EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
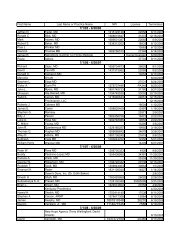
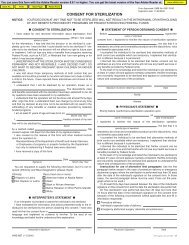
KY<strong>EOB</strong>741742743744745746747748749KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESMEDICAID DESCRIPTIONCLAIM DENIED. RECIPIENT LIMITED TO 2DIAGNOSTIC ULTRASOUNDS PER 9MONTHS. MEDICAL NECESSITY MUSTSUPPORT UNUSUAL CIRCUMSTANCES.DIAGNOSIS CODE MUST INDICATE MEDICALNECESSITY. 741 50DETAIL DENIED. PROCEDURE CODE 00210LIMITED TO ONE UNIT PER RECIPIENT, PERPROVIDER, PER 12 MONTHS. 742 119PROCEDURE CODE 04211 LIMITED TO 1UNIT PER TOOTH, PER 12 MONTHS, PERRECIPIENT, PER PROVIDER. 743 119CLAIM/DETAIL DENIED. PROCEDURE CODESXH100, X0058, 99199, AND 99499 ARELIMITED TO 40 UNITS OF SERVICE PER DATEOF STATE. CHECK THE UNITS OF SERVICEBILLED FOR ERRORS. 744 119CLAIM/DETAIL DENIED. PROCEDURE CODEX0058 CANNOT BE BILLED BY A SCHOOLBASED PROVIDER AND A COMMUNITYMENTAL HEALTH PROVIDER ON THE SAMEDATE OF SERVICE. 745 B7REVENUE/PROCEDURE CODE INVALID FORPROVIDER TYPE. 146 8CLAIM DETAIL DENIED. PROCEDURE CODESX0078, X0079, AND X0098 (ANYCOMBINATION) LIMITED TO FORTY HOURSPER SEVEN DAY PERIOD. 747 119REVENUE/PROCEDURE CODE INVALID FORPLACE OF SERVICE. 148 5CLAIM DETAIL DENIED. PROCEDURE CODEX0063 LIMITED TO 168 HOURS PER SIXMONTHS. 749 119HIPAA ADJ RSN CODEDESCRIPTIONThese are non-covered servicesbecause this is not deemed a`medical necessity' by the payer.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.The procedure code isinconsistent with the providertype/specialty (taxonomy).Benefit maximum for this timeperiod has been reached.The procedure code/bill type isinconsistent with the place ofservice.Benefit maximum for this timeperiod has been reached.HIPAAREMARKM139M76M90M90M53M63MA66M139MA66M139HIPAA REMARK CODEDESCRIPTIONDenied services exceed the coveragelimit for the demonstration.Missing/in<strong>com</strong>plete/invalid diagnosisor condition.Not covered more than once in a 12month period.Not covered more than once in a 12month period.Missing/in<strong>com</strong>plete/invalid days orunits of service.We do not pay for more than one ofthese on the same day.In<strong>com</strong>plete/invalid principalprocedure code <strong>and</strong>/or date.Denied services exceed the coveragelimit for the demonstration.Missing/in<strong>com</strong>plete/invalid principalprocedure code or date.Denied services exceed the coveragelimit for the demonstration.750 DRUG/DRUG INTERACTION. 750 96 Non-covered charge(s). N14Payment denied because thisprocedure code/ modifier wasREVENUE/PROCEDURE CODE INVALID FORinvalid on the date of service or751 DATE OF SERVICE. 151 B18 claim submission.M50Payment denied because thisprocedure code/ modifier wasinvalid on the date of service or752 REVENUE CODE MISSING/INVALID. 152 B18 claim submission.M50753INVALID REVENUE CODE. CHARGES NOTALLOWED. 146, 148, 151, 152, 510 B18Payment denied because thisprocedure code/ modifier wasinvalid on the date of service orclaim submission.754 EARLY REFILL. 754 N14755756757758NON-REIMBURSABLE FOR THIS PROVIDERTYPE/DOS. EFFECTIVE FOR DOS 10/01/90AND AFTER, DRUGS MUST BE BILLED BYMEDICAID PARTICIPATING PHARMACY. 755 A1 Claim denied charges. N95CLIA ID MISSING OR INVALID. CHARGESMOVED TO NON-COVERED. 756 96 Non-covered charge(s). MA120CHARGES MOVED TO NON-COVERED.RTSUP CAN ONLY BE REIMBURSED WHENCHARGES FOR RT ARE BILLED FOR THESAME DATES OF SERVICE. 757 96 Non-covered charge(s).PROVIDER NOT CLIA CERTIFIED TO BILLNON-WAIVERED LAB CODE. CHARGESMOVED TO NON-COVERED. 758 B7PROVIDER NOT CLIA CERTIFIED TO BILLNON-WAIVERED OR NON-MICROSCOPY LABCODE. CHARGES MOVED TO NON-COVERED. 759 B7This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.759760 INFERRED DRUG/DISEASE PRECAUTION. 760 96 Non-covered charge(s).761 DRUG/AGE PRECAUTION. 761 96 Non-covered charge(s).762 MEDICAL CONDITION ALERT. 762 96 Non-covered charge(s).M50MA51MA51Payment based on a contractualamount or agreement, fee schedule,or maximum allowable amountMissing/in<strong>com</strong>plete/invalid revenuecode(s).Missing/in<strong>com</strong>plete/invalid revenuecode(s).Missing/in<strong>com</strong>plete/invalid revenuecode(s).Payment based on a contractualamount or agreement, fee schedule,or maximum allowable amountThis provider type/provider specialtymay not bill this service.Missing/in<strong>com</strong>plete/invalid CLIAcertification number.Missing/in<strong>com</strong>plete/invalid CLIAcertification number for laboratoryservices billed by physician officelaboratory.Missing/in<strong>com</strong>plete/invalid CLIAcertification number for laboratoryservices billed by physician officelaboratory.Page 37 of 46 Date: 3/30/2005