EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
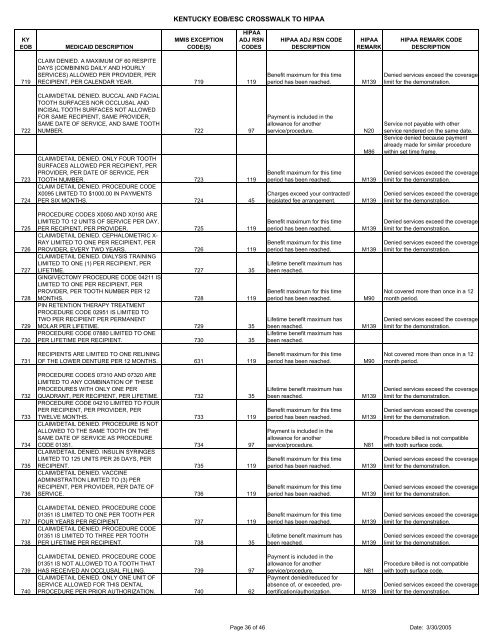
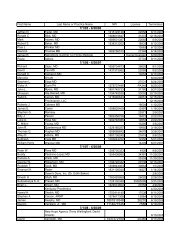
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION719CLAIM DENIED. A MAXIMUM OF 60 RESPITEDAYS (COMBINING DAILY AND HOURLYSERVICES) ALLOWED PER PROVIDER, PERRECIPIENT, PER CALENDAR YEAR. 719 119Benefit maximum for this timeperiod has been reached.M139Denied services exceed the coveragelimit for the demonstration.722723724CLAIM/DETAIL DENIED. BUCCAL AND FACIALTOOTH SURFACES NOR OCCLUSAL ANDINCISAL TOOTH SURFACES NOT ALLOWEDFOR SAME RECIPIENT, SAME PROVIDER,SAME DATE OF SERVICE, AND SAME TOOTHNUMBER. 722 97CLAIM/DETAIL DENIED. ONLY FOUR TOOTHSURFACES ALLOWED PER RECIPIENT, PERPROVIDER, PER DATE OF SERVICE, PERTOOTH NUMBER. 723 119CLAIM DETAIL DENIED. PROCEDURE CODEX0095 LIMITED TO $1000.00 IN PAYMENTSPER SIX MONTHS. 724 45Payment is included in theallowance for anotherservice/procedure.Benefit maximum for this timeperiod has been reached.Charges exceed your contracted/legislated fee arrangement.N20M86M139M139Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.725726727728729730PROCEDURE CODES X0050 AND X0150 ARELIMITED TO 12 UNITS OF SERVICE PER DAY,PER RECIPIENT, PER PROVIDER. 725 119CLAIM/DETAIL DENIED. CEPHALOMETRIC X-RAY LIMITED TO ONE PER RECIPIENT, PERPROVIDER, EVERY TWO YEARS. 726 119CLAIM/DETAIL DENIED. DIALYSIS TRAININGLIMITED TO ONE (1) PER RECIPIENT, PERLIFETIME. 727 35GINGIVECTOMY PROCEDURE CODE 04211 ISLIMITED TO ONE PER RECIPIENT, PERPROVIDER, PER TOOTH NUMBER PER 12MONTHS. 728 119PIN RETENTION THERAPY TREATMENTPROCEDURE CODE 02951 IS LIMITED TOTWO PER RECIPIENT PER PERMANENTMOLAR PER LIFETIME. 729 35PROCEDURE CODE 07880 LIMITED TO ONEPER LIFETIME PER RECIPIENT. 730 35Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Lifetime benefit maximum hasbeen reached.Benefit maximum for this timeperiod has been reached.Lifetime benefit maximum hasbeen reached.Lifetime benefit maximum hasbeen reached.M139M139M90M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Not covered more than once in a 12month period.Denied services exceed the coveragelimit for the demonstration.731RECIPIENTS ARE LIMITED TO ONE RELININGOF THE LOWER DENTURE PER 12 MONTHS. 631 119Benefit maximum for this timeperiod has been reached.M90Not covered more than once in a 12month period.732733734735736PROCEDURE CODES 07310 AND 07320 ARELIMITED TO ANY COMBINATION OF THESEPROCEDURES WITH ONLY ONE PERQUADRANT, PER RECIPIENT, PER LIFETIME. 732 35PROCEDURE CODE 04210 LIMITED TO FOURPER RECIPIENT, PER PROVIDER, PERTWELVE MONTHS. 733 119CLAIM/DETAIL DENIED. PROCEDURE IS NOTALLOWED TO THE SAME TOOTH ON THESAME DATE OF SERVICE AS PROCEDURECODE 01351. 734 97CLAIM/DETAIL DENIED. INSULIN SYRINGESLIMITED TO 125 UNITS PER 26 DAYS, PERRECIPIENT. 735 119CLAIM/DETAIL DENIED. VACCINEADMINISTRATION LIMITED TO (3) PERRECIPIENT, PER PROVIDER, PER DATE OFSERVICE. 736 119Lifetime benefit maximum hasbeen reached.Benefit maximum for this timeperiod has been reached.Payment is included in theallowance for anotherservice/procedure.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139N81M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Procedure billed is not <strong>com</strong>patiblewith tooth surface code.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.737738CLAIM/DETAIL DENIED. PROCEDURE CODE01351 IS LIMITED TO ONE PER TOOTH PERFOUR YEARS PER RECIPIENT. 737 119CLAIM/DETAIL DENIED. PROCEDURE CODE01351 IS LIMITED TO THREE PER TOOTHPER LIFETIME PER RECIPIENT. 738 35Benefit maximum for this timeperiod has been reached.Lifetime benefit maximum hasbeen reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.739740CLAIM/DETAIL DENIED. PROCEDURE CODE01351 IS NOT ALLOWED TO A TOOTH THATHAS RECEIVED AN OCCLUSAL FILLING. 739 97CLAIM/DETAIL DENIED. ONLY ONE UNIT OFSERVICE ALLOWED FOR THIS DENTALPROCEDURE PER PRIOR AUTHORIZATION. 740 62Payment is included in theallowance for anotherservice/procedure.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.N81M139Procedure billed is not <strong>com</strong>patiblewith tooth surface code.Denied services exceed the coveragelimit for the demonstration.Page 36 of 46 Date: 3/30/2005