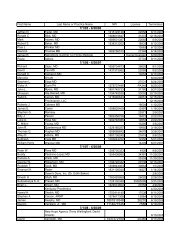
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
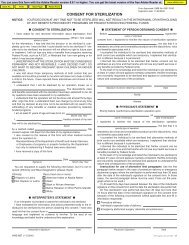
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION242243244245246248249NO LEVEL 2 PRICING RECORD FOUND FORMODIFIERS TC OR 26. 242 16PROCEDURE CODE Y2870 INVALID FORDATES OF SERVICE 10/15/94 AND AFTERFOR THIS PROVIDER TYPE. 243 8PROVIDER HAS NOT MET ALLREQUIREMENTS FOR BILLING OTHERLABORATORY AND X-RAY SERVICES. 244 B7Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.The procedure code isinconsistent with the providertype/specialty (taxonomy).This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.THESE SERVICES MAY BE BILLED ONLY BY ARECIPIENT'S HOSPICE PROVIDER. 245 B7N3280022-ROUTINE VENIPUNCTURE SINGLEHOMEBOUND NURSING HOME OR SNF NOTALLOWED SAME DOS/RECIPIENT/PROVIDERAS 80020-BLOOD COLLECTIONVENIPUNCTURE. 346 96 Non-covered charge(s). N20CLAIM DENIED. SURGEON AND ASSISTANTSURGEON BILLING NOT ALLOWED ON SAMEFORM. 248 54Multiple physicians/ assistants arenot covered in this case.PAYMENT REDUCED BECAUSE OURRECORDS SHOW RECIPIENT WAS NOT I NFACILITY FOR ALL OF THE TOTAL BILLEDDAYS. 249 A1 Claim denied charges. MA32N65M67M86M53Procedure code or procedure ratecount cannot be determined, or wasnot on file, for the date of service/provider.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).Provider performing service mustsubmit claim.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for same/similarprocedure within set time frame.Missing/in<strong>com</strong>plete/invalid number ofcovered days during the billingperiod.Missing/in<strong>com</strong>plete/invalid days orunits of service.250251THIS RECIPIENT IS NOT ON OUR ELIGIBILITYFILE. PLEASE VERIFY RECIPIENT MAIDNUMBER. 250 31INCORRECT RECIPIENT IDENTIFICATIONNUMBER. 251 31Claim denied as patient cannot beidentified as our insured.Claim denied as patient cannot beidentified as our insured.MA31N32Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong> ending dates of the period billed.Provider performing service mustsubmit claim.252253254255256RECIPIENT NAME ON CLAIM DOES NOTMATCH RECIPIENT NAME ON THE MEDICAIDELIGIBILITY DATABASE FOR THE MAIDNUMBER SUBMITTED ON YOUR CLAIM. 252 140OUR RECORDS INDICATE THE RECIPIENTWAS DECEASED PRIOR TO THE ENDINGDATE OF SERVICE. 253 13THE RECIPIENT IS NOT ELIGIBLE ON THECLAIM SERVICE DATES. 254, 259, 265 2627Patient/insured healthidentification number <strong>and</strong> namedo not match.RECIPIENT HAS MEDICARE PART B. PLEASEBILL MEDICARE FOR THESE SUPPLIES. 255 96 Non-covered charge(s). MA64OUR RECORDS INDICATE THAT THISRECIPIENT MAY BE ELIGIBLE FORMEDICARE. PLEASE BILL MEDICARE FIRST.IF MEDICARE DENIES THIS SERVICE,RESUBMIT WITH PROOF OF DENIAL. 256 22MA36Missing/in<strong>com</strong>plete/invalid patientname.The date of death precedes thedate of service.Expenses incurred prior tocoverage. N30 Recipient ineligible for this service.Expenses incurred after coverageterminated.Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Payment adjusted because thiscare may be covered by anotherpayer per coordination of benefits.MA04MA83MA64Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information waseither not reported or was illegible.Did not indicate whether we are theprimary or secondary payer. Refer toItem 11 in the HCFA-1500instructions for assistance.Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Page 13 of 46 Date: 3/30/2005