Anxiety CALM Intervention Manual - Regal Medical Group
Anxiety CALM Intervention Manual - Regal Medical Group
Anxiety CALM Intervention Manual - Regal Medical Group
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
1<br />
PETER P. ROY-BYRNE M.D.<br />
MICHELLE G. CRASKE Ph.D.<br />
MURRAY B. STEIN M.D., M.P.H.<br />
GREER SULLIVAN M.D., M.H.S.<br />
Adapted from IMPACT <strong>Intervention</strong> <strong>Manual</strong>:<br />
By Jurgen Unutzer M.D., M.P.H
2<br />
TABLE OF CONTENTS<br />
1. Project Overview . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-5<br />
2. <strong>CALM</strong>: Team Roles . . . . . . . . . . . . . . . . . . . . . . . . . 6-14<br />
3. Stepped Care for <strong>Anxiety</strong>: Overview . . . . . . . . . . . 15-20<br />
4. Introduction to Working with Anxious Patients . . . 21-25<br />
5. The Initial Patient Contact: Setting the Stage . . . . . 26-31<br />
6. Course of Treatment . . . . . . . . . . . . . . . . . . . . . . . . . 32-38<br />
7. Psychopharmacology Stepped Care Approach. . . 39-47<br />
8. Psychiatric Evaluation . . . . . . . . . . . . . . . . . . . . . . . 48-49<br />
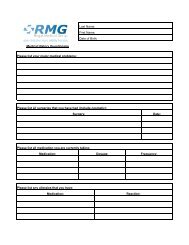
9. Documenting and Tracking Clinical Encounters … 50-51<br />
10. <strong>Anxiety</strong> Management Guide for the PCP . . . . . . . . . 52-61<br />
11. Handling of Emergencies . . . . . . . . . . . . . . . . . . . . . 62-64<br />
12. Supporting Materials . . . . . . . . . . . . . . . . . . . . . . . . . 65-66<br />
13. Acknowledgments . . . . . . . . . . . . . . . . . . . . . . . . . . . 67
3<br />
1. PROJECT OVERVIEW<br />
THE CLINICAL IMPORTANCE OF ANXIETY IN PRIMARY CARE<br />
<strong>Anxiety</strong> disorders are prevalent, highly co-morbid with one another, and<br />
often chronic in the primary care setting.<br />
Both depression and anxiety disorders more commonly present in primary care<br />
clinical settings than in mental health specialty settings. Although the treatment of<br />
depression in primary care settings has received much more attention, anxiety<br />
disorders as a group are more common than depression with a lifetime<br />
prevalence of 29% versus 21% for depression. Furthermore, anxiety disorders<br />
are often more chronic, persistent, and less episodic than depressive disorders.<br />
The most common anxiety disorders presenting in primary care clinical settings<br />
are panic disorder, generalized anxiety disorder, social anxiety disorder, and<br />
post-traumatic stress disorder, each with an estimated primary care prevalence<br />
of at least 5%. At least half of the people presenting with an anxiety disorder in<br />
primary care will have more than one anxiety disorder, and over 50% of persons<br />
with one anxiety disorder have co-morbid depression. Appropriately treating<br />
anxiety will likely have an impact on many depressed patients since the effective<br />
treatment approaches share certain similarities. This is particularly true for those<br />
patients who are the most severely ill, since anxiety with co-morbid depression<br />
has more severe symptoms, greater functional impairment, and a more chronic<br />
and persistent course.<br />
<strong>Anxiety</strong> disorders are associated with functional disability, impaired quality<br />
of life, and increased costs related to over utilization of medical services.<br />
<strong>Anxiety</strong> is associated with impairment in physical, mental and social functioning.<br />
Because the onset of many anxiety disorders occurs during the critical<br />
developmental stages of adolescence or young adulthood, persons with anxiety<br />
disorders may not achieve their full level of functioning. Reflecting this, many<br />
studies show a disproportionate number of persons with anxiety disorders are<br />
unable to hold a job and receive public assistance and/or disability support.<br />
Some anxiety disorders are associated with increased use of medical services,<br />
as common anxiety symptoms such as shortness of breath or chest pain may<br />
mimic important physical health symptoms. The resulting increase in<br />
unnecessary medical costs makes anxiety a major public health problem.<br />
<strong>Anxiety</strong> is poorly recognized and inadequately treated in primary care<br />
settings.<br />
<strong>Anxiety</strong> is less readily recognized than depression by both primary care providers<br />
(PCPs) and community mental health clinicians. A number of reports have<br />
documented that anxious patients see a number of non-psychiatric physicians<br />
before being appropriately diagnosed. The limited data we have on rates of
4<br />
primary care anxiety treatment suggest that medications are used infrequently<br />
(i.e., in only about 30% of cases), and often incorrectly. Utilization of effective<br />
psychological treatments is even less frequent. Finally, evidence indicates that<br />
anxiety treatment is complicated by poor adherence, which often leads to poor<br />
outcomes.<br />
Despite the availability of evidence-based treatments for anxiety disorders<br />
and preliminary effectiveness trials focusing on panic disorder, “userfriendly”<br />
models of delivering evidence-based anxiety treatments that can<br />
be easily applied in primary care have not been systematically investigated.<br />
Most patients have more than one anxiety disorder, frequently along with<br />
depression, making it confusing for the PCP to decide where to focus treatment<br />
and how to combine treatments for separate disorders. The competing demands<br />
of co-morbid medical conditions also limit the extent to which anxiety can be<br />
addressed. Patients’ receptivity to anxiety care may depend on their<br />
socioeconomic status, ethnic and cultural background, and attitudes and beliefs<br />
about (or preferences for) different treatments. Different systems of care are<br />
organized in different ways depending on the communities they serve and their<br />
funding sources. A model of care delivery that takes these factors into account is<br />
sorely needed.<br />
PROJECT GOAL<br />
The goal of this research project – entitled “<strong>CALM</strong>: Coordinated <strong>Anxiety</strong> Learning<br />
and Management” is to test an approach to assist PCPs deliver more effective<br />
treatment to persons with anxiety disorders.. We have developed a unified<br />
approach to detecting and treating a range of commonly occurring anxiety<br />
disorders (specifically panic disorder, generalized anxiety disorder, social phobia,<br />
and posttraumatic stress disorder) that is likely to be feasible and effective in<br />
primary care settings. The project will have unique features not previously<br />
utilized in first generation anxiety effectiveness studies in primary care. These<br />
include fewer exclusion criteria so that a broader range of patients will be eligible<br />
to participate, attention to patient’s preferences for treatment options, patient<br />
activation/motivational enhancement, and individually tailored psychological or<br />
psychopharmacological treatment.<br />
A key feature of the intervention is the anxiety clinical specialist (ACS) who will<br />
(1) assist the PCP by monitoring medication tolerability and adherence (for<br />
patients where medication is prescribed) and (2) provide cognitive behavioral<br />
therapy (CBT) when appropriate. The study is designed to be conducted with a<br />
diverse population of subjects in urban and rural areas and university and<br />
community settings. We hope to involve approximately 40% ethnic minority<br />
and/or Spanish-speaking patients.
5<br />
PROJECT ORGANIZATION<br />
<strong>CALM</strong> is funded by a grant from the National Institute of Mental Health (NIMH). It<br />
is carried out by research teams in Seattle, Los Angeles, San Diego, and Little<br />
Rock, with each team working with several primary care clinic sites.<br />
To maximize ethnic and socioeconomic class diversity, several sites are using<br />
low-income community health centers or special ethnic-minority HMOs as<br />
primary care recruitment sites. In each city, approximately 250 adults with one of<br />
the four common anxiety disorders in primary care will be identified by the<br />
primary care physician (PCP) and referred. PCPs may refer patients with known<br />
anxiety disorders directly to the study; if desired, they may use a simple five-item<br />
screen provided by study personnel to facilitate identification of anxiety disorders<br />
among their patients. Patients interested in participating are evaluated for<br />
eligibility by the ACS. Eligible patients then receive a baseline phone<br />
assessment from RAND survey interviewers and are then randomized to the<br />
<strong>CALM</strong> intervention or treatment as usual (TAU).<br />
All subjects (in both <strong>CALM</strong> and TAU arms of the study) are assessed<br />
independently by telephone by specially trained RAND interviewers (who will not<br />
know about treatment assignment) at baseline (before starting treatment), and at<br />
6, 12, and 18 months. These interviews will include the primary outcome<br />
measures for the study.<br />
OVERVIEW OF THE INTERVENTION STRATEGY<br />
The intervention (<strong>CALM</strong>) will be delivered by a diverse team of professionals at<br />
the primary care clinic. An anxiety clinical specialist (ACS) in the primary care<br />
clinic will conduct an initial assessment and, during an initial visit, will provide<br />
education, activation and preparatory techniques to encourage patients to pursue<br />
one of the available evidence based treatments. The ACS will coordinate all care<br />
for anxiety with the patient’s regular primary care provider (PCP), keep him/her<br />
informed of the patient’s progress through e-mail, fax, or other methods, and<br />
provide sustained monitoring and follow-up of the patient. Depending on the<br />
patient’s treatment choice, the ACS will either support anti-anxiety medication<br />
treatment by the PCP (who consults with the study psychiatrist as needed) or will<br />
deliver a manual-based form of CBT for anxiety. The ACS will receive<br />
supervision from a team psychiatrist. An expert psychologist at each site will<br />
additionally provide weekly CBT supervision for the ACS. Supervision can occur<br />
by telephone or in person depending on preference and logistics. A PCP<br />
“champion” will serve as a liaison between team members, other clinic PCPs<br />
and clinic staff and will meet with the ACS and team psychiatrist on a regular<br />
basis (e.g., once monthly). The team psychiatrist will be available to consult in<br />
person on patients who do not improve with a first treatment intervention and will<br />
then arrive at a plan for further treatment (augmenting the initial modality or<br />
adding the alternative modality) with the rest of the team.
6<br />
2. COORDINATED ANXIETY LEARNING & MANAGEMENT<br />
(<strong>CALM</strong>)<br />
THE INTERVENTION TEAM<br />
This chapter will describe in more detail the roles and responsibilities of each<br />
member of the intervention team. Please note that this intervention includes the<br />
patient as an active collaborator in treatment. To encourage patients to more<br />
actively participate in their treatment, those in the intervention arm of the study<br />
will receive an initial educational intervention via the ACS. This intervention<br />
(described more fully in Chapter 5) will include education about anxiety disorders,<br />
motivational enhancement, and assistance in identifying and overcoming barriers<br />
to treatment. In addition, patients in the intervention arm will receive educational<br />
materials (e.g., brochures) that describe the nature and treatment of the various<br />
anxiety disorders. They will also have the option of viewing a video tape (and/or<br />
access to a study web site) that also details the clinical characteristics and<br />
presentation of these disorders, their ability to mimic medical disorders, and the<br />
good clinical response to both pharmacologic and cognitive behavioral<br />
treatments.<br />
PATIENT’S PRIMARY CARE PROVIDER (PCP)<br />
The intervention is organized to support each PCP in the care of his or her<br />
anxious patients. Thus, the PCP will be at the center of the intervention team<br />
and will be responsible for initiating and maintaining pharmacologic anxiety<br />
treatment, in addition to usual treatment of comorbid or underlying medical<br />
problems and referrals to specialty care. All medication treatment decisions will<br />
be made by the PCP, using their own clinical experience and information in this<br />
manual. The PCP also plays an important role in encouraging the patient’s<br />
participation in the intervention activities. All PCPs will receive an initial training<br />
and orientation session on the project, as well as focused instruction on the<br />
pharmacological treatment of anxiety disorders. The PCP will have quick access<br />
(by phone or in-person if requested) to the study psychiatrist for “curbside<br />
consults”.<br />
We encourage PCPs to refer patients whom they already know to be anxious.<br />
We also strongly recommend the use of brief screeners within the clinic for<br />
identification of additional patients. This is important because the majority of<br />
anxiety disorders presenting in primary care clinics go undetected in routine care.<br />
For each patient referred to the study the primary care provider will receive<br />
information on: (1) whether a referred patient came for the screening<br />
appointment; (2) what the results of the screening interview were (i.e., MINI<br />
diagnoses and whether the patient is eligible for the study); (3) to which group<br />
the patient (if eligible) has been randomized. For those patients who enter the<br />
study and who are randomized to the intervention arm, the primary care provider<br />
can expect to receive regular feedback from the ACS regarding the patient’s
7<br />
clinical progress. The mechanism for this feedback will be tailored to<br />
accommodate the preferences of the PCP.<br />
Additional information in this manual especially relevant to the PCP can be found<br />
in Chapters 7 and 10. Chapter 7 describes in detail the stepped care approach<br />
and contains pertinent information about medications typically used to treat<br />
anxiety disorders. Chapter 10 presents an overview of anxiety management for<br />
the PCP and provides a list of questions that patients often ask about anxiety<br />
treatment along with appropriate responses to these questions.<br />
THE ANXIETY CLINICAL SPECIALIST (ACS)<br />
The ACS plays a central role in the <strong>CALM</strong> study. There are four main<br />
responsibilities of the ACS: (1) explaining the study to each patient referred by<br />
the PCP such that each potential study subject can make an informed decision<br />
regarding participation in the study; (2) for those patients who elect to participate<br />
in the study, conducting an initial assessment to determine eligibility for the<br />
study; (3) for those patients who are randomized to the <strong>CALM</strong> intervention arm,<br />
to work closely with the patient, PCP and study psychiatrist to manage and<br />
document the treatment process; and (4) for those patients in the <strong>CALM</strong><br />
intervention arm who elect to receive cognitive behavioral therapy (CBT), to<br />
deliver the CBT treatment. The ACS will receive training from study personnel<br />
regarding each of these four responsibilities. In addition, the ACS will participate<br />
in ongoing, intensive clinical supervision from both the study psychiatrist and the<br />
expert psychologist. Each of these responsibilities is described below.<br />
(1) Explaining the study. All potential subjects in this study will be referred by<br />
the PCP. The ACS will explain the purpose of the study and the overall design of<br />
the study to each referred patient and will be responsible for obtaining informed<br />
consent for the study. It will, therefore, be necessary for the ACS to be<br />
completely familiar with all aspects of the <strong>CALM</strong> intervention so that questions<br />
and concerns can be appropriately addressed. The ACS will need to be able to<br />
rapidly develop rapport with referred patients and understand special issues and<br />
concerns that are common to persons with anxiety disorders. (Refer to Chapter<br />
4 for a detailed description of these issues.) Preferably, these discussions with<br />
the potential subjects will occur in person but may sometimes be conducted by<br />
telephone. Training activities related to this responsibility will include role-playing<br />
so that ACS’s can become optimally comfortable with this process.<br />
(2) Conducting an initial assessment. For those subjects who elect to<br />
participate, the ACS will administer the MINI Diagnostic Interview, which is a<br />
structured clinical interview, to determine whether or not the potential subjects<br />
meet inclusion criteria for the study (i.e., are between the ages of 18-75 and<br />
suffer from one of the 4 anxiety disorders under consideration). This interview will<br />
also determine if subjects have a condition that would exclude them from the<br />
study such as schizophrenia, bipolar I disorder, or alcohol or substance<br />
dependence. This interview is expected to require between 30 and 45 minutes.
8<br />
At the end of the assessment the ACS should be able to conclusively determine<br />
whether or not the potential subject is eligible to participate. If the ACS has any<br />
questions regarding eligibility, the study psychiatrist and/or the project principal<br />
investigator should be contacted as soon as possible to assist in making this<br />
determination.<br />
The ACS will enter data obtained during this assessment into the secure, webbased<br />
database (described in Chapter 9). This information will be viewed<br />
centrally by study personnel at RAND who will initiate a telephone baseline<br />
interview to collect additional data and then randomly assign each eligible patient<br />
to either the <strong>CALM</strong> intervention or treatment-as-usual (TAU) arm of the study. All<br />
4 clinical sites in this national study will enter data into this central database such<br />
that randomization occurs centrally for all subjects entering the project.<br />
The ACS will subsequently be informed regarding the results of the<br />
randomization and will then reiterate and review with the patient what to expect,<br />
based on the group they have been assigned to. Those in the TAU arm will<br />
continue usual treatment with their PCP but will be interviewed by phone at<br />
baseline, 6, 12, and 18 months regarding their symptoms and progress. The ACS<br />
is expected to have no further contact with the patients randomized to the TAU<br />
arm of the study. Those who enter the <strong>CALM</strong> intervention arm will receive<br />
identical phone interviews at baseline, 6, 12 and 18 months but will also receive<br />
the additional clinical services included in the <strong>CALM</strong> intervention.<br />
All phone interviews for all subjects in the study nationally will be conducted by a<br />
survey research group at RAND, and the information collected in these<br />
interviews will comprise the primary outcome measures of the study. Therefore, it<br />
is imperative that the ACS ensure that accurate contact information is available<br />
for all subjects.<br />
(3) Working closely with the PCP and study psychiatrist to manage the<br />
treatment process. For those patients who enter the <strong>CALM</strong> intervention arm,<br />
the ACS will be responsible for following the patient and enlisting the assistance<br />
of the PCP and study psychiatrist as needed. Intensive supervision for all<br />
aspects of treatment will be provided as described briefly below.<br />
All patients in the <strong>CALM</strong> intervention will require management regardless of<br />
whether or not they elect to be treated with medications, CBT, or both. This<br />
section will briefly outline the ACS’s activities needed for optimal, overall<br />
management and the section after will focus on issues specifically related to<br />
provision of CBT.<br />
3a. The ACS will need to be familiar with local resources available to assist study<br />
patients with a number of issues, such as barriers to care (e.g., childcare and<br />
transportation resources), assistance with formal and informal substance abuse<br />
treatment services, and other appropriate local services. One of the first
9<br />
activities of the ACS should be to begin compiling a list of pertinent local<br />
resources.<br />
3b. The ACS will need to negotiate an optimal method to provide ongoing<br />
feedback to the PCP regarding patients’ progress and will confer with the PCP<br />
“champion” ( see page 12) to formulate a plan for the particular clinic. It will be<br />
crucial for the ACS to keep each patient’s PCP informed about the patient’s<br />
progress and any questions or problems that arise during treatment, with minimal<br />
effect on physician burden. At the beginning of the study, the ACS should make a<br />
point of personally introducing him/herself to each PCP in the clinic (though this<br />
may not be feasible in large practices with many PCPs), providing a brief<br />
introduction to the study and the role for the ACS. He or she should also ask<br />
each PCP about their preferred method for being contacted about patient-related<br />
matters (i.e., telephone, e-mail, pager, or direct in-clinic communication).<br />
3c. For all patients randomized to the <strong>CALM</strong> intervention arm the ACS will<br />
provide an initial intervention with the patient. The intervention has multiple<br />
components, including education about anxiety disorders and a discussion of<br />
treatment options. (Because this initial session is so important, we present a<br />
more detailed account of its content in Chapter 5.) During this session, the<br />
patient is presented with the two available treatment modalities, which are<br />
described in sufficient detail that the patient can appreciate their relative<br />
advantages and drawbacks and make an informed decision about which<br />
treatment to pursue. All patients will have the option to receive medication or<br />
CBT or both. The ACS is responsible for assisting the patient in making a<br />
treatment choice that is right for them.<br />
The ACS will also assist patients to identify potential barriers to treatment and<br />
means to overcome them, and will also provide motivational enhancement. The<br />
initial visit with the ACS focuses on patient education and activation, given that<br />
non-adherence with primary care behavioral treatment is common, and such<br />
education and activation have been shown to improve adherence. Motivational<br />
enhancement techniques will be used to identify barriers to treatment, and to<br />
strategize about ways of overcoming these barriers. The patient will be strongly<br />
encouraged to utilize the educational materials, and impediments to doing so will<br />
also be identified (e.g., problems with literacy or the availability of a VCR (VCRs<br />
will increasingly be an issue – DVD possible?) or computer access) so that these<br />
barriers might be overcome (e.g., use of a surrogate significant other for reading,<br />
use of an on-site VCR in the clinic to watch the videotape, recommendation to<br />
access web-based materials through a local public library). Components of this<br />
initial intervention may be repeated during the course of treatment as needed.<br />
3d. Once a patient has chosen a specific treatment option, the ACS is<br />
responsible for initiating the treatment option. This might include informing the<br />
PCP about the need for medication, initiating a course of CBT to be provided by<br />
the ACS, or both, depending on the patient’s previous treatment and current
10<br />
treatment preferences. In some clinics, PCPs may have already provided a<br />
medication prescription to the patient at the time of study referral. In all cases,<br />
the ACS will document the treatment plan, using structured forms, which will be<br />
entered into the secure web-based database, and reviewed by the study<br />
psychiatrist. A printed copy will be provided to the PCP who may or may not<br />
elect to put this in the patient’s chart.<br />
3e. The ACS will closely track patients’ clinical progress and will complete<br />
standard ratings at each visit for the purpose of monitoring progress. This will be<br />
accomplished via face-to-face meetings and phone contacts. The ACS may<br />
provide audiotapes of in person or phone sessions, which patients can replay to<br />
remind them of important suggestions, answers to key concerns they have had<br />
about their treatment, etc. The ACS will be responsible for entering information<br />
about follow-up visits and clinical progress into a web-based tracking system that<br />
will allow for easy overview and tracking of the ACS’s patient load. This database<br />
and ratings entered into it will also serve as a basis for the ACS’s weekly<br />
supervision by the study psychiatrist as well as for weekly CBT supervision by<br />
the psychologist.<br />
Some patients are expected to more rapidly achieve clinically significant<br />
improvement than others, who may require additional steps in treatment. In<br />
close consultation with the study psychiatrist and expert psychologist, the ACS<br />
will also need to assist in transitioning patients through the additional steps<br />
needed to achieve clinically significant improvement. Although these steps are<br />
tailored for each patient, their overall design is described in Chapter 3.<br />
Each of the four clinical sites will develop an “action plan” to be used in instances<br />
of clinical emergency, such as when a subject expresses suicidal thoughts. The<br />
ACS is required to assist in development of the local site’s plan and to<br />
consistently assess patients’ status regarding possible emergencies.<br />
3f. After patients reach a level of symptom relief and functioning with which they<br />
(and the PCP) are satisfied, the ACS and the patient will develop a relapse<br />
prevention plan (which will be entered into the Web system) and the ACS will<br />
follow the patient with monthly telephone contacts throughout the remainder of<br />
the year of treatment. Additional in-person contacts designed to reduce relapse<br />
risk will be an option, depending on the patient’s clinical status. The ACS will<br />
continue to document treatment response and services provided to the<br />
intervention patients using a web based clinical information system. In this way,<br />
patients who require additional treatment interventions will be identified, and<br />
modification to the treatment plan can be initiated as required.<br />
3g. The ACS will be expected to participate in regular and ongoing local<br />
supervisory sessions (weekly or bi-weekly) with the local study psychiatrist.<br />
During the meeting, the ACS will go over his or her case load and discuss all new<br />
patients and their treatment plans as well as ongoing patients who are
11<br />
experiencing difficulties with their treatments or not responding as expected.<br />
Patient discussions will be linked to clinical status evaluations measured with the<br />
use of simple rating instruments that the ACS will administer (see “Web-based<br />
Clinical Management System” below). The liaison PCP will attend at least one of<br />
these meetings per month to help problem-solve any clinic systems-related<br />
issues. The meetings will also facilitate effective and efficient communication<br />
between all members of the clinical team. The liaison PCP and team psychiatrist<br />
will be available to the ACS during the rest of the week by telephone or email to<br />
answer clinical or logistical questions. The liaison PCP in particular will be most<br />
helpful in answering questions about clinic logistics and comorbid medical<br />
problems, whereas the team psychiatrist will be most helpful with questions<br />
related to anxiety, anxiety psychopharmacologic treatment, and other comorbid<br />
psychiatric disorders.<br />
In addition, the ACS will participate in monthly national study teleconferences<br />
with ACSs and study psychiatrists from all four sites so that each will have the<br />
opportunity to learn from the experiences of their peers across the national study.<br />
These conferences will discuss any perceived problems with study logistics, skills<br />
developed in the process of the study, and tips regarding clinical management.<br />
(4) Finally, for those patients in the <strong>CALM</strong> intervention arm who select<br />
CBT, the ACS is directly responsible for scheduling and delivering the CBT.<br />
Ideally, the CBT sessions will be delivered in the office of the PCP in space<br />
specifically provided for the study. A typical course of CBT will involve 6<br />
sessions, although in some cases additional CBT may be necessary. The ACS,<br />
who is not expected to have expertise in the delivery of CBT when hired for the<br />
position, will receive intensive face-to-face training in the delivery of effective<br />
CBT. Since many subjects will have co-occurring disorders, the CBT will be<br />
targeted to the disorder identified by the patient as the one most bothersome or<br />
severe (see the CBT Treatment <strong>Manual</strong>). The ACS will receive ongoing<br />
supervision either in person or by phone by an expert psychologist. This<br />
supervision will cover issues pertaining to the application of CBT to each client’s<br />
needs and the obstacles to therapeutic improvement. In addition, some CBT<br />
sessions will be audiotaped and checked for fidelity to the CBT method by study<br />
personnel.<br />
PRIMARY CARE PROVIDER “CHAMPION”<br />
Each treatment team will have a primary care provider who will function as a<br />
liaison (or study “champion”) between the treatment team, the primary care clinic,<br />
and other PCPs in the clinic. The main role of the physician champion at each<br />
site will be to help solve logistical problems that inevitably arise in the conduct of<br />
a complex study such as this. He or she will also be responsible for keeping the<br />
study fresh in the minds of primary care providers by routinely reminding them<br />
about its goals at clinic meetings. As their level of familiarity and expertise with<br />
anxiety management grows as a result of their learning experiences throughout<br />
the study (e.g., attendance at weekly team meetings where treatment
12<br />
approaches are discussed in detail), this physician may choose to take a more<br />
active role in direct supervision of the ACS at their site. The intent is to develop<br />
local expertise in anxiety management at the PCP level that, eventually, may<br />
translate into better “staying power” of the intervention at these sites once the<br />
study is completed. PCP liaisons, like any of the other participating PCPs, will<br />
also carry their own caseload of patients who may be enrolled in the study.<br />
THE TEAM PSYCHIATRIST<br />
The team psychiatrist has three essential responsibilities.<br />
1. Clinical supervision of the ACS:<br />
The psychiatrist will meet or conference by phone weekly (or bi-weekly, as<br />
determined by the caseload) with the ACS and the rest of the study team to<br />
review treatment plans for all newly enrolled cases and all cases not improving<br />
as expected. Specifically, the psychiatrist will provide advice about how to<br />
overcome patient psychological barriers to continuing treatment and how to<br />
maximize patient self-activation by promoting good health habits (e.g., diet,<br />
exercise, regular sleep-wake cycle, staying socially and recreationally active);<br />
provide targeted education about the nature and treatment of anxiety to<br />
reinforce ACS activity; help to interpret effects of medical illness on symptoms<br />
and possible interactions with treatment; evaluate clinical status and progress<br />
thus far in treatment and alert the ACS if there is a need to re-contact the PCP<br />
about medications. The psychiatrist will also be available to the ACS by beeper<br />
to discuss clinical questions or emergencies. In general, the role is to review<br />
the treatment plan and progress, to help the ACS understand when to stay the<br />
course and when adjustments need to be made, and to be available for<br />
emergencies.<br />
2. Consultation to the PCP:<br />
The psychiatrist will be available for consultation (by telephone in most cases<br />
and in-person if requested) regarding medication issues on an as-needed<br />
basis. This consultation will help the PCP use the medication algorithm in this<br />
manual more effectively by reviewing the patient’s clinical status in light of the<br />
algorithm rules, presenting the various options, and determining which<br />
algorithm option to pursue. Psychiatrists will see all patients receiving treatment<br />
beyond the initial step, so phone consultation for initial step patients is entirely<br />
confined to discussion of dose adjustments and, in infrequent cases where<br />
there has been no response by week 6, to switches to a second antidepressant<br />
(or other medication).<br />
3. Direct patient consultation on “treatment resistant” cases
13<br />
The team psychiatrist assesses all patients who do not have an adequate<br />
response to treatment after 12 weeks for a one-time on site consultation.<br />
For this purpose, an incomplete response will be defined as failure to achieve a<br />
total score of 8 or lower on the OASIS and a score of 5 on the PHQ-3 (includes<br />
PHQ-2 plus “fatigue” item).<br />
The psychiatrist will also see the subset of patients who are not responding to<br />
two full treatment trials (each 12 weeks in length) in primary care for an extended<br />
consultation (1-2 follow-up visits) in the primary care clinic. If the psychiatrist<br />
decides that a patient’s mental health would be better managed in a specialty<br />
mental health setting, he/she may make a referral to the appropriate setting in<br />
consultation with the treatment team (if such a referral is possible and available).<br />
Extended consultation will not replace activities normally performed by the ACS<br />
such as CBT, but will be focused on a more comprehensive diagnostic evaluation<br />
and assessment (see next section), treatment recommendations, and possibly<br />
more complex psychopharmacological management in collaboration with the<br />
patient’s ACS and PCP.<br />
During an average week, study psychiatrists will spend their time on the project<br />
as follows:<br />
1. Weekly caseload supervision meetings with the rest of the study team<br />
(ACS and PCP) - I hour.<br />
2. PRN consultation to the ACS or PCPs during the week, available on<br />
beeper - 30 minutes.<br />
3. One time consultation (in person) for patients who are not showing a<br />
significant clinical response to the first line treatment initiated in primary<br />
care after 12 weeks – 2 hours.<br />
4. Extended consultation (up to 2 follow-up visits) for patients who do not<br />
show improvement after this initial consultation plus a second 12-week<br />
treatment trial with the PCP and the ACS. These visits are anticipated to<br />
involve less than 20% of the intervention patients – 1 hour.<br />
In addition, psychiatrists will, in collaboration with the ACS at the supervision<br />
meetings, review each patient’s progress at the completion of each step of<br />
treatment so that decisions can be made with the ACS regarding the next<br />
treatment step.<br />
THE EXPERT PSYCHOLOGIST<br />
The expert psychologist provides weekly supervision to the ACS for all ongoing<br />
CBT cases. The expert psychologist will have been involved in the ACS training<br />
and will therefore be in an excellent position to provide supervision. The<br />
psychologist may also consult directly with the patient at Step 2 or 3, if an<br />
adequate response to CBT has not occurred and if, (i) following psychiatric<br />
consultation, there are no medical or diagnostic factors contributing to non-
esponse, (ii) the patient is unwilling to pursue medication options, and (iii)<br />
attaining optimal response will require further CBT augmentation.<br />
14
15<br />
INTERVENTION FLOWCHART AND TIMELINE<br />
Baseline:<br />
--Patient completes a screen that is reviewed by the PCP who makes a referral if deemed<br />
appropriate or the PCP makes direct referral based on his or her own evaluation.<br />
-- Patient is interviewed by the ACS to confirm anxiety disorder and absence of exclusions<br />
-- Patient is interviewed by RAND randomized and scheduled for initial visit<br />
Initial Treatment Course:<br />
(Usually step one treatment)<br />
- Antidepressant or CBT<br />
- ACS has weekly contact<br />
with patient and keeps PCP<br />
informed of progress<br />
Assessment of<br />
Treatment<br />
Response<br />
None or<br />
incomplete<br />
response to<br />
treatment<br />
or worsens<br />
Consultation<br />
with team<br />
psychiatrist<br />
Step 2 or 3<br />
treatment as<br />
indicated<br />
Remission of<br />
<strong>Anxiety</strong><br />
Syndrome<br />
Maintenance Phase:<br />
- Relapse Prevention Plan<br />
- Monthly follow-up calls/visits
16<br />
3. STEPPED CARE FOR ANXIETY<br />
All patients enrolled in this project will meet diagnostic criteria for one of<br />
the four most common anxiety disorders in primary care (Panic Disorder<br />
[PD], Generalized <strong>Anxiety</strong> Disorder [GAD], Social <strong>Anxiety</strong> Disorder [SAD] or<br />
Posttraumatic Stress Disorder [PTSD]). They may differ in their prior history of<br />
mood and anxiety disorders, past treatments, current treatments, and the extent<br />
of medical and psychiatric comorbidities. Some patients already will be receiving<br />
treatment, most likely with antidepressants. Our experience and published<br />
studies indicate that approximately one in three patients with these anxiety<br />
disorders will already be receiving appropriate – though not necessarily optimal –<br />
pharmacological management at the time of study entry. Others may be<br />
receiving treatments of questionable or limited benefit. Others may have had<br />
counseling but still experience substantial symptoms and distress. Some patients<br />
may have a chronic course with early onset, while others may be experiencing<br />
their first episode of anxiety, perhaps in response to a life stressor or in<br />
association with a major medical illness.<br />
The ultimate goals of treatment are to (1) achieve symptomatic remission (see<br />
below) and return to optimal psychosocial functioning and to (2) prevent<br />
relapse and recurrence of anxiety. Because of the variation in each patient’s<br />
clinical circumstances it is not possible to specify a uniform treatment approach<br />
that will be a perfect fit for each patient. The stepped care treatment algorithm<br />
outlined in the next few pages provides a general guideline to be followed in<br />
treating intervention patients. Within this guideline, the treatment team will use<br />
clinical judgment to ensure that patients enter the stepped care algorithm at the<br />
correct step and that each patient has a treatment plan that is personalized to his<br />
or her clinical circumstances. This algorithm does not substitute for clinical<br />
judgment and experience. Rather, it is intended to prioritize evidence-based<br />
approaches to anxiety management, while recognizing that extant guidelines for<br />
anxiety management are, for the most part, consensus documents, given the<br />
absence of strong evidence for many specific treatment situations. There is still<br />
considerable uncertainty about optimal treatment approaches, and our algorithm<br />
constitutes only a common suggested starting point, with the experience of the<br />
team psychiatrist and psychologist (and, over time, the growing experience of the<br />
ACS and the PCPs) determining the course of treatment beyond the initial step.<br />
Published medication treatment guidelines from the American Psychiatric<br />
Association (APA, 1998) exist only for panic disorder and are now six years out<br />
of date and do not discuss the use of newer medications. Consensus guidelines<br />
using a Delphi method exist for PTSD and are five years out of date. The<br />
American Psychiatric Association will issue in late 2006 or early 2007 new<br />
treatment guidelines for panic disorder, but these are not available at this writing.<br />
For panic disorder and PTSD pharmacotherapy, these guidelines have been<br />
adapted and updated with newer information (e.g., Ballenger et al, 2000) to yield<br />
the suggested approaches described here. For GAD and SAD pharmacotherapy,
17<br />
the recommended stepped care algorithms are based on our synthesis of several<br />
consensus statements (Ballenger et al 1998; 2001). Finally, the World Council on<br />
<strong>Anxiety</strong> met in September 2000 and established consensus guidelines for the<br />
long-term treatment of anxiety disorders (CNS Spectrums 8: 2003). This<br />
includes specific papers outlining recommendations for long term treatment of<br />
panic disorder (Pollack et al 2003), GAD (Allgulander et al 2003), SAD (Van<br />
Ameringen et al 2003) and PTSD (Stein et al 2003).<br />
In terms of psychotherapy, the American Psychiatric Association (APA)<br />
advocates CBT as the psychosocial treatment of choice for panic disorder in their<br />
panic disorder Practice Guidelines (APA, 1998). Further, CBT for panic<br />
disorder/agoraphobia, generalized anxiety disorder, obsessive compulsive<br />
disorder, posttraumatic stress disorder, and social phobia has been deemed wellestablished<br />
or probably efficacious according to stringent guidelines set forth by<br />
the Task Force on Promotion and Dissemination of Psychological Procedures<br />
(Chambless et al., 1998).<br />
Stepped care treatment algorithm<br />
Step 1 (12 weeks—times are rough estimates)<br />
Step 1 is initiated in the primary care clinic in collaboration with the patient’s<br />
PCP. It will be the initial treatment step for the vast majority of intervention<br />
patients. Only the occasional patient who has just completed and failed what<br />
appears to be an adequate trial of Step 1 treatment should be considered to start<br />
at Step 2. If further medication is desired, a consultation with the psychiatrist is<br />
indicated (see Chapter 8). For patients already on prescription medication from<br />
their PCP at the time of study entry who opt for CBT, no consultation would be<br />
necessary. In addition, as described below, patients currently abusing alcohol<br />
will be referred to substance use treatments. Patients already involved in some<br />
non-CBT form of psychotherapy may continue this if they wish.<br />
This step begins with first line medication or CBT 2 , based on the outcome of the<br />
initial patient education session with the ACS, in which patients choose either<br />
medication or CBT after being familiarized with the advantages and<br />
disadvantages of each. If, after a thorough discussion of pros and cons of the<br />
treatments, the patient expresses a strong preference for beginning both<br />
medication and psychotherapy together, this will be accommodated<br />
Initial Treatment Choice: CBT<br />
Patients with a preference for this modality will start CBT in Step 1 (see CBT<br />
<strong>Manual</strong> in the appendix for details on this treatment modality). The patient who<br />
has a strong preference for starting both treatments simultaneously will start CBT<br />
and pharmacotherapy together.
18<br />
Initial Treatment Choice: Medication<br />
Patients with a preference for this modality will start medication in Step 1. See<br />
Chapter 8 for a detailed discussion of medications, side effect management,<br />
procedures for selection and dosing, and algorithms for the different steps of<br />
medication treatment.<br />
Medication OR CBT<br />
(usually an SSRI-titrated<br />
to therapeutic dose)<br />
Evaluate response to step 1 treatment.<br />
Patients who achieve remission (total score of 8 on the 5-item OASIS and score<br />
of 5 on PHQ-3), go to maintenance treatment. Others go to step 2 unless they<br />
insist they are improved enough and want to stop<br />
MED in step 1 CBT in step 1<br />
Very Good Response?<br />
Very Good Response?<br />
no* yes no yes<br />
Step 2 Maintenance Step 2 Maintenance<br />
(*If no response at 6 weeks (no reduction of at least one point in at least two OASIS<br />
items) or intolerant of first medication tried, switch to another first-line medication,<br />
usually within class (e.g., try a different SSRI)).<br />
MAINTENANCE TREATMENT<br />
Pharmacotherapy: Monthly phone calls should focus on continued medication<br />
adherence, improved health habits and the development of a relapse prevention<br />
plan (see Chapter 6).. Continue for at least one year, based on available relapse<br />
data with maintenance pharmacotherapy. At this point, tapered discontinuation<br />
may be considered if the patient is in or near remission (i.e., there are no residual<br />
anxiety or depressive symptoms present, and the patient reports excellent<br />
functioning to the ACS), does not have a history of recurrent depression or<br />
chronic anxiety, and there is an absence of ongoing medical and psychosocial<br />
stressors that might precipitate an imminent relapse. All decisions to taper<br />
medication should be reviewed with the consulting psychiatrist. If the patient<br />
prefers to stay on medication for the time being, this should not be discouraged.<br />
In this case, re-review by the PCP 3-6 months later should be planned.
19<br />
CBT: Monthly phone booster sessions will be provided by the ACS, focusing on<br />
reinforcement of cognitive behavioral skills and details of the relapse prevention<br />
plan (see CBT manual for details)<br />
Step 2 (12 weeks— times are rough estimates)<br />
Step 2 is preceded by an in-person psychiatric consultation (see Chapter 8)<br />
during which the case is reviewed and there is careful discussion with the ACS<br />
and patient about the patient’s preferences for adding the other modality or<br />
augmenting (or amplifying, in the case of providing additional CBT sessions) the<br />
current modality they are already receiving (12 weeks).<br />
Treatment Selection at Step 2:<br />
Decisions at Step 2 are guided by whether a patient has failed to respond (i.e.,<br />
no reduction of at least one point on at least two OASIS items or poor treatment<br />
tolerability) or whether they have had a partial response but failed to achieve<br />
remission (total score of 8 or lower on the 5-item OASIS and score of 5 or lower<br />
on PHQ-3). As in all steps, patient preference is a major guide in determining the<br />
next treatment to be pursued, although patients will be encouraged to accept<br />
treatment with the modality (medication or CBT) they have not tried, given the<br />
data on the advantages of combined treatment in panic disorder, and<br />
uncontrolled reports of benefit in partially responsive cases of other anxiety<br />
disorders. However, some CBT patients may prefer not to take medication, and<br />
require additional CBT. Likewise, some medication patients may prefer not to<br />
pursue CBT and will require additional medication. The procedures for<br />
augmentation of CBT with additional CBT are outlined in the CBT manual (where<br />
this is being considered, the psychologist will be involved in the decision).<br />
Procedures for additional medication treatments are provided in Chapter 8.<br />
(Medication in Step 1) (CBT in Step 1)<br />
Partial response to step 1<br />
Pharmacologically<br />
augment AD<br />
or<br />
add CBT<br />
No response<br />
Switch to CBT<br />
or<br />
Switch to different<br />
AD type<br />
Partial response<br />
Additional CBT<br />
sessions (augment)<br />
and/or<br />
add 1 st line AD<br />
No response<br />
Additional CBT<br />
sessions<br />
(switch focus)<br />
and/or<br />
add1 st line AD<br />
Evaluate response to Step 2 treatment<br />
Patients with full response go to maintenance treatment.<br />
Others are considered for Step 3.
20<br />
Step 3 and 4 6 (24-36 weeks)<br />
Consider:<br />
Further CBT augmentation, but only in select cases approved by the<br />
expert psychologist after seeing the patient in consultation (MICHELLE?)<br />
Trial of 2 nd or 3 rd type of antidepressant<br />
Combination of medication and CBT (if not already tried in step 2)<br />
Other augmentation of antidepressants (if patient has had a partial<br />
response to an antidepressant in step 2) 5<br />
Referral to specialty mental health care for more ongoing treatment if<br />
there is a need for couples or family therapy, more specific substance<br />
abuse treatment, or there are complex psychological issues such as<br />
childhood sexual abuse or maltreatment.<br />
.<br />
Even patients who have been referred for specialty mental health care (e.g.,<br />
additional psychotherapy) will remain in the study. The ACS will follow them with<br />
regular (at least monthly) telephone calls and keep the patient’s regular PCP<br />
apprised of progress.<br />
7 Additional Treatments to be Considered During the <strong>Intervention</strong>:<br />
Additional treatments that may be considered by the ACS or the treatment team<br />
at any stage in the treatment course include:<br />
1. Referrals to self help groups such as AA and NA<br />
2. Referrals to support groups run by ALANON or caregiver support groups<br />
3. Referrals to other community resources<br />
Each ACS should develop and maintain a local resource list for such referrals<br />
(see Appendix A).<br />
SPECIAL POPULATIONS<br />
1. Patients with comorbid depression: In general, patients with comorbid<br />
depression who opt for medication should be treated using antidepressants<br />
such as SSRIs or SNRIs. In non-responsive patients, supplementation with a<br />
second antidepressant rather than a benzodiazepine may be preferable.<br />
Consultation with the team psychiatrist can be helpful in making treatment<br />
plans for patients with comorbid depression and anxiety disorders. Patients<br />
electing a course of CBT whose depression does not concurrently improve<br />
with their anxiety, should be encouraged to consider an antidepressant<br />
medication.<br />
2. Patients with comorbid alcohol or substance abuse: A patient with<br />
anxiety and comorbid alcohol abuse should be routinely referred for<br />
treatment of alcohol abuse.They should usually be referred for alcohol abuse<br />
specialty treatment as available and to a self-help group such as AA or NA.<br />
At times, it is prudent to initiate substance abuse treatment before starting an
21<br />
antidepressant because symptoms of anxiety may occasionally remit with<br />
successful treatment of the alcohol or substance abuse. At other times,<br />
however, untreated anxiety symptoms can fuel substance abuse and make<br />
adherence to (and even attendance at) AA unlikely. The decision when to<br />
start anxiety treatment is a complex one, and the team psychiatrist should be<br />
consulted to assist with this decision.<br />
3. Patients with bipolar II (“atypical bipolar”) disorder Although the<br />
diagnostic interview at study entry should identify patients with a bipolar<br />
diagnosis and eliminate anyone with unstable bipolar illness, atypical bipolar<br />
illness remains a major cause of treatment-refractory anxiety symptoms.<br />
Such individuals are often suffering from “mixed states” and the use of<br />
anticonvulsant medication or lithium is frequently required for symptom<br />
control. Such individuals may need to be referred to specialty mental health<br />
settings, although select cases could be initially managed by the PCP in<br />
conjunction with the psychiatrist who can recommend an initial trial of either<br />
lithium, valproate or an atypical anti-psychotic. If these patients are not<br />
referred to specialty treatment, they should have a consult with the study<br />
psychiatrist, face to face, before a recommendation is made.<br />
Patients with recurrence during the course of the one-year treatment<br />
program return to the step after the one they stopped at (likely Step 2 or<br />
Step 3).
22<br />
4. INTRODUCTION TO WORKING WITH ANXIOUS PATIENTS<br />
Working with Anxious Patients:<br />
To empower each patient to be an active participant in treatment, it is vital to<br />
establish a therapeutic alliance with the patient. Persons with anxiety, like many<br />
individuals with mental disorders, feel ashamed and stigmatized by their<br />
symptoms. They have often functioned quite well before symptom onset and<br />
frequently experience a strong sense of isolation because of their difficulties.<br />
While there is often an immediate beneficial effect when someone seeks them<br />
out, explores their symptoms with them and provides encouragement and advice<br />
about effective treatment and overcoming their anxiety, the nature of anxiety<br />
symptoms can cause therapeutic obstacles. These can include excessive<br />
reassurance-seeking from the mental health professional that, while providing<br />
temporary relief, is reinforcing of this behavior and maladaptive over time;<br />
indecisiveness that may look like procrastination or lack of motivation, but instead<br />
often represents fear of making mistakes or failure; and, most importantly,<br />
avoidant behavior such that patients may appear resistant or non-adherent when<br />
they are choosing avoidance due to excessive fear and anxiety. Also, prominent<br />
symptoms of over-arousal may make it difficult for patients to focus and efficiently<br />
process information during sessions. Symptoms of depression that often<br />
accompany anxiety may also cause difficulties with motivation and initiative and<br />
may need to be distinguished from avoidance.<br />
During the initial contacts, the ACS communicates his or her enthusiasm and<br />
interest in the patient’s well being. Throughout the initial assessment and<br />
psychoeducational session, the patient should begin to understand that the ACS<br />
is someone with whom they will be in ongoing contact. This person will know the<br />
particulars of their situation and can help them access resources in the study and<br />
communicate with the rest of their care team. It is important for the ACS to be<br />
seen as an empathic, trustworthy, knowledgeable and capable advocate who will<br />
work collaboratively with the entire treatment team. Empathy is important in initial<br />
sessions of CBT, but confidence and directiveness become more important<br />
features in later sessions. This stance will facilitate the patient’s adherence to<br />
either medication or CBT treatment when “rough spots” are encountered and<br />
discouragement sets in. The ACS can help the patient stay focused on treatment<br />
goals and support efforts to reach them. Importantly, the ACS will teach skills for<br />
managing distress rather than provide direct reassurance, which only<br />
encourages dependency and relapse.<br />
It is vital to understand each patient’s perspective and how their anxiety<br />
symptoms fit in with their life. Only then can the clinician’s understanding of<br />
anxiety be articulated in a meaningful way so that the patient will become an<br />
active collaborator in treatment. Communications need to be uncomplicated and<br />
non-judgmental. The patient should feel like an active member of the treatment<br />
team with an important role directing treatment. Patient self monitoring of their
23<br />
behaviors is one way of facilitating their input. A biopsychosocial model that<br />
emphasizes the hard-to-control factors of innate genetic vulnerability, along with<br />
the role of psychosocial stressors and coping style (which the patient may have<br />
more control over with help from the ACS and their own self-activation) provides<br />
a useful framework for discussing the diagnosis of anxiety with patients.<br />
Medication and CBT target different aspects of this “cycle of anxiety” but both<br />
ultimately rely on the patient making ongoing life changes.<br />
In discussing anxiety with patients, it is helpful to mention that:<br />
<br />
<br />
<br />
<br />
<br />
<br />
anxiety is common<br />
anxiety can cause or aggravate a wide range of symptoms, including<br />
physical symptoms<br />
anxiety affects the body, behavior and thinking<br />
anxiety is a set of behaviors and ways of thinking that are reinforced over<br />
time, not a character defect or weakness<br />
recovery from anxiety is the rule, not the exception<br />
the good news is that anxiety can almost always be treated with either<br />
medications or CBT (or some combination )<br />
At times, the ACS may find that he or she does not feel as effective with some<br />
patients. The ACS may even become concerned by the patient’s anxiety, and<br />
fail to provide the necessary reinforcement and encouragement to anxious<br />
patients to directly face anxiety provoking situations rather than avoid them. The<br />
ACS will discuss such concerns during the weekly team meeting in order to get<br />
support and avoid any negative outcomes for either the ACS or the patient.<br />
Usually, exploring one’s own reactions with a skilled colleague helps future<br />
patient interactions go more smoothly. Most often the issue in treating anxiety is<br />
the patient’s unwillingness to complete assigned tasks. Rather than view this as<br />
“resistance” the ACS will be taught to conceptualize it as a part of the avoidance<br />
of the anxious syndrome and help the patient think of ways to overcome this<br />
avoidance.<br />
An important issue the ACS must address early on with each patient is the<br />
limitations of what can be done for the patient within the parameters of the<br />
intervention protocol. If there are questions about this, they will be brought up by<br />
the ACS early on in the intervention team meetings and discussed with the<br />
patient.<br />
In working with anxious patients it is crucial to provide the specific focus and<br />
goal-setting that may be difficult for them because of the way anxiety affects their<br />
ability to process information and stay on task. It is therefore important to set the<br />
agenda for each patient visit, focusing on the patient’s anxiety symptoms<br />
(including avoidance), the resolution of which is the goal of treatment, whether<br />
medication or CBT. This means allowing but limiting discussion of other life
24<br />
issues, so that these issues do not become a major focus of meetings, and thus<br />
detract from the CBT.<br />
Working with Ethnic Minority Patients and Those Disadvantaged by Income:<br />
One must always be mindful of patients’ cultural backgrounds. Culture is not<br />
synonymous with ethnic group. Individuals within ethnic groups vary<br />
considerably in their values, identity, and behaviors. One way to think of culture<br />
is the meaning that people give to events and life experiences. Thus, being<br />
familiar with a patient’s cultural beliefs about medicine and mental illness will help<br />
the ACS to communicate effectively with the patient and will increase the<br />
probability that patients will adhere to treatment. When therapists understand<br />
how patients define their symptoms, the salience they give to events, and their<br />
life experiences, they are better able to negotiate an effective treatment plan and<br />
provide quality care. While it is impossible to know all nuances of each culture,<br />
there are overarching themes to keep in mind when working with ethnic minority<br />
and disadvantaged populations. These include distrust of mainstream<br />
organizations and research, mental health stigma, access barriers, perceptions<br />
of mental illness, and acculturation.<br />
Distrust: It can sometimes take a long time to establish a relationship with<br />
disadvantaged and ethnic minority patients, particularly if the ACS is seen as part<br />
of a research project, rather than a treatment team. A common perception is that<br />
research studies recruit disadvantaged individuals to be “guinea pigs” and many<br />
people resist putting themselves in such a position. Also, some ethnic minorities<br />
have been mistreated in medical studies and recruited into studies that ultimately<br />
made incorrect conclusions supporting racial inequality. This mistrust is<br />
especially strong regarding medication use, which may be perceived as a means<br />
to control the patient. Finding ways to articulate and encourage the theme of<br />
patient self-activation serves as one antidote to this perception. Conversely,<br />
sometimes the opposite can happen. That is, because so few individuals have<br />
reached out and offered to help, a disadvantaged individual can sometimes<br />
expect more than can be realistically delivered. Therefore, the ACS must set<br />
clear and realistic expectations from the beginning of treatment so that the<br />
patient does not feel betrayed or short-changed.<br />
Stigma: For many, seeking mental health treatment in the general medical<br />
setting is safer than attending a specialty mental health clinic. It is important to<br />
discuss with patients their beliefs and attitudes about anxiety and any fears they<br />
may have about people in their community finding out they are in treatment for<br />
anxiety. It is likely that psychoeducation will help to dispel misconceptions about<br />
mental health treatment and will orient patients to psychotherapy and medication<br />
approaches. While some of the cultural stigma around treatment for mental and<br />
emotional problems may be counteracted by use of psychoeducational materials,<br />
these materials may have to be reviewed in the sessions if patients are unwilling<br />
to bring them home because of a concern that these materials will be found by
25<br />
family or friends. The ACS should seek to personalize psychoeducational<br />
material and the intervention.<br />
Access Barriers: Many disadvantaged patients may have difficulty making<br />
regular appointments because of the many demands on their time (e.g.,<br />
responsibility for child care) and the unavailability of resources such as childcare<br />
and transportation. The treatment sessions may be viewed as just one more in<br />
an endless series of stressors and obstacles they must overcome in their daily<br />
life. Cost of care is also a crucial issue and should prompt careful consideration<br />
of ongoing medication expenses and the availability of cheaper, generic forms.<br />
When patients present with competing and complex demands, it will be important<br />
to offer them compelling reasons to support their treatment participation. For<br />
example, treatment for anxiety may enable them to develop better coping skills,<br />
allow them to be a stronger support for their family, and improve their overall<br />
quality of life. Patients may need frequent encouragement and praise for their<br />
efforts to adhere to treatment in spite of many competing demands. For<br />
individuals with strong family ties and a predominant focus on the family (e.g.,<br />
Latina women), the ACS may emphasize that helping themselves will in turn help<br />
the family.<br />
Cultural Beliefs: An understanding of a patient’s clinical presentation in the<br />
context of his/her cultural and/or religious background may have important<br />
implications for diagnosis, adherence and treatment outcome. For example,<br />
some Latinos may explain their anxious symptomatology using cultural idioms of<br />
distress such as “ataques de nervios” (includes symptoms such as<br />
uncontrollable shouting, attacks of crying, trembling, heat in chest rising into<br />
head, aggression, being out of control, dissociative experiences, fainting, suicidal<br />
gestures, etc.) and “nervios” (includes symptoms such as headaches, irritability,<br />
stomach disturbances, sleep difficulties, nervousness, easy tearfulness, inability<br />
to concentrate, trembling, tingling sensations, dizziness with occasional vertigolike<br />
symptoms). In such instances, these symptoms may fall within a normal<br />
range of distress relative to the norms of their cultural group; however, in other<br />
cases, their symptoms may extend beyond normative levels of severity and<br />
signify the presence of an anxiety, mood, and/or somatoform disorders. Similarly,<br />
some individuals may emphasize the importance of spiritual issues when<br />
explaining their distress (e.g., anxiety and depression may be attributed to a<br />
spiritual crisis). Acknowledging the significance of the belief system and<br />
integrating it into overall conceptualizations may foster provider-patient trust and<br />
better clinical care.<br />
Acculturation: Patients less acculturated to mainstream American society may<br />
be particularly unfamiliar with the process of seeking mental health treatment.<br />
These individuals may be more likely to experience problems with access and<br />
stigma related barriers to treatment. Simultaneously, individuals may be exposed<br />
to numerous acculturative stressors including the immigration process itself,<br />
intergenerational conflicts, unemployment, discrimination, and alienation that
26<br />
may contribute to anxiety in their lives. Less acculturated patients may need<br />
more education about the treatment process itself as well as the logistics of<br />
receiving treatment.<br />
Working with Family Members and Significant Others:<br />
In most cases, it will be helpful for the ACS to involve family members or<br />
significant others in the treatment of the anxious patient. The ACS should always<br />
discuss with the patient how family members and significant others will feel about<br />
the diagnosis of anxiety and any proposed treatments. The ACS may encourage<br />
the patient to share educational materials or the videotape with significant others<br />
or suggest to talk or meet with important family members to educate them about<br />
anxiety and to ask them to support the patient’s treatment plan. This could<br />
include help with adherence to medications or perhaps plans made during CBT<br />
treatment, such as the help of significant others as coaches or facilitators during<br />
in vivo exposure to anxiety producing situations, as long as it does not enhance<br />
dependency on the significant other. Involvement of significant others in aspects<br />
of behavioral health has also been shown to increase attendance
27<br />
5. INITIAL PATIENT CONTACT: SETTING THE STAGE<br />
Patients will either be referred to the study by their PCP, or “self-referred” with<br />
the agreement of their PCP, as would be done in usual practice. The patient is<br />
then interviewed by the ACS to determine eligibility for the study. This interview<br />
(which includes the MINI diagnostic interview) will take place either in the clinic,<br />
possibly at the same visit (if the patient has time) or over the phone in the next<br />
few days. The ACS should make every effort to meet the patient in person in the<br />
clinic, if only to arrange to contact him or her by telephone. Following the<br />
completion of this initial eligibility assessment, the patient (if eligible) is assessed<br />
by the phone interviewers at RAND to assess baseline clinical status and to be<br />
randomized to the intervention or treatment as usual. If the patient is assigned to<br />
the intervention, the ACS will re-contact the patient by telephone to arrange an<br />
initial visit at the primary care clinic. The goals of this initial call/contact are as<br />
follows:<br />
1. Arrange for a scheduled appointment<br />
2. Answer any questions or concerns the patient may have at this point.<br />
INITIAL VISIT WITH ANXIETY CLINICAL SPECIALIST (ACS) – (USUALLY WEEK 1)<br />
This visit will focus on initial clinical assessment, patient education about various<br />
treatment options, and discussion of initial treatment plans. The visit is also<br />
designed to increase the patient’s motivation and commitment to treatment.<br />
Goals:<br />
The goal of the first visit with the patient is to: establish a working alliance,<br />
restate their principal anxiety problem and place it in his or her unique medical<br />
and psychosocial context; identify and strategize about perceived barriers to<br />
receiving treatment; educate about CBT and medication so that he or she can<br />
make an informed choice and be more prepared for treatment; increase<br />
motivation and readiness to change;and provide information to enhance outcome<br />
and self efficacy expectancies for treatment.<br />
This is to be a collaborative process during which the ACS and patient discuss<br />
issues together. The ACS should refrain from providing information outside the<br />
domain of anxiety and depression and their symptoms and treatment. However,<br />
in some instances, present concerns of the patient are so pressing that it would<br />
hinder the therapeutic alliance were the ACS not to address these concerns. In<br />
such instances, the ACS may briefly divert from the anxiety and depressionfocused<br />
treatment to provide support and guidance about other prevailing life<br />
concerns. Every effort should be made to get back on track with treatment within<br />
the same session, ideally by discussing the patient’s anxiety/depression and/or<br />
decisions about treatment modality in the context of these current concerns.
28<br />
Summary Statement:<br />
The ACS begins by asking patients to provide a description of their presenting<br />
problems; the ACS reflects what the patient is saying and responds with<br />
empathy. Then the ACS provides feedback of the results from the baseline<br />
assessment to the patient, avoiding psychological jargon and stigmatizing<br />
language as much as possible. This includes a brief review of the current<br />
symptoms and symptom complexes (disorders) that the patient has endorsed on<br />
the MINI diagnostic interview and asking the patient whether he or she feels that<br />
his or her problems have been captured accurately. In addition to reviewing<br />
symptoms, the ACS reviews the patient’s history of prior anxiety or depression<br />
episodes, prior treatment history, co-existing medical or social problems that may<br />
serve as stressors that exacerbate anxiety, difficulties with social, personal,<br />
family, or work functioning, and availability of social supports. Finally, the ACS<br />
provides a summary statement of the patient’s concerns, which includes the<br />
principal anxiety symptoms that are most troubling to them, how they are<br />
affecting or restricting important activities and functions, how these symptoms<br />
might be aggravated by recent life stressors (e.g. losses, separations, life<br />
changes, financial pressures, or medical problems), and which family or friends<br />
are available to help support the patient in their treatment and in their drive to<br />
gain more self-control and take an active role in their recovery. During this<br />
process, the ACS should de-stigmatize diagnoses as much as possible and<br />
provide an accurate message of hope for recovery. The stance of the ACS<br />
should be to develop as much discrepancy as possible between the patient’s life<br />
as it currently is (with high anxiety) and the life that they would like to have (with<br />
lowered anxiety) in order to help maximize readiness to change and engagement<br />
in treatment. Helpful techniques to utilize in this portion of the session include:<br />
Express Empathy: Here, the ACS seeks to communicate respect for the<br />
client, with a style that is a blend of “supportive companion” and<br />
“knowledgeable consultant”. Persuasion should be gentle, subtle, and<br />
carried out with the assumption that it is only the client who can decide to<br />
change and affect change.<br />
Develop Discrepancy: During the discussion of the MINI and other<br />
anxiety scores, the ACS should seek to enhance the patient’s perception<br />
of the discrepancy between “where they are and where they want to be”.<br />
Avoid Argumentation: Since argumentation and direct confrontation<br />
tend to increase resistance and decrease readiness to change, the ACS<br />
here does not make any attempt to force the patient to accept or admit a<br />
diagnostic label, prove, or convince the patient of anything. Instead, the<br />
ACS seeks to help the patient accurately view the consequences of living<br />
with high anxiety (and avoidance). The goal is for the patient to begin<br />
voicing the arguments for change themselves, rather than the ACS.<br />
Roll with Resistance: The key point here is that ambivalence about<br />
change is viewed as normal, not pathological, and to be explored openly.<br />
The ACS will invite (but not impose) new ways of thinking about<br />
problems and how to solve them, and seek to evoke solutions from the<br />
patient. Techniques might include simple reflection, reflection with
29<br />
<br />
amplification, double-sided reflection, shifting focus, and “rolling<br />
with”.<br />
Support Self-Efficacy: Maximum motivation and commitment to change<br />
require a specific belief on the part of the patient that he or she can<br />
change their anxiety problems. Eliciting statements that reflect selfefficacy<br />
and describing the kind of things that successful people do in<br />
treatments for anxiety (and that the client can do them) will help increase<br />
a sense of self-efficacy. Once the client chooses a treatment option,<br />
summarizing the reasons for their choice and highlighting any efficacy<br />
suggested in the decision making process is also a good idea.<br />
Comment [s1]: These techniques are<br />
all covered in the MET manual which is<br />
free on the web and not very long. I am<br />
thinking it might be a good reading to<br />
assign. Pretty simple concepts I think and<br />
can be read in about an hour. If you like<br />
the amount of detail I’ve added here, we<br />
could just add a footnote here saying that<br />
these come from the MET manual and<br />
cite it. ---Stacy<br />
Perceived Barriers to Mental Health Treatment:<br />
Next, the ACS discusses with the patient their past and current impressions of<br />
and perceived barriers to treatment for anxiety. To facilitate this, the ACS and<br />
patient will review a perceived barriers checklist that will include the following<br />
items:<br />
1. Logistical<br />
i. time<br />
ii. child/elder care<br />
iii. transportation, travel<br />
iv. scheduling<br />
2. Social<br />
i. privacy/confidentiality<br />
ii. family/significant others objection to treatment<br />
iii. embarrassment or fear of what others would think<br />
3. Psychological<br />
i. beliefs about treatment<br />
ii. adverse personal treatment experiences<br />
iii. adverse prior treatment experiences of family or friend<br />
4. Cultural<br />
5. Other patient-specific barriers or concerns<br />
Comment [s2]: My suggestion would<br />
be to do this after they have seen the<br />
video and have a sense of whether they<br />
will choose CBT or meds. That way, the<br />
discussion might be a bit more focused to<br />
the actual pros and cons of doing the<br />
treatment they will do and serve to further<br />
increase motivation and commitment to<br />
change<br />
Barriers pertaining to financial cost and access as they pertain to the use of<br />
medications will also be considered (e.g. use of medication samples for patients<br />
with limited funds of high medication co-pays).<br />
The ACS will discuss with patients the nature of their perceived barriers,<br />
especially in relation to prior experiences, and brainstorm with the patient<br />
potential ways of dealing with them. For issues of daycare or transportation,<br />
consideration will be given to community resources or the involvement of family<br />
or friends as support mechanisms. For social stigma, consideration will be given<br />
to ways of discussing or not discussing their problem and their treatment with<br />
others, and ways of handling time away from work or family in order to attend<br />
treatment sessions.
30<br />
In addition, the ACS will engage patient in a discussion about their beliefs about<br />
therapy and medication. Beliefs about treatment efficacy are particularly<br />
important to address given our previous finding that beliefs predict treatment<br />
attendance. The goal of the discussion is to correct overly negative or mistaken<br />
beliefs about the therapy process, and give information about the treatment,<br />
thereby increasing the patient’s outcome expectancies. The other goal is to<br />
continue to try to help the patient weigh the balance between the “cost” of<br />
change vs. the “cost” of living with high levels of anxiety, and help tip the balance<br />
in favor of change by highlighting the discrepancy between where the patient is<br />
and where they want to be.<br />
EDUCATION ABOUT TREATMENT<br />
This section is designed to provide patients with sufficient detail about CBT and<br />
medications for anxiety disorders so that they can make an informed treatment<br />
decision. In addition, the information is intended to prepare patients for engaging<br />
in treatment by familiarizing them with the treatment process, correcting<br />
treatment myths, and enhancing patients’ expectations for positive outcomes and<br />
their self-efficacy for being able to complete treatment.<br />
[Present the following information in a discussion format, encouraging the patient<br />
to ask questions throughout, and addressing the negative beliefs that they<br />
endorsed on the Beliefs Questionnaires.]<br />
A) Cognitive Behavioral Therapy<br />
Cognitive Behavioral Therapy provides a set of skills for dealing with<br />
excessive anxiety. These skills are learned during sessions with me and are<br />
practiced between sessions. First, you’ll learn all about anxiety and anxiety<br />
symptoms so that you understand more about what is happening to you, how<br />
your anxiety developed, and what is maintaining it over time Second, skills are<br />
taught for replacing overly negative or anxious thoughts and ruminations (i.e., the<br />
things people “think” to themselves in certain situations) with more realistic<br />
thoughts. This is important because how anxious we feel is closely tied to what<br />
we tell ourselves and what we think about. In addition, CBT teaches ways of<br />
shifting attention onto things that need to get done and away from excessive<br />
worrying. Third, CBT teaches ways of directly facing places, people, or things<br />
that are anxiety-inducing. This builds a sense of control. This is called exposure<br />
therapy, and it is done in a gradual way so that you build confidence with each<br />
step.<br />
Because CBT is a learning process, the positive effects last after the CBT<br />
sessions are over. In fact CBT has been demonstrated to be a very effective<br />
treatment for anxiety disorders in many different studies with many different types<br />
of people. Between 70 and 90% of people who complete CBT make significant<br />
improvements in their lives and are significantly less anxious. It seems that the<br />
best results come from being fully committed to the learning and the exercises –<br />
Comment [s3]: I wonder about<br />
writing this in a more conversational style<br />
so that the ACS might be more likely to<br />
follow it more uniformly? Let me know<br />
what you think and if you agree I’ll revise<br />
a bit more. SSW
31<br />
the more you practice, the better the results. However, it does take effort and<br />
CBT needs to be a priority for it to work. That is, it is not a good choice to do CBT<br />
half-heartedly.<br />
Usually, CBT lasts anywhere from 4 to 12 sessions. In this program, we<br />
will be offering 6 initial sessions of CBT. In most studies, the positive effects start<br />
to appear after about four sessions. This means meeting with me here at the<br />
clinic about once per week, about 45 minutes each time, for up to 6 times. Each<br />
time we would talk a little about how you were feeling. Then, I would show you<br />
the skills and we would practice them together and then you would practice them<br />
on your own. Also, I would give you a workbook that summarizes everything you<br />
are learning with me, and copies of the audiotapes of our sessions (OR ACCESS<br />
VIA COMPUTER OR CD) so that you can refer to the information whenever you<br />
want.<br />
At this point the patient can either view a short video tape segment<br />
demonstrating a therapist talking with a patient about their cognitions or their<br />
behaviors or, as a way of demonstrating the treatment, the ACS can take an<br />
example of a situation that the patient avoids and briefly describe how exposure<br />
therapy would be arranged for that avoidance.<br />
The ACS should then ask the patient if he or she has questions about CBT, its<br />
effectiveness or what is involved in making it work.<br />
B) Medications<br />
Medications decrease panic and anxiety by changing the availability of<br />
neurotransmitters within or between nerve cells. This initial effect initiates many<br />
other effects in the brain as the brain adjusts to these neurotransmitter changes.<br />
This process of adjustment often takes several weeks, which is why medications<br />
usually don’t work immediately. During this adjustment the brain “rebalances”<br />
itself. Therefore medication is not giving your brain something extra it lacks, or<br />
taking away something it has too much of. Rather, it is helping your brain work<br />
more efficiently doing the job it has to do of combating stress. Imagine that the<br />
brain has a stress thermostat that keeps it in balance as different stresses impact<br />
on it, just like a thermostat keeps a room at the same temperature despite<br />
changes in the outside temperature. <strong>Anxiety</strong> may occur when the set point that<br />
sets the ideal stress level (or temperature) gets moved too high or too low. The<br />
process of rebalancing moves the set point back to the middle so that the brain<br />
can work much like before.<br />
Medications are highly effective for anxiety problems, with many studies<br />
across many different types of people showing that anywhere from 70 to 90% of<br />
those who complete the medication treatment have significant improvements in<br />
their lives and significant reductions in their anxiety. The positive effects usually<br />
begin to appear after four to six weeks. However, medications are not very<br />
effective if they are not taken at the right dose, are not taken in a consistent<br />
manner, or are discontinued too soon. Typically, medications are prescribed for
32<br />
the duration of at least a year. Sometimes relapse can happen once the<br />
medications are withdrawn, but this is much less of a problem if the withdrawal is<br />
done carefully under supervision and if you learn other ways of coping with stress<br />
and anxiety.<br />
If you elect to take medications, I would meet with you weekly for the first<br />
two weeks and then at two to four week intervals after this, depending on how<br />
you are responding to the medication. We might also substitute telephone<br />
sessions for meetings depending on your preference as well as on how much we<br />
need to cover in the sessions, which will depend in large part on how you are<br />
responding. The purpose of the meetings is to make sure you are responding<br />
positively to the medications (i.e. that your symptoms are improving) and that any<br />
side-effects you experience can be eliminated by adjusting the medications.<br />
At this point the ACS asks the patient questions regarding medications and their<br />
previous history with medication such as which ones have been used, whether<br />
they were effective, and the side effects. Side effects are addressed by<br />
describing them as normal bodily adjustments to medications, which are not<br />
dangerous.<br />
SELF EFFICACY AND OUTCOME EXPECTANCIES<br />
At this point the patient rates on 0-8 point scales the degree of positive outcome<br />
expectancy and self-efficacy (their conviction in their own ability to carry out the<br />
treatment) for CBT as well as for medication (see below). Any scores lower than<br />
8 provide the opportunity to ask “Why is the rating not an 8? What contributes to<br />
that lower rating?” Responses will provide an opportunity for the ACS to correct<br />
any misinterpretations or myths. For example, patients may believe that their<br />
long-standing anxiety symptoms are not treatable, that their anxiety represents a<br />
personality trait that cannot be changed, or that because past treatments did not<br />
work, new treatments will not work. The ACS will address these issues in a<br />
realistic fashion. These ratings will be repeated at every ACS session.<br />
Outcome expectancy:<br />
How likely is it that your anxiety can be successfully treated?<br />
0----------1----------2----------3----------4----------5----------6----------7----------8<br />
Not at Possibly 50/50 Very Likely Certainly<br />
All<br />
Self-efficacy expectancy:<br />
How likely is it you can do what is necessary to make anxiety treatment<br />
successful?<br />
0----------1----------2----------3----------4----------5----------6----------7----------8
33<br />
Not at Possibly 50/50 Very Likely Certainly<br />
All<br />
Choice:<br />
The patient will then be asked to make a decision about which treatment they<br />
would prefer or be given more education materials (brochures and videos) to<br />
consider and then return to the ACS with their decision. The patient will be<br />
encouraged to choose one modality initially, although patients strongly<br />
desiring both treatments will be accommodated.<br />
At the end of the visit, the ACS will complete an Initial Visit Worksheet and<br />
consult with the patient’s primary care provider about the initial treatment plan,<br />
ideally on the day of the initial visit but not later than 2 days after the initial visit.<br />
After the conclusion of the session, the ACS will send a handwritten letter to<br />
increase probability of return. Anecdotally these can be extremely helpful in<br />
reducing early dropout. The following is an example.<br />
“Dear Mr. X:<br />
This is just a note to say that I’m glad you came in today. I agree with you that<br />
there are some serious concerns for you to deal with, and I appreciate how<br />
openly you are exploring them. You are already seeing some ways in which you<br />
might make a healthy change, and (your wife seems very caring and willing to<br />
help – if appropriate and an SO has been discussed). I think that together you (if<br />
referring to spouse) or we (if ACS and patient) will be able to find a way through<br />
these problems. I look forward to seeing you again on Tuesday the 24 th at 2:00.<br />
Sincerely, ACS
34<br />
6. COURSE OF TREATMENT-FOCUS ON STEP 1<br />
Overview:<br />
Because patients will enter the study at different stages of treatment, the general<br />
procedure outlined below will not apply to all cases. The following describes the<br />
‘typical’ course for a newly diagnosed patient with one of the four anxiety<br />
disorders, who is not in active treatment at the initial visit. Patients who are<br />
already part-way into Step 1 treatments (i.e., antidepressant medication or CBT)<br />
at the time of the initial visit will usually continue to complete Step 1 unless the<br />
current treatment is poorly tolerated (this will most often apply to medications<br />
rather than CBT, although conceivably a patient may be receiving CBT and not<br />
responding well). Patients who enter after having recently completed what<br />
appears to be good quality step one treatment will be discussed in the team<br />
meeting with the team psychiatrist and may enter at Step 2. The majority of<br />
patients, however, will enter at Step 1.<br />
Pharmacotherapy:<br />
If the patient and the PCP decide to start with medications, the PCP will write a<br />
prescription after consulting the medication algorithm provided to them. The<br />
prescription should occur as close as possible to the initial ACS patient visit; in<br />
some cases that PCP may already have written the prescription when first seeing<br />
and identifying the patient, prior to randomization. After initiating medication<br />
treatment, the ACS will have phone contact with the patient within one week to<br />
make sure the prescription has been filled and the patient is not experiencing any<br />
side effects that might lead to early treatment dropout. A guideline on how to<br />
manage medication side effects is provided in the previous section on steppedcare.<br />
The ACS will then have weekly contact with the patient during the initial acute<br />
treatment phase, and may then decrease to contact every two to four weeks<br />
depending on the patient’s progress. A guideline for routine contact might be<br />
weeks 1, 2, 4, 8, and 12. These contacts can be in person or by telephone as<br />
clinically indicated. Especially for the early contacts, in person visits are generally<br />
recommended. Early contacts will focus on the recognition and management of<br />
early treatment side effects and the possibility of worsening anxiety symptoms.<br />
Regulation of health habits (sleep, diet, exercise, behavioral activity) will also be<br />
recommended to facilitate adjustment to both medication and symptoms. Later<br />
follow-up contacts will focus on adherence to ongoing treatment, progress in<br />
anxiety symptom reduction and continued improvement in health habits.<br />
During each follow-up contact, the ACS will assess the patient’s anxiety and<br />
depression symptoms using a set of rating forms that can be completed by the<br />
patient in 2-3 minutes in the waiting room before a visit and scored by the ACS at<br />
the start of each session. These rating forms are shown below. Review of the
35<br />
rating scales often provides a good opportunity to start a discussion of changes<br />
in the patient’s symptoms. In addition, at the start of each session the ACS will<br />
monitor the patient’s perceived self-efficacy and outcome expectancy for<br />
treatment success in order to address recurring barriers to treatment<br />
involvement. Decisions about changes in treatment, based on these ratings, will<br />
be made with the consulting psychiatrist at regular team meetings.<br />
Overall <strong>Anxiety</strong> Severity and Impairment Scale (OASIS)<br />
The following items ask about anxiety and fear. For each item, circle the number for the answer that best<br />
describes your experience over the past week.<br />
1. In the past week, how often have you felt anxious?<br />
0 = No anxiety in the past week.<br />
1 = Infrequent anxiety. Felt anxious a few times.<br />
2 = Occasional anxiety. Felt anxious as much of the time as not. It was hard to relax.<br />
3 = Frequent anxiety. Felt anxious most of the time. It was very difficult to relax.<br />
4 = Constant anxiety. Felt anxious all of the time and never really relaxed.<br />
2. In the past week, when you have felt anxious, how intense or severe was your anxiety?<br />
0 = Little or None: <strong>Anxiety</strong> was absent or barely noticeable.<br />
1 = Mild: <strong>Anxiety</strong> was at a low level. It was possible to relax when I tried. Physical symptoms were<br />
only slightly uncomfortable.<br />
2 = Moderate: <strong>Anxiety</strong> was distressing at times. It was hard to relax or concentrate, but I could do it<br />
if I tried. Physical symptoms were uncomfortable.<br />
3 = Severe: <strong>Anxiety</strong> was intense much of the time. It was very difficult to relax or focus on anything<br />
else. Physical symptoms were extremely uncomfortable.<br />
4 = Extreme: <strong>Anxiety</strong> was overwhelming. It was impossible to relax at all. Physical symptoms were<br />
unbearable.<br />
3. In the past week, how often did you avoid situations, places, objects, or activities because of<br />
anxiety or fear?<br />
0 = None: I do not avoid places, situations, activities, or things because of fear.<br />
1 = Infrequent: I avoid something once in a while, but will usually face the situation or confront the<br />
object. My lifestyle is not affected.<br />
2 = Occasional: I have some fear of certain situations, places, or objects, but it is still manageable. My<br />
lifestyle has only changed in minor ways. I always or almost always avoid the things I fear when<br />
I’m alone, but can handle them if someone comes with me.<br />
3 = Frequent: I have considerable fear and really try to avoid the things that frighten me. I have made<br />
significant changes in my life style to avoid the object, situation, activity, or place.<br />
4 = All the Time: Avoiding objects, situations, activities, or places has taken over my life. My lifestyle<br />
has been extensively affected and I no longer do things that I used to enjoy.<br />
4. In the past week, how much did your anxiety interfere with your ability to do the things you needed to<br />
do at work, at school, or at home?<br />
0 = None: No interference at work/home/school from anxiety<br />
1 = Mild: My anxiety has caused some interference at work/home/school. Things are more difficult,<br />
but everything that needs to be done is still getting done.<br />
2 = Moderate: My anxiety definitely interferes with tasks. Most things are still getting done, but few<br />
things are being done as well as in the past.
36<br />
3 = Severe: My anxiety has really changed my ability to get things done. Some tasks are still being<br />
done, but many things are not. My performance has definitely suffered.<br />
4 = Extreme: My anxiety has become incapacitating. I am unable to complete tasks and have had to<br />
leave school, have quit or been fired from my job, or have been unable to complete tasks at home<br />
and have faced consequences like bill collectors, eviction, etc.<br />
5. In the past week, how much has anxiety interfered with your social life and relationships?<br />
0 = None: My anxiety doesn’t affect my relationships.<br />
1 = Mild: My anxiety slightly interferes with my relationships. Some of my friendships and other<br />
relationships have suffered, but, overall, my social life is still fulfilling<br />
2 = Moderate: I have experienced some interference with my social life, but I still have a few close<br />
relationships. I don’t spend as much time with others as in the past, but I still socialize<br />
sometimes.<br />
3 = Severe: My friendships and other relationships have suffered a lot because of anxiety. I do not<br />
enjoy social activities. I socialize very little.<br />
4 = Extreme: My anxiety has completely disrupted my social activities. All of my relationships<br />
have suffered or ended. My family life is extremely strained.<br />
PHQ 3<br />
Over the last two weeks, how often have you been bothered by any of the following problems?<br />
Not at all Several days More than half the days Nearly every day<br />
0 1 2 3<br />
1. Little interest or pleasure in doing things<br />
2. Feeling down, depressed, or hopeless<br />
3. Feeling tired or having little energy<br />
Outcome expectancy:<br />
How likely is it that your anxiety can be successfully treated?<br />
0----------1----------2----------3----------4----------5----------6----------7----------8<br />
Not at Possibly 50/50 Very Likely Certainly<br />
All<br />
Self-efficacy expectancy:<br />
How likely is it you will be able to do what is necessary to make anxiety treatment successful?<br />
0----------1----------2----------3----------4----------5----------6----------7----------8<br />
Not at Possibly 50/50 Very Likely Certainly<br />
All<br />
The ACS will document all follow-up contacts on the Web-based systems and a<br />
printout of this document can be shared with the PCP, and placed in the patient’s<br />
primary care chart at the discretion of the PCP. Patients who participate in the<br />
study will have provided consent for sharing this health-related information with<br />
their PCP.
37<br />
In most cases, the 2-week follow-up contact will be in-person with the ACS, but<br />
subsequent follow-ups can be conducted by telephone if the ACS feels this is<br />
clinically reasonable and the patient prefers this.<br />
CBT:<br />
If the patient and the PCP decide to start with a trial of CBT, the ACS will<br />
schedule the patient for his or her initial session at the primary care clinic.<br />
Patients started in CBT as the first line of treatment will be seen for up to 6<br />
sessions by the ACS in the clinic (see CBT manual). These sessions will usually<br />
be scheduled weekly but not less frequently than every other week. As with<br />
pharmacotherapy, each session will begin with an assessment of (1) patient<br />
symptom status using the symptom ratings and (2) patient self-efficacy and<br />
outcome efficacy to assess barriers to treatment engagement. The content of<br />
the CBT sessions is outlined in detail in the CBT treatment manual.<br />
General Treatment Issues:<br />
The ACS consults with the patient’s PCP and the study psychiatrist or<br />
psychologist as needed if the patient is experiencing symptoms or problems not<br />
easily addressed by the ACS. The patient may require additional PCP visits if<br />
such problems are not easily resolved by the ACS. Many patients will have a<br />
visit with their PCP at week 4. If the patient is doing well and this visit can be<br />
easily accomplished by the ACS, the patient and PCP may decide to skip this<br />
visit. The ACS will inform the PCP (using the PCP’s preferred method of<br />
communication, e.g., e-mail, fax, letter) of the patient’s progress and to prompt<br />
the PCP to reinforce certain key steps in the patient’s treatment during the<br />
primary care visit.<br />
If at any time patient attendance or interest wanes, as indicated by lack of<br />
attendance, or lack of completion of assignments in the case of CBT, or lowered<br />
expectancy ratings on the scales of self-efficacy and outcome expectancy, the<br />
reasons for the decreased engagement will be addressed. Sometimes this may<br />
require a phone call to the patient who is not attending sessions expressly to<br />
brainstorm perceived barriers to attending treatment. The ACS will re-assess for:<br />
<br />
<br />
<br />
<br />
New or ongoing barriers to treatment (e.g., scheduling issues, family<br />
issues)<br />
Negative reactions to the treatment (e.g., side effects,<br />
unpleasant emotions, disparities between initial expectations and<br />
process of treatment thus far) and consideration of ways of managing<br />
these issues<br />
Negative outcome expectancies (e.g., judging that treatment will not<br />
work) and consideration of the evidence<br />
Negative self-efficacy (e.g., judging that they cannot carry out the<br />
treatment) and consideration of ways of building self-efficacy through<br />
designing smaller tasks to be accomplished
38<br />
In each case, the ACS and patient will problem solve so that treatment<br />
engagement is renewed.<br />
The ACS will immediately contact and consult with the PCP (and the team<br />
psychiatrist as needed) if the patient develops any of the following serious<br />
problems:<br />
<br />
<br />
<br />
<br />
<br />
acute suicidal symptoms<br />
psychotic symptoms<br />
manic symptoms<br />
suspected alcohol or drug abuse or dependence (including prescription<br />
medications)<br />
side-effects that are especially bothersome to the patient and are felt to<br />
compromise the patient’s health and/or their continuation in treatment.<br />
In order not to unduly overburden the PCP with side-effect concerns,<br />
the ACS may first consult with the study psychiatrist to see if an<br />
immediate call to the PCP is warranted.<br />
An outline of a general approach to the evaluation and treatment of<br />
psychiatric emergencies such as acute suicidality can be found in the<br />
appendix of this manual. Each clinical team will adapt this approach to<br />
their clinic needs and operations. This plan starts with an evaluation by the<br />
ACS or the study psychiatrist whenever possible but must also be integrated with<br />
the response mechanisms for psychiatric emergencies generally available in<br />
each system of care. It is especially important to assure coverage during times<br />
when the ACS or study psychiatrist is not immediately available (although it<br />
should be noted that a study psychiatrist will always be “on-call” by pager), and to<br />
ensure that treatment plans for psychiatric emergencies involve the regular<br />
treatment team whenever possible.<br />
Assessment of initial treatment course – (usually week 12)<br />
All patients will have a visit with the ACS and primary care provider about 12<br />
weeks after enrollment. This assessment can occur a bit earlier IF the patient<br />
entered treatment mid-way through step 1 (i.e., patients enters and has already<br />
been on an adequate dose of an antidepressant for 4 weeks). The purpose of<br />
this contact is to formally assess response to the initial course of treatment. The<br />
OASIS and PHQ-3 will be used to assess status and change. Patients who<br />
achieve remission, defined as a total score of 8 or less on the OASIS and a score<br />
of 5 or less on the PHQ-3 will go on to maintenance treatment.<br />
Patients who have not achieved remission to the first line of treatment will be<br />
discussed in the weekly team meeting and will likely be seen for a consultation<br />
by the study psychiatrist. After this consultation, the ACS will decide with the<br />
patient’s PCP and the patient on subsequent treatment following the guidelines<br />
provided by the stepped care model above. These patients will ordinarily enter
39<br />
the next step, unless the patient expresses good satisfaction with his/her level of<br />
symptom control and functioning, and expresses a desire to maintain the current<br />
treatment. In these circumstances (obviously this will involve only those patients<br />
who have clearly had SOME response to treatment indicated by measurable<br />
reduction in ratings on the OASIS items and the in PHQ-3 scores), the patient will<br />
be considered to have had a very good to excellent response and will enter<br />
maintenance treatment.<br />
MAINTENANCE TREATMENT<br />
Patients who have had a very good to excellent treatment response will meet<br />
with the ACS to complete a Relapse Prevention Plan (these plans can be found<br />
in the WEB-based system). They will be followed by the ACS with monthly<br />
telephone calls, and will be encouraged to call their PCP or the ACS if symptoms<br />
of anxiety return or if they have questions regarding treatment. All patients are<br />
encouraged to stay on continuation treatment (either full dose of the<br />
antidepressant that led to clinical response or monthly maintenance CBT) for the<br />
duration of the year-long intervention phase. Patients at high risk for relapse will<br />
be identified by enumerating the presence of known risk factors, which include:<br />
multiple anxiety disorders, co-morbid depression, co-morbid personality disorder,<br />
ongoing chronic psychosocial stress or medical illness or failure to respond to<br />
first step treatment. Those with the presence of one or more of these are<br />
encouraged to continue maintenance treatments for at least 2 years. Patients<br />
showing signs of recurrence or relapse during this follow-up period will be<br />
discussed in the clinical team meeting and may be scheduled for additional<br />
follow-up visits with the PCP or the ACS as clinically indicated.<br />
Patients entering the study on active treatments (i.e., patients who have recently<br />
been started on an antidepressant) may not follow this exact timeline. They will<br />
also complete the initial assessment and treatment planning session with the<br />
ACS, and they will be closely followed by the ACS (i.e., weekly phone or in<br />
person contacts as needed) until they are in remission from the anxiety<br />
symptoms. The timing of other follow-up contacts with the ACS, the PCP, or the<br />
study psychiatrist may vary depending on the patient’s progress in treatment.<br />
For example, a patient entering the study who appears to have failed a good trial<br />
of a first or second line medication treatment in primary care, and is uninterested<br />
in pursuing CBT, may have a psychiatric consultation earlier in the course of<br />
treatment (i.e., in weeks 1-2).<br />
Termination<br />
The ACS will follow each intervention patient for one year. At the end of the oneyear<br />
follow-up period, the ACS will meet with the patient and PCP to transition<br />
the care of the patient back to the PCP. At this point, the treatment team may<br />
make additional recommendations for ongoing treatment and provide referrals to<br />
other resources that may be helpful in the patient’s ongoing treatment.
Termination can evoke feelings of sadness, fear, or uncertainty in patients and<br />
providers. A clear termination, however, can be an essential phase of the<br />
therepeutic relationship. Termination signals that the study goals have been<br />
reached, but more importantly, offers the opportunity to review the improvements<br />
a patient has made, to identify what has and has not helped, and finally to<br />
discuss future goals and plans for achieving them. Arrangements for transitions<br />
are reviewed, and any feelings or concerns related to termination can be<br />
addressed. An ACS who anticipates difficulties with termination should discuss<br />
these with the patient’s PCP and the treatment team in order to prevent negative<br />
outcomes for either the patient or the ACS.<br />
40
41<br />
7. PSYCHOPHARMACOLOGY STEPPED CARE APPROACH<br />
Initial Treatment Choice: Medication<br />
For those choosing pharmacotherapy, selection of initial medication will be the<br />
first and most important task. Medication selection guidelines are based on the<br />
premise that, for pharmacologic treatment purposes, there are more similarities<br />
than differences among the four anxiety disorders (PD, GAD, SAD, and PTSD).<br />
For example, based on randomized controlled trials (RCTs), selective serotonin<br />
reuptake inhibitors (SSRIs) and venlafaxine extended-release are efficacious for<br />
all four disorders; benzodiazepines are efficacious for Panic Disorder, GAD and<br />
SAD (but probably not for PTSD, though rigorous RCTs are lacking).<br />
Selection of medication depends on whether patients have received prior<br />
pharmacotherapy for the treatment of a mood and anxiety disorder. An SSRI is<br />
the treatment of choice for patients who have never received prior<br />
pharmacotherapy (and do not have a history strongly suggestive of bipolar<br />
disorder). In addition to treating any of the four anxiety disorders, SSRIs will both<br />
treat the frequent presence of comorbid MDD and lower the risk of future MDD<br />
episodes. Exceptions would be a history of serious adverse events<br />
(including allergic reactions) from an SSRI, or failure to respond to what is<br />
judged to be two adequate trials of SSRIs, in which case consultation with<br />
the psychiatrist is encouraged before a starting medication is chosen.<br />
For those with prior medication treatment histories, the particular SSRI that<br />
proved beneficial in the past would usually be the one to start with. Cost may<br />
also enter into the decision: Given that several of the SSRIs are now available in<br />
generic form, consideration should be given to using them preferentially.<br />
Similarly, formulary restrictions may guide SSRI use in some healthcare systems.<br />
In patients with prior response to benzodiazepines, a trial of an SSRI is still<br />
generally recommended (unless there has been failure to respond to two or more<br />
SSRIs, or a history of intolerance to two or more SSRIs). Even though some<br />
SSRIs have FDA approval for particular anxiety disorders, there is no evidence<br />
that one SSRI is better than any of the others in the treatment of the four anxiety<br />
disorders being treated in <strong>CALM</strong>. Furthermore, although there are subtle group<br />
differences in side-effect profiles among medications (which can manifest as<br />
much larger tolerability differences for individual patients), there is no evidence<br />
that a particular SSRI should have a preferential position in the treatment of<br />
these disorders. Accordingly, as noted above, unless there are compelling<br />
reasons to do otherwise (e.g., history of good – or poor – response to a particular<br />
SSRI in the past), formulary (cost) should be the driving consideration in<br />
selection of initial SSRI.
42<br />
Fluoxetine<br />
(Prozac and<br />
generic)<br />
Paroxetine<br />
(Paxil and<br />
generic)<br />
(or Paxil-CR)<br />
Sertraline<br />
(Zoloft)<br />
Citalopram<br />
(Celexa and<br />
generic)<br />
Escitalopram<br />
(Lexapro)<br />
ANXIOLYTIC<br />
EFFICACY*<br />
Panic**, PTSD*<br />
Panic**, GAD**,<br />
SAD**, PTSD**<br />
Panic**, GAD*,<br />
SAD**, PTSD**<br />
Panic*<br />
Panic*, GAD**,<br />
SAD*<br />
SSRI ANTIDEPRESSANT OPTIONS<br />
ADVANTAGES<br />
Generic available<br />
Long 1/2 life<br />
(No withdrawal)<br />
Generic available. Most<br />
extensively studied<br />
across these anxiety<br />
disorders<br />
Least stimulating<br />
No P450 3A4 effects<br />
Well-studied across<br />
these 4 anxiety<br />
disorders<br />
Least P4502D6 effects<br />
Minimal P4503A4 effects<br />
Intermediate 1/2 life<br />
(Less withdrawal)<br />
Generic available. No<br />
P450 effects<br />
No P450 effects<br />
DISADVANTAGES<br />
Most stimulating<br />
Longer 1/2 life<br />
Most sedating. Shorter ½ life<br />
and worse withdrawal<br />
Most diarrhea<br />
*RCTs but no FDA-approved indication<br />
**FDA-approved indication as of December, 2005<br />
If a patient has had a definite prior response to a non-SSRI antidepressant and<br />
the patient prefers, this antidepressant may be used, regardless of whether it is a<br />
dual-reuptake inhibitor (SNRI), mirtazapine, or TCA (unless the patient has SAD,<br />
which is not thought to be TCA-responsive). If the patient has had non-response<br />
or side-effects to two prior SSRIs, choose between an SNRI (e.g., venlafaxine<br />
XR or, possibly, duloxetine [though, at the time of this writing, the utility of this<br />
particular SNRI in the treatment of anxiety disorders is unknown] or a GABAergic<br />
strategy (benzodiazepines or gabapentin) unless the patient has PTSD,<br />
which has not been shown to be GABA-responsive, or major depression. Some<br />
of these strategies will resemble those used in later steps (2 and 3) of the<br />
treatment protocol (see below). In general, selection among antidepressants<br />
should be based on the patient’s history of medication side-effects, if available.<br />
The side effect table in the next section (titration of initial treatment) can be used<br />
as a guide. For example, in the patient with severe insomnia, one might select a
43<br />
relatively more sedating SSRI such as paroxetine. For the patient with prominent<br />
GI side-effects, one might avoid sertraline to begin with. However, as noted<br />
elsewhere in this manual, response and side-effects are often idiosyncratic.<br />
Therefore, unless particular side-effects are anticipated on the basis of the<br />
patient’s prior experience with SSRIs or SNRIs, cost (and/or formulary)<br />
considerations should generally drive antidepressant selection.<br />
OTHER NON-SSRI ANTIDEPRESSANT OPTIONS<br />
ANXIOLYTIC<br />
EFFICACY*<br />
Panic**, GAD**,<br />
SAD**, PTSD<br />
ADVANTAGES<br />
DISADVANTAGES<br />
Venlafaxine ER<br />
(Effexor XR)<br />
No P450 effects<br />
Short ½ life<br />
Withdrawal with missed dose<br />
or sudden discontinuation<br />
Increased BP at >225 mg<br />
Mirtazapine<br />
(Remeron)<br />
No controlled studies<br />
in anxiety disorders<br />
Rare open reports<br />
Sedation<br />
Oversedation<br />
Increased appetite<br />
and weight gain<br />
Rare agranulocytosis<br />
Duloxetine<br />
(Cymbalta)<br />
No controlled studies<br />
in anxiety disorders<br />
Rare open reports<br />
Unknown<br />
Nausea<br />
Clomipramine<br />
Far fewer controlled<br />
trials, but some<br />
evidence in Panic<br />
GAD, PTSD<br />
Sedation<br />
Can take at bedtime<br />
Very sedating<br />
Weight gain common<br />
Low therapeutic index<br />
*RCTs but no FDA-approved indication<br />
**FDA-approved indication as of December, 2005<br />
A final consideration involves the management of concomitant medication that<br />
the patient may be taking that will not be a first line treatment choice. Most often<br />
this will involve use of either benzodiazepines or low dose, sedating TCAs. For<br />
benzodiazepines, if the patient is on a regular schedule, the PCP should continue<br />
them for at least the first three months of the study so that benzodiazepine<br />
withdrawal symptoms do not complicate or interfere with anti-anxiety response to<br />
antidepressants. The benzodiazepines should be prescribed using a pharmacokinetically<br />
appropriate schedule so as to minimize daily withdrawal or inter-dose<br />
anxiety. If, however, they are only being taken on an as-needed basis (four or<br />
fewer times a week) the PCP and ACS will attempt to help the patient minimize<br />
use and attempt to gradually stop use during the first months of the study.
44<br />
In the case of regular use of low dose, sedating antidepressants, such as<br />
amitriptyline or trazodone, these may be continued at low bedtime doses for the<br />
first several months of the study or, if needed, for the duration, in order not to<br />
exacerbate sleep disturbance.<br />
Titration of Initial Medication Treatment:<br />
SSRIs should be started at low doses typically recommended for anxiety and<br />
titrated to a therapeutic dose over a period of 4-6 weeks. Initial response to<br />
antidepressant medications usually occurs within 4-6 weeks. If there is no<br />
response after 4-6 weeks to an antidepressant at a therapeutic dose, but the<br />
medication is well-tolerated, the dose may be titrated up to the maximum dose<br />
for another 6 weeks. However, some patients find it very discouraging to take a<br />
medicine with no obvious benefit for this length of time. If the ACS, in discussion<br />
with the patient, feels that the therapeutic relationship (and adherence) is likely to<br />
suffer, a switch (usually within class to another SSRI) may be considered for<br />
patients with no response at 4-6 weeks. Another reason to switch before the end<br />
of Step 1 is if the initial antidepressant is poorly tolerated. In that case, the<br />
recommendation would be to switch within class (e.g., one SSRI to a different<br />
SSRI). If there is a partial response by weeks 4-6, a full trial (10-12 weeks) of the<br />
antidepressant at a higher therapeutic dose is recommended. The table below<br />
depicts typical titration schedule guidelines.<br />
Medication Begin Week<br />
1<br />
Week<br />
2<br />
Week<br />
3<br />
Week<br />
4<br />
Top Doses<br />
Fluoxetine<br />
Paroxetine*<br />
Sertraline<br />
Citalopram<br />
Escitalopram<br />
Venlafaxine ER<br />
Duloxetine<br />
Nortriptyline<br />
5 mg<br />
QAM<br />
10 mg<br />
QAM or<br />
QHS<br />
25 mg<br />
QAM<br />
10 mg<br />
QAM<br />
5 mg<br />
QAM<br />
37.5 mg<br />
QAM<br />
20 mg<br />
QHS<br />
25 mg<br />
QHS<br />
10 mg 20 mg 20 mg 30 mg 40 mg<br />
20 mg 20 mg 20 mg 30 mg 50 mg<br />
50 mg 50 mg 50 mg 100 mg 200 mg<br />
20 mg 20 mg 20 mg 30 mg 50 mg<br />
10 mg<br />
QAM<br />
75 mg<br />
QAM<br />
20 mg<br />
BID<br />
50 mg<br />
QHS<br />
10 mg<br />
QAM<br />
75 mg<br />
QAM<br />
20 mg<br />
BID<br />
75 mg<br />
QHS<br />
10 mg<br />
QAM<br />
150 mg<br />
QAM<br />
30 MG<br />
BID<br />
75 mg<br />
QHS<br />
10 mg<br />
QAM<br />
225 mg<br />
QAM<br />
30 MG<br />
BID<br />
100 mg<br />
QHS<br />
20 mg QAM<br />
225 mg<br />
QAM<br />
30 MG<br />
BID<br />
125 mg<br />
QHS<br />
* Paroxetine-CR may also be considered (in which case equivalent dosing is<br />
from 12.5mg/d to 62.5 mg/d), though, in most instances, formulary constraints<br />
will favor immediate release paroxetine
45<br />
During this 3 month time period, adjunctive medication to help with sleep<br />
problems is allowed and would include trazodone (an inexpensive generic),<br />
zolpidem (Ambien), zaleplon (Sonata), eszopiclone (Lunesta) or in the case of<br />
intractable PTSD nightmares, prazosin. If, after 2-4 weeks, patients cannot<br />
tolerate a particular treatment (i.e., intolerable side effects even with careful<br />
titration and clinical management), consider restarting Step 1 by switching to an<br />
alternative antidepressant or, if the side effects have now made the patient<br />
averse to continuing further medication trials, CBT. The ACS in this case will<br />
make a determination before the originally scheduled 12 week time-point, a<br />
necessary alteration in order to provide appropriately tailored treatment for the<br />
individual. Management of the side effect may include, beyond routine dose<br />
reduction with an attempt to preserve efficacy, a substitution of another<br />
antidepressant on the list with a more benign side-effect profile for that individual.<br />
Strategies for managing common side effects of antidepressants are outlined<br />
below.<br />
Adverse Effect Fluoxetine Sertraline Paroxetine Citalopram or Nortriptyline<br />
Escitalopram<br />
Headache - - -<br />
Agitation/<br />
<strong>Anxiety</strong><br />
- - <br />
Tremor <br />
Insomnia - <br />
Drowsiness <br />
Fatigue - <br />
Confusion - - - - -<br />
Dizziness - - <br />
Anti-cholinergic* - - -<br />
Sweating - - - <br />
Weight Gain <br />
GI - - <br />
Sexual <br />
Venlafaxine**<br />
Increases occurrence<br />
Decreases occurrence<br />
* “Anticholinergic” side-effects include dry<br />
mouth, constipation, urinary hesitancy or<br />
retention, blurred vision<br />
** Can increase blood pressure; must be<br />
monitored
46<br />
MANAGING COMMON SRI SIDE-EFFECTS IN THE<br />
TREATMENT OF ANXIETY DISORDERS<br />
Adapted from Preskorn, J Clin Psychiatry 1995; 56 (suppl6)<br />
Problem<br />
Suggested Management<br />
Insomnia 1. Move dosing to early part of day<br />
2. Add trazodone 50-100 mg at bedtime<br />
3. In men concerned about priapism, use zolpidem 10 mg,<br />
zaleplon 10 mg, or esczopiclone 2 mg, if there are no<br />
concerns regarding abuse<br />
5 Add doxepin or amitriptyline 25-50 mg at bedtime<br />
6 Switch antidepressant (e.g., to paroxetine or citalopram)<br />
Nausea/Diarrhea 1. Take with food<br />
2. Encourage patient persistence (should reduce with time)<br />
3. Reduce dose for 4-7 days, then reintroduce higher dose<br />
4. Switch antidepressant (usually to another SSRI)<br />
5. Add H 2 -blocker or Proton Pump Inhibitor (PPI) for<br />
dyspepsia; Lomotil, acidophilous for diarrhea<br />
Sedation 1. Move dosing to bedtime<br />
2. Encourage patient persistence (may reduce with time)<br />
3. Switch antidepressant (e.g., to fluoxetine or sertraline)<br />
Delayed Ejaculation/ 1. Add sildenafil [Viagra] 50-100 mg or other comparable Rx<br />
Anorgasmia 2. Add bupropion 75 mg QAM – BID<br />
3. Switch to mirtazapine<br />
Assessing Treatment Response:<br />
An adequate trial of Step 1 treatment means that patients have completed an 8-<br />
12 week antidepressant (usually SSRI) trial at a sufficient dose (see above for<br />
dosing guidelines) or a trial of up to 6 sessions of CBT. The OASIS and PHQ-3<br />
will be used by the ACS to determine response. Patients who have achieved<br />
remission following step 1 treatment should proceed to relapse prevention<br />
planning and maintenance treatment (see below).<br />
Step 2<br />
Stage 1 Medication Treatment Failures. Generally, these recommendations have<br />
been less well-established in controlled trials. One failed SSRI trial should<br />
prompt consideration of a second SSRI. Patients who have “failed” (i.e., either<br />
due to poor response or poor tolerability) adequate trials of two first-line<br />
antidepressants at step 1 (usually one or more SSRIs) should be considered for<br />
a trial of a first-line antidepressant from a different class. The choice of the<br />
second agent may vary depending on the clinical circumstances (psychiatric
47<br />
consultation will be helpful with this decision). If the first trial was with an SSRI or<br />
if the patient has a comorbid depression, a dual reuptake inhibitor (also known as<br />
a serotonin-norepinephrine reuptake inhibitor [SNRI]) such as venlafaxine<br />
extended-release is recommended for a 2 nd trial. If there is absolutely no<br />
evidence of depression and somatic symptoms of anxiety are particularly<br />
prominent, a primary GABA-ergic agent such as a benzodiazepine or another<br />
agent such as gabapentin or pregabalin would also be an option. Patients may<br />
also be considered for a trial of another ‘newer’ antidepressant such as<br />
mirtazapine or duloxetine at a therapeutic dose, although there is minimal<br />
controlled data supporting their use in anxiety disorders. Bupropion is not<br />
recommended for primary treatment of anxiety disorders, due to a lack of<br />
evidence as to its efficacy for these conditions.<br />
At this stage, there needs to be careful review of the common indications or<br />
considerations for the use of benzodiazepines in anxious patients.<br />
Benzodiazepines are contraindicated for patients with substance abuse<br />
problems and usually prior substance abuse history or as monotherapy in<br />
patients with significant concomitant depression. Benzodiazepines are<br />
indicated if there is a history of non-response to two different antidepressants<br />
classes or if there is severe medical illness or other problems providing<br />
contraindications to using other antidepressants. The other common reason for<br />
benzodiazepine prescription (severe symptoms and disability requiring<br />
immediate attention early in the course of care) can be offset by the availability of<br />
the ACS in this protocol (for patients assigned to the intervention group) who will<br />
have regular weekly meetings for the first few weeks with the patient and provide<br />
support and encouragement, which is often an adequate substitute for the use of<br />
benzodiazepines in the primary care setting. However, some patients may<br />
require supplemental benzodiazepines in the first few weeks if symptoms are too<br />
severe.<br />
Benzodiazepines may also be preferred for the bipolar II patient since some<br />
antidepressants may precipitate mania or increased cyclicity of mood. Preferred<br />
medications are alprazolam 2.0 – 6.0 mg daily (usually split into TID or QID<br />
dosage) lorazepam 1.0-3.0 mg daily (usually split into TID or QID dosage) or<br />
clonazepam 1.0 – 4.0 mg daily (usually split into BID dosage). The longer-acting<br />
benzodiazepines (e.g. clonazepam or extended release alprazolam) are<br />
preferable to minimize interdose anxiety.<br />
Finally, when benzodiazepines are being considered but (relative)<br />
contraindications are evident (e.g., personal history of alcohol abuse now in<br />
remission), some consideration should be given to using alternatives such as<br />
gabapentin [Neurontin] or pregabalin [Lyrica]. Gabapentin is nearly devoid of risk<br />
of drug-drug interactions, making it a good choice for patients with multiple<br />
comorbid medical illnesses and medications. It must be given on a TID schedule<br />
(total daily dose 900-3600) and will usually be much more costly than<br />
benzodiazepines. The role (and dosing) for pregabalin in treatment of anxiety
48<br />
disorders outside of GAD or SAD, and particularly as an adjunct to<br />
antidepressant treatment, is currently unclear. It should be remembered that<br />
benzodiazepines have a long history of use, and strong evidence of<br />
demonstrated efficacy. Unless there are contraindications to their use, they<br />
should generally be tried prior to using the newer, more expensive medications<br />
like gabapentin or pregabalin.<br />
Stage 1 Medication Partial-Responders. It will be assumed that all medication<br />
partial-responders have had their antidepressant dose pushed to the maximum<br />
dose and are still non-responsive. In general, augmentation strategies are less<br />
preferable in primary care because they require closer clinical monitoring, more<br />
complex drug regimens, and often greater expense to the patient. There are,<br />
however, times when a patient has had a partial response to an initial<br />
antidepressant agent and augmentation with another medication is clinically<br />
indicated. The team psychiatrist will have seen the patient and can help in<br />
making the appropriate decision and providing guidance. The two general<br />
strategies to be pursued are: combination of an SSRI with a GABA-ergic agent<br />
(e.g. benzodiazepine or gabapentin [or pregabalin]); and combination of an SSRI<br />
and a noradrenergic antidepressant (e.g., nortriptyline or desipramine). While this<br />
latter strategy is unproven in anxiety disorders, it has good support in the<br />
treatment of depression. When SSRIs are combined with TCAs, serum levels of<br />
the TCA should be checked to avoid toxicity resulting from drug interactions (see<br />
appendix C). In some circumstances of combined depressive and anxiety<br />
symptoms (e.g., where sexual side-effects hamper compliance to other<br />
medications), a combination of bupropion and a benzodiazepine may also be<br />
considered. Combinations of SSRIs or venlafaxine with mirtazapine may also be<br />
considered.<br />
Additional strategies such as augmentation with the atypical anti-psychotics<br />
olanzapine, risperidone, quetiapine, or aripiprazole (see below) may be<br />
considered in later stages after further consultation with the team psychiatrist.<br />
Steps 3 and 4:<br />
Patients who have not had a full response at Step 2 should be discussed in the<br />
weekly team meeting and strongly considered for an additional psychiatric<br />
consultation that could last more than one session, in the primary care clinic (see<br />
below). At this step the psychiatrist may suggest and initiate a number of<br />
treatments in consultation with the ACS and the patient’s PCP. There is no<br />
evidence base to guide care at this juncture. Rather, the choice of treatment at<br />
this step depends on the clinical situation, the resources available, and the<br />
patient’s treatment preferences.<br />
Recommended treatment strategies for Step 3 include:
49<br />
nd<br />
rd<br />
1. A trial of a 2 or 3 type of antidepressant (TCAs could be considered;<br />
MAOIs may need to be considered especially in cases of refractory<br />
PD and SAD)<br />
2. Combination of antidepressant and benzodiazepine (or benzodiazepine<br />
alternative, as described above), if this has not already been tried at an<br />
earlier step.<br />
3. Other augmentation strategies such as augmentation of either SSRIs or<br />
venlafaxine ER with the atypical anti-psychotics olanzapine, risperidone,<br />
quetiapine, or aripiprazole. This may be especially worthwhile if the patient<br />
has had a partial response to treatment at Step 2. It should be noted that<br />
although there is growing evidence that adding an atypical antipsychotic<br />
may be a useful strategy for refractory depression, the evidence base in<br />
anxiety disorders is considerably less well-developed.
50<br />
8. PSYCHIATRIC EVALUATION FOR PERSISTENT ANXIETY<br />
Psychiatric evaluations for persistent anxiety have two major objectives:<br />
1. To clarify the diagnosis including the specific psychiatric disorder(s)<br />
and comorbid medical problem(s) or medication(s) that must be<br />
considered in developing a treatment plan;<br />
2. To develop a treatment plan for Step 2 or 3 and, when indicated, to<br />
initiate treatment in cooperation with the ACS and the patient’s<br />
PCP.<br />
The following table lists a number of factors to explore during the initial<br />
consultation. The results of such consultations should be documented by the<br />
team psychiatrist using the web-based data entry form. Also, psychiatric<br />
evaluation is conducted with the patient after a full enquiry with the ACS<br />
regarding issues of perceived barriers to treatment, disparities between the<br />
patient’s treatment expectations and process, as well as their outcome and<br />
efficacy expectations over the course of treatment thus far.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
1. Evaluate for other psychiatric disorders<br />
bipolar disorder<br />
other anxiety disorders not already recognized<br />
obsessive compulsive disorder<br />
psychotic disorder or psychosis<br />
somatization or somatoform disorders<br />
alcohol or substance abuse (includes prescription drugs)<br />
cognitive impairment/dementia<br />
personality disorders and maladaptive coping mechanisms<br />
2. Consider medical disorders or medications that may contribute<br />
to anxiety<br />
substance use problems<br />
surreptitious benzodiazepine use<br />
obstructive sleep apnea<br />
complex partial epilepsy<br />
surreptitious opiate use<br />
cardiopulmonary conditions (e.g., asthma; CHF)<br />
thyroid disease, either hypo or hyper<br />
caffeinism<br />
OTC cold preparations<br />
herbal preparations (e.g., weight loss or “energy-enhancing”<br />
compounds)<br />
steroids<br />
bronchodilators<br />
anemia
51<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
3. Consider anxiogenic health habits<br />
sleep deprivation<br />
sedentary lifestyle (lack of exercise)<br />
social use of alcohol or caffeine<br />
smoking<br />
4. Explore prior treatment history<br />
adequacy of treatments attempted<br />
attitudes toward treatments and providers<br />
successes<br />
failures<br />
relevant treatment history in close relatives<br />
5. Address problems with adherence in consideration of the<br />
barriers already identified by the ACS<br />
different explanatory model—patient does not feel understood<br />
cultural barriers<br />
secondary gain<br />
life stressors (care giving, unresolved grief, financial)<br />
instrumental barriers (finances, transportation, time)<br />
cognitive impairment<br />
side effects<br />
patient demoralization<br />
6. Address psychosocial issues in greater detail (e.g. history of<br />
abuse)<br />
The web-based ‘record’ of psychiatric consultation covers most of the factors to<br />
be considered during an evaluation and leaves room to record a diagnostic<br />
formulation and treatment recommendations
52<br />
9. DOCUMENTING AND TRACKING CLINICAL ENCOUNTERS<br />
USING THE WEB-BASED CLINICAL INFORMATION SYSTEM<br />
The <strong>Anxiety</strong> Clinical Specialist (ACS) will use a web-based clinical information<br />
system to track each patient’s progress throughout the one-year intervention<br />
period. He or she will use a personal computer (a stand-alone PC or a laptop)<br />
and a standard web browser (Microsoft Internet Explorer version 5.0 or higher) to<br />
log on to a secure server at the coordinating center and enter a unique login ID<br />
and password. The ACS will complete a new enrollment form for each<br />
intervention patient and will then enter an initial assessment, follow-up<br />
assessments, treatment plans, or a relapse prevention plan as treatment<br />
proceeds. Samples of these data entry forms are being developed.<br />
Data entry can occur ‘on line’ during a patient session, after a patient session, or<br />
at the end of the day. If data are not entered in ‘real time’, the ACS should make<br />
notes using a paper copy of the relevant form and should enter the data as soon<br />
as possible (usually the same day). Blank copies of the data acquisition forms<br />
can be printed off the password protected section for investigators on the main<br />
study web site. During the data entry, the ACS will have to enter the patient’s<br />
study ID number and initials, as the database will store information entered by<br />
these identifiers. After completion of a data entry form, the server will ‘validate’<br />
the form, perform ‘range checks’ on certain data entry fields and will prompt the<br />
ACS for corrections if data entered are not consistent with ranges specified for<br />
particular ‘fields’. This will allow for better data quality and more uniformity in the<br />
treatment intervention. After each contact form is completed and checked, the<br />
ACS will submit the form to the server, where it will be stored in a database. The<br />
server will then format the information, which should be printed ‘on site’. A copy<br />
of each form should be placed in the patient’s study record, and additional copies<br />
can be shared with the patient and the PCP as clinically appropriate. A copy of<br />
each note may also be placed in the patient’s regular clinic record at the<br />
discretion of the PCP. All completed forms can be accessed on the web site and<br />
updated or modified at anytime.<br />
The ACS or other site investigators can also log on to the secure server and<br />
request an updated caseload tracking report of all intervention patients that will<br />
show if specific intervention activities have been completed or not or a progress<br />
report on an individual patient.<br />
STANDARDIZATION OF INTERVENTION<br />
The clinical database will be searched regularly at the UW site, which will be<br />
coordinating the intervention implementation, to identify potential clinical<br />
problems or problems in adherence to the intervention protocol. Examples might<br />
include cases where patients don’t appear to be on active treatments (i.e.,<br />
antidepressants at adequate doses or CBT), or where patients don’t seem to
53<br />
have follow-up contacts as specified in the intervention protocol. The program<br />
will generate prompts to identify potential problems to each ACS each time he or<br />
she logs on to the system.<br />
The database at the coordinating center will also be used to track the<br />
implementation of the intervention at all study clinics, and it is thus very important<br />
that all clinical contacts (both in person and telephone) are recorded as<br />
completely as possible.<br />
ASSURING PRIVACY AND CONFIDENTIALITY OF PATIENT INFORMATION<br />
Patient information gathered for this study is sensitive and must be regarded as<br />
highly confidential. Even the fact that the patient is enrolled in the study should<br />
be viewed as private and confidential. All study materials that identify patients by<br />
name and/or number must be kept in locked files or secure locations when not in<br />
use. Only the ACS and the principal investigator at each site should have access<br />
to documents that link patient study ID numbers to their other identifying<br />
information (i.e., name, address, telephone numbers, or medical record<br />
numbers). It is possible that primary care providers will choose to put forms into<br />
patients’ regular medical records. This decision is made at the discretion of the<br />
patient and his/her primary care provider.
54<br />
10. PCP’S GUIDE FOR ANXIETY MANAGEMENT<br />
The following guidelines are to be used by the PCP in their day to day<br />
management of anxious patients<br />
Seven Key Challenges in Managing <strong>Anxiety</strong><br />
1. Make a diagnosis and include all diagnoses to start.<br />
2. Educate and recruit the patient as a partner in treatment.<br />
3. Start with a single treatment modality and match to patient<br />
preferences.<br />
4. Use correct medication doses and/or work in collaboration with<br />
skilled practitioners of evidence-based (i.e., CBT) psychotherapy<br />
5. Treat long enough initially. Patients often take 10-12 weeks to<br />
respond.<br />
6. Follow outcomes and adjust treatment as needed. Consider<br />
consultation if patient is not improving.<br />
7. Treat long enough to prevent relapses (6-12 months) and know the<br />
signs of high risk for relapse.<br />
Diagnosing <strong>Anxiety</strong> in Primary Care<br />
SIGNS AND SYMPTOMS OF ANXIETY<br />
<br />
<br />
<br />
Cognitive symptoms: worry, rumination, anxious preoccupation,<br />
cognitive distortions such as catastrophization (imagining the worst<br />
outcome), overestimating the risk of something bad happening,<br />
overgeneralization, overpersonalization<br />
Physiologic symptoms: palpitations, shortness of breath, dizziness,<br />
nausea, diarrhea, hot and cold flashes, sweating, numbness and<br />
tingling, derealization, depersonalization, muscle tension, insomnia<br />
Behavioral signs: avoidance of various activities, hypervigilance
55<br />
Conditions Characterized by Anxious Symptoms<br />
PANIC DISORDER (PD)<br />
Recurrent panic attacks, at least some spontaneous (panic attacks are sudden<br />
bursts of anxiety accompanied by at least several cardiorespiratory,<br />
gastrointestinal, autonomic or otoneurological symptoms)<br />
Persistent fear of future attacks, or change in behavior because of attacks (e.g.<br />
going to emergency room, asking for medical tests), or phobic avoidance (e.g.<br />
restricting activity, driving, going to stores etc) because of attacks<br />
GENERALIZED ANXIETY DISORDER (GAD)<br />
Unrealistic, hard to control, persistent worry about numerous life situations, for at<br />
least 6 months, 50% of the time<br />
At least 3 of 6 symptoms (insomnia, poor concentration, restlessness, fatigue,<br />
irritability, muscle tension)<br />
SOCIAL ANXIETY DISORDER (SAD)<br />
Marked or persistent fear of social or performance situations in which one is<br />
exposed to unfamiliar people or possible scrutiny by others and fears<br />
embarrassment or humiliation<br />
Exposure to these situations provokes anxiety, which may take the form of panic<br />
attacks<br />
The situations are then avoided or endured with dread<br />
POST TRAUMATIC STRESS DISORDER (PTSD)<br />
Exposure to a life-threatening or personal integrity-threatening traumatic event<br />
Reexperiencing of the event by flashbacks, nightmares, recurrent recollections,<br />
etc.<br />
Persistent avoidance of reminders of the trauma and numbing of general<br />
responsiveness (i.e. detached, estranged, no future orientation)<br />
Persistent symptoms of arousal (insomnia, irritability, hypervigilance, startle)<br />
OBSESSIVE COMPULSIVE DISORDER (OCD)<br />
Recurrent obsessions and compulsions that are time-consuming and interfering<br />
Not covered by <strong>CALM</strong>; refer to regular mental health care resources
56<br />
Talking to Patients About <strong>Anxiety</strong><br />
A biopsychosocial model that emphasizes the hard to control factors of innate<br />
genetic vulnerability and medical illness, along with the role of psychosocial<br />
stressors and coping style, which the patient may have more control over with<br />
help from the ACS and their own self-activation, provides a useful framework for<br />
discussing the diagnosis of anxiety with patients. The cycle of anxiety model<br />
(next page) can be helpful in discussing the topic of anxiety with patients as it<br />
emphasizes the multiple factors that contribute to anxiety and the ways in which<br />
treatments address these factors. All factors can ultimately cause brain chemical<br />
changes and both medications and CBT can reverse these changes.<br />
THE CYCLE OF ANXIETY<br />
HEALTH HABITS<br />
Poor diet<br />
Inadequate sleep<br />
Caffeine and alcohol use<br />
Lack of exercise<br />
STRESSORS<br />
<strong>Medical</strong> illness<br />
Pain<br />
Family or Marital problems<br />
Work problems<br />
GENETIC FACTORS<br />
Family history of panic<br />
Early childhood anxiety<br />
THOUGHTS AND FEELINGS<br />
Something is wrong with my body<br />
Worry about everything<br />
Can’t cope<br />
I’m out of control<br />
Depression<br />
PHYSICAL<br />
Muscle Tension<br />
Shortness of breath<br />
Flushing & chills<br />
Palpitations<br />
Chest Pain<br />
Dizziness<br />
CBT TO IMPROVE COPING<br />
BEHAVIOR<br />
Increased doctor visits<br />
because of health<br />
worries.<br />
Avoidance of places<br />
that make me anxious.<br />
Hypervigilance.<br />
Use of alcohol<br />
to cope.<br />
MEDICATIONS<br />
In discussing anxiety with patients, it is quite helpful to mention that:<br />
1. <strong>Anxiety</strong> is common in primary care.<br />
2. <strong>Anxiety</strong> can cause or aggravate a wide range of symptoms, including<br />
physical symptoms.<br />
3. <strong>Anxiety</strong> affects the body, behavior and thinking.<br />
4. <strong>Anxiety</strong> is an illness, not a character defect or weakness.<br />
5. Recovery from anxiety is the rule, not the exception.<br />
6. The good news is that anxiety can almost always be treated with either<br />
medications or psychotherapy.
57<br />
It can be very useful to refer patients to high-quality sources of information about<br />
anxiety disorders. We particularly recommend the materials available at the<br />
<strong>Anxiety</strong> Disorders Association of America website (www.adaa.org).<br />
Troubleshooting:<br />
What to Do if Patients Don’t Improve as Expected<br />
When patients do not recover or progress with therapies as expected,<br />
there are a variety of well understood and described factors that are likely<br />
contributing to this failure to progress. These include:<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Wrong Diagnosis<br />
Insufficient Dose or Treatment length<br />
Adherence Problem<br />
Side Effects<br />
Ongoing life stressors<br />
Ongoing medical problems<br />
Psychological barriers to recovery<br />
Unrecognized substance abuse<br />
Other co-morbid psychiatric disorders, including personality<br />
disorders<br />
These factors will be carefully evaluated and addressed with a revised<br />
treatment plan during Psychiatric Consultation.
58<br />
Patient Information about Medication<br />
How do anti-anxiety medications work?<br />
Both life stresses and medical problems can change chemical messengers<br />
in the brain that maintain the balance in how you feel emotionally and physically.<br />
Some people are more prone than others to developing these kinds of<br />
imbalances; this tendency may run in families and be at least partly genetic in<br />
origin. This chemical imbalance results in some of the common symptoms of<br />
anxiety such as worry, nervousness, heart palpitations, sweating, digestive<br />
upset, insomnia, and avoidance of stressful situations. Antidepressant<br />
medications, originally developed to treat depression, have been found to be the<br />
most broadly effective medications for a range of anxiety disorders. Thus, these<br />
medications are the most commonly used anti-anxiety medications and can help<br />
restore a normal balance of these chemical messengers, helping to relieve<br />
emotional and physical symptoms.<br />
Antidepressants can take up to 8 weeks to work. It usually takes two to<br />
four weeks until people start feeling better emotionally and physically. This<br />
improvement may be gradual, and often, family members of friends may notice a<br />
difference in how you are doing before you do. Some symptoms may improve<br />
first and other symptoms may take more time to improve. Benzodiazepines<br />
belong to a class of anti-anxiety medication that works more quickly, usually<br />
within a week. These medications are often not the first choice, because they<br />
are not effective against some symptoms, such as depression, that often<br />
accompany anxiety. They also have a potential for abuse, if the person has had<br />
previous or current problems with alcohol or other drugs.<br />
Once you are feeling better, do not stop the medication right away. Your<br />
doctor may recommend taking the medication for 12 months or longer to prevent<br />
a relapse of your anxiety.<br />
How to find the right medication for you:<br />
Scientific studies show that medications do not differ in the percentage of<br />
patients that get better. However, different medications are effective for different<br />
people, and the side effects of the medications differ. Some medications also<br />
may cost more than others. Your doctor can help you decide which medication<br />
may be best for you.<br />
Between 50% and 80% of patients will improve after 4 to 8 weeks on a<br />
medication. By working together, you and your doctor can decide whether the<br />
medication you started is the right one for you. If you need to switch to another<br />
medication because of side effects or because you are not substantially<br />
improved, chances are still excellent that you will improve on a second<br />
medication. Sometimes, medications may be combined, if one works partially,<br />
to get a “full” and complete effect.
59<br />
What about side effects:<br />
Some people experience side effects when taking medications. While<br />
annoying, they are rarely dangerous to your health. They usually occur the first<br />
few weeks and then gradually decrease as your body adapts to the medication.<br />
Because of these early side effects, patients sometimes feel a little worse before<br />
they start getting better and may give up too soon. If you have side effects that<br />
are bothering you, discuss these with your doctor or your anxiety clinical<br />
specialist. Your doctor will help you determine if these side effects will decrease<br />
over time or if you should decrease or switch your medications.<br />
Some of the side effects that can occur with medications include: nausea,<br />
headaches, jitteriness, weight gain, diarrhea, insomnia, sedation, dizziness,<br />
difficulty in achieving orgasm<br />
Remember:<br />
1. Take the medications every day, as prescribed by your doctor.<br />
2. Keep track of any side effects and discuss them with your doctor.<br />
3. Sudden discontinuation of any of these medications can cause<br />
withdrawal symptoms so always taper your medication down before stopping it.<br />
4. It takes 4-10 weeks for most medications to work, with the exception of<br />
benzodiazepines, which can work more rapidly.<br />
5. Continue to take the medication even when you feel better.<br />
6. Don’t stop taking medications before talking with your primary care provider.<br />
Patient Information about CBT<br />
What is CBT?<br />
CBT stands for Cognitive Behavior Therapy. CBT is a well researched form of<br />
therapy that helps people with anxiety problems feel less anxious and stop<br />
avoiding things they would like to do because of anxiety.<br />
How does CBT work?<br />
CBT focuses on helping people change thinking patterns and behavior patterns<br />
that contribute to high levels of anxiety. With the help of a CBT therapist, people<br />
learn how to:<br />
Weaken the connections between tough situations and “knee-jerk” or<br />
habitual reactions to them<br />
Calm their minds and bodies, so they can feel better, think more clearly,<br />
and make more effective decisions
60<br />
Understand how their problems work, what triggers them, and what they<br />
can do to stop the “typical chains” of events that are keeping them from<br />
more satisfying lives<br />
Learn new, more effective ways of coping with distress and regulating<br />
emotions<br />
Understand how certain thinking patterns may contribute to problems and<br />
how to change them.<br />
What is doing the treatment like? What will the therapist ask me to do<br />
exactly?<br />
You can expect your therapist to:<br />
-Listen to what you have to say and be empathetic – they will work to<br />
understand you and what you are experiencing<br />
-Be active in treatment – they work with you to understand and solve your<br />
problems (that means they ask questions and give you feedback, not sit there<br />
silently!).<br />
-Come up with a brief, focused plan to help you start feeling better. CBT<br />
focuses on helping people feel better as soon as possible.<br />
-Be present-focused. This means that a CBT therapist will not assume that<br />
all your problems are due to childhood/past issues. This is NOT to say that if<br />
these are important to you and your treatment, they will not focus on them. It<br />
simply means that unlike some forms of psychotherapy, CBT does not assume<br />
that all our problems are necessarily linked to early childhood issues.<br />
-Work hard with you to decrease your anxiety in and out of sessions!<br />
Will it be a lot of work?<br />
CBT does require activity and work on your part. This is because work and<br />
practice outside of sessions are very important to help you get used to new ways<br />
of responding that don’t keep you anxious all the time! It’s a good idea to think<br />
about doing CBT “all the way”. Your therapist will be with you every step of the<br />
way to help you and provide support. But, it does require work.<br />
I feel really bad. Doesn’t this mean I need medications?<br />
Both CBT and medications are good forms of treatment, and studies show that<br />
both are effective even for severe anxiety. So, feeling really anxious or down<br />
doesn’t mean that CBT is a bad choice.<br />
How long will it take to work?<br />
Everyone responds differently, so it’s hard to say exactly how long it takes for<br />
CBT to work. However, many people start to feel better by around the 4 th<br />
session, and some people experience benefits even sooner.
61<br />
Common Questions about <strong>Anxiety</strong> Medications<br />
1. How do medications work?<br />
Medications help restore the correct balance of certain chemicals<br />
called neurotransmitters in the brain.<br />
2. My problem is inability to sleep. How can medication help this?<br />
In many cases, poor sleep is a by-product of anxiety. Once the<br />
anxiety improves, sleep often improves as well.<br />
Antidepressants can help restore sleep, even in people who do not<br />
have anxiety or depression. They are better than sleeping pills<br />
because they are not habit forming, and are less likely to impair<br />
concentration or coordination.<br />
3. I have a problem with pain. How can anxiety medication help with<br />
this?<br />
Some antidepressants have been shown to be successful in a<br />
number of pain conditions (diabetic neuropathy, phantom limb<br />
pain), even in the absence of anxiety or depression.<br />
Antidepressants may also help restore normal sleep and reverse a<br />
vicious cycle of pain and sleep problems.<br />
4. I have a lot of stress in my life. How can a medication help with<br />
this?<br />
Life stress can worsen symptoms of anxiety. <strong>Anxiety</strong> can then<br />
worsen the impact of such stressors (such as work stress, family<br />
problems, physical disabilities or financial worries) and your ability<br />
to cope with them. Treating the anxiety can help some patients<br />
break out of this vicious cycle.<br />
5. Are anti-anxiety medications addictive?<br />
The kind of anti-anxiety medication most likely to be recommended<br />
for you will be an antidepressant. Antidepressants are not habitforming<br />
or addictive. They do not produce a high feeling, but slowly<br />
alter the amount of certain chemicals called neurotransmitters in<br />
the brain over a number of weeks. Restoring the levels to a more<br />
normal balance usually brings the depression under control.<br />
Some people have been taking antidepressants continually for up<br />
to 30 years without any significant (physical or psychological)<br />
adverse effects. Still, it is important that the antidepressants not be<br />
stopped suddenly, as side-effects can develop with abrupt<br />
discontinuation.<br />
Benzodiazepines, taken regularly under a doctor’s supervision, are<br />
very unlikely to produce a high or the need for increasing doses
62<br />
over time, unless someone already has or has had in the past a<br />
problem with drug or alcohol abuse.<br />
However, benzodiazepines do produce physical tolerance<br />
and so cannot be abruptly discontinued; they must be<br />
gradually tapered down to avoid withdrawal symptoms.<br />
This characteristic is another one of the reasons that<br />
antidepressants are a first choice for anxiety treatment.<br />
6. My problem is more depression than anxiety. How will these<br />
medications help?<br />
In many cases, depression may be a by-product, or later stage, of<br />
anxiety. Antidepressants will help both these conditions.<br />
7. How long will it take the medications to work?<br />
For antidepressants, it usually takes from 4-6 weeks for patients to<br />
start feeling better. Small improvements in some symptoms are not<br />
easily noticeable, although if you keep track of the intensity of your<br />
symptoms with a diary, you can often see differences in 1-2 weeks.<br />
If the anxiety has not improved after 4-6 weeks by at least 25%,<br />
you may need an increase in the dose or change to another<br />
medication.<br />
8. How long will I have to take the medication?<br />
Once you have completely recovered from your anxiety, you should<br />
stay on the medication for at least a year. Deciding to stop after this<br />
depends on how long you had the anxiety before, how intense the<br />
symptoms were, and how much they interfered with your life. Your<br />
primary care provider will help you decide when the time is right to<br />
stop the medication.<br />
For people who have had longstanding problems with anxiety from<br />
childhood or early adulthood, and for people who may have<br />
continuing, ongoing stress in their life due to medical problems or<br />
other life circumstances, continuing the medication may be helpful.<br />
For people who have had shorter problems with anxiety and<br />
periods of feeling very well without anxiety in the recent past, and<br />
for those who are not facing too much ongoing stress, gradually<br />
stopping the medication after a year might make sense.<br />
9. Are there any dangerous side effects?<br />
Side effects from medications are usually mild. You should ask<br />
your doctor or anxiety clinical specialist (who will coordinate with<br />
your doctor) what to expect and what to do if you have a problem.<br />
In many cases, your body will get used to the medication and you<br />
won’t be bothered with the side effect for long. In other cases, your<br />
doctor may suggest you lower the dose, add another medication, or
63<br />
<br />
change to another medication. If used properly, there are no<br />
dangerous or life-threatening side effects.<br />
If you have any questions or concerns about side effects, you<br />
should not hesitate to bring these up with your primary care<br />
provider. By letting your doctor know how the medicine affects you,<br />
you can help him/her choose the best medication and dose that<br />
work for you.<br />
10. Is it safe to take anti-anxiety medications together with alcohol or<br />
other medications?<br />
In general, antidepressants can be safely taken with other<br />
medications. However, some antidepressants may increase or<br />
decrease the amounts of other medications in the body, so you<br />
should let your doctor or anxiety clinical specialist know exactly<br />
which other medications you are taking so that he/she can be sure<br />
there are not problems.<br />
All anti-anxiety medications, but especially benzodiazepines, can<br />
increase the sedating effects of alcohol. Be careful to avoid alcohol<br />
intake while on these medications. Be especially cautious about<br />
driving or using heavy machinery until you know how these<br />
medications affect you.<br />
11. What should I do if I miss the medication one day?<br />
Don’t “double up” and take the dose you forgot. Just resume taking<br />
your medication as prescribed.<br />
12. Can I stop the medication once I am feeling better?<br />
No. You would be at high risk for having the anxiety come back<br />
and may experience some temporary withdrawal symptoms.<br />
Treatment for at least 12 months makes sense for almost everyone,<br />
and after that, stopping the medication is a decision that must be<br />
individualized for each person, based on the nature and duration of<br />
their anxiety and other emotional problems. It is best to talk about<br />
this with your doctor, and develop a plan for when and how to stop<br />
taking medication.<br />
13. Will I get better?<br />
With adequate treatment, between 50 and 80% of patients will<br />
experience a complete recovery.<br />
Remember, if the first medication or approach does not work, your<br />
doctor will try additional medications or other therapies that are<br />
likely to help you.
64<br />
11. HANDLING EMERGENCIES<br />
Acute suicidality-<br />
For patients endorsing acute suicidal ideation while in the presence of the<br />
ACS, the ACS will provide immediate assistance and referral. Initially, the ACS<br />
will ascertain, using our suicide assessment and protocol form (see next page),<br />
how imminent the patient’s risk of self-harm is. If the patient rates their own<br />
suicidality at a level of four or higher on the seven point scale, or if the ACS<br />
suspects that the patient is at that level despite the patient’s own ratings, the<br />
ACS will ascertain whether or not the person can control their impulses to harm<br />
themselves. If the patient indicates that they are incapable, or unsure of their<br />
ability to refrain from harming themselves, the ACS will take the necessary and<br />
recommended steps outlined on our form. In addition, if, for any reason, the ACS<br />
believes the patient is less capable than they indicate of preventing harm to<br />
themselves, they are to proceed with the suicide protocol as it is outlined on our<br />
form. As a matter of protocol, the ACS will make contact with the patient’s PCP<br />
and the study psychiatrist or psychologist to provide further assistance to the<br />
patient, or to simply discuss the event and the actions the ACS took.<br />
Acute manic or psychotic episode-<br />
While people with bipolar 1 disorder or any psychotic disorder should have<br />
been excluded from this study, if manic or psychotic symptoms emerge over the<br />
duration of treatment, the ACS will immediately contact the consulting<br />
psychiatrist and together they will contact the patient’s PCP and devise a<br />
strategy to treat the patient. This may include an immediate in person<br />
consultation with the psychiatrist if feasible, referral to a psychiatric emergency<br />
service if more structure or physical containment is required to manage the<br />
patient, prescription of anti-manic medication, and contacting the person’s<br />
immediate family, significant other, or others living with the person.<br />
Severe side-effects-<br />
If a patient experiences severe side-effects from their prescribed<br />
medication, the ACS will contact the patient’s PCP and refer the patient to their<br />
provider to adjust the patient’s prescription as necessary. Guidelines for<br />
changing prescriptions are laid out in this manual within the medication algorithm.<br />
The study psychiatrist is available for consultation to the PCP at their discretion.<br />
Further, if necessary, the patient may have an in-person session with the<br />
psychiatrist to discuss the prescription options. If the ACS is uncertain whether<br />
an immediate call to the PCP is necessary they may first consult the psychiatrist.<br />
Alcohol and substance abuse (including prescription medications)-<br />
A patient that is found to be misusing or abusing alcohol or drugs will be<br />
referred to their PCP and will be provided with contact information for local drug<br />
or alcohol counseling and rehabilitation services by the ACS. The patient’s PCP<br />
will be alerted to the situation. In addition the ACS will discuss the counter<br />
productivity of substance misuse with regards to their anxiety treatment program.
65<br />
Suicidality Risk Assessment and Protocol<br />
The suicide assessment protocol is to be initiated whenever the patient indicates any suicide intent.<br />
Suicide intent is defined as any communication related to wanting to kill oneself or wanting to be<br />
dead, either spoken out loud or indicated on a questionnaire. This protocol should also be initiated if<br />
you have any reason to suspect suicide ideation might be present, even if the patient did not<br />
communicate this directly.<br />
1. On a scale of 1 to 7, what is your intent to kill yourself right now? Date Time<br />
Low 1 2 3 4 5 6 7 High<br />
2. If "4" or higher, ask: Do you believe you could control your impulses? Yes No<br />
3. If ''no'' or if any reason to suspect that the patient is at risk, ask the following:<br />
a) Suicide planning and/or preparation- Do you have a plan on how you would kill yourself?<br />
b) Suicide note written or in progress- Have you written or started a letter to others about killing<br />
yourself?<br />
c) Methods available or easily obtained- Refer back to plan and ask: Do you have<br />
available to you?<br />
d) Precautions against discovery or intervention; deception or concealment about timing, place,<br />
etc. Consider plan and ask: Does anyone know about your plan?<br />
e) Indirect references to own death, arrangements for death- Consider plan and ask: Have you<br />
made any preparations for your death?<br />
f) History of suicide attempts- Have you ever attempted suicide previously?<br />
g) Recent disruption or loss of interpersonal relationship; negative environmental changes in past<br />
month; recent psychiatric hospital discharge-Ask: Have you suffered any recent losses or serious<br />
stressors or changes or problems in your relationships?<br />
h) Isolation- Ask: Have you been particularly isolated lately?<br />
i) Abrupt clinical change, either negative or positive-Ask: Have you recently experienced a drastic<br />
change in your mood-either feeling really "up" or really "down"?<br />
j) Current hopelessness, anger, or both-Ask: Are you currently feeling hopeless (like things will never<br />
get better)? Are you currently feeling a lot of anger?<br />
k) Depressive turmoil, severe anxiety, panic attacks, severe mood cycling-Ask: Are you<br />
experiencing a lot of depression, anxiety, panic attacks or extreme "ups and downs"?<br />
1) Alcohol consumption/drug use-Ask: In the last week, have you been drinking alcoholic beverages<br />
or using recreational drugs? A lot more than normal? Assess frequency quantity, and recency.<br />
Remain with the patient or on the phone until risk is lowered. If over the telephone, tell the patient that you<br />
would like to consult with the study investigator and ask the patient for a commitment not to harm<br />
himself/herself and to stay present and available for a return phone call within the next 10 minutes. Page the<br />
study investigator for directions. Use emergency means (dial 911) if necessary.<br />
Check which actions taken (must always do items in bold):<br />
a. Referred to positive thing(s) in patient's life;<br />
b. Focused on what he/she can do about his/her feelings;<br />
c. Ask patient to list and call people in his/her support network;<br />
d. Made sure he/she had emergency numbers (including crisis line and clinic numbers);<br />
e. Contracted with patient to not harm self or engage in suicidal acts;<br />
f. Ask patient to call for professional help (psychiatrist/therapist/PCP/crisis line/ER);<br />
g. Had patient call you back to confirm patient took positive actions;<br />
h. Referred patient to clinic staff/PCP in waiting room;<br />
i. Accompanied patient to Emergency Room;<br />
j. Contacted 911 (danger to life is imminent and patient refuses help); Time<br />
k. Contacted CDMHP office; Who did you speak with?<br />
l. Contacted subject’s PCP within 24 hours; Date Time<br />
m. Contacted Study Investigator within 24 hours; Date Time<br />
n. Other<br />
o. Completed Adverse Event Report
66<br />
12. SUPPORTING MATERIALS<br />
This manual makes reference to numerous consensus guidelines and<br />
reviews of evidence-based studies supporting the recommendations<br />
contained herein. Following is a list of supporting materials for these<br />
statements of fact and other recommendations that were used in<br />
preparing and documenting this manual.<br />
C. Allgulander, B. Bandelow, E. Hollander, S. A. Montgomery, D. J. Nutt, A. Okasha, M. H.<br />
Pollack, D. J. Stein, and R. P. Swinson. WCA recommendations for the long-term treatment of<br />
generalized anxiety disorder. CNS.Spectr. 8 (8 Suppl 1):53-61, 2003.<br />
J. C. Ballenger, J. R. T. Davidson, Y. Lecrubier, D. J. Nutt, J. Bobes, D. C. Beidel, Y. Ono, and H.<br />
G. M. Westenberg. Consensus statement on social anxiety disorder from the International<br />
Consensus <strong>Group</strong> on Depression and <strong>Anxiety</strong>. J Clin Psychiatry 59 (suppl. 17):54-60, 1999.<br />
J. C. Ballenger, J. R. Davidson, Y. Lecrubier, D. J. Nutt, E. B. Foa, R. C. Kessler, A. C.<br />
MacFarlane, and A. Y. Shalev. Consensus statement on posttraumatic stress disorder from<br />
the International Consensus <strong>Group</strong> on Depression and <strong>Anxiety</strong>. J Clin Psychiatry 61 (suppl<br />
5):60-66, 2000.<br />
D. L. Chambless and S. D. Hollon. Defining empirically supported therapies. J Consult<br />
Clin.Psychol. 66 (1):7-18, 1998.<br />
J. R. Davidson. Use of benzodiazepines in social anxiety disorder, generalized anxiety disorder,<br />
and posttraumatic stress disorder. J Clin.Psychiatry 65 Suppl 5:29-33, 2004.<br />
A. C. Doyle and M. H. Pollack. Establishment of remission criteria for anxiety disorders. J<br />
Clin.Psychiatry 64 Suppl 15:40-45, 2003.<br />
G. Fricchione. Clinical practice. Generalized anxiety disorder. N.Engl.J Med 351 (7):675-682,<br />
2004.<br />
J. P. Hambrick, J. W. Weeks, G. C. Harb, and R. G. Heimberg. Cognitive-behavioral therapy for<br />
social anxiety disorder: supporting evidence and future directions. CNS.Spectr. 8 (5):373-381,<br />
2003.<br />
F. Kapczinski, M. S. Lima, J. S. Souza, and R. Schmitt. Antidepressants for generalized anxiety<br />
disorder. Cochrane Database Syst Rev (2):CD003592, 2003.<br />
B. A. Lauria-Horner and R. B. Pohl. Pregabalin: a new anxiolytic. Expert.Opin.Investig.Drugs 12<br />
(4):663-672, 2003.<br />
M. R. Mavissakalian and J. M. Perel. Long-term maintenance and discontinuation of imipramine<br />
therapy in panic disorder with agoraphobia. Arch.Gen Psychiatry 56 (9):821-827, 1999.<br />
A. Raj. Overview and treatment of social anxiety disorder. Manag.Care 13 (6 Suppl<br />
Depression):52-57, 2004.<br />
M. A. Raskind, E. R. Peskind, E. D. Kanter, E. C. Petrie, A. Radant, C. E. Thompson, D. J. Dobie,<br />
D. Hoff, R. J. Rein, K. Straits-Troster, R. G. Thomas, and M. M. McFall. Reduction of<br />
nightmares and other PTSD symptoms in combat veterans by prazosin: A placebo-controlled<br />
study. Am.J.Psychiatry 160 (2):371-373, 2003.
67<br />
K. Rickels, M. H. Pollack, D. E. Feltner, R. B. Lydiard, D. L. Zimbroff, R. J. Bielski, K. Tobias, J. D.<br />
Brock, G. L. Zornberg, and A. C. Pande. Pregabalin for treatment of generalized anxiety<br />
disorder: a 4-week, multicenter, double-blind, placebo-controlled trial of pregabalin and<br />
alprazolam. Arch Gen Psychiatry 62:1022-1030, 2005.<br />
E. N. Ringdahl, S. L. Pereira, and J. E. Delzell, Jr. Treatment of primary insomnia. J Am.Board<br />
Fam.Pract. 17:212-219, 2004.<br />
J. F. Rosenbaum and M. H. Pollack. The pharmacotherapy of panic disorder. In: Panic Disorder<br />
and Its Treatment, edited by J. F. Rosenbaum and M. H. Pollack, New York:Marcel Dekker,<br />
Inc., 1998, p. 153-180.<br />
P. P. Roy-Byrne, M. B. Stein, A. Bystritsky, and W. Katon. Pharmacotherapy of panic disorder:<br />
Guidelines for the family practitioner. Journal of the American Board of Family Practice<br />
11:282-290, 1998.<br />
F. B. Schoenfeld, C. R. Marmar, and T. C. Neylan. Current concepts in pharmacotherapy for<br />
posttraumatic stress disorder. Psychiatric Services 55:519-531, 2004.<br />
J. Sareen and M. B. Stein. Pharmacotherapy for anxiety disorders in the new millenium. Psychiatr<br />
Clin North Am 7:173-186, 2000.<br />
S. Seedat and M. B. Stein. Double-blind, placebo-controlled assessment of combined<br />
clonazepam with paroxetine compared with paroxetine monotherapy for generalized social<br />
anxiety disorder. J.Clin.Psychiatry 65 (2):244-248, 2004.<br />
D. J. Stein, M. Versiani, T. Hair, and R. Kumar. Efficacy of paroxetine for relapse prevention in<br />
social anxiety disorder: a 24-week study. Arch Gen Psychiatry 59:1111-1118, 2002.<br />
M. B. Stein, M. R. Liebowitz, R. B. Lydiard, W. Bushnell, and I. P. Gergel. Paroxetine treatment of<br />
generalized social anxiety disorder (social phobia): a randomized controlled trial. Journal of<br />
the American <strong>Medical</strong> Association 280:708-713, 1998.<br />
M. B. Stein, C. D. Sherbourne, M. G. Craske, A. Means-Christensen, A. Bystritsky, W. Katon, G.<br />
Sullivan, and P. P. Roy-Byrne. Quality of care for primary care patients with anxiety disorders.<br />
Am J Psychiatry 161:2230-2237, 2004.<br />
M. Van Ameringen, C. Allgulander, B. Bandelow, J. H. Greist, E. Hollander, S. A. Montgomery, D.<br />
J. Nutt, A. Okasha, M. H. Pollack, D. J. Stein, and R. P. Swinson. WCA recommendations for<br />
the long-term treatment of social phobia. CNS.Spectr. 8 (8 Suppl 1):40-52, 2003.
68<br />
13. Acknowledgments<br />
We are grateful for the consultation and advice of Jeanne Miranda PhD<br />
and David Takeuchi PhD who reviewed and provided comments regarding<br />
the section on working with ethnic minority and disadvantaged patients.<br />
We also wish to express our thanks to the many psychiatrists,<br />
psychologists, nurses, primary care physicians, other allied health<br />
professionals, and healthcare consumers who have shared their anxiety<br />
treatment experiences with us over the years. Although this manual is<br />
intended to strongly favor the implementation of evidence-based<br />
guidelines, the authors recognize that such guidelines are sorely lacking<br />
when it comes to the treatment of refractory anxiety disorders, in<br />
particular. Thus, many of the recommendations contained herein stem<br />
from the experiences of skilled clinicians, whose clinical wisdom is used to<br />
buttress the hard evidence when such evidence is lacking. We trust that<br />
this will be a temporary state, and that the evidence base will grow to fully<br />
meet the needs of practitioners in the years to come.<br />
We are also grateful to the physician-investigators at the University of<br />
Seattle and <strong>Group</strong> Health Cooperative in Seattle – including Jurgen<br />
Unutzer, Greg Simon, and Wayne Katon, among others – upon whose<br />
work in depression in primary care our own work in general, and this<br />
manual in principle, is patterned.<br />
This work was supported by NIMH grants to the authors.