EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
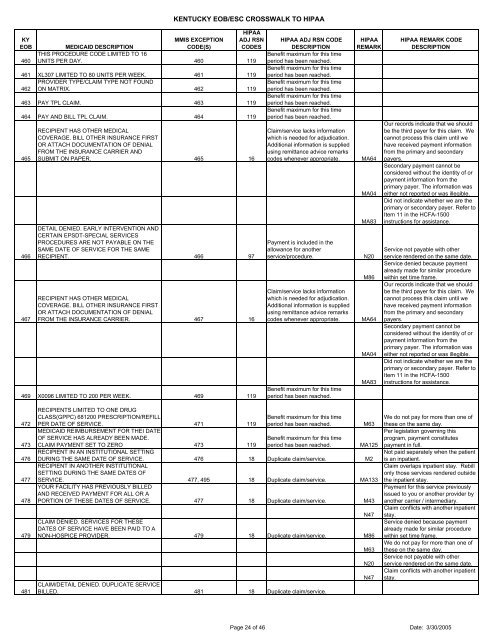
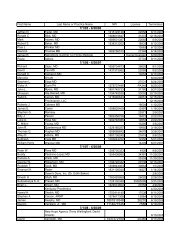
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>460MMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESMEDICAID DESCRIPTIONTHIS PROCEDURE CODE LIMITED TO 16UNITS PER DAY. 460 119461 XL307 LIMITED TO 80 UNITS PER WEEK. 461 119PROVIDER TYPE/CLAIM TYPE NOT FOUND462 ON MATRIX. 462 119463 PAY TPL CLAIM. 463 119464 PAY AND BILL TPL CLAIM. 464 119465466467RECIPIENT HAS OTHER MEDICALCOVERAGE. BILL OTHER INSURANCE FIRSTOR ATTACH DOCUMENTATION OF DENIALFROM THE INSURANCE CARRIER ANDSUBMIT ON PAPER. 465 16DETAIL DENIED. EARLY INTERVENTION ANDCERTAIN EPSDT-SPECIAL SERVICESPROCEDURES ARE NOT PAYABLE ON THESAME DATE OF SERVICE FOR THE SAMERECIPIENT. 466 97RECIPIENT HAS OTHER MEDICALCOVERAGE. BILL OTHER INSURANCE FIRSTOR ATTACH DOCUMENTATION OF DENIALFROM THE INSURANCE CARRIER. 467 16469 X0096 LIMITED TO 200 PER WEEK. 469 119HIPAA ADJ RSN CODEDESCRIPTIONBenefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.Payment is included in theallowance for anotherservice/procedure.Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.Benefit maximum for this timeperiod has been reached.HIPAAREMARKMA64MA04MA83N20M86MA64MA04MA83HIPAA REMARK CODEDESCRIPTIONOur records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information waseither not reported or was illegible.Did not indicate whether we are theprimary or secondary payer. Refer toItem 11 in the HCFA-1500instructions for assistance.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information waseither not reported or was illegible.Did not indicate whether we are theprimary or secondary payer. Refer toItem 11 in the HCFA-1500instructions for assistance.472473476477478479481RECIPIENTS LIMITED TO ONE DRUGCLASS(GPPC) 681200 PRESCRIPTION/REFILLPER DATE OF SERVICE. 471 119MEDICAID REIMBURSEMENT FOR THEI DATEOF SERVICE HAS ALREADY BEEN MADE.CLAIM PAYMENT SET TO ZERO 473 119RECIPIENT IN AN INSTITUTIONAL SETTINGBenefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M63MA125DURING THE SAME DATE OF SERVICE. 476 18 Duplicate claim/service. M2RECIPIENT IN ANOTHER INSTITUTIONALSETTING DURING THE SAME DATES OFSERVICE. 477, 495 18 Duplicate claim/service. MA133YOUR FACILITY HAS PREVIOUSLY BILLEDAND RECEIVED PAYMENT FOR ALL OR APORTION OF THESE DATES OF SERVICE. 477 18 Duplicate claim/service. M43N47CLAIM DENIED. SERVICES FOR THESEDATES OF SERVICE HAVE BEEN PAID TO ANON-HOSPICE PROVIDER. 479 18 Duplicate claim/service. M86CLAIM/DETAIL DENIED. DUPLICATE SERVICEBILLED. 481 18 Duplicate claim/service.M63N20N47We do not pay for more than one ofthese on the same day.Per legislation governing thisprogram, payment constitutespayment in full.Not paid separately when the patientis an inpatient.Claim overlaps inpatient stay. Rebillonly those services rendered outsidethe inpatient stay.Payment for this service previouslyissued to you or another provider byanother carrier / intermediary.Claim conflicts with another inpatientstay.Service denied because paymentalready made for similar procedurewithin set time frame.We do not pay for more than one ofthese on the same day.Service not payable with otherservice rendered on the same date.Claim conflicts with another inpatientstay.Page 24 of 46 Date: 3/30/2005