EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
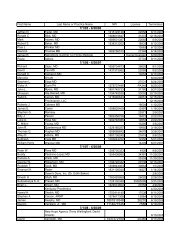
KY<strong>EOB</strong>273KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKMEDICAID DESCRIPTIONCLAIM/DETAIL DENIED. PROCEDURE CODE01351 IS LIMITED TO CERTAIN TOOTHNUMBERS. 273 A1 Claim denied charges. N39HIPAA REMARK CODEDESCRIPTIONProcedure code is not <strong>com</strong>patiblewith tooth number/letter274RECIPIENT TREATMENT AUTHORIZATIONINFORMATION NOT FOUND ON INPATIENTHOSPITAL FILE. 274 1562Payment adjusted because thesubmitted authorization number ismissing, invalid, or does not applyto the billed services or provider.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.M62Missing/in<strong>com</strong>plete/invalid treatmentauthorization code.275INPATIENT HOSPITAL TREATMENTAUTHORIZATION NUMBER MISSING ORINVALID. 113, 274 1562Payment adjusted because thesubmitted authorization number ismissing, invalid, or does not applyto the billed services or provider.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.M62Missing/in<strong>com</strong>plete/invalid treatmentauthorization code.276DETAIL DENIED. THIS SERVICE NOTPAYABLE FOR EMPOWER NON-EMERGENCYTRANSPORTATION RECIPIENTS. 276 96 Non-covered charge(s). N30 Recipient ineligible for this service.277278THE ATTACHED THIRD PARTYDOCUMENTATION IS NOT SUFFICIENT.CONTACT UNISYS PROVIDER RELATIONSFOR ASSISTANCE. 277, 279, 280, 281, 377, 467 16CLAIM DENIED. CLAIM/DOCUMENTATIONINDICATES THIRD PARTY PAYMENT WASRECEIVED BY RECIPIENT. 279, 280, 281, 282, 283, 467 100Claim/service lacks informationwhich is needed for adjudication.Additional information is suppliedusing remittance advice remarkscodes whenever appropriate.Payment made topatient/insured/responsible party.N225MA92MA92In<strong>com</strong>plete/invaliddocumentation/orders/ notes/summary/ report/ invoice.Missing/in<strong>com</strong>plete/invalid primaryinsurance information.Missing/in<strong>com</strong>plete/invalid primaryinsurance information.279280281282CLAIM/DETAIL INDICATES RECIPIENT HASOTHER INSURANCE BUT NO INSURANCEAMOUNT ENTERED ON CLAIM. 279 22A1CLAIM DENIED. YOUR CLAIM INDICATES THISSERVICE IS DUE TO A WORK-RELATEDACCIDENT/INJURY. PLEASE BILL OTHERINSURANCE FIRST. 280 19Payment adjusted because thiscare may be covered by anotherpayer per coordination of benefits.Claim denied charges.Claim denied because this is awork-related injury/illness <strong>and</strong>thus the liability of the Worker'sCompensation Carrier.RECIPIENT HAS OTHER MEDICALCOVERAGE. BILL OTHER INSURANCE FIRSTOR ATTACH DOCUMENTATION OF DENIALFROM THE INSURANCE CARRIER. 281, 465 A1 Claim denied charges. MA64THE RECIPIENT HAS MEDICARE PART A.PLEASE BILL MEDICARE. 282 109Claim not covered by thispayer/contractor. You must sendthe claim to the correctpayer/contractor.MA92MA64MA04MA83MA04MA83MA64MA04Missing/in<strong>com</strong>plete/invalid primaryinsurance information.Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information waseither not reported or was illegible.Did not indicate whether we are theprimary or secondary payer. Refer toItem 11 in the HCFA-1500instructions for assistance.Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information waseither not reported or was illegible.Did not indicate whether we are theprimary or secondary payer. Refer toItem 11 in the HCFA-1500instructions for assistance.Our records indicate that we shouldbe the third payer for this claim. Wecannot process this claim until wehave received payment informationfrom the primary <strong>and</strong> secondarypayers.Secondary payment cannot beconsidered without the identity of orpayment information from theprimary payer. The information waseither not reported or was illegible.Page 15 of 46 Date: 3/30/2005