EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
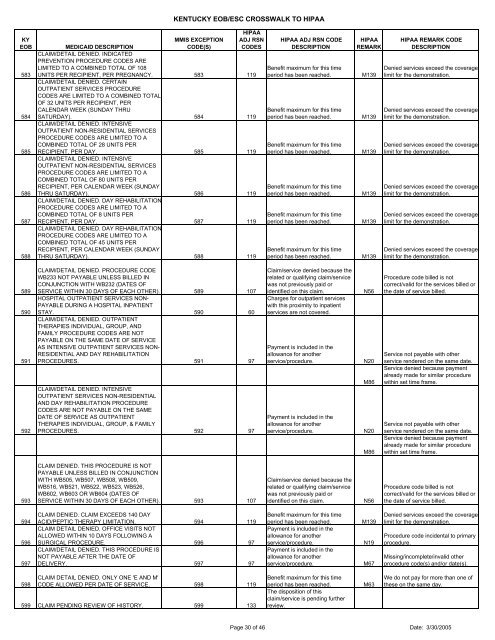
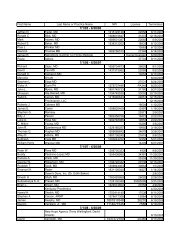
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>583584585586587588HIPAAADJ RSNCODESMMIS EXCEPTIONMEDICAID DESCRIPTIONCODE(S)CLAIM/DETAIL DENIED. INDICATEDPREVENTION PROCEDURE CODES ARELIMITED TO A COMBINED TOTAL OF 108UNITS PER RECIPIENT, PER PREGNANCY. 583 119CLAIM/DETAIL DENIED. CERTAINOUTPATIENT SERVICES PROCEDURECODES ARE LIMITED TO A COMBINED TOTALOF 32 UNITS PER RECIPIENT, PERCALENDAR WEEK (SUNDAY THRUSATURDAY). 584 119CLAIM/DETAIL DENIED. INTENSIVEOUTPATIENT NON-RESIDENTIAL SERVICESPROCEDURE CODES ARE LIMITED TO ACOMBINED TOTAL OF 28 UNITS PERRECIPIENT, PER DAY. 585 119CLAIM/DETAIL DENIED. INTENSIVEOUTPATIENT NON-RESIDENTIAL SERVICESPROCEDURE CODES ARE LIMITED TO ACOMBINED TOTAL OF 80 UNITS PERRECIPIENT, PER CALENDAR WEEK (SUNDAYTHRU SATURDAY). 586 119CLAIM/DETAIL DENIED. DAY REHABILITATIONPROCEDURE CODES ARE LIMITED TO ACOMBINED TOTAL OF 8 UNITS PERRECIPIENT, PER DAY. 587 119CLAIM/DETAIL DENIED. DAY REHABILITATIONPROCEDURE CODES ARE LIMITED TO ACOMBINED TOTAL OF 45 UNITS PERRECIPIENT, PER CALENDAR WEEK (SUNDAYTHRU SATURDAY). 588 119HIPAA ADJ RSN CODEDESCRIPTIONBenefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.HIPAAREMARKM139M139M139M139M139M139HIPAA REMARK CODEDESCRIPTIONDenied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.589590591592CLAIM/DETAIL DENIED. PROCEDURE CODEWB233 NOT PAYABLE UNLESS BILLED INCONJUNCTION WITH WB232 (DATES OFSERVICE WITHIN 30 DAYS OF EACH OTHER). 589 107HOSPITAL OUTPATIENT SERVICES NON-PAYABLE DURING A HOSPITAL INPATIENTSTAY. 590 60CLAIM/DETAIL DENIED. OUTPATIENTTHERAPIES INDIVIDUAL, GROUP, ANDFAMILY PROCEDURE CODES ARE NOTPAYABLE ON THE SAME DATE OF SERVICEAS INTENSIVE OUTPATIENT SERVICES NON-RESIDENTIAL AND DAY REHABILITATIONPROCEDURES. 591 97CLAIM/DETAIL DENIED. INTENSIVEOUTPATIENT SERVICES NON-RESIDENTIALAND DAY REHABILITATION PROCEDURECODES ARE NOT PAYABLE ON THE SAMEDATE OF SERVICE AS OUTPATIENTTHERAPIES INDIVIDUAL, GROUP, & FAMILYPROCEDURES. 592 97Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.Charges for outpatient serviceswith this proximity to inpatientservices are not covered.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.N56N20M86N20M86Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.593CLAIM DENIED. THIS PROCEDURE IS NOTPAYABLE UNLESS BILLED IN CONJUNCTIONWITH WB505, WB507, WB508, WB509,WB516, WB521, WB522, WB523, WB526,WB602, WB603 OR WB604 (DATES OFSERVICE WITHIN 30 DAYS OF EACH OTHER). 593 107Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.N56Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.594596597CLAIM DENIED. CLAIM EXCEEDS 140 DAYACID/PEPTIC THERAPY LIMITATION. 594 119CLAIM DETAIL DENIED. OFFICE VISITS NOTALLOWED WITHIN 10 DAYS FOLLOWING ASURGICAL PROCEDURE. 596 97CLAIM/DETAIL DENIED. THIS PROCEDURE ISNOT PAYABLE AFTER THE DATE OFDELIVERY. 597 97Benefit maximum for this timeperiod has been reached.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.M139N19M67Denied services exceed the coveragelimit for the demonstration.Procedure code incidental to primaryprocedure.Missing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).598CLAIM DETAIL DENIED. ONLY ONE 'E AND M'CODE ALLOWED PER DATE OF SERVICE. 598 119599 CLAIM PENDING REVIEW OF HISTORY. 599 133Benefit maximum for this timeperiod has been reached.The disposition of thisclaim/service is pending furtherreview.M63We do not pay for more than one ofthese on the same day.Page 30 of 46 Date: 3/30/2005