Cancer Program Annual Report - St. Clair Hospital
Cancer Program Annual Report - St. Clair Hospital
Cancer Program Annual Report - St. Clair Hospital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
2011<br />
<strong>Cancer</strong> <strong>Program</strong> <strong>Annual</strong> <strong>Report</strong><br />
December 30, 2011<br />
With <strong>Cancer</strong> Registry Data from 2010<br />
12/1/2011
<strong>Cancer</strong> Committee <strong>Report</strong> for 2011<br />
During 2011, The <strong>St</strong>. <strong>Clair</strong> <strong>Hospital</strong> <strong>Cancer</strong> Care <strong>Program</strong> has maintained the high standards of<br />
the American College of Surgeons’ Commission on <strong>Cancer</strong>. Our program provides all patients<br />
with a full range of diagnostic, treatment, and supportive services through the continuum of<br />
cancer care. Accomplishments in <strong>Cancer</strong> Care for 2011:<br />
The <strong>Cancer</strong> <strong>Program</strong> is approved as a Comprehensive Community <strong>Cancer</strong> Center by the<br />
American College of Surgeons Commission on <strong>Cancer</strong>.<br />
Richard Maley, Jr., M.D. continues to serve as our <strong>Cancer</strong> Liaison Physician and keeps the<br />
<strong>Cancer</strong> Committee informed through quarterly presentations of National <strong>Cancer</strong> Data Base<br />
information of <strong>St</strong>. <strong>Clair</strong> patients.<br />
<strong>St</strong>ate of the art radiation techniques are available to our patients on-site through a<br />
collaborative partnership with UPMC <strong>Cancer</strong> Centers. Treatments available are: 3-D conformal<br />
External Beam Radiation; Intensity Modulated Radiation Therapy (IMRT) for the treatment of<br />
breast, prostate, lung, and head & neck cancers; prostate seed program; and superficial electron<br />
treatments for skin lesions or to give boost treatments to surgical margins.<br />
The <strong>Cancer</strong> Care Committee continues to have weekly <strong>Cancer</strong> Care Conferences with<br />
either a prospective, retrospective, or didactic presentation. The <strong>Cancer</strong> Care Conference is<br />
attended by physicians from a variety of medical specialties, as well as nursing staff and other<br />
disciplines. Major cancer sites such as prostate, breast, colon, lung, and bladder, as well as other,<br />
less common primary site, have been topics of discussion and case presentation. Greater than<br />
90 cases have been presented.<br />
A monthly Breast Conference has been added to discuss cases with multidisciplinary<br />
team input. In addition a weekly radiation oncology roundtable occurs to discuss current cases.<br />
Internal auditing demonstrates that the tumor registry data is timely and compliant.<br />
The <strong>Cancer</strong> Care Conference has been approved for Continuing Education Credits for<br />
nurses.<br />
A focus on survivorship is evidence through our supportive services. In 2011 over 1,000<br />
oncology patients received rehabilitative services in the form of ostomy care, Physical Therapy,<br />
Occupational Therapy, and Speech Therapy. The <strong>Cancer</strong> <strong>Program</strong> provided South Hills<br />
Community residents with free cancer screenings and community programming. A new Head<br />
and Neck <strong>Cancer</strong> Support Group has been added to the repertoire of established support groups.<br />
Navigational services are now offered to newly diagnosed patients on the inpatient<br />
oncology unit. Designated nurses ensure that patients have all appointments scheduled and all<br />
necessary information to continue their care once they are discharged.<br />
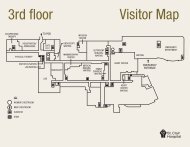
The Sipe Infusion Center was opened in July 2011. The new center is 3 times larger than<br />
the former infusion center and provides an updated and comfortable space for oncology<br />
outpatients at <strong>St</strong>. <strong>Clair</strong> hospital.<br />
In the year 2011, we continued to work towards our primary goals of prevention, early<br />
diagnosis, optimal treatment, rehabilitation, psychosocial support, and quality end of life care, to<br />
decrease mortality and morbidity of cancer in the United <strong>St</strong>ates.<br />
Anthony R. Haradin, M.D.<br />
Medical Director, <strong>Cancer</strong> Center at <strong>St</strong>. <strong>Clair</strong> <strong>Hospital</strong>
2011 CANCER CARE COMMITTEE ROSTER<br />
NAME TITLE DEPARTMENT/SECTION<br />
REQIURED PHYSICIAN MEMBERS<br />
Anthony R. Haradin, M.D. Medical Director, Hematology/Oncology<br />
<strong>Cancer</strong> Center<br />
Co-Chairman<br />
Robert Werner, M.D. Active Physician Radiation Oncology<br />
Co-Chairman<br />
Richard Maley, Jr., M.D. Active Physician Thoracic Surgery<br />
<strong>Cancer</strong> Liaison Physician<br />
Ronald Fierro, M.D. Active Physician Hematology/Oncology<br />
Leigh Nadler, M.D. Active Physician Colorectal Surgery<br />
Susanna B. Levitt, M.D. Active Physician Pathology<br />
Kris Ellis, M.D. Active Physician Radiology<br />
AD HOC PHYSICIAN MEMBERS<br />
Kevin Bordeau, M.D. Active Physician Urology<br />
Robert W. Bragdon, M.D. Active Physician Plastic Surgery<br />
David V. Glorioso, M.D. Active Physician Gastroenterology<br />
Sandra Jones-Gordon, M.D. Active Physician Internal Medicine<br />
Keith Lagnese, M.D. Active Physician Internal Medicine<br />
Evan Restelli, M.D. Active Physician Pulmonary<br />
Kenneth von der Porten, M.D. Active Physician Psychiatry<br />
<strong>St</strong>ephen F. Wawrose, M.D. Active Physician Otolaryngology<br />
Jason Whalen, M.D. Active Physician Dermatology<br />
G. Alan Yeasted, M.D. Vice President Medical Affairs<br />
Myles Zuckerman, M.D. Active Physician Family Practice<br />
REQUIRED NON-PHYSICIAN MEMBERS<br />
Barb Girod, BSN, MBA, RN Director <strong>Cancer</strong> <strong>Program</strong> Administrator<br />
Sarah Darby, RHIA, CTR Oncology Registry Sup. <strong>Cancer</strong> <strong>Program</strong><br />
Rosemary Miller, BSN, MSN, RN Oncology Nurse <strong>Cancer</strong> <strong>Program</strong><br />
Karen Gasper, BSN, RN OCN CHPN Palliative Care <strong>Cancer</strong> <strong>Program</strong><br />
Cindy Loughman, BSN, MA, RN Quality Analyst Office of Healthcare QI<br />
Karen Zientarski, BSN, RN Case Management Case Management Services<br />
Kristen Willoughby, RHIA Oncology Registrar <strong>Cancer</strong> <strong>Program</strong><br />
ADDITIONAL/AD HOC MEMBERS<br />
Nora Helfrich<br />
Community Member<br />
Diane White Representative American <strong>Cancer</strong> Society<br />
Marjorie Mills, LCP Spiritual Counselor Pastoral Care<br />
Kyra Williams Physical Therapist Physical Therapy<br />
Joan Massella, MEd, RN, MBA Administrative Vice Nursing<br />
Barry Vance, Pharm.D. Pharmacist Pharmacy<br />
Jan Hilterman, RN OCN IV Nurse Infusion Center<br />
Jean Lewis, MS RD Dietitian Nutritional Services<br />
Eve-Ellen Mandler Director Medical Records<br />
Rachel Mayo Representative American <strong>Cancer</strong> Society<br />
Sherry Rowsick, MSW/LSW Social Worker Social Services<br />
1
Hormone Therapy Compliance <strong>St</strong>udy<br />
Fall 2011<br />
Kevin P. Bordeau, MD, FACS<br />
Introduction<br />
Prostate <strong>Cancer</strong> remains the second most common form of cancer in men<br />
worldwide, with approximately 2.6 million men being diagnosed since 1995, and nearly<br />
375,000 have lost their lives to the disease from 1995 to 2007. Although prostate cancer is<br />
often thought of as a slow growing disease, it still has some fairly aggressive variants which<br />
can cause not only death, but significant morbidity. The recent controversy over PSA<br />
screening does not highlight this fact and therefore it is the opinion of the urologic<br />
community that PSA testing can be a valuable tool in diagnosing and treating men with<br />
prostate cancer.<br />
Once a diagnosis of prostate cancer has been determined, disease factors such as<br />
the pre-treatment PSA, Gleason score and digital rectal exam can be combined with patient factors such as age,<br />
body habitus and co-morbidities to determine an appropriate treatment plan. The disease factors are used to<br />
stratify patients as low, intermediate or high risk according to the following parameters:<br />
Low Risk: PSA< 10 ng/mL and a Gleason score of 6 or less<br />
Intermediate Risk: PSA >10 to 20 ng/mL or a Gleason score of 7 or<br />
palpable disease on DRE<br />
High Risk: PSA> 20 ng/mL or a Gleason score of 8 to 10<br />
The treatment of the disease will vary according to the risk stratification. Options range from active<br />
surveillance (i.e. monitoring the PSA without any form of active treatment), LHRH agonist therapy only, which<br />
reduces the PSA and shrinks the cancer but does not definitively cure the cancer, radiation options including<br />
brachytherapy and intensity modulated radiation therapy, and surgical removal. Randomized controlled studies<br />
have shown that the combination of radiation therapy and LHRH agonist therapy is superior to radiation alone for<br />
intermediate and high risk patients. It is, therefore, standard practice to give LHRH agonist therapy prior, during<br />
and after radiation for these patients.<br />
In an effort to strive to achieve excellent outcomes in our prostate cancer patients, we have undertaken this<br />
study to look at our compliance with accepted treatment guidelines.<br />
Methods<br />
A retrospective chart review was performed by the staff from our office and the cancer registry, looking at<br />
charts from 2009 and 2010, with an initial diagnosis of prostate cancer. These patients were then stratified based<br />
on the above risk levels, and it was determined whether the patients that received radiation therapy did in fact<br />
receive LHRH agonist therapy in accordance with accepted guidelines.<br />
2
Results<br />
In 2009 thorough 2010, 99 patients were diagnosed with prostate<br />
cancer at <strong>St</strong>. <strong>Clair</strong> <strong>Hospital</strong>. Of these patients, a total of 61 received LHRH<br />
agonist therapy. When we looked more specifically at those patients that<br />
received radiation therapy, 41 patients with intermediate or high risk<br />
prostate cancer received radiation therapy, either brachytherapy or<br />
combined brachytherapy and IMRT, and 36 of those received LHRH<br />
agonist therapy. This is a compliance rate of 87.8%.<br />
Discussion<br />
The purpose of our study was to take an objective look at our<br />
compliance with standard cancer treatment guidelines, specifically those<br />
for intermediate and high risk prostate cancer. In doing so, we hope to<br />
highlight the appropriate treatment protocols and police our compliance<br />
with them in an effort to maximize the care of our cancer patients and our<br />
outcomes.<br />
There are several limitations to this study starting with its<br />
retrospective nature and the fact that it does not include patients that may<br />
have either left our practice to have their care elsewhere or those that we<br />
saw as second opinions after the diagnosis had already been made. In<br />
general, the compliance rate of 87.8% also does not consider those<br />
patients that may technically meet the criteria for intermediate risk<br />
disease, but may have small volume disease and do not want to be<br />
subjected to the side effects of LHRH agonist therapy which include hot<br />
flashes, weight gain, and osteoporosis. There is also some increasing<br />
evidence that diabetes and cardiovascular disease has been linked to long<br />
term LHRH agonist treatment. The study also does not allow us to look at<br />
the duration of LHRH therapy which is even more dictated by how well<br />
patients are tolerating therapy. Although two and a half years of therapy<br />
is indicated for high risk disease, some patients do not comply with this<br />
based on their side effects, where as others may have no side effects at all.<br />
At this time, the 5 year relative survival rate for prostate cancer at<br />
<strong>St</strong> <strong>Clair</strong> is 97.3%, as compared to 99.6% nationwide. Although we are<br />
close, we hope that optimizing compliance with stated guidelines can<br />
improve our survival rate and equal if not surpass the national numbers.<br />
3
Services<br />
Rehab Services Evaluation<br />
Occupational Therapy: Occupational Therapy (OT) was consulted in 410 cancer patients in 2010. Risk assessment<br />
screening is completed by nursing staff on admission. A physician referral is required to order an OT evaluation.<br />
OT evaluates patient’s ability to perform activities of daily living and assess patients’ ability to return to previous<br />
level of functioning. OT is available to address pts with Lymphedema as well. OT services are available 7 days per<br />
week.<br />
Physical Therapy: Physical Therapy (PT) was consulted in 702 cancer patients in 2010. Risk assessment screening<br />
is completed by nursing staff on admission. A physician referral is required to order a PT evaluation. PT works<br />
with patients on functional mobility, strength and discharge recommendations based on the goals of the patient.<br />
PT services are available 7 days per week.<br />
Speech Therapy: Speech Therapy (ST) was consulted on 87 patients with cancer diagnosis in 2010. Nursing staff<br />
provide swallow risk assessment screening on admission. A physician referral is required for ST Consult. ST<br />
works with patients on swallowing, communication, cognitive issues, and provides diet recommendations for pts<br />
with swallowing issues. ST is also an integral component of the Modified Barium Swallow test. ST services are<br />
available 6 days per week.<br />
All rehab services provide documentation in the patients chart regarding goals, progress, discharge plan<br />
recommendations as well as education. 41 cancer patient charts were reviewed for rehab services notes. 100%<br />
compliance was noted in all instances except for 3 charts which did not have goals however these patients were<br />
independent and did not require skilled therapy services and were discharged from service after evaluation. Goals<br />
were not applicable in these 3 cases.<br />
<strong>Report</strong> on iLogic Inreach ® navigational technique and outcomes<br />
iLogic Inreach navigational system is used to aid in the retrieval of viable specimens during<br />
difficult bronchoscopy cases. Richard Maley Jr., MD has been using the iLogic® system at <strong>St</strong>.<br />
<strong>Clair</strong> <strong>Hospital</strong> since June of 2010. A retrospective quality study was performed. Twenty-three<br />
bronchoscopies were performed utilizing navigation technique from June 2010 to May 2011.<br />
The study reveals that 83% yielded adequate specimen for diagnosis and treatment decisions.<br />
Patient Care<br />
Comprehensive oncology care is provided for patients at <strong>St</strong>. <strong>Clair</strong> <strong>Hospital</strong>. Inpatient and outpatient facilities are<br />
supported by a full complement of interdisciplinary professionals. Oncology/hematology, surgery, radiation<br />
oncology, nursing, nutrition, rehabilitation, case management, social services, clinical pharmacology, spiritual<br />
counsel, palliative care and hospice work together to provide care throughout the continuum of a cancer diagnosis.<br />
<strong>St</strong>ate of the art radiation therapies are provided by an on-site partnership with UPMC <strong>Cancer</strong> Centers. Outside<br />
services such as the American <strong>Cancer</strong> Society and community representatives are consulted to assist in the<br />
evaluation and support of patient care.<br />
Support <strong>Program</strong>s<br />
Supportive and educational programs for staff, patients, and the community round out the <strong>St</strong>. <strong>Clair</strong> comprehensive<br />
cancer program. <strong>St</strong>aff receives oncology specific education and chemotherapy administration training to validate<br />
and ensure competency. Fifteen outreach programs, including cancer screenings, educational seminars, spiritual<br />
and counseling support services, and involvement in community events, were held in 2011. <strong>Cancer</strong> support groups<br />
are offered on a regular basis to enhance survivorship quality of life. Navigation through the complex system of<br />
oncology care is provided to all newly diagnosed cancer patients and a robust library provides educational<br />
materials for patients and staff.<br />
4
Grand Opening:<br />
Sipe Infusion Center<br />
July 2011<br />
July marked the opening of the Sipe Infusion Center. This capital improvement was made possible through a<br />
generous donation of a <strong>St</strong>. <strong>Clair</strong> patient. Denny Sipe was a frequent visitor to <strong>St</strong>. <strong>Clair</strong>’s Infusion Center. As part of<br />
his legacy he wanted to leave behind a comfortable place for all cancer patients to be treated. Design of the center<br />
included input from patients and staff as well as incorporating research on the design of infusion centers.<br />
The bright space includes many amenities for patient comfort, privacy, and safety. Eleven treatment chairs are<br />
arranged in pods of one or two chairs with sliding glass windows separating the pods. The design allows patients<br />
to choose private space or the ability to converse with fellow patients. Reclining treatment chairs are equipped<br />
with heat and massage and a<br />
pivoting table for meal trays and<br />
refreshments. Four private<br />
bedrooms are available for those<br />
patients requiring day-long<br />
treatments or protective isolation.<br />
The nurses’ work stations are only<br />
steps away from the treatment<br />
chairs, keeping patients in a clear<br />
line of sight even when nurses are<br />
documenting care in the electronic<br />
record. The close proximity of<br />
care givers to patients provides a<br />
sense of security to patients<br />
receiving complex therapies. The<br />
nursing staff is trained in<br />
chemotherapy administration and<br />
treatment of side effects.<br />
The Sipe Infusion Center provides convenience with hours of operation 7 days a week. This schedule allows<br />
patients the flexibility to continue their current lifestyle with family and work.<br />
<strong>St</strong>aff of the Sipe Infusion Center provides services for inpatients and outpatients. This includes chemotherapy<br />
administrations, blood transfusions, PICC insertions, and therapeutic phlebotomies. Other services available<br />
include care, repair and declotting of central lines, IV fluid and medication administration, injections and some<br />
diagnostic procedures.<br />
5
Percentage of New Cases of <strong>Cancer</strong><br />
Oncology Registry <strong>Report</strong><br />
<strong>St</strong>. <strong>Clair</strong> <strong>Hospital</strong>’s Oncology Registry is staffed by one full-time Registry Supervisor and a full-time registrar<br />
both of whom are Certified Tumor Registrars (CTR). A Registered Nurse works in the Registry 3 days a week<br />
coordinating <strong>Cancer</strong> Care Conferences and facilitating education credits for the nursing staff. The Registry<br />
supervisor and registrar perform all functions of the registry which includes case finding, abstracting, follow-up<br />
and reporting to the <strong>St</strong>ate Department of Health and National <strong>Cancer</strong> Data Base (NCDB). The Registry utilizes<br />
the Metriq <strong>Cancer</strong> Registry software package, which enables the Registry to maintain accurate data collection,<br />
prepare multiple reports, and respond to various requests for data and Oncology Registry information. The<br />
Oncology Registry staff abstract data according to the 2010 FORDS (Facility Oncology Registry Data<br />
<strong>St</strong>andards) Manual.<br />
The Seventh Edition of the AJCC (American Joint Committee on <strong>Cancer</strong>) provides staging guidelines for<br />
physicians and the Oncology Registrars. As members of the <strong>Cancer</strong> Care Committee, the Oncology Registry<br />
staff assists in the preparation for and attends quarterly <strong>Cancer</strong> Care Committee meetings and collaborated with<br />
other members to conduct Quality Improvement and Patient Care Evaluation <strong>St</strong>udies.<br />
All Registry staff attends the weekly <strong>Cancer</strong> Care Conferences. In 2010, the Oncology Registry staff regularly<br />
attended continuing education sessions provided by such organizations as the Pennsylvania Association of<br />
<strong>Cancer</strong> Registrars, Pennsylvania Department of Health and the National <strong>Cancer</strong> Registrars Association.<br />
2010 Incidence of <strong>Cancer</strong><br />
<strong>St</strong>. <strong>Clair</strong> vs. PA and U.S. Estimates<br />
Based on ACS <strong>Cancer</strong> Facts & Figures-2010<br />
25.0<br />
20.0<br />
15.0<br />
10.0<br />
5.0<br />
0.0<br />
<strong>St</strong>. <strong>Clair</strong><br />
PA<br />
U.S.<br />
Top Five Sites<br />
Figure 1 see incidence.xls<br />
Figure 1 illustrates the leading sites of cancer incidence for <strong>St</strong>. <strong>Clair</strong> <strong>Hospital</strong>, Pennsylvania, and the United<br />
<strong>St</strong>ates. The most frequently occurring sites are prostate, lung, colorectal, breast, and bladder. This data also<br />
includes female only breast cancer cases. The state and national data is taken from the American <strong>Cancer</strong><br />
Society’s 2010 edition of <strong>Cancer</strong> Facts and Figures and includes estimated figures. With the reference date<br />
being 1993, the Oncology Registry database consists of over 12,060 analytic cases.<br />
6
1993<br />
1994<br />
1995<br />
1996<br />
1997<br />
1998<br />
1999<br />
2000<br />
2001<br />
2002<br />
2003<br />
2004<br />
2005<br />
2006<br />
2007<br />
2008<br />
2009<br />
2010<br />
Number of Cases<br />
1100<br />
1000<br />
900<br />
800<br />
700<br />
600<br />
500<br />
1993-2010 Trend Analysis <strong>St</strong>. <strong>Clair</strong> <strong>Hospital</strong> <strong>Cancer</strong> Cases<br />
# Analytic Cases Ascession Year # Accessioned Cases<br />
Figure 2 see trend analyis.xls<br />
Figure 2 shows the number of analytic cases versus the number of cases accessioned. The number of both<br />
accessioned and analytic cases has greatly increased this year. This is felt to be due to surgical additions to the<br />
<strong>St</strong> <strong>Clair</strong> staff increasing the number of cancer directed surgeries performed at <strong>St</strong> <strong>Clair</strong> <strong>Hospital</strong> in 2010.<br />
No data submission was requested by the NCDB in 2010 in anticipation of the planned 2011 submission<br />
schedule increasing the frequency of reporting to every two months and providing more timely data analysis as<br />
a result. <strong>St</strong>. <strong>Clair</strong> <strong>Hospital</strong> will meet reporting guidelines in 2011 as required by the American College of<br />
Surgeons Commission on <strong>Cancer</strong>. This evaluation will enable the hospital to analyze those patients diagnosed<br />
through 2010 at <strong>St</strong>. <strong>Clair</strong> <strong>Hospital</strong> and compare with those diagnosed at other facilities accredited by the<br />
American College of Surgeons. The purpose of this study is to analyze the stage of disease at diagnosis and<br />
treatment modality chosen with the NCBD composite data.<br />
7
PRIMARY SITE<br />
2010 Frequency <strong>Report</strong>/Analytic Cases<br />
Total #<br />
Cases<br />
% of Total<br />
Cases Sex AJCC <strong>St</strong>age<br />
M F 00 01 02 03 04' N/A Unk<br />
Tongue 8 0.9% 7 1 0 4 0 1 2 0 1<br />
Salivary Gland 1 0.1% 0 1 0 0 1 0 0 0 0<br />
Floor of the Mouth 1 0.1% 1 0 0 0 1 0 0 0 0<br />
Gum & Other Mouth 2 0.2% 1 1 0 1 0 0 1 0 0<br />
Nasopharynx 1 0.1% 0 1 0 0 0 1 0 0 0<br />
Oropharynx 1 0.1% 1 0 0 0 0 0 1 0 0<br />
Hypopahrynx 1 0.1% 1 0 0 0 0 0 1 0 0<br />
Esophagus 8 0.9% 5 3 0 2 0 1 1 0 4<br />
<strong>St</strong>omach 18 2.1% 11 7 0 5 1 4 2 0 6<br />
Small Intestine 4 0.5% 0 4 0 0 0 1 2 1 0<br />
Colon 87 10.1% 47 40 8 19 24 16 17 0 3<br />
Rectosigmoid Junction 8 0.9% 6 2 0 3 1 1 3 0 0<br />
Rectum 30 3.5% 15 15 2 15 3 5 3 0 2<br />
Anus, Anal Canal 2 0.2% 0 2 0 0 0 1 0 0 1<br />
Liver-Intrahep Bile Ducts 4 0.5% 4 0 0 1 1 0 2 0 0<br />
Other Billiary 3 0.3% 2 1 0 0 1 0 1 1 0<br />
Pancreas 11 1.3% 9 2 0 1 1 0 8 0 1<br />
Perit, Omen & Mesen 2 0.2% 0 2 0 0 0 2 0 0 0<br />
Other Digestive Organs 1 0.1% 0 1 0 0 0 0 0 1 0<br />
Larynx 5 0.6% 5 0 0 2 0 2 1 0 0<br />
Bronchus and Lung 121 14.1% 58 63 0 19 16 36 43 0 7<br />
Soft Tiss Inc Heart 4 0.5% 3 1 0 3 0 1 0 0 0<br />
Skin/Melanoma 9 1.0% 6 3 0 4 1 0 1 0 3<br />
Non-Epithelial Skin 3 0.3% 2 1 0 1 1 0 0 0 1<br />
Basal & Squamous Skin 1 0.1% 0 1 1 0 0 0 0 0 0<br />
Breast 185 21.5% 3 182 49 50 33 17 10 0 26<br />
Cervix Uteri 7 0.8% 0 7 1 5 0 1 0 0 0<br />
Corpus Uteri 34 4.0% 0 34 0 24 2 2 3 0 3<br />
Ovary 21 2.4% 0 21 0 5 0 8 8 0 0<br />
Vagina 1 0.1% 0 1 0 1 0 0 0 0 0<br />
Vulva 6 0.7% 0 6 2 2 0 1 0 0 1<br />
Prostate Gland 60 7.0% 60 0 0 10 25 4 8 0 13<br />
Testis 2 0.2% 2 0 0 2 0 0 0 0 0<br />
Penis 1 0.1% 1 0 1 0 0 0 0 0 0<br />
Spermatic Cord 2 0.2% 2 0 0 0 0 0 0 2 0<br />
Bladder 59 6.9% 42 17 31 17 6 1 1 0 3<br />
Kidney & Renal Pel 25 2.9% 17 8 1 13 0 9 2 0 0<br />
Ureter 3 0.3% 1 2 2 0 1 0 0 0 0<br />
Other Urinary Organs 2 0.2% 2 0 2 0 0 0 0 0 0<br />
Brain 2 0.2% 2 0 0 0 0 0 0 2 0<br />
Cranial Nerves/Oth Nerv<br />
Sys 8 0.9% 3 5 0 0 0 0 0 8 0<br />
Thyroid Gland 29 3.4% 9 20 0 18 2 2 0 0 7<br />
Oth Endocrine/Thym 1 0.1% 1 0 0 0 0 0 0 1 0<br />
Hodgkins Lymphoma 9 1.0% 5 4 0 4 4 0 1 0 0<br />
Non-Hodgkin Lymph 32 3.7% 11 21 0 8 7 6 9 0 2<br />
Multiple Myeloma 11 1.3% 3 8 0 0 0 0 0 11 0<br />
Leukemias 3 0.3% 3 0 0 0 0 0 0 3 0<br />
Mesothelioma 2 0.2% 1 1 0 1 0 1 0 0 0<br />
Misc Sites 19 2.2% 11 8 0 0 0 0 0 19 0<br />
TOTAL 860 99.4% 363 497 100 240 132 124 131 49 84<br />
FIGURE 4<br />
8