EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
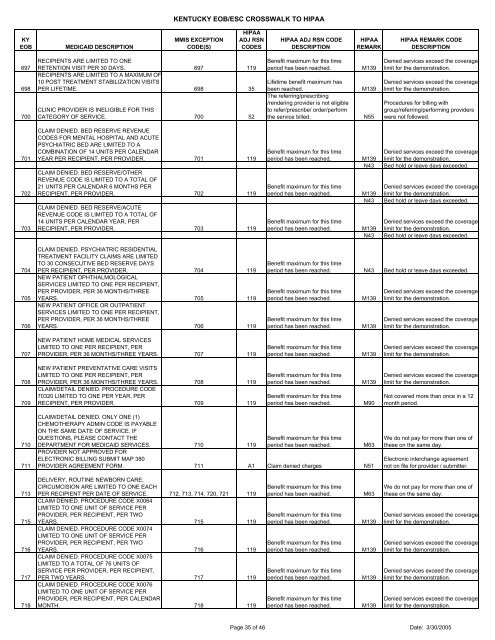
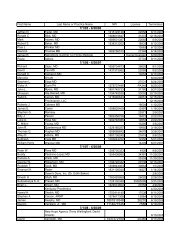
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>MEDICAID DESCRIPTIONMMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESHIPAA ADJ RSN CODEDESCRIPTIONHIPAAREMARKHIPAA REMARK CODEDESCRIPTION697698700RECIPIENTS ARE LIMITED TO ONERETENTION VISIT PER 30 DAYS. 697 119RECIPIENTS ARE LIMITED TO A MAXIMUM OF10 POST TREATMENT STABILIZATION VISITSPER LIFETIME. 698 35CLINIC PROVIDER IS INELIGIBLE FOR THISCATEGORY OF SERVICE. 700 52Benefit maximum for this timeperiod has been reached.Lifetime benefit maximum hasbeen reached.The referring/prescribing/rendering provider is not eligibleto refer/prescribe/ order/performthe service billed.M139M139N55Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Procedures for billing withgroup/referring/performing providerswere not followed.701702703CLAIM DENIED. BED RESERVE REVENUECODES FOR MENTAL HOSPITAL AND ACUTEPSYCHIATRIC BED ARE LIMITED TO ACOMBINATION OF 14 UNITS PER CALENDARYEAR PER RECIPIENT, PER PROVIDER. 701 119CLAIM DENIED. BED RESERVE/OTHERREVENUE CODE IS LIMITED TO A TOTAL OF21 UNITS PER CALENDAR 6 MONTHS PERRECIPIENT, PER PROVIDER. 702 119CLAIM DENIED. BED RESERVE/ACUTEREVENUE CODE IS LIMITED TO A TOTAL OF14 UNITS PER CALENDAR YEAR, PERRECIPIENT, PER PROVIDER. 703 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139N43M139N43M139N43Denied services exceed the coveragelimit for the demonstration.Bed hold or leave days exceeded.Denied services exceed the coveragelimit for the demonstration.Bed hold or leave days exceeded.Denied services exceed the coveragelimit for the demonstration.Bed hold or leave days exceeded.704705706CLAIM DENIED. PSYCHIATRIC RESIDENTIALTREATMENT FACILITY CLAIMS ARE LIMITEDTO 30 CONSECUTIVE BED RESERVE DAYSPER RECIPIENT, PER PROVIDER. 704 119NEW PATIENT OPHTHALMOLOGICALSERVICES LIMITED TO ONE PER RECIPIENT,PER PROVIDER, PER 36 MONTHS/THREEYEARS. 705 119NEW PATIENT OFFICE OR OUTPATIENTSERVICES LIMITED TO ONE PER RECIPIENT,PER PROVIDER, PER 36 MONTHS/THREEYEARS. 706 119Benefit maximum for this timeperiod has been reached. N43 Bed hold or leave days exceeded.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M139Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.707NEW PATIENT HOME MEDICAL SERVICESLIMITED TO ONE PER RECIPIENT, PERPROVIDER, PER 36 MONTHS/THREE YEARS. 707 119Benefit maximum for this timeperiod has been reached.M139Denied services exceed the coveragelimit for the demonstration.708709NEW PATIENT PREVENTATIVE CARE VISITSLIMITED TO ONE PER RECIPIENT, PERPROVIDER, PER 36 MONTHS/THREE YEARS. 708 119CLAIM/DETAIL DENIED. PROCEDURE CODE70320 LIMITED TO ONE PER YEAR, PERRECIPIENT, PER PROVIDER. 709 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M139M90Denied services exceed the coveragelimit for the demonstration.Not covered more than once in a 12month period.710711CLAIM/DETAIL DENIED. ONLY ONE (1)CHEMOTHERAPY ADMIN CODE IS PAYABLEON THE SAME DATE OF SERVICE. IFQUESTIONS, PLEASE CONTACT THEDEPARTMENT FOR MEDICAID SERVICES. 710 119Benefit maximum for this timeperiod has been reached.M63PROVIDER NOT APPROVED FORELECTRONIC BILLING SUBMIT MAP 380PROVIDER AGREEMENT FORM. 711 A1 Claim denied charges N51We do not pay for more than one ofthese on the same day.Electronic interchange agreementnot on file for provider / submitter.713715716717718DELIVERY, ROUTINE NEWBORN CARE,CIRCUMCISION ARE LIMITED TO ONE EACHPER RECIPIENT PER DATE OF SERVICE. 712, 713, 714, 720, 721 119CLAIM DENIED. PROCEDURE CODE X0064LIMITED TO ONE UNIT OF SERVICE PERPROVIDER, PER RECIPIENT, PER TWOYEARS. 715 119CLAIM DENIED. PROCEDURE CODE X0074LIMITED TO ONE UNIT OF SERVICE PERPROVIDER, PER RECIPIENT, PER TWOYEARS. 716 119CLAIM DENIED. PROCEDURE CODE X0075LIMITED TO A TOTAL OF 76 UNITS OFSERVICE PER PROVIDER, PER RECIPIENT,PER TWO YEARS. 717 119CLAIM DENIED. PROCEDURE CODE X0076LIMITED TO ONE UNIT OF SERVICE PERPROVIDER, PER RECIPIENT, PER CALENDARMONTH. 718 119Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.Benefit maximum for this timeperiod has been reached.M63M139M139M139M139We do not pay for more than one ofthese on the same day.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Page 35 of 46 Date: 3/30/2005