EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
EOB Codes and Descriptions - Kymmis.com
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
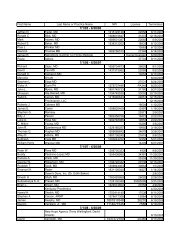
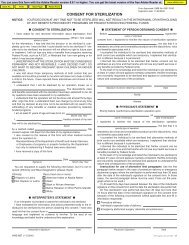
KENTUCKY <strong>EOB</strong>/ESC CROSSWALK TO HIPAAKY<strong>EOB</strong>518MMIS EXCEPTIONCODE(S)HIPAAADJ RSNCODESMEDICAID DESCRIPTIONCLAIM/DETAIL DENIED. INITIAL TOOTHEXTRACTION LIMITED TO ONE PERDOS/RECIPIENT /PROVIDER. USEPROCEDURE 07120 FOR EACH ADDITIONALTOOTH EXTRACTED 318 119HIPAA ADJ RSN CODEDESCRIPTIONBenefit maximum for this timeperiod has been reached.HIPAAREMARKM63HIPAA REMARK CODEDESCRIPTIONWe do not pay for more than one ofthese on the same day.519CLAIM DENIED. REIMBURSEMENT FORCIRCUMCISION WITHIN TEN DAYS OFDELIVERY IS INCLUDED IN DELIVERY FEE. 519 97Payment is included in theallowance for anotherservice/procedure.M15N19Separately billed services/tests havebeen bundled as they are considered<strong>com</strong>ponents of the same procedure.Separate payment is not allowed.Procedure code incidental to primaryprocedure.520MAINTENANCE DRUG DAYS SUPPLY LESSTHAN 30 DAYS. 520, 523 91 Dispensing fee adjustment. N14Payment based on a contractualamount or agreement, fee schedule,or maximum allowable amount521COMPREHENSIVE CLIENT RE-EVALUATIONNOT ALLOWED WITHIN 12 MONTHS OFCOMPREHENSIVE CLIENT EVALUATION. 521 119Benefit maximum for this timeperiod has been reached.M139Denied services exceed the coveragelimit for the demonstration.522523524525COMPREHENSIVE CLIENT RE-EVALUATIONLIMITED TO ONCE PER LIFE TIME. 522 119RESIDENTIAL COMPONENT SERVICE NOTALLOWED WITH IN-HOME SCL SERVICES ONTHE SAME DOS. 323 97IN-HOME SCL SERVICES NOT ALLOWEDWITH RESIDENTIAL COMPONENT SERVICESON THE SAME DOS. 324 97IN-PATIENT RECIPIENTS ARE LIMITED TOONE ATTENDANCE AND ONECONSULTATION PER ADMISSION. 628, 647 97Benefit maximum for this timeperiod has been reached.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.Payment is included in theallowance for anotherservice/procedure.M139N20N20MA133Denied services exceed the coveragelimit for the demonstration.Service not payable with otherservice rendered on the same date.Service not payable with otherservice rendered on the same date.Claim overlaps inpatient stay. Rebillonly those services rendered outsidethe inpatient stay.526527528529IN-PATIENT RECIPIENTS WHO HAVE HADORAL SURGERY ARE LIMITED TO 1ATTENDANCE AND/OR 1 CONSULTATIONPER DATE OF SERVICE PER PROVIDER. 526 97ADDITIONAL SERVICES TO THE SAMETOOTH ARE DISALLOWED IF THE TOOTHPayment is included in theallowance for anotherservice/procedure.M139MA133HAS BEEN PREVIOUSLY EXTRACTED. 400 18 Duplicate claim/service. M139ADDITIONAL SERVICES TO THE SAMETOOTH ARE DISALLOWED ON THE SAMEPayment is included in theDOS AS A CROWN PROCEDURE OR Aallowance for anotherFRACTURED INCISAL BUILD-UP. 402 97 service/procedure.N20CROWN AND BUILD UP PROCEDURES AREDISALLOWED IF ADDITIONAL DENTALSERVICES HAVE BEEN PAID FOR THE SAMETOOTH SAME DOS. 326 97Payment is included in theallowance for anotherservice/procedure.M86Denied services exceed the coveragelimit for the demonstration.Claim overlaps inpatient stay. Rebillonly those services rendered outsidethe inpatient stay.Denied services exceed the coveragelimit for the demonstration.Service not payable with otherservice rendered on the same date.Service denied because paymentalready made for similar procedurewithin set time frame.530531532533534535536CLAIM PAID. CLAIM HAS BEEN REDUCED BYTHE AMOUNT OF THE DISPENSING FEE. 481, 520, 521, 522 91 Dispensing fee adjustment. N14PURCHASE UNITS BILLED EXCEEDSMAXIMUM ALLOWED FOR THIS PRIORPayment denied/reduced forAUTHORIZATION CHECK YOUR MAP-9absence of, or exceeded, precertification/authorization.FORM. 531 62M139RENTAL UNITS/CHARGES BILLED EXCEEDSMAXIMUM ALLOWED FOR THIS PRIORAUTHORIZATION CHECK YOUR MAP-9FORM. 532 62CLAIM DENIED. PRIOR AUTHORIZATION NOTON FILE OR DOES NOT MATCH CLAIMINFORMATION. 533 62CLAIM DENIED. PROCEDURE CODE X0064CANNOT BE BILLED IN CONJUNCTION WITHOTHER PROCEDURE CODES. 534 97PLEASE BILL BABY'S HOSPITAL STAY AFTERMOTHER'S DISCHARGE ON SEPARATECLAIM FORM, USING BABY'S OWN NAMEPayment denied/reduced forabsence of, or exceeded, precertification/authorization.Payment denied/reduced forabsence of, or exceeded, precertification/authorization.Payment is included in theallowance for anotherservice/procedure.M139N54N56Payment based on a contractualamount or agreement, fee schedule,or maximum allowable amountDenied services exceed the coveragelimit for the demonstration.Denied services exceed the coveragelimit for the demonstration.Claim information is inconsistent withpre-certified/authorized services.Procedure code billed is notcorrect/valid for the services billed orthe date of service billed.AND NUMBER. 535 A1 Claim denied charges. N61 Rebill services on separate claims.THE MEDICARE EOMB INDICATES THIS IS ADUPLICATE BILLING. PLEASE SUBMIT THEORIGINAL EOMB INDICATING THEDEDUCTIBLE AND CO-INSURANCEMissing/in<strong>com</strong>plete/invalid priorAMOUNTS. 536 18 Duplicate claim/service. N4 insurance carrier <strong>EOB</strong>.Page 27 of 46 Date: 3/30/2005