Thrombophilia in Pregnancy - Skin & Allergy News
Thrombophilia in Pregnancy - Skin & Allergy News
Thrombophilia in Pregnancy - Skin & Allergy News
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Have a different op<strong>in</strong>ion? Concurr<strong>in</strong>g comments?<br />
Email a Letter to the Editor at carol.saunders@QHC.com.<br />
VIEWPOINT<br />
A Professional Op<strong>in</strong>ion Article<br />
<strong>Thrombophilia</strong> <strong>in</strong> <strong>Pregnancy</strong>:<br />
Stop Overscreen<strong>in</strong>g and<br />
Overtreat<strong>in</strong>g!<br />
Graham Gaylord Ashmead, MD<br />
Venous thromboembolism (VTE) and<br />
adverse pregnancy outcomes (APO) are<br />
potential complications of pregnancy.<br />
The risk of VTE <strong>in</strong> pregnancy is 1.8%<br />
and with recurrent VTE can be 11.1%. 1,2 Normal<br />
pregnancy is a hypercoagulable state evolved to<br />
protect from hemorrhage at delivery. <strong>Thrombophilia</strong>s<br />
<strong>in</strong> pregnancy are associated with VTE<br />
(20% to 40%) and APO, 2 but rout<strong>in</strong>e screen<strong>in</strong>g is<br />
not the answer.<br />
<strong>Thrombophilia</strong>s are too common and costly<br />
to screen asymptomatic patients. The most<br />
common <strong>in</strong>herited thrombophilias <strong>in</strong> white<br />
women <strong>in</strong> the United States are factor V Leiden<br />
(8%) and prothromb<strong>in</strong> G20210A mutation<br />
(3%). Less frequent are deficiencies of anticoagulants<br />
prote<strong>in</strong> C, prote<strong>in</strong> S, and antithromb<strong>in</strong><br />
III. <strong>Thrombophilia</strong> charges can be more<br />
than those for a delivery; however, what about<br />
positive test<strong>in</strong>g <strong>in</strong> 10% of the population?<br />
What about treatment risks? What about<br />
patient and physician anxiety?<br />
First trimester pregnancy loss does not benefit<br />
from thrombophilia screen<strong>in</strong>g. Second or<br />
third trimester loss does not differ <strong>in</strong> patients<br />
with factor V Leiden deficiency. Late fetal loss is<br />
associated with homozygosity for mutation of<br />
methylenetetrahydrofolate reductase (MTHFR)<br />
gene but only <strong>in</strong> the absence of folic acid supplementation.<br />
Known thrombophilias are not<br />
associated with 75% of isolated and 50% of<br />
familial thrombosis. 3<br />
For some thrombophilias, there is no need to<br />
screen everyone as most are be<strong>in</strong>g treated.<br />
Hyperhomocyste<strong>in</strong>emia or MTHFR mutations<br />
occur <strong>in</strong> 10% of the healthy US population. Therapy<br />
is folate (4 mg/day), vitam<strong>in</strong> B 12<br />
(250 mcg/day),<br />
Graham Gaylord Ashmead, MD, is Vice Chair and Chief,<br />
Division of Maternal Fetal Medic<strong>in</strong>e, Department of Obstetrics<br />
and Gynecology, W<strong>in</strong>throp University Hospital, M<strong>in</strong>eola, NY.<br />
and vitam<strong>in</strong> B 6<br />
(25 mg/day) supplementation.<br />
Folate <strong>in</strong> cereals and prenatal vitam<strong>in</strong>s makes<br />
pregnancy screen<strong>in</strong>g unnecessary.<br />
Indiscrim<strong>in</strong>ate pregnancy screen<strong>in</strong>g can<br />
cause problems. I saw an asymptomatic patient<br />
on baby aspir<strong>in</strong> expect<strong>in</strong>g hepar<strong>in</strong> because of a<br />
prote<strong>in</strong> S deficiency. Prote<strong>in</strong> S deficiency has an<br />
<strong>in</strong>cidence of 0.5%. 4 The risk of pregnant patients<br />
with known prote<strong>in</strong> S deficiency hav<strong>in</strong>g a VTE<br />
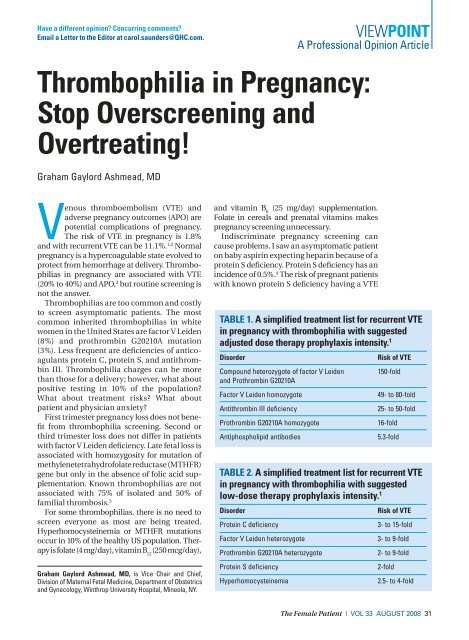
TABLE 1. A simplified treatment list for recurrent VTE<br />
<strong>in</strong> pregnancy with thrombophilia with suggested<br />
adjusted dose therapy prophylaxis <strong>in</strong>tensity. 1<br />
Disorder<br />
Compound heterozygote of factor V Leiden<br />
and Prothromb<strong>in</strong> G20210A<br />
Factor V Leiden homozygote<br />
Antithromb<strong>in</strong> III deficiency<br />
Prothromb<strong>in</strong> G20210A homozygote<br />
Antiphospholipid antibodies<br />
Risk of VTE<br />
150-fold<br />
49- to 80-fold<br />
25- to 50-fold<br />
16-fold<br />
5.3-fold<br />
TABLE 2. A simplified treatment list for recurrent VTE<br />
<strong>in</strong> pregnancy with thrombophilia with suggested<br />
low-dose therapy prophylaxis <strong>in</strong>tensity. 1<br />
Disorder<br />
Prote<strong>in</strong> C deficiency<br />
Factor V Leiden heterozygote<br />
Prothromb<strong>in</strong> G20210A heterozygote<br />
Prote<strong>in</strong> S deficiency<br />
Hyperhomocyste<strong>in</strong>emia<br />
Risk of VTE<br />
3- to 15-fold<br />
3- to 9-fold<br />
2- to 9-fold<br />
2-fold<br />
2.5- to 4-fold<br />
The Female Patient | VOL 33 AUGUST 2008 31
VIEWPOINT<br />
<strong>Thrombophilia</strong> <strong>in</strong> <strong>Pregnancy</strong><br />
TABLE 3. How can we stop overscreen<strong>in</strong>g for<br />
thrombophilia?<br />
• Asymptomatic patients should not be rout<strong>in</strong>ely screened.<br />
• Screen patients with:<br />
• A history of VTE<br />
• Unexpla<strong>in</strong>ed fetal loss greater than 12 weeks<br />
• Severe preeclampsia or HELLP syndrome, especially preterm<br />
• Severe fetal growth restriction, especially preterm<br />
• Family history of thrombosis<br />
• Start with a limited screen<strong>in</strong>g for:<br />
• Factor V Leiden mutation<br />
• Prothromb<strong>in</strong> G20210A mutation<br />
• Functional prote<strong>in</strong> S and C deficiencies (lower S levels <strong>in</strong><br />
pregnancy)<br />
• AT-III deficiency<br />
• Lupus anticoagulant<br />
• Homocyste<strong>in</strong>e level (if not on folate)<br />
• Anticardiolip<strong>in</strong> antibodies<br />
• Most asymptomatic pregnant patients with thrombophilia (no VTE or<br />
APO) do not require treatment.<br />
• Asymptomatic patients can benefit from UFH or LMWH throughout<br />
pregnancy when the patient presents:<br />
• AT-III deficiency<br />
• Homozygotes or compound heterozygotes for the factor V Leiden<br />
or prothromb<strong>in</strong> G20210A mutations<br />
• For asymptomatic pregnant thrombophilia patients, use short-term<br />
UFH or LMWH for risk factors (ie, multiple family members with VTE).<br />
• Treat appropriately, us<strong>in</strong>g the consensus report. 1<br />
<strong>in</strong> pregnancy is 22%, but as prote<strong>in</strong> S activity<br />
normally falls dur<strong>in</strong>g pregnancy, the ‘cutoff’ is<br />
lower (20% to 35% 2 ): the patient was normal.<br />
Treatments for thrombophilia have risks,<br />
whether it is aspir<strong>in</strong> (bleed<strong>in</strong>g) or hepar<strong>in</strong> (bruis<strong>in</strong>g,<br />
bleed<strong>in</strong>g, thrombocytopenia, hepar<strong>in</strong><br />
allergy and rash, osteopenia, <strong>in</strong>ability to receive<br />
regional anesthesia at delivery, and bleed<strong>in</strong>g at<br />
delivery). 1-4 Such risks are unnecessary.<br />
Patients with a history of VTE and thrombophilia<br />
should receive prophylaxis with low<br />
molecular weight hepar<strong>in</strong> (LMWH) or unfractionated<br />
hepar<strong>in</strong> (UFH), specific to the risk of<br />
VTE (Tables 1 and 2). Prophylaxis with LMWH<br />
or UFH may be considered antepartum and<br />
six weeks postpartum. Pregestational full<br />
anticoagulation should be ma<strong>in</strong>ta<strong>in</strong>ed dur<strong>in</strong>g<br />
pregnancy.<br />
Antifactor-Xa levels can be monitored by<br />
LMWH with a peak target range (drawn 3 to 4<br />
hours after subcutaneous adm<strong>in</strong>istration) of<br />
0.5 to 1.0 IU/mL <strong>in</strong> therapeutic sett<strong>in</strong>gs, twice<br />
daily. Trough levels (12 hours) should be 0.2 to<br />
0.4 IU/mL for therapeutic LMWH.<br />
Substitute LMWH with UFH at 36 week’s gestation<br />
or prior to delivery. Anticoagulation<br />
problems with delivery or regional anesthesia<br />
are unlikely to occur 12 hours from prophylactic<br />
or 24 hours from therapeutic LMWH. Discont<strong>in</strong>ue<br />
UFH <strong>in</strong> labor or 6 to 8 hours prior to<br />
cesarean delivery (skip morn<strong>in</strong>g dose for AM<br />
cesarean), and restart anticoagulation 12 hours<br />
after delivery or remov<strong>in</strong>g epidural catheter.<br />
One LMWH regimen for VTE is enoxapar<strong>in</strong><br />
sodium 40 mg (4000 IU) QD for prophylaxis and<br />
1 mg/kg (100 IU) BID for therapy. Prophylactic<br />
UFH can be 5000, 7500 or 10,000 units subcutaneously<br />
BID <strong>in</strong> the first, second, and third trimesters.<br />
Because LMWH and UFH do not cross<br />
the placenta, they are safe for breast feed<strong>in</strong>g.<br />
Consider calcium (1200 mg/day) and Vitam<strong>in</strong> D<br />
(800 IU) and check platelet counts. Treatment<br />
regimens are <strong>in</strong> a 2007 consensus report. 1<br />
Elim<strong>in</strong>at<strong>in</strong>g superfluous screen<strong>in</strong>g, while<br />
treat<strong>in</strong>g appropriately, should restore balance<br />
<strong>in</strong> pregnancy thrombophilia management<br />
(Table 3).<br />
The author reports no actual or potential conflicts<br />
of <strong>in</strong>terest <strong>in</strong> relation to this article.<br />
REFERENCES<br />
1. Duhl AJ, Paidas MJ, Ural SH, et al. Antithrombotic therapy<br />
and pregnancy: consensus report and recommendations<br />
for prevention and treatment of venous thromboembolism<br />
and adverse pregnancy outcomes. Am J Obstet Gynecol.<br />
2007;197(5):457.e1-21.<br />
2. James AH, Grotequt CA, Brancazio LR, Brown H. Thromboembolism<br />
<strong>in</strong> pregnancy: recurrence and its prevention.<br />
Sem<strong>in</strong> Per<strong>in</strong>atol. 2007;31(3):167-175.<br />
3. American College of Obstetricians and Gynecologists.<br />
ACOG Practice Bullet<strong>in</strong>. Management of recurrent early<br />
pregnancy loss. Number 24, February 2001. Int J Gynaecol<br />
Obstet. 2002;78(2):179-190.<br />
4. Auerbach RD, Lockwood CJ. Clott<strong>in</strong>g Disorders. In: James<br />
DK, Steer PJ, We<strong>in</strong>er CP, Gonik B, eds. High Risk <strong>Pregnancy</strong>:<br />
Management Options. 3 rd ed. London: Saunders; 2006:<br />
925-937.<br />
32 The Female Patient | VOL 33 AUGUST 2008 www.femalepatient.com