Jan-Mar, 2011 - Indian Journal of Pharmacy Practice
Jan-Mar, 2011 - Indian Journal of Pharmacy Practice
Jan-Mar, 2011 - Indian Journal of Pharmacy Practice
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
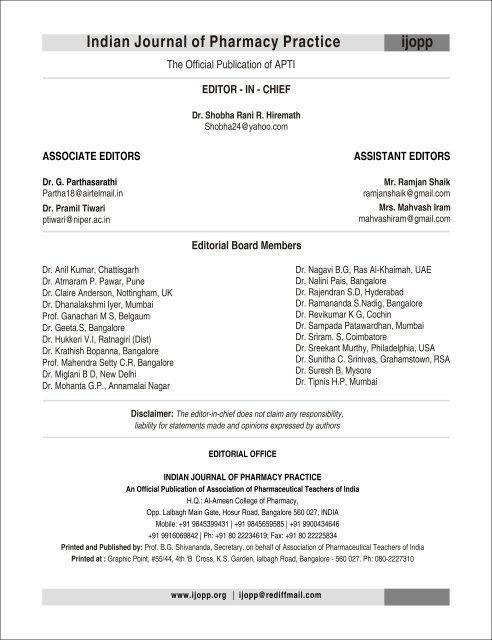
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
ijopp<br />
The Official Publication <strong>of</strong> APTI<br />
EDITOR - IN - CHIEF<br />
Dr. Shobha Rani R. Hiremath<br />
Shobha24@yahoo.com<br />
ASSOCIATE EDITORS<br />
Dr. G. Parthasarathi<br />
Partha18@airtelmail.in<br />
Dr. Pramil Tiwari<br />
ptiwari@niper.ac.in<br />
ASSISTANT EDITORS<br />
Mr. Ramjan Shaik<br />
ramjanshaik@gmail.com<br />
Mrs. Mahvash Iram<br />
mahvashiram@gmail.com<br />
Editorial Board Members<br />
Dr. Anil Kumar, Chattisgarh<br />
Dr. Atmaram P. Pawar, Pune<br />
Dr. Claire Anderson, Nottingham, UK<br />
Dr. Dhanalakshmi Iyer, Mumbai<br />
Pr<strong>of</strong>. Ganachari M S, Belgaum<br />
Dr. Geeta.S, Bangalore<br />
Dr. Hukkeri V.I, Ratnagiri (Dist)<br />
Dr. Krathish Bopanna, Bangalore<br />
Pr<strong>of</strong>. Mahendra Setty C.R, Bangalore<br />
Dr. Miglani B D, New Delhi<br />
Dr. Mohanta G.P., Annamalai Nagar<br />
Dr. Nagavi B.G, Ras Al-Khaimah, UAE<br />
Dr. Nalini Pais, Bangalore<br />
Dr. Rajendran S.D, Hyderabad<br />
Dr. Ramananda S.Nadig, Bangalore<br />
Dr. Revikumar K G, Cochin<br />
Dr. Sampada Patawardhan, Mumbai<br />
Dr. Sriram. S, Coimbatore<br />
Dr. Sreekant Murthy, Philadelphia, USA<br />
Dr. Sunitha C. Srinivas, Grahamstown, RSA<br />
Dr. Suresh B, Mysore<br />
Dr. Tipnis H.P, Mumbai<br />
Disclaimer: The editor-in-chief does not claim any responsibility,<br />
liability for statements made and opinions expressed by authors<br />
EDITORIAL OFFICE<br />
INDIAN JOURNAL OF PHARMACY PRACTICE<br />
An Official Publication <strong>of</strong> Association <strong>of</strong> Pharmaceutical Teachers <strong>of</strong> India<br />
H.Q.: Al-Ameen College <strong>of</strong> <strong>Pharmacy</strong>,<br />
Opp. Lalbagh Main Gate, Hosur Road, Bangalore 560 027, INDIA<br />
Mobile: +91 9845399431 | +91 9845659585 | +91 9900434646<br />
+91 9916069842 | Ph: +91 80 22234619; Fax: +91 80 22225834<br />
Printed and Published by: Pr<strong>of</strong>. B.G. Shivananda, Secretary, on behalf <strong>of</strong> Association <strong>of</strong> Pharmaceutical Teachers <strong>of</strong> India<br />
Printed at : Graphic Point, #55/44, 4th ‘B’ Cross, K.S. Garden, lalbagh Road, Bangalore - 560 027. Ph: 080-2227310<br />
www.ijopp.org | ijopp@rediffmail.com
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
ijopp<br />
Editorial<br />
Review Articles<br />
♦HER2/neu vaccines fight against Breast Cancer<br />
Rajasekhar P ............................................................................................................................................................. 1- 13<br />
♦Contribution <strong>of</strong> drug interactions to burden <strong>of</strong> preventable ADR'S: Approches to predict and prevent drug interactions.<br />
Raval D K, Saraswathy N, Meghani N M, Shah H K ................................................................................................14 -17<br />
♦Survey and evaluation <strong>of</strong> various epidemiological factors in a multiethnic diabetic Population in ras Al-Khaimah, UAE.<br />
Smitha F, Meenakshi J, Padma R, Multani S K .......................................................................................................18 - 25<br />
♦Impact <strong>of</strong> educational interventions on Adverse Drug Reaction reporting<br />
Ganachari M S, Patil PA, Soham S, Nidhi Z ........................................................................................................... 26 - 31<br />
Contents<br />
♦Awareness about ways <strong>of</strong> transmission <strong>of</strong> AIDS and its treatment among university students in Pakistan<br />
Tehzeeb-ul-Nisa, Imran Qadir M, Hibba-tul-Baseer, Dure-Shehwar, Farzana C, Irfan M ...................................... 32 - 35<br />
♦Study <strong>of</strong> prescribing patterns <strong>of</strong> antibiotics used in the management <strong>of</strong> various infectious diseases<br />
Azizullah S G, Jabeen G, Shobna J, Kaleemuddin S, Mohiuddin ........................................................................ 36 - 40<br />
♦A study on prescription pattern <strong>of</strong> antihypertensives<br />
Preethi M, PraveenKumar NVRT, Lekshmi S, Manna PK, Mohanta GP, Parimalakrishnan S,<br />
Sudarshan S. ............................................................................................................................................................41- 44<br />
♦Evaluation <strong>of</strong> prescribing pattern <strong>of</strong> clinicians in out-patient departments <strong>of</strong> a South <strong>Indian</strong> teaching hospital<br />
Ramesh A, Suhaj A ................................................................................................................................................45 - 49<br />
♦Impact <strong>of</strong> patient counseling on Knowledge, Attitude, <strong>Practice</strong> and Quality <strong>of</strong> Life in patients with Type II Diabetes<br />
mellitus and Hypertension.<br />
Praveena P, Usman S, Deepika B, Raghu Kumar V, Mohanta G P, Manna P K, Manavalan R. ........................... 50 -54<br />
♦Influience <strong>of</strong> pharmacist provided education on Quality <strong>of</strong> Life in patients with HIV/AIDS-a study<br />
Ramesh A, Dinesh K, Nagavi B G, Mothi S N, Parthasarathy G............................................................................. 55 - 60<br />
♦Drug use and dosing in patients with renal impairment<br />
Veera Raghavulu B, Shravani K, PrabhakarReddy V, Manohar Babu S ................................................................ 61 - 67<br />
♦Prescription errors in Guntur district <strong>of</strong> Andhra Pradesh- A retrospective study<br />
Pulla Reddy M, Vijayapandi P, Aruna kanth CH, karthikeyan R ............................................................................ 68 - 70
Dear Readers,<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
ijopp<br />
Editorial<br />
As pharmacists we should always keep ourselves abreast <strong>of</strong> the latest developments in the field <strong>of</strong> medicines.<br />
Currently the concept <strong>of</strong> personalized medicine is receiving much attention all over the world. Drug therapy is now moving<br />
from right drug for the disease to individualization <strong>of</strong> therapy.<br />
As we have all seen at some point or the other, drug response can vary from patient to patient.<br />
The aim <strong>of</strong> individualized treatment is to match the right drug to the right patient and, in some cases, even to design the<br />
appropriate treatment for patients according to their genotype.<br />
Pharmacogenomics, a branch <strong>of</strong> pharmacology deals with the influence <strong>of</strong> genetic variation on drug response and has<br />
presently caught the attention <strong>of</strong> researchers globally.<br />
After extensive research in this field, it has been found that Single Nucleotide Polymorphism (SNP), the variations in DNA,<br />
at a single base are actually responsible for the variations in drug response among patients. These SNPs are the markers<br />
that can correlate drug response and genetic makeup.<br />
Possible genetic markers for diseases such as cancers, heart diseases, diabetes, bipolar disorders and schizophrenia have<br />
been identified. For e.g. Allele A1 at polymorphism A correlates with coronary artery disease and the individuals with this<br />
may be at an increased risk for the same. Risk genes for schizophrenia are on chromosomes 22, chromosome 13 and<br />
chromosome 8.<br />
Individuals <strong>of</strong> any age could be tested to determine the risk pr<strong>of</strong>iles for the occurrence <strong>of</strong> future disease. Infants can be tested<br />
for genetic diseases at birth.<br />
In gene pr<strong>of</strong>iling, DNA and protein chips are used, for e.g. p53 DNA chip is used popularly for the identification and gene<br />
screening <strong>of</strong> cancer risks.<br />
SNP genotyping is also helpful to track the path <strong>of</strong> infectious diseases. Pharmacogenomic data can establish an early<br />
warning system for severe infections due to a particular sensitive genetic makeup <strong>of</strong> the patient.<br />
Severe adverse reactions to drugs can be prevented with the help <strong>of</strong> pharmacogenomics. For e.g. carbamazepine, an<br />
antiepileptic drug causes Stevens-Johnson Syndrome, a life threatening reaction in few patients and upon analysis it is<br />
understood that HLA-B*1502 gene is responsible for the same .<br />
The doctor while treating certain cases where there is a need, can now actually get the patient's genome analyzed to<br />
prescribe the drugs that are most effective and having least adverse effects to the individual patients. Though the method is<br />
very expensive, it can prove worthy in saving a few lives.<br />
Thus, Pharmacogenomics is the new hope <strong>of</strong> personalised medicine.<br />
Our readers are invited to share their views on the latest happenings in the field as “letter to editor”.<br />
I request you all to send quality research articles, case reports and review articles as always.<br />
Looking forward for write ups in variety <strong>of</strong> topics and varied research work in this year.<br />
Dr. Shobha Rani R. Hiremath<br />
Editor-in-Chief<br />
www.ijopp.org | ijopp@rediffmail.com
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
Association <strong>of</strong> Pharmaceutical Teachers <strong>of</strong> India<br />
HER2/neu vaccines fight against Breast Cancer<br />
Rajasekhar P<br />
Department <strong>of</strong> Biotechnology, Sreenidhi Institute <strong>of</strong> Science and Technology, Yamnampet, Ghatkesar, R.R.District,<br />
Andhra Pradesh, India.<br />
A B S T R A C T<br />
Breast cancer is the most common diagnosed cancer among women. Breast cancer is a malignant tumour that starts from cells <strong>of</strong> the breast. In<br />
recent decades, medical science has uncovered some important reasons why breast cancers do not all behave alike. One <strong>of</strong> those reasons has<br />
to do with HER2, the human epidermal growth factor receptor 2. The HER2/neu oncogenic protein is a well-described tumour antigen that has<br />
been immunologically defined in patients with multiple different tumour types that overexpress HER2/neu. HER2 receptors are the product <strong>of</strong> a<br />
gene also called HER2, which is expressed in the normal, milk-producing cells (known as epithelial cells) that line the ducts <strong>of</strong> the breast. A result<br />
<strong>of</strong> HER 2 positive is important, as it indicates that the cancer can be treated with Herceptin in combination with other chemotherapy drugs. If<br />
cancer is diagnosed as HER2 positive, it is most likely aggressive. Regardless <strong>of</strong> tumour type, endogenous immunity to HER2/neu has two<br />
predominant characteristics. First, pre-existent immunity is detectable in only a minority <strong>of</strong> the patients, and secondly, detectable HER2/neu<br />
specific immunity is <strong>of</strong> low magnitude. Thus, initial vaccine strategies have focused on boosting HER2/neu immunity to a higher magnitude in<br />
patients with pre-existent low-level immunity and creating it in the majority <strong>of</strong> patients vaccinated. Early results from clinical trials demonstrate<br />
that significant levels <strong>of</strong> HER2/neu specific T-cell and immunity can be generated with active immunization and that the immune response is<br />
durable after vaccinations have ended. Furthermore, despite the generation <strong>of</strong> CD8+ and CD4,T cells responsive to HER2/neu, there is no<br />
evidence <strong>of</strong> autoimmunity directed against tissues that express basal levels <strong>of</strong> the protein. Vaccines that stimulate antibody immunity against<br />
HER2/neu may also be <strong>of</strong> benefit in the treatment or prevention <strong>of</strong> HER2/neu overexpressing cancers. The development <strong>of</strong> cancer vaccines<br />
targeting the HER-2/neu oncogenic protein may be useful adjuvants to standard therapy and aid in the prevention <strong>of</strong> relapse in patients whose<br />
tumours overexpress the protein. Starting treatment as soon as possible will help improve survival, as well as help to prevent recurrence.<br />
Key Words: Breast cancer, HER2/neu, vaccine.<br />
Submitted: 2/2/<strong>2011</strong><br />
Accepted: 14/2/<strong>2011</strong><br />
INTRODUCTION<br />
The breast is the upper ventral region <strong>of</strong> humans which are<br />
modified sudoriferous (sweat) glands which produce milk in<br />
women, and in some rare cases, in men. The breasts <strong>of</strong> a<br />
female contain the mammary glands, which secrete milk used<br />
to feed infants. Both men and women develop breasts from<br />
the same embryological tissues. However, at puberty, female<br />
sex hormones, mainly estrogen, promote breast development<br />
which does not occur in men. As a result, women's' breasts<br />
become far more prominent than those <strong>of</strong> men. Each breast<br />
has one nipple surrounded by the areola. The color <strong>of</strong> the<br />
areola varies from pink to dark brown and has several<br />
sebacious glands. In women, the larger mammary glands<br />
within the breast produce the milk. They are distributed<br />
throughout the breast, with two-thirds <strong>of</strong> the tissue found<br />
Address for Correspondence:<br />
Dr. RAJASEKHAR PINNAMANENI, Taduvayi, <strong>Jan</strong>gareddigudem Mandal, West Godavari<br />
District, Andhra Pradesh-534 447. India<br />
E-mail: pinnamaneniraj@gmail.com<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
within 30 mm <strong>of</strong> the base <strong>of</strong> the nipple. These are drained to<br />
the nipple by between 4 and 18 lactiferous ducts, where each<br />
duct has its own opening. The network formed by these ducts<br />
is complex, like the tangled roots <strong>of</strong> a tree. It is not always<br />
arranged radially, and branches close to the nipple. The ducts<br />
near the nipple do not act as milk reservoirs but lactiferous<br />
sinuses do not, in fact, exist. Instead, most milk is actually in<br />
the back <strong>of</strong> the breast, and when suckling occurs, the smooth<br />
muscles <strong>of</strong> the gland push more milk forward. The remainder<br />
<strong>of</strong> the breast is composed <strong>of</strong> connective tissue (collagen and<br />
elastin), adipose tissue (fat), and Cooper's ligaments. The<br />
ratio <strong>of</strong> glands to adipose tissues rises from 1:1 in nonlactating<br />
women to 2:1 in lactating women (Fig. 1).<br />
Breast cancer originates from breast tissue, most commonly<br />
from the inner lining <strong>of</strong> milk ducts or the lobules that supply<br />
the ducts with milk. Cancers originating from ducts are<br />
known as ductal carcinomas; those originating from lobules<br />
are known as lobular carcinomas. There are many different<br />
types <strong>of</strong> breast cancer, with different stages (spread),<br />
aggressiveness, and genetic makeup; survival varies greatly<br />
1
Rajasekhar P- HER2/neu Vaccines fight against Breast Cancer<br />
Fig.1: Female breast is made up mainly <strong>of</strong> lobules (milk-producing<br />
glands), ducts (tiny tubes that carry the milk from the lobules to the<br />
nipple), and stroma (fatty tissue and connective tissue surrounding<br />
the ducts and lobules, blood vessels, and lymphatic vessels).<br />
Fig.2: Treating HER2 Positive Breast Cancer<br />
depending on those factors. Computerized models are<br />
available to predict survival. With best treatment and<br />
dependent on staging, 10-year disease-free survival varies<br />
from 98% to 10%. Worldwide, breast cancer comprises<br />
10.4% <strong>of</strong> all cancer incidences among women, making it the<br />
second most common type <strong>of</strong> non-skin cancer (after lung<br />
cancer) and the fifth most common cause <strong>of</strong> cancer death.<br />
Breast cancer is about 100 times more common in women<br />
than in men, although males tend to have poorer outcomes due<br />
to delays in diagnosis.<br />
Breast cells have receptors on their surface and in their<br />
cytoplasm and nucleus. Chemical messengers such as<br />
hormones bind to receptors, and this causes changes in the<br />
cell. Breast cancer cells may or may not have three important<br />
receptors: estrogen receptor (ER), progesterone receptor<br />
(PR), and HER2/neu. HER2/neu stands for "Human<br />
Epidermal growth factor Receptor 2" and is a protein giving<br />
higher aggressiveness in breast cancers. It is a member <strong>of</strong> the<br />
Erb B protein family, more commonly known as the<br />
epidermal growth factor receptor family. HER2/neu has also<br />
been designated as CD340 and p185. It is encoded by the<br />
HER2 gene that sends control signals to the cells, telling them<br />
to grow, divide, and make repairs. A healthy breast cell has 2<br />
copies <strong>of</strong> the HER2 gene. Some kinds <strong>of</strong> breast cancer get<br />
started when a breast cell has more than 2 copies <strong>of</strong> that gene,<br />
and those copies start over-producing the HER2 protein. As a<br />
result, the affected cells grow and divide much too quickly.<br />
Knowing the HER2 status is an important part <strong>of</strong> diagnosis<br />
(Fig. 2).<br />
Function<br />
HER2 is a cell membrane surface-bound receptor tyrosine<br />
kinase and is normally involved in the signal transduction<br />
pathways leading to cell growth and differentiation. It is<br />
encoded within the genome by HER2/neu, a known protooncogene.<br />
HER2 is thought to be an orphan receptor, with<br />
none <strong>of</strong> the EGF family <strong>of</strong> ligands able to activate it.<br />
However, ErbB receptors dimerise on ligand binding, and<br />
HER2 is the preferential dimerisation partner <strong>of</strong> other<br />
1<br />
members <strong>of</strong> the ErbB family. The HER2 gene is a<br />
protooncogene located at the long arm <strong>of</strong> human chromosome<br />
2<br />
17(17q21-q22).<br />
HER2 and cancer<br />
Approximately 15-20 percent <strong>of</strong> breast cancers have an<br />
amplification <strong>of</strong> the HER2/neu gene or overexpression <strong>of</strong> its<br />
3<br />
protein product (Fig.3). Overexpression <strong>of</strong> this receptor in<br />
breast cancer is associated with increased disease recurrence<br />
and worse prognosis. Because <strong>of</strong> its prognostic role as well as<br />
its ability to predict response to trastuzumab (Herceptin US<br />
brand name), breast tumours are routinely checked for<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
2
Rajasekhar P- HER2/neu Vaccines fight against Breast Cancer<br />
Fig.3: Three-dimensional structure <strong>of</strong> the human epidermal growth<br />
factor 2 (HER-2) protein monomer with subdomains I-IV labelled<br />
Positive vs. Negative Test Results<br />
If the breast cancer is tested for HER2 status, the results will<br />
be graded as positive or negative. If the results are graded as<br />
HER2 positive, it means that the HER2 genes are overproducing<br />
the HER2 protein, and that those cells are growing<br />
rapidly and creating the cancer. If the results are graded HER2<br />
negative, then the HER2 protein is not causing the cancer.<br />
Treatment forHER2 positive breast cancer<br />
overexpression <strong>of</strong> HER2/neu. Overexpression also occurs in<br />
other cancer such as ovarian cancer, stomach cancer, and<br />
biologically aggressive forms <strong>of</strong> uterine cancer, such as<br />
4<br />
uterine serous endometrial carcinoma.<br />
The oncogene neu is so-named because it was derived from a<br />
rodent glioblastoma cell line, which is a type <strong>of</strong> neural<br />
tumour, hence 'neu.' HER2 is named because it has a similar<br />
structure to human epidermal growth factor receptor, or<br />
HER1. ErbB2 was named for its similarity to ErbB (avian<br />
erythroblastosis oncogene B), the oncogene later found to<br />
code for EGFR. Gene cloning showed that neu, HER2, and<br />
ErbB2 were the same.<br />
HER2 is co-localized, and thus most <strong>of</strong> the time co-amplified<br />
with the gene GRB7, which is also a proto-oncogene (active<br />
in e.g. breast cancer, testicular germ cell tumour, gastric<br />
cancer, and esophageal cancer).<br />
Tests for HER2 breast cancer<br />
ImmunoHistoChemistry (IHC) - this test measures the<br />
production <strong>of</strong> the HER2 protein by the tumour. The test results<br />
are ranked as 0, 1+, 2+, or 3+. If the results are 3+, the cancer is<br />
HER2-positive.<br />
Herceptin (trastuzumab) is a drug which is currently being<br />
used to treat HER2 positive breast cancer. It is a targeted<br />
therapy, and is also referred to as an immune treatment. This<br />
drug will be given intravenously, once every 2-3 weeks. Once<br />
it is in the regulatory system, Herceptin targets the HER2<br />
protein production (Fig. 4). This helps to stop the growth <strong>of</strong><br />
the HER2 positive cancer cells.<br />
Some results <strong>of</strong> Herceptin treatment include shrinkage <strong>of</strong><br />
HER2 positive tumours, before surgery; gets rid <strong>of</strong> HER2<br />
positive cancer cells that have spread beyond the original<br />
tumour and helps prevent recurrence (return) <strong>of</strong> the HER2<br />
positive cancer if it was a 2 cm or larger tumour, or if the<br />
cancer had spread to the lymph nodes.<br />
Clinically, HER2/neu is important as the target <strong>of</strong> the<br />
monoclonal antibody trastuzumab (marketed as Herceptin).<br />
Trastuzumab is only effective in breast cancer where the<br />
HER2/neu receptor is overexpressed. One <strong>of</strong> the mechanisms<br />
<strong>of</strong> how traztuzumab works after it binds to HER2 is by<br />
5<br />
increasing p27, a protein that halts cell proliferation.<br />
Overexpression <strong>of</strong> the HER2 gene can be suppressed by the<br />
amplification <strong>of</strong> other genes and the use <strong>of</strong> the drug Herceptin.<br />
Research is currently being conducted to discover which<br />
disregulated genes may have this desired effect. Another<br />
Fig.4: Trastuzumab complexed with HER-2 protein.s<br />
extracellular subdomain II<br />
Fluorescence In Situ Hybridization (FISH) - this test uses<br />
fluorescent probes to look at the number <strong>of</strong> HER2 gene copies<br />
in a tumour cell. If there are more than 2 copies <strong>of</strong> the HER2<br />
gene, then the cancer is HER2 positive.<br />
HER2 is a gene, is it inherited<br />
This genetic problem is not inherited from the parents. The<br />
most likely cause <strong>of</strong> this problem is aging, and wear and tear<br />
on the body. It is not yet known if environmental factors<br />
(pollution, smoke, fumes) are part <strong>of</strong> the cause <strong>of</strong> this<br />
problem.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
3
Rajasekhar P- HER2/neu Vaccines fight against Breast Cancer<br />
3<br />
monoclonal antibody, Pertuzumab , which inhibits<br />
dimerization <strong>of</strong> HER2 and HER3 receptors, is in advanced<br />
clinical trials.<br />
The expression <strong>of</strong> HER2/ERBB2 protein is regulated by<br />
estrogen receptors. Furthermore estradiol and tamoxifen<br />
acting through the estrogen receptor normally down regulates<br />
the expression <strong>of</strong> HER2/ERBB2. However when the ratio <strong>of</strong><br />
the coactivator AIB-3 exceeds that <strong>of</strong> the corepressor PAX2,<br />
the expression <strong>of</strong> HER2/ERBB2 is upregulated in the<br />
presence <strong>of</strong> tamoxifen leading to tamoxifen resistant breast<br />
6,7<br />
cancer.<br />
Vaccines to fight cancer<br />
A vaccine is a very common way <strong>of</strong> building up the immune<br />
system to fight infection. Using vaccines to fight breast cancer<br />
is relatively new, however, and still considered experimental.<br />
A vaccine for breast cancer may consist <strong>of</strong> an antigen cocktail<br />
<strong>of</strong> weakened or essentially dead elements <strong>of</strong> breast cancer<br />
cells that could stimulate an antibody response. The cancer<br />
vaccine might be prepared from one's own deactivated cancer<br />
cells, or from extracts <strong>of</strong> breast cancer cells cultivated in a<br />
laboratory. Vaccines like this are only available in clinical<br />
trials. But as soon as these vaccines are proven effective and<br />
win FDA-approval, they will become available outside <strong>of</strong><br />
clinical trials.<br />
The vaccine is given by injection (usually under the skin).<br />
Once the immune system becomes aware <strong>of</strong> the antigens in<br />
the vaccine, it responds by making antibodies. Hopefully<br />
these antibodies will able to attack and destroy any remaining<br />
cancer cells. Later, if any new cancer cells appear, the<br />
circulating antibodies <strong>of</strong> the vaccine-educated immune<br />
system would destroy them also.<br />
Challenges <strong>of</strong> cancer vaccines<br />
Although vaccines have a strong track record in fighting<br />
many serious infections (such as polio, mumps, and measles),<br />
they are very much in the experimental stage for cancer. One<br />
problem is the way cancer progresses. It begins when one <strong>of</strong><br />
the normal cells becomes abnormal and starts multiplying out<br />
<strong>of</strong> control, generation after generation. Each generation<br />
produces variations.<br />
Eventually the cancer has countless faces, with a limitless<br />
variety <strong>of</strong> antigens that need to be targeted by antibodies. The<br />
cancer vaccine, however, results in a limited number <strong>of</strong><br />
antibodies against the specific cancer cell antigens that were<br />
in the original vaccine preparation. These antibodies may not<br />
be effective against the full range <strong>of</strong> newly developing cancer<br />
cells.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
In addition, an effective vaccine must summon antibodies that<br />
target the bad cells and leave normal cells alone. The trick is to<br />
catch the cancer cells as soon as they form, and make the<br />
vaccine with cancer cell parts that are not shared by normal<br />
cells.<br />
Researchers are investigating ways to identify cancer cells at<br />
this very early stage. This could be done perhaps with<br />
chemicals that would tag the problem cells, and then alter<br />
them enough so that the immune system perceives them as<br />
abnormal and attacks them.<br />
Cancer patients can be immunized with vaccines<br />
targeting tumour antigens and develop antigen specific<br />
immune responses.<br />
Several cancer vaccine studies have demonstrated that<br />
patients can develop tumour antigen specific immune<br />
responses post-immunization, and that these immune<br />
responses are associated with only minimal side-effects. A<br />
variety <strong>of</strong> vaccine strategies, as well as vaccines targeting<br />
different tumour antigens, have been shown to be<br />
immunogenic using highly quantitative assays to assess the T<br />
cell response. As examples, in a recent phase I study, patients<br />
with advanced breast and ovarian cancer were vaccinated<br />
with autologous dendritic cells (DC) pulsed with HER2/neuor<br />
MUC1-derived peptides. Intracellular interferon gamma<br />
chromium (IFN) staining and Cr-release assays were used to<br />
assess response; peptide-specific cytotoxic T lymphocytes<br />
(CTL) were detected in five out <strong>of</strong> 10 patients In addition,<br />
MAGE3- and CEA peptide specific CD8+ T cells were<br />
observed in one patient treated with MUC1 peptide pulsed<br />
DCs and MUC1 peptide-specific T cells were observed in<br />
8<br />
another patient vaccinated with HER2/neu-derived peptides.<br />
Another strategy that elicited measurable tumour antigen<br />
specific immunity involved vaccination with a replicationdefective<br />
avipox vaccine containing the gene for CEA. In a<br />
phase I study, 20 patients with advanced CEA expressing<br />
carcinomas were immunized with the recombinant vaccine.<br />
Three different dose levels were used and the majority <strong>of</strong><br />
patients vaccinated with the two higher dose levels had<br />
statistically significant increases in CEA-specific CTL<br />
9<br />
precursors after vaccination, as compared to baseline. Two <strong>of</strong><br />
3 patients at the lowest dose also had a significant increase in<br />
precursor frequency after immunization. Finally, in a phase I<br />
study by Lee et al, forty-eight patients with high-risk resected<br />
stage III/IV melanoma were immunized with two tumour<br />
10<br />
antigen epitope peptides derived from gp100 and tyrosinase.<br />
The peptides, in incomplete Freud's adjuvant, were<br />
4
Rajasekhar P- HER2/neu Vaccines fight against Breast Cancer<br />
administered with or without IL-12. Thirty-seven <strong>of</strong> 42<br />
patients showed positive immune responses post vaccination<br />
by flow cytometry assays using tetramers constructed with<br />
gp100 and tyrosinase peptides. Studies such as these<br />
increasingly demonstrate that patients with cancer can be<br />
vaccinated against antigens expressed by their tumours.<br />
Clinical investigations are now focusing on what types <strong>of</strong><br />
immune responses generated would predict therapeutic<br />
efficacy and how to optimize immunity based on particular<br />
vaccine strategy.<br />
HER2/neu protein is a well-defined tumour antigen in<br />
variety <strong>of</strong> solid tumours and an established candidate<br />
antigen for eliciting tumour specific immunity<br />
The HER2/neu protein consists <strong>of</strong> an extracellular ligand<br />
binding domain, a short transmembrane domain, and<br />
11,12<br />
cytoplasmic protein tyrosine kinase domain. Binding <strong>of</strong><br />
ligand to the extracellular domain (ECD) leads to<br />
dimerization that stimulates the tyrosine kinase activity <strong>of</strong> the<br />
receptor and triggers autophosphorylation <strong>of</strong> residues within<br />
the intracellular cytoplasmic domain. These phosphorylated<br />
residues then serve as anchoring sites for signalling molecules<br />
involved in the regulation <strong>of</strong> intracellular signaling cascades<br />
11<br />
and, thus, malignant cell growth.<br />
HER2/neu protein is a good vaccine target from both a<br />
biologic and an immunologic standpoint. HER2/neu has been<br />
most extensively studied within the framework <strong>of</strong> breast<br />
cancer where it is known to be overexpressed in about 30% <strong>of</strong><br />
all breast cancer and is associated with a poor clinical<br />
13<br />
prognosis. Subsequently, it has been shown by many<br />
investigators that patients with a variety <strong>of</strong> different tumour<br />
types that overexpress the HER2/neu protein can have both<br />
14<br />
antibody and T cell immunity directed against HER2/neu.<br />
Investigations <strong>of</strong> HER2/neu specific antibodies in patients<br />
with breast cancer demonstrate that responses can be detected<br />
in patients with early stage disease indicating that the<br />
presence <strong>of</strong> antibodies is not simply a reflection <strong>of</strong> tumour<br />
15<br />
burden. Furthermore, detection <strong>of</strong> antibodies to HER2/neu<br />
also correlated to protein overexpression in the patient's<br />
primary tumour. Antibodies to HER2/neu have been found in<br />
the sera <strong>of</strong> patients with colon cancer; titers <strong>of</strong> >1:1000 were<br />
detected in 8 <strong>of</strong> 57 (14%) <strong>of</strong> patients with colorectal cancer<br />
compared to 0 <strong>of</strong> 200 (0%) <strong>of</strong> the normal control population.<br />
Similar to the immune response in breast cancer patients, the<br />
ability to detect HER2/neu antibodies correlated with<br />
overexpression <strong>of</strong> the protein in the patient's primary<br />
16<br />
tumour.<br />
Moreover, in prostate cancer detection <strong>of</strong> HER2/neu specific<br />
antibodies was most prevalent in the subgroup <strong>of</strong> patients<br />
17<br />
with androgen independent disease. Existent T cell<br />
immunity to the oncogenic protein, both T helper and CTL,<br />
have been detected in patients with HER2/neu<br />
overexpressing tumours. The identification <strong>of</strong> T-cells that can<br />
respond to HER2/neu indicates a portion <strong>of</strong> the T cell<br />
repertoire will recognize this self-antigen. CD4+ T cell<br />
responses were evaluated in patients with advanced stage<br />
18<br />
HER2/neu positive tumours. A minority, approximately<br />
10% <strong>of</strong> patients were found to have antibody and T cell<br />
immunity directed against HER2/neu. Cytotoxic T cells<br />
(CTL) capable <strong>of</strong> lysing HER2/neu overexpressing tumour<br />
cell lines have been identified in both the peripheral blood and<br />
tumours <strong>of</strong> patients bearing a variety <strong>of</strong> HER2/neu<br />
19-24<br />
overexpressing tumours. Testing <strong>of</strong> vaccine strategies<br />
targeting a tumour antigen where there is already some level<br />
<strong>of</strong> pre-existent immunity may facilitate assessment <strong>of</strong> the<br />
generation <strong>of</strong> immunity after vaccination. Presumably, it is<br />
easier to boost a low-level pre-existent immune response than<br />
prime naïve T cells to recognize a self-protein. Generating an<br />
active immune response directed against the HER2/neu<br />
protein has several potential clinical advantages. Portions <strong>of</strong><br />
this transmembrane protein are likely to be available to both<br />
the class I and II antigen processing pathways, thus,<br />
stimulating both a T helper cell and a cytotoxic T cell (CTL)<br />
immune response. In addition to CTL, antibody immunity<br />
could potentially be generated by active immunization<br />
against appropriate epitopes involved in receptor signalling.<br />
Durable concentrations <strong>of</strong> functional antibodies binding the<br />
extracellular domain (ECD) <strong>of</strong> the growth factor receptor<br />
could have therapeutic impact. Vaccination, if effective,<br />
would stimulate immunologic memory and could result in the<br />
prevention <strong>of</strong> relapse after standard therapy, such as surgery<br />
and radiation.<br />
HER2/neu protein serves as a model antigen for testing<br />
immunization strategies targeting self proteins<br />
Recent studies have identified self-proteins as tumour<br />
25-27<br />
antigens. These proteins are not mutated and are clearly<br />
25-27<br />
immunogenic in patients with cancer. Many <strong>of</strong> these<br />
proteins are present at much higher concentrations in<br />
malignant cells than in the normal cells. Indeed, the peptide<br />
repertoire display in the MHC when a protein is<br />
overexpressed may be distinctly different from the peptides<br />
present in resting MHC where that same protein is present at<br />
basal levels. HER2/neu vaccine development has focused on<br />
strategies that will allow tolerance to be circumvented. Early<br />
studies have evaluated peptide vaccines to stimulate<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
5
Rajasekhar P- HER2/neu Vaccines fight against Breast Cancer<br />
immunity to HER- 2/neu. The ability to mount an immune<br />
response is related to the immunodominance <strong>of</strong> specific<br />
antigenic determinants during natural immunologic<br />
processing <strong>of</strong> intact protein antigens.<br />
However, only a minor fraction <strong>of</strong> potential determinants in<br />
an antigen are presented in an immunodominant manner,<br />
28<br />
while the remaining peptides are ignored. Physiological<br />
mechanisms <strong>of</strong> immunologic tolerance to self prevent the<br />
induction <strong>of</strong> an immune response to self proteins, such as<br />
HER2/neu. Dominantly processed self-determinants are<br />
28,29<br />
thought to be efficient in tolerance induction. However, in<br />
every self-antigen, there are sequestered determinants that are<br />
unable to induce tolerance, therefore, could be<br />
28<br />
immunogenic. These subdominant epitopes may trigger the<br />
threshold for T-cell activation and immune recognition if they<br />
are presented in abundance, such as when a self-protein<br />
becomes overexpressed.<br />
Overexpression <strong>of</strong> the HER2/neu protein may result in<br />
subdominant peptides being presented in higher<br />
concentration in the major histocompatibility complex<br />
(MHC), thus, triggering a T cell response. Abundance <strong>of</strong><br />
subdominant epitopes in MHC molecules expressed on<br />
cancer cells could result in overexpressed self-proteins<br />
functioning as tumour specific antigens. An alternative<br />
hypothesis is that subdominant epitopes are more effectively<br />
presented by efficient antigen presenting cells (APC) such as<br />
dendritic cells (DC) and that DC are activated by<br />
inflammatory signals from the local tumour immune<br />
30<br />
microenvironment.<br />
Studies in animal models have shown that peptide based<br />
vaccines can effectively immunize against neu in animal<br />
models. Several groups have used rats as an experimental<br />
model for neu. Rat neu is highly homologous to human neu<br />
and has similar basal tissue distribution as human. Previous<br />
investigators had shown that rats could not be immunized<br />
with rat neu protein in the context <strong>of</strong> rat ECD in a vaccinia<br />
31<br />
vector. Subsequent investigations validated those findings<br />
by vaccinating rats with purified rat neu in a classic<br />
32<br />
immunization regimen Rats were tolerant to rat neu.<br />
However, rats could be effectively immunized with rat neu<br />
peptides designed for eliciting CD4+ T cell responses.<br />
Antibody and T cell responses specific for both the<br />
immunizing peptides and protein were generated in the<br />
32<br />
peptide immunized animals.<br />
Pre-clinical development <strong>of</strong> HER2/neu peptide based<br />
vaccines for the generation <strong>of</strong> T cell immunity<br />
Translating the development <strong>of</strong> peptide vaccines from<br />
animals into humans required the identification <strong>of</strong><br />
appropriate peptide epitopes. Both class I and class II binding<br />
peptides have been identified. Computer modeling programs<br />
have been effective in predicting potential immunogenic<br />
epitopes <strong>of</strong> self proteins such as HER2/neu and early studies<br />
have focused on evaluating constructed peptides for signs <strong>of</strong><br />
immune reactivity in patients with HER2/neu positive<br />
14<br />
tumours. Rongcun and colleagues identified HER2/neu<br />
specific HLA-A2.1 restricted CTL epitopes, which were able<br />
to elicit CTL that specifically killed peptide-sensitized target<br />
cells, and, most, importantly, a HER2/neu-transfected cell<br />
33<br />
line and autologous tumour cells.<br />
A similar strategy involves defining candidate epitopes by<br />
34<br />
their MHC-binding motif and class I affinity. Identified high<br />
affinity peptides are then tested for in vitro reactivity with<br />
peripheral blood mononuclear cells (PBMC) from normal<br />
donors and the ability to induce tumour reactive CTLs. Many<br />
peptides that bind A*0201 also exhibit degenerate binding to<br />
multiple alleles thus, an A2 supertype multi-epitope vaccine<br />
35<br />
could be designed to provide broad population coverage.<br />
Modelling programs to predict class II epitopes are also<br />
widely available. An example is the computer protein<br />
sequence analysis package, T Sites, which used two searching<br />
algorithms. The first is the AMPHI algorithm for identifying<br />
motifs according to charge and polarity patterns. The second<br />
is the Rothbard and Taylor algorithm for identifying motifs<br />
36<br />
according to charge and polarity patterns. Each <strong>of</strong> the<br />
searching algorithms has empirically been successful in<br />
identifying a substantial proportion (50-70%) <strong>of</strong> helper T cell<br />
36,37<br />
epitopes in foreign proteins. HER2/neu peptides predicted<br />
by both algorithms were constructed and were 15-18 amino<br />
14<br />
acids in length. PBMC, obtained from breast cancer patients<br />
with HER2/neu overexpressing tumours were analyzed for a<br />
proliferative T cell response to HER2/neu potential<br />
immunogenic peptides. Seven <strong>of</strong> 26 HER2/neu specific<br />
putative class II peptides tested demonstrated the ability to<br />
elicit T cell responses, in vitro, in at least 20% <strong>of</strong> breast cancer<br />
14<br />
patients evaluated.<br />
The ability <strong>of</strong> a single peptide to generate immune responses<br />
in multiple individuals <strong>of</strong> diverse MHC backgrounds is not<br />
unique. Universal epitopes for class II have been defined for<br />
38,39<br />
tetanus toxoid. Investigations such as those described<br />
above, lay the foundation for the first generation <strong>of</strong> human<br />
clinical trials <strong>of</strong> HER2/neu specific cancer vaccines, focusing<br />
on peptide immunization.<br />
Human clinical trials <strong>of</strong> vaccines targeting the HER2/neu<br />
oncogenic protein; generating T cell immunity<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 6
Rajasekhar P- HER2/neu Vaccines fight against Breast Cancer<br />
Vaccines designed to stimulate a cytotoxic T cell response<br />
to HER2/neu<br />
The cytotoxic T cell has been considered the primary effector<br />
cell <strong>of</strong> the immune system capable <strong>of</strong> eliciting an anti-tumour<br />
response. The predominant experimental method <strong>of</strong><br />
stimulating a CTL response in vivo has been to vaccinate<br />
individuals with tumour cells or viruses recombinant for<br />
tumour antigens that can infect viable cells so that proteins are<br />
expressed inside the cell and are processed and presented in<br />
the MHC class I antigen processing pathway. An alternative<br />
effective vaccination strategy to elicit CTL uses a single<br />
soluble peptide that is identical or similar to naturally<br />
processed peptides that are present in class I MHC molecules<br />
along with adjuvant. An HLA-A2 binding peptide, p369-377,<br />
derived from the protein sequence <strong>of</strong> HER 2/neu ECD has<br />
been used extensively in clinical trials to generate CTL<br />
specific for cells overexpressing HER2/neu in vivo via active<br />
immunization.<br />
In an initial clinical study, HLA-A2 positive patients with<br />
metastatic HER2/neu overexpressing breast, ovarian, or<br />
colorectal carcinomas were immunized with 1 mg <strong>of</strong> p369-<br />
377 admixed in incomplete Freund's adjuvant (IFA) every 3<br />
40<br />
weeks. Peptide specific CTL were isolated and expanded<br />
from the peripheral blood <strong>of</strong> patients after 2 or 4<br />
immunizations. The CTL could lyse HLA matched peptide<br />
pulsed target cells but could not lyse HLA matched tumours<br />
expressing the HER2/neu protein. Even when tumours were<br />
treated with IFN to upregulate class I, the CTL lines generated<br />
from the patients would not respond to the peptide presented<br />
endogenously on tumour cells. An additional problem in<br />
using single HLA binding epitopes is that without CD4+ T-<br />
cell help, responses generated are short lived and nondurable.<br />
More recently a similar study was performed,<br />
immunizing patients with p369-377 using GM-CSF as an<br />
41<br />
adjuvant. GMCSF is a recruitment and maturation factor for<br />
skin DC, Langerhans cells (LC) and theoretically may allow<br />
more efficient presentation <strong>of</strong> peptide epitopes than standard<br />
adjuvants such as IFA.<br />
Six HLA-A2 patients with HER2/neu-overexpressing<br />
cancers received 6 monthly vaccinations with 500 mcg <strong>of</strong><br />
HER2/neu peptide, p369-377, admixed with 100 mcg <strong>of</strong> GM-<br />
CSF. The patients had either stage III or IV breast or ovarian<br />
cancer. Immune responses to the p369-377 were examined<br />
using an IFN ELIspot assay. Prior to vaccination, the median<br />
precursor frequency, defined as precursors/106 PBMC, to<br />
p369-377 was not detectable. Following vaccination,<br />
HER2/neu peptide-specific precursors developed to p369-<br />
377 in just 2 <strong>of</strong> 4 evaluable subjects. The responses were<br />
short-lived and not detectable at 5 months after the final<br />
vaccination. Immunocompetence was evident as patients had<br />
detectable T cell responses to tetanus toxoid and influenza.<br />
These results demonstrate that HER2/neu MHC class I<br />
epitopes can induce HER2/neu peptide-specific IFNproducing<br />
CD8+ T cells. However, the magnitudes <strong>of</strong> the<br />
responses were low, as well as short-lived. Theoretically, the<br />
addition <strong>of</strong> CD4+ T cell help would allow the generation <strong>of</strong><br />
lasting immunity.<br />
A successful vaccine strategy in generating peptide specific<br />
CTL capable <strong>of</strong> lysing tumour expressing HER2/neu and<br />
resulting in durable immunity involved immunizing patients<br />
with putative T-helper epitopes <strong>of</strong> HER2/neu which had,<br />
embedded in the natural sequence, HLA-A2 binding motifs <strong>of</strong><br />
HER2/neu. Thus, both CD4+ T cell help and CD8+ specific<br />
epitopes were encompassed in the same vaccine. In this trial,<br />
19 HLA-A2 patients with HER2/neu overexpressing cancers<br />
received a vaccine preparation consisting <strong>of</strong> putative<br />
42<br />
HER2/neu helper peptides. Contained within these<br />
sequences were the HLA-A2 binding motifs. Patients<br />
developed both HER2/neu specific CD4+ and CD8+ T cell<br />
responses. The level <strong>of</strong> HER2/neu immunity was similar to<br />
viral and tetanus immunity. In addition, the peptide-specific T<br />
cells were able to lyse tumour. The responses were long-lived<br />
and detectable for greater than 1 year after the final<br />
vaccination in selected patients. These results demonstrate<br />
that HER2/neu MHC class II epitopes containing<br />
encompassed MHC class I epitopes are able to induce longlasting<br />
HER2/neu-specific IFN-producing CD8 T cells.<br />
Vaccines designed to stimulate a T helper response to<br />
HER2/neu<br />
Pre-existent immune responses to HER2/neu are <strong>of</strong> low<br />
magnitude. Stimulating an effective T helper response is a<br />
way to boost antigen specific immunity as CD4+ T-cells<br />
generate the specific cytokine environment required to<br />
support an evolving immune response. Furthermore, either<br />
CTL or antibody immunity may have an effect on HER2/neu<br />
overexpressing tumour growth. Targeting CD4+ T cells in a<br />
vaccine strategy would result in the potential to augment<br />
either <strong>of</strong> these arms <strong>of</strong> the immune system.<br />
Putative T helper subdominant peptide epitopes, derived from<br />
the HER2/neu protein sequence, were predicted by computer<br />
modeling, and screened for immune reactivity using PBMC<br />
14<br />
from patients with breast and ovarian cancer. Vaccines were<br />
generated each composed <strong>of</strong> three different peptides, each 15-<br />
18 amino acids in length . Patients with advanced stage<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 7
Rajasekhar P- HER2/neu Vaccines fight against Breast Cancer<br />
HER2/neu overexpressing breast, ovarian, and non-small cell<br />
lung cancer were enrolled and 38 patients finished the<br />
43<br />
planned course <strong>of</strong> 6 immunizations. Patients received 500<br />
mcg <strong>of</strong> each peptide admixed in GM-CSF in an effort to<br />
44<br />
mobilize LC in vivo as an adjuvant to peptide immunization.<br />
Ninety-two percent <strong>of</strong> patients developed T cell immunity to<br />
HER2/neu peptides and over 60% to a HER2/neu protein<br />
domain. Thus, immunization with peptides resulted in the<br />
generation <strong>of</strong> T cells that could respond to protein.<br />
Furthermore, at 1-year followup, immunity to the HER2/neu<br />
protein persisted in 38% <strong>of</strong> patients. Immunity elicited by<br />
active immunization with CD4+ T helper epitopes was<br />
durable. An additional finding <strong>of</strong> this study was that epitope<br />
spreading was observed in 84% <strong>of</strong> patients and significantly<br />
correlated with the generation <strong>of</strong> HER2/neu protein-specific<br />
T cell immunity (p=0.03). Epitope, or determinant spreading,<br />
45<br />
is a phenomenon first described in autoimmune disease and<br />
has been associated with both MHC Class I- and MHC Class<br />
46,47<br />
II-restricted responses. Epitope spreading represents the<br />
generation <strong>of</strong> an immune response to a particular portion <strong>of</strong> an<br />
immunogenic protein and then the natural spread <strong>of</strong> that<br />
immunity to other areas <strong>of</strong> the protein or even to other<br />
antigens present in the environment. In this study, epitope<br />
spreading reflected the extension <strong>of</strong> a significant T cell<br />
immune response to portions <strong>of</strong> the HER2/neu protein that<br />
were not contained in the patient's vaccine. Epitope spreading<br />
represents a broadening <strong>of</strong> the immune response and could<br />
indicate endogenous processing <strong>of</strong> antigen at sites <strong>of</strong><br />
30<br />
inflammation initiated by a specific T cell response. That is,<br />
the initial immune response can create a microenvironment at<br />
the tumour-site that enhances the presence <strong>of</strong> local immune<br />
effector cells present. These immune cells, e.g. APC and T<br />
cells, may begin to respond more effectively to tumour<br />
antigen that is present in the body. Another recently reported<br />
vaccine trial immunizing breast and ovarian cancer patients<br />
with autologous DC pulsed with MUC-1 or HER2/neu<br />
8<br />
peptides resulted in epitope spreading. In this trial 10 patients<br />
were immunized. Half the patients developed CD8+ T cell<br />
precursors to their immunizing peptides.<br />
Moreover, some patients developed new immunity to other<br />
tumour antigens expressed in their cancers such as CEA and<br />
MAGE-3. Most clinical trials <strong>of</strong> cancer vaccines focus on the<br />
detection <strong>of</strong> a newly generated immune response or the<br />
magnitude <strong>of</strong> the antigen specific immune response elicited<br />
after active immunization. However, if epitope spreading<br />
indicates an immune microenvironment capable <strong>of</strong> producing<br />
an endogenous polyclonal immune response, it may be an<br />
endpoint that could potentially reflect an improved clinical<br />
outcome.<br />
Methods to augment immunity to HER2/neu in clinical<br />
trials <strong>of</strong> HER2/neu specific vaccines<br />
Recent studies have evaluated vaccine strategies focused to<br />
maximize the role <strong>of</strong> the most efficient APC, the DC or skin<br />
LC, in eliciting effective immunity to self. One such strategy<br />
is to use cytokines involved in DC production and maturation<br />
as vaccine adjuvants. Flt3-ligand (FL) is a cytokine which,<br />
when administered systemically, can increase numbers <strong>of</strong><br />
48<br />
circulating DC greater than 40 fold. Human DC generated by<br />
the administration <strong>of</strong> FL have been shown to be functional and<br />
48<br />
can stimulate T cells in vitro. Furthermore, activation <strong>of</strong> DC<br />
in vivo by FL has been shown to be an effective way <strong>of</strong><br />
circumventing tolerance during active immunization in<br />
49<br />
animal models. Studies have been performed in the neu<br />
transgenic mouse, immunizing the animals to a self-tumour<br />
antigen, neu, using FL as a vaccine adjuvant to mobilize DC in<br />
50<br />
vivo. The timing <strong>of</strong> vaccine administration corresponded to<br />
51,52<br />
the kinetics <strong>of</strong> in vivo DC mobilization in animals ; early<br />
administration when few circulating DC are present,<br />
midpoint administration when DC precursors are increasing<br />
the peripheral blood, and finally vaccination at the end <strong>of</strong> the<br />
FL cycle when DC are at peak concentrations. During a 10-<br />
day administration <strong>of</strong> FL a HER2/neu ICD protein vaccine<br />
was administered at 3 time-points. Animals receiving the<br />
vaccine midpoint in the FL cycle generated HER2/neu ICD<br />
specific immunity whereas mice immunized at the end <strong>of</strong> the<br />
FL cycle did not. In general, neu specific immunity generated<br />
using FL resulted in T cells that predominantly secreted IFN, a<br />
Type 1 associated cytokine, rather than IL-4, a Type 2<br />
50<br />
associated cytokine.<br />
Mobilizing DC in vivo as a vaccine adjuvant to augment<br />
HER2/neu specific immunity<br />
Based on the data generated in rodent models, 10 patients with<br />
HER2/neu overexpressing cancers were enrolled to receive a<br />
HER2/neu peptide-based vaccine targeting the ICD <strong>of</strong> the<br />
53<br />
HER2/neu protein. The peptides in the vaccine were the<br />
same as those used in one <strong>of</strong> the arms <strong>of</strong> the trial described<br />
43<br />
above. All patients received FL 20 mcg/kg/day s.c. for 14<br />
days. Five patients received the HER2/neu peptide-based<br />
vaccine alone intradermally midpoint in one FL cycle and 5<br />
patients received the vaccine admixed with 150 mcg <strong>of</strong> GM-<br />
CSF intradermally midpoint in the FL cycle. Including FL as a<br />
vaccine adjuvant was effective in boosting the precursor<br />
frequency <strong>of</strong> IFN secreting HER2/neu specific T cells. After<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 8
Rajasekhar P- HER2/neu Vaccines fight against Breast Cancer<br />
the completion <strong>of</strong> all immunizations, patients in each group<br />
developed detectable IFN producing T cell specific for the<br />
ICD protein. The small sample size <strong>of</strong> each group, however,<br />
did not allow a statistically significant comparison <strong>of</strong> immune<br />
responses between the FL alone and FL with GM-CSF arms.<br />
Recent investigations have demonstrated FL and GM-CSF<br />
may stimulate different subsets <strong>of</strong> DC in vivo and that the<br />
cytokine microenvironment elicited, either Type 1 or Type 2,<br />
is markedly influenced by the particular DC subset generated.<br />
Evaluating a murine model <strong>of</strong> cancer, using tumours<br />
engineered to express either GM-CSF or FL, demonstrated<br />
GM-CSF engineered cells were more potent in inducing an<br />
54<br />
anti-tumour response. GM-CSF elicited a diverse cytokine<br />
environment consisting <strong>of</strong> both Th1 and Th2 immune<br />
effectors. In contrast, immune responses generated with FL<br />
expressing tumour cells were specifically restricted to a Th1<br />
54<br />
phenotypic response. Data from human clinical trials using<br />
FL as a vaccine adjuvant support that FL is associated with the<br />
development <strong>of</strong> a strong Type 1 response. The detection <strong>of</strong><br />
antigen specific cytokine production without concomitant<br />
measurable clonal proliferation has been reported and is<br />
potentially a reflection <strong>of</strong> a strongly restricted Type 1<br />
55<br />
response.<br />
Balancing immunity with autoimmunity in cancer<br />
vaccine development<br />
The addition <strong>of</strong> FL in the vaccine regimen was associated with<br />
the development <strong>of</strong> autoimmune phenomenon in some<br />
patients. In general, the vaccine regimens including FL were<br />
well tolerated. One patient had grade 1 serologic<br />
abnormalities (ANA, anti-SSA, anti-dsDNA). A second<br />
patient, who had Stage IV breast cancer, developed grade 2<br />
toxicity with serologic abnormalities and self limiting Sicca<br />
syndrome characterized by dry eyes and dry mouth 3 months<br />
after the completion <strong>of</strong> the vaccine regimen. This patient did<br />
not develop any detectable immunity to HER2/neu peptides<br />
or protein after active immunization. None <strong>of</strong> the patients<br />
immunized on any reported HER2/neu specific vaccine trial<br />
developed any evidence <strong>of</strong> autoimmune phenomenon<br />
directed against tissues that express basal levels <strong>of</strong><br />
HER2/neu.<br />
HER2/neu specific vaccines designed at stimulating<br />
functional antibody immunity<br />
Studies in both animals and human demonstrate that infusion<br />
<strong>of</strong> high concentrations <strong>of</strong> neu specific antibodies can mediate<br />
an anti-tumour response. For example, in a murine breast<br />
cancer tumour model, investigators show that 50% <strong>of</strong> animals<br />
did not spontaneously develop breast cancer when treated<br />
56<br />
with a neu-specific antibody directed against the ECD.<br />
These successful results in animal models have been<br />
translated to human clinical trials. Several investigations<br />
indicate passive HER2/neu antibody infusion may have a<br />
marked therapeutic effect in patients with HER2/neu<br />
57,58<br />
overexpressing tumours. Recent clinical trials show an<br />
overall response rate <strong>of</strong> 26% when a HER2/neu specific<br />
monoclonal antibody, trastuzumab, is used as first line<br />
59<br />
monotherapy. Furthermore, when trastuzmab was used in<br />
conjunction with chemotherapy in patients with metastatic<br />
HER2/neu overexpressing breast cancer, a longer time to<br />
disease progression, overall response rate, and longer<br />
duration <strong>of</strong> response was observed than in those patients who<br />
58<br />
received chemotherapy alone. Data such as these are<br />
evidence that an antibody response against HER2/neu may<br />
have a therapeutic benefit. In addition, studies <strong>of</strong> antibody<br />
infusion provide a target concentration target for the level <strong>of</strong><br />
antibody needed to potentially mediate that anti-tumour<br />
60<br />
response. The drawback with passive antibody infusion,<br />
however, is that the monoclonal antibodies are short-lived and<br />
are cleared from the circulation. A vaccine strategy, which<br />
would generate an endogenous antibody response may result<br />
in more durable antibody levels. This type <strong>of</strong> strategy would<br />
be potentially useful in both treatment <strong>of</strong> HER2/neu<br />
overexpressing cancer and protection from tumour<br />
recurrence or development.<br />
Generation <strong>of</strong> HER2/neu specific antibody immunity<br />
after a peptide based vaccine<br />
Antibody responses were assessed in the patients immunized<br />
with a HER2/neu peptide based vaccine designed to elicit T<br />
43<br />
helper responses. The peptides chosen for immunization<br />
14<br />
were potential T helper epitopes. Vaccinating patients to<br />
augment a CD4+ T cell response, however, may stimulate a<br />
concomitant B cell response to neu as has been shown in<br />
32<br />
animal models. Sixty-two patients were evaluable for the<br />
assessment <strong>of</strong> antibody immunity to HER2/neu. Forty-seven<br />
percent <strong>of</strong> all patients developed an antibody response to<br />
HER2/neu peptides, range 0-21.6 mcg/ml. Antibody<br />
responses to the HER2/neu protein, after peptide<br />
immunizations however, were detected in only 23% <strong>of</strong><br />
patients, range 0-9.3 mcg/ml. Furthermore, the magnitude <strong>of</strong><br />
the HER2/neu protein specific antibody response elicited<br />
after peptide immunization was <strong>of</strong> lower magnitude than the<br />
antibody response generated to a control foreign antigen<br />
immunization with KLH (mean 0.5 mcg/ml vs. mean 16.5<br />
mcg/ml respectively).<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 9
Rajasekhar P- HER2/neu Vaccines fight against Breast Cancer<br />
HER2/neu specific monoclonal antibodies, such as<br />
trastuzumab, have been shown to elicit an anti-tumour<br />
response when used alone or in combination with<br />
58,59<br />
chemotherapy. In preclinical models, inhibition <strong>of</strong> tumour<br />
growth required antibody concentrations between 1 and 23<br />
60<br />
mcg/ml. Clinical studies <strong>of</strong> trastuzumab have targeted a<br />
minimum serum trough concentration <strong>of</strong> 10 mcg/ml as a level<br />
61<br />
considered necessary for a therapeutic response in humans.<br />
The level <strong>of</strong> HER2/neu specific antibodies elicited on this<br />
study did not fall into the range <strong>of</strong> what would be expected to<br />
stimulate a therapeutic response. Preclinical investigations<br />
are ongoing to determine peptide epitopes that may elicit<br />
functional HER2/neu specific antibody immunity.<br />
Defining functional HER2/neu specific antibody epitopes<br />
for use in cancer vaccines<br />
Another aspect <strong>of</strong> peptide epitope prediction would be to<br />
identify peptide portions <strong>of</strong> the HER2/neu ECD that would be<br />
appropriate to target with an antibody response. Although<br />
many HER2/neu specific antibodies inhibit the growth <strong>of</strong><br />
cancer cells, some antibodies have no effect on cell growth,<br />
62<br />
while others even actively stimulate cancer growth. This<br />
wide range <strong>of</strong> biological effects is thought to be related to the<br />
epitope specificity <strong>of</strong> the antibodies and to consequent<br />
62<br />
changes in receptor signalling. An alternative to the use <strong>of</strong><br />
passive antibody therapy would be active immunization<br />
against the HER2/neu ECD. However, inappropriately<br />
induced immune responses could have untoward effects on<br />
cancer growth. Therefore, it is crucial to identify epitopes on<br />
HER2/neu that are targeted by stimulatory and inhibitory<br />
antibodies in order to ensure the induction <strong>of</strong> a beneficial<br />
endogenous antibody response.<br />
In a recent study, investigators constructed HER2/neu gene<br />
fragment phage display libraries to epitope-map a number <strong>of</strong><br />
HER2/neu specific antibodies with different biological<br />
62<br />
effects on tumour cell growth. Regions responsible for<br />
opposing effects <strong>of</strong> antibodies were identified and then used<br />
to immunize mice. The epitopes <strong>of</strong> three antibodies, N12,<br />
N28, and L87 were successfully located to peptide epitope<br />
binding regions <strong>of</strong> HER2/neu. While N12 inhibited tumour<br />
cell proliferation, N28 stimulated the proliferation <strong>of</strong> a subset<br />
<strong>of</strong> breast cancer cell lines overexpressing HER2/neu. The<br />
peptide region recognized by N12 was used as an immunogen<br />
to selectively induce an inhibitory immune response in mice.<br />
Mice immunized with the peptide developed antibodies that<br />
recognized both the peptide and native HER2/neu. More<br />
importantly, HER2/neu specific antibodies purified from<br />
mouse sera were able to inhibit up to 85% <strong>of</strong> tumour cell<br />
proliferation in vitro. This study provides direct evidence <strong>of</strong><br />
the functional relationship <strong>of</strong> HER2/neu specific antibodies<br />
generated by active immunization. Using peptide regions that<br />
contain multiple inhibitory B cell epitopes is likely to be<br />
63<br />
superior to the use <strong>of</strong> single epitope immunogens.<br />
CONCLUSION<br />
Since the HER2/neu protein was first identified a decade ago<br />
significant progress has been made in understanding the<br />
function <strong>of</strong> the molecule in cancer initiation as well as the<br />
development <strong>of</strong> HER2/neu targeted therapies that are in<br />
human clinical trials today. Whereas passive infusion <strong>of</strong><br />
HER2/neu specific antibodies has already shown great<br />
promise as a therapeutic, active immunization with<br />
HER2/neu specific vaccines are just starting human clinical<br />
trials. Although effective immunization <strong>of</strong> cancer patients is a<br />
significant scientific hurdle, it is one that can be<br />
accomplished. The prevention <strong>of</strong> recurrence <strong>of</strong> HER2/neu<br />
overexpressing tumours would be aided by the development<br />
<strong>of</strong> an anti-tumour immune response and the generation <strong>of</strong><br />
immunologic memory specific for HER2/neu after effective<br />
vaccination.<br />
Ultimately, we will be using the best defense to fight cancer,<br />
the human immune system. It is a very challenging thing to<br />
do. We hope we have reached a point where we can make it<br />
useful to patients.<br />
Abbreviations<br />
APC: antigen presenting cell; CEA: carcinoembryonic<br />
antigen; CTL: cytotoxic T cell; DC: dendritic cell; ECD:<br />
extracellular domain; FL: Flt-3 Ligand; GM-CSF:<br />
granulocyte macrophage stimulating factor; HLA: human<br />
leukocyte antigen; ICD: intracellular domain; IFA:<br />
incomplete Freund's adjuvant; IFN: interferon gamma; IL:<br />
interleukin; IVS: in vitro stimulation; LC: Langerhans cell;<br />
MHC: major histocompatibility antigen; MUC: mucin;<br />
NSCLC: non-small cell lung cancer; PBMC: peripheral blood<br />
mononuclear cell; TCR: T cell receptor; Th: T helper cell.<br />
REFERENCES<br />
1. Olayioye MA. Update on HER2 as a target for cancer<br />
therapy: intracellular signalling pathways ErbB2/HER2<br />
and family members. Breast Cancer Res 2001;<br />
3(6):385–389.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 10
Rajasekhar P- HER2/neu Vaccines fight against Breast Cancer<br />
2. Coussens L, Yang-Feng TL, Liao YC, Chen E, Gray A,<br />
Mc Grath J, Seeburg PH, Libermann TA. Tyrosine<br />
Kinase Receptor with Extensive Homology to EGF<br />
Receptor Shares Chromosomal Location with neu<br />
Oncogene. Science 1985; 230(4730):1132–1139.<br />
3. Entrez Gene: ErbB2 v-erb-b2 erythroblastic leukemia<br />
viral oncogene homologue 2, neuro/glioblastoma derived<br />
o n c o g e n e h o m o l o g u e ( a v i a n ) .<br />
http://www.ncbi.nlm.nih.gov/sites/entrezDb=gene&C<br />
md=ShowDetailView&TermToSearch=2064.<br />
4. Santin AD, Bellone S, Roman JJ, McKenney JK,<br />
Pecorelli S. Trastuzumab treatment in patients with<br />
advanced or recurrent endometrial carcinoma<br />
overexpressing HER2/neu. Int J Gynaecol Obstet 2008;<br />
102(2):128–131.<br />
5. Le XF, Franz P, Robert B. HER2-targeting antibodies<br />
modulate the cyclin-dependent kinase inhibitor p27Kip1<br />
via multiple signaling pathways. Cell Cycle 2005;<br />
4(1):87–95.<br />
6. Study sheds new light on tamoxifen resistance. Cordis<br />
News. Cordis. 2008. http://cordis.europa.eu/fetch<br />
CALLER=EN_NEWS&ACTION=D&SESSION=&R<br />
CN=30093.<br />
7. Hurtado A, Holmes KA, Geistlinger TR, Hutcheson IR,<br />
Nicholson RI, Brown M., et.al. Regulation <strong>of</strong> ERBB2 by<br />
oestrogen receptor-PAX2 determines response to<br />
tamoxifen. Nature 2008; 456 (7222): 663.<br />
8. Brossart P, Wirths S, Stuhler G. Induction <strong>of</strong> cytotoxic T-<br />
lymphocyte responses in vivo after vaccinations with<br />
peptide-pulsed dendritic cells. Blood 2000; 96:3102-<br />
3108.<br />
9. <strong>Mar</strong>shall JL, Hawkins MJ, Tsang KY. Phase I study in<br />
cancer patients <strong>of</strong> a replication-defective avipox<br />
recombinant vaccine that expresses human<br />
carcinoembryonic antigen. J Clin Oncol 1999; 17:332-<br />
337.<br />
10. Lee P, Wang F, Kuniyoshi J. Effects <strong>of</strong> interleukin-12 on<br />
the immune response to a multipeptide vaccine for<br />
resected metastatic melanoma. J Clin Oncol 2001;<br />
19:3836-3847.<br />
11. Olayioye MA, Neve RM, Lane HA, Hynes NE. The ErbB<br />
signaling network: receptor heterodimerization in<br />
development and cancer. Embo J 2000; 19:3159-3167.<br />
12. Samanta A, LeVea CM, Dougall WC, Qian X, Greene MI.<br />
Ligand and p185c-neu density govern receptor<br />
interactions and tyrosine kinase activation. Proc Natl<br />
Acad Sci 1994; 91:1711-1715.<br />
13. Slamon DJ, Clark GM, Wong SG. Human breast cancer:<br />
correlation <strong>of</strong> relapse and survival with amplification <strong>of</strong><br />
the HER2/neu oncogene. Science 1987; 235:177-182.<br />
14. Disis ML, Cheever MA. HER2/neu oncogenic protein:<br />
issues in vaccine development. Crit Rev Immunol 1998;<br />
18:37-45.<br />
15. Disis ML, Pupa SM, Gralow JR. High-titer HER2/neu<br />
protein-specific antibody can be detected in patients with<br />
early-stage breast cancer. J Clin Onc 1997; 15:3363-<br />
3367.<br />
16. Ward RL Hawkins N, Coomber D, Disis ML Antibody<br />
immunity to the HER2/neu oncogenic protein in patients<br />
with colorectal cancer. Hum Immunol 1999; 60:510-515.<br />
17. McNeel DG, Nguyen LD, Storer BE. Antibody immunity<br />
to prostate cancer associated antigens can be detected in<br />
the serum <strong>of</strong> patients with prostate cancer. J Urol 2000;<br />
164:1825-1829.<br />
18. Disis ML, Knutson KL, Schiffman K, Rinn K, McNeel<br />
DG. Pre-existent immunity to the HER2/neu oncogenic<br />
protein in patients with HER2/neu overexpressing breast<br />
and ovarian cancer. Breast Cancer Res Treat 2000;<br />
62:245-252.<br />
19. Ioannides CG, Whiteside TL. T cell recognition <strong>of</strong> human<br />
tumours: implications for molecular immunotherapy <strong>of</strong><br />
cancer. Clin Immunol Immunopathol 1993; 66:91-106.<br />
20. Yoshino I, Goedegebuure PS, Peoples GE. HER2/neuderived<br />
peptides are shared antigens among human nonsmall<br />
cell lung cancer and ovarian cancer. Cancer Res<br />
1994; 54:3387-3390.<br />
21. Peoples GE, Goedegebuure PS, Smith R. Breast and<br />
ovarian cancer-specific cytotoxic T lymphocytes<br />
recognize the same HER2/neu-derived peptide. Proc Natl<br />
Acad Sci, USA 1995; 92:432-436.<br />
22. Peiper M, Goedegebuure PS, Izbicki JR, Eberlein TJ.<br />
Pancreatic cancer associated ascites-derived CTL<br />
recognize a nine-amino- acid peptide GP2 derived from<br />
HER2/neu. Anticancer Res 1999; 19:2471-2475.<br />
23. Brossart P, Stuhler G, Flad T. HER2/neu-derived peptides<br />
are tumour-associated antigens expressed by human renal<br />
cell and colon carcinoma lines and are recognized by in<br />
vitro induced specific cytotoxic T lymphocytes. Cancer<br />
Res 1998. 58:732-736.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 11
Rajasekhar P- HER2/neu Vaccines fight against Breast Cancer<br />
24. Kono K, Rongcun Y, Charo J. Identification <strong>of</strong><br />
HER2/neu-derived peptide epitopes recognized by<br />
gastric cancer-specific cytotoxic T lymphocytes. Int J<br />
Cancer 1998; 78:202- 208.<br />
25. Pardoll DM. A new look for the 1990s. Nature 1994;<br />
369:357-358.<br />
26. Houghton AN. Cancer antigens: immune recognition <strong>of</strong><br />
self and altered self. J Exp Med 1994; 180:1-4.<br />
27. Disis ML, Cheever MA. Oncogenic proteins as tumour<br />
antigens. In: Alt F, <strong>Mar</strong>rack P, eds. Current Opinion in<br />
Immunology. Vol. 5. London: Current Biology Ltd.;<br />
1996; 637-642.<br />
28. Sercarz EE, Lehmann PV, Ametani A. Dominance and<br />
crypticity <strong>of</strong> T cell antigenic determinants. Annu Rev<br />
Immunol 1993; 11:729-766.<br />
29. Nanda NK, Sercarz EE. Induction <strong>of</strong> anti-self-immunity<br />
to cure cancer. Cell 1995. 82:13- 17.<br />
30. Sercarz EE. Driver clones and determinant spreading. J<br />
Autoimmun 2000; 14:275-277.<br />
31. Bernards R, Destree A, McKenzie S. Effective tumour<br />
immunotherapy directed against an oncogene-encoded<br />
product using a vaccinia virus vector. Proc Natl Acad Sci<br />
U S A 1987; 84:6854-6858.<br />
32. Disis ML, Gralow JR, Bernhard H. Peptide-based, but not<br />
whole protein, vaccines elicit immunity to HER2/neu, an<br />
oncogenic self-protein. J Immunol 1996; 156:3151-3158.<br />
33. Rongcun Y, Salazar-Onfray F, Charo J. Identification <strong>of</strong><br />
new HER2/neu-derived peptide epitopes that can elicit<br />
specific CTL against autologous and allogeneic<br />
carcinomas and melanomas. J Immunol 1999; 163:1037-<br />
1044.<br />
34. Keogh E, Fikes J, Southwood S. Identification <strong>of</strong> new<br />
epitopes from four different tumour-associated antigens:<br />
recognition <strong>of</strong> naturally processed epitopes correlates<br />
with HLA-A0201-binding affinity. J Immunol 2001;<br />
167:787-796.<br />
35. Feller DC de la Cruz V. Identifying antigenic T-cell sites.<br />
Nature 1991; 349:720-721.<br />
36. Roscoe DM, Jung SH, Benhar I. Primate antibody<br />
response to immunotoxin: serological and computeraided<br />
analysis <strong>of</strong> epitopes on a truncated form <strong>of</strong><br />
Pseudomonas exotoxin. Infect Immun 1994; 62:5055-<br />
5065.<br />
37. Bisset LR, Fierz W. Using a neural network to identify<br />
potential HLA-DR1 binding sites within proteins. J Mol<br />
Recognit 1993; 6:41-48.<br />
38. Panina-Bordignon P, Tan A, Termijtelen A. Universally<br />
immunogenic T cell epitopes: promiscuous binding to<br />
human MHC class II and promiscuous recognition by T<br />
cells. Eur J Immunol 1989; 19:2237-2242.<br />
39. Valmori D, Sabbatini A, Lanzavecchia A, Corradin G,<br />
Matricardi PM. Functional analysis <strong>of</strong> two tetanus toxin<br />
universal T cell epitopes in their interaction with DR1101<br />
and DR1104 alleles. J Immunol 1994; 152:2921-2929.<br />
40. Zaks TZ, Rosenberg SA Immunization with a peptide<br />
epitope (p369-377) from HER2/neu leads to peptidespecific<br />
cytotoxic T lymphocytes that fail to recognize<br />
HER2/neu+ tumours. Cancer Res 1998; 58:4902-4908.<br />
41. Knutson KL, Schiffman K, Cheever MA, Disis ML.<br />
Immunization <strong>of</strong> cancer patients with a HER2/neu, HLA-<br />
A2 peptide, p369- 377, results in short-lived peptidespecific<br />
immunity. Clin Cancer Res 2002; 8:1014-1018.<br />
42. Knutson KL, Schiffman K, Disis ML. Immunization with<br />
a HER2/neu helper peptide vaccine generates HER-<br />
2/neu CD8 T-cell immunity in cancer patients. J Clin<br />
Invest 2001; 107:477-484.<br />
43. Disis ML, Gooley TA, Rinn K. Generation <strong>of</strong> T-cell<br />
immunity to the HER2/neu protein after active<br />
immunization with HER2/neu Peptide-based vaccines. J<br />
Clin Oncol 2002; 20:2624-2632.<br />
44. Disis ML, Bernhard H, Shiota FM. Granulocytemacrophage<br />
colony-stimulating factor: an effective<br />
adjuvant for protein and peptide-based vaccines. Blood<br />
1996; 88:202-210.<br />
45. Lehmann PV, Forsthuber T, Miller A, Sercarz EE.<br />
Spreading <strong>of</strong> T-cell autoimmunity to cryptic determinants<br />
<strong>of</strong> an autoantigen. Nature 1992; 358:155-157.<br />
46. el-Shami K, Tirosh B, Bar-Haim E. MHC class I-<br />
restricted epitope spreading in the context <strong>of</strong> tumour<br />
rejection following vaccination with a single<br />
immunodominant CTL epitope. Eur J Immunol 1999;<br />
29:3295-3301.<br />
47. Vanderlugt CJ, Miller SD. Epitope spreading. Curr Opin<br />
Immunol 1996; 8:831-836.<br />
48. <strong>Mar</strong>askovsky E, Daro E, Roux E. In vivo generation <strong>of</strong><br />
human dendritic cell subsets by Flt3 ligand. Blood 2000;<br />
96:878-884.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 12
Rajasekhar P- HER2/neu Vaccines fight against Breast Cancer<br />
49. Pulendran B, Smith JL, Jenkins M. Prevention <strong>of</strong><br />
peripheral tolerance by a dendritic cell growth factor: flt3<br />
ligand as an adjuvant. J Exp Med 1998; 188:2075-2082.<br />
50. Smorlesi A, Shiota F, Disis ML. Flt3-ligand (Flt3l), as a<br />
vaccine adjuvant, results in the generation <strong>of</strong> antigen<br />
specific IFN producing T cells after immunization.<br />
Proceedings <strong>of</strong> the American Association for Cancer<br />
Research 1999; 40:313-313.<br />
51. Lynch DH. Induction <strong>of</strong> dendritic cells (DC) by Flt3<br />
Ligand (FL) promotes the generation <strong>of</strong> tumour-specific<br />
immune responses in vivo. Crit Rev Immunol 1998;<br />
18:99-107.<br />
52. <strong>Mar</strong>askovsky E, Brasel K, Teepe M. Dramatic increase in<br />
the numbers <strong>of</strong> functionally mature dendritic cells in Flt3<br />
ligand-treated mice: multiple dendritic cell<br />
subpopulations identified. J Exp Med 1996; 184:1953-<br />
1962.<br />
53. Disis ML, Rinn K, Knutson KL. Flt3 ligand as a vaccine<br />
adjuvant in association with HER2/neu peptide- based<br />
vaccines in patients with HER2/neu-overexpressing<br />
cancers. Blood 2002; 99:2845-2850.<br />
54. Mach N, Gillessen S, Wilson SB. Differences in dendritic<br />
cells stimulated in vivo by tumours engineered to secrete<br />
granulocyte-macrophage colony-stimulating factor or<br />
Flt3- ligand. Cancer Res 2000; 60:3239-3246.<br />
55. vanderVeen RC, Dietlin TA, Pen L, Gray JD. Nitric oxide<br />
inhibits the proliferation <strong>of</strong> T-helper 1 and 2 lymphocytes<br />
without reduction in cytokine secretion. Cell Immunol<br />
1999; 193:194-201.<br />
56. Katsumata M, Okudaira T, Samanta A. Prevention <strong>of</strong><br />
breast tumour development in vivo by downregulation <strong>of</strong><br />
the p185neu receptor. Nat Med 1995; 1:644-648.<br />
57. Cobleigh MA, Vogel CL, Tripathy D. Multinational study<br />
<strong>of</strong> the efficacy and safety <strong>of</strong> humanized anti-HER2<br />
monoclonal antibody in women who have HER2-<br />
overexpressing metastatic breast cancer that has<br />
progressed after chemotherapy for metastatic disease. J<br />
Clin Oncol 1999; 17:2639-2648.<br />
58. Slamon DJ, Leyland-Jones B, Shak S. Use <strong>of</strong><br />
chemotherapy plus a monoclonal antibody against HER2<br />
for metastatic breast cancer that overexpresses HER2.<br />
NEJM 2001; 344:783-792.<br />
59. Vogel CL, Cobleigh MA, Tripathy D. First-line herceptin<br />
monotherapy in metastatic breast cancer. Oncology 2001;<br />
61 S2:37-42.<br />
60. Leyland-Jones B, Arnold A, Gelmon K. Pharmacologic<br />
insights into the future <strong>of</strong> trastuzumab. Ann Oncol 2001;<br />
12:S43-47.<br />
61. Baselga J, Tripathy D, Mendelsohn J. Phase II study <strong>of</strong><br />
weekly intravenous recombinant humanized antip185HER2<br />
monoclonal antibody in patients with<br />
HER2/neu-overexpressing metastatic breast cancer. J<br />
Clin Oncol 1996; 14:737-744.<br />
62. Yip YL, Smith G, Koch J, Dubel S, Ward RL.<br />
Identification <strong>of</strong> epitope regions recognized by tumour<br />
inhibitory and stimulatory anti-ErbB-2 monoclonal<br />
antibodies: implications for vaccine design. J Immunol<br />
2001; 166:5271-5278.<br />
63. Dakappagari NK, Douglas DB, Triozzi PL, Stevens VC,<br />
Kaumaya PT. Prevention <strong>of</strong> mammary tumours with a<br />
chimeric HER2 B-cell epitope peptide vaccine. Cancer<br />
Res 2000; 60:3782-3789.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 13
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
Association <strong>of</strong> Pharmaceutical Teachers <strong>of</strong> India<br />
Contribution <strong>of</strong> drug interactions to burden <strong>of</strong> preventable ADR'S: Approches<br />
to predict and prevent drug interactions.<br />
Raval D K, Saraswathy N, Meghani N M, Shah H K<br />
SVKM's NMIMS School <strong>of</strong> <strong>Pharmacy</strong> & Technology Management., Vile-Parle (W), MUMBAI - 400056. INDIA.<br />
A B S T R A C T<br />
During the course <strong>of</strong> treatment, drug prescribed to patients produce certain effects other than desired or expected effects. These are referred as<br />
adverse drug reactions which concern both patient as well as physician. People usually attribute these effects to either overdose or<br />
inappropriate medications or more drugs are prescribed by physician. ADRs are one <strong>of</strong> the leading causes <strong>of</strong> morbidity and mortality in health<br />
care and also associated with increased cost <strong>of</strong> treatment. Now a day's incidence <strong>of</strong> ADRs increases exponentially after a patient is on 4 or more<br />
medicines. Drug interaction represents 3-5% <strong>of</strong> preventable ADRs. Hence efforts are necessary to reduce unnecessary prescribing and this is<br />
where it becomes important to understand basic drug interactions. Given a choice between no treatment and effective treatment with a risk <strong>of</strong><br />
toxicity, physician usually selects latter one. Our job is to maximize the benefit and minimize the risk, but before we can minimize the risk, we<br />
must first be able to assess it accurately. Thus, health care practitioner must develop their own system <strong>of</strong> approach to prevent undesirable drug<br />
interactions; up-to-date database is valuable as well as frequent consultation with other members <strong>of</strong> healthcare team, like pharmacists and<br />
nurses, is essential.<br />
Key Words: Drug interactions, adverse drug reactions, Burden.<br />
Submitted: 17/11/2010<br />
Accepted: 30/12/2010<br />
INTRODUCTION<br />
An interaction is said to occur when effect <strong>of</strong> one drug is<br />
changed by presence <strong>of</strong> other drug(s), food, drink or<br />
1<br />
environmental chemicals. When therapeutic combination<br />
could lead to an unexpected change in condition <strong>of</strong> the patient,<br />
this would be described as an interaction <strong>of</strong> potential clinical<br />
significance. The incidence <strong>of</strong> adverse drug reactions has<br />
been estimated between 2.2 to 30% in hospitalized patients<br />
2-5<br />
and 9.2 to 70.3% in ambulatory patients. Drug interactions<br />
are important in clinical practice and accounts for 2 to 5% for<br />
6<br />
preventable ADR's.<br />
system failure is lack <strong>of</strong> knowledge <strong>of</strong> pharmacovigilance to<br />
the individuals actually involved in prescribing i.e, the<br />
physician.<br />
Following chart will show the factors responsible for ADR's:<br />
Fig 1: predisposing factors which influences the ADR's<br />
Why ADRs are so high<br />
There are several reason which indicates the reason for having<br />
high incidence <strong>of</strong> ADRs which include 1) number <strong>of</strong> drug<br />
prescribed are high, 2) increasing number <strong>of</strong> new drugs in<br />
market, 3) the lack <strong>of</strong> formal system for monitoring adverse<br />
7<br />
drug reactions. The cost <strong>of</strong> management <strong>of</strong> drug induced<br />
illness is very high also. Fortunately, there are various studies<br />
which indicate that most <strong>of</strong> ADR's are preventable provided<br />
that drugs are used rationally. Most common reason for<br />
Address for Correspondence:<br />
Raval DK, SVKM's NMIMS School <strong>of</strong> <strong>Pharmacy</strong> & Technology Management., Vile-Parle<br />
(W), MUMBAI - 400056. INDIA.<br />
8<br />
What Kind <strong>of</strong> Drug Requires Special Attention<br />
Some drugs with a little low quantity than expected will cause<br />
no effect or with little high quantity than expected will be<br />
dangerous. This is called having “narrow therapeutic index”<br />
and if patient is prescribed such drug then any interaction<br />
could be dangerous or fatal.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
14
Raval DK- Contribution <strong>of</strong> Drug Interactions to Burden <strong>of</strong> Preventable ADR'S: Approches to Predict and Prevent Drug Interactions<br />
Drugs to watch out for include:<br />
1) some drugs used to treat depression<br />
2) some antihistamines,<br />
3) drugs to control heart rhythm,<br />
4) some pain killer derived from opium,<br />
5) drugs to thin blood, including coumadin,<br />
6) methadone and buprenorphine<br />
7) drugs to treat erectile dysfunctions, like Viagra<br />
8) some drugs used to treat tuberculosis, mainly rifampin.<br />
Reasons for drug interactions<br />
Prescribing pattern <strong>of</strong> the drug is the major factor which is<br />
responsible for drug interactions and some <strong>of</strong> the reason for<br />
drug interactions can include<br />
1) Drug interactions can occur even before drugs enter the<br />
body due to drug or formulation incompatibility, or at any<br />
point in the process <strong>of</strong> absorption, distribution, metabolism,<br />
and elimination.<br />
Drug withdrawal<br />
Drug interaction<br />
Non-drug therapies<br />
Diagnostic tests and procedures<br />
Underlying illnesses<br />
Intercurrent illnesses<br />
Timing <strong>of</strong> events<br />
Common, spontaneous events<br />
Transient, episodic events<br />
Irreversible events<br />
Tolerance<br />
Specific treatment clouding dechallenges.<br />
Prophylactic treatment clouding rechallenges.<br />
Fig 2: incidence <strong>of</strong> ADR reported by health care pr<strong>of</strong>essionals<br />
and consumers.<br />
2) Drugs can bind to each other in IV lines or the GI tract,<br />
preventing absorption and reducing systemic availability.<br />
3) Several important interactions occur through competition<br />
at drug transporters.<br />
4) Finally, interactions can occur at the level <strong>of</strong> drug action,<br />
such as the combination <strong>of</strong> verapamil, a calcium channel<br />
blocker, and a β-blocker. Both slow the heart rate by different<br />
mechanisms, and the combination is relatively<br />
contraindicated because heart block can result.<br />
5) A large number <strong>of</strong> important interactions do occur in the<br />
liver and GI tract due to changes in the rates <strong>of</strong> drug<br />
metabolism brought about by other medicines that are<br />
inducers or inhibitors <strong>of</strong> drug metabolism.<br />
9<br />
Source <strong>of</strong> difficulty in reporting ADR's<br />
Before a given clinical manifestation or event can be labeled<br />
as an ADR, there are two separate requirements that should be<br />
met: (1) the event must, in fact, be 'adverse'; and (2) a drug<br />
must be demonstrated, within 'reasonable' likelihood, to be<br />
the cause.<br />
9<br />
Difficult factors in establishing the causal link <strong>of</strong> ADRs<br />
Recently introduced drug<br />
Multiple drugs<br />
Number <strong>of</strong> ADR's Reported in Last Ten Years.<br />
This above graphical presentation shows that consumer<br />
incidence <strong>of</strong> ADR is very high and it is increasing year by<br />
year. Also consumer <strong>of</strong> drug is also becoming aware about<br />
drug and reporting adverse drug reaction which is the<br />
requirement to reduce the adverse drug reactions. Of this, as<br />
literature says, 3-5% <strong>of</strong> reactions are preventable and this<br />
reactions are mainly due to drug interactions. It is clearly<br />
observed that drug interaction is a kind <strong>of</strong> burden to the<br />
adverse drug reactions which could have been prevented.<br />
Various approaches to prevent drug interactions and<br />
ADR's<br />
Prescribing pattern is the major reason due to which incidence<br />
<strong>of</strong> drug interactions increases so increasing awareness<br />
amongst the health care pr<strong>of</strong>essionals is the major goal. There<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
15
Raval DK- Contribution <strong>of</strong> Drug Interactions to Burden <strong>of</strong> Preventable ADR'S: Approches to Predict and Prevent Drug Interactions<br />
are misconceptions <strong>of</strong> health care pr<strong>of</strong>essionals regarding<br />
reporting ADR which should be clarified which includes<br />
1) All ADR's are reported by the time a drug is marketed.<br />
2) Hard to determine, if a drug is responsible for evidence.<br />
So it is essential to clarify their doubts and feedback should be<br />
provided so that reporting will increase.<br />
Drug Interaction Monitoring Program<br />
Occurrence <strong>of</strong> drug interactions should be monitored closely<br />
in susceptible patients and in patients on drug combinations<br />
with likelihood <strong>of</strong> interactions. A team consisting <strong>of</strong><br />
physician, pharmacologists, pharmacists and nurses should<br />
keep a close eye on the patient's conditions, medication and<br />
the prognosis. For the early detection and prevention <strong>of</strong> DIs<br />
there is a need for establishing DI monitoring programs.<br />
Monitoring program should identify the DIs occurring in the<br />
hospital, develop intervention strategies and evaluate the<br />
impact <strong>of</strong> the interaction.<br />
The identification <strong>of</strong> the DIs can be done by maintaining the<br />
patient pr<strong>of</strong>ile and checking the interactions based on the<br />
existing literature. The interactions should be categorized<br />
based on their severity. Following these steps, strategies<br />
should be made in order to prevent the occurrence <strong>of</strong><br />
interactions, at least the severe ones. The intervention<br />
strategies may include peer group discussion, discussion<br />
among the Drug and Therapeutics Committee (DTC)<br />
members and discussion with junior doctors etc. Following<br />
the intervention the impact <strong>of</strong> the intervention should be<br />
analyzed by comparing the incidence with the pre<br />
intervention data. The importance <strong>of</strong> DIs should be taught to<br />
the medical students, pharmacists and nurses so that a team<br />
effort can be made by them in the future.<br />
Benefits <strong>of</strong> Reporting ADR's<br />
An ongoing ADR-monitoring and reporting program can<br />
provide benefits to the organization, pharmacists, other health<br />
care pr<strong>of</strong>essionals, and patients. These benefits include (but<br />
are not limited to) the following.<br />
1. Providing an indirect measure <strong>of</strong> the quality <strong>of</strong><br />
pharmaceutical care through identification <strong>of</strong> preventable<br />
ADRs and anticipatory surveillance for high-risk drugs or<br />
patients.<br />
2. Complementing organizational risk-management activities<br />
and efforts to minimize liability.<br />
3. Assessing the safety <strong>of</strong> drug therapies, especially recently<br />
approved drugs.<br />
4. Measuring ADR incidence.<br />
5. Educating health care pr<strong>of</strong>essionals and patients about drug<br />
effects and increasing their level <strong>of</strong> awareness regarding<br />
ADRs.<br />
6. Providing quality-assurance screening findings for use in<br />
drug-use evaluation programs.<br />
7. Measuring the economic impact <strong>of</strong> ADR prevention as<br />
manifested through reduced hospitalization, optimal and<br />
economical drug use, and minimized organizational liability.<br />
Role <strong>of</strong> Pharmacist<br />
Pharmacists should exert leadership in the development,<br />
maintenance, and ongoing evaluation <strong>of</strong> ADR programs.<br />
They should obtain formal endorsement or approval <strong>of</strong> such<br />
programs through appropriate committees (e.g., a pharmacy<br />
and therapeutics committee and the executive committee <strong>of</strong><br />
the medical staff) and the organization's administration. In<br />
settings where applicable, input into the design <strong>of</strong> the program<br />
should be obtained from the medical staff, nursing staff,<br />
quality improvement staff, medical records department, and<br />
[10, 11-13]<br />
risk managers. The pharmacist should facilitate<br />
1. Analysis <strong>of</strong> each reported ADR,<br />
2. Identification <strong>of</strong> drugs and patients at high risk for being<br />
involved in ADRs,<br />
3. The development <strong>of</strong> policies and procedures for the ADRmonitoring<br />
and reporting program,<br />
4. A description <strong>of</strong> the responsibilities and interactions <strong>of</strong><br />
pharmacists, physicians, nurses, risk managers, and other<br />
health pr<strong>of</strong>essionals in the ADR program,<br />
5. Use <strong>of</strong> the ADR program for educational purposes,<br />
6. Development, maintenance, and evaluation <strong>of</strong> ADR<br />
records within the organization,<br />
7. The organizational dissemination and use <strong>of</strong> information<br />
obtained through the ADR program,<br />
8. Reporting <strong>of</strong> serious ADRs to the FDA or the manufacturer<br />
(or both), and<br />
9. Publication and presentation <strong>of</strong> important ADRs to the<br />
medical community.<br />
Direct patient care roles for pharmacists should include<br />
patient counseling on ADRs, identification and<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
16
Raval DK- Contribution <strong>of</strong> Drug Interactions to Burden <strong>of</strong> Preventable ADR'S: Approches to Predict and Prevent Drug Interactions<br />
documentation in the patient's medical record <strong>of</strong> high-risk<br />
patients, monitoring to ensure that serum drug concentrations<br />
remain within acceptable therapeutic ranges, and adjusting<br />
doses in appropriate patients (e.g., patients with impaired<br />
renal or hepatic function).<br />
REFERENCES<br />
1. Stockley I H. Drug interaction: a source book <strong>of</strong> adverse<br />
interaction, their mechanisms, clinical importance and<br />
management. 5th ed. Pharmaceutical Press, London 1999.<br />
2. Gosney M, Tallis R. Prescription <strong>of</strong> contraindicated and<br />
interacting drugs in elderly patients admitted to hospital.<br />
Lancet 1984; 1:564-567<br />
3. Kinney E. Expert system detection <strong>of</strong> drug interactions:<br />
results in consecutive patients. Comput Biomed Res<br />
1986; 19: 462-467.<br />
4. Dambro MR, Kallgren MA. Drug interaction in a clinic<br />
using COSTER. Comput Biol Med 1988; 18:31-38,<br />
5. Shinn AF, Shrewsbury RP, Anderson KW. Development<br />
<strong>of</strong> a computerized drug database (MEDICOM) for use in a<br />
patient specific environment. Drug Inf J 1983; 17:205-<br />
210.<br />
6. Classen DC, Pestotnick SL, Evans RS, Burke JP.<br />
Computer surveillance <strong>of</strong> adverse drug events in hospital<br />
patients. JAMA 1991; 266: 2847-2851.<br />
7. Bates DW. Spell N, Cullen DJ et al. The costs <strong>of</strong> adverse<br />
drug reactions in hospitalised patients. JAMA 1997; 277:<br />
301-307.<br />
8. Fact sheet number 407, Drug Interactions, revised edition<br />
2009.<br />
9. Kramer MS Difficulty in assessing adverse effects <strong>of</strong><br />
drugs, Br. J. clin. Pharmac. (1981), 11, 105S-110S.<br />
10.Karch FE, Lasagna L. Toward the operational<br />
identification <strong>of</strong> adverse drug reactions. Clin Pharmacol<br />
Ther. 1977; 21:247–254.<br />
11. S w a n s o n K M , L a n d r y J P, A n d e r s o n R P.<br />
<strong>Pharmacy</strong>coordinated, multidisciplinary adverse drug<br />
reaction program. Top Hosp Pharm Manage. 1992;<br />
12(Jul):49–59.<br />
12. Flowers P, Dzierba S, Baker O. A continuous quality<br />
improvement team approach to adverse drug reaction<br />
reporting. Top Hosp Pharm Manage. 1992; 12(Jul):<br />
60–67.<br />
13. Guharoy SR. A pharmacy-coordinated, multidisciplinary<br />
approach for successful implementation <strong>of</strong> an adverse<br />
drug reaction reporting program. Top HospPharm<br />
Manage. 1992; 12(Jul):68–74.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
17
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
Association <strong>of</strong> Pharmaceutical Teachers <strong>of</strong> India<br />
Survey and evaluation <strong>of</strong> various epidemiological factors in a multiethnic<br />
Diabetic Population in Ras Al-Khaimah, UAE.<br />
1 2 3 4<br />
Smitha F , Meenakshi J , Padma R , Multani S K<br />
Department <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong>, RAK College <strong>of</strong> Pharmaceutical Sciences, RAK Medical and Health Sciences<br />
1, 3<br />
University, Ras Al Khaimah, UAE.<br />
Department <strong>of</strong> Pathology, RAK College <strong>of</strong> Medical Sciences, RAK Medical and<br />
2<br />
Khaimah, UAE.<br />
Health Sciences University, Ras Al<br />
4<br />
Endocrinologist, Al Zahrawi Hospital. Ras Al Khaimah, UAE<br />
A B S T R A C T<br />
Submitted: 3/1/<strong>2011</strong><br />
Diabetes Mellitus is a major public health problem in UAE with a prevalence rate reaching 24% in national citizens and 17.4% in expatriates. In<br />
the year 2010, UAE is ranked as the second highest worldwide for diabetes prevalence. However, there is a lack <strong>of</strong> epidemiological data on the<br />
prevalence <strong>of</strong> diabetes in UAE and other Arab countries. Hence, the present study was undertaken. The data was evaluated for the following<br />
parameters like the predisposing factors, associated co-morbidities and the prescription pattern in diabetic patients. This retrospective study<br />
included data collected from the case records <strong>of</strong> all the diabetic patients who visited the out-patient clinic <strong>of</strong> department <strong>of</strong> endocrinology and<br />
diabetes <strong>of</strong> a private hospital in Ras Al Khaimah, UAE. Case records <strong>of</strong> 143 subjects (123 were males and 20 were females) with type-II diabetes<br />
mellitus were analyzed in the study. The mean age <strong>of</strong> the patients was 46.69 ± 7.70 years and the mean age at onset <strong>of</strong> type-II diabetes mellitus<br />
2<br />
was 39.83 + 7.60 years. The mean BMI <strong>of</strong> the study population was 26.8 + 3.78 kg/m . The associated co-morbidities were hypertension<br />
(58.7%), dyslipidemia (87.4%) and both hypertension and dyslipidemia (47.6%). The most commonly prescribed antidiabetic drug class was<br />
biguanides (metformin) followed by suphonylureas (glimeperide), thiazolidinediones (rosiglitazone) and DPP4 Inhibitors (vildagliptin). As<br />
monotherapy, metformin was the preferred drug <strong>of</strong> choice. The most prevalent multiple drug therapy was a three drug combination <strong>of</strong><br />
glimeperide, metformin and rosiglitazone. This study strongly highlights the need for patient education on diet control, lifestyle modifications,<br />
use <strong>of</strong> antidiabetics and concomitant drugs, monitoring <strong>of</strong> blood glucose and aggressive treatment <strong>of</strong> diabetes to prevent associated<br />
complications.<br />
Keywords: Diabetes mellitus, predisposing factors, co-morbidities, prescription pattern, anti-diabetic drugs.<br />
Accepted: 14/2/<strong>2011</strong><br />
Address for Correspondence:<br />
Smitha C F, Department <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong>, RAK College <strong>of</strong> Pharmaceutical Sciences,<br />
RAK Medical and Health Sciences University,P O Box 11172 Ras Al Khaimah, UAE.<br />
E- mail: smithafrancis2003@yahoo.co.in<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
18
Smitha F - Survey and evaluation <strong>of</strong> various Epidemiological Factors in a Multiethnic Diabetic Population in Ras Al Khaimah, UAE.<br />
Gender<br />
Mean Age<br />
Mean BMI<br />
Waist Circumference<br />
Family History<br />
Table 1: Patient Demographic Status<br />
123 male (86.01%)<br />
20 female (13.98%)<br />
39.83 ±7.6 years<br />
2<br />
26.8±3.78kg/m<br />
95.26+ 9.37<br />
76.3%<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
19
Smitha F - Survey and evaluation <strong>of</strong> various Epidemiological Factors in a Multiethnic Diabetic Population in Ras Al Khaimah, UAE.<br />
Appendix<br />
RAK Medical & Health Sciences University<br />
Data collection form<br />
Name <strong>of</strong> the hospital :<br />
Name <strong>of</strong> the treating doctor :<br />
File number :<br />
Contact no :<br />
Ethnicity :<br />
Occupation :<br />
Age :<br />
Sex :<br />
Duration <strong>of</strong> diabetes :<br />
Age <strong>of</strong> onset :<br />
Family history <strong>of</strong> diabetes :<br />
Height :<br />
Weight :<br />
BMI :<br />
WC :<br />
BP :<br />
<strong>Mar</strong>ital status :<br />
Lifestyle factors : sedentary/active<br />
Exercise :<br />
Diet : veg/ non-veg<br />
Smoking :<br />
Alcohol :<br />
Co-morbidities :<br />
DIAGNOSIS: …………………………………………………………………………………<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 20
Smitha F - Survey and evaluation <strong>of</strong> various Epidemiological Factors in a Multiethnic Diabetic Population in Ras Al Khaimah, UAE.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 21
Smitha F - Survey and evaluation <strong>of</strong> various Epidemiological Factors in a Multiethnic Diabetic Population in Ras Al Khaimah, UAE.<br />
Table 2: Monotherapy<br />
No <strong>of</strong> Patients<br />
Table 3: Combination therapy<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
22
Smitha F - Survey and evaluation <strong>of</strong> various Epidemiological Factors in a Multiethnic Diabetic Population in Ras Al Khaimah, UAE.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 23
Smitha F - Survey and evaluation <strong>of</strong> various Epidemiological Factors in a Multiethnic Diabetic Population in Ras Al Khaimah, UAE.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 24
Smitha F - Survey and evaluation <strong>of</strong> various Epidemiological Factors in a Multiethnic Diabetic Population in Ras Al Khaimah, UAE.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 25
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
Association <strong>of</strong> Pharmaceutical Teachers <strong>of</strong> India<br />
Impact <strong>of</strong> educational interventions on Adverse Drug Reaction reporting<br />
1 2 1 1<br />
Ganachari M S* , Patil P A , Soham S , Nidhi Z<br />
1<br />
Department <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong>, KLE University's College <strong>of</strong> <strong>Pharmacy</strong>, Belgaum-590010, Karnataka, India<br />
2<br />
Department <strong>of</strong> Pharmacology, Jawaharlal Nehru Medical College, Belgaum-590010, Karnataka, India<br />
A B S T R A C T<br />
Submitted: 28/12/2010<br />
Accepted: 6/1/<strong>2011</strong><br />
Adverse Drug Reactions (ADR) have become a major health concern. This study was carried out to determine the impact <strong>of</strong> educational<br />
interventions with the assistance <strong>of</strong> pharmacist on the knowledge and attitudes <strong>of</strong> healthcare pr<strong>of</strong>essionals for ADR and its reporting. In preintervention<br />
survey, healthcare pr<strong>of</strong>essionals were surveyed using a questionnaire to assess their knowledge and attitudes regarding ADR and<br />
its reporting and obtain their suggestions to improve ADR reporting. After this survey, 2 workshops were conducted on pharmacovigilance. One<br />
teaching program was conducted for nursing staff. Informative booklets on Guidelines for reporting ADR were prepared and distributed to all<br />
healthcare pr<strong>of</strong>essionals. After this a post intervention survey was conducted to reassess the knowledge and attitudes <strong>of</strong> healthcare<br />
pr<strong>of</strong>essionals regarding ADR reporting. In pre-intervention survey, 124 had experienced ADR in their day to day practice, while only 84 had<br />
reported ADR. In post-intervention survey, 111 had reported an ADR. In pre-intervention survey, 116 knew the definition <strong>of</strong> ADR, 49 knew the<br />
grading <strong>of</strong> ADR based on severity, while 30 knew grading based on causality. In post intervention survey, 127 healthcare pr<strong>of</strong>essionals knew the<br />
definition <strong>of</strong> ADR, 81 knew the grading <strong>of</strong> ADR based on severity while, 77 knew the grading <strong>of</strong> ADR based on causality. Lack <strong>of</strong> awareness, lack<br />
<strong>of</strong> assistance, busy schedule, lack <strong>of</strong> incentives, inadequate availability <strong>of</strong> ADR reporting forms were identified as major barriers in ADR<br />
reporting. This study shows that there is a need to create awareness and impart knowledge to healthcare pr<strong>of</strong>essionals regarding ADR and its<br />
reporting. If adequate practical training and education is given consistently, then definitely the attitude <strong>of</strong> healthcare pr<strong>of</strong>essionals can be<br />
changed and ADR reporting can be improved.<br />
Key Words: Adverse Drug Reactions, healthcare, educational intervention<br />
INTRODUCTION<br />
According to World Health organisation, Adverse Drug<br />
Reaction (ADR) is “a reaction which is noxious and<br />
unintended and which occurs at doses normally used in<br />
humans for prevention, diagnosis or therapy <strong>of</strong> disease, or for<br />
1<br />
the modification <strong>of</strong> physiological functions” ADRs are the<br />
major cause <strong>of</strong> morbidity and mortality in the patients,<br />
resulting in increased length <strong>of</strong> stay in hospital and in turn<br />
2<br />
increased cost <strong>of</strong> healthcare . ADRs are also one <strong>of</strong> the major<br />
3,4 th th<br />
causes <strong>of</strong> hospitalisation. ADRs are 4 to 6 leading cause <strong>of</strong><br />
death in United States only after heart disease, cancer, stroke,<br />
5<br />
pulmonary disease and accidents.<br />
With numerous drugs entering into the market, ADRs have<br />
become very important clinical issue for patient safety.<br />
Though the medicines are assessed for safety and efficacy by<br />
the clinical trials before marketing, it is very difficult to<br />
Address for Correspondence:<br />
M. S. Ganachari, Pr<strong>of</strong>essor and Head, Department <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong>, KLE University's<br />
College <strong>of</strong> <strong>Pharmacy</strong>, Nehru Nagar, Belgaum-590010, Karnataka, India<br />
Email: msganchari@gmail.com<br />
identify all the rare ADRs as well as actual incidence due to<br />
small sample size, short duration and restricted study criteria.<br />
Hence it is essential to monitor the drugs for ADRs. Health<br />
care pr<strong>of</strong>essionals play a very important role in ADR<br />
reporting. Health care pr<strong>of</strong>essionals help in identification <strong>of</strong><br />
6,7<br />
signals and evaluate the safety <strong>of</strong> drugs by reporting ADR.<br />
As the doctors are the first ones to use any new drug entering<br />
the market, they play a key role in identifying any adverse<br />
effects <strong>of</strong> the drugs. Information provided by them could be <strong>of</strong><br />
much help to assess the safety <strong>of</strong> any drug. Hence, it becomes<br />
essential to motivate the healthcare pr<strong>of</strong>essionals to report<br />
any adverse drug reactions they come across.<br />
Studies have shown that educational interventions can<br />
improve ADR reporting by health care pr<strong>of</strong>essionals. Hence<br />
this study was carried out to determine the impact <strong>of</strong><br />
educational interventions on the knowledge and attitudes <strong>of</strong><br />
healthcare pr<strong>of</strong>essionals for ADR and its reporting.<br />
METHOD<br />
This prospective cross-sectional study was carried out after<br />
procuring approval from Institutional Ethics Committee. The<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
26
Ganachari MS- Impact <strong>of</strong> Educational Interventions on Adverse Drug Reaction Reporting<br />
study was conducted in a Tertiary Care Hospital in a South<br />
<strong>Indian</strong> city. The study was conducted in three phases:<br />
1. Pre-interventional survey<br />
2. Interventions<br />
3. Post-intervention survey<br />
One hundred and sixty three health care pr<strong>of</strong>essionals<br />
(includes doctors, nurses and pharmacists) were surveyed<br />
using a questionnaire to assess their knowledge regarding<br />
pharmacovigilance and obtain their suggestions to improve<br />
pharmacovigilance activity. The pharmacist took verbal<br />
consent from all the participants and explained them the<br />
purpose <strong>of</strong> the survey. Each health care pr<strong>of</strong>essional was<br />
explained the questionnaire and then the questionnaire were<br />
handed over to the participants to fill. After conducting the<br />
pre-intervention survey, all the filled questionnaires were<br />
analysed to determine the knowledge and attitudes <strong>of</strong> health<br />
care pr<strong>of</strong>essionals for pharmacovigilance and suggestions<br />
made by them to improve pharmacovigilance activities in the<br />
hospital.<br />
After pre-interventional survey, teaching program was<br />
carried out to create awareness among nursing staff regarding<br />
pharmacovigilance. A book on guidelines for reporting<br />
adverse drug reactions in the hospital was developed and<br />
distributed to all the healthcare pr<strong>of</strong>essionals. Book contained<br />
all the details like definition <strong>of</strong> ADR, grading <strong>of</strong> ADR based<br />
on severity and causality, importance <strong>of</strong> ADR reporting, how<br />
and where to report ADR and information to be included<br />
while reporting ADR. Two workshops were conducted on<br />
“Pharmacovigilance” to improve knowledge regarding ADR<br />
and its reporting systems among the healthcare pr<strong>of</strong>essionals.<br />
The workshops elaborated on: ADR, its definition, grading <strong>of</strong><br />
ADR based on severity and causality, importance <strong>of</strong> ADR<br />
reporting, global ADR reporting systems and guidelines on<br />
ADR reporting. In these workshops, healthcare pr<strong>of</strong>essionals<br />
were given practical exposure <strong>of</strong> filling an ADR reporting<br />
forms by providing them dummy ADR cases. ADR reports<br />
Drop boxes were made available with sufficient number <strong>of</strong><br />
reporting forms at each nursing stations.<br />
After the educational interventions, a post intervention survey<br />
was conducted using same questionnaire that was used in preintervention<br />
survey. Same healthcare pr<strong>of</strong>essionals were<br />
approached and provided the questionnaire to fill. After<br />
attending all the questions the questionnaire was retrieved and<br />
data was analysed.<br />
Student's paired t-test was used to analyse the change in<br />
knowledge and attitude and determine the significance.<br />
RESULTS<br />
Demography<br />
During the study period, 163 health care pr<strong>of</strong>essionals<br />
participated in the pre-intervention survey and 150<br />
participated in post-intervention survey. For analysis <strong>of</strong> data<br />
only those 150 participants were considered who participated<br />
in both the surveys. Out <strong>of</strong> these 150 participants, 58 were<br />
doctors (physicians, house surgeons, residents), 72 were<br />
nurses and 20 were pharmacists. There were 13 dropouts<br />
(7.97%) as these healthcare pr<strong>of</strong>essionals could not be<br />
contacted for various reasons.<br />
Attitudes <strong>of</strong> the healthcare pr<strong>of</strong>essionals toward ADR and<br />
its reporting<br />
Out <strong>of</strong> 150 healthcare pr<strong>of</strong>essionals in the pre-interventional<br />
survey, only 84 (56.0%) had actually reported an ADR. Out <strong>of</strong><br />
these healthcare pr<strong>of</strong>essionals who reported ADR, 46<br />
(30.67%) had reported it verbally, 10 (6.67%) had reported it<br />
in written form while, 28 (18.67%) had reported ADR<br />
verbally as well as in written form. These healthcare<br />
pr<strong>of</strong>essionals had reported ADR to either colleagues (56,<br />
37.33%) or pharmacists working in pharmacovigilance group<br />
(44, 29.34%). Out <strong>of</strong> the total 38 respondents who had<br />
reported ADR in written form, 18 had reported ADR in last six<br />
months. Out <strong>of</strong> 66 (44.01%) healthcare pr<strong>of</strong>essionals who had<br />
never reported an ADR, 18(12.0%) felt that due to lack <strong>of</strong> time<br />
they had never reported an ADR, while 4 (2.67%) were not<br />
interested to report an ADR. Eleven (7.33%) felt that not<br />
reporting an ADR does not affect the patient care, while 59<br />
(39.34%) were not aware where to report an ADR.<br />
In post-intervention survey, out <strong>of</strong> 150 healthcare<br />
pr<strong>of</strong>essionals, 111(74.01%) said that they had reported an<br />
ADR, out <strong>of</strong> which 51 (34.0%) had reported it verbally, 27<br />
(18.0%) had reported it in written form while 33 (22.0%) had<br />
reported it verbally as well as in written form. Eighty six<br />
(57.33%) had reported ADR to colleagues while 67 (44.67%)<br />
had reported it to pharmacists. Out <strong>of</strong> these total 60 healthcare<br />
pr<strong>of</strong>essionals who had reported an ADR in written form, 30<br />
had reported ADR in past six months. This also shows that 22<br />
pr<strong>of</strong>essionals started reporting ADR after intervention. There<br />
is improvement in the attitude <strong>of</strong> healthcare pr<strong>of</strong>essionals<br />
towards ADR reporting but statistically it is not significant<br />
(p= 0.1335 using paired t- test).<br />
Table 1 shows the number <strong>of</strong> healthcare pr<strong>of</strong>essionals and<br />
their attitudinal responses in pre-interventional survey and<br />
post-interventional survey.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 27
Ganachari MS- Impact <strong>of</strong> Educational Interventions on Adverse Drug Reaction Reporting<br />
No.<br />
1<br />
2<br />
3<br />
4<br />
5<br />
Attitude questions<br />
Do you experience ADRs<br />
in your day to day practice<br />
Have you ever reported ADR<br />
that you came across Yes<br />
Doctors<br />
n1=58<br />
Doctors<br />
N1=58<br />
Nurses<br />
n2=72<br />
Nurses<br />
N2=72<br />
Pharmacists Pharmacists<br />
n3=20 N3=20<br />
Total<br />
n=150<br />
Total<br />
N=150<br />
32.00% 32.00% 40.00% 40.00% 10.66% 10.66% 82.66% 82.66%<br />
20.00% 28.67% 25.33% 32.67% 10.67% 12.67% 56.00% 74.00%<br />
No 18.67% 10.0% 22.67% 15.33% 2.67% 0.67% 44.01% 26.00%<br />
If yes, how do you report<br />
Verbal 10.67% 12.00% 17.33% 18.67% 02.67% 03.33% 30.67% 34.00%<br />
Written 02.67% 10.67% 02.67%<br />
Both 06.67% 06.00% 05.33%<br />
To whom*<br />
06.0% 01.33% 01.34% 06.67% 18.00%<br />
08.00% 06.67% 08.00% 18.67% 22.00%<br />
Colleague’s 14.00% 24.00% 15.33% 21.33% 08.00% 12.00% 37.33% 57.33%<br />
Pharmacist 06.67% 18.67% 12.67% 14.00% 10.00% 12.00% 29.34% 44.67%<br />
If no, why*<br />
No Time<br />
Not interested<br />
Does not effect patient care<br />
Not aware where to report<br />
Table 1: Attitude <strong>of</strong> healthcare pr<strong>of</strong>essionals for ADR reporting<br />
04.67% 02.00% 05.33% 04.00% 02.00% 0.67% 12.00% 60.67%<br />
0% 0% 02.67 % 0% 0% 0% 02.67% 0%<br />
06.00 % 02.67% 01.33 % 0% 0% 0% 07.33% 02.67%<br />
16.00% 08.67% 22.67% 07.33% 0.67% 0% 39.34% 16.00%<br />
* sum <strong>of</strong> % not equal to 100% as the multiple answers can be chosen for the question. n, n1, n2, n3 are pre intervention results and N, N1, N2, N3 are<br />
post intervention results. Comparison <strong>of</strong> attitude <strong>of</strong> healthcare pr<strong>of</strong>essionals in pre- and post- intervention survey: p= 0.1335 using paired t- test.<br />
Knowledge <strong>of</strong> healthcare pr<strong>of</strong>essionals regarding ADR<br />
and its reporting<br />
While considering knowledge regarding ADR and its<br />
reporting, 116 (77.33%) knew the definition <strong>of</strong> ADR in preinterventional<br />
survey. Forty nine (32.66%) healthcare<br />
pr<strong>of</strong>essionals knew the grading <strong>of</strong> ADR based on severity,<br />
while 30 (20.0%) knew the grading, based on causality.<br />
Ninety four (62.67%) health care pr<strong>of</strong>essionals knew the<br />
relationship between ADR and patient characteristics, 113<br />
(75.33%) knew the relationship between ADR and<br />
prescription errors and 97 (64.66%) were aware <strong>of</strong><br />
relationship between ADR and patient education. Only 62<br />
(41.33%) healthcare pr<strong>of</strong>essionals knew the information to be<br />
included to report an ADR.<br />
After the educational interventions for healthcare<br />
pr<strong>of</strong>essionals, in the post-interventional survey, 127 (84.67%)<br />
healthcare pr<strong>of</strong>essionals knew the definition <strong>of</strong> ADR. 81<br />
(54.0%) healthcare pr<strong>of</strong>essionals knew the grading <strong>of</strong> ADR<br />
based on severity while, 77 (51.33%) knew the grading <strong>of</strong><br />
ADR based on causality. One hundred and fifteen (76.67%)<br />
healthcare pr<strong>of</strong>essionals knew the relationship between ADR<br />
and patient characteristics, while 130 (86.67%) knew the<br />
relationship between ADR and prescription errors and 118<br />
(78.67%) were aware <strong>of</strong> relationship between ADR and<br />
patient education. One hundred and twenty four (82.67%)<br />
healthcare pr<strong>of</strong>essionals knew the information to be included<br />
to report an ADR. There is statistically significant<br />
improvement in the knowledge <strong>of</strong> healthcare pr<strong>of</strong>essionals<br />
(p =0.0078**).<br />
Table 2 shows the number <strong>of</strong> healthcare pr<strong>of</strong>essionals and<br />
their responses related to knowledge <strong>of</strong> ADR and its<br />
reporting, in pre-interventional survey and postinterventional<br />
survey.<br />
Barriers to ADR reporting<br />
Various barriers to ADR reporting mentioned by healthcare<br />
pr<strong>of</strong>essionals are shown in the figure 1. It was identified in pre<br />
intervention survey that maximum number <strong>of</strong> healthcare<br />
Fig.1: Barriers to ADR reporting identified during pre- and postintervention<br />
survey and change in ADR reporting during that period.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
28
Ganachari MS- Impact <strong>of</strong> Educational Interventions on Adverse Drug Reaction Reporting<br />
No.<br />
1<br />
2<br />
3<br />
4<br />
Knowledge questions<br />
Do you know definition<br />
<strong>of</strong> ADR<br />
Doctors<br />
n1=58<br />
Doctors<br />
N1=58<br />
Nurses<br />
n2=72<br />
Nurses<br />
N2=72<br />
Pharmacists Pharmacists<br />
n3=20 N3=20<br />
Total<br />
n=150<br />
Do you know grading<br />
12.00% 18.67% 13.33% 25.33% 07.33% 10.00% 32.66%<br />
<strong>of</strong> ADR<br />
Are you aware <strong>of</strong> relationship between ADR and,<br />
Patient characteristics<br />
Prescription errors<br />
Patient education<br />
Do you know information<br />
included to report ADR<br />
Table 2: Knowledge <strong>of</strong> healthcare pr<strong>of</strong>essionals<br />
Total<br />
N=150<br />
32.67% 34.67% 35.33% 37.33% 09.33% 12.67% 77.33 % 84.67%<br />
30.67% 34.00% 20.00% 30.67% 12.00% 12.0% 62.67% 76.67%<br />
30.00% 35.33% 34.00% 38.67% 11.30% 12.67% 75.33% 86.67%<br />
27.33% 34.0% 25.33% 32.0% 12.00% 12.67% 64.66% 78.67%<br />
15.33% 32.67% 16.00% 37.33% 10.00% 12.67% 41.33%<br />
54.00%<br />
82.67%<br />
5<br />
Do you think awareness <strong>of</strong><br />
ADR will improve reporting<br />
35.33% 38.67% 46.67% 46.67% 12.67% 13.33% 94.67 98.67%<br />
6<br />
Are you aware <strong>of</strong> ADR<br />
grading based on causality<br />
07.33% 21.33% 06.00% 18.67% 06.67% 11.33% 20.00% 51.33%<br />
7<br />
Are you aware <strong>of</strong> recent<br />
drug withdrawn<br />
21.33% 28.67% 22.00% 30.67% 10.67% 12.67% 54.00% 72.0%<br />
n, n1, n2, n3 are pre intervention results and N, N1, N2, N3 are post intervention results. Comparison <strong>of</strong><br />
knowledge <strong>of</strong> healthcare pr<strong>of</strong>essionals in pre- and post- intervention survey: p= 0.0078** using paired t- test.<br />
pr<strong>of</strong>essionals felt that lack <strong>of</strong> awareness regarding ADR<br />
reporting system is the major deterrent to ADR reporting.<br />
After educational interventions, only about half <strong>of</strong> them felt<br />
that lack <strong>of</strong> awareness is barrier to ADR reporting<br />
Suggestions to improve ADR reporting<br />
Various suggestions were provided by healthcare<br />
pr<strong>of</strong>essionals to improve ADR reporting. One hundred and<br />
forty three (95.34%) suggested that inclusion <strong>of</strong><br />
pharmacovigilance in Under Graduate and Post Graduate<br />
curriculum can improve ADR reporting. One hundred and<br />
forty five (96.67%) healthcare pr<strong>of</strong>essionals felt that<br />
establishing pharmacovigilance centre can facilitate ADR<br />
reporting. Compulsory reporting was suggested by 126<br />
(84.0%) healthcare pr<strong>of</strong>essionals as another option to<br />
improve ADR reporting. Eighty two (54.67%) healthcare<br />
pr<strong>of</strong>essionals felt that prescription monitoring can also help in<br />
identifying ADR and early ADR reporting. Seventy eight<br />
(52.0%) health care pr<strong>of</strong>essionals also felt that legal<br />
compulsion to report can improve ADR reporting.<br />
DISCUSSION<br />
In pre-intervention survey 84 healthcare pr<strong>of</strong>essionals had<br />
reported ADR previously, though 124 had experienced ADR<br />
in their day to day practice. Sixty two healthcare pr<strong>of</strong>essionals<br />
had never reported ADR. The reason for under reporting<br />
mentioned were lack <strong>of</strong> awareness, lack <strong>of</strong> time, lack <strong>of</strong><br />
interest and disbelief that reporting does not affect patient<br />
care. Similar reasons were identified as discouraging factors<br />
8,9, 10, 11, 12<br />
to reporting an ADR in various other studies. Hence<br />
various steps like educational interventions to create<br />
awareness for ADR reporting and utilising assistance <strong>of</strong><br />
pharmacist to report ADR are needed to be taken in the<br />
directions to overcome these deterrents. Studies have shown<br />
13,14,15,16<br />
that creating awareness can improve ADR reporting.<br />
The effect <strong>of</strong> educational interventions can be observed from<br />
the results <strong>of</strong> post-intervention survey which clearly showed<br />
that there is an improvement in attitude towards ADR<br />
reporting with increased number <strong>of</strong> healthcare pr<strong>of</strong>essionals<br />
reporting the ADR. The results show that there is<br />
improvement in attitude towards ADR reporting, but it is not<br />
significant (p= 0.1335 using paired t- test). This may be<br />
attributed to short term interventions. Further studies should<br />
be done to assess the change in attitude after continuous and<br />
long term interventions. It is also important to note that there<br />
is significant improvement in the knowledge <strong>of</strong> ADR and its<br />
reporting system (p= 0.0078 using paired t- test). There is<br />
7.34% increase in knowledge regarding ADR definition,<br />
while 21.34% increase in knowledge regarding grading <strong>of</strong><br />
ADR based on severity and 31.33% improvement in<br />
knowledge regarding grading <strong>of</strong> ADR based on causality.<br />
Increased number <strong>of</strong> healthcare pr<strong>of</strong>essionals now knew the<br />
information to be included while reporting an ADR, which<br />
can facilitate ADR reporting. Hence results <strong>of</strong> this study are<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 29
Ganachari MS- Impact <strong>of</strong> Educational Interventions on Adverse Drug Reaction Reporting<br />
consistent with the results <strong>of</strong> previous studies in which<br />
educational interventions had played an important role in<br />
13,14,17<br />
creating awareness for ADR and its reporting.<br />
Busy schedule and lack <strong>of</strong> assistance were found to be<br />
deterrent in ADR reporting. The same reason was identified as<br />
8,10<br />
barrier in many other studies. Hindering factors like busy<br />
schedule and lack <strong>of</strong> assistance can be overcome by provision<br />
<strong>of</strong> assistance by clinical pharmacists. The same was done to<br />
overcome these deterrent factors. Pharmacists were<br />
appointed to assist the doctors and nurses in filling ADR<br />
forms and reporting ADR. Previous studies have shown that<br />
the ADR reports submitted by pharmacists provide valuable<br />
18<br />
information, which is complimentary to physician's reports.<br />
Studies have also shown that pharmacists have adequate<br />
19<br />
knowledge for reporting an ADR and their assistance can<br />
20,21,22<br />
definitely improve ADR reporting. Moreover in most<br />
countries as the pharmacist are considered eligible to report,<br />
they can also forward adverse drug reaction reports to<br />
national centres. It is found that reports from pharmacists are<br />
more complete and appropriate when compared to other<br />
22<br />
healthcare pr<strong>of</strong>essionals. According to International<br />
Pharmaceutical Federation (FIP), “An important clinical<br />
responsibility <strong>of</strong> the pharmacist is in the early detection <strong>of</strong><br />
ADRs and other drug-related problems as well as monitoring<br />
the effectiveness <strong>of</strong> medicines. The pharmacist, as a part <strong>of</strong><br />
the healthcare team, is a source <strong>of</strong> both information and<br />
critical evaluation <strong>of</strong> drug information. The pharmacist's<br />
expertise is vital to the application <strong>of</strong> the safety pr<strong>of</strong>ile <strong>of</strong> a<br />
23<br />
medicine to the needs <strong>of</strong> a particular patient”. Many studies<br />
have shown that pharmacists have highly positive attitude and<br />
believe that ADR reporting is their pr<strong>of</strong>essional<br />
responsibility, indicating that appropriate education<br />
regarding reporting can make significant improvement in<br />
18,19<br />
ADR reporting. Pharmacists must understand their role in<br />
promoting safe use <strong>of</strong> medicines and hence actively involve in<br />
detection as well as reporting <strong>of</strong> ADRs.<br />
Inadequate availability <strong>of</strong> ADR reporting forms was<br />
identified as another discouraging factor for reporting ADR.<br />
To overcome this, ADR reporting forms were made freely<br />
available at the nursing stations in all the wards. ADR drop<br />
boxes were provided in each ward so that it becomes easy for<br />
doctors and nurses to fill the ADR form and drop in the ADR<br />
drop box while working in the wards only. The reports were<br />
later collected by the pharmacists and patients were followed<br />
up by them for more detailed information. This reduced the<br />
burden on doctors and nurses to submit ADR reports to ADR<br />
reporting centres. Moreover this whole process becomes less<br />
time consuming. Studies have shown that providing ADR<br />
reporting forms in sufficient quantity to the healthcare<br />
24<br />
pr<strong>of</strong>essionals can raise the number <strong>of</strong> ADR reporting. Same<br />
was seen in our study where there was increased reporting <strong>of</strong><br />
ADR in written form after providing ADR reporting forms<br />
and ADR drop boxes at nursing stations.<br />
Thus this study shows that by overcoming the barriers<br />
mentioned by healthcare pr<strong>of</strong>essionals, the ADR reporting<br />
can be improved. Though the improvement is not statistically<br />
significant which may be attributed to short term study<br />
interventions, but if the long term interventions are done<br />
continuously, then there might be statistically significant<br />
improvement in attitude towards ADR reporting.<br />
Few healthcare pr<strong>of</strong>essionals also felt that lack <strong>of</strong><br />
incentives/remuneration could be a barrier to ADR reporting.<br />
A study had shown that providing remuneration for reporting<br />
an ADR can considerably increase the rates <strong>of</strong> reporting drug<br />
reactions, but more evaluation <strong>of</strong> the use <strong>of</strong> remuneration is<br />
26<br />
required.<br />
Other suggestions like inclusion <strong>of</strong> pharmacovigilance in<br />
UG/PG curriculum and establishment <strong>of</strong> pharmacovigilance<br />
centre in tertiary care hospitals are worth considering and<br />
implementing to improve ADR reporting. It is important to<br />
note here that teaching the students right from the Under<br />
Graduate level regarding pharmacovigilance can stimulate<br />
them towards pharmacovigilance and major obstacles like<br />
lack <strong>of</strong> awareness can be overcome. Majority <strong>of</strong> the<br />
participants suggested that compulsory reporting or legal<br />
compulsion to report can improve ADR reporting. This<br />
suggestion is also valuable as it is found that maximum<br />
number <strong>of</strong> ADR reports come from nations in which ADR<br />
27<br />
reporting is compulsory.<br />
CONCLUSION<br />
This study shows that there is a direct need to create<br />
awareness among the health care pr<strong>of</strong>essionals regarding<br />
ADR and its reporting. The study also proves that with<br />
adequate practical training and education, the attitude <strong>of</strong> the<br />
health care pr<strong>of</strong>essionals can be influenced positively which<br />
may in turn have positive impact on number <strong>of</strong> ADRs<br />
reported. Pharmacist can play a very important role in<br />
facilitating pharmacovigilance activities by assisting doctors<br />
and nurses in reporting ADR. There is a need to conduct and<br />
encourage Continuing Pr<strong>of</strong>essional Development to<br />
consistently stimulate healthcare pr<strong>of</strong>essionals to report ADR<br />
and ensure patient safety.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 30
Ganachari MS- Impact <strong>of</strong> Educational Interventions on Adverse Drug Reaction Reporting<br />
REFERENCES<br />
1. World health organization collaborating centre for<br />
International drug monitoring. Geneva: World health<br />
o r g a n i z a t i o n . 1 9 8 4 , W H O p u b l i c a t i o n<br />
DEM/NC/84.153(E).<br />
2. Classen DC, Pestotnik SL, Evans S, Lloyd JF, Burke JP.<br />
Adverse Drug Events in Hospitalized patients: excess<br />
length <strong>of</strong> stay, extra costs and attributable mortality.<br />
JAMA 1997; 227(4): 301-306.<br />
3. Pirmohamed M, James S, Meakin S, Green C, Scott AK,<br />
Walley TJ et al. Adverse drug reactions as cause <strong>of</strong><br />
admission to hospital: prospective analysis <strong>of</strong> 18820<br />
patients. BMJ 2004; 329: 15-19.<br />
4. Brvar M, Fokter N, Bunc M, Mozina M. The frequency <strong>of</strong><br />
adverse drug reaction related admissions according to<br />
method <strong>of</strong> detection, admission urgency and medical<br />
department specialty. BMC Clinical pharmacology 2009;<br />
9:8.<br />
5. Lazarou J, Pomeranz BH, Corey PN. Incidence <strong>of</strong><br />
Adverse drug reactions in hospitalised patients: A Meta<br />
analysis <strong>of</strong> prospective studies. JAMA 1998; 279(15):<br />
1200-1205.<br />
6. Wysowski DK, Swartz L. Adverse drug event<br />
surveillance and drug withdrawals in the United States,<br />
1969-2002: the importance <strong>of</strong> reporting suspected<br />
reactions. Arch Intern Med 2005; 165:1363-1369.<br />
7. Ahmad SR. Adverse drug event monitoring at the food<br />
and drug administration: Your report can make a<br />
difference. J Gen Intern Med 2003; 18:57-60.<br />
8. Ekman E, Backstrom M. Attitudes among hospital<br />
physicians to the reporting <strong>of</strong> adverse drug reactions in<br />
Sweden. Eur J Clin Pharmacol 2009; 65(1):43-46.<br />
9. Zolezzi M, Parsotam N. Adverse drug reaction reporting<br />
in New Zealand: implication for pharmacists.<br />
Therapeutics and clinical risk management 2005;<br />
1(3):181-188.<br />
10. Oshikoya KA, Awobusuyi JO. Perceptions <strong>of</strong> doctors to<br />
adverse drug reaction reporting in a teaching hospital in<br />
Lagos, Nigeria. BMC Clinical Pharmacology 2009; 9:14.<br />
11. McGettigan P, Golden J, Conroy RM Arthur N, Feely J.<br />
Reporting <strong>of</strong> adverse drug reactions by hospital doctors<br />
and response to intervention. Br J Clin Pharmacol 1997;<br />
44(1):98-100.<br />
12. Belton KJ, Lewis SC, Payne S, Rawlins MD. Attitudinal<br />
survey <strong>of</strong> adverse drug reaction reporting by medical<br />
practitioners in the United Kingdom. Br J Clin Pharmacol<br />
1995; 39(3):223-226.<br />
13. Figueiras A, Herdeiro MT, Polonia J, Gestal-Otero JJ. An<br />
educational intervention to improve physician reporting<br />
<strong>of</strong> adverse drug reactions. A clustered randomized<br />
controlled trial. JAMA 2006; 269(9):1086-1093.<br />
14. Scott HD, Renshaw AT, Rosenbaum SE, Waters WJ,<br />
Green M, Andrews LG et al. Physician reporting <strong>of</strong><br />
adverse drug reactions- results <strong>of</strong> the Rhode Island<br />
adverse drug reaction reporting project. JAMA 1990;<br />
263(13):1785-1788.<br />
15. Davis D, Thomson O'Brien MA, Freemantle N, Wolf FM,<br />
Mazmanian P, Vaisey AT. Impact <strong>of</strong> formal Continuing<br />
Medical Education: Do conferences, workshops, rounds<br />
and other traditional continuing education activities<br />
change physician behaviour or healthcare outcomes<br />
JAMA 1999; 282(9):867-874.<br />
16. Davis DA, Thomson MA, Oxman AD, Haynes RB.<br />
Changing Physician performance- A systematic review<br />
<strong>of</strong> the effect <strong>of</strong> continuing medical education strategies.<br />
JAMA 1995; 274(9):700-705.<br />
17. Tabali M, Jeschke E, Bockelbrink A, Witt CM, Willich<br />
SN, Ostermann T et al. Educational intervention to<br />
improve physician reporting <strong>of</strong> adverse drug reaction<br />
(ADRs) in a primary care setting in complementary and<br />
alternative medicine. BMC Public Health 2009; 9:274.<br />
18. Gedde-Dahl A, Harg P, Stenberg-Nilsen H, Buajordet M,<br />
Granas AG, Horn AM. Characteristics and quality <strong>of</strong><br />
adverse drug reaction reports by pharmacists in Norway.<br />
Pharmacoepidemiol Drug Saf 2007; 16:999-1005.<br />
19. Green CF, Mottram DR, Rowe PH, Pirmohamed M.<br />
Attitudes and knowledge <strong>of</strong> hospital pharmacist to<br />
adverse drug reaction reporting. Br J Clin Pharmacol<br />
2001; 51(1):81-86.<br />
20. Winstanley PA, Irvin LE, Smith JC, Orme ML,<br />
Breckenridge AM. Adverse drug reactions: a hospital<br />
pharmacy based reporting scheme. Br J Clin Pharmacol<br />
1989; 28:113-116.<br />
21. Ramesh M, Parathasarthi G. Adverse drug reactions<br />
reporting: Attitudes and Perceptions <strong>of</strong> medical<br />
practitioners. Asian <strong>Journal</strong> <strong>of</strong> Pharmaceutical and<br />
Clinical Research 2009; 2(2):10-14.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 30
Ganachari MS- Impact <strong>of</strong> Educational Interventions on Adverse Drug Reaction Reporting<br />
22. Kees VanGroothest MD, Olsson S, Couper M, Berg LJ.<br />
Pharmacists' role in reporting adverse drug reactions in an<br />
international perspective. Pharmacoepidemiol Drug Saf<br />
2004; 13:457-464.<br />
23. FIP statement <strong>of</strong> policy. The role <strong>of</strong> the pharmacist in<br />
pharmacovigilance. International Pharmaceutical<br />
Federation. Brazil;2006. Available from: URL:<br />
http://www.fip.org/www/uploads/database_file.phpid=<br />
273&table_id=<br />
24. Castel JM, Figueras A, Pedros C, Laporte JR, Capella D.<br />
Stimulating adverse drug reaction reporting: effect <strong>of</strong> a<br />
drug safety bulletin and <strong>of</strong> including yellow cards in<br />
prescription pads. Drug Saf 2003; 26(14):1049-1055.<br />
25. Granas AG, Buajordet m, Stenberg- Nilsen H, Harg P,<br />
Horn AM. Pharmacists' attitudes towards the reporting <strong>of</strong><br />
suspected adverse drug reactions in Norway.<br />
Pharmacoepidemiol Drug Saf 2007; 16:429-434.<br />
26. Feely J, Moriarty S, Conner PO. Stimulating reporting <strong>of</strong><br />
adverse drug reactions by using a fee. BMJ 1990; 300:22-<br />
23.<br />
27. UR35. Uppsala reports October 2006. [online] October<br />
2006 [cited Jun 2010]. Available from: URL: www.whoumc.org/graphics/9628.pdf<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 32
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
Association <strong>of</strong> Pharmaceutical Teachers <strong>of</strong> India<br />
Awareness about ways <strong>of</strong> transmission <strong>of</strong> AIDS and its treatment among<br />
university students in Pakistan<br />
1 1<br />
Tehzeeb-ul-Nisa, Imran Qadir M *, Hibba-tul-Baseer, Dure-Shehwar, Farzana C , Irfan M<br />
College <strong>of</strong> <strong>Pharmacy</strong>, G.C. University, Faisalabad, Pakistan<br />
1<br />
Institute <strong>of</strong> Pharmaceutical Sciences, University <strong>of</strong> Veterinary and Animal Sciences, Lahore, Pakistan.<br />
A B S T R A C T<br />
To assess knowledge <strong>of</strong> students about AIDS, its ways <strong>of</strong> transmission and its treatment. Students (N = 500) at a public university in the Pakistan<br />
completed a questionnaire during November 2008 to February 2010 assessing knowledge <strong>of</strong> students about AIDS, its ways <strong>of</strong> transmission and<br />
its treatment. 99.00% students knew that AIDS is incurable. But less number <strong>of</strong> students were aware about the different ways <strong>of</strong> transmission <strong>of</strong><br />
AIDS. It is concluded from the study that the knowledge about the ways <strong>of</strong> transmission <strong>of</strong> AIDS must be increased to prevent the disease.<br />
Key Words: AIDS, transmission, Awareness, knowledge<br />
Submitted: 14/11/2010<br />
Accepted: 21/12/2010<br />
INTRODUCTION<br />
Human immunodeficiency virus (HIV) is the causative agent<br />
<strong>of</strong> acquired immunodeficiency syndrome (AIDS). HIV is a<br />
member <strong>of</strong> the genus Lentivirus <strong>of</strong> family Retroviridae. Most<br />
<strong>of</strong> the Lentiviruses are responsible for a variety <strong>of</strong><br />
neurological and immunological diseases, but not directly<br />
1,2<br />
implicated in malignancies.<br />
AIDS was first properly defined by Centers for Disease<br />
Control (CDC), USA in December 1981 as a disease causing<br />
acquired immunodeficiency. AIDS is an appropriate name<br />
because people acquire the condition rather than inheriting it;<br />
because it results in a deficiency within the immune system<br />
and because it is a syndrome with a number <strong>of</strong> manifestations,<br />
3<br />
rather than a single disease. In 1983, Luc Montagnier and his<br />
co-workers at the Pasteur Institute in France first discovered<br />
4<br />
the virus that causes AIDS. They called it lymphadenopathyassociated<br />
virus (LAV). A year later, Robert Gallo and<br />
associates <strong>of</strong> the United States confirmed the discovery <strong>of</strong> the<br />
virus, but they renamed it human T-lymphotropic virus type-<br />
5<br />
III “HTLV-III”. The dual discovery led to considerable<br />
scientific disagreement, and it was not until President<br />
Mitterrand <strong>of</strong> France and President Reagan <strong>of</strong> the USA met,<br />
the major issues were resolved. In 1986, both the French and<br />
the U.S. names for the virus itself were dropped in favour <strong>of</strong><br />
6<br />
the new term, human immunodeficiency virus.<br />
Address for Correspondence:<br />
M. Imran Qadir,<br />
E-mail: mrimranqadir@hotmail.com<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
HIV transmission from one person to the other requires a<br />
direct exchange <strong>of</strong> body fluids, such as blood or blood<br />
products, breast milk, semen, or vaginal secretions, most<br />
commonly as a result <strong>of</strong> sexual activity or the sharing <strong>of</strong><br />
needles among drug users. Such transmission may also occur<br />
from mother to baby during pregnancy or at birth. Saliva,<br />
tears, urine, feces, and sweat do not appear to transmit the<br />
3,6,7,8<br />
virus.<br />
Pakistan is one <strong>of</strong> the developing countries <strong>of</strong> South Asia.<br />
Reporting the country's first case in 1987, the National AIDS<br />
Control Program (NACP) <strong>of</strong> the Government <strong>of</strong> Pakistan<br />
reports a cumulative total <strong>of</strong> 1813 HIV/AIDS cases and an<br />
estimated HIV prevalence <strong>of</strong> 0.1 % as <strong>of</strong> October 2001.<br />
Pakistan enjoyed with the low prevalence phase <strong>of</strong> epidemic<br />
from 1987 to 2003. By 1999, approximately three-fourths <strong>of</strong><br />
reported HIV infections in Pakistan occurred in migrant<br />
workers returning from the Arab Gulf states. Since then,<br />
HIV/AIDS infections are increasingly being found among<br />
injecting drug users (IDUs), commercial sex workers<br />
(CSWs), and prison inmates. In 2003, an outbreak <strong>of</strong> HIV<br />
among injecting drug users (IDUs) in one city heralded the<br />
onset <strong>of</strong> HIV epidemic in the country. Currently the national<br />
average prevalence <strong>of</strong> HIV among injecting drug users is<br />
nearly 20%. It has been reported that throughout the world,<br />
the most rapid increase in HIV infection is in Southeast Asian<br />
countries including India and Pakistan. From the United<br />
Nations and Government report, the number <strong>of</strong> HIV/AIDS<br />
cases has been increased upto 85,000 ranging from lowest<br />
estimate 46,000 to highest estimate 210,000.<br />
33
Imran Q M-Awareness about ways <strong>of</strong> transmission <strong>of</strong> AIDS and its treatment among university students in Pakistan<br />
(http://en.wikipedia.org,www.un.org.pk/unaids,www.pacpn<br />
wfp.gov.pk, www.amfar.org).<br />
OBJECTIVES<br />
AIDS is incurable disease. Only the way to escape from AIDS<br />
is the prevention from its transmission. Objective <strong>of</strong> the<br />
present study was to investigate the extent <strong>of</strong> knowledge <strong>of</strong><br />
the student about the treatment and ways <strong>of</strong> transmission <strong>of</strong><br />
AIDS.<br />
Methodology<br />
A questionnaire was developed and the study was conducted<br />
from November 2008 to February 2010. A total <strong>of</strong> 500<br />
students from different departments <strong>of</strong> GC University,<br />
Faisalabad, Pakistan were invited to participate in the study.<br />
Faisalabad is the third largest city <strong>of</strong> Pakistan and is known for<br />
its textile industry, in fact known as the Manchester <strong>of</strong><br />
Pakistan. Faisalabad district had a population <strong>of</strong> about 5.4<br />
million.<br />
The questionnaire as given in Appendix 1 contains 5<br />
questions regarding awareness about ways <strong>of</strong> transmission<br />
and treatment <strong>of</strong> AIDS: What is AIDS What is infective<br />
agent <strong>of</strong> AIDS What are the ways <strong>of</strong> AIDS transmission<br />
What is treatment <strong>of</strong> AIDS What are the ways for prevention<br />
from AIDS The results were compared by making the<br />
percentage among the respondent.<br />
RESULTS<br />
Out <strong>of</strong> 500 students, 348 answered the questionnaire and the<br />
remaining did not responded. Knowledge <strong>of</strong> the students <strong>of</strong><br />
GC University, Faisalabad, Pakistan about AIDS in percent <strong>of</strong><br />
the total respondent is given in Table.1. 78.74% <strong>of</strong> the<br />
students did not know what is AIDS Knowledge <strong>of</strong> the<br />
students <strong>of</strong> GC University, Faisalabad, Pakistan about<br />
infective agent <strong>of</strong> AIDS is given in Table.2. 58.91% students<br />
knew that HIV is the infective agent <strong>of</strong> AIDS. Knowledge <strong>of</strong><br />
the GC university students about treatment <strong>of</strong> AIDS is given<br />
in Table.3. 99.00% students knew that AIDS is incurable. GC<br />
University students' knowledge about ways <strong>of</strong> transmission<br />
<strong>of</strong> AIDS is given in Table.4. 53.74% people knew that AIDS<br />
may be transmitted by unprotected sex. Only 4.02% people<br />
knew that AIDS may be transmitted by mother to child during<br />
feeding and birth. 48.85% people knew that AIDS may be<br />
transmitted by sharing unsterilized instruments/injections.<br />
43.67% people knew that AIDS may be transmitted by<br />
transfusion <strong>of</strong> contaminated blood.<br />
DISCUSSION<br />
AIDS is an infectious disease caused by the human<br />
immunodeficiency virus (HIV). Researches are being done to<br />
9<br />
invent the medicines for treatment <strong>of</strong> AIDS. However, now a<br />
10<br />
days prevention is approachable than treatment. Prevention<br />
may be only possible when the people know the ways <strong>of</strong><br />
transmission <strong>of</strong> AIDS. Many <strong>of</strong> the factors that contribute to<br />
Table.1 Knowledge <strong>of</strong> the students <strong>of</strong> GC University, Faisalabad, Pakistan about AIDS (% <strong>of</strong> Respondent)<br />
Sl.No What is AIDS Male Female Toatal<br />
1 A disease which damage immune system 7.47 12.07 19.54<br />
2 Wrong information<br />
1.15 0.57 1.72<br />
3 Have no information<br />
25 53.74 78.74<br />
Table.2. Knowledge <strong>of</strong> the students <strong>of</strong> GC University, Faisalabad, Pakistan about infective<br />
agent <strong>of</strong> AIDS (% <strong>of</strong> Respondent)<br />
Sl.No Causative agent <strong>of</strong> AIDS Male Female Toatal<br />
1 Virus (HIV)<br />
20.40 38.51 58.91<br />
2 Wrong information<br />
1.15 0.29 1.44<br />
3 Have no information<br />
17.24 22.41 39.65<br />
Table.3. Knowledge <strong>of</strong> the students <strong>of</strong> GC University, Faisalabad, Pakistan<br />
about treatment <strong>of</strong> AIDS (% <strong>of</strong> Respondent)<br />
Sl.No Treatment <strong>of</strong> AIDS Male Female Toatal<br />
1 Incurable<br />
38.70 61.19 99.00<br />
2 Wrong information<br />
0.09 0.02 0.11<br />
3 Have no information<br />
0 0 0<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
34
Imran Q M-Awareness about ways <strong>of</strong> transmission <strong>of</strong> AIDS and its treatment among university students in Pakistan<br />
Table 4: Knowledge <strong>of</strong> the students <strong>of</strong> GC University, Faisalabad, Pakistan about<br />
ways <strong>of</strong> transmission <strong>of</strong> AIDS (% <strong>of</strong> Respondent)<br />
Sl.No Ways <strong>of</strong> AIDS transmission Male Female Toatal<br />
1 Unprotected sex<br />
28.74 25.00 53.74<br />
2 Mother to child during feeding and birth 0.57 3.45 4.02<br />
3<br />
4<br />
5<br />
6<br />
Sharing unsterilised instruments/injections<br />
Transfusion <strong>of</strong> contaminated blood<br />
Wrong information<br />
Wrong information<br />
18.97 29.88 48.85<br />
12.64 31.03 43.67<br />
4.31 5.46 9.77<br />
9.48 13.51 22.99<br />
the spread <strong>of</strong> HIV are inextricably link to social structures and<br />
conditions that shape individual abilities to control exposure<br />
to risk <strong>of</strong> infection in Pakistan. Poverty is a major<br />
development concern in Pakistan, and may be an important<br />
facilitating factor in the further spread <strong>of</strong> HIV. The poor suffer<br />
not just limitations in income but such limitations also<br />
increase the likelihood that those who are most vulnerable are<br />
the least able to protect themselves from HIV infection, and<br />
once infected, are the least able to gain access to the health and<br />
social support that they need. Gender inequalities may also<br />
play a significant role in further spread <strong>of</strong> HIV in Pakistan.<br />
Pakistani women in general have lower socioeconomic status,<br />
less mobility, and less decision-making power than do<br />
Pakistani men, all <strong>of</strong> which contribute to their vulnerability to<br />
HIV.<br />
Some individuals and groups are especially vulnerable to<br />
HIV/AIDS due to their social status, particular behavior<br />
patterns, or other special characteristics. Female sex workers<br />
(FSW) and female migrant workers are for the most part<br />
unable to negotiate safer sexual practices, are <strong>of</strong>ten exploited<br />
and abused, and have little resources due to their marginal<br />
social status and because <strong>of</strong> limited legal protection. Injecting<br />
drug users (IDUs) are at high risk <strong>of</strong> HIV infection because<br />
they <strong>of</strong>ten engage in unsafe practices such as the sharing <strong>of</strong><br />
needles and syringes.<br />
CONCLUSION<br />
Almost all the students <strong>of</strong> GC University, Faisalabad,<br />
Pakistan know that AIDS is incurable. But few students were<br />
aware about the ways <strong>of</strong> transmission <strong>of</strong> AIDS. A strategy to<br />
increase the knowledge <strong>of</strong> students about the ways <strong>of</strong><br />
transmission <strong>of</strong> AIDS should be developed as the infection<br />
and spread <strong>of</strong> AIDS may only be prevented by knowledge.<br />
Some suggested strategies include conducting conferences,<br />
workshops, training course and also to organize 1 day camps<br />
to impart knowledge to the students about AIDS.<br />
REFERENCES<br />
1. Gardner MB, Endres M, Barry PA. The simian<br />
retroviruses: SIV and SRV. In: The retroviridae (Levy JA,<br />
ed). New York (NY): Plenum Press 1994:133-276.<br />
2. Luciw PA. Human immunodeficiency virus and their<br />
replication. In: Field virology (Fields BN, Knippe DM,<br />
Howley PM, eds). Philadelphia (PA): Lippincott-Raven<br />
1996:1881-1952.<br />
3. Connor S, Kingman S. The search for the virus, the<br />
scientific discovery <strong>of</strong> AIDS and the quest for a cure.<br />
Penguin Books 1998:14<br />
4. Barre-Sinoussi F, Chermann JC, Rey F, Nugeyre MT,<br />
Chamaret S, Gruest J, et.al. Isolation <strong>of</strong> a T-lymphotropic<br />
retrovirus from a patient at risk for Acquired Immune<br />
D e f i c i e n c y S y n d r o m e ( A I D S ) . S c i e n c e<br />
1983;220:868–871.<br />
5. Popovic M, Sarngadharan MG, Read E, Gallo RC.<br />
Detection, isolation, and continuous production <strong>of</strong><br />
cytopathic retroviruses (HTLV-III) from patients with<br />
AIDS and pre-AIDS. Science 1984; 224:497-500.<br />
6. C<strong>of</strong>fin J, Haase A, Levy JA, Montagnier L, Oroszlan S,<br />
Teich N, et.al. What to call the AIDS virus. Nature 1986;<br />
321:310.<br />
7. Blankson JN, Persaud D, Siliciano RF. The challenge <strong>of</strong><br />
viral reservoirs in HIV-1 infection. Annu Rev Med 2002;<br />
53:557-593.<br />
8. Busch MP, Amad Z El, Sheppard HW, Ascher MS, Lang<br />
W. Primary HIV-1 Infection. N Engl J Med 1991;<br />
325:733.<br />
9. Qadir MI, Malik SA. HIV Fusion Inhibitors. Rev Med<br />
Virol 2010, 20:23-33.<br />
10. Kain WD. Population Education News 1992; 19(4):14-<br />
16.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
35
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
Association <strong>of</strong> Pharmaceutical Teachers <strong>of</strong> India<br />
Study <strong>of</strong> prescribing patterns <strong>of</strong> antibiotics used in the management <strong>of</strong><br />
various infectious diseases<br />
Azizullah S G*, Jabeen G, Shobna J, Kaleemuddin S, Mohiuddin<br />
Bharat Institute <strong>of</strong> Technology (<strong>Pharmacy</strong>), Mangalpally (V) Ibrahimpatnam, Rangareddy (Dist), A.P, India, 501510.<br />
A B S T R A C T<br />
Submitted: 10/12/2010<br />
Accepted: 3/1/<strong>2011</strong><br />
The Antibiotic prescribing patterns, Demographic pr<strong>of</strong>ile and Prevalence <strong>of</strong> Infectious diseases were prospectively studied in 110 (67 male and<br />
43 female) hospitalized patients suffering with various infectious diseases at KIMS, Secunderabad over a period <strong>of</strong> 9 months. The patients were<br />
distributed into different age groups. Patients less than 20 years were excluded from the study. The maximum number <strong>of</strong> patients 37 (33.63%)<br />
was in the age group <strong>of</strong> 60-69 and the least number <strong>of</strong> patients 2 (1.8%) were found in 20-29 age group. The Body Mass Index <strong>of</strong> most <strong>of</strong> the<br />
patients 64 (58.18%) were found to be in the normal range, 20 (18.2%) patients were found to be as underweight and 26 (23.62%) patients were<br />
scrutinized as overweight. 57 (52.72%) patients underwent dual therapy, 38 (34.56%) patients underwent triple therapy and 7 (6.36%) patients<br />
underwent monotherapy and 7 (6.36%) patients were treated with more than three drugs. The present study reveals that, dual therapy<br />
(Cilastin+Imipenem) was maximally used in the management <strong>of</strong> various types <strong>of</strong> infectious diseases. The CNS infections were present as major<br />
infections, in majority <strong>of</strong> patients during the study period. Diabetes mellitus was found to be present as a major co-morbid condition in majority <strong>of</strong><br />
patients along with Hypertension, Hypothyroidism and Seizures.<br />
Key words: Antibiotics, Demographic pr<strong>of</strong>ile, Seizure, Hypothyroidism.<br />
INTRODUCTION<br />
Despite decades <strong>of</strong> dramatic progress in their treatment and<br />
prevention, infectious diseases remain a major cause <strong>of</strong> death<br />
and debility and are responsible for worsening the living<br />
conditions <strong>of</strong> many millions <strong>of</strong> people around the world.<br />
Infections frequently challenge the physician's diagnostic<br />
skill and must be considered in the differential diagnoses <strong>of</strong><br />
syndromes affecting every organ system.1<br />
Antibiotics are the most frequently prescribed drugs among<br />
hospitalized patients especially in intensive care and surgical<br />
department. Programs designed to encourage appropriate<br />
antibiotic prescriptions in health institutions are an important<br />
element in quality <strong>of</strong> care, infection control and cost<br />
containment.2-5<br />
Antibiotics were once considered 'miracle drugs' and have<br />
been used for decades to effectively treat a variety <strong>of</strong> bacterial<br />
infections. Unfortunately, widespread use and misuse<br />
worldwide have led to the emergence <strong>of</strong> 'super bugs' and other<br />
drug-resistant bacteria.6–8 Unnecessary use <strong>of</strong> antibiotics has<br />
Address for Correspondence:<br />
Azizulla SG, Bharat Institute <strong>of</strong> Technology (<strong>Pharmacy</strong>), Mangalpally (V) Ibrahimpatnam,<br />
Rangareddy (Dist), A.P, India, 501510.<br />
Email : azizghori2005@yahoo.co.in<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
also given rise to an increased risk <strong>of</strong> side effects, high costs<br />
and effects requiring medical attention.<br />
The purpose <strong>of</strong> this study is to create awareness among the<br />
physicians about the efficient and rational prescribing pattern<br />
systems <strong>of</strong> various medications especially antibiotics in order<br />
to make sure the usage <strong>of</strong> antibiotics in a rational way.<br />
The serious complications and unwanted reactions reported<br />
due to inappropriate prescribing <strong>of</strong> antibiotics, has been found<br />
to be increasing predominantly. Hence, these consequences<br />
made me to urge in carrying out the study.<br />
MATERIAL AND METHODS<br />
The study was performed at KIMS Hospital, Secunderabad. A<br />
prospective observational study was carried out for a period<br />
<strong>of</strong> 9 months in 110 hospitalized patients by scrutinizing the<br />
inpatients case sheets. All the patients treated with Antibiotics<br />
for various infections, admitted in Intensive care unit <strong>of</strong><br />
KIMS hospital, patients who were willing to participate, were<br />
included in the study. Patients below the age <strong>of</strong> 18 years and<br />
patients who are not willing to participate in the study were<br />
excluded. Patients were divided into different groups<br />
according to their age and sex. Data for the present study was<br />
collected by scrutinizing inpatient case sheets. The data<br />
collected was analyzed for the prescribing patterns <strong>of</strong><br />
36
Azizulla S G - Study <strong>of</strong> prescribing patterns <strong>of</strong> antibiotics used in the management <strong>of</strong> various infectious diseases<br />
antibiotics and demographic pr<strong>of</strong>ile <strong>of</strong> the patients.<br />
The patients enrolled in the study were grouped based on the<br />
number <strong>of</strong> Antibiotics prescribed.<br />
Group 1-Monotherapy-Single Antibiotic was used, Group 2-<br />
Dual therapy-Two Antibiotics were used, Group 3-Triple<br />
therapy-Three Antibiotics were used and Group 4- More than<br />
three Antibiotics were used.<br />
RESULTS AND DISCUSSION<br />
Demographic Pr<strong>of</strong>ile<br />
Gender Distribution:<br />
The results reveal that 67 patients were male and 43 patients<br />
were females out <strong>of</strong> 110 patients. Careful literature reveals<br />
that there is no correlation between gender and occurrence <strong>of</strong><br />
infections.<br />
Age Distribution:<br />
Table 1 shows the distribution <strong>of</strong> patients recruited for the<br />
study in different age groups. The results reveals that<br />
maximum number <strong>of</strong> patients (37) were found to be in age<br />
group <strong>of</strong> 60-69, followed by 31 patients belongs to the age<br />
group <strong>of</strong> 50-59.only (2) patients were found to be in the age<br />
Table1: Age (in years) distribution<br />
Age in years (Yrs) No. <strong>of</strong> patients Percentage (%)<br />
20-29 02 1.8<br />
30-39 09 8.2<br />
40-49 22 20<br />
50-59 31 28.2<br />
60-69 37 33.63<br />
70-79 06 5.45<br />
80-89 03 2.72<br />
Total(*N) 110 100<br />
Table 2: Educational status<br />
Occupation No. <strong>of</strong> patients Percentage (%)<br />
Grade-0<br />
(uneducated) 36 32.72<br />
Grade- 1<br />
(up to 9 th standard) 28 25.45<br />
Grade-2<br />
(SSC/Inter) 26 23.63<br />
Grade-3<br />
(Graduates/postgraduates) 20 18.20<br />
Total (*N) 110 100<br />
group <strong>of</strong> 20-29.<br />
Careful literature study reveals that there is no correlation<br />
between age and occurrence <strong>of</strong> infections.<br />
Educational Status:<br />
Table 2 shows the Educational status <strong>of</strong> the patients recruited<br />
for the present study. The results reveal that the maximum<br />
number <strong>of</strong> patients 36 was belonged to grade-0 i.e.<br />
Uneducated, least number <strong>of</strong> patients 20 were belonged to<br />
grade-3 (graduates and postgraduates). Careful literature<br />
study reveals that there is no correlation between educational<br />
status and occurrence <strong>of</strong> infections<br />
Body Mass Index (BMI):<br />
Table 3 shows the BMI <strong>of</strong> the patients recruited for the present<br />
study. The results reveal that the maximum numbers <strong>of</strong><br />
patients i.e.; (64) were found to be <strong>of</strong> normal BMI. Only 20<br />
patients were belonged to underweight group.<br />
Prescription Patterns:<br />
For the purpose <strong>of</strong> analyzing the prescribing patterns <strong>of</strong><br />
Antibiotics in the treatment <strong>of</strong> Infections the<br />
pharmacotherapy was classified as Monotherapy, Dual<br />
therapy, Triple therapy and more than three. The results reveal<br />
that the maximum numbers <strong>of</strong> patients i.e.58 were underwent<br />
dual therapy followed by 38 patients with triple therapy. 7<br />
patients <strong>of</strong> each were underwent with More than three and<br />
Monotherapy respectively.<br />
Monotherapy:<br />
Table 5 shows the Types <strong>of</strong> Monotherapy followed during the<br />
Table 3: Body Mass Index (BMI)<br />
BMI No. <strong>of</strong> patients Percentage (%)<br />
Underweight (27.5) 26 23.62<br />
Total (*N) 110 100<br />
Table 4: Prescription patterns<br />
Therapy No. <strong>of</strong> patients Percentage (%)<br />
Monotherapy 07 6.36<br />
Dual therapy 58 52.72<br />
Triple therapy 38 34.56<br />
More than three 07 6.36<br />
Total 110 100<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
37
Azizulla S G - Study <strong>of</strong> prescribing patterns <strong>of</strong> antibiotics used in the management <strong>of</strong> various infectious diseases<br />
study period. The results reveal that out <strong>of</strong> 7 patients, who<br />
underwent Monotherapy, Amikacin was found to be used in 4<br />
patients followed by Meropenem in 3 patients.<br />
Dual Therapy:<br />
Table 6 shows the Details <strong>of</strong> Dual therapy used during the<br />
study period. The results reveal that out <strong>of</strong> 58 patients who<br />
underwent Dual therapy, Cilastin+Imipenem was used in 15<br />
patients followed by 8 patients <strong>of</strong> each were found to be<br />
treated with Ofloxacin + Ornidazole, Cefipime + Tazobactum<br />
respectively. 7 patients were treated with Piperacillin +<br />
Tazobactum. Only 2 patients were found to be treated with<br />
Meropenem + Fluconazole.<br />
Triple Therapy:<br />
Table 7 shows the details <strong>of</strong> Triple therapy. The results reveal<br />
that, out <strong>of</strong> 38 patients who underwent triple therapy, 17<br />
patients were treated with Ceftrioxone + Cilastin + Imipenem<br />
followed by 13 patients treated with Amikacin + Piperacillin<br />
+ Tazobactum. Only 3 patients were treated with Amikacin +<br />
Salbactum + Cefipyrazone. It was found that in triple therapy<br />
at least one fixed dose combination present in single branded<br />
drugs were used along with another drug.<br />
Table5: Drugs used in Monotherapy<br />
Mono Therapy No. <strong>of</strong> patients Percentage (%)<br />
Amikacin 04 57.14<br />
Meropenem 03 42.86<br />
Total(*N) 07 100<br />
Table 6: Drugs used in Dual therapy<br />
Sl. Dual therapy No. <strong>of</strong> Percentage<br />
No patients (%)<br />
1 Cilastin + Imepenem 15 25.86<br />
2 Meropenem + Vancomycin 04 6.89<br />
3 Fluconazole + Colomycin 04 6.89<br />
4 Ofloxacin + Ornidazole 08 13.79<br />
5 Piperacillin + Tazobactum 07 12.06<br />
6 Colomycin + Imepenem 03 5.17<br />
7 Cefazolin + Amikacin 04 6.89<br />
8 Meropenem + Teicoplanin 03 5.17<br />
9 Cefipime + Tazobactum 08 13.79<br />
10 Meropenem + Fluconazole 02 3.49<br />
Total(*N) 58 100<br />
Table 7: Drugs used in Triple therapy<br />
Triple Therapy No. <strong>of</strong> Percentage<br />
patients (%)<br />
Ceftrioxone +<br />
(Cilastin+Imipenem) 17 44.7<br />
Amikacin<br />
(Piperacillin + Tazobactum) 13 34.21<br />
Amikacin<br />
(Salbactum + Cefipyrazone) 03 7.89<br />
Fluconazole<br />
(Cefipime + Tazobactum) 05 13.17<br />
Total (*N) 38 100<br />
Table 8: Therapy in which More than three drugs has been used<br />
More than 3 Drugs No. <strong>of</strong> Percentage<br />
patients (%)<br />
1.(Piperacillin + Tazobactum)<br />
+<br />
(Cilastin + Imipenem) 04 57.14<br />
2.(Amoxycillin + Clavulanic<br />
acid) +<br />
(Salbactum + Cefipyrazone)<br />
+<br />
(Cilastin + Imipenem) 03 42.86<br />
Total (*N) 07 100<br />
More Than Three drugs:<br />
The table 8 shows the details <strong>of</strong> More than 3 drugs that were<br />
used. The results reveals that 4 patients were treated with 4<br />
antibiotics which were found in two fixed dose combination<br />
followed by 3 patients treated with 6 antibiotics which were<br />
found in three fixed dose combinations.<br />
Details <strong>of</strong> Infections:<br />
The results reveal that CNS Infections were found to be<br />
present in majority <strong>of</strong> patients ie; 51 patients, followed by 35<br />
patients with UTI and 22 patients with RTI.<br />
Details <strong>of</strong> Comorbidities found during the study:<br />
The results reveal that majority <strong>of</strong> the patients were found<br />
with multiple comorbidities i.e. 67 patients followed by 31<br />
patients with Single co morbidity and 12 patients without<br />
comorbidity were found.<br />
Details <strong>of</strong> Single Co-morbidity:<br />
The results reveal that Diabetes mellitus was found to be<br />
present in 21 patients out <strong>of</strong> 31 patients having single co<br />
morbidity and 10 patients with Hypertension<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
38
Azizulla S G - Study <strong>of</strong> prescribing patterns <strong>of</strong> antibiotics used in the management <strong>of</strong> various infectious diseases<br />
Details <strong>of</strong> Multiple Co-morbidities:<br />
The results reveal that out <strong>of</strong> 67 patients having multiple<br />
comorbidities 31 patients were found with Diabetes mellitus<br />
+ Hypertension followed by 12 patients with Diabetes<br />
mellitus + Seizure, 9 patients with Diabetes mellitus +<br />
Hypothyroidism and 8 patients with Diabetes mellitus +<br />
Hypertension + Hypothyroidism.<br />
CONCLUSION<br />
As there is a strong epidemic rise <strong>of</strong> Infectious diseases in our<br />
country, the present prospective study was carried out to<br />
assess the Prescribing patterns <strong>of</strong> antibiotics.<br />
In order to find out the prevalence <strong>of</strong> Infectious diseases the<br />
age range was divided as per the need. During the study, the<br />
maximum number <strong>of</strong> patients ie; 37 were found to be in the<br />
age group <strong>of</strong> 60-69 years.<br />
Further it was found that 64 patients were to be <strong>of</strong> normal<br />
weight.<br />
The Prescription patterns used to treat the various infections<br />
in the present study, reveals that Dual therapy ie; (Cilastin +<br />
Imipenem) was maximally used.<br />
The CNS infections were present as major infections in<br />
majority <strong>of</strong> the patients ie; 51 during the study period.<br />
Diabetes mellitus was found to be present as a major comorbid<br />
condition in majority <strong>of</strong> patients along with<br />
Hypertension, Hypothyroidism and Seizures.<br />
In India, the role <strong>of</strong> clinical pharmacy is still in infancy stage,<br />
but the clinical pharmacist can keep the physicians abreast<br />
about the latest antibiotics and their usage, in order to make<br />
sure the use <strong>of</strong> antibiotics in a rational way.<br />
The present study was restricted only for a period <strong>of</strong> 9 months<br />
so therefore the exact prescription pattern cannot be revealed,<br />
in order to do so the study should be carried out for a long<br />
period <strong>of</strong> time.<br />
ACKNOWLEDGEMENTS<br />
The authors are thankful to Dr. Bhaskar Rao, Director <strong>of</strong><br />
KIMS, Secunderabad, Andhra Pradesh, India for providing<br />
necessary facilities to carry out this research project. We are<br />
thankful to Dr. Chalapathi Rao, Director, Education<br />
Department, KIMS. The authors are also grateful to all<br />
doctors who supported during this project in KIMS.<br />
REFERENCES<br />
1. Kasper and Hauser “Harrison's principles <strong>of</strong> internal<br />
medicine”.16th edn:Boston;Mc Graw-Hill Medical<br />
publishing division (p) LTD;2005,695.<br />
2. Goldman DA, Weinstein RA, Wenzel RP. Strategies to<br />
prevent and control the emergence <strong>of</strong> antimicrobial<br />
resistant micro-organisms in hospital. JAMA 1996;<br />
275:234-249.<br />
3. Stevenson RC, et al. Measuring the saving attributable to<br />
an antibiotic prescription policy. J Hosp Infect 1988;<br />
11:16-25.<br />
4. Lesar TS, Briceland LL. Survey <strong>of</strong> antibiotic control<br />
policies in university-affiliated teaching institutions. Ann<br />
Pharmacother 1996; 30:31-34.<br />
5. Strum W. Effects <strong>of</strong> a restrictive antibiotics policy on<br />
clinical efficacy <strong>of</strong> antibiotics and susceptibility patterns<br />
<strong>of</strong> organisms. Eur J Microbiol Infect Dis 1990; 9:381-<br />
389.<br />
6. Russell AD, et.al. Possible link between bacterial<br />
resistance and use <strong>of</strong> antibiotics and biocides. Antimicrob<br />
Agents Chemother 1998; 42:2151.<br />
7. Arason VA, et.al. The role <strong>of</strong> antimicrobial use in the<br />
epidemiology <strong>of</strong> resistant pneumococci: a 10-year follow<br />
up. Microb Drug Resist 2006; 12:169–176.<br />
8. Paulsen IT, et.al. Role <strong>of</strong> mobile DNA in the evolution <strong>of</strong><br />
vancomycin-resistant Enterococcus faecalis. Science<br />
2003; 299: 2071–2074.<br />
9. Kumari Indira K.S et.al., Antimicrobial prescription<br />
patterns for common acute infections in some rural &<br />
urban health facilities <strong>of</strong> India, <strong>Indian</strong> J Med Res August<br />
2008; 128:165-171.<br />
10. Rocio Fernandez Urrusuno et.al., Antibiotic prescribing<br />
patterns and hospital admissions with respiratory and<br />
urinary tract infections, Eur J Pharmacology 2008;<br />
64:1005-1011.<br />
11. Robert A. Fowler et.al., Variability in Antibiotic<br />
Prescribing Patterns and Outcomes in Patients with<br />
Clinically Suspected Ventilator-Associated Pneumonia<br />
Chest 2003; 123(3):835-844.<br />
12. Christopher H S, Chan et.al., A prospective study <strong>of</strong><br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 39
Azizulla S G - Study <strong>of</strong> prescribing patterns <strong>of</strong> antibiotics used in the management <strong>of</strong> various infectious diseases<br />
antibiotic prescribing patterns and clinical outcomes in<br />
patients with community-acquired pneumonia, J Hong<br />
Kong Med Assoc 1991; 43(4):226-229.<br />
13. Yanina Balabanova et.al., Antimicrobial prescribing<br />
patterns for respiratory diseases including tuberculosis in<br />
Russia: a possible role in drug resistance, <strong>Journal</strong> <strong>of</strong><br />
Antimicrobial Chemotherapy 2004; 54:673–679.<br />
14. Norberto Krivoy et.al., Antibiotic prescription and cost<br />
patterns in a general intensive care unit, <strong>Pharmacy</strong><br />
<strong>Practice</strong> 2007; 5(2):67-73.<br />
15. Kees J. Gortera et.al., Risk <strong>of</strong> recurrent acute lower<br />
urinary tract infections and prescription pattern <strong>of</strong><br />
antibiotics in women with and without diabetes in<br />
primary care, Oxford journals medicine family practice<br />
2010; 27(4):379-385.<br />
16. Cecilia Big et.al., Viral Infections <strong>of</strong> the Central Nervous<br />
System: A Case-Based Review, Clinical Medicine &<br />
Research November 2009:864-869.<br />
17. Svein Gjelstad et.al., GPs' antibiotic prescription patterns<br />
for respiratory tract infections - still room for<br />
improvement, Scandinavian <strong>Journal</strong> <strong>of</strong> Primary Health<br />
Care December 2009; 27(4):208–215.<br />
18. Lifang Dong et.al., Antibiotic prescribing patterns in<br />
village health clinics across 10 provinces <strong>of</strong> Western<br />
China, <strong>Journal</strong> <strong>of</strong> Antimicrobial Chemotherapy 2008;<br />
62:410–415.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 40
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
Association <strong>of</strong> Pharmaceutical Teachers <strong>of</strong> India<br />
A study on prescription pattern <strong>of</strong> Antihypertensives<br />
Preethi M*, PraveenKumar N V R T, Lekshmi S, Manna P K, Mohanta G P, Parimalakrishnan S,<br />
Sudarshan S.<br />
Department <strong>of</strong> <strong>Pharmacy</strong>, Annamalai University, Annamalai Nagar – 608002. Tamil Nadu, India.<br />
A B S T R A C T<br />
Submitted: 18/11/2010<br />
Accepted: 16/12/2010<br />
Hypertension is a universal disease and knowledge <strong>of</strong> existing prescribing patterns in the treatment <strong>of</strong> hypertension can provide useful<br />
information for improving clinical practice in this field. The aim <strong>of</strong> our present study was to identify and evaluate the prescribing pattern <strong>of</strong><br />
antihypertensives. This was a prospective observational study and was approved by IRB. Out <strong>of</strong> 1262 prescriptions, the overall sex distribution<br />
<strong>of</strong> study population showed 62.6% <strong>of</strong> male and 37.4% <strong>of</strong> female patients. Total distribution <strong>of</strong> patients with respect to age group showed that<br />
highest number <strong>of</strong> patients was found in the age group <strong>of</strong> 60-69 years (31.3%) and least was found between 20-29 years age group (1.1%).<br />
Majority <strong>of</strong> males in the study population (43.29%) were found to have both the habits <strong>of</strong> smoking and alcohol. Among concomitant diseases that<br />
were related to hypertension Coronary artery disease was highest (67.78%) and giddiness was least (1.7%). In case <strong>of</strong> diseases unrelated to<br />
hypertension Type II diabetes mellitus was observed as highest (38.7%) and acute gastroenteritis was recorded least (5.68%). Overall 43.5%<br />
patients were treated with single antihypertensive drug and 53.8% were treated with antihypertensive drug combinations. The study revealed<br />
that in monotherapy category six classes <strong>of</strong> drugs were used that includes ACE Inhibitors, loop diuretics, calcium channel blockers, β- Blockers,<br />
followed by Angiotensin II antagonists and K Sparing Diuretics. ACE Inhibitors were prescribed most whereas K Sparing diuretics were least<br />
used. From the results <strong>of</strong> this study, we concluded that there is a considerable scope <strong>of</strong> improvement for the use <strong>of</strong> diuretics.<br />
INTRODUCTION<br />
Hypertension is a common disease that is defined as<br />
persistently elevated arterial blood pressure (BP). Although<br />
elevated BP was perceived to be necessary for adequate<br />
perfusion <strong>of</strong> essential organs, it is now identified as one <strong>of</strong> the<br />
most significant risk factors for cardiovascular disease in the<br />
world wide. Hypertension is the most common<br />
cardiovascular disease. Pooling <strong>of</strong> epidemiological studies<br />
shows that hypertension is present in 25% urban and 10%<br />
rural subjects in India. An estimate reveals that there are 31.5<br />
million hypertensive patients in rural and 34 million in urban<br />
populations. A total <strong>of</strong> 70% <strong>of</strong> these would be Stage I<br />
hypertension (systolic BP 140-159 and/or diastolic BP 90-99<br />
1<br />
mmHg.<br />
Antihypertensive agents are among the most used therapeutic<br />
classes. The approach to the pharmacological treatment <strong>of</strong><br />
hypertension is guided by international recommendations,<br />
and adherence to treatment is known to result in effective<br />
prevention <strong>of</strong> cardiovascular risk. Although many drug<br />
Address for Correspondence:<br />
Motaparthi Preethi, Pharm D Intern, Department <strong>of</strong> <strong>Pharmacy</strong>, Annamalai University,<br />
Annamalai Nagar – 608002.Tamil Nadu, India<br />
E-mail : motaparthi_preethi@yahoo.co.in<br />
classes are effective in prevention <strong>of</strong> cardiovascular events<br />
i.e., diuretics, β-blockers, calcium channel blockers,<br />
angiotensin converting enzyme inhibitors, guidelines differ<br />
with regard to which drug class is to be considered as first<br />
choice for the initial treatment <strong>of</strong> hypertension with no<br />
complications.²<br />
Thiazide diuretics have been recommended by the seventh<br />
th 3<br />
report <strong>of</strong> the joint National Committee (JNC 7 ) and the<br />
4<br />
British Hypertension society as the preferred first-line<br />
antihypertensive due to its affordability and evidence on its<br />
efficacy in the prevention <strong>of</strong> cardiovascular events in those<br />
5<br />
with hypertension.<br />
OBJECTIVES<br />
The present study was conducted to identify and evaluate the<br />
prescribing pattern <strong>of</strong> antihypertensives.<br />
METHODOLOGY<br />
The study was prospective observational study and conducted<br />
in tertiary medical teaching hospital situated in the South<br />
India. Patients with hypertension <strong>of</strong> either sex, above 18years<br />
<strong>of</strong> age, with or without co morbidities who met the inclusion<br />
criteria were included in the study. Hypertensive patients who<br />
were pregnant and patients with significant hepatic and renal<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
41
Preethi M- A Study on prescription pattern <strong>of</strong> Antihypertensives<br />
disease were excluded from the study. The Institutional<br />
Human Ethical Committee <strong>of</strong> Annamalai University,<br />
Chidambaram approved the study.<br />
Fig.2: Distribution <strong>of</strong> study population with respect to age group<br />
STUDY DESIGN<br />
Patient enrollment<br />
Patients were enrolled in the study based on inclusion and<br />
exclusion criteria. Following patient enrollment, baseline<br />
information was collected on a standard data documentation<br />
form which contained patient name, age, date <strong>of</strong> admission,<br />
inpatient number, date <strong>of</strong> discharge, social history, reason for<br />
admission, past medical and medication history.<br />
Materials<br />
1. Patient standard data collection form.<br />
2. Prescriptions <strong>of</strong> the patients.<br />
RESULTS AND DISCUSSION<br />
A total <strong>of</strong> 1262 patients who met the inclusion criteria were<br />
selected for the study. The following were results obtained.<br />
Out <strong>of</strong> 1262 patients, the overall sex distribution <strong>of</strong> the study<br />
population showed that there were more (63.6%) male<br />
patients as male patients were at higher risk for hypertension<br />
compared to female patients (37.4%) and this is illustrated in<br />
Fig 1.<br />
It was found that majority <strong>of</strong> the study population were<br />
admitted to the hospital with chief complaints <strong>of</strong> chest pain<br />
318(36.25%), followed by Breathlessness 202(23.03%), and<br />
cough with breathlessness 115(13.11%). The other reasons<br />
for admission were vertigo, epistaxis, and weakness. These<br />
reasons were related to hypertension and as cardiac disease is<br />
major risk factor for hypertension more patients were<br />
admitted with complaint <strong>of</strong> chest pain (fig 4).<br />
Among the reasons unrelated to hypertension diabetes<br />
mellitus was found highest with 43.75% followed by cough<br />
with expectoration 111(28.83%), abdominal pain 48(12.46%)<br />
and others 15.06% (fig 5).<br />
Fig.3: Demographic data based on social habits:<br />
Total distribution <strong>of</strong> patients with respect to age group<br />
showed that highest number <strong>of</strong> patients were found between<br />
the age group <strong>of</strong> 60-69years 395(31.3%) followed by 27.5%<br />
between the age group <strong>of</strong> 50-59years and least number <strong>of</strong><br />
patients were found between 20-29 age group with 1.10%<br />
(Fig 2).<br />
Majority <strong>of</strong> males in the study population 342(43.3%) were<br />
found to have both habits <strong>of</strong> smoking and alcohol followed by<br />
habit <strong>of</strong> only alcohol consumption 169(21.39%), only<br />
smoking 149(18.86%). Only 16.45% were found to be non<br />
smokers and non alcoholics (Fig 3).<br />
Fig.4: Reasons for admission observed in study population<br />
related to hypertension<br />
Fig.1: Demographic data based on sex<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
42
Preethi M- A Study on prescription pattern <strong>of</strong> Antihypertensives<br />
Among concomitant diseases that were related to<br />
hypertension it was found that coronary artery disease was<br />
highest 568(67.78%) followed by Cardio Vascular Accident<br />
173(20.64%) and least was found be giddiness with 1.7%<br />
(fig6).<br />
Coming to diseases unrelated to hypertension Type II diabetes<br />
mellitus was highest 125(38.7%) followed by Chronic<br />
Obstructive Pulmonary Disease 48(14.9%), Bronchial<br />
Asthma 44(13.62%) and least was to be both Acute<br />
Gastroenteritis and lower respiratory tract infections with<br />
24(7.43%). Systemic hypertension cases were found to be<br />
101(8%). As cardiac diseases are major risk factors more<br />
cases were present (fig 7).<br />
Overall, 549(43.5%) patients were treated with a Single<br />
antihypertensive drug and 679(53.8%) were treated with<br />
antihypertensive drug combinations. Antihypertensive drug<br />
combinations were used more because majority <strong>of</strong> patients<br />
had uncontrolled blood pressure levels.<br />
The study revealed that in monotherapy category six classes<br />
<strong>of</strong> drugs were used. These were ACE Inhibitors 298(54.28%),<br />
loop diuretics 88(16.02%), calcium channel blockers<br />
91(16.57%), β- Blockers 29(5.3%), followed by Angiotensin<br />
Fig.5: Reasons for admission observed in study population<br />
unrelated to hypertension<br />
Fig.7 Distribution <strong>of</strong> patients with respect to concomitant<br />
diseases unrelated to hypertension<br />
II antagonists 24(4.37%) and K Sparing Diuretics. Among<br />
Monotherapy, ACE Inhibitors were prescribed most because<br />
these are effective and cheaper and K Sparing diuretics are<br />
least used as these were costlier (fig 8).<br />
Among those who were treated with drug combinations,<br />
70.25% received two drugs, and a two drug combination <strong>of</strong><br />
ACE Inhibitors and Loop diuretics were given to majority <strong>of</strong><br />
patients with 27.25% followed by ACE inhibitors and β-<br />
blockers with 26.2% and the drug combination β- blocker and<br />
Ag II Antagonist was least prescribed with 1.04% (fig 9).<br />
In three drug combination therapy combination <strong>of</strong> ACE<br />
Inhibitors, β-blockers and loop diuretics were prescribed<br />
major with 25.54% and least prescribed were combination <strong>of</strong><br />
Ag II Antagonist, β-blocker and ACE Inhibitor with 2.7% (fig<br />
10).<br />
In combination therapy 27.68% received three drugs, usage <strong>of</strong><br />
four drugs is uncommon and only 2.06% patients were<br />
prescribed four drug combinations (fig 11).<br />
A total <strong>of</strong> about 34 hypertensive patients were not prescribed<br />
any <strong>of</strong> the anti hypertensive drug.<br />
Fig.6: Concomitant diseases observed in study population<br />
related to hypertension<br />
Fig.8: Single drug therapy:<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
43
Preethi M- A Study on prescription pattern <strong>of</strong> Antihypertensives<br />
Fig.9: Two drug combination<br />
In studies conducted by Samir Malhotra, R. S. Karan,<br />
P.Pandhi, Sanjay Jain showed that among 1076 prescriptions<br />
evaluated β-adrenoreceptor blocking agents were most<br />
prescribed with 51% followed by calcium channel blockers<br />
(47%), and ACEI (46%). combination therapy was used<br />
commonly than monotherapy. In two combination therapy, a<br />
drug combination <strong>of</strong> ACEI and β-blocker were prescribed<br />
most with 39.9%, in three drug combination therapy a<br />
combination <strong>of</strong> ACEI, β-blocker and calcium channel blocker<br />
were prescribed more with 11.9% and in four drug<br />
combination therapy, the most commonly prescribed was a<br />
combination <strong>of</strong> ACEI, β-blocker, calcium channel blocker<br />
and α-blocker with 0.7%.<br />
CONCLUSION<br />
Fig.10: Three drug combination:<br />
Despite the availability <strong>of</strong> a wide range <strong>of</strong> antihypertensive<br />
drugs, hypertension and its complications are still important<br />
causes <strong>of</strong> adult morbidity and mortality. More than 50% <strong>of</strong><br />
treated hypertensive patients have a blood pressure greater<br />
than 140/90mm Hg (uncontrolled hypertension). The present<br />
study represents the current prescribing trend for antihypertensive<br />
agents and it highlights certain shortcomings in<br />
the existing prescribing practice. There is a considerable<br />
scope for improvement, particularly the under-utilization <strong>of</strong><br />
diuretics in the present prescribing pattern <strong>of</strong> antihypertensive<br />
drugs. In our study, it was observed that the<br />
treatment for patients depends upon the condition and<br />
severity <strong>of</strong> the patient as well as experience <strong>of</strong> the physician, it<br />
may or may not reflect the JNC VII.<br />
REFERENCES<br />
1. Hum J. Trends in hypertension epidemiology in India.<br />
Hypertens 2004 Feb; 18(2):73-78.<br />
Fig.11: Four drug combinations:<br />
2. Messerli HF, Grossman E, Goldbourt U. Are betablockers<br />
are efficacious as first line therapy for<br />
hypertension in the elderly : A Systemic review. JAMA<br />
1998; 279:1903-1907.<br />
3. The seventh report <strong>of</strong> the Joint National Committee<br />
(JNC) on Prevention, Detection, Evaluation and<br />
Treatment <strong>of</strong> high Blood Pressure. US Department <strong>of</strong><br />
Health and Human Services; May, 2003.<br />
4. British hypertension society guidelines for hypertension<br />
management 1999. BMJ 319(7210) 630-635.<br />
Note: The other 34 patients were not prescribed any <strong>of</strong> the antihypertensives<br />
5. Amery A, Birkenhager W, Brixko P, Bulpitt C, Clement D,<br />
Deruyttere M, et.al. Mortality and morbidity results from<br />
the European working party on high blood pressure in the<br />
elderly trial. Lancet 1985; 1:1349–1354.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 44
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
Association <strong>of</strong> Pharmaceutical Teachers <strong>of</strong> India<br />
Evaluation <strong>of</strong> prescribing pattern <strong>of</strong> clinicians in out-patient departments <strong>of</strong> A<br />
South <strong>Indian</strong> teaching hospital<br />
Ramesh A*, Suhaj A<br />
Department <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong>, JSS College <strong>of</strong> <strong>Pharmacy</strong>, Mysore- 15.<br />
A B S T R A C T<br />
Submitted: 17/11/2010<br />
Accepted: 21/12/2010<br />
A prospective study was conducted to study the drug usage pattern <strong>of</strong> clinicians in out-patient departments at a South <strong>Indian</strong> tertiary care<br />
teaching hospital. WHO prescribing indicators were used to asses the prescribing behavior <strong>of</strong> the clinicians in four select out-patient<br />
departments such as Medicine, Orthopaedics, Paediatrics and Surgery. Randomly 15 to 20 prescriptions per day were selected for review.<br />
Average number <strong>of</strong> drugs prescribed per prescription was found to be 2.32. Percentage <strong>of</strong> drugs prescribed from W.H.O essential drug list was<br />
found to be 75%. Number <strong>of</strong> prescriptions with antibiotics and injections were 23% and 5% respectively. Average consultation time with each<br />
patient was found to be 6-10 minutes. Percentage <strong>of</strong> drugs prescribed by generic name was found to be 5%. Results <strong>of</strong> the study showed a<br />
considerable scope for improving the prescribing pattern <strong>of</strong> clinicians in OPD clinics. Generic prescribing and continuing education on rational<br />
use <strong>of</strong> drugs may improve the prescribing behaviour. Preparation and distribution <strong>of</strong> a hospital formulary may further strengthen the rational use<br />
<strong>of</strong> drugs.<br />
Keywords: Prescribing pattern, Out Patient Department, WHO Prescribing indicators<br />
INTRODUCTION<br />
Drug therapy is primarily initiated to prevent, cure or control<br />
1<br />
the diseases in human beings. Selection <strong>of</strong> medicines mainly<br />
depends on the extent <strong>of</strong> the anticipated benefits and the<br />
minimum unwanted effects with the medication. No drug is<br />
considered to be safe, even when prescribed in therapeutic<br />
doses. Appropriate selection <strong>of</strong> drugs helps in achieving the<br />
desired therapeutic outcomes in patients. In recent times, drug<br />
therapy is becoming more complex, thus making appropriate<br />
prescribing increasingly challenging. Drug related mortality<br />
and morbidity are indeed becoming serious concern for<br />
patients and health care pr<strong>of</strong>essionals. This is warranting<br />
rational selection <strong>of</strong> medicines for treating patients.<br />
According to World Health Organization (WHO), rational use<br />
<strong>of</strong> drugs requires that patients' receive medications<br />
appropriate to their clinical needs, in doses that meet their<br />
own individual requirements, for an adequate period <strong>of</strong> time,<br />
1<br />
and at the affordable cost. WHO has listed out 366 drugs as<br />
2<br />
essential drugs that can take care <strong>of</strong> majority <strong>of</strong> the diseases.<br />
WHO has developed certain indicators to evaluate the drug<br />
usage pattern in various health care facilities. They are<br />
prescribing indicators, patient indicators, facility indicators<br />
Address for Correspondence:<br />
Dr. Ramesh Adepu, Pr<strong>of</strong>essor, Department <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong>, JSS College <strong>of</strong><br />
<strong>Pharmacy</strong>,Mysore- 570 015.<br />
Email: adepu63@rediffmail.com<br />
and complimentary indicators. These indicators are used to<br />
monitor treatment practices and prescribing behavior <strong>of</strong> the<br />
3<br />
clinicians.<br />
Process <strong>of</strong> diagnosis and prescribing pattern in tertiary care<br />
teaching hospital is a complex process. Heavy patient load,<br />
huge number <strong>of</strong> pharmaceutical formulations with irrational<br />
combinations, non-availability <strong>of</strong> evidenced-based treatment<br />
guidelines, and pressures from the pharmaceutical companies<br />
are certain factors that influences the drug prescribing<br />
practices <strong>of</strong> clinicians in tertiary care teaching hospital. This<br />
may <strong>of</strong>ten lead to inappropriate prescribing.<br />
Jagadguru Shree Shivarathreeshwara (JSS) Hospital, Mysore<br />
is a multi specialty tertiary care teaching hospital. On an<br />
average <strong>of</strong> 500-600 patients are being treated in out-patient<br />
departments (OPD) <strong>of</strong> various specialties such as medicine,<br />
orthopedics, pediatrics, surgery, psychiatry, neurology,<br />
nephrology, urology, pulmonology, gynecology, dermatology<br />
on daily basis. Consultants, senior doctors, junior doctors and<br />
postgraduates treat the patients in these out-patient<br />
departments. Prescribing pattern may vary based on their<br />
position, qualification and experience. Thus, it is necessary to<br />
assess the prescribing practices <strong>of</strong> the clinicians at JSS<br />
Hospital. The present study is designed to analyze the drug<br />
usage pattern <strong>of</strong> clinicians using WHO prescribing indicators<br />
in selected out-patient departments <strong>of</strong> JSS Medical College<br />
Teaching Hospital, Mysore.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
45
Ramesh A- Evaluation <strong>of</strong> Prescribing Pattern <strong>of</strong> Clinicians in out-patient Departments <strong>of</strong> A South <strong>Indian</strong> Teaching Hospital<br />
METHODOLOGY<br />
This is an open labelled prospective study, conducted over a<br />
period <strong>of</strong> eight months. The Institutional ethical committee <strong>of</strong><br />
JSS College <strong>of</strong> <strong>Pharmacy</strong> approved the study and permission<br />
was also taken from the Medical Superintendent <strong>of</strong> JSS<br />
Medical College Teaching Hospital.<br />
Collection <strong>of</strong> data<br />
Medication records <strong>of</strong> patients visiting the out-patient clinics<br />
<strong>of</strong> Medicine, Paediatrics, Orthopaedics, and Surgery<br />
departments were reviewed on daily basis. Prescriptions were<br />
selected randomly (about 15-20 prescriptions per day) and<br />
reviewed for the purpose <strong>of</strong> the study. Therapeutic data like<br />
name <strong>of</strong> the drugs, dose, route, frequency, duration, total<br />
number <strong>of</strong> drugs per prescription, number <strong>of</strong> antibiotics and<br />
injections per prescription and average consultation time with<br />
each patient were collected and documented in a suitably<br />
designed documentation form.<br />
Analysis <strong>of</strong> collected data<br />
All the collected data was subjected for analysis using WHO<br />
prescribing indicators. From the collected data, the average<br />
numbers <strong>of</strong> drugs per prescription, the percentage <strong>of</strong> drugs<br />
prescribed from essential drug list (compared with WHO<br />
essential drug list), the percentage <strong>of</strong> encounters with<br />
antibiotics and injections prescribed and the average<br />
consultation time with each patient were assessed.<br />
RESULTS<br />
Data was collected over a period <strong>of</strong> 36 days in each out-patient<br />
department clinics <strong>of</strong> pediatrics, medicine, orthopedics and<br />
surgery. During the study period, 2122 patients visited and<br />
received 2,108 prescriptions from the selected OPD clinics.<br />
Fourteen patients did not receive any prescription. Details <strong>of</strong><br />
number <strong>of</strong> prescriptions reviewed from each department are<br />
presented in Table 1.<br />
Number <strong>of</strong> drugs prescribed<br />
In the present study, 492 (23%) prescriptions contain one<br />
drug, 794 (37%) prescriptions contain two drugs, 479 (23%)<br />
prescriptions contain three drugs, and 337 (16%)<br />
prescriptions contain four drugs. Details <strong>of</strong> the drugs<br />
prescribed in each department are presented in Table 2.<br />
Average number <strong>of</strong> drugs per prescription<br />
During the study period, a total <strong>of</strong> 4,895 drugs were<br />
prescribed in 2108 prescriptions. The average number <strong>of</strong><br />
drugs per prescription was found to be 2.32. Details <strong>of</strong><br />
average numbers <strong>of</strong> drugs per prescription are presented in<br />
Table 3.<br />
Number <strong>of</strong> drugs from WHO essential drug list<br />
Among 4,895 drugs prescribed, 3,686 (75%) drugs belong to<br />
WHO essential drug list. Number <strong>of</strong> drugs prescribed from<br />
WHO essential drug list was found to be high in medicine<br />
department (83%), followed by paediatrics department<br />
(80%), surgery department (70%), and least were found in<br />
orthopaedics department (65%). Details <strong>of</strong> drugs prescribed<br />
from WHO essential drug list is presented in Table 4.<br />
Table 1. Number <strong>of</strong> prescriptions reviewed from each department<br />
Department Number <strong>of</strong> prescriptions (%)<br />
Paediatrics 522 (25)<br />
Medicine 536 (25)<br />
Orthopaedics 540 (26)<br />
Surgery 510 (24)<br />
Total 2108 (100)<br />
Table 3: Details <strong>of</strong> average number <strong>of</strong> drugs per Prescription.<br />
Department<br />
Total No. <strong>of</strong><br />
drugs<br />
Total No. <strong>of</strong><br />
prescriptions<br />
Average No.<br />
<strong>of</strong> drugs per<br />
prescription<br />
Paediatrics 984 522 1.88<br />
Medicine 1657 536 3.09<br />
Orthopaedics 1122 540 2.07<br />
Surgery 1132 510 2.22<br />
Total 4895 2108 2.32<br />
Number<br />
<strong>of</strong> drugs<br />
Table 2: Number <strong>of</strong> drugs prescribed in each department<br />
No. <strong>of</strong> prescriptions in Departments<br />
Paediatrics Medicine Orthopaedics Surgery<br />
Total (%)<br />
1 231 044 146 071 492 (23)<br />
2 153 106 244 291 794 (37)<br />
3 105 149 112 113 479 (23)<br />
4 033 231 038 035 337 (16)<br />
5 000 006 000 000 006(00.28)<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
46
Ramesh A- Evaluation <strong>of</strong> Prescribing Pattern <strong>of</strong> Clinicians in out-patient Departments <strong>of</strong> A South <strong>Indian</strong> Teaching Hospital<br />
Table 4: Number <strong>of</strong> drugs from WHO essential drug list.<br />
Total number <strong>of</strong> Number <strong>of</strong> drugs<br />
Department<br />
drugs prescribed from WHO list (%)<br />
Paediatrics 984 788 (80)<br />
Medicine 1657 1382 (83)<br />
Orthopaedics 1122 724 (65)<br />
Surgery 1132 192 (70)<br />
Total 4895 3686 (75)<br />
Prescriptions with injections:<br />
Of the 2,108 prescriptions reviewed during the study period,<br />
110 prescriptions contained 134 injections. Among 134<br />
injections prescribed, majority injections [73% (n=98)]<br />
belong to analgesics (dicl<strong>of</strong>enac), followed by tetanus toxoid<br />
18% (n=24), triamcinolone 6% (n=8) and followed by<br />
vitamin-D injection 3% (n=4). Details <strong>of</strong> the injections<br />
prescribed in each department are presented in Table 5.<br />
Prescriptions with antibiotics<br />
Out <strong>of</strong> 2,108 prescriptions reviewed during the study period,<br />
478 (23%) prescriptions contained antibiotics. Among them,<br />
467 (98%) prescriptions contained one antibiotic, two<br />
antibiotics were found in four prescriptions and four<br />
antibiotics were found in seven prescriptions. Details <strong>of</strong> the<br />
prescriptions with antibiotics are presented in Table 6.<br />
Percentage <strong>of</strong> drugs prescribed by generic name<br />
Among 4895 drugs prescribed, only 244 (5%) drugs were<br />
prescribed by generic name. Prescriptions given by brand<br />
name may have risk <strong>of</strong> wrong drug dispensing, as many brand<br />
names sound similar and confusing. Pharmaceutical<br />
companies spend great percentage <strong>of</strong> amount for marketing<br />
the brands. If clinicians prescribe drugs by generic names,<br />
cost <strong>of</strong> the drugs may be reduced by 40 –60% and the patients<br />
may be economic benefited.<br />
Average consultation time per patient<br />
During the study period, 2,122 patients visited the OPD<br />
clinics <strong>of</strong> the selected departments. In the present study, the<br />
consultation time was found to be 6-10 minutes for majority<br />
<strong>of</strong> patients who visited the OPD clinics. Details <strong>of</strong><br />
consultation time per patient are presented in Table 7.<br />
DISCUSSION<br />
Prescriptions' containing one drug was more in paediatrics<br />
out-patient department compared to other out-patient<br />
departments. Because, many patients diagnosed in<br />
Table 5: Details <strong>of</strong> Injections prescribed from each department<br />
Drugs Route <strong>of</strong> Indication<br />
Number <strong>of</strong> patients<br />
Total (%)<br />
prescribed administration<br />
Pediatrics Medicine Orthopedics Surgery<br />
Dicl<strong>of</strong>enac IM Pain 00 22 56 20 98 (73)<br />
Tetanus- toxoid IM Injuries 00 04 08 12 24 (18)<br />
Triamcinolone Intradermal Keloid 00 00 00 08 08 (6)<br />
Vitamin-D IM Vitamin-D 04 00 00 00 04 (3)<br />
Deficiency<br />
Number <strong>of</strong><br />
Antibiotic<br />
Table 6: Details <strong>of</strong> the number <strong>of</strong> antibiotics prescribed from each department<br />
No. <strong>of</strong> patient in Department<br />
Paediatrics Medicine Orthopaedics Surgery<br />
Total (%)<br />
1 129 114 20 204 467(98)<br />
2 04 00 00 00 4(1)<br />
3 02 05 00 00 7(1)<br />
Consultation<br />
time (in min)<br />
Table 7: Average consultation time per patient<br />
Number <strong>of</strong> patients<br />
Paediatrics Medicine Orthopaedics Surgery<br />
Total (%)<br />
<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
47
Ramesh A- Evaluation <strong>of</strong> Prescribing Pattern <strong>of</strong> Clinicians in out-patient Departments <strong>of</strong> A South <strong>Indian</strong> Teaching Hospital<br />
paediatrics department were with upper respiratory tract<br />
infections and fever. Recommended treatment for fever is<br />
paracetamol. Upper respiratory tract infections may not<br />
require antibiotics; hence clinicians prescribed only cough<br />
syrup to manage the situation. Prescriptions containing two<br />
drugs were more from surgery outpatient department. This is<br />
mainly because; most frequent causes for patients to visit the<br />
surgery department OPD clinics were APD or gastritis. The<br />
present study results reveal that, clinicians prescribe one<br />
Proton pump inhibitor and one deworming agent in majority<br />
cases. Prescriptions containing three and four drugs were<br />
more from medicine out-patient department. This is because,<br />
patients visit the medicine OPD clinics are <strong>of</strong>ten with comorbid<br />
conditions such as hypertension with diabetes or APD<br />
or other cardiovascular problems. Thus clinicians used more<br />
drugs.<br />
In the present study, average number <strong>of</strong> drugs per prescription<br />
was found to be 2.32. This average may be considered as<br />
normal. In a study conducted in Manipal teaching hospital in<br />
Pokhara, Nepal to assess the prescribing pattern <strong>of</strong> the<br />
doctors, the average number <strong>of</strong> drugs prescribed per<br />
4<br />
prescription was reported as 2.15. In another study conducted<br />
in Singapore to assess the prescribing behavior <strong>of</strong> doctors in<br />
Alexandra Hospital, Singapore, the results <strong>of</strong> the study<br />
reveals that, average number <strong>of</strong> drugs per prescription was<br />
5<br />
reported as 2.6. Another hospital based study conducted in<br />
India to assess the prescription pattern by the doctors using<br />
defined daily dosage (DDD) concept also reported that<br />
6<br />
average number <strong>of</strong> drugs per prescription as 2.5. Other<br />
hospital based studies have reported figure <strong>of</strong> 3-5 drugs per<br />
7,8<br />
prescription. The findings <strong>of</strong> the present study are similar to<br />
the findings <strong>of</strong> the above studies. More number <strong>of</strong> drugs in a<br />
prescription may increase the risk for potential drug-drug<br />
9<br />
interactions and adverse drug reactions. As a result; patients<br />
may not get the best possible therapeutic benefit.<br />
WHO has defined essential drugs as those that satisfy the<br />
10<br />
health care needs <strong>of</strong> the majority <strong>of</strong> the population. As per<br />
the latest WHO essential drug list, 366 drugs are considered as<br />
essential drugs. Drugs listed in the essential drugs list are safe,<br />
efficacious and economical. Thus, WHO encourages<br />
clinicians to choose drugs from essential drug list (EDL). In<br />
the present study, the results reveal that 75% <strong>of</strong> drugs were<br />
chosen from essential drug list. This percentage is considered<br />
to be high when compared with the studies conducted in other<br />
places. In a similar study conducted in Madurai city, results<br />
report that number <strong>of</strong> prescribed drugs belongs to essential<br />
11<br />
drug list was 51%. In another study conducted in Pokhara,<br />
Nepal, in a tertiary care teaching hospital, number <strong>of</strong> drugs<br />
4<br />
used from the essential drug list was 40%. When compared to<br />
the findings <strong>of</strong> other studies, the findings <strong>of</strong> the present study<br />
suggest that, prescribers are more rational in the selection <strong>of</strong><br />
drugs.<br />
Among the injectables prescribed, dicl<strong>of</strong>enac was found to be<br />
high in orthopaedics department. This is mainly because<br />
patients visit orthopaedics department OPD clinics with<br />
complaints <strong>of</strong> bone and joint inflammation. Although<br />
dicl<strong>of</strong>enac is not listed in essential drug list, <strong>of</strong>ten it is<br />
frequently used to relieve inflammatory conditions because<br />
<strong>of</strong> its efficacy. Other injectable drugs which were used due to<br />
the situational demand.<br />
Infectious diseases are considered as major cause <strong>of</strong><br />
10<br />
morbidity and mortality in developing countries. In treating<br />
the infections, antibiotics are <strong>of</strong>ten misused. Studies in India<br />
and overseas also have shown great irrationality in antibiotic<br />
usage. In the present study, prescriptions given with<br />
antibiotics were 23% <strong>of</strong> the total prescriptions. Majority<br />
antibiotics were used in surgery followed by paediatrics<br />
department. Drug categories prescribed were penicillins,<br />
cephalosporins, flouroquinolones and macrolides. Among the<br />
cephalosporins prescribed, only cephalexin is present in the<br />
essential drug list. Where as cefuroxime, cefotaxim and<br />
cefpodoxime are not present in essential drug list. From the<br />
category <strong>of</strong> flouroquinolones, only cipr<strong>of</strong>loxacin is present in<br />
the essential drug list and lev<strong>of</strong>loxacin, <strong>of</strong>loxacin,<br />
norfloxacin are not recommended in essential drug list.<br />
Among the macrolides, azithromycin and erythromycin are<br />
present in essential drug list, where as roxithromycin is not<br />
listed in the essential drug list. The findings <strong>of</strong> the present<br />
study show that antibiotics are inappropriately used.<br />
Irrational use <strong>of</strong> antibiotics may develop microbial resistance<br />
to antibiotics. This further warrants using higher antibiotics,<br />
which may pose financial burden to the patients. In the present<br />
study, only one antibiotic was used for treating majority<br />
infections. Two and four antibiotics were used in case <strong>of</strong><br />
tuberculosis in paediatrics and adult population. In a study<br />
conducted in Kathmandu Medical University, pertaining to<br />
the antibiotic usage, the results revealed that number <strong>of</strong><br />
12<br />
antibiotics used in patients were 2-3 which is very high<br />
compared to the results <strong>of</strong> the present study.<br />
An appropriate diagnosis is an important component in the<br />
rational drug therapy. For correct diagnosis, clinicians should<br />
spend more time in evaluating the signs, symptoms and<br />
laboratory investigations. So more the consultation time<br />
better the chances <strong>of</strong> right diagnosis. In the present study, the<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 48
Ramesh A- Evaluation <strong>of</strong> Prescribing Pattern <strong>of</strong> Clinicians in out-patient Departments <strong>of</strong> A South <strong>Indian</strong> Teaching Hospital<br />
consultation time was found to be 6-10 minutes for majority<br />
<strong>of</strong> patients who visited the OPD clinics. This may be because<br />
<strong>of</strong> heavy patient load.<br />
CONCLUSION<br />
In conclusion, results <strong>of</strong> the study showed a considerable<br />
scope for improving the prescribing pattern <strong>of</strong> drugs in OPD<br />
clinics. Improvement can be observed, if prescribers are<br />
provided with feed back, continuing education on rational use<br />
<strong>of</strong> drugs and prescribing by generic names. Preparation and<br />
distribution <strong>of</strong> a hospital formulary may further strengthen the<br />
rational use <strong>of</strong> drugs.<br />
ACKNOWLEDGEMENTS<br />
The authors are sincerely thankful to JSS Mahavidyapeetha,<br />
Principal, JSS College <strong>of</strong> <strong>Pharmacy</strong>, Dr. G. Parthasarathi,<br />
Head and other staff <strong>of</strong> Dept. <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong>, and<br />
Physicians <strong>of</strong> JSS Medical College Teaching Hospital,<br />
Mysore.<br />
REFERENCES<br />
1. Francisco A, Edson P, Sergia M S, Leonardo G, Jose M,<br />
Luiza H P, et al. Analysis <strong>of</strong> medical prescriptions<br />
dispensed at health centers in Belo Horizonte, Minas<br />
Gerais, Brasil. Cadernos de Saude publica-Avaliacao de<br />
prescricoes medicas avidas 2003;1-13.<br />
th<br />
2. The 14 WHO Model List <strong>of</strong> Essential Medicines.<br />
Geneva, <strong>Mar</strong>ch 2005.<br />
3. Mahendra B, Anil Kumar, Shrinivas K. Study on the<br />
Prescribing and Dispensing <strong>Practice</strong>s <strong>of</strong> NSAID at<br />
Punjab University Health Centre. The <strong>Indian</strong> <strong>Journal</strong> <strong>of</strong><br />
Hospital <strong>Pharmacy</strong> 2006; XLIII(2):64-68.<br />
4. Ravishankar, Partha P, Shenoy N. Prescribing pattern in<br />
medical out-patients. Clinmed May 2002; 16:1-8.<br />
5. Yap K B, Chan K M. The prescribing pattern <strong>of</strong> hospital<br />
doctors. Singapore Med J 1998; 39(11):496-500.<br />
6. Srishyla MV, Krishnamurthy M, Nagarani MA, Clare<br />
SM, Andrade C, Venkataraman BV. Prescription audit in<br />
an <strong>Indian</strong> hospital setting using the DDD (Defined Daily<br />
Dose) concept. <strong>Indian</strong> J Pharmacol 1994; 26:23-28.<br />
7. Kumar H, Gupta U, Garg KC, Agarwal KK. A study <strong>of</strong><br />
trend <strong>of</strong> drug usage in a hospital unit. <strong>Indian</strong> J Pharmacol<br />
1986; 18:50-53.<br />
8. Sood B, Verma RK, Gulati PV. Diagnosis and treatment in<br />
a general hospital. The clinician 1984; 48:263-270.<br />
9. Neis SA, Spielberg SP. Principles <strong>of</strong> therapeutics In:<br />
Gilman GA, Hardman JG, Limbird LE, Molin<strong>of</strong>f PB,<br />
Ruddon PW, editors. The pharmacological basis <strong>of</strong><br />
therapeutics. McGraw-Hill, New York 1995: 43-62.<br />
10. Molly Thomas. Rational Drug use and the Essential Drug<br />
Concept. In G Parthasarathi, Karin Nyfort-Hansen, Milap<br />
C Nahata. A textbook <strong>of</strong> clinical pharmacy practice. First<br />
publication. Orient Longman Private Limited 2004; 72-<br />
83.<br />
11. George Kutty, Narmada Sambasivam, Nagarajan M. A<br />
study on prescribing pattern in Madurai city. <strong>Indian</strong><br />
<strong>Journal</strong> <strong>of</strong> Pharmacology 2002; 34: 361-362.<br />
12. Pallike N. Prescribing pattern <strong>of</strong> Antibiotics in pediatric<br />
hospital <strong>of</strong> Kathmandu Valley. Kathmandu University<br />
Medical <strong>Journal</strong> 2004; 2:6-12.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 49
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
Association <strong>of</strong> Pharmaceutical Teachers <strong>of</strong> India<br />
Impact <strong>of</strong> patient counseling on Knowledge, Attitude, <strong>Practice</strong> and Quality <strong>of</strong><br />
Life in patients with Type II Diabetes mellitus and Hypertension.<br />
*<br />
Praveena P , Usman S, Deepika B, Raghu Kumar V, Mohanta G P, Manna P K, Manavalan R.<br />
Department <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong>, Annamalai University, Annamalai Nagar, Chidambaram, Tamil Nadu, India.<br />
A B S T R A C T<br />
Submitted: 14/11/2010<br />
The aim <strong>of</strong> this study was to assess the impact <strong>of</strong> pharmacist provided patient counseling on treatment outcomes and quality <strong>of</strong> life in<br />
hypertensive and type II diabetes mellitus patients, improving their knowledge, attitude and practice. It was a randomized prospective controlled<br />
study. Patients selected were divided into control and test groups. Patients in the test group were counseled and given information about the<br />
management <strong>of</strong> the disease, whereas control group received the information only at the end <strong>of</strong> the study. The follow up was carried out over a<br />
period <strong>of</strong> six months in which the KAP and quality <strong>of</strong> life <strong>of</strong> the patients was assessed. The scores were evaluated and statistically analyzed. A<br />
comparative study was made between the pre counseling and post counseling scores <strong>of</strong> control and test groups. A total <strong>of</strong> 41 patients, 21 control<br />
and 20 test were included in the study. A statistically significant difference (p 0.001).The control group scores <strong>of</strong> both PCS and<br />
MCS were not significantly different even after counseling. A significant difference (p
Praveena P- Impact <strong>of</strong> patient counseling on Knowledge, Attitude, <strong>Practice</strong> and Quality <strong>of</strong> Life in patients with Diabetes mellitus Type II and Hypertension.<br />
It is well documented that safe and effective drug therapy<br />
occurs most frequently when patients are well informed about<br />
medications, their use and life style modifications necessary<br />
2<br />
for the management <strong>of</strong> disease. Hence KAP studies can be<br />
carried out to assess the patient's knowledge, attitude and<br />
practice towards disease. Patient counseling can be used as<br />
an aid to assess and improve it. The ultimate goal <strong>of</strong><br />
counseling is to provide information about Knowledge,<br />
Attitude and <strong>Practice</strong> (KAP) needed for disease management,<br />
3<br />
thereby enhancing therapeutic outcomes. The therapeutic<br />
outcomes indirectly reflects the Quality <strong>of</strong> Life (QoL) <strong>of</strong> the<br />
patients. This study was undertaken to assess the role <strong>of</strong><br />
patient counseling in self management <strong>of</strong> blood sugar and<br />
blood pressure levels by patients with coexisting diabetes and<br />
hypertension. This study was designed to increase the<br />
awareness among patients and other health care pr<strong>of</strong>essionals<br />
about the importance <strong>of</strong> patient counseling. This study should<br />
focus on the Knowledge, Attitude, <strong>Practice</strong> and quality <strong>of</strong> life<br />
in patients with both diabetes and hypertension to assess the<br />
impact <strong>of</strong> patient counseling.<br />
METHODS<br />
The study was prospective randomized study. It was<br />
conducted for a six months period i.e from November 2009 to<br />
April 2010, at Rajah Muthaiah Medical College Hospital<br />
(RMMCH), Annamalai University in Chidambaram, Tamil<br />
Nadu, India. This study was designed to assess KAP and QoL<br />
scores <strong>of</strong> patients with diabetes and hypertension. The study<br />
was approved by the institutional ethics committee.<br />
Patient enrollment:<br />
Patients with both diabetes type 2 and hypertension <strong>of</strong> either<br />
sex with age above 30 years <strong>of</strong> age with or without comorbidities<br />
, who consented to participate were enrolled in the<br />
study using the inclusion and exclusion criteria. The enrolled<br />
patients were divided into control and test groups.<br />
Baseline data was collected using patient data collection<br />
form. Baseline blood pressure , blood sugar levels were<br />
measured. KAP, QoL scores were obtained through patient<br />
counseling. The follow-up was carried out over a period <strong>of</strong> 2<br />
months. The control group patients were given basic<br />
information whereas the test group were given extensive<br />
counseling, and education about disease management. The<br />
control group was provided with detailed education after the<br />
study was completed.<br />
MATERIALS<br />
Relevant patient data needed for the study was obtained from<br />
1) Patient data collection form<br />
2) Patient's prescriptions<br />
3) Patient interview<br />
4) KAP questionnaire<br />
5) Short form- 12 ( SF-12)<br />
KAP questionnaire : This questionnaire was designed to<br />
assess the patient's knowledge about their disease and their<br />
attitude, practice in disease management. It contained 25<br />
questions <strong>of</strong> which 18 are knowledge questions and attitude,<br />
practice questions were 7.<br />
Short Form - 12: This quality <strong>of</strong> life questionnaire contains<br />
12 questions which measures Physical Component<br />
Summary(PCS), Mental Component Summary(MCS).<br />
Data analysis : In the analysis <strong>of</strong> KAP questionnaire for the<br />
knowledge questions, each question was scored as one (1) for<br />
a correct answer and as zero (0) for an incorrect answer. For<br />
the practice questions, adhering to the guidelines for disease<br />
management or instructions from the patient's health care<br />
provider merited a score <strong>of</strong> 1; nonadherence was given a score<br />
<strong>of</strong> 0. QoL was given a score from 0-100 for both PCS and<br />
MCS.Student's t test was used to analyze and compare the pre<br />
counseling and post counseling blood pressure levels and<br />
blood sugar levels and KAP, QoL scores. A p value less than<br />
0.001 was considered significant.<br />
RESULTS<br />
A total <strong>of</strong> 50 patients were enrolled in the study <strong>of</strong> which 41<br />
patients [control(21), test(20)] who completed al follow up<br />
visits were included in analysis. The other 9 patients withdrew<br />
from the study for unknown reasons. Out <strong>of</strong> 41 patients in the<br />
study 26(63.4%) were female and 15(36.5%) were male.<br />
There was no significant difference seen between the baseline<br />
values <strong>of</strong> the two groups with respect to education level and<br />
number <strong>of</strong> medications being used. The age distribution was<br />
as follows<br />
1. 30 to 40 years <strong>of</strong> age are 05 patients (12.1%)<br />
2. 41 to 50 years <strong>of</strong> age are 13 patients (31.7%)<br />
3. 51 to 60 years <strong>of</strong> age are 15 patients (36.5%)<br />
KAP study<br />
KAP questionnaire contains a total <strong>of</strong> 25 questions <strong>of</strong> which<br />
18 are knowledge questions and 7 are attitude/practice<br />
question.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 51
Praveena P- Impact <strong>of</strong> patient counseling on Knowledge, Attitude, <strong>Practice</strong> and Quality <strong>of</strong> Life in patients with Diabetes mellitus Type II and Hypertension.<br />
Comparison <strong>of</strong> KAP scores at baseline and final follow-up<br />
At baseline all patients had poor KAP scores. At the end <strong>of</strong> the<br />
study patients in the test group who received extensive<br />
counseling about disease management showed significant<br />
difference in their KAP scores when compared to baseline<br />
data (p0.01).(Table1 and 2), (Figure 1<br />
and 2).<br />
Comparison <strong>of</strong> pre-counseling and post-counseling QoL<br />
scores<br />
At baseline patients <strong>of</strong> both test and control groups showed<br />
poor quality <strong>of</strong> life. The post counseling PCS scores <strong>of</strong> final<br />
Table 1: Effect <strong>of</strong> Patient Counsling on Knowledge Outcomes<br />
Mean±SEM<br />
group Pre counseling Post counseling<br />
Control (21) 9.762±0.32 10.10±0.217<br />
Test (20) 8.7±0.317 11.95±0.5355<br />
*P value < 0.01 is significant as calculated by t- test.<br />
Fig. 1: Effect <strong>of</strong> Patient Counseling on knowledge outcomes<br />
follow-up showed significant difference from that <strong>of</strong> precounseling<br />
scores at baseline. No significant difference was<br />
found incase <strong>of</strong> control group. MCS scores were not<br />
significantly improved for both test and control groups.<br />
(Table 3 and 4), (Figure 3 and 4)<br />
Comparison <strong>of</strong> pre-counseling scores <strong>of</strong> Therapeutic<br />
outcomes with post-counseling scores at final follow-up<br />
A significant reduction in systolic and diastolic blood<br />
pressure and blood sugar levels was found at the final followup.<br />
(Table 5,6 and 7). The graphical representation <strong>of</strong><br />
significant difference <strong>of</strong> systolic blood pressure levels,<br />
diastolic blood pressure levels and blood sugar levels was<br />
Table 3: Effect <strong>of</strong> Patient Counseling on Physical Component<br />
Summary(pcs):<br />
Mean±SEM<br />
group Pre counseling Post counseling<br />
Control (21) 42.48±2.136 44.77±1.342<br />
Test (20) 44.19±1.342 49.71±.622<br />
Fig 3: Effect <strong>of</strong> Patient Counseling on Physical Component<br />
Summary(pcs):<br />
Table 2: Effect <strong>of</strong> Patient Counseling on Attitiude and <strong>Practice</strong> outcomes<br />
Mean±SEM<br />
group Pre counseling Post counseling<br />
Control (21) 3.571±0.2809 3.810±0.2026<br />
Test (20) 3.2±.22 5.1±.1433<br />
Fig. 2: Effect <strong>of</strong> Patient Counseling on Attitude and <strong>Practice</strong> outcomes<br />
Table 4: Effect <strong>of</strong> Patient Counseling on Mental Component<br />
Summary(mcs):<br />
Mean±SEM<br />
group Pre counseling Post counseling<br />
Control (21) 46.68±1.125 46.33±0.910<br />
Test (20) 47.78±1.761 48.55±1.168<br />
Fig. 4: Effect <strong>of</strong> Patient Counseling on Mental Component<br />
Summary(mcs):<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
52
Praveena P- Impact <strong>of</strong> patient counseling on Knowledge, Attitude, <strong>Practice</strong> and Quality <strong>of</strong> Life in patients with Diabetes mellitus Type II and Hypertension.<br />
Table 5: Effect <strong>of</strong> Patient Counseling on Blood<br />
Pressure Levels(systolic):<br />
Mean±SEM<br />
group Pre counseling Post counseling<br />
Control (21) 139.3±1.629 138.6±1.73<br />
Test (20) 131.3±2.483 125.8±1.324<br />
Fig 5: Effect <strong>of</strong> Patient Counseling on Blood<br />
Pressure Levels(systolic):<br />
Table 7: Effect <strong>of</strong> Patient Counseling on Blood Sugar Levels<br />
Mean±SEM<br />
group Pre counseling Post counseling<br />
Control (21) 130.6±7.144 128.3±5.5733<br />
Test (20) 131.4±8.144 116.0±.765<br />
Fig 7: Effect <strong>of</strong> Patient Counseling on Blood Sugar Levels<br />
Table 6: Effect <strong>of</strong> Patient Counselingon Blood Pressure<br />
Levels (diastolic):<br />
Mean±SEM<br />
group Pre counseling Post counseling<br />
Control (21) 90.24±1.707 88.33±1.260<br />
Test (20) 90.00±1.308 84.75±1.056<br />
Fig. 6: Effect <strong>of</strong> Patient Counselingon Blood Pressure<br />
Levels (diastolic):<br />
with hypertension understanding <strong>of</strong> their disease, drug<br />
therapy, and lifestyle changes i.e disease management (blood<br />
sugar and blood pressure levels) and quality <strong>of</strong> life.<br />
Knowledge, Attitude and <strong>Practice</strong><br />
Subish Palaian, Leelavathy D Acharya et al. , evaluated the<br />
results <strong>of</strong> counseling in selected diabetic patients about their<br />
knowledge, attitude and practice and concluded that patient<br />
counseling by a clinical pharmacist improved knowledge<br />
scores, but this improved knowledge did not lead to<br />
4<br />
appropriate attitudes or practice. In this study at baseline all<br />
patients had poor knowledge, attitude and practice towards<br />
their disease. At the end <strong>of</strong> the study patients in the test group<br />
who received extensive counseling about disease<br />
management showed significant difference in their KAP<br />
scores when compared to baseline data.<br />
Quality <strong>of</strong> life (QOL)<br />
shown (Figure 5,6 and 7).<br />
DISCUSSION<br />
The management <strong>of</strong> hypertension and diabetes requires longterm<br />
treatment which may cause side effects that impair<br />
quality <strong>of</strong> life and lead to problems with medication<br />
adherence. Studies have shown that when community<br />
pharmacists were involved in the care <strong>of</strong> these patients,<br />
significant improvements in Knowledge, Attitude, practice,<br />
Quality <strong>of</strong> Life, blood pressure levels and blood sugar levels<br />
<strong>of</strong> patients were achieved. Our study evaluated the impact <strong>of</strong><br />
pharmacist-provided counseling in terms <strong>of</strong> diabetic patients<br />
The quality <strong>of</strong> life in diabetic patients with hypertension was<br />
assessed using Short Form-12 (SF-12) where the Physical<br />
Component Summary (PCS) and Mental Component<br />
Summary(MCS) were assessed separately. The mean PCS<br />
scores before counseling and after counseling for test group<br />
were found to be significantly different when compared to<br />
control group which are not significant. No significant<br />
difference was observed between the mean MCS scores <strong>of</strong> pre<br />
counseling and post counseling test and control groups. From<br />
this statistical analysis it was found that patient counseling<br />
had improved quality <strong>of</strong> life with respect to Physical<br />
component Summary. The MCS was not affected by patient<br />
counseling.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 53
Praveena P- Impact <strong>of</strong> patient counseling on Knowledge, Attitude, <strong>Practice</strong> and Quality <strong>of</strong> Life in patients with Diabetes mellitus Type II and Hypertension.<br />
Blood Pressure and Blood sugar levels<br />
Mean scores <strong>of</strong> systolic, diastolic blood pressure and blood<br />
sugar levels before counseling and after counseling for test<br />
groups were found to be significantly different.(p< 0.001).<br />
Mean scores <strong>of</strong> systolic, diastolic blood pressure and blood<br />
sugar levels before counseling and after counseling for<br />
control group were not significantly different.(p>0.001). This<br />
implies that the improvement in knowledge, attitude and<br />
practice decreased the blood pressure and blood glucose<br />
levels which ultimately improved quality <strong>of</strong> life (PCS).<br />
LIMITATIONS<br />
Our study has limitations with respect to attitude and practice<br />
scores as these were assessed based on patient interview<br />
instead <strong>of</strong> observing the patient's actual practice for disease<br />
management. Our sample size is small and confounding<br />
factors like patient counseling and knowledge attained by<br />
other sources was not considered.<br />
CONCLUSION<br />
Health related quality <strong>of</strong> life is increasingly viewed as a<br />
therapeutic outcome and is gradually gaining the same level<br />
<strong>of</strong> importance as clinical or physiological outcome<br />
parameters. (eg: blood pressure, blood sugar levels) this study<br />
aimed to assess impact <strong>of</strong> pharmacist provided patient<br />
education on treatment out comes, KAP& QOL <strong>of</strong> patients<br />
with coexisting diabetes and hypertension.<br />
At base line all patients had poor knowledge and attitude<br />
towards their disease and thus poor QOL (PCS, MCS). At the<br />
end <strong>of</strong> the study patients <strong>of</strong> test group received extensive<br />
counseling regarding their disease and its management<br />
showed greater improvement in treatment outcomes (blood<br />
pressure & blood sugar levels), KAP& QOL than in patients<br />
in control group.<br />
Our study confirms that improvement in knowledge <strong>of</strong> the<br />
disease and its management had positive impact on treatment<br />
outcomes and quality <strong>of</strong> life (PCS). At the same time it is<br />
noticed that counseling had no effect on mental component<br />
summary <strong>of</strong> the patient's quality <strong>of</strong> life. This study thus<br />
emphasis the impact <strong>of</strong> pharmacist provided patient<br />
counseling on KAP & QOL in patients with diabetes mellitus<br />
type-II and hypertension.<br />
REFERENCES<br />
1. Hsueh W A, Anderson P W. Hypertension, the endothelial<br />
cell, and the vascular complications <strong>of</strong> diabetes mellitus.<br />
Hypertension 1999; (20) :253-263.<br />
2. Parthasarathi G, Karin Nyfort-Hansen, Milap c Nahata. A<br />
Textbook <strong>of</strong> Clinical <strong>Practice</strong> <strong>Pharmacy</strong>: Essential<br />
th<br />
concepts and skills. 4 edition. 2007:43 -53.<br />
3. Roger and Walker. Clinical <strong>Pharmacy</strong> and Therapeutics.<br />
th<br />
4 edition. 2005; 265-275,629-650.<br />
4. Subhish P, Leelavathy D A, Padma Guru M, Ravi Shankar<br />
P, Nidin Mohan N, Nibu P N. Knowledge, Attitude and<br />
practice outcomes: Evaluating the impact <strong>of</strong> counseling<br />
in hospitalized diabetic patients in India, <strong>Journal</strong> <strong>of</strong><br />
Pharmacotherapy, 2006, 31(7): 381-396.<br />
5. Viral N S, Kamdar P K. Assessing the knowledge,<br />
attitudes and practice <strong>of</strong> type 2 diabetes among patients <strong>of</strong><br />
Saurashtra region, Gujarat. International <strong>Journal</strong> <strong>of</strong><br />
Diabetes in Developing Countries 2009; 29(3): 118-122.<br />
6. Weinberger M, Kirkman M. The relationship between<br />
glycemic control and health-related quality <strong>of</strong> life in<br />
patients with non-insulin-dependent diabetes mellitus.<br />
Med Care 1994;32:1173–1181<br />
7. Kapur A, Shishoo S, Ahuja MMS. Diabetes care in India:<br />
Physicians perceptions attitudes and practices (DIAPP-2<br />
study). Int J Diabetes Dev Countries 1998;18:124–130.<br />
8. Line A, Bovette P. KAP on hypertension in a country in<br />
epidemiological transition. Hypertension 1998; 31:1136-<br />
1145.<br />
9. Rubin RR, Peyrot M. Quality <strong>of</strong> life and diabetes.<br />
Diabetes Metab Res Rev 1999; 15(3):205-218.<br />
10. Bardage C. Hypertension and health-related quality <strong>of</strong><br />
life an epidemiological study in Sweden. <strong>Journal</strong> <strong>of</strong><br />
Clinical Epidemiology 2002; 54( 2): 172-181.<br />
11. Heather P W, Joli D F, Kelly R, Elinor C C. Assessment <strong>of</strong><br />
patient knowledge <strong>of</strong> diabetic goals, self-reported<br />
medication adherence, and goal attainment. <strong>Pharmacy</strong><br />
practic, 2006; 4(4): 183-190.<br />
12. Amanda H, William W. Health related quality <strong>of</strong> life and<br />
treatment compliance with diabetes care. Disease<br />
management 2006, 9(4), 195-200.<br />
13. Ramesh A, Rasheed A, Nagavi B G. Effect <strong>of</strong> patient<br />
counseling on quality <strong>of</strong> life in type-2 diabetes mellitus<br />
patients in two selected South <strong>Indian</strong> community<br />
pharmacies: A study. <strong>Indian</strong> J Pharm Sci 2007; 69: 519-<br />
24.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 54
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
Association <strong>of</strong> Pharmaceutical Teachers <strong>of</strong> India<br />
Influience <strong>of</strong> pharmacist provided education on Quality <strong>of</strong> Life in patients with<br />
HIV/AIDS-a study<br />
1 2 3 4 1<br />
Ramesh A* , Dinesh K , Nagavi B G , Mothi S N , Parthasarathy G<br />
1<br />
Department <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong>, JSS College <strong>of</strong> <strong>Pharmacy</strong>, SS Nagara, Mysore – 570 015<br />
2<br />
Manager, Bangalore. ,<br />
3<br />
Dean, RAK Medical & Health Sciences, Dubai.<br />
4<br />
Chairman, Asha Kirana, Center for AIDS Care and Research, Mysore, India.<br />
A B S T R A C T<br />
Submitted: 30/11/2010<br />
Accepted: 4/1/<strong>2011</strong><br />
An open labeled cross sectional study was conducted to assess the influence <strong>of</strong> patient counseling on Quality <strong>of</strong> Life (QoL) in patients living with<br />
HIV/AIDS (PLWA). Patients meeting the eligibility criteria were enrolled in to the study. Knowledge, attitude and practices (KAP) <strong>of</strong> the patients<br />
towards the disease management was analysed by using a suitably designed and validated KAP questionnaire at base line and at final follow up<br />
for all the patients. Structured counseling was provided to patients regarding the disease, drugs and life style modifications. Validated and<br />
Kannada translated WHO-QoL questionnaire was administered to assess the influence <strong>of</strong> education on health related quality <strong>of</strong> life (HRQoL) on<br />
all the enrolled patients. Paired't' test was used to assess the changes in QoL scores from baseline to final follow up. Sixty four patients<br />
completed all follow ups <strong>of</strong> the study. Demographic parameters like employment, income, education and absence <strong>of</strong> symptoms showed<br />
significant influence on QoL. Patients, who were on symptomatic treatment, showed significant improvement only in psychological (p
Ramesh A- Influience <strong>of</strong> pharmacist provided education on Quality <strong>of</strong> Life in patients with HIV/AIDS-a study<br />
6<br />
with HIV. Unlike developed nations where Anti-Retroviral<br />
Treatment (ART) is the management standard, in developing<br />
nations counseling and treatment <strong>of</strong> opportunistic infections<br />
(OIs) are the strategies <strong>of</strong> disease management. This strategy<br />
is neither resource intensive nor requires extensive use <strong>of</strong><br />
7<br />
technology.<br />
Objective <strong>of</strong> this prospective study was to assess the impact <strong>of</strong><br />
education / counseling on knowledge, attitude and practice<br />
(KAP) and QoL in patients living with HIV<br />
MATERIALS AND METHODS<br />
The present study was a prospective cross sectional<br />
observational study conducted at a South <strong>Indian</strong> NGO centre<br />
for AIDS care and research over a period <strong>of</strong> nine months.<br />
Patients meeting the inclusion criteria were enrolled in to the<br />
study after obtaining the written informed consent.<br />
Institutional ethical committee has approved the study.<br />
Study pharmacist received the suitable education and training<br />
from the AIDS counselors before initiating the project. The<br />
demographic, clinical, lab and medication information <strong>of</strong> the<br />
enrolled patients was documented in a suitably designed<br />
patient pr<strong>of</strong>ile form and the information was kept<br />
confidential. Enrolled patients were classified as<br />
asymptomatic and symptomatic according to the WHO<br />
staging. Validated Kannada version <strong>of</strong> Knowledge, Attitudes<br />
and <strong>Practice</strong>s (KAP) questionnaire containing questions<br />
regarding HIV infection, mode <strong>of</strong> transmission, prevention,<br />
treatment/cure, life style modifications and myths and<br />
misconception about the disease was administered at baseline<br />
and final follow up to assess the patients' knowledge,<br />
perception and management <strong>of</strong> the disease.<br />
Kannada translated and validated WHO Health related QoL<br />
8<br />
questionnaire brief version (WHO – QoL BREF) containing<br />
26 items covering four domains such as physical,<br />
psychological, social, and environmental domains was<br />
st nd<br />
administered at base line, 1 ,2 , and final follow ups. Scores<br />
in each domain range from 4 - 20, and higher scores reflected<br />
the better QoL.<br />
The study pharmacist provided the education to the enrolled<br />
patients about their infection, medications, nutrition and life<br />
style modifications complimented with suitably designed<br />
information leaflets. Patients were also counseled about the<br />
difference between being HIV positive and having AIDS,<br />
prevention and management <strong>of</strong> opportunistic infections.<br />
Psychological counseling was also provided to reduce the<br />
stressors associated with HIV disease to the patients and also<br />
to their care givers.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
Paired t-test and correlation coefficient were used to assess<br />
the statistical significance <strong>of</strong> the results.<br />
RESULTS AND DISCUSSION<br />
A total <strong>of</strong> 98 patients satisfying the inclusion criteria were<br />
enrolled in to the study. Among them 64 (65%) patients<br />
completed all the follow ups and the remaining 34 (35%)<br />
patients were considered as dropouts due to personal and<br />
health reasons. Demographic details, disease history,<br />
medication history <strong>of</strong> the study patients were presented in<br />
Table.1.<br />
Age (Year), Mean<br />
18-30<br />
31-45<br />
>45<br />
Sex<br />
Male<br />
Female<br />
<strong>Mar</strong>ital status<br />
<strong>Mar</strong>ried<br />
Unmarried<br />
HIV risk factor<br />
Sex<br />
Blood and needles<br />
Others<br />
Educational Level<br />
Illiterates<br />
Primary/high school<br />
SSLC<br />
Pre-university<br />
Degree<br />
Employment<br />
Employed<br />
Unemployed / Housewives<br />
Income/Month (Rs)<br />
10,000<br />
Patients on ART<br />
Disease Stage<br />
Asymptomatic<br />
Symptomatic<br />
Table 1: Demographic details <strong>of</strong> the study subjects<br />
35 (56%)<br />
22 (34%)<br />
7 (10%)<br />
41 (64%)<br />
23 (36%)<br />
50 (78%)<br />
14 (22%)<br />
57 (86%)<br />
5 (11%)<br />
2 (3%)<br />
20 (31%)<br />
11 (19%)<br />
17 (25%)<br />
5 (10%)<br />
11 (15%)<br />
42(65 %)<br />
22 (35%)<br />
--<br />
50 (78%)<br />
8 (12%)<br />
6 (10%)<br />
10 (15%)<br />
29 (40%)<br />
35 (60%)<br />
Influence <strong>of</strong> education on improvement <strong>of</strong> scores <strong>of</strong> the<br />
knowledge, attitude and practices (KAP) was presented in<br />
Figure. 1<br />
The WHO - QOL BREF Questionnaire was used to assess the<br />
quality <strong>of</strong> life in HIV infected patients. The scores <strong>of</strong> all the<br />
domains i. e. physical health, psychological domain, social<br />
56
Ramesh A- Influience <strong>of</strong> pharmacist provided education on Quality <strong>of</strong> Life in patients with HIV/AIDS-a study<br />
Fig.1.Pre and Post counseling Knowledge, Attitude<br />
and <strong>Practice</strong>s (KAP) scores<br />
Fig.2: Comparison <strong>of</strong> change in QoL scores from<br />
Base Line to Final Follow up<br />
KAP Questions<br />
1. HIV infection spreads by unprotected sex, blood transfusion, sharps<br />
and needles.<br />
2. Symptoms <strong>of</strong> HIV/AIDS include weight loss, persistent fever, diarrhea,<br />
cough and opportunistic infections<br />
3. The disease will be cured if the symptoms <strong>of</strong> the infection are cured.<br />
4. Other infections may occur if the disease is not treated with suitable anti<br />
retroviral drugs.<br />
5. Shaking hands, sharing the food and clothes with HIV patients may<br />
transmit the infection.<br />
6. Patients with HIV/AIDS can do their routine job.<br />
7. HIV patients can have sex with their partners using condoms.<br />
8. Counseling to relatives and friends <strong>of</strong> HIV patients may motivate them to<br />
support the HIV patients<br />
9. Regular follow up with the doctor and taking antiretrovirals agents may<br />
keep the infection in control.<br />
10. Hygienic practices, nutritious diet, rest and medication adherence will<br />
improve the health condition<br />
relationship and environmental domain were calculated.<br />
Higher scores indicated better quality <strong>of</strong> life.<br />
QoL scores <strong>of</strong> patients with symptomatic treatment in various<br />
follow ups are given in Table.2 and the QoL scores <strong>of</strong> patients<br />
receiving ART in various follow ups are given in Table.3. The<br />
overall QoL scores <strong>of</strong> the enrolled patients are given in<br />
Figure.2.<br />
QOL is a dynamic continuum, relating to many aspects <strong>of</strong><br />
one's life. Social relationships, financial situations, workrelated<br />
issues, physical limitations, and intellectual<br />
challenges all play a role in determining QOL and satisfaction<br />
within the health care setting. Self-perception <strong>of</strong> how these<br />
factors negatively or positively influence one's QOL also<br />
9,10<br />
exerts a strong influence.<br />
Quality <strong>of</strong> life outcomes are important in persons with HIV<br />
because <strong>of</strong> prolonged physical and psychosocial<br />
consequences <strong>of</strong> the disease. The stress and loss associated<br />
with HIV/AIDS is pr<strong>of</strong>ound and <strong>of</strong>ten compounded by<br />
societal stigma. Persons with HIV/AIDS face many problems<br />
in day-to-day living and their ability to cope influences their<br />
quality <strong>of</strong> life and the disease progression. Monitoring and<br />
enhancing quality <strong>of</strong> life during the disease trajectory<br />
becomes more important than following the disease and<br />
providing symptomatic relief. This study was conducted to<br />
identify common quality <strong>of</strong> life domains affected due to HIV<br />
infection and strategies to improve better quality <strong>of</strong> life as the<br />
disease is chronic with poor prognosis.<br />
Table. 2. Change in QoL Scores in Different Domains at Baseline and each Follow up in Patients<br />
Recieving Antiretroviral Therapy<br />
DOMAINS Baseline Follow Up-1 Follow Up-2<br />
Physical health<br />
Psychological<br />
domain<br />
Social<br />
relationship<br />
Environmental<br />
domain<br />
10.56<br />
10.00<br />
11.00<br />
13.56<br />
10.78 (p>0.05)<br />
11.22 ( p=0.002 )<br />
12.00 ( p=0.002 )<br />
13.67 (p>0.05)<br />
11.44 (p=0.009)<br />
(p=0.04)<br />
11.44 ( p0.05)<br />
12.22 ( p0.05)<br />
13.22 (p>0.05)<br />
(p>0.05)<br />
Follow Up-3<br />
13.56 (p=0.007)<br />
(p=0.02)<br />
(p>0.05)<br />
13.67 ( p0.05)<br />
(p>0.05)<br />
13.22 ( p0.05)<br />
13.22 (p>0.05)<br />
(p>0.05)<br />
(p>0.05)<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
57
Ramesh A- Influience <strong>of</strong> pharmacist provided education on Quality <strong>of</strong> Life in patients with HIV/AIDS-a study<br />
Table 3: Change <strong>of</strong> QoL scores in various follow ups in patients receiving symptomatic treatment<br />
DOMAINS Baseline Follow Up-1 Follow Up-2 Follow Up-3<br />
Physical health<br />
Psychological<br />
domain<br />
Social<br />
relationship<br />
Environmental<br />
domain<br />
10.18<br />
9.64<br />
10.24<br />
12.01<br />
9.90 (p>0.05)<br />
10.54 ( p=0.001 )<br />
11.12 ( p=0.001 )<br />
12.35 (p>0.05)<br />
10.07 (p>0.05)<br />
(p>0.05)<br />
11.28( p0.05)<br />
11.75 ( p0.05)<br />
11.26 (p>0.05)<br />
(p>0.05)<br />
10.01 (p>0.05)<br />
(p>0.05)<br />
(p>0.05)<br />
11.36 ( p0.05)<br />
(p>0.05)<br />
11.72 ( p0.05)<br />
(p>0.05)<br />
11.35 (p>0.05)<br />
(p>0.05)<br />
(p>0.05)<br />
During the course <strong>of</strong> the study, 35% <strong>of</strong> the enrolled patients<br />
dropped out from the study due to fear <strong>of</strong> their serostatus<br />
disclosure, dissatisfaction with medical services, absence <strong>of</strong><br />
symptoms, financial problems and transportation difficulties.<br />
Majority study subjects were male and married and in many<br />
cases both partners got infected. In most <strong>of</strong> the cases, the<br />
source <strong>of</strong> infection was through sexual route attributing to the<br />
fact that the safe sexual practices are poor in our population.<br />
The educational background <strong>of</strong> the study subjects ranges from<br />
illiterates to university graduates. This indicates that<br />
HIV/AIDS is not a disease that confines to a particular<br />
segment <strong>of</strong> the society. Half <strong>of</strong> the study population has<br />
income less than Rs. 3000 per month and was found as a major<br />
barrier for poor affordability to antiretroviral therapy.<br />
Knowledge and awareness regarding the disease plays an<br />
important role in the patient's practices towards the<br />
management <strong>of</strong> the disease. A validated KAP questionnaire<br />
was administered at base line and final follow up to assess the<br />
influence <strong>of</strong> the patient counseling. At base line, the subjects'<br />
knowledge was good with respect to transmission, risk<br />
factors, however many <strong>of</strong> the respondents were having poor<br />
knowledge regarding symptoms, treatment, prognosis <strong>of</strong> the<br />
disease, and lifestyle modifications. A significant<br />
improvement was observed in the overall KAP scores at the<br />
final follow up suggesting the influence <strong>of</strong> education. Many<br />
studies have corroborated the influence <strong>of</strong> counseling on<br />
2,3<br />
knowledge and therapeutic outcomes.<br />
Many patients believe that HIV could be transmitted through<br />
mosquito bite, sharing food, clothes and other utility items.<br />
This is mainly due to myths and misconceptions prevailing in<br />
our society. During the counseling these myths can be<br />
removed. Many patients were unaware regarding the<br />
prognosis <strong>of</strong> the disease due to lack <strong>of</strong> information. Structured<br />
patient education <strong>of</strong>fers moral support addresses certain<br />
issues like ART usage, lifestyle modifications, safe sex<br />
10,11<br />
practices.<br />
Validated WHO-QoL brief version, a quality <strong>of</strong> life<br />
instrument administered on study population at base line and<br />
all the subsequent follow ups. WHO-QOL brief version is a<br />
generic questionnaire and has been extensively applied on<br />
people with medical illness including HIV, and shown to be<br />
reliable and valid. This questionnaire measures the QoL<br />
mainly on four domains. These domains are physical health,<br />
psychological, social relationship and environmental domain.<br />
Previous studies have shown that physical, psychological and<br />
social functions were impaired in people living with<br />
12,13<br />
HIV/AIDS. This was the reason for selecting WHO-QoL<br />
questionnaire for our study in order to target these domains in<br />
assessing quality <strong>of</strong> life.<br />
In the present study, patients receiving symptomatic<br />
treatment reported to score low QoL scores compared to the<br />
patients on ART. This may be due to inadequate medical care.<br />
In patients on ART, it was observed that the scores in<br />
psychological and social relationship domain were decreased.<br />
This poor score may be due to social stigma and social<br />
isolation by the friends and relatives. In order to overcome<br />
this problem, counseling to their relatives and friends may<br />
14<br />
improve the acceptance <strong>of</strong> the patient by the society.<br />
The quality <strong>of</strong> life scores at baseline were correlated with<br />
socio demographics and illness related variables. The lack <strong>of</strong><br />
significant association between QoL scores and variables<br />
such as age, gender, and source <strong>of</strong> infection is consistent with<br />
2<br />
previous findings. Some studies have also found that women<br />
15<br />
reported lower levels <strong>of</strong> QoL compared to men. But this<br />
trend was not observed in our study population. The variable<br />
<strong>of</strong> age shown an influence on QoL scores as the age advances<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
58
Ramesh A- Influience <strong>of</strong> pharmacist provided education on Quality <strong>of</strong> Life in patients with HIV/AIDS-a study<br />
the physical deterioration <strong>of</strong> the organs will influence the<br />
physical domain. Nevertheless we did not find this trend in<br />
our study and our findings are consistent with other many<br />
11<br />
studies, which found no relationship between QoL and age.<br />
A significant association <strong>of</strong> QoL scores and marital status was<br />
observed in our study. This may be due to the fact that,<br />
married persons may have greater resource constraints and<br />
more numbers <strong>of</strong> people being infected (spouse and / or<br />
16<br />
children) which will further hamper the quality <strong>of</strong> life. In the<br />
present study a non significant association was observed<br />
between the employment and QoL. Many studies have shown<br />
that the association between QoL and work status is primarily<br />
related to physical health rather than dimensions <strong>of</strong> well<br />
being.<br />
The most significant finding <strong>of</strong> our study is the strong<br />
association between stage <strong>of</strong> infection (symptomatic or<br />
asymptomatic) and QoL, highlighting the relationship<br />
between the QoL and number, frequency and severity <strong>of</strong> HIV<br />
related symptoms. Higher education and higher income level<br />
were associated with better quality <strong>of</strong> life because these<br />
patients scored higher on environmental domains than their<br />
counterparts with low education and low-income group.<br />
The psychological domain assesses the patients' mental<br />
health that includes bodily image, negative feeling, positive<br />
feeling, self-esteem, spirituality/personal beliefs, thinking,<br />
learning, memory and concentration. At base line the scores<br />
were disrupted due to the stress associated with HIV disease.<br />
Improvements in most items were observed in subsequent<br />
follow-ups. This improvement was observed due to<br />
behavioural interventions in the form <strong>of</strong> counseling and<br />
psychological support. The impact <strong>of</strong> behavioural<br />
interventions to assist patients in dealing with the stress <strong>of</strong> the<br />
17<br />
disease has been well documented in the literature.<br />
Moreover, many studies were observed that in stressful life<br />
events, psychological counseling improves the adverse<br />
15<br />
effects <strong>of</strong> stressors.<br />
The social relationship domain comprises the assessment <strong>of</strong><br />
social support, personal relationship and sexual activity. The<br />
scores at base line on all items were adversely affected<br />
because <strong>of</strong> fear and stigma associated with the disease.<br />
Counseling the patient's spouse/husband, relatives and<br />
friends helped in improving the acceptance <strong>of</strong> patient. Social<br />
acceptance improved the QoL scores in subsequent follow<br />
1<br />
ups. Murdaugh C et.al described that social support is the<br />
major factor in improving quality <strong>of</strong> life in HIV infection. The<br />
major components <strong>of</strong> social support are emotional and<br />
2<br />
informational support. Susan S et.al showed that satisfaction<br />
with informational support will be a good predictor for better<br />
QoL.<br />
Physical health includes work capacity, energy/fatigue,<br />
mobility, pain, sleep, rest and dependence on medicines and<br />
medical aids. This domain was affected predominantly in<br />
symptomatic patients. Improvement was observed especially<br />
in patients receiving antiretroviral therapy, but this<br />
improvement was not seen in patients who were on treatment<br />
for opportunistic infections. Many studies have shown the<br />
improvement <strong>of</strong> HIV related constitutional symptoms in<br />
7<br />
patients receiving antiretroviral therapy.<br />
Environmental domain includes the assessment <strong>of</strong><br />
satisfaction <strong>of</strong> the patients with education, financial status,<br />
medical facilities, home environment, transportation etc. At<br />
baseline environmental domain had better scores but later the<br />
scores were found declined may be due to dissatisfaction with<br />
medical facilities, poor cooperation from family members<br />
and inadequate transportation facilities to ART centers.<br />
Improvement in overall quality <strong>of</strong> life scores was not<br />
consistent with all the patients. Patients on antiretroviral<br />
treatment showed significant improvement in overall QoL<br />
compared to those receiving only symptomatic treatment for<br />
opportunistic infections. This lack <strong>of</strong> improvement in QoL<br />
may be attributed to decline in physical health and increase in<br />
18<br />
medical expenses due to frequent illness.<br />
This study concludes that structured education provided by<br />
the pharmacist to patients living with AIDS improved their<br />
awareness regarding the disease, coping with disease related<br />
challenges and in turn improved the overall quality <strong>of</strong> life<br />
scores showing a strong association <strong>of</strong> education with<br />
therapeutic outcomes and QoL.<br />
ACKNOWLEDGEMENTS<br />
Authors whole heartedly thank JSS University, Principal, JSS<br />
College <strong>of</strong> <strong>Pharmacy</strong>, all the counselors at Asha Kirana and all<br />
the patients who participated in the study.<br />
REFERENCES<br />
1. Murdaugh C. Health-related quality <strong>of</strong> life in HIV<br />
disease: Achieving a balance. J Asso Nurses in AIDS<br />
Care. 1998;9:59-71.<br />
2. Susan S, J Mohr, N Singh et al. Quality <strong>of</strong> life in patients<br />
with human immunodeficiency virus infection: impact<br />
<strong>of</strong> social support, coping style and hopelessness. Int. J<br />
STD AIDS. 1999;10:383-391.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
59
Ramesh A- Influience <strong>of</strong> pharmacist provided education on Quality <strong>of</strong> Life in patients with HIV/AIDS-a study<br />
3. Nunes JA. Raymond SJ. Nicholas PK et.al. Social<br />
support, Quality <strong>of</strong> life, Immune function, and Health in<br />
persons living with HIV. J Holis Nursing. 1995;13:174-<br />
198.<br />
4. Lubeck DP, Fries JF. Changes in quality <strong>of</strong> life among<br />
persons with HIV infection. Qual Life Res. 1992;1:359-<br />
66.<br />
5. Gaitunde V R. HIV disease in India: Treatment<br />
Guidelines. YRG Care. 2000; 51-57 and 71-77.<br />
6. Sandra A N. The role <strong>of</strong> Pharmacists in Caring for<br />
People Living with HIV/AIDS: A Canadian Position<br />
Paper. Canadian J Hosp Pharm 2000;53:92-103.<br />
7. Richard D, Gerber, William R, Lender king, et.al.<br />
Quality <strong>of</strong> life Evaluation Trial <strong>of</strong> Zidovudine Therapy<br />
in Patients with Mildly Symptomatic HIV Infection.<br />
Ann Intern Med 1992;116:961-966.<br />
8. World Health Organization. WHOQOL-BREF.<br />
Introduction, Administration, Scoring and Generic<br />
Version <strong>of</strong> the Assessment. Field Trial Version 1996<br />
Dec.<br />
9. Sousa KH, Holzemer WL, Henry SB et.al. Dimensions<br />
<strong>of</strong> health-related quality <strong>of</strong> life in persons living with<br />
HIV disease. J Advanced Nursing. 1999;29:178-87.<br />
10. Berra K. The Effect <strong>of</strong> Lifestyle Interventions on<br />
Quality <strong>of</strong> Life and Patient Satisfaction with Health and<br />
Health Care. J Cardio Nursing. 2003;18:319-325.<br />
11. Prabha S C. Psychological and sexual adjustment<br />
among persons living with HIV. MADHYAM. 2000;<br />
20-24.<br />
12. Bing EG, Hays RD, Jacobson LP et.al. Health-related<br />
quality <strong>of</strong> life among people with HIV disease: results<br />
from the Multicenter AIDS Cohort Study. Qual Life<br />
Res. 2000;9:55-63.<br />
13. Spirig R. Support groups for people living with<br />
HIV/AIDS: a review <strong>of</strong> literature. <strong>Journal</strong> <strong>of</strong> the<br />
Association <strong>of</strong> Nurses in AIDS Care. 1998;9:43-55.<br />
14. Sherbourne CD, Hays RD, Fleishman JA, et.al. Impact<br />
<strong>of</strong> psychiatric conditions on health-related quality <strong>of</strong><br />
life in persons with HIV infection. Am J<br />
Psychiatry.2000;157:248-54.<br />
15. Sowell RL, Seals BF, Moneyham L et.al. Quality <strong>of</strong> life<br />
in HIV-infected women in the south-eastern United<br />
States. AIDS Care. 1997; 9:501-12.<br />
16. Cunningham WE, Shapiro MF, Hays RD et.al.<br />
Constitutional symptoms and health-related quality <strong>of</strong><br />
life in patients with symptomatic HIV disease. Am J<br />
Med.1998; 104:129-36.<br />
17. Hays RD, Shapiro MF. An overview <strong>of</strong> generic healthrelated<br />
quality <strong>of</strong> life measures for HIV research. Qual<br />
Life Res. 1992; 1:91-7.<br />
18. Globe DR, Hays RD, Cunningham WE. Associations <strong>of</strong><br />
clinical parameters with health-related quality <strong>of</strong> life in<br />
hospitalized persons with HIV disease. AIDS Care.<br />
1999; 11:71-86.<br />
19. Franchi D, Wenzel RP. Measuring health-related<br />
quality <strong>of</strong> life among patients infected with Human<br />
Immunodeficiency virus. Clinical Infectious Diseases.<br />
1998; 26:20-6.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 60
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
Association <strong>of</strong> Pharmaceutical Teachers <strong>of</strong> India<br />
Drug use and dosing in patients with renal impairment<br />
Veera Raghavulu B*, Shravani K, PrabhakarReddy V, ManoharBabu S.<br />
St. Peter's Institute <strong>of</strong> Pharmaceutical Sciences, Vidyanagar, Hanumakonda, Warangal, Andhra Pradesh, India.<br />
Submitted: 30/11/2010<br />
Accepted: 4/1/<strong>2011</strong><br />
INTRODUCTION<br />
Chronic kidney disease is a worldwide public health problem<br />
with an increasing incidence and prevalence, poor outcomes,<br />
1<br />
and high costs. Current evidence suggests that some <strong>of</strong> these<br />
adverse outcomes can be prevented or delayed by early<br />
2<br />
detection and treatment. Many drugs and metabolites are<br />
eliminated through the kidney. Inappropriate use <strong>of</strong> drugs in<br />
patients with renal impairment (RI) may therefore be harmful<br />
3,4<br />
and have deleterious effects. The use <strong>of</strong> drugs in patients<br />
with reduced renal function can give rise to problems for<br />
5<br />
several reasons: reduced renal excretion <strong>of</strong> a drug or its<br />
metabolite may cause toxicity; sensitivity to some drugs and<br />
is increased even if elimination is unpaired; many side-effects<br />
are tolerated poorly by patients with renal impairment; some<br />
drugs are not effective when renal function is reduced; many<br />
<strong>of</strong> these problems can be avoided by reducing the dose or by<br />
6<br />
using alternative drugs. The aim <strong>of</strong> this study to know the<br />
drug use and dosing prescribed for patients with reduced renal<br />
function. The objective was to identify the use <strong>of</strong> renal risk<br />
drugs and frequency <strong>of</strong> drug-related problems in relation to<br />
risk rules in renal impairment, establishing the frequency <strong>of</strong><br />
inappropriate dosing at the time <strong>of</strong> discharge in accordance<br />
with renal function.<br />
METHODS<br />
All medication records <strong>of</strong> the renal impaired patients who had<br />
been discharged from general medicine department from the<br />
Rohini Multispeciality hospital through the discharge<br />
counseling service during the period <strong>of</strong> December 2009 to<br />
June 2010 were studied. A data collection form was specially<br />
prepared for this purpose. Renal function <strong>of</strong> each patient was<br />
estimated by calculating the estimated GFR based on the<br />
average <strong>of</strong> the last 2 serum creatinine levels during admission.<br />
Each drug in the prescription <strong>of</strong> each patient was analyzed<br />
critically whether it could be prescribed in patients with<br />
impaired renal functions. Dosage adjustments are usually<br />
Address for Correspondence:<br />
Veera Raghavulu. Bitra, St. Peter's Institute <strong>of</strong> Pharmaceutical Sciences, Vidyanagar,<br />
Hanumakonda, Warangal, Andhra Pradesh, India.<br />
E-mail: raghavab27@yahoo.com<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
7,8,9<br />
recommended when the GFR decreases to 50 ml/min.<br />
Therefore in all patients with an estimated GFR less than<br />
2<br />
51ml/min/1.73m , prescriptions at discharge were reviewed<br />
to identify the need for dosage adjustment related to renal<br />
function and for contraindications.<br />
Inclusion criteria:<br />
Renal impaired and renal transplanted patients (eGFR <<br />
2<br />
51ml/min/1.73m ) <strong>of</strong> both sex,<br />
Adults and children were included in this study.<br />
Exclusion criteria:<br />
2<br />
Patients who had eGFR > 50ml/min/1.73m<br />
Pregnant and lactating women.<br />
Classification <strong>of</strong> drug related problems (DRPs)<br />
DRPs were defined in accordance with the definition <strong>of</strong><br />
Pharmaceutical Care Network Europe: a drug related<br />
problem is an event or circumstance involving drug therapy<br />
that actually or potentially interferes with desired health<br />
10<br />
outcomes. The patient were assessed for DRPs <strong>of</strong> 12<br />
categories: need for an additional drug i.e. according to<br />
evidence-based guidelines, unnecessary drug, non-optimal<br />
drug, non-optimal dose, no further need <strong>of</strong> drug, drug<br />
interaction, need for monitoring, adverse drug reaction<br />
(ADR), medical chart error, compliance problems, therapy<br />
discussions and counselling to patients in need <strong>of</strong> drug<br />
10<br />
information. For the DRP drug interaction, only those<br />
regarded to be clinically important, were included.<br />
DATA SOURCE<br />
To assess the need for dosage adjustment, we referred to the<br />
following Drug prescribing in renal failure: dosing guidelines<br />
7<br />
for adults , Clinical Nephrotoxins: Renal Injury from Drugs<br />
8<br />
and Chemicals and Drug Dosing Adjustments in Patients<br />
with Chronic Kidney Disease. If guidelines differed among<br />
these references, either the lowest percentage <strong>of</strong> the usual<br />
dose or the maximum interval prolongation was applied.<br />
To evaluate the drug-drug interactions, we referred to the<br />
following handbooks:<br />
61
Veera Raghavulu B - Drug use and Dosing in Patients with Renal Impairment<br />
Stockley's Drug Interactions: a source book <strong>of</strong> interactions,<br />
11<br />
their mechanisms, clinical importance and management ,<br />
Drug Interaction Facts 2005. Facts and Comparisons:<br />
12<br />
A to Z Drug Facts and MED facts: Pocket guide <strong>of</strong> drug<br />
13<br />
interactions.<br />
STATISTICAL ANALYSIS<br />
The data were analyzed in SPSS 15.0 for Windows. To test for<br />
differences between patients with mild, moderate and severe<br />
renal impairment, one way ANOVA independent samples<br />
were used. P-values
Comparison <strong>of</strong> the three grades <strong>of</strong> RI with total number <strong>of</strong><br />
b<br />
drugs, renal risk drugs per patient, number <strong>of</strong> DRP per patient<br />
and other risk factors were made. Significant differences were<br />
found as shown in the table 2.<br />
Renal risk drugs<br />
A total <strong>of</strong> 1718 drugs were found to be prescribed for 215 RI<br />
patients. Of 1718 drugs, 551 were found to be renal risk<br />
drugs. Table 3 shows the category <strong>of</strong> renal risk drugs: 299<br />
(53%) drugs were those that required dosage adjustments,<br />
219 (40%) were drugs to be used with caution and 33 (6%)<br />
drugs which were to be avoided. Drugs recommended to be<br />
avoided were used by 9 patients in mild RI; 4 patients in<br />
moderate RI and 14 patients in severe RI.<br />
Risk rule for<br />
drugs in RI<br />
Dose Adjustment<br />
Reduce dose in mild to<br />
moderate RI<br />
Reduce dose in<br />
severe RI<br />
Start with small doses<br />
Caution<br />
Caution<br />
Caution, monitor serum<br />
concentration<br />
Increased cerebral<br />
sensitivity<br />
Avoid<br />
Avoid in mild to<br />
moderate RI<br />
Avoid in severe RI<br />
Veera Raghavulu B - Drug use and Dosing in Patients with Renal Impairment<br />
No. <strong>of</strong><br />
patients<br />
Of 215 renal impaired patients, 153 patients used two or more<br />
renal risk drugs.<br />
b<br />
The most common DRP for all patients with RI irrespective<br />
<strong>of</strong> their severity was non-optimal dose (75) as compared to<br />
non-optimal drug (33) or drug-drug interactions (56) or the<br />
need for monitoring (34) (Table 6).<br />
Generally there was a trend towards an increasing number <strong>of</strong><br />
non-optimal drug and drug-drug interaction with<br />
deteriorating renal function<br />
The commonest drug classes used in renal impaired patients<br />
b<br />
linked to DRP were Anti-bacterials (52 occurrences), ACE<br />
inhibitors (26 occurrences), oral hypoglycaemic drugs (15<br />
occurrences), allopurinol (12 occurrences), ranitidine (9<br />
Table 3: USE OF RENAL RISK DRUGS IN 215 PATIENTS WITH RENAL IMPAIRMENT (RI) AND FREQUENCY OF DRUG-RELATED<br />
PROBLEMS (DRPs) IN RELATION TO RISK RULES IN RI (n=551)<br />
No. <strong>of</strong> renal risk No. <strong>of</strong> renal risk<br />
drugs identified in drugs associated<br />
b<br />
each category (% with DRPs (% <strong>of</strong><br />
<strong>of</strong> drugs on discharge) renal risk drugs)<br />
183 299(17 %) 73(24 %) 112<br />
113<br />
70<br />
19<br />
135<br />
110<br />
16<br />
36<br />
27<br />
13<br />
14<br />
157<br />
122<br />
20<br />
219 (13 %)<br />
160<br />
19<br />
40<br />
33 (2 %)<br />
16<br />
17<br />
24 (15 %)<br />
47 (39 %)<br />
4 (20 %)<br />
35 (16 %)<br />
22 (14 %)<br />
13 (68 %)<br />
0<br />
33 (100 %)<br />
16 (100 %)<br />
17 (100 %)<br />
No. <strong>of</strong><br />
b<br />
DRPs<br />
46<br />
60<br />
6<br />
43<br />
25<br />
18<br />
0<br />
41<br />
23<br />
18<br />
Most frequent<br />
drugs associated<br />
b<br />
with DRP<br />
cefixime, quinapril<br />
Ranitidine,<br />
allopurinol<br />
Benzodiazepines<br />
Enalapril, quinapril<br />
Ciclosporin,<br />
sulphamethoxazole<br />
Metformin,<br />
spironolactone<br />
nitr<strong>of</strong>urantoin<br />
Aspirin, glimepride,<br />
glipizide<br />
a<br />
The number <strong>of</strong> patients in each main risk rule category is lower than the sum <strong>of</strong> patients in subgroups. The reason is that each patient<br />
b<br />
may belong to more than one <strong>of</strong> the subgroups, see Subjects and methods section. DRPs included: non-optimal drug, non-optimal<br />
dose, drug-drug interaction and need for monitoring.<br />
Table 4: Renal Risk Drugs as Proportions <strong>of</strong> all Drugs used by Various Degrees <strong>of</strong> Renal Impairment<br />
Renal impairment No. <strong>of</strong> Patients No. <strong>of</strong> drugs No. (%) <strong>of</strong> renal Ratio <strong>of</strong> renal risk<br />
(No. <strong>of</strong> drugs risk drugs drugs/all drugs per<br />
per patient)<br />
patient (mean)<br />
Mild (eGFR 20-50 mL/<br />
2<br />
minute/1.73 m ) 48 352 (7.33) 109 (31) 0.29<br />
Moderate (eGFR 10-20 mL/<br />
2<br />
minute/1.73 m ) 89 745 (8.37) 223 (30) 0.28<br />
Severe (eGFR < 10 mL/<br />
2<br />
minute/1.73 m ) 72 621 (7.96) 216 (35) 0.34<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
63
Veera Raghavulu B - Drug use and Dosing in Patients with Renal Impairment<br />
No. <strong>of</strong> renal risk<br />
drugs used<br />
Table 5: Distribution <strong>of</strong> 551 renal risk drugs in 215 Patients with Renal Impairment<br />
No. <strong>of</strong> patients No. <strong>of</strong> patients No. <strong>of</strong> patients<br />
required dosage required drugs to required drugs to<br />
adjustments n=183 be used with be avoided n=27<br />
Total No. <strong>of</strong><br />
patients used renal<br />
risk drugs n=215<br />
caution n=135<br />
Single drug 47 12 3 62<br />
Two drugs 45 41 8 60<br />
Three drugs 41 32 5 42<br />
Four drugs 16 16 2 17<br />
Five drugs 12 12 3 12<br />
Six drugs 18 18 6 18<br />
Seven drugs 2 2 0 2<br />
Eight drugs 2 2 0 2<br />
b<br />
Table 6: Comparison <strong>of</strong> Mild, Moderate and Severe Renal Impaired Patients with Regard to DRP<br />
b<br />
b<br />
b<br />
b No. <strong>of</strong> DRP in No. <strong>of</strong> DRP in No. <strong>of</strong> DRP in<br />
DRP<br />
mild RI n=48 moderate RI n=89 severe RI n=78<br />
Non-optimal dose 7 17 51<br />
Non-optimal drug 12 4 17<br />
Drug-drug interaction 22 21 13<br />
Need for monitoring 16 9 9<br />
Table: 7 Comparison <strong>of</strong> Mild, Moderate and Severe Renal Impaired Patients with Regard to<br />
b<br />
mean number Of DRP per Patient<br />
b<br />
DRP<br />
b<br />
b<br />
b<br />
No. <strong>of</strong> DRP per No. <strong>of</strong> DRP per No. <strong>of</strong> DRP per<br />
patient for mild patient for moderate patient for severe<br />
RI (mean) n=48 RI (mean) n=89 RI (mean) n=78<br />
Non-optimal dose 0.15 0.19 0.65<br />
Non-optimal drug 0.25 0.05 0.22<br />
Drug-drug interaction 0.17 0.19 0.63<br />
Need for monitoring 0.46 0.23 0.17<br />
Table 8: Comparison <strong>of</strong> Mild, Moderate and Severe Renal Impaired Patients<br />
b<br />
Mild vs<br />
DRP<br />
Mild vs Mild vs Moderate<br />
Moderate<br />
Moderate RI Severe RI vs SevereRI<br />
vs SevereRI<br />
Non-optimal dose NS < 0.05 < 0.05 < 0.01<br />
Non-optimal drug < 0.01 NS < 0.01 < 0.0001<br />
Drug-drug interaction NS < 0.01 < 0.01 NS<br />
Need for monitoring < 0.01 < 0.01 NS < 0.001<br />
occurrences), aspirin (8 occurrences) and atenolol (4<br />
occurrences).<br />
In 299 drugs for 162 patients required dosage adjustments<br />
according to renal function as recommended by guidelines.<br />
This adjustment was done in 224 drugs. The other 75 drugs<br />
were not adjusted involving 27 % <strong>of</strong> the patients. Table 9<br />
shows required versus implemented dosage adjustments<br />
according to guidelines in patients with renal impairment.<br />
Of the 551 renal risk drugs, 33(6 %) drugs which were<br />
recommended to be avoided according to renal function as per<br />
7<br />
guidelines were prescribed to the 27 patients with renal<br />
impairments (RI). Table 10 shows the list <strong>of</strong> these drugs used.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 64
Veera Raghavulu B - Drug use and Dosing in Patients with Renal Impairment<br />
b<br />
Fig. 1: Distribution <strong>of</strong> the drug-related problems (DRP ) per patient in<br />
hospitalized patients with different stages <strong>of</strong> renal function<br />
Fig.2: No. <strong>of</strong> Occurrences <strong>of</strong> drugs<br />
Egfr<br />
10-50<br />
mL/min/1.73 m<br />
Veera Raghavulu B - Drug use and Dosing in Patients with Renal Impairment<br />
DISCUSSION<br />
Drugs recommended to be used with caution, avoided or<br />
given with dose adjustment (renal risk drugs) in the case <strong>of</strong><br />
reduced renal function were commonly used in patients with<br />
Renal Impairment (RI). Apparently, the recommendations<br />
were only followed to a limited degree, as the utilization rates<br />
<strong>of</strong> renal risk drugs were high in patients with severe RI than in<br />
patients with mild to moderate RI.<br />
We found that in general, more drugs were prescribed per<br />
patient in the patients with moderate to severe renal<br />
impairment than in patients with mild renal impairment. The<br />
main reason for this was that the patients in the former group<br />
were older and had more accompanying co-morbidities: for<br />
example diabetes and hypertension, which evoke decline <strong>of</strong><br />
renal function in addition to the genuine age-related decline.<br />
Thus, the pharmacotherapy <strong>of</strong> the elderly becomes more<br />
abundant and more complex, contributing to the high<br />
proportion <strong>of</strong> renal risk drugs being used in patients with<br />
moderate to severe RI.<br />
The identification <strong>of</strong> high numbers <strong>of</strong> DRPs in patients with<br />
renal impairment is probably a result <strong>of</strong> special awareness <strong>of</strong><br />
DRPs within the multidisciplinary team, particularly so<br />
among the clinical pharmacists who, among other tasks, were<br />
specifically screening for DRPs. Attention to the occurrence<br />
<strong>of</strong> DRPs is a valuable way <strong>of</strong> monitoring drug therapy,<br />
helping physicians and other health care workers to act and<br />
adjust drug regimens before adverse events arise. Hege<br />
Salvesen Blix et al showed that among these, particular<br />
attention should be paid to the DRPs such as non-optimal<br />
dose, need for monitoring, non-optimal drug, drug<br />
interactions and adverse drug reactions, since these occurred<br />
more frequently in patients with non-adequate renal function,<br />
and besides, with a trend <strong>of</strong> more frequent occurrence with<br />
14<br />
increased severity <strong>of</strong> renal impairment. Our study identified<br />
DRPs such as non-optimal dose, need for monitoring, nonoptimal<br />
drug and drug-drug interactions, in patients with<br />
reduced renal function. DRPs were frequently associated with<br />
the use <strong>of</strong> renal risk drugs.<br />
The recommendation lists for renal risk drugs are long and<br />
include many drugs in common use, also drugs which are<br />
important and beneficial for patients with certain renal<br />
15<br />
diseases, for example, ACE inhibitors. Usually such<br />
substances do not create problems. However, these drugs<br />
must be used cautiously. Moreover, the drug<br />
recommendation lists address only single substances and do<br />
not give any guidance on how to handle the combination <strong>of</strong><br />
several renal risk drugs. Combinations <strong>of</strong> renal risk drugs may<br />
increase the hazards for patients with reduced renal function.<br />
We found that most patients received not only one renal risk<br />
drug but a combination <strong>of</strong> two or more. The question <strong>of</strong> how to<br />
combine renal risk drugs has not been addressed in the<br />
literature.<br />
The study by Vidal L et al (2005), shown that remarkable<br />
variations in definitions and recommendations, based on<br />
scarce data, make the available sources <strong>of</strong> these guidelines<br />
16<br />
less reliable . Physicians may refrain from dosage<br />
adjustments because <strong>of</strong> these confusing and <strong>of</strong>ten conflicting<br />
sources. A dynamic alert system would be useful to monitor<br />
the dosage <strong>of</strong> certain drugs in relation to a patient's renal<br />
function. Linking medication data to renal function<br />
parameters <strong>of</strong>fers the clinical pharmacist the ability to check<br />
medication pr<strong>of</strong>iles more quickly and accurately, which<br />
seems to be the solution to reducing medication errors and<br />
17<br />
improving pharmaceutical care. Further research is<br />
necessary before the specifications <strong>of</strong> such a system can be<br />
developed according to the needs and wishes <strong>of</strong> pharmacists<br />
and physicians.<br />
LIMITATIONS<br />
By performing this study in only one hospital, there is the<br />
possibility that our findings represent a unique situation. The<br />
time <strong>of</strong> discharge was chosen for the analysis because these<br />
patients are leaving the hospital with medication prescribed<br />
primarily for chronic use. Because patients with impaired<br />
renal function are vulnerable for an adverse drug event after<br />
hospitalization, drugs should be prescribed judiciously.<br />
Monitoring medication records at discharge could be a useful<br />
18<br />
tool to prevent rehospitalization.<br />
In our population, renal function was estimated using<br />
Modification <strong>of</strong> Diet in Renal Disease (MDRD) equation.<br />
This equation was developed in patients with chronic kidney<br />
disease, who were predominantly white and did not have<br />
diabetic kidney disease or a kidney transplant. The equation<br />
has been validated for African Americans but no other ethnic<br />
groups. The authors report that this method is more accurate at<br />
19<br />
estimating GFR than the Cockcr<strong>of</strong>t and Gault equation.<br />
However, the equation assumes that all patients have a body<br />
2<br />
surface area (BSA) <strong>of</strong> 1.73 m . For patients with a BSA less<br />
2<br />
than 1.73 m the eGFR is likely to overestimate their kidney<br />
2<br />
function and for patients with a BSA greater than 1.73 m the<br />
eGFR is likely to underestimate their kidney function. Use <strong>of</strong><br />
the patient's actual BSA will overcome this problem, but this<br />
requires the patient's height and weight to be available.<br />
CONCLUSION<br />
A clinical pharmacist in a nephrology unit is a valuable asset<br />
in monitoring drug dosing in RI patients. These patients are<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 66
Veera Raghavulu B - Drug use and Dosing in Patients with Renal Impairment<br />
<strong>of</strong>ten prescribed with drugs that have to be used with caution<br />
or avoid or dose reduced according to the grade <strong>of</strong> renal<br />
5<br />
impairment. The British National Formulary , Drug<br />
7<br />
prescribing in renal failure: dosing guidelines for adults and<br />
Renal drug handbook which gives a valuable guidance to<br />
clinical pharmacists on ward rounds in nephrology unit.<br />
These Guidelines can be implemented in a dynamic alert<br />
system that could help physicians and pharmacists to adapt<br />
drug dosing in patients with renal impairment. Such a<br />
computerized knowledge system, which would select patients<br />
at risk and link laboratory data to pharmacy data, can provide<br />
uniformity in dosing advice regardless <strong>of</strong> the healthcare<br />
pr<strong>of</strong>essional. This would lead to continuous and<br />
comprehensive screening <strong>of</strong> all contraindicated drugs and<br />
inadequate dosages. It should be remembered that the Official<br />
reduced doses recommended in product literature are <strong>of</strong>ten<br />
exceeded in practice, especially after lower doses have been<br />
tried. We believe that the above mentioned are essential to<br />
optimize pharmaceutical care for RI patients.<br />
ACKNOWLEDGEMENTS<br />
Authors wish to acknowledge T. Jayapal Reddy, Director,<br />
St.Peter's Institute <strong>of</strong> Pharmaceutical Sciences, Warangal<br />
(A.P) for the infrastructural facilities and moral support.<br />
REFERENCES<br />
1. Levey AS, Coresh J, Balk E et al. National Kidney<br />
Foundation practice guidelines for chronic kidney<br />
disease: evaluation, classification, and stratification. Ann<br />
Intern Med 2003; 139:137–147.<br />
2. St Peter WL, Khan SS, Ebben JP, Pereira BJ Collins AJ,<br />
Chronic kidney disease: the distribution <strong>of</strong> health care<br />
dollars. Kidney Int 2004; 66:313–321<br />
3. Turnheim K. Drug therapy in the elderly. Exp Gerontol<br />
2004; 39: 1731–1738<br />
4. Manian FA, Stone WJ, Alford RH. Adverse antibiotic<br />
effects associated with renal insufficiency. Rev Infect Dis<br />
1990; 12:236–249<br />
5. British National Formulary, 54th ed. London: British<br />
Medical Association and Royal Pharmaceutical Society<br />
<strong>of</strong> Great Britain, 2007.<br />
6. Ashley Caroline, Clare Introduction to Renal<br />
Therapeutics, Pharmaceutical Press, 2008.<br />
8. <strong>Mar</strong>c E. BROE DE, George AP, Clinical Nephrotoxins:<br />
rd<br />
Renal Injury from Drugs and Chemicals, 3 ed. Springer<br />
Science+Business Media, LLC, 2008.<br />
9. Myrna Y. Harleen, Drug Dosing Adjustments in Patients<br />
with Chronic Kidney Disease, American Academy <strong>of</strong><br />
Family Physicians, Am Fam Physician 2007; 75:1487-<br />
96.<br />
10. DRP-classification: van Mil Consultancy,<br />
Pharmaceutical Care Network Europe, V3.01. 2002<br />
11. Stockley's IH. Drug Interactions: a source book <strong>of</strong><br />
interactions, their mechanisms, clinical importance and<br />
management, 8 th ed. Pharmaceutical Press, 2008.<br />
12. David S. Tatro, Tatro DS (ed). Drug Interaction Facts<br />
2005. Facts and Comparisons, St. Louis,MO, 2005.<br />
13. George R. Bailie,Curtis A. Johnson, Nancy A. Masonand<br />
Wendy L, St. Peter. MED facts: Pocket guide <strong>of</strong> drug<br />
interactions, Nephrology pharmacy associates, Bone<br />
Care International, Inc.2000.<br />
14. Salvesen HB, Kirsten KV, Moger TA and Reikvam A.<br />
Use <strong>of</strong> renal risk drugs in hospitalized patients with<br />
impaired renal function—an underestimated problem.<br />
Nephrol Dial Transplant (2006) 21: 3164–3171<br />
15. Shlipak MG. Pharmacotherapy for heart failure in patients<br />
with renal insufficiency. Ann Intern Med 2003;<br />
138:917–924<br />
16. Vidal L, Shavit M, Fraser A et al. Systematic comparison<br />
<strong>of</strong> four sources <strong>of</strong> drug information regarding adjustment<br />
<strong>of</strong> dose for renal function. BMJ 2005; 331:263–266.<br />
17. Schiff GD, Klass D, Peterson J, Shah G, Bates DW.<br />
Linking laboratory and pharmacy: opportunities for<br />
reducing errors and improving care. Arch Intern Med<br />
2003;163:893-900.<br />
18. Wasserfallen J, Livio F, Buclin T, Tillet L, Yersin B,<br />
Biollaz J. Rate, type, and cost <strong>of</strong> adverse drug reactions in<br />
emergency department admissions. Eur J Intern Med<br />
2001;12:442-447.<br />
19. Poggio ED, Wang X, Greene T, Van Lente F, Hall PM.<br />
Performance <strong>of</strong> the modification <strong>of</strong> diet in renal disease<br />
and Cockcr<strong>of</strong>t-Gault equations in the estimation <strong>of</strong> GFR<br />
in health and in chronic kidney disease. J Am Soc Nephrol<br />
2005;16:459-466..<br />
7. Aron<strong>of</strong>f GR, Berns JS, Brier ME, et al. Drug prescribing in<br />
renal failure: dosing guidelines for adults. 4th ed.<br />
Philadelphia: American College <strong>of</strong> Physicians, American<br />
Society <strong>of</strong> Internal Medicine, 1999.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong> 67
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong><br />
Association <strong>of</strong> Pharmaceutical Teachers <strong>of</strong> India<br />
Prescription errors in Guntur district <strong>of</strong> Andhra Pradesh- A retrospective<br />
study<br />
1 1 2 3<br />
Pulla Reddy M* , Vijayapandi P , Aruna kanth C H , karthikeyan R<br />
1<br />
Department <strong>of</strong> Pharmacology, The Erode College <strong>of</strong> <strong>Pharmacy</strong> & Research Institute, Erode -638112, T.N.<br />
2<br />
Department <strong>of</strong> Analytical Chemistry,Governor States University, Illinois, Chicago, U.S.A.<br />
3<br />
Department <strong>of</strong> pharmacognosy, Vignan <strong>Pharmacy</strong> College, Vadlamudi, Guntur.<br />
A B S T R A C T<br />
During the course <strong>of</strong> treatment, drug prescribed to patients produce certain effects other than desired or expected effects. These are referred as<br />
adverse drug reactions which concern both patient as well as physician. People usually attribute these effects to either overdose or<br />
inappropriate medications or more drugs are prescribed by physician. ADRs are one <strong>of</strong> the leading causes <strong>of</strong> morbidity and mortality in health<br />
care and also associated with increased cost <strong>of</strong> treatment. Now a day's incidence <strong>of</strong> ADRs increases exponentially after a patient is on 4 or more<br />
medicines. Drug interaction represents 3-5% <strong>of</strong> preventable ADRs. Hence efforts are necessary to reduce unnecessary prescribing and this is<br />
where it becomes important to understand basic drug interactions. Given a choice between no treatment and effective treatment with a risk <strong>of</strong><br />
toxicity, physician usually selects latter one. Our job is to maximize the benefit and minimize the risk, but before we can minimize the risk, we<br />
must first be able to assess it accurately. Thus, health care practitioner must develop their own system <strong>of</strong> approach to prevent undesirable drug<br />
interactions; up-to-date database is valuable as well as frequent consultation with other members <strong>of</strong> healthcare team, like pharmacists and<br />
nurses, is essential.<br />
Key Words: Drug interactions, adverse drug reactions, Burden.<br />
Submitted: 5/2/<strong>2011</strong><br />
Accepted: 14/2/<strong>2011</strong><br />
INTRODUCTION<br />
The screening <strong>of</strong> prescriptions and intervention process<br />
commences with the pharmacist's initial assessment for<br />
completeness and legibility <strong>of</strong> the prescriptions. Prescription<br />
deficiencies formed a large proportion <strong>of</strong> errors identified in<br />
1<br />
prescription screening . This is mainly due to the attitude <strong>of</strong><br />
some prescribers who are always in a hurry and hence<br />
unwilling to spend a little more time in writing clear and<br />
complete prescriptions. However the extra time spent on the<br />
prescription will help to ensure that the patient receives the<br />
treatment that is intended by the prescriber. Additionally, the<br />
prescriber will be well compensated for the time taken by not<br />
2<br />
having to answer enquires from pharmacist . Errors in<br />
prescribing may be classified into two main types, errors <strong>of</strong><br />
omission and errors <strong>of</strong> commission. Errors <strong>of</strong> omission are<br />
defined as prescriptions with essential information missing,<br />
while errors <strong>of</strong> commission involve wrongly written<br />
3<br />
information in the prescriptions . Non-compliance with<br />
prescription writing requirements involves mainly errors <strong>of</strong><br />
Address for Correspondence:<br />
Raval DK, SVKM's NMIMS School <strong>of</strong> <strong>Pharmacy</strong> & Technology Management., Vile-Parle<br />
(W), MUMBAI - 400056. INDIA.<br />
4<br />
omission. A study by Ingrim et al ., in an outpatient pharmacy<br />
department found that the overall rate <strong>of</strong> prescription noncompliance<br />
was 14.4%. In this study, the pharmacist spent<br />
16.3 hours each day for correcting prescription errors. Other<br />
studies found that the rate <strong>of</strong> prescribing errors between 2.6%<br />
5-11<br />
to 15.4% . Studies on the types <strong>of</strong> prescribing errors in India<br />
appeared scarce in the literature. Therefore, the present study<br />
was conducted to evaluate the extent <strong>of</strong> non-compliance with<br />
prescribing writing requirements.<br />
MATERIAL AND METHODS<br />
Material: Photocopies <strong>of</strong> prescriptions were collected from<br />
different pharmacy stores in Guntur district <strong>of</strong> Andhra<br />
Pradesh, India<br />
Duration: The study was conducted during <strong>Jan</strong>uary 2009 to<br />
November 2009.<br />
Inclusion Criteria: Prescriptions having at least one<br />
prescription error were included in this study.<br />
Methods<br />
Parameters <strong>of</strong> Audit for Standard format <strong>of</strong> the prescription<br />
1. Patient identity: Name and address <strong>of</strong> the patient. Also<br />
age and weight in case <strong>of</strong> pediatric patients.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
68
Pulla Reddy M - Prescription Errors in Guntur district <strong>of</strong> Andhra Pradesh- A retrospective study<br />
2. Date on which the prescription was issued.<br />
Fig 1: Percentage errors committed in the total screening prescriptions<br />
3. Superscription symbol: Rx meaning “take thou” or<br />
“recipe”.<br />
4. Inscription: which includes the name <strong>of</strong> drugs, dose,<br />
dosage forms, and total amount <strong>of</strong> medication prescribed.<br />
5. Subscription: the dispensing and compounding<br />
instructions to the pharmacist as regards to form and<br />
quantities to be dispensed or supplied.<br />
6. Transcription or Signa: the direction to the patient for use<br />
<strong>of</strong> drugs.<br />
7. Prescriber's identity: Name, address and qualification.<br />
Retrospective Screening <strong>of</strong> Prescriptions<br />
The study was conducted in five different pharmacy stores in<br />
Guntur district <strong>of</strong> Andhra Pradesh state, India. The pharmacy<br />
stores receiving more than 100 prescriptions per day and was<br />
operated by at least one registered pharmacist; one trainee<br />
pharmacist and one pharmacy assistant were included in this<br />
study. The study involved retrospective screening <strong>of</strong> new<br />
prescriptions received by the above pharmacies. A researcher<br />
with pharmacy training but not a staff <strong>of</strong> the pharmacy<br />
collected the prescriptions during the study and screened<br />
them retrospectively. Any prescription that did not comply<br />
12, 13<br />
with one or more <strong>of</strong> the legal or prescription requirements<br />
would be considered as non -compliance and this was<br />
recorded in the standard form.<br />
RESULTS<br />
Totally 256 prescriptions were received during the study. Out<br />
<strong>of</strong> which 231 prescriptions were identified and included<br />
which contained atleast one prescription error. Of these<br />
prescriptions, 70.5% did not follow at least one <strong>of</strong> the legal or<br />
procedural requirements and the errors are classified in table 1<br />
& Fig 1. It was further noted that 172 prescriptions had<br />
mentioned diagnosis in it. Of the 231 prescriptions 37% <strong>of</strong><br />
patient's hadn't completely purchased the ordered<br />
prescription. The researcher who screened the prescriptions<br />
Table 1: Classification <strong>of</strong> Prescription Errors based on Standard<br />
17<br />
Format <strong>of</strong> the Prescription (n=231)<br />
Errors Frequency Percentage Error (%)<br />
Patient ’ s identity 3 36<br />
Age 62 11<br />
Sex 163 2<br />
Date 19 3<br />
Registration number 15.5 26.8<br />
Prescriber’s name 4.7 70.5<br />
Prescriber’s signature 0.8 8.2<br />
was unable to read many prescriptions while pharmacist in<br />
charge had managed to read these prescriptions.<br />
DISCUSSION<br />
Out <strong>of</strong> 256 prescriptions, only 25 prescriptions complied with<br />
all the legal requirements <strong>of</strong> the Standard prescription. This<br />
alarms a need <strong>of</strong> clear writing and completeness <strong>of</strong><br />
prescriptions from physician's side. Some useful points for<br />
2,14<br />
prescription writing have been suggested elsewhere. These<br />
included writing the patients full name, printing the name <strong>of</strong><br />
drugs especially those newly marketed medications and those<br />
infrequently prescribed agents, indicating the strength and<br />
dosage form <strong>of</strong> all drugs prescribed even if only single<br />
strength or dosage form is available. The rate <strong>of</strong> noncompliance<br />
to the legal or procedural requirements varied<br />
from 70.5% without physician's registration number. The<br />
seriousness <strong>of</strong> such non- compliance will lead to open ends to<br />
the quack doctors. The absence <strong>of</strong> the patient's age and sex<br />
would not normally prevent the dispensing <strong>of</strong> the<br />
prescription. It could be easily resolved with the patient or the<br />
holder <strong>of</strong> the prescription if required. Whereas absence <strong>of</strong> the<br />
prescribers signature would invalidate the prescription and<br />
cause in convenience to the patient and staff involved. This<br />
especially crucial if the prescription was for psychotropic or<br />
controlled drugs. More than 25.54 % <strong>of</strong> the prescriptions don't<br />
have diagnosis in it. This may be more helpful in the case<br />
where the patient visits another doctor during their drug<br />
therapy. Whether a prescription is legible or not depends on<br />
the assessor's familiarity with the handwriting <strong>of</strong> the<br />
prescriber as well as information provided in the prescription.<br />
This has been demonstrated in the present study where the<br />
researcher faced difficulties in reading many prescriptions as<br />
compared to the pharmacist <strong>of</strong> that pharmacy who managed to<br />
read all prescriptions. However, it should be emphasized that<br />
prescriptions should be easily read by anyone involved in the<br />
dispensing activities since the prescriptions could be filled by<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
69
Pulla Reddy M - Prescription Errors in Guntur district <strong>of</strong> Andhra Pradesh- A retrospective study<br />
any pharmacy. This is especially important since many drugs<br />
tend to have similar names such as ambroxil, amoxil, cetrizet,<br />
14<br />
cetricet, losec, lasix. This type <strong>of</strong> error may be reduced if the<br />
indication <strong>of</strong> the drug prescribed or the medical problem <strong>of</strong><br />
the patient is also written in the prescription as suggested by<br />
15<br />
Robinson. It is demonstrated that an elegant and clear<br />
prescription can cut transaction errors by 84% and save more<br />
16<br />
than 2.5 million dollars in adverse drug reaction. Therefore,<br />
all prescriptions should be clearly and adequately written and<br />
if possible printed to prevent such medication errors. The<br />
implementation <strong>of</strong> electronic prescription will probably<br />
eliminate some <strong>of</strong> these problems.<br />
CONCLUSION<br />
The results <strong>of</strong> the present study show a low compliance rate to<br />
the legal and procedural requirements in prescription writing.<br />
This alarms a need for pharmacy and medical educators to<br />
further emphasize the importance <strong>of</strong> writing clear and<br />
complete prescriptions. It also calls for the implementation <strong>of</strong><br />
educational and monitoring programs to bring more<br />
awareness to all concerned so as to reduce the rate <strong>of</strong> noncompliance<br />
and hence minimize the occurrence <strong>of</strong><br />
prescribing errors.<br />
REFERENCES<br />
1. Rupp MT, Schondelmeyer SW, Wilson GT, Krause JE.<br />
Documenting prescribing errors and pharmacist<br />
interventions in community pharmacy practice. Am<br />
Pharm 1988; NS28(9):30-37.<br />
2. Cohen MR, Davis NM. Complete prescription orders<br />
reduce medication errors. Am Pharm 1992; NS32:24-25.<br />
3. Rupp MT. Screening for prescribing errors. Am Pharm<br />
1991; NS31:71-78.<br />
4. Ingrim NB, Hokanson JA, Guernsey BG, Doutre WH,<br />
Blair CW Jr, Verrett TJ. Physician noncompliance with<br />
prescription writing requirements. Am J Hosp Pharm<br />
1983; 40:414- 417.<br />
5. Christensen DB, Campbell WH, Madsen S, Hartzema<br />
AG, Nudelman PM. Documenting outpatient problem<br />
intervention activities <strong>of</strong> pharmacists in an HMO. Med<br />
Care 1981; 19:105- 117.<br />
6. Folli HL, Poole RL, Benitz WE, Russo JC. Medication<br />
error prevention by clinical pharmacists in two children's<br />
hospital. Pediatrics 1987; 79:718-722.<br />
7. Morrill GB, Barreuther C. Screening discharged<br />
prescriptions. Am J Hosp Pharm 1988; 45:1904-1905.<br />
8. Hawkey CJ, Hodgson S, Norman A, Daneshmend TK,<br />
Garner ST. Effect <strong>of</strong> reactive pharmacy intervention on<br />
quality <strong>of</strong> hospital prescribing. BMJ 1990; 300:986-990.<br />
9. Bates DW, Boyle DL, Vander Vliet MB, Schneider J,<br />
Leape LL. Relationship between medication errors and<br />
adverse drug events. J Gen Intern Med 1995; 10:199-205.<br />
10. Lesar TS, Briceland L, Stein DS. Factors related to errors<br />
in medication prescribing. JAMA 1997; 277:312-317.<br />
11. Lesar TS, Lomaestro BM, Pohl H. Medication<br />
prescribing errors in a teaching hospital. A 9-year<br />
experience. Arch Intern Med 1997; 157:1569-1576.<br />
12. Aiken, M.G. and Pugh, A. L.G. pharmaceutical practice,<br />
st<br />
1 Ed., Churchill living stone, Edinburg, 1991:61-72<br />
13. Allen, L.V.Jr. Remington's. The science and practice <strong>of</strong><br />
th<br />
pharmacy 20 Ed., B.I. Publications, India, 2000:1706-<br />
1715.<br />
14. Aronson JK. Confusion over similar drug names:<br />
Problems and solutions. Drug Safety 1995; 12(3):155-<br />
160.<br />
15. Robinson A. An ounce <strong>of</strong> prevention could eliminate<br />
most prescription-writing errors. Can Med Assoc J 1994;<br />
151:659-661.<br />
16. Bates, D.W., Leape, L.L., Cullen DJ, et al. Effect <strong>of</strong><br />
Computerized Physician Order Entry and a Team<br />
Intervention on Prevention <strong>of</strong> Serious Medication Errors<br />
JAMA, 1998;280:1311-1316.<br />
17. Neville, R.G., Robertson, F., Livingstone, S., Crombie,<br />
I.K, Classification <strong>of</strong> prescription errors, <strong>Journal</strong> <strong>of</strong> the<br />
Royal College <strong>of</strong> General Practitioners, 1989;39:110-<br />
112.<br />
<strong>Indian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Pharmacy</strong> <strong>Practice</strong> Volume 4 Issue 1 <strong>Jan</strong>-<strong>Mar</strong>, <strong>2011</strong><br />
70