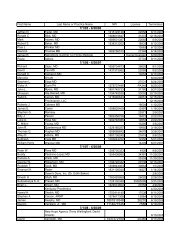
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
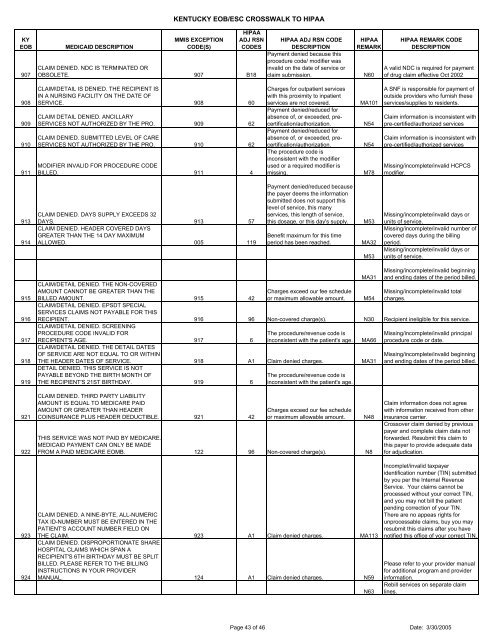
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>907MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESCLAIM DENIED. NDC IS TERMINATED OROBSOLETE. 907 B18HIPAA ADJ RSN CODEDESCRIPTIONPayment denied because thisprocedure code/ modifier wasinvalid on the date of service orclaim submission.HIPAAREMARKN60HIPAA REMARK CODEDESCRIPTIONA valid NDC is required for paymentof drug claim effective Oct 2002908909910911CLAIM\DETAIL IS DENIED. THE RECIPIENT ISIN A NURSING FACILITY ON THE DATE OFSERVICE. 908 60CLAIM DETAIL DENIED. ANCILLARYSERVICES NOT AUTHORIZED BY THE PRO. 909 62CLAIM DENIED. SUBMITTED LEVEL OF CARESERVICES NOT AUTHORIZED BY THE PRO. 910 62MODIFIER INVALID FOR PROCEDURE CODEBILLED. 911 4Charges for outpatient serviceswith this proximity to inpatientservices are not covered.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.The procedure code isinconsistent with the modifierused or a required modifier ismissing.MA101N54N54M78A SNF is responsible for payment ofoutside providers who furnish theseservices/supplies to residents.Claim information is inconsistent withpre-certified/authorized servicesClaim information is inconsistent withpre-certified/authorized servicesMissing/in<strong>com</strong>plete/invalid HCPCSmodifier.913914CLAIM DENIED. DAYS SUPPLY EXCEEDS 32DAYS. 913 57CLAIM DENIED. HEADER COVERED DAYSGREATER THAN THE 14 DAY MAXIMUMALLOWED. 005 119Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.Benefit maximum for this timeperiod has been reached.M53MA32M53Missing/in<strong>com</strong>plete/invalid days orunits of service.Missing/in<strong>com</strong>plete/invalid number ofcovered days during the billingperiod.Missing/in<strong>com</strong>plete/invalid days orunits of service.915916917918919CLAIM/DETAIL DENIED. THE NON-COVEREDAMOUNT CANNOT BE GREATER THAN THEBILLED AMOUNT. 915 42CLAIM/DETAIL DENIED. EPSDT SPECIALSERVICES CLAIMS NOT PAYABLE FOR THISCharges exceed our fee scheduleor maximum allowable amount.MA31M54Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong> ending dates of the period billed.Missing/in<strong>com</strong>plete/invalid totalcharges.RECIPIENT. 916 96 Non-covered charge(s). N30 Recipient ineligible for this service.CLAIM/DETAIL DENIED. SCREENINGPROCEDURE CODE INVALID FORThe procedure/revenue code isMissing/in<strong>com</strong>plete/invalid principalRECIPIENT'S AGE. 917 6 inconsistent with the patient's age. MA66 procedure code or date.CLAIM/DETAIL DENIED. THE DETAIL DATESOF SERVICE ARE NOT EQUAL TO OR WITHINTHE HEADER DATES OF SERVICE. 918 A1 Claim denied charges. MA31DETAIL DENIED. THIS SERVICE IS NOTPAYABLE BEYOND THE BIRTH MONTH OFTHE RECIPIENT'S 21ST BIRTHDAY. 919 6The procedure/revenue code isinconsistent with the patient's age.Missing/in<strong>com</strong>plete/invalid beginning<strong>and</strong> ending dates of the period billed.921922923924CLAIM DENIED. THIRD PARTY LIABILITYAMOUNT IS EQUAL TO MEDICARE PAIDAMOUNT OR GREATER THAN HEADERCOINSURANCE PLUS HEADER DEDUCTIBLE. 921 42Charges exceed our fee scheduleor maximum allowable amount.THIS SERVICE WAS NOT PAID BY MEDICARE.MEDICAID PAYMENT CAN ONLY BE MADEFROM A PAID MEDICARE EOMB. 122 96 Non-covered charge(s). N8CLAIM DENIED. A NINE-BYTE, ALL-NUMERICTAX ID-NUMBER MUST BE ENTERED IN THEPATIENT'S ACCOUNT NUMBER FIELD ONTHE CLAIM. 923 A1 Claim denied charges. MA113CLAIM DENIED. DISPROPORTIONATE SHAREHOSPITAL CLAIMS WHICH SPAN ARECIPIENT'S 6TH BIRTHDAY MUST BE SPLITBILLED. PLEASE REFER TO THE BILLINGINSTRUCTIONS IN YOUR PROVIDERMANUAL. 124 A1 Claim denied charges. N59N48N63Claim information does not agreewith information received from otherinsurance carrier.Crossover claim denied by previouspayer <strong>and</strong> <strong>com</strong>plete claim data notforwarded. Resubmit this claim tothis payer to provide adequate datafor adjudication.In<strong>com</strong>plet/invalid taxpayeridentification number (TIN) submittedby you per the Internal RevenueService. Your claims cannot beprocessed without your correct TIN,<strong>and</strong> you may not bill the patientpending correction of your TIN.There are no appeas rights forunprocessable claims, buy you mayresubmit this claims after you havenotified this office of your correct TIN.Please refer to your provider manualfor additional program <strong>and</strong> providerinformation.Rebill services on separate claimlines.Page 43 of 46 Date: 3/30/2005