EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
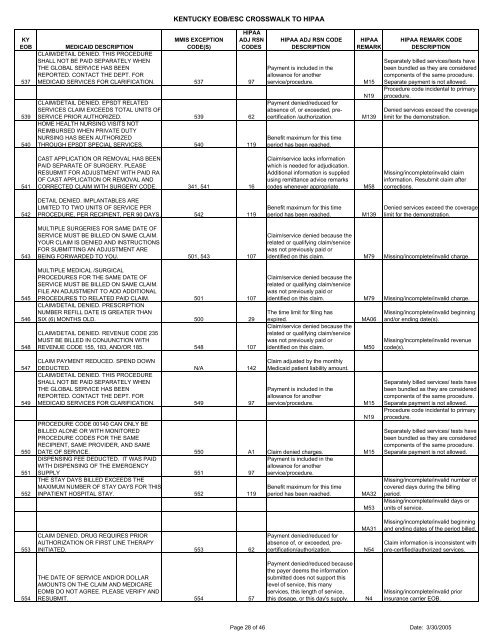
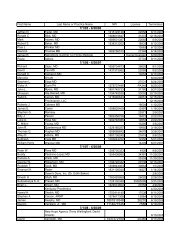
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>537539540MMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESMEDICAID DESCRIPTIONCLAIM/DETAIL DENIED. THIS PROCEDURESHALL NOT BE PAID SEPARATELY WHENTHE GLOBAL SERVICE HAS BEENREPORTED. CONTACT THE DEPT. FORMEDICAID SERVICES FOR CLARIFICATION. 537 97CLAIM/DETAIL DENIED. EPSDT RELATEDSERVICES CLAIM EXCEEDS TOTAL UNITS OFSERVICE PRIOR AUTHORIZED. 539 62HOME HEALTH NURSING VISITS NOTREIMBURSED WHEN PRIVATE DUTYNURSING HAS BEEN AUTHORIZEDTHROUGH EPSDT SPECIAL SERVICES. 540 119HIPAA ADJ RSN CODEDESCRIPTIONPayment is included in theallowance for anotherservice/procedure.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Benefit maximum for this timeperiod has been reached.HIPAAREMARKM15N19M139HIPAA REMARK CODEDESCRIPTIONSeparately billed services/tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Procedure code incidental to primaryprocedure.Denied services exceed the coveragelimit for the demonstration.541CAST APPLICATION OR REMOVAL HAS BEENPAID SEPARATE OF SURGERY. PLEASERESUBMIT FOR ADJUSTMENT WITH PAID RAOF CAST APPLICATION OR REMOVAL ANDCORRECTED CLAIM WITH SURGERY CODE. 341, 541 16Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.M58Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.542DETAIL DENIED. IMPLANTABLES ARELIMITED TO TWO UNITS OF SERVICE PERPROCEDURE, PER RECIPIENT, PER 90 DAYS. 542 119Benefit maximum for this timeperiod has been reached.M139Denied services exceed the coveragelimit for the demonstration.543545546548MULTIPLE SURGERIES FOR SAME DATE OFSERVICE MUST BE BILLED ON SAME CLAIM.YOUR CLAIM IS DENIED AND INSTRUCTIONSFOR SUBMITTING AN ADJUSTMENT AREBEING FORWARDED TO YOU. 501, 543 107MULTIPLE MEDICAL /SURGICALPROCEDURES FOR THE SAME DATE OFSERVICE MUST BE BILLED ON SAME CLAIM.FILE AN ADJUSTMENT TO ADD ADDITIONALPROCEDURES TO RELATED PAID CLAIM. 501 107CLAIM/DETAIL DENIED. PRESCRIPTIONNUMBER REFILL DATE IS GREATER THANSIX (6) MONTHS OLD. 500 29CLAIM/DETAIL DENIED. REVENUE CODE 235MUST BE BILLED IN CONJUNCTION WITHREVENUE CODE 155, 183, AND/OR 185. 548 107Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim. M79 Missing/in<strong>com</strong>plete/invalid charge.Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim. M79 Missing/in<strong>com</strong>plete/invalid charge.The time limit for filing hasexpired.Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.MA06M50Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong>/or ending date(s).Missing/in<strong>com</strong>plete/invalid revenuecode(s).547549550551552CLAIM PAYMENT REDUCED. SPEND DOWNDEDUCTED. N/A 142CLAIM/DETAIL DENIED. THIS PROCEDURESHALL NOT BE PAID SEPARATELY WHENTHE GLOBAL SERVICE HAS BEENREPORTED. CONTACT THE DEPT. FORMEDICAID SERVICES FOR CLARIFICATION. 549 97Claim adjusted by the monthlyMedicaid patient liability amount.Payment is included in theallowance for anotherservice/procedure.N19PROCEDURE CODE 00140 CAN ONLY BEBILLED ALONE OR WITH MONITOREDPROCEDURE CODES FOR THE SAMERECIPIENT, SAME PROVIDER, AND SAMEDATE OF SERVICE. 550 A1 Claim denied charges. M15DISPENSING FEE DEDUCTED. IT WAS PAIDWITH DISPENSING OF THE EMERGENCYSUPPLY 551 97THE STAY DAYS BILLED EXCEEDS THEMAXIMUM NUMBER OF STAY DAYS FOR THISINPATIENT HOSPITAL STAY. 552 119Payment is included in theallowance for anotherservice/procedure.Benefit maximum for this timeperiod has been reached.M15MA32M53Separately billed services/ tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Procedure code incidental to primaryprocedure.Separately billed services/ tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Missing/in<strong>com</strong>plete/invalid number ofcovered days during the billingperiod.Missing/in<strong>com</strong>plete/invalid days orunits of service.553CLAIM DENIED. DRUG REQUIRES PRIORAUTHORIZATION OR FIRST LINE THERAPYINITIATED. 553 62Payment denied/reduced forabsence of, or exceeded, precertification/authorization.MA31N54Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong> ending dates of the period billed.Claim information is inconsistent withpre-certified/authorized services.554THE DATE OF SERVICE AND/OR DOLLARAMOUNTS ON THE CLAIM AND MEDICAREEOMB DO NOT AGREE. PLEASE VERIFY ANDRESUBMIT. 554 57Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.N4Missing/in<strong>com</strong>plete/invalid priorinsurance carrier <strong>EOB</strong>.Page 28 of 46 Date: 3/30/2005