Nurses Day! - Birmingham Children's Hospital
Nurses Day! - Birmingham Children's Hospital
Nurses Day! - Birmingham Children's Hospital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
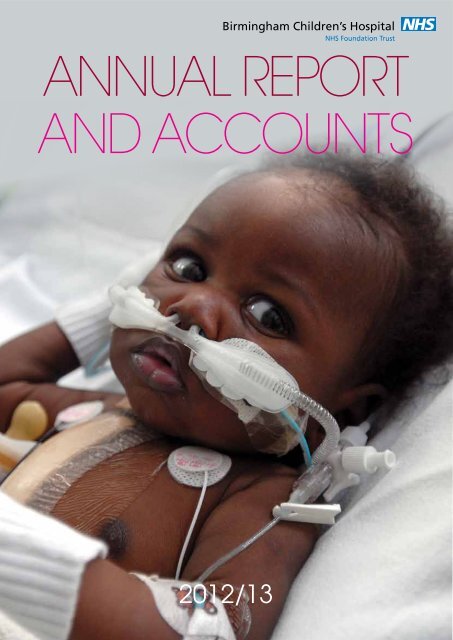
ANNUAL REPORT<br />
AND ACCOUNTS<br />
2012/13
ANNUAL REPORT VIDEOS<br />
CONTENTS<br />
To go to the section you want, click on the picture above it<br />
This year, to make our Annual Report more<br />
interactive and easy to digest, we are using video<br />
to tell the story of our year.<br />
To watch our short videos visit our hospital website<br />
www.bch.nhs.uk/corporate/annual-report<br />
or scan the QR code on this page.<br />
We have four videos available which show how<br />
we’ve performed against our strategic objectives<br />
throughout the year. These objectives help us<br />
focus on maintaining our high standards, improving<br />
them even further and planning for the future too.<br />
1. Chief Executive’s Introduction<br />
2. Delivering excellent care today<br />
3. Striving to make it even better<br />
4. Shaping excellent care for tomorrow<br />
When you see this icon on a page in<br />
Section One of the report, it means you<br />
can watch a film summarising the key<br />
points in that section.<br />
WATCH THE VIDEO<br />
INTRODUCTION<br />
Chairman & Chief Executive’s Foreword<br />
Who we are and what we do<br />
Our year at a glance<br />
SECTION THREE<br />
Our Quality Report<br />
SECTION ONE<br />
Our journey through the year<br />
SECTION FOUR<br />
Annual Governance Statement<br />
SECTION TWO<br />
The Governance of our Organisation<br />
SECTION FIVE<br />
Summary Financial Statements
INTRODUCTION<br />
WATCH THE VIDEO<br />
BACK TO CONTENTS PAGE<br />
Chairman & Chief Executive’s Foreword<br />
This year we proudly celebrated our hospital’s 150th anniversary – for 150 years we have<br />
been making a difference to the lives of countless children, young people and their families<br />
from <strong>Birmingham</strong>, the West Midlands, across the UK and beyond.<br />
We’ve taken the opportunity to look back at where<br />
we’ve come from, where we are today and where<br />
we want to be in the future. In true <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong> style we made sure it was a<br />
year we wouldn’t forget, with lots of events and<br />
activities to celebrate and reward our staff who<br />
work tirelessly, day in, day out, to provide excellent<br />
care to our children and young people. Without<br />
them, we wouldn’t be where we are today.<br />
Keith Lester,<br />
Interim Chairman<br />
However, amongst the<br />
celebrations we’ve<br />
also had our busiest<br />
year ever, with more<br />
patients than we’ve<br />
ever seen before.<br />
We have coped well<br />
by changing our<br />
patient pathways and<br />
making significant<br />
improvements to our<br />
facilities to make sure<br />
we can continue to deliver<br />
our high quality services<br />
to more patients.<br />
This includes<br />
the opening of our Paediatric Intensive Care Unit<br />
(PICU) extension, which increases our capacity<br />
to 26 beds and 31 by 2014, and the launch of<br />
our new outpatient pharmacy, which has made<br />
it significantly quicker and easier for families to<br />
collect their child’s medicine before they go home.<br />
These developments provide a strong foundation<br />
to develop our services for children and young<br />
people with serious heart problems. Congenital<br />
heart services are currently under national review<br />
and at the end of 2012/13 we await the final<br />
outcome.<br />
A number of innovative projects also came to<br />
fruition during the year to help us improve our<br />
services and patient experience, including our 24-<br />
hour Paediatric Assessment Clinical intervention<br />
and Education (PACE) team, which was launched<br />
to further support staff and parents of patients<br />
who they feel may be deteriorating. It has been<br />
a resounding success already and we look<br />
forward to seeing how the team develops further<br />
throughout the year.<br />
Supporting PACE is our revolutionary Parental<br />
Concern Project, funded by the Health Foundation,<br />
to look at how we can help parents play a more<br />
active role in their child’s care by developing an<br />
effective assessment tool which measures their<br />
levels of concern. This will continue into 2013/14.<br />
Our award-winning Maple food ordering system,<br />
which gives children and young people an easy<br />
way to choose the food they want and reduce food<br />
waste has been a big hit, as has our revolutionary<br />
new Feedback App for smart phones, which gives<br />
patients and families a new way to give instant<br />
feedback on their experiences, good or bad, and<br />
allows us to respond and make improvements in<br />
real-time.<br />
Another significant achievement has been our new<br />
Dignity Giving Suit. Working with staff, children<br />
and young people we have created a new outfit<br />
to replace the traditional backless hospital gown<br />
to give our young patients more dignity during all<br />
stages of their care. The impact has already been<br />
huge and some of our patients love them so much<br />
they want to take them home!<br />
Health Promotion has been an important theme<br />
throughout the year for our patients, families and<br />
our 3,300 staff. We’re leading the way regionally<br />
and nationally with our work on the Making Every<br />
Contact Count initiative to use every opportunity<br />
we have with patients and families to deliver<br />
brief health advice. We have also launched our<br />
staff Health and Wellbeing Strategy which details<br />
our commitment to supporting staff with fun and<br />
interactive ways to stay happy and healthy.<br />
We’ve also welcomed a number of high profile<br />
visitors to our hospital during the year. Health<br />
Minister Dr Dan Poulter came to speak to ward<br />
staff about our feedback app and hear how our<br />
Safer Children Audit No Harm initiative (SCAN) is<br />
helping to reduce harm, and Lord Howe came to<br />
learn more about our groundbreaking work in the<br />
field of rare diseases. Secretary of State Andrew<br />
Lansley officially launched our £3.7m 3T MRI<br />
scanner on the 64th anniversary of the NHS and<br />
Prime Minister David Cameron visited a few weeks<br />
later to spend time with our nursing teams on their<br />
ward rounds following the publication of the new<br />
Nursing and Care Quality Forum report in May.<br />
But of course this year has been a landmark<br />
year for the NHS with Sir Robert Francis QC’s<br />
final report into failings at Mid Staffordshire NHS<br />
Foundation Trust. It has given every organisation<br />
the opportunity to pause and think about the<br />
services we provide. We have responded by<br />
generating a large scale discussion across<br />
the Trust to see how we can make further<br />
improvements to ensure we continue to provide<br />
high quality, dignified care at all times. This will<br />
conclude in September 2013 and we already have<br />
some powerful material from staff which we can<br />
act upon to improve patient care further.<br />
Nationally, the NHS has been preparing for<br />
major changes to the way that local and national<br />
specialised services are commissioned. This has<br />
led to the development of fewer larger specialist<br />
centres with more expert staff who can better<br />
treat rare conditions and improve outcomes. It’s<br />
a mark of the clinical excellence at <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong> that we have been designated<br />
as a specialist centre for both epilepsy surgery and<br />
major trauma.<br />
4 5<br />
Looking forward, we know we face a growing<br />
population of younger people across the West<br />
Midlands over the next few years. Teamed with<br />
a worrying trend of conditions like asthma and<br />
obesity, developments in medical technology<br />
and an increase in demand for our specialised<br />
services, we know we will be treating lots more<br />
children and young people in the near future.<br />
To make sure that we have the world-class<br />
facilities that our children, young people and<br />
families need and deserve, we have been busy<br />
exploring options for a new hospital, either at<br />
Steelhouse Lane or alongside our partners at<br />
the Queen Elizabeth <strong>Hospital</strong> and <strong>Birmingham</strong><br />
Women’s <strong>Hospital</strong> in Edgbaston. There is still a lot<br />
more work to be done on this, which will continue<br />
throughout the year, and we will be working closely<br />
with staff, our patients and families and partners to<br />
make sure we get this important decision right.<br />
The NHS, like the rest of the public sector, is<br />
facing severe financial pressures as a result of<br />
the national economic situation. During 2012/13<br />
we made over £8 million of efficiency savings. In<br />
2013/14 we will work with our staff to ensure that<br />
we can continue to deliver this level of savings as<br />
the financial challenges are set to continue.<br />
We’ve had another very exciting year at<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong><br />
with many significant<br />
developments, achievements<br />
and plans in place for a<br />
great future.<br />
We are well on our<br />
way to achieving<br />
our vision of<br />
becoming the<br />
leading children’s<br />
healthcare provider<br />
and look forward<br />
to continuing our<br />
hospital’s great<br />
legacy for another<br />
150 years to<br />
come.<br />
David Melbourne,<br />
Interim Chief Executive
6 7<br />
BACK TO CONTENTS PAGE<br />
Who we are and what we do<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation Trust provides the widest range of children’s health<br />
services for young patients from <strong>Birmingham</strong>, the West Midlands and beyond, with over 240,000 patient<br />
visits every year.<br />
We are a nationally designated specialist centre for epilepsy surgery and a trauma centre for the West<br />
Midlands, a national transplant centre, and a centre of excellence for complex heart conditions, the<br />
treatment of burns, cancer, and liver and kidney disease. We also have one of the largest Child and<br />
Adolescent Mental Health Services in the country with a dedicated Eating Disorder Unit and Acute<br />
Assessment Unit for regional referrals of children and young people with the most serious problems (Tier 4).<br />
Our hospital has:<br />
l 354 beds across 22 wards at Steelhouse Lane<br />
and our Child and Adolescent Mental Health<br />
(CAMHS) site at Parkview;<br />
l 34 specialties (including liver transplant surgery,<br />
cardiac surgery, burns, major trauma,<br />
craniofacial surgery, blood and marrow<br />
transplantation, specialised respiratory and<br />
dermatology, neurology, cystic fibrosis, Child and<br />
Adolescent Mental Health Services);<br />
l 11 Nationally Commissioned Services;<br />
l 12 theatres (including our Hybrid and<br />
Laparoscopic theatres);<br />
l £3.7m 3T MRI scanner which supports<br />
pioneering research into brain tumours in<br />
children;<br />
l 150,000 outpatient visits a year;<br />
l 50,000 Emergency Department patients a year;<br />
l 39,000 inpatient admissions to hospital each year;<br />
l 61 parent and family accommodation rooms –<br />
the largest facility in Europe;<br />
l KIDS regional emergency transport service;<br />
l Wellcome Clinical Research Facility;<br />
l 26 bedded PICU (to increase to 31 next year);<br />
l £233m annual income;<br />
l 3,330 staff.<br />
Education<br />
As one of the UK’s leading paediatric teaching<br />
centres we go to great lengths to target, teach,<br />
nurture and develop the skills of our present and<br />
future workforce, to enable access to training and<br />
education and to foster life-long learning. Our aim<br />
is that all staff are appropriately equipped and<br />
qualified for the work they do and continue to learn<br />
and develop in their time with us. We continually<br />
examine our practice and look at ways to innovate<br />
and improve the service we all deliver so that our<br />
children, young people and families receive a firstclass<br />
service.<br />
Research<br />
Research is a fundamental part of what we do<br />
at the hospital and we are leading the way with<br />
pioneering international research into:<br />
l Childhood cancer;<br />
l Inherited metabolic disorders / rare diseases;<br />
l Liver disease;<br />
l Infection, inflammation and immunity;<br />
l Nutrition, growth and metabolism in childhood;<br />
l Drug use in children;<br />
l Relapsed and refractory acute lymphoblastic<br />
leukaemia;<br />
l Infant neuroblastoma; Infant brain tumours.
BACK TO CONTENTS PAGE<br />
Our<br />
Mission<br />
Our<br />
Vision<br />
Our<br />
Values<br />
To provide outstanding care and treatment to all<br />
children and young people who choose and need<br />
to use our services, and to share and spread new<br />
knowledge and practice, so we are always at the<br />
forefront of what is possible.<br />
To be the leading provider of healthcare for<br />
children and young people, giving them care and<br />
support – whatever treatment they need – in a<br />
hospital without walls.<br />
We know that organisations which have strong<br />
values and behaviours do well and that employees<br />
are engaged, happy and motivated in their work.<br />
We’ve worked closely with staff to develop and<br />
embed our values in all that we do at <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong> and we will continue to ensure<br />
that they underpin the way we care for our patients<br />
and each other.<br />
To help us do this, we have six strategic objectives which focus us on where we<br />
are now and what we want to achieve in<br />
Delivering excellent<br />
care today...<br />
Every child<br />
and young<br />
person<br />
requiring<br />
access<br />
to care at<br />
<strong>Birmingham</strong><br />
Children’s<br />
<strong>Hospital</strong> will<br />
be admitted<br />
in a timely<br />
way, with no<br />
unneccessary<br />
waiting along<br />
their pathway<br />
Every child<br />
and young<br />
person<br />
cared for by<br />
<strong>Birmingham</strong><br />
Children’s<br />
<strong>Hospital</strong> will<br />
be provided<br />
with safe,<br />
high quality<br />
care, and<br />
a fantastic<br />
patient<br />
and family<br />
experience<br />
Striving to make it<br />
even better...<br />
Every<br />
member<br />
of staff<br />
working for<br />
<strong>Birmingham</strong><br />
Children’s<br />
<strong>Hospital</strong> will<br />
be looking<br />
for, and<br />
delivering<br />
better ways<br />
of providing<br />
outstanding<br />
care, at better<br />
value<br />
Every<br />
member<br />
of staff<br />
working for<br />
<strong>Birmingham</strong><br />
Children’s<br />
<strong>Hospital</strong><br />
will be a<br />
champion for<br />
children and<br />
young people<br />
Shaping excellent care<br />
for tomorrow...<br />
We will<br />
strengthen<br />
<strong>Birmingham</strong><br />
Children’s<br />
<strong>Hospital</strong> as<br />
a provider of<br />
Specialised<br />
and Highly<br />
Specialised<br />
Services,<br />
so that we<br />
become<br />
the leading<br />
provider of<br />
children’s<br />
healthcare<br />
in the UK<br />
Our ‘journey through the year’ section from page 12 details how<br />
we’ve been delivering against each of these strategic objectives.<br />
We will<br />
continue<br />
to develop<br />
<strong>Birmingham</strong><br />
Children’s<br />
<strong>Hospital</strong> as<br />
a provider of<br />
outstanding<br />
local<br />
services:<br />
‘a hospital<br />
without<br />
walls’,<br />
working<br />
in close<br />
partnership<br />
with other<br />
organisations<br />
Trust<br />
Patients and families will trust us to have the<br />
knowledge and ability to give them the very highest<br />
quality of care, and as colleagues we will trust<br />
each other to our jobs well.<br />
Commitment<br />
We will always show commitment to achieving the<br />
very best possible outcomes for our patients and<br />
families, working collaboratively with colleagues to<br />
achieve this.<br />
Compassion<br />
We will always be friendly, approachable and alert<br />
to what our patients, families and colleagues need.<br />
Courage<br />
We will always have the courage to stand up for<br />
what is right, raise concerns, challenge the status<br />
quo and improve care at all times.<br />
Respect<br />
Whatever the needs or beliefs of our children,<br />
young people and families, we will always do all we<br />
can to tailor their care and make their experience a<br />
good one. As colleagues we will respect and value<br />
differences to create a great place to work.<br />
8 9
BACK TO CONTENTS PAGE<br />
Our year at a glance<br />
April May June<br />
July<br />
Oct<br />
Prime Minister David<br />
Cameron joined<br />
nursing teams on ward<br />
rounds, sparked by<br />
the publication of the<br />
new Nursing and Care<br />
Quality Forum report<br />
Our hospital’s<br />
150th<br />
birthday!<br />
Our £4m Children’s<br />
Cancer Centre<br />
fundraising appeal<br />
launched<br />
BCH<br />
Cardiac Surgeon,<br />
Mr David Barron,<br />
became an<br />
ITV <strong>Day</strong>break<br />
Health Hero<br />
Sec of State Andrew Lansley<br />
launches our<br />
£3.7m 3T MRI scanner<br />
<strong>Nurses</strong> <strong>Day</strong>!<br />
Celebrating the<br />
outstanding<br />
contribution of our<br />
nursing teams<br />
Nov Dec Jan Feb March<br />
BCH becomes a regional epilepsy surgery centre<br />
Our new outpatient<br />
pharmacy, the<br />
Medicine Chest,<br />
opens to patients<br />
and families<br />
Launch of our<br />
Dignity Giving<br />
Suits<br />
Doors open to our new<br />
Paediatric Intensive Care Unit,<br />
making us the largest unit in the country<br />
JLS gives<br />
some of our<br />
special<br />
young patients<br />
a Christmas<br />
to remember<br />
Launch of our patient<br />
and family feedback<br />
app – an NHS first<br />
10 11
SECTION ONE<br />
WATCH THE VIDEO<br />
BACK TO CONTENTS PAGE<br />
Our journey through the year<br />
Delivering excellent care today<br />
Every child and young person requiring access to care at <strong>Birmingham</strong> Children’s <strong>Hospital</strong><br />
will be admitted in a timely way, with no unnecessary waiting along their pathway.<br />
For yet another year running, the number of<br />
children and young people who used <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong> has grown. We’ve worked hard<br />
during the year to develop and grow our services<br />
so that we can continue to provide world-class<br />
care for all of our children and young people, and<br />
more quickly, whether this be in our hospital, at our<br />
Child and Adolescent Mental Health Service at our<br />
Parkview site in Moseley, out in the community or<br />
at home.<br />
As one of the country’s leading specialist hospitals,<br />
lots of children and young people with very serious<br />
or life-threatening conditions come to us in need<br />
of care from our specialist teams in theatres and<br />
intensive care. This unfortunately means that from<br />
time to time we have to reschedule less urgent<br />
procedures.<br />
Nobody wants to wait a long time to see a doctor<br />
or consultant or have an operation cancelled,<br />
so over the last year we have made significant<br />
changes to the way we work to help reduce our<br />
waiting times.<br />
We’ve created space for an extra 11 beds in our<br />
brand new, bright and modern Paediatric Intensive<br />
Care Unit (PICU) extension which opened in<br />
November 2012. The unit also includes a new<br />
breast feeding room, two parents’ rooms, a<br />
bedroom and a reception area.<br />
This increases our total capacity to 31 beds, 26 of<br />
which are open now, which will make us the largest<br />
single site unit in the UK. This means we can care<br />
for more of the sickest children and young people<br />
who need our help every year and reduce the wait<br />
for surgery.<br />
Our new £2.1m Paediatric Assessment Unit (PAU),<br />
which opened in February 2012, has been a<br />
resounding success and has gone from strength to<br />
strength throughout the year.<br />
Built in the space which formed the old ward 14,<br />
PAU offers a place for children and young people<br />
needing short medical or surgical admissions to<br />
the hospital (around 24 hours or less), making<br />
access to care quicker and ensuring they get the<br />
right treatment and care in the right place, at the<br />
right time.<br />
This is an important stage in the development<br />
of our emergency care pathway which provides<br />
a much better patient experience overall by<br />
improving patient flows through the hospital as<br />
these patients don’t need to be managed alongside<br />
highly complex patients on other hospital wards.<br />
We are really proud that we have been able<br />
to maintain our high standards of care whilst<br />
increasing our capacity and flow, which is evident<br />
in the positive patient feedback we regularly<br />
receive from our children, young people and<br />
families.<br />
Our Kids Intensive Care and Decision Support<br />
service (KIDS) has gone from strength to strength<br />
with another extremely busy year.<br />
The 24/7 service, which specialises in the<br />
management of critically ill children presenting to<br />
their local hospitals and during transfer to intensive<br />
care, moved to a new bespoke operations centre<br />
with state of the art telecommunications in May<br />
2012. St John Ambulances and drivers are now<br />
onsite with the KIDS team which has dramatically<br />
reduced the KIDS mobilisation time and allows<br />
even closer team working.<br />
12 13<br />
This is the first time I’ve been to children’s with my<br />
little boy I can’t thank the staff enough! They are so,<br />
so polite and kind you forget you’re in a hospital.<br />
Amazing people and place, sounds like I’m talking<br />
about Disneyland lol. I will be talking about it for<br />
weeks to come.
BACK TO CONTENTS PAGE<br />
Having extensively used the KIDS Service over this weekend, I just wanted<br />
to thank you for such a fantastic service that you all provide. It is not just the<br />
securing of intensive care beds and retrieval, but more importantly the support<br />
provided to the paediatricians throughout the region does not make them feel<br />
isolated when faced with a very sick child – I think this is the most valuable part<br />
of the service.<br />
At a time when reconfiguration of children’s services is high on the agenda with<br />
proposed fewer inpatient units, the model that KIDS provides for supporting sick<br />
children and healthcare professionals away from the major centres provides an<br />
excellent model for emulation.<br />
Dr Sanjeev Deshpande,<br />
Consultant Neonatologist, Royal Shrewsbury <strong>Hospital</strong><br />
During 2012/13 the service received 1,668<br />
referrals (an increase of 354 from 2011/12) for<br />
advice and transport of young patients between<br />
local hospitals and children’s intensive care units<br />
in the Midlands, as well as to and from other units<br />
across the UK. Of these, 1,275 were transported -<br />
815 by KIDS and 456 on request by KIDS to other<br />
teams.<br />
Another 400 patients received advice and input<br />
from a KIDS consultant which allowed them to<br />
remain at their local hospital. Feedback from these<br />
hospitals has been very positive. Parents and<br />
carers of children who were able to travel with their<br />
child to PICU in our new ambulances have told us<br />
We’ve also had the builders in this year to create<br />
a new state-of-the-art outpatient pharmacy, the<br />
Medicine Chest, which is making it quicker and<br />
easier for families to collect their prescription onsite<br />
before they go home.<br />
The brand new facility, which opened in January, is<br />
bright, modern and child-friendly and gives families<br />
access to specialist paediatric pharmacists to talk<br />
14 15<br />
about their child’s medicine. It’s also home to a<br />
high-tech automated robot which selects medicines<br />
for dispensing.<br />
Having our own dedicated outpatient pharmacy<br />
means we can supply the most suitable medicines<br />
based on our prescriptions which are tailored<br />
specifically for children, ensuring they are of<br />
the highest quality and cost effective. Since we<br />
opened, waiting times have reduced dramatically<br />
from 45 minutes to an average of just 12 which<br />
means our families can get home quicker.
16 17<br />
BACK TO CONTENTS PAGE<br />
Delivering excellent care today<br />
Every child and young person cared for by <strong>Birmingham</strong> Children’s <strong>Hospital</strong> will be<br />
provided with safe, high quality care, and a fantastic patient and family experience.<br />
Children, young people and their families have a<br />
right to be treated in a safe environment where no<br />
avoidable harm is suffered. We want to be a place<br />
where safety is everyone’s top priority and this is<br />
reflected in our Safety Strategy.<br />
Our strategy sets challenging annual targets<br />
to measure our progress and the effectiveness<br />
of interventions. The 2012/13 targets included<br />
avoidable pressure ulcers, medication incidents<br />
resulting in harm, Central Venous Catheter (CVC)<br />
related blood stream infections and life threatening<br />
events which could have been predicted and<br />
prevented. A detailed breakdown of these safety<br />
targets and the results ccan be found in the Quality<br />
Report from page 92.<br />
We’re really pleased with how we are doing but<br />
know that there is always more we can to do<br />
improve patient safety. We will continue to monitor<br />
our progress against these targets to ensure that<br />
we work towards eliminating avoidable harm at<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong>.<br />
Listening to what our children, young people and<br />
families tell us is something that we’re good at.<br />
Over the year we’ve continued to work hard to<br />
embed patient experience into our daily practice<br />
and we are leading the way with our active<br />
participation and engagement with children and<br />
young people.<br />
We have seen the visibility and influence of our<br />
Young Person’s Advisory Group (YPAG) continue<br />
to grow and they have played a key role in decision<br />
making and planning at the hospital as well as<br />
nationally. They have helped plan our Annual Staff<br />
Awards and presented at our AGM in September,<br />
helped us redesign our outpatients area and<br />
theatres and played an important part in the second<br />
consultation with Professor Steve Field about the<br />
role of young people in the NHS Constitution. Plans<br />
are also underway, in collaboration with the Royal<br />
College of Paediatrics and Child Health (RCPCH)<br />
and National Youth Symposium to be held later in<br />
2013 or early 2014.
18 19<br />
BACK TO CONTENTS PAGE<br />
Since April 2012, in preparation for the Department<br />
of Health’s national Friends and Family test, which<br />
commenced in April 2013, we have been asking<br />
parents and carers on their day of discharge how<br />
likely it is they would recommend the hospital<br />
to friends or family. A ‘net promoter’ score is<br />
generated from their responses.<br />
We have asked almost 2,000 parents and carers<br />
and saw a rapid rise from an initial score of 52 to 81<br />
in June 2012 where it has since stayed consistently<br />
within the top quartile score of all acute trusts<br />
across the NHS Midlands and East region.<br />
But as we are a children’s hospital we want to find<br />
out what children and young people think about our<br />
hospital too, so in addition to parents and carers we<br />
introduced a young person’s version of the question<br />
at the same time. 97% of children and young<br />
people ‘agree a bit’ or ‘agree a lot’ that they would<br />
tell their friends and family that this was a good<br />
hospital.<br />
But no matter what we score on the Friends and<br />
Family test we never stop doing all that we can to<br />
improve the way we do things.<br />
We want our patient experience programme<br />
to provide mechanisms and processes<br />
that enable every child and young<br />
person, from all cultures and backgrounds, to tell<br />
us in a way they want to about their experience<br />
of the hospital and their care to influence future<br />
development, design and delivery for all children<br />
and young people. This is why we use a toolkit<br />
approach which includes verbal feedback, mystery<br />
shoppers, focus groups, email and text messaging,<br />
feedback cards, patient experience walkabouts,<br />
creative arts and much more.<br />
Most importantly, it remains our objective to put the<br />
child, young person and family at the heart of all<br />
we do, ensuring that we listen to and respond to<br />
what they are telling us. With that in mind we have<br />
developed and launched our new <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong> Feedback app to make patient<br />
and family feedback quicker, easier and more<br />
effective than ever before.<br />
The app is the first of its type in the NHS and<br />
enables patients and families to interact with us<br />
in an innovative new way and send their thoughts<br />
and comments directly to the ward or area they<br />
have visited with the simple click of a button.<br />
The anonymous message goes straight to the<br />
manager in charge so it can be addressed in realtime<br />
and also goes unedited on our website so that<br />
other people can benefit from reading it too.<br />
The messages and comments from the app,<br />
alongside our feedback cards, texts and emails,<br />
is collated, reviewed and analysed to pick up any<br />
emerging themes or issues that we need to take<br />
action on.<br />
Following a pilot on two of our wards, we have<br />
rolled the app out across the Trust and have had<br />
hundreds of messages through so far. The vast<br />
majority have been positive, which is great as it’s<br />
important that we celebrate a job well done by our<br />
teams, but we’ve also had constructive feedback<br />
about improvements that we can make too.<br />
One parent used the app to let us know that the<br />
lock on the toilet door was sticking and another<br />
suggested some improvements we could make<br />
to the disabled facilities on one of wards, which<br />
is something we’re looking into as part of future<br />
developments.
20 21<br />
20 21<br />
Case study<br />
BACK TO CONTENTS PAGE<br />
Parents of two year old Lola, Paul Dolan and<br />
Michelle Cook from Redditch in Worcestershire,<br />
used the app for the first time on one of our surgical wards.<br />
Technology is always changing and this is a<br />
great way to give comments about how you<br />
feel as a parent and it lets the hospital know<br />
about the great work they’re doing too.<br />
It was really easy to download the app and give our<br />
feedback and I got a message back from the ward<br />
manager within an hour, which was great. It’s good to<br />
know that someone’s taking what you say seriously<br />
and is there to act on your feedback straightaway.
BACK TO CONTENTS PAGE<br />
Another project we’ve worked on to improve<br />
our patient experience has been to redesign the<br />
traditional backless and fiddly NHS hospital gown.<br />
The dignity of our patients is so important to us<br />
and we want our children and young people to<br />
feel comfortable and secure while they’re with<br />
us. Throughout the year we’ve been working with<br />
young people and fashion industry experts to<br />
produce our innovative new Dignity Giving Suits<br />
which protects our patients’ modesty while allowing<br />
quick, easy and dignified access for their procedure<br />
and follow-up care.<br />
A short sleeved top and cut-off trousers is joined<br />
with Velcro at several key points so it can be used<br />
in every possible theatre and post-operative care<br />
scenario. This could be for complex heart surgery,<br />
the insertion of a neck line or hernia repair, or<br />
accessing a plaster cast on a broken arm.<br />
Based entirely on the needs of our<br />
young patients and their clinical<br />
requirements, the innovative<br />
design is the first of its type in<br />
the NHS, truly fit-for-purpose<br />
and something we know that<br />
children and young people<br />
want. Since its launch in<br />
February 2013 we’ve<br />
had lots of interest from<br />
hospitals around the UK<br />
about how they can use<br />
the suits too.<br />
WATCH THE VIDEO<br />
Artist’s <strong>Birmingham</strong> impression Children’s of the respiratory <strong>Hospital</strong>—Sleep centre’s Room— sleep testing Respiratory room Services<br />
Job no. 4271<br />
Option A<br />
In January we started work on a six-month project<br />
to improve the patient and family experience for<br />
children and young people with lung problems,<br />
such as cystic fibrosis, sleep disordered breathing,<br />
asthma and those who may be oxygen and<br />
ventilator dependant.<br />
Thanks to a £500k donation to the hospital’s charity<br />
from a local newspaper, The Sunday Mercury,<br />
we have been able to start work on our new<br />
Respiratory Centre, which brings all our respiratory<br />
services together in one location, rather than being<br />
spread across the hospital site.<br />
The modern unit will have a second lung function<br />
testing area, a counselling room and three purpose<br />
built sleep testing bedrooms.<br />
Sleep disruption or deprivation can be caused by<br />
a vast number of different conditions and can have<br />
a real impact on a child or young person’s school<br />
life and behaviour. The sleep testing rooms will<br />
be decorated just like a child’s bedroom at home<br />
so they feel relaxed and comfortable which will<br />
improve the way our doctors can monitor their<br />
breathing and how it affects their sleep.<br />
We’ve also made changes and improvements over<br />
at our Child and Adolescent Mental Health Service<br />
(CAMHS) Parkview site too.<br />
22 23<br />
Last year we opened our Irwin Ward – a dedicated<br />
inpatient eating disorder unit which is helping our<br />
patients get quicker and better access to treatment.<br />
The 12 bedded unit is one of only four specialist<br />
centres of its type in the NHS which treats 12 to 18<br />
year olds. Since it opened we are pleased to report<br />
a 100% success rate in helping 20 young people<br />
with eating disorders get back to a healthy weight.<br />
This success is testament to the team’s<br />
commitment to not only working with the young<br />
people themselves but their families too. We expect<br />
parents to play a key part in the recovery process<br />
as they know them best and can help hugely while<br />
they are with us, as well as when they’re back at<br />
home, so they can regain control over their lives.<br />
Also at Parkview we ran a successful 12-month<br />
pilot to trial a Place of Safety - a specialised suite<br />
for young people who are detained by police under<br />
the Mental Health Act. The Place of Safety provides<br />
a comfortable and safe alternative to a police cell,<br />
which we know has a detrimental and negative<br />
impact on them and their families in a time of crisis.<br />
The pilot has gone well, with several young people<br />
accessing the Place of Safety over the last 12<br />
months. Future development plans for the Parkview<br />
site include a specially designed suite attached to<br />
one of the inpatient units so that we can ensure<br />
our young patients in need receive an excellent<br />
standard of care in the best environment possible.
WATCH THE VIDEO<br />
BACK TO CONTENTS PAGE<br />
Striving to make it even better<br />
Every member of staff working for <strong>Birmingham</strong> Children’s <strong>Hospital</strong> will be looking for and<br />
delivering better ways of providing outstanding care, at better value.<br />
Every day our staff go the extra mile to meet our<br />
strategic objectives of delivering excellent care and<br />
our incredibly talented workforce have taken the<br />
initiative to design and deliver a number of projects<br />
over the year which are already reaping rewards<br />
and leading the way on a national scale.<br />
In January we launched our Paediatric Assessment<br />
Clinical intervention and Education (PACE) team<br />
to give ward staff and parents an additional 24-<br />
hour support service for patients they feel may be<br />
deteriorating but don’t necessarily require intensive<br />
care, or when they are particularly worried about a<br />
child’s condition.<br />
The PACE team acts as an advocate for nurses<br />
and parents with concerns. The strong relationship<br />
they have with senior nursing and medical staff in<br />
our Paediatric Intensive Care Unit (PICU) means<br />
that they are able to escalate concerns quickly and<br />
effectively so that the child is assessed as early as<br />
possible.<br />
In the first two months of operation, the PACE team<br />
saw an average of 30 children a week and both<br />
staff and parents have really seen the benefits.<br />
They feel that their concerns have been listened to<br />
and addressed more effectively and deteriorating<br />
children were helped more quickly. Children are<br />
also coming out of PICU earlier because the ward<br />
staff have felt well supported to care for highly<br />
dependent children, freeing up more bed spaces for<br />
our sickest children.<br />
24 25<br />
Complementary to PACE is another innovative<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> project - the<br />
Parental Concern Project – funded by the Health<br />
Foundation’s Shine programme.<br />
Parents have a unique insight about their child’s<br />
health and we take their concerns just as seriously<br />
as other healthcare observations. We value their<br />
views and involve them in the decision making<br />
processes about their child’s care as much as<br />
possible but do recognise that families sometimes<br />
feel that their concerns aren’t listened to with the<br />
seriousness that they would like. This important<br />
project is looking at how we can develop an<br />
observation framework to help parents play a more<br />
active role in their child’s care.<br />
There is currently no assessment tool available<br />
within the NHS to capture parental observations<br />
about when a child might not be ‘themselves’.<br />
Instead we rely on verbal communication between<br />
clinical teams and families around particular<br />
observations, which can sometimes be open to<br />
interpretation around the level of concern and the<br />
appropriate resulting action.<br />
Throughout 2013 the project team will continue to<br />
work with families to develop and test approaches,<br />
put ideas into practice and gather evidence about<br />
what works and what doesn’t, with high hopes that<br />
the outcomes will act as a blueprint for other health<br />
organisations across the UK.
Striving to make it even better<br />
Every member of staff working for <strong>Birmingham</strong> Children’s <strong>Hospital</strong> will be a champion for<br />
children and young people.<br />
We are incredibly proud of our staff at <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong> who day in, day out, deliver<br />
outstanding patient care to our children, young<br />
people and families.<br />
This year has seen the launch of our People<br />
Strategy which sets out to staff how we will support<br />
them now and in the future, bringing together four<br />
key areas:<br />
1. Developing our People<br />
Our staff have established an outstanding<br />
reputation for care and innovative advances in<br />
research, teaching and technology in <strong>Birmingham</strong>,<br />
the West Midlands, UK and overseas.<br />
We offer excellent education with robust<br />
frameworks to assure the quality of delivery and<br />
assessment. Our portfolio includes accreditation<br />
status for the Institute of Leadership and<br />
Management and our own Vocational Centre<br />
– BCH Live - where we provide access to<br />
apprenticeships for new and existing staff. During<br />
the year we have also expanded our range of<br />
e-learning materials enabling staff to access<br />
learning more flexibly.<br />
We continue to create and embed a culture of<br />
continuous learning so that all staff have the<br />
opportunity to reach their full potential while<br />
enabling us to develop new roles and ways of<br />
working.<br />
2. Managing our People<br />
We have continued to grow our workforce<br />
throughout the year in line with the increased<br />
demand for our services and have redesigned the<br />
way some are delivered so that staff feel more<br />
satisfied about the contribution they make.<br />
We currently employ 3,330 people and at the end<br />
of March 2013 our staff turnover rate was 7.95% -<br />
well within our target of 9%.<br />
Through the Business Planning processes we<br />
have reviewed each service and anticipated where<br />
potential changes in supply and demand of staff<br />
may impact on us in the future. For example, over<br />
the next two years we plan to invest in Nurse<br />
Practitioner roles as we know the number of junior<br />
doctors will reduce in the coming years. This means<br />
we need to consider how we deliver our core<br />
business in alternative ways to ensure our patients<br />
and families continue to get the very best health<br />
care and support.<br />
BACK TO CONTENTS PAGE<br />
Involving staff in changes to the workplace has<br />
been a key focus this year. Our 2012 NHS Staff<br />
Survey showed that we are improving, with 54%<br />
of staff who responded agreeing that they feel<br />
involved in changes that affect their work/area and<br />
department, compared to 46% in 2011.<br />
We have spent this year perfecting a prerecruitment<br />
assessment tool which assesses the<br />
values and behaviours of prospective applicants<br />
who want to work at the hospital, ensuring that<br />
they are well suited and display behaviours<br />
which are aligned to our values. This involved<br />
around 200 staff who took part in workshops and<br />
questionnaires to develop the assessment process<br />
which will begin in April 2013.<br />
26 27
BACK TO CONTENTS PAGE<br />
A robust workforce planning framework has also<br />
been developed to support managers to assess<br />
the productivity of their people as a resource and<br />
predict workforce and educational requirements in<br />
line with service developments.<br />
Diversity and inclusion is also important to us at<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong>. We want to build<br />
an organisational culture that ensures we deliver<br />
personalised care to children and young people<br />
and make <strong>Birmingham</strong> Children’s <strong>Hospital</strong> the<br />
employer of choice, attracting and developing a<br />
diverse workforce to ensure we deliver our strategic<br />
priorities and unlock untapped potential.<br />
We launched our Diversity and Inclusion Action<br />
Plan in April 2013 which aims to meet the needs of<br />
our diverse population, ensure we meet regulatory<br />
requirements and have a strong corporate<br />
reputation and community profile.<br />
3. Caring for our people<br />
The health and wellbeing of our staff, as well as<br />
our patients and families, is incredibly important<br />
to us as because without our staff we wouldn’t be<br />
able to do what we do. To help everyone stay fit<br />
and able to work we have continued to take steps<br />
to support improvements in wellbeing to not only<br />
maximise attendance at work but also to encourage<br />
conversations about health and wellbeing at<br />
appraisal.<br />
The London Olympics provided an opportunity<br />
in summer to get staff involved in fun, healthy<br />
activities, such as a static charity bike challenge,<br />
and the theme for our Annual General Meeting<br />
in September was health promotion, with healthy<br />
food and drink stalls, advice and fun and interactive<br />
activities for staff to get involved in.<br />
In March we launched our Health and Wellbeing<br />
Strategy to bring together everything that we’re<br />
doing to support staff and empower individuals to<br />
make healthy choices and give them the tools to<br />
help improve their physical and mental wellbeing.<br />
We also intend to build upon the success of<br />
challenges such as the pedometer challenge where<br />
staff were encourage to walk as many steps as<br />
possible over six weeks to win a prize. This was<br />
an incredibly successful initiative and hundreds of<br />
people took part.<br />
An exciting new resource for staff is our BCH<br />
Health Club which offers members exclusive<br />
information and access to activities such as<br />
exercise classes, slimming club, stop smoking and<br />
mental health services tailored specifically to their<br />
needs. This has already attracted lots of interest<br />
from staff, with over 500 members so far.<br />
Our Health and Wellbeing Strategy also sets out<br />
our commitment to using the thousands of contacts<br />
that we have with families at the hospital every year<br />
to improve their health and wellbeing too. We do<br />
this through Making Every Contact Count (MECC),<br />
an initiative that trains staff to deliver brief healthy<br />
lifestyle advice in the right way at the right time.<br />
We’ve done this really well at <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong>, making a positive impact on<br />
the health of many children by supporting parents<br />
to stop smoking, referring children to local healthy<br />
weight groups and giving out healthy start vitamins<br />
to prevent vitamin D deficiency.<br />
28 29<br />
But for us, caring for our people is not just about<br />
supporting health and wellbeing. It’s also important<br />
to recognise and celebrate their successes. This<br />
year we launched our Star of the Month Awards<br />
(see pages 32 and 33 for our Stars Gallery) which<br />
follow on from the success of our Annual Staff<br />
Recognition Awards and give us the chance to<br />
reward staff throughout the year for their great work<br />
and commitment to our Trust Values.<br />
But it’s not just internal awards that our fantastic<br />
workforce is winning - our Learning Disability<br />
Nurse, Raj Jhamat won a national Nursing<br />
Standard Child Health Award this year for creating<br />
the UK’s first Punjabi DVD about autism.<br />
Raj works with patients and families from<br />
<strong>Birmingham</strong>’s South Asian communities on the<br />
wards and in their homes to help them understand
BACK TO CONTENTS PAGE<br />
autism. She said: “I was surprised and delighted to<br />
have received the Child Health Award. I now feel<br />
even more inspired to continue to develop my work<br />
with the parents of patients with learning disabilities<br />
and continue to make life better for them.”<br />
Dr Jim Gray, Head of Microbiology and his team<br />
were recognised at the national NHS Innovation<br />
Challenge Prizes, where they were highly<br />
commended for their work in reducing MSSA<br />
bloodstream infections in children who receive their<br />
parenteral nutrition at home. The hard work of the<br />
team reduced the numbers of infections by a third<br />
and it is hoped that this example of good practice<br />
will be rolled out across the hospital.<br />
The Facilities team has won a number of awards for<br />
the development of meal ordering system, Maple,<br />
including the Innovation in the use of Technology<br />
and Systems category at the 2012 British Institute<br />
of Facilities Management’s (BIFM) awards; the<br />
i-fm.net Facilities Management Technology<br />
award; Health Estates and Facilities Management<br />
Association (HefmA) Innovation Award and Team<br />
Award 2012.<br />
Several hospital teams were recognised for another<br />
year running at the <strong>Birmingham</strong> Chamber of<br />
Commerce Awards where we won the Excellence<br />
in Innovation award for Maple, the Formula 1<br />
technology we are using in PICU and our patient<br />
and family feedback app.<br />
Our Staff Library also won the Strategic Health<br />
Authority Library Lead’s Sally Hernando award,<br />
which rewards and recognises innovations in<br />
library and knowledge services. The Library’s<br />
Flickr photostream was entered for the award and<br />
commended for its innovation in marketing library<br />
services.<br />
At <strong>Birmingham</strong> Children’s <strong>Hospital</strong> we really care<br />
about what our staff think too as their views are<br />
fundamental to providing high quality care. We<br />
make sure we listen and give everyone the chance<br />
to be involved in decisions about our future strategy<br />
and the development of services.<br />
Consultation with our staff led to the development<br />
of refreshed strategic objectives for 2012/13 and<br />
they also participated in the 10th national NHS Staff<br />
Survey which showed that real progress has been<br />
made in the number of staff appraised in the last 12<br />
months and the sense of job satisfaction felt by staff<br />
(for full Staff Survey results see page 85).<br />
We also have regular staff polls on the intranet<br />
which means we can take a snapshot of how staff<br />
feel throughout the year and whether they would<br />
recommend the hospital to friends and family as a<br />
place to work or receive treatment. This means we<br />
can address any concerns right away and do what<br />
we can to improve their experience at work.<br />
4. Organisational Development<br />
To ensure our hospital is as effective as it can be<br />
it is vital to have a planned approach. Central to<br />
our organisational strategy is that our staff know<br />
what role they have to play and how they will be<br />
supported at work. Our focus this year has been to<br />
develop leadership capabilities at every level within<br />
every profession, and to embed organisational<br />
values and behaviours into everything we do.<br />
This includes internal systems and processes, for<br />
example staff will be asked to assess how they<br />
regularly display our values and behaviours within<br />
their annual appraisal.<br />
Learning Disability Nurse, Raj Jhamat, picking up her Nursing Standard award<br />
The facilities team collecting their BIFM award<br />
WATCH THE VIDEO<br />
30 31
BACK TO CONTENTS PAGE<br />
Our Stars of the Month Gallery<br />
December 2012<br />
Gemma Powell<br />
Junior Sister, Emergency Department<br />
Gemma was nominated<br />
for the ‘Unsung<br />
Hero’ category by<br />
a senior member of<br />
her team for showing<br />
courage, compassion,<br />
commitment and being<br />
caring while she led the<br />
Emergency Department<br />
through a difficult and<br />
very busy period. Her<br />
colleagues said she was<br />
a fantastic role model<br />
for how she ensured<br />
the team was supported<br />
throughout.<br />
February 2013<br />
Dr Shirin Beebeejaun<br />
Foundation Year 1 Trainee Doctor,<br />
Respiratory Medicine<br />
Shirin was nominated by a senior colleague<br />
for demonstrating exemplary commitment,<br />
compassion and respect in her first ever<br />
paediatric posting as a doctor. When the team<br />
was a member of staff short, she stepped up<br />
to the challenge to ensure that all tasks were<br />
completed successfully and that children and<br />
young people received the same high level of<br />
care. She was also nominated for demonstrating<br />
great understanding of patient and family<br />
problems, prioritising them appropriately and<br />
acting in a very caring way.<br />
January 2013<br />
Alison Jeremy<br />
Head of Speech and Language Therapy<br />
Alison received several<br />
nominations from her<br />
colleagues in the ‘Best Boss’<br />
and ‘Unsung Hero’ categories<br />
for remaining cheerful and<br />
positive through challenging<br />
times of change within the<br />
department when she had only<br />
recently taken over the role of<br />
head of the department. She<br />
supported staff throughout and<br />
made sure that the team were<br />
still able to deliver their care to<br />
the best possible standard.<br />
March 2013<br />
Elaine Ross, Domestic, Ward 15<br />
Elaine was nominated by<br />
a family on Ward 15 for<br />
being an ‘unsung hero’.<br />
They particularly wanted to<br />
acknowledge how supportive<br />
and compassionate Elaine<br />
was during a difficult time. The<br />
family specifically mentioned<br />
Elaine’s positive attitude, how<br />
polite she is and her caring and<br />
trustworthy manner. She wholly<br />
demonstrates our Trust values<br />
in everything she does while still<br />
providing a great service in her<br />
regular duties as a domestic on<br />
the ward.<br />
32 33
BACK TO CONTENTS PAGE<br />
WATCH THE VIDEO<br />
Shaping excellent care for tomorrow<br />
We will strengthen <strong>Birmingham</strong> Children’s <strong>Hospital</strong> as a provider of Specialised and Highly<br />
Specialised Services, so that we become the leading provider of children’s healthcare in the UK.<br />
In March 2012 we were designated as a Paediatric<br />
Major Trauma Centre for the West Midlands region,<br />
putting us at the heart of a trauma network which is<br />
saving more lives and improving patient care.<br />
Major trauma is a serious injury which threatens<br />
life, such as major head injuries, multiple injuries,<br />
spinal injuries and severe knife or gunshot wounds.<br />
These patients need 24/7 care from a wide range of<br />
clinical services and experts to help them get better<br />
quickly and improve their quality of life.<br />
As part of the designation we have improved<br />
the way that our young patients access<br />
physiotherapists, occupational therapists and<br />
speech and language therapists, and recruited<br />
more consultants, doctors and nurses so that we<br />
can provide everything that a major trauma patient<br />
needs on a single site. More than 100 major trauma<br />
patients have benefited from the new service since<br />
it began.<br />
In November 2012 we also became one of four<br />
nationally designated centres for epilepsy surgery.<br />
Epilepsy is a common condition which significantly<br />
affects quality of life of over 6,000 children in<br />
West Midlands alone. No matter how extreme or<br />
mild they are, seizures caused by epilepsy are<br />
unpredictable and managing them can be very<br />
difficult. On the whole, epilepsy can be controlled<br />
using drugs, however 30-40% of cases are drugresistant,<br />
which is where surgery can help.<br />
The national designation brings with it funding<br />
for additional staff and cutting-edge equipment to<br />
increase the number of dedicated beds for video<br />
telemetry from one to three, so we can treat three<br />
times more children each year and help transform<br />
their lives.<br />
34 35
Case study<br />
Worcestershire<br />
teenager,<br />
Jonathan<br />
Beale,<br />
was diagnosed with epilepsy in October 2011 after ongoing investigations into the<br />
cause of his long-term dyslexia and blackouts.<br />
Since then his condition has been controlled with drugs but his last two brain<br />
scans showed that an abnormality was getting slightly bigger. It was then that<br />
Jonathan decided he wanted it removed so he could lead a normal teenage life,<br />
start driving lessons and become a joiner.<br />
Consultant neurosurgeons, Richard Walsh and Desiderio Rodrigues used a<br />
high-tech navigation system to pinpoint the exact location of the abnormality and<br />
safely remove it without causing damage to his brain.<br />
Patients are usually awake and talking just a few hours after surgery and the<br />
majority are back home within a week. There is over an 80% chance that after a<br />
year Jonathan will never experience seizures again.<br />
Jonathan said: “Despite my parents being a bit anxious about it, it wasn’t a hard<br />
decision for me to take to have the surgery, as I knew this thing in my head was<br />
stopping me lead a normal life.<br />
“Until I’ve got a clean bill of health from the doctors I won’t be able to apply for<br />
my provisional licence, or operate machinery without supervision on my college<br />
course. I hope the surgery has done the job and I can get back to living a normal<br />
life with my friends and family.”<br />
At <strong>Birmingham</strong> Children’s <strong>Hospital</strong> we also<br />
specialise in heart surgery, particularly the most<br />
complex conditions thanks to the pioneering skills<br />
of our cardiac surgeons and specialist nursing<br />
teams who help care for so many babies, children<br />
and young people from across the UK each year.<br />
Our £4.9m angiography and hybrid theatre suite<br />
is supporting this by enabling our surgeons to<br />
perform surgery that would have previously<br />
required two operations, in just one, which<br />
drastically reduces the impact of surgery on<br />
children and their families and helps us see more<br />
patients too.<br />
Looking forward, we know we face a population<br />
which is growing and we know that more children<br />
and young people will need our help for more<br />
l 11 PICU beds<br />
l 7 PICU beds (£500k)<br />
l 2 Theatres (£2.3m)<br />
l Cancer Unit (£2m)<br />
l Heart Investigations<br />
Unit (£2m)<br />
l Parkview<br />
development (£10m)<br />
BACK TO CONTENTS PAGE<br />
complex conditions in the future too. We’re<br />
committed to continuing to deliver high quality<br />
care in the present while we plan for the future<br />
and have this year expanded capacity in our<br />
PICU to 31 beds (26 now open and 31 by 2014)<br />
and vastly improved our facilities across the<br />
hospital for our patients and families.<br />
In December our Board of Directors also agreed<br />
an estates strategy (below) which will ensure<br />
that between now and 2020, when we plan to<br />
have a new hospital, we have the space, facilities<br />
and staff to care for more patients. This includes<br />
more PICU and inpatient beds, two new theatres,<br />
a new West Midlands Cancer Centre and<br />
developments at our Child and Adolescent Mental<br />
Health Service (CAMHS) at Parkview.<br />
Now Short Medium Long<br />
31 PICU beds 38 PICU beds 49 PICU beds 50-58 PICU beds<br />
l 38 inpatient beds (£2m)<br />
l 11 PICU beds (£2m)<br />
l HDU/LTV (£1.7m)<br />
New <strong>Hospital</strong>:<br />
l 15 theatres + 4 high spec<br />
treatment rooms<br />
l Single room accommodation<br />
36 37
Looking specifically at the new hospital, a lot of<br />
work has been carried out during the year to look<br />
at how we can redevelop at Steelhouse Lane, as<br />
well as other options to work more closely and<br />
effectively with our partners to create top quality<br />
facilities that our patients and families deserve.<br />
Although there are benefits to our current Victorian<br />
Steelhouse Lane site, it does have its limitations<br />
as it was built for another era and we have used<br />
nearly every spare inch to squeeze in more<br />
facilities.<br />
A lot of our work crosses over with other services<br />
in the city, such as <strong>Birmingham</strong> Women’s <strong>Hospital</strong><br />
and the Queen Elizabeth <strong>Hospital</strong> in Edgbaston,<br />
so we have been looking at whether it would be<br />
feasible to have a standalone hospital there or<br />
a joint option with the Women’s <strong>Hospital</strong> and we<br />
have commitment from all Trusts to work closely<br />
together to develop these proposals further.<br />
But we are still in the very early stages of this<br />
process and any potential expansion or relocation<br />
of our hospital would certainly not happen before<br />
2020, so we’ve got a few years to make sure we<br />
get it right.<br />
Providing excellent care and facilities is central to<br />
all that we do at <strong>Birmingham</strong> Children’s <strong>Hospital</strong><br />
but there is a huge amount of work that goes on<br />
behind the scenes in research that helps us find<br />
cures and better treatments to help our young<br />
patients now and in the future.<br />
As an organisation, research excellence is<br />
measured according to our recruitment onto<br />
clinical trials. Currently there are around 200 active<br />
clinical trials and this year alone we have entered<br />
almost 2,000 patients into clinical trials – a record<br />
for the Trust – and next year we are forecasting<br />
even more. The Medicines for Children Research<br />
Network (MCRN) has been supporting this work,<br />
ensuring that trials are performed efficiently and to<br />
the highest standard across the NHS.<br />
One of our leading researchers, Dr Andrew Peet,<br />
was this year successfully awarded a prestigious<br />
Professorship with the National Institute for Health<br />
Research (NIHR). This support, worth £1.8m,<br />
means that Dr Peet can dedicate more time to<br />
promote research that can be used to improve<br />
treatment straight away – called translational<br />
research. His team is developing scans which can<br />
help diagnose brain tumours, plan surgery and<br />
select patients for the best treatments and he will<br />
be leading the way internationally at the highest<br />
academic levels, putting paediatric research on the<br />
map globally.<br />
In addition, one of our paediatricians, Dr Jeremy<br />
Kirk, has taken on the prestigious role of<br />
Director of the <strong>Birmingham</strong> and Black Country<br />
Comprehensive Local Research Network (CLRN)<br />
- the only paediatrician in the country to hold such<br />
a role.<br />
The <strong>Birmingham</strong> and Black Country CLRN is one<br />
of the largest in the UK and one of 25 across<br />
England that form the NIHR’s Comprehensive<br />
Clinical Research Network, which provides support<br />
for clinical trials and other studies so that patients<br />
can benefit from new and better treatments, and<br />
we can learn how to improve NHS healthcare for<br />
the future.<br />
Jeremy has already helped triple the number of<br />
children and young people recruited into research<br />
studies over the last year, ranking us ahead of both<br />
Great Ormond Street <strong>Hospital</strong> and Alder Hey.<br />
Dr Andrew Peet<br />
Case study<br />
Dr Jeremy Kirk<br />
Director of the <strong>Birmingham</strong> and Black Country<br />
Comprehensive Local Research Network<br />
Dr Pam Kearns also became a Professor this<br />
year and has now taken up the role as Director of<br />
the Cancer Research Clinical Trials Unit (CTU) at<br />
the University of <strong>Birmingham</strong>. The CTU provides<br />
support for all children’s cancer trials that are<br />
running across the UK.<br />
Dr Francis Mussai was also appointed as Senior<br />
Lecturer in Oncology in summer 2012. His<br />
research interest is the way in which the body’s<br />
own immune system can be used to fight cancer.<br />
One of the many life-saving research trials which<br />
began this year was the UK National Randomised<br />
Trial of Children and Young Adults with Acute<br />
38 39<br />
BACK TO CONTENTS PAGE<br />
“It’s my job to stimulate research<br />
in all areas of healthcare, and<br />
the experience I have from<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong><br />
will be invaluable, as even though<br />
we are a small hospital, we have<br />
run many clinical trials over the<br />
years, and have tripled patient<br />
recruitment in the last year alone.<br />
“This is an exciting time for<br />
research in the UK. There<br />
are huge opportunities for the<br />
health sector in <strong>Birmingham</strong>,<br />
the Black Country and wider<br />
West Midlands to be involved in<br />
world-class research and I relish<br />
the opportunity to help secure<br />
projects and trials that will benefit<br />
not only children and young<br />
people, but anyone who needs<br />
to use NHS services in the future<br />
too.”<br />
Lymphoblastic Leukaemia and Lymphoma (UKALL<br />
2011) which is led nationally by our Consultant<br />
Paediatric Haematologist, Sarah Lawson.<br />
UKALL 2011 follows a similar trial in 2003 which<br />
resulted in better cure rates and reduced side<br />
effects and brings more hope to our leukaemia<br />
patients and their families as we can continue vital<br />
trials into new drugs and treatment.<br />
It also supports the creation of a research network<br />
across the West Midlands to bridge the divide<br />
between children and young adults, which has not<br />
been done before.
At <strong>Birmingham</strong> Children’s <strong>Hospital</strong> we also carry<br />
out world-leading research and treatment for<br />
children with rare diseases which affect less than<br />
one in 100,000 children. Although rare diseases<br />
can affect many different parts of the body, the<br />
one thing that is common is that they all require<br />
care and treatment from several different specialist<br />
areas and if unrecognised they can lead to severe<br />
disabilities.<br />
We are the second largest provider of nationally<br />
commissioned rare diseases services in the UK<br />
with 11, and because of our expertise we aspire to<br />
become a National Rare Diseases Centre and will<br />
be working towards this over the next year.<br />
In March 2013, we became the first centre in the<br />
UK to use a novel new treatment for children with<br />
a rare and life-threatening liver disease - Crigler<br />
Najjar Syndrome. The trial aims to replace the<br />
diseased liver cells by restoring normal function<br />
with the infusions of liver stem cells. The hope is<br />
that these healthy stem cells will ‘seed’ into the<br />
liver and correct the faulty metabolism that children<br />
with this disease suffer with. One patient so far has<br />
had this treatment with more lined up. Results from<br />
this trial should become available within the next<br />
two years.<br />
In July 2012 we were selected as one of four<br />
centres to join a new year-long pilot study for<br />
the Department of Health’s National Newborn<br />
Screening Programme to test for some additional<br />
rare diseases.<br />
Currently, all babies are tested at birth for five<br />
conditions through the ‘heel prick test’. As part of<br />
the pilot, newborns are being tested for five more<br />
to look at outcomes and whether they should<br />
be permanently added to the national screening<br />
programme.<br />
The pilot is going well and to date we have picked<br />
up two cases at <strong>Birmingham</strong> Children’s <strong>Hospital</strong> –<br />
one mild isovaleric aciduria and one maple syrup<br />
urine disease – which is a great result as it means<br />
that we can now treat the children much earlier,<br />
prevent severe complications and help them live<br />
longer and healthier lives.<br />
One of these children, Habul Khatoon from<br />
<strong>Birmingham</strong> was diagnosed in October 2012 with<br />
maple syrup urine disease when she was just a<br />
few days old. This is a serious genetic metabolic<br />
disorder which stops the body breaking down<br />
amino acids in protein rich food. If these acids<br />
accumulate and are left or not managed properly,<br />
it can lead to coma, brain damage and death in<br />
newborn babies.<br />
Thanks to the early intervention and ongoing<br />
treatment from our metabolic team, Habul is<br />
growing and developing normally and looking<br />
forward to a much brighter future.<br />
Case study<br />
BACK TO CONTENTS PAGE<br />
Noah and Ruby<br />
from Sandwell<br />
Baby Habul and mum Fahmeeda Khatoon pictured with Inherited Metabolic Specialists<br />
Professor Anita MacDonald and Dr Anupam Chakropani<br />
Rebekah Youlden and Arron Harvey from Sandwell<br />
are supporting the Newborn Screening Programme<br />
pilot as their two youngest children, Noah (4) and<br />
Ruby (2) have glutaric aciduria type 1 (GA1), which<br />
means that they cannot break down protein which<br />
causes harmful substances to build up in their<br />
bodies.<br />
Noah was just 10 months old when he first became<br />
ill and it wasn’t until he had spent three weeks in a<br />
local hospital that he was diagnosed with GA1. The<br />
length of time from birth until his diagnosis meant<br />
that damage to Noah’s brain had already begun.<br />
He is now in a wheelchair but can take steps in his<br />
specially built walker, he attends school and can eat<br />
with his family after spending two and a half years<br />
being fed through a nasogastric tube.<br />
40 41<br />
Two year old Ruby on the other hand was<br />
diagnosed at just 12 days old and started on a<br />
limited protein diet and medication straight away to<br />
lessen the damage to her body and brain and she<br />
is developing normally for her age.<br />
Her parents are all too aware of the importance of<br />
early diagnosis. Mum Rebekah said: “Noah is a<br />
lovely little boy who always has a smile on his face<br />
but people find it hard to believe that he and Ruby<br />
have the same disease because Ruby is walking<br />
and talking and Noah is in a wheelchair and can’t<br />
do all the things his sister can. If the heel prick test<br />
had been able to test for GA1, Noah’s life would<br />
have been so different.”
Shaping excellent care for tomorrow<br />
We will continue to develop <strong>Birmingham</strong> Children’s <strong>Hospital</strong> as a provider of outstanding local<br />
services - ‘a hospital without walls’ - working in close partnership with other organisations.<br />
At <strong>Birmingham</strong> Children’s <strong>Hospital</strong> we now have<br />
over 240,000 patient visits every year – more than<br />
ever before - and although we do all we can to<br />
make the hospital experience the best it can be, we<br />
know that nowhere is as comfortable as home.<br />
This is why we’ve been working with partners to<br />
set up services to provide treatment and care out<br />
in the community and in people’s own homes,<br />
giving those with stable conditions a choice for the<br />
first time. Not only does this help increase their<br />
independence, it gives them greater control of their<br />
care.<br />
One new service is our Child and Adolescent<br />
Mental Health Service (CAMHS) Home Treatment<br />
Service which supports many children and young<br />
people at home with their families instead of them<br />
being admitted onto an inpatient psychiatric ward.<br />
The 24/7 service covers the entire city of<br />
<strong>Birmingham</strong> for young people aged 12 – 18 and<br />
we’ve worked in partnership with <strong>Birmingham</strong><br />
and Solihull Mental Health Foundation Trust to<br />
make sure that our older teens have a seamless<br />
transition into adult services for their future care<br />
and treatment.<br />
Our <strong>Hospital</strong> at Home service has also expanded<br />
over the last year, taking more patients from more<br />
specialties, such as general paediatrics, plastics,<br />
neurology, oncology and haematology.<br />
Working in partnership with community nurses<br />
and health visitors, our team of five supports the<br />
care of children and young people across the city<br />
of <strong>Birmingham</strong> and Solihull. This helps us save<br />
hospital beds for those who need them the most.<br />
Children and young people from South and Central<br />
<strong>Birmingham</strong> with diabetes are also benefitting from<br />
care at home through the Diabetes Home Care Unit<br />
which has grown over the year and moved into a<br />
new dedicated unit within our Steelhouse Lane site.<br />
The team works closely with nurseries and schools,<br />
providing expert advice to other regional paediatric<br />
diabetes teams. It offers a 24/7 phone support<br />
service and weekend drop in clinics to the 335<br />
children and young people with Type 1 and Type<br />
2 diabetes, Cystic Fibrosis related diabetes and<br />
secondary diabetes from conditions such as cancer<br />
or organ transplants, Bardet-Biedl, Alstrom and<br />
Wolfram Syndrome.<br />
As the number of diabetes patients we see is<br />
always growing, we have had commitment from<br />
the Board of Directors to expand by recruiting more<br />
staff, including a social worker and family support<br />
worker. This has helped secure funding from local<br />
commissioners to provide more training for staff<br />
and resources for patients and families, helping<br />
us take huge steps closer to becoming a leading<br />
centre in the UK.<br />
BACK TO CONTENTS PAGE<br />
We have also continued to work closely with<br />
our NHS and local authority partners on the<br />
<strong>Birmingham</strong> and Solihull Acute Paediatric Service<br />
Review and we are leading the development of a<br />
Children’s Health Network.<br />
Networks and their development are a fundamental<br />
priority for the Trust and this particular network<br />
brings together clinicians from providers across<br />
primary, secondary and tertiary care to look at how<br />
we need to work in partnership and plan for the<br />
future to make sure that children and young people<br />
receive high quality, safe and effective care, no<br />
matter what their condition is, how old they are or<br />
where they live.<br />
Other networks at <strong>Birmingham</strong> Children’s <strong>Hospital</strong><br />
include our oncology and cardiac networks which<br />
are delivered in a ‘hub and spoke’ style. This<br />
is where we act as the ‘hub’ of expertise and<br />
deliver care through our ‘spoke’ partners such the<br />
University <strong>Hospital</strong>s Coventry and Warwickshire<br />
NHS Trust, enabling us to see patients closer to<br />
home and strengthening the expertise of our district<br />
hospital partners. These relationships will become<br />
more important and will be further strengthened as<br />
time continues, particularly if further reconfiguration<br />
plans such as Safe and Sustainable take place.<br />
WATCH THE VIDEO<br />
CAMHS Home Treatment team picking up the Perfect Partnerships staff recognition award<br />
42 43
BACK TO CONTENTS PAGE<br />
The Impact of Fundraising<br />
Fundraising continues to play a vital role in<br />
supporting the work of the hospital. It enables us<br />
to fund additional facilities and equipment, support<br />
medical research and provide the extras that make<br />
being in hospital a more comfortable and less<br />
distressing experience for children, young people<br />
and their families.<br />
Highlights for the year include:<br />
This year we raised more<br />
than ever before<br />
- £4.43m!<br />
Key facts for the year:<br />
l We had a record 4,162 individual supporters.<br />
l In July we launched our biggest fundraising<br />
appeal ever, the £4m Children’s Cancer Centre<br />
Appeal, for a new unit to improve the lives of our<br />
3,000 cancer patients and their families. We have<br />
already reached the £1m mark which means a<br />
brand new state-of-the-art unit is now within<br />
reach.<br />
l Our ‘Hundred Heroes’ event in February<br />
recognised our top 100 supporters for the year<br />
who collectively raised £660,000 over the last<br />
12 months. One of these was the family of<br />
patient Poppy Guilder who has a brain tumour.<br />
They have raised a staggering £180,000 over the<br />
last nine years for research at the hospital<br />
and last year, thanks to new improved scanning<br />
equipment and the research they’ve made<br />
possible, doctors were able to remove more of<br />
their daughter’s tumour than they ever thought<br />
possible.<br />
l Over 1,000 supporters took part in the Great<br />
<strong>Birmingham</strong> Run, raising £200k for us. This<br />
makes us the largest charity team at the event<br />
with the largest presence on the day.<br />
l We received a £471,000 donation from the Give<br />
a Child Health Charitable Trust, which was our<br />
largest donation of the year and is funding a new<br />
respiratory centre at the hospital.<br />
l General fundraising activities enabled the charity<br />
to award a grant of £300k to <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong> Research Foundation to fund<br />
high quality, internationally recognised research,<br />
and have enabled our academic trainees to<br />
become leaders of paediatric research.<br />
l 78 corporate partners around the region pledged<br />
their support to the hospital.<br />
l Merging the Trust and fundraising Facebook<br />
pages meant that over 15,000 people now have<br />
regular communication from both teams.<br />
l Our biggest area of growth has been in support<br />
from schools which has doubled since last year.<br />
l Our first ever charity ball raised £75,000 in one<br />
night for the Children’s Cancer Centre Appeal.<br />
What does the future hold for 2013/14?<br />
Looking to the future, we are going to be investing<br />
more in long term sustainable fundraising activities.<br />
Legacy fundraising and Regular Giving are just<br />
two areas that we will focus on that will offer stable<br />
income growth. By developing these we hope to<br />
increase our unrestricted funding streams to enable<br />
more charitable grants to be awarded which in<br />
turn will have a big impact on the hospital and the<br />
patients in our care.<br />
l The fundraising team is looking to increase its<br />
impact even further with an ambitious £5.4m<br />
target.<br />
l £3m still to raise to build our world class<br />
Children’s Cancer Centre; £120k partnership with<br />
national organisation, Wesleyan Assurance<br />
Society.<br />
l £70k specially designed sensory garden that will<br />
cater to the senses of children and young people<br />
with learning difficulties with scented flowers,<br />
calming music and multiple textures to touch<br />
around the garden.<br />
44 45
SECTION TWO<br />
BACK TO CONTENTS PAGE<br />
The Governance of our Organisation<br />
Directors’ Report<br />
Brief history of the Trust and its statutory background<br />
The <strong>Birmingham</strong> and Midland Free <strong>Hospital</strong> was<br />
founded in 1862 and moved to Steelhouse Lane<br />
in <strong>Birmingham</strong> in 1998. The hospital Trust was<br />
granted Foundation Trust status on 1 February<br />
2007 under the Health and Social Care (Community<br />
Health and Standards) Act 2003.<br />
The Trust’s Executive Directors<br />
and Non-Executive Directors in 2012/13<br />
The Trust also owns a second site located at<br />
Parkview in Moseley which hosts the Child and<br />
Adolescent Mental Health Service (CAMHS).<br />
The Trust provides services from a range of<br />
accommodation in the community and in several<br />
partner acute organisations.<br />
Ms Sarah-Jane Marsh Chief Executive Officer (maternity leave from November 2012)<br />
Mrs Michelle McLoughlin<br />
Dr Vinod Diwakar<br />
Chief Nursing Officer<br />
Chief Medical Officer<br />
Mr David Melbourne Chief Finance Officer/Interim Chief Executive Officer (from November 2012)<br />
Mr Phil Foster Interim Chief Finance Officer (from November 2012)<br />
Mr David Eltringham Chief Operating Officer (until September 2012)<br />
Mr Tim Atack Chief Operating Officer (from September 2012)<br />
Mrs Theresa Nelson<br />
Chief Officer for Workforce Development<br />
Ms Joanna Davis Chairman (until sick leave 16 April 2012)<br />
Mr Keith Lester Deputy Chairman/Interim Chairman (from 16 April 2012)<br />
Mrs Judith Green<br />
Mr Colin Horwath<br />
Professor Jon Glasby<br />
Deputy Chairman, Engagement and Participation<br />
Deputy Chairman, Strategy and Partnerships<br />
Non Executive Director<br />
Mr Zubair Khan Non Executive Director (until December 2012)<br />
Mrs Elaine Simpson<br />
Non Executive Director<br />
Mr Roger Peace Non Executive Director (from July 2012)<br />
Statement as to disclosures<br />
to auditors<br />
So far as each individual Director is aware, there<br />
is no relevant audit information of which the Trust’s<br />
auditor is unaware. Each Director has taken all<br />
the steps they ought to have taken as a Director in<br />
order to make themselves aware of any relevant<br />
audit information and to establish that the Trust’s<br />
auditor is aware of that information.<br />
Principle activities of the Trust<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust provides the widest range of children’s health<br />
services for young patients from <strong>Birmingham</strong>, the<br />
West Midlands and beyond, with over 240,000<br />
patient visits every year. We are one of the UK’s<br />
four standalone children’s hospitals, one of 37<br />
providers of specialised children’s services, and<br />
one of the UK’s 246 trusts providing hospital<br />
paediatric services to the local population. We<br />
provide 11 national services, 30+ services to<br />
children and young people in the West Midlands,<br />
and general and emergency services to the south<br />
and central population of <strong>Birmingham</strong>.<br />
We are characterised by a unique collocation of all<br />
the services, specialist expertise and diagnostic<br />
and treatment resources that a sick child needs.<br />
The population is characterised by diseases which<br />
have one or more of the following characteristics:<br />
rarity, complexity, co-morbidity, unresponsiveness<br />
to conventional therapy, age or acuity.<br />
Significant Research &<br />
Development Activities<br />
Information about research and development can<br />
be found at pages 38-41 and 120.<br />
Operating & Financial Review<br />
With 2012/13 being another challenging period for<br />
the NHS it is pleasing that the Trust ended the year<br />
achieving its key financial targets and delivering<br />
another strong set of results. Given the wider<br />
financial environment it was unrealistic to expect a<br />
performance on a par with 2011/12 so the surplus<br />
we reached of £6.3m should be regarded as an<br />
excellent achievement.<br />
The reduced surplus compared to 2011/12 was<br />
mirrored by a reduction in earnings before interest,<br />
tax, depreciation and amortisation (EBITDA) to<br />
7.2% for the financial year, down from 8.1% in<br />
2011/12. This 11% decrease on 2011/12’s position<br />
is a result of:<br />
a) The Trust being increasingly affected by the<br />
method of reimbursement for emergency care<br />
for activity over a specific threshold agreed with<br />
commissioners. This activity is paid at 30% of<br />
the national tariff and does not fully reflect the<br />
costs incurred in treating these patients.<br />
b) Provisions set aside for the impact of workforce<br />
issues in Community CAMHS and junior doctors.<br />
The impact of austerity measures across the<br />
public sector have hit the Trust particularly hard<br />
with a potential 25% reduction in our Community<br />
CAMHs funding which will impact upon the<br />
numbers of staff in this service.<br />
c) The costs of providing additional capacity within<br />
the Trust outside of core working hours.<br />
d) Inflation and cost pressure levels being higher<br />
than expected especially in Estates and on gas<br />
and electricity.<br />
e) Continued difficulty in fully realising the cost<br />
efficiency targets.<br />
The Trust maintains a Register of Interests of Directors and Governors that may be accessed via the Trust’s<br />
Publication Scheme available on the Trust’s website.<br />
46 47
Table 1: Patient Activity 2008/9-2012/13<br />
2012/13 2011/12 2010/11 2009/10 2008/9<br />
Revised Outpatient attendances 152,820 147,276 147,292 143,291 141,088<br />
ED attendances 49,335 47,592 46,274 45,142 45,585<br />
Inpatient (I/P) admissions:<br />
Emergency admissions 14,854 13,935 14,143 11,898 11,544<br />
<strong>Day</strong>-case admissions 18,951 17,816 16,131 16,258 15,296<br />
Inpatient admissions 6,491 7,532 6,809 6,385 5,980<br />
Total I/P admissions 40,296 39,283 37,083 34,541 32,820<br />
Total patient episodes 242,451 234,151 230,649 222,974 219,493<br />
The increase in Outpatient attendances reversed<br />
the pattern of the previous two years with the<br />
increase in new attendances out-stripping the rise<br />
in follow-ups.<br />
It cost just over £225 million to run the Trust<br />
during the year, a 6.8% increase on 2011/12.<br />
However, there are a number of significant nonrecurrent<br />
or technical costs included within this<br />
figure, which when removed indicate an underlying<br />
movement of 4.3% on 2011/12. The two highest<br />
spend categories, Employees and Drugs, have<br />
seen above average increases of 8.0% and 7.4%<br />
respectively. The cost of running the estate has<br />
experienced a rise of over 25% in 2012/13.<br />
We employed 156 more staff at the end of March<br />
2013 than at the beginning of April 2012, with an<br />
average increase over the year of 102 additional<br />
staff. Doctors and nursing staff saw the largest<br />
year-on-year growth at 9.5% and 6.2%. On average<br />
we paid staff 4% more in 2012/13 than in 2011/12<br />
which reflects the skill mix changes across the<br />
Trust arising out of key developments, such as the<br />
expansion of the Paediatric Intensive Care Unit as<br />
well as the method of delivery of increased activity.<br />
During the year we saved £8.1 million in planned<br />
cost releasing savings (£10.1 million in 2011/12),<br />
which contributed towards the nationally<br />
determined efficiency target. This represents 76%<br />
of the target we set at the beginning of the year<br />
(96% of the 2011/12 target was achieved). Although<br />
£8m was the in-year target for 2012/13 it was the<br />
impact of non-recurrent element of the 2011/12<br />
programme carried forward that caused difficulties.<br />
We have been mindful of this as an issue in setting<br />
our target for 2013/14. In terms of actual financial<br />
savings, this is the second highest level ever<br />
achieved by the Trust. We improved on our system<br />
of ensuring that these cost savings did not impact<br />
on the safety and quality of services delivered; as<br />
part of this every savings scheme was signed off by<br />
at least two clinicians including the Chief Medical<br />
Officer and the Chief Nurse.<br />
Investment in maintaining our estate and the<br />
development of new facilities and equipment<br />
replacement is currently funded from the surpluses<br />
that we make. During 2012/13, £9.5 million was<br />
invested in new capital schemes with some of these<br />
schemes due for completion during the 2013/14<br />
financial year. It is pleasing to note that the level<br />
of assets under construction at the end of the year<br />
has reduced by £4m in year which means that vital<br />
elements of our strategic investment programme<br />
have become operational, with the expanded PICU<br />
capacity being the most notable.<br />
The range of strategic schemes underway included:<br />
l Emergency Department remodelling;<br />
l Refurbishment of Outpatients;<br />
l Trust infrastructure work;<br />
l Respiratory development.<br />
All these developments have helped to increase<br />
the capacity of the hospital and contributed to<br />
improving the care we provide.<br />
During the year the Trust has further developed its<br />
work looking at the provision of a new hospital to<br />
ensure that in 10 years time the Trust continues to<br />
be in a position to deliver world class children’s<br />
services.<br />
The analysis we have undertaken to date indicates<br />
that over the next decade the Trust will need to<br />
develop new facilities if it is to meet the challenges<br />
of continuing to deliver high quality care.<br />
In December 2012 the Board received the strategic<br />
outline case that presented options for the future<br />
site of the hospital. After considering this analysis<br />
it was decided that more detailed work should<br />
continue. This work will examine the development<br />
of a hospital on the Steelhouse Lane site or the<br />
development of a new facility on the health campus<br />
at Edgbaston, in close proximity to University<br />
<strong>Hospital</strong>s <strong>Birmingham</strong> NHS Foundation Trust<br />
(UHB). The option of a move to a health campus in<br />
Edgbaston has support from the Board of Directors<br />
and key partners including UHB, University of<br />
<strong>Birmingham</strong> and <strong>Birmingham</strong> Women’s <strong>Hospital</strong><br />
NHS Foundation Trust. The next stage of the<br />
project is to undertake a more detailed assessment<br />
through the development of an outline business<br />
case followed by a formal public consultation.<br />
Our trading position is reflected in our cash<br />
balances. These have continued to improve over<br />
the medium term such that we had £36.2 million<br />
in cash or cash equivalents at the end of the<br />
financial year (£33.7 million in 2011/12). Despite<br />
the extensive capital programme, cash increased<br />
by £2.4 million in the year, which will allow further<br />
reinvestment in 2013/14.<br />
48 49<br />
BACK TO CONTENTS PAGE<br />
In 2012/13, using the opportunities afforded by<br />
our status as a foundation trust, we established a<br />
wholly owned subsidiary, <strong>Birmingham</strong> Children’s<br />
<strong>Hospital</strong> Services Limited, and <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong> Pharmacy Limited, for the<br />
purpose of building and operating a new Outpatient<br />
Pharmacy, The Medicine Chest. This innovative<br />
and cutting-edge development provides the<br />
opportunity to deliver cost effective, specialist<br />
outpatient pharmacy services. The Medicine Chest<br />
opened in January 2013 and is already having a<br />
positive impact on patient experience, with a better<br />
environment and a much faster service.<br />
Fundraising income through <strong>Birmingham</strong> Children’s<br />
<strong>Hospital</strong>s Charities increased - despite the wider<br />
economic recession - at £4.43 million (2011/12<br />
£3.2 million). In 2012/13 we celebrated our 150th<br />
birthday and launched our Cancer Centre Appeal<br />
to raise £3.5 million to improve the facilities for<br />
younger children receiving treatment for cancer at<br />
the hospital.<br />
Given the growth in population, changes in medical<br />
technology and high rates of inflation compared<br />
to that assumed in the NHS financial settlement,<br />
the Trust will have to make £24 million of savings<br />
over the next four years. This is part of the £20<br />
billion of efficiencies that the NHS Chief Executive<br />
announced would be required nationally and is<br />
reflected in Monitor’s financial assumptions for<br />
the same period. With austerity measures due to<br />
continue to at least 2017, the Trust’s approach to<br />
cost improvements and efficiencies has to change.<br />
Our financial position provides a sound foundation<br />
to address the challenges resulting from the<br />
national savings priorities. We have plans in place<br />
to achieve the majority of the required savings in<br />
2013/14 through reducing administration costs,<br />
transforming clinical services and by continuing to<br />
deliver clinical services in the most cost-effective<br />
way. As part of this process we will continue<br />
to work in partnership with our commissioners<br />
to ensure that children are treated in the most<br />
appropriate setting for their condition.<br />
The Trust, along with a number of other NHS<br />
specialist children’s providers, has continued to<br />
successfully work with the Department of Health on<br />
the appropriate level of the ‘top-up’ to the national<br />
tariff for specialist paediatric services. The Trust<br />
currently receives a supplement of £17 million<br />
per annum to recognise the additional costs of<br />
providing specialist children’s services and this<br />
continues to be reviewed by the Department of<br />
Health and from 2013/14, Monitor.
50 51<br />
BACK TO CONTENTS PAGE<br />
During the year the Board approved a revised<br />
financial framework which complemented the<br />
existing financial strategy of the Trust. The aims of<br />
the strategy remain to:<br />
l Imporove the quality of service that reduce variation, waste and harm.<br />
l Provide the resource to deliver world class patient centred care.<br />
l Provide the funding for a productive, motivated and professional workforce.<br />
l Provide better value for money.<br />
l Deliver affordable, world class health services for children and young people.<br />
The strategy will be delivered through the<br />
following six components:<br />
l Using a mixed funding strategy for major new infrastructure investment.<br />
l Developing a clear financial framework - to monitor financial stability and investment .<br />
l Delivering the necessary efficiency savings.<br />
l Improving financial literacy across the organisation.<br />
l Developing NHS and non NHS business opportunities.<br />
l Recognising charitable funds as a core component of the funding mix.<br />
Finance Statements<br />
The Trust’s accounts have been prepared under a<br />
direction issued by Monitor. The Trust has complied<br />
with the cost allocation and charging requirements<br />
set out in HM Treasury and Office of Public Sector<br />
Information Guidance.<br />
The Trust has complied with the requirement that<br />
the income from the provision of goods and services<br />
for the purposes of the health service in England<br />
must be greater than the income from the provision<br />
of goods and services for any other purposes.<br />
Financial risk management objectives<br />
and policies<br />
Our Finance and Resources Committee oversees<br />
the cash management and investment strategy<br />
which is based on Monitor best practice and is<br />
reviewed by our auditors. This places surplus cash<br />
on short-term deposit in the most secure accounts.<br />
During 2012/13 the Committee agreed revisions<br />
to the policy which serve to address concerns<br />
regarding levels of sovereign debt and the strength<br />
of financial institutions. Cashflow forecasts are<br />
updated on a weekly basis to ensure that no<br />
cashflow and liquidity risks are evident. Looking<br />
to the future cashflow planning is undertaken<br />
for the Trust’s long-term modelling with the risk<br />
rating impact - including the new Risk Assessment<br />
Framework and its greater focus on liquidity - now<br />
being incorporated.<br />
The Committee also scrutinises all our major capital<br />
investment and consultant appointments to ensure<br />
they fall in line with our service strategy and are<br />
affordable and provide value for money.<br />
With the increased importance of efficiency savings<br />
the Committee has scrutinised the delivery of the<br />
savings plan during the year to ensure that the<br />
approach does not impact on the quality of services<br />
provided. This has extended to our Commissioners<br />
with whom our CIP Governance Structure has been<br />
shared.<br />
The Trust’s activities expose it to a variety of<br />
financial risks, though due to their nature the<br />
degree of exposure is reduced compared to that<br />
faced by many business entities. The financial<br />
risks are mainly credit and inflation risks with<br />
minimal exposure to market or liquidity risks.<br />
The nature of how the Trust is financed exposes<br />
it to a degree of customer credit risk. The Trust<br />
regularly reviews the level of actual and contracted<br />
activity with commissioners to ensure that any<br />
income risk is resolved at a high level at the<br />
earliest available opportunity. The Trust mitigates<br />
its exposure to credit risk through regular review<br />
of receivables due and by calculating a bad debt<br />
provision.<br />
The Trust has exposure to annual price increases<br />
of medical and non-medical supplies and services<br />
arising out of its core healthcare activities. This risk<br />
is mitigated through, for example, transferring the<br />
risk to suppliers by contract tendering, negotiating<br />
fixed purchase costs and in the case of external<br />
agency staff costs via the operation of the Trust’s<br />
own staff bank.<br />
Details of other risks and uncertainties facing the<br />
Trust are described in the Annual Governance<br />
Statement at page 144.<br />
Details of the impact of the Trust’s business on the<br />
environment are set out in the Sustainability Report<br />
on page 88.<br />
Contractual arrangements<br />
The organisations with whom the Trust has<br />
contractual or other arrangements which are<br />
essential to the business of the Trust are:<br />
l Sodexo – patient, staff and visitor catering<br />
services<br />
l St Paul’s Transport – taxi service for<br />
patients, staff and light goods<br />
l B Braun Sterilog (<strong>Birmingham</strong>) Ltd –<br />
medical devices sterilisation services<br />
l AAH Pharmaceuticals Ltd – pharmaceutical<br />
wholesaler<br />
l NHS Supply Chain – procurement services<br />
l NHS Blood and Transplant – supply of blood,<br />
organs and tissue<br />
l St John’s Ambulance – PICU retrieval<br />
services<br />
l A4 MTS – non-emergency patient<br />
ambulance services<br />
l McKesson – staff payroll services<br />
l Healthcare at Home –nursing/logistics<br />
services to enable patients to receive<br />
treatments at home<br />
l Medco Healthcare - nursing/logistics services<br />
to enable patients to receive treatments at<br />
home<br />
l NHS Shared Business Services – supply of<br />
procurement and financial services<br />
l PWC, EC Harris and BDO - advisors on the<br />
Trust’s Estate Strategy<br />
l Bupa Home Healthcare Ltd - nursing/logistics<br />
services to enable patients to receive<br />
treatments at home.
Partnerships<br />
During 2012/13 the Trust has entered into formal<br />
arrangements with the following organisations,<br />
which are essential to the Trust’s business:<br />
l <strong>Birmingham</strong> Children’s <strong>Hospital</strong> Pharmacy<br />
Limited (BCH Pharmacy). This company<br />
is a wholly owned subsidiary of <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong> Health Services, which<br />
is a wholly owned subsidiary of the Trust.<br />
BCH Pharmacy is responsible for the<br />
operation of the Medicine Chest, the new<br />
Outpatient Pharmacy located at the front of<br />
our Steelhouse Lane site (see above).<br />
l Sandwell and West <strong>Birmingham</strong><br />
<strong>Hospital</strong>s NHS Trust. We have entered<br />
into an arrangement with Sandwell and<br />
West <strong>Birmingham</strong> <strong>Hospital</strong>s NHS Trust for<br />
the provision of a joint Estates Management<br />
Service.<br />
Policy and payment of creditors<br />
We liaise closely with our suppliers to ensure there<br />
are no unintentional cash problems. We are aiming<br />
to comply with the target of all payable invoices to<br />
be paid within 30 days. It is disappointing that this<br />
has deteriorated slightly compared to last year and<br />
there is still more work we can do in this area. We<br />
did not incur any interest charges under the Late<br />
Payment of Commercial Debts Act 1998.<br />
Figure 1: Creditors BPPC Value % Cumulative 2011/12 – 2012/13<br />
100%<br />
95%<br />
Going concern<br />
After making enquiries, the Directors have a<br />
reasonable expectation that we have adequate<br />
resources to continue in operational existence<br />
for the foreseeable future. Monitor’s draft Risk<br />
Assessment Framework assesses the risk to the<br />
continuity of services.<br />
Using the proposed measures we have the lowest<br />
level of risk with a continuity of service rating<br />
reporting that we have sufficient financial headroom<br />
and liquidity. For this reason, the Directors continue<br />
to adopt the going concern basis in preparing the<br />
accounts.<br />
Pensions and Benefits<br />
Accounting policies for pensions and other<br />
retirement benefits are set out in note 1.03 to the<br />
accounts. Details of senior managers’ remuneration<br />
can be found in the Remuneration Report at page 61.<br />
Ill health retirements and redundancies<br />
There were five ill health retirements in 2012/13.<br />
The value of these is £314k, which will be borne<br />
by the NHS Business Services Agency (Pensions<br />
Division).<br />
A number of redundancies occurred during the year.<br />
Details associated with these are as follows.<br />
Table 2: Redundancies 2012/13<br />
Counter Fraud<br />
BACK TO CONTENTS PAGE<br />
One of the basic principles of public sector<br />
organisations is the proper use of public funds.<br />
The Counter Fraud service at BCH aims to prevent<br />
fraudulent activity which threatens this principle.<br />
Informing staff of their responsibilities, encouraging<br />
them to think about how their behaviour is a<br />
major control against fraud, and helping them<br />
spot fraud and raise concerns are at the core of<br />
developing a counter fraud culture. This has been<br />
achieved by the inclusion of counter fraud training<br />
at the core of our mandatory training programme,<br />
supplemented with an online learning module.<br />
Staff have responded, telling us about concerns<br />
where they work and allowing us to tackle those<br />
issues, investigate worries and make necessary<br />
improvements. Together with other sources of<br />
intelligence this has helped us develop a riskprioritised<br />
programme of fraud prevention. We aim<br />
to build on this approach in 2013/14, creating a work<br />
plan which gets to the heart of where fraud may be<br />
a risk in our organisation so that we can put in the<br />
necessary controls to safeguard public funds.<br />
Our Staff<br />
Information and Consultation<br />
We believe that the views of our staff are<br />
fundamental when considering change in the<br />
long, short and medium term, be it in relation to<br />
our estate, clinical matters or the development of<br />
services. We involve our staff in all decisions about<br />
our future strategy and the development of services.<br />
90%<br />
85%<br />
80%<br />
75%<br />
70%<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Target<br />
Actual 12-13<br />
Actual 11-12<br />
Exit Package Cost Band Number of Number of Other Total Number of<br />
Compulsory Departures Exit Packages<br />
Redundancies Agreed by Cost Band<br />
BACK TO CONTENTS PAGE<br />
Consultation with our staff led to the development<br />
of refreshed strategic objectives for 2012/13.<br />
At a monthly Chief Executive’s Briefing, open to<br />
all staff members, the Chief Executive and other<br />
Executive Team members and senior staff provide<br />
information to staff on significant issues and<br />
developments in the Trust to ensure they are kept<br />
fully informed and engaged. Presentations made<br />
during the year have covered areas including:<br />
l Developments in the Respiratory Unit, Lung<br />
Function and Diabetes Home Care;<br />
l SHINE 2012: Quantifying Parental Concern to<br />
Strengthen their Voice<br />
l Young Person’s Advisory Group<br />
l Medium Term Estates Strategy<br />
l Our Future Estates Project<br />
l The BCH Feedback App Pilot<br />
l Critical Care<br />
l Flu Campaign<br />
l <strong>Hospital</strong> Handover<br />
l New Outpatient Pharmacy (Medicine Chest)<br />
l People Strategy 2012-15; The Productive<br />
Operating Theatre<br />
l CAMHS Home Treatment Service<br />
l National NHS staff survey results.<br />
The Trust intranet was redesigned in 2012/13<br />
and provides a central location for a diverse and<br />
continually updated range of information for staff,<br />
from Trust policies and guidance, to recruitment<br />
toolkits and information about each ward and<br />
department. All presentations and videos from<br />
Chief Executive Briefings are also available on the<br />
intranet, allowing access for staff who are unable<br />
to attend the briefing sessions.<br />
We have also implemented a regular staff poll on<br />
the intranet, which surveys staff about things like<br />
whether they would recommend the hospital to<br />
friends and family as a place to work or receive<br />
treatment. We also used this process to find out<br />
the health and wellbeing needs of our staff. The<br />
results of this led to the development of our Health<br />
and Wellbeing Strategy which was launched in<br />
2013.<br />
In addition to encouraging staff to take part in the<br />
annual national Staff Survey, we ask clinical staff<br />
to take part in an annual Staff Safety Survey to<br />
enable us to understand the safety culture of the<br />
organisation and identify areas that may need<br />
development.<br />
Following the publication of the Francis Report<br />
on Mid Staffordshire NHS Foundation Trust in<br />
February 2012 a process was developed to obtain<br />
feedback from staff through a series of listening<br />
events about:<br />
l How we listen to and learn from staff, patients,<br />
families and carers and share this better<br />
throughout the Trust<br />
l How we can work better together in our current<br />
teams to improve patient care and outcomes<br />
with the resources that are available to us<br />
today<br />
l How we can make staff feel more valued and<br />
supported in their jobs.<br />
This process is continuing into 2013/14 and will<br />
culminate in a week-long event in September.<br />
We have also consulted with staff on:<br />
l The behaviours that demonstrate Trust values;<br />
l Internal communications<br />
l Intranet development<br />
l New CAMHS website<br />
l New hospital project<br />
l Feedback App<br />
l Dignity Giving Suits.<br />
Monthly budget reports are distributed to managers<br />
and we continue to report on the financial position<br />
of service lines with this information available to a<br />
range of staff. During the year we have continued<br />
to expand the use of service line financial<br />
information and enhanced the level of information<br />
available to staff and clinicians. Localised training<br />
is undertaken for both core financial duties and<br />
service line information.<br />
Learning from a staff survey undertaken in 2011/12<br />
is shaping the Finance department’s strategy and<br />
objectives. In March 2012 the Finance Department<br />
invested in The Healthcare Financial Management<br />
Association (HFMA) e-learning package which<br />
is suitable for all healthcare professionals and<br />
anyone who wants to gain an awareness and<br />
understanding about aspects of NHS Finance.<br />
The Finance department has assisted in the<br />
Trust’s Consultant Development Programme which<br />
seeks to broaden the knowledge base of the next<br />
generation of clinical leaders.<br />
A detailed Resources Report is contained within<br />
the monthly Public Board of Directors papers which<br />
are available for all staff.<br />
Raising Concerns at Work<br />
Encouraging our staff to have the confidence to<br />
raise any concerns they may have at work has<br />
continued to be of importance to us throughout<br />
2012. To support the updated Whistle Blowing<br />
procedures we have introduced an internal intranet<br />
page to clarify how staff can raise concerns<br />
about work both internally and externally. We<br />
have also updated our Employment Contract to<br />
emphasise the importance of creating an open and<br />
transparent culture with regard to raising concerns<br />
at work.<br />
Mandatory induction and refresher training for<br />
all staff includes risk management training which<br />
encourages staff to report incidents by explaining<br />
why it is important that every incident, including<br />
near misses, is reported. This is so that we can<br />
monitor the safety of processes, identify areas that<br />
must be improved, and learn from our experiences.<br />
54 55<br />
We have also established new systems especially<br />
for trainee doctors to raise concerns. Our Doctors<br />
in Training Safety Hotline provides a mechanism<br />
for concerns about safety to be raised at an early<br />
stage, before any harm is caused. Our Trainee<br />
Advice and Liaison Service (TALS) has been<br />
designed to mimic our Patient Advice and Liaison<br />
Service (PALS). The aim of the service is to help<br />
resolve issues and provide information and advice,<br />
which can include how to escalate any concerns.<br />
Health & Wellbeing<br />
In March 2013 we formally launched our strategy<br />
for improving the health and wellbeing of staff,<br />
children and families. The cornerstone of the<br />
strategy is our responsibility to promote improved<br />
health outcomes for patients. We want to be<br />
ambassadors for initiatives that reduce risk to<br />
health, and to promote healthy lifestyles by<br />
example and through our services. In order to<br />
achieve this we must also meet the health and<br />
wellbeing needs of our most valued resource – our<br />
staff.<br />
We have continued to work closely with<br />
Occupational Health and Staff Support Providers to<br />
ensure the service meets the needs of our staff. In<br />
2012/13 we added a second clinic day which has<br />
allowed more of our staff to access clinical support<br />
onsite, minimising disruption to our services.<br />
Table 3: Table 3:Occupational Health Service Activity 2011/12 – 2012/13<br />
2011/12 2012/13<br />
Number of Referrals 311 376<br />
Number of Pre-employment Screening Assessments 988 1277
A large proportion of staff referrals to the<br />
Occupational Health Service during 2012/13<br />
related to musculoskeletal problems of the lower<br />
limb and back. In response to this, as part of our<br />
Health and Wellbeing Strategy, we are developing<br />
ways to support staff before such problems<br />
develop. We are also reviewing the management<br />
of stress and ways of improving working lives<br />
in addition to the free staff counselling service<br />
available to all staff.<br />
Table 4: Sickness levels –<br />
Trust-wide and directorate 2009/10 – 2012/13<br />
In 2012/13 we repeated our previous year’s flu<br />
campaign with an aim to immunise every staff<br />
member with the flu vaccination.<br />
Throughout 2012/13 the Trust has focused on<br />
improving attendance at work with a combination<br />
of early intervention programmes and facilitating<br />
return to work schemes.<br />
We have set a 3% sickness rate target, which is<br />
regularly monitored and incorporated in our Safety<br />
Dashboard to help us understand where there may<br />
be staff pressures and where this has the potential<br />
to affect the quality of care.<br />
Directorate 2009/10 2010/11 2011/12 2012/13<br />
Clinical Support Services 3.57% 3.68% 3.30% 3.13%<br />
Medical 2.91% 2.90% 3.81% 4.42%<br />
Specialised Services 5.01% 4.33% 4.01% 4.00%<br />
Surgical 4.36% 3.43% 2.98% 3.10%<br />
CAMHS 4.00% 3.85% 4.14% 4.57%<br />
Corporate 4.08% 3.64% 3.52% 2.95%<br />
Trust-wide 4.01% 3.64% 3.66% 3.71%<br />
Equal Opportunities<br />
Our Diversity and Inclusion Strategy sets out our<br />
commitment to ensuring equality and human rights<br />
will be taken into account in everything we do, both<br />
as an employer and a provider of healthcare.<br />
The standards laid out in our Recruitment and<br />
Selection Policy are applied to all candidates for<br />
posts and the Trust’s Recruitment and Selection<br />
Toolkit provides advice on equal opportunities. The<br />
aim of the policy is to ensure that all applicants<br />
who declare a disability are offered an interview if<br />
they meet the minimum requirements for the post.<br />
Monitoring and auditing is used to help identify and<br />
eliminate possible discrimination and to constantly<br />
improve recruitment processes.<br />
All employees that become disabled during their<br />
employment are managed through the sickness<br />
policy or capability policy and all efforts are made<br />
to ensure ongoing employment with reasonable<br />
adjustments, training and career development.<br />
Other Trust policies which ensure equal<br />
opportunities for all staff include:<br />
l Maternity Leave policy;<br />
l Flexible and Family Friendly Working Policy;<br />
l Dignity at Work Policy, which describes<br />
our processes to provide a positive working<br />
environment to with zero tolerance to bullying<br />
and harassment.<br />
Social and Community Issues<br />
It is our ambition to be the employer and service<br />
provider of choice and an advocate for children<br />
and young people in <strong>Birmingham</strong> and the West<br />
Midlands. This means more than providing acute<br />
health care. It also means taking the opportunities<br />
provided by our position in the community, and<br />
using our specialist knowledge and skills to help<br />
improve health outcomes and future opportunities<br />
for children and young people, whatever their<br />
ethnic, cultural or social background.<br />
Working to meet this ambition requires us to<br />
engage with our service users and the community<br />
to find out what they want and need. It’s also<br />
important that we look to the future to make sure<br />
we are prepared for the challenges to come over<br />
the next 20 years. As the population in <strong>Birmingham</strong><br />
and the West Midlands rises it is becoming<br />
increasingly diverse and the population of children<br />
and young people is expected to rise dramatically.<br />
We need to make sure our future strategy is able<br />
to meet the changing needs of our community.<br />
Being a champion for children and young people<br />
is one of our strategic objectives. We believe<br />
that developing our position as an advocate and<br />
provider of public health advice will help improve<br />
the lives of the children and young people who use<br />
our services and who live in the West Midlands.<br />
BACK TO CONTENTS PAGE<br />
We have a range of initiatives that will help us<br />
meet these goals:<br />
l Our Health and Wellbeing Strategy sets out<br />
our commitment to using every opportunity<br />
to improve the health and wellbeing of the<br />
children, young people and families we see<br />
at the hospital. We do this through Making<br />
Every Contact Count (MECC) - an initiative<br />
that asks all NHS staff to deliver brief<br />
healthy lifestyle advice in the right way at<br />
the right time. Over the last year this work<br />
has been having a positive impact through<br />
supporting parents to stop smoking,<br />
referring children to local healthy weight<br />
groups, and giving out healthy start vitamins<br />
to prevent vitamin D deficiency.<br />
l Healthwatch <strong>Birmingham</strong> is a new<br />
organisation being set up to provide<br />
an independent voice for the people of<br />
<strong>Birmingham</strong> and to help shape and improve<br />
local health and social care services. We<br />
have started working with them to ensure<br />
that young people are able to participate.<br />
l Our Widening Participation Team helps us<br />
deliver our priority to improve opportunities<br />
for our most junior members of staff by<br />
supporting them to develop their careers.<br />
The team also works with community<br />
partners to offer apprenticeships,<br />
internships and work experience to young<br />
people.<br />
l We are working with the <strong>Birmingham</strong><br />
Muslim community to develop a wider<br />
understanding of organ donation.<br />
l The Young Person’s Advisory Group<br />
(YPAG)are growing as an influential voice<br />
both within the hospital and in the<br />
wider NHS community, providing views on<br />
developments to our services and on the<br />
NHS Future Forum and NHS Constitution.<br />
l We are becoming a national leader in<br />
our learning disability work, particularly in<br />
engagement with patients and families from<br />
Asian communities.<br />
56 57
BACK TO CONTENTS PAGE<br />
Health and Safety Performance<br />
The most significant risks to the non-clinical safety<br />
of our patients, staff and visitors are monitored by<br />
our Non-Clinical Risk Coordinating Committee.<br />
A Non-Clinical Safety Report is presented every<br />
two months to our Quality Committee to provide<br />
assurance about what is being done to make sure<br />
our environment and practices are as safe and<br />
secure as they can be.<br />
In 2012/13 there have been:<br />
l No Dangerous Occurrences as defined in<br />
Reporting of Injuries Diseases and Dangerous<br />
Occurrences Regulations (RIDDOR)<br />
l No Diseases as defined in RIDDOR<br />
l One Major Injury as defined in RIDDOR<br />
(a visitor fell down a step in a public corridor)<br />
l No HSE improvement notices<br />
l No HSE prohibition notices<br />
l Two fires:<br />
A small electrical fire in an office block<br />
kitchen<br />
Deep fat fryer oil ignited causing fire in<br />
catering department.<br />
l No Non-Clinical Safety related Serious Incidents<br />
Requiring Investigation<br />
l No non-clinical safety related Never Events.<br />
experience, safeguarding and infection control, as<br />
well as progress against our safety strategy, and<br />
quality projects such as the Safety Thermometer<br />
and our programme of Quality Walkabouts.<br />
This Quality Report is considered by the Board of<br />
Directors every month alongside our Resources<br />
Report, which provides details of the Trust’s<br />
financial performance and examines the Trust’s<br />
activity levels, access to our services and<br />
workforce indicators, such as sickness levels,<br />
turnover, and targets for mandatory training and<br />
appraisal. This report helps the Board identify<br />
where pressures at work may be having an impact<br />
on our staff, which could in turn impact on the<br />
quality of services.<br />
At the beginning of 2012/13 - following an<br />
independent governance review - we established<br />
a new committee structure, which aimed to<br />
support the Board to focus on the right things by<br />
strengthening the committees that report to it.<br />
The Finance and Investment Committee became<br />
the Finance and Resources Committee, with a<br />
widened remit to consider all the Trust’s resources,<br />
including the most important – our staff. A new<br />
Quality Committee was set up which receives<br />
information about patient safety, non-clinical<br />
safety, patient experience, staff engagement<br />
and regulatory compliance. At each meeting<br />
the Committee undertakes a detailed review<br />
of a quality theme identified as an area that<br />
needs greater focus. In 2012/13 the Committee<br />
considered the following themes:<br />
l Learning Disabilities –<br />
Providing Personalised Care;<br />
The Board Assurance Framework (BAF) provides<br />
a structure and process to enable the Board to<br />
understand and focus on the risks to achieving the<br />
organisation’s strategic objectives and to assist the<br />
Board in discharging its responsibility for internal<br />
control. The content of and processes surrounding<br />
the BAF were reviewed by the Internal Auditor in<br />
2012/13. The review gave significant assurance,<br />
but a number of recommendations were made for<br />
improvement, and these are being implemented.<br />
All reports to the Board and its committees detail<br />
any potential impact on compliance with the Care<br />
Quality Commission’s (CQC) 16 core essential<br />
standards of quality and safety. This information -<br />
together with the Board’s regular reviews of quality<br />
- provides an oversight of areas which might be at<br />
risk of non-compliance with the standards.<br />
In 2012 both the Trust’s locations, at Parkview and<br />
Steelhouse Lane, received a routine, unannounced<br />
inspection from CQC. The review of CAMHS at<br />
Parkview found full compliance with the standards<br />
reviewed.<br />
The review at Steelhouse Lane found a minor<br />
non-compliance with standard 14: Supporting<br />
workers. This finding related to a concern raised<br />
by some of our theatre staff about the way<br />
they were supported, particularly in relation to<br />
the implementation of a new way of working in<br />
Theatres.<br />
In response we have changed the way we are<br />
implementing the new process and have engaged<br />
closely with the theatre staff to fully understand<br />
their concerns and address them. In addition, we<br />
have developed new ways of reporting potential<br />
workforce issues to the Board and its committees,<br />
to identify as early as possible when our staff<br />
may be feeling unhappy, unsupported, or under<br />
pressure.<br />
When considering the quality of our services, it<br />
is essential to consider whether anybody is at a<br />
disadvantage because of certain characteristics.<br />
In 2012/13 the Board of Directors held a workshop<br />
to consider diversity and inclusion and began to<br />
prepare a strategy for how the Trust can become<br />
the healthcare provider and employer of choice by<br />
responding to the unique needs of every patient<br />
and every member of staff.<br />
The Board agreed that, while it is not included in<br />
the Equality Legislation, a characteristic that is<br />
relevant to people’s health and the way people<br />
access health services is socio-economic status.<br />
The Quality Committee will therefore consider<br />
in 2013/14 how this characteristic can be<br />
incorporated into the Trust’s Diversity and Inclusion<br />
Strategy.<br />
The Trust is satisfied that there are no material<br />
inconsistencies between the Annual Governance<br />
Statement, the Annual Report, the Quality Report,<br />
and the annual and quarterly Board statements<br />
required by the Compliance Framework.<br />
More information about quality governance and<br />
quality can be found in our Quality Report at page<br />
92 and in the Annual Governance Statement on<br />
page 144.<br />
Enhanced Quality Governance<br />
Reporting<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust is continually striving to improve the quality<br />
of the services it provides, in terms of safety,<br />
patient experience and clinical effectiveness.<br />
Quality continues to be at the heart of our strategic<br />
objectives which ensures a constant focus on<br />
quality at all levels of the Trust, including meetings<br />
of the Board and its committees.<br />
Every Board meeting agenda is aligned to these<br />
strategic objectives and the Board of Directors<br />
receives reports describing progress in and risks<br />
to achieving our goals. This includes an integrated<br />
Quality Report, which provides an overview of the<br />
main indicators of quality across the Trust. This<br />
includes high risks, incidents, mortality, patient<br />
l Caring for our Staff = Better Care;<br />
l Medication Omission – Sepsis;<br />
l Developing a Palliative Care Service;<br />
l The potential quality impact on our CAMHS and<br />
other services if funding is reduced.<br />
In February 2013 our Internal Auditor completed<br />
a review of the Trust’s Quality Governance<br />
arrangements against Monitor’s Quality<br />
Governance Framework. This review found<br />
that the Trust meets Monitor’s criteria, and<br />
provides ‘significant assurance’ that the Trust’s<br />
arrangements are sound. A small number of areas<br />
were identified that could be improved, and we<br />
are implementing the recommendations of the<br />
Internal Auditor so we can ensure that our quality<br />
governance arrangements are the best they can<br />
be.<br />
58 59
BACK TO CONTENTS PAGE<br />
Consultations<br />
l Providing patient stories<br />
Remuneration Report<br />
Information not subject to audit<br />
Appointments and Remuneration<br />
Committee<br />
We apply the principles of good corporate<br />
governance in relation to the Directors’<br />
remuneration defined in the Companies Act 2006<br />
and interpreted for NHS Foundation Trusts.<br />
The remuneration, terms and conditions of<br />
employment of Executive Directors are determined<br />
by the Appointments and Remuneration<br />
Committee, a committee of the Board of Directors.<br />
The Committee is chaired by the Trust Chairman<br />
and members include two Non-Executive Directors.<br />
The Chief Executive Officer and the Company<br />
Secretary attend by invitation to provide advice<br />
and assist the Committee in their consideration of<br />
matters such as succession planning.<br />
During 2012/13 we consulted with YPAG, children,<br />
young people, patients, parents and families on:<br />
l New CAMHS website; Feeback App<br />
l Dignity Giving Suits<br />
l Outpatient department redesign<br />
l Outpatient Pharmacy design and name<br />
(Medicine Chest)<br />
l Specialist <strong>Hospital</strong> Services<br />
l NHS Constitution development<br />
l Theatre pathway project.<br />
Children, young people, patients, parents and<br />
families have also participated in:<br />
l Outpatient Department Redesign Steering<br />
Group<br />
l Delivering training for staff on participation and<br />
learning disability issues<br />
l Learning Disabilities Steering Group<br />
l Development of a parent drop-in session<br />
l Emergency Care Pathway development<br />
l Patient handover project<br />
l ‘Shine’ project to develop a tool to measure<br />
parental concerns about their child’s condition<br />
l Leukaemia multi-disciplinary team user survey.<br />
We have also engaged with the Health Overview<br />
and Scrutiny Committee on our future strategy.<br />
Future Developments<br />
In 2012/13 we plan to:<br />
l Develop our Rare Diseases Strategy;<br />
l Commence capital works for the expansion<br />
of theatres, PICU and cancer services and<br />
improvements in the Emergency and main<br />
Outpatients departments<br />
l Develop with our partners a <strong>Birmingham</strong><br />
Children’s Network, that enables high quality,<br />
high value health care for children and young<br />
people across <strong>Birmingham</strong><br />
l Develop a cultural barometer<br />
l Implement an E-Prescribing system<br />
l Develop our Advanced Nurse Practitioner<br />
workforce.<br />
Table 5: Appointments and Remuneration Committee Attendance 2012/13<br />
Appointments & Remuneration Committee – Members’ attendance 2012/13<br />
Member Sept 2012 Nov 2012 Total<br />
Keith Lester, Interim Chairman 4 4 2/2<br />
Judith Green Senior Independent Director* n/a 4 1/1<br />
Elaine Simpson, Non-Executive Director 4 4 2/2<br />
Roger Peace, Non-Executive Director 4 n/a 1/1<br />
* Judith Green replaced Roger Peace on the Committee in November 2012.<br />
When determining the remuneration of<br />
Directors, the Appointments and Remuneration<br />
Committee considered the advice provided by the<br />
Department of Health in relation to the uplift in<br />
salaries for senior managers, referred to national<br />
benchmarking information and took into account<br />
the recommendations of the NHS Review Body.<br />
In line with the national pay freeze, the Directors<br />
did not receive a remuneration increase in<br />
2012/13. The Directors did not receive the national<br />
pay uplift of 1% from 1 April 2013.<br />
No element of the remuneration of Executive<br />
Directors is subject to performance conditions,<br />
although performance is reviewed through the<br />
appraisal process. There are no non-cash benefits<br />
60 61<br />
or elements of remuneration that are not cash,<br />
other than the Lease Car Scheme. All contracts are<br />
permanent with notice periods of six months.<br />
The terms and conditions of contract and the<br />
remuneration of the Chairman and Non-Executive<br />
Directors are determined by the Nominations<br />
Committee, a committee of the Council of Governors<br />
(see page 82). Non-executive directors receive no<br />
benefits or entitlements other than expenses and are<br />
not entitled to termination payments.<br />
The appointment of the Chairman and Non-<br />
Executive Directors can be terminated by the<br />
agreement of the majority of the Council of<br />
Governors at a general meeting of the Council of<br />
Governors.
Senior Manager Service Contracts<br />
A senior manager is defined as an Executive or<br />
Non-Executive Director of the Board.<br />
Table 6: Senior Manager Service Contract Details<br />
Senior Manager Title Date of Unexpired Notice Provision for<br />
contract term period compensation<br />
for early<br />
termination<br />
Mrs Joanna Davis Chairman 01/11/2003 10 months 1 month none<br />
(informal)<br />
Mr Keith Lester Interim Chairman 01/12/2003 22 months 1 month none<br />
(informal)<br />
Mrs Judith Green Deputy Chairman 01/04/2006 10 months 1 month none<br />
(informal)<br />
Mr Colin Horwath Deputy Chairman 01/05/2008 14 months 1 month none<br />
informal)<br />
Professor Jon Glasby Non-Executive 01/06/2010 3 months 1 month none<br />
Director<br />
(informal)<br />
Mr Zubair Khan Non-Executive 01/06/2011 term ended n/a none<br />
Director<br />
December<br />
2012<br />
Mrs Elaine Simpson Non-Executive 08/02/2012 11 months 1 month none<br />
Director<br />
(informal)<br />
Roger Peace Non-Executive 03/07/2012 3 months 1 month none<br />
Director<br />
(informal)<br />
Ms Sarah Jane Marsh Chief Executive 01/09/2010 n/a – 6 months none<br />
Officer (substantive) permanent<br />
appointment<br />
Mr David Melbourne Chief Finance 01/11/2009 n/a – 6 months none<br />
Officer/Interim Chief<br />
permanent<br />
Executive Officer<br />
appointment<br />
Dr Vin Diwakar Chief Medical 09/10/2009 n/a – 6 months none<br />
Officer<br />
permanent<br />
appointment<br />
Mrs Michelle Chief Nursing 01/08/2007 n/a – 6 months none<br />
McLoughlin Officer permanent<br />
appointment<br />
Mr David Eltringham Chief Operating 06/11/2009 Appointment n/a none<br />
Officer<br />
ended<br />
September<br />
2012<br />
Mrs Theresa Nelson Chief Officer for 06/06/2011 n/a – 6 months none<br />
Workforce<br />
permanent<br />
Development<br />
appointment<br />
Mr Tim Atack Chief Operating 17/09/2012 n/a – 6 months none<br />
Officer<br />
permanent<br />
appointment<br />
Mr Phil Foster Interim Chief 01/11/2012 Fixed term to n/a none<br />
Finance Officer June 2013<br />
Information Subject to Audit: Salary and Pension<br />
entitlements of senior managers<br />
Table 7: Remuneration 2012-13 1st April 2012 to 31st March 2013<br />
62 63<br />
BACK TO CONTENTS PAGE<br />
Name and Title Salary Other<br />
Remuneration<br />
Benefits<br />
in Kind<br />
Notes (bands (bands Rounded<br />
of of to the<br />
£5,000) £5,000) neareste<br />
£100<br />
Mrs Joanna Davis Chairman 4 40-45 0 0<br />
Mr Keith Lester Non-Executive/Interim Chairman 5 25-30 0 0<br />
Mrs Judith Green Non-Executive Director/Deputy 6 15-20 0 0<br />
Chair, Engagement<br />
and Participation<br />
Mr Colin Horwath Non-Executive Director/Deputy 7 15-20 0 0<br />
Chair, Strategy and Partnerships<br />
Ms Sarah-Jane Marsh Chief Executive Officer 8 135-140 0 0<br />
Mr David Melbourne Chief Financial Officer/Interim 9 125-130 0 2,300<br />
Chief Executive Officer<br />
Mr Philip Foster Interim Chief Finance Officer 10 35-40 0 0<br />
Director<br />
Mr David Eltringham Chief Operating Officer 11 45-50 0 0<br />
Mr Tim Atack Chief Operating Office 12 50-55 0 0<br />
Mrs Michelle Chief Nursing Officer<br />
McLoughlin 100-105 0 0<br />
Dr Vinod Diwakar Chief Medical Officer 40-45 115-120 2,400<br />
Mrs Theresa Nelson Chief Officer for 100-105 0 2,400<br />
Workforce Development<br />
Miss Elaine Simpson Non-Executive Director 10-15 0 0<br />
Mr Zubair Khan Non-Executive Director 13 10-15 0 0<br />
Professor Jon Glasby Non-Executive Director 15-20 0 0<br />
Mr Roger Peace Non-Executive Director 14 10-15 0 0<br />
Total<br />
2012/13 935-940 115-120 7,100<br />
Total<br />
2011/12 795-800 145-150 4,600<br />
Notes:<br />
1) The definition of Senior Managers includes only the Chief Officers and the Non-Executive Directors.<br />
These are the senior officers of the Trust having Board of Director voting powers.<br />
2) Benefit in kind relates to lease cars.<br />
3) Other Remuneration relates to work not directly related to Chief Officer duties.<br />
4) Ms Joanna Davis commenced sick leave on 16th April 2012.<br />
5) Mr Keith Lester took up position as Interim Chairman from 4th July 2012.<br />
6) Mrs Judith Green and took up position as Deputy Chair, Engagement and Participation from 4th July 2012.<br />
7) Mr Colin Horwath took up position as Deputy Chair, Strategy and Partnerships from 4th July 2012.<br />
8) Ms Sarah-Jane Marsh started Maternity Leave from 1st November 2012.<br />
9) Mr David Melbourne took up position as Interim Chief Executive from 1st November 2012.<br />
10) Mr Phil Foster took up position as Interim Chief Finance Officer from 1st November 2012.<br />
11) Mr David Eltringham resigned his position as Chief Operating Officer from 14th September 2012.<br />
12) Mr Tim Atack took up position as Chief Operating Officer from 17th September 2012.<br />
13) Mr Mohammed Zubair Khan ended his term as Non Executive Director on 31st December 2012.<br />
14) Mr Roger Peace took up position as Non Executive Director from 4th July 2012.
64 65<br />
Table 8: Remuneration 2011-12 1st April 2011 to 31st March 2012<br />
Name and Title Salary Other Benefits<br />
Remuneration in Kind<br />
Notes (bands of (bands of Rounded<br />
£5,000) £5,000) to the<br />
£000 £000 nearest<br />
£100<br />
Ms Joanna Davis Chairman 50-55 0 0<br />
Ms Sarah-Jane Marsh Chief Executive Officer 155-160 0 0<br />
Mr David Melbourne Deputy Chief Executive 115-120 0 2,300<br />
Chief Financial Officer<br />
Mr David Eltringham Chief Operating Officer 100-105 0 0<br />
Mrs Michelle<br />
Chief Nursing Officer<br />
McLoughlin 100-105 0 0<br />
Dr Vinod Diwakar Chief Medical Officer 3 40-45 115-120 2,300<br />
Mr Garrett Taylor<br />
Mrs Theresa Nelson<br />
Chief Officer for Governance<br />
and Education 4 and 5 20-25 30-35 0<br />
Chief Officer for<br />
Workforce Development 6 60-65 0 0<br />
Mrs Judith Green Non Executive Director 10-15 0 0<br />
Mrs Elaine Simpson Non Executive Director 7 0-5 0 0<br />
Mr Colin Horwath Non Executive Director 10-15 0 0<br />
Mr Keith Lester Non Executive Director 15-20 0 0<br />
Mr Zubair Khan Non Executive Director 8 10-15 0 0<br />
Professor Jon Glasby Non Executive Director 10-15 0 0<br />
Mr Niels de Vos Non Executive Director 9 0-5 0 0<br />
Total 795-800 145-150 4,600<br />
Notes:<br />
1) The definition of Senior Managers includes only the Chief Officers and the Non-Executive Directors.<br />
These are the senior officers of the Trust having Board of Director voting powers.<br />
2) Benefit in kind relates to lease cars.<br />
3) The Other Remuneration relates to work not directly related to Chief Officer duties.<br />
4) Mr Garrett Taylor, Chief Officer for Governance and Education resigned his post with effect from<br />
17th June 2011.<br />
5) The Other Remuneration relates to the contractual package due to Mr Taylor on his resignation.<br />
6) Mrs Theresa Nelson, Chief Officer for Workforce Development took up post with effect from<br />
1st September 2011.<br />
7) Mrs Elaine Simpson took up position as Non Executive Director with effect from 1st February 2012.<br />
8) Mr Zubair Khan took up position as Non Executive Director with effect from 1st June 2011.<br />
9) Mr Niels de Vos resigned his position as Non Executive Director effective from 31st May 2011.<br />
Real<br />
increase/<br />
(decrease)<br />
in pension<br />
and<br />
related<br />
lump sum<br />
at age 60<br />
Total<br />
accrued<br />
pension<br />
and<br />
related<br />
lump sum<br />
at age<br />
60 at 31<br />
March<br />
2013<br />
Notes:<br />
1) The Real increase in pension and related lump sum at age 60 has been compared with a zero balance last year.<br />
Cash<br />
Equivalent<br />
Transfer<br />
Value at<br />
31 March<br />
2013<br />
Cash<br />
Equivalent<br />
Transfer<br />
Value at<br />
31 March<br />
2012<br />
As Non-Executive members do not receive pensionable remuneration, there will be no entries in respect of pensions for Non-Executive members.<br />
BACK TO CONTENTS PAGE<br />
Real<br />
Increase/<br />
(decrease)<br />
in Cash<br />
Equivalent<br />
Transfer<br />
Value<br />
Employers<br />
Contribution<br />
to<br />
Stakeholder<br />
Pension<br />
(bands (bands To To To To<br />
Name and Title Notes of of nearest nearest nearest nearest<br />
£2,500) £5,000) £1,000 £1,000 £1,000 £100<br />
Ms Sarah-Jane Marsh Chief Executive Officer 10.00-12.50 85-90 272 234 38 0<br />
Mr David Melbourne Chief Financial Officer/Interim<br />
Chief Executive Officer 17.50-20.50 150-155 691 587 104 0<br />
Mr David Eltringham Chief Operating Officer 15.00-17.50 115-120 446 372 74 0<br />
Mrs Michelle McLoughlin Chief Nursing Officer 10.00-12.50 125 531 471 60 0<br />
Dr Vinod Diwakar Chief Medical Officer 5.00-7.50 130 523 486 37 0<br />
Mr Tim Atack Chief Operating Officer 1 120.00-122.50 120-125 518 0 518 0<br />
Mrs Theresa Nelson Chief Officer for Workforce<br />
Development 0.00-2.50 35-40 159 151 8 0<br />
Mr Philip Foster Interim Chief Finance Officer 1 102.50-105.50 105-110 414 0 414 0<br />
A Cash Equivalent Transfer Value (CETV) is the actuarially assessed capital value of the pension scheme benefits accrued by a member at a particular point in time. The benefits valued are<br />
the member’s accrued benefits and any contingent spouse’s pension payable from the scheme. A CETV is a payment made by a pension scheme, or arrangement to secure pension benefits<br />
in another pension scheme or arrangement when the member leaves a scheme and chooses to transfer the benefits accrued in their former scheme. The pension figures shown relate to the<br />
benefits that the individual has accrued as a consequence of their total membership of the pension scheme, not just their service in a senior capacity to which the disclosure applies. The CETV<br />
figures, and from 2004-05 the other pension details, include the value of any pension benefits in another scheme or arrangement which the individual has transferred to the NHS pension<br />
scheme. They also include any additional pension benefit accrued to the member as a result of their purchasing additional years of pension service in the scheme at their own cost. CETVs are<br />
calculated within the guidelines and framework prescribed by the institute and Faculty of Actuaries.<br />
Table 9: Pension Benefits 2012-13
BACK TO CONTENTS PAGE<br />
The slight reduction in the ratio is a result of the remuneration of the highest paid director remaining<br />
unchanged whilst the median salary has increased slightly. This increase in the median salary is a<br />
consequence of clinical developments that have increased the medical and nursing workforce (6% and 4%<br />
respectively) at a higher rate than non-clinical. The clinical workforce associated with these developments<br />
has an average salary that is higher than the non-clinical workforce.<br />
Signed…………………………………………….. Date: 29 May 2013<br />
David Melbourne, Interim Chief Executive Officer<br />
Real Increase/(Decrease) in CETV - This reflects the increase in CETV effectively funded by the employer. It takes account of the increase in accrued<br />
pension due to inflation, contributions paid by the employee (including the value of any benefits transferred from another pension scheme or arrangement)<br />
and uses common market valuation factors for the start and end of the period.<br />
Real<br />
increase/<br />
(decrease)<br />
in pension<br />
and<br />
related<br />
lump sum<br />
at age 60<br />
Total<br />
accrued<br />
pension<br />
and<br />
related<br />
lump sum<br />
at age<br />
60 at 31<br />
March<br />
2012<br />
Cash<br />
Equivalent<br />
Transfer<br />
Value at<br />
31 March<br />
2012<br />
Cash<br />
Equivalent<br />
Transfer<br />
Value at<br />
31 March<br />
2011<br />
Real<br />
Increase/<br />
(decrease)<br />
in Cash<br />
Equivalent<br />
Transfer<br />
Value<br />
Employers<br />
Contribution<br />
to<br />
Stakeholder<br />
Pension<br />
(bands (bands To To To To<br />
Name and Title Notes of of nearest nearest nearest nearest<br />
£2,500) £5,000) £1,000 £1,000 £1,000 £100<br />
Table 10: Pension Benefits 2011-12<br />
Director and Governor Expenses<br />
Table 11 Expenses paid to Directors<br />
Total Expenses paid<br />
Name on Payslips for 2012/13<br />
Ms Joanna Davis £282.53<br />
Mr Keith Lester £1,996.32<br />
Mrs Judith Green £657.73<br />
Mr Colin Horwath<br />
NIL<br />
Table 12 Expenses paid to Governors<br />
Name<br />
Total Expenses paid<br />
Mr David Akuoko £152.50<br />
Mrs Jenny Robinson £10.00<br />
Mr Anthony Veal £65.65<br />
Ms Sarah-Jane Marsh Chief Executive Officer 6.75-7.00 70-80 234 156 78 0<br />
Ms Sarah-Jane Marsh £33.00<br />
Mr David Melbourne Deputy Chief Executive/<br />
Financial Officer 11.25-11.50 130-135 587 476 111 0<br />
Mr David Eltringham Chief Operating Officer 5.00-5.25 100-105 372 292 80 0<br />
Mr David Melbourne £296.80<br />
Mr Philip Foster £356.19<br />
Mrs Michelle McLoughlin Chief Nursing Officer 10.5-10.75 110-115 471 373 98 0<br />
Dr Vinod Diwakar Chief Medical Officer 5.75-6.00 125-130 486 389 97 0<br />
Mr Garrett Taylor Chief Officer for Governance<br />
and Education 1.00-1.25 40-45 169 161 8 0<br />
Mrs Theresa Nelson Chief Officer for Workforce<br />
Development 1 37.50-38.00 35-40 151 0 151 0<br />
Mr David Eltringham NIL<br />
Mr Tim Atack<br />
NIL<br />
Mrs Michelle McLoughlin NIL<br />
Dr Vinod Diwakar NIL<br />
Notes:<br />
1) The Real increase in pension and related lump sum at age 60 has been compared with a zero balance the previous year.<br />
Mrs Theresa Nelson £601.47<br />
Median Remuneration<br />
Mrs Elaine Simpson<br />
NIL<br />
The banded remuneration of the highest paid director at the Trust in the 2012/13 financial year was £160,000-£165,000 (2011/12, £160,000-£165,000). This was 5.88 times (2011/12, 6.12 times)<br />
the median remuneration of the workforce, which was £27,625 (2010/11, £26,556).<br />
Total remuneration includes salary, non-consolidated performance related pay, benefits-in-kind as well as severance payments. It does not include pension contributions and the cash equivalent<br />
transfer value of pensions.<br />
Mr Zubair Khan £230.48<br />
Professor Jon Glasby £330.00<br />
Mr Roger Peace NIL<br />
66 67
68 69<br />
NHS Foundation Trust Code of Governance<br />
Council of Governors<br />
Constitutionally formed, the Council of Governors<br />
has the following key responsibilities:<br />
l Strategic – Providing advice on our general<br />
direction and ensuring that our plans assist in<br />
the delivery of our long-term goals<br />
l Guardianship – Ensuring that the Board of<br />
Directors conform to the terms of authorisation,<br />
acting as a trustee of the Trust<br />
l Advisory – Providing advice to the Board of<br />
Directors to ensure that we continue to deliver<br />
services to meet the needs of the members,<br />
patients, parents, families and the wider local<br />
communities.<br />
The Council of Governors is specifically<br />
responsible for:<br />
l Representing the views of the members and<br />
acting as a source of information on members’<br />
needs<br />
l Working with the Board of Directors to inform<br />
the future strategic direction and development<br />
plan<br />
l Appointing (and removing) the Chairman and<br />
Non-Executive Directors<br />
l Setting the salary levels of the Chairman and<br />
Non-Executive Directors<br />
l Approving the appointment of the Chief<br />
Executive Officer; Appointing the External<br />
Auditor<br />
l Receiving copies of our annual reports, annual<br />
accounts and the External Auditor’s report<br />
l Holding the Non-Executive Directors individually<br />
and collectively to account<br />
The Board of Directors is legally accountable<br />
for the services we provide and is specifically<br />
responsible for:<br />
l Setting the strategic direction (having taken into<br />
account the Council of Governors’ views)<br />
l Ensuring that clinical services provide highquality<br />
and safe care for patients, parents and<br />
their families<br />
l Ensuring that governance arrangements are<br />
implemented to provide assurance that there<br />
are safe systems of internal control in place<br />
l Ensuring that a rigorous performance<br />
management framework is implemented which<br />
ensures that we continue to be a high performer<br />
against national and local targets<br />
l Ensuring that we are at all times compliant with<br />
our Terms of Authorisation.<br />
The Constitution sets out the key responsibilities<br />
of the Board of Directors. The accountability<br />
framework defines the committees of the Board<br />
and sets out within the approved terms of<br />
reference the responsibilities for each of these<br />
committees. Non-Executive Directors are members<br />
(or the Chair) of each of these committees.<br />
Composition of the Council of Governors<br />
The Council of Governors comprises 18 elected<br />
governors (10 public governors, one carer<br />
governor, three patient governors and four<br />
staff governors) and nine appointed governors<br />
(from four Primary Care Trusts and five partner<br />
organisations). The PCT governor posts are<br />
currently vacant following a review of the<br />
commissioning arrangements for the Trust. One<br />
partner organisation governor post (Extended<br />
Schools) is currently vacant as this organisation<br />
no longer exists. The Council of Governors will<br />
consider an alternative partner organisation to<br />
be represented by a governor. The Council of<br />
Governors is chaired by The Interim Chairman,<br />
Mr Keith Lester. The Vice Chair and Lead<br />
Governor is Public Governor for <strong>Birmingham</strong>,<br />
Mr Philip Crombie.<br />
l Approving any amendments to the Core<br />
Constitution.<br />
Members of the Council of Governors
BACK TO CONTENTS PAGE<br />
Table 13: Composition of the Council of Governors and attendance at meetings 2012/13<br />
Governor Constituency/Class Tenure Attendance<br />
Mr Philip Crombie <strong>Birmingham</strong> 3 years from September 2010<br />
(second term) 4/4<br />
Mr Mark Kelly <strong>Birmingham</strong> 3 years from September 2011 1/4<br />
Mr David Akuoko <strong>Birmingham</strong> 3 years from September 2010 1/4<br />
Mr Brian Stokes Dudley/Walsall/Wolverhampton 3 years from September 2010<br />
(second term) 4/4<br />
Mr Ian Evans-Fisher Herefordshire/Worcestershire 3 years from September 2010 4/4<br />
Mr Anthony Veal Solihull 3 years from September 2010<br />
(second term) 2/4<br />
Mr Brian Broughton Coventry/Warwickshire Term ended September 2012 2/4<br />
Mr Martin Cossum Sandwell 3 years from January 2011 2/4<br />
Mr Robert Foster Staffordshire/Shropshire 3 years from September 2011<br />
(second non-consecutive term) 4/4<br />
Mr Tim Edwards Staffordshire/Shropshire 3 years from April 2011 4/4<br />
Mrs Sarah Simon Coventry/Warwickshire 3 years from November 2012 2/2<br />
Mrs Jenny Robinson Carer 3 years from September 2010 4/4<br />
Mr Joshua Millwood Patient 3 years from January 2011 2/4<br />
Miss Ellie Milner Patient 3 years from January 2011 2/4<br />
Miss Emma Wilson Patient 3 years from September 2011 2/4<br />
Dr Robert Sunderland Medical/Dental Term ended September 2013 1/2<br />
Mrs Karen Kelly Non Clinical 3 years from September 2011 4/4<br />
Ms Bernadette Weeks Nursing 3 years from September 2010<br />
(second term) 3/4<br />
Mr David Rist Other Clinical Term ended September 2012 0/2<br />
Dr Michael Kuo Medical/Dental 3 years from November 2012 1/2<br />
Carl Harris Other Clinical 3 years from November 2012 2/2<br />
Ms Hilary Brown University of <strong>Birmingham</strong> 3 years from September 2010 3/4<br />
Professor Stuart Brand <strong>Birmingham</strong> City University Resigned September 2012 2/3<br />
Professor Ian Blair <strong>Birmingham</strong> City University 3 years from November 2012 1/1<br />
Table 14: Directors’ attendance at Council of Governors Meetings<br />
Director Position Attendance<br />
Mr Keith Lester Interim Chairman 4/4<br />
Mrs Judith Green Non-Executive Director 2/4<br />
Mr Colin Horwath Non-Executive Director 0/4<br />
Professor Jon Glasby Non-Executive Director 0/4<br />
Mr Zubair Khan Non-Executive Director (until December 2012) 2/3<br />
Mrs Elaine Simpson Non-Executive Director 3/4<br />
Mr Roger Peace Non-Executive Director (from July 2012) 1/2<br />
Ms Sarah Jane Marsh Chief Executive Officer (maternity leave from November 2012) 1/2<br />
Mr David Melbourne Chief Finance Officer/Interim Chief Executive 4/4<br />
Dr Vin Diwakar Chief Medical Officer 3/4<br />
Mrs Michelle McLoughlin Chief Nursing Officer 4/4<br />
Mr David Eltringham Chief Operating Officer (to September 2012) 0/2<br />
Mrs Theresa Nelson Chief Officer for Workforce Development 0/4<br />
Mr Tim Atack Chief Operating Officer (from September 2012) 0/2<br />
Mr Phil Foster Interim Chief Finance Officer (from November 2012) 2/2<br />
Council of Governors Elections 2012/13<br />
One election was held in 2012/13 for three vacant<br />
positions on the Council of Governors, all of which<br />
were filled.<br />
Table 15: Governor Election Results 2012<br />
Governor Election Autumn 2012<br />
Constituency Turnout Successful Candidate<br />
Public: Coventry/Warwickshire Uncontested Mrs Sarah Simon<br />
Staff: Medical Dental Uncontested Dr Michael Kuo<br />
Staff: Other Clinical 18.6% Mr Carl Harris<br />
Ms Caroline Anson<br />
Mrs Katy Cook<br />
<strong>Birmingham</strong> Voluntary<br />
Service Council Resigned August 2012 0/2<br />
<strong>Birmingham</strong> Voluntary<br />
Service Council Resigned March 2013 1/2<br />
Cllr Valerie Seabright <strong>Birmingham</strong> City Council 3 years from November 2012 1/1<br />
Directors are invited by the Council to attend meetings of the Council of Governors to present reports and information.<br />
70 71
72 73<br />
BACK TO CONTENTS PAGE<br />
Declaration of Interests of the Council<br />
of Governors<br />
All members of the Council of Governors are<br />
required to make known at each meeting any<br />
interest they have in the matters being discussed.<br />
They also make an annual declaration of interests<br />
which is recorded in the Register of Interests. The<br />
Board of Directors is satisfied that the Governors<br />
hold no material interests in organisations where<br />
those organisations or related parties are likely<br />
to do business, or are possibly seeking to do<br />
business with <strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS<br />
Foundation Trust.<br />
The Register of Interests of the Council of<br />
Governors is held by the Company Secretary and<br />
can be accessed by contacting:<br />
The Company Secretary<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust<br />
Steelhouse Lane<br />
<strong>Birmingham</strong><br />
B4 6NH<br />
Governors are also involved in the governance<br />
structure through membership of and attendance<br />
at Board sub-committees, including the Patient<br />
Experience and Participation Committee, the<br />
Learning Disabilities Project group and the<br />
Diversity and Inclusion Steering Group. The<br />
Organ Donation Committee is chaired by a public<br />
governor, Mr Ian-Evans Fisher, with support from<br />
the Senior Independent Director.<br />
In 2012/13 the Council of Governors agreed to<br />
establish a Governors Scrutiny Committee, to<br />
provide a forum to support the Council to meet its<br />
new obligations under the Health and Social Care<br />
Act 2012, in particular, to hold the Non-Executive<br />
Directors to account.<br />
Board of Directors<br />
The Board of Directors is made up of the<br />
Chairman, six Non-Executive Directors and six<br />
Executive Directors, including the Chief Executive<br />
Officer, with the Non-Executive members having<br />
the voting majority.<br />
Senior Independent Director/Deputy Chairman<br />
Mr Keith Lester was appointed Senior Independent<br />
Director in October 2008. When he was appointed<br />
Interim Chairman in July 2012, Judith Green,<br />
another Non-Executive Director was appointed<br />
Senior Independent Director. The principal<br />
responsibilities of the role include:<br />
l Representing to the Board any stakeholders’<br />
concerns when all other communication<br />
channels have been exhausted or are<br />
considered inappropriate<br />
l Acting as a point of contact for Governors to<br />
raise concerns which have not been resolved or<br />
addressed by the Chief Executive Officer or<br />
other Executive Directors<br />
l Being available to the Governors through<br />
periodic attendance at the Council of Governors<br />
meetings.<br />
The role of Deputy Chair is shared between Judith<br />
Green and Colin Horwath as follows:<br />
l Judith Green, Deputy Chair, Engagement<br />
& Participation: Deputy Chair of the Council of<br />
Governors<br />
l Colin Horwath, Deputy Chair, Strategy &<br />
Partnerships: Deputy Chair of the Board of<br />
Directors.<br />
Meetings of the Board of Directors<br />
The Board of Directors met a total 11 times in<br />
2012/13. Individual attendance at those meetings<br />
is set out on the next page.<br />
Relationship between the Council of Governors<br />
and the Board of Directors<br />
Governors’ views are shared with the Board of<br />
Directors through the formal meetings of the<br />
Council, which is chaired by the Chairman,<br />
who presides over the Board of Directors. The<br />
Executive and Non-Executive Directors are invited<br />
to attend the meetings to present reports and<br />
information.<br />
In addition, the Council of Governors and the<br />
Board of Directors hold two joint meetings a<br />
year where the Governors contribute to the<br />
development of the<br />
Trust’s strategic<br />
direction and<br />
vision.<br />
All the Non-Executive Directors of the Board are<br />
considered to be independent.<br />
The Trust also has non-voting Directors who attend<br />
the Board for the relevant agenda item to provide<br />
operational advice and support.<br />
<strong>Day</strong>-to-day management of the Trust is delegated<br />
to the Chief Executive Officer. The Chief Executive<br />
Officer, the Chief Officers, Directors and Clinical<br />
Directors are responsible for the effective delivery<br />
of the strategy and annual plan. They are also<br />
responsible for the operational management of the<br />
organisation.<br />
The appointment, length of appointment and<br />
removal of Non-Executive Directors is agreed by<br />
the Nominations Committee and approved by the<br />
Council of Governors.<br />
Mrs Joanna Davis was reappointed Chairman<br />
of the Trust for a further term of three years<br />
from 1 February 2011. This reappointment was<br />
recommended by the Nominations Committee<br />
and approved by the Council of Governors on 5<br />
January 2011. In April 2012 Joanna Davis was<br />
diagnosed with an illness that would require an<br />
extended period of absence. Keith Lester, the<br />
Deputy Chairman took the role of Chairman on an<br />
acting basis until the Council of Governors formally<br />
appointed Mr Lester as Interim Chairman on 3 July<br />
2012.
BACK TO CONTENTS PAGE<br />
Table 16: Board Meeting Attendance 2012/13<br />
Non Executive Directors<br />
Name Role Appointment/ Board<br />
Reappointment Date Attendance<br />
From<br />
Mr Keith Lester Interim Chairman July 2012 Feb 2015 11/11<br />
Mrs Judith Green Deputy Chair, Engagement & Participation July 2012 Feb 2014 10/11<br />
Mr Colin Horwath Deputy Chair, Strategy & Partnerships May 2010 May 2014 10/11<br />
Prof. Jon Glasby Non Executive Director June 2011 June 2013 10/11<br />
To<br />
Background of Board Members<br />
Mr Keith Lester<br />
Interim Chairman<br />
Appointed:<br />
Experience:<br />
Qualifications: ACIB<br />
February 2007 - reappointed for a further three<br />
year term in February 2010, and for a further<br />
two year term in February 2013 (Interim<br />
Chairman from July 2012)<br />
Previously Regional Director for Lloyds TSB<br />
Corporate and Commercial Banking: Mid<br />
Corporate Business Advisory Consultant<br />
Mr Zubair Khan Non Executive Director June 2011 Dec 2012 7/8<br />
Mrs Elaine Simpson Non Executive Director Feb 2013 Feb 2014 9/11<br />
Mr Roger Peace Non Executive Director July 2012 July 2013 8/8<br />
Executive Directors<br />
Name Role Appointment Date Board<br />
Attendance<br />
From<br />
Ms Sarah Jane Marsh Chief Executive Officer June 2009 Present 6/6<br />
(maternity leave from November 2012) (substantive)<br />
Mr David Melbourne Chief Finance Officer/ Nov 2009 Present 10/11<br />
Interim Chief Executive<br />
Dr Vin Diwakar Chief Medical Officer Aug 2009 Present 10/11<br />
Mrs Michelle McLoughlin Chief Nursing Officer Aug 2007 Present 11/11<br />
To<br />
Mrs Judith Green<br />
Deputy Chairman, Engagement & Participation/<br />
Senior Independent Director<br />
Appointed:<br />
February 2007- reappointed for a further three<br />
year term in February 2010, and for a further<br />
one year term in February 2013 (Deputy<br />
Chairman/Senior Independent Director from July<br />
2012)<br />
Experience: A family lawyer and a children’s advocate for 21<br />
years. Former Member of the Law Society<br />
Family and Children’s Panels. 12 years<br />
experience in post- graduate education<br />
administration and a governor of three King<br />
Edward Foundation Schools. Currently Vice-<br />
Chair of King Edward VI Camp Hill Boys School<br />
and main Foundation Governor since 1994.<br />
Mr David Eltringham Chief Operating Officer Nov 2009 Sept 2012 3/4<br />
Mrs Theresa Nelson<br />
Chief Officer for Workforce<br />
Development Sept 2011 Present 11/11<br />
Mr Tim Atack Chief Operating Officer Sept 2012 Present 6/7<br />
Qualifications: BA Hons English; Solicitor<br />
Mr Colin Horwath<br />
Deputy Chairman, Strategy & Partnerships<br />
Mr Phil Foster Interim Chief Finance Officer Nov 2012 June 2012 5/5<br />
Balance, Completeness and Appropriateness<br />
of the Board<br />
The Executive Directors and Non-Executive<br />
Directors of the Board provide a balance and<br />
breadth of knowledge, experience and skills.<br />
The Executive Directors have at a senior level<br />
considerable NHS experience in a range of<br />
areas including medicine, nursing, strategic and<br />
operational planning, research and workforce<br />
development. Their expertise is complemented<br />
by the Non-Executive Directors who have<br />
extensive experience in commerce, banking,<br />
accounting, audit, research, family law, education,<br />
marketing, social care, education and community<br />
relations. The Nominations Committee and the<br />
Remuneration Committee consider the balance<br />
and breadth of knowledge, experience and skills<br />
required on the Board at each appointment and<br />
reappointment of directors.<br />
Appointed:<br />
Experience:<br />
74 75<br />
May 2008 - reappointed for a further three year<br />
term May 2011 (Deputy Chairman from July<br />
2012)<br />
Audit Partner, KPMG, with responsibility to<br />
develop public sector audit practice in the<br />
Midlands.<br />
Qualifications: BSc, CIPFA, ACA, PIIA.
BACK TO CONTENTS PAGE<br />
Professor Jon Glasby<br />
Non Executive Director<br />
Mr Roger Peace<br />
Non Executive Director<br />
Appointed:<br />
Experience:<br />
Qualifications:<br />
June 2010; reappointed for a further two year<br />
term June 2011<br />
Professor of Health and Social Care and<br />
Director of the Health Services Management<br />
Centre, University of <strong>Birmingham</strong>. Qualified<br />
social worker.<br />
BA Hons (history), MA/DipSW (social work),<br />
PhD (social policy), PG Cert (teaching and<br />
learning in higher Education)<br />
Appointed:<br />
Experience:<br />
Qualifications:<br />
July 2012 for a one year term<br />
A Chartered Accountant, currently Chief<br />
Financial Officer of learndirect Ltd, the online<br />
training business. Previously held various board<br />
positions with Severn Trent Plc including CFO of<br />
the US division during the 1990s and<br />
subsequently UK divisional Managing Director<br />
BA(Hons) Economics, MBA, FCA<br />
Mr Zubair Khan<br />
Non Executive Director<br />
Appointed: June 2011- term ended December 2012<br />
Ms Sarah-Jane Marsh<br />
Chief Executive Officer<br />
Appointed: June 2009<br />
Experience:<br />
Qualifications:<br />
Forensic Scene Manager with West Midlands<br />
Police; Accredited ACAS Mediator, Chair of<br />
Nelson Mandela Primary school Governing<br />
Body, former member of the General Teaching<br />
Council and Heart of England Magistrates<br />
Advisory Committee.<br />
BA Hons English; Solicitor<br />
Experience:<br />
Joined the NHS via the Graduate Management<br />
Scheme, holding various roles in Primary and<br />
Secondary Care and at the Department of<br />
Health. Previously Director of Planning and<br />
Productivity at Walsall <strong>Hospital</strong>s NHS Trust.<br />
Appointed Chief Operating Officer at BCH in<br />
December 2007, and Chief Executive Officer in<br />
June 2009.<br />
Qualifications:<br />
BA (Hons), History, MA, Russian and Eastern<br />
European Studies, MSc, Health Care<br />
Management<br />
Mrs Elaine Simpson<br />
Non-Executive Director<br />
Appointed:<br />
February 2012 - re-appointed for a further one<br />
year term February 2013<br />
Mr David Melbourne<br />
Chief Finance Officer/Interim Chief Executive (from<br />
November 2012)<br />
Experience:<br />
Qualifications:<br />
25 years experience in Local Government<br />
working in senior roles across a number of<br />
North-West local education authorities. For five<br />
of those years working in Sefton as the Chief<br />
Education Officer. From 2002-2012 employed by<br />
Serco initially as Managing Director and<br />
subsequently as Global Director of Education<br />
and Children’s Services. Member of the<br />
Association of Directors of Children’s Services.<br />
BSc (Hons) Mathematics, Post-Graduate<br />
Diploma in Guidance and Counselling;<br />
Post-Graduate Management Qualification<br />
Appointed: November 2009<br />
Experience:<br />
Qualifications:<br />
Previously a senior management consultant<br />
at KPMG; various Director of Finance roles in<br />
the NHS in Derbyshire and Lincolnshire from<br />
2001 until 2005. Previously Director of<br />
Resources & Deputy Chief Executive at Heart of<br />
<strong>Birmingham</strong> Teaching PCT.<br />
BA (Hons) Economics & History, MBA, CPFA,<br />
ACA<br />
76 77
BACK TO CONTENTS PAGE<br />
Dr Vinod Diwakar<br />
Chief Medical Officer<br />
Mrs Theresa Nelson<br />
Chief Officer for Workforce Development<br />
Appointed: August 2009<br />
Experience:<br />
Qualifications:<br />
Chair of the Acute Care Theme, Children and Young<br />
People’s Outcomes Forum; Member of the DH<br />
Future Forum Expert Working Group on the NHS<br />
Constitution; Consultant Paediatrician since 2002,<br />
Undergraduate Clinical Sub Dean 2002-05,<br />
Postgraduate Clinical Tutor 2002-07, Associate<br />
Director for the NHS Clinical Governance Support<br />
Team 2002-04, Associate Postgraduate Dean at NHS<br />
West Midlands Workforce Deanery 2005-07, Member of<br />
the Expert Working Group on Ambulatory Care for the Ill<br />
Child Module of the National Service Framework on<br />
Children and Young People 2003-04. Appointed Interim<br />
Director of Strategy at <strong>Birmingham</strong> Children’s <strong>Hospital</strong> in<br />
March 2009, and Chief Medical Officer in September<br />
2009.<br />
MBBS, MRCP (UK), FRCPCH, MMedEd, FHEA<br />
Mr Tim Atack<br />
Chief Operating Officer<br />
Appointed: September 2012<br />
Appointed:<br />
Experience:<br />
Qualifications:<br />
Appointed June 2011 as Director of Workforce.<br />
Appointed September 2011 as Chief Officer<br />
for Workforce Development<br />
Previous roles include Director of Human Resources<br />
at Good Hope <strong>Hospital</strong>; Deputy Director of Human<br />
Resources & Head of Organisational Development<br />
at Heart of England Foundation Trust and National<br />
Lead for Clinical Leadership for the Department of<br />
Health. Prior to 2003 roles included senior<br />
commercial, financial and HR roles with Marks and<br />
Spencer PLC.<br />
FCIPD; NLP Practitioner and Executive Coach<br />
Mrs Michelle McLoughlin<br />
Chief Nursing Officer<br />
Appointed: August 2007<br />
Experience:<br />
Over 10 years NHS Board experience. Previously Chief<br />
Operating Officer at Sandwell & West <strong>Birmingham</strong><br />
<strong>Hospital</strong>s NHS Trust and at University <strong>Hospital</strong>s NHS<br />
Trust. Appointed Director of ICT & Performance at BCH in<br />
2010.<br />
Experience:<br />
A career with experience in acute hospitals and the<br />
community in a variety of nursing and management<br />
roles. Previous clinical roles across many paediatric<br />
specialities in district general hospitals and teaching<br />
hospitals. Clinical experience at ward sister and<br />
clinical nurse specialist level. Previous clinical roles<br />
in the community caring for adults, frail elderly,<br />
children and young people. Previous role as Deputy<br />
Director of Nursing.<br />
Qualifications:<br />
BSC (Hons) Mathematics with Computing<br />
Mr Phil Foster<br />
Interim Chief Finance Officer<br />
Qualifications:<br />
MSc, RGN, RSCN, DN<br />
Appointed: November 2012 - June 2013<br />
Mr David Eltringham<br />
Chief Operating Officer<br />
Appointed: November 2009 – September 2012<br />
Experience:<br />
Qualifications:<br />
Joined the NHS after working within private accounting<br />
practice. In over 24 years within the NHS has worked in<br />
various senior roles within acute (district general and<br />
specialist hospitals) and mental health services.<br />
CPFA<br />
Experience:<br />
Qualifications:<br />
Previously worked in a number of nursing roles at<br />
University <strong>Hospital</strong>s <strong>Birmingham</strong> and Alexandra <strong>Hospital</strong> in<br />
Redditch; 2 years working in the private healthcare sector;<br />
Education and Professional Developmen Manager and<br />
subsequently Clinical Lead for NHS Direct (<strong>Birmingham</strong><br />
the Black Country and Solihull). Came to <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong> in 2004 to manage the Medical<br />
Directorate; appointed Assistant Director for CAMHS in<br />
2007. Appointed Interim Chief Operating Officer March<br />
2009 and appointed to the substantive role in November<br />
2009.<br />
MBA, BAEd (Hons); Registered Nurse (Adult);<br />
Diploma in Nursing Science, DNSc<br />
Evaluation of the Board of Directors<br />
The Board of Directors has continuously reviewed<br />
its compliance with the Code of Governance<br />
and has identified one area where it has chosen<br />
to follow a different approach to that set out by<br />
Monitor. This relates to the recommendation<br />
that Executive Directors should be subject to<br />
review and reappointment at regular intervals<br />
78 79<br />
of no more than five years. We have chosen to<br />
maintain our existing management and contractual<br />
arrangements for Executive Directors.<br />
Directors and Governors are required on an annual<br />
basis to give a clear pledge to the code of conduct<br />
and accountability, which encompasses the Nolan<br />
principles and Code of Governance.
BACK TO CONTENTS PAGE<br />
Performance of the Board of Directors, its<br />
committees and individual Directors has been<br />
evaluated in accordance with the Code of<br />
Governance. This included:<br />
l Annual appraisal and Performance<br />
Development Review for each Executive<br />
Director by the Chief Executive (reviewed sixmonthly)<br />
l Annual appraisal and Performance<br />
Development Review of Chief Executive by<br />
the Chairman (reviewed six-monthly)<br />
l Discussion of performance of Executive<br />
Directors at Appointments and Remuneration<br />
Committee<br />
l Annual performance and development<br />
reviews of each Non-Executive Director by the<br />
Chairman<br />
l Discussion of performance of Non-<br />
Executive Directors (including the Chairman)<br />
at the Nominations Committee<br />
l Independent Governance Review by Capsticks<br />
and Good Governance Institute Alliance<br />
– a review of the governance structures and<br />
information flows to the Board. This resulted in<br />
the implementation of a new structure for<br />
2012/13 and redesigned reporting to the Board<br />
l Annual Review of each Board committee<br />
l Internal Audit of quality governance<br />
arrangements.<br />
Declarations of Interests<br />
All members of the Board of Directors are required<br />
to make known at each meeting any interest.<br />
This information is also recorded in the Register<br />
of Interests. The Board is satisfied the Directors<br />
hold no material interests in organisations where<br />
those organisations or related parties are likely<br />
to do business, or are possibly seeking to do<br />
business, with <strong>Birmingham</strong> Children’s <strong>Hospital</strong><br />
NHS Foundation Trust.<br />
The Register of Interests of the Board of Directors<br />
is held by the Company Secretary and can be<br />
accessed by contacting:<br />
The Company Secretary<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust<br />
Steelhouse Lane<br />
<strong>Birmingham</strong><br />
B4 6NH<br />
Audit Committee<br />
The Audit Committee provides an objective review<br />
of our systems and processes for governance,<br />
internal controls and risk management. In addition<br />
the Audit Committee is responsible for:<br />
l Making recommendations to the Council of<br />
Governors on the appointment of the external<br />
auditors, reviewing and agreeing the external<br />
audit plan, receiving external audit reports,<br />
letters and management responses<br />
l Making recommendations to the Board of<br />
Directors on the appointment of the internal<br />
auditors; approving the internal audit strategy<br />
and work plan<br />
l Monitoring and assessing the work of the<br />
auditors, ensuring that they maintain<br />
independence, objectivity and effectiveness<br />
l Reviewing the Annual Report and financial<br />
statements before they are submitted to the<br />
Board of Directors.<br />
The Audit Committee is chaired by Mr Colin<br />
Horwath, a Non-Executive Director. The<br />
membership includes two other Non-Executive<br />
Directors, supported by an independent advisory<br />
member. The meetings are regularly attended<br />
at the invitation of the Chair by the Interim Chief<br />
Finance Officer, the Company Secretary, the<br />
Internal Auditor and the External Auditor.<br />
The Audit Committee has met on six occasions<br />
during the year to carry out its duties. The 2012/13<br />
Annual Programme of the Committee had a<br />
thematic approach to the assurance process<br />
and to meet the requirements of the DH Audit<br />
Committee checklist (designed to assess the<br />
effectiveness of the Committee) and addressed the<br />
following key themes:<br />
a. Value for money and workforce;<br />
b. Quality, patient safety and patient experience;<br />
c. Financial standing;<br />
d. Assurance mechanisms in the Trust;<br />
e. Effectiveness of the Audit Committee;<br />
f. Review of year-end statements;<br />
g. Annual Accounts and Quality Report.<br />
The Committee also:<br />
l Received and considered reports on the work<br />
of the Local Counter Fraud Specialist<br />
l Reviewed and approved draft Annual Accounts,<br />
Annual Governance Statement and the Annual<br />
Report prior to adoption by the Board<br />
l Reviewed the format of and processes in<br />
relation to the Board Assurance Framework,<br />
aligning the thematic review of each Committee<br />
to its content<br />
l Received and considered reports from<br />
the internal and external auditors and in<br />
particular focused on the implementation of the<br />
recommendations arising from these reports.<br />
Where the External Auditor provides non-audit<br />
services, these are overseen by the Audit<br />
Committee. The Audit Committee is assured<br />
that the External Auditor’s internal controls and<br />
appropriate challenge by the Committee ensure<br />
that auditor objectivity and independence is<br />
safeguarded.<br />
Table 17: Audit Committee Attendance 2012/13<br />
Members Apr 201 May 2012 Oct 2012 Dec 2012 Feb 2013 Total<br />
Colin Horwath, 4 4 4 4 4 5/5<br />
Chairman<br />
Judith Green, 4 4 4 4 4 5/5<br />
Non Executive Director<br />
Elaine Simpson, 4 4 4 4 x 4/5<br />
Non-Executive Director<br />
Roger Peace, 4 4 n/a n/a n/a 2/2<br />
Advisory Member*<br />
Maxine Penlington, n/a n/a 4 4 4 3/3<br />
Advisory Member**<br />
* Roger Peace became a Non-Executive Director in July 2012 and ceased membership of the Audit Committee.<br />
** Maxine Penlington became an Advisory Member of the Committee in October 2012.<br />
80 81
82 83<br />
BACK TO CONTENTS PAGE<br />
Nominations Committee<br />
The Nominations Committee is a committee of<br />
the Council of Governors. The Committee is<br />
responsible for the identification and nomination of<br />
non-executive directors (including the Chairman),<br />
giving consideration to succession planning and<br />
the balance of skills, expertise and experience<br />
required on the Board of Directors.<br />
The Committee also oversees the terms and<br />
conditions of employment and remuneration of all<br />
Non-Executive Directors for the approval of the<br />
Council of Governors.<br />
During 2012/13 the Nominations Committee made<br />
the following decisions, which were recommended<br />
to and accepted by the Council of Governors:<br />
1. Keith Lester is appointed Interim Chairman<br />
2. Keith Lester is reappointed for a two year term<br />
from February 2013.<br />
3. Judy Green is reappointed for a one year term<br />
as non-executive director from February 2013.<br />
4. Elaine Simpson is reappointed for a one year<br />
term from February 2013.<br />
5. Roger Peace is appointed Non-Executive<br />
Director for a one year term from July 2012.<br />
Table 18: Nominations Committee attendance 2012/13<br />
Foundation Trust Membership<br />
Eligibility Criteria<br />
Membership of <strong>Birmingham</strong> Children’s <strong>Hospital</strong><br />
NHS Foundation Trust is open to:<br />
l Any person who is or has been a patient/<br />
service user of <strong>Birmingham</strong> Children’s <strong>Hospital</strong><br />
in the last five years<br />
l Any person who is or has been a parent/carer<br />
of a patient/service user of <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong> in the last five years<br />
l All permanent staff members<br />
l Any member of the public aged 10 or over who<br />
lives in one of the following constituencies:<br />
<strong>Birmingham</strong><br />
Sandwell<br />
Solihull<br />
Walsall, Wolverhampton and Dudley<br />
Staffordshire and Shropshire<br />
Coventry and Warwickshire<br />
Herefordshire and Worcestershire<br />
Nominations Committee – Members’ attendance 2012/13<br />
July Nov<br />
Members 2012 2012 Total<br />
Mr Keith Lester, Interim Chairman 4 4 2/2<br />
Mr Philip Crombie, Lead Governor: Public – <strong>Birmingham</strong> 4 4 2/2<br />
Mr Brian Stokes, Governor: Public – Dudley / Walsall / Wolverhampton 4 4 2/2<br />
Mr Stuart Brand, Governor: Partner – <strong>Birmingham</strong> City University 4 n/a 1/1<br />
Mr Tim Edwards, Governor: Public – Staffordshire / Shropshire 4 4 2/2<br />
Mr Ian Evans-Fisher, Governor: Public – Herefordshire / Worcestershire 4 4 2/2<br />
Ms Hilary Brown, Governor: University of <strong>Birmingham</strong> 4 4 2/2<br />
Membership Numbers<br />
The Trust set and achieved a target of 10,000<br />
members by 2010/11 and aimed to sustain this<br />
level for 2012/13. The number of members in each<br />
constituency in March 2012 and March 2013 is<br />
shown below.<br />
Table 19: Membership Growth in 2012/13<br />
Constituency Members 31 March 2012 Members 31 March 2013<br />
Total Public Members 3,947 3,956<br />
Total Patient/Carer Members 4,516 4,524<br />
Total Staff Members 2,913 3,027<br />
GRAND TOTAL 11,376 11,507<br />
Membership Strategy<br />
We met our membership target of 10,000 members<br />
in 2010/11. We maintained a total membership of<br />
over 11,000 members during 2012/13 and aim to<br />
continue to maintain this level during 2013/14 by:<br />
l Focussing membership communication through<br />
the Trust’s new website, including an online<br />
membership application form and the<br />
development of a members area<br />
l Encouraging young people to join the Young<br />
Person’s Advisory Group (YPAG) and thereby<br />
becoming Foundation Trust members if they are<br />
not already<br />
l Demonstrating achievements of members,<br />
such as YPAG, to encourage new members to<br />
join<br />
l Supporting Governors to communicate with<br />
members and the public<br />
l Publicising ways for members to get involved,<br />
including:<br />
Consultations<br />
Council of Governors meetings<br />
Public Board meetings<br />
Celebrations<br />
Events<br />
Annual General Meeting<br />
Members can communicate with Governors by<br />
contacting the Chairman’s Office:<br />
0121 333 8533<br />
foundation-trust.office@bch.nhs.uk<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong><br />
NHS Foundation Trust<br />
Steelhouse Lane<br />
<strong>Birmingham</strong><br />
B4 6NH<br />
Details of how to contact some of the Governors<br />
by direct email can also be found on the Council of<br />
Governors page on the Trust website:<br />
www.bch.nhs.uk.<br />
l Encouraging members to communicate with<br />
Governors through the Trust website.
Regulatory Ratings<br />
Staff Survey Report<br />
BACK TO CONTENTS PAGE<br />
Table 20: Regulatory Ratings 2011/12<br />
2011/12<br />
Rating Annual Plan Quarter 1 Quarter 2 Quarter 3 Quarter 4<br />
2011/12<br />
Finance risk rating 4 4 4 4 4<br />
Governance risk rating Green Green Green Green Green<br />
Mandatory Services risk rating Green Green Green Green Green<br />
Safety Assurance System in place n/a Green Green Green Green<br />
risk rating (new for 2011/12)<br />
Approach to Staff Engagement<br />
Our staff are the most important part of our<br />
hospital. We cannot deliver excellence for<br />
children and young people unless we have<br />
excellent staff.<br />
Part of our commitment to our staff is to have<br />
excellent communication, excellent engagement<br />
and always be open to listening to new and<br />
innovative ideas.<br />
Table 22: Staff Survey Improvement Plan & Outcome 2011<br />
Our People Strategy - launched in June 2012 - sets<br />
out how we intend to focus on genuine engagement<br />
with our staff to develop their support for radical<br />
service redesign and continued improvements in<br />
organisational performance.<br />
An important element of this is the national staff<br />
survey which our staff take part in every year.<br />
We identified a number of themes for improvement<br />
in the 2011 Staff Survey and made a commitment to<br />
take the following action.<br />
Theme What we said What we did<br />
w Embed the Leading Change framework for<br />
genuine consultation<br />
w Embedded the revised Performance Appraisal<br />
process and provided re-training for managers<br />
Table 21: Regulatory Ratings 2012/13<br />
2012/13<br />
Staff<br />
Involvement<br />
w Embed the revised appraisal process and<br />
provide re-training for managers<br />
w Involve staff in influencing decisions through<br />
the values work<br />
w Enhanced consultation and communication<br />
around organisational change<br />
w Successfully launched and embedded the<br />
Trust values<br />
w Developed new ways to listen to our staff<br />
Rating Annual Plan Quarter 1 Quarter 2 Quarter 3 Quarter 4<br />
2012/13 (predicted)<br />
Finance risk rating 4 4 4 4 4<br />
Governance risk rating Green Green Green Green Green<br />
Mandatory Services risk rating Green Green Green Green Green<br />
Safety Assurance System in place Green Green Green Green Green<br />
risk rating (new for 2011/12)<br />
Health and<br />
Wellbeing<br />
at Work<br />
w Design and implement a health and wellbeing<br />
at work strategy which integrates with the<br />
public health agenda<br />
w Review areas where we know work pressures<br />
are significant and support the implementation<br />
of actions to address this<br />
w Develop a coordinated staff support strategy<br />
enhancing internal and external partnerships<br />
w Identify initiatives to support health and<br />
wellbeing at work<br />
w Reviewed those areas where we know work<br />
pressures are significant, and supported the<br />
implementation of required actions to address<br />
this.<br />
w Identified from staff local interventions /<br />
initiatives which could be offered by the Trust<br />
to support health and wellbeing at work.<br />
w Introduced work-based stress risk<br />
assessments<br />
Explanation of the risk ratings<br />
Monitor uses the risk rating as a guide to the<br />
intensity of scrutiny under which we operate. At<br />
the end of each annual assessment and quarterly<br />
review, each foundation trust receives risk ratings<br />
and a summary of key issues to be followed up by<br />
the Board or Monitor.<br />
The Financial and Governance risk ratings are<br />
primarily based on a defined set of indicators.<br />
Monitor also uses other sources of information to<br />
confirm or challenge this assessment.<br />
The Safety Assurance System in place risk rating<br />
was introduced by Monitor in 2011/12 and is a self<br />
assessment by the Trust. Monitor uses a range of<br />
information sources to assess this response.<br />
Mandatory Services relates to a range of services<br />
that the Trust is required to provide, which were set<br />
as part of its authorisation process. Any significant<br />
reduction or ceasing of these services could impact<br />
on this rating.<br />
Summary of <strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS<br />
Foundation Trust’s performance in 2012/13<br />
The Trust planned to be green across all the<br />
ratings for the year. It has self assessed as being<br />
green rated across all the risk ratings for each<br />
quarter, and this has been confirmed by Monitor for<br />
Quarter 1, Quarter 2 and Quarter 3. Monitor is due<br />
to report in June our Quarter 4 assessment and we<br />
expect this to confirm our self assessment.<br />
All of the Governance performance metrics were<br />
met for each quarter.<br />
Recognising<br />
and<br />
Rewarding<br />
Staff<br />
Culture<br />
and<br />
Working<br />
Environment<br />
w Introduce work based stress risk assessments<br />
w Develop a culture where managers deliver<br />
effective praise and recognition to staff<br />
supported with the launch of Trust values and<br />
the appraisal system<br />
w Increase opportunities for local and Trust wide<br />
recognition<br />
w Review loyalty and long service reward<br />
scheme<br />
w Encourage managers and clinical leaders to<br />
understand the local position<br />
w Work with staff through the values workshops<br />
to create the environment that enhances their<br />
experience at work<br />
w Develop robust methods of reviewing exit data<br />
and put in place mitigating actions<br />
84 85<br />
w Promoted a culture where managers recognise<br />
staff supported by the launch of Trust values<br />
and the appraisal system.<br />
w Increased opportunities for local and Trustwide<br />
recognition via Star of the Month.<br />
w Reviewed loyalty and long service award<br />
scheme.<br />
w Encouraged managers and clinical leaders to<br />
understand the local position<br />
w Worked with staff through the Trust values<br />
workshops to create an environment to<br />
enhance their experience at work<br />
w Developed the staff poll to more regularly test<br />
how staff feel.
BACK TO CONTENTS PAGE<br />
Throughout 2012/13 we have also continued to engage with staff as described at pages 53/54.<br />
Summary of 2012/13 performance<br />
N.B. national average is the average of specialist acute trusts, not all trusts.<br />
Table 23: Staff Survey 2012 – Response Rate<br />
Response Rate<br />
Table 24: Staff Survey 2012 – most improved scores<br />
Most Improved<br />
Where we improved the most compared to 2011<br />
2012 2012 2011 Variance<br />
national Results Results 2011-2012<br />
average<br />
52% 46% 50% - 4%<br />
2012 2012 2011 Variance<br />
national Results Results 2011-2012<br />
average<br />
KF7. Percentage of staff appraised in the last 12 months. 75% 86% 75% + 11%<br />
Action Plans for Improvement and future priorities<br />
and targets<br />
We have identified further themes for improvement<br />
from the 2012 Staff Survey and plan to take the<br />
actions described below.<br />
Table 27: Staff Survey Improvement Plan 2012<br />
Theme<br />
Staff<br />
engagement<br />
& satisfaction<br />
What we will do<br />
w Hold monthly staff forums with Chief Executive and Chief Officers.<br />
w Executive Team will regularly visit areas of the Trust.<br />
w Continue to publicise and embrace ‘star of the month’, publicly recognising employee<br />
contributions.<br />
w Undertake bi-monthly staff polls on the intranet to understand the mood of staff better.<br />
KF23. Staff job satisfaction. 3.45 3.57 3.45 + 0.12<br />
Table 25: Staff Survey 2012 – highest ranking scores<br />
Highest Ranking<br />
Where we ranked the highest against other<br />
acute specialist trusts in England<br />
2012 2012 2011 Variance<br />
national Results Results 2011-2012<br />
average<br />
KF7. Percentage of staff appraised in last 12 months. 83% 86% 75% + 11%<br />
KF8. Percentage of staff having well structured<br />
appraisals within the last 12 months. 36% 39% 34% + 5%<br />
KF14. Percentage of staff reporting errors, near misses<br />
or incidents witnessed in the last 12 months. 92% 92% 93% + 1%<br />
KF17. Percentage of staff experiencing physical<br />
violence from staff in the last 12 months. 2% 1% 0 + 1%<br />
KF18. Percentage of staff experiencing harassment,<br />
bullying or abuse from patients, relative or the public<br />
in the last 12 months. 21% 19% n/a -<br />
Table 26: Staff Survey 2012 – lowest ranking scores<br />
Lowest Ranking<br />
Where we compared least favourably against other<br />
acuter specialist trusts in England<br />
2012 2012 2011 Variance<br />
national Results Results 2011-2012<br />
average<br />
KF3. Work pressure felt by staff. 2.88 3.05 n/a -<br />
KF10. Percentage of staff receiving health and safety<br />
training in the last 12 months. 76% 65% 83% -18%<br />
KF11. Percentage of staff suffering work related stress<br />
in the last 12 months. 32% 43% 29% -14 %<br />
KF20. Percentage of staff feeling pressure in last<br />
3 months to attend work when feeling unwell. 23% 30% 22% -8%<br />
Health,<br />
wellbeing &<br />
safety<br />
Clear roles,<br />
responsibilities<br />
and<br />
rewarding<br />
jobs<br />
Equality &<br />
diversity<br />
Personal<br />
development,<br />
training &<br />
support<br />
w Re-engage the Health and Wellbeing Steering Group.<br />
w Extend BCH offer of health and wellbeing resources to staff at work.<br />
w Help line managers to understand staff stresses and anxieties and manage them appropriately.<br />
w Continue signposting staff support and occupational health services and use staff and patient<br />
feedback to improve services.<br />
w Ensure that patient satisfaction scores are discussed and action plans are formulated to<br />
address any key themes emerging.<br />
w Encourage ongoing, meaningful dialogue between line managers and staff so teams are<br />
aware of activity levels Trust-wide.<br />
w Establish Diversity & Inclusion Steering Group.<br />
w 2012/13 Diversity and Inclusion Plan to be shared with staff and patients.<br />
w Provide personal support to Directorate Management Teams to understand specific personal<br />
development and training needs.<br />
w Continue to promote the Career Advisory service.<br />
w Continue to utilise the revised appraisal process, training managers in using it to its full<br />
potential thereby providing clarity about individuals’ roles and training needs.<br />
w Robustly monitor training statistics at Directorate monthly and quarterly performance reviews<br />
to target improvement drives and share best practice.<br />
KF25. Staff motivation at work. 3.88 3.72 3.77 -0.05<br />
86 87
Sustainability Report<br />
Introduction and Commitment<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust is committed to reducing its impact on the<br />
environment.<br />
We recognise our environmental obligations and<br />
are committed to delivering carbon savings during<br />
the next 2 years, to meet a 10% saving against the<br />
2007 baseline by 2015.<br />
Energy Consumption<br />
Our total energy consumption has risen during the<br />
year, from 22,967 to 29,647 MWh. Our relative<br />
energy consumption has changed during the year,<br />
from 0.39 to 0.5 MWh/square metre.<br />
As part of our commitment to reduce carbon<br />
emissions, we installed a Combined Heat and<br />
Power (CHP) plant which has been in operation<br />
since September 2010. The CHP generates most of<br />
BACK TO CONTENTS PAGE<br />
the electricity, hot water and heating required at our<br />
Steelhouse Lane site.<br />
Renewable energy represents 12.6% of our total<br />
energy use. In addition, we generate 57.7% of our<br />
energy on site through the CHP. We have made<br />
arrangements to purchase electricity generated<br />
from renewable sources via the GPS energy<br />
procurement service.<br />
Sustainability underpins all aspects of the<br />
Trust’s service delivery and development and<br />
sits alongside quality of patient experience,<br />
effectiveness of services and safety for patients<br />
and staff as a Trust priority. We are, therefore,<br />
encouraged by the progress made so far in<br />
delivering the sustainability strategy.<br />
We have put plans in place to reduce carbon<br />
emissions and improve our environmental<br />
sustainability. Over the next 10 years we expect to<br />
save £85,000 as a result of these measures.<br />
MWh<br />
Figure 3: Energy Consumption 2008/09 - 2012/13<br />
Energy Consumption<br />
35000.00<br />
30000.00<br />
25000.00<br />
20000.00<br />
15000.00<br />
10000.00<br />
?<br />
Electricity<br />
Other<br />
Renewables<br />
Coal<br />
Figure 2: Expenditure on energy 2008/09-2012/13<br />
£1,800,000<br />
£1,600,000<br />
£1,400,000<br />
£1,200,000<br />
£1,000,000<br />
£800,000<br />
£600,000<br />
£400,000<br />
£200,000<br />
0<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
Expenditure on Energy<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
£<br />
2008/09 2009/10 2010/11 2011/12 2012/13<br />
2008/09 2009/10 2010/11 2011/12 2012/13<br />
Energy costs have increased by 10% in 2012/13 compared to the previous year. Much of this increase<br />
can be attributed to the colder weather over the winter. Water consumption increased by 3,854 cubic meters in 2012/13.<br />
5000.00<br />
0.00<br />
2008/09 2009/10 2010/11 2011/12 2012/13<br />
Figure 4: Water Consumption 2008/09-2012/13<br />
100000<br />
90000<br />
80000<br />
70000<br />
60000<br />
50000<br />
40000<br />
30000<br />
20000<br />
10000<br />
0<br />
88 89<br />
Water consumption in cubic metres<br />
Gas<br />
Oil
BACK TO CONTENTS PAGE<br />
Carbon Emissions<br />
A sustainable, low carbon NHS offers an<br />
opportunity to save money while helping to create<br />
a quality resilient healthcare service. To meet these<br />
challenges we are committed to, and expect to<br />
meet as a minimum, our environmental obligations<br />
to exceed a 10% carbon savings required overall<br />
by the Department of Health by 2015.<br />
Carbon Saving Measures<br />
We have committed resources during 2012/13<br />
to deliver carbon reduction projects and have<br />
identified areas completed and additional areas<br />
for improvement during 2013/14.<br />
Carbon saving projects completed to date<br />
Project area<br />
Objectives<br />
Figure 5: Carbon Emissions 2008/09 - 2012/13<br />
Installation of software which automatically shuts<br />
down PCs when not in use<br />
To reduce the Trust’s electricity demands and<br />
reduce CO2 emissions<br />
12000<br />
Carbon Emissions<br />
Commence programme for installation of variable<br />
speed drives and ensure all new installations are<br />
equipped with VSDs.<br />
To reduce the Trust’s electricity demands and<br />
reduce CO2 emissions<br />
Tonnes CO2e<br />
10000<br />
8000<br />
6000<br />
4000<br />
Project area<br />
Continuation of the replacement of the Ozone<br />
damaging R22 refrigeration plant<br />
Installation of improved roof and plant room<br />
insulation<br />
Carbon saving projects planned or on-going<br />
Objectives<br />
To reduce the risk of detrimental effects on the<br />
environment<br />
To reduce the Trust’s heating demands and<br />
reduce CO2 emissions<br />
2000<br />
0<br />
2008/09 2009/10 2010/11 2011/12 2012/13<br />
Commencement of programme for installation of<br />
intelligent lighting controls<br />
Improved heating and ventilation controls<br />
To reduce the Trust’s electricity demands and<br />
reduce CO2 emissions<br />
To reduce the Trust’s heating demands and<br />
reduce CO2 emissions<br />
(Water &<br />
Waste)<br />
Rail Road Air Gas Electricity<br />
Measured greenhouse gas emissions have increased by 1,047 tonnes this year.<br />
Carbon Reduction Commitment Performance<br />
Our total emissions under the government’s Carbon Reduction<br />
Commitment (CRC) Energy Efficiency Scheme for 2012/13 have<br />
reduced to 5,489 tonnes of CO2 (compared with 5,553 tonnes of CO2<br />
for 2011/12). The carbon allowances required to cover these emissions<br />
for 2012/13 will cost £73,500 (based on the current price of carbon at<br />
£12 per tonne).<br />
Procurement policy<br />
Installation of Smart metering at the main<br />
hospital site<br />
Carry out review and update of current statutory<br />
Display Energy Certificates (DECs)<br />
Introduction / completion of active waste<br />
segregation<br />
Designing new buildings and refurbishments to<br />
be as energy efficient as possible<br />
Moving to paper and bottle free Board meetings<br />
ATOM – Ambulance Taxi Operational<br />
Management<br />
Maple – Electronic Food Ordering<br />
To reduce the risk of detrimental effects on the<br />
environment.<br />
To enable the Trust to accurately measure<br />
energy use to enable management of efficiency<br />
and reduce CO2 emissions<br />
To enable the Trust to accurately report energy<br />
use to enable management of efficiency and<br />
reduce CO2 emissions<br />
To enable the Trust to reduce the impact on land<br />
fill reduce costs’ & reduce the risk of detrimental<br />
effects on the environment<br />
To reduce the risk of detrimental effects on the<br />
environment<br />
To reduce the risk of detrimental effects on the<br />
environment<br />
To reduce the Trust’s heating demands and<br />
reduce CO2 emissions<br />
To reduce the Trust’s heating demands and<br />
reduce CO2 emissions<br />
90 91
SECTION THREE<br />
Our Quality Report<br />
Chief Executive’s Statement on Quality<br />
Our organisation is committed to putting the quality<br />
of care we provide at the centre of everything that<br />
we do. We have ensured that this remains at the<br />
forefront of our agenda by embedding it as the first<br />
of our six strategic objectives.<br />
This commitment is not just about maintaining<br />
the status quo but about continual learning and<br />
improvement. There is no health care organisation<br />
worldwide that can’t in some way improve the<br />
services it provides for its patients and our hospital<br />
is no exception.<br />
During the year our Quality Committee has become<br />
central to this agenda, ensuring that there is a<br />
continual oversight and challenge as to how we<br />
can further improve what we do. This is enhanced<br />
through the work programme of the Board of<br />
Directors - its agenda is structured to focus on<br />
service quality and safety first and foremost. This is<br />
achieved through a range of methods, for example<br />
a detailed quality report is scrutinised, discussed<br />
and debated on a monthly basis. We also use<br />
patient stories and quality walkabouts to ensure<br />
that we look beyond the figures within the report.<br />
We are proud of some of the initiatives and<br />
innovations that have been developed over the past<br />
year to improve quality. We recognise that feedback<br />
from our staff about the services that we provide<br />
and their own experience of working at the Trust<br />
is invaluable in the quality agenda. For example,<br />
we have developed tools to support junior doctors<br />
(Training Advice & Liaison Service) and to capture<br />
their experience of training at the hospital.<br />
Recognising the hard work and commitment of<br />
staff as our most valuable asset is important to the<br />
Trust. We launched a monthly ‘Star of the Month’<br />
award during the last year and some of the stories<br />
of staff working in a diverse range of roles are truly<br />
inspirational. Each year we celebrate the work<br />
of our staff with an annual awards event saying<br />
thank you for their contribution over the past twelve<br />
months.<br />
We have also used technology to improve the<br />
quality of the patient experience. Our App for<br />
Smart Phones allows us to capture the experience<br />
of our patients and their families in real time and<br />
quickly address any issues. All these responses<br />
are captured live on our public website increasing<br />
transparency of the whole process.<br />
We are rightly upheld at a local, regional and<br />
national level for the work that we do on patient<br />
experience. We are proud of the various ways in<br />
which we engage with children and young people<br />
to address how we can improve our services. Our<br />
Young Persons Advisory Group (YPAG) has been<br />
visited most recently by Dr Hilary Cass, president of<br />
the Royal College of Paediatrics and Child Health,<br />
and had input into a range of service areas and<br />
initiatives. For example, the group helped design<br />
a new Dignity Giving Suit to replace the traditional<br />
backless robes used in hospitals.<br />
To the best of my knowledge the information<br />
contained in this Quality Account is accurate.<br />
………………………………………………<br />
David Melbourne, Interim Chief Executive<br />
Priorities for Improvement<br />
At <strong>Birmingham</strong> Children’s <strong>Hospital</strong>, ensuring that we<br />
provide a high quality service is central to everything<br />
we do and this is embedded within our strategy.<br />
We are always looking for ways that we can improve<br />
the quality of our services. This can include making<br />
the experience better for the patients and families<br />
that use our services; changing the way we work so<br />
we can treat every patient that needs or chooses<br />
to come to BCH without any delays; making<br />
things safer than ever before and improving health<br />
outcomes for the diverse range of children and<br />
young people that we see every day.<br />
It is important that we focus our resources on making<br />
improvements where they are needed most, so we<br />
continually monitor and analyse a wide range of<br />
information that tells us where we could do better.<br />
This includes:<br />
l Listening to the children, young people and<br />
families that use our services. There are lots of<br />
ways they can tell us what they think, and<br />
we take account of it all to work out what’s most<br />
important to them:<br />
Complaints, comments and concerns<br />
Feedback cards<br />
Surveys<br />
Patient stories<br />
Feedback App<br />
Websites like NHS Choices and<br />
Patient Opinion<br />
Consultations<br />
Mystery Shoppers<br />
l Listening to our staff. The views of the staff who<br />
work in our hospital every day are vital and we<br />
encourage them to tell us what they think<br />
through surveys, consultations and feedback<br />
events. It’s also really important that we keep an<br />
eye on their happiness and make sure they’re<br />
fully supported so that they are able to deliver<br />
the best services they can.<br />
l Listening to others. The views of BCH groups<br />
like the Young Person Advisory Group help us<br />
focus on how to make the improvements that are<br />
needed.<br />
l Analysing information about the quality of<br />
services, such as patient safety incidents and<br />
clinical audits.<br />
l Using best practice examples, national targets<br />
and learning from and benchmarking with other<br />
organisations.<br />
92 93<br />
BACK TO CONTENTS PAGE<br />
Using this information has helped us to identify<br />
Quality Priorities, which are the main areas we<br />
want to focus on to improve quality. Each priority<br />
has a goal and a way of measuring our progress in<br />
reaching it. These relate to the three elements of<br />
quality: Patient Experience, Clinical Effectiveness,<br />
and Safety. The priorities we are reporting on this<br />
year are:<br />
In 2013/14 we will also report on some additional<br />
priorities that we have been developing during<br />
2012/13:<br />
Safety:<br />
Patient Experience:<br />
Patient Experience<br />
Emergency Department Transfers<br />
Staff Survey<br />
Food and Nutrition<br />
Tertiary Inpatient Referrals<br />
Play and Activities<br />
Cancelled Operations<br />
Clinical Effectiveness<br />
Nursing Care Quality Indicators<br />
CAMH Service User Satisfaction<br />
Asthma Care<br />
Health Promotion<br />
Safety<br />
Pressure Ulcers<br />
Preventing MRSA<br />
Reducing Acute Life Threatening Events, and<br />
Cardiac and Respiratory Arrests<br />
Reducing Healthcare Acquired Infections in PICU<br />
Reducing MSSA<br />
Zero Avoidable Deaths Reducing rates of<br />
Clostridium Difficile<br />
Reducing Medication Incidents Resulting in Harm<br />
WHO Safe Surgery Checklist Completion<br />
Extravasation Injuries<br />
Friends and Family test<br />
(for children and young<br />
people)<br />
Clinical Effectiveness: Implementing the Sepsis<br />
Care Bundle<br />
These priorities and what we’ve achieved in<br />
2012/13 are set out over the next few pages of this<br />
Quality Account.
BACK TO CONTENTS PAGE<br />
Listening to Patients and Families: Food & Nutrition<br />
A healthy diet can help patients get better quicker<br />
and go home earlier. Having tasty food, with plenty<br />
of choice, which meets everyone’s needs, is vital to<br />
the wellbeing of our children and young people, and<br />
ensures they have a good experience while they<br />
are in hospital.<br />
Figure 6: Percentage of patients weighed and measured per Quarter 2011/12 - 2012/13<br />
GOAL:<br />
100% patients<br />
weighed and<br />
measured<br />
MEASURE:<br />
% weighed<br />
and measured<br />
per quarter<br />
100%<br />
90%<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
99% 95% 93% 95% 97% 98% 98% 96%<br />
How have we done?<br />
Until 2012 these questions were answered through<br />
a Food Survey but in 2012 we started asking the<br />
questions during our regular Catering Quality<br />
Walkabouts when we carry our checks on food<br />
service on wards and address any immediate<br />
issues. This way we can only ask a few children<br />
and young people at a time, so next year we want<br />
to develop new ways of getting views from as many<br />
people as possible.<br />
What are we doing to improve?<br />
In 2012/13 we introduced a new electronic<br />
food ordering system called MAPLE which was<br />
developed with local software developer Ambinet<br />
and our caterer Sodexo. MAPLE is an interactive,<br />
fun way for our patients to order their meals<br />
and is programmed to meet individual dietary<br />
requirements. MAPLE has been really successful –<br />
our patients and families say it is practical and easy<br />
to use and it has received five awards.<br />
The MAPLE food ordering system means that<br />
children and young people will now always be able<br />
to order what they want from the menu. We will<br />
consult with our Young Person Advisory Group<br />
(YPAG) about new questions we should ask<br />
children and young people to ensure we get the<br />
information we need to help us improve. Food will<br />
also be a theme of YPAG walkabouts in 2013/14.<br />
0%<br />
Quarter 1 Quarter 2 Quarter 3 Quarter 4 Quarter 1 Quarter 2 Quarter 3 Quarter 4<br />
2011/12 2011/12 2011/12 2011/12 2012/13 2012/13 2012/13 2012/13<br />
How have we done?<br />
We have continued to perform really well with this<br />
measure. We will continue to monitor this but as we<br />
have demonstrated sustained high performance we<br />
will not report it separately from the other Nursing<br />
Care Quality Indicators (NCQIs) next year.<br />
In 2013/14 we will be focusing on offering<br />
appropriate healthy eating advice where it is<br />
needed. We will also be using a new electronic<br />
process to collect the NCQI data which will allow us<br />
to monitor this every month rather than quarterly,<br />
which will help us address issues more quickly.<br />
Figure 7: Percentage of patients who choose what they want and are<br />
happy with their choice – 2009/2012/13<br />
GOAL:<br />
year on year<br />
improvement in<br />
patients being<br />
happy with<br />
food<br />
MEASURE:<br />
% of patients who choose<br />
what they want & are happy<br />
with their choice<br />
100%<br />
90%<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
0%<br />
2009 May - 10 Dec - 10 2011 2012 2012/13<br />
The food is alright –<br />
better than I expected.<br />
Generally the food<br />
tastes nice.<br />
Everything is good except<br />
for the food. Food needs to<br />
be improved.<br />
I like the way my<br />
food order follows<br />
me round the<br />
hospital on MAPLE<br />
so when I move<br />
wards I still get the<br />
meals I’ve ordered.<br />
I choose what<br />
I want from<br />
the menu<br />
I am happy<br />
with the choice<br />
I am given at<br />
mealtimes<br />
94 95
BACK TO CONTENTS PAGE<br />
Listening to Patients and Families: Play & Activities<br />
Play and activities are important for the wellbeing<br />
of all children and young people who spend time<br />
in hospital. They can also provide an essential<br />
distraction from distressing aspects of care. It’s<br />
important that activities, toys and equipment are<br />
of good quality, are age appropriate, and easily<br />
accessible. We categorise feedback about play and<br />
activities as either ‘positive’ or ‘need to improve’.<br />
Figure 8: Percentage of positive and ‘need to improve’ comments received<br />
2011/12 & 2012/13<br />
Play and Activities Feedback 2012/13<br />
GOAL:<br />
year on year<br />
improvement in<br />
positive<br />
feedback<br />
MEASURE:<br />
% of positive feedback<br />
compared to<br />
‘need to improve’<br />
100%<br />
90%<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
0%<br />
How have we done?<br />
54%<br />
Positive<br />
46%<br />
The picture is very similar to last year. Having the<br />
right toys, equipment and activities continues to<br />
be really important to people who visit and stay<br />
at our hospital. ‘Need to Improve’ comments can<br />
include things we need to change or do better, like<br />
provide more things to do for older children and<br />
young people. These comments also include lots<br />
of suggestions about different toys, games and<br />
activities that children and young people would<br />
really like to be available. It’s important that we<br />
continue to monitor everything that people are<br />
saying so we know where we need to do better<br />
and understand what it is that children and young<br />
people want and need.<br />
Need to improve<br />
53%<br />
2011/12 2012/13<br />
47%<br />
I liked that the nurses gave<br />
me colouring books and<br />
pens when I was bored.<br />
Although my child enjoyed<br />
playing in the playroom it was<br />
quite small and not easily<br />
accessible if the patient is<br />
on IVs etc, and have a dripstand<br />
attached to them.<br />
There was no adolescent<br />
room like there is on<br />
other wards.<br />
l We will run a ‘promoting happy parenting’ course<br />
to help parents with the challenges they face<br />
when their children are in hospital.<br />
l We will improve information about play and<br />
activities so that children, young people and<br />
families know what is available at the hospital.<br />
l We will share our play and activity resources<br />
better between wards to ensure that more<br />
children and young people in the hospital have<br />
opportunities use everything that is available.<br />
l We will ask our volunteers to support<br />
improvements in play and activities.<br />
Listening to Patients and Families: Emergency Department Transfers<br />
Until 2010/11 patients who came to our Emergency<br />
Department were regularly transferred to other<br />
hospitals after treatment because there were no<br />
inpatient beds available. This was a really bad<br />
experience for patients and their families so we<br />
adapted our processes and procedures to ensure<br />
this would change.<br />
Figure 9: Patients transferred out of ED per month 2010/11 - 2012/13<br />
GOAL:<br />
all patients<br />
who attend ED &<br />
require<br />
inpatient care<br />
will be<br />
admitted<br />
MEASURE:<br />
number of patients<br />
transferred out of ED<br />
per month<br />
Number of patients transferred<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
How have we done?<br />
We have continued to follow the processes we set<br />
in 2010/11 and maintained our objective for most of<br />
the year. In July 2012 one patient was transferred<br />
out. This has been reviewed, and while the decision<br />
to transfer was clinically right, there were processes<br />
that could have been followed that would have<br />
avoided the need for this transfer.<br />
We will continue to monitor this indicator but we<br />
will not report this as a quality priority in our next<br />
Quality Account if we continue to perform well.<br />
0<br />
A M J J A S O N D J F M<br />
2010/11<br />
2011/12<br />
2012/13<br />
What are we doing to improve?<br />
l We will be investing all our 2013/14 allocation<br />
for improving patient experience by upgrading<br />
the ward play areas.<br />
l We have a new weekly Stay and Play group to<br />
provide patients and siblings the opportunity to<br />
play in a supportive environment. Feedback from<br />
initial sessions is really positive.<br />
l We are developing an activity book for children<br />
and young people who come to the Emergency<br />
Department to entertain and educate them<br />
about what they might see and what might<br />
happen to them while they are there. This is<br />
linked to activities in schools to educate young<br />
people about accessing health care.<br />
l We are creating a Play Charter which will allow<br />
us to set some specific, measurable objectives to<br />
support improvements in play.<br />
96 97
BACK TO CONTENTS PAGE<br />
Listening to Patients and Families: Tertiary Inpatient Referrals<br />
When a child or young person needs to come to<br />
BCH for urgent inpatient care from home or from<br />
another hospital, it’s important that their admission<br />
is not delayed as this could have a negative impact<br />
on their care. In 2010/11 we decided to make sure<br />
delays did not happen and put processes in place<br />
to meet our goal.<br />
Figure 10: Number of patients not offered a BCH bed within 24 hours 2010/11 - 2012/13<br />
GOAL:<br />
all children<br />
referred for<br />
urgent inpatient<br />
care will be<br />
admitted<br />
within 24<br />
hours<br />
MEASURE:<br />
number of children<br />
per month not offered<br />
a bed within 24 hours<br />
of urgent referral<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
2010 - 11<br />
2011 - 12<br />
2012 - 13<br />
Listening to Patients and Families: Cancelled Operations<br />
Patients, families and staff have told us that when<br />
an operation has to be cancelled by the hospital<br />
this can have a huge impact. It might mean travel<br />
arrangements and time off school and work have to<br />
be rearranged and could also mean that tests and<br />
assessments have to be done again. We know this<br />
can be very stressful and inconvenient.<br />
There are times when we can’t avoid cancelling<br />
operations because of emergencies like transplants<br />
which can’t wait, or when another operation is more<br />
complex than expected, so it takes longer than<br />
planned. Sometimes an operation can’t go ahead<br />
because there aren’t enough beds that day on PICU<br />
to care for the patient after the operation.<br />
Over the last few years we have been working hard<br />
to try to reduce the number of operations that we<br />
cancel, especially those that we cancel on the actual<br />
day. At the same time we have been finding ways to<br />
make the experience better for patients and families<br />
when we can’t avoid cancelling their operation.<br />
0<br />
A M J J A S O N D J F M<br />
Figure 11: Monthly cancelled operations 2010/11 - 2012/13<br />
How have we done?<br />
With more people than ever before wanting<br />
to access our services, 2012/13 was a really<br />
challenging year and our staff had to work very<br />
hard to meet our goal.<br />
What are we doing to improve?<br />
Meeting our goal while demand for our services<br />
increases means we need to increase the capacity<br />
in our hospital. This does not necessarily mean<br />
creating physical space for more beds. It’s also<br />
important that we find ways of reducing the time<br />
that people need to spend in hospital, and the<br />
number of times they need to be admitted, so that<br />
more beds are available. Some examples of what<br />
we are doing to achieve this are:<br />
l Developing services like <strong>Hospital</strong> @ Home so<br />
some children can be discharged earlier<br />
l Improving discharge processes so that once a<br />
child is ready to be discharged this happens<br />
much quicker<br />
l Developing our outpatient services so that<br />
children with long-term conditions like Diabetes<br />
and Asthma are less likely to deteriorate and<br />
need admission to hospital<br />
l Improving flow through the hospital so that<br />
people can get into wards quicker and can be<br />
discharged earlier<br />
l Establishing new services like our Paediatric<br />
Assessment Clinical Intervention and Education<br />
(PACE) team (see page 99) which supports high<br />
dependency patients on wards and allows earlier<br />
access to PICU for children and young people<br />
who need it.<br />
Other examples can be found on page 99 in the<br />
section about cancelled operations.<br />
GOAL:<br />
no more<br />
than 0.8% of<br />
operations<br />
cancelled<br />
on the day<br />
MEASURE:<br />
number of operations<br />
cancelled on the day<br />
per month<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
How have we done?<br />
We have not met our target, with 1.68% of<br />
operations cancelled on the day. We have been<br />
experiencing our highest ever activity levels, which<br />
has put pressure on our theatres, PICU and wards,<br />
and we were therefore unable to meet our goal<br />
in 2012/13. Opening our new PICU extension in<br />
November 2012 helped us improve, and in January<br />
2013 we launched our new (PACE) team which<br />
frees up more beds for our sickest children when<br />
they have had an operation.<br />
0<br />
A M J J A S O N D J F M<br />
Whoever told us was<br />
very nice, supportive, and<br />
apologetic.<br />
98 99<br />
You learn to understand that<br />
emergencies come first. You put<br />
everything back into perspective a<br />
little while afterwards but at the time<br />
we were really upset.<br />
2010 - 11<br />
2011 - 12<br />
2012 - 13<br />
When you’ve been told how<br />
important it is to get the<br />
operation done you start to<br />
get really worried that it’s not<br />
happening and you get more<br />
and more worried that she<br />
will be getting worse.
What else are we doing to improve?<br />
Improving the experience for children,<br />
young people and families<br />
Because we know that we will always have to<br />
cancel some less urgent operations we have been<br />
talking to patients and families to understand how<br />
we can make the experience better when this<br />
happens. We know that communication is really<br />
important, so they know what’s going on as early<br />
as possible. We also know we need to make sure<br />
our staff are trained in the best ways to talk to<br />
families when their operation is cancelled, so that<br />
they give them all the information they need and<br />
are able to support them when they’re upset or<br />
angry.<br />
Identifying all the reasons for cancellations<br />
and taking action<br />
We have set up a Task and Finish Group which is<br />
examining the reasons for all cancelled operations<br />
very closely to identify ways we can improve.<br />
They are already making progress, for example<br />
patients are now contacted three days before<br />
their operation to make sure they have all the<br />
information they need.<br />
Improving processes like discharge, so beds<br />
are available more quickly<br />
We have changed the model of care on the<br />
Medical <strong>Day</strong> Care Unit so that it is now nurse-led.<br />
This means that each child and young person<br />
is admitted, treated and discharged by a named<br />
nurse. This has reduced delays for these patients<br />
along every step of their pathway, ensuring not<br />
only a speedy stay with us, but a fantastic patient<br />
journey.<br />
Reviewing patient pathways, to improve flow<br />
through wards<br />
The Surgical <strong>Day</strong> Care Unit cares for children<br />
requiring short stay surgery. We have changed<br />
the way we work on this Unit to a 23-hour model<br />
which means that some children can have<br />
procedures later in the day, and be discharged<br />
up to 11pm, and other children who require an<br />
overnight stay can be discharged at 7am. Patients,<br />
parents and carers have given very positive<br />
feedback about these changes as they appreciate<br />
being able to return to their home environment as<br />
soon as possible. By switching to this new way of<br />
working, we have maximised capacity, ensuring<br />
cancellations due to lack of beds has been<br />
significantly reduced.<br />
In 2013/14 we will also be:<br />
Opening more beds to increase capacity<br />
l Another five beds are planned in PICU for 2013.<br />
l We are opening more day beds/treatment chairs<br />
in the Medical <strong>Day</strong> Unit, which will allow us to<br />
treat more patients in the Unit, freeing up beds<br />
on the inpatient wards.<br />
Developing new areas to improve the<br />
experience and increase capacity<br />
Some of our parents and children have said that they<br />
do not like being in a bed before an operation as this<br />
can make them more anxious. To make this better we<br />
are creating a new lounge area in the Surgical <strong>Day</strong><br />
Care Unit where children can stay and play until they<br />
are ready to walk to theatre for their operation. Only<br />
once they have had their operation will they need to<br />
be in a bed to recover. This new way of working will<br />
help us free up more beds, allowing us to do more<br />
operations every day.<br />
Expanding our Pre-Admission Service to prevent<br />
avoidable delays<br />
We are developing this service to ensure that all<br />
children and young people will have access to it, which<br />
will help prevent cancellations caused by things like:<br />
l Families changing their minds about having an<br />
operation<br />
l Incorrect listing of an operation<br />
l Children having eaten too close to the planned<br />
operation.<br />
Developing plans to increase physical capacity<br />
We know we need more physical operating capacity<br />
due to increasing demand so we are working on plans<br />
to open more theatres.<br />
Working with other children’s hospitals to see<br />
what we can learn from the way that they work<br />
Every children’s hospital is unique, with different<br />
services meeting a range of different needs, but we<br />
can all learn from each other to make sure all children<br />
have a fantastic experience. We have set up a group<br />
with other children’s hospitals around the country to<br />
see if we can learn from each other about ways of<br />
reaching our goals.<br />
Listening to our Staff: Staff Survey<br />
Staff are our most important resource.<br />
Understanding their views about the quality of our<br />
services is crucial to ensuring that we can make<br />
improvements where they are needed.<br />
Figure 12: Key Staff Survey Results 2009 - 2012<br />
MEASURE:<br />
% of staff who agree that<br />
they would be happy with<br />
the standard of care<br />
at the Trust<br />
MEASURE:<br />
% of staff who agree<br />
that care of patients is<br />
the Trust’s top priority<br />
Figure 13: Staff Satisfaction Score 2011/12<br />
How have we done?<br />
There has been very little change in the results<br />
but we are disappointed not to have done better.<br />
2012/13 was a challenging year for our staff due<br />
to higher levels of activity and more patients with<br />
complex needs, and we know they have been<br />
working really hard to make sure children, young<br />
people and their families have safe, high quality<br />
care and a fantastic patient experience.<br />
What are we doing to improve?<br />
We are developing new ways to monitor how<br />
our staff are feeling - such as sickness absence<br />
and staff turnover - and we integrate this with<br />
information about the safety and quality of<br />
services. This helps us predict which areas might<br />
be coming under pressure. We are also doing lots<br />
100 101<br />
3.45<br />
100%<br />
90%<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
0%<br />
64%<br />
3.58 3.67<br />
BCH Score BCH Score Acute Specialist<br />
2011 2012 Trusts Score 2012<br />
85%<br />
65%<br />
87%<br />
BACK TO CONTENTS PAGE<br />
GOAL:<br />
year on year<br />
improvement in<br />
response to key<br />
staff survey<br />
questions<br />
2009 2010 2011 2012<br />
Care of patients is my Trust’s priority<br />
If a friend or relative needed treatment, I would be happy with the standard<br />
of care provided by this Trust<br />
MEASURE:<br />
staff job satisfaction<br />
score<br />
70%<br />
86% 83%<br />
76%<br />
more to gather the views of our staff throughout<br />
the year, keep them informed and support them<br />
to continue to provide the best services possible.<br />
Other methods we are adopting to improve staff<br />
experience include:<br />
l ‘Star of the Month’ nominated by staff, patients<br />
and families<br />
l Regular polls to help us understand staff mood<br />
l Launch of a new Health and Wellbeing Strategy<br />
with lots of opportunities for staff to improve their<br />
health and get support when they need it<br />
l Helping our leaders to support their staff when<br />
they feel stressed<br />
l Annual Night of Stars and Long Service Awards<br />
to reward outstanding contributions<br />
l Engaging with staff to obtain their views on<br />
themes arising out of the Francis report<br />
(see page 54)
BACK TO CONTENTS PAGE<br />
Providing Even Better Nursing Care:<br />
Nursing Care Quality Indicators (NCQIs)<br />
Excellent nursing care is vital to ensuring our<br />
patients are safe, have a good experience and<br />
have good clinical outcomes. In 2010/11 we<br />
developed quality indicators in the most important<br />
areas. A new indicator was added for cannula care<br />
in 2012/13.<br />
Providing Even Better Nursing Care: Asthma Care<br />
When children and young people with asthma use<br />
an inhaler, it’s essential that they use it properly to<br />
get the full benefits.<br />
It’s also important that we ensure that they are<br />
involved in decisions about their care and we do<br />
this by agreeing their care plan with them and<br />
giving them a copy.<br />
GOAL:<br />
year<br />
improvememnt<br />
in performance<br />
against<br />
each NCQI<br />
MEASURE:<br />
quarterly Trust-wide<br />
performance<br />
Observations:<br />
making sure any<br />
problems are<br />
detected quickly.<br />
Pain management:<br />
understanding the<br />
patient’s pain and giving<br />
the right pain medicine.<br />
Personal hygiene:<br />
helping patients clean<br />
their teeth and wash.<br />
Food and nutrition:<br />
weighing and measuring<br />
patients and providing<br />
the right support.<br />
Drug administration:<br />
keeping drugs secure<br />
and giving the right<br />
medicine.<br />
Cannula care:<br />
avoiding injuries caused<br />
by cannules.<br />
Skin care:<br />
avoiding skin damage<br />
caused by pressure.<br />
Communication:<br />
involving patients and<br />
their families in care<br />
planning and talking to<br />
them in the right way.<br />
MEASURE:<br />
BTS National Audit<br />
- BCH performance compared<br />
to national benchmark<br />
100<br />
80<br />
60<br />
GOAL:<br />
every child with<br />
asthma will<br />
agree a<br />
written care<br />
plan<br />
Figure 15: BTS National Audit Performance 2010 - 2012<br />
GOAL:<br />
every child<br />
will have an<br />
inhaler<br />
health check<br />
every year<br />
2010 2011 2012<br />
40<br />
Figure 14: NCQI Performance 2010/11 - 2012/13<br />
20<br />
100%<br />
90%<br />
80%<br />
70%<br />
60%<br />
50%<br />
2010/11<br />
2011/12<br />
0<br />
BCH<br />
National<br />
BCH<br />
National<br />
BCH<br />
National<br />
Device technique assessed<br />
40%<br />
30%<br />
20%<br />
10%<br />
0%<br />
Observations<br />
Nutrition<br />
How have we done?<br />
Skin<br />
Pain<br />
Drug administration<br />
Communication<br />
Hygiene<br />
Cannula care<br />
2012/13<br />
What are we doing to improve?<br />
How have we done?<br />
We continue to perform above the national<br />
average (which has improved), but our<br />
performance has dipped compared to the last two<br />
years. This is really disappointing as we know from<br />
previous years that we are able to do this well.<br />
What are we doing to improve?<br />
During 2013/14 we will be looking into ways of<br />
ensuring that adherence to the asthma care<br />
pathway is embedded in normal clinical practice.<br />
Written asthma care plan given<br />
We have continued to do really well, with<br />
improvements in every indicator in 2012/13,<br />
especially in pain management. We are also<br />
really pleased with such high performance in our<br />
first year in monitoring cannula care.<br />
We are creating an electronic method to collect<br />
performance data which will allow us to monitor<br />
this every month rather than just quarterly. This will<br />
enable us to identify and address any issues much<br />
earlier.<br />
We will also amend the asthma care pathway to<br />
reflect the new NICE Asthma Quality Standards.<br />
We will report on our progress in our next Quality<br />
Account.<br />
102 103
BACK TO CONTENTS PAGE<br />
Providing Even Better Nursing Care: Pressure Ulcers<br />
Improving Health Outcomes: Health Promotion<br />
Some of our patients - in particular the sickest<br />
patients on PICU - are at risk of developing<br />
pressure ulcers which, if left untreated, can become<br />
very serious. We are working toward the complete<br />
eradication of pressure ulcers, in line with the<br />
ambition of the whole NHS.<br />
We have an important role to play in improving<br />
general health outcomes and reducing health<br />
inequalities for children and young people. Good<br />
general health for the whole family is even more<br />
important when a child becomes ill or has a longterm<br />
condition.<br />
GOAL:<br />
improve health<br />
outcomes in the<br />
long-term<br />
and reduce<br />
health<br />
inequalities<br />
Figure 16: Pressure Ulcer rates 2012/13<br />
GOAL:<br />
zero<br />
pressure ulcers<br />
of<br />
grade 2<br />
or above<br />
2.5<br />
2<br />
Ask 25% of<br />
children aged<br />
over 12 if they smoke<br />
Offer advice to<br />
90% of children<br />
who say they smoke<br />
MEASURE:<br />
number of avoidable<br />
grade 2 or above<br />
pressure ulcers<br />
1.5<br />
1<br />
0.5<br />
0<br />
M A M J J A S O N D J F M<br />
Measures<br />
Ask 25% of<br />
parents/carers<br />
if they smoke<br />
Offer advice to<br />
50% of parents/carers<br />
who say they smoke<br />
How have we done?<br />
We have done really well in 2012/13.<br />
l Whenever a pressure ulcer is identified the<br />
patient’s care is reviewed by a clinical expert.<br />
So far in 2012/13, the care provided in all<br />
cases has been appropriate.<br />
Pressure Ulcers Grades Explained<br />
1: Reddening skin<br />
Ask 25% of<br />
children aged<br />
over 12 if they drink<br />
or take drugs<br />
Offer advice to<br />
70% of children<br />
who say they drink<br />
or take drugs<br />
l There have been no grade 3 or 4 pressure<br />
ulcers.<br />
2: Skin loss to one or two layers of skin<br />
l Zero Grade 2 pressure ulcers have been<br />
categorised as avoidable.<br />
l The number of Grade 2 pressure ulcers has<br />
decreased over the year.<br />
What are we doing to improve?<br />
We have been asked to contribute to the<br />
development of NICE guidance on paediatric<br />
pressure ulcers so that the improvements that<br />
we have achieved will benefit children and young<br />
people in hospitals across the NHS.<br />
3. Full thickness skin loss involving<br />
damage to the underlying tissue<br />
4. Extensive damage to muscle, bone<br />
or supporting structures.<br />
How have we done?<br />
We have done really well in 2012/13.<br />
l We have met all of our goals.<br />
l Referrals to Stop Smoking services have<br />
significantly increased.<br />
l We have achieved status as a World Health<br />
Organisation (WHO) Health Promoting<br />
<strong>Hospital</strong> so we now part of an international<br />
network of hospitals that aim to improve health<br />
by developing structures, cultures, decisions<br />
and processes.<br />
104 105<br />
What are we doing to improve?<br />
l We are providing training and awareness<br />
sessions for staff.<br />
l We have established a smoking referral<br />
pathway.<br />
l We have new data recording systems so that<br />
we can monitor the impact of our work.<br />
l We are displaying information about alcohol on<br />
screens in the main Outpatients department.
BACK TO CONTENTS PAGE<br />
Improving Health Outcomes: CAMH Service User Satisfaction<br />
Measuring the difference our services make to the<br />
people who use them helps us to understand what<br />
we are doing well and where we might need to<br />
make improvements.<br />
Figure 17: CAMHS Questionnaire Scores 2011/12 - 2012/13<br />
80%<br />
GOAL:<br />
61% of people<br />
feel they have<br />
a better health<br />
outcome as<br />
a result of<br />
using<br />
CAMHS<br />
Reducing Infection: Reducing Healthcare Acquired Infections in PICU<br />
Our sickest patients on our Paediatric Intensive<br />
Care Unit (PICU) are most at risk of healthcare<br />
associated infections (HCAIs). This can be very<br />
serious and means they have to spend more time<br />
in hospital. Reducing the risk of infections for these<br />
patients can help them get well quicker and be<br />
discharged earlier.<br />
Figure 18: HCAIs in PICU 2011/12 - 2012/13<br />
GOAL:<br />
reduce Central<br />
Venous Catheter<br />
(CVC) infections<br />
GOAL:<br />
reduce Ventilator<br />
Associated<br />
Pneumonia<br />
MEASURE:<br />
% of people who say that<br />
since using CAMHS they feel<br />
a bit better/much better<br />
(improvement score)<br />
70%<br />
60%<br />
1.8<br />
1.6<br />
MEASURE:<br />
% of people who say that<br />
using CAMHS has made<br />
their problems quite a lot<br />
or a great deal better<br />
50%<br />
40%<br />
30%<br />
20%<br />
MEASURE:<br />
less than 1.4 CVC<br />
infections<br />
per 1,000 patient days<br />
10%<br />
( helpful score) MEASURE:<br />
0%<br />
Helpful Helpful Improvement Improvement<br />
Parent Service User Parent Service User<br />
2011/12<br />
less than 1.73 incidents<br />
of VAP<br />
per 1,000 ventilator days<br />
1.4<br />
1.2<br />
1<br />
0.8<br />
0.6<br />
0.4<br />
0.2<br />
2011/12<br />
2012/13<br />
2012/13<br />
0<br />
Rate of CVC infections per 1,000<br />
CVC - patient days<br />
Rate of Ventilator Associated<br />
Pneumonia (VAP) per 1,000<br />
ventilator days<br />
How have we done?<br />
We have met the national target for all questions<br />
except the percentage of service users who feel<br />
the service has helped to make their problems<br />
better.<br />
What are we doing to improve?<br />
We are improving the way that we engage with<br />
young people to better understand their views on<br />
CAMHS. We have set up focus groups to ensure<br />
that we ask young people about the specific<br />
care pathways they are on to support redesign<br />
and development. We are also improving our<br />
website with the help of our young people and<br />
their families and providing further opportunities<br />
for them to give us their views through the Trust<br />
feedback app.<br />
How have we done?<br />
We have achieved our goal and improved on<br />
last year’s performance in relation to Ventilator<br />
Associated Pneumonia (VAP). We have shared<br />
the VAP results with the International Forum on<br />
Quality and Safety in Healthcare.<br />
We have seen a small increase in our Central<br />
Venous Catheter (CVC) infection rate in 2012/13.<br />
Although this is still below our target rate of<br />
1.4, we are investigating the reasons for this to<br />
determine what we can do to reduce this rate<br />
even further.<br />
106 107<br />
What are we doing to improve?<br />
We are now monitoring rates of infections in other<br />
areas of the hospital too, with most wards doing<br />
well.<br />
We will continue to develop the practices we have<br />
put in place and to learn from every infection that<br />
does occur to reduce the rate of infections in PICU<br />
and across the hospital to a minimum level.
108 109<br />
Reducing Infection: Reducing Rates of Clostridium Difficile<br />
Clostridium difficile are bacteria present naturally<br />
in the gut of around two-thirds of children and 3%<br />
of adults. C.difficile does not cause any problems<br />
in healthy people. However, some antibiotics used<br />
to treat other health conditions can interfere with<br />
the balance of ‘good’ bacteria in the gut. When this<br />
happens, the bacteria can multiply and produce<br />
toxins, which cause illness such as diarrhoea and<br />
fever. As C.difficile infections are usually caused<br />
by antibiotics, most cases happen in a healthcare<br />
environment. Reducing rates of C.difficile in<br />
hospitals is a national priority.<br />
Figure 19: C.Difficile infections 2010/11 - 2012/13<br />
3<br />
GOAL:<br />
no more than 1<br />
infection during the<br />
year<br />
Reducing Infection: Preventing MRSA<br />
Blood stream infections with MRSA can be very<br />
serious for people who are unwell and can result<br />
in additional treatment and an increased length of<br />
stay.<br />
Figure 20: MRSA infections 2007/08 - 2012/13<br />
3<br />
2<br />
1<br />
BACK TO CONTENTS PAGE<br />
GOAL:<br />
maintain a<br />
zero level<br />
of MRSA<br />
MEASURE:<br />
number of infections<br />
per year<br />
2<br />
1<br />
MEASURE:<br />
number of infections<br />
per year<br />
0<br />
2007/08 2008/09 2009/10 2010/11 2011/12 2012/13<br />
How have we done?<br />
For the second year in a row we have had no<br />
MRSA infections at all.<br />
0<br />
2010/11 2011/12 2012/13<br />
How have we done?<br />
We had one case of C.difficile in 2012/13 and made<br />
sure that the ward where this occurred had extra<br />
cleaning until there was no trace of C.difficile in the<br />
environment. We also carried out tests in other high<br />
risk wards and found no C.difficile at all.<br />
What are we doing to improve?<br />
We have tried out a new sampling technique and<br />
now carry out extra testing to identify patients who<br />
do not have true C.difficile infection but might be<br />
carrying the bacteria which could put other patients<br />
at risk. Early identification and protection measures<br />
reduce this risk.<br />
What are we doing to improve?<br />
Achieving this goal has been a challenge in<br />
2012/13, particularly with some patients who are<br />
at very high risk of MRSA bacteraemia. We will<br />
continue to practice everything we have learned<br />
that has ensured that we have had no MRSA<br />
infections since 2010, and we will continue to<br />
apply new best practice and learning from other<br />
organisations.
110 111<br />
Reducing Infection: Reducing MSSA<br />
MSSA is a common bacteria carried on the skin of<br />
30% of the population. MSSA bloodstream infection<br />
is a risk for some of our patients, especially those<br />
who have a central venous catheter (CVC).<br />
Figure 21: MSSA post 48 hours rates 2011/12 - 2012/13<br />
5<br />
GOAL:<br />
10% reduction<br />
in post 48 hour<br />
hospital acquired<br />
infections<br />
Providing the Safest Possible Care: Medication Incidents<br />
We encourage staff to report every incident, from<br />
the most serious to near-misses. At BCH we use<br />
a lot of medicines so there are many opportunities<br />
for errors to occur, and medication incidents are the<br />
most frequently reported incident type. We want to<br />
see a high number of reported medication incidents<br />
at a low level of harm, as this shows a good safety<br />
culture.<br />
Figure 22: Medication Incidents (Harm Category) 2012/13<br />
80<br />
BACK TO CONTENTS PAGE<br />
GOAL:<br />
reduce proportion<br />
of medication incidents<br />
resulting in harm to less<br />
than 1% of all madication<br />
incidents and keep<br />
those causing<br />
serious harm<br />
at zero<br />
MEASURE:<br />
number of infections<br />
per month<br />
4<br />
3<br />
2<br />
1<br />
2011 - 12<br />
2012 - 13<br />
MEASURE:<br />
medication incidents<br />
resulting in harm<br />
as a % of all<br />
medication incidents<br />
70<br />
60<br />
50<br />
40<br />
No Harm<br />
Minor, Non<br />
Permanent Harm<br />
(up to 1 month)<br />
Moderate, Semi<br />
Permanent Harm<br />
(up to 1 month)<br />
0<br />
A M J J A S O N D J F M<br />
MEASURE:<br />
number of medication<br />
incidents resulting<br />
in serious harm<br />
30<br />
20<br />
10<br />
Severe<br />
Catastrophic,<br />
Death<br />
Near Miss<br />
How have we done?<br />
0<br />
A M J J A S O N D J F M<br />
In 2011/12, our first year of monitoring, we achieved<br />
substantial reductions, exceeding our target. In<br />
2012/13 it has been challenging to reduce this any<br />
further, with a similar number of infections during<br />
both years. We did not therefore meet our target.<br />
We have analysed every MSSA infection to identify<br />
the cause and any opportunity to prevent them.<br />
Dr Jim Gray, Head of Microbiology and his team<br />
were recognised at the national NHS Innovation<br />
Challenge Prizes, where they were highly<br />
commended for their work in reducing MSSA<br />
bloodstream infections in children who receive their<br />
parenteral nutrition at home. The hard work of the<br />
team reduced the numbers of infections by a third<br />
and it is hoped that this example of good practice<br />
will be rolled out across the hospital.<br />
What are we doing to improve?<br />
We believe we can improve even further and will<br />
focus in particular in 2013/14 on reducing MSSA as<br />
contaminants in blood cultures.<br />
How have we done?<br />
We have met both goals: 0.94% of all medication<br />
incidents caused harm. Zero medication incidents<br />
caused serious harm.<br />
We take every incident seriously and next year we<br />
want to see a further reduction in the percentage of<br />
incidents that cause any harm at all.<br />
What are we doing to improve?<br />
We have created detailed easy to read staff<br />
guidance on all high risk injectable drugs.<br />
We have developed standardised labels for<br />
marking high risk drug infusions.<br />
We have reviewed the ward stock arrangements<br />
so that most high risk drugs need to be specifically<br />
ordered from our pharmacy department. This<br />
means that the pharmacy staff can highlight any<br />
guidance when issuing the drug.<br />
We will deliver additional training on preparing<br />
liquid medication.<br />
We will develop standardised guidelines for each<br />
drug which will be reviewed at regular intervals.<br />
We have introduced the role of Medicines Safety<br />
<strong>Nurses</strong> to act as local educators and champions<br />
of best practice.<br />
We have included additional guidance on good<br />
prescribing practice on the junior doctors’ induction.<br />
We have produced dose calculators for a number<br />
of intravenous medications to minimise the chance<br />
of making a calculation error.
BACK TO CONTENTS PAGE<br />
Providing the Safest Possible Care: Acute Life-Threatening Events (ALTEs),<br />
Cardiac Arrests and Respiratory Arrests<br />
Good monitoring on wards means that we will<br />
pick up deteriorating patients more quickly and<br />
avoid preventable emergency and life- threatening<br />
events.<br />
Figure 23: Emergency Events 2012/13<br />
GOAL:<br />
reduce the number<br />
of life threatening<br />
events which<br />
were preventable<br />
and could have<br />
been predicted by<br />
monitoring to zero<br />
Providing the Safest Possible Care: Mortality<br />
Thankfully, the number of deaths at BCH is very<br />
low relative to the number of patients we treat and<br />
the seriousness and complexity of their illnesses.<br />
We review every individual death to see if there<br />
is anything we can learn, and to ensure that no<br />
death is avoidable.<br />
GOAL:<br />
zero avaiodable<br />
deaths<br />
Figure 24: Deaths and deaths per 1,000 admissions 2011/12 - 2012/13<br />
11<br />
10<br />
MEASURE:<br />
number of cardiac arrests<br />
on PICU and those<br />
that were preventable<br />
MEASURE:<br />
absolute number<br />
of deaths<br />
14<br />
12<br />
9<br />
10<br />
8<br />
7<br />
6<br />
MEASURE:<br />
number of cardiac arrests<br />
on wards, ED and theatres<br />
and those<br />
that were preventable<br />
MEASURE:<br />
number of deaths<br />
per 1,000 admissions<br />
8<br />
6<br />
4<br />
5<br />
4<br />
3<br />
MEASURE:<br />
number of<br />
respiratory arrests<br />
and those<br />
that were preventable<br />
MEASURE:<br />
number of deaths<br />
that were avoidable<br />
2<br />
0<br />
A M J J A S O N D J F M A M J J A S O N D J F M<br />
2011 2012 2013<br />
2<br />
Deaths<br />
Deaths per 1,000 admissions<br />
1<br />
0<br />
MEASURE:<br />
number of ALTEs<br />
and those<br />
that were preventable<br />
M A M J J A S O N D J F M<br />
No of Cardiac Arrests (ex PIC)<br />
No of Respiratory Arrests<br />
How have we done?<br />
During 2012/13 there have been no preventable<br />
acute life-threatening events (ALTEs), cardiac<br />
arrests or respiratory arrests. We have therefore<br />
reached our goal this year.<br />
No of Cardiac Arrests (PICU)<br />
No of ALTEs<br />
What are we doing to improve?<br />
We will continue to review each event to identify<br />
any learning that could prevent or help predict<br />
events in the future.<br />
We are developing a pre-transfer checklist for<br />
Extracorporeal Life Support (ECLS) to ensure all<br />
monitoring functioning is checked.<br />
How have we done?<br />
There were more deaths in 2012/13 than in the<br />
previous year but the number of deaths per 1,000<br />
admissions has remained at a very similar level,<br />
which suggests this reflects the increased number<br />
of patients that we treated. We also, however, look<br />
at a wide range of other information, including<br />
details of every individual death to identify any care<br />
failings that may have contributed to the death.<br />
Our reviews have found that no deaths during<br />
2012/13 were avoidable.<br />
What are we doing to improve?<br />
We will continue to monitor mortality rates in<br />
a number of different ways to ensure that any<br />
concerns are identified and that we learn from<br />
every death in case there was anything we could<br />
have done differently.<br />
In 2013/14 we will also commission independent<br />
reviews of our mortality review processes to ensure<br />
they are of the highest quality and to identify any<br />
ways that they can be improved.<br />
More information about the way we review mortality<br />
can be found at page 131.<br />
112 113
114 115<br />
Providing the Safest Possible Care: WHO Safe Surgery Checklists<br />
Research by the World Health Organisation (WHO)<br />
has confirmed that the use of the WHO Safe<br />
Surgery Checklist significantly reduces surgical<br />
morbidity and mortality. The checklist should be<br />
completed at three stages of surgery.<br />
Figure 25: Overall WHO Checklist Compliance: March 2011 - January 2013<br />
MEASURE:<br />
rate of completion of WHO<br />
checklist in eligible<br />
cases at each stage<br />
100%<br />
90%<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
How have we done?<br />
In September 2012 our theatres department<br />
implemented an e-checklist to improve compliance<br />
and safety by making completion of all fields a<br />
mandatory requirement of the system. Since then<br />
overall compliance has been consistently high.<br />
We will continue to monitor completion of the<br />
checklist but if compliance continues to be high, we<br />
will not report on this in our next Quality Account.<br />
0%<br />
GOAL:<br />
100% completion<br />
of WHO<br />
checklist in<br />
every<br />
eligible case<br />
M A M J J A S O N D J F M A M J J A S O N D J F M<br />
2011 2012 2013<br />
New Priorities for 2013/14:<br />
Extravasation<br />
Why is this a priority?<br />
When medicine is given into a vein, it can leak into<br />
and damage the surrounding tissue and cause a<br />
potentially serious injury. This can be a particular<br />
problem for children.<br />
What have we been doing?<br />
We have developed a Nursing Care Quality<br />
Indicator (NCQI) for cannula care which focuses<br />
on accurate observations, dressing changes and<br />
observations of early signs of an injury. We are<br />
also reviewing medication involved in extravasation<br />
incidents, to identify whether there are specific<br />
associations between the medication used and the<br />
likelihood of injury.<br />
Goal<br />
Reduce the episodes of harm from extravasation<br />
injuries by 25% year on year.<br />
Measure<br />
We will use a new process: SCAN (Safe Children<br />
Audit – No harm) to monitor the number of<br />
extravasation injuries per month.<br />
Sepsis Care<br />
Why is this a priority?<br />
The rate of mortality from Septic Shock in children<br />
is approximately 10%. Survival is significantly<br />
increased if antibiotics are given within an hour<br />
of diagnosis (as well as other treatment such as<br />
intra-venous fluids). At BCH we treat many patients<br />
who are at high risk of sepsis, such as oncology<br />
patients or those who are immuno-compromised.<br />
Our complex patients sometimes need unusual<br />
antibiotics. Sepsis can be difficult to detect so it’s<br />
essential we act quickly as soon as it is detected.<br />
What have we been doing?<br />
We have developed a Sepsis Care Pathway bundle<br />
which describes what must be done when a patient<br />
has sepsis. This has been piloted in the Emergency<br />
Department and is being implemented on PICU<br />
before complete roll-out to other areas in 2013/14.<br />
Goal<br />
All patients needing antibiotics as defined by the<br />
care pathway should receive them within 1 hour of<br />
prescription.<br />
Measure<br />
100% compliance with Sepsis Care Pathway<br />
monitored by way of audit.<br />
Friends & Family Test<br />
BACK TO CONTENTS PAGE<br />
Why is this a priority?<br />
A helpful way for any organisation to<br />
measure what the users of their services<br />
think of them is to ask them whether they would<br />
promote them to their friends or family.<br />
What have we been doing?<br />
Last year our commissioners asked us to ask<br />
this question of all adults within 18-24 hours of<br />
discharge. As all of our patients are under 18, it was<br />
important to us to make sure that their views are<br />
recorded too. So with the help of a group of young<br />
people we developed a similar more meaningful<br />
question for young people and put this to children<br />
and young people from the age of 10. We have<br />
also developed a smart phone app, which people<br />
can use to give us their feedback.<br />
Goal<br />
Improvement on the first quartile score.<br />
Measure<br />
Number of promoters minus the number of<br />
detractors.
116 117<br />
Statements of assurance on the<br />
quality of our services<br />
Review of Services<br />
During 2012/13 <strong>Birmingham</strong> Children’s <strong>Hospital</strong><br />
NHS Foundation Trust provided and/or subcontracted<br />
37 NHS services.<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust has reviewed all the data available to them<br />
on the quality of care in all of these NHS services.<br />
The income generated by the NHS services<br />
reviewed in 2012/13 represents 100 per cent of the<br />
total income generated from the provision of NHS<br />
services by <strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS<br />
Foundation Trust for 2012/13.<br />
On a regular basis, the Board reviews the<br />
following data which enables a comprehensive<br />
understanding of the three dimensions of quality<br />
– patient safety, clinical effectiveness and patient<br />
experience across every service provided by the<br />
Trust:<br />
Quality Report – this report includes details of the<br />
following:<br />
l Major clinical risks<br />
l Incident analysis<br />
l Mortality<br />
l Serious Incidents<br />
l Emergency clinical events<br />
l Never Events<br />
l Performance against Safety Strategy objectives<br />
l Patient Feedback<br />
l Quality walkabouts<br />
l Formal complaints<br />
l PALS concerns<br />
l Surveys<br />
Resources Report – in addition to financial<br />
performance this report includes the following:<br />
l Activity<br />
l Performance against our objectives relating to<br />
access to our services<br />
l Workforce indicators including:<br />
Rates of appraisals<br />
Mandatory training attendance<br />
Sickness rates and analysis<br />
Turnover<br />
Use of temporary staff<br />
Consideration of these reports together provides<br />
an overview of areas in the Trust where there<br />
might be concerns about the quality of care.<br />
Members of the Board, senior hospital staff,<br />
Governors and members of the Young People’s<br />
Advisory Group undertake regular Quality<br />
Walkabouts to the wards, where the focus is on<br />
either safety or patient experience.<br />
The walkabout involves ward observations and<br />
discussions with members of the ward multidisciplinary<br />
teams, patients and families to<br />
identify any safety or patient experience issues<br />
or concerns. The outcome of the walkabout is fed<br />
back to the ward staff with a requirement to take<br />
action where improvements are necessary.<br />
The Clinical Risk and Quality Assurance<br />
Committee has delegated responsibility from the<br />
Board for reviewing risks to safety and quality and<br />
identifying and monitoring actions to address these<br />
risks and improve quality.<br />
This Committee reports to the Quality Committee<br />
which is responsible for driving the Trust’s quality<br />
strategy, bringing the three elements of quality<br />
together, allowing integrated reporting to the Board<br />
of Directors.<br />
In 2010/11 we developed a Safety Dashboard,<br />
which acts as an early warning system. It allows an<br />
aggregated comparison of safety metrics against<br />
each ward and department and incorporates a<br />
series of defined ‘triggers’ which, in combination,<br />
may indicate problems with safety or quality in a<br />
specific area.<br />
The dashboard approach allows us to really<br />
focus on the areas where potential for harm is<br />
the highest. Whenever the dashboard identifies<br />
a potential concern a more detailed analysis<br />
is provided for the area in question and this is<br />
considered in depth at the Clinical Risk and Quality<br />
Assurance Committee.<br />
Participation in Clinical Audit and<br />
National Confidential Enquiries<br />
During 2012/13, 15 national clinical audits and<br />
one national confidential enquiry covered NHS<br />
services that <strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS<br />
Foundation Trust provides.<br />
During 2012/13 <strong>Birmingham</strong> Children’s <strong>Hospital</strong><br />
NHS Foundation Trust participated in 100%<br />
of national clinical audits and 100% national<br />
confidential enquiries of the national clinical audits<br />
and national confidential enquiries that it was<br />
eligible to participate in.<br />
BACK TO CONTENTS PAGE<br />
Table 28: National Clinical Audits and National Confidential Enquiries 2012/13 –<br />
eligibility, relevance, participation and percentage cases submitted<br />
Audit<br />
The national clinical audits and national<br />
confidential enquiries that the Trust was eligible to<br />
participate in during 2012/13 are as follows: (see<br />
table below).<br />
The national clinical audits and national<br />
confidential enquiries that <strong>Birmingham</strong> Children’s<br />
<strong>Hospital</strong> NHS Foundation Trust participated in, and<br />
for which data collection was completed during<br />
2012/13, are listed below alongside the number<br />
of cases submitted to each audit or enquiry as<br />
a percentage of the number of registered cases<br />
required by the terms of that audit or enquiry.<br />
Relevant Participation % Cases<br />
Paediatric asthma (British Thoracic Society) Yes Yes 95%<br />
Childhood epilepsy (RCPH National Childhood Epilepsy Audit) Yes Yes 100%<br />
Fever in children (CEM) Yes Yes 100%<br />
Paediatric intensive care (PICANet) Yes Yes Ongoing<br />
Paediatric cardiac surgery (NICOR Congenital Heart Disease Audit) Yes Yes 100%<br />
Diabetes (RCPH National Paediatric Diabetes Audit) Yes Yes 100%<br />
Potential donor audit (NHS Blood & Transplant) Yes Yes 100%<br />
Ulcerative colitis & Crohn’s disease (UK IBD Audit) Yes Yes 100%<br />
Cardiac arrhythmia (Cardiac Rhythm Management Audit) Yes Yes 100%<br />
Renal replacement therapy (Renal Registry) Yes Yes 100%<br />
Renal transplantation (NHSBT UK Transplant Registry) Yes Yes 100%<br />
Severe trauma (Trauma Audit & Research Network) Yes Yes 100%<br />
Bedside transfusion (National Comparative Audit of Blood Transfusion) Yes Yes 100%<br />
National review of Asthma Deaths (NRAD) Yes Yes 100%<br />
Maternal, infant and newborn programme (MBRRACE-UK)* Yes Yes 100%<br />
Mental Health programme: National Confidential Inquiry into Suicide Yes Yes 100%<br />
and Homicide for people with Mental Illness (NCISH)
118 119<br />
BACK TO CONTENTS PAGE<br />
The reports of 25 national clinical audits were<br />
reviewed by the Trust in 2012/13 and the Trust<br />
intends to take the following actions to improve the<br />
quality of healthcare provided:<br />
The results of 25 local clinical audits were<br />
reviewed by the Trust in 2012/13 and the Trust<br />
intends to take the following actions to improve the<br />
quality of healthcare provided:<br />
BTS Paediatric Asthma Audit (2012)<br />
l The use of the Asthma/Wheeze care pathway will be audited.<br />
l Patients admitted with severe/life threatening exacerbation of asthma will now have a<br />
follow up appointment booked following discharge.<br />
l Feedback will be given to the BTS regarding the use of peak flow and length of stay and its<br />
use in the national audit.<br />
Paediatric cardiac surgery (NICOR Congenital Heart Disease Audit) (2012)<br />
l Continue to liaise with Heart Suite suppliers to rectify the misplacement of co-morbid data<br />
and the placing of more than one code in a diagnostic or procedure field.<br />
l Regularly export the BCH data from the Congenital Database to review the procedures<br />
analysis against the algorithm and locally held data (reverse validation).<br />
l All therapeutic implantable devices and electrophysiological procedures in patients with<br />
congenital heart disease will now be submitted to congenital CCAD.<br />
Severe trauma (Trauma Audit & Research Network) (2012)<br />
l A Working Group is reviewing rehabilitation services including patient journeys.<br />
l Collate data for the region, comparing key metrics between each Major Trauma Centre and<br />
Trauma Unit to inform the ongoing development of trauma networks.<br />
Diabetes(2012)<br />
l The diabetes PREM questionnaire has been distributed in the diabetes clinics.<br />
Tissue Viability - Annual Audit of Pressure Ulcers<br />
The tissue viability assessment tool and wound assessment paperwork will be united into a skin<br />
care bundle.<br />
Burns Ward - Assessment and Referral of Burns in ED<br />
More education is planned for staff regarding referral guidelines and the level of detail required<br />
during assessment.<br />
Emergency Department - Left before treatment / Triage<br />
l Regular triage training for staff to be arranged.<br />
l Clarification of police role to be highlighted to all staff.<br />
l New doctors to be made aware of the Left Before Triage guideline as part of their<br />
induction training.<br />
Palliative Care - Clinical audit on advanced care plan for management of cardiorespiratory<br />
arrest in children and young person with advanced malignancy<br />
Ensure all staff are aware of the importance of early palliative discussions and are aware of and<br />
are using the Palliative Care Toolkits.<br />
Ophthalmology - An innovative approach to paediatric fundus photography<br />
Continue to use this method as it has been proven successful. Audit results to be published in<br />
Ophthalmology Journal 2013.<br />
Pain Management (College of Emergency Medicine 2012)<br />
l Pain set as a priority for the Emergency Department.<br />
l Re-evaluation of scores has improved since the implementation of a reminder stamp<br />
at triage.<br />
Audiology - Bone anchored hearing aids (BAHA) in very young children<br />
The decision to implant a BAHA in children between the ages of three and five years<br />
will continue to be made on a case by case basis with the inclusion of the family and<br />
multidisciplinary team.<br />
Neurology - Guillain Barre syndrome (GBS)<br />
Ensure the departmental guidelines are up to date and accessible. MRI scan to be added to the<br />
list of investigations required for patients with GBS.
Participation in Clinical Research<br />
The number of patients receiving NHS services<br />
provided by <strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS<br />
Foundation Trust that were recruited during that<br />
period to participate in research by a research<br />
ethics committee was 2,863.<br />
This demonstrates our continued improvement<br />
in this area over the last four years as we work<br />
towards our aim that every child and young person<br />
treated at the hospital is either offered participation<br />
in a research project or is aware that research is<br />
a major driver to our desire to deliver the best and<br />
safest clinical care in the country.<br />
Figure 26: Numbers of patients recruited to<br />
participate in research 2009/10 - 2012/13<br />
1797<br />
2079<br />
2573<br />
2863<br />
A good way of finding out how well we are doing<br />
on clinical research is to monitor the number of<br />
peer reviewed research publications - excluding<br />
abstracts and letters - that we deliver each year.<br />
When a research publication is reviewed by other<br />
professionals, or ‘peers’, this ensures that it is of a<br />
high enough standard to be used to help develop<br />
treatments for patients. Another important indicator<br />
of research quality is the impact factor of the<br />
journals in which the research is published, which<br />
reflects the number of times the journal is cited by<br />
other researchers and the number of citations of<br />
particular publications over a period of time.<br />
Figure 27: Peer Reviewed Publications per<br />
year 2008/09 - 2012/13<br />
141<br />
178<br />
225<br />
271<br />
218<br />
BACK TO CONTENTS PAGE<br />
Table 29: Schemes agreed for Quality Improvement and Innovation 2012/13<br />
CQUIN Goal Name WM PCT Cluster WMSCT Total End of year<br />
Goal Weight Value Goal Weight Value Value Performance<br />
Safety Thermometer - National 1 10% £179,659 1 5% £92,320 £271,979 Targets met<br />
Safety Thermometer - 2 10% £179,659 7 5% £92,320 £271,979 Targets met<br />
Paediatric Specific<br />
Friends & Family Test - 3A 4% £71,863 8a 1% £23,080 £94,944 Targets met<br />
Regional<br />
Friends & Family Test - 3B 4% 71,863 8b 1% £23,080 £94,944 Targets met<br />
Board Minutes<br />
Friends & Family Test - 3C 4% £71,863 8c 1% £23,080 £94,944 Targets met<br />
Weekly Reporting<br />
Friends & Family Test - 3D 4% £71,863 8d 1% £23,080 £94,944 Targets met<br />
Performance Improvement<br />
Net Promoter - 4 16% £287,454 9 5% £92,320 £379,774 Targets met<br />
Paediatric Specific<br />
Healthy Lifestyles - Smoking 5A 8% £143,727 £143,727 Targets met<br />
Healthy Lifestyles - Alcohol 5B 6% £114,981 £114,981 Targets met<br />
2009/10 2010/11 2011/12 2012/13 2008/09 2009/10 2010/11 2011/12 2012/13<br />
One of our strategic objectives is to strengthen<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong>’s position as a<br />
provider of specialised and highly specialised<br />
services, so that we become the leading provider<br />
of Children’s Healthcare in the UK. To help us<br />
achieve this, we are implementing a Research &<br />
Development Strategy towards becoming a leader<br />
in paediatric clinical research.<br />
Clinical research is important as it helps us to<br />
understand conditions and improve and discover<br />
new treatments, resulting in improved quality of<br />
care for patients.<br />
Use of the CQUIN Framework<br />
A proportion of <strong>Birmingham</strong> Children’s <strong>Hospital</strong><br />
NHS Foundation Trust’s income in 2012/13 was<br />
conditional upon achieving quality improvement<br />
and innovation goals agreed between <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong> NHS Foundation Trust and<br />
any person or body they entered into a contract,<br />
agreement or arrangement with for the provision<br />
of NHS services, through the Commissioning<br />
for Quality and Innovation (CQUIN) payment<br />
framework.<br />
The exception to this is the Quality Improvement<br />
Development Innovation Scheme (QIDIS) used by<br />
the National Specialised Commissioning Team to<br />
support Trusts to improve the quality of care and<br />
clinical outcomes for nationally designated services,<br />
replacing CQUIN arrangements for those services.<br />
Further details of the agreed goals for 2012/13<br />
and for the following 12 month period are available<br />
online at: https://commissioning.supply2health.nhs.<br />
uk/eContracts/Documents/cquin-guidance.pdf<br />
Healthy Lifestyles - 5C 2% £28,745 £28,745 Targets met<br />
Making Every Contact Count<br />
CAMHS QNCC 6 16% £287,454 £287,454 Targets met<br />
Antimicrobial Stewardship 7 16% £287,454 £287,454 Targets met<br />
Implementation of clinical 2 10% £184,641 £184,641 Targets met<br />
dashboards for specialised<br />
services<br />
(PIC) To minimise the number 3 10% £184,641 £184,641 Targets met<br />
of patients undergoing<br />
unplanned extubation<br />
CAMHS Tier 4: Education, 4 5% £92,320 £92,320 Targets met<br />
training and meaningful activity<br />
CAMHS Tier4: Patient 5 5% £92,320 £92,320 Targets met<br />
Involvement in Recruitment<br />
CAMHS Tier4: Feasibility study 6 5% £92,320 £92,320 Targets met<br />
for conversion to single<br />
room accommodation<br />
Local CQUIN: Enhancing HDU 10 25% £461,602 £461,602 Targets met<br />
Local CQUIN: CNS Pathway 11 20% £369,282 £369,282 Targets met<br />
Planned CQUIN income 100% £1,796,585 100% £1,846,409 £3,642,994<br />
Other Commissioners £276,508<br />
Total Planned CQUIN income £3,919,502<br />
120 121
122 123<br />
BACK TO CONTENTS PAGE<br />
The monetary total for the amount of income<br />
conditional upon achieving CQUIN goals in 2012/13<br />
and the monetary total for the associated payment<br />
in 2011/12 is detailed below:<br />
Table 30: CQUIN income data 2011/12 and 2012/13<br />
2011/12 2012/13<br />
Percentage of income conditional upon achieving goals (total value £3.92m) 1.5% 2.5%<br />
Income not achieved 0 0<br />
Table 31: Schemes agreed for Quality Improvement Development Innovation Scheme<br />
(QIDIS) 2012/13<br />
Service Nature of Scheme Contract QIDIS QIDIS<br />
Value Value (of 2.5%)<br />
Alstrom Syndrome Dashboard Scheme 10% / PPE Scheme 20% / 109,842 824 30%<br />
No Strategic Schemes<br />
Bardet Biedl Syndrome Dashboard Scheme 10% / PPE Scheme 20% / 193,017 4,826 100%<br />
(Children) Strategic Schemes 70%<br />
Complex Childhood Dashboard Scheme 10% / PPE Scheme 20% / 712,399 17,810 100%<br />
Osteogenesis Imperfecta Strategic Schemes 70%<br />
Craniofacial Surgery For Dashboard Scheme 10% / PPE Scheme 20% / 2,030,299 50,757 100%<br />
Congenital Conditions Strategic Schemes 70%<br />
Epidermolysis Bullosa Dashboard Scheme 10% / PPE Scheme 20% / 559,367 13,984 100%<br />
Strategic Schemes 70%<br />
ECMO For Reversible No schemes as cost per case and not eligible 273,845 - 0%<br />
Respiratory Failure (Children) for QIDIS payments<br />
Liver Transplantation (Children) Dashboard Scheme 10% / PPE Scheme 20% / 3,740,250 93,506 100%<br />
Strategic Schemes 70%<br />
Lysosomal Storage Disorders Dashboard Scheme 10% / PPE Scheme 20% / 428,579 10,714 100%<br />
(Children) Strategic Schemes 70%<br />
Retinoblastoma Dashboard Scheme 10% / no PPE Scheme / 1,207,673 13,586 45%<br />
Strategic Schemes 35%<br />
Small Bowel Transplantation Dashboard Scheme 10% / no PPE Scheme / 1,215,533 3,039 10%<br />
(Children)<br />
no Strategic Scheme<br />
Specialist Paediatric Liver Dashboard Scheme 10% / PPE Scheme 20% / 2,845,056 71,126 100%<br />
Disease Strategic Schemes 70%<br />
Wolfram Syndrome Dashboard Scheme 10% / PPE Scheme 20% / 160,048 1,200 30%<br />
no Strategic Scheme<br />
Total 13,475,908 281,372 84%<br />
Liver Transplantation Income deferred to 2013/14 to cover costs -54,000<br />
(Children)<br />
not yet incurred<br />
Net Total 227,372<br />
Care Quality Commission<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust is required to register with the Care Quality<br />
Commission (CQC) and its current registration<br />
status is:<br />
Registered to carry out the following legally<br />
regulated services:<br />
l Transport services, triage and medical advice<br />
provided remotely<br />
l Treatment of disease, disorder or injury<br />
l Assessment or medical treatment for persons<br />
detained under the Mental Health Act 1983<br />
l Surgical procedures<br />
l Diagnostic and screening procedures<br />
l Management of supply of blood and blood<br />
derived products<br />
The Care Quality Commission has not taken<br />
enforcement action against <strong>Birmingham</strong> Children’s<br />
<strong>Hospital</strong> NHS Foundation Trust during 2012/13.<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust has not participated in special reviews or<br />
investigations by the Care Quality Commission<br />
during 2012/13.<br />
On 6 November 2012 the CQC undertook a<br />
routine, unannounced inspection of CAMHS at our<br />
Parkview Clinic, to assess compliance with the<br />
following standards:<br />
04: Care and welfare of people who use services<br />
06: Cooperating with other providers<br />
07: Safeguarding people who use services from<br />
abuse<br />
13: Staffing<br />
The CQC found that the services at Parkview met<br />
all these standards.<br />
On 21 November 2012 the CQC undertook a<br />
routine, unannounced inspection of the Trust’s<br />
services at our main site at Steelhouse Lane, to<br />
assess compliance with the following standards:<br />
04: Care and welfare of people who use services<br />
09: Management of medicines<br />
11: Safety, availability and suitability of equipment<br />
14: Supporting workers<br />
The CQC found that the services at Steelhouse<br />
Lane were compliant with the first three of these<br />
standards, but found that action was needed to<br />
ensure compliance with standard 14: Supporting<br />
workers. The evidence CQC collected in theatres<br />
identified some minor concerns about the risks<br />
relating to how staff were supported in this area.<br />
CQC issued a compliance action to ensure that<br />
improvements to support staff are made. We have<br />
taken the following actions to ensure we are now<br />
compliant with this standard:<br />
l Recruited to vacant posts in theatres<br />
l Changed and improved the way we were<br />
implementing our Integrated Theatre Recovery<br />
Team Project<br />
l Strengthened, developed, and added to<br />
arrangements for supporting and engaging with<br />
staff in theatres.<br />
Data Quality<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust submitted records during 2012/13 to the<br />
Secondary Uses service for inclusion in the<br />
<strong>Hospital</strong> Episode Statistics which are included in<br />
the latest published data.<br />
The percentage of records in the published data<br />
which included the patient’s valid NHS Number<br />
was:<br />
98.6% for admitted patient care<br />
99.5% for outpatient care and<br />
98.3% for accident and emergency care<br />
The percentage of records in the published<br />
data which included the patient’s valid General<br />
Practitioner Registration Code was:<br />
100% for admitted patient care<br />
100% for outpatient care and<br />
100% for accident and emergency care<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust’s Information Governance Assessment Report<br />
overall score for 2012/13 was 82% and was graded<br />
green (satisfactory).
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust will be taking the following actions to improve<br />
data quality:<br />
l Having made significant improvements against<br />
the data quality items published centrally we are<br />
now progressing to developing further local data<br />
quality indicators. These will include looking at<br />
timeliness of data capture.<br />
l We have expanded our Data Quality Group and<br />
will use this forum to push forward the data<br />
quality agenda.<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust was subject to the Payment by Results clinical<br />
coding audit during the reporting period by the Audit<br />
Commission and the error rates reported in the<br />
latest published audit for that period for diagnoses,<br />
treatment and investigation coding (clinical coding)<br />
were:<br />
Diagnosis:<br />
N/A<br />
(not part of the 2012/13 audit)<br />
Treatment (procedure): 10.3%<br />
Investigations: 10.4%<br />
150 cases were reviewed within the sample.<br />
Note: the results should not be extrapolated further<br />
than the actual sample audited.<br />
Core National Indicators<br />
Due to the time it takes central bodies to collate and<br />
publish some of the data, sometimes comparative<br />
figures are not available at all (N/A). It should also<br />
be appreciated that some of the ‘Highest’ and<br />
‘Lowest’ performing Trusts on some of the data<br />
may not be directly comparable to <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong>.<br />
There are several core national indicators that are<br />
not applicable to <strong>Birmingham</strong> Children’s <strong>Hospital</strong>,<br />
because they relate to adult patients/services<br />
only, or due to the specialist nature of many of our<br />
services. These indicators include:<br />
l Summary <strong>Hospital</strong>-level Mortality Indicator<br />
(SHMI) – though we do provide details of a<br />
different mortality indicator at page 113 which<br />
compares our mortality rates with those of a<br />
range of other children’s services.<br />
l The percentage of patient deaths with palliative<br />
care.<br />
l The percentage of patients on Care Programme<br />
Approach who were followed up within 7 days<br />
after discharge from psychiatric in-patient care.<br />
l The percentage of admissions to acute wards for<br />
which the Crisis Resolution Home Treatment<br />
Team acted as a gatekeeper during the reporting<br />
period.<br />
l Patient reported outcome measures scores.<br />
l The Trust’s responsiveness to the personal<br />
needs of its patients.<br />
l Patient experience of community mental health<br />
services.<br />
l The percentage of patients who were admitted<br />
to hospital and who were risk assessed for<br />
venous thromboembolism.<br />
<strong>Hospital</strong> Readmissions: The percentage of patients readmitted to <strong>Birmingham</strong> Children’s<br />
<strong>Hospital</strong> within 28 days of being discharged in 2012/13<br />
AGE 2011/12 2012/13 National Average Highest Trust Lowest Trust<br />
0 to 14<br />
15 or over<br />
N/A<br />
AGE 2010/11 2011/12 2012/13 National Average Highest Trust Lowest Trust<br />
2010/11<br />
0 - 15 11.14% 10.0% 9.97% 10.15%<br />
16 or over 9.9% 11.0% 7.7% 11.42%<br />
N/A<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust considers that these percentages are as<br />
described for the following reasons:<br />
Between 2010/11 and 2012/13 we undertook a<br />
monthly audit including a detailed review of every<br />
emergency readmission and reported this to our<br />
commissioners. There have been no concerns with<br />
the discharge decision in any of the cases.<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust intends to take the following actions to<br />
improve these percentages, and so the quality of its<br />
services, by:<br />
We will continue to regularly monitor emergency<br />
readmissions to identify any concerns.<br />
Staff Survey: Percentage of staff who would<br />
recommend the Trust to family or friends<br />
2011 2012 2012 Average Acute Trust<br />
85% 83% 87%<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust considers that this percentage is as described<br />
for the following reasons:<br />
We acknowledge that the result is slightly below<br />
the national average and that this has remained<br />
consistent over the last few years.<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust intends to take the following actions to<br />
improve this percentage, and so the quality of its<br />
services, by:<br />
We are taking steps to improve the way we support<br />
and engage with staff and act on their views and<br />
concerns. Central to these plans in 2013/14 is<br />
our approach to responding to the Francis report.<br />
From March 2013 we have been holding listening<br />
events with staff, which over 250 staff members<br />
have attended so far. Staff at these events are<br />
encouraged to be completely open, demonstrating<br />
their commitment to our values – courage, trust,<br />
respect, commitment and compassion. The<br />
listening events will culminate in a week of events<br />
in September when we will focus on actions to<br />
address the issues that have been raised.<br />
Our Quality Walkabouts now also include a focus<br />
on staff health and wellbeing.<br />
We have put in place a process by which<br />
anonymous email contact can be made direct to the<br />
Chief Executive Officer to raise any concerns or to<br />
provide views. We have also put in place processes<br />
124 125<br />
BACK TO CONTENTS PAGE<br />
to ensure we listen to and act upon the concerns<br />
of specific staff groups, for example, our Trainee<br />
Advice & Liaison Service (TALS) and Safety Hotline<br />
for junior doctors.<br />
During 2013/14 we will be regularly undertaking<br />
a staff poll, asking them whether they would<br />
recommend the Trust as a place to be treated to<br />
friends and family, so that we can monitor this<br />
more regularly during the year and act on any poor<br />
results more quickly. The percentage of positive<br />
responses to this question has risen during the<br />
early part of the year to 98%.<br />
C.difficile: rate per 100,000 bed days of cases<br />
of C.difficile infection reported within the Trust<br />
amongst patients aged 2 or over<br />
2011/12 2011/12 2011/12 2011/12<br />
National Highest Lowest<br />
Average Trust Trust<br />
1.9 21.8 50.9 0.0<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust considers that this rate is as described for the<br />
following reasons: There was one case of C.Difficile<br />
at the Trust in 2011/12.<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust intends to take/has taken the following<br />
actions to improve this rate, and so the quality of its<br />
services, by: Actions we are taking to minimise the<br />
risk of C.Difficile are described at page 108.<br />
Patient Safety Incidents: the number and rate<br />
of patient safety incidents reported, and the<br />
number and percentage of such patient safety<br />
incidents that resulted in severe harm or death<br />
This year is the first time that this indicator has<br />
been required to be included within the Quality<br />
Report alongside comparative data provided,<br />
where possible, from the Health and Social Care<br />
Information Centre. The National Reporting and<br />
Learning Service (NRLS) was established in<br />
2003. The system enables patient safety incident<br />
reports to be submitted to a national database on a<br />
voluntary basis designed to promote learning.<br />
It is mandatory for NHS trusts in England to<br />
report all serious patient safety incidents to the<br />
Care Quality Commission as part of the Care<br />
Quality Commission registration process. To avoid<br />
duplication of reporting, all incidents resulting in<br />
death or severe harm should be reported to the<br />
NRLS who then report them to the Care Quality<br />
Commission. Although it is not mandatory, it is<br />
common practice for NHS Trusts to reports patient<br />
safety incidents under the NRLS’s voluntary<br />
arrangements.
126 127<br />
As there is not a nationally established and<br />
regulated approach to reporting and categorising<br />
patient safety incidents, different trusts may choose<br />
to apply different approaches and guidance to<br />
reporting, categorisation and validation of patient<br />
safety incidents. The approach taken to determine<br />
the classification of each incident, such as those<br />
‘resulting in severe harm or death’, will often rely on<br />
clinical judgement. This judgement may, acceptably,<br />
Number of patient safety<br />
incidents (acute specialist)<br />
Rate of patient safety<br />
incidents per 100 patient<br />
admissions (acute specialist)<br />
Percentage of such patient<br />
safety incidents that resulted<br />
in severe harm or death<br />
(small acute)<br />
differ between professionals. In addition, the<br />
classification of the impact of an incident may be<br />
subject to a potentially lengthy investigation which<br />
may result in the classification being changed. This<br />
change may not be reported externally and the data<br />
held by a trust may not be the same as that held by<br />
the NRLS. Therefore, it may be difficult to explain<br />
the differences between the data reported by the<br />
Trusts as this may not be comparable.<br />
Oct 2011-March 2012 Oct 2011-March 2012 Oct 2011-March 2012<br />
BCH Highest Trust Lowest Trust<br />
1,370 1,935 66<br />
7.77 12.03 3.36<br />
0.36% 2.36% 0.00%<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust considers that this number and/or rate is as<br />
described for the following reasons:<br />
Other information<br />
Linking our priorities to the priorities of the NHS<br />
QUALITY<br />
STRAND<br />
Effectiveness<br />
QUALITY DOMAIN<br />
(NHS OUTCOMES FRAMEWORK)<br />
Preventing people from dying<br />
prematurely<br />
Enhancing quality of life<br />
for people with<br />
long-term conditions<br />
Helping people to recover<br />
from episodes of ill health<br />
or following injury<br />
BACK TO CONTENTS PAGE<br />
BCH QUALITY<br />
INDICATOR<br />
Nursing Care Quality Indicators<br />
Asthma Care<br />
Health Promotion<br />
Implementing the Sepsis Care Bundle<br />
Food & nutrition<br />
Nursing Care Quality Indicators<br />
Asthma Care<br />
Health Promotion<br />
Food & nutrition<br />
Nursing Care Quality Indicators<br />
Health Promotion<br />
CAMH Service User satisfaction<br />
Implementing the Sepsis Care Bundle<br />
We are pleased to note the high number of reported<br />
incidents and the low percentage of these that<br />
resulted in severe harm or death compared with the<br />
national average, as this indicates an open safety<br />
culture.<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust intends to take/has taken the following actions<br />
to improve this number and/or rate, and so the<br />
quality of its services, by:<br />
Patient<br />
Experience<br />
Ensuring that people have<br />
a positive experience of care<br />
Food & nutrition<br />
Play & activities<br />
Emergency department transfers<br />
Tertiary inpatient referrals<br />
Cancelled operations<br />
Friends & Family Test<br />
l Actions we are taking to monitor and improve our<br />
safety culture are described on page 131.<br />
l We investigate and learn from every incident.<br />
l We take actions to address safety issues<br />
identified through safety monitoring and<br />
analysis.<br />
l Safety themes identified through incident<br />
analysis are addressed through safety targets<br />
as part of our Safety Strategy – for example,<br />
extravasation injuries and medication incidents.<br />
Safety<br />
Treating and caring for people<br />
in a safe environment;<br />
and protecting them<br />
from avoidable harm<br />
Pressure ulcers<br />
Reducing Healthcare Acquired Infections in PICU<br />
Reducing rates of C.Difficile<br />
Preventing MRSA<br />
Reducing MRSA<br />
Medication Incidents<br />
Acute life threatening events, Cardiac Arrests<br />
and Respiratory Arrests<br />
Zero avoidable deaths<br />
WHO Safe Surgery checklists<br />
Extravasation injuries
BACK TO CONTENTS PAGE<br />
Overview of Quality of Care<br />
Complaints<br />
We take all complaints about our services very<br />
seriously and ensure that the way we respond is<br />
tailored to the individual and that we answer all<br />
of their concerns. Our Chief Executive is involved<br />
in every response and writes personally to each<br />
individual. Responding to a complaint can include<br />
meetings with clinical staff and senior managers,<br />
including the Chief Executive.<br />
Formal complaints often originate in a concern<br />
raised with PALS (Patient Advice and Liaison<br />
Service) which supports families in obtaining the<br />
response they need in the best way for them. We<br />
encourage people to use our Formal Complaints<br />
service and PALS as, if something has gone wrong<br />
we want to know about it so we can try to put it<br />
right, learn from it and improve. This information,<br />
when combined with other quality information about<br />
our services, can also help us identify when there<br />
are other problems.<br />
Fortunately, compared to the numbers of patients<br />
we see every day, we receive very few formal<br />
complaints. Each one is considered in detail and<br />
incorporated into our Safety Dashboard and our<br />
Quality Report.<br />
Figure 28: Numbers of formal complaints per month/per 1,000 admissions<br />
(This data is governed by local definitions)<br />
15<br />
10<br />
5<br />
0<br />
J F M A M J J A S O N D J F M A M J J A S O N D J F M<br />
2011<br />
Complaints<br />
Complaints per 1000 Admissions<br />
2012<br />
2013<br />
As part of the formal complaints investigation<br />
process, we identify any areas in which the quality<br />
of the services could be improved, and make<br />
appropriate recommendations. These range from<br />
reminders to staff about proper practices and<br />
behaviour, to fundamental changes in practice and<br />
documentation. We regularly follow up on these<br />
recommendations to make sure action has been<br />
taken.<br />
As a result of these recommendations a number of<br />
changes have been made, including:<br />
l Radiology: An area has been identified where families can discuss issues privately.<br />
l Surgical <strong>Day</strong> Care: To avoid any discrepancy in recording weight and therefore incorrect<br />
calculation of medication, the same member of staff who checks a child’s weight now also<br />
writes the weight on the drug chart.<br />
l Communication processes between Radiology and Rheumatology secretaries about<br />
appointments have been improved.<br />
l All wards: The handover process has been improved to ensure speciality patients on outlying<br />
wards are more clearly identified.<br />
l All clinical areas: A new discharge form has been designed to prevent failure to follow-up.<br />
l The Breast-feeding training programme has been re-launched.<br />
l Learning Disabilities: increased awareness has been raised amongst staff about the<br />
importance of the Trust Learning Disabilities Passport and care pathways.<br />
l The experience of a family will be used as a learning example for doctors in training.<br />
l Heart Investigation Unit: A test results tracking process has been introduced.<br />
Figure 29: Pattern of complaints per top 5 categories, 2010/11 - 2012/13 admissions<br />
(This data is governed by local definitions)<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4<br />
2011<br />
2012<br />
2013<br />
Waiting, delays & cancellations<br />
Staff Attitude<br />
Quality of Treatment<br />
Communication<br />
Other<br />
In order to see whether there are any themes<br />
amongst the complaints we receive, we group the<br />
issues raised in each complaint into categories.<br />
The pattern of complaints received about the 5<br />
main categories is set out above.<br />
In January 2013 the Patient Association published<br />
a report: Complaint handling in NHS Trusts<br />
signed up to the CARE campaign, which is based<br />
on information about the complaint handling<br />
systems and processes of a random sample of<br />
trusts. <strong>Birmingham</strong> Children’s <strong>Hospital</strong> was one<br />
of the randomly selected trusts and is included<br />
anonymously within the report. The Patients<br />
Association wrote to us and gave us some<br />
positive feedback about what they have seen of<br />
our systems and processes, in particular they<br />
said: “<strong>Birmingham</strong> Children’s <strong>Hospital</strong> appears<br />
committed to being a learning organisation.<br />
An example of this is your unique approach of<br />
measuring complaints against Trust values within<br />
the Quality Report”.<br />
Incidents<br />
We have robust systems for managing incidents<br />
and in 2011/12 were awarded NHSLA level 3, the<br />
highest level for compliance with the NHS Litigation<br />
Authority Risk Management Standards. In 2012 we<br />
128 129<br />
carried out a ‘Lean’ process on our investigation<br />
management system to ensure it is as efficient<br />
as it can be. This means investigations can now<br />
be concluded more quickly, which is better for the<br />
patients and families involved and allows us to start<br />
implementing learning from the incident earlier than<br />
we previously could.<br />
In 2013 our Internal Auditors gave an opinion<br />
of ‘significant assurance’ about our incident<br />
management processes.<br />
We encourage all members of staff to report all<br />
incidents, errors and near misses so we can<br />
make improvements, work out what went wrong,<br />
identify themes and drive quality improvements in<br />
everything we do. We share learning from incidents<br />
through our Safety Circular, a staff publication<br />
which provides news on safety issues and changes<br />
made as a result of incidents and incident analysis.<br />
Our Quality Report - which is published on our<br />
website - also includes information about incidents,<br />
which any member of staff or the public can read.
BACK TO CONTENTS PAGE<br />
Some of the major changes we have made as<br />
a result of learning from incidents and incident<br />
analysis include:<br />
l Development of a sepsis care pathway.<br />
l Development of new techniques for weighing patients on PICU to allow us to manage their<br />
nutritional status more effectively.<br />
l New guidance documents to allow more effective checking of medication in theatres when it is<br />
prepared by anaesthetists.<br />
Patient Safety Incidents by Harm Category 2011/12 - 2012/13<br />
Year Total No Harm Minor, Non Moderate, Semi Severe, Severe Catastrophic,<br />
Incidents Permanent Harm Permanent Harm Permanent Harm Death<br />
2011/12 4198
BACK TO CONTENTS PAGE<br />
Figure 31: SMR Funnel Plot February 2013<br />
250<br />
200<br />
150<br />
Marker by<br />
TRUST NAME<br />
Color by<br />
Alert Level<br />
Amber<br />
Green<br />
Shape by<br />
Peer Flag<br />
Pre-selected Peer(s)<br />
Your Organisation<br />
What are people talking about? This Word Cloud<br />
demonstrates by their size the most frequently used<br />
words in all the patient feedback we received in<br />
2012/13. The larger the word, the more frequently it<br />
has been used.<br />
RRM<br />
100<br />
50<br />
0 20 40 60 80 100 120 140 160 180<br />
Number of Expected Deaths<br />
Patient Feedback<br />
Listening to what our children, young people and<br />
their families tell us about their experiences at BCH<br />
and their views about our services is vital in making<br />
sure we continue good practice, and make changes<br />
where improvements are needed.<br />
It is really important that we gather this feedback in<br />
lots of different ways so we can make sure we are<br />
taking account of everyone’s views. We call this<br />
our Patient Experience Toolbox, and we load all the<br />
information we obtain into our Patient Experience<br />
Database which helps us identify themes or areas<br />
that need closer attention. It also helps us make<br />
sure that we can let our staff know when we receive<br />
really good feedback.<br />
The toolbox includes patient surveys, quality<br />
walkabouts, patient stories, mystery shoppers,<br />
focus groups, feedback cards and direct feedback<br />
like letters and comments. Combining this<br />
with information about patient experience from<br />
other sources – such as PALS contacts and<br />
formal complaints - provides an overall picture<br />
of individual wards and departments and of the<br />
whole Trust. It also helps us see what we do well<br />
and identify areas for improvement. As a result of<br />
this work we have set new quality objectives and<br />
made service improvements in areas like food,<br />
play, communication, environment and patient<br />
information.<br />
As well as looking at what we need to improve,<br />
it is also important to look at what patients and<br />
their families tell us we do well. This provides vital<br />
learning about how we can improve other areas,<br />
and it is important to take this into account when<br />
we are thinking about changing something. Sharing<br />
positive feedback with staff about the work that they<br />
do also supports and motivates them to deliver the<br />
highest quality of care that they can.<br />
132 133
Examples of patient feedback<br />
Very long wait.<br />
None of the vending<br />
machines worked<br />
making the stay even<br />
more unbearable.<br />
Waiting times<br />
should be clearly<br />
published.<br />
I think that you<br />
need to make<br />
more rooms for<br />
people to get<br />
checked<br />
quicker.<br />
Friendly and helpful,<br />
answered all my<br />
questions even though I<br />
was nervous.<br />
Transfer on to theatre<br />
trolley in corridor slightly<br />
embarrassing even<br />
though staff did their best<br />
to maintain my dignity, not<br />
much space.<br />
Could not fault the<br />
whole stay, everyone<br />
so helpful, kind &<br />
friendly. We felt a<br />
little sad to leave.<br />
Patient Information<br />
Too many<br />
questions<br />
get asked on<br />
admission. We<br />
should get<br />
a day or two to<br />
settle in.<br />
Caring and<br />
understanding nature of<br />
the nurses was amazing.<br />
Very supportive. Cannot<br />
put into words what<br />
it meant to have this<br />
service so that we could<br />
be at home at Christmas.<br />
(<strong>Hospital</strong> @Home)<br />
Didn’t treat me<br />
ike a little kid.<br />
Explained to me so<br />
I understood and it<br />
gave me<br />
confidence.<br />
Your theatre<br />
environment<br />
is brilliant, less<br />
traumatic. You made<br />
us feel at ease<br />
and were always<br />
available to answer<br />
questions.<br />
The Family Health Information Centre provides a<br />
free and confidential health information service for<br />
our children, young people and their families, and<br />
support for staff in the production of quality patient<br />
information.<br />
In direct response to feedback from our patients<br />
and families - who told us they would like to access<br />
information without leaving the ward - we have<br />
looked at new ways of making sure they are able<br />
We have spent<br />
over £100 in car<br />
parking which<br />
has had a huge<br />
impact on our<br />
Christmas.<br />
Pain relief monitoring<br />
could be improved<br />
and planned better<br />
when coming to move<br />
a child around after<br />
operations for<br />
the first time.<br />
When I first came to<br />
Parkview I hated it. I missed<br />
my family and friends. When I<br />
left Parkview, I felt as if<br />
I was leaving behind my<br />
family. The staff are amazing.<br />
If it wasn’t for the<br />
staff at Parkview,<br />
I wouldn’t be<br />
alive today.<br />
To ensure better<br />
communication links<br />
were put into place between<br />
surgeons, specialists, social services<br />
and other services that the OT dept<br />
have to liaise with on a daily basis,<br />
that will allow a better<br />
and smoother<br />
transition between<br />
hospital and home.<br />
Thank you for the<br />
fantastic care and<br />
support we received<br />
from the whole<br />
cardiac team.....from<br />
housekeepers on<br />
the ward to surgeons<br />
in theatre were<br />
outstanding.<br />
An 8 year old girl<br />
commented during<br />
her EEG that she was<br />
happy and enjoying<br />
her test, she said ‘this<br />
test is good, I am not<br />
scared at all’.<br />
A big thank you to all the<br />
A&E staff on Thursday<br />
who looked after my<br />
daughter who was brought<br />
in wheezing. They were all<br />
very caring and she was<br />
constantly monitored by the<br />
team. They were very busy<br />
but still able to give her<br />
excellent care.<br />
Whenever my<br />
daughter was scared<br />
there was always<br />
someone that made<br />
her feel better.<br />
to access the information they need at the right<br />
time along their patient journey. In 2012/13 we<br />
piloted weekly drop-in health information sessions<br />
on wards and in the Parent Accommodation, and<br />
weekly health information and awareness sessions<br />
in the main Outpatients department. In 2013/14 we<br />
will continue to look for new ways to improve the<br />
information service to improve the quality of the<br />
patient experience.<br />
Performance against National Priorities<br />
Table 32: Performance against National priorities 2012/13<br />
134 135<br />
BACK TO CONTENTS PAGE<br />
National Priority Target Performance 2012/13<br />
C-Diff 3 cases or less per year - Target met – 1 case<br />
locally agreed threshold<br />
MRSA 2 cases or less per year - Target met – no cases<br />
locally agreed threshold<br />
MSSA Pre 48 hours Monitoring only (but reduced)<br />
Post 48 hours - 10% reduction<br />
Target not met<br />
E.Coli Pre 48 hours Monitoring only<br />
Post 48 hours<br />
Monitoring only<br />
All cancers; 31 day wait Surgery (94%) Target met<br />
for second or subsequent Anti cancer drug treatments (98%) Target met<br />
treatments Radiotherapy (94%) Target met<br />
All cancers: 62 day wait From GP referral to treatment (85%) Target met<br />
for first treatment From consultant screening service Target met<br />
referral (90%)<br />
18.3 weeks (as of April 2011) Referral to treatment waiting times - Target met<br />
non admitted (95th percentile)<br />
23 weeks (as of April 2011) Referral to treatment waiting times - Target met<br />
admitted (95th percentile)<br />
All cancers: 31 day wait from diagnosis to first treatment (96%) Target met<br />
All cancers: two week wait from referral to date first seen (93%) Target met<br />
Total time in A&E<br />
95% of patients time taken from arrival to Target met<br />
discharge/admission < 4 hours.<br />
18 weeks 90% admitted patients at the end of Target met<br />
each month<br />
95% non admitted patients at the end of<br />
each month<br />
Ambulance Turnaround Number over 60 minutes Monitoring only<br />
% over 60 minutes Monitoring only<br />
Number over 30 minutes<br />
Monitoring only<br />
% over 30 minutes Monitoring only<br />
Operations cancelled on the 95% of those patients we Target met<br />
those not admitted within cancel within 28 days<br />
28 days<br />
Single Sex Accommodation 0 breaches Target not met – 2 breaches<br />
Breaches<br />
Emergency Readmissions Emergency readmissions within 28 days Monitoring only<br />
of discharge from hospital as a % of all Age 0-15: 9.97%<br />
relevant admissions. Age 16+: 7.7%
Targets Not Met<br />
Single Sex Accommodation Breaches<br />
During 2012/13 we reported two single sex<br />
accommodation breaches. In both cases there<br />
was insufficient space for a short period on our<br />
Teenage Cancer Trust ward. We discussed this<br />
with the young people involved and offered them<br />
single sex accommodation on another ward. Both<br />
young people opted to stay on the ward as their<br />
preference was to remain with other people of their<br />
age group.<br />
As part of the planned redesign of our Oncology<br />
Unit we will incorporate more single rooms which<br />
will mean this is less likely to happen.<br />
We continue to ask all our children and young<br />
people when they are admitted whether they would<br />
prefer single sex accommodation, and in 2012/13<br />
we were able to meet everyone’s wishes except<br />
in the two cases described above. The feedback<br />
we have from the majority of children and young<br />
people is that their priority is to be treated with<br />
people of a similar age, rather than the same<br />
gender.<br />
Cancelled Operations<br />
Please see page 80 for details.<br />
MSSA<br />
Please see page 91 for details.<br />
Commissioners<br />
BACK TO CONTENTS PAGE<br />
Statements from stakeholders<br />
<strong>Birmingham</strong> South Central Clinical Commissioning<br />
Group (BSC CCG) as coordinating commissioner<br />
for <strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS<br />
Foundation Trust (BCH) welcomes the opportunity<br />
to provide this statement for their 2012/13 Quality<br />
Account.<br />
A draft copy of the Quality Account was received<br />
by BSC CCG on the 22nd April 2013 and the<br />
statement has been developed from the information<br />
presented to date. Feedback on the draft account<br />
has been received from <strong>Birmingham</strong> Cross City<br />
CCG, Solihull CCG and NHS England Area Team<br />
as the lead for specialised commissioning.<br />
We have reviewed the content of the Quality<br />
Account and confirm that this complies with the<br />
prescribed information, form and content as set out<br />
by Monitor and the Department of Health.<br />
This is a comprehensive report that clearly<br />
demonstrates progress within the Trust. It identifies<br />
where the organisation has done well, where<br />
further improvement is required and what actions<br />
are needed to achieve these goals. The Quality<br />
Account sets out the priorities for improving patient<br />
safety, patient experience and clinical effectiveness<br />
in 2013/14 across services provided by BCH.<br />
The information provided within this Account<br />
presents a balanced report of the quality of<br />
healthcare services BCH provides and is, to<br />
the best of our knowledge accurate and fairly<br />
interpreted. The range of services described and<br />
priorities for improvement are representative based<br />
on the information that is available to us. We agree<br />
with and support the priorities set for this year.<br />
in order to drive improvements in the quality of<br />
care. Further development and implementation<br />
of the feedback App and the Children and Young<br />
Person’s version of the Friends and Family Test are<br />
just two examples of initiatives designed to ensure<br />
that users of the service are listened to and issues<br />
addressed can be continually monitored and acted<br />
on.<br />
Cancelled Operations continues to be a challenge<br />
for the Trust and we will continue to work with and<br />
support BCH to review the effectiveness of the<br />
range of interventions currently being implemented<br />
to improve the current position. As part of this work<br />
BCH remain focused on the impact on children<br />
and families when operations are cancelled and<br />
improving the patient experience.<br />
The Quality Account reflects a number of the<br />
performance quality indicators which are monitored<br />
monthly along with areas for improvement at<br />
the CCG / Trust Clinical Quality Review Group<br />
mandated by the service contract. We are also<br />
invited to the Trust’s Clinical Risk and Assurance<br />
Committee and any Root Cause Analysis meetings<br />
following occurrence of serious incidents.<br />
We have made some specific comments to the<br />
Trust directly in relation to their plan. Namely, we<br />
would like further information regarding outcomes<br />
and levels of improvement they are working<br />
towards, the specific actions being taken to address<br />
capacity issues, further narrative and detail to<br />
support analysis of the mortality data, inclusion of<br />
an assurance statement on Equality and Diversity<br />
and Safeguarding and alignment of their priorities to<br />
the five domains of the NHS Outcomes Framework.<br />
BCH places significant emphasis on its safety<br />
agenda, with an open and transparent culture,<br />
and this is reflected throughout the account<br />
with work continuing on the development of the<br />
safety dashboard and further implementation of<br />
the paediatric version of the safety thermometer<br />
(Safety SCAN). A review of the incident<br />
investigation management system to allow earlier<br />
implementation of learning and evidence of<br />
changes that have been made as a result of this<br />
learning reinforces the priority the Trust is placing<br />
on implementing further quality improvements<br />
during 2013/14.<br />
BCH continue to develop innovative ways to<br />
capture the experience of patients and their families<br />
136 137<br />
Through this Quality Account and ongoing quality<br />
assurance process, BCH clearly demonstrate their<br />
commitment to improving the quality of care and<br />
services delivered for children, young people and<br />
families.<br />
We look forward to continuing to work with and<br />
support the Trust in delivering this year’s quality<br />
targets within the Quality Account.<br />
Dr Raj Ramachandram<br />
Chair – <strong>Birmingham</strong> South Central Clinical<br />
Commissioning Group Quality and Safety<br />
Committee
<strong>Birmingham</strong> Health Overview and Scrutiny<br />
Committee<br />
<strong>Birmingham</strong> Health Overview and Scrutiny<br />
Committee have declined on this occasion to<br />
provide comments on our draft Quality Account<br />
2012/13.<br />
Healthwatch <strong>Birmingham</strong><br />
We sent our draft Quality Account 2012/13 to<br />
Healthwatch <strong>Birmingham</strong> for information. As a<br />
newly established organisation they were not able<br />
to provide comments this year.<br />
Council of Governors<br />
The Council of Governors welcomes the<br />
opportunity to comment on <strong>Birmingham</strong> Children’s<br />
<strong>Hospital</strong> NHS Foundation Trust’s Quality Account<br />
2012/13.<br />
The Quality Account is an excellent demonstration<br />
of the commitment of the Board of Directors to<br />
continual quality improvement.<br />
The content of the Quality Account reflects well the<br />
matters presented to the Council of Governors by<br />
the Board of Directors and the experience of the<br />
Governors in attending Quality Walkabouts to the<br />
Trust’s wards and departments.<br />
The Account provides a well balanced overview of<br />
safety, patient experience and clinical effectiveness<br />
and brings the patient experience to life through<br />
direct examples of patient and family feedback,<br />
including feedback about areas where the Trust<br />
needs to improve. We would welcome more of the<br />
patient voice in next year’s Account.<br />
We are impressed by the achievements described<br />
within the report and the Trust’s clear ambition to go<br />
beyond these achievements in the delivery of high<br />
quality care and excellent patient experience. This<br />
is demonstrated by the Trust’s innovations, such<br />
as the DG suit which replaces backless hospital<br />
gowns, the MAPLE food ordering system and the<br />
patient feedback app.<br />
The report is open and transparent, making it<br />
clear when the Trust has not met its objectives,<br />
explaining why this is the case and, most<br />
importantly, what is being done to improve the<br />
situation.<br />
successful conclusion. We also acknowledge<br />
and welcome the external scrutiny by the CQC<br />
in helping the Trust identify areas that can be<br />
improved.<br />
We endorse the approach of the Board to listening<br />
and responding to the concerns and views of<br />
patients, families and staff, which is apparent within<br />
the Account. A good example of this approach<br />
is the process adopted to respond to the recent<br />
Francis report, which is centred on listening events<br />
with staff. These listening events are part of a<br />
wider appraisal of the culture of the organisation<br />
as a whole. This appraisal reflects the Trust’s<br />
commitment to promoting a listening culture and<br />
the well-being of patients and staff.<br />
While we won’t compromise on quality of care or<br />
patient experience, we recognise that not all our<br />
future aspirations for the hospital and the patients<br />
and families it serves can be met within the current<br />
site constraints and governors will be working with<br />
the Board on plans for the future development of<br />
the organisation.<br />
We support the Trust in its approach to being a<br />
listening and learning organisation and encourage<br />
all patients, families and staff to use the range of<br />
methods available to provide their views, in the<br />
knowledge that they will be listened to and acted<br />
upon.<br />
Governors’ Scrutiny Committee on behalf of the<br />
Council of Governors of <strong>Birmingham</strong> Children’s<br />
<strong>Hospital</strong> NHS Foundation Trust<br />
16 May 2013<br />
BACK TO CONTENTS PAGE<br />
Statement of Directors’ responsibilities<br />
in respect of the Quality Report<br />
The Directors are required under the Health Act<br />
2009 and the National Health Service (Quality<br />
Accounts) Regulations 2010 as amended to<br />
prepare Quality Accounts for each financial year.<br />
Monitor has issued guidance to NHS foundation<br />
trust boards on the form and content of annual<br />
quality reports (which incorporate the above legal<br />
requirements) and on the arrangements that<br />
foundation trust boards should put in place to<br />
support the data quality for the preparation of the<br />
quality report.<br />
In preparing the Quality Report, directors are<br />
required to take steps to satisfy themselves that:<br />
l The content of the Quality Report meets the<br />
requirements set out in the NHS Foundation<br />
Trust Annual Reporting Manual 2012-13.<br />
l The content of the Quality Report is not<br />
inconsistent with internal and external sources of<br />
information including:<br />
Board minutes and papers for the period April<br />
2012 to June 2013.<br />
Papers relating to quality reported to the<br />
Board over the period April 2012 to June<br />
2013.<br />
Feedback from the commissioners dated<br />
14 May 2013.<br />
Feedback from governors dated<br />
16 May 2013.<br />
The Trust’s complaints report published<br />
under regulation 18 of the Local Authority<br />
Social Services and NHS Complaints<br />
Regulations 2009, dated 29 April 2013.<br />
The national staff survey 2012.<br />
The Head of Internal Audit’s annual opinion<br />
over the trust’s control environment dated.<br />
CQC quality and risk profile dated February<br />
2013.<br />
l The Quality Report presents a balanced picture<br />
of the NHS Foundation Trust’s performance over<br />
the period covered.<br />
l The performance information reported in the<br />
Quality Report is reliable and accurate.<br />
l There are proper internal controls over the<br />
collection and reporting of the measures of<br />
performance included in the Quality Report,<br />
and these controls are subject to review to<br />
confirm that they are working effectively in<br />
practice.<br />
l The data underpinning the measures of<br />
performance reported in the Quality Report is<br />
robust and reliable, conforms to specified data<br />
quality standards and prescribed definitions,<br />
is subject to appropriate scrutiny and review;<br />
and the Quality Report has been prepared<br />
in accordance with Monitor’s annual reporting<br />
guidance (which incorporates the Quality<br />
Accounts regulations) (published at www.<br />
monitor-nhsft.gov.uk/annualreportingmanual) as<br />
well as the standards to support data quality for<br />
the preparation of the Quality Report<br />
(available at www.monitor-nhsft.gov.uk/<br />
annualreportingmanual)).<br />
The Directors confirm to the best of their knowledge<br />
and belief they have complied with the above<br />
requirements in preparing the Quality Report.<br />
By order of the Board<br />
29 May 2013 .............................................................<br />
Interim Chairman<br />
29 May 2013 ............................................................<br />
This open culture reflects the experience of<br />
Governors at Council meetings where members of<br />
the Board welcome questions, respond positively<br />
to challenge and rapidly address issues to a<br />
138 139<br />
Interim Chief Executive
How we have engaged people in<br />
setting priorities for improving quality<br />
BACK TO CONTENTS PAGE<br />
Foundation Trust Governors<br />
l At quarterly meetings governors are provided<br />
with our Quality Report, Resources Report and<br />
information on Trust developments.<br />
l Governors take part in scheduled Quality<br />
Walkabouts.<br />
l At meetings of the Council of Governors,<br />
governors take part in Quality Walkabouts and<br />
visit new developments to better understand the<br />
Trust’s services and the issues that are<br />
important to patients, families and staff.<br />
l Twice a year we hold a joint meeting between<br />
the Council of Governors and the Board of<br />
Directors to consider the future strategy of the<br />
Trust and developments within the Trust and the<br />
NHS which are relevant to the Trust’s strategy.<br />
l Governors are engaged in our governance<br />
structure, with governors as members of<br />
committees and groups.<br />
l A Public Governor chairs our Organ Donation<br />
Committee.<br />
l A new Committee of the Council of Governors,<br />
the Governors Scrutiny Committee, has been<br />
established, which provides a forum for more<br />
detailed debate and challenge on quality and<br />
resources issues and strategic developments.<br />
l The Governors selected one of the quality<br />
indicators for review by the External Auditor.<br />
Our Staff<br />
l Our Board and Governor Quality Walkabouts<br />
involve engagement with staff as well as patients<br />
and families.<br />
l Surveys, including the national annual Staff<br />
Survey and our own Staff Safety Survey.<br />
l Regular staff polls.<br />
l Staff attendance at public Board meetings.<br />
l Chief Executive Briefings<br />
l Francis Report consultation and listening events.<br />
Our patients and families<br />
l Quality Walkabouts.<br />
l Food walkabouts.<br />
l Direct patient feedback through feedback cards,<br />
feedback app and other means.<br />
l Patient stories which accompany reports to<br />
the Board to help bring issues to life.<br />
l Focus groups on particular issues.<br />
l Mystery Shoppers.<br />
l Taking account of concerns raised through<br />
formal complaints and the PAL Service<br />
l Surveys Consultation on potential new<br />
developments<br />
Young Person’s Advisory Group (YPAG)<br />
l Consultations on Outpatients redesign.<br />
l Consultation on Theatres redesign.<br />
l Consultation on Safer Handover at Night project.<br />
l Regular Quality Walkabouts.<br />
l Reviewing adolescent spaces on wards.<br />
l Parent representatives on the Learning<br />
Disabilities Steering Group<br />
l Feedback from CAMHS parents and young<br />
people by way of an exit interview (Chi Esq)<br />
Healthwatch Steering Group and<br />
Development Group<br />
Our Lead for Patient Experience & Participation<br />
is a member of these groups which will oversee<br />
the consultation process for the development of<br />
Healthwatch England, which will be established<br />
from the existing Local Involvement Networks in<br />
April 2013.<br />
How to provide feedback on the<br />
Quality Report<br />
Despite the improvements in the quality of services<br />
we have seen over the last year, we know we’re<br />
always learning about how things can be done<br />
even better.<br />
At the heart of everything we do are our patients,<br />
their families and the communities that we serve.<br />
That’s why we’re always interested in hearing from<br />
you – whether you have a suggestion on how we<br />
can provide care more innovatively, or whether you<br />
had an experience you think we could improve on.<br />
140 141<br />
We actively encourage people to get in touch and<br />
stay in touch with us, so if you have any ideas<br />
about how we could make this Quality Account<br />
even better we’d like to hear from you.<br />
To tell us about what you think, please contact our<br />
Communications Department on 0121 333 8535<br />
or communications@bch.nhs.uk
142 143<br />
BACK TO CONTENTS PAGE<br />
Statement of the Chief Executive’s<br />
responsibilities as the Accounting<br />
Officer of <strong>Birmingham</strong> Children’s<br />
<strong>Hospital</strong> NHS Foundation Trust<br />
The NHS Act 2006 states that the Chief Executive<br />
is the Accounting Officer of the NHS Foundation<br />
Trust. The relevant responsibilities of the<br />
Accounting Officer, including their responsibility for<br />
the propriety and regularity of public finances for<br />
which they are answerable, and for the keeping of<br />
proper accounts, are set out in the NHS Foundation<br />
Trust Accounting Officer Memorandum issued by<br />
the Independent Regulator of NHS Foundation<br />
Trusts (Monitor).<br />
Under the NHS Act 2006, Monitor has directed<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust to prepare for each financial year a statement<br />
of accounts in the form and on the basis set out in<br />
the Accounts Direction. The accounts are prepared<br />
on an accruals basis and must give a true and fair<br />
view of the state of affairs of <strong>Birmingham</strong> Children’s<br />
<strong>Hospital</strong> NHS Foundation Trust and of its income<br />
and expenditure, total recognised gains and losses<br />
and cash flows for the financial year.<br />
In preparing the accounts, the Accounting Officer<br />
is required to comply with the requirements of the<br />
NHS Foundation Trust Annual Reporting Manual<br />
and in particular to:<br />
l Observe the Accounts Direction issued by<br />
Monitor, including the relevant accounting<br />
and disclosure requirements, and apply suitable<br />
accounting policies on a consistent basis;<br />
The Accounting Officer is responsible for keeping<br />
proper accounting records which disclose with<br />
reasonable accuracy at any time the financial<br />
position of the NHS Foundation Trust and to enable<br />
him/her to ensure that the accounts comply with<br />
requirements outlined in the above mentioned<br />
Act. The Accounting Officer is also responsible for<br />
safeguarding the assets of the NHS Foundation<br />
Trust and hence for taking reasonable steps for<br />
the prevention and detection of fraud and other<br />
irregularities.<br />
To the best of my knowledge and belief, I have<br />
properly discharged the responsibilities set out in<br />
Monitor’s NHS Foundation Trust Accounting Officer<br />
Memorandum.<br />
Signed…………………………………………..<br />
Date: 29 May 2013<br />
David Melbourne<br />
Interim Chief Executive<br />
l Make judgements and estimates on a<br />
reasonable basis;<br />
l State whether applicable accounting standards<br />
as set out in the NHS Foundation Trust Annual<br />
Reporting Manual have been followed, and<br />
disclose and explain any material departures in<br />
the financial statements; and<br />
l Prepare the financial statements on a going<br />
concern basis.
SECTION FOUR<br />
BACK TO CONTENTS PAGE<br />
Annual Governance Statement<br />
Scope of responsibility<br />
As Accounting Officer, I have responsibility for<br />
maintaining a sound system of internal control that<br />
supports the achievement of the NHS Foundation<br />
Trust’s policies, aims and objectives, whilst<br />
safeguarding the public funds and departmental<br />
assets for which I am personally responsible, in<br />
accordance with the responsibilities assigned to<br />
me. I am also responsible for ensuring that the<br />
NHS Foundation Trust is administered prudently<br />
and economically and that resources are applied<br />
efficiently and effectively. I also acknowledge my<br />
responsibilities as set out in the NHS Foundation<br />
Trust Accounting Officer Memorandum.<br />
The purpose of the system of<br />
internal control<br />
The system of internal control is designed to<br />
manage risk to a reasonable level rather than<br />
to eliminate all risk of failure to achieve policies,<br />
aims and objectives; it can therefore only provide<br />
reasonable and not absolute assurance of<br />
effectiveness. The system of internal control is<br />
based on an ongoing process designed to identify<br />
and prioritise the risks to the achievement of<br />
the policies, aims and objectives of <strong>Birmingham</strong><br />
Children’s <strong>Hospital</strong> NHS Foundation Trust, to<br />
evaluate the likelihood of those risks being<br />
realised and the impact should they be realised,<br />
and to manage them efficiently, effectively and<br />
economically. The system of internal control has<br />
been in place in <strong>Birmingham</strong> Children’s <strong>Hospital</strong><br />
NHS Foundation Trust for the year ended 31 March<br />
2013 and up to the date of approval of the annual<br />
report and accounts.<br />
Capacity to handle risk<br />
Leadership<br />
The Board of Directors is responsible for the<br />
management of key risks. Key risks are described<br />
within the Board Assurance Framework which is<br />
considered every month by the Board of Directors.<br />
In addition, risks are clearly defined within the<br />
reports presented to the Board by the Executive<br />
Directors. This process is supplemented on a<br />
quarterly basis when the self assessment of the<br />
financial, activity and service risks is made for<br />
submission to the independent regulator, Monitor.<br />
The Trust’s Risk Management policies clearly set<br />
out responsibilities for risk management within<br />
the organisation. As Chief Executive Officer I<br />
have overall responsibility and accountability<br />
for risk management. This is shared with the<br />
Executive Directors who are responsible for<br />
ensuring that the risk management framework is<br />
systematically implemented and developed across<br />
the organisation. In addition they, through the Board<br />
of Directors’ committee structure, are responsible<br />
for providing assurance to the Board of Directors<br />
that risk management continues to be an essential<br />
element of all management systems and corporate<br />
planning, as well as the setting of strategy and<br />
objectives. The committees for 2012/13 included<br />
the Quality Committee and the Finance and<br />
Resources Committee, which are both chaired by<br />
Independent Non-Executive Directors, with nonexecutive<br />
and executive director membership.<br />
The sub-committees which monitor risks to safety,<br />
quality and workforce objectives include the Clinical<br />
Risk and Quality Assurance Committee, the Non-<br />
Clinical Risk Coordinating Committee, the Patient<br />
Experience and Participation Committee and the<br />
Strategic Workforce Committee.<br />
Staff training and guidance<br />
A range of risk management and information<br />
governance training is provided to staff and there<br />
are policies in place to describe their role and<br />
responsibilities in relation to the identification<br />
and management of risk. This includes an online<br />
training resource for refresher training. This<br />
ensures that risks are actively managed at all levels<br />
of the organisation. The importance of feedback to<br />
staff on incidents reported is stressed at all levels of<br />
training.<br />
changes have been made to mandatory training<br />
related to medicines management, observation and<br />
monitoring, and resuscitation.<br />
Bespoke risk management training has also been<br />
developed for Board members and directors to<br />
enable them to fully understand their role and<br />
responsibilities in relation to risk management.<br />
The risk and control framework<br />
The Trust’s risk management policies ensure that<br />
risk management is embedded in the activities of the<br />
organisation in a number of ways:<br />
l Both Corporate and Directorate objectives are<br />
risk assessed and inform the Board<br />
Assurance Framework, which is reviewed<br />
regularly by the Board of Directors and the<br />
Audit Committee.<br />
l The Trust has achieved level 3 compliance with<br />
the NHS Litigation Authority (Clinical Negligence<br />
Scheme for Trusts) Risk Management<br />
Standards. This demonstrates not only that there<br />
are clearly defined and embedded policies in<br />
place to address risk but also that those policies<br />
are monitored on an ongoing basis and that<br />
action is taken when those policies are not<br />
effective.<br />
To ensure the quality of local management of<br />
incidents, we deliver training (level 2) for all local<br />
managers. This is an interactive session which<br />
covers day-to-day management of risks at a<br />
local level, investigation tips and techniques for<br />
managing incidents and complaints and guidance<br />
on how to carry out robust risk assessment and<br />
how to use the risk register appropriately.<br />
Level 3 ‘Risk Leaders’ training has been designed<br />
for members of staff that need a high level of<br />
expertise in risk management. The session is<br />
focused on Root Cause Analysis techniques<br />
and processes, includes some advanced risk<br />
management techniques and introduces the role<br />
and development of assurance frameworks.<br />
Training implications are considered as part of<br />
all Root Cause Analysis investigations. As a<br />
direct result of learning from these investigations,<br />
144 145<br />
l Risks to information are managed<br />
through the use of the NHS Information<br />
Governance Toolkit. The Trust’s policy provides<br />
a documented mechanism for the immediate<br />
reporting and investigation of actual or<br />
suspected information security breaches/ losses<br />
and potential ulnerabilities/weaknesses within<br />
the Trust.<br />
The Information Governance Toolkit<br />
submissions and the annual plan to improve<br />
compliance with the relevant standards is<br />
approved and regularly reviewed by the<br />
Regulatory Compliance Committee, which<br />
reports to the Board via the Quality Committee.<br />
Following a self-assessment and submission the<br />
overall score against the Information<br />
Governance Toolkit for 2012/13 was 82% and<br />
graded Green (‘Satisfactory’).
l There are structured processes in place for<br />
incident reporting and the investigation of<br />
Serious Incidents Requiring Investigation<br />
(SIRIs), complaints and litigation cases. Regular<br />
audits are undertaken of these processes to<br />
ensure they are appropriately followed and are<br />
effective. The outcomes of these audits are<br />
reported to the Clinical Risk and Quality<br />
Assurance Committee.<br />
l Incident reporting is openly encouraged across<br />
the Trust through training, the use of online<br />
incident reporting, and the communication of<br />
positive outcomes as a result of reporting of<br />
incidents, errors and near misses. Ward<br />
inspections to check compliance with CQC<br />
standards provide assurance that staff know how<br />
to repor incidents.<br />
l A non-executive director is invited to participate<br />
in the Root Cause Analysis of every SIRI. This<br />
helps ensure a good Board level understanding<br />
of risk management processes in the<br />
organisation.<br />
l All papers presented to the Board of Directors<br />
and Board committees contain an assessment of<br />
key regulatory or statutory impacts, including<br />
equality, diversity and human rights and<br />
compliance with standards including NHS<br />
Litigation Authority risk management standards<br />
and CQC essential standards of quality and<br />
safety.<br />
l The Trust attends and submits a performance,<br />
compliance and risk report to the Trust’s<br />
Commissioner’s monthly Clinical Quality Review<br />
Group.<br />
l A representative of the Trust’s Commissioners is<br />
invited to attend the Trust’s monthly Clinical Risk<br />
and Quality Assurance Committee and is invited<br />
to participate in the Root Cause Analysis of<br />
SIRIs.<br />
l All quality initiatives and Cost Improvement<br />
Plans require a quality impact assessment,<br />
which is scrutinised by the Chief Medical Officer<br />
or Chief Nursing Officer before approval.<br />
l Risk appetite is determined in relation to specific<br />
matters reviewed by the Board through detailed<br />
consideration of risk and benefit analysis.<br />
Key Quality Governance Arrangements<br />
The Trust has continued to refine its approach to<br />
the analysis of incidents, potential incidents and<br />
near misses, in order to identify and communicate<br />
learning points and necessary actions. This<br />
commitment to developing an environment of<br />
honesty and openness, where mistakes and<br />
untoward incidents are identified quickly and dealt<br />
with in a positive and responsive way, has been<br />
successful in engaging clinical staff. This approach<br />
to learning is also informed by various sources<br />
of information including surveys, patient and staff<br />
feedback, service reviews, and clinical audits.<br />
A regular Safety Dashboard is produced for<br />
each Clinical Directorate, which incorporates an<br />
overview of data such as incident reports, SIRIs,<br />
complaints and Nursing Care Quality Indicators<br />
(NCQI) performance per ward/department to<br />
highlight potential issues or concerns about<br />
safety or quality of services. The dashboard<br />
allows an aggregated review and comparison of<br />
these metrics against each individual ward and<br />
department and incorporates a series of defined<br />
‘triggers’ which, in combination, may indicate<br />
problems with safety or quality in a specific area.<br />
This allows the Directorate Management Teams<br />
and Board committee responsible for safety to<br />
focus attention where it may be required and acts<br />
as an early warning system. From 2012, the Safety<br />
Dashboard has also identified the departments<br />
implementing a Cost Improvement Plan (CIP) so<br />
an assessment can be made as to whether the<br />
project is affecting quality and safety. Workforce<br />
information is also included, as indications of low<br />
staff engagement can act as an early warning<br />
about a possible impact on our services.<br />
In 2011/12 a Patient Safety Strategy was<br />
developed which maps out the Trust’s journey<br />
towards safer care. The Strategy is updated each<br />
year and sets out a series of clearly defined,<br />
measureable safety targets to achieving the Trust’s<br />
aim to eliminate any less than perfect care. These<br />
targets are produced through a process of risk<br />
analysis, identifying areas for improvement through<br />
data sources such as SIRIs, incident reporting,<br />
complaints, litigation and patient experience<br />
feedback, as well as national guidance and best<br />
practice benchmarking. We believe that focussing<br />
our efforts on a targeted list of specific projects will<br />
have a significant impact on the amount of harm<br />
which is suffered by our patients.<br />
The Trust’s Values – which were agreed in<br />
consultation with staff – have been embedded<br />
during 2012/13 in our recruitment, induction<br />
and appraisal processes. This ensures that all<br />
new staff demonstrate our Values and that the<br />
behaviours of all staff and the decisions that we<br />
make are rooted in our values. Commitment to<br />
these values – respect, trust, compassion, courage<br />
and commitment - also encourages openness<br />
and transparency, which supports robust quality<br />
governance arrangements centred on learning.<br />
The Trust commissioned an external review of<br />
its governance structures in 2011/12 to ensure<br />
they are fit for purpose and provide the Board<br />
of Directors with sufficient, high quality, timely<br />
information. As a result of this review, the<br />
governance structure was redesigned to include 2<br />
new Board Committees:<br />
l Quality Committee, the aim of which is to<br />
provide strategic direction and overview of all<br />
issues related to the quality of care and service<br />
provision, allowing integrated quality reporting to<br />
the Board of Directors.<br />
l Finance and Resources Committee, to review all<br />
matters relating to resources, including finance,<br />
investment, workforce and information<br />
technology, and to provide strategic direction on<br />
negotiating the risk environment.<br />
This new structure was implemented in 2012/13<br />
and its effectiveness was assessed at the end of<br />
the year.<br />
The Quality Report provides an overview of<br />
the main indicators of quality across the Trust,<br />
including high risks, incidents, mortality, patient<br />
experience, safeguarding and infection control, as<br />
well as progress against our Safety Strategy and<br />
quality projects such as the Safety Thermometer<br />
and our programme of Quality Walkabouts.<br />
The report is considered every month by the<br />
Board alongside our Resources Report, which,<br />
in addition to giving details of the Trust’s financial<br />
performance, examines the Trust’s activity<br />
levels, including the way people are accessing<br />
our services; and workforce indicators, such as<br />
sickness levels, turnover, and mandatory training<br />
and appraisal targets, to allow an assessment<br />
of the impact of activity levels on our staff. The 2<br />
reports together provide a broad perspective of<br />
all the factors that make up the Trust’s system of<br />
internal control.<br />
In February 2013 our Internal Auditor completed<br />
a review of the Trust’s Quality Governance<br />
arrangements that ensure compliance with<br />
Monitor’s Quality Governance Framework. This<br />
review found that the Trust meets Monitor’s criteria,<br />
146 147<br />
BACK TO CONTENTS PAGE<br />
and provides ‘significant assurance’ that the Trust’s<br />
arrangements are sound. A small number of areas<br />
were identified which could be improved, and<br />
we are implementing the recommendations of the<br />
Internal Auditor so we can ensure that our quality<br />
governance arrangements are the best they can be.<br />
In 2012 both the Trust’s locations, at Parkview and<br />
at Steelhouse Lane, received an unannounced<br />
inspection from CQC. The review of the CAMH<br />
Services at Parkview found full compliance with the<br />
standards reviewed.<br />
The review at Steelhouse Lane found a minor noncompliance<br />
with standard 14: Supporting workers.<br />
This finding related to a concern raised by some<br />
Theatre staff about the way they were supported,<br />
particularly in relation to the implementation of a<br />
new way of working in Theatres.<br />
In response we have changed the way we are<br />
implementing the new process, and have engaged<br />
closely with the Theatre staff to fully understand<br />
their concerns and address them. In addition, we<br />
have developed new ways of reporting potential<br />
workforce issues to the Board and its committees<br />
to identify as early as possible when our staff<br />
may be feeling unhappy, unsupported, or under<br />
pressure. We have also added further workforce<br />
metrics to the Safety Dashboard to help us better<br />
identify when a ward or department may be coming<br />
under pressure, and where that could have an<br />
impact on the quality of care.<br />
The Trust is fully compliant with the registration<br />
requirements of the Care Quality Commission.<br />
As an employer with staff entitled to membership of<br />
the NHS Pension Scheme, control measures are in<br />
place to ensure all employer obligations contained<br />
within the Scheme regulations are complied with.<br />
This includes ensuring that deductions from salary,<br />
employer’s contributions and payments into the<br />
Scheme are in accordance with the Scheme<br />
rules, and that member Pension Scheme records<br />
are accurately updated in accordance with the<br />
timescales detailed in the Regulations.<br />
Control measures are in place to ensure that all<br />
the Trusts obligations under equality, diversity and<br />
human rights legislation are complied with.<br />
The Trust has undertaken risk assessments and<br />
Carbon Reduction Delivery Plans are in place<br />
in accordance with emergency preparedness<br />
and civil contingency requirements, as based<br />
on UKCIP 2009 weather projects, to ensure<br />
that this organisation’s obligations under the<br />
Climate Change Act and the Adaptation Reporting<br />
requirements are complied with.
148 149<br />
BACK TO CONTENTS PAGE<br />
Major Risks<br />
Table 33: Major Organisational Risks<br />
Risk<br />
Failure to ensure the staff<br />
culture is aligned to the Trust’s<br />
strategic objectives could impact<br />
on achievement of the Trust’s<br />
strategic objectives and on the<br />
delivery of high quality care and<br />
patient experience.<br />
Planned reductions in funding<br />
could impact on the delivery<br />
of the Trust’s services, affect<br />
the quality of care and patient<br />
experience and impact on<br />
achievement of the Trust’s<br />
strategic objectives.<br />
Under developed workforce<br />
plans could impact on the<br />
delivery of the Trust’s services,<br />
affect the quality of care and<br />
patient experience and impact<br />
on achievement of the Trust’s<br />
strategic objectives.<br />
Failure to deliver our Cost<br />
Improvement Plans could<br />
impact on the delivery of the<br />
Trust’s services, affect the<br />
quality of care and patient<br />
experience and impact on<br />
achievement of the Trust’s<br />
strategic objectives.<br />
A delay in delivery of the<br />
strategic outline case for the<br />
new hospital project could<br />
impact on achievement of the<br />
Trust’s strategic objectives.<br />
Management & Mitigation<br />
l Seek feedback from staff through a range of means and embed<br />
the output and associated actions into Trust reporting systems<br />
l Embed results from local surveys and staff polls into performance<br />
indicators and leadership appraisals with a goal of 10%<br />
improvement each year<br />
l Develop a cultural barometer for use across all parts of the<br />
organisation<br />
l Improve the regularity and quality of staff briefing<br />
l Work with the <strong>Birmingham</strong> Director of Public Health to develop a<br />
health impact assessment of proposed funding changes<br />
l Engage with staff, patients and families on the potential solutions<br />
to reduction in resources<br />
l Identify and develop alternative service scenarios that will better<br />
use public resources across the whole of the children’s mental<br />
health budget<br />
l Deliver improved workforce productivity through more efficient<br />
use of the temporary workforce and re-profiling of the total<br />
workforce<br />
l Shift from junior medics to advanced practitioners<br />
l Shift in WTE from nurses to support workers<br />
l Review the medical administration function<br />
l Improve experience and quality of clinical education placements<br />
for all clinical staff<br />
l Improvement in students and juniors recommending BCH as a<br />
place to train by 10%<br />
l Set a financial plan for 2013/14 that requires an achievable<br />
CIP target<br />
l Review legacy CIPs carried forward from 2012/13<br />
l Strengthen PMO function and its monitoring mechanisms<br />
l Revise focus on CIP at performance reviews<br />
l Enhance the CIP Governance framework especially with regards<br />
to Quality Impact Assessments<br />
l Regular formal engagement with key stakeholders<br />
l Board level review of progress and barriers to moving the project<br />
forward<br />
l Programme board with key partners re-established<br />
l Project infrastructure of key partners being established<br />
l Development of detailed plan with key milestones<br />
During 2012/13 some internal control issues<br />
emerged relating to the management of junior<br />
doctor rotas. These issues created risks in relation<br />
to the Trust’s ability to demonstrate full compliance<br />
with the Working Time Regulations and the New<br />
Deal arrangements. The issues also created<br />
financial risks. A detailed risk analysis provided<br />
assurance that the risk to patient safety was low.<br />
Management of these risks and the processes<br />
put in place to address the internal control issues<br />
were closely monitored by the Board of Directors<br />
and its committees, including the Audit Committee.<br />
Support and leadership was provided by Executive<br />
and Non-Executive Directors.<br />
A review by the West Midlands Deanery in March<br />
2013 provided assurance on the quality of the new<br />
processes and systems. An independent review<br />
has been commissioned by the Audit Committee to<br />
provide additional assurance that these processes<br />
and systems are embedded and sustainable.<br />
The Board of Directors is satisfied that the actions<br />
taken have addressed the internal control issues.<br />
Review of economy, efficiency and<br />
effectiveness of the use of resources<br />
The Trust has a range of processes embedded<br />
throughout the organisation to ensure that<br />
resources are used economically, efficiently and<br />
effectively.<br />
In reviewing the key risks of the organisation<br />
through the Board Assurance Framework the<br />
Board considers the effectiveness of the internal<br />
controls compared with the risks. On a regular<br />
basis it also reviews progress against the annual<br />
service plans and the financial plan that results<br />
from this. The Board is supported in the process<br />
by a regular, in-depth review by the Finance and<br />
Resources Committee of the Trust’s financial<br />
position, business cases for significant revenue<br />
and capital investments, and the investment of<br />
cash balances.<br />
Table 34: Internal Audit limited assurance opinion<br />
Clinical Coding: Outpatient &<br />
Emergency<br />
The review found weaknesses<br />
in the coding processes,<br />
including validation and audit.<br />
The Audit Committee supports the delivery of<br />
effective, efficient and economic services through:<br />
l Undertaking a range of thematic reviews,<br />
including workforce, financial standing,<br />
arrangements to deliver quality services and the<br />
effectiveness of the assurance process.<br />
l Considering the coverage of external<br />
and internal audit and reviewing progress<br />
on implementing internal and external audit<br />
recommendations.<br />
The Trust uses a comprehensive internal audit<br />
service as part of its assurance process. An annual<br />
internal audit work programme is risk based and<br />
progress and amendments are reported to the<br />
Audit Committee.<br />
A new Internal Auditor was appointed in 2012/13,<br />
which provided the opportunity for a fresh, in depth<br />
review of the Trust’s risk and quality governance<br />
processes. Significant assurance was given in the<br />
following reviews:<br />
1. Board Assurance Framework<br />
2. Risk Management<br />
3. CQC compliance<br />
4. CAS alerts<br />
5. Clinical Audit<br />
6. SIRI process<br />
7. Quality Governance<br />
8. Directorate Governance<br />
The Internal Auditor gave limited assurance as<br />
follows in table 34 below.<br />
Review Control weakness Action<br />
Programme of formal audit<br />
and regular spot checks to<br />
be established. Longer-term<br />
adoption of automated process.
A range of management processes are<br />
embedded within the operational management<br />
of the organisation that provides a framework for<br />
ensuring that value for money is secured from the<br />
resources available. These include:<br />
l Monthly review of management accounts by<br />
budget holders.<br />
l Monthly performance meetings at directorate<br />
level to assess progress against service and<br />
financial plans, and quarterly meetings to pick<br />
up major performance and service issues.<br />
l The use of a patient level costing system<br />
available to decision makers that identifies the<br />
resources used in the provision of care at a<br />
patient, HRG, specialty and directorate level.<br />
l The use of a programme management<br />
approach to the delivery of efficiency saving<br />
targets built upon a clinician’s assessment of<br />
the impact of any such proposal on the<br />
quality of care.<br />
l The use of a range of benchmark information to<br />
assess the economy and efficiency of services<br />
including with other specialist children’s<br />
hospitals.<br />
Annual Quality Report<br />
The directors are required under the Health Act<br />
2009 and the National Health Service (Quality<br />
Accounts) Regulations 2010 (as amended) to<br />
prepare Quality Accounts for each financial year.<br />
Monitor has issued guidance to NHS foundation<br />
trust boards on the form and content of annual<br />
Quality Reports which incorporate the above legal<br />
requirements in the NHS Foundation Trust Annual<br />
Reporting Manual.<br />
Production of the Quality Report is led by the Chief<br />
Medical Officer and by a core group that includes<br />
senior medical and nursing staff with explicit<br />
responsibilities for quality. The quality indicators<br />
contained within the quality report cover the three<br />
elements of quality and arise from: the Trust’s<br />
Strategic Objectives; the Safety Strategy; locally<br />
developed CQUIN schemes (Commissioning for<br />
Quality and Innovation); national schemes; and<br />
engagement with patients, families and staff.<br />
Performance against these indicators is regularly<br />
reported to the Board of Directors.<br />
Data Quality and Security<br />
Each year the External Auditor undertakes a<br />
review of the data quality and accuracy of a<br />
selection of the indicators reported in the Quality<br />
Report. This includes an indicator selected by the<br />
Council of Governors. Since the first Quality Report<br />
the following indicators have been reviewed:<br />
l MRSA<br />
l MSSA<br />
l C.Difficile<br />
l Cancer waits<br />
l 28 day readmissions<br />
l Patient safety incidents resulting in severe harm<br />
l Emergency Department Transfers<br />
l PICU infections<br />
l Cancelled operations<br />
This provides assurance in relation to these<br />
particular indicators and learning about data<br />
quality and accuracy for other data management<br />
purposes.<br />
The Trust recognises the importance of good<br />
data quality to measure the quality of our care<br />
and organisational performance, to identify<br />
where we need to improve and to measure<br />
improvement. The Trust uses data as part of daily<br />
operational management and regular performance<br />
management, with a range of daily, weekly and<br />
monthly performance reports including those<br />
reviewed by the Board of Directors. This led to the<br />
development of additional performance metrics<br />
and identified a need to improve the data quality of<br />
some of our performance metrics. We established<br />
a Data Quality Group to identify and address<br />
data quality issues and meet the Level 3 NHS<br />
Information Governance Data Quality Standards.<br />
A review of Trust data quality is included in the<br />
Internal Auditor’s annual plan.<br />
There have been no serious lapses in data security<br />
in 2012/13.<br />
Review of effectiveness<br />
As Accounting Officer, I have responsibility for<br />
reviewing the effectiveness of the system of<br />
internal control. My review of the effectiveness of<br />
the system of internal control is informed by the<br />
work of the internal auditors, clinical audit and the<br />
executive managers and clinical leads within the<br />
NHS Foundation Trust that have responsibility for<br />
the development and maintenance of the internal<br />
control framework. I have drawn on the content of<br />
the Quality Report attached to this Annual Report<br />
and other performance information available to<br />
me. My review is also informed by comments<br />
made by the external auditors in their management<br />
letter and other reports. I have been advised on<br />
the implications of the result of my review of the<br />
effectiveness of the system of internal control<br />
by the Board, the Audit Committee, the Quality<br />
Committee and the Finance and Resources<br />
Committee, and a plan to address weaknesses<br />
and ensure continuous improvement of the system<br />
is in place.<br />
My review has taken into account the work of the<br />
previous 12 months and is also informed in the<br />
following ways:<br />
l Through the Executive Directors and managers<br />
who have particular responsibilities for the<br />
development and maintenance of the system<br />
of internal control and the Board Assurance<br />
Framework.<br />
l A comprehensive review of all data available<br />
about quality of care across all services which<br />
has been used to inform the Quality Account.<br />
l The Head of Internal Audit provides me with<br />
an opinion on the overall arrangements for<br />
gaining assurance through the Board Assurance<br />
Framework with regard to the principal risks<br />
considered by their work. This is complemented<br />
by a programme of agreed audit activity by<br />
Internal Audit. This programme facilitates a<br />
review of existing controls and recommends<br />
appropriate remedial actions or systems<br />
redesign. Reports from Internal Audit are<br />
presented to the Audit Committee and any<br />
control issues are reported to the Board and<br />
managed by the Executive Directors.<br />
l The results of the work undertaken by<br />
the External Auditors including their opinion<br />
on the annual accounts.<br />
l The assessment of compliance with the CQC<br />
essential standards of quality and safety,<br />
the NHS Litigation Authority risk management<br />
standards, the Information Governance Toolkit<br />
and the results of staff and patient surveys.<br />
150 151<br />
l The published results of the quarterly<br />
performance management process undertaken<br />
by Monitor.<br />
l Annual performance indicators published by<br />
the Department of Health.<br />
l Through the Audit Committee, which receives<br />
the reviews of the Trust’s systems of internal<br />
control, including the governance arrangements,<br />
as part of the audit programme, assisting<br />
the Board with its responsibilities to strengthen<br />
and improve the effectiveness of the assurance<br />
framework.<br />
l Through the Quality Committee which provides<br />
the strategic direction for the development and<br />
implementation of effective quality governance,<br />
ensuring that quality is critically reviewed to<br />
improve outcomes for children, young people<br />
and their families.<br />
l Through the Clinical Risk and Quality<br />
Assurance Committee, (which reports to the<br />
Quality Committee), which provides leadership<br />
on the development and implementation of<br />
effective clinical governance, including clinical<br />
audit, and monitors progress against the Safety<br />
Strategy.<br />
l Through the Finance and Resources<br />
Committee, which provides the strategic<br />
direction for the development of workforce<br />
strategies, and ensures appropriate systems of<br />
control are in place in relation to investments<br />
and the financial position.<br />
The Head of Internal Audit and the Audit<br />
Committee have advised me that substantial<br />
assurance can be given that there is a generally<br />
sound system of internal control on key financial<br />
and management processes, which are designed<br />
to meet the organisation’s objectives, and controls<br />
are generally being applied consistently.<br />
Conclusion<br />
No significant internal control issues have been<br />
identified other than those described within this<br />
statement.<br />
Signed…………………………………………<br />
29 May 2013<br />
David Melbourne<br />
Interim Chief Executive Officer<br />
BACK TO CONTENTS PAGE
152 153<br />
SECTION FIVE<br />
BACK TO CONTENTS PAGE<br />
Summary Financial Statements<br />
The key statements from within the Annual<br />
Accounts are detailed below in the same format<br />
as they are represented in the Annual Accounts.<br />
‘Notes’ cited in each key statement refer to the<br />
Notes to the Accounts, which can be found in the<br />
full set of Accounts.<br />
The summary financial statements do not<br />
contain sufficient information to allow as full an<br />
understanding of the results of the Trust as would<br />
be provided by the full Annual Accounts. A full set of<br />
Annual Accounts are available, free of charge, by<br />
contacting the Chief Finance Officer:<br />
Chief Finance Officer<br />
<strong>Birmingham</strong> Children’s <strong>Hospital</strong> NHS Foundation<br />
Trust<br />
Steelhouse Lane<br />
<strong>Birmingham</strong><br />
B4 6NH<br />
Or by visiting the Trust’s website:<br />
www.bch.nhs.uk<br />
Foreword<br />
These accounts for the year ended 31 March 2013<br />
have been prepared by <strong>Birmingham</strong> Children’s<br />
<strong>Hospital</strong> NHS Foundation Trust in accordance with<br />
paragraphs 24 and 25 of Schedule 7 to the National<br />
Health Service Act 2006 in the form which Monitor<br />
has, with the approval of HM Treasury, directed.<br />
The auditor’s report on the full annual report and<br />
accounts was unqualified.<br />
David Melbourne<br />
Interim Chief Executive Officer<br />
Date: 29 May 2013<br />
Statement of Comprehensive Income for the year ended 31 March 2013<br />
31 March 2013 31 March 2012<br />
Note £000 £000<br />
Operating Income from continuing operations 2 233,709 223,958<br />
Operating surplus from continuing operations 3 (225,082) (210,843)<br />
OPERATING SURPLUS 8,627 13,115<br />
FINANCE COSTS<br />
Finance income 8 668 357<br />
Finance expense - financial liabilities 9 (469) (471)<br />
PDC Dividends payable (2,558) (2,187)<br />
NET FINANCE COSTS (2,359) (2,301)<br />
Surplus from continuing operations 6,268 10,814<br />
SURPLUS FOR THE YEAR 6,268 10,814<br />
Other comprehensive income<br />
Impairments (8,665) -<br />
Revaluations 12,877 40<br />
Other reserve movements (62) (29)<br />
TOTAL COMPREHENSIVE INCOME FOR THE YEAR 10,418 10,825<br />
Prior period adjustments - -<br />
Merger adjustments - -<br />
TOTAL COMPREHENSIVE INCOME FOR THE YEAR 10,418 10,825<br />
All income and expenditure is derived from continuing operations.
BACK TO CONTENTS PAGE<br />
Note: Allocation of Comprehensive Income for the period:<br />
There are no Minority Interests in the Trust, therefore the surplus for the year of £6,268k (2012: £10,814k)<br />
and the Total Comprehensive Income of £10,418k (2012: £10,825k) are wholly attributable to the Trust.<br />
Statement of Financial Position as at 31 March 2013<br />
Statement of Changes In Taxpayers’ Equity<br />
Non-current assets<br />
31 March 2013 31 March 2012<br />
Note £000 £000<br />
Operating surplus from continuing operations 11 178 158<br />
Property, plant and equipment 12 95,040 90,050<br />
Trade and other receivables 22 1,251 1,095<br />
Total non-current assets 96,470 91,303<br />
Current assets<br />
Inventories 21 3,955 3,635<br />
Trade and other receivables 22 12,714 14,957<br />
Cash and cash equivalents 25 36,173 33,730<br />
Total current assets 52,842 52,322<br />
Current liabilities<br />
Trade and other payables 26 (19,564) (25,031)<br />
Borrowings 27 (152) (152)<br />
Provisions 31 (2,562) (223)<br />
Other liabilities 29 (3,841) (8,015)<br />
Total current liabilities (26,119) (33,421)<br />
Total assets less current liabilities 123,193 110,204<br />
Non-current liabilities<br />
Borrowings 27 (1,365) (1,516)<br />
Provisions 31 (2,389) (15)<br />
Other liabilities 29 (1,777) (1,429)<br />
Total non-current liabilities (5,531) (2,960)<br />
Total assets employed 117,662 107,244<br />
Financed by<br />
Public Dividend Capital 86,222 86,222<br />
Revaluation reserve 33 12,771 8,604<br />
Income and expenditure reserve 18,669 12,418<br />
Total taxpayers’ and others’ equity 117,662 107,244<br />
Public<br />
Income and<br />
Dividend Revaluation Expenditure<br />
Total Capital Reserve Reserve<br />
£000 £000 £000 £000<br />
Taxpayers’ Equity at 1 April 2012 107,244 86,222 8,604 12,418<br />
Surplus for the year 6,268 - - 6,268<br />
Impairments (8,665) - (8,665) -<br />
Revaluations - property, plant and equipment 12,877 - 12,877 -<br />
Transfer to retained earnings on disposal of assets - - (45) 45<br />
Other reserve movements (62) - - (62)<br />
Taxpayers’ Equity at 31 March 2013 117,662 86,222 12,771 18,669<br />
Public<br />
Income and<br />
Dividend Revaluation Expenditure<br />
Total Capital Reserve Reserve<br />
£000 £000 £000 £000<br />
Taxpayers’ Equity at 1 April 2011 -<br />
as previously stated 96,419 86,222 8,564 1,633<br />
Surplus for the year 10,814 - - 10,814<br />
Revaluations - property, plant and equipment 40 - 40 -<br />
Other reserve movements (29) - - (29)<br />
Taxpayers’ Equity at 31 March 2012 107,244 86,222 8,604 12,418<br />
The financial statements were approved by the Board of Directors and authorised for issue on their behalf by:<br />
.............................. Date.............................................. Interim Chief Executive<br />
154 155
156<br />
Statement of Cash Flows for the Year Ended 31 March 2013<br />
Cash flows from operating activities<br />
31 March 2013 31 March 2012<br />
Note £000 £000<br />
Operating surplus from continuing operations 8,627 13,115<br />
Operating surplus 8,627 13,115<br />
Non-cash income and expense:<br />
Depreciation and amortisation 3 5,631 5,097<br />
Impairments 3 2,525 -<br />
Loss on disposal 3 30 -<br />
Non-cash donations/grants credited to income 105 -<br />
Dividends accrued and not paid or received - 41<br />
Amortisation of PFI credit 565 -<br />
(Increase)/Decrease in Trade and Other Receivables 2,087 (4,883)<br />
(Increase)/Decrease in Inventories (320) 217<br />
Increase/(Decrease) in Trade and Other Payables (5,467) 3,874<br />
Increase/(Decrease) in Other Liabilities (3,826) 74<br />
Increase in Provisions 4,713 16<br />
Other movements in operating cash flows (390) (208)<br />
NET CASH GENERATED FROM OPERATIONS 14,280 17,343<br />
Cash flows from investing activities<br />
Interest received 668 357<br />
Purchase of intangible assets - (45)<br />
Purchase of Property, Plant and Equipment (9,519) (16,269)<br />
Net cash used in investing activities (8,851) (15,957)<br />
Cash flows from financing activities<br />
Interest element of Private Finance Initiative obligations (469) (319)<br />
PDC Dividend paid (2,517) (2,140)<br />
Net cash used in financing activities (2,986) (2,459)<br />
Increase/(decrease) in cash and cash equivalents 2,443 (1,073)<br />
Cash and Cash equivalents at 1 April 33,730 34,803<br />
Cash and Cash equivalents at 31 March 25.1 36,173 33,730