Management of Extravasation of Cytotoxic Drugs in Children
Management of Extravasation of Cytotoxic Drugs in Children
Management of Extravasation of Cytotoxic Drugs in Children
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
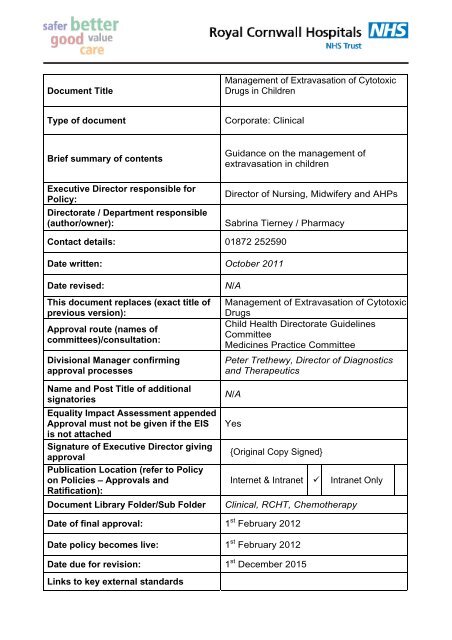
Document Title<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong><br />
<strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Type <strong>of</strong> document<br />
Corporate: Cl<strong>in</strong>ical<br />
Brief summary <strong>of</strong> contents<br />
Executive Director responsible for<br />
Policy:<br />
Directorate / Department responsible<br />
(author/owner):<br />
Guidance on the management <strong>of</strong><br />
extravasation <strong>in</strong> children<br />
Director <strong>of</strong> Nurs<strong>in</strong>g, Midwifery and AHPs<br />
Sabr<strong>in</strong>a Tierney / Pharmacy<br />
Contact details: 01872 252590<br />
Date written: October 2011<br />
Date revised:<br />
This document replaces (exact title <strong>of</strong><br />
previous version):<br />
Approval route (names <strong>of</strong><br />
committees)/consultation:<br />
Divisional Manager confirm<strong>in</strong>g<br />
approval processes<br />
Name and Post Title <strong>of</strong> additional<br />
signatories<br />
Equality Impact Assessment appended<br />
Approval must not be given if the EIS<br />
is not attached<br />
Signature <strong>of</strong> Executive Director giv<strong>in</strong>g<br />
approval<br />
Publication Location (refer to Policy<br />
on Policies – Approvals and<br />
Ratification):<br />
Document Library Folder/Sub Folder<br />
N/A<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong><br />
<strong>Drugs</strong><br />
Child Health Directorate Guidel<strong>in</strong>es<br />
Committee<br />
Medic<strong>in</strong>es Practice Committee<br />
Peter Trethewy, Director <strong>of</strong> Diagnostics<br />
and Therapeutics<br />
N/A<br />
Yes<br />
{Orig<strong>in</strong>al Copy Signed}<br />
Internet & Intranet Intranet Only<br />
Cl<strong>in</strong>ical, RCHT, Chemotherapy<br />
Date <strong>of</strong> f<strong>in</strong>al approval: 1 st February 2012<br />
Date policy becomes live: 1 st February 2012<br />
Date due for revision: 1 st December 2015<br />
L<strong>in</strong>ks to key external standards
Related Documents: See Appendix 6<br />
Suggested Keywords:<br />
Tra<strong>in</strong><strong>in</strong>g Need Identified<br />
<strong>Extravasation</strong>, Chemotherapy<br />
Yes - All nurses tra<strong>in</strong>ed <strong>in</strong> <strong>in</strong>itial<br />
chemotherapy tra<strong>in</strong><strong>in</strong>g, and to attend<br />
oncology update day annually<br />
This document is only valid on the day <strong>of</strong> pr<strong>in</strong>t<strong>in</strong>g<br />
Controlled Document<br />
This document has been created follow<strong>in</strong>g the Royal Cornwall Hospitals NHS Trust<br />
Policy on Document Production. It should not be altered <strong>in</strong> any way without the<br />
express permission <strong>of</strong> the author or their L<strong>in</strong>e Manager.<br />
Policy Template
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong><br />
<strong>Children</strong><br />
V1.0<br />
October 2011<br />
Policy Template<br />
Page 3 <strong>of</strong> 22
Version Control Table<br />
Date<br />
Version<br />
No<br />
Summary <strong>of</strong> Changes<br />
F<strong>in</strong>al amendments approved; EIA<br />
20.12.07 V1.0 Completed; document published<br />
Changes Made by<br />
(Name and Job Title)<br />
Jo Blogs<br />
Manager<br />
All or part <strong>of</strong> this document can be released under the Freedom <strong>of</strong> Information Act<br />
2000<br />
This document is to be reta<strong>in</strong>ed for 10 years from the date <strong>of</strong> expiry.<br />
Policy Template<br />
Page 4 <strong>of</strong> 22
Table <strong>of</strong> Contents<br />
1. Purpose and Scope ..................................................................................6<br />
2. Def<strong>in</strong>ition...................................................................................................6<br />
3. Ownership and Responsibilities................................................................7<br />
4. Monitor<strong>in</strong>g <strong>of</strong> the patient ...........................................................................7<br />
5. Patient Education......................................................................................7<br />
6. Signs and Symptoms................................................................................8<br />
7. Treatment <strong>of</strong> Peripheral L<strong>in</strong>e <strong>Extravasation</strong>..............................................9<br />
8. Treatment <strong>of</strong> <strong>Extravasation</strong> from Central Venous Access Devices:<br />
PICC’s, Hickman L<strong>in</strong>es & Portacaths.............................................................12<br />
9. Mixed <strong>Extravasation</strong>s..............................................................................13<br />
10. Documentation ....................................................................................13<br />
11. Monitor<strong>in</strong>g compliance and effectiveness ...........................................14<br />
12. Updat<strong>in</strong>g and Review ..........................................................................14<br />
13. Equality and Diversity..........................................................................14<br />
Appendix 1: <strong>Drugs</strong> commonly used <strong>in</strong> Paediatric oncology and their<br />
classification ..................................................................................................15<br />
Appendix 2: Non- <strong>Cytotoxic</strong> <strong>Extravasation</strong>....................................................16<br />
Appendix 3 : <strong>Extravasation</strong> Kit Contents.......................................................17<br />
Appendix 4 : Guidel<strong>in</strong>es for Best Practice When Adm<strong>in</strong>ister<strong>in</strong>g Intravenous<br />
Infusions ........................................................................................................18<br />
Appendix 5: Patient Information Sheet...........................................................19<br />
Appendix 6 - References ...............................................................................20<br />
Appendix 7.Initial Equality Impact Assessment Screen<strong>in</strong>g Form ...................21<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 5
1. Purpose and Scope<br />
1.1 This document outl<strong>in</strong>es guidel<strong>in</strong>es for the rapid treatment <strong>of</strong> extravasation <strong>in</strong>juries<br />
<strong>in</strong> paediatric patients with<strong>in</strong> Royal Cornwall Hospital Trust, exclud<strong>in</strong>g neonates,<br />
for which there is a separate policy.<br />
1.2 It provides a guidel<strong>in</strong>e to assist practitioners <strong>in</strong> the care <strong>of</strong> patients who may have<br />
experienced an extravasation <strong>in</strong>jury.<br />
1.3 It will provide a basis for the nurs<strong>in</strong>g staff to recognise ways <strong>in</strong> which to help<br />
prevent extravasation and how to recognise when an extravasation has occurred.<br />
2. Def<strong>in</strong>ition<br />
2.1 <strong>Extravasation</strong> is the leakage or accidental <strong>in</strong>filtration <strong>of</strong> <strong>in</strong>travenous drugs <strong>in</strong>to the<br />
surround<strong>in</strong>g tissues from the ve<strong>in</strong>. This can lead to an immediate <strong>in</strong>flammatory<br />
pa<strong>in</strong>ful reaction and with some drugs may result <strong>in</strong> local tissue destruction<br />
(necrosis) and other complications.<br />
<br />
<br />
<br />
<br />
Neutrals do not cause ulceration and are unlikely to produce an acute<br />
reaction or progress to necrosis.<br />
Irritants are capable <strong>of</strong> caus<strong>in</strong>g <strong>in</strong>flammation and irritation. They rarely<br />
proceed to the breakdown <strong>of</strong> tissues. They do have the potential to cause<br />
ulceration, but only if a large amount has extravasated <strong>in</strong>to the tissue.<br />
Exfoliants are capable <strong>of</strong> caus<strong>in</strong>g <strong>in</strong>flammation and shedd<strong>in</strong>g <strong>of</strong> the sk<strong>in</strong>, but<br />
are less likely to cause tissue death. They can cause pa<strong>in</strong><br />
Vesicants are drugs that have the potential to cause blister<strong>in</strong>g and ulceration,<br />
which when left untreated can lead to tissue damage and necrosis.<br />
2.2 It is recognised that prevention <strong>of</strong> extravasation is <strong>of</strong> importance and particularly<br />
when adm<strong>in</strong>ister<strong>in</strong>g vesicants or irritants the precautions should be taken to<br />
m<strong>in</strong>imise the risk <strong>of</strong> extravasation, see appendix 4.<br />
2.3 It is accepted that there are also other contribut<strong>in</strong>g factors that can affect each<br />
<strong>in</strong>dividual patient’s risk <strong>of</strong> extravasation.<br />
2.4 There are many different drugs that can equally be as destructive <strong>in</strong> the damage<br />
that they can cause if extravasation occurs, the ma<strong>in</strong> bulk <strong>of</strong> this document<br />
relates to cytotoxic chemotherapy, but the procedure outl<strong>in</strong>ed can be used for all<br />
vesicant drugs. Please note that there is a separate guidel<strong>in</strong>e for the<br />
extravasation <strong>of</strong> non-cytotoxic drugs <strong>in</strong> the neonate.<br />
2.5 Cancer drugs have been grouped <strong>in</strong>to 5 categories based on their potential to<br />
cause tissue damage, see appendix 1.<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 6
3. Ownership and Responsibilities<br />
3.1 The Trust Lead for Cancer Chemotherapy is responsible for ensur<strong>in</strong>g the<br />
implementation and adherence to these guidel<strong>in</strong>es. The Specialist<br />
Cl<strong>in</strong>ical Pharmacists <strong>in</strong> Paediatrics will aid the Cancer Lead <strong>in</strong> this role.<br />
3.2 The ward manager <strong>of</strong> Sennen ward is responsible for the education and<br />
development <strong>of</strong> nurs<strong>in</strong>g staff <strong>in</strong> the handl<strong>in</strong>g, adm<strong>in</strong>istration and disposal<br />
<strong>of</strong> cytotoxic drugs.<br />
3.3 It is the <strong>in</strong>dividual practitioner’s responsibility to ensure the tra<strong>in</strong><strong>in</strong>g they<br />
have received is appropriate, and rema<strong>in</strong>s updated.<br />
3.4 Ward requirements:<br />
3.4.1. Each cl<strong>in</strong>ical area where vesicant cytotoxic drugs are adm<strong>in</strong>istered<br />
must have a Paediatric <strong>Extravasation</strong> Kit available (i.e. Sennen ward and<br />
Gwithian Unit)<br />
3.4.2. Monthly checks <strong>of</strong> the <strong>Extravasation</strong> kit are the responsibility nurse<br />
<strong>in</strong> charge. This requires a check <strong>of</strong> the contents and the expiry date, and<br />
these checks should be recorded <strong>in</strong> the record book provided for this<br />
prupose.<br />
3.4.3. Replacement paediatric extravasation kits are available from<br />
pharmacy<br />
4. Monitor<strong>in</strong>g <strong>of</strong> the patient<br />
4.1 Dur<strong>in</strong>g adm<strong>in</strong>istration <strong>of</strong> <strong>in</strong>travenous medication the <strong>in</strong>jection site should be<br />
clearly visible and monitored for redness and swell<strong>in</strong>g regularly (see Appendix 4:<br />
“Guidel<strong>in</strong>es for best practice” for more detailed <strong>in</strong>formation on monitor<strong>in</strong>g<br />
requirements).<br />
5. Patient Education<br />
5.1 Patients/parents/guardians should be educated to the fact that extravasation is a<br />
potential risk <strong>of</strong> receiv<strong>in</strong>g chemotherapy when consent is obta<strong>in</strong>ed.<br />
5.2 Patient preference to cannulation site (if required) should be taken <strong>in</strong>to account,<br />
but education given as to why good placement and rotation <strong>of</strong> site is required.<br />
5.3 Education should encourage patients to <strong>in</strong>form nurs<strong>in</strong>g staff if they have pa<strong>in</strong>,<br />
st<strong>in</strong>g<strong>in</strong>g, burn<strong>in</strong>g or a change <strong>in</strong> sensation at cannulation site from start <strong>of</strong> the<br />
<strong>in</strong>fusion.<br />
5.4 In the advent <strong>of</strong> an extravasation patients should be provided with both verbal<br />
and written <strong>in</strong>formation, see appendix 5<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 7
6. Signs and Symptoms<br />
An extravasation should be suspected if one or more <strong>of</strong> the follow<strong>in</strong>g symptoms have<br />
occurred:<br />
6.1 The patient compla<strong>in</strong>s <strong>of</strong> burn<strong>in</strong>g, st<strong>in</strong>g<strong>in</strong>g, pa<strong>in</strong> or any discomfort at the <strong>in</strong>jection<br />
site. This should be dist<strong>in</strong>guished from a feel<strong>in</strong>g <strong>of</strong> cold that may occur with some<br />
drugs. The patient is <strong>of</strong>ten the first person to become aware that someth<strong>in</strong>g is<br />
wrong with the IV therapy, so <strong>in</strong>struct them at the beg<strong>in</strong>n<strong>in</strong>g <strong>of</strong> treatment to <strong>in</strong>form<br />
staff <strong>of</strong> any acute change dur<strong>in</strong>g treatment.<br />
6.2 Observation <strong>of</strong> swell<strong>in</strong>g, redness, mottl<strong>in</strong>g or blister<strong>in</strong>g at the <strong>in</strong>jection site. This<br />
should be dist<strong>in</strong>guished from the ‘nettle rash’ or ‘flare’ effect seen with some<br />
drugs.<br />
6.3 Care should be tak<strong>in</strong>g when no ‘flash back’ or blood return is obta<strong>in</strong>ed on<br />
aspiration. However, this is not a sign <strong>of</strong> extravasation if found <strong>in</strong> isolation and the<br />
presence <strong>of</strong> blood does not exclude extravasation<br />
6.4 There is <strong>in</strong>creased resistance felt on the plunger <strong>of</strong> the syr<strong>in</strong>ge <strong>of</strong> a bolus drug<br />
adm<strong>in</strong>istration, this however, could be due to possible changes <strong>in</strong> the position <strong>of</strong><br />
the body.<br />
6.5 There is absence <strong>of</strong> free flow or the rate <strong>of</strong> flow is remarkably reduced. This may<br />
not be recognisable when us<strong>in</strong>g an <strong>in</strong>fusion pump.<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 8
7. Treatment <strong>of</strong> Peripheral L<strong>in</strong>e <strong>Extravasation</strong><br />
Action<br />
1 Stop the adm<strong>in</strong>istration <strong>of</strong> the cytotoxic drug<br />
immediately, leav<strong>in</strong>g the cannula <strong>in</strong> place.<br />
Rationale<br />
To prevent further <strong>in</strong>filtration and to allow aspiration <strong>of</strong><br />
the drug to be attempted (see below)<br />
2 Expla<strong>in</strong> what has been suspected <strong>of</strong><br />
happen<strong>in</strong>g and next procedure to the<br />
patient/parent/guardian.<br />
To obta<strong>in</strong> patient’s and/or carer’s co-operation and<br />
consent.<br />
3 Disconnect any IV tub<strong>in</strong>g from the<br />
<strong>in</strong>travenous cannula, do not remove the<br />
cannula. Attempt to aspirate as much drug<br />
as possible with a new syr<strong>in</strong>ge.<br />
To prevent further <strong>in</strong>fusion through the l<strong>in</strong>e.<br />
To remove any residual drug.<br />
4 Contact a senior member <strong>of</strong> nurs<strong>in</strong>g and<br />
<strong>in</strong>form medical staff.<br />
Obta<strong>in</strong> the experience <strong>of</strong> other colleagues<br />
Obta<strong>in</strong> Paediatric <strong>Extravasation</strong> Kit<br />
5 Mark the area with a pen and take digital<br />
pictures if possible (after patient consent)<br />
To enable the size <strong>of</strong> the area to be evaluated and<br />
recalled at first presentation.<br />
7 Remove the cannula<br />
Adm<strong>in</strong>ister pa<strong>in</strong> relief as required<br />
8 Use flow sheet below and/or table<br />
(Appendix 1) to identify agent and<br />
determ<strong>in</strong>e action to be taken<br />
Ensure patient comfort<br />
To identify specific relevant <strong>in</strong>structions<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 9
Peripheral extravasation identified<br />
Stop <strong>in</strong>fusion, Leave cannula <strong>in</strong> place, Aspirate as much <strong>of</strong> the drug as possible us<strong>in</strong>g a new 10mL syr<strong>in</strong>ge, contact senior<br />
member <strong>of</strong> staff/medical staff, Mark area with pen, Remove cannula, Treat as follows:<br />
Group 1 <strong>Drugs</strong><br />
Non-vesicants/neutrals<br />
Asparag<strong>in</strong>ase, Bleomyc<strong>in</strong>, Cladrib<strong>in</strong>e,<br />
Cyclophosphamide, Cytarab<strong>in</strong>e, Fludarab<strong>in</strong>e,<br />
Ifosfamide, Melphalan, Rituximab<br />
If large volume seek advice from St. Chad’s<br />
If possible recannulate<br />
<strong>in</strong> opposite<br />
arm and recommence<br />
chemotherapy<br />
Group 2 & 3 <strong>Drugs</strong><br />
Inflammitants & Irritants<br />
Carboplat<strong>in</strong>, Cisplat<strong>in</strong>,<br />
Etoposide, Etoposide<br />
Phosphate, Ir<strong>in</strong>otecan,<br />
Methotrexate, Topotecan<br />
Draw up 100mg hydrocortisone and<br />
adm<strong>in</strong>ister S/C <strong>in</strong> a clockwise direction<br />
around circumference <strong>of</strong> the extravasation<br />
site followed by a th<strong>in</strong> layer <strong>of</strong> topical<br />
hydrocortisone 1% cream<br />
Use the relevant heat/cold pack to apply warm/cold compression<br />
Apply heat/ cold pack for one hour post <strong>in</strong>cident and then for 20 m<strong>in</strong> four times a day<br />
for 48hrs.<br />
Group 4 & 5<br />
Exfoliants and<br />
Vesicants<br />
Amsacr<strong>in</strong>e,<br />
Carmust<strong>in</strong>e<br />
Dact<strong>in</strong>omyc<strong>in</strong><br />
Daunorubic<strong>in</strong>*<br />
Doxorubic<strong>in</strong>*,<br />
Epirubic<strong>in</strong>,<br />
Idarubic<strong>in</strong><br />
Mitomyc<strong>in</strong><br />
Mitoxantrone<br />
Apply topical DMSO every 2<br />
hours at the extravasation<br />
site (DO NOT apply to<br />
healthy sk<strong>in</strong>) followed by<br />
topical hydrocortisone 1%<br />
cream. See also note below.<br />
* for Liposomal preparation<br />
delay DMSO for 8–12 hours<br />
Group 5<br />
V<strong>in</strong>ca<br />
Alkaloids<br />
V<strong>in</strong>blast<strong>in</strong>e,<br />
V<strong>in</strong>crist<strong>in</strong>e,<br />
V<strong>in</strong>des<strong>in</strong>e,<br />
V<strong>in</strong>orelb<strong>in</strong>e<br />
Dissolve 1500 units<br />
Hyaluronidase <strong>in</strong> 1mL water for<br />
<strong>in</strong>jection. Adm<strong>in</strong>ister<br />
Hyaluronidase 0.1-0.2mL S/C <strong>in</strong> a<br />
clockwise direction around<br />
circumference <strong>of</strong> the<br />
extravasation site. Gently<br />
massage area to facilitate<br />
dispersal <strong>of</strong> drug.<br />
Elevate limb for up to 48 hrs. Give prescribed analgesia & PO chlorphenam<strong>in</strong>e prn for<br />
comfort. If any concerns contact St. Chads, Birm<strong>in</strong>gham for advice (0121 5543801)<br />
Complete necessary documentation (medical notes, DATIX and green card). Ensure<br />
patient has appropriate follow up arrangements.<br />
<strong>Drugs</strong> requir<strong>in</strong>g heat pack <strong>in</strong> red, those for<br />
cold pack <strong>in</strong> blue<br />
Apply heat pack for 1 hour<br />
post & then for 20m<strong>in</strong> every<br />
4hrs for 48hrs. Apply a th<strong>in</strong><br />
layer <strong>of</strong> Hydrocortisone 1%<br />
cream and cover with 2<br />
squares <strong>of</strong> gauze and<br />
bandage <strong>in</strong>to position<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 10
DMSO (Dimethyl Sulphoxide):<br />
DMSO is stored <strong>in</strong> the chemotherapy cupboard on Sennen ward. When used or<br />
go<strong>in</strong>g out <strong>of</strong> date, please ensure the ward pharmacist is made aware so replacement<br />
supplies can be arranged.<br />
DMSO is an unlicensed medication, and as such records <strong>of</strong> its use need to be kept.<br />
When us<strong>in</strong>g DMSO please ensure that the record form is completed and returned to<br />
the ward pharmacist.<br />
DMSO should be prescribed by the medical team before giv<strong>in</strong>g, and is for<br />
EXTERNAL use only<br />
Gloves must be worn when apply<strong>in</strong>g DMSO – it may harm healthy sk<strong>in</strong>.<br />
After the first 24 hours treatment, for the next 7-14 days apply a th<strong>in</strong> layer <strong>of</strong> DSMO<br />
every 6 hours us<strong>in</strong>g a cotton bud, alternat<strong>in</strong>g with topical hydrocortisone cream every<br />
6 hours (a preparation applied every 3 hours on an alternate basis), check<strong>in</strong>g the<br />
area for erythema regularly. If blister<strong>in</strong>g occurs, stop treatment with DMSO and<br />
seek advice from St. Chad’s<br />
For liposomal preparations at 8-12 hours post <strong>in</strong>cidence apply DSMO 2-hourly for the<br />
next 24 hours, and then 4 times a day for a further 10-14 days.<br />
Do not use an occlusive cover. If required cover once the area is dry.<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 11
8. Treatment <strong>of</strong> <strong>Extravasation</strong> from Central Venous<br />
Access Devices: PICC’s, Hickman L<strong>in</strong>es & Portacaths<br />
8.1 Although less likely to occur an extravasation occurr<strong>in</strong>g from an <strong>in</strong>dwell<strong>in</strong>g<br />
central l<strong>in</strong>e can be particularly problematic because <strong>of</strong> the depth <strong>of</strong> the l<strong>in</strong>e and<br />
the potential <strong>of</strong> slower development <strong>of</strong> signs and symptoms.<br />
8.2 <strong>Extravasation</strong> can either occur <strong>in</strong> the tunnelled section or <strong>in</strong> the deep section <strong>of</strong><br />
the implanted l<strong>in</strong>e:<br />
8.3 <strong>Extravasation</strong> can occur due to fracture <strong>of</strong> the catheter, perforation <strong>of</strong> the<br />
superior vena cava, formation <strong>of</strong> a fibr<strong>in</strong> sheath on catheter or <strong>in</strong>complete<br />
placement or dislodgement <strong>of</strong> the needle.<br />
8.4 Patients should be educated to the possibility <strong>of</strong> this happen<strong>in</strong>g and that burn<strong>in</strong>g<br />
or pa<strong>in</strong> on adm<strong>in</strong>istration is not normal and should be reported immediately.<br />
8.5 Follow steps as above, leav<strong>in</strong>g the central l<strong>in</strong>e <strong>in</strong> place. The l<strong>in</strong>e should be x-ray<br />
and removed as soon as cl<strong>in</strong>ically appropriate.<br />
8.6 Referral to plastic surgeon should be made<br />
Immediate Action<br />
1 Stop the adm<strong>in</strong>istration <strong>of</strong> the cytotoxic drug<br />
immediately, leav<strong>in</strong>g the central l<strong>in</strong>e <strong>in</strong> place.<br />
Rationale<br />
To prevent further <strong>in</strong>filtration.<br />
Prompt action to m<strong>in</strong>imise damage is important.<br />
2 Expla<strong>in</strong> what has been suspected <strong>of</strong> happen<strong>in</strong>g<br />
and next procedure to the<br />
patient/parent/guardian.<br />
To obta<strong>in</strong> patient’s and/or carer’s co-operation and<br />
consent.<br />
3 Attempt to aspirate as much drug as possible<br />
with a new syr<strong>in</strong>ge.<br />
To remove any residual drug.<br />
4 Mark the area with a pen and take digital pictures<br />
if possible<br />
To enable the size <strong>of</strong> the area to be evaluated and<br />
recalled at first presentation.<br />
5 Immediately refer to a senior member <strong>of</strong> medical<br />
staff<br />
The potential for damage is much greater than with<br />
a peripheral l<strong>in</strong>e.<br />
6 Refer to plastic surgeon For specialist <strong>in</strong>put<br />
7 Complete all documentation. Green Card<br />
(available <strong>in</strong> the extravasation kit), DATIX,<br />
medical and nurs<strong>in</strong>g notes<br />
Record all actions taken (see below)<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 12
9. Mixed <strong>Extravasation</strong>s<br />
In the event <strong>of</strong> an extravasation where different agents may have been given the<br />
follow<strong>in</strong>g applies.<br />
9.1 The order <strong>of</strong> priority is vesicant, exfoliant, irritant.<br />
9.2 For drugs <strong>of</strong> different classifications apply the temperature compress <strong>of</strong> the drug<br />
that takes priority.<br />
9.3 For drugs <strong>of</strong> the same classification a cold compress takes priority over a hot<br />
compress.<br />
10. Documentation<br />
Each <strong>in</strong>cident <strong>of</strong> extravasation must be carefully recorded, with an accurate account<br />
<strong>of</strong> the event and signed by the report<strong>in</strong>g nurse.<br />
10.1 Demographic:<br />
<br />
<br />
<br />
<br />
<br />
Patient demographic details (name, address, and hospital number).<br />
Date and time <strong>of</strong> <strong>in</strong>cident.<br />
Cl<strong>in</strong>ical area<br />
Chemotherapy protocol and drug sequence.<br />
Patient’s symptoms and appearance <strong>of</strong> site.<br />
10.2 Description <strong>of</strong> IV access<br />
<br />
<br />
<br />
<br />
Needle size and type<br />
Insertion site and number <strong>of</strong> attempts,<br />
Flash back present.<br />
Drug adm<strong>in</strong>istration technique i.e. ‘bolus or <strong>in</strong>fusion’.<br />
10.3 <strong>Extravasation</strong> area<br />
<br />
<br />
<br />
<br />
Approximate amount <strong>of</strong> drug extravasated.<br />
Appearance <strong>of</strong> area<br />
Diameter, length and width <strong>of</strong> area effected<br />
Photograph, if taken.<br />
10.4 Step by step <strong>of</strong> action taken<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Amount aspirated<br />
Cold/hot applied<br />
Antidote given<br />
Nurs<strong>in</strong>g team and medical person notified.<br />
Patient’s comments, compla<strong>in</strong>ts and statements.<br />
Referrals made<br />
Patient <strong>in</strong>formation sheet given and follow up arranged<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 13
10.5 National Database<br />
• A national database <strong>of</strong> extravasation <strong>in</strong>cidents is be<strong>in</strong>g compiled by<br />
Andrew Stanley, St. Chad’s unit, Dudley road, Birm<strong>in</strong>gham. Report<strong>in</strong>g<br />
cards should be sent follow<strong>in</strong>g any extravasation and are available<br />
<strong>in</strong>side the extravasation kit. www.extravasation.org.uk<br />
11. Monitor<strong>in</strong>g compliance and effectiveness<br />
All <strong>Extravasation</strong>s will be recorded and DATIX as pre policy. An audit <strong>of</strong> these will<br />
be completed once a year and presented at the Paediatric Chemotherapy Multi<br />
Discipl<strong>in</strong>ary team meet<strong>in</strong>gs, by the author (overseen by the Trust Lead for<br />
Cancer Chemotherapy).<br />
Element to be<br />
monitored<br />
Lead<br />
Tool<br />
Frequency<br />
Report<strong>in</strong>g<br />
arrangements<br />
Act<strong>in</strong>g on<br />
recommendations<br />
and Lead(s)<br />
Change <strong>in</strong><br />
practice and<br />
lessons to be<br />
shared<br />
All chemotherapy extravasations with the child health<br />
directorate<br />
Sabr<strong>in</strong>a Tierney, Specialist Cl<strong>in</strong>ical Pharmacist<br />
(paediatrics)<br />
Audit observ<strong>in</strong>g type <strong>of</strong> drug that extravasated, cannula<br />
position, length <strong>of</strong> time cannula <strong>in</strong>, antidote<br />
Audit completed yearly<br />
Presented to Paediatric Multi-Displ<strong>in</strong>ary Team<br />
Paediatric Chemotherapy MDT lead – Nicki Gilbertson,<br />
Paediatric Consultant<br />
<strong>Extravasation</strong>s education to be provided and staff to be kept<br />
up to date with new developments <strong>in</strong> this area.<br />
All nurs<strong>in</strong>g staff to ma<strong>in</strong>ta<strong>in</strong> tra<strong>in</strong><strong>in</strong>g, <strong>in</strong>clud<strong>in</strong>g annual update<br />
day.<br />
12. Updat<strong>in</strong>g and Review<br />
12.1. This policy will be reviewed every 3 years by the Paediatric Guidel<strong>in</strong>es<br />
Committee<br />
13. Equality and Diversity<br />
13.1. This document complies with the Royal Cornwall Hospitals NHS Trust<br />
service Equality and Diversity statement.<br />
13.2. The Initial Equality Impact Assessment Screen<strong>in</strong>g Form is at Appendix 1.<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 14
Appendix 1: <strong>Drugs</strong> commonly used <strong>in</strong> Paediatric oncology<br />
and their classification<br />
(Taken from www.extravasation.org.uk)<br />
Chemotherapy agent<br />
Amsacr<strong>in</strong>e<br />
Asparag<strong>in</strong>ase<br />
Bleomyc<strong>in</strong><br />
Campath (Alemtuzumab)<br />
Carboplat<strong>in</strong><br />
Carmust<strong>in</strong>e<br />
Cisplat<strong>in</strong><br />
Cladrib<strong>in</strong>e<br />
Cyclophosphamide<br />
Cytarab<strong>in</strong>e<br />
Dact<strong>in</strong>omyc<strong>in</strong>/act<strong>in</strong>omyc<strong>in</strong> D<br />
Daunorubic<strong>in</strong><br />
Doxorubic<strong>in</strong><br />
Epirubic<strong>in</strong><br />
Etoposide<br />
Etoposide Phosphate<br />
Fludarab<strong>in</strong>e<br />
Gemcitab<strong>in</strong>e<br />
Idarubic<strong>in</strong><br />
Ifosfamide<br />
Ir<strong>in</strong>otecan<br />
Liposomal Daunorubic<strong>in</strong><br />
Liposomal Doxorubic<strong>in</strong><br />
Melphalan<br />
Methotrexate<br />
Mitomyc<strong>in</strong> C<br />
Mitozantrone<br />
Rituximab<br />
Thiotepa<br />
Topotecan<br />
V<strong>in</strong>blast<strong>in</strong>e<br />
V<strong>in</strong>crist<strong>in</strong>e<br />
V<strong>in</strong>des<strong>in</strong>e<br />
V<strong>in</strong>orelb<strong>in</strong>e<br />
Broad category<br />
Vesicant<br />
Neutral<br />
Non-vesicant/neutral<br />
Non-vesicant/neutral<br />
Irritants/<strong>in</strong>flammatants<br />
Vesicant<br />
Exfoliant. Treat as Irritants/<strong>in</strong>flammatants<br />
Non-vesicant/neutral<br />
Non-vesicant/neutral<br />
Non-vesicant/neutral<br />
Vesicant<br />
Vesicant<br />
Vesicant<br />
Vesicant<br />
Irritants/<strong>in</strong>flammatants<br />
Irritants/<strong>in</strong>flammatants<br />
Non-vesicant/neutral<br />
Non-vesicant/neutral<br />
Vesicant<br />
Non-vesicant/neutral<br />
Irritants/<strong>in</strong>flammatants<br />
Exfoliants/irritants/<strong>in</strong>flammatants. Treat as<br />
vesicant<br />
Exfoliants/irritants/<strong>in</strong>flammatants. Treat as<br />
vesicant<br />
Non-vesicant/neutral<br />
Irritants/<strong>in</strong>flammatants<br />
Vesicant<br />
Exfoliants/irritants/<strong>in</strong>flammatants. Treat as<br />
vesicant<br />
Non-vesicant/neutral<br />
Non-vesicant/neutral<br />
Exfoliants<br />
V<strong>in</strong>ca-alkaloids<br />
V<strong>in</strong>ca-alkaloids<br />
V<strong>in</strong>ca-alkaloids<br />
V<strong>in</strong>ca-alkaloids<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 15
Appendix 2: Non- <strong>Cytotoxic</strong> <strong>Extravasation</strong><br />
Determ<strong>in</strong>e which type <strong>of</strong> drug has extravasated, then us<strong>in</strong>g the table; follow the<br />
treatment procedure for that class <strong>of</strong> extravasated drug.<br />
IRRITANTS<br />
Adrenal<strong>in</strong>e<br />
(H)<br />
Amiodarone<br />
(C)<br />
Clarithromyc<strong>in</strong><br />
(C)<br />
Diazemuls<br />
(C)<br />
Dobutam<strong>in</strong>e<br />
(H)<br />
Dopam<strong>in</strong>e<br />
(H)<br />
Erythromyc<strong>in</strong><br />
(C)<br />
Foscarnet<br />
(C)<br />
Noradrenal<strong>in</strong>e<br />
(H)<br />
Phenobarbitone<br />
(C)<br />
Promethaz<strong>in</strong>e<br />
(C)<br />
Vancomyc<strong>in</strong><br />
(C)<br />
VESICANTS<br />
Aciclovir<br />
(C)<br />
Am<strong>in</strong>ophyll<strong>in</strong>e<br />
(H)<br />
Amphoteric<strong>in</strong><br />
(C)<br />
Calcium Chloride<br />
(H)<br />
Calcium Gluconate<br />
(H)<br />
Cefotaxime<br />
(C)<br />
Diazepam<br />
(C)<br />
Digox<strong>in</strong><br />
(C)<br />
Fluoresce<strong>in</strong><br />
(C)<br />
Ganciclovir<br />
(C)<br />
Hypertonic NaCl sol n > 5% (H)<br />
Phentolam<strong>in</strong>e<br />
(C)<br />
Parentral Nutrition<br />
(H)<br />
Phenyto<strong>in</strong><br />
(H)<br />
Potassium Chloride<br />
(>40mmols/l) (H)<br />
Sodium Bicarbonate<br />
(H)<br />
Ven<strong>of</strong>er<br />
(C)<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 16
Appendix 3 : <strong>Extravasation</strong> Kit Contents<br />
An <strong>Extravasation</strong> Kit is to be stored <strong>in</strong> all areas where the adm<strong>in</strong>istration <strong>of</strong><br />
cytotoxic drugs occurs. The kit conta<strong>in</strong>s all the drugs and equipment that<br />
maybe needed <strong>in</strong> the event <strong>of</strong> an extravasation. The kit should be checked<br />
regularly and re-supplied from pharmacy as required.<br />
Hyaluronidase 1500 units <strong>in</strong>jection.<br />
Chlorphenam<strong>in</strong>e 4mg tablets<br />
Hydrocortisone Sodium Phosphate <strong>in</strong>jection 100mg x 2<br />
Hydrocortisone 1% cream.<br />
Water for <strong>in</strong>jection (5ml).<br />
Heat Pad - <strong>in</strong>stant<br />
Cold Pad (<strong>in</strong> freezer on ward)<br />
2mL Syr<strong>in</strong>ges x 2<br />
19G needles x 2 (for draw<strong>in</strong>g up)<br />
25G needles x 4 (for <strong>in</strong>jection)<br />
Alcohol swabs<br />
10mL syr<strong>in</strong>ge x 1<br />
Indelible pen<br />
<strong>Extravasation</strong> policy<br />
<strong>Extravasation</strong> Report Card (Green Card)<br />
Patient <strong>in</strong>formation leaflet<br />
DMSO is not conta<strong>in</strong>ed <strong>in</strong> the kit but is available on Sennen ward, <strong>in</strong> the<br />
chemotherapy cupboard<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 17
Appendix 4 : Guidel<strong>in</strong>es for Best Practice When Adm<strong>in</strong>ister<strong>in</strong>g Intravenous Infusions<br />
Prevent<strong>in</strong>g<br />
<strong>Extravasation</strong><br />
<strong>in</strong> Infants and<br />
<strong>Children</strong> .<br />
Guidel<strong>in</strong>es<br />
for best<br />
practice.<br />
Assess the<br />
Risk<br />
Check the<br />
Site<br />
•<strong>Extravasation</strong> <strong>in</strong>jures are more common and severe <strong>in</strong> <strong>Children</strong> and Neonates.<br />
•Infants may not be able to localise or report pa<strong>in</strong>.<br />
•Confused and sedated patients are more at risk.<br />
•Does the patient have reduced sensation I.e. peripheral neuropathy.<br />
•Repeated <strong>in</strong>travenous <strong>in</strong>fusions and <strong>in</strong>jections <strong>in</strong>creases the risk. I.e. Ex premature<br />
babies who have had repeat cannulations.<br />
•Cover cannula site with designated transparent IV dress<strong>in</strong>g.<br />
•Select age appropriate dress<strong>in</strong>g. Spl<strong>in</strong>t / Tubigrip / Bandage. Do not apply too tightly.<br />
•Ensure <strong>in</strong>sertion site can be easily observed.<br />
•Check site hourly whilst <strong>in</strong>fusion is runn<strong>in</strong>g for:<br />
•Redness, Swell<strong>in</strong>g, Leak<strong>in</strong>g, Track<strong>in</strong>g, Loss <strong>of</strong> colour to limb, Pa<strong>in</strong> at site,<br />
St<strong>in</strong>g<strong>in</strong>g, Absent or sluggish blood return.<br />
•Verify patency <strong>of</strong> the site prior to the <strong>in</strong>fusion and hourly throughout. If there are any<br />
doubts STOP and INVESTIGATE. Resite the cannula if the patency <strong>of</strong> the cannulation<br />
is still not entirely satisfactory. NOTE: If extravasation suspected cannula should<br />
rema<strong>in</strong> <strong>in</strong> situe follow extravasation policy<br />
•Record location, condition <strong>of</strong> the site, verification <strong>of</strong> patency and patient responses.<br />
Report if necessary.<br />
•Parents should be asked if there are any new signs <strong>of</strong> irritability <strong>in</strong> their child dur<strong>in</strong>g<br />
<strong>in</strong>fusion.<br />
Check<br />
the<br />
Device<br />
•Check the device hourly and record: Prescribed rate, actual hourly rate, total volume <strong>in</strong>fused, pressure<br />
and alarm limits.<br />
•Check clamps, giv<strong>in</strong>g set and attachment to cannula are secure and correctly loaded <strong>in</strong>to the device.<br />
•Always check the site as well as the pump pressures. This should be done hourly. High pump<br />
pressures alone are not a reliable <strong>in</strong>dication <strong>of</strong> extravasation.<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review:<br />
•Pump pressures should be set at m<strong>in</strong>imum. Any changes should be documented and rational given.<br />
•Sign/Initial fluid chart to demonstrate checks carried out.<br />
18
Appendix 5: Patient Information Sheet<br />
UWhat is <strong>Extravasation</strong><br />
<strong>Extravasation</strong> is the leakage (or accidental <strong>in</strong>filtration) <strong>of</strong> drugs outside <strong>of</strong> the ve<strong>in</strong> and <strong>in</strong>to the<br />
surround<strong>in</strong>g tissues. With some drugs, this may lead to an immediate pa<strong>in</strong>ful reaction, and result <strong>in</strong><br />
local tissue damage.<br />
You may have noticed pa<strong>in</strong>; st<strong>in</strong>g<strong>in</strong>g, swell<strong>in</strong>g or other changes to the sk<strong>in</strong> at the site <strong>of</strong> drug<br />
adm<strong>in</strong>istration, or the nurse may have noticed that the drug was not flow<strong>in</strong>g <strong>in</strong> easily.<br />
UWhy did this happen<br />
Extrava sation is a rare but known complication <strong>of</strong> <strong>in</strong>travenous chemotherapy. It is impossible to<br />
prevent this even though we take all possible precautions. The important th<strong>in</strong>g is that it has been<br />
detected and treated.<br />
UWhy is extravasation a problem<br />
It can potentially lead to pa<strong>in</strong>, stiffness and tissue damage.<br />
UWhat treatment have I received to prevent tissue damage<br />
The nurse has given you the recommended treatment for the extravasation that you have<br />
experienced.<br />
You will have been <strong>in</strong>structed to apply either a cold or warm pack to the area for 20 m<strong>in</strong>utes, four<br />
times a day for two days.<br />
It is also advised to keep your arm elevated as much as possible.<br />
Although this will help to m<strong>in</strong>imise the chance <strong>of</strong> develop<strong>in</strong>g further problems, you will need to keep<br />
check<strong>in</strong>g the area every day.<br />
UCheck<strong>in</strong>g the area<br />
Once a day, check the area for the follow<strong>in</strong>g:<br />
• Has the area changed colour or <strong>in</strong>creased <strong>in</strong> redness<br />
• Is the area blister<strong>in</strong>g, peel<strong>in</strong>g or flak<strong>in</strong>g<br />
• Is the area more uncomfortable<br />
• Is the pa<strong>in</strong> mak<strong>in</strong>g it difficult for you to exercise the arm or hand<br />
What else do I need to do<br />
• Gently exercise the affected arm or hand.<br />
• Take mild pa<strong>in</strong>killers if required.<br />
• Do not apply any other lotions, creams or o<strong>in</strong>tments unless you have been <strong>in</strong>structed to do so by<br />
a doctor or nurse.<br />
• Do not expose the area to strong sunlight.<br />
• Avoid wear<strong>in</strong>g tight cloth<strong>in</strong>g around the affected area.<br />
• Protect the affected area when bath<strong>in</strong>g (or hav<strong>in</strong>g a shower) so that it does not get wet.<br />
When should I contact you<br />
If you answered YES to any <strong>of</strong> the questions <strong>in</strong> the checklist above, or if you have any other<br />
concerns, then you should contact Sennen ward (01872 252069)<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 19
Appendix 6 - References<br />
The National <strong>Extravasation</strong> Information Service. Protocol for <strong>Management</strong> <strong>of</strong><br />
Chemotherapy <strong>Extravasation</strong>. www.extravasation.org.uk<br />
Wendy Saegenschnitter, Vanessa McLelland (Bristol <strong>Children</strong>’s Hospital). Prescrib<strong>in</strong>g,<br />
Handl<strong>in</strong>g and Adm<strong>in</strong>istration <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> for Stem Cell Transplant and Paediatric<br />
Haematology & Oncology Patients. July 2010<br />
NOTE: This guidel<strong>in</strong>e is an adaption <strong>of</strong> the Royal Cornwall Hospitals Trust document<br />
“<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> Adults” produced by Lisa Nicholls,<br />
Cl<strong>in</strong>ical Nurse Specialist <strong>in</strong> Cancer care,<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 20
Appendix 7.Initial Equality Impact Assessment Screen<strong>in</strong>g Form<br />
Name <strong>of</strong> service, strategy, policy or project (hereafter referred to as policy) to be<br />
assessed: <strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Directorate and service area:<br />
Child Health<br />
Name <strong>of</strong> <strong>in</strong>dividual complet<strong>in</strong>g<br />
assessment: Sabr<strong>in</strong>a Tierney<br />
Is this a new or exist<strong>in</strong>g Procedure<br />
Exist<strong>in</strong>g<br />
Telephone: 01872 252590<br />
1. Procedure Aim* To provide cl<strong>in</strong>ical staff with clear guidel<strong>in</strong>es on the care <strong>of</strong><br />
patients who have experienced an extravasation<br />
2. Procedure Objectives* To provide a basis for the nurs<strong>in</strong>g care that is required for<br />
patients that have experienced an extravasation<br />
3. Procedure – <strong>in</strong>tended<br />
Outcomes*<br />
<strong>Extravasation</strong> is treated <strong>in</strong> a safe manner<br />
4. How will you measure<br />
the outcome<br />
5. Who is <strong>in</strong>tended to<br />
benefit from the<br />
Procedure<br />
6a. Is consultation<br />
required with the<br />
workforce, equality<br />
groups etc. around this<br />
procedure<br />
b. If yes, have these<br />
groups been consulted<br />
c. Please list any groups<br />
who have been consulted<br />
about this procedure.<br />
All staff <strong>in</strong>volved <strong>in</strong> the giv<strong>in</strong>g <strong>of</strong> chemotherapy<br />
Yes<br />
Yes<br />
Paediatric Oncology MDT<br />
Paediatric Guidel<strong>in</strong>es Committee<br />
*Please see Glossary<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 21
7. The Impact<br />
Please complete the follow<strong>in</strong>g table us<strong>in</strong>g ticks. You should refer to the EIA guidance<br />
notes for areas <strong>of</strong> possible impact and also the Glossary if needed.<br />
Where you th<strong>in</strong>k that the policy could have a positive impact on any <strong>of</strong> the equality<br />
group(s) like promot<strong>in</strong>g equality and equal opportunities or improv<strong>in</strong>g relations<br />
with<strong>in</strong> equality groups, tick the ‘Positive impact’ box.<br />
Where you th<strong>in</strong>k that the policy could have a negative impact on any <strong>of</strong> the equality<br />
group(s) i.e. it could disadvantage them, tick the ‘Negative impact’ box.<br />
Where you th<strong>in</strong>k that the policy has no impact on any <strong>of</strong> the equality group(s) listed<br />
below i.e. it has no effect currently on equality groups, tick the ‘No impact’ box.<br />
Equality<br />
Group<br />
Age<br />
Disability<br />
Faith and<br />
Belief<br />
Gender<br />
Race<br />
Sexual<br />
Orientation<br />
Positive<br />
Impact<br />
Negative<br />
Impact<br />
No<br />
Impact<br />
<br />
<br />
<br />
<br />
<br />
<br />
Reasons for decision<br />
Procedure available to all patients<br />
who require treatment.<br />
Procedure available to all patients<br />
who require treatment.<br />
Procedure available to all patients<br />
who require treatment.<br />
Procedure available to all patients<br />
who require treatment.<br />
Procedure available to all patients<br />
who require treatment.<br />
Procedure available to all patients<br />
who require treatment.<br />
You will need to cont<strong>in</strong>ue to a full Equality Impact Assessment if the follow<strong>in</strong>g have<br />
been highlighted:<br />
A negative impact and<br />
No consultation (this excludes any policies which have been identified as not<br />
requir<strong>in</strong>g consultation).<br />
8. If there is no evidence that<br />
the policy promotes equality,<br />
equal opportunities or improved<br />
relations - could it be adapted<br />
so that it does How<br />
Full statement <strong>of</strong> commitment to policy <strong>of</strong><br />
equal opportunities is <strong>in</strong>cluded <strong>in</strong> the policy<br />
Please sign and date this form.<br />
Keep one copy and send a copy to the Human Resources Team, c/o<br />
Royal Cornwall Hospitals NHS Trust, Human Resources Department, Lamorna House,<br />
Penvent<strong>in</strong>nie Lane, Truro, Cornwall, TR1 3LJ<br />
They will<br />
arrange for a summary <strong>of</strong> the results to be published on the Trust’s web site.<br />
Signed ________________________________________<br />
Date _________________________________________<br />
<strong>Management</strong> <strong>of</strong> <strong>Extravasation</strong> <strong>of</strong> <strong>Cytotoxic</strong> <strong>Drugs</strong> <strong>in</strong> <strong>Children</strong><br />
Ratified: Review: 22