Collaborative Atorvastatin Diabetes Study (CARDS) - Lipids Online
Collaborative Atorvastatin Diabetes Study (CARDS) - Lipids Online
Collaborative Atorvastatin Diabetes Study (CARDS) - Lipids Online
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Collaborative</strong> <strong>Atorvastatin</strong> <strong>Diabetes</strong> <strong>Study</strong> (<strong>CARDS</strong>)<br />
Commentary by Harold Bays, MD, FACP<br />
<strong>Collaborative</strong> <strong>Atorvastatin</strong> <strong>Diabetes</strong> <strong>Study</strong> (<strong>CARDS</strong>)<br />
Introduction<br />
According to the World Health Organization, approximately 200 million people worldwide currently have<br />
type 2 diabetes mellitus, a prevalence that has been predicted to increase to 366 million by 2030.<br />
Atherosclerotic coronary heart disease (CHD) is the most common cause of morbidity and mortality in<br />
patients with type 2 diabetes. Among diabetic patients, atherosclerosis accounts for about 80% of all<br />
mortality; three-quarters of these deaths are due to CHD, and one-quarter are due to cerebral or peripheral<br />
vascular disease. <strong>Diabetes</strong> mellitus is associated with a 2- to 4-fold increased risk of CHD, as well as an<br />
increased risk of dying after a myocardial infarction (MI) compared with patients without diabetes. In<br />
addition, there is a sizable increase in out-of-hospital mortality or sudden death even after the first MI.<br />
Given this CHD risk burden, the National Cholesterol Education Program (NCEP) Adult Treatment Panel<br />
(ATP) III has emphasized that patients with diabetes should be regarded as having CHD risk equivalent to<br />
that of patients with known CHD. Similarly, European guidelines on cardiovascular disease prevention<br />
note that the risk of developing an MI is the same for diabetic patients as it is for nondiabetic patients with<br />
a prior MI. Therefore, the same aggressive lipid treatment goals should be applied to both diabetic and<br />
CHD patients, even if the former have no evidence of existing CHD. While organizations such as the<br />
American <strong>Diabetes</strong> Association have suggested widespread statin use in virtually all patients with type 2<br />
diabetes, the clinical trial evidence suggesting the effectiveness and safety of lipid lowering for primary<br />
prevention in diabetes patients with lower levels of LDL-C has not been clear.<br />
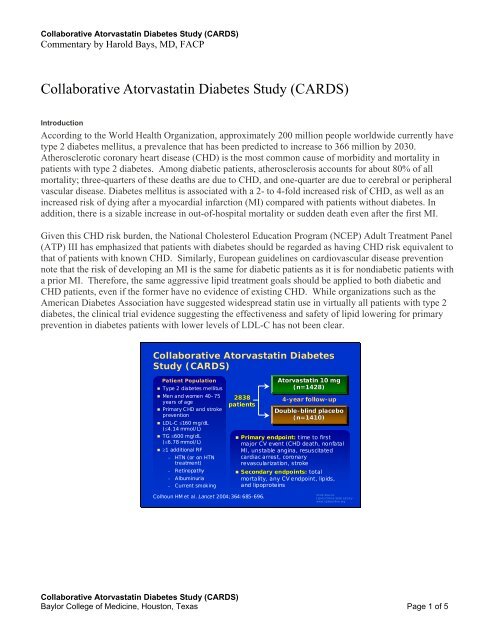
<strong>Collaborative</strong> <strong>Atorvastatin</strong> <strong>Diabetes</strong><br />
<strong>Study</strong> (<strong>CARDS</strong>)<br />
Patient Population<br />
• Type 2 diabetes mellitus<br />
• Men and women 40–75<br />
years of age<br />
• Primary C HD and stroke<br />
prevention<br />
• LDL-C ≤160 mg/dL<br />
(≤4.14 mmol/L)<br />
• TG ≤600 mg/dL<br />
(≤6.78 mmol/L)<br />
• ≥1 additional RF<br />
– HTN (or on HTN<br />
treatment)<br />
– Retinopathy<br />
– Albuminuria<br />
– Current smoking<br />
2838<br />
patients<br />
<strong>Atorvastatin</strong> 10 mg<br />
(n=1428)<br />
4-year follow-up<br />
Double-blind blind placebo<br />
(n=1410)<br />
• Primary endpoint: time to first<br />
major CV event (CHD death, nonfatal<br />
MI, unstable angina, resuscitated<br />
cardiac arrest, coronary<br />
revascularization, stroke<br />
• Secondary endpoints: total<br />
mortality, any CV endpoint, lipids,<br />
and lipoproteins<br />
Colhoun HM et al. Lancet 2004;364:685-696.<br />
Slide Source:<br />
<strong>Lipids</strong> <strong>Online</strong> Slide Library<br />
www.lipidsonline.org<br />
<strong>Collaborative</strong> <strong>Atorvastatin</strong> <strong>Diabetes</strong> <strong>Study</strong> (<strong>CARDS</strong>)<br />
Baylor College of Medicine, Houston, Texas Page 1 of 5
<strong>Collaborative</strong> <strong>Atorvastatin</strong> <strong>Diabetes</strong> <strong>Study</strong> (<strong>CARDS</strong>)<br />
Commentary by Harold Bays, MD, FACP<br />
<strong>CARDS</strong>: Patient Baseline Characteristics<br />
Age<br />
Mean (SD) years<br />
70<br />
Placebo<br />
(n = 1410)<br />
61.8 (8.0)<br />
529 (38%)<br />
708 (50%)<br />
173 (12%)<br />
Women<br />
453 (32%)<br />
White ethnicity<br />
1326 (94%)<br />
BMI<br />
Mean (SD), kg/m 2 28.8 (3.5)<br />
Obese (BMI >30 kg/m 2 ) 538 (38%)<br />
<strong>Atorvastatin</strong><br />
(n = 1428)<br />
61.5 (8.3)<br />
558 (39%)<br />
703 (49%)<br />
167 (12%)<br />
456 (32%)<br />
1350 (95%)<br />
28.7 (3.6)<br />
515 (36%)<br />
Colhoun HM et al. Lancet 2004;364:685-696.<br />
Reprinted with permission from Elsevier.<br />
Slide Source:<br />
<strong>Lipids</strong> <strong>Online</strong> Slide Library<br />
www.lipidsonline.org<br />
Key Points<br />
The <strong>Collaborative</strong> <strong>Atorvastatin</strong> <strong>Diabetes</strong> <strong>Study</strong> (<strong>CARDS</strong>) was a multicenter, randomized, placebocontrolled,<br />
4-year, double-blind trial of atorvastatin 10 mg/day that was the first to evaluate statin therapy<br />
prospectively and specifically in patients with type 2 diabetes. <strong>Study</strong> participants were patients aged 40–75<br />
years with type 2 diabetes, low-density lipoprotein cholesterol (LDL-C) concentration 160 mg/dL or less,<br />
fasting triglycerides 600 mg/dL or less, and at least one additional risk factor (hypertension, retinopathy,<br />
microalbuminuria or macroalbuminuria, or current smoking) but no history of CHD, cerebrovascular<br />
accident, or severe peripheral vascular disease. Randomization was completed in June 2001. Follow-up was<br />
initially planned to be endpoint driven, concluding after the occurrence of 304 primary endpoints.<br />
However, as a result of a significant benefit demonstrated by atorvastatin at an interim analysis, the<br />
independent steering committee of <strong>CARDS</strong> stopped the trial earlier than planned, after 149 primary<br />
endpoints.<br />
Of 4053 subjects screened, 3249 (80%) entered baseline assessment, and 2838 (70%) were randomized;<br />
1410 subjects were allocated placebo (1398 [99.1%] of whom completed follow-up) and1428 to<br />
atorvastatin 10 mg/day (1421 [99.5%] of whom completed follow-up). The median time of follow-up was<br />
3.9 years. Baseline characteristics were similar between treatment groups. During the course of the study,<br />
some placebo group subjects were administered nonstudy statin. The percentage of patients taking at least<br />
one lipid-lowering drug (including atorvastatin) in the atorvastatin group was 90%, 87%, 86%, and 78% at<br />
years 1, 2, 3, and 4, respectively, with an average of 85% atorvastatin use over the duration of the study.<br />
The percentage of patients taking at least one lipid-lowering drug in the placebo group was 2%, 7%, 12%,<br />
and 15% at years 1, 2, 3, and 4, respectively, with an average of 9% nonstudy drug use over the duration of<br />
the study.<br />
The group treated with atorvastatin 10 mg/day had an average 26% (54 mg/dL) reduction in total<br />
cholesterol and 40% (46 mg/dL) reduction in LDL-C. The average reduction in triglyceride levels was<br />
19%, with a 1% increase in HDL-C levels compared with placebo.<br />
The relative risk reduction in the primary endpoint of first acute CHD event (MI including silent infarction,<br />
unstable angina, acute CHD death, resuscitated cardiac arrest), coronary revascularization procedures, or<br />
<strong>Collaborative</strong> <strong>Atorvastatin</strong> <strong>Diabetes</strong> <strong>Study</strong> (<strong>CARDS</strong>)<br />
Baylor College of Medicine, Houston, Texas Page 2 of 5
<strong>Collaborative</strong> <strong>Atorvastatin</strong> <strong>Diabetes</strong> <strong>Study</strong> (<strong>CARDS</strong>)<br />
Commentary by Harold Bays, MD, FACP<br />
stroke (fatal or nonfatal) was significantly reduced by 37% with atorvastatin 10 mg/day compared with<br />
placebo (P=0.001). Stroke was significantly reduced by 48% (P=0.016) and all-cause mortality was<br />
reduced by 27% (P=0.059). The reduction in CHD, stroke, and mortality endpoints with atorvastatin may<br />
have been understated because (1) some of the placebo group received nonstudy statin treatment and (2) the<br />
trial was stopped 2 years early for ethical reasons. Had the trial been allowed to continue, the differences in<br />
CHD and stroke outcomes between treatment groups may have been greater.<br />
There was no difference in the overall frequency of adverse events or serious adverse events between the<br />
treatment groups. No cases of rhabdomyolysis were reported. One case of myopathy was reported in each<br />
group. Myalgia was reported in 72 and 61 patients in the placebo and atorvastatin groups, respectively. The<br />
number of patients who discontinued study drug because of muscle-related events was 9 in the placebo<br />
group and 7 in the atorvastatin group.<br />
<strong>CARDS</strong>: Patient Baseline <strong>Lipids</strong><br />
Total cholesterol (mg/dL)<br />
(mmol/L)<br />
LDL cholesterol (mg/dL)<br />
(mmol/L)<br />
HDL cholesterol (mg/dL)<br />
(mmol/L)<br />
Placebo<br />
(n = 1410)<br />
Mean (SD)<br />
207 (32)<br />
5.35 (0.82)<br />
117 (27)<br />
3.02 (0.70)<br />
55 (13)<br />
1.42 (0.34)<br />
<strong>Atorvastatin</strong><br />
(n = 1428)<br />
Mean (SD)<br />
207 (32)<br />
5.36 (0.83)<br />
118 (28)<br />
3.04 (0.72)<br />
54 (12)<br />
1.39 (0.32)<br />
Triglycerides* (mg/dL)<br />
(mmol/L)<br />
148 (104–212)<br />
1.67 (1.17–2.40)<br />
150 (106–212)<br />
1.70 (1.20–2.40)<br />
*Median (interquartile range)<br />
Colhoun HM et al. Lancet 2004;364:685-696.<br />
Reprinted with permission from Elsevier.<br />
Slide Source:<br />
<strong>Lipids</strong> <strong>Online</strong> Slide Library<br />
www.lipidsonline.org<br />
<strong>CARDS</strong>: Lipid Levels by Treatment<br />
Total Cholesterol (mg/dL)<br />
Average difference 26%,<br />
54 mg/dL; P
<strong>Collaborative</strong> <strong>Atorvastatin</strong> <strong>Diabetes</strong> <strong>Study</strong> (<strong>CARDS</strong>)<br />
Commentary by Harold Bays, MD, FACP<br />
<strong>CARDS</strong>: Effect of <strong>Atorvastatin</strong> on the Primary<br />
Endpoint: Major CV Events Including Stroke<br />
Cumulative Hazard, (%)<br />
Placebo<br />
<strong>Atorvastatin</strong><br />
15<br />
10<br />
5<br />
Relative Risk Reduction 37% (95% CI, 17–52)<br />
P = 0.001<br />
Placebo<br />
127 events<br />
0<br />
0 1 2 3 4<br />
Years<br />
1410<br />
1428<br />
1351<br />
1392<br />
Colhoun HM et al. Lancet 2004;364:685-696.<br />
Reprinted with permission from Elsevier.<br />
1306<br />
1361<br />
1022<br />
1074<br />
<strong>Atorvastatin</strong><br />
83 events<br />
651<br />
694<br />
4.75<br />
305<br />
328<br />
Slide Source:<br />
<strong>Lipids</strong> <strong>Online</strong> Slide Library<br />
www.lipidsonline.org<br />
<strong>CARDS</strong>: Adverse and Serious Adverse Events<br />
Type of Event<br />
Serious adverse event<br />
possibly associated<br />
with study drug<br />
Discontinued for AE<br />
Rhabdomyolysis<br />
Myopathy AE report<br />
CPK ≥10 × ULN<br />
ALT ≥3 × ULN<br />
AST ≥3 × ULN<br />
Patients (%) with Event<br />
Placebo<br />
(n = 1410)<br />
20 (1.1%)<br />
145 (10%)<br />
0<br />
1 (0.1%)<br />
10 (0.7%)<br />
14 (1%)<br />
4 (0.3%)<br />
<strong>Atorvastatin</strong> 10 mg<br />
(n = 1428)<br />
19 (1.1%)<br />
122 (9%)<br />
0<br />
1 (0.1%)<br />
2 (0.1%)<br />
17 (1%)<br />
6 (0.4%)<br />
Colhoun HM et al. Lancet 2004;364:685-696.<br />
Slide Source:<br />
<strong>Lipids</strong> <strong>Online</strong> Slide Library<br />
www.lipidsonline.org<br />
Implications and Clinical Relevance<br />
<strong>CARDS</strong> showed that in patients with type 2 diabetes mellitus with lower LDL-C levels, atorvastatin 10 mg<br />
daily was safe, well tolerated, and significantly efficacious in reducing the risk of first CHD events.<br />
<strong>CARDS</strong> supports recommendations such as that made by the American <strong>Diabetes</strong> Association that patients<br />
with type 2 diabetes mellitus should be considered as candidates for statin treatment—even at lower LDL-C<br />
levels. Subgroup analysis revealed that irrespective of whether the baseline LDL-C was at or above, or<br />
below the median of 120 mg/dL, atorvastatin patients in both subgroups had similar relative risk reductions<br />
of 37–38% for the primary endpoint.<br />
Previous support for the benefits of statin therapy in diabetes patients had been derived from the<br />
extrapolation of data from primary and secondary CHD prevention trials that included nondiabetic<br />
populations. Because <strong>CARDS</strong> was the first study to evaluate statin therapy prospectively and specifically<br />
in patients with type 2 diabetes mellitus, and because it was one of the few primary prevention trials<br />
<strong>Collaborative</strong> <strong>Atorvastatin</strong> <strong>Diabetes</strong> <strong>Study</strong> (<strong>CARDS</strong>)<br />
Baylor College of Medicine, Houston, Texas Page 4 of 5
<strong>Collaborative</strong> <strong>Atorvastatin</strong> <strong>Diabetes</strong> <strong>Study</strong> (<strong>CARDS</strong>)<br />
Commentary by Harold Bays, MD, FACP<br />
conducted, <strong>CARDS</strong> significantly adds to the data from post hoc analyses of other clinical trials that have<br />
shown efficacy in reducing CHD events in patients with type 2 diabetes mellitus with lipid-altering drugs.<br />
Primary Prevention Trials of Lipid-Altering<br />
Therapy Including Patients with <strong>Diabetes</strong><br />
Trial<br />
Diabetic,*<br />
n<br />
Total N<br />
in<br />
<strong>Study</strong><br />
Lipid-Altering<br />
Drug, mg/d<br />
CHD* Risk vs<br />
Placebo in Diabetic<br />
Patients, %<br />
<strong>CARDS</strong> †<br />
2,838<br />
2,838<br />
<strong>Atorvastatin</strong> 10<br />
–37 (p=.001)<br />
AFCAPS<br />
155<br />
6,605<br />
Lovastatin 20–40 ‡<br />
–44 (NS)<br />
HPS §<br />
2,912<br />
7,150<br />
Simvastatin 40<br />
–33 (p=.0003)<br />
ASCOT<br />
2,532<br />
10,305<br />
<strong>Atorvastatin</strong> 10<br />
–16 (NS)<br />
PROSPER<br />
623<br />
5,804<br />
Pravastatin 40<br />
+27 (NS)<br />
HHS<br />
135<br />
4,081<br />
Gemfibrozil 1200<br />
–68 (NS)<br />
* By history<br />
† Prospective trial in diabetic subjects; others are subgroup analyse s<br />
‡ Mean 30 mg/d<br />
§ Type 1 or 2 diabetes<br />
Bays H et al. Future Cardiology 2005;1:39-59. 59. | Colhoun HM et al. Lancet 2004;364:685-696. 696. |<br />
Downs JR et al. JAMA 1998;279:1615-1622. 1622. | HPS <strong>Collaborative</strong> Group. Lancet 2003;361:2005-<br />
2016. | Sever PS et al. Lancet 2003;361:1149-1158. 1158. | S hepherd J et al. Lancet 2002;360:1623-<br />
1630. | Koskinen P et al. <strong>Diabetes</strong> Care 1992;15:820-825. 825.<br />
Slide Source:<br />
<strong>Lipids</strong> <strong>Online</strong> Slide Library<br />
www.lipidsonline.org<br />
Secondary Prevention Trials of Lipid-Altering<br />
Therapy Including Patients with <strong>Diabetes</strong><br />
Total N<br />
Trial<br />
Diabetic,<br />
n<br />
in<br />
<strong>Study</strong><br />
4S<br />
Reanalysis<br />
202†<br />
483‡<br />
4,444<br />
CARE<br />
586† 4,159<br />
LIPID 1,077‡ 9,014<br />
LIPS §<br />
202† 1,677<br />
HPS § 3,051† 13,386<br />
4D <br />
1,255† 1,255<br />
VA-HIT 769‡ 2,351<br />
DAIS || 418† 418<br />
*Includes stroke in 4D and VA-HIT<br />
†By history<br />
‡By history or glucose ≥126 mg/dL<br />
CHD* Risk vs<br />
Lipid-A ltering Placebo in Diabetic<br />
Drug, mg/d<br />
Patients, %<br />
Simvastatin 20–40 –55 (p=.002)<br />
–42 (p=.001)<br />
Pravastatin 40 –25 (p=.05)<br />
Pravastatin 40 –19 (NS)<br />
Fluvastatin 80 –47 (p=.04)<br />
Simvastatin 40 –18 (p=.002)<br />
<strong>Atorvastatin</strong> 20 –8 (NS)<br />
Gemfibrozil 1,200 –32 (p=.004)<br />
Fenofibrate 200 –23 (NS)<br />
§ Type 1 or 2 diabetes<br />
Prospective trial in diabetic subjects; others<br />
are subgroup analyses<br />
|| Angiographic study<br />
Bays H et al. Future C ar diology 2005;1:39-59. 59. | Pyör älä K et al. Dia betes Car e 1997;20:614- 620. | Ha ffne r SM<br />
et al. Arch I ntern Med 1999; 159: 2661-2667. 2667. | Goldberg RB et al. Circ ulati on 1998;98:2513-2519. 2519. | KeechA et<br />
al. Di abetes Care 2003;26:2713-2721. 2721. | Serruys PWJ C et al. JAMA 2002;287:3215-3222. 3222. | HPS C ollabor ative<br />
Gro up. Lancet 2003;361:2005-2016. 2016. | Wanner C. Presented at AS N annual meeting, 2004. | Rubins HB et al.<br />
Arch Intern Med 2002;162:2597-2604. 2604. | DAIS Investigators. Lancet 2001;357:905-910. 910.<br />
Slide Source:<br />
<strong>Lipids</strong> <strong>Online</strong> Slide Library<br />
www.lipidsonline.org<br />
<strong>Collaborative</strong> <strong>Atorvastatin</strong> <strong>Diabetes</strong> <strong>Study</strong> (<strong>CARDS</strong>)<br />
Baylor College of Medicine, Houston, Texas Page 5 of 5