Artificial Insemination
Artificial Insemination
Artificial Insemination
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Ch36-A03309.qxd 1/23/07 5:16 PM Page 539<br />
Section 6 Infertility and Recurrent Pregnancy Loss<br />
Chapter<br />
36<br />
<strong>Artificial</strong> <strong>Insemination</strong><br />
Ashok Agarwal and Shyam S. R. Allamaneni<br />
INTRODUCTION<br />
<strong>Artificial</strong> insemination is an assisted conception method that can<br />
be used to alleviate infertility in selected couples. The rationale<br />
behind the use of artificial insemination is to increase the gamete<br />
density near the site of fertilization. 1 The effectiveness of artificial<br />
insemination has been clearly established in specific subsets of<br />
infertile patients such as those with idiopathic infertility, infertility<br />
related to a cervical factor, or a mild male factor infertility<br />
(Table 36-1). 2,3 An accepted advantage of artificial insemination<br />
is that it is generally less expensive and invasive than other<br />
assisted reproductive technology (ART) procedures. 4<br />
This chapter provides a comprehensive description of<br />
indications for artificial insemination, issues to consider before<br />
donor insemination, complications associated with intrauterine<br />
insemination (IUI), factors affecting the success of artificial<br />
insemination, and the current evidence available on effectiveness<br />
of artificial insemination for different indications.<br />
HISTORY<br />
<strong>Artificial</strong> insemination has been used in clinical medicine for<br />
more than 200 years for the treatment of infertile couples. In<br />
1785 John Hunter, a Scottish surgeon from London, advised a<br />
man with hypospadias to collect his semen and have his wife<br />
inject it into her vagina. This was the first documented case of<br />
successful artificial insemination in a human.<br />
In the second half of the nineteenth century, numerous reports<br />
were published of human artificial insemination in France, England,<br />
Germany, and the United States. In 1909, the first account of<br />
successful donor artificial insemination was published in the<br />
United States. By 1949, improved methods of freezing and<br />
thawing sperm were being reported.<br />
Today, artificial insemination is frequently used in the treatment<br />
of couples with various causes of infertility, including ovulatory<br />
dysfunction, cervical factor infertility, and unexplained infertility<br />
as well as those with infertility caused by endometriosis, male,<br />
and immunologic factors. <strong>Artificial</strong> insemination with donor semen<br />
has become a well-accepted method of conception.<br />
GENERAL CONSIDERATIONS<br />
Semen Sources<br />
The source of semen for artificial insemination can be either<br />
from the woman’s male partner or from a donor, who usually<br />
remains anonymous. When donor insemination first became<br />
widely available, the terms homologous artificial insemination<br />
and heterologous artificial insemination were used to differentiate<br />
these two alternative sources. However, the use of these biomedical<br />
terms in this manner is at variance with their scientific<br />
meaning, where they denote different species or organisms (as in,<br />
e.g., homologous and heterologous tissue grafts).<br />
In the latter half of the 20th century, the terms artificial<br />
insemination, donor (AID) and artificial insemination, husband<br />
(AIH) found common use. However, the widespread use of the<br />
acronym AIDS for acquired immunodeficiency syndrome resulted<br />
in the replacement of AID with therapeutic donor insemination<br />
(TDI). An analogous alternative term for AIH has not evolved,<br />
probably in part because of the increasingly common situation<br />
where the woman’s partner is not her legal husband. In this chapter,<br />
artificial insemination using these two standard sperm sources<br />
will be designated simply as partner and donor insemination.<br />
Techniques<br />
Several different techniques have been used for artificial<br />
insemination. The original technique used for over a century was<br />
intravaginal insemination, where an unprocessed semen sample<br />
is placed high in the vagina.<br />
In the latter half of the 20th century, the cervical cap was<br />
developed to maintain the highest concentration of semen at the<br />
external os of the cervix. It was soon discovered that placing the<br />
semen sample into the endocervix (intracervical insemination)<br />
resulted in pregnancy rates similar to that obtainable using a cervical<br />
cap and superior to those seen with high vaginal insemination. 5<br />
Intrauterine Versus Intracervical <strong>Insemination</strong><br />
A major breakthrough came in the 1960s when methods were<br />
developed for extracting enriched samples of motile sperm from<br />
semen. These purified samples were free of proteins and prostaglandins,<br />
and thus could be placed within the uterus using a<br />
technique designated intrauterine insemination (IUI). This<br />
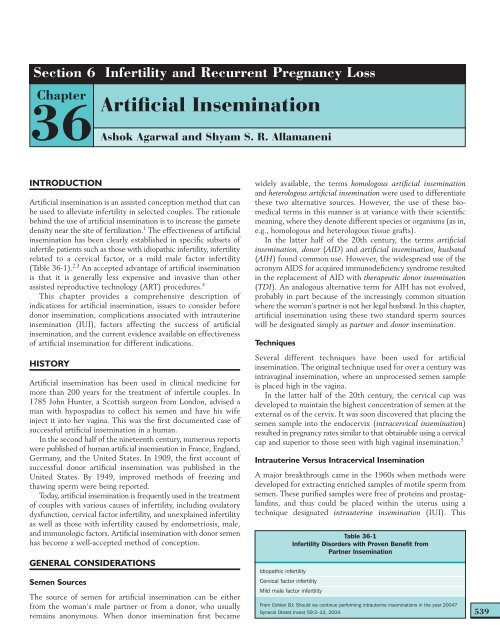
Table 36-1<br />
Infertility Disorders with Proven Benefit from<br />
Partner <strong>Insemination</strong><br />
Idiopathic infertility<br />
Cervical factor infertility<br />
Mild male factor infertility<br />
From Cohlen BJ: Should we continue performing intrauterine inseminations in the year 2004<br />
Gynecol Obstet Invest 59:3–13, 2004.<br />
539
Ch36-A03309.qxd 1/23/07 5:16 PM Page 540<br />
Section 6<br />
Infertility and Recurrent Pregnancy Loss<br />
540<br />
technique was found to result in pregnancy rates 2 to 3 times<br />
those of intracervical insemination. However, intracervical<br />
insemination is still utilized in some practices. 5<br />
In an effort to further improve pregnancy rates, techniques<br />
were developed to place washed sperm samples directly into the<br />
tubes via transcerival cannulation (intratubal insemination) or<br />
into the peritoneal cavity via a needle placed through the posterior<br />
cul-de-sac (intraperitoneal insemination). Another technique<br />
developed in Europe, termed fallopian tube sperm perfusion,<br />
involves pressure injection of a large volume (4 mL) of washed<br />
sperm sample while the cervix is sealed to prevent reflux of the<br />
sample. 6 This technique appears to have a higher pregnancy rate<br />
than IUI in couples with unexplained infertility. The remainder<br />
of these technically difficult approaches have never been shown<br />
to result in better pregnancy rates than IUI. One prospective,<br />
randomized study found that simultaneous intratubal insemination<br />
actually decreased the pregnancy rates associated with IUI. 7<br />
In modern clinical practice in the United States, IUI is the<br />
predominant technique used for artificial insemination.<br />
EVALUATION<br />
Male Evaluation<br />
Semen Analysis<br />
The male partner is initially evaluated by obtaining a complete<br />
semen analysis and screen for sperm antibodies. A minimum of<br />
two samples provided over 1 to 2 months is analyzed. A third<br />
sample may be required if there is a discrepancy between<br />
the initial samples. All samples should be provided after 48 to<br />
72 hours of sexual abstinence. Samples should be analyzed within<br />
2 hours of collection.<br />
Antisperm Antibodies<br />
Male antisperm antibodies are found in approximately 10% of<br />
semen samples from infertile couples. Men with antisperm antibodies<br />
attached to their sperm are classified as having immunologic<br />
infertility. These antibodies are believed to decrease fertility by<br />
inducing agglutination or immobilization of the sperm. Studies<br />
have identified multiple antisperm antibodies that correspond to<br />
a variety of sperm components.<br />
There are multiple known risk factors for the development of<br />
male antisperm antibodies. 8 Vasectomy results in the development<br />
of antisperm antibodies in the majority of men. After successful<br />
vasovasostomy, more than half of these men will have detectable<br />
sperm-bound antibodies. The pregnancy rates will depend on<br />
many factors, including the titer and quantity of gross agglutination.<br />
Obstructive azospermia from any cause (e.g., congenital absence<br />
of the vas deferens, cystic fibrosis, infant hernia repair) increases<br />
the risk of antisperm antibodies. Reproductive infections (e.g.,<br />
epididymitis, prostatitis, or orchitis) are also associated with<br />
antisperm antibodies.<br />
Antisperm antibody tests are performed as a routine part of<br />
a complete semen analysis during the initial infertility evaluation.<br />
The most commonly used test in clinical practice is probably the<br />
immunobead assay. 8 This quantitative assay evaluates live sperm<br />
and indicates percent bound, antibody isotype, and binding<br />
location. For routine screening, some andrology laboratories<br />
use a commercially available mixed antiglobulin reaction assay<br />
(SpermMar).<br />
Male subfertility is significantly increased when the antisperm<br />
antibody level is greater than 50%. 9,10 Antisperm antibodies<br />
interfere with sperm–zona pellucida binding and prevent embryo<br />
cleavage and early development.<br />
Complete Evaluation<br />
In the presence of persistently abnormal results on semen<br />
analysis, a complete history, physical examination, and laboratory<br />
evaluation is performed to find and treat any potentially reversible<br />
abnormalities (see Chapter 35).<br />
Female Evaluation<br />
The female partner should undergo a basic infertility evaluation<br />
so that any correctable factors can be identified and treated<br />
before artificial insemination (see Chapter 34). In addition to a<br />
detailed history and physical examination, each woman considering<br />
partner or donor insemination should be evaluated with<br />
an imaging technique, usually a hysterosalpingogram, to document<br />
patent tubes. Unless oral or injectable medications are used to<br />
induce superovulation, ovulatory function should be evaluated<br />
with a urinary luteinizing hormone (LH) detection kit and midluteal<br />
serum progesterone level. Further evaluation is required<br />
in the event of detection of any clinical or laboratory abnormalities.<br />
In the past, a great deal of time was spent investigating the<br />
possibility of cervical factor infertility by evaluating the character<br />
and sperm survivability in periovulatory cervical mucus, using<br />
what is termed a postcoital test. This test had many false-positive<br />
results, because it depended more on timing in the cycle and<br />
hormonal status than on static cervical characteristics. Except<br />
for exclusion of cervicitis during pelvic examination, timed<br />
evaluation of cervical mucus and sperm interaction is infrequently<br />
included in a fertility examination. This is because partner IUI<br />
is used as a basic fertility enhancement method for the majority<br />
of couples who have otherwise been unable to conceive regardless<br />
of diagnosis.<br />
INDICATIONS<br />
Partner <strong>Insemination</strong><br />
Partner insemination was originally developed as a treatment for<br />
male factor infertility. With the advent of IUI, partner insemination<br />
has been found to be an excellent treatment for a range of diagnoses,<br />
including cervical factor infertility, unexplained infertility,<br />
and subfertility, on the basis of other diagnoses or therapeutic<br />
measures (Table 36-2). This ability of partner insemination to<br />
increase pregnancy rates regardless of diagnosis has made this<br />
technique one of the fundamental approaches to infertility<br />
treatment today.<br />
Male Factor Infertility<br />
Partner insemination appears to be of clear benefit when the<br />
couple’s infertility is the result of any condition that makes it<br />
difficult to place semen high in the vagina during coitus. Male<br />
conditions resulting in this situation are termed ejaculatory failure.<br />
The most common causes of ejaculatory failure are impotence,<br />
severe hypospadias, and retrograde ejaculation. A unique condition<br />
that has been found to be treatable with artificial insemination<br />
is impotence secondary to spinal cord injury. 11
Ch36-A03309.qxd 1/23/07 5:16 PM Page 541<br />
Chapter 36<br />
<strong>Artificial</strong> <strong>Insemination</strong><br />
Table 36-2<br />
Indications and Contraindications for Partner <strong>Insemination</strong><br />
Indications<br />
Male Factor Infertility<br />
Disorders of semen density, motility,<br />
and morphology (mild oligospermia,<br />
asthenozoospermia,<br />
teratozoospermia)<br />
Immunologic factors<br />
Ejaculatory failure<br />
Mechanical factors (malformed<br />
urethra, hypospadias)<br />
Female Factor Infertility<br />
Cervical factor<br />
Vaginismus<br />
Mild endometriosis<br />
Ovulatory dysfunction<br />
Unexplained Fertility<br />
Contraindications<br />
Absolute Contraindications<br />
Rh blood factor incompatibility<br />
Medical conditions that could endanger<br />
the patient’s life<br />
A partner with hereditable disease<br />
Cervical neoplasia<br />
Blocked tubes<br />
Active genital tract infection in either<br />
partner<br />
Relative Contraindications<br />
Severely abnormal semen parameters<br />
Multiple failures at previous partner<br />
insemination attempts<br />
Recent chemotherapy or radiotherapy<br />
Coexisting multiple infertility etiologies<br />
Pelvic surgery<br />
Older age woman<br />
An Adjunct to Other Infertility Treatments<br />
Partner IUI appears to be of value for increasing per cycle fecundity<br />
when inducing ovulation in women with ovulatory dysfunction. 13<br />
After ovulation induction with clomiphene citrate, partner IUI<br />
might work by overcoming the decreased cervical mucus<br />
associated with the use of clomiphene. 14 With gonadotropins,<br />
partner IUI might compensate for subtle changes in sperm transport<br />
within the uterus or tubes related to marked alterations<br />
in circulating estrogen and progesterone levels associated with<br />
their use.<br />
Partner IUI also appears to be of some benefit when women<br />
with mild and minimal endometriosis are trying to achieve pregnancy.<br />
After appropriate surgical treatment, the monthly improvement<br />
in fecundity with partner IUI appears to be similar to that<br />
seen in patients with idiopathic infertility. 15<br />
Women with severe endometriosis or tubal disease have a far<br />
lower fecundity rate and often an increased rate of ectopic pregnancies.<br />
For this reason, these patients appear to benefit more<br />
from IVF than from partner IUI combined with superovulation.<br />
Partner insemination is also commonly used as a treatment<br />
for male factor infertility documented by repeated abnormal<br />
results on semen analysis. In couples where there is mild male<br />
factor infertility, defined as a progressive sperm motility of at<br />
least 20% to 30%, the prognosis appears to be good with partner<br />
insemination. Theoretically, increasing the number of motile<br />
sperm reaching the egg should improve fertility whenever<br />
decreased numbers and motility of normally functioning sperm<br />
is the primary problem.<br />
Unfortunately, the pregnancy rates after partner IUI for the<br />
treatment of severe male factor infertility have been disappointing.<br />
12 This is probably because markedly abnormal<br />
parameters on routine semen analysis often reflect a sperm defect<br />
that decreases the ability to fertilize eggs. This type of defect is<br />
unlikely to be overcome by increasing the number of sperm to<br />
which the egg is exposed at the site of fertilization. In patients<br />
with severely abnormal parameters on semen analysis and those<br />
with male factor infertility not amenable to partner insemination,<br />
more effective treatment will be either donor insemination or<br />
in vitro fertilization (IVF) with intracytoplasmic sperm injection<br />
(ICSI).<br />
Female Factor Infertility<br />
Female reproductive conditions can also make it difficult to<br />
place semen high in the vagina during coitus. Such conditions that<br />
can benefit from partner insemination include severe vaginismus<br />
and other psychological problems, and less common anatomic<br />
conditions. Little data exists documenting the success of partner<br />
insemination for these conditions.<br />
Women with cervical factor infertility will benefit from IUI,<br />
because this approach bypasses the cervical abnormalities that<br />
decrease fertility. This includes women with abnormal cervical<br />
mucus secondary to noninfectious chronic cervicitis and women<br />
with scant mucus or cervical stenosis, usually the result of<br />
cervical surgery. However, even women with a normal cervix<br />
and mucus appear to benefit from IUI, because the cervix<br />
appears to be the limiting factor in sperm reaching the site of<br />
fertilization in the tube.<br />
Unexplained Infertility<br />
Unexplained (i.e., idiopathic) infertility is diagnosed after all<br />
known etiologies of infertility have been excluded. In these cases,<br />
semen analyses are normal and there is no evidence of any female<br />
causes of infertility, such as ovulation defects, tubal factor,<br />
endometriosis, and cervical factor. The average incidence of<br />
unexplained infertility is approximately 15% among infertile<br />
couples.<br />
In couples with unexplained infertility, partner IUI has been<br />
demonstrated to improve pregnancy rates when used in conjunction<br />
with superovulation. 13 In a meta-analysis of almost<br />
1000 superovulation cycles for unexplained infertility, partner<br />
IUI was found to almost double pregnancy rates (20%) compared<br />
to timed intercourse alone (11%).<br />
Partner IUI appears to overcome one or more unknown fertility<br />
deficiencies that we cannot currently detect. Theoretically, this<br />
might be decreased sperm transport from the vagina to the tube<br />
secondary to either a sperm defect or an abnormality in sperm<br />
transport mechanisms in the female reproductive tract. In other<br />
cases, a subtle sperm fertilization defect might exist that is surmounted<br />
by increasing the absolute number of sperm reaching<br />
the egg.<br />
Donor <strong>Insemination</strong><br />
In the past, the only available options for couples with severe male<br />
factor infertility (e.g., severe oligospermia, or failure to conceive<br />
using partner insemination) desiring children were either donor<br />
insemination or adoption. Since the widespread availability of<br />
IVF using ICSI, many couples with severe male factor infertility<br />
have chosen to procreate their own genetic children using these<br />
techniques. However, donor insemination remains an option<br />
when IVF/ICSI has been unsuccessful. Alternatively, many<br />
candidates for IVF/ICSI initially choose donor insemination<br />
because it is less invasive and ultimately more likely to achieve<br />
pregnancy for couples with limited resources.<br />
Some women choose donor insemination because they are<br />
not candidates for IVF/ICSI. Perhaps the most obvious situation<br />
is women without male partners who seek pregnancy. The use<br />
of donor insemination is also indicated when the male partner<br />
541
Ch36-A03309.qxd 1/23/07 5:16 PM Page 542<br />
Section 6<br />
Infertility and Recurrent Pregnancy Loss<br />
542<br />
has no viable sperm (i.e., azoospermia) or when IVF/ICSI fails<br />
to achieve fertilization. Finally, men with a known genetic<br />
disorder often choose donor insemination to avoid transmission<br />
to their children.<br />
Donor Selection<br />
Couples choose a donor from profiles of nonidentifiable<br />
information. This information usually includes racial or ethnic<br />
background, blood type, physical characteristics, and certain<br />
social characteristics. Many women who become pregnant as a<br />
result of donor insemination desire to use the same donor for<br />
further pregnancies.<br />
Donor Evaluation<br />
Thorough evaluation of all potential sperm donors (other than<br />
sexually intimate partners) is necessary to avoid inadvertent<br />
transmission of sexually transmitted diseases or known genetic<br />
syndromes. 16 All donors undergo a review of relevant medical<br />
records, personal and family history, and a physical examination.<br />
Determination of normal semen characteristics is extremely<br />
important. In addition, blood grouping and karyotyping is<br />
performed.<br />
Each donor must be screened for risk factors and clinical<br />
evidence of communicable diseases, including:<br />
● human immunodeficiency virus types 1 and 2<br />
● human T-lymphotropic virus types I and II<br />
● hepatitis B and C<br />
● cytomegalovirus<br />
● human transmissible spongiform encephalopathy (including<br />
Creutzfeldt-Jakob disease)<br />
● Treponema pallidum<br />
● Chlamydia trachomatis<br />
● Neisseria gonorrheae<br />
If the donor is deemed acceptable and is aware of the ethical<br />
and legal implications, semen can be collected. All donor semen<br />
samples are cryopreserved and quarantined for 6 months. Before<br />
a donor sample is used for insemination, the donor is retested<br />
and determined if eligible.<br />
Success Rate<br />
The actual per cycle fecundity rate with donor IUI is dependent<br />
on multiple factors. A meta-analysis of seven studies demonstrated<br />
that IUI yielded a higher pregnancy rate per cycle<br />
than intracervical insemination with donor frozen sperm. 17<br />
Overall, the average live birth rate per cycle of donor IUI is<br />
approximately 10%. 18<br />
IUI TIMING, COST, AND FREQUENCY<br />
Timing<br />
Timing of insemination in relationship to ovulation is one of the<br />
crucial factors in the success of IUI. Although viable sperm<br />
remain in the female reproductive tract for up to 120 hours<br />
after coitus, the best pregnancy rates are obtained when IUI is<br />
performed as close as possible to ovulation. 19,20<br />
In the past, IUI was performed on the estimated day of<br />
ovulation based on basal body temperature rises during previous<br />
cycles. However, to optimize fecundity, modern prospective<br />
timing strategies are based on either detection of a urinary LH<br />
surge or administration of an ultrasound-timed dose of human<br />
chorionic gonadotropin (hCG ) to trigger ovulation.<br />
LH Surge<br />
A commonly used method for timing of IUI is based on urinary<br />
LH measurement. Ovulation occurs 40 to 45 hours after the<br />
onset of the LH surge. 21 <strong>Insemination</strong> is thus planned for the<br />
day after detection of a rise in urinary LH. This approach offers<br />
the simplest and most cost-effective of the indirect methods<br />
for predicting ovulation and is just as effective in achieving<br />
pregnancy as more complex ones. 22,23<br />
Ultrasound and Human Chorionic Gonadotropin<br />
Transvaginal ultrasonography is widely used to monitor the size<br />
of the follicles and to assess the timing of ovulation. Follicles<br />
become recognizable once they grow to 2 to 3 mm in diameter.<br />
After 8 mm, linear follicular growth occurs at a rate of approximately<br />
2 to 3 mm per day. Ovulation occurs during a natural<br />
cycle when the lead follicle reaches 15 to 24 mm in size.<br />
Injection of hCG can be given to induce predictable ovulation<br />
when at least one follicle diameter is between 17 and 21 mm.<br />
For optimal pregnancy rates, IUI is scheduled 24 to 36 hours<br />
after the injection.<br />
IUI Cost<br />
The cost-effectiveness of the treatment is an important consideration<br />
when deciding on the most appropriate infertility<br />
treatment option. 24 The cost of insemination varies from clinic<br />
to clinic, but is presently less than $500 per IUI, including sperm<br />
preparation and injection of the prepared sample. This compares<br />
favorably with the cost of other appropriate ART approaches.<br />
Even when the cost of ovulation induction medication and<br />
monitoring are included, the cost per live birth for IUI after<br />
superovulation has been calculated to be less than half the cost<br />
of IVF treatment. 25<br />
IUI Frequency<br />
It is recommended that IUI be performed either one or two<br />
times during each cycle. Performing two inseminations per cycle<br />
is likely to be especially advantageous when timing in relationship<br />
to ovulation is less precise. Although it seems intuitive that<br />
fecundity should be increased by two inseminations per cycle, it<br />
remains inconclusive whether the increased fecundity is worth<br />
doubling the patients’ cost and inconvenience compared to one<br />
insemination per cycle. 26–30 A recent meta-analysis of more than<br />
1000 IUI cycles revealed a slightly higher but statistically<br />
insignificant difference between the per cycle fecundity rate for<br />
two inseminations (14.9%) compared to one insemination per<br />
cycle (11.4%). 31 Accordingly, one well-timed insemination appears<br />
to offer the best balance between efficacy and cost.<br />
SPERM PREPARATION FOR IUI<br />
Sperm preparation methods are used to process semen samples<br />
such that viable sperm are separated from seminal plasma. This<br />
is necessary before IUI to avoid the consequences of intrauterine<br />
injecting of semen plasma proteins and prostaglandins. 32<br />
Although seminal plasma protects the spermatozoa from stressful
Ch36-A03309.qxd 1/23/07 5:16 PM Page 543<br />
Chapter 36<br />
<strong>Artificial</strong> <strong>Insemination</strong><br />
Table 36-3<br />
Common Techniques Used for Sperm Preparation Prior to<br />
Intrauterine <strong>Insemination</strong><br />
Washing<br />
Swim-up techniques<br />
Swim-up from pellet<br />
Swim-up from ejaculate<br />
Swim-up from ejaculate into hyaluronic acid<br />
Density gradient centrifugation<br />
Glass wool filtration<br />
Mechanical aids<br />
conditions such as oxidative stress, 33 it also contains factors that<br />
inhibit the fertilizing ability of the spermatozoa and reduce the<br />
induction of capacitation. 34,35 Sperm preparation involves removing<br />
the seminal plasma efficiently and quickly and eliminating dead<br />
sperm, leukocytes, immature germ cells, epithelial cells, and<br />
microbial contamination. Several methods for sperm preparation<br />
are currently used (Table 36-3).<br />
The ideal sperm preparation method recovers highly functional<br />
spermatozoa and enhances sperm quality and function without<br />
inducing damage. It is also cost-effective and allows for the<br />
processing of a large volume of the ejaculate, which in turn<br />
maximizes the number of spermatozoa that are available. 36 The<br />
ideal sperm preparation method minimizes the risk of reactive<br />
oxygen species generation, which can adversely affect DNA<br />
integrity and sperm function in vitro. 33,37 Several preparation<br />
methods incorporate methylxanthines and pentoxifyllines to<br />
increase sperm motility and improve the fertilization outcome.<br />
The first step in sperm preparation is the performance of a<br />
semen analysis according to the World Health Organization<br />
(WHO) standards to determine the prewash quality of the<br />
sample. Throughout the semen analysis and preparation, it is<br />
important to use sterile technique and media both to minimize<br />
the risk of iatrogenic intrauterine infection and because sperm<br />
can be damaged by bacterial contamination.<br />
Swim-up Techniques<br />
Swim-up techniques are based on active self-migration of motile<br />
spermatozoa into the washing medium. Allowing sperm to swim<br />
up from ejaculate avoids the need for centrifugation, which can<br />
lead to oxidative damage of the sperm. However, this technique<br />
can be used only for ejaculate with a high degree of progressive<br />
motile spermatozoa, because the percentage of motile sperm<br />
recovered depends on sperm motility.<br />
For the swim-up technique, a layer of wash media is gently<br />
layered over the semen sample. The sample is incubated so that<br />
the motile sperm can swim out of the semen sample into the<br />
media. The media is then carefully removed from the semen<br />
fluid and used for IUI. If the initial semen sample has normal<br />
sperm parameters, recovery of reasonable number of sperm with at<br />
least 90% motility is common. The entire procedure takes 2 hours.<br />
Basic Sperm Washing<br />
Sperm washing, the oldest and perhaps the simplest technique,<br />
removes the seminal fluid with little enrichment of motile sperm.<br />
The semen sample is diluted in a sperm wash media containing<br />
antibiotics and protein supplements in a conical centrifuge tube.<br />
The specimen is centrifuged such that all cells congregate in a<br />
pellet, and the supernatant wash solution is carefully removed.<br />
The pellet is resuspended in wash media, and the centrifugation<br />
is repeated. The final pellet, from which all seminal fluid has<br />
been eliminated, is resuspended in a small volume of wash media<br />
for IUI. The entire procedure takes less than an hour.<br />
Density Gradient Centrifugation<br />
The density gradient method is a sperm washing method that<br />
both removes semen fluid and separates living sperm from other<br />
material, including dead sperm cells, white blood cells, and<br />
bacteria. For this method, a density gradient is prepared by<br />
layering suspensions of different concentrations of coated colloidal<br />
silica particles (e.g., Percoll) in a conical centrifuge tube, with<br />
the higher concentrations more superior. The liquefied semen<br />
sample is placed over the upper layer and the tube is centrifuged.<br />
The supernatant is removed from the pellet, and the process is<br />
repeated. The final pellet is resuspended in wash media and used<br />
for IUI. Density gradient sperm washes take approximately 1 hour.<br />
Glass Wool Filtration<br />
The glass wool filtration method is another method for removing<br />
seminal fluid and separating living sperm from other cellular<br />
material after sperm has been washed. For this technique, the<br />
semen samples are first diluted with wash media and centrifuged<br />
in a manner similar to sperm washing. The resulting pellet is<br />
resuspended in wash media and placed on glass wool columns,<br />
created by inserting glass wool into the barrel of a 3-mL syringe.<br />
The washed sperm solution is allowed to filter through the<br />
column by gravity, and the filtrate is collected for IUI.<br />
Which Preparation Method is the Best<br />
Presently, there is no general consensus as to the best sperm<br />
preparation technique for IUI. In general, swim-up, simple sperm<br />
washing, density gradient centrifugation, and glass wool filtration<br />
methods all effectively produce adequate sperm samples. However,<br />
some preparation techniques appear better suited for<br />
particular types of samples; thus, the technique chosen should<br />
be tailored to individual samples.<br />
The preparation techniques most commonly used today are<br />
the double density gradient centrifugation and the glass wool<br />
filtration sperm washing techniques. These techniques have<br />
been shown to improve the number of morphologic normal<br />
spermatozoa with grade A motility and with normal chromatin<br />
condensation in the prepared sample. 38–40 In addition, these<br />
techniques best reduce the amount of reactive oxygen species<br />
and leukocytes in the prepared sample and provide spermatozoa<br />
with minimal chromatin and nuclear DNA anomalies and high<br />
nuclear maturity rates.<br />
For semen samples with normal or near-normal sperm parameters,<br />
one study has shown that swim-up and density gradient<br />
techniques result in higher pregnancy rates compared to the<br />
washing, swim-down, and refrigeration/heparin techniques. 41<br />
For poor samples, the density gradient centrifugation and glass<br />
wool filtration techniques appear to be superior. In cases of very<br />
low sperm counts, simple sperm washing will recover the highest<br />
number of sperm, both motile and nonmotile.<br />
543
Ch36-A03309.qxd 1/23/07 5:16 PM Page 544<br />
Section 6<br />
Infertility and Recurrent Pregnancy Loss<br />
A<br />
curved tip is directed in a new course and re-advanced. This<br />
procedure is continued until the catheter can be advanced<br />
without resistance approximately 5 to 6 cm into the uterine<br />
cavity. Rarely, a cervical tenaculum is required to apply downward<br />
traction on the cervix to “straighten” an exceptionally<br />
tortuous canal.<br />
A second method for navigation of the endocervical canal for<br />
IUI is by using a semirigid yet flexible catheter that has no<br />
memory. 42 Pressure is used to force the catheter to follow the<br />
course of the canal. This technique often requires the use of a<br />
cervical tenaculum to apply countertraction. Because the diameter<br />
of some of these types of catheters is usually larger in caliber<br />
(greater than 3 mm), dilatation is sometimes required in the<br />
presence of cervical stenosis.<br />
544<br />
B<br />
Figure 36-1 Intrauterine insemination catheters: A, Tefcat catheter<br />
attached to a syringe (Cook Group, Bloomington, Ind.); B, CryoBioSystem<br />
catheter (CryoBioSystem, Paris).<br />
IUI TECHNIQUE<br />
IUI is performed using one of several commercially available<br />
intrauterine insemination catheters connected to a 2-mL syringe<br />
(Fig. 36-1). With the fully awake patient in a dorsal lithotomy<br />
position, the cervix is visualized with a bivalve vaginal speculum.<br />
After excess vaginal secretions are wiped from the external<br />
cervical os, the tip of a thin flexible catheter is passed into the<br />
uterine cavity, and the sperm sample, suspended in less than 1 mL<br />
of wash media, is gently expelled high in the uterine cavity.<br />
Increased resistance during injection suggests that the catheter<br />
is kinked or the tip might be inadvertently lodged in the endometrium<br />
or tubal ostia. In this situation, the catheter should be<br />
withdrawn 1 cm, and injection reattempted. After IUI, the<br />
catheter is slowly removed and the patient allowed to remain<br />
supine for 10 minutes after insemination in case she experiences<br />
a vasovagal reaction.<br />
Occasionally, there is difficulty navigating the often tortuous<br />
course of the endocervical canal with the tip of the insemination<br />
catheter. There are two common approaches to this blind<br />
procedure. Most commonly, a thin catheter (external diameter<br />
less than 2 mm) with a “memory” is used so that the tip can be<br />
bent 20 to 90 degrees , thus allowing angular navigation in<br />
any direction by carefully twisting the catheter as it is gently<br />
advanced. Resistance in any direction requires that the catheter<br />
tip be withdrawn a matter of millimeters, twisted such that the<br />
FACTORS THAT PREDICT PREGNANCY RATES<br />
The highest pregnancy rates with IUI are seen within three to<br />
four cycles. 43 The average live birth rate per cycle is approximately<br />
10%. 18 Cumulative pregnancy rates depend on the characteristics<br />
of the couples being treated. In most reports, the<br />
cumulative pregnancy rate reaches plateau after three to six cycles.<br />
It is difficult to predict with certainty whether pregnancy will<br />
occur. Several models have been proposed but have not been<br />
validated. 44,45<br />
Male Factors That Predict IUI Success<br />
Men who have normal seminal characteristics have a higher<br />
chance of initiating a successful pregnancy as a result of IUI than<br />
those with abnormal results on semen analysis. This association<br />
is probably related to two associated factors. First, an abnormal<br />
semen analysis is often associated with an impaired fertilization<br />
capacity. Secondly, pregnancy rates positively correlate with the<br />
total number of motile sperm recovered for IUI, and this number<br />
is often lower in men with abnormal results on semen analysis.<br />
Semen Analysis Characteristics<br />
Semen characteristics clearly affect IUI outcome. 46 IUI is a<br />
successful treatment for mild male factor infertility, defined as a<br />
total motile sperm count of more than 5 million and Kruger<br />
morphology of more than 5%. 47 In a study in patients with mild<br />
male factor infertility, a live birth rate of 19% per cycle was<br />
reported. 47<br />
When prepreparation semen analyses characteristics are<br />
evaluated, the chances of pregnancy after IUI correlate best with<br />
morphology. A meta-analysis of six studies using strict morphology<br />
criteria (Kruger) showed that when the prewashed semen<br />
specimen had more than 4% normal sperm morphology, the<br />
chances of pregnancy after IUI were significantly increased. 48<br />
If the WHO standards were used to evaluate sperm morphology,<br />
the presence of more than 30% abnormal sperm in the ejaculate<br />
adversely influenced the pregnancy rate. 49<br />
Total Motile Sperm Count<br />
The sperm variable most clearly associated with pregnancy rates<br />
after IUI is the total motile sperm count after sperm wash or<br />
swim-up. In a retrospective study of 9963 IUI cycles, the likelihood<br />
of subsequent pregnancy was maximized when the IUI<br />
sample contained more than 4 million motile sperm numbers
Ch36-A03309.qxd 1/23/07 5:16 PM Page 545<br />
Chapter 36<br />
<strong>Artificial</strong> <strong>Insemination</strong><br />
and sperm motility was greater than 60%. 50 Total motile sperm<br />
count was reported to affect IUI outcome in 1115 cycles in 332<br />
infertile couples. 51 No pregnancy occurred in cases where the<br />
total motile sperm count before semen preparation was less<br />
than 1 × 10 6 .<br />
Sperm DNA Damage Tests<br />
Efforts have been made to find objective assessments of sperm<br />
quality that will predict pregnancy outcomes in men with abnormal<br />
results on semen analysis. Three experimental assessments are<br />
the sperm chromatin structure assay, DNA fragmentation index,<br />
and terminal deoxynuceotidyl transferase-mediated deoxyuridine<br />
triphosphate-nick end labeling (TUNEL).<br />
The sperm chromatin structure assay provides an objective<br />
assessment of sperm chromatin integrity and can be useful as a<br />
fertility marker. 52 In a recent study, DNA damage as measured<br />
using this test was found to predict the outcome of IUI.<br />
The DNA fragmentation index (DFI) has been shown to be<br />
negatively correlated with the overall pregnancy rate in women<br />
undergoing IUI, IVF, or ICSI. 53 The chances of achieving pregnancy<br />
are significantly lower when the sperm DFI is greater than<br />
27% after IUI processing. 54<br />
TUNEL evaluates the degree of sperm DNA fragmentation<br />
and stability. 55 In one study, lower degrees of DNA<br />
fragmentation after IUI sperm preparation correlated with<br />
higher pregnancy rates, and no pregnancy occurred when<br />
more than 12% of sperm in an IUI specimen were TUNELpositive.<br />
Hypo-osmotic Swelling Test<br />
The hypo-osmotic swelling test evaluates the membrane integrity<br />
of the sperm tail, detects the differences on the sperm surface,<br />
and detects subtle damage in membrane properties, which<br />
reduces the ability of spermatozoa to induce a viable embryo. 56<br />
A sample “passes” the hypo-osmotic swelling test when at least<br />
50% of sperm in an IUI sample swell. 57 Sperm specimens that<br />
fail the hypo-osmotic swelling test appear to have decreased<br />
fertilizing ability, and thus pregnancy rates after IUI are lower.<br />
The miscarriage rate was also higher when result of hypo-osmotic<br />
swelling test was less than 50%.<br />
Antisperm Antibodies<br />
Both IUI and IVF appear to be effective in treating subfertility<br />
in men with antisperm antibodies, although IVF/ICSI appears<br />
to have higher pregnancy rates per cycle than IUI. 58 However,<br />
to date no large prospective, randomized, controlled trial has<br />
compared IUI to IVF/ICSI in men with antisperm antibodies.<br />
In severe cases of antisperm antibodies, especially when the<br />
sperm head is involved, IVF/ICSI will often be required to<br />
achieve pregnancy. 59,60<br />
Female Factors That Predict IUI Success<br />
Many studies have examined the different variables affecting<br />
pregnancy rates after IUI. 25,61–64 The influence of lifestyle habits<br />
(e.g., smoking, caffeine consumption, and weight) is unclear but<br />
is most probably significant. There appear to be several important<br />
female factors that are useful in predicting pregnancy rates after<br />
IUI. These factors are maternal age, duration of infertility, and<br />
fenale infertility factors. 65<br />
Maternal Age<br />
A woman’s age is an indirect indicator for oocyte quality, and it<br />
has a significant effect on the pregnancy rates. An age-related<br />
decline in female fecundity has been documented in women<br />
undergoing IUI. 43,64 Successful pregnancy rates decrease after<br />
age 35 and reduce dramatically after age 40. However, pregnancies<br />
can occur at relatively advanced maternal ages, and satisfactory<br />
pregnancy rates can be obtained with IUI among women<br />
age 40 to 42. 66,67<br />
Duration of Infertility<br />
The longer the duration of infertility, the lower the pregnancy<br />
rates are after IUI. 25,43,65 Although the precise limits of infertility<br />
duration for recommending IUI have not been clearly established,<br />
the pregnancy rate may be seriously compromised when infertility<br />
has lasted 3 or more years.<br />
Female Fertility Factors<br />
The success of artificial insemination depends not only on the<br />
quality of oocytes and spermatozoa, but also on the receptivity<br />
of the endometrium. In a retrospective study, the presence of<br />
uterine anomalies negatively affected the success of IUI. 65<br />
Endometrial thickness and pattern is also predictive of IUI<br />
success. In a study on women undergoing controlled ovarian<br />
hyperstimulation and IUI, a trilaminar endometrium on the day<br />
of IUI provided a favorable prediction of pregnancy. However,<br />
endometrial thickness and Doppler surveys of the spiral and<br />
uterine arteries and dominant follicle gave no useful predictive<br />
value. 68 A study evaluated the role of endometrial volume<br />
measurement in predicting the pregnancy rate in women receiving<br />
controlled ovarian hyperstimulation and IUI. 69 An endometrial<br />
volume of less than 2 mL on three-dimensional ultrasound on<br />
the day of insemination was associated with a poor likelihood of<br />
pregnancy.<br />
Pregnancy rates after IUI are dependent on ovum pickup and<br />
transport. It follows that pregnancy rates after IUI are decreased<br />
by other causes of female infertility, including tubal factor and<br />
endometriosis.<br />
RISKS AND COMPLICATIONS<br />
Complications associated with IUI are extremely uncommon.<br />
Most of the complications that occur are related to the<br />
medications used to recruit multiple follicles before IUI.<br />
Pelvic Infections<br />
Limited cramping during or after an IUI procedure from the<br />
catheter or cervical tenaculum is common. These symptoms are<br />
self-limiting and should resolve within hours of the procedure.<br />
Continued discomfort can be an indication of a developing pelvic<br />
infection, which has been estimated to occur in less than 2 per<br />
1000 IUI procedures. 63 Early diagnosis and treatment are<br />
essential in these rare cases to minimize the risk to the patient,<br />
particularly that of subsequent decreased fertility.<br />
Vasovagal Reaction<br />
Vasovagal reactions can occur as a result of manipulation of the<br />
cervix. The resulting vasodilation and decreased heart rate can<br />
lead to hypotension, most commonly manifest by diaphoresis in<br />
545
Ch36-A03309.qxd 1/23/07 5:16 PM Page 546<br />
Section 6<br />
Infertility and Recurrent Pregnancy Loss<br />
546<br />
a supine patient. Sitting or standing increases the risk of syncope,<br />
which is unlikely to occur supine. Persistent symptomatic vasovagal<br />
reactions in a supine patient will often respond to the<br />
patient crossing her legs. 70 More severe cases might require<br />
treatment with intramuscular atropine injection (0.5 mg).<br />
Allergic Reaction<br />
Allergic reactions, including anaphylaxis, can occur after IUI in<br />
response to potential allergens in the wash media. Reactions<br />
have been reported to both the bovine serum albumin and<br />
antibiotics (penicillin and streptomycin) commonly used in the<br />
wash media. 71,72 Of these, penicillin allergies are the most<br />
common in the general population. Allergic reactions after IUI<br />
can range from a mild skin rash to life-threatening anaphylaxis<br />
with laryngeal edema, bronchospasm, and hypotension. For the<br />
rare patient experiencing an allergic reaction after IUI, the use<br />
of wash media free of albumin and antibiotics is advised.<br />
Antisperm Antibodies<br />
When IUI was first introduced, there was a concern that the<br />
procedure could result in the development of serum antisperm<br />
antibodies. Fortunately, after 40 years of experience, it appears<br />
that exposure of the upper reproductive tract to washed<br />
spermatozoa during IUI does not stimulate the appearance of<br />
clinically significant female antisperm antibodies. 73<br />
Pregnancy-Related Complications<br />
Multiple Pregnancies<br />
The risk of multiple pregnancies is not increased by IUI.<br />
However, medications used to recruit multiple follicles before<br />
IUI do increase this risk. Clomiphene citrate is associated with<br />
a twin risk of 5% to 10% and rare higher-order multiples.<br />
Injectable gonadotropins are associated with multiple pregnancy<br />
rates of 14% to 39%. 74–76 Careful monitoring of the number of<br />
periovulatory follicles and peak estradiol levels might decrease<br />
the rate of multiple pregnancies. 61,74,77 In general, women are at<br />
high risk if they are younger than age 30, have more than six<br />
preovulatory follicles, and a peak serum estradiol level greater<br />
than 1000 pg/mL.<br />
Spontaneous Abortion and Ectopic Pregnancy<br />
The risk of spontaneous abortion appears to be increased after<br />
IUI compared to the fertile population and is in the range of<br />
20% to 25%. 1,78 The increased risk is probably not directly<br />
attributed to IUI but is most likely due to the underlying infertility<br />
problem. Likewise, ectopic pregnancy rates depend largely on<br />
the presence of predisposing factors such as tubal disease and do<br />
not appear to be attributed to the IUI procedure. 79<br />
PSYCHOLOGICAL, ETHICAL, AND LEGAL<br />
ISSUES OF DONOR INSEMINATION<br />
Parents<br />
Donor insemination has more psychological implications than<br />
partner insemination. Before donor insemination, several issues<br />
should be discussed in detail, including the couple’s desire or<br />
need to start a family, the alternatives that the male partner has<br />
to procreate his own genetic children, and financial factors.<br />
It is recommended that the couple undergo counseling before<br />
the procedure so that they can both face their feelings concerning<br />
infertility, donor insemination, and other concerns. The<br />
male partner may experience a loss of self-esteem and fear<br />
losing his partner because of infertility. Both partners may feel<br />
guilty or angry toward each other for having an infertility problem.<br />
Infertility tends to separate the couple, especially when one side<br />
is uncooperative. Support groups or professional counseling can<br />
be helpful.<br />
Offspring<br />
There are expert opinions both for and against disclosing to the<br />
child that he or she is the product of donor insemination. Before<br />
undergoing donor IUI, the couple should decide if they plan to<br />
disclose the nature of the procedure and the biologic implications<br />
to their friends, relatives and, ultimately, their child. If<br />
knowledge of the procedure is shared with friends and relatives,<br />
there is always the risk that the truth will be disclosed to the<br />
child by someone other than the parents. These sometimesunderappreciated<br />
issues can cause unnecessary grief if not<br />
adequately addressed prior to therapy.<br />
Legal Issues<br />
It is imperative that both partners understand the legal issues<br />
concerning donor insemination. Before donor insemination, both<br />
partners should sign an informed consent that clearly states the<br />
rights and obligations of the parties involved and those of the<br />
child. Although laws vary from state to state, when sperm is<br />
obtained from a sperm bank, the donor universally has no legal<br />
access to the couple’s identity. In cases where couples elect to<br />
use a donor known to them, an attorney should be obtained to<br />
draft the appropriate papers to terminate any parental rights of<br />
the donor and give the couple full custody of any subsequent<br />
child. In some states, the child conceived from donor sperm<br />
may have the right to obtain identifying information about the<br />
donor once they reach adulthood.<br />
●<br />
●<br />
●<br />
●<br />
●<br />
●<br />
●<br />
PEARLS<br />
<strong>Artificial</strong> insemination is a useful and cost-effective treatment<br />
option in selected groups of infertile couples.<br />
Infertility due to cervical factor and mild male factor (without<br />
any associated female factor) can be treated with intrauterine<br />
insemination without ovarian stimulation.<br />
<strong>Artificial</strong> insemination appears to be more cost-effective and<br />
simple compared to the IVF/ICSI if the couples are selected<br />
appropriately.<br />
In spite of extensive research, we are still not able to predict<br />
the success of artificial insemination in a specific couple.<br />
Duration of the infertility negatively impacts the artificial<br />
insemination success.<br />
Couples with unexplained infertility have better success with<br />
artificial insemination than natural intercourse.<br />
Couples with unexplained infertility should use controlled<br />
ovarian hyperstimulation along with the artificial insemination.
Ch36-A03309.qxd 1/23/07 5:16 PM Page 547<br />
Chapter 36<br />
<strong>Artificial</strong> <strong>Insemination</strong><br />
REFERENCES<br />
1. Allen NC, Herbert CM 3rd, Maxson WS, et al: Intrauterine insemination:<br />
A critical review. Fertil Steril 44:569–580, 1985.<br />
2. Keck C, Gerber-Schafer C, Wilhelm C, et al: Intrauterine insemination<br />
for treatment of male infertility. Int J Androl 20(Suppl 3):55–64, 1997.<br />
3. Cohlen BJ: Should we continue performing intrauterine inseminations<br />
in the year 2004 Gynecol Obstet Invest 59:3–13, 2004.<br />
4. Goverde AJ, McDonnell J, Vermeiden JP, et al: Intrauterine insemination<br />
or in vitro fertilisation in idiopathic subfertility and male subfertility: A<br />
randomised trial and cost-effectiveness analysis. Lancet 355:13–18,<br />
2000.<br />
5. Coulson C, McLaughlin EA, Harris S, et al: Randomized controlled trial<br />
of cervical cap with intracervical reservoir versus standard intracervical<br />
injection to inseminate cryopreserved donor semen. Hum Reprod<br />
11:84–87, 1996.<br />
6. Cantineau AE, Heineman MJ, Al-Inany H, Cohlen BJ: Intrauterine<br />
insemination versus Fallopian tube sperm perfusion in non-tubal subfertility:<br />
A systematic review based on a Cochrane Review. Hum Reprod<br />
19:2721–2729, 2004.<br />
7. Hurd WW, Randolph JF Jr, Ansbacher R, et al: Comparison of intracervical,<br />
intrauterine, and intratubal techniques for donor insemination.<br />
Fertil Steril 59:339–342, 1993.<br />
8. Ombelet W, Menkveld R, Kruger TF, Steeno O: Sperm morphology<br />
assessment: Historical review in relation to fertility. Hum Reprod Update<br />
1:543–557, 1995.<br />
9. Bronson R, Cooper G, Rosenfeld D: Sperm antibodies: Their role in<br />
infertility. Fertil Steril 42:171–183, 1984.<br />
10. Barratt CL, McLeod ID, Dunphy BC, Cooke ID: Prognostic value of<br />
two putative sperm function tests: Hypo-osmotic swelling and bovine<br />
sperm mucus penetration test (Penetrak). Hum Reprod 7:1240–1244,<br />
1992.<br />
11. Ohl DA, Wolf LJ, Menge AC, et al: Electroejaculation and assisted<br />
reproductive technologies in the treatment of anejaculatory infertility.<br />
Fertil Steril 76:1249–1255, 2001.<br />
12. Montanaro Gauci M, Kruger TF, Coetzee K, et al: Stepwise regression<br />
analysis to study male and female factors impacting on pregnancy rate<br />
in an intrauterine insemination programme. Andrologia 33:135–141,<br />
2001.<br />
13. Zeyneloglu HB, Arici A, Olive DL, Duleba AJ: Comparison of intrauterine<br />
insemination with timed intercourse in superovulated cycles<br />
with gonadotropins: A meta-analysis. Fertil Steril 69:486–491, 1998.<br />
14. Sovino H, Sir-Petermann T, Devoto L: Clomiphene citrate and ovulation<br />
induction. Reprod Biomed Online 4:303–310, 2002.<br />
15. Tummon IS, Asher LJ, Martin JS, Tulandi T: Randomized controlled<br />
trial of superovulation and insemination for infertility associated with<br />
minimal or mild endometriosis. Fertil Steril 68:8–12, 1997.<br />
16. ASRM: New guidelines for the use of semen donor insemination: 1990.<br />
The American Fertility Society. Fertil Steril 53:1S–13S, 1990.<br />
17. Goldberg JM, Mascha E, Falcone T, Attaran M: Comparison of intrauterine<br />
and intracervical insemination with frozen donor sperm: A metaanalysis.<br />
Fertil Steril 72:792–795, 1999.<br />
18. Rowell P, Braude P: Assisted conception. I—General principles. BMJ<br />
327:799–801, 2003.<br />
19. Weinberg CR, Wilcox AJ: A model for estimating the potency and<br />
survival of human gametes in vivo. Biometrics 51:405–412, 1995.<br />
20. Gould JE, Overstreet JW, Hanson FW: Assessment of human sperm<br />
function after recovery from the female reproductive tract. Biol Reprod<br />
31:888–894, 1984.<br />
21. Lenton EA, Woodward B: Natural-cycle versus stimulated-cycle IVF: Is<br />
there a role for IVF in the natural cycle J Assist Reprod Genet<br />
10:406–408, 1993.<br />
22. Zreik TG, Garcia-Velasco JA, Habboosh MS, et al: Prospective,<br />
randomized, crossover study to evaluate the benefit of human chorionic<br />
gonadotropin-timed versus urinary luteinizing hormone-timed intrauterine<br />
inseminations in clomiphene citrate-stimulated treatment cycles. Fertil<br />
Steril 71:1070–1074, 1999.<br />
23. Deaton JL, Clark RR, Pittaway DE, et al: Clomiphene citrate ovulation<br />
induction in combination with a timed intrauterine insemination: The<br />
value of urinary luteinizing hormone versus human chorionic gonadotropin<br />
timing. Fertil Steril 68:43–47, 1997.<br />
24. Van Voorhis BJ, Sparks AE, Allen BD, et al: Cost-effectiveness of<br />
infertility treatments: A cohort study. Fertil Steril 67:830–836, 1997.<br />
25. Nuojua-Huttunen S, Tomas C, Bloigu R, et al: Intrauterine insemination<br />
treatment in subfertility: An analysis of factors affecting outcome. Hum<br />
Reprod 14:698–703, 1999.<br />
26. Matilsky M, Geslevich Y, Ben-Ami M, et al:. Two-day IUI treatment<br />
cycles are more successful than one-day IUI cycles when using<br />
frozen–thawed donor sperm. J Androl 19:603–607, 1998.<br />
27. Ransom MX, Blotner MB, Bohrer M, et al: Does increasing frequency<br />
of intrauterine insemination improve pregnancy rates significantly during<br />
superovulation cycles Fertil Steril 61:303–307, 1994.<br />
28. Cohlen BJ, te Velde ER, van Kooij RJ, et al: Controlled ovarian hyperstimulation<br />
and intrauterine insemination for treating male subfertility:<br />
A controlled study. Hum Reprod 13:1553–1558, 1998.<br />
29. Arici A, Byrd W, Bradshaw K, et al: Evaluation of clomiphene citrate<br />
and human chorionic gonadotropin treatment: A prospective, randomized,<br />
crossover study during intrauterine insemination cycles. Fertil Steril<br />
61:314–318, 1994.<br />
30. Alborzi S, Motazedian S, Parsanezhad ME, Jannati S: Comparison of the<br />
effectiveness of single intrauterine insemination (IUI) versus double<br />
IUI per cycle in infertile patients. Fertil Steril 80:595–599, 2003.<br />
31. Osuna C, Matorras R, Pijoan JI, Rodriguez-Escudero FJ: One versus two<br />
inseminations per cycle in intrauterine insemination with sperm from<br />
patients’ husbands: A systematic review of the literature. Fertil Steril<br />
82:17–24, 2004.<br />
32. Alvarez JG: Nurture vs nature: How can we optimize sperm quality<br />
J Androl 24:640–648, 2003.<br />
33. Saleh R, Agarwal A: Oxidative stress and male infertility: From research<br />
bench to clinical practice. J Androl 23:737–752, 2002.<br />
34. Mortimer D: Sperm preparation methods. J Androl 21:357–366,<br />
2000.<br />
35. Rogers BJ, Perreault SD, Bentwood BJ, et al: Variability in the human–<br />
hamster in vitro assay for fertility evaluation. Fertil Steril 39:204–211,<br />
1983.<br />
36. Yamamoto Y, Maenosono S, Okada H, et al: Comparisons of sperm<br />
quality, morphometry and function among human sperm populations<br />
recovered via SpermPrep II filtration, swim-up and Percoll density<br />
gradient methods. Andrologia 29:303–310, 1997.<br />
37. Aitken RJ, Clarkson JS: Significance of reactive oxygen species and<br />
antioxidants in defining the efficacy of sperm preparation techniques.<br />
J Androl 9:367–376, 1988.<br />
38. Erel CT, Senturk LM, Irez T, et al: Sperm-preparation techniques for<br />
men with normal and abnormal semen analysis. A comparison. J Reprod<br />
Med 45:917–922, 2000.<br />
39. Sakkas D, Tomlinson M: Assessment of sperm competence. Semin<br />
Reprod Med 18:133–139, 2000.<br />
40. Hammadeh ME, Kuhnen A, Amer AS, et al: Comparison of sperm<br />
preparation methods: Effect on chromatin and morphology recovery<br />
rates and their consequences on the clinical outcome after in vitro<br />
fertilization embryo transfer. Int J Androl 24:360–368, 2001.<br />
41. Carrell DT, Kuneck PH, Peterson CM, et al: A randomized, prospective<br />
analysis of five sperm preparation techniques before intrauterine<br />
insemination of husband sperm. Fertil Steril 69:122–126, 1998.<br />
42. Makler A: A simple technique to increase success rate of artificial<br />
insemination. Int J Gynaecol Obstet 18:19–21, 1980.<br />
43. Plosker SM, Jacobson W, Amato P: Predicting and optimizing success in<br />
an intra-uterine insemination programme. Hum Reprod 9:2014–2021,<br />
1994.<br />
44. Agarwal A, Sharma RK, Nelson DR: New semen quality scores developed<br />
by principal component analysis of semen characteristics. J Androl<br />
24:343–352, 2003.<br />
547
Ch36-A03309.qxd 1/23/07 5:16 PM Page 548<br />
Section 6<br />
Infertility and Recurrent Pregnancy Loss<br />
45. Bedaiwy MA, Sharma RK, Alhussaini TK, et al: The use of novel semen<br />
quality scores to predict pregnancy in couples with male-factor infertility<br />
undergoing intrauterine insemination. J Androl 24:353–360, 2003.<br />
46. Hendin BN, Falcone T, Hallak J, et al: The effect of patient and semen<br />
characteristics on live birth rates following intrauterine insemination: A<br />
retrospective study. J Assist Reprod Genet 17:245–252, 2000.<br />
47. Zayed F, Lenton EA, Cooke ID: Comparison between stimulated in<br />
vitro fertilization and stimulated intrauterine insemination for the<br />
treatment of unexplained and mild male factor infertility. Hum Reprod<br />
12:2408–2413, 1997.<br />
48. Van Waart J, Kruger TF, Lombard CJ, Ombelet W: Predictive value of<br />
normal sperm morphology in intrauterine insemination (IUI): A<br />
structured literature review. Hum Reprod Update 7:495–500, 2001.<br />
49. van Noord-Zaadstra BM, Looman CW, Alsbach H, et al: Delaying childbearing:<br />
Effect of age on fecundity and outcome of pregnancy. BMJ<br />
302:1361–1365, 1991.<br />
50. Stone BA, Vargyas JM, Ringler GE, et al: Determinants of the outcome<br />
of intrauterine insemination: Analysis of outcomes of 9963 consecutive<br />
cycles. Am J Obstet Gynecol 180:1522–1534, 1999.<br />
51. Campana A, Sakkas D, Stalberg A, et al: Intrauterine insemination:<br />
Evaluation of the results according to the woman’s age, sperm quality,<br />
total sperm count per insemination and life table analysis. Hum Reprod<br />
11:732–736, 1996.<br />
52. Richthoff J, Spano M, Giwercman YL, et al: The impact of testicular<br />
and accessory sex gland function on sperm chromatin integrity as<br />
assessed by the sperm chromatin structure assay (SCSA). Hum Reprod<br />
17:3162–3169, 2002.<br />
53. Saleh RA, Agarwal A, Nada EA, et al: Negative effects of increased<br />
sperm DNA damage in relation to seminal oxidative stress in men<br />
with idiopathic and male factor infertility. Fertil Steril 79(Suppl 3):<br />
1597–1605, 2003.<br />
54. Bungum M, Humaidan P, Spano M, et al: The predictive value of sperm<br />
chromatin structure assay (SCSA) parameters for the outcome of<br />
intrauterine insemination, IVF and ICSI. Hum Reprod 19:1401–1408,<br />
2004.<br />
55. Duran EH, Morshedi M, Taylor S, Oehninger S: Sperm DNA quality<br />
predicts intrauterine insemination outcome: A prospective cohort study.<br />
Hum Reprod 17:3122–3128, 2002.<br />
56. Tartagni M, Schonauer MM, Cicinelli E, et al: Usefulness of the hypoosmotic<br />
swelling test in predicting pregnancy rate and outcome in<br />
couples undergoing intrauterine insemination. J Androl 23:498–502,<br />
2002.<br />
57. Ombelet W, Deblaere K, Bosmans E, et al: Semen quality and intrauterine<br />
insemination. Reprod Biomed Online 7:485–492, 2003.<br />
58. Ohl DA, Naz RK: Infertility due to antisperm antibodies. Urology<br />
46:591–602, 1995.<br />
59. McLachlan RI: Basis, diagnosis and treatment of immunological infertility<br />
in men. J Reprod Immunol 57:35–45, 2002.<br />
60. Lombardo F, Gandini L, Dondero F, Lenzi A: Antisperm immunity in<br />
natural and assisted reproduction. Hum Reprod Update 7:450–456,<br />
2001.<br />
61. Dickey RP, Olar TT, Taylor SN, et al: Relationship of follicle number,<br />
serum estradiol, and other factors to birth rate and multiparity in human<br />
menopausal gonadotropin-induced intrauterine insemination cycles. Fertil<br />
Steril 56:89–92, 1991.<br />
62. Dickey RP, Olar TT, Taylor SN, et al: Relationship of follicle number and<br />
other factors to fecundability and multiple pregnancy in clomiphene<br />
citrate-induced intrauterine insemination cycles. Fertil Steril 57:613–619,<br />
1992.<br />
63. Mathieu C, Ecochard R, Bied V, et al: Cumulative conception rate<br />
following intrauterine artificial insemination with husband’s spermatozoa:<br />
Influence of husband’s age. Hum Reprod 10:1090–1097, 1995.<br />
64. Tomlinson MJ, Amissah-Arthur JB, Thompson KA, et al: Prognostic<br />
indicators for intrauterine insemination (IUI): Statistical model for IUI<br />
success. Hum Reprod 11:1892–1896, 1996.<br />
65. Steures P, van der Steeg JW, Mol BW, et al: Prediction of an ongoing<br />
pregnancy after intrauterine insemination. Fertil Steril 82:45–51, 2004.<br />
66. Haebe J, Martin J, Tekepety F, et al: Success of intrauterine insemination<br />
in women aged 40–42 years. Fertil Steril 78:29–33, 2002.<br />
67. Khalil MR, Rasmussen PE, Erb K, et al: Homologous intrauterine<br />
insemination. An evaluation of prognostic factors based on a review of<br />
2473 cycles. Acta Obstet Gynecol Scand 80:74–81, 2001.<br />
68. Tsai HD, Chang CC, Hsieh YY, et al: <strong>Artificial</strong> insemination. Role of endometrial<br />
thickness and pattern, of vascular impedance of the spiral and<br />
uterine arteries, and of the dominant follicle. J Reprod Med 45:195–200,<br />
2000.<br />
69. Zollner U, Zollner KP, Blissing S, et al: Impact of three-dimensionally<br />
measured endometrial volume on the pregnancy rate after intrauterine<br />
insemination. Zentralbl Gynakol 125:136–141, 2003.<br />
70. Krediet CT, van Dijk N, Linzer M, et al: Management of vasovagal<br />
syncope: Controlling or aborting faints by leg crossing and muscle tensing.<br />
Circulation 106:1684–1689, 2002.<br />
71. Smith YR, Hurd WW, Menge AC, et al: Allergic reactions to penicillin<br />
during in vitro fertilization and intrauterine insemination. Fertil Steril<br />
58:847–849, 1992.<br />
72. Sonenthal KR, McKnight T, Shaughnessy MA, et al: Anaphylaxis during<br />
intrauterine insemination secondary to bovine serum albumin. Fertil<br />
Steril 56:1188–1191, 1991.<br />
73. Moretti-Rojas I, Rojas FJ, Leisure M, et al: Intrauterine inseminations<br />
with washed human spermatozoa does not induce formation of antisperm<br />
antibodies. Fertil Steril 53:180–182, 1990.<br />
74. Valbuena D, Simon C, Romero JL, et al: Factors responsible for multiple<br />
pregnancies after ovarian stimulation and intrauterine insemination with<br />
gonadotropins. J Assist Reprod Genet 13:663–668, 1996.<br />
75. Goldfarb JM, Peskin B, Austin C, Lisbona H: Evaluation of predictive<br />
factors for multiple pregnancies during gonadotropin/IUI treatment.<br />
J Assist Reprod Genet 14:88–91, 1997.<br />
76. Tur R, Buxaderas C, Martinez F, et al: Comparison of the role of cervical<br />
and intrauterine insemination techniques on the incidence of multiple<br />
pregnancy after artificial insemination with donor sperm. J Assist Reprod<br />
Genet 14:250–253, 1997.<br />
77. Pasqualotto EB, Falcone T, Goldberg JM, et al: Risk factors for multiple<br />
gestation in women undergoing intrauterine insemination with ovarian<br />
stimulation. Fertil Steril 72:613–618, 1999.<br />
78. Lalich RA, Marut EL, Prins GS, Scommegna A: Life table analysis<br />
of intrauterine insemination pregnancy rates. Am J Obstet Gynecol<br />
158:980–984, 1988.<br />
79. Aboulghar MA, Mansour RT, Serour GI: Ovarian superstimulation in<br />
the treatment of infertility due to peritubal and periovarian adhesions.<br />
Fertil Steril 51:834–837, 1989.<br />
548