EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
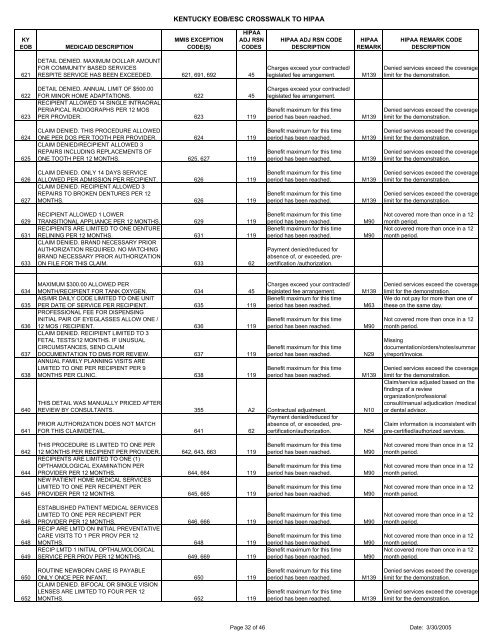
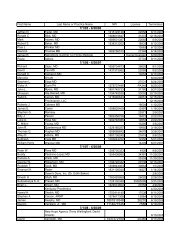
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION621DETAIL DENIED. MAXIMUM DOLLAR AMOUNTFOR COMMUNITY BASED SERVICESRESPITE SERVICE HAS BEEN EXCEEDED. 621, 691, 692 45Charges exceed your contracted/legislated fee arrangement.M139Denied services exceed the coveragelimit for the demonstration.622623DETAIL DENIED. ANNUAL LIMIT OF $500.00FOR MINOR HOME ADAPTATIONS. 622 45RECIPIENT ALLOWED 14 SINGLE INTRAORALPERIAPICAL RADIOGRAPHS PER 12 MOSPER PROVIDER. 623 119Charges exceed your contracted/legislated fee arrangement.Benefit maximum for this timeperiod has been reached.M139Denied services exceed the coveragelimit for the demonstration.624625CLAIM DENIED. THIS PROCEDURE ALLOWEDONE PER DOS PER TOOTH PER PROVIDER. 624 119CLAIM DENIED/RECIPIENT ALLOWED 3REPAIRS INCLUDING REPLACEMENTS OFONE TOOTH PER 12 MONTHS. 625, 627 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.626627CLAIM DENIED. ONLY 14 DAYS SERVICEALLOWED PER ADMISSION PER RECIPIENT. 626 119CLAIM DENIED. RECIPIENT ALLOWED 3REPAIRS TO BROKEN DENTURES PER 12MONTHS. 626 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.629631633RECIPIENT ALLOWED 1 LOWERTRANSITIONAL APPLIANCE PER 12 MONTHS. 629 119RECIPIENTS ARE LIMITED TO ONE DENTURERELINING PER 12 MONTHS. 631 119CLAIM DENIED. BRAND NECESSARY PRIORAUTHORIZATION REQUIRED. NO MATCHINGBRAND NECESSARY PRIOR AUTHORIZATIONON FILE FOR THIS CLAIM. 633 62Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.M90M90Not covered more than once in a 12month period.Not covered more than once in a 12month period.634635636637638640641MAXIMUM $300.00 ALLOWED PERMONTH/RECIPIENT FOR TANK OXYGEN. 634 45AIS/MR DAILY CODE LIMITED TO ONE UNITPER DATE OF SERVICE PER RECIPIENT. 635 119PROFESSIONAL FEE FOR DISPENSINGINITIAL PAIR OF EYEGLASSES ALLOW ONE /12 MOS / RECIPIENT. 636 119CLAIM DENIED. RECIPIENT LIMITED TO 3FETAL TESTS/12 MONTHS. IF UNUSUALCIRCUMSTANCES, SEND CLAIMDOCUMENTATION TO DMS FOR REVIEW. 637 119ANNUAL FAMILY PLANNING VISITS ARELIMITED TO ONE PER RECIPIENT PER 9MONTHS PER CLINIC. 638 119Charges exceed your contracted/legislated fee arrangement.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.THIS DETAIL WAS MANUALLY PRICED AFTERREVIEW BY CONSULTANTS. 355 A2 Contractual adjustment. N10Payment denied/reduced forPRIOR AUTHORIZATION DOES NOT MATCHabsence of, or exceeded, precertification/authorization.FOR THIS CLAIM/DETAIL. 641 62N54M139M63M90N29M139Denied services exceed the coveragelimit for the demonstration.We do not pay for more than one ofthese on the same day.Not covered more than once in a 12month period.Missingdocumentation/orders/notes/summary/report/invoice.Denied services exceed the coveragelimit for the demonstration.Claim/service adjusted based on thefindings of a revieworganization/professionalconsult/manual adjudication /medicalor dental advisor.Claim information is inconsistent withpre-certified/authorized services.642644645THIS PROCEDURE IS LIMITED TO ONE PER12 MONTHS PER RECIPIENT PER PROVIDER. 642, 643, 663 119RECIPIENTS ARE LIMITED TO ONE (1)OPTHAMOLOGICAL EXAMINATION PERPROVIDER PER 12 MONTHS. 644, 664 119NEW PATIENT HOME MEDICAL SERVICESLIMITED TO ONE PER RECIPIENT PERPROVIDER PER 12 MONTHS. 645, 665 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M90M90M90Not covered more than once in a 12month period.Not covered more than once in a 12month period.Not covered more than once in a 12month period.646648649ESTABLISHED PATIENT MEDICAL SERVICESLIMITED TO ONE PER RECIPIENT PERPROVIDER PER 12 MONTHS. 646, 666 119RECIP ARE LMTD ON INITIAL PREVENTATIVECARE VISITS TO 1 PER PROV PER 12MONTHS. 648 119RECIP LMTD 1 INITIAL OPTHALMOLOGICALSERVICE PER PROV PER 12 MONTHS. 649, 669 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M90M90M90Not covered more than once in a 12month period.Not covered more than once in a 12month period.Not covered more than once in a 12month period.650652ROUTINE NEWBORN CARE IS PAYABLEONLY ONCE PER INFANT. 650 119CLAIM DENIED. BIFOCAL OR SINGLE VISIONLENSES ARE LIMITED TO FOUR PER 12MONTHS. 652 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Page 32 of 46 Date: 3/30/2005