EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
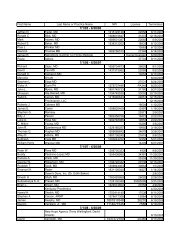
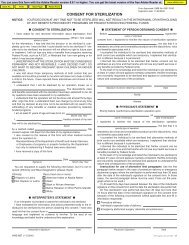
KY<strong>EOB</strong>555556MEDICAID DESCRIPTIONKENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESPLEASE ATTACH THE PART B MEDICAREEXPLANATION OF BENEFITS AND REBILL. 555 129CLAIM/DETAIL DENIED. RECIPIENT MUST BEAN INPATIENT IN THE NURSING FACILITY. 556 60HIPAA ADJ RSN CODEDESCRIPTIONPayment denied - Prior processinginformation appears incorrect.Charges for outpatient serviceswith this proximity to inpatientservices are not coveredHIPAA HIPAA REMARK CODEREMARKDESCRIPTIONMissing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim afterM58 corrections.M2Not paid separately when patient isan inpatient557CLAIM DENIED. SECOND LINEANTIHISTAMINE NOT PAYABLE WITHIN FIVEDAYS OF A FIRST LINE ANTIHISTAMINE. 557 57558 H0039 LIMITED TO 32 UNITS PER DAY. 119Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.Benefit maximum for this timeperiod has been reached.559560567568569570571572573574575576577578579580581582CLAIM DENIED. THIS CLAIM EXCEEDS THEMONTHLY MAXIMUM UNITS FOR THIS NDC. 559 119Benefit maximum for this timeperiod has been reached.M139Payment denied/reduced forDETAIL DENIED. PRIOR AUTHORIZEDabsence of, or exceeded, precertification/authorization.AMOUNT HAS BEEN EXCEEDED. 560 62M139CLAIM DENIED. NO WAIVER LIABILITYBUCKET FOR MONTH OF SERVICE. 267 A1 Claim denied charges. N58Payment denied/reduced forDETAIL DENIED. PRIOR AUTHORIZEDabsence of, or exceeded, precertification/authorization.AMOUNT HAS BEEN EXCEEDED. 568 62M139DETAIL DENIED. PRIOR AUTHORIZEDAMOUNT HAS BEEN EXCEEDED. 569 62ANCILLARY CHARGES NOT ALLOWED WITHPATIENT REVENUE CODES 180 OR 185. 096 60CLAIM DETAIL DENIED. PROCEDURE CODESX0100, X0101, AND X0102 CANNOT BEBILLED ON THE SAME DATE OF SERVICEFOR THE SAME RECIPIENT BY THE SAME ORDIFFERENT PROVIDER. 577 97Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.DETAIL DENIED. PRIOR AUTHORIZEDAMOUNT HAS BEEN EXCEEDED. 570 62M139PRIOR AUTHORIZATION REQUIRED IF 30DAYS OF THERAPY EXCEEDED DURING ABenefit maximum for this time365 DAY PERIOD. 571 119 period has been reached.DETAIL DENIED. LEAD INVESTIGATION INTHE HOME LIMITED TO TWO (2) SERVICESBenefit maximum for this timePER SIX MONTHS. 572 119 period has been reached.M139DETAIL DENIED. POST HAZARD ABATE INHOME LIMITED TO ONE (1) SERVICE PER 12Benefit maximum for this timeMONTHS. 573 119 period has been reached.M90Payment denied/reduced forCLAIM DENIED. PRIOR AUTHORIZEDabsence of, or exceeded, precertification/authorization.AMOUNT HAS BEEN EXCEEDED. 574 62M139REVENUE CODE INVALID FOR DATES OFSERVICE. 095 A1 Claim denied charges. M50Charges for outpatient serviceswith this proximity to inpatientservices are not covered.M50PRIOR AUTHORIZATION REQUIRED IF 60DAYS OF THERAPY EXCEEDED DURING A 3YEAR PERIOD. 578 11962CLAIM/DETAIL DENIED. REVENUE CODE 581LIMITED TO 80 UNITS PER RECIPIENT PERCALENDAR WEEK (SUNDAY THROUGHSATURDAY). 579 119CLAIM/DETAIL DENIED. THE ANNUALLIMITATION OF $1000.00 PER RECIPIENTFOR MINOR HOME ADAPTATIONS HAS BEENEXCEEDED. 180, 580 45CLAIM/DETAIL DENIED. UNIVERSALPREVENTION PROCEDURE CODES ARELIMITED TO A COMBINED TOTAL OF EIGHTUNITS PER RECIPIENT, PER PREGNANCY. 581 119CLAIM/DETAIL DENIED. SELECTIVEPREVENTION PROCEDURE CODES ARELIMITED TO A COMBINED TOTAL OF 76UNITS PER RECIPIENT, PER PREGNANCY. 582 119Payment is included in theallowance for anotherservice/procedure.Benefit maximum for this timeperiod has been reached.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Benefit maximum for this timeperiod has been reached.Charges exceed your contracted/legislated fee arrangement.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139N20M86M139M139M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Missing/in<strong>com</strong>plete/invalid patientliability amount.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Not covered more than once in a 12month period.Denied services exceed the coveragelimit for the demonstration.Missing/in<strong>com</strong>plete/invalid revenuecode(s).Missing/in<strong>com</strong>plete/invalid revenuecode(s).Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Page 29 of 46 Date: 3/30/2005