com</strong>plete/ invalid providerM57 identifier.CLAIM DENIED. TO DATE OF SERVICEMissing/in<strong>com</strong>plete/ invalid “to”087 EQUAL TO DATE OF RECEIPT. 087 110 Billing date predates service date. M59 date(s) of service.CLAIM DENIED. CLAIM INVOICE DATE088 MISSING/INVALID. 088 A1 Claim denied charges. MA52 Missing/in<strong>com</strong>plete/ invalid date.089 DETAIL CHARGE MISSING OR INVALID. 089 A1 Claim denied charges. M79 Missing/in<strong>com</strong>plete/invalid charge.Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim after090corrections.091092Missing/in<strong>com</strong>plete/ invalid pathologyreport.093094095096097098099100101Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedTHIS SERVICE DENIED. PLEASE RESUBMITWITH HISTORY AND PHYSICAL NOTES. 182, 183 16using remittance advice remarkscodes whenever appropriate. N29PHYSICIAN SIGNATURE AND DATE ONCONSENT FORM MUST BE ON OR AFTERDATE OF SERVICE 181 A1 Claim denied charges. N3CONSENT FORM IS ILLEGIBLE. RESUBMITLEGIBLE COPY WITH CLAIM 181, 183 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N28RECIPIENT'S SIGNATURE ON CONSENTFORM MUST BE ON OR BEFORE DATE OFSERVICE. 183 A1 Claim denied charges. N3MA52DATES OF SERVICE ON CLAIM ANDCONSENT FORM DISAGREE. 181 A1 Claim denied charges. N3RECIPIENT MUST BE 21 TO LEGALLY SIGNTHE FEDERAL STERILIZATION CONSENTFORM. 181 6The procedure/revenue code isinconsistent with the patient's age.N28PERSON OBTAINING CONSENT MUST SIGNON OR AFTER DATE OF RECIPIENTSIGNATURE BUT PRIOR TO THESTERILIZATION PROCEDURE. CLAIM NOTPAYABLE BY MEDICAID. 181 A1 Claim denied charges. N3N28DETAIL FROM DATE OF SERVICE MISSINGOR INVALID. 100 A1 Claim denied charges. M52DETAIL TO DATE OF SERVICE MISSING ORINVALID. 101 A1 Claim denied charges. M59N28N3N28N3Missingdocumentation/orders/notes/summary/report/invoice.Missing/in<strong>com</strong>plete/ invalid consentform.Consent form requirements notfulfilled.Missing/in<strong>com</strong>plete/invalid consentform.Consent form requirements notfulfilled.Missing/in<strong>com</strong>plete/invalid consentform.Missing/in<strong>com</strong>plete/invalid date.Missing/in<strong>com</strong>plete/invalid consentform.Consent form requirements notfulfilled.Missing/in<strong>com</strong>plete/invalid consentform.Consent form requirements notfulfilled.Missing/in<strong>com</strong>plete/invalid consentform.Consent form requirements notfulfilled.Missing/in<strong>com</strong>plete/invalid “from”date(s) of service.Missing/in<strong>com</strong>plete/invalid “to”date(s) of service.Page 5 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION102103106CLAIM DETAIL DENIED. LATE BILLING DATEOF SERVICE PAST ONE YEAR FILING LIMIT.VERIFIES THAT EACH DETAIL OF A CLAIM ISRECEIVED WITHIN 1 YEAR FROM THE DATEOF WHICH THE SERVICE WAS RENDERED. 102 29The time limit for filing hasexpired.MA119MISSING OR ALTERED RECIPIENTSIGNATURE OR DATE ON CONSENT FORMIS NOT ACCEPTABLE. CLAIM NOT PAYABLEBY MEDICAID. 181, 183 A1 Claim denied charges. N29INCLUDED IN FLAT FEE FOR MAJORPROCEDURES. (Hospice Recipient EligibilityStatus - Recycle Edit) 106 97Payment is included in theallowance for anotherservice/procedure.N28N19Provider level adjustment for lateclaim filing applies to this claim.Missingdocumentation/orders/notes/summary/report/invoice.Consent form requirements notfulfilled.Procedure code incidental to primaryprocedure.107INCLUDED IN REIMBURSEMENT FOR OFFICEVISIT (Hospice Recipient) 107 97Payment is included in theallowance for anotherservice/procedure.108 CONSENT FORM IS INCOMPLETE 181, 183 A1 Claim denied charges. N3109N28INCORRECT STERILIZATION CONSENTFORM USED. 181 A1 Claim denied charges. N3110 CLAIM SUSPENDED FOR REVIEW.001 - 003, 005 - 009, 011 -013, 015 - 016, 018 - 019,022, 026, 030, 035 - 036,043, 048, 050 - 060, 062 -063, 065 - 068, 070 - 074,078 - 079, 082 - 084, 087 -088, 094 - 097, 100 - 107,113, 115, 117, 121, 123 -124, 127, 129, 136 - 137,141 - 142, 144, 146 - 150,152 - 154, 156, 158, 162,164 - 177, 179 - 183, 185,186, 190, 193 - 196, 198,200 - 201, 204 - 205, 210 -211, 214 - 216, 220, 223,232, 235, 240, 242 - 245,255, 257, 273, 283, 303, 305,307, 325, 327, 330, 332 -333, 354 - 355, 368 - 372,374 - 377, 393, 398, 412,510 - 512, 574, 640, 673,696, 700, 777, 828, 830 -837, 889 - 893, 895 - 896,898, 900 - 901, 904, 906 -908, 912, 915 - 919, 923,927 - 928, 931, 933, 950,953 - 954, 956 - 959, 964 -968, 972 - 978, 981 - 982,984 - 989, 991 - 997. 133The disposition of thisclaim/service is pending furtherreview.M14N28No separate payment for an injectionadministered during an office visit,<strong>and</strong> no payment for a full office visit ifthe patient only received an injection.Missing/in<strong>com</strong>plete/invalid consentform.Consent form requirements notfulfilled.Missing/in<strong>com</strong>plete/invalid consentform.Consent form requirements notfulfilled.The claim information has also beenforwarded to Medicaid for review.MA07The disposition of thisclaim/service is pending furtherreview. MA67 Correction to a prior claim.111 ADJUSTMENT REQUEST IN PROCESS 133CLAIM DENIED. DOCUMENTATIONATTACHED WAS INSUFFICIENT TO WAIVEONE YEAR FILING LIMITATION. PLEASE CALLUNISYS PROVIDER SERVICES FOR112 ASSISTANCE. 008, 102 A1 Claim denied charges. N225In<strong>com</strong>plete/invaliddocumentation/orders/ notes/summary/ report/ invoice.16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.MA119Provider level adjustment for lateclaim filing applies to this claim.113CLAIM DENIED. REQUIREDDOCUMENTATION MISSING/INCOMPLETE.(Hospice - QMB Esc 245 only) 180, 245, 284, 355, 654, 670 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N29Missingdocumentation/orders/notes/summary/report/invoice.Page 6 of 46 Date: 3/30/2005
KY<strong>EOB</strong>114115116117118119KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKMEDICAID DESCRIPTIONREQUIRED CONSENT FORMDOCUMENTATION WAS NOT COMPLETEDPRIOR TO STERILIZATION PROCEDURE.CLAIM NOT PAYABLE BY MEDICAID. 181 A1 Claim denied charges. N3N28Adjustment amount representsPAYMENT APPLIED TO RECEIVABLE.collection against receivable(Hospital) 115 88 created in prior overpayment.DOCUMENTATION OF MEDICAL NECESSITYREQUIRED. CONSULT YOUR PROVIDERMANUAL. 180 A1 Claim denied charges. N29THIS TYPE OF BILL NOT VALID FOR DRG-RELATED CLAIM 117 A1 Claim denied charges.OUR RECORDS INDICATE PAID IN FULL BYMEDICARE. 118 96 Non-covered charge(s). M43NOT COVERED UNDER THE PROGRAMEXCEPT UNDER EPSDT. 119 96 Non-covered charge(s). N59HIPAA REMARK CODEDESCRIPTIONMissing/in<strong>com</strong>plete/invalid consentform.Consent form requirements notfulfilled.Missingdocumentation/orders/notes/summary/report/invoice.Payment for this service previouslyissued to you or another provider byanother carrier/intermediary.Please refer to your provider manualfor additional program <strong>and</strong> providerinformation.120121122123124125126127128LAB PROCESSING CHARGE INCLUDED INFLAT FEE. 120 97Payment is included in theallowance for anotherservice/procedure.M15Separately billed services/tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Procedure code incidental to primaryprocedure.N19THIS SERVICE IS NOT PAYABLE FOR A QMB-ONLY RECIPIENT 121 96 Non-covered charge(s). N30 Recipient ineligible for this service.Our records indicate that we shouldbe the third payer for this claim. WeTHIS SERVICE WAS NOT APPROVED BYcannot process this claim until weMEDICARE. PLEASE RESUBMIT THIShave received payment informationSERVICE TO MEDICAID WITH A COPY OFfrom the primary <strong>and</strong> secondaryTHE MEDICARE EOMB. 122 A1 Claim denied charges. MA64 payers.CLAIM DENIED. THIS CLAIM MAY NOT SPANTHE RECIPIENT'S 1ST BIRTHDAY. PLEASEREFER TO THE BILLING INSTRUCTIONS INYOUR PROVIDER MANUAL. 123 6CLAIM DENIED. MENTAL HOSPITALSERVICES ARE NOT PAYABLE FORRECIPIENTS AGE 22 THROUGH 64. 124 (pend only), 144 6The procedure/revenue code isinconsistent with the patient's age. N30 Recipient ineligible for this service.The procedure/revenue code isinconsistent with the patient's age. N30 Recipient ineligible for this service.Missing/in<strong>com</strong>plete/invalid toothnumber/letter.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.THE TOOTH NUMBER IS MISSING ORINVALID. 125, 128 A1 Claim denied charges. N37PROCEDURE CODE(S) IS INVALID FOROTHER THAN ANTERIOR TOOTH NUMBERS. 126 A1 Claim denied charges. N56CLAIM/DETAIL DENIED. TOOTH SURFACE ISINVALID. 127 A1 Claim denied charges. N75THE TOOTH NUMBER IS MISSING ORINVALID. 128 A1 Claim denied charges. N37Missing/in<strong>com</strong>plete/invalid toothsurface information.Missing/in<strong>com</strong>plete/invalid toothnumber/letter.130131THE DAILY LIMITATION FOR THISPROCEDURE CODE HAS BEEN EXCEEDED. 130, 872 119CERTAIN TITLE V PROCEDURE CODES ARELIMITED TO A COMBINED TOTAL OF 12HOURS PER DAY. 131, 870 119132 SERVICE NOT AUTHORIZED. 132 38Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Services not provided orauthorized by designated(network/primary care) providers.N54Claim information is inconsistent withpre-certified/authorized services.134 MAP-34 FORM INCOMPLETE. 255, 256, 282, 283 16136137PLEASE INDICATE THE CORRECT PLACE OFSERVICE CODE. 136 5CLAIM DENIED. SERVICES MUST BE BILLEDIN CONJUNCTION WITH APPROPRIATEROOM CHARGES. 137 107138 CLAIM DENIED. LOCK-IN RECIPIENT. 640 38XH100 LIMITED TO 20 UNITS PER CALENDAR139 YEAR, PER RECIPIENT. 139 119Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.The procedure code/bill type isinconsistent with the place ofservice.Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.Services not provided orauthorized by designatedN29M77Missingdocumentation/orders/notes/summary/report/invoice.Missing/in<strong>com</strong>plete/invalid place ofservice.(network/primary care) providers. N30 Recipient ineligible for this service.Benefit maximum for this timeperiod has been reached.Page 7 of 46 Date: 3/30/2005
KY<strong>EOB</strong>140141142143144145146147148149150151152153154155156157MEDICAID DESCRIPTIONKENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESCLAIM PENDING REVIEW. RECIPIENT IS APOTENTIAL LOCK-IN RECIPIENT. 140 38HIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTIONServices not provided orauthorized by designated(network/primary care) providers. N30 Patient ineligible for this service.The disposition of thisclaim/service is pending further133 review.Payment denied because thisprocedure code/ modifier wasPROCEDURE CODE MODIFIERinvalid on the date of service ofMISSING/INVALID. 141 B18 claim submission.M78PREGNANCY INDICATOR FOR REIPIENT AGEOR SEX. 142 A1 Claim denied charges.The procedure code isCLAIM DETAIL DENIED. REVENUE CODEinconsistent with the providerINVALID FOR PROVIDER TYPE 143 8 type/specialty (taxonomy).M50SHOULD BE BILLED BY PROVIDER OFSERVICE. 144 A1 Claim denied charges. N32THIS PROCEDURE IS NOT CERTIFIED FORTHIS LABORATORY. 145, 374 A1 Claim denied charges. MA51This provider was notcertified/eligible to be paid for thisTHIS PROCEDURE IS NOT COVERED FORprocedure/ service on this date ofTHIS PROVIDER TYPE. 146, 374 B7 service.M67The procedure code isinconsistent with the provider8 type/specialty (taxonomy).PROCEDURE CODE IS NOT ALLOWED WITHPROVIDER TYPE MODIFIER. 147 8THIS PROCEDURE IS NOT APPROPRIATEFOR THIS PLACE OF SERVICE. 148 585The procedure code isinconsistent with the providertype/specialty (taxonomy).Payment adjusted becausetreatment was deemed by thepayer to have been rendered in aninappropriate or invalid place ofservice.The procedure code/bill type isinconsistent with the place ofservice.THIS PROCEDURE/NDC IS NOTAPPROPRIATE FOR THE RECIPIENT'S AGE. 149 6The procedure/revenue code isinconsistent with the patient's age. N56The procedure/revenue code isTHIS PROCEDURE IS INVALID FOR THEinconsistent with the patient'sRECIPIENT'S SEX. 150 7 gender.MA66Payment denied because thisprocedure code/ modifier wasCLAIM DENIED. PROCEDURE NDC CODEinvalid on the date of service ofINVALID FOR DATES OF SERVICE 151, 158 B18 claim submission.MA66Payment denied because thisprocedure code/ modifier wasPROCEDURE/NDC/ REVENUE CODE INVALIDinvalid on the date of service ofOR NOT ON FILE. 152 B18 claim submission.M67PROCEDURE CODE INVALID FOR DIAGNOSISThe diagnosis is inconsistent withCODE 153, 181, 182 11 the procedure.MA66The procedure code isinconsistent with the modifierPROCEDURE CODE INVALID FOR PROVIDERused or a required modifier isTYPE MODIFIER. 154 4 missing.MA66PLEASE RESUBMIT WITH APPROPRIATEGROUP PROVIDER NUMBER IN CLINIC FIELDAND/OR INDIVIDUAL PROVIDER NUMBER INBILLING FIELD. 155 A1 Claim denied charges. N55THE INTERIM RATE FOR THIS PROCEDUREHAS NOT BEEN ESTABLISHED FOR THISPROVIDER. 374 A1 Claim denied charges. N65PROCEDURE CODE INVALID FOR PROVIDERSPECIALTY. 157, 374 B6158 CLAIM DENIED DUE TO INJURY DIAGNOSIS. 158 118This payment is adjusted whenperformed/billed by this type ofprovider, by this type of provider inthis type of facility, or by a providerof this specialty.The procedure code isinconsistent with the providertype/specialty (taxonomy).The diagnosis is inconsistent withthe procedure.N56M78N79N56M64Missing/in<strong>com</strong>plete/invalid HCPCSmodifier.Missing/in<strong>com</strong>plete/invalid revenuecode(s).Provider performing service mustsubmit claim.Missing/in<strong>com</strong>plete/invalid CLIAcertification number for laboratoryservices billed by physician officelaboratory.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Missing/in<strong>com</strong>plete/invalid HCPCSmodifier.Service billed is not <strong>com</strong>patible withpatient location information.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Procedure for billing with group /referring / performing providers werenot followed.Procedure code or procedure ratecount cannot be determined, or wasnot on file, for the date of service/provider.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Missing/in<strong>com</strong>plete/invalid otherdiagnosis.Page 8 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION159160161162164165166167168169170171172173174175176177MORE THAN ONE VISIT PER DETAIL DATEOF SERVICE NOT ALLOWED. EACH VISITMUST BE BILLED AS SEPARATE LINE ITEMS. 159 96 Non-covered charge(s). N63PROCEDURE INVALID FOR TOOTH NUMBERINDICATED. 160 A1 Claim denied charges. N39CLAIM DENIED. REVENUE CODE INVALIDFOR DATE OF SERVICE 161 B18Payment denied because thisprocedure code/ modifier wasinvalid on the date of service orclaim submission.CLAIM DENIED. ANTINEOPLASTIC DRUGSAND CHEMOTHERAPY ADMIN ARE PAYABLEONLY IF THE DIAGNOSIS IS MALIGNANCY. 162 96 Non-covered charge(s).11The diagnosis is inconsistent withthe procedure.PRIMARY SURGICAL PROCEDURE CODEMISSING OR NOT ON FILE. 164 A1 Claim denied charges. MA66SECONDARY SURGICAL PROCEDURE CODEMISSING OR NOT ON FILE. 165 A1 Claim denied charges. M67CLAIM/DETAIL DENIED. PRIMARY SURGICALPROCEDURE CODE INVALID FORRECIPIENT'S AGE. 166 6The procedure/revenue code isinconsistent with the patient's age.SECONDARY SURGICAL PROCEDURE CODEINVALID FOR RECIPIENTS AGE. 167 6The procedure/revenue code isinconsistent with the patient's age. M67The procedure/revenue code isPRIMARY SURGICAL PROCEDURE CODEinconsistent with the patient'sINVALID FOR RECIPIENTS SEX. 168 7 gender.MA66The procedure/revenue code isSECONDARY SURGICAL PROCEDURE CODEinconsistent with the patient'sINVALID FOR RECIPIENTS SEX 169 7 gender.M67PRIMARY SURGICAL PROCEDURE CODEINVALID FOR DATE OF SERVICE. 170 A1 Claim denied charges. MA66SECONDARY SURGICAL PROCEDURE CODEINVALID FOR DATE OF SERVICE. 171 A1 Claim denied charges. M67PRIMARY SURGICAL PROCEDURE CODEThe diagnosis is inconsistent withINVALID FOR DIAGNOSIS CODE 172 11 the procedure.MA66SECONDARY SURGICAL PROCEDURE CODEThe diagnosis is inconsistent withINVALID FOR DIAGNOSIS CODE 173 11 the procedure.M67PROVIDER ON REVIEW FOR PRIMARYSURGICAL PROCEDURE 174 A1 Claim denied charges. MA66The referring/prescribing/rendering provider is not eligible toPROVIDER ON REVIEW FOR SECONDARYrefer/prescribe/ order/perform theSURGICAL PROCEDURE 175 52 service billed.PRIMARY SURGICAL PROCEDURE CODEINDICATED AS ON REVIEW 176 A1 Claim denied charges. MA66SECONDARY SURGICAL PROCEDURE CODEINDICATED AS ON REVIEW 177 A1 Claim denied charges. M67M50MA66Rebill services on separate claimlines.Procedure code is not <strong>com</strong>patiblewith tooth number/letter.Missing/in<strong>com</strong>plete/invalid revenuecode(s).Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).178EXPECTED DATE OF DELIVERY MUST BE ATLEAST 30 DAYS FROM DATE OF CONSENT. 181 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N3N28Missing/in<strong>com</strong>plete/invalid consentform.Consent form requirements notfulfilled.179180CLAIM DENIED-PLEASE RESUBMIT CLAIMWITH REPORT OF PROCEDUREPERFORMED. 179 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N29DETAIL PROCEDURE INDICATE AS ONREVIEW. 180 96 Non-covered charge(s). M67MA07Missingdocumentation/orders/notes/summary/report/invoice.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).The claim information has also beenforwarded to Medicaid for review181RESUBMIT WITH FEDERAL STERILIZATIONCONSENT FORM ATTACHED. 181 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N3N28Missing/in<strong>com</strong>plete/invalid consentform.Consent form requirements notfulfilled.Page 9 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION182RESUBMIT W/OPERATIVE NOTES OREXPLANATION OF PROCEDURE. 180, 182, 183, 355 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.M29Missing/in<strong>com</strong>plete/invalid operativereport.183RESUBMIT W/HYSTERECTOMY CONSENTFORM ATTACHED. 183 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N3N28Missing/in<strong>com</strong>plete/invalid consentform.Consent form requirements notfulfilled.184RESUBMIT WITH MAP-235 OR MAP-236ATTACHED IF APPROPRIATE. 182 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.M58Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.185CONSENT FORM MUST BE SIGNED BYRECIPIENT 30 DAYS PRIOR TOSTERILIZATION 181 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N3N28Missing/in<strong>com</strong>plete/invalid consentform.Consent form requirements notfulfilled.186187STERILIZATION MUST BE 180 DAYS OR LESSFROM DATE CONSENT SIGNED BYRECIPIENT. 181 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N28STAMPED SIGNATURES AREUNACCEPTABLE. 187 A1 Claim denied charges. N3N3N28Missing/in<strong>com</strong>plete/invalid consentform.Consent form requirements notfulfilled.Missing/in<strong>com</strong>plete/invalid consentform.Consent form requirements notfulfilled.188CLAIM DENIED. DOCUMENTATION NEEDEDFOR CLAIM PROCESSING INCLUDESAUDIOLOGIST RECOMMENDATION, MEDICALCLEARANCE STATEMENT, AND INVOICE. 180 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N29Missingdocumentation/orders/notes/summary/report/invoice.189190191192193194195196CONSENT FORM MUST BE SIGNED ANDDATED AT LEAST 72 HOURS PRIOR TOSTERILIZATION PROCEDURE IN CASES OFEMERGENCY SURGERY OR PREMATUREDELIVERY. 181 16THE CLAIM DIAGNOSIS IS MISSING ORINVALID. PLEASE ENTER THE APPROPRIATEDIAGNOSIS CODE AND RESUBMIT THECLAIM. 190 47THE SECONDARY DIAGNOSIS IS INVALID.PLEASE ENTER THE APPROPRIATEDIAGNOSIS CODE AND RESUBMIT THECLAIM. 191 47THIS DIAGNOSIS IS NOT COVERED FOR THERECIPIENTS AGE. 192 9THE SECONDARY DIAGNOSIS IS INVALIDFOR THE RECIPIENT'S AGE. 193 9PRIMARY DIAGNOSIS IS INVALID FORRECIPIENT'S SEX. 194 10THE SECONDARY DIAGNOSIS IS INVALIDFOR RECIPIENT SEX. 195 10HEADER DIAGNOSIS OR COMBINATION OF 2ON REVIEW 196 47Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.This (these) diagnosis(es) is (are)not covered, missing, or areinvalid.This (these) diagnosis(es) is (are)not covered, missing, or areinvalid.The diagnosis is inconsistent withthe patient's age.The diagnosis is inconsistent withthe patient's age.The diagnosis is inconsistent withthe patient's gender.The diagnosis is inconsistent withthe patient's gender.This (these) diagnosis(es) is (are)not covered, missing, or areinvalid.N3N28MA63M64M76M76M64M76M76M64MA63Missing/in<strong>com</strong>plete/invalid consentform.Consent form requirements notfulfilled.Missing/in<strong>com</strong>plete/invalid principaldiagnosis.Missing/in<strong>com</strong>plete/invalid otherdiagnosis.Missing/in<strong>com</strong>plete/invalid diagnosisor condition.Missing/in<strong>com</strong>plete/invalid diagnosisor condition.Missing/in<strong>com</strong>plete/invalid otherdiagnosis.Missing/in<strong>com</strong>plete/invalid diagnosisor condition.Missing/in<strong>com</strong>plete/invalid diagnosisor condition.Missing/in<strong>com</strong>plete/invalid otherdiagnosis.Missing/in<strong>com</strong>plete/invalid principaldiagnosis.198DATES OF SERVICE FOR THIS CLAIM TYPEMUST ALL BE FROM THE SAME MONTH. 198 A1 Claim denied charges. MA31Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong> ending dates of the period billed.Page 10 of 46 Date: 3/30/2005
KY<strong>EOB</strong>200201202203KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAHIPAAADJ RSNCODESMEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKThe referring/prescribing/rendering provider is not eligible toCLAIM/DETAIL DENIED. PROVIDER ONrefer/prescribe/ order/perform theREVIEW FOR THIS DIAGNOSIS. 200 52 service billed.N35THIS DIAGNOSIS IS NOT PAYABLE FOR THISThe diagnosis is inconsistent withPROVIDER TYPE. 201 12 the provider type.M76REC ARE LIMITED TO 1 EPSDT SCREENINGPER TIME SPAN ACCORDING TO THELifetime benefit maximum hasPERIODICITY SCHEDULE. 654 35 been reached.M139CLAIM/DETAIL DENIED. PROCEDURE CODEMODIFIER AG OR TYPE OF SERVICE 7 OR BNOT ALLOWED FOR DATES OF SERVICEAFTER 12/12/94. 203 A1 Claim denied charges. M78This (these) diagnosis(es) is (are)not covered, missing, or areinvalid.MA63204INVALID DIAGNOSIS CODE. CONTACT THEDEPARTMENT FOR MEDICAID SERVICES. 204 47DIAGNOSIS CODE INVALID FOR PROVIDERThe diagnosis is inconsistent with205 TYPE 205 12 the provider type.M76This provider was notcertified/eligible to be paid for thisCLAIM DENIED. RENDERING PROVIDER ISprocedure/ service on this date of206 NOT ELIGIBLE FOR THE DATE OF SERVICE. 206 B7 service.DETAIL DIAGNOSIS INVALID FOR PATIENT'SThe diagnosis is inconsistent with207 AGE. 207 9 the patient's age.M76THIS PROCEDURE IS NOT COVERED FORThe diagnosis is inconsistent with208 THIS DIAGNOSIS 208 11 the procedure.CLAIM DENIED. MOST ANESTHESIASERVICES MUST BE BILLED USINGANESTHESIA PROCEDURE CODES209 BEGINNING WITH 0. 209 A1 Claim denied charges. N56This (these) diagnosis(es) is (are)CLAIM/DETAIL DENIED. THIRD HEADERnot covered, missing, or are210 DIAGNOSIS ON REVIEW. 210 47 invalid.M64211212213214215216217218CLAIM/DETAIL DENIED. THIRD DIAGNOSIS ISNOT ON FILE. 211 47CLAIM/DETAIL DENIED. DETAIL DIAGNOSISINDICATOR INVALID. 212 47THE FOURTH DIAGNOSIS IS MISSING ORINVALID. PLEASE ENTER THE APPROPRIATEDIAGNOSIS CODE AND RESUBMIT THECLAIM. 213 47CLAIM/DETAIL DENIED. SECONDARYHEADER DIAGNOSIS ON REVIEW. 214 47CLAIM/DETAIL DENIED. RECIPIENT'S AGENOT WITHIN VALID RANGES FOR THIRDDIAGNOSIS. 215 9CLAIM/DETAIL DENIED. THIRD DIAGNOSISNOT VALID FOR RECIPIENT'S SEX. 216 10THE FOURTH DIAGNOSIS IS NOT COVEREDFOR THE RECIPIENT' AGE. 217 9FOURTH DIAGNOSIS IS INVALID FORRECIPIENT'S SEX. 218 10219 FOURTH HEADER DIAGNOSIS ON REVIEW. 219 47SERVICE(S) NOT COVERED BY MEDICAID.PRIMARY DIAGNOSIS CODE INDICATESSUBSTANCE ABUSE/CHEMICAL220 DEPENDENCY. 220 47221222THE PROVIDER IS NOT ELIGIBLE ON DATE(S)OF SERVICE (Provider Has Died) 221 B7THE PROVIDER IS NOT ELIGIBLE ON DATE(S)OF SERVICE (Provider Has Been Cancelled) 222 B7This (these) diagnosis(es) is (are)not covered, missing, or areinvalid.This (these) diagnosis(es) is (are)not covered, missing, or areinvalid.This (these) diagnosis(es) is (are)not covered, missing, or areinvalid.This (these) diagnosis(es) is (are)not covered, missing, or areinvalid.The diagnosis is inconsistent withthe patient's ageThe diagnosis is inconsistent withthe patient's gender.The diagnosis is inconsistent withthe patient's ageThe diagnosis is inconsistent withthe patient's gender.This (these) diagnosis(es) is (are)not covered, missing, or areinvalid.This (these) diagnosis(es) is (are)not covered, missing, or areinvalid.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.M64M49M58M64M64M76M64M76M64M76M64M64M64HIPAA REMARK CODEDESCRIPTIONProgram integrity/utilization reviewdecision.Missing/in<strong>com</strong>plete/invalid diagnosisor condition.Denied services exceed the coveragelimit for the demonstration.Missing/in<strong>com</strong>plete/invalid HCPCSmodifier.Missing/in<strong>com</strong>plete/invalid principaldiagnosis.Missing/in<strong>com</strong>plete/invalid diagnosisor condition.Missing/in<strong>com</strong>plete/invalid diagnosisor condition.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Missing/in<strong>com</strong>plete/invalid otherdiagnosis.Missing/in<strong>com</strong>plete/invalid otherdiagnosis.Missing/in<strong>com</strong>plete/invalid valuecode(s) or amount(s).Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/invalid otherdiagnosis.Missing/in<strong>com</strong>plete/invalid otherdiagnosis.Missing/in<strong>com</strong>plete/invalid diagnosisor condition.Missing/in<strong>com</strong>plete/invalid otherdiagnosis.Missing/in<strong>com</strong>plete/invalid diagnosisor condition.Missing/in<strong>com</strong>plete/invalid otherdiagnosis.Missing/in<strong>com</strong>plete/invalid diagnosisor condition.Missing/in<strong>com</strong>plete/invalid otherdiagnosis.Missing/in<strong>com</strong>plete/invalid otherdiagnosis.Missing/in<strong>com</strong>plete/invalid otherdiagnosis.Page 11 of 46 Date: 3/30/2005
KY<strong>EOB</strong>223225226MEDICAID DESCRIPTIONKENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESTHE PROVIDER IS NOT ELIGIBLE ON DATE(S)OF SERVICE (Provider Has Been Suspended) 223 B7HIPAA ADJ RSN CODEDESCRIPTIONThis provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.HIPAAREMARKHIPAA REMARK CODEDESCRIPTIONMissing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.NO HISTORY MATCH FOUND, PLEASERESUBMIT. 225 107M58CANNOT BE PROCESSED ON THIS CLAIMFORM. 226 A1 Claim denied charges. N34 Incorrect claim form for this service.227 CLAIM OVERLAPS YOUR FISCAL YEAR END. 227 A1 Claim denied charges.228229230231232THE PROVIDER IS NOT ELIGIBLE FOR DATEOF SERVICE. 228 B7CLAIM/DETAIL DENIED. BILLING PROVIDERNUMBER INVALID OR NOT ON PROVIDERFILE. 229 B7THE CLINIC IS NOT ELIGIBLE FOR THE CLAIMDATES OF SERVICE. 230 B7CLAIM/DETAIL DENIED. BILLING PROVIDERNAME DOES NOT MATCH THE NAME ONPROVIDER FILE. 231 B7CLAIM/DETAIL DENIED. ACTION REASONCODE INDICATES PROVIDER IS ON REVIEW. 232 B7233 UPIN MISSING OR INVALID. 233 52234235236237238239240241CLAIM/DETAIL DENIED. REFERRINGPROVIDER FLAG SET TO SUSPEND FORREVIEW. 234 52SERVICE NOT PROVIDED UNDER THEThis provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.The referring/prescribing/rendering provider is not eligible torefer/prescribe/ order/perform theservice billed.The referring/prescribing/rendering provider is not eligible torefer/prescribe/ order/perform theservice billed.MEDICAID PROGRAM. 146, 182, 355 96 Non-covered charge(s).PERFORMING PROVIDER NOT ASSOCIATEDWITH THE BILLING PROVIDER. 236 52CLAIM DENIED. CLINIC PROVIDER NUMBERNOT ON FILE. 237 52CLAIM DENIED. BILLINGPHYSICIAN/PROVIDER NOT LISTED ASMEMBER OF CLINIC. 238 B7DETAIL PROVIDER NUMBER INVALID OR NOTON FILE. 239 B7MODIFIER 26 OR 50 CANNOT BE BILLEDWITH THIS PROCEDURE CODE. 240 4PENDING CONFIRMATION OF PROVIDERELIGIBILITY.080, 086, 108, 109, 110, 111,112, 206, 221, 222, 228, 229,289, 301, 829, 241 B7The referring/prescribing/rendering provider is not eligible torefer/prescribe/ order/perform theservice billed.The referring/prescribing/rendering provider is not eligibleto refer/prescribe/ order/performthe service billed.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.The procedure code isinconsistent with the modifierused or a required modifier ismissing.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.M57M58MA112MA29N35M33N31M57M58N31MA112M57M78Missing/in<strong>com</strong>plete/invalid provideridentifier.Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/invalid grouppractice information.Missing/in<strong>com</strong>plete/invalid providername, city, state, or zip code.Program integrity/utilization reviewdecision.Missing/in<strong>com</strong>plete/invalid UPIN forthe ordering/referring /performingprovider.Missing/in<strong>com</strong>plete/invalidprescribing/referring/attendingprovider license number.Missing/in<strong>com</strong>plete/invalid provideridentifier.Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/invalidprescribing/referring/attendingprovider license number.Missing/in<strong>com</strong>plete/invalid grouppractice information.Missing/in<strong>com</strong>plete/invalid provideridentifier.Missing/in<strong>com</strong>plete/invalid HCPCSmodifier.Page 12 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION242243244245246248249NO LEVEL 2 PRICING RECORD FOUND FORMODIFIERS TC OR 26. 242 16PROCEDURE CODE Y2870 INVALID FORDATES OF SERVICE 10/15/94 AND AFTERFOR THIS PROVIDER TYPE. 243 8PROVIDER HAS NOT MET ALLREQUIREMENTS FOR BILLING OTHERLABORATORY AND X-RAY SERVICES. 244 B7Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.The procedure code isinconsistent with the providertype/specialty (taxonomy).This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.THESE SERVICES MAY BE BILLED ONLY BY ARECIPIENT'S HOSPICE PROVIDER. 245 B7N3280022-ROUTINE VENIPUNCTURE SINGLEHOMEBOUND NURSING HOME OR SNF NOTALLOWED SAME DOS/RECIPIENT/PROVIDERAS 80020-BLOOD COLLECTIONVENIPUNCTURE. 346 96 Non-covered charge(s). N20CLAIM DENIED. SURGEON AND ASSISTANTSURGEON BILLING NOT ALLOWED ON SAMEFORM. 248 54Multiple physicians/ assistants arenot covered in this case.PAYMENT REDUCED BECAUSE OURRECORDS SHOW RECIPIENT WAS NOT I NFACILITY FOR ALL OF THE TOTAL BILLEDDAYS. 249 A1 Claim denied charges. MA32N65M67M86M53Procedure code or procedure ratecount cannot be determined, or wasnot on file, for the date of service/provider.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).Provider performing service mustsubmit claim.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for same/similarprocedure within set time frame.Missing/in<strong>com</strong>plete/invalid number ofcovered days during the billingperiod.Missing/in<strong>com</strong>plete/invalid days orunits of service.250251THIS RECIPIENT IS NOT ON OUR ELIGIBILITYFILE. PLEASE VERIFY RECIPIENT MAIDNUMBER. 250 31INCORRECT RECIPIENT IDENTIFICATIONNUMBER. 251 31Claim denied as patient cannot beidentified as our insured.Claim denied as patient cannot beidentified as our insured.MA31N32Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong> ending dates of the period billed.Provider performing service mustsubmit claim.252253254255256RECIPIENT NAME ON CLAIM DOES NOTMATCH RECIPIENT NAME ON THE MEDICAIDELIGIBILITY DATABASE FOR THE MAIDNUMBER SUBMITTED ON YOUR CLAIM. 252 140OUR RECORDS INDICATE THE RECIPIENTWAS DECEASED PRIOR TO THE ENDINGDATE OF SERVICE. 253 13THE RECIPIENT IS NOT ELIGIBLE ON THECLAIM SERVICE DATES. 254, 259, 265 2627Patient/insured healthidentification number <strong>and</strong> namedo not match.RECIPIENT HAS MEDICARE PART B. PLEASEBILL MEDICARE FOR THESE SUPPLIES. 255 96 Non-covered charge(s). MA64OUR RECORDS INDICATE THAT THISRECIPIENT MAY BE ELIGIBLE FORMEDICARE. PLEASE BILL MEDICARE FIRST.IF MEDICARE DENIES THIS SERVICE,RESUBMIT WITH PROOF OF DENIAL. 256 22MA36Missing/in<strong>com</strong>plete/invalid patientname.The date of death precedes thedate of service.Expenses incurred prior tocoverage. N30 Recipient ineligible for this service.Expenses incurred after coverageterminated.Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Payment adjusted because thiscare may be covered by anotherpayer per coordination of benefits.MA04MA83MA64Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information waseither not reported or was illegible.Did not indicate whether we are theprimary or secondary payer. Refer toItem 11 in the HCFA-1500instructions for assistance.Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Page 13 of 46 Date: 3/30/2005
KY<strong>EOB</strong>257KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTIONMEDICAID DESCRIPTIONOUR RECORDS INDICATE THAT THERECIPIENT WAS OVER 21 YRS OLD ON THEDATE(S) OF SERVICE. THE RECIPIENT ISNOT ELIGIBLE FOR THE SERVICE(S). 257 96 Non-covered charge(s). N30 Recipient ineligible for this service.258 MEDICARE SUSPECT/DENTAL. 258 22259THE RECIPIENT HAS MEDICARE PART B.PLEASE BILL MEDICARE. 259 226109The procedure/revenue code isinconsistent with the patient's age.Payment adjusted because thiscare may be covered by anotherpayer per coordination of benefits.Payment adjusted because thiscare may be covered by anotherpayer per coordination of benefits.Claim not covered by thispayer/contractor. You must sendthe claim to the correctpayer/contractor.MA64MA64MA04MA83Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information waseither not reported or was illegible.Did not indicate whether we are theprimary or secondary payer. Refer toItem 11 in the HCFA-1500instructions for assistance.260261CLAIM DENIED. THE KENTUCKY MEDICALASSISTANCE PROGRAM IS ONLYRESPONSIBLE FOR BUY-IN PREMIUMS FORTHIS RECIPIENT. MEDICAID CLAIMS ARE NOTREIMBURSABLE FOR THIS RECIPIENT. 260 96 Non-covered charge(s). N192OUR RECORDS INDICATE THAT THERECIPIENT WAS DECEASED PRIOR TO THEENDING DATE OF SERVICE. 261 13RECIPIENT IS NOT ELIGIBLE ON THE DATEThe date of death precedes thedate of service.Patient is a Medicaid/QualifiedMedicare Beneficiary.262 OF SERVICE. 259, 262 A1 Claim denied charges. N30 Recipient ineligible for this service.Expenses incurred prior to26 coverage.Expenses incurred after coverage27 terminated.CLAIM DENIED. RECIPIENT NOT ELIGIBLE263 FOR PORTION OF DATES OF SERVICE. 263 A1 Claim denied charges. N30 Recipient ineligible for this service.Expenses incurred prior to26 coverage.Expenses incurred after coverage27 terminated.Claim denied as patient cannot beMissing/in<strong>com</strong>plete/invalid patient264 RECIPIENT NAME IS MISSING. 264 31 identified as our insured.MA36 name.INCORRECT RECIPIENT IDENTIFICATIONClaim denied as patient cannot be265 NUMBER. 265 31 identified as our insured.RECIPIENT NOT ELIGIBLE FOR WAIVER266 SERVICES. 266 96 Non-covered charge(s). N30 Recipient ineligible for this service.267WAIVER PAYMENT AMOUNT REDUCED DUETO RECIPIENT CONTINUING INCOME 267 142Claim adjusted by the monthlyMedicaid patient liability amount.268269270RECIPIENT MAID NUMBER ON CLAIM DOESNOT MATCH THE RECIPIENT MAID NUMBERON ATTACHED ELIGIBILITY CARD. 248, 249, 259, 262, 263, 265 140CLAIM DENIED. TARGETED CASEMANAGEMENT SERVICES ARE NOTPAYABLE TO RECIPIENTS ENROLLED IN AWAIVER OR HOSPICE PROGRAM. 269 B9Patient/insured healthidentification number <strong>and</strong> namedo not match.96 Non-covered charge(s). MA61Missing/in<strong>com</strong>plete/invalid socialsecurity number or health insuranceclaim number.Services not covered because thepatient is enrolled in a Hospice. N30 Recipient ineligible for this service.CLAIM DENIED. THIS SERVICE IS NOTPAYABLE FOR A MODEL WAIVER RECIPIENT. 270 96 Non-covered charge(s). N30 Recipient ineligible for this service.271CLAIM DENIED. RECIPIENT AVAILABLEINCOME INFORMATION NOT ON FILE FORTHE MONTH OF SERVICE. PLEASECONTACT DMS AT 502-564-6885. 271 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N58Missing/in<strong>com</strong>plete/invalid patientliability amount.Page 14 of 46 Date: 3/30/2005
KY<strong>EOB</strong>273KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKMEDICAID DESCRIPTIONCLAIM/DETAIL DENIED. PROCEDURE CODE01351 IS LIMITED TO CERTAIN TOOTHNUMBERS. 273 A1 Claim denied charges. N39HIPAA REMARK CODEDESCRIPTIONProcedure code is not <strong>com</strong>patiblewith tooth number/letter274RECIPIENT TREATMENT AUTHORIZATIONINFORMATION NOT FOUND ON INPATIENTHOSPITAL FILE. 274 1562Payment adjusted because thesubmitted authorization number ismissing, invalid, or does not applyto the billed services or provider.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.M62Missing/in<strong>com</strong>plete/invalid treatmentauthorization code.275INPATIENT HOSPITAL TREATMENTAUTHORIZATION NUMBER MISSING ORINVALID. 113, 274 1562Payment adjusted because thesubmitted authorization number ismissing, invalid, or does not applyto the billed services or provider.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.M62Missing/in<strong>com</strong>plete/invalid treatmentauthorization code.276DETAIL DENIED. THIS SERVICE NOTPAYABLE FOR EMPOWER NON-EMERGENCYTRANSPORTATION RECIPIENTS. 276 96 Non-covered charge(s). N30 Recipient ineligible for this service.277278THE ATTACHED THIRD PARTYDOCUMENTATION IS NOT SUFFICIENT.CONTACT UNISYS PROVIDER RELATIONSFOR ASSISTANCE. 277, 279, 280, 281, 377, 467 16CLAIM DENIED. CLAIM/DOCUMENTATIONINDICATES THIRD PARTY PAYMENT WASRECEIVED BY RECIPIENT. 279, 280, 281, 282, 283, 467 100Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.Payment made topatient/insured/responsible party.N225MA92MA92In<strong>com</strong>plete/invaliddocumentation/orders/ notes/summary/ report/ invoice.Missing/in<strong>com</strong>plete/invalid primaryinsurance information.Missing/in<strong>com</strong>plete/invalid primaryinsurance information.279280281282CLAIM/DETAIL INDICATES RECIPIENT HASOTHER INSURANCE BUT NO INSURANCEAMOUNT ENTERED ON CLAIM. 279 22A1CLAIM DENIED. YOUR CLAIM INDICATES THISSERVICE IS DUE TO A WORK-RELATEDACCIDENT/INJURY. PLEASE BILL OTHERINSURANCE FIRST. 280 19Payment adjusted because thiscare may be covered by anotherpayer per coordination of benefits.Claim denied charges.Claim denied because this is awork-related injury/illness <strong>and</strong>thus the liability of the Worker'sCompensation Carrier.RECIPIENT HAS OTHER MEDICALCOVERAGE. BILL OTHER INSURANCE FIRSTOR ATTACH DOCUMENTATION OF DENIALFROM THE INSURANCE CARRIER. 281, 465 A1 Claim denied charges. MA64THE RECIPIENT HAS MEDICARE PART A.PLEASE BILL MEDICARE. 282 109Claim not covered by thispayer/contractor. You must sendthe claim to the correctpayer/contractor.MA92MA64MA04MA83MA04MA83MA64MA04Missing/in<strong>com</strong>plete/invalid primaryinsurance information.Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information waseither not reported or was illegible.Did not indicate whether we are theprimary or secondary payer. Refer toItem 11 in the HCFA-1500instructions for assistance.Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information waseither not reported or was illegible.Did not indicate whether we are theprimary or secondary payer. Refer toItem 11 in the HCFA-1500instructions for assistance.Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information waseither not reported or was illegible.Page 15 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>283284285MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESOUR RECORDS INDICATE RECIPIENT HASMEDICARE PART B, PLEASE BILL MEDICARE. 283 109OUR RECORDS INDICATE THAT THISRECIPIENT IS ELIGIBLE FOR HOSPICECOVERAGE BY MEDICARE. PLEASE BILLMEDICARE FIRST. 284 109REGIONAL ANESTHESIA PROCEDURECODES MAY NOT BE BILLED USING TYPE OFSERVICE 07, MODIFIER AG, OR MORE THANONE UNIT OF SERVICE PER DATE OFSERVICE. 185 4HIPAA ADJ RSN CODEDESCRIPTIONClaim not covered by thispayer/contractor. You must sendthe claim to the correctpayer/contractor.Claim not covered by thispayer/contractor. You must sendthe claim to the correctpayer/contractor.The procedure code isinconsistent with the modifierused or a required modifier ismissing.HIPAA HIPAA REMARK CODEREMARKDESCRIPTIONOur records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondaryMA64 payers.Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information wasMA04 either not reported or was illegible.Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondaryMA64 payers.Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information wasMA04 either not reported or was illegible.Did not indicate whether we are theprimary or secondary payer. Refer toItem 11 in the HCFA-1500MA83 instructions for assistance.N56Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.286287288289290THIS PROCEDURE CODE IS LIMITED TO ONEUNIT OF SERVICE PER DATE OF SERVICE. 186, 635 57PROFESSIONAL COMPONENT REVENUECODE MUST BE BILLED WITH THECORRESPONDING TECHNICAL COMPONENTREVENUE CODE. 187 107PROFESSIONAL COMPONENT REVENUECODE MUST BE BILLED WITHCORRESPONDING TECHNICAL REVENUECODE. CHARGES MOVED TO NON-COVERED. 187 107RENDERING PROVIDER NUMBER MISSINGOR INVALID . 289 B7248, 249, 250, 251, 252, 253,PENDING CONFIRMATION OF RECIPIENT 254, 259, 290, 291, 310, 399,ELIGIBILITY.494 133Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.The disposition of thisclaim/service is pending furtherreview.M63M66M66M57We do not pay for more than one ofthese on the same day.Our records indicate that you billeddiagnostic tests subject to pricelimitations <strong>and</strong> the procedure codesubmitted includes a professional<strong>com</strong>ponent. Only the technical<strong>com</strong>ponent is subject to pricelimitations. Please submit thetechnical <strong>and</strong> professional<strong>com</strong>ponents of this service asseparate line items.Our records indicate that you billeddiagnostic tests subject to pricelimitations <strong>and</strong> the procedure codesubmitted includes a professional<strong>com</strong>ponent. Only the technical<strong>com</strong>ponent is subject to pricelimitations. Please submit thetechnical <strong>and</strong> professional<strong>com</strong>ponents of this service asseparate line items.Missing/in<strong>com</strong>plete/invalid provideridentifier.291292293PENDING POSSIBLE OTHER INSURANCEINVOLVEMENT. 291, 462, 467 22CLAIM SUSPENDED FOR BUY-IN ELIGIBILITYREVIEW. 292 133CLAIM SUSPENDED FOR ELIGIBILITYREVIEW. 910 133Payment adjusted because thiscare may be covered by anotherpayer per coordination of benefits.The disposition of thisclaim/service is pending furtherreview.The disposition of thisclaim/service is pending furtherreview.294KENPAC RECIPIENT. REFERRING PROVIDERNUMBER IS MISSING OR IS NOT THEKENPAC PRIMARY PHYSICIAN/CLINICNUMBER FOR THE DATE(S) OF SERVICE. 290 38Services not provided orauthorized by designated(network/primary care) providers.M68Missing/in<strong>com</strong>plete/invalid attendingor referring physician identification.Page 16 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAA HIPAA REMARK CODEREMARKDESCRIPTIONMissing/in<strong>com</strong>plete/invalid providerM57 identifier.295296BILLING OR REFERRING KENPAC PROVIDERNUMBER IS MISSING OR IS NOT THEKENPAC PHYSICIAN/CLINIC FOR DATE(S)BILLED. KENPAC REFERRING PROVIDERNUMBER SHOULD BE ENTERED IN FIELD 19. 291 38CLAIM DENIED. TYPE OF SERVICE DOESNOT MATCH PROCEDURE MODIFIER. 296 4297 RECIPIENT IS NOT ELIGIBLE FOR HOSPICE. 297 28A1RECIPIENT IS NOT ELIGIBLE FOR HOSPICE298 FOR BILLED DATES OF SERVICE. 298 28A1HOSPICE RECIPIENT. OUR FILES SHOWRECIPIENT IS COVERED BY ANOTHERHOSPICE PROVIDER FOR BILLED DATE(S)299 OF SERVICE. 299 B9SERVICE PAYS ZERO FOR PRIMARY CARE300 AND RURAL HEALTH CLAIMS 119301Services not provided orauthorized by designated(network/primary care) providers.The procedure code isinconsistent with the modifierused or a required modifier ismissing.Coverage not in effect at the timeM68M57MA66Missing/in<strong>com</strong>plete/invalid attendingor referring physician identification.Missing/in<strong>com</strong>plete/invalid provideridentifier.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.the service was provided. N30 Recipient ineligible for this service.Claim denied charges.Coverage not in effect at the timethe service was provided. N30 Recipient ineligible for this service.Claim denied charges.Services not covered because thepatient is enrolled in a Hospice. N30 Recipient ineligible for this service.Benefit maximum for this timeperiod has been reached.Procedures for billing withgroup/referring/performing providerswere not followed.RENDERING PROVIDER NOT LISTED AS AMEMBER OF THE BILLING GROUP. 301 A1 Claim denied charges. N55303THIS SERVICE MUST BE BILLED FOR AMINIMUM OF 8 UNITS PER DATE OFSERVICE. 303 57Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.M53Missing/in<strong>com</strong>plete/invalid days orunits of service.304305OFFICE EMERGENCY NOT COVERED SAMEDATE OF SERVICE AS ANORPLANT/REMOVAL 347, 348 57CLAIM/DETAIL DENIED. THIS PROCEDURECODE IS INVALID FOR THE PROVIDERPROFESSIONAL CODE (1ST DIGIT OFMODIFIER). 305 B18Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.Payment denied because thisprocedure code/ modifier wasinvalid on the date of service ofclaim submission.N20M86N56Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.306307A HOSPICE RECIPIENT - RECYCLE FOR EDIT298. 106, 306 B9CLAIM/DETAIL DENIED. THIS PROCEDURECODE IS NOT PAYABLE UNLESS BILLED INCONJUNCTION WITH OTHER DESIGNATEDPROCEDURES. 307 107Services not covered because thepatient is enrolled in a Hospice. N30 Recipient ineligible for this service.Claim/service denied because therelated or qualifying claim/serviceProcedure code billed is notwas not previously paid orcorrect/valid for the services billed oridentified on this claim.N56 the date of service billed.308310311DETAIL DENIED. REQUIREDDOCUMENTATION IS MISSING OR DOES NOTVERIFY THAT MEDICAL ASSISTANCE WASPROVIDED. 180 16NEW ADMISSION NOT PAYABLE BECAUSEClaim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.OF NON-COMPLIANCE 310 96 Non-covered charge(s). MA41CORRECTED PAYMENT PER ADJUSTMENTREQUEST. 125M29Missing/in<strong>com</strong>plete/invalid operativereport.Missing/in<strong>com</strong>plete/invalidaddmission type.Payment adjusted due to asubmission/billing error(s).Additional information is suppliedusing the remittance adviceremarks codes wheneverappropriate. MA67 Correction to a prior claim.316319CLAIM/DETAIL PAID. CLAIMS HISTORYREFLECTS THE TOOTH NUMBERPREVIOUSLY EXTRACTED. PLEASE CHECKRECORDS AND VERIFY TOOTH NUMBER. 316, 400 18 Duplicate claim/service. N39INCORRECT PROVIDER NUMBERSUBMITTED - PAYMENT DELAYED. 319 133The disposition of thisclaim/service is pending furtherreview.M57Procedure code is not <strong>com</strong>patiblewith tooth number/letter.Missing/in<strong>com</strong>plete/invalid provideridentifier.Page 17 of 46 Date: 3/30/2005
KY<strong>EOB</strong>321322325KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAHIPAAADJ RSNCODESMMIS EXCEPTIONMEDICAID DESCRIPTIONCODE(S)EPSDT SCREENING PROCEDURES ARE NOTPAYABLE WITHIN 30 DAYS OF AN EPSDTRELATED PROCEDURES. 321 97EPSDT RELATED PROCEDURES ARE NOTPAYABLE WITHIN 30 DAYS OF AN EPSDTSCREENING PROCEDURES. 322 97CLAIM/DETAIL DENIED. SCREENINGPROCEDURE CODE INVALID FORRECIPIENT'S AGE. 325 6HIPAA ADJ RSN CODEDESCRIPTIONPayment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.The procedure/revenue code isinconsistent with the patient's age.HIPAA HIPAA REMARK CODEREMARKDESCRIPTIONService denied because paymentalready made for similar procedureM86 within set time frame.Service denied because paymentalready made for similar procedureM86 within set time frame.MA66Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.326327328329330331CLAIM DENIED. BILL/INVOICE MUSTACCOMPANY CLAIM. 326 16PROCEDURE/NDC REQUIRES PRIORAUTHORIZATION. 327, 332, 355, 681, 104 62PRIMARY SURGICAL PROCEDUREREQUIRES PRIOR AUTHORIZATION. 328 62SECONDARY SURGICAL PROCEDUREREQUIRES PRIOR AUTHORIZATION 329 62DETAIL DENIED. DETAIL UNITS BILLEDEXCEED UNITS PRIOR AUTHORIZED. 330 62PAYMENT REDUCED BY AMOUNTPREVIOUSLY PAID. POST OP INCLUDED INPROCEDURE. 331, 371 97Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Payment is included in theallowance for anotherservice/procedure.N29M144Missingdocumentation/orders/notes/summary/report/invoice.Pre-/post-operative care payment isincluded in the allowance for surgery/ procedure.Payment denied/reduced for333NONSTEROIDAL ANTI-INFLAMMATORYDRUGS REQUIRE PRIOR AUTHORIZATION. 333 62absence of, or exceeded, precertification/authorization.334 SUPPLY NOT COVERED ON RENTAL ITEM. 334, 404 96 Non-covered charge(s).D3Claim/service denied becauseinformation to indicate if thepatient owns the equipment thatrequires the part or supply wasmissing.M15Separately billed services/tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.335 LACKS REPORT TO JUSTIFY HIGHER FEE. 335 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N29Missingdocumentation/orders/notes/summary/report/invoice.33734034134257CATHETERIZATION PROCEDURES80021,80023 AND 80024 NOT ALLOWEDSAME DOS/RECIPIENT/ PROVIDER. 336, 337, 338, 339 97ONLY THREE FOLLOW UP EXAMS ALLOWEDDURING THE SIX MONTH PERIODFOLLOWING THE FITTING OF A HEARINGAID. 340 119AN OFFICE VISIT, ER VISIT ORCONSULTATION ARE NOT PAYABLE ON THESAME DATE OF SERVICE AS A HOSPITALADMISSION. 341 B14AN OFFICE VISIT AND/OR ER VISIT ARE NOTPAYABLE ON THE SAME DATE OF SERVICEAS A CONSULTATION. 342 B14Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.Payment is included in theallowance for anotherservice/procedure.Benefit maximum for this timeperiod has been reached.Payment denied because only onevisit or consultation per physicianper day is covered.Payment denied because only onevisit or consultation per physicianper day is covered.N20M86M139N20M86N20M86Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Denied services exceed the coveragelimit for the demonstration.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Page 18 of 46 Date: 3/30/2005
KY<strong>EOB</strong>343344345MEDICAID DESCRIPTIONKENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONCLAIM MASS ADJUSTED DUE TO ARETROACTIVE RATE CHANGE 343 A2 Contractual adjustment. M80AN OFFICE VISIT IS NOT PAYABLE ON THEPayment is included in theSAME DATE OF SERVICE AS ANallowance for anotherEMERGENCY ROOM VISIT. 344 97 service/procedure.N2080020-BLOOD COLLECTION VENIPUNCTURENOT ALLOWED SAME DOS/RECIPIENT/PROVIDER AS 80022-ROUTINEVENIPUNCTURE SINGLE HOMEBOUNDNURSING HOME OR SNF. 345 97Payment is included in theallowance for anotherservice/procedure.HIPAA HIPAA REMARK CODEREMARKDESCRIPTIONNot covered when performed duringthe same session/date as apreviously processed service for thepatient.N20Service not payable with otherservice rendered on the same date.Service not payable with otherservice rendered on the same date.347348349DENTURE RELATED EMERGENCY SERVICES09110 AND UPPER OR LOWER DENTURERELINE 05750 NOT PAYABLE ON SDOS 347 9597ROOM CHARGES REDUCED TO SEMIPRIVATE RATE. 348 78EMERGENCY DENTAL PROCEDURES ANDEXTRACTION PROCEDURES NOT PAYABLEON SDOS. 349, 350 97Benefits adjusted. Planprocedures not followed.Payment is included in theallowance for anotherservice/procedure.Non-Covered days/Room chargeadjustment.Payment is included in theallowance for anotherservice/procedure.M63M63We do not pay for more than one ofthese on the same day.We do not pay for more than one ofthese on the same day.350351DETAIL DENIED. FILLINGS ARE NOTPAYABLE FOR THE SAME TOOTH AND THESAME DATE OF SERVICE AS EMERGENCYSERVICES (09110) OR SEALANTS (01351). 351, 352 97INCORRECT NUMBER OF DAYS COVEREDAND NON-COVERED. 351 78Payment is included in theallowance for anotherservice/procedure.Non-Covered days/Room chargeadjustment.N20M86MA33M53Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Missing/in<strong>com</strong>plete/invalidnoncovered days during the billingperiod.Missing/in<strong>com</strong>plete/invalid days orunits of service.352353CLAIM DENIED. INAPPROPRIATEPROCEDURE CODE USED. 355 B8INDIVIDUAL ALLERGY TESTINGPROCEDURES ARE NOT PAYABLE WITHW0308-MAXIMUM ALLOWABLE PER ALLERGYTESTING OF SERVICE. 353, 405 97Claim/service notcovered/reduced becausealternative services wereavailable, <strong>and</strong> should have beenutilized.Payment is included in theallowance for anotherservice/procedure.MA31N56M71Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong> ending dates of the period billed.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Total payment reduced due tooverlap of tests billed.354355356CLAIM DENIED. LITER FLOW PER MINUTEAND NUMBER OF HOURS MUST BEPRESENT TO PROCESS CLAIM. 355 16FEE ADJUSTED TO MAXIMUM ALLOWABLEAMOUNT 355, 621 B5Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.Payment adjusted becausecoverage/ program guidelineswere not met or were exceeded.CLAIM/DETAIL DENIED AFTER REVIEW BYMEDICAL CONSULTANTS. 355 A1 Claim denied charges. N10N14M85Payment based on a contractualamount or agreement, fee schedule,ormaximum allowable amount.Claim/service adjusted based on thefindings of a revieworganization/professionalconsult/manual adjudication /medicalor dental advisor.Subjected to review of physicianevaluation <strong>and</strong> managementservices.Missingdocumentation/orders/notes/summary/report/invoice.357 INVOICE MUST HAVE ITEM BILLED NOTED. 357 A1 Claim denied charges. N29Payment adjusted due to asubmission/billing error(s).Additional information is suppliedusing the remittance adviceREFER TO THE ADJUSTMENT REASONremarks codes whenever359 CODE. 359 125 appropriate. MA67 Correction to a prior claim.360 FEE ADJUSTED PER CLAIM CREDIT. 360 88Adjustment amount representscollection against receivablecreated in prior overpayment. MA67 Correction to a prior claim.Page 19 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>361MMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESMEDICAID DESCRIPTIONGENERAL OPHTHALMOLOGICAL SERVICESNOT PAYABLE ON THE SAME DATE OFSERVICE AS SPECIAL OPHTHALMOLOGICALSERVICES. 361, 362 97HIPAA ADJ RSN CODEDESCRIPTIONPayment is included in theallowance for anotherservice/procedure.HIPAAREMARKN20M86HIPAA REMARK CODEDESCRIPTIONService not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.362363PATIENT LIABILITY APPLIED TO ALLOWEDAMOUNT FOR THIS CLAIM. 362 142ROOT REMOVAL NOT PAYABLE ON SAMEDATE OF SERVICE AS THE TOOTHEXTRACTION 364, 365 97364 PAYMENT REDUCED BY OTHER INSURANCE 23Claim adjusted by the monthlyMedicaid patient liability amount.Payment is included in theallowance for anotherservice/procedure.Payment adjusted becausecharges have been paid byanother payer.N20M86Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.365 FEE ADJUSTED TO MAXIMUM ALLOWABLE. 42Charges exceed our fee scheduleor maximum allowable amount.N14Payment based on a contractualamount or agreement, fee schedule,or maximum allowable amount.366367368369370371372373CLAIM DENIED. BILLED AMOUNT MAY NOTEXCEED $50.00 PER UNIT OF SERVICE. 366 42THIS SERVICE PAID COINSURANCE AND/ORDEDUCTIBLE. 367 119PROVIDER IS NOT ELIGIBLE TO BILL FORHOME HEALTH SUPPLIES AND/OR VISITS. 368 B7ORIGINAL PSYCHIATRIC EVALUATION ANDREGULAR HOSPITAL ADMISSION NOTPAYABLE ON SAME DATE OF SERVICE. 309, 407 97PAYMENT MODE NOT FOUND FOR BILLINGPROVIDER 370 B7REIMBURSEMENT RATE NOT FOUND FORDATE OF SERVICE 371 B7HOSPITAL FOLLOW-UP VISITS ANDORIGINAL PSYCHIATRIC DIAGNOSTICEVALUATION AND/OR FOLLOW-UPPSYCHIATRIC CARE ARE NOT ALLOWEDFOR SAME DATE OF SERVICE. 373, 408 97UNITS OF SERVICE HAVE BEEN REDUCEDTO THE REMAINING PRIOR AUTHORIZEDQUANTITY. 539 62Charges exceed our fee scheduleor maximum allowable amount.Benefit maximum for this timeperiod has been reached.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.Payment is included in theallowance for anotherservice/procedure.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.Payment is included in theallowance for anotherservice/procedure.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.M139MA125N65N20M86N65N65N20M86Denied services exceed the coveragelimit for the demonstration.Per legislation governing thisprogram, payment constitutespayment in full.Procedure code or procedure ratecount cannot be determined, or wasnot on file, for the date of service/provider.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Procedure code or procedure ratecount cannot be determined, or wasnot on file, for the date of service/provider.Procedure code or procedure ratecount cannot be determined, or wasnot on file, for the date of service/provider.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.374REPAYMENT PORTION OF THISADJUSTMENT HAS BEEN DENIED.RECOUPMENT IS UNDER FINANCIAL ITEMS. 374 A1 Claim denied charges.376 CLAIM DENIED. MAC FIELD INVALID. 376 A1 Claim denied charges.377RECIPIENT INCOME/PATIENT LIABILITYDEDUCTION NOT APPLICABLE FOR THISCLAIM. 377 42Charges exceed our fee scheduleor maximum allowable amount.379 PAID BY MEDICAID 42Charges exceed our fee scheduleor maximum allowable amount.MA125Per legislation governing thisprogram, payment constitutespayment in full.380CO-PAY WAS DEDUCTED FROMREIMBURSEMENT. 3 Co-payment Amount. N14Payment based on a contractualamount or agreement, fee schedule,or maximum allowable amount.381CERTAIN SPECIFIED PROCEDURES ARENOT REIMBURSABLE FOR THE SAME DATEOF SERVICE AS EMERGENCY ROOM VISIT 381, 382 97Payment is included in theallowance for anotherservice/procedure.N20M86Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Page 20 of 46 Date: 3/30/2005
KY<strong>EOB</strong>382KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKMEDICAID DESCRIPTIONDETAIL DENIED. BILLED AMOUNT FORIMPLANTABLES MUST BE GREATER THAN$100.00. 355 A1 Claim denied charges. M54HIPAA REMARK CODEDESCRIPTIONMissing/in<strong>com</strong>plete/invalid totalcharges.383CERTAIN INCIDENTAL SURGERIES ARE NOTREIMBURSABLE FOR THE SAME DATE OFSERVICE AS ABDOMINAL SURGERY. 383, 384 97Payment is included in theallowance for anotherservice/procedure.N20M86Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.384DETAIL DENIED. INVOICE MUST BEATTACHED WHEN BILLING IMPLANTABLES. 384 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N29Missingdocumentation/orders/notes/summary/report/invoice.385386387388CERTAIN INCIDENTAL PROCEDURES ARENOT REIMBURSABLE FOR THE SAME DATEOF SERVICE AS A D.& C. PROCEDURE. 385, 386 97DETAIL DENIED. INVOICE AMOUNT MUSTMATCH BILLED AMOUNT. 355 42CERTAIN INCIDENTAL SURGERIES ANDPELVIC SURGERIES ARE NOTREIMBURSABLE FOR THE SAME DATE OFSERVICE. 387, 388 97Payment is included in theallowance for anotherservice/procedure.Charges exceed our fee scheduleor maximum allowable amount.Payment is included in theallowance for anotherservice/procedure.M86THIS REVENUE CODE IS NOT PAYABLEWHEN BILLED WITH ALL INCLUSIVEANCILLARY REVENUE CODE (240). CHARGESMOVED TO NON-COVERED. 188 96 Non-covered charge(s). M50Payment is included in theallowance for another97 service/procedure.389 PAID CLAIM BASED UPON MEDICAL REVIEW. 670 B5DETAIL DENIED. PROCEDURE CODE X0091NOT PAYABLE ON THE SAME DATE OF391 SERVICE AS X0061, X0088, OR X0089. 391 97Payment adjusted becausecoverage/ program guidelineswere not met or were exceeded.Payment is included in theallowance for anotherservice/procedure.N20M86N29N20N10N20M86Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Missingdocumentation/orders/notes/summary/report/invoice.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Missing/in<strong>com</strong>plete/invalid revenuecode(s).Claim/service adjusted based on thefindings of a revieworganization/professionalconsult/manual adjudication /medicalor dental advisor.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.392393394DETAIL DENIED. PROCEDURE CODES X0061,X0088, AND X0089 NOT PAYABLE ON THESAME DATE OF SERVICE AS X0091. 392 97CLAIM DENIED. THE PRIMARY DIAGNOSISCODE IS NOT VALID FOR THIS PROVIDERTYPE. 393 12HOURLY RESPITE SERVICES NOT ALLOWEDFOR SAME DATE OF SERVICE AS DAILYRESPITE SERVICES. 394 97Payment is included in theallowance for anotherservice/procedure.The diagnosis is inconsistent withthe provider type.Payment is included in theallowance for anotherservice/procedure.N20M86MA63N20Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Missing/in<strong>com</strong>plete/invalid principaldiagnosis.Service not payable with otherservice rendered on the same date.395396397THE AMOUNT PAID BY OTHER INSURANCEEQUALS OR EXCEEDS THE AMOUNT OFMEDICAID REIMBURSEMENT FOR THISSERVICE. THE CLAIM IS PAID IN FULL.RECIPIENT SHALL NOT BE BILLED BALANCE. 23DAILY RESPITE SERVICES NOT ALLOWEDFOR SAME DATE OF SERVICE AS HOURLYRESPITE SERVICES. 396 97ACCOMMODATION REVENUE CODES MUSTBE BILLED ON AN INPATIENT CLAIM. 097 5Payment adjusted becausecharges have been paid byanother payer.Payment is included in theallowance for anotherservice/procedure.The procedure code/bill type isinconsistent with the place ofservice.N23N20M86Patient liability may be affected dueto coordination of benefits with othercarriers <strong>and</strong>/or maximum benefitprovisions.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Page 21 of 46 Date: 3/30/2005
KY<strong>EOB</strong>398399MEDICAID DESCRIPTIONKENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONThe procedure code isinconsistent with the modifierused or a required modifier ismissing.HIPAAREMARKHIPAA REMARK CODEDESCRIPTIONCLAIM/DETAIL DENIED. THE PROCEDURECODE MODIFIER IS MISSING OR INVALID. 398 4M78Missing/in<strong>com</strong>plete/invalid HCPCSmodifier.CLAIM/DETAIL DENIED. THIS SERVICE NOTCOVERED FOR THIS RECIPIENT. 399 96 Non-covered charge(s). N30 Recipient is ineligible for this service403404409410411412413414415416417PLEASE GIVE THE DATE(S) OF SURGERYAND RETURN THE INVOICE TO THIS OFFICE. 403 16NURSING FACILITY PRIOR AUTHORIZATIONNOT ON FILE - RECYCLE FOR EDIT 332. 104, 404 62INVALID PROVIDER TYPE BILLED ON CLAIMFORM. 009 52133Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.The disposition of thisclaim/service is pending furtherreview.The referring/prescribing/rendering provider is not eligibleto refer/prescribe/ order/performFORMAT INVALID FOR ELECTRONIC CLAIMS.PLEASE CONTACT ECS HELP DESK AT 1-800-205-4696. 009, 410 A1 Claim denied charges. M60MA31Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong> ending dates of the period billed.the service billed. N34 Incorrect claim form for this service.Rejected without appeal rights due toinvalid CMN form or format.Resubmit with <strong>com</strong>pleted, OMBapprovedform or in an approvedformat.DUE TO THE END OF YOUR FISCAL YEAR,PLEASE REBILL THESE MULTIPLE MONTHSOF SERVICE ON SEPARATE INVOICES - ONEINVOICE FOR EACH MONTH. 411 A1 Claim denied charges. N74DETAIL DENIED. ONLY ONE DATE OFSERVICE ALLOWED PER DETAIL. 412 96 Non-covered charge(s). N20Resubmit with multiple claims, eachclaim covering services provided inonly one calendar month.Service not payable with otherservice rendered on the same date.Patient not enrolled in the billingproviders managed care plan on thedate of service.RECIPIENT NOT ENROLLED IN MANAGEDCARE DURING DATES OF SERVICE. 413 96 Non-covered charge(s). N52Payment for charges adjusted.Charges are covered under aRECIPIENT ENROLLED IN MANAGED CAREcapitation agreement/ managedDURING DATES OF SERVICE. 414 24 care plan N30 Recipient ineligible for this service.FFS CLAIM HAS A MANAGED CAREPROVIDER TYPE. 415 24Payment for charges adjusted.Charges are covered under acapitation agreement/ managedcare planPayment for charges adjusted.Charges are covered under acapitation agreement/ managedcare planCAPITATION RATE NOT WITHIN DATES OFSERVICE. 416 24CLAIM DENIED. INVALID OR MISSINGCAPITATION INDICATOR. 417 A1 Claim denied charges.N65Procedure code or procedure ratecount cannot be determined, or wasnot on file, for the date of service/provider.418 CLAIM DENIED. INVALID ENCOUNTER TYPE. 418 A1 Claim denied charges.419 CLAIM DENIED. INVALID ENC RECEIPT DATE. 419 A1 Claim denied charges.420CLAIM DENIED. INVALID ENC PAYMENTAMOUNT. 420 A1 Claim denied charges.421CLAIM DENIED. INVALID ENC PAYMENTDATE. 421 A1 Claim denied charges.422CLAIM DENIED. INVALID ENC ADJUSTMENTTCN. 422 A1 Claim denied charges.423CLAIM DENIED. INVALID RECIP NOT ELIGFOR PHYSICAL. 423 A1 Claim denied charges. N30 Recipient ineligible for this service424CLAIM DENIED. INVALID RECIP NOT ELIGFOR BEHAVIORAL. 424 A1 Claim denied charges. N30 Recipient ineligible for this service425DETAIL DENIED. ENCOUNTER-ONLYPROCEDURE CODE. THIS PROCEDURECODE IS NOT PAYABLE FOR FEE-FOR-SERVICE CLAIMS. 425 A1 Claim denied charges. M67Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).427428429CLAIM DENIED. RESUBMIT AN ADJUSTMENTON RELATED PAID CLAIM WITHJUSTIFICATION FOR DUPLICATED SERVICE. 490 97Payment is included in theallowance for anotherservice/procedure.M86Service denied because paymentalready made for similar procedurewithin set time frame.We do not pay for more than one ofthese on the same day.M63FFS NOT ALLOWED, RECIP ELIGIBLE FORBEHAVIORAL HEALTH MANAGED CARE. 428 A1 Claim denied charges. N30 Recipient ineligible for this serviceCLAIM DENIED. PARTNERSHIP NUMMISMATCH 429 A1 Claim denied charges.Page 22 of 46 Date: 3/30/2005
KY<strong>EOB</strong>KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAHIPAAADJ RSNCODESMMIS EXCEPTIONMEDICAID DESCRIPTIONCODE(S)CLAIM DENIED. ENCOUNTER, INV. TCN TOCREDIT 430 A1 Claim denied charges.HIPAA ADJ RSN CODEDESCRIPTION430This provider was notcertified/eligible to be paid for thisprocedure/ service on this date of431 RESERVED FOR MANAGED CARE. 431 B7 service.CLAIM DENIED. SEQ# MISMATCH ACROSS432 CLAIM. 432 A1 Claim denied charges.CLAIM DENIED. VOID/RESUB INVALID FOR433 XOVER. 433 A1 Claim denied charges.434 RESERVED FOR MANAGED CARE. 434 A1 Claim denied charges.435 RESERVED FOR MANAGED CARE. 435436 RESERVED FOR MANAGED CARE. 436437440441442443CLAIM DENIED. CERTAIN OUTPATIENTHOSPITAL CHARGES ARE NOT PAYABLEWITHIN 3 DAYS PRIOR TO AN INPATIENTHOSPITAL ADMISSION (AND VICE VERSA). 437 97REVENUE CODE 582 LIMITED TO 4 UNITSPER CALENDAR WEEK (SUNDAY THROUGHSATURDAY) 440 119PROCEDURE CODES 99244 AND 99245 ARELIMITED CUMULATIVELY TO ONE UNIT PERDAY PER RECIPIENT 441 97THIS PROCEDURE CODE IS NOT PAYABLEON THE SAME DATE OF SERVICE ASPROCEDURE CODES 99244 AND 99245 442 97PROCEDURE CODES 99244 AND 99245 ARENOT PAYABLE ON THE SAME DATE OFSERVICE AS CERTAIN OTHER TITLE VPROCEDURE CODES 443 97PLEASE CORRECT INVALID OR MISSING NDCPayment is included in theallowance for anotherservice/procedure.Benefit maximum for this timeperiod has been reached.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.HIPAAREMARKHIPAA REMARK CODEDESCRIPTION444 NUMBER. 444 A1 Claim denied charges. M119 National Drug code (NDC) needed.PROCEDURE CODE 99244 IS LIMITED TOONE PER FIVE YEARS, PER RECIPIENT, PERBenefit maximum for this time445 PROVIDER 445 119 period has been reached.PROCEDURE CODE 99245 IS LIMITED TOONE PER FIVE YEARS, PER RECIPIENT, PERBenefit maximum for this time446 PROVIDER 446 119 period has been reached.Benefit maximum for this time447 X0079 LIMITED TO 8 UNITS PER DAY 447 119 period has been reached.The disposition of thisRECIPIENT NOT ON ELIGIBILITY FILE -claim/service is pending further448 SUSPEND FOR EDIT 250. 248 133 review. N30 Recipient ineligible for this service.449450THE RECIPIENT ELIGIBILITY MAID NUMBERON THE MEDICAID CARD ATTACHED WITHYOUR CLAIM IS INCORRECT. 249 31CLAIM DETAIL DENIED. ASSESSMENTPROCEDURES ARE LIMITED TO ONE (1) PERRECIPIENT, PER PROVIDER DURING THERECIPIENT'S ASSESSMENT PERIOD ON THEPRIOR AUTHORIZATION FILE FOR THE CASEMANAGEMENT. 450 119Claim denied as patient cannot beidentified as our insured.Benefit maximum for this timeperiod has been reached.MA61N55Missing/in<strong>com</strong>plete/invalid socialsecurity number or health insuranceclaim numberProcedures for billing withgroup/referring/performing providerswere not followed.451CLAIM DETAIL DENIED. UNABLE TO APPLYASSESSMENT PROCEDURE LIMITATION DUETO NO CASE MANAGEMENT ON PRIORAUTHORIZATION FILE. CONTACT PRO. 451 62Payment denied/reduced forabsence of, or exceeded, precertification/authorization.M139N10Denied services exceed the coveragelimit for the demonstration.Claim/service adjusted based on thefindings of a revieworganization/professionalconsult/manual adjudication /medicalor dental advisor.452 X0080 LIMITED TO 12 UNITS PER WEEK 452 119X0061, X0088, X0089 AND X0103 LIMITED TO453 1 UNIT, CUMULATIVELY, PER DAY 453 119454 X0079 LIMITED TO 32 UNITS PER DAY. 454 119THIS PROCEDURE CODE LIMITED TO 48455 UNITS PER DAY. 455 119THIS PROCEDURE CODE LIMITED TO 16456 UNITS PER DAY. 456 119457 X0100 AND X0101 LIMITED TO ONE UNIT. 457 119458 X0063 LIMITED TO $150.00 PER DAY. 458 119CLAIM/DETAIL DENIED. PROCEDURES WITHGT MODIFIER ARE LIMITED TO FOUR (4) PER459 CALENDAR YEAR. 459 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.N54Claim information is inconsistent withpre-certified/authorized services.Page 23 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>460MMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESMEDICAID DESCRIPTIONTHIS PROCEDURE CODE LIMITED TO 16UNITS PER DAY. 460 119461 XL307 LIMITED TO 80 UNITS PER WEEK. 461 119PROVIDER TYPE/CLAIM TYPE NOT FOUND462 ON MATRIX. 462 119463 PAY TPL CLAIM. 463 119464 PAY AND BILL TPL CLAIM. 464 119465466467RECIPIENT HAS OTHER MEDICALCOVERAGE. BILL OTHER INSURANCE FIRSTOR ATTACH DOCUMENTATION OF DENIALFROM THE INSURANCE CARRIER ANDSUBMIT ON PAPER. 465 16DETAIL DENIED. EARLY INTERVENTION ANDCERTAIN EPSDT-SPECIAL SERVICESPROCEDURES ARE NOT PAYABLE ON THESAME DATE OF SERVICE FOR THE SAMERECIPIENT. 466 97RECIPIENT HAS OTHER MEDICALCOVERAGE. BILL OTHER INSURANCE FIRSTOR ATTACH DOCUMENTATION OF DENIALFROM THE INSURANCE CARRIER. 467 16469 X0096 LIMITED TO 200 PER WEEK. 469 119HIPAA ADJ RSN CODEDESCRIPTIONBenefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.Payment is included in theallowance for anotherservice/procedure.Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.Benefit maximum for this timeperiod has been reached.HIPAAREMARKMA64MA04MA83N20M86MA64MA04MA83HIPAA REMARK CODEDESCRIPTIONOur records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information waseither not reported or was illegible.Did not indicate whether we are theprimary or secondary payer. Refer toItem 11 in the HCFA-1500instructions for assistance.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information waseither not reported or was illegible.Did not indicate whether we are theprimary or secondary payer. Refer toItem 11 in the HCFA-1500instructions for assistance.472473476477478479481RECIPIENTS LIMITED TO ONE DRUGCLASS(GPPC) 681200 PRESCRIPTION/REFILLPER DATE OF SERVICE. 471 119MEDICAID REIMBURSEMENT FOR THEI DATEOF SERVICE HAS ALREADY BEEN MADE.CLAIM PAYMENT SET TO ZERO 473 119RECIPIENT IN AN INSTITUTIONAL SETTINGBenefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M63MA125DURING THE SAME DATE OF SERVICE. 476 18 Duplicate claim/service. M2RECIPIENT IN ANOTHER INSTITUTIONALSETTING DURING THE SAME DATES OFSERVICE. 477, 495 18 Duplicate claim/service. MA133YOUR FACILITY HAS PREVIOUSLY BILLEDAND RECEIVED PAYMENT FOR ALL OR APORTION OF THESE DATES OF SERVICE. 477 18 Duplicate claim/service. M43N47CLAIM DENIED. SERVICES FOR THESEDATES OF SERVICE HAVE BEEN PAID TO ANON-HOSPICE PROVIDER. 479 18 Duplicate claim/service. M86CLAIM/DETAIL DENIED. DUPLICATE SERVICEBILLED. 481 18 Duplicate claim/service.M63N20N47We do not pay for more than one ofthese on the same day.Per legislation governing thisprogram, payment constitutespayment in full.Not paid separately when the patientis an inpatient.Claim overlaps inpatient stay. Rebillonly those services rendered outsidethe inpatient stay.Payment for this service previouslyissued to you or another provider byanother carrier / intermediary.Claim conflicts with another inpatientstay.Service denied because paymentalready made for similar procedurewithin set time frame.We do not pay for more than one ofthese on the same day.Service not payable with otherservice rendered on the same date.Claim conflicts with another inpatientstay.Page 24 of 46 Date: 3/30/2005
KY<strong>EOB</strong>482483MEDICAID DESCRIPTIONKENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAHIPAAADJ RSNCODESMMIS EXCEPTIONCODE(S)470, 472, 473, 474, 475, 480,481, 483, 484, 485, 486, 488,490 18 Duplicate claim/service.HIPAA ADJ RSN CODEDESCRIPTIONCLAIM/DETAIL DENIED. DUPLICATE SERVICEBILLED.DUPLICATE ANESTHESIA SERVICE BILLEDBY PHYSICIAN AND NURSE ANESTHETIST. 487 18 Duplicate claim/service.HIPAAREMARKHIPAA REMARK CODEDESCRIPTION484ONLY ONE ANESTHESIA ALLOWED PER DOSPER RECIPIENT. 487 119Benefit maximum for this timeperiod has been reached.M139M63Denied services exceed the coveragelimit for the demonstration.We do not pay for more than one ofthese on the same day.486487DETAIL PLACE OF SERVICE NOT COVEREDTHROUGH THE PODIATRY PROGRAM. 093 96 Non-covered charge(s). N38ROUTINE FOOT CARE IS NOT PAYABLE FORThe diagnosis is inconsistent withTHIS DIAGNOSIS. 094 11 the procedure.Missing/in<strong>com</strong>plete/invalid place ofservice.489490CLAIM DENIED. THIS SERVICE WASPREVIOUSLY PAID TO ANOTHER PROVIDER. 489 B13CONSECUTIVE OUTPATIENT SERVICES ARENON-PAYABLE DURING A HOSPITALINPATIENT STAY. 590 60Previously paid. Payment for thisclaim/service may have beenprovided in a previous payment.Charges for outpatient serviceswith this proximity to inpatientservices are not covered.M86M63N20N47Service denied because paymentalready made for similar procedurewithin set time frame.We do not pay for more than one ofthese on the same day.Service not payable with otherservice rendered on the same date.Claim conflicts with another inpatientstay.491CLAIM DENIED. RECIPIENT IN ANOTHERINSTITUTIONAL SETTING DURING THE SAMEDATES OF SERVICE. 491 B13Previously paid. Payment for thisclaim/service may have beenprovided in a previous payment.MA133N47Claim overlaps inpatient stay. Rebillonly those services rendered outsidethe inpatient stay.Claim conflicts with another inpatientstay.492DCBS RECIPIENTS MAY NOT RECEIVE TITLEV SERVICES AND IMPACT PLUS/CHMCSERVICES ON THE SAME DATE OF SERVICE. 492 97Payment is included in theallowance for anotherservice/procedure.493494496497498DCBS RECIPIENTS MAY NOT RECEIVE THESAME DCBS MENTAL HEALTH SERVICESFROM TWO DIFFERENT SUB-PROVIDERSON THE SAME DATE OF SERVICE. 493 97DETAIL DENIED. THIS SERVICE IS NOTPAYABLE BEYOND THE BIRTH MONTH OFTHE RECIPIENT'S 18TH BIRTHDAY. 494 6ONLY ONE (1) ANESTHESIA\IV SEDATIONALLOWED PER DATE OF SERVICE PERRECIPIENT. 496 119CLAIM/DENIED. RESUBMIT AN ADJUSTMENTON UNISYS ADJUSTMENT REQUEST FORM. 497 138CLAIM DENIED. ONLY ONE PAYMENTALLOWED PER RECIPIENT, PER DATE OFSERVICE. 498 35Payment is included in theallowance for anotherservice/procedure.The procedure/revenue code isinconsistent with the patient's age.Benefit maximum for this timeperiod has been reached.M63We do not pay for more than one ofthese on the same day.Claim/service denied. Appealprocedures not followed or timelimits not met. N34 Incorrect claim form for this service.Lifetime benefit maximum hasbeen reached.M63We do not pay for more than one ofthese on the same day.499 CLAIM PENDING REVIEW OF HISTORY.The following exceptioncodes apply to this <strong>EOB</strong>: 130-131, 139, 302, 304, 306, 308-309, 311-318, 321-324, 326,331, 334-335, 337-339, 341-343, 347-352, 358, 360-365,373, 381-388, 391-392, 394,396, 400-404, 406-408, 441-442, 445-446, 466, 468, 471,474, 477-484, 486-493, 495-496, 498, 501, 533-534, 537,539-540, 542, 548-553, 556,560, 569-570, 579-592, 606,641, 643, 651-662, 667-668,670, 672, 674-677, 680-683,685-686, 688-693, 695, 697-698, 701-710, 712-714, 722,724, 729-730, 732-735, 737-740, 742-744, 747, 749, 791,798-819, 820, 822-823, 825-827, 846, 852-860, 862-863,879-880, 883-885, 887 133The disposition of thisclaim/service is pending furtherreview.Page 25 of 46 Date: 3/30/2005
KY<strong>EOB</strong>500501KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAHIPAAADJ RSNCODESMMIS EXCEPTIONMEDICAID DESCRIPTIONCODE(S)CLAIM DENIED. BIFOCAL OR SINGLE VISIONLENSES LIMITED TO TWO SETS PER 12MONTHS. 500, 524 119PROFESSIONAL FEE-DISPENSING SERVICEALLOWED ONE PER 12 MONTHS PERRECIPIENT. 501 119502 ONE FAMILY PLANNING SERVICE PER DOS. 302 119ANNUAL FAMILY PLANNING VISITS LIMITEDTO 1 PER RECIPIENT PER NINE MONTHS503 PER CLINIC. 503, 523 119FAMILY PLANNING RECIPIENTS LIMITED TOONE INITIAL VISIT PER PROVIDER PER504 THREE YEAR PERIOD. 304 119505506507508509510511HIPAA ADJ RSN CODEDESCRIPTIONBenefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.HIPAAREMARKRECIPIENT IN INSTITUTIONAL SETTINGDURING SAME DATE OF SERVICE. 478, 505 18 Duplicate claim/service. MA133Payment is included in theCBC AND COMPONENTS NOT ALLOWEDallowance for anotherSAME DOS. 306 97 service/procedure.N20PACKAGE OF 12 TESTS AND COMPONENTSNOT ALLOWED SAME DOS. 507 97COMPLETE BLOOD COUNT ANDCOMPONENTS NOT ALLOWED SAME DOS. 308 97RECIPIENTS ARE LIMITED ON INITIAL ANDFOLLOW UP VISITS TO ONE PER YEAR PERPROVIDER FOR DOS PRIOR TO SEPT. 1,1985. 642 119RECIPIENTS LIMITED ON SELECTED INITIALAND FOLLOW UP VISITS TO 1 PER DATE OFSERVICE. 510 119PAYMENT FOR REVISION OFARTERIOVENOUS SHUNT IS INCLUDED INFEE FOR INITIAL INSERTION WHENREVISION IS PERFORMED WITHIN 21 DAYSOF ORIGINAL PROCEDURE. 311, 401 97Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Payment is included in theallowance for anotherservice/procedure.M139M90M63M139M139M86M71M71M90M63M15N19HIPAA REMARK CODEDESCRIPTIONDenied services exceed the coveragelimit for the demonstration.Not covered more than once in a 12month period.We do not pay for more than one ofthese on the same day.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Claim overlaps inpatient stay. Rebillonly those services rendered outsidethe inpatient stay.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Total payment reduced due tooverlap of tests billed.Total payment reduced due tooverlap of tests billed.Not covered more than once in a 12month period.We do not pay for more than one ofthese on the same day.Separately billed services/ tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Procedure code incidental to primaryprocedure.512CLAIM DENIED. FOLLOW UP VISIT INCLUDEDIN REIMBURSEMENT FOR DELIVERY. 312 97Payment is included in theallowance for anotherservice/procedure.M15N19Separately billed services/ tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Procedure code incidental to primaryprocedure.513CLAIM DENIED. FOLLOW-UP HOSPITALVISITS INCLUDED IN REIMBURSEMENT FORC-SECTION. 313 97Payment is included in theallowance for anotherservice/procedure.M15N19Separately billed services/tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Procedure code incidental to primaryprocedure.514515516517CAST APPLICATION/ REMOVAL INCLUDED INREIMBURSEMENT FOR SURGERY. 314, 341 97CLAIM DENIED CULTURES/SMEARS NOTALLOWED SAME DOS FOR SAMECONDITION. 315, 335 97Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.EXTRACTION OR EXPOSURE OF TOOTHDISALLOWED IF PREVIOUSLY EXTRACTEDOR EXPOSED. 316 18 Duplicate claim/service.CLAIM DENIED. EMERGENCY SERVICESLIMITED TO ONE PER DOS PER RECIPIENTPER PROVIDER. 317 119Benefit maximum for this timeperiod has been reached.M15N19N20M86M63Separately billed services/tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Procedure code incidental to primaryprocedure.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.We do not pay for more than one ofthese on the same day.Page 26 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>518MMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESMEDICAID DESCRIPTIONCLAIM/DETAIL DENIED. INITIAL TOOTHEXTRACTION LIMITED TO ONE PERDOS/RECIPIENT /PROVIDER. USEPROCEDURE 07120 FOR EACH ADDITIONALTOOTH EXTRACTED 318 119HIPAA ADJ RSN CODEDESCRIPTIONBenefit maximum for this timeperiod has been reached.HIPAAREMARKM63HIPAA REMARK CODEDESCRIPTIONWe do not pay for more than one ofthese on the same day.519CLAIM DENIED. REIMBURSEMENT FORCIRCUMCISION WITHIN TEN DAYS OFDELIVERY IS INCLUDED IN DELIVERY FEE. 519 97Payment is included in theallowance for anotherservice/procedure.M15N19Separately billed services/tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Procedure code incidental to primaryprocedure.520MAINTENANCE DRUG DAYS SUPPLY LESSTHAN 30 DAYS. 520, 523 91 Dispensing fee adjustment. N14Payment based on a contractualamount or agreement, fee schedule,or maximum allowable amount521COMPREHENSIVE CLIENT RE-EVALUATIONNOT ALLOWED WITHIN 12 MONTHS OFCOMPREHENSIVE CLIENT EVALUATION. 521 119Benefit maximum for this timeperiod has been reached.M139Denied services exceed the coveragelimit for the demonstration.522523524525COMPREHENSIVE CLIENT RE-EVALUATIONLIMITED TO ONCE PER LIFE TIME. 522 119RESIDENTIAL COMPONENT SERVICE NOTALLOWED WITH IN-HOME SCL SERVICES ONTHE SAME DOS. 323 97IN-HOME SCL SERVICES NOT ALLOWEDWITH RESIDENTIAL COMPONENT SERVICESON THE SAME DOS. 324 97IN-PATIENT RECIPIENTS ARE LIMITED TOONE ATTENDANCE AND ONECONSULTATION PER ADMISSION. 628, 647 97Benefit maximum for this timeperiod has been reached.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.M139N20N20MA133Denied services exceed the coveragelimit for the demonstration.Service not payable with otherservice rendered on the same date.Service not payable with otherservice rendered on the same date.Claim overlaps inpatient stay. Rebillonly those services rendered outsidethe inpatient stay.526527528529IN-PATIENT RECIPIENTS WHO HAVE HADORAL SURGERY ARE LIMITED TO 1ATTENDANCE AND/OR 1 CONSULTATIONPER DATE OF SERVICE PER PROVIDER. 526 97ADDITIONAL SERVICES TO THE SAMETOOTH ARE DISALLOWED IF THE TOOTHPayment is included in theallowance for anotherservice/procedure.M139MA133HAS BEEN PREVIOUSLY EXTRACTED. 400 18 Duplicate claim/service. M139ADDITIONAL SERVICES TO THE SAMETOOTH ARE DISALLOWED ON THE SAMEPayment is included in theDOS AS A CROWN PROCEDURE OR Aallowance for anotherFRACTURED INCISAL BUILD-UP. 402 97 service/procedure.N20CROWN AND BUILD UP PROCEDURES AREDISALLOWED IF ADDITIONAL DENTALSERVICES HAVE BEEN PAID FOR THE SAMETOOTH SAME DOS. 326 97Payment is included in theallowance for anotherservice/procedure.M86Denied services exceed the coveragelimit for the demonstration.Claim overlaps inpatient stay. Rebillonly those services rendered outsidethe inpatient stay.Denied services exceed the coveragelimit for the demonstration.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.530531532533534535536CLAIM PAID. CLAIM HAS BEEN REDUCED BYTHE AMOUNT OF THE DISPENSING FEE. 481, 520, 521, 522 91 Dispensing fee adjustment. N14PURCHASE UNITS BILLED EXCEEDSMAXIMUM ALLOWED FOR THIS PRIORPayment denied/reduced forAUTHORIZATION CHECK YOUR MAP-9absence of, or exceeded, precertification/authorization.FORM. 531 62M139RENTAL UNITS/CHARGES BILLED EXCEEDSMAXIMUM ALLOWED FOR THIS PRIORAUTHORIZATION CHECK YOUR MAP-9FORM. 532 62CLAIM DENIED. PRIOR AUTHORIZATION NOTON FILE OR DOES NOT MATCH CLAIMINFORMATION. 533 62CLAIM DENIED. PROCEDURE CODE X0064CANNOT BE BILLED IN CONJUNCTION WITHOTHER PROCEDURE CODES. 534 97PLEASE BILL BABY'S HOSPITAL STAY AFTERMOTHER'S DISCHARGE ON SEPARATECLAIM FORM, USING BABY'S OWN NAMEPayment denied/reduced forabsence of, or exceeded, precertification/authorization.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Payment is included in theallowance for anotherservice/procedure.M139N54N56Payment based on a contractualamount or agreement, fee schedule,or maximum allowable amountDenied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Claim information is inconsistent withpre-certified/authorized services.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.AND NUMBER. 535 A1 Claim denied charges. N61 Rebill services on separate claims.THE MEDICARE EOMB INDICATES THIS IS ADUPLICATE BILLING. PLEASE SUBMIT THEORIGINAL EOMB INDICATING THEDEDUCTIBLE AND CO-INSURANCEMissing/in<strong>com</strong>plete/invalid priorAMOUNTS. 536 18 Duplicate claim/service. N4 insurance carrier <strong>EOB</strong>.Page 27 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>537539540MMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESMEDICAID DESCRIPTIONCLAIM/DETAIL DENIED. THIS PROCEDURESHALL NOT BE PAID SEPARATELY WHENTHE GLOBAL SERVICE HAS BEENREPORTED. CONTACT THE DEPT. FORMEDICAID SERVICES FOR CLARIFICATION. 537 97CLAIM/DETAIL DENIED. EPSDT RELATEDSERVICES CLAIM EXCEEDS TOTAL UNITS OFSERVICE PRIOR AUTHORIZED. 539 62HOME HEALTH NURSING VISITS NOTREIMBURSED WHEN PRIVATE DUTYNURSING HAS BEEN AUTHORIZEDTHROUGH EPSDT SPECIAL SERVICES. 540 119HIPAA ADJ RSN CODEDESCRIPTIONPayment is included in theallowance for anotherservice/procedure.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Benefit maximum for this timeperiod has been reached.HIPAAREMARKM15N19M139HIPAA REMARK CODEDESCRIPTIONSeparately billed services/tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Procedure code incidental to primaryprocedure.Denied services exceed the coveragelimit for the demonstration.541CAST APPLICATION OR REMOVAL HAS BEENPAID SEPARATE OF SURGERY. PLEASERESUBMIT FOR ADJUSTMENT WITH PAID RAOF CAST APPLICATION OR REMOVAL ANDCORRECTED CLAIM WITH SURGERY CODE. 341, 541 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.M58Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.542DETAIL DENIED. IMPLANTABLES ARELIMITED TO TWO UNITS OF SERVICE PERPROCEDURE, PER RECIPIENT, PER 90 DAYS. 542 119Benefit maximum for this timeperiod has been reached.M139Denied services exceed the coveragelimit for the demonstration.543545546548MULTIPLE SURGERIES FOR SAME DATE OFSERVICE MUST BE BILLED ON SAME CLAIM.YOUR CLAIM IS DENIED AND INSTRUCTIONSFOR SUBMITTING AN ADJUSTMENT AREBEING FORWARDED TO YOU. 501, 543 107MULTIPLE MEDICAL /SURGICALPROCEDURES FOR THE SAME DATE OFSERVICE MUST BE BILLED ON SAME CLAIM.FILE AN ADJUSTMENT TO ADD ADDITIONALPROCEDURES TO RELATED PAID CLAIM. 501 107CLAIM/DETAIL DENIED. PRESCRIPTIONNUMBER REFILL DATE IS GREATER THANSIX (6) MONTHS OLD. 500 29CLAIM/DETAIL DENIED. REVENUE CODE 235MUST BE BILLED IN CONJUNCTION WITHREVENUE CODE 155, 183, AND/OR 185. 548 107Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim. M79 Missing/in<strong>com</strong>plete/invalid charge.Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim. M79 Missing/in<strong>com</strong>plete/invalid charge.The time limit for filing hasexpired.Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.MA06M50Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong>/or ending date(s).Missing/in<strong>com</strong>plete/invalid revenuecode(s).547549550551552CLAIM PAYMENT REDUCED. SPEND DOWNDEDUCTED. N/A 142CLAIM/DETAIL DENIED. THIS PROCEDURESHALL NOT BE PAID SEPARATELY WHENTHE GLOBAL SERVICE HAS BEENREPORTED. CONTACT THE DEPT. FORMEDICAID SERVICES FOR CLARIFICATION. 549 97Claim adjusted by the monthlyMedicaid patient liability amount.Payment is included in theallowance for anotherservice/procedure.N19PROCEDURE CODE 00140 CAN ONLY BEBILLED ALONE OR WITH MONITOREDPROCEDURE CODES FOR THE SAMERECIPIENT, SAME PROVIDER, AND SAMEDATE OF SERVICE. 550 A1 Claim denied charges. M15DISPENSING FEE DEDUCTED. IT WAS PAIDWITH DISPENSING OF THE EMERGENCYSUPPLY 551 97THE STAY DAYS BILLED EXCEEDS THEMAXIMUM NUMBER OF STAY DAYS FOR THISINPATIENT HOSPITAL STAY. 552 119Payment is included in theallowance for anotherservice/procedure.Benefit maximum for this timeperiod has been reached.M15MA32M53Separately billed services/ tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Procedure code incidental to primaryprocedure.Separately billed services/ tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Missing/in<strong>com</strong>plete/invalid number ofcovered days during the billingperiod.Missing/in<strong>com</strong>plete/invalid days orunits of service.553CLAIM DENIED. DRUG REQUIRES PRIORAUTHORIZATION OR FIRST LINE THERAPYINITIATED. 553 62Payment denied/reduced forabsence of, or exceeded, precertification/authorization.MA31N54Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong> ending dates of the period billed.Claim information is inconsistent withpre-certified/authorized services.554THE DATE OF SERVICE AND/OR DOLLARAMOUNTS ON THE CLAIM AND MEDICAREEOMB DO NOT AGREE. PLEASE VERIFY ANDRESUBMIT. 554 57Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.N4Missing/in<strong>com</strong>plete/invalid priorinsurance carrier <strong>EOB</strong>.Page 28 of 46 Date: 3/30/2005
KY<strong>EOB</strong>555556MEDICAID DESCRIPTIONKENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESPLEASE ATTACH THE PART B MEDICAREEXPLANATION OF BENEFITS AND REBILL. 555 129CLAIM/DETAIL DENIED. RECIPIENT MUST BEAN INPATIENT IN THE NURSING FACILITY. 556 60HIPAA ADJ RSN CODEDESCRIPTIONPayment denied - Prior processinginformation appears incorrect.Charges for outpatient serviceswith this proximity to inpatientservices are not coveredHIPAA HIPAA REMARK CODEREMARKDESCRIPTIONMissing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim afterM58 corrections.M2Not paid separately when patient isan inpatient557CLAIM DENIED. SECOND LINEANTIHISTAMINE NOT PAYABLE WITHIN FIVEDAYS OF A FIRST LINE ANTIHISTAMINE. 557 57558 H0039 LIMITED TO 32 UNITS PER DAY. 119Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.Benefit maximum for this timeperiod has been reached.559560567568569570571572573574575576577578579580581582CLAIM DENIED. THIS CLAIM EXCEEDS THEMONTHLY MAXIMUM UNITS FOR THIS NDC. 559 119Benefit maximum for this timeperiod has been reached.M139Payment denied/reduced forDETAIL DENIED. PRIOR AUTHORIZEDabsence of, or exceeded, precertification/authorization.AMOUNT HAS BEEN EXCEEDED. 560 62M139CLAIM DENIED. NO WAIVER LIABILITYBUCKET FOR MONTH OF SERVICE. 267 A1 Claim denied charges. N58Payment denied/reduced forDETAIL DENIED. PRIOR AUTHORIZEDabsence of, or exceeded, precertification/authorization.AMOUNT HAS BEEN EXCEEDED. 568 62M139DETAIL DENIED. PRIOR AUTHORIZEDAMOUNT HAS BEEN EXCEEDED. 569 62ANCILLARY CHARGES NOT ALLOWED WITHPATIENT REVENUE CODES 180 OR 185. 096 60CLAIM DETAIL DENIED. PROCEDURE CODESX0100, X0101, AND X0102 CANNOT BEBILLED ON THE SAME DATE OF SERVICEFOR THE SAME RECIPIENT BY THE SAME ORDIFFERENT PROVIDER. 577 97Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.DETAIL DENIED. PRIOR AUTHORIZEDAMOUNT HAS BEEN EXCEEDED. 570 62M139PRIOR AUTHORIZATION REQUIRED IF 30DAYS OF THERAPY EXCEEDED DURING ABenefit maximum for this time365 DAY PERIOD. 571 119 period has been reached.DETAIL DENIED. LEAD INVESTIGATION INTHE HOME LIMITED TO TWO (2) SERVICESBenefit maximum for this timePER SIX MONTHS. 572 119 period has been reached.M139DETAIL DENIED. POST HAZARD ABATE INHOME LIMITED TO ONE (1) SERVICE PER 12Benefit maximum for this timeMONTHS. 573 119 period has been reached.M90Payment denied/reduced forCLAIM DENIED. PRIOR AUTHORIZEDabsence of, or exceeded, precertification/authorization.AMOUNT HAS BEEN EXCEEDED. 574 62M139REVENUE CODE INVALID FOR DATES OFSERVICE. 095 A1 Claim denied charges. M50Charges for outpatient serviceswith this proximity to inpatientservices are not covered.M50PRIOR AUTHORIZATION REQUIRED IF 60DAYS OF THERAPY EXCEEDED DURING A 3YEAR PERIOD. 578 11962CLAIM/DETAIL DENIED. REVENUE CODE 581LIMITED TO 80 UNITS PER RECIPIENT PERCALENDAR WEEK (SUNDAY THROUGHSATURDAY). 579 119CLAIM/DETAIL DENIED. THE ANNUALLIMITATION OF $1000.00 PER RECIPIENTFOR MINOR HOME ADAPTATIONS HAS BEENEXCEEDED. 180, 580 45CLAIM/DETAIL DENIED. UNIVERSALPREVENTION PROCEDURE CODES ARELIMITED TO A COMBINED TOTAL OF EIGHTUNITS PER RECIPIENT, PER PREGNANCY. 581 119CLAIM/DETAIL DENIED. SELECTIVEPREVENTION PROCEDURE CODES ARELIMITED TO A COMBINED TOTAL OF 76UNITS PER RECIPIENT, PER PREGNANCY. 582 119Payment is included in theallowance for anotherservice/procedure.Benefit maximum for this timeperiod has been reached.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Benefit maximum for this timeperiod has been reached.Charges exceed your contracted/legislated fee arrangement.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139N20M86M139M139M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Missing/in<strong>com</strong>plete/invalid patientliability amount.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Not covered more than once in a 12month period.Denied services exceed the coveragelimit for the demonstration.Missing/in<strong>com</strong>plete/invalid revenuecode(s).Missing/in<strong>com</strong>plete/invalid revenuecode(s).Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Page 29 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>583584585586587588HIPAAADJ RSNCODESMMIS EXCEPTIONMEDICAID DESCRIPTIONCODE(S)CLAIM/DETAIL DENIED. INDICATEDPREVENTION PROCEDURE CODES ARELIMITED TO A COMBINED TOTAL OF 108UNITS PER RECIPIENT, PER PREGNANCY. 583 119CLAIM/DETAIL DENIED. CERTAINOUTPATIENT SERVICES PROCEDURECODES ARE LIMITED TO A COMBINED TOTALOF 32 UNITS PER RECIPIENT, PERCALENDAR WEEK (SUNDAY THRUSATURDAY). 584 119CLAIM/DETAIL DENIED. INTENSIVEOUTPATIENT NON-RESIDENTIAL SERVICESPROCEDURE CODES ARE LIMITED TO ACOMBINED TOTAL OF 28 UNITS PERRECIPIENT, PER DAY. 585 119CLAIM/DETAIL DENIED. INTENSIVEOUTPATIENT NON-RESIDENTIAL SERVICESPROCEDURE CODES ARE LIMITED TO ACOMBINED TOTAL OF 80 UNITS PERRECIPIENT, PER CALENDAR WEEK (SUNDAYTHRU SATURDAY). 586 119CLAIM/DETAIL DENIED. DAY REHABILITATIONPROCEDURE CODES ARE LIMITED TO ACOMBINED TOTAL OF 8 UNITS PERRECIPIENT, PER DAY. 587 119CLAIM/DETAIL DENIED. DAY REHABILITATIONPROCEDURE CODES ARE LIMITED TO ACOMBINED TOTAL OF 45 UNITS PERRECIPIENT, PER CALENDAR WEEK (SUNDAYTHRU SATURDAY). 588 119HIPAA ADJ RSN CODEDESCRIPTIONBenefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.HIPAAREMARKM139M139M139M139M139M139HIPAA REMARK CODEDESCRIPTIONDenied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.589590591592CLAIM/DETAIL DENIED. PROCEDURE CODEWB233 NOT PAYABLE UNLESS BILLED INCONJUNCTION WITH WB232 (DATES OFSERVICE WITHIN 30 DAYS OF EACH OTHER). 589 107HOSPITAL OUTPATIENT SERVICES NON-PAYABLE DURING A HOSPITAL INPATIENTSTAY. 590 60CLAIM/DETAIL DENIED. OUTPATIENTTHERAPIES INDIVIDUAL, GROUP, ANDFAMILY PROCEDURE CODES ARE NOTPAYABLE ON THE SAME DATE OF SERVICEAS INTENSIVE OUTPATIENT SERVICES NON-RESIDENTIAL AND DAY REHABILITATIONPROCEDURES. 591 97CLAIM/DETAIL DENIED. INTENSIVEOUTPATIENT SERVICES NON-RESIDENTIALAND DAY REHABILITATION PROCEDURECODES ARE NOT PAYABLE ON THE SAMEDATE OF SERVICE AS OUTPATIENTTHERAPIES INDIVIDUAL, GROUP, & FAMILYPROCEDURES. 592 97Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.Charges for outpatient serviceswith this proximity to inpatientservices are not covered.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.N56N20M86N20M86Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.593CLAIM DENIED. THIS PROCEDURE IS NOTPAYABLE UNLESS BILLED IN CONJUNCTIONWITH WB505, WB507, WB508, WB509,WB516, WB521, WB522, WB523, WB526,WB602, WB603 OR WB604 (DATES OFSERVICE WITHIN 30 DAYS OF EACH OTHER). 593 107Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.N56Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.594596597CLAIM DENIED. CLAIM EXCEEDS 140 DAYACID/PEPTIC THERAPY LIMITATION. 594 119CLAIM DETAIL DENIED. OFFICE VISITS NOTALLOWED WITHIN 10 DAYS FOLLOWING ASURGICAL PROCEDURE. 596 97CLAIM/DETAIL DENIED. THIS PROCEDURE ISNOT PAYABLE AFTER THE DATE OFDELIVERY. 597 97Benefit maximum for this timeperiod has been reached.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.M139N19M67Denied services exceed the coveragelimit for the demonstration.Procedure code incidental to primaryprocedure.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).598CLAIM DETAIL DENIED. ONLY ONE 'E AND M'CODE ALLOWED PER DATE OF SERVICE. 598 119599 CLAIM PENDING REVIEW OF HISTORY. 599 133Benefit maximum for this timeperiod has been reached.The disposition of thisclaim/service is pending furtherreview.M63We do not pay for more than one ofthese on the same day.Page 30 of 46 Date: 3/30/2005
KY<strong>EOB</strong>MEDICAID DESCRIPTIONKENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODES600 EYE EXAM LIMITED TO OPTOMETRIST. 600 B58HIPAA ADJ RSN CODEDESCRIPTIONPayment adjusted becausecoverage/ program guidelineswere not met or were exceeded.The procedure code isinconsistent with the providertype/specialty (taxonomy).HIPAAREMARKHIPAA REMARK CODEDESCRIPTION601602ONLY 3 FOLLOW UP EXAMS ARE ALLOWEDPER 6 MONTHS. 601 119CLAIM DENIED. LIMIT 2 ROUTINEORTHODONTICS PER RECIPIENT PER 12MONTHS 602 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.603604CLAIM DENIED. EACH RECIPIENT ALLOWEDONE FULL MOUTH RADIOGRAPHY EVERY 2YEARS PER PROVIDER. 603 119Benefit maximum for this timeperiod has been reached.M139MORE THAN 2 OF THE COMPONENT TESTSOF A CBC PERFORMED ON THE SAME DOSMUST BE BILLED AS A CBC. 604 A1 Claim denied charges. N19Denied services exceed the coveragelimit for the demonstration.Procedure code incidental to primaryprocedure.605ONLY FOUR PSYCHIATRIC PROCEDURESALLOWED PER YEAR, PER PROVIDER, PERRECIPIENT. 605 119Benefit maximum for this timeperiod has been reached.M15M139Separately billed services/tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowedDenied services exceed the coveragelimit for the demonstration.606607608609610PROCEDURE CODE 02951 CAN ONLY BEBILLED ALONE OR WITH MONITOREDPROCEDURE CODES FOR THE SAMERECIPIENT, SAME PROVIDER, SAME DATEOF SERVICE, AND SAME TOOTH NUMBER. 606 107EACH RECIPIENT ALLOWED 4 SINGLEBITEWING X-RAYS PER 12 MONTHS PERPROVIDER. 607 119CLAIM DENIED. THIS SERVICE IS LIMITED TOONE PER RECIPIENT, PER PROVIDER, PERCALENDAR MONTH. 639, 651 119CLAIM DENIED. ONE DENTALPROPHYLAXIS/FLUORIDE TREATMENT PERRECIPIENT PER 12 MONTH PERIOD. 609 119CLAIM DENIED. EACH RECIPIENT ALLOWEDONE UPPER TRANSITIONAL APPLIANCE PER12 MONTHS. 610 119Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.N56M139M139M90M90Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Not covered more than once in a 12month period.Not covered more than once in a 12month period.611612613614615616617RECIPIENT ALLOWED THREE TRANSITIONALAPPLIANCE REPAIRS PER 12 MONTHS. 611 119ONLY 9 UNITS (ADULT DAY HABILITATION)ALLOWED PER DATE OF SERVICE PERRECIPIENT. 612 119RESIDENTIAL RESPITE DAILY SERVICEALLOWED FOR ONLY 30 CONSECUTIVEDAYS. 613 119RECIPIENT ALLOWED ONLY 30CONSECUTIVE DAY OF IN-HOME RESPITEDAILY SERVICE. 614 119MAXIMUM OF 40 DAYS RESIDENTIALRESPITE COMBINING DAILY AND HOURLYSERVICES PER RECIPIENT PER CALENDARYEAR. 615 119MAXIMUM OF 60 DAYS IN-HOME RESPITEALLOWED COMBINING DAILY AND HOURLYSERVICES PER RECIPIENT PER CALENDARYEAR. 616 119RECIPIENT ALLOWED 1 INITIAL OFFICE VISITWITH COMPLETE DIAGNOSIS PER 9MONTHS. 617 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139M139M139M139M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.618ONLY ONE DELIVERY ALLOWED PERRECIPIENT/9 MOS. 618 119Benefit maximum for this timeperiod has been reached.M139Denied services exceed the coveragelimit for the demonstration.619620RECIPIENT ALLOWED POST-PARTUM CARE2 TIMES PER YEAR. 619 119MAXIMUM DAILY DOSE EXCEEDED - PRIORAUTHORIZATION REQUIRED. 620, 632 11962Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.M139Denied services exceed the coveragelimit for the demonstration.Page 31 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION621DETAIL DENIED. MAXIMUM DOLLAR AMOUNTFOR COMMUNITY BASED SERVICESRESPITE SERVICE HAS BEEN EXCEEDED. 621, 691, 692 45Charges exceed your contracted/legislated fee arrangement.M139Denied services exceed the coveragelimit for the demonstration.622623DETAIL DENIED. ANNUAL LIMIT OF $500.00FOR MINOR HOME ADAPTATIONS. 622 45RECIPIENT ALLOWED 14 SINGLE INTRAORALPERIAPICAL RADIOGRAPHS PER 12 MOSPER PROVIDER. 623 119Charges exceed your contracted/legislated fee arrangement.Benefit maximum for this timeperiod has been reached.M139Denied services exceed the coveragelimit for the demonstration.624625CLAIM DENIED. THIS PROCEDURE ALLOWEDONE PER DOS PER TOOTH PER PROVIDER. 624 119CLAIM DENIED/RECIPIENT ALLOWED 3REPAIRS INCLUDING REPLACEMENTS OFONE TOOTH PER 12 MONTHS. 625, 627 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.626627CLAIM DENIED. ONLY 14 DAYS SERVICEALLOWED PER ADMISSION PER RECIPIENT. 626 119CLAIM DENIED. RECIPIENT ALLOWED 3REPAIRS TO BROKEN DENTURES PER 12MONTHS. 626 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.629631633RECIPIENT ALLOWED 1 LOWERTRANSITIONAL APPLIANCE PER 12 MONTHS. 629 119RECIPIENTS ARE LIMITED TO ONE DENTURERELINING PER 12 MONTHS. 631 119CLAIM DENIED. BRAND NECESSARY PRIORAUTHORIZATION REQUIRED. NO MATCHINGBRAND NECESSARY PRIOR AUTHORIZATIONON FILE FOR THIS CLAIM. 633 62Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.M90M90Not covered more than once in a 12month period.Not covered more than once in a 12month period.634635636637638640641MAXIMUM $300.00 ALLOWED PERMONTH/RECIPIENT FOR TANK OXYGEN. 634 45AIS/MR DAILY CODE LIMITED TO ONE UNITPER DATE OF SERVICE PER RECIPIENT. 635 119PROFESSIONAL FEE FOR DISPENSINGINITIAL PAIR OF EYEGLASSES ALLOW ONE /12 MOS / RECIPIENT. 636 119CLAIM DENIED. RECIPIENT LIMITED TO 3FETAL TESTS/12 MONTHS. IF UNUSUALCIRCUMSTANCES, SEND CLAIMDOCUMENTATION TO DMS FOR REVIEW. 637 119ANNUAL FAMILY PLANNING VISITS ARELIMITED TO ONE PER RECIPIENT PER 9MONTHS PER CLINIC. 638 119Charges exceed your contracted/legislated fee arrangement.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.THIS DETAIL WAS MANUALLY PRICED AFTERREVIEW BY CONSULTANTS. 355 A2 Contractual adjustment. N10Payment denied/reduced forPRIOR AUTHORIZATION DOES NOT MATCHabsence of, or exceeded, precertification/authorization.FOR THIS CLAIM/DETAIL. 641 62N54M139M63M90N29M139Denied services exceed the coveragelimit for the demonstration.We do not pay for more than one ofthese on the same day.Not covered more than once in a 12month period.Missingdocumentation/orders/notes/summary/report/invoice.Denied services exceed the coveragelimit for the demonstration.Claim/service adjusted based on thefindings of a revieworganization/professionalconsult/manual adjudication /medicalor dental advisor.Claim information is inconsistent withpre-certified/authorized services.642644645THIS PROCEDURE IS LIMITED TO ONE PER12 MONTHS PER RECIPIENT PER PROVIDER. 642, 643, 663 119RECIPIENTS ARE LIMITED TO ONE (1)OPTHAMOLOGICAL EXAMINATION PERPROVIDER PER 12 MONTHS. 644, 664 119NEW PATIENT HOME MEDICAL SERVICESLIMITED TO ONE PER RECIPIENT PERPROVIDER PER 12 MONTHS. 645, 665 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M90M90M90Not covered more than once in a 12month period.Not covered more than once in a 12month period.Not covered more than once in a 12month period.646648649ESTABLISHED PATIENT MEDICAL SERVICESLIMITED TO ONE PER RECIPIENT PERPROVIDER PER 12 MONTHS. 646, 666 119RECIP ARE LMTD ON INITIAL PREVENTATIVECARE VISITS TO 1 PER PROV PER 12MONTHS. 648 119RECIP LMTD 1 INITIAL OPTHALMOLOGICALSERVICE PER PROV PER 12 MONTHS. 649, 669 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M90M90M90Not covered more than once in a 12month period.Not covered more than once in a 12month period.Not covered more than once in a 12month period.650652ROUTINE NEWBORN CARE IS PAYABLEONLY ONCE PER INFANT. 650 119CLAIM DENIED. BIFOCAL OR SINGLE VISIONLENSES ARE LIMITED TO FOUR PER 12MONTHS. 652 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Page 32 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION653654655656657658659660CLAIM/DETAIL DENIED. A PRESCRIPTIONCAN ONLY BE BILLED 6 TIMES. 653 119RECIPIENT ALLOWED FILLINGS FOR UP TOFIVE SURFACES PER TOOTH PER DOS PERPROVIDER. 654 119MAXIMUM OF 14 CONSECUTIVE HOSPITALRESERVE DAYS ALLOWED PER RECIPIENTPER PROVIDER. 655 119MAXIMUM OF 15 NON-HOSPITAL RESERVEDAYS ALLOWED PER RECIPIENT PERCALENDAR YEAR. 656 119MAXIMUM OF 45 HOSPITAL RESERVE DAYSALLOWED PER RECIPIENT PER CALENDARYEAR. 657 119MAXIMUM OF 15 CONSECUTIVE HOSPITALRESERVE DAYS ALLOWED PER RECIPIENTPER PROVIDER. 658 119MAXIMUM OF 30 CONSECUTIVE RESERVEDAYS ALLOWED PER RECIPIENT PERPROVIDER. 659 119MAXIMUM OF 45 RESERVE DAYS PERRECIPIENT PER PROVIDER PER CALENDARYEAR. 660 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Benefit maximum for this timeperiod has been reached. N43 Bed hold or leave days exceeded.Benefit maximum for this timeperiod has been reached. N43 Bed hold or leave days exceeded.Benefit maximum for this timeperiod has been reached. N43 Bed hold or leave days exceeded.Benefit maximum for this timeperiod has been reached. N43 Bed hold or leave days exceeded.Benefit maximum for this timeperiod has been reached. N43 Bed hold or leave days exceeded.Benefit maximum for this timeperiod has been reached. N43 Bed hold or leave days exceeded.661CLAIM DENIED. READMISSION WITHIN 30DAYS OF LAST DISCHARGE DATE/THROUGHDATE. PLEASE RESUBMIT WITH MEDICALDOCUMENTATION. 670 119Benefit maximum for this timeperiod has been reached.N29Missingdocumentation/orders/notes/summary/report/invoice.66266566666716A MAXIMUM OF 14 INPATIENT HOSPITALDAYS PER ADMISSION AND READMISSIONPER RECIPIENT. 662 119VENIPUNCTURE/ CATHETERIZATIONPROCEDURES 80020, 80022, 80023, 80024,36415 NOT ALLOWED SAME DOS/CLAIM/DETAIL DENIED. PROVIDER NOT CLIACERTIFIED TO BILL NON-WAVERED OR NON-MICROSCOPY LAB CODE. 512 B7THIS PROCEDURE IS LIMITED TO ONESERVICE PER RECIPIENT PER SAME DATEOF SERVICE. 661, 662, 667 119Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.Benefit maximum for this timeperiod has been reached.RECIPIENT/PROVIDER. 635 96 Non-covered charge(s). N20This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.MA51Benefit maximum for this timeperiod has been reached.M139M63Denied services exceed the coveragelimit for the demonstration.Service not payable with otherservice rendered on the same date.Missing/in<strong>com</strong>plete/invalid CLIAcertification number for laboratoryservices billed by physician officelaboratory.We do not pay for more than one ofthese on the same day.668PROCEDURE CODE XR000 IS LIMITED TO NOMORE THAN 2 UNITS OF SERVICE PER DATEOF SERVICE. 668 57119Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this days supply.Benefit maximum for this timeperiod has been reached.M139Denied services exceed the coveragelimit for the demonstration.669670DAYS REDUCED, A MAXIMUM OF 14CONSECUTIVE HOSPITAL RESERVE DAYSALLOWED PER RECIPIENT,PER PROVIDER. 669 119DAYS REDUCED, A MAXIMUM OF 15 NON-HOSPITAL RESERVE DAYS ALLOWED PERRECIPIENT,PER PROVIDER,PER CALENDARYEAR. 670 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139N43M139N43Denied services exceed the coveragelimit for the demonstration.Bed hold or leave days exceeded.Denied services exceed the coveragelimit for the demonstration.Bed hold or leave days exceeded.671MEDICAID WILL PAY FOR ONLY ONECARDIAC CATHETER PROCEDURE PER DAY. 671 119Benefit maximum for this timeperiod has been reached.673 CPT LEVEL CODE MISSING OR INVALID. 673 A1 Claim denied charges.674PROCEDURE CODE V5020 IS LIMITED TOTHREE PER RECIPIENT PER PROVIDER PERSIX MONTHS. 674 119Benefit maximum for this timeperiod has been reached.675DAYS REDUCED, A MAXIMUM OF 45 TOTALDAYS PER RECIPIENT, PER PROVIDER, PERCALENDAR QUARTER. 675 119Benefit maximum for this timeperiod has been reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Page 33 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>676MMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESMEDICAID DESCRIPTIONPROCEDURE W0030 CAN ONLY BEPERFORMED 150 TO 210 DAYS 5 TO 7MONTHS AFTER PERFORMING PROCEDUREV5090. 676 119HIPAA ADJ RSN CODEDESCRIPTIONBenefit maximum for this timeperiod has been reached.HIPAAREMARKM139HIPAA REMARK CODEDESCRIPTIONDenied services exceed the coveragelimit for the demonstration.57Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.677678679PROCEDURE CODE LIMITED TO ONE PER 60DAYS. 677 119RECIPIENTS ARE LIMITED TO A MAXIMUM OF10 MONTHLY STABILIZATION VISITS DURINGPHASE I TREATMENT CONTACT DMS FORFURTHER CONSIDERATION. 678 119CLAIM/DETAIL DENIED. ONLY ONE HANDSPROCEDURE CODE ALLOWED PERRECIPIENT PER DATE OF SERVICE. 679 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.680FAMILY AND/OR GROUP PSYCHOTHERAPYLMTD TO ONE PER DATE OF SERVICE. 680 119Benefit maximum for this timeperiod has been reached.M139Denied services exceed the coveragelimit for the demonstration.681682EVEN WITH DOCUMENTATION OF PATIENT'SCONDITION NECESSITATING ADMISSION TOA LESSER FACILITY, REIMBURSEMENT FORBOTH FACILITIES CANNOT EXCEED AMAXIMUM OF 14 DAYS. 670 119CLAIM DENIED. REIMBURSEMENT CANNOTEXCEED A MAXIMUM OF 14 DAYS PERADMISSION. 670 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.683684685686687MODEL WAIVER RECIPIENTS ARE LIMITEDTO 16 HOURS OF NURSING/ RESPIRATORYSERVICES PER DATE OF SERVICE. 683 119MODEL WAIVER RESPIRATORY SERVICESARE LIMITED TO ONE UNIT PER RECIPIENTPER DATE OF SERVICE. 684 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M63CLAIM/DETAIL DENIED. A HOSPICE SERVICEHAS BEEN PAID FOR SAME RECIPIENT/SAMEDATE(S) OF SERVICE. 685 A1 Claim denied charges. M86CLAIM/DETAIL DENIED. HOSPICE RESPITESERVICES ARE LIMITED TO FIVECONSECUTIVE DAYS PER RECIPIENT. 686 119UNITS BILLED EXCEED MAXIMUM FOR THISPRIOR AUTHORIZATION. 688 62Benefit maximum for this timeperiod has been reached.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.M139N20M139M53Denied services exceed the coveragelimit for the demonstration.We do not pay for more than one ofthese on the same day.Service denied because paymentalready made for similar procedurewithin set time frame.Service not payable with otherservice rendered on the same date.Denied services exceed the coveragelimit for the demonstration.Missing/in<strong>com</strong>plete/invalid days orunits of service.688689MODEL WAIVER DOLLAR LIMIT HAS BEENMET. 688 35RECIPIENTS ARE LIMITED TO A MAXIMUM OF365 ORAL CONTRACEPTIVE UNITS PER 12MONTH PERIOD. 689 119Lifetime benefit maximum hasbeen reached.Benefit maximum for this timeperiod has been reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.690691692693694695696CLAIM DENIED. TARGETED CASEMANAGEMENT SERVICES ARE LIMITED TO 1PER CALENDAR MONTH, PER RECIPIENT. 690 119CLAIM/DETAIL DENIED. CLIA ID MISSING ORINVALID. 510 B7CLAIM/DETAIL DENIED. PROVIDER NOT CLIACERTIFIED TO BILL NON-WAVERED LABCODE. 511 B7COMPREHENSIVE ORTHODONTIC EXAMLIMITED TO ONE PER RECIPIENT PER 12MONTHS. 693 119COMPREHENSIVE ORTHODONTIC EXAMLIMITED TO TWO (2) PER RECIPIENT PERLIFETIME. 694 119RECIPIENTS ARE LIMITED TO A MAXIMUM OF24 MONTHLY RETENTION VISITS PERLIFETIME. 695 35Benefit maximum for this timeperiod has been reached.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Lifetime benefit maximum hasbeen reached.M139PROFESSIONAL COMPONENT CHARGESMUST BE BILLED ON HCFA-1500. 696 A1 Claim denied charges. N200M139MA51M90M139Denied services exceed the coveragelimit for the demonstration.Missing/in<strong>com</strong>plete/invalid CLIAcertification number for laboratoryservices billed by physician officelaboratory.Not covered more than once in a 12month period.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.The professional <strong>com</strong>ponent must bebilled separately.Page 34 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION697698700RECIPIENTS ARE LIMITED TO ONERETENTION VISIT PER 30 DAYS. 697 119RECIPIENTS ARE LIMITED TO A MAXIMUM OF10 POST TREATMENT STABILIZATION VISITSPER LIFETIME. 698 35CLINIC PROVIDER IS INELIGIBLE FOR THISCATEGORY OF SERVICE. 700 52Benefit maximum for this timeperiod has been reached.Lifetime benefit maximum hasbeen reached.The referring/prescribing/rendering provider is not eligibleto refer/prescribe/ order/performthe service billed.M139M139N55Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Procedures for billing withgroup/referring/performing providerswere not followed.701702703CLAIM DENIED. BED RESERVE REVENUECODES FOR MENTAL HOSPITAL AND ACUTEPSYCHIATRIC BED ARE LIMITED TO ACOMBINATION OF 14 UNITS PER CALENDARYEAR PER RECIPIENT, PER PROVIDER. 701 119CLAIM DENIED. BED RESERVE/OTHERREVENUE CODE IS LIMITED TO A TOTAL OF21 UNITS PER CALENDAR 6 MONTHS PERRECIPIENT, PER PROVIDER. 702 119CLAIM DENIED. BED RESERVE/ACUTEREVENUE CODE IS LIMITED TO A TOTAL OF14 UNITS PER CALENDAR YEAR, PERRECIPIENT, PER PROVIDER. 703 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139N43M139N43M139N43Denied services exceed the coveragelimit for the demonstration.Bed hold or leave days exceeded.Denied services exceed the coveragelimit for the demonstration.Bed hold or leave days exceeded.Denied services exceed the coveragelimit for the demonstration.Bed hold or leave days exceeded.704705706CLAIM DENIED. PSYCHIATRIC RESIDENTIALTREATMENT FACILITY CLAIMS ARE LIMITEDTO 30 CONSECUTIVE BED RESERVE DAYSPER RECIPIENT, PER PROVIDER. 704 119NEW PATIENT OPHTHALMOLOGICALSERVICES LIMITED TO ONE PER RECIPIENT,PER PROVIDER, PER 36 MONTHS/THREEYEARS. 705 119NEW PATIENT OFFICE OR OUTPATIENTSERVICES LIMITED TO ONE PER RECIPIENT,PER PROVIDER, PER 36 MONTHS/THREEYEARS. 706 119Benefit maximum for this timeperiod has been reached. N43 Bed hold or leave days exceeded.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.707NEW PATIENT HOME MEDICAL SERVICESLIMITED TO ONE PER RECIPIENT, PERPROVIDER, PER 36 MONTHS/THREE YEARS. 707 119Benefit maximum for this timeperiod has been reached.M139Denied services exceed the coveragelimit for the demonstration.708709NEW PATIENT PREVENTATIVE CARE VISITSLIMITED TO ONE PER RECIPIENT, PERPROVIDER, PER 36 MONTHS/THREE YEARS. 708 119CLAIM/DETAIL DENIED. PROCEDURE CODE70320 LIMITED TO ONE PER YEAR, PERRECIPIENT, PER PROVIDER. 709 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M90Denied services exceed the coveragelimit for the demonstration.Not covered more than once in a 12month period.710711CLAIM/DETAIL DENIED. ONLY ONE (1)CHEMOTHERAPY ADMIN CODE IS PAYABLEON THE SAME DATE OF SERVICE. IFQUESTIONS, PLEASE CONTACT THEDEPARTMENT FOR MEDICAID SERVICES. 710 119Benefit maximum for this timeperiod has been reached.M63PROVIDER NOT APPROVED FORELECTRONIC BILLING SUBMIT MAP 380PROVIDER AGREEMENT FORM. 711 A1 Claim denied charges N51We do not pay for more than one ofthese on the same day.Electronic interchange agreementnot on file for provider / submitter.713715716717718DELIVERY, ROUTINE NEWBORN CARE,CIRCUMCISION ARE LIMITED TO ONE EACHPER RECIPIENT PER DATE OF SERVICE. 712, 713, 714, 720, 721 119CLAIM DENIED. PROCEDURE CODE X0064LIMITED TO ONE UNIT OF SERVICE PERPROVIDER, PER RECIPIENT, PER TWOYEARS. 715 119CLAIM DENIED. PROCEDURE CODE X0074LIMITED TO ONE UNIT OF SERVICE PERPROVIDER, PER RECIPIENT, PER TWOYEARS. 716 119CLAIM DENIED. PROCEDURE CODE X0075LIMITED TO A TOTAL OF 76 UNITS OFSERVICE PER PROVIDER, PER RECIPIENT,PER TWO YEARS. 717 119CLAIM DENIED. PROCEDURE CODE X0076LIMITED TO ONE UNIT OF SERVICE PERPROVIDER, PER RECIPIENT, PER CALENDARMONTH. 718 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M63M139M139M139M139We do not pay for more than one ofthese on the same day.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Page 35 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION719CLAIM DENIED. A MAXIMUM OF 60 RESPITEDAYS (COMBINING DAILY AND HOURLYSERVICES) ALLOWED PER PROVIDER, PERRECIPIENT, PER CALENDAR YEAR. 719 119Benefit maximum for this timeperiod has been reached.M139Denied services exceed the coveragelimit for the demonstration.722723724CLAIM/DETAIL DENIED. BUCCAL AND FACIALTOOTH SURFACES NOR OCCLUSAL ANDINCISAL TOOTH SURFACES NOT ALLOWEDFOR SAME RECIPIENT, SAME PROVIDER,SAME DATE OF SERVICE, AND SAME TOOTHNUMBER. 722 97CLAIM/DETAIL DENIED. ONLY FOUR TOOTHSURFACES ALLOWED PER RECIPIENT, PERPROVIDER, PER DATE OF SERVICE, PERTOOTH NUMBER. 723 119CLAIM DETAIL DENIED. PROCEDURE CODEX0095 LIMITED TO $1000.00 IN PAYMENTSPER SIX MONTHS. 724 45Payment is included in theallowance for anotherservice/procedure.Benefit maximum for this timeperiod has been reached.Charges exceed your contracted/legislated fee arrangement.N20M86M139M139Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.725726727728729730PROCEDURE CODES X0050 AND X0150 ARELIMITED TO 12 UNITS OF SERVICE PER DAY,PER RECIPIENT, PER PROVIDER. 725 119CLAIM/DETAIL DENIED. CEPHALOMETRIC X-RAY LIMITED TO ONE PER RECIPIENT, PERPROVIDER, EVERY TWO YEARS. 726 119CLAIM/DETAIL DENIED. DIALYSIS TRAININGLIMITED TO ONE (1) PER RECIPIENT, PERLIFETIME. 727 35GINGIVECTOMY PROCEDURE CODE 04211 ISLIMITED TO ONE PER RECIPIENT, PERPROVIDER, PER TOOTH NUMBER PER 12MONTHS. 728 119PIN RETENTION THERAPY TREATMENTPROCEDURE CODE 02951 IS LIMITED TOTWO PER RECIPIENT PER PERMANENTMOLAR PER LIFETIME. 729 35PROCEDURE CODE 07880 LIMITED TO ONEPER LIFETIME PER RECIPIENT. 730 35Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Lifetime benefit maximum hasbeen reached.Benefit maximum for this timeperiod has been reached.Lifetime benefit maximum hasbeen reached.Lifetime benefit maximum hasbeen reached.M139M139M90M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Not covered more than once in a 12month period.Denied services exceed the coveragelimit for the demonstration.731RECIPIENTS ARE LIMITED TO ONE RELININGOF THE LOWER DENTURE PER 12 MONTHS. 631 119Benefit maximum for this timeperiod has been reached.M90Not covered more than once in a 12month period.732733734735736PROCEDURE CODES 07310 AND 07320 ARELIMITED TO ANY COMBINATION OF THESEPROCEDURES WITH ONLY ONE PERQUADRANT, PER RECIPIENT, PER LIFETIME. 732 35PROCEDURE CODE 04210 LIMITED TO FOURPER RECIPIENT, PER PROVIDER, PERTWELVE MONTHS. 733 119CLAIM/DETAIL DENIED. PROCEDURE IS NOTALLOWED TO THE SAME TOOTH ON THESAME DATE OF SERVICE AS PROCEDURECODE 01351. 734 97CLAIM/DETAIL DENIED. INSULIN SYRINGESLIMITED TO 125 UNITS PER 26 DAYS, PERRECIPIENT. 735 119CLAIM/DETAIL DENIED. VACCINEADMINISTRATION LIMITED TO (3) PERRECIPIENT, PER PROVIDER, PER DATE OFSERVICE. 736 119Lifetime benefit maximum hasbeen reached.Benefit maximum for this timeperiod has been reached.Payment is included in theallowance for anotherservice/procedure.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139N81M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Procedure billed is not <strong>com</strong>patiblewith tooth surface code.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.737738CLAIM/DETAIL DENIED. PROCEDURE CODE01351 IS LIMITED TO ONE PER TOOTH PERFOUR YEARS PER RECIPIENT. 737 119CLAIM/DETAIL DENIED. PROCEDURE CODE01351 IS LIMITED TO THREE PER TOOTHPER LIFETIME PER RECIPIENT. 738 35Benefit maximum for this timeperiod has been reached.Lifetime benefit maximum hasbeen reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.739740CLAIM/DETAIL DENIED. PROCEDURE CODE01351 IS NOT ALLOWED TO A TOOTH THATHAS RECEIVED AN OCCLUSAL FILLING. 739 97CLAIM/DETAIL DENIED. ONLY ONE UNIT OFSERVICE ALLOWED FOR THIS DENTALPROCEDURE PER PRIOR AUTHORIZATION. 740 62Payment is included in theallowance for anotherservice/procedure.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.N81M139Procedure billed is not <strong>com</strong>patiblewith tooth surface code.Denied services exceed the coveragelimit for the demonstration.Page 36 of 46 Date: 3/30/2005
KY<strong>EOB</strong>741742743744745746747748749KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESMEDICAID DESCRIPTIONCLAIM DENIED. RECIPIENT LIMITED TO 2DIAGNOSTIC ULTRASOUNDS PER 9MONTHS. MEDICAL NECESSITY MUSTSUPPORT UNUSUAL CIRCUMSTANCES.DIAGNOSIS CODE MUST INDICATE MEDICALNECESSITY. 741 50DETAIL DENIED. PROCEDURE CODE 00210LIMITED TO ONE UNIT PER RECIPIENT, PERPROVIDER, PER 12 MONTHS. 742 119PROCEDURE CODE 04211 LIMITED TO 1UNIT PER TOOTH, PER 12 MONTHS, PERRECIPIENT, PER PROVIDER. 743 119CLAIM/DETAIL DENIED. PROCEDURE CODESXH100, X0058, 99199, AND 99499 ARELIMITED TO 40 UNITS OF SERVICE PER DATEOF STATE. CHECK THE UNITS OF SERVICEBILLED FOR ERRORS. 744 119CLAIM/DETAIL DENIED. PROCEDURE CODEX0058 CANNOT BE BILLED BY A SCHOOLBASED PROVIDER AND A COMMUNITYMENTAL HEALTH PROVIDER ON THE SAMEDATE OF SERVICE. 745 B7REVENUE/PROCEDURE CODE INVALID FORPROVIDER TYPE. 146 8CLAIM DETAIL DENIED. PROCEDURE CODESX0078, X0079, AND X0098 (ANYCOMBINATION) LIMITED TO FORTY HOURSPER SEVEN DAY PERIOD. 747 119REVENUE/PROCEDURE CODE INVALID FORPLACE OF SERVICE. 148 5CLAIM DETAIL DENIED. PROCEDURE CODEX0063 LIMITED TO 168 HOURS PER SIXMONTHS. 749 119HIPAA ADJ RSN CODEDESCRIPTIONThese are non-covered servicesbecause this is not deemed a`medical necessity' by the payer.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.The procedure code isinconsistent with the providertype/specialty (taxonomy).Benefit maximum for this timeperiod has been reached.The procedure code/bill type isinconsistent with the place ofservice.Benefit maximum for this timeperiod has been reached.HIPAAREMARKM139M76M90M90M53M63MA66M139MA66M139HIPAA REMARK CODEDESCRIPTIONDenied services exceed the coveragelimit for the demonstration.Missing/in<strong>com</strong>plete/invalid diagnosisor condition.Not covered more than once in a 12month period.Not covered more than once in a 12month period.Missing/in<strong>com</strong>plete/invalid days orunits of service.We do not pay for more than one ofthese on the same day.In<strong>com</strong>plete/invalid principalprocedure code <strong>and</strong>/or date.Denied services exceed the coveragelimit for the demonstration.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Denied services exceed the coveragelimit for the demonstration.750 DRUG/DRUG INTERACTION. 750 96 Non-covered charge(s). N14Payment denied because thisprocedure code/ modifier wasREVENUE/PROCEDURE CODE INVALID FORinvalid on the date of service or751 DATE OF SERVICE. 151 B18 claim submission.M50Payment denied because thisprocedure code/ modifier wasinvalid on the date of service or752 REVENUE CODE MISSING/INVALID. 152 B18 claim submission.M50753INVALID REVENUE CODE. CHARGES NOTALLOWED. 146, 148, 151, 152, 510 B18Payment denied because thisprocedure code/ modifier wasinvalid on the date of service orclaim submission.754 EARLY REFILL. 754 N14755756757758NON-REIMBURSABLE FOR THIS PROVIDERTYPE/DOS. EFFECTIVE FOR DOS 10/01/90AND AFTER, DRUGS MUST BE BILLED BYMEDICAID PARTICIPATING PHARMACY. 755 A1 Claim denied charges. N95CLIA ID MISSING OR INVALID. CHARGESMOVED TO NON-COVERED. 756 96 Non-covered charge(s). MA120CHARGES MOVED TO NON-COVERED.RTSUP CAN ONLY BE REIMBURSED WHENCHARGES FOR RT ARE BILLED FOR THESAME DATES OF SERVICE. 757 96 Non-covered charge(s).PROVIDER NOT CLIA CERTIFIED TO BILLNON-WAIVERED LAB CODE. CHARGESMOVED TO NON-COVERED. 758 B7PROVIDER NOT CLIA CERTIFIED TO BILLNON-WAIVERED OR NON-MICROSCOPY LABCODE. CHARGES MOVED TO NON-COVERED. 759 B7This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.759760 INFERRED DRUG/DISEASE PRECAUTION. 760 96 Non-covered charge(s).761 DRUG/AGE PRECAUTION. 761 96 Non-covered charge(s).762 MEDICAL CONDITION ALERT. 762 96 Non-covered charge(s).M50MA51MA51Payment based on a contractualamount or agreement, fee schedule,or maximum allowable amountMissing/in<strong>com</strong>plete/invalid revenuecode(s).Missing/in<strong>com</strong>plete/invalid revenuecode(s).Missing/in<strong>com</strong>plete/invalid revenuecode(s).Payment based on a contractualamount or agreement, fee schedule,or maximum allowable amountThis provider type/provider specialtymay not bill this service.Missing/in<strong>com</strong>plete/invalid CLIAcertification number.Missing/in<strong>com</strong>plete/invalid CLIAcertification number for laboratoryservices billed by physician officelaboratory.Missing/in<strong>com</strong>plete/invalid CLIAcertification number for laboratoryservices billed by physician officelaboratory.Page 37 of 46 Date: 3/30/2005
KY<strong>EOB</strong>MEDICAID DESCRIPTIONKENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONCharges do not meetqualifications for emergent/urgentcare.763SERVICES RENDERED DO NOT MEET DMSCRITERIA FOR DENTAL EMERGENCY. 180 40DIAGNOSIS AND DESCRIPTION OFTREATMENT ARE REQUIRED FOR DENTAL764 EMERGENCY. 180 40765 THERAPEUTIC DUPLICATION. 765 96 Non-covered charge(s).766 ? 96 Non-covered charge(s).767 INGREDIENT DUPLICATION. 767 96 Non-covered charge(s).768 ALCOHOL PRECAUTION. 768 96 Non-covered charge(s).769 BREAST FEEDING PRECAUTION. 769 96 Non-covered charge(s).770 DRUG/FOOD INTERACTION. 770 96 Non-covered charge(s).771 DRUG/LAB CONFLICT. 771 96 Non-covered charge(s).772 CALL HELP DESK (1-800-807-1232). 772 96 Non-covered charge(s).773 INVALID DUR CONFLICT CODE. 773 96 Non-covered charge(s).774 INVALID DUR INTERVENTION CODE. 774 96 Non-covered charge(s).775 INVALID DUR OUTCOME CODE. 775 96 Non-covered charge(s).777791792793794Charges do not meetqualifications for emergent/urgentcare.HIPAAREMARKCLAIM DENIED. PHARMACY CLAIMS MUST BEBILLED THROUGH POS. 777 A1 Claim denied charges. M117CLAIM DETAIL DENIED. REVENUE CODE 580IS LIMITED TO 45 UNITS (HOURS) PER WEEKBenefit maximum for this time(SUNDAY THROUGH SATURDAY). 791 119 period has been reached.M139CLAIM DETAIL DENIED. ONLY ON<strong>EOB</strong>STETRICAL VISIT ALLOWED IN AN EIGHTWEEK PERIOD. 792 119CLAIM DETAIL DENIED. ONLY ONECOMPREHENSIVE VISIT ALLOWED EVERY 50WEEKS. 793 119CLAIM/DETAIL DENIED. EPIDURALINJECTIONS FOR CONTROL OF PAIN SHALLBE LIMITED TO 3 INJECTIONS PER 6MONTHS PER RECIPIENT. 794 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.N29M139HIPAA REMARK CODEDESCRIPTIONMissingdocumentation/orders/notes/summary/report/invoice.Not covered unless supplier files anelectronic media claim (EMC).Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.795796CLAIM/DETAIL DENIED. THE MONTHLY(CALENDAR MONTH) LIMITATION FOR THISPROCEDURE CODE HAS BEEN EXCEEDED. 795 119CLAIM/DETAIL DENIED. THE ANNUAL(CALENDAR YEAR) LIMITATION FOR THISPROCEDURE CODE HAS BEEN EXCEEDED. 796 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.797 <strong>EOB</strong> IS NOT ON EXCEPTION CONTROL FILE 797798PROCEDURE CODE XZ299 IS LIMITED TO$150.00 PER CALENDAR MONTH PERRECIPIENT, PER PROVIDER. 798 119Benefit maximum for this timeperiod has been reached.M139Denied services exceed the coveragelimit for the demonstration.799800801REVENUE CODE 270 CANNOT EXCEED$2,000 BILLED AMOUNT PER MONTH.PLEASE RESUBMIT WITH ITEMIZED INVOICEFOR SUPPLIES FOR ENTIRE MONTH. 799 45CLAIM DENIED. PROCEDURE CODES X0074AND X0075 NOT PAYABLE ON SAME DATEOF SERVICE AS X0076. 800 97CLAIM DENIED. PROCEDURE CODE X0076NOT PAYABLE ON THE SAME DATE OFSERVICE AS X0074 OR X0075. 801 97Charges exceed your contracted/legislated fee arrangement.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.M54N20M86N20M86Missing/in<strong>com</strong>plete/invalid totalcharges.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.802803PROCEDURE CODE 00150 DISALLOWED BYSAME PROVIDER FOR SAME RECIPIENT ONTHE SAME DATE OF SERVICE ASPROCEDURES 09110 OR 00140. 802, 803 97RECIPIENT APPLIED INCOME NOT CURRENTFOR DOS - RECYCLE FOR EDIT 271. 103, 803 133Payment is included in theallowance for anotherservice/procedure.The disposition of thisclaim/service is pending furtherreview.N20M80M86N23Service not payable with otherservice rendered on the same date.Not covered when performed duringthe same session/date as apreviously processed service for thepatient.Service denied because paymentalready made for similar procedurewithin set time frame.Patient liability may be affected dueto coordination of benefits with othercarriers <strong>and</strong>/or maximum benefitprovisions.Page 38 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>808810HIPAAADJ RSNCODESMMIS EXCEPTIONMEDICAID DESCRIPTIONCODE(S)MONTHLY DIALYSIS PROCEDURE CODESARE NOT REIMBURSABLE FOR THE SAMEOR OVERLAPPING DATE OF SERVICE ASDAILY DIALYSIS PROCEDURE CODES. 808, 809 97HEMODIALYSIS PROCEDURE CODES ARENOT REIMBURSABLE FOR THE SAME OROVERLAPPING DATES OF SERVICE ASEVALUATION AND MANAGEMENTPROCEDURE CODES. 810, 811 97HIPAA ADJ RSN CODEDESCRIPTIONPayment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.HIPAAREMARKN20N20HIPAA REMARK CODEDESCRIPTIONService not payable with otherservice rendered on the same date.Service not payable with otherservice rendered on the same date.812814815816818ADDITIONAL SURGICAL PROCEDURES ARENOT PAYABLE ON SAME DATE OF SERVICEBY SAME PROVIDER FOR SAME RECIPIENTWHEN BILLING PROCEDURE 07910. 812, 813 97CLAIM DETAIL DENIED. THIS PROCEDURECODE NOT PAYABLE ON THE SAME DATEOF SERVICE AS X0063, X0096, OR XL307. 814 97CLAIM DETAIL DENIED. THIS PROCEDURECODE NOT PAYABLE ON THE SAME DATEOF SERVICE AS COMMUNITY RESIDENTIALSERVICES. 815 97CAST REMOVAL OR REPAIR HAS BEEN PAIDWITH APPLICATION OF CAST. IFUNRELATED PROCEDURES, SEND CLAIMWITH DOCUMENTATION OF UNRELATEDPROCEDURES TO THE DMS FOR REVIEW. 816, 817 97VENIPUNCTURE OR ARTERIAL PUNCTURE ISNOT ALLOWED ON THE SAME DATE OFSERVICE AS OTHER MONITOREDPROCEDURES. 551, 818, 819 97Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.N20M86N20M86N20M86M86M63N20M86Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Service denied because paymentalready made for similar procedurewithin set time frame.We do not pay for more than one ofthese on the same day.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.820821822824825826827BILLING OR REFERRING KENPAC PROVIDERNUMBER IS MISSING OR IS NOT THEKENPAC PHYSICIAN/CLINIC FOR DATE(S)BILLED. KENPAC REFERRING PROVIDERNUMBER SHOULD BE ENTERED IN FIELD 19. 820 M68CLAIM DETAIL DENIED. LIMITATIONEXCEEDED, PRIOR AUTHORIZATIONREQUIRED. 821 62X-RAY PROCEDURE NOT ALLOWED WITHIN12 MONTHS OF (00210) INTRAORALCOMPLETE SERIES. 822, 823 119DETAIL DENIED. PROCEDURE CODE 08670NOT PAYABLE WITHIN 24 MONTHS OFCERTAIN OTHER PROCEDURE CODES IFBILLED FOR THE SAME RECIPIENT BY THESAME PROVIDER. 824 119DETAIL DENIED. THIS PROCEDURE CODENOT PAYABLE WITHIN 24 MONTHS OF 08670IF BILLED FOR THE SAME RECIPIENT BY THESAME PROVIDER. 825 97PROCEDURE CODE 09110 NOT PAYABLE IFPAYMENT HAS BEEN MADE FOR OTHERDENTAL PROCEDURE CODES FOR THESAME DATE OF SERVICE. 826 97THIS PROCEDURE CODE IS NOT PAYABLE IFPAYMENT HAS BEEN MADE FORPROCEDURE CODE 09110 FOR THE SAMEDATE OF SERVICE. 827 97Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.M57M86M86M86N20M86N20Missing/in<strong>com</strong>plete/invalid attendingor referring physician identification.Missing/in<strong>com</strong>plete/invalid provideridentifier.Service denied because paymentalready made for similar procedurewithin set time frame.Service denied because paymentalready made for same/similarprocedure within set time frame.Service denied because paymentalready made for similar procedurewithin set time frame.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Service not payable with otherservice rendered on the same date.Page 39 of 46 Date: 3/30/2005
KY<strong>EOB</strong>828829MEDICAID DESCRIPTIONKENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESCLAIM/DETAIL DENIED. THIS REVENUE CODEIS NOT PAYABLE FOR THIS PROVIDERSPECIALTY CODE. 828 B7CLAIM/DETAIL DENIED. PROVIDER NOTELIGIBLE TO RECEIVE PAYMENT FORSERVICES PROVIDED TO KCHIP PHASE IIIRECIPIENTS. 829 B7HIPAA ADJ RSN CODEDESCRIPTIONThis provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.Provider contracted/ negotiatedrate expired or not on file.830 NO DRG FOUND 830 147CLAIM DENIED. DRG CANNOT USE831 DIAGNOSIS CODE. 831 A8 Claim denied; ungroupable DRG MA6396 Non-covered charge(s).832 CLAIM DENIED. DRG CRITERIA NOT MET. 832 A8 Claim denied; ungroupable DRG96 Non-covered charge(s).833 CLAIM DENIED. DRG INVALID AGE. 833 A8 Claim denied; ungroupable DRGThe diagnosis is inconsistent with9 the patient's age.96 Non-covered charge(s).834 DRG INVALID SEX. 834 A8 Claim denied; ungroupable DRG10The diagnosis is inconsistent withthe patient's gender.96 Non-covered charge(s).835 DRG INVALID DISCHARGE STATUS. 835 A8 Claim denied; ungroupable DRG N5096 Non-covered charge(s).836 DRG INVALID PRINCIPLE DIAGNOSIS. 836 A8 Claim denied; ungroupable DRG MA6396 Non-covered charge(s).CLAIM DENIED. DRG DENY 469 THROUGH837 470 837 A8 Claim denied; ungroupable DRG96 Non-covered charge(s).838 RESERVED FOR DRG 96 Non-covered charge(s).839 RESERVED FOR DRG 96 Non-covered charge(s).HIPAA HIPAA REMARK CODEREMARKDESCRIPTIONService denied because paymentalready made for similar procedureM86 within set time frame.M50Missing/in<strong>com</strong>plete/invalid revenuecode(s).Missing/in<strong>com</strong>plete/invalid principaldiagnosis.Missing/in<strong>com</strong>plete/invalid dischargeinformation.Missing/in<strong>com</strong>plete/invalid principaldiagnosis.840 PROCEDURE CODE HAS BEEN REBUNDLED. 840 97842Payment is included in theallowance for anotherservice/procedure.N19PROCEDURE CODE IS MUTUALLYEXCLUSIVE. 842 96 Non-covered charge(s). MA66843 PROCEDURE CODE IS INCIDENTAL. 843 96 Non-covered charge(s). N19M15Separately billed services/tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Procedure code incidental to primaryprocedure.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Procedure code incidental to primaryprocedure.844PROCEDURE CODE IS NOT INDICATED FORSEPARATE REIMBURSEMENT. 844 97Payment is included in theallowance for anotherservice/procedure.M15N19Separately billed services/tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Procedure code incidental to primaryprocedure.845 VISIT IS WITHIN ONE DAY PRE OP RANGE. 845 97846PROCEDURE CODE INCLUDES UNILATERALAND BILATERAL PERFORMANCE 846 97Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.M15M144Separately billed services/tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Pre-/post-operative care payment isincluded in the allowance for surgery/ procedure.847 PROCEDURE IS A BILATERAL OR DUPLICATE 847 18 Duplicate claim/service.848PLEASE PAY SPECIFIED PROCEDURECODES. 848849PROCEDURE DOES NOT REQUIRE ANASSISTANT SURGEON. 849 54Multiple physicians/ assistants arenot covered in this case.850851PROCEDURE CODE IS INVALID FORPATIENTS AGE. 850, 852 6PROCEDURE CODE IS INVALID FORPATIENTS SEX. 852 7The procedure/revenue code isinconsistent with the patient's age.The procedure/revenue code isinconsistent with the patient'sgender.MA66MA66Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Page 40 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION852853GMIS - INAPPROPRIATE PROCEDURE CODEFOR RECIPIENT'S AGE. 850, 852 6The procedure/revenue code isinconsistent with the patient's age.PEDIATRIC PROCEDURE AGE SHOULD BE 1TO 17 YEARS 850, 852 96 Non-covered charge(s).MA66Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.6The procedure/revenue code isinconsistent with the patient's age.854MATERNITY PROCEDURE AGE SHOULD BE12 - 55 YEARS. 850 6856 PROCEDURE NOT INDICATED FOR A MALE 856 7857PROCEDURE NOT INDICATED FOR AFEMALE 856 7The procedure/revenue code isinconsistent with the patient's age.The procedure/revenue code isinconsistent with the patient'sgender.The procedure/revenue code isinconsistent with the patient'sgender.MA66MA66Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.858 CLAIM DENIED. COSMETIC PROCEDURE. 858 50These are non-covered servicesbecause this is not deemed a`medical necessity' by the payer.859 CLAIM DENIED. DUPLICATE PROCEDURE. 846 18 Duplicate claim/service.860CLAIM DENIED. EXPERIMENTALPROCEDURE. 860 96 Non-covered charge(s).861 CLAIM DENIED. OBSOLETE PROCEDURE. 861 96 Non-covered charge(s). MA66PROCEDURE CODES DOES NOT REQUIREMultiple physicians/ assistants are863 AN Assistant SURGEON 863 54 not covered in this case.The procedure code/bill type isPROCEDURE CODE IS INVALID FORinconsistent with the place of864 LOCATION. 864 5 service.MA66PROCEDURE CODE NEEDS TO BE865 REPLACED. 865 A1 Claim denied charges. N19866867MA66PROCEDURE NEEDS TO BE REPLACED FORSURFACES BILLED. 866 A1 Claim denied charges. N19MA66PROCEDURE CODE NEEDS TO BEREPLACED FOR SURFACES BILLED. 867 A1 Claim denied charges. N19MA66Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Procedure code incidental to primaryprocedure.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Procedure code incidental to primaryprocedure.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Procedure code incidental to primaryprocedure.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.879CLAIM DENIED. PROCEDURE REQUIRESDOCUMENTATION 879 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.N29Missingdocumentation/orders/notes/summary/report/invoice.880CLAIM DENIED. PROCEDURE CODE IS FORPATIENTS UP TO AGE 14 880 6The procedure/revenue code isinconsistent with the patient's age.881882883884885CLAIM DENIED. PROCEDURE CODE IS FORPATIENTS OVER AGE 14. 880 6The procedure/revenue code isinconsistent with the patient's age.CLAIM DENIED. COSMETIC PROCEDURENOT PAYABLE BY MEDICAID 882 96 Non-covered charge(s).50These are non-covered servicesbecause this is not deemed a`medical necessity' by the payer.CLAIM DENIED. DUPLICATE PROCEDUREHAS BEEN PAID. 883 18 Duplicate claim/service. M86CLAIM DENIED PROCEDURE IS CONSIDEREDEXPERIMENTAL 884 96 Non-covered charge(s).55Claim/service denied becauseprocedure /treatment is deemedexperimental/ investigational bythe payer.CLAIM DENIED. PROCEDURE ISCONSIDERED OBSOLETE. 885 N65M63N2096 Non-covered charge(s). M67Service denied because paymentalready made for similar procedurewithin set time frame.We do not pay for more than one ofthese on the same day.Service not payable with otherservice rendered on the same date.Procedure code or procedure ratecount cannot be determined, or wasnot on file, for the date of service/provider.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).Page 41 of 46 Date: 3/30/2005
KY<strong>EOB</strong>886MEDICAID DESCRIPTIONKENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESCLAIM DENIED. INAPPROPRIATEPROCEDURE CODE BILLED. 862, 886 B18888 GMIS-VISIT IS WITHIN THE POST OP RANGE. 888 97CLAIM/DETAIL DENIED. THIS PROCEDURECODE IS NOT PAYABLE IF BILLED WITH A889 SUBSTANCE ABUSE DIAGNOSIS CODE. 889 11CLAIM/DETAIL DENIED. THIS PROCEDURE ISNOT PAYABLE IF BILLED WITHOUT ONE OFTHE DESIGNATED PREGNANCY DIAGNOSIS890 CODES. 890 11CLAIM/DETAIL DENIED. THIS PROCEDURECODE NOT PAYABLE IF BILLED WITHOUTONE OF THE DESIGNATED SUBSTANCE891 ABUSE DIAGNOSIS CODES. 891 11893894895UNITS OF SERVICE GREATER THAN THEREMAINING PRIOR AUTHORIZED AMOUNT. 893 62DETAIL DENIED. THE PRIOR AUTHORIZEDAMOUNT FOR THIS PROCEDURE HAS BEENMET. 894 62RELATED HISTORY OF MORE THAN 25TCNS. 895HIPAA ADJ RSN CODEDESCRIPTIONPayment denied because thisprocedure code/ modifier wasinvalid on the date of service orclaim submission.Payment is included in theallowance for anotherservice/procedure.The diagnosis is inconsistent withthe procedure.The diagnosis is inconsistent withthe procedure.The diagnosis is inconsistent withthe procedure.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.HIPAAREMARK896CLAIM HAS FAILED MORE THAN 24 ERRORCODES. PLEASE CORRECT AND RESUBMIT. 896 A1 Claim denied charges. M58This provider was notCLAIM DENIED TO PROVIDER NUMBERcertified/eligible to be paid for this99999997 FOR REBATCH OR RETURNprocedure/ service on this date of897 REASONS. 897 B7 service.M57898 TOO MANY CLAIMS IN CYCLE 898899 DENIED PER PROVIDER REQUEST 899 A1 Claim denied charges.THE RX NUMBER MUST BE COMPLETED TOPROCESS YOUR CLAIM. PLEASE COMPLETE900 AND RESUBMIT YOUR CLAIM. 900 A1 Claim denied charges. M58DRUG QUANTITY IS REQUIRED. COMPLETETHE MISSING INFORMATION AND RESUBMIT901 YOUR CLAIM. 901 A1 Claim denied charges. M123M67M144MA63N56N56M139M139M53HIPAA REMARK CODEDESCRIPTIONMissing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).Pre-/post-operative care payment isincluded in the allowance for surgery/ procedure.Missing/in<strong>com</strong>plete/invalid principaldiagnosis.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/invalid provideridentifier.Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/invalid name,strength, or dosage of the drugfurnished.Missing/in<strong>com</strong>plete/invalid days orunits of service.902CLAIM DENIED. DRUG QUANTITY BILLEDFOR ESTABLISHED MINIMUM/ MAXIMUMQUANTITIES. 902 57Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.M53Missing/in<strong>com</strong>plete/invalid days orunits of service.903CLAIM DENIED. DRUG DAYS SUPPLYMISSING OR INVALID. 903 57Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.M53Missing/in<strong>com</strong>plete/invalid days orunits of service.904CLAIM DENIED. NDC IS RATED DESI FORCLAIM DATE OF SERVICE. 904 N60A valid NDC is required for paymentof drug claim effective Oct 2002905906CLAIM CREDIT QUANTITY MUST BE EQUALTO OR LOWER THAN ORIGINAL CLAIMQUANTITY, PLEASE RESUBMIT. 905 107PRESCRIBING PROVIDER'S LICENSENUMBER MISSING INVALID OR NOT ON KYMEDICAID FILE. 906 B757Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.MA66M58M53N31In<strong>com</strong>plete/invalid principalprocedure code <strong>and</strong>/or date.Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/invalid days orunits of service.Missing/in<strong>com</strong>plete/invalidprescribing/referring/attendingprovider license number.Page 42 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>907MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESCLAIM DENIED. NDC IS TERMINATED OROBSOLETE. 907 B18HIPAA ADJ RSN CODEDESCRIPTIONPayment denied because thisprocedure code/ modifier wasinvalid on the date of service orclaim submission.HIPAAREMARKN60HIPAA REMARK CODEDESCRIPTIONA valid NDC is required for paymentof drug claim effective Oct 2002908909910911CLAIM\DETAIL IS DENIED. THE RECIPIENT ISIN A NURSING FACILITY ON THE DATE OFSERVICE. 908 60CLAIM DETAIL DENIED. ANCILLARYSERVICES NOT AUTHORIZED BY THE PRO. 909 62CLAIM DENIED. SUBMITTED LEVEL OF CARESERVICES NOT AUTHORIZED BY THE PRO. 910 62MODIFIER INVALID FOR PROCEDURE CODEBILLED. 911 4Charges for outpatient serviceswith this proximity to inpatientservices are not covered.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.The procedure code isinconsistent with the modifierused or a required modifier ismissing.MA101N54N54M78A SNF is responsible for payment ofoutside providers who furnish theseservices/supplies to residents.Claim information is inconsistent withpre-certified/authorized servicesClaim information is inconsistent withpre-certified/authorized servicesMissing/in<strong>com</strong>plete/invalid HCPCSmodifier.913914CLAIM DENIED. DAYS SUPPLY EXCEEDS 32DAYS. 913 57CLAIM DENIED. HEADER COVERED DAYSGREATER THAN THE 14 DAY MAXIMUMALLOWED. 005 119Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.Benefit maximum for this timeperiod has been reached.M53MA32M53Missing/in<strong>com</strong>plete/invalid days orunits of service.Missing/in<strong>com</strong>plete/invalid number ofcovered days during the billingperiod.Missing/in<strong>com</strong>plete/invalid days orunits of service.915916917918919CLAIM/DETAIL DENIED. THE NON-COVEREDAMOUNT CANNOT BE GREATER THAN THEBILLED AMOUNT. 915 42CLAIM/DETAIL DENIED. EPSDT SPECIALSERVICES CLAIMS NOT PAYABLE FOR THISCharges exceed our fee scheduleor maximum allowable amount.MA31M54Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong> ending dates of the period billed.Missing/in<strong>com</strong>plete/invalid totalcharges.RECIPIENT. 916 96 Non-covered charge(s). N30 Recipient ineligible for this service.CLAIM/DETAIL DENIED. SCREENINGPROCEDURE CODE INVALID FORThe procedure/revenue code isMissing/in<strong>com</strong>plete/invalid principalRECIPIENT'S AGE. 917 6 inconsistent with the patient's age. MA66 procedure code or date.CLAIM/DETAIL DENIED. THE DETAIL DATESOF SERVICE ARE NOT EQUAL TO OR WITHINTHE HEADER DATES OF SERVICE. 918 A1 Claim denied charges. MA31DETAIL DENIED. THIS SERVICE IS NOTPAYABLE BEYOND THE BIRTH MONTH OFTHE RECIPIENT'S 21ST BIRTHDAY. 919 6The procedure/revenue code isinconsistent with the patient's age.Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong> ending dates of the period billed.921922923924CLAIM DENIED. THIRD PARTY LIABILITYAMOUNT IS EQUAL TO MEDICARE PAIDAMOUNT OR GREATER THAN HEADERCOINSURANCE PLUS HEADER DEDUCTIBLE. 921 42Charges exceed our fee scheduleor maximum allowable amount.THIS SERVICE WAS NOT PAID BY MEDICARE.MEDICAID PAYMENT CAN ONLY BE MADEFROM A PAID MEDICARE EOMB. 122 96 Non-covered charge(s). N8CLAIM DENIED. A NINE-BYTE, ALL-NUMERICTAX ID-NUMBER MUST BE ENTERED IN THEPATIENT'S ACCOUNT NUMBER FIELD ONTHE CLAIM. 923 A1 Claim denied charges. MA113CLAIM DENIED. DISPROPORTIONATE SHAREHOSPITAL CLAIMS WHICH SPAN ARECIPIENT'S 6TH BIRTHDAY MUST BE SPLITBILLED. PLEASE REFER TO THE BILLINGINSTRUCTIONS IN YOUR PROVIDERMANUAL. 124 A1 Claim denied charges. N59N48N63Claim information does not agreewith information received from otherinsurance carrier.Crossover claim denied by previouspayer <strong>and</strong> <strong>com</strong>plete claim data notforwarded. Resubmit this claim tothis payer to provide adequate datafor adjudication.In<strong>com</strong>plet/invalid taxpayeridentification number (TIN) submittedby you per the Internal RevenueService. Your claims cannot beprocessed without your correct TIN,<strong>and</strong> you may not bill the patientpending correction of your TIN.There are no appeas rights forunprocessable claims, buy you mayresubmit this claims after you havenotified this office of your correct TIN.Please refer to your provider manualfor additional program <strong>and</strong> providerinformation.Rebill services on separate claimlines.Page 43 of 46 Date: 3/30/2005
KY<strong>EOB</strong>925926927928931KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAHIPAAADJ RSNCODESMMIS EXCEPTIONMEDICAID DESCRIPTIONCODE(S)CLAIM/ DETAIL DENIED. VENIPUNCTUREAND ARTERIAL PUNCTURE NOT ALLOWEDON SAME DATE OF SERVICE AS OTHERMONITORED PROCEDURES. 925 97CLAIMS/DETAIL DENIED. THIS SERVICE NOTPAYABLE ON THE SAME DATEOF SERVICE AS VENIPUNCTURE ANDARTERIAL PUNCTURE.926 97HIPAA ADJ RSN CODEDESCRIPTIONPayment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.HIPAAREMARKCLAIM DENIED. THE CLINIC NUMBER MUSTBE ENTERED. 927 A1 Claim denied charges. MA82DETAIL DENIED. A VALID 5-DIGIT MODIFIERMUST BE ENTERED. 928 4CLAIM DENIED. COMPOUND CODE MISSINGOR INVALID. 931 B18The procedure code isinconsistent with the modifierused or a required modifier ismissing.Payment denied because thisprocedure code/ modifier wasinvalid on the date of service orclaim submission.933CLAIM DENIED. UNIT DOSE INDICATORMISSING OR INVALID. 933 A1 Claim denied charges. M123935 DRUG INCOMPATIBILITY ALERT. 751 96 Non-covered charge(s).944 LOW DOSE ALERT. 752 96 Non-covered charge(s).945 HIGH DOSE ALERT. 753 96 Non-covered charge(s).946 LATE REFILL. 755 96 Non-covered charge(s).947 MINIMUM DURATION ALERT. 756 96 Non-covered charge(s).948 MAXIMUM DURATION ALERT. 757 96 Non-covered charge(s).949 DRUG ALLERGY ALERT. 758 96 Non-covered charge(s).MA112M78N60HIPAA REMARK CODEDESCRIPTIONMissing/in<strong>com</strong>plete/invalidprovider/supplier billingnumber/identifier or billing name,address, city, state, zip code, orphone number.Missing/in<strong>com</strong>plete/invalid grouppractice information.Missing/in<strong>com</strong>plete/invalid HCPCSmodifier.A valid NDC is required for paymentof drug claim effective Oct 2002Missing/in<strong>com</strong>plete/invalid name,strength, or dosage of the drugfurnished.950951952953954955956957958CLAIM DENIED. THIS SERVICE IS NOTPAYABLE FOR PSYCHIATRIC RESIDENTIALTREATMENT FACILITY RECIPIENTS. 950 96 Non-covered charge(s). N30 Recipient ineligible for this service.THIS SERVICE IS NOT COVERED BYMEDICAID. 959 96 Non-covered charge(s).REIMBURSEMENT FOR THIS SERVICE ISINCLUDED IN THE TOTAL PAYMENTAMOUNT. 952 B15CLAIM DETAIL DENIED. ONLY ONE UNIT OFSERVICE ALLOWED PER MODIFIER. 953 119CLAIM DETAIL DENIED. THE PROCEDURECODE MODIFIER IS MISSING OR INVALID. 954 4CLAIM/DETAIL DENIED. PROVIDERSPECIALTY INVALID FOR MODIFIER GT. 955 B18THIS PROFESSIONAL CANNOT BILL THISPROCEDURE CODE. 956 8CMHC PROCEDURES X0054 OR X0152PAYABLE ONLY WHEN BILLED WITHANOTHER CMHC PROCEDURE CODE 957 107EFFECTIVE WITH DATES OF SERVICE ONOR AFTER 070193, A FIVE- DIGIT MODIFIERMUST BE BILLED ON COMMUNITY MENTALHEALTH CENTER CLAIMS. 958 4Payment adjusted because thisprocedure/service is not paidseparately.Benefit maximum for this timeperiod has been reached.The procedure code isinconsistent with the modifierused or a required modifier ismissing.Payment denied because thisprocedure code/ modifier wasinvalid on the date of service orclaim submission.The procedure code isinconsistent with the providertype/specialty (taxonomy).Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.The procedure code isinconsistent with the modifierused or a required modifier ismissing.M63M78N95N95N56M78We do not pay for more than one ofthese on the same day.Missing/in<strong>com</strong>plete/invalid HCPCSmodifier.This provider type/provider specialtymay not bill this service.This provider type/provider specialtymay not bill this service.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Missing/in<strong>com</strong>plete/invalid HCPCSmodifier.959 PRIOR ADVERSE DRUG REACTION. 759 96 Non-covered charge(s).960THIS REVENUE CODE IS NOT PAYABLEWHEN BILLED WITH ALL INCLUSIVEACCOMMODATION REVENUE CODE 100.CHARGES MOVED TO NON-COVERED. 960 97Payment is included in theallowance for anotherservice/procedure.THIS REVENUE CODE IS NOT PAYABLEWHEN BILLED WITH ALL INCLUSIVEREVENUE CODE 101 AND ALL INCLUSIVEPayment is included in theANCILLARY REVENUE CODE 240. CHARGESallowance for another961 MOVED TO NON-COVERED. 961 97 service/procedure.962 PREGNANCY ALERT. 763 96 Non-covered charge(s).963 DRUG/GENDER ALERT. 764 96 Non-covered charge(s).N34M50M50Incorrect claim form for this service.Missing/in<strong>com</strong>plete/invalid revenuecode(s).Missing/in<strong>com</strong>plete/invalid revenuecode(s).Page 44 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION964965966967968969970971972973974CLAIM DENIED. PSYCHIATRIC RESIDENTIALTREATMENT FACILITY SERVICES ARE NOTPAYABLE TO RECIPIENTS OVER AGE 21. 964 6CLAIM DENIED. CHILDREN'S TARGETEDCASE MANAGEMENT SERVICES ARE NOTPAYABLE TO RECIPIENTS OVER AGE 20. 965 6CLAIM DENIED. ADULT TARGETED CASEMANAGEMENT SERVICES ARE NOTPAYABLE TO RECIPIENTS UNDER AGE 18. 966 6CLAIM DENIED. REIMBURSEMENT FOR THISREVENUE CODE IS LIMITED TO TWO UNITSOF SERVICE PER DAY. 967 119CLAIM DENIED. REIMBURSEMENT FOR THISREVENUE CODE IS LIMITED TO ONE UNIT OFSERVICE PER DAY. 968 119THIS PROCEDURE CODE REQUIRES THEENTRY OF A VALID QUADRANT CODE IN THEThe procedure/revenue code isinconsistent with the patient's age.The procedure/revenue code isinconsistent with the patient's age.The procedure/revenue code isinconsistent with the patient's age.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.TOOTH NUMBER FIELD. 969 A1 Claim denied charges. M58THIS PROCEDURE REQUIRES THE ENTRYOF A VALID ARCH CODE IN THE TOOTHNUMBER FIELD. 970 A1 Claim denied charges. M58Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedLITER FLOW PER MINUTE AND/OR NUMBEROF HOURS MISSING OR INVALID. 971 16using remittance advice remarkscodes whenever appropriate. M125CLAIM DENIED. PROCEDURE CODES FORMILEAGE, OXYGEN, AND SUPPLIES MUSTMATCH THE BASE RATE CATEGORY. 972 A1 Claim denied charges. M51N65PROCEDURE CODE 02951 IS LIMITED TOBenefit maximum for this timeONE TOOTH PER DETAIL. 973 119 period has been reached.M53DUPLICATE TOOTH NUMBERS ARE NOTALLOWED ON THE SAME DETAIL FORPROCEDURE CODE 04211. 974 18 Duplicate claim/service. M53M53M63N63Missing/in<strong>com</strong>plete/invalid days orunits of service.We do not pay for more than one ofthese on the same day.Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/invalidinformation on the period of time forwhich the service/supply/equipmentwill be needed.Missing/in<strong>com</strong>plete/invalid procedurecode(s) <strong>and</strong>/or rates.Procedure code or procedure ratecount cannot be determined, or wasnot on file, for the date of service/provider.Missing/in<strong>com</strong>plete/invalid days orunits of service.Missing/in<strong>com</strong>plete/invalid days orunits of service.Rebill services on separate claimlines.975UNITS MUST EQUAL NUMBER OF TEETHPER DETAIL FOR PROCEDURE CODE 04211. 975 A1 Claim denied charges. M53PIN RETENTION THERAPY PROCEDURE02951 IS LIMITED TO PERMANENT MOLARS976 ONLY. 976 A1 Claim denied charges. N56The referring/prescribing/rendering provider is not eligible torefer/prescribe/ order/perform the977 TYPE OF BILL INVALID FOR PROVIDER TYPE. 977 52 service billed.MA30978979981982CLAIM DENIED. ONLY ONE BASE RATEPROCEDURE CODE ALLOWED PER CLAIM. 978 A1 Claim denied charges. N56CLAIM DENIED. EMERGENCYTRANSPORTATION CLAIMS WITH DATES OFSERVICE ON OR AFTER 7/1/95 MUST BESUBMITTED ON PAPER. 979 A1 Claim denied charges. N56PROVIDER NOT ALLOWED TO BILL CLAIMSON PAPER. 981 A1 Claim denied charges. M117CLAIM/DETAIL DENIED. VACCINEPROCEDURE CODE MUST BE BILLED USINGThe procedure code isMODIFIER 26 FOR ADMINISTRATION TOinconsistent with the modifierINDICATE VACCINE OBTAINED FROMused or a required modifier isPRIVATE SOURCE. 982 4 missing.M78Missing/in<strong>com</strong>plete/invalid days orunits of service.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Missing/in<strong>com</strong>plete/invalid type ofbill.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Not covered unless supplier files anelectronic media claim (EMC).Missing/in<strong>com</strong>plete/invalid HCPCSmodifier.984985MEDICARE EOMB DOES NOT INDICATE THATCOINSURANCE AND DEDUCTIBLE AMOUNTSARE DUE. 984 16DETAIL DENIED. THIS PROCEDURE LIMITEDTO TWO UNITS OF SERVICE. 985 119Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.Benefit maximum for this timeperiod has been reached.N48M53Claim information does not agreewith information received from otherinsurance carrier.Missing/in<strong>com</strong>plete/invalid days orunits of service.986DETAIL DENIED. PROCEDURE CODE A0420MUST ALSO BE BILLED WHEN AN EXTRAMILEAGE PROCEDURE CODE IS BILLEDWITH A ROUND TRIP PROCEDURE CODE. 986 107Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.N56Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Page 45 of 46 Date: 3/30/2005
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION987988989990991DETAIL DENIED. PROCEDURE CODES A0070AND A0422 LIMITED TO 1 UNIT OF SERVICEIF BASE RATE INDICATES ONE WAY TRIP. 987 119HEADER MEDICARE ALLOWED AMOUNT ISNOT EQUAL TO THE SUM OF THE DETAILBenefit maximum for this timeperiod has been reached.MEDICARE ALLOWED AMOUNTS. 988 A1 Claim denied charges. M54M79CLAIM/DETAIL DENIED. RETURN MILEAGENOT PAYABLE WHEN BILLING FOR ONEWAY TRIP. 989 96 Non-covered charge(s). M67DETAIL DENIED. SERVICES NOT PAYABLEBEYOND THE MONTH OF THE RECIPIENT'STHIRD BIRTHDAY. 997 6UB92 CLAIM DOES NOT HAVE ANY DETAILLINES 991The procedure/revenue code isinconsistent with the patient's age.N56M53MA66Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Missing/in<strong>com</strong>plete/invalid totalcharges.Missing/in<strong>com</strong>plete/invalid charge.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).Missing/in<strong>com</strong>plete/invalid days orunits of service.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.992993994DETAIL DENIED. PROCEDURE CODE INVALIDFOR PROVIDER TYPE 13. 992 8CLAIM/DETAIL DENIED. SERVICES NOTPAYABLE ON SAME DATE OF SERVICE ASAIR AMBULANCE. 993 97CLAIM/DETAIL DENIED. MILEAGEPROCEDURE CODES NOT PAYABLE SAMEDATE OF SERVICE AS ADDITIONALPASSENGER PROCEDURE CODES. 994 97The procedure code isinconsistent with the provider type.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.M86995 ADJUSTMENT IN DENIED STATUS. 995 A1 Claim denied charges.NUMBER OF STUDENTS IN GROUP MISSING996 OR INVALID. 996 A1 Claim denied charges. M53MA66N20M86N20Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Missing/in<strong>com</strong>plete/invalid days orunits of service.997998CLAIM PAID ZERO DUE TO INVALIDPRESCRIBER LICENSE NUMBER. PLEASERESUBMIT AN ADJUSTMENT WITHCORRECTED VALID PRESCRIBER LICENSENUMBER. 906 17CLAIM TEMPORARILY SUSPENDED UNTILNEW FEE UPDATE IS IMPLEMENTED. 998 133999 PENDING FOR REVIEW. 999 133Payment adjusted becauserequested information was notprovided or wasinsufficient/in<strong>com</strong>plete. Additionalinformation is supplied using theremittance advice remarks codeswhenever appropriate.The disposition of thisclaim/service is pending furtherreview.The disposition of thisclaim/service is pending furtherreview.M58N31MA07Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/invalidprescribing/referring/attendingprovider license number.The claim information has also beenforwarded to Medicaid for review.Page 46 of 46 Date: 3/30/2005