ABATACEPT - MetroPlus Health Plan
ABATACEPT - MetroPlus Health Plan
ABATACEPT - MetroPlus Health Plan
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
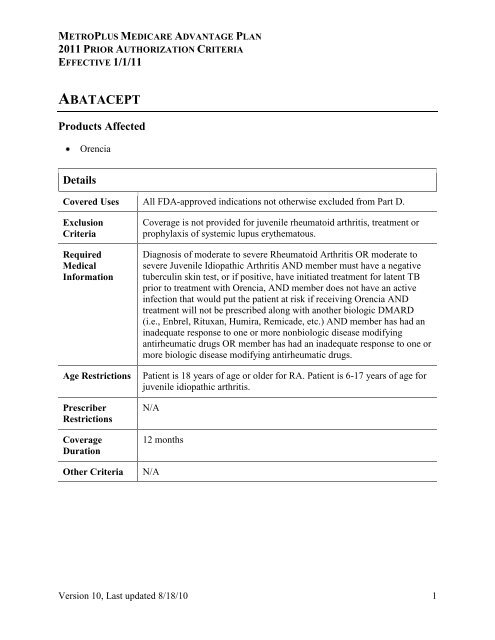
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
<strong>ABATACEPT</strong><br />
Products Affected<br />
Orencia<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage is not provided for juvenile rheumatoid arthritis, treatment or<br />
prophylaxis of systemic lupus erythematous.<br />
Diagnosis of moderate to severe Rheumatoid Arthritis OR moderate to<br />
severe Juvenile Idiopathic Arthritis AND member must have a negative<br />
tuberculin skin test, or if positive, have initiated treatment for latent TB<br />
prior to treatment with Orencia, AND member does not have an active<br />
infection that would put the patient at risk if receiving Orencia AND<br />
treatment will not be prescribed along with another biologic DMARD<br />
(i.e., Enbrel, Rituxan, Humira, Remicade, etc.) AND member has had an<br />
inadequate response to one or more nonbiologic disease modifying<br />
antirheumatic drugs OR member has had an inadequate response to one or<br />
more biologic disease modifying antirheumatic drugs.<br />
Patient is 18 years of age or older for RA. Patient is 6-17 years of age for<br />
juvenile idiopathic arthritis.<br />
N/A<br />
12 months<br />
N/A<br />
Version 10, Last updated 8/18/10 1
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
ADALIMUMAB<br />
Products Affected<br />
Humira INJ 40MG/0.8ML<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage is not provided for use of Humira in combination with other<br />
biologics e.g., Enbrel, Kineret or Remicade.<br />
Diagnosis<br />
N/A<br />
N/A<br />
12 months<br />
N/A<br />
Version 10, Last updated 8/18/10 2
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
ANABOLIC STEROIDS<br />
Products Affected<br />
Anadrol-50<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Known or suspected carcinoma of the prostate or male breast, carcinoma<br />
of the breast in females with hypercalcemia, pregnancy, nephrosis,<br />
hypercalcemia, severe hepatic impairment<br />
Approve if treatment is for: anemia caused by deficient red cell<br />
production (documented hematocrit less than 33 or hemoglobin less than<br />
12), hereditary angioedema, involuntary weight loss following extensive<br />
surgery, chronic infections, or severe trauma, failure to gain or maintain at<br />
least 90% of ideal body weight without definite pathophysiologic reasons,<br />
chronic corticosteroid administration, osteoporosis related bone pain<br />
N/A<br />
N/A<br />
6 months<br />
N/A<br />
Version 10, Last updated 8/18/10 3
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
ANAKINRA<br />
Products Affected<br />
Kineret<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
N/A<br />
Diagnosis of moderate to severe Rheumatoid Arthritis AND patient must<br />
have neutrophil counts assessed prior to beginning therapy, monthly for 3<br />
months and then quarterly thereafter for up to a year AND patient does<br />
not have an active infection AND treatment will not be prescribed with<br />
another biologic DMARD. Patient must also have had an inadequate<br />
response to at least one biologic and nonbiologic DMARD<br />
Patient must be 18 years or older<br />
N/A<br />
12 months<br />
N/A<br />
Version 10, Last updated 8/18/10 4
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
CERTOLIZUMAB<br />
Products Affected<br />
Cimzia<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
N/A<br />
Approve for FDA approved indications AND patient does not have a<br />
documented active infection, patient has been evaluated for tuberculosis<br />
risk factors and tested for latent infection prior to initiation of therapy and<br />
will be assessed periodically during therapy AND patient has failed to<br />
achieve symptom control after an adherent trial to conventional therapy<br />
AND patient has failed Remicade or Humira for Crohn's disease or Enbrel<br />
and Humira for rheumatoid arthritis<br />
Patient must be 18 years or older<br />
N/A<br />
3 months, then reassess for extension of PA x 1 yr.<br />
N/A<br />
Version 10, Last updated 8/18/10 5
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
DEGARELIX<br />
Products Affected<br />
Firmagon<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage not provided for females<br />
Diagnosis of advanced or metastatic prostate cancer OR patient has as an<br />
intermediate to high risk of disease recurrence AND orchiectomy is not<br />
indicated or not acceptable to the patient AND estrogen therapy is not<br />
indicated or not acceptable to the patient<br />
Patient must be at least 18 years of age<br />
N/A<br />
12 months<br />
N/A<br />
Version 10, Last updated 8/18/10 6
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
DICLOFENAC PATCH<br />
Products Affected<br />
Flector<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
N/A<br />
Approve if used for the topical treatment of acute pain due to minor<br />
strains, sprains, and contusions AND documented trial and failure of an<br />
oral NSAID or documented swallowing disorder<br />
N/A<br />
N/A<br />
12 months<br />
N/A<br />
Version 10, Last updated 8/18/10 7
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
ELTROMBOPAG<br />
Products Affected<br />
Promacta TABS 25MG, 50MG<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Concomitant use with other platelet-stimulating agents such as<br />
romiplostim or oprelvekin, Patient has failed to respond to therapy with<br />
eltrombopag following at least 4 weeks at the maximum dose,<br />
Eltrombopag is being used to normalize platelet count rather than to<br />
reduce the risk of bleeding in patients with chronic ITP,<br />
Chemotherapy/drug-induced thrombocytopenia, Treatment of<br />
thrombocytopenia due to causes other than chronic ITP, Patients who<br />
have previously failed therapy with eltrombopag<br />
Patient has a diagnosis of relapsed/refractory chronic ITP (greater than 6<br />
months) AND Prescriber and patient are enrolled in the Promacta Cares<br />
program (1-877-9-PROMACTA) AND Patient’s baseline platelet count is<br />
less than 50,000/mcL AND Patient’s degree of thrombocytopenia and<br />
clinical condition increases the risk for bleeding AND Patient is intolerant<br />
to splenectomy, and has had an insufficient response or is intolerant to<br />
corticosteroids and immune globulin OR Patient had a splenectomy with<br />
an inadequate response and had an insufficient response or is intolerant to<br />
corticosteroids and immune globulin.<br />
Patient is 18 years of age or older.<br />
N/A<br />
3 months<br />
N/A<br />
Version 10, Last updated 8/18/10 8
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
ERYTHROPOIETINS<br />
Products Affected<br />
Aranesp Albumin Free<br />
Epogen<br />
Procrit<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage not provided for prophylactic use to prevent chemotherapyinduced<br />
anemia or tumor hypoxia, sickle cell anemia, anemia associated<br />
only with radiotherapy or treatment of acute or chronic myelogenous<br />
leukemias or erythroid cancers, anemia of cancer not related to cancer<br />
treatment, anemia associated with iron deficiency, folate deficiency, B-12<br />
deficiency, hemolysis, or bone marrow fibrosis<br />
Pretreatment hemoglobin (Hgb) level must be less than 13 in anemic<br />
patients at high risk for perioperative blood loss and less than 10 for all<br />
other indications AND patient must have adequate iron stores prior to<br />
therapy AND patient must not have uncontrolled hypertension AND<br />
patient has not been diagnosed with antibody-mediated pure red cell<br />
aplasia AND other causes of anemia have been ruled out<br />
N/A<br />
N/A<br />
12 months<br />
Part B vs D Determination - if patient has end stage renal disease and is<br />
on dialysis, covered under Part B. Otherwise covered under Part D.<br />
Version 10, Last updated 8/18/10 9
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
FENTANYL CITRATE BUCCAL<br />
Products Affected<br />
Fentora<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage not provided in the management of acute or postoperative pain,<br />
opiod non-tolerant patients, patients with known intolerance or<br />
hypersensitivity to the drug or fentanyl<br />
Diagnosis of cancer and use is for breakthrough cancer pain AND other<br />
formulary short acting narcotics have been ineffective, not tolerated, or<br />
contraindicated AND patient is opioid tolerant and taking at least 60 mg<br />
morphine/day or an equianalgesic dose of another opioid for a week or<br />
longer<br />
Patient must be at least 18 years of age<br />
N/A<br />
6 months<br />
N/A<br />
Version 10, Last updated 8/18/10 10
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
GOSERELIN<br />
Products Affected<br />
«TableStart:Rx1»«Tradename»<br />
«DosageForm»<br />
«Strength»«TableEnd:Rx1»<br />
«TableStart:Rx2»«Tradename»<br />
«DosageForm»<br />
«Strength»«TableEnd:Rx2»<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Coverage is not provided for carcinoma of pancreas, chronic pelvic pain<br />
of female, In vitro fertilization, ovarian cancer, precocious puberty,<br />
uterine leiomyoma, females who are pregnant or lactating,the 10.8 mg<br />
dose is not indicated for use in women, continued therapy or restarted<br />
after malignant disease progression constituting treatment failure,<br />
concomitant use with other LHRH agents, experimental/investigational<br />
uses including indications not supported by CMS recognized compendia<br />
Diagnosis of advanced or metastatic prostate cancer OR patient has as an<br />
intermediate to high risk of disease recurrence AND orchiectomy is not<br />
indicated or not acceptable to the patient AND estrogen therapy is not<br />
indicated or not acceptable to the patient. Diagnosis of hormone receptor<br />
(ER and/or PR +) positive advanced breast cancer in pre- or<br />
perimenopausal female or male patient, only the 3.6 mg dosage form is<br />
approved for advanced breast cancer. Diagnosis of endometriosis AND<br />
patient has had an inadequate pain control response or intolerance to:<br />
Danazol (six month trial) OR Combination [estrogen/progesterone] Oral<br />
Contraceptives (six month trial) OR Progestins (six month trial), only the<br />
3.6 mg dosage form is approved for endometriosis.Diagnosis of<br />
dysfunctional uterine bleeding AND Patient is scheduled for endometrial<br />
ablation, only the 3.6 mg is approved for Endometrial<br />
Thinning/Endometrial Hypoplasia for Dysfunctional Uterine Bleeding<br />
Patient must be 18 years or older.<br />
For oncology uses only, prescriber is an oncologist or an individual highly<br />
familiar with prescribing and monitoring of oncology related medications<br />
Adv Prostate Cancer, Invasive Breast Cancer 12 mth. Endometriosis 6<br />
mth. Endometrial thinning 2 mth<br />
Version 10, Last updated 8/18/10 11
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
Other Criteria<br />
N/A<br />
Version 10, Last updated 8/18/10 12
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
GROWTH HORMONES<br />
Products Affected<br />
Genotropin<br />
Genotropin Miniquick<br />
Humatrope<br />
Humatrope Combo Pack<br />
Norditropin Cartridge<br />
Norditropin Nordiflex Pen INJ<br />
10MG/1.5ML<br />
Nutropin<br />
Nutropin Aq<br />
Nutropin Aq Pen<br />
Omnitrope INJ 5.8MG<br />
Saizen INJ 5MG<br />
Saizen Click.easy<br />
Serostim<br />
Tev-tropin<br />
Zorbtive<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage is not provided for constitutional delayed growth<br />
Diagnosis<br />
N/A<br />
N/A<br />
12 months<br />
N/A<br />
Version 10, Last updated 8/18/10 13
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
IMMUNE GLOBULIN<br />
Products Affected<br />
Carimune Nanofiltered INJ 3GM<br />
Gamastan S/d<br />
Gammagard Liquid<br />
Gamunex<br />
Octagam<br />
Vivaglobin<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage is not provided in patients with selective IgA deficiency, history<br />
of anaphylactic reaction or hypersensitivity to immune globulin<br />
preparations<br />
Diagnosis<br />
N/A<br />
N/A<br />
6 months<br />
N/A<br />
Version 10, Last updated 8/18/10 14
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
MECASERMIN<br />
Products Affected<br />
Increlex<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage is not provided in the presence of: Concurrent treatment with<br />
growth hormone or Pharmacologic doses of corticosteroids, Allergy to<br />
mecasermin (ICF-1) or any component of the formulation, growth<br />
promotion in patients with closed epiphyses, active or suspected<br />
neoplasia, diagnosis of growth failure in adults<br />
1) diagnosis of growth failure due to severe primary IGFD with (a)height<br />
standard deviation less than-3.0, (b) basal IGF-1 standard deviation<br />
scoreless than-3.0 and (c) normal or elevated growth hormone levels OR<br />
(2) diagnosis of growth failure due to growth hormone deletion with<br />
neutralizing antibodies to growth hormone AND (3) treating physician is<br />
an endocrinologist or has consulted with an endocrinologist AND (4)<br />
patient does NOT have any of the following conditions: growth hormone<br />
deficiency, malnutrition, hypothyroidism or chronic treatmetn with<br />
pharmacologic doses of anti-inflammatory steroids.<br />
Patient must be a pediatric patient that is at least 2 years of age<br />
Prescribing physician must be an endocrinologist<br />
12 months<br />
N/A<br />
Version 10, Last updated 8/18/10 15
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
METHYLNALTREXONE<br />
Products Affected<br />
Relistor<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage is not provided for use nausea, vomiting, pruritis, or urinary<br />
retention related to morphine or other opioids.<br />
Diagnosis of opioid-induced constipation in patients with advanced illness<br />
AND patient is receiving palliative care AND documented trial and<br />
insufficient response to laxative therapy AND no known or suspected<br />
mechanical gastrointestinal obstruction (contraindication) AND no severe<br />
or persistent diarrhea (therapy should be discontinued in cases of severe<br />
or persistent diarrhea)<br />
N/A<br />
N/A<br />
4 months<br />
Use of methylnaltrexone in this diagnosis has not been studied beyond<br />
four months.<br />
Version 10, Last updated 8/18/10 16
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
NABILONE<br />
Products Affected<br />
Cesamet<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
N/A<br />
Diagnosis of cancer with chemotherapy-induced nausea/vomitting AND<br />
failure to reach desired outcomes with use of two conventional<br />
antiemetics<br />
Patient must be at least 18 years of age<br />
N/A<br />
6 months<br />
N/A<br />
Version 10, Last updated 8/18/10 17
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
PAZOPANIB<br />
Products Affected<br />
Votrient<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage is not provided for Patients on concomitant tyrosine kinase<br />
inhibitors, Patients who have experienced significant disease progression<br />
while on pazopanib, Indications not supported by CMS-recognized<br />
compendia.<br />
Diagnosis of advanced renal cell carcinoma<br />
Patient is 18 years of age or older<br />
Prescriber is an oncologist or a healthcare provider highly familiar with<br />
prescribing and monitoring of oncology medications<br />
6 months<br />
N/A<br />
Version 10, Last updated 8/18/10 18
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
PEGFILGRASTIM<br />
Products Affected<br />
Neulasta<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
N/A<br />
Approve if anticipated that patient will require at least 10 days of white<br />
blood cell CSF therapy AND drug will be used as primary prophylaxis of<br />
febrile neutropenia associated with myelosuppresive chemotherapy OR<br />
patient's risk of febrile neutropenia is as least 20% or has risk factors if<br />
less than 20%, OR patient is receiving a dose density chemotherapy<br />
regimen OR patient had neutropenic complication from a prior cycle of<br />
chemotherapy OR patient had an autologous BMT or PBPC OR patient<br />
has diffuse aggressive lymphoma, is at least 65 years old, and being<br />
treated with curative chemotherapy OR patient is receiving radiation<br />
therapy, not on chemotherapy, and expected to have prolonged delays in<br />
treatment secondary to neutropenia<br />
N/A<br />
Patient is under the care of a physician with experience in prescribing<br />
pegfilgrastim<br />
4 months<br />
N/A<br />
Version 10, Last updated 8/18/10 19
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
PEGVISOMANT<br />
Products Affected<br />
Somavert<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage not provided for Cancer, Insulin resistance, McCune-Albright<br />
syndrome, Turner syndrome<br />
Patient has a diagnosis of acromegaly AND Patient has had inadequate<br />
response to surgery and/or radiation therapy and/or other medical<br />
therapies, or these therapies are not appropriate.<br />
Patient is 18 years of age or older<br />
Prescriber is an endocrinologist or an individual familiar with prescribing<br />
and monitoring acromegaly related medications<br />
12 months<br />
N/A<br />
Version 10, Last updated 8/18/10 20
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
RILONACEPT<br />
Products Affected<br />
Arcalyst<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Neonatal-Onset Multisystem Inflammatory Disease (NOMID), also<br />
referred to as Chronic Infantile Neurologic Cutaneous Articular<br />
Syndrome (CINCA), Familial Mediterranean Fever (FMF), TNF<br />
Receptor-Associated Periodic Syndromes (TRAPS),<br />
Hyperimmunoglobulinemia D with periodic fever syndrome [HIDS] (also<br />
known as Hyper-IgD syndrome with periodic fever), Pyogenic arthritis,<br />
pyoderma gangrenosum, and acne syndrome [PAPA], Pediatric<br />
granulomatous arthritis (which encompasses familial Blau syndrome and<br />
the sporadic early-onset sarcoidosis), Deficiency of IL-1 receptor<br />
antagonist (DIRA), Pseudogout, Schnitzler syndrome, Systemic Juvenile<br />
Idiopathic Arthritis (SJIA), Gout (acute, chronic), Majeed syndrome,<br />
Cherubism, Adult-onset Still disease, Asthma, Chronic obstructive<br />
pulmonary disorder (COPD), Diabetes (type 1 or type 2), Prediabetes,<br />
Atherosclerosis, Rheumatoid arthritis, Wet age-related macular<br />
degeneration<br />
Patient has diagnosis of Familial Cold Autoinflammatory Syndrome<br />
(FCAS) OR Muckle-Wells Syndrome (MWS) diagnosed by, or upon<br />
consultation with or recommendation of, an immunologist, allergist,<br />
dermatologist, rheumatologist, neurologist or other medical specialist<br />
(medical specialty should be indicated by prescriber) AND Patient has<br />
been screened for latent tuberculosis (TB) infection and is negative or if<br />
positive, has been treated by standard medical practice for TB AND<br />
Patient has received all recommended vaccinations AND Patient is not<br />
receiving concomitant therapy with TNF inhibitors (i.e., certolizumab<br />
[CIMZIA], etanercept [ENBREL], adalimumab [HUMIRA], infliximab<br />
[REMICADE]) or other IL-1 blockers (i.e. anakinra [KINERET],<br />
canakinumab [ILARIS])<br />
Patient must be at least 12 year of age<br />
Diagnosed by, or upon consultation with or recommendation of, an<br />
immunologist, allergist, dermatologist, rheumatologist, neurologist or<br />
Version 10, Last updated 8/18/10 21
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
other medical specialist (medical specialty should be indicated by<br />
prescriber)<br />
Coverage<br />
Duration<br />
Other Criteria<br />
12 months<br />
N/A<br />
Version 10, Last updated 8/18/10 22
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
SARGRAMOSTIM<br />
Products Affected<br />
Leukine<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
N/A<br />
Diagnosis<br />
N/A<br />
Physician with experience in prescribing sargramostim<br />
4 months<br />
N/A<br />
Version 10, Last updated 8/18/10 23
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
SILDENAFIL<br />
Products Affected<br />
Revatio<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage not provided for Sexual dysfunction as a result of<br />
antidepressant drug adverse reaction, Depression - Erectile Dysfunction,<br />
Diabetes mellitus - Erectile dysfunction, Dialysis procedure - Erectile<br />
dysfunction, Drug-induced impotence, Erectile dysfunction - Generalized<br />
atherosclerosis, Erectile dysfunction - Lower urinary tract symptoms, In<br />
combination with alfuzosin, Erectile dysfunction - Parkinson's disease,<br />
Erectile dysfunction - Peyronie's disease, Erectile dysfunction -<br />
Prostatectomy, Erectile dysfunction - Radiation therapy, Erectile<br />
dysfunction - Resection of rectum, Erectile dysfunction - Spina bifida,<br />
Erectile dysfunction - Spinal cord injury, Female sexual arousal disorder,<br />
Secondary Raynaud's phenomenon, Sexual dysfunction - Spinal cord<br />
injury.<br />
Diagnosis of Pulmonary Arterial Hypertension [PAH] (WHO Group I,<br />
WHO/NYHA functional class II, III or IV) AND Patient has undergone<br />
acute vasoreactivity testing and had a negative response or an initial<br />
positive response with subsequent failure of therapy with an oral calcium<br />
channel blocker (CCB) or the patient is unstable or has severe right-heart<br />
failure or a contraindication to CCB therapy AND Patient is not taking<br />
any of the following drugs concomitantly: organic nitrates in any form,<br />
ritonavir or other potent CYP3A4 inhibitors, Viagra or any other PDE5<br />
inhibitors AND Patients with hypoxia should receive concomitant oxygen<br />
therapy.<br />
N/A<br />
Prescription is written by a pulmonologist or cardiologist or<br />
documentation of consultation with pulmonologist or cardiologist<br />
Initial approval in new patients 6 months. Renewals annually thereafter.<br />
N/A<br />
Version 10, Last updated 8/18/10 24
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
SODIUM OXYBATE<br />
Products Affected<br />
Xyrem<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage is not provided for patients being treated with sedative hypnotic<br />
agents, patients with succinic semialdehyde dehydrogenase deficiency, a<br />
rare disorder is an inborn error of metabolism variably characterized by<br />
mental retardation, hypotonia, and ataxia.<br />
Documented (i.e., multiple sleep latency test) diagnosis of narcolepsy<br />
with excessive daytime sleepiness, cataplexy, or both. For a diagnosis of<br />
fibromyalgia, patients must try/fail two FDA approved drugs used for the<br />
treatment of fibromyalgia.<br />
Patients greater than 16 years of age.<br />
N/A<br />
Approval given for up to 3 years<br />
N/A<br />
Version 10, Last updated 8/18/10 25
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
TERIPARATIDE<br />
Products Affected<br />
Forteo<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
N/A<br />
Postmenopausal female with a diagnosis of osteoporosis OR male with<br />
diagnosis of hypogonadal osteoporosis with one of the following: history<br />
of osteoporotic fracture, multiple risk factors for fracture, trial and failure<br />
of oral bisphophonate, documented contraindication or intolerance to oral<br />
bisphophonate therapy<br />
Patient must be 18 years or older.<br />
N/A<br />
12 months<br />
N/A<br />
Version 10, Last updated 8/18/10 26
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
TREPROSTINIL-INJ<br />
Products Affected<br />
Remodulin<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage not provided for Heart failure and Peripheral ischemia (Severe).<br />
Diagnosis of Pulmonary Arterial Hypertension [PAH] (WHO Group I) in<br />
Class III - IV patients OR Diagnosis of PAH (WHO Group I) in Class II<br />
patients who do not respond adequately to or are unable to tolerate<br />
conventional therapy, such as REVATIO (sildenafil), ADCIRCA<br />
(tadalafil), TRACLEER (bosentan) or LETAIRIS (ambrisentan) AND<br />
Patient has undergone acute vasoreactivity testing and had a negative<br />
response or an initial positive response with subsequent failure of therapy<br />
with an oral calcium channel blocker (CCB) or the patient is unstable or<br />
has severe right-heart failure or a contraindication to CCB therapy AND<br />
Patients with hypoxia should receive concomitant oxygen therapy.<br />
N/A<br />
Prescription is written by a pulmonologist or cardiologist or<br />
documentation of consultation with pulmonologist or cardiologist<br />
Initial approval in new patients 6 months. Renewals annually thereafter.<br />
N/A<br />
Version 10, Last updated 8/18/10 27
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
ZICONOTIDE<br />
Products Affected<br />
«TableStart:Rx1»«Tradename»<br />
«DosageForm»<br />
«Strength»«TableEnd:Rx1»<br />
«TableStart:Rx2»«Tradename»<br />
«DosageForm»<br />
«Strength»«TableEnd:Rx2»<br />
Details<br />
Covered Uses All FDA-approved indications not otherwise excluded from Part D.<br />
Exclusion<br />
Criteria<br />
Required<br />
Medical<br />
Information<br />
Age Restrictions<br />
Prescriber<br />
Restrictions<br />
Coverage<br />
Duration<br />
Other Criteria<br />
Coverage not included for chronic cancer pain, ischemia, post-operative<br />
pain history of psychosis, known hypersensitivity to ziconotide or any of<br />
its formulation components, OR Patients with concomitant treatment or<br />
medical conditions that would render IT administration hazardous such as<br />
the presence of infection at the microinfusion injection site, uncontrolled<br />
bleeding diathesis, or spinal canal obstruction that impairs circulation of<br />
cerebrospinal fluid.<br />
Diagnosis of severe chronic, intractable pain related or unrelated to<br />
cancer, AND The patient has documented inadequate response,<br />
intolerable adverse events, or contraindications to IT morphine or IT<br />
hydromorphone (see Note). AND The patient with non-cancer pain has<br />
documented failure or intolerance (over a 6-month period) of other<br />
conservative treatment modalities such as: pharmacologic, surgical,<br />
psychological, physical. AND The patient with non-cancer pain has had a<br />
documented psychological evaluation both to rule-out that the pain is not<br />
psychological in nature and that the patient will benefit and be able to<br />
cope with the demands of an IDDS and IT drug therapy AND Ziconotide<br />
will be infused via an implanted Medtronic SynchroMed® EL,<br />
SynchroMed® II infusion system, or Smiths Medical MD CADD-Micro®<br />
ambulatory infusion pump.<br />
The patient is 18 years of age or older.<br />
Prescribed by a pain specialist or anesthesiologist who has experience<br />
with the use of IT pain medications.<br />
6 months<br />
Note: According to the American Academy of Pain Medicine proposed<br />
Version 10, Last updated 8/18/10 28
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
guidelines for the management of chronic pain, IT therapy should be<br />
administered through a permanently implanted drug-delivery system<br />
(IDDS). An IDDS for the administration of IT pain medications is<br />
considered medically necessary in the following types of patients<br />
experiencing pain: Cancer-pain patients who: Have documented failure or<br />
intolerance of opioids or other analgesics, AND Have a life expectancy of<br />
greater than 3 months, AND Do not have tumor encroachment on the<br />
thecal sac, AND Have no contraindications to implantation of the device<br />
Non-cancer patients who: Have documented failure or intolerance (over a<br />
6-month period) of other conservative treatment modalities such as:<br />
pharmacologic, surgical, psychological, physical, AND Had a<br />
psychological evaluation performed to determine that the pain is not<br />
psychological in origin and that benefit would occur with implantation of<br />
a device, AND Have no contraindications to the implantation of the<br />
device.<br />
Version 10, Last updated 8/18/10 29
METROPLUS MEDICARE ADVANTAGE PLAN<br />
2011 PRIOR AUTHORIZATION CRITERIA<br />
EFFECTIVE 1/1/11<br />
30