EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
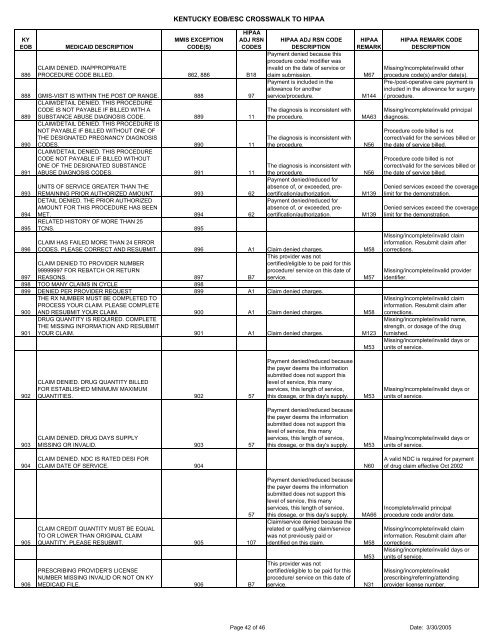
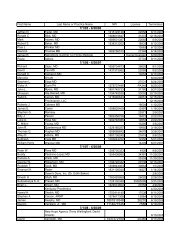
KY<strong>EOB</strong>886MEDICAID DESCRIPTIONKENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESCLAIM DENIED. INAPPROPRIATEPROCEDURE CODE BILLED. 862, 886 B18888 GMIS-VISIT IS WITHIN THE POST OP RANGE. 888 97CLAIM/DETAIL DENIED. THIS PROCEDURECODE IS NOT PAYABLE IF BILLED WITH A889 SUBSTANCE ABUSE DIAGNOSIS CODE. 889 11CLAIM/DETAIL DENIED. THIS PROCEDURE ISNOT PAYABLE IF BILLED WITHOUT ONE OFTHE DESIGNATED PREGNANCY DIAGNOSIS890 CODES. 890 11CLAIM/DETAIL DENIED. THIS PROCEDURECODE NOT PAYABLE IF BILLED WITHOUTONE OF THE DESIGNATED SUBSTANCE891 ABUSE DIAGNOSIS CODES. 891 11893894895UNITS OF SERVICE GREATER THAN THEREMAINING PRIOR AUTHORIZED AMOUNT. 893 62DETAIL DENIED. THE PRIOR AUTHORIZEDAMOUNT FOR THIS PROCEDURE HAS BEENMET. 894 62RELATED HISTORY OF MORE THAN 25TCNS. 895HIPAA ADJ RSN CODEDESCRIPTIONPayment denied because thisprocedure code/ modifier wasinvalid on the date of service orclaim submission.Payment is included in theallowance for anotherservice/procedure.The diagnosis is inconsistent withthe procedure.The diagnosis is inconsistent withthe procedure.The diagnosis is inconsistent withthe procedure.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.HIPAAREMARK896CLAIM HAS FAILED MORE THAN 24 ERRORCODES. PLEASE CORRECT AND RESUBMIT. 896 A1 Claim denied charges. M58This provider was notCLAIM DENIED TO PROVIDER NUMBERcertified/eligible to be paid for this99999997 FOR REBATCH OR RETURNprocedure/ service on this date of897 REASONS. 897 B7 service.M57898 TOO MANY CLAIMS IN CYCLE 898899 DENIED PER PROVIDER REQUEST 899 A1 Claim denied charges.THE RX NUMBER MUST BE COMPLETED TOPROCESS YOUR CLAIM. PLEASE COMPLETE900 AND RESUBMIT YOUR CLAIM. 900 A1 Claim denied charges. M58DRUG QUANTITY IS REQUIRED. COMPLETETHE MISSING INFORMATION AND RESUBMIT901 YOUR CLAIM. 901 A1 Claim denied charges. M123M67M144MA63N56N56M139M139M53HIPAA REMARK CODEDESCRIPTIONMissing/in<strong>com</strong>plete/invalid otherprocedure code(s) <strong>and</strong>/or date(s).Pre-/post-operative care payment isincluded in the allowance for surgery/ procedure.Missing/in<strong>com</strong>plete/invalid principaldiagnosis.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/invalid provideridentifier.Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/invalid name,strength, or dosage of the drugfurnished.Missing/in<strong>com</strong>plete/invalid days orunits of service.902CLAIM DENIED. DRUG QUANTITY BILLEDFOR ESTABLISHED MINIMUM/ MAXIMUMQUANTITIES. 902 57Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.M53Missing/in<strong>com</strong>plete/invalid days orunits of service.903CLAIM DENIED. DRUG DAYS SUPPLYMISSING OR INVALID. 903 57Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.M53Missing/in<strong>com</strong>plete/invalid days orunits of service.904CLAIM DENIED. NDC IS RATED DESI FORCLAIM DATE OF SERVICE. 904 N60A valid NDC is required for paymentof drug claim effective Oct 2002905906CLAIM CREDIT QUANTITY MUST BE EQUALTO OR LOWER THAN ORIGINAL CLAIMQUANTITY, PLEASE RESUBMIT. 905 107PRESCRIBING PROVIDER'S LICENSENUMBER MISSING INVALID OR NOT ON KYMEDICAID FILE. 906 B757Payment denied/reduced becausethe payer deems the informationsubmitted does not support thislevel of service, this manyservices, this length of service,this dosage, or this day's supply.Claim/service denied because therelated or qualifying claim/servicewas not previously paid oridentified on this claim.This provider was notcertified/eligible to be paid for thisprocedure/ service on this date ofservice.MA66M58M53N31In<strong>com</strong>plete/invalid principalprocedure code <strong>and</strong>/or date.Missing/in<strong>com</strong>plete/invalid claiminformation. Resubmit claim aftercorrections.Missing/in<strong>com</strong>plete/invalid days orunits of service.Missing/in<strong>com</strong>plete/invalidprescribing/referring/attendingprovider license number.Page 42 of 46 Date: 3/30/2005